- See us on facebook
- See us on twitter
- See us on youtube
- See us on linkedin
- See us on instagram

Researchers treat depression by reversing brain signals traveling the wrong way
A new study led by Stanford Medicine researchers is the first to reveal how magnetic stimulation treats severe depression: by correcting the abnormal flow of brain signals.
May 15, 2023 - By Nina Bai
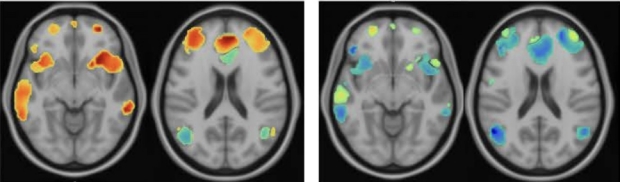
Brain images from a patient with major depression before (left) and after treatment with Stanford neuromodulation therapy, which restores the normal timing of activity in the anterior cingulate cortex. Nolan Williams Lab
Powerful magnetic pulses applied to the scalp to stimulate the brain can bring fast relief to many severely depressed patients for whom standard treatments have failed. Yet it’s been a mystery exactly how transcranial magnetic stimulation, as the treatment is known, changes the brain to dissipate depression. Now, research led by Stanford Medicine scientists has found that the treatment works by reversing the direction of abnormal brain signals.
The findings also suggest that backward streams of neural activity between key areas of the brain could be used as a biomarker to help diagnose depression.
“The leading hypothesis has been that TMS could change the flow of neural activity in the brain,” said Anish Mitra , MD, PhD, a postdoctoral fellow in psychiatry and behavioral sciences. “But to be honest, I was pretty skeptical. I wanted to test it.”
Mitra had just the tool to do it. As a graduate student at Washington University in Saint Louis, in the lab of Mark Raichle, MD, he developed a mathematical tool to analyze functional magnetic resonance imaging, or fMRI — commonly used to locate active areas in the brain. The new analysis used minute differences in timing between the activation of different areas to also reveal the direction of that activity.
In the new study , published May 15 in the Proceedings of the National Academy of Sciences , Mitra and Raichle teamed up with Nolan Williams , MD, associate professor of psychiatry and behavioral sciences, whose team has advanced the use of magnetic stimulation, personalized to each patient’s brain anatomy, to treat profound depression. The FDA-cleared treatment, known as Stanford neuromodulation therapy , incorporates advanced imaging technologies to guide stimulation with high-dose patterns of magnetic pulses that can modify brain activity related to major depression. Compared with traditional TMS, which requires daily sessions over several weeks or months, SNT works on an accelerated timeline of 10 sessions each day for just five days.
“This was the perfect test to see if TMS has the ability to change the way that signals flow through the brain,” said Mitra, who is lead author of the study. “If this doesn’t do it, nothing will.”
Raichle and Williams are senior authors of the study.

Anish Mitra
Timing is everything
The researchers recruited 33 patients who had been diagnosed with treatment-resistant major depressive disorder. Twenty-three received SNT treatment, and 10 received a sham treatment that mimicked SNT but without magnetic stimulation. They compared data from these patients with that of 85 healthy controls without depression.
When they analyzed fMRI data across the whole brain, one connection stood out. In the normal brain, the anterior insula, a region that integrates bodily sensations, sends signals to a region that governs emotions, the anterior cingulate cortex.
“You could think of it as the anterior cingulate cortex receiving this information about the body — like heart rate or temperature — and then deciding how to feel on the basis of all these signals,” Mitra said.
In three-quarters of the participants with depression, however, the typical flow of activity was reversed: The anterior cingulate cortex sent signals to the anterior insula. The more severe the depression, the higher the proportion of signals that traveled the wrong way.
“What we saw is that who’s the sender and who’s the receiver in the relationship seems to really matter in terms of whether someone is depressed,” Mitra said.
“It’s almost as if you’d already decided how you were going to feel, and then everything you were sensing was filtered through that,” he said. “The mood has become primary.”
“That’s consistent with how a lot of psychiatrists see depression,” he added. “Even things that are quite joyful to a patient normally are suddenly not bringing them any pleasure.”
When depressed patients were treated with SNT, the flow of neural activity shifted to the normal direction within a week, coinciding with a lifting of their depression.
Those with the most severe depression — and the most misdirected brain signals — were the most likely to benefit from the treatment.
“We’re able to undo the spatio-temporal abnormality so that people’s brains look like those of normal, healthy controls,” Williams said.

Nolan Williams
A biomarker for depression
A challenge of treating depression has been the lack of insight into its biological mechanisms. If a patient has a fever, there are various tests — for a bacterial or viral infection, for example — that could determine the appropriate treatment. But for a patient with depression, there are no analogous tests.
“This is the first time in psychiatry where this particular change in biology — the flow of signals between these two brain regions — predicts the change in clinical symptoms,” Williams said.
Not everyone with depression has this abnormal flow of neural activity, and it may be rare in less severe cases of depression, Williams said, but it could serve as an important biomarker for triaging treatment for the disorder. “The fMRI data that allows precision treatment with SNT can be used both as a biomarker for depression and a method of personalized targeting to treat its underlying cause,” he said.
“When we get a person with severe depression, we can look for this biomarker to decide how likely they are to respond well to SNT treatment,” Mitra said.
“Behavioral conditions like depression have been difficult to capture with imaging because, unlike an obvious brain lesion, they deal with the subtlety of relationships between various parts of the brain,” said Raichle, who has studied brain imaging for more than four decades. “It’s incredibly promising that the technology now is approaching the complexity of the problems we’re trying to understand."
The researchers plan to replicate the study in a larger group of patients. They also hope others will adopt their analytic technique to uncover more clues about the direction of brain activity hidden in fMRI data. “As long as you have good clean fMRI data, you can study this property of the signals,” Mitra said.
The study was funded by a Brain and Behavior Research Foundation Young Investigator Award, the NIMH Biobehavioral Research Awards for Innovative New Scientists award (grant R01 5R01MH122754-02), Charles R. Schwab, the David and Amanda Chao Fund II, the Amy Roth PhD Fund, the Neuromodulation Research Fund, the Lehman Family, the Still Charitable Trust, the Marshall and Dee Ann Payne Fund, the Gordie Brookstone Fund, the Mellam Family Foundation, and the Baszucki Brain Research Fund.
About Stanford Medicine
Stanford Medicine is an integrated academic health system comprising the Stanford School of Medicine and adult and pediatric health care delivery systems. Together, they harness the full potential of biomedicine through collaborative research, education and clinical care for patients. For more information, please visit med.stanford.edu .
Artificial intelligence
Exploring ways AI is applied to health care

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 18 June 2020
Advances in depression research: second special issue, 2020, with highlights on biological mechanisms, clinical features, co-morbidity, genetics, imaging, and treatment
- Julio Licinio 1 &
- Ma-Li Wong 1
Molecular Psychiatry volume 25 , pages 1356–1360 ( 2020 ) Cite this article
10k Accesses
11 Citations
4 Altmetric
Metrics details
The current speed of progress in depression research is simply remarkable. We have therefore been able to create a second special issue of Molecular Psychiatry , 2020, focused on depression, with highlights on mechanisms, genetics, clinical features, co-morbidity, imaging, and treatment. We are also very proud to present in this issue a seminal paper by Chottekalapanda et al., which represents some of the last work conducted by the late Nobel Laureate Paul Greengard [ 1 ]. This brings to four the number of papers co-authored by Paul Greengard and published in our two 2020 depression special issues [ 1 , 2 , 3 , 4 ].
The research content of this special depression issue starts with Chottekalapanda et al.’s outstanding contribution aimed at determining whether neuroadaptive processes induced by antidepressants are modulated by the regulation of specific gene expression programs [ 1 ]. That team identified a transcriptional program regulated by activator protein-1 (AP-1) complex, formed by c-Fos and c-Jun that is selectively activated prior to the onset of the chronic SSRI response. The AP-1 transcriptional program modulated the expression of key neuronal remodeling genes, including S100a10 (p11), linking neuronal plasticity to the antidepressant response. Moreover, they found that AP-1 function is required for the antidepressant effect in vivo. Furthermore, they demonstrated how neurochemical pathways of BDNF and FGF2, through the MAPK, PI3K, and JNK cascades, regulate AP-1 function to mediate the beneficial effects of the antidepressant response. This newly identified molecular network provides “a new avenue that could be used to accelerate or potentiate antidepressant responses by triggering neuroplasticity.”
A superb paper by Schouten et al. showed that oscillations of glucocorticoid hormones (GC) preserve a population of adult hippocampal neural stem cells in the aging brain [ 5 ]. Moreover, major depressive disorder (MDD) is characterized by alterations in GC-related rhythms [ 6 , 7 ]. GC regulate neural stem/precursor cells (NSPC) proliferation [ 8 , 9 ]. The adrenals secrete GC in ultradian pulses that result in a circadian rhythm. GC oscillations control cell cycle progression and induce specific genome-wide DNA methylation profiles. Schouten et al. studied primary hippocampal NSPC cultures and showed that GC oscillations induced lasting changes in the methylation state of a group of gene promoters associated with cell cycle regulation and the canonical Wnt signaling pathway. Furthermore, in a mouse model of accelerated aging, they showed that disruption of GC oscillations induced lasting changes in dendritic complexity, spine numbers and morphology of newborn granule neurons. Their results indicate that GC oscillations preserve a population of GR-expressing NSPC during aging, preventing their activation possibly by epigenetic programming through methylation of specific gene promoters. These important observations suggest a novel mechanism mediated by GC that controls NSPC proliferation and preserves a dormant NSPC pool, possibly contributing to neuroplasticity reserve in the aging brain.
MDD has a critical interface with addiction and suicide, which is of immense clinical and research importance [ 10 ]. Peciña et al. have reviewed a growing body of research indicating that the endogenous opioid system is directly involved in the regulation of mood and is dysregulated in MDD [ 11 ]. Halikere et al. provide evidence that addiction associated N40D mu-opioid receptor variant modulates synaptic function in human neurons [ 12 ].
Two papers by Amare et al. and Coleman et al. examine different genetic substrates for MDD, identifying novel depression-related loci as well as studying the interface with trauma [ 13 , 14 ].
The dissection of MDD clinical phenotypes, including their interface with other illnesses is a topic of several articles in this special issue. Belvederi Murri et al. examined the symptom network structure of depressive symptoms in late-life in a large European population in the 19 country Survey of Health, Ageing, and Retirement in Europe (SHARE) (mean age 74 years, 59% females, n = 8557) [ 15 ]. They showed that the highest values of centrality were in the symptoms of death wishes, depressed mood, loss of interest, and pessimism. Another article focused on a specific feature of MDD, namely changes in appetite. Simmons et al. aimed at explaining why some individuals lose their appetite when they become depressed, while others eat more, and brought together data on neuroimaging, salivary cortisol, and blood markers of inflammation and metabolism [ 16 ]. Depressed participants experiencing decreased appetite had higher cortisol levels than other subjects, and their cortisol values correlated inversely with the ventral striatal response to food cues. In contrast, depressed participants experiencing increased appetite exhibited marked immunometabolic dysregulation, with higher insulin, insulin resistance, leptin, c-reactive protein (CRP), interleukin 1 receptor antagonist (IL-1RA), and IL-6, and lower ghrelin than subjects in other groups, and the magnitude of their insulin resistance correlated positively with the insula response to food cues. Their findings support the existence of pathophysiologically distinct depression subtypes for which the direction of appetite change may be an easily measured behavioral marker.
Mulugeta et al. studied the association between major depressive disorder and multiple disease outcomes in the UK Biobank ( n = 337,536) [ 17 ]. They performed hypothesis-free phenome-wide association analyses between MDD genetic risk score (GRS) and 925 disease outcomes. MDD was associated with several inflammatory and hemorrhagic gastrointestinal diseases, and intestinal E. coli infections. MDD was also associated with disorders of lipid metabolism and ischemic heart disease. Their results indicated a causal link between MDD and a broad range of diseases, suggesting a notable burden of co-morbidity. The authors concluded that “early detection and management of MDD is important, and treatment strategies should be selected to also minimize the risk of related co-morbidities.” Further information on the shared mechanisms between coronary heart disease and depression in the UK Biobank ( n = 367,703) was explored by Khandaker et al. [ 18 ]. They showed that family history of heart disease was associated with a 20% increase in depression risk; however, a genetic risk score that is strongly associated with CHD risk was not associated with depression. Their data indicate that comorbidity between depression and CHD arises largely from shared environmental factors.
In a systematic review and meta-analysis of cohort studies, Wang et al. examined the interface of depression and anxiety in relation to cancer incidence and mortality [ 19 ]. Their analyses suggest that depression and anxiety may have an etiologic role and prognostic impact on cancer, although there is potential reverse causality.
Several papers in this issue examine imaging in MDD, either to unravel the underlying disease processes or to identify imaging biomarkers of treatment response. Let us first look at the studies focused on elucidating brain circuitry alterations in MDD. Arterial spin labeling (ASL) was used by Cooper et al. to measure cerebral blood flow (CBF; perfusion) in order to discover and replicate alterations in CBF in MDD [ 20 ]. Their analyses revealed reduced relative CBF (rCBF) in the right parahippocampus, thalamus, fusiform, and middle temporal gyri, as well as the left and right insula, for those with MDD. They also revealed increased rCBF in MDD in both the left and the right inferior parietal lobule, including the supramarginal and angular gyri. According to the authors, “these results (1) provide reliable evidence for ASL in detecting differences in perfusion for multiple brain regions thought to be important in MDD, and (2) highlight the potential role of using perfusion as a biosignature of MDD.” Further data on imaging in MDD was provided by a coordinated analysis across 20 international cohorts in the ENIGMA MDD working group. In that paper, van Velzen et al. showed that in a coordinated and harmonized multisite diffusion tensor imaging study there were subtle, but widespread differences in white matter microstructure in adult MDD, which may suggest structural disconnectivity [ 21 ].
Four articles in this special issue examine imaging biomarkers of treatment response. Greenberg et al. studied reward-related ventral striatal activity and differential response to sertraline versus placebo in depressed using functional magnetic resonance imaging while performing a reward task [ 22 ]. They found that ventral striatum (VS) dynamic response to reward expectancy (expected outcome value) and prediction error (difference between expected and actual outcome), likely reflecting serotonergic and dopaminergic deficits, was associated with better response to sertraline than placebo. Their conclusion was that treatment measures of reward-related VS activity may serve as objective neural markers to advance efforts to personalize interventions by guiding individual-level choice of antidepressant treatment. Utilizing whole-brain functional connectivity analysis to identify neural signatures of remission following antidepressant treatment, and to identify connectomic predictors of treatment response, Korgaonkar et al. showed that intrinsic connectomes are a predictive biomarker of remission in major depressive disorder [ 23 ]. Based on their results that team proposed that increased functional connectivity within and between large-scale intrinsic brain networks may characterize acute recovery with antidepressants in depression. Repple et al. created connectome matrices via a combination of T1-weighted magnetic resonance imaging (MRI) and tractography methods based on diffusion-weighted imaging severity of current depression and remission status in 464 MDD patients and 432 healthy controls [ 24 ]. Reduced global fractional anisotropy (FA) was observed specifically in acute depressed patients compared to fully remitted patients and healthy controls. Within the MDD patients, FA in a subnetwork including frontal, temporal, insular, and parietal nodes was negatively associated with symptom intensity, an effect remaining when correcting for lifetime disease severity. Their findings provide new evidence of MDD to be associated with structural, yet dynamic, state-dependent connectome alterations, which covary with current disease severity and remission status after a depressive episode. The effects of electroconvulsive therapy (ECT), the most effective treatment for depression, on the dentate gyrus (DG) were studied by Nuninga et al. through an optimized MRI scan at 7-tesla field strength, allowing sensitive investigation of hippocampal subfields [ 25 , 26 ]. They documented a large and significant increase in DG volume after ECT, while other hippocampal subfields were unaffected. Furthermore, an increase in DG volume was related to a decrease in depression scores, and baseline DG volume predicted clinical response. These findings suggest that the volume change of the DG is related to the antidepressant properties of ECT, possibly reflecting neurogenesis.
Three articles report new directions for antidepressant therapeutics. Papakostas et al. presented the results of a promising phase 2, double-blind, placebo-controlled study of NSI-189 phosphate, a novel neurogenic compound, in MDD patients [ 27 ]. As the endogenous opioid system is thought to play an important role in the regulation of mood, Fava et al. studied the buprenorphine/samidorphan combination as an investigational opioid system modulator for adjunctive treatment of MDD in two phase 3, randomized, double-blind, placebo-controlled studies that utilized the same sequential parallel-comparison design [ 28 ]. One of the studies achieved the primary endpoint, namely change from baseline in Montgomery–Åsberg Depression Rating Scale (MADRS)-10 at week 5 versus placebo) and the other study did not achieve the primary endpoint. However, the pooled analysis of the two studies demonstrated consistently greater reduction in the MADRS-10 scores from baseline versus placebo at multiple timepoints, including end of treatment. These data provide cautious optimism and support further controlled trials for this potential new treatment option for patients with MDD who have an inadequate response to currently available antidepressants. Fava et al. also report the results of a double-blind, placebo-controlled, dose-ranging trial of intravenous (IV) ketamine as adjunctive therapy in treatment-resistant depression, using four doses of ketamine and a control [ 29 , 30 ]. They show that there was evidence for the efficacy of the two higher doses of IV ketamine and no clear or consistent evidence for clinically meaningful efficacy of the two lower doses studied.
Overall, in this issue, immense progress in depression research is provided by outstanding studies that highlight advances in our understanding of MDD biology, clinical features, co-morbidity, genetics, brain imaging (including imaging biomarkers), and treatment. Building on the groundbreaking articles from our previous 2020 special issues on stress and behavior [ 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 ] and on depression [ 2 , 3 , 4 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 ], we are proud that the stunning progress presented here found its home in our pages. From inception in 1996, we have aimed at making Molecular Psychiatry promote the integration of molecular medicine and clinical psychiatry [ 63 ]. It is particularly rewarding to see that goal achieved so spectacularly in this second 2020 special issue on MDD, a disorder of gene-environment interactions that represents a pressing public health challenge, with an ever increasing impact on society [ 64 , 65 , 66 ]. We are privileged to have in these two 2020 depression special issues four remarkable papers from Paul Greengard’s teams that provide substantial new data on the mechanisms of antidepressant action [ 1 , 2 , 3 , 4 ]. Such profound advances in basic science are needed to facilitate and guide future translational efforts needed to advance therapeutics [ 67 , 68 ].
Chottekalapanda R, et al. AP-1 controls the p11-dependent antidepressant response. Mol Psychiatry. 2020. https://doi.org/10.1038/s41380-020-0767-8 .
Sagi Y, et al. Emergence of 5-HT5A signaling in parvalbumin neurons mediates delayed antidepressant action. Mol Psychiatry. 2019. https://doi.org/10.1038/s41380-019-0379-3 .
Oh SJ, et al. Hippocampal mossy cell involvement in behavioral and neurogenic responses to chronic antidepressant treatment. Mol Psychiatry. 2019. https://doi.org/10.1038/s41380-019-0384-6 .
Shuto T, et al. Obligatory roles of dopamine D1 receptors in the dentate gyrus in antidepressant actions of a selective serotonin reuptake inhibitor, fluoxetine. Mol Psychiatry. 2018. https://doi.org/10.1038/s41380-018-0316-x .
Schouten M, et al. Circadian glucocorticoid oscillations preserve a population of adult hippocampal neural stem cells in the aging brain. Mol Psychiatry. 2019. https://doi.org/10.1038/s41380-019-0440-2 .
Kling MA, et al. Effects of electroconvulsive therapy on the CRH-ACTH-cortisol system in melancholic depression: preliminary findings. Psychopharmacol Bull. 1994;30:489–94.
CAS PubMed Google Scholar
Sternberg EM, Licinio J. Overview of neuroimmune stress interactions. Implications for susceptibility to inflammatory disease. Ann NY Acad Sci. 1995;771:364–71.
Article CAS Google Scholar
Bornstein SR, et al. Stress-inducible-stem cells: a new view on endocrine, metabolic and mental disease? Mol Psychiatry. 2019;24:2–9. https://doi.org/10.1038/s41380-018-0244-9 .
Article CAS PubMed Google Scholar
Rubin de Celis MF, et al. The effects of stress on brain and adrenal stem cells. Mol Psychiatry. 2016;21:590–3. https://doi.org/10.1038/mp.2015.230 .
Soares-Cunha C, et al. Nucleus accumbens medium spiny neurons subtypes signal both reward and aversion. Mol Psychiatry. 2019. https://doi.org/10.1038/s41380-019-0484-3 .
Pecina M, et al. Endogenous opioid system dysregulation in depression: implications for new therapeutic approaches. Mol Psychiatry. 2019;24:576–87, https://doi.org/10.1038/s41380-018-0117-2 .
Halikere A, et al. Addiction associated N40D mu-opioid receptor variant modulates synaptic function in human neurons. Mol Psychiatry. 2019. https://doi.org/10.1038/s41380-019-0507-0 .
Amare AT, et al. Bivariate genome-wide association analyses of the broad depression phenotype combined with major depressive disorder, bipolar disorder or schizophrenia reveal eight novel genetic loci for depression. Mol Psychiatry. 2019. https://doi.org/10.1038/s41380-018-0336-6 .
Coleman JRI, et al. Genome-wide gene-environment analyses of major depressive disorder and reported lifetime traumatic experiences in UK Biobank. Mol Psychiatry. 2020 https://doi.org/10.1038/s41380-019-0546-6 .
Belvederi Murri M, Amore M, Respino M, Alexopoulos GS. The symptom network structure of depressive symptoms in late-life: results from a European population study. Mol Psychiatry. 2018. https://doi.org/10.1038/s41380-018-0232-0 .
Article PubMed Google Scholar
Simmons WK, et al. Appetite changes reveal depression subgroups with distinct endocrine, metabolic, and immune states. Mol Psychiatry. 2018. https://doi.org/10.1038/s41380-018-0093-6 .
Article PubMed PubMed Central Google Scholar
Mulugeta A, Zhou A, King C, Hypponen E. Association between major depressive disorder and multiple disease outcomes: a phenome-wide Mendelian randomisation study in the UK Biobank. Mol Psychiatry. 2019. https://doi.org/10.1038/s41380-019-0486-1 .
Khandaker GM, et al. Shared mechanisms between coronary heart disease and depression: findings from a large UK general population-based cohort. Mol Psychiatry. 2019. https://doi.org/10.1038/s41380-019-0395-3 .
Wang YH, et al. Depression and anxiety in relation to cancer incidence and mortality: a systematic review and meta-analysis of cohort studies. Mol Psychiatry. 2019. https://doi.org/10.1038/s41380-019-0595-x .
Cooper CM, et al. Discovery and replication of cerebral blood flow differences in major depressive disorder. Mol Psychiatry. 2019. https://doi.org/10.1038/s41380-019-0464-7 .
van Velzen LS, et al. White matter disturbances in major depressive disorder: a coordinated analysis across 20 international cohorts in the ENIGMA MDD working group. Mol Psychiatry. 2019. https://doi.org/10.1038/s41380-019-0477-2 .
Greenberg T, et al. Reward related ventral striatal activity and differential response to sertraline versus placebo in depressed individuals. Mol Psychiatry. 2019. https://doi.org/10.1038/s41380-019-0490-5 .
Korgaonkar MS, Goldstein-Piekarski AN, Fornito A & Williams, LM Intrinsic connectomes are a predictive biomarker of remission in major depressive disorder. Mol Psychiatry. 2019. https://doi.org/10.1038/s41380-019-0574-2 .
Repple J, et al. Severity of current depression and remission status are associated with structural connectome alterations in major depressive disorder. Mol Psychiatry. 2019. https://doi.org/10.1038/s41380-019-0603-1 .
Nuninga JO, et al. Volume increase in the dentate gyrus after electroconvulsive therapy in depressed patients as measured with 7T. Mol Psychiatry. 2019. https://doi.org/10.1038/s41380-019-0392-6 .
Koch SBJ, Morey RA & Roelofs K. The role of the dentate gyrus in stress-related disorders. Mol Psychiatry. 2019. https://doi.org/10.1038/s41380-019-0572-4 .
Papakostas GI, et al. A phase 2, double-blind, placebo-controlled study of NSI-189 phosphate, a neurogenic compound, among outpatients with major depressive disorder. Mol Psychiatry. 2019. https://doi.org/10.1038/s41380-018-0334-8 .
Fava M, et al . Opioid system modulation with buprenorphine/samidorphan combination for major depressive disorder: two randomized controlled studies. Mol Psychiatry. 2018. https://doi.org/10.1038/s41380-018-0284-1 .
Fava M, et al. Correction: double-blind, placebo-controlled, dose-ranging trial of intravenous ketamine as adjunctive therapy in treatment-resistant depression (TRD). Mol Psychiatry. 2019. https://doi.org/10.1038/s41380-018-0311-2 .
Fava M, et al. Double-blind, placebo-controlled, dose-ranging trial of intravenous ketamine as adjunctive therapy in treatment-resistant depression (TRD). Mol Psychiatry. 2018. https://doi.org/10.1038/s41380-018-0256-5 (2018).
Licinio J. Advances in research on stress and behavior: special issue, 2020. Mol Psychiatry 2020;25:916–7. https://doi.org/10.1038/s41380-020-0741-5 .
Martinez ME, et al. Thyroid hormone overexposure decreases DNA methylation in germ cells of newborn male mice. Mol Psychiatry. 2020;25:915 https://doi.org/10.1038/s41380-020-0732-6 .
Martinez ME, et al. Thyroid hormone influences brain gene expression programs and behaviors in later generations by altering germ line epigenetic information. Mol Psychiatry. 2020;25:939–50. https://doi.org/10.1038/s41380-018-0281-4 .
Le-Niculescu H, et al. Towards precision medicine for stress disorders: diagnostic biomarkers and targeted drugs. Mol Psychiatry. 2020;25:918–38. https://doi.org/10.1038/s41380-019-0370-z .
Torres-Berrio A, et al. MiR-218: a molecular switch and potential biomarker of susceptibility to stress. Mol Psychiatry. 2020;25:951–64. https://doi.org/10.1038/s41380-019-0421-5
Sillivan SE, et al. Correction: MicroRNA regulation of persistent stress-enhanced memory. Mol Psychiatry. 2020;25:1154 https://doi.org/10.1038/s41380-019-0452-y .
Sillivan SE, et al. MicroRNA regulation of persistent stress-enhanced memory. Mol Psychiatry. 2020;25:965–76. https://doi.org/10.1038/s41380-019-0432-2 .
Shi MM, et al. Hippocampal micro-opioid receptors on GABAergic neurons mediate stress-induced impairment of memory retrieval. Mol Psychiatry. 2020;25:977–92. https://doi.org/10.1038/s41380-019-0435-z .
Mayo LM, et al. Protective effects of elevated anandamide on stress and fear-related behaviors: translational evidence from humans and mice. Mol Psychiatry. 2020;25:993–1005. https://doi.org/10.1038/s41380-018-0215-1 .
Qu N, et al. A POMC-originated circuit regulates stress-induced hypophagia, depression, and anhedonia. Mol Psychiatry. 2020;25:1006–21. https://doi.org/10.1038/s41380-019-0506-1 .
Fox ME, et al. Dendritic remodeling of D1 neurons by RhoA/Rho-kinase mediates depression-like behavior. Mol Psychiatry. 2020;25:1022–34. https://doi.org/10.1038/s41380-018-0211-5 .
Jin J, et al. Ahnak scaffolds p11/Anxa2 complex and L-type voltage-gated calcium channel and modulates depressive behavior. Mol Psychiatry. 2020;25:1035–49. https://doi.org/10.1038/s41380-019-0371-y .
Ben-Yehuda H, et al. Maternal Type-I interferon signaling adversely affects the microglia and the behavior of the offspring accompanied by increased sensitivity to stress. Mol Psychiatry. 2020;25:1050–67. https://doi.org/10.1038/s41380-019-0604-0 .
Pearson-Leary J, et al. The gut microbiome regulates the increases in depressive-type behaviors and in inflammatory processes in the ventral hippocampus of stress vulnerable rats. Mol Psychiatry. 2020;25:1068–79. https://doi.org/10.1038/s41380-019-0380-x .
Walker WH 2nd, et al. Acute exposure to low-level light at night is sufficient to induce neurological changes and depressive-like behavior. Mol Psychiatry. 2020;25:1080–93. https://doi.org/10.1038/s41380-019-0430-4 .
Lei Y, et al. SIRT1 in forebrain excitatory neurons produces sexually dimorphic effects on depression-related behaviors and modulates neuronal excitability and synaptic transmission in the medial prefrontal cortex. Mol Psychiatry. 2020;25:1094–111. https://doi.org/10.1038/s41380-019-0352-1 .
Sargin D, et al. Mapping the physiological and molecular markers of stress and SSRI antidepressant treatment in S100a10 corticostriatal neurons. Mol Psychiatry. 2020;25:1112–29. https://doi.org/10.1038/s41380-019-0473-6 .
Article Google Scholar
Iob E, Kirschbaum C, Steptoe A. Persistent depressive symptoms, HPA-axis hyperactivity, and inflammation: the role of cognitive-affective and somatic symptoms. Mol Psychiatry. 2020;25:1130–40. https://doi.org/10.1038/s41380-019-0501-6 .
Cabeza de Baca T, et al. Chronic psychosocial and financial burden accelerates 5-year telomere shortening: findings from the Coronary Artery Risk Development in Young Adults Study. Mol Psychiatry. 2020;25:1141–53. https://doi.org/10.1038/s41380-019-0482-5 .
Licinio J & Wong ML. Advances in depression research: special issue, 2020, with three research articles by Paul Greengard. Mol Psychiatry. 2020;25:1156–58. https://doi.org/10.1038/s41380-020-0781-x .
Teissier A, et al. Early-life stress impairs postnatal oligodendrogenesis and adult emotional behaviour through activity-dependent mechanisms. Mol Psychiatry. 2019. https://doi.org/10.1038/s41380-019-0493-2 .
Zhang Y, et al. CircDYM ameliorates depressive-like behavior by targeting miR-9 to regulate microglial activation via HSP90 ubiquitination. Mol Psychiatry. 2018. https://doi.org/10.1038/s41380-018-0285-0 .
Tan A, et al. Effects of the KCNQ channel opener ezogabine on functional connectivity of the ventral striatum and clinical symptoms in patients with major depressive disorder. Mol Psychiatry. 2018. https://doi.org/10.1038/s41380-018-0283-2 .
Kin K, et al. Cell encapsulation enhances antidepressant effect of the mesenchymal stem cells and counteracts depressive-like behavior of treatment-resistant depressed rats. Mol Psychiatry. 2018. https://doi.org/10.1038/s41380-018-0208-0 .
Orrico-Sanchez A, et al. Antidepressant efficacy of a selective organic cation transporter blocker in a mouse model of depression. Mol Psychiatry. 2019. https://doi.org/10.1038/s41380-019-0548-4 .
Han Y, et al. Systemic immunization with altered myelin basic protein peptide produces sustained antidepressant-like effects. Mol Psychiatry. 2019. https://doi.org/10.1038/s41380-019-0470-9 .
Wittenberg GM, et al. Effects of immunomodulatory drugs on depressive symptoms: a mega-analysis of randomized, placebo-controlled clinical trials in inflammatory disorders. Mol Psychiatry. 2019. https://doi.org/10.1038/s41380-019-0471-8 .
Beydoun MA, et al. Systemic inflammation is associated with depressive symptoms differentially by sex and race: a longitudinal study of urban adults. Mol Psychiatry. 2019. https://doi.org/10.1038/s41380-019-0408-2 .
Felger JC, et al. What does plasma CRP tell us about peripheral and central inflammation in depression? Mol Psychiatry. 2018. https://doi.org/10.1038/s41380-018-0096-3 .
Clark SL, et al. A methylation study of long-term depression risk. Mol Psychiatry. 2019. https://doi.org/10.1038/s41380-019-0516-z .
Aberg KA, et al. Methylome-wide association findings for major depressive disorder overlap in blood and brain and replicate in independent brain samples. Mol Psychiatry. 2018. https://doi.org/10.1038/s41380-018-0247-6 .
Wei YB, et al. A functional variant in the serotonin receptor 7 gene (HTR7), rs7905446, is associated with good response to SSRIs in bipolar and unipolar depression. Mol Psychiatry. 2019. https://doi.org/10.1038/s41380-019-0397-1 .
Licinio J. Molecular Psychiatry: the integration of molecular medicine and clinical psychiatry. Mol Psychiatry. 1996;1:1–3.
Steenblock C, et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the neuroendocrine stress axis. Mol Psychiatry. 2020. https://doi.org/10.1038/s41380-020-0758-9 .
Wong ML, Dong C, Andreev V, Arcos-Burgos M, Licinio J. Prediction of susceptibility to major depression by a model of interactions of multiple functional genetic variants and environmental factors. Mol Psychiatry. 2012;17:624–33. https://doi.org/10.1038/mp.2012.13 .
Article CAS PubMed PubMed Central Google Scholar
Lee SH, Paz-Filho G, Mastronardi C, Licinio J, Wong ML. Is increased antidepressant exposure a contributory factor to the obesity pandemic? Transl Psychiatry. 2016;6:e759 https://doi.org/10.1038/tp.2016.25 .
Bornstein SR, Licinio J. Improving the efficacy of translational medicine by optimally integrating health care, academia and industry. Nat Med. 2011;17:1567–9. https://doi.org/10.1038/nm.2583 .
Licinio J, Wong ML. Launching the ‘war on mental illness’. Mol Psychiatry. 2014;19:1–5. https://doi.org/10.1038/mp.2013.180 .
Download references
Author information
Authors and affiliations.
State University of New York, Upstate Medical University, Syracuse, NY, 13210, USA
Julio Licinio & Ma-Li Wong
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Julio Licinio .
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Licinio, J., Wong, ML. Advances in depression research: second special issue, 2020, with highlights on biological mechanisms, clinical features, co-morbidity, genetics, imaging, and treatment. Mol Psychiatry 25 , 1356–1360 (2020). https://doi.org/10.1038/s41380-020-0798-1
Download citation
Published : 18 June 2020
Issue Date : July 2020
DOI : https://doi.org/10.1038/s41380-020-0798-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Upregulation of carbonic anhydrase 1 beneficial for depressive disorder.
Acta Neuropathologica Communications (2023)
Introducing a depression-like syndrome for translational neuropsychiatry: a plea for taxonomical validity and improved comparability between humans and mice
- Iven-Alex von Mücke-Heim
- Lidia Urbina-Treviño
- Jan M. Deussing
Molecular Psychiatry (2023)
Reply to: “The serotonin theory of depression: a systematic umbrella review of the evidence” published by Moncrieff J, Cooper RE, Stockmann T, Amendola S, Hengartner MP, Horowitz MA in Molecular Psychiatry (2022 Jul 20. doi: 10.1038/s41380-022-01661-0)
- Lucie Bartova
- Rupert Lanzenberger
- Siegfried Kasper
Is the serotonin hypothesis/theory of depression still relevant? Methodological reflections motivated by a recently published umbrella review
- Hans-Jürgen Möller
- Peter Falkai
European Archives of Psychiatry and Clinical Neuroscience (2023)
The heterogeneity of late-life depression and its pathobiology: a brain network dysfunction disorder
- Kurt A. Jellinger
Journal of Neural Transmission (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Logo Left Content

Logo Right Content
Stanford University School of Medicine blog

Imagining virtual reality as a simple tool to treat depression
Some of the 17 million Americans afflicted with major depressive disorder each year may soon receive a surprising new prescription from their clinician: Have fun on a virtual reality device.
Engaging in activities that make you feel good may seem like overly simplistic advice, especially when directed at people with severe depression. But the science behind this idea, called "behavioral activation," is well established. Multiple studies have found that encouraging people to get outside, exercise, socialize, volunteer or immerse themselves in enjoyable activities in a prescribed, systematic way can help ease the symptoms of depression.
- Virtual reality helps people with hoarding disorder practice decluttering
Now, Stanford researchers have discovered that engaging in these behaviors within a virtual reality system may show just as much efficacy in treating depression as carrying them out in the real world. And for those depressed to a level that makes leaving the house a challenge, it could provide the benefits of getting outside -- and even motivate them to get out.

"People who might otherwise have barriers to getting treatment might be open to using this technology in their own homes," said Kim Bullock, MD , a clinical professor of psychiatry and behavioral sciences.
The study by Bullock's team, published in JMIR Mental Health , followed 26 people with major depressive disorder. Half were assigned traditional behavioral activation, and half used a virtual reality headset to participate in activities ranging from table tennis and mini-golf to touring foreign cities or attending shows. People in both groups saw their depression scores decrease by similar amounts.
"We've found that using virtual reality in an outpatient group of patients was both simple and efficacious in treating symptoms of depression," said Bullock, founder and director of Stanford's Neurobehavioral Clinic and Virtual Reality and Immersive Technologies (VRIT) program. "It can reduce the barriers to getting mental health treatment in a number of ways."
Bullock and her colleagues at the Stanford VRIT program have long studied the diverse ways to treat mental illnesses with virtual reality (VR) platforms, in which users donning headsets are immersed in simulated, three-dimensional environments.
Previous studies have examined how VR can be used to conduct therapy appointments, help people overcome anxieties and phobias, ease pain, learn social skills, and treat eating disorders and hoarding . But few research projects had focused on how to use the technology to treat anything as pervasive as major depressive disorder or other mood disorders
Depression impacts so many people right now, and we thought VR could have a large impact. Kim Bullock
"Depression impacts so many people right now, and we thought VR could have a large impact," said Bullock, who received support for the project from the Neuroscience:Translate Grant Program . "There can be significant barriers to behavioral activation in some patients -- they might be stuck in a hospital bed, or not have the means to access joyful activities or the motivation to leave their house. We started wondering whether simulated, pleasant activities might be a good first step for some people."
Bullock, along with clinical assistant professor Margot Paul, PsyD , first carried out a small feasibility study to see whether people with depression could use a VR headset with pre-loaded videos to engage in behavioral activation homework assigned by their therapist. After positive feedback from participants, the researchers conducted the randomized, controlled trial to test the efficacy of a more immersive and interactive VR approach.

The participants in the trial, all adults diagnosed with major depressive disorder who had not recently changed medications, met weekly with a clinical psychologist at Stanford who assigned them behavioral activation homework between sessions -- scheduling and committing to at least four pleasurable activities each week, either in virtual reality or real life.
Thirteen people in the study received a VR Meta Quest 2 headset as well as a list of potential activity ideas they could engage in using the headset, including games, travel videos, fitness classes, chat programs and education apps. The other 13 people were told to plan and partake in real life activities in a more typical fashion -- by going on outings in their community or socializing with friends.
After four weeks, both groups saw a significant decrease in their symptoms of depression and their depression rating on a widely used scale. Moreover, many people who had used the VR devices said the virtual activities had helped push them to get out of the house and be more involved in in-person activities.
"One of the most common pieces of feedback we got was that using the VR inspired people to get out and do things in the real world," Paul said. "These virtual activities got their motors running just enough to get out of bed."
- Stanford Medicine uses augmented reality for real-time data visualization during surgery
The only negative feedback pertained to learning how to set up the device, as well as the need for alerts or reminders to keep people accountable for engaging in the behavioral activation. Paul and Bullock have since developed a companion VR behavioral activation app that will help address some of these concerns.
The team says larger and longer-term studies are needed to find the best ways to administer virtual behavioral activation, as well as which patient populations might be best targeted with the VR treatment. They also think more efforts are needed to inform clinicians -- from therapists and psychologists to primary care doctors -- about how to prescribe VR behavioral activation appropriately.
These virtual activities got their motors running just enough to get out of bed. Margot Paul
But Paul, Bullock and their colleagues at Stanford VRIT believe the cost and ease of many VR platforms -- especially those that use mobile phones inserted into cheap cardboard headsets -- make it an easy treatment to scale up. They also believe the technology's relatability to a younger audience can only bring more openness to treating serious conditions like depression.
"As something that seems cool to young people, it serves not only to enhance but also de-stigmatize mental health treatments," Bullock said.
Illustration: Emily Moskal
More news about depression
- Serious talk about moods with bipolar disorder expert Po Wang
- Pilot study shows ketogenic diet improves severe mental illness
- Psychoactive drug ibogaine effectively treats traumatic brain injury in special ops military vets
- Human Neural Circuitry program seeks to investigate deepest mysteries of brain function, dysfunction
- Ketamine's effect on depression may hinge on hope
- Stanford Medicine-led research identifies a subtype of depression
- Researchers treat depression by reversing brain signals traveling the wrong way
- Stanford Medicine researchers find possible cause of depression after stroke
Popular posts

Are long COVID sufferers falling through the cracks?
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Biological, Psychological, and Social Determinants of Depression: A Review of Recent Literature
Olivia remes.
1 Institute for Manufacturing, University of Cambridge, Cambridge CB3 0FS, UK
João Francisco Mendes
2 NOVA Medical School, Universidade NOVA de Lisboa, 1099-085 Lisbon, Portugal; ku.ca.mac@94cfj
Peter Templeton
3 IfM Engage Limited, Institute for Manufacturing, University of Cambridge, Cambridge CB3 0FS, UK; ku.ca.mac@32twp
4 The William Templeton Foundation for Young People’s Mental Health (YPMH), Cambridge CB2 0AH, UK
Associated Data
Depression is one of the leading causes of disability, and, if left unmanaged, it can increase the risk for suicide. The evidence base on the determinants of depression is fragmented, which makes the interpretation of the results across studies difficult. The objective of this study is to conduct a thorough synthesis of the literature assessing the biological, psychological, and social determinants of depression in order to piece together the puzzle of the key factors that are related to this condition. Titles and abstracts published between 2017 and 2020 were identified in PubMed, as well as Medline, Scopus, and PsycInfo. Key words relating to biological, social, and psychological determinants as well as depression were applied to the databases, and the screening and data charting of the documents took place. We included 470 documents in this literature review. The findings showed that there are a plethora of risk and protective factors (relating to biological, psychological, and social determinants) that are related to depression; these determinants are interlinked and influence depression outcomes through a web of causation. In this paper, we describe and present the vast, fragmented, and complex literature related to this topic. This review may be used to guide practice, public health efforts, policy, and research related to mental health and, specifically, depression.
1. Introduction
Depression is one of the most common mental health issues, with an estimated prevalence of 5% among adults [ 1 , 2 ]. Symptoms may include anhedonia, feelings of worthlessness, concentration and sleep difficulties, and suicidal ideation. According to the World Health Organization, depression is a leading cause of disability; research shows that it is a burdensome condition with a negative impact on educational trajectories, work performance, and other areas of life [ 1 , 3 ]. Depression can start early in the lifecourse and, if it remains unmanaged, may increase the risk for substance abuse, chronic conditions, such as cardiovascular disease, and premature mortality [ 4 , 5 , 6 , 7 , 8 ].
Treatment for depression exists, such as pharmacotherapy, cognitive behavioural therapy, and other modalities. A meta-analysis of randomized, placebo-controlled trials of patients shows that 56–60% of people respond well to active treatment with antidepressants (selective serotonin reuptake inhibitors, tricyclic antidepressants) [ 9 ]. However, pharmacotherapy may be associated with problems, such as side-effects, relapse issues, a potential duration of weeks until the medication starts working, and possible limited efficacy in mild cases [ 10 , 11 , 12 , 13 , 14 ]. Psychotherapy is also available, but access barriers can make it difficult for a number of people to get the necessary help.
Studies on depression have increased significantly over the past few decades. However, the literature remains fragmented and the interpretation of heterogeneous findings across studies and between fields is difficult. The cross-pollination of ideas between disciplines, such as genetics, neurology, immunology, and psychology, is limited. Reviews on the determinants of depression have been conducted, but they either focus exclusively on a particular set of determinants (ex. genetic risk factors [ 15 ]) or population sub-group (ex. children and adolescents [ 16 ]) or focus on characteristics measured predominantly at the individual level (ex. focus on social support, history of depression [ 17 ]) without taking the wider context (ex. area-level variables) into account. An integrated approach paying attention to key determinants from the biological, psychological, and social spheres, as well as key themes, such as the lifecourse perspective, enables clinicians and public health authorities to develop tailored, person-centred approaches.
The primary aim of this literature review: to address the aforementioned challenges, we have synthesized recent research on the biological, psychological, and social determinants of depression and we have reviewed research from fields including genetics, immunology, neurology, psychology, public health, and epidemiology, among others.
The subsidiary aim: we have paid special attention to important themes, including the lifecourse perspective and interactions between determinants, to guide further efforts by public health and medical professionals.
This literature review can be used as an evidence base by those in public health and the clinical setting and can be used to inform targeted interventions.
2. Materials and Methods
We conducted a review of the literature on the biological, psychological, and social determinants of depression in the last 4 years. We decided to focus on these determinants after discussions with academics (from the Manchester Metropolitan University, University of Cardiff, University of Colorado, Boulder, University of Cork, University of Leuven, University of Texas), charity representatives, and people with lived experience at workshops held by the University of Cambridge in 2020. In several aspects, we attempted to conduct this review according to PRISMA guidelines [ 18 ].
The inclusion and exclusion criteria are the following:
- - We included documents, such as primary studies, literature reviews, systematic reviews, meta-analyses, reports, and commentaries on the determinants of depression. The determinants refer to variables that appear to be linked to the development of depression, such as physiological factors (e.g., the nervous system, genetics), but also factors that are further away or more distal to the condition. Determinants may be risk or protective factors, and individual- or wider-area-level variables.
- - We focused on major depressive disorder, treatment-resistant depression, dysthymia, depressive symptoms, poststroke depression, perinatal depression, as well as depressive-like behaviour (common in animal studies), among others.
- - We included papers regardless of the measurement methods of depression.
- - We included papers that focused on human and/or rodent research.
- - This review focused on articles written in the English language.
- - Documents published between 2017–2020 were captured to provide an understanding of the latest research on this topic.
- - Studies that assessed depression as a comorbidity or secondary to another disorder.
- - Studies that did not focus on rodent and/or human research.
- - Studies that focused on the treatment of depression. We made this decision, because this is an in-depth topic that would warrant a separate stand-alone review.
- Next, we searched PubMed (2017–2020) using keywords related to depression and determinants. Appendix A contains the search strategy used. We also conducted focused searches in Medline, Scopus, and PsycInfo (2017–2020).
- Once the documents were identified through the databases, the inclusion and exclusion criteria were applied to the titles and abstracts. Screening of documents was conducted by O.R., and a subsample was screened by J.M.; any discrepancies were resolved through a communication process.
- The full texts of documents were retrieved, and the inclusion and exclusion criteria were again applied. A subsample of documents underwent double screening by two authors (O.R., J.M.); again, any discrepancies were resolved through communication.
- a. A data charting form was created to capture the data elements of interest, including the authors, titles, determinants (biological, psychological, social), and the type of depression assessed by the research (e.g., major depression, depressive symptoms, depressive behaviour).
- b. The data charting form was piloted on a subset of documents, and refinements to it were made. The data charting form was created with the data elements described above and tested in 20 studies to determine whether refinements in the wording or language were needed.
- c. Data charting was conducted on the documents.
- d. Narrative analysis was conducted on the data charting table to identify key themes. When a particular finding was noted more than once, it was logged as a potential theme, with a review of these notes yielding key themes that appeared on multiple occasions. When key themes were identified, one researcher (O.R.) reviewed each document pertaining to that theme and derived concepts (key determinants and related outcomes). This process (a subsample) was verified by a second author (J.M.), and the two authors resolved any discrepancies through communication. Key themes were also checked as to whether they were of major significance to public mental health and at the forefront of public health discourse according to consultations we held with stakeholders from the Manchester Metropolitan University, University of Cardiff, University of Colorado, Boulder, University of Cork, University of Leuven, University of Texas, charity representatives, and people with lived experience at workshops held by the University of Cambridge in 2020.
We condensed the extensive information gleaned through our review into short summaries (with key points boxes for ease of understanding and interpretation of the data).
Through the searches, 6335 documents, such as primary studies, literature reviews, systematic reviews, meta-analyses, reports, and commentaries, were identified. After applying the inclusion and exclusion criteria, 470 papers were included in this review ( Supplementary Table S1 ). We focused on aspects related to biological, psychological, and social determinants of depression (examples of determinants and related outcomes are provided under each of the following sections.
3.1. Biological Factors
The following aspects will be discussed in this section: physical health conditions; then specific biological factors, including genetics; the microbiome; inflammatory factors; stress and hypothalamic–pituitary–adrenal (HPA) axis dysfunction, and the kynurenine pathway. Finally, aspects related to cognition will also be discussed in the context of depression.
3.1.1. Physical Health Conditions
Studies on physical health conditions—key points:
- The presence of a physical health condition can increase the risk for depression
- Psychological evaluation in physically sick populations is needed
- There is large heterogeneity in study design and measurement; this makes the comparison of findings between and across studies difficult
A number of studies examined the links between the outcome of depression and physical health-related factors, such as bladder outlet obstruction, cerebral atrophy, cataract, stroke, epilepsy, body mass index and obesity, diabetes, urinary tract infection, forms of cancer, inflammatory bowel disorder, glaucoma, acne, urea accumulation, cerebral small vessel disease, traumatic brain injury, and disability in multiple sclerosis [ 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 ]. For example, bladder outlet obstruction has been linked to inflammation and depressive behaviour in rodent research [ 24 ]. The presence of head and neck cancer also seemed to be related to an increased risk for depressive disorder [ 45 ]. Gestational diabetes mellitus has been linked to depressive symptoms in the postpartum period (but no association has been found with depression in the third pregnancy trimester) [ 50 ], and a plethora of other such examples of relationships between depression and physical conditions exist. As such, the assessment of psychopathology and the provision of support are necessary in individuals of ill health [ 45 ]. Despite the large evidence base on physical health-related factors, differences in study methodology and design, the lack of standardization when it comes to the measurement of various physical health conditions and depression, and heterogeneity in the study populations makes it difficult to compare studies [ 50 ].
The next subsections discuss specific biological factors, including genetics; the microbiome; inflammatory factors; stress and hypothalamic–pituitary–adrenal (HPA) axis dysfunction, and the kynurenine pathway; and aspects related to cognition.
3.1.2. Genetics
Studies on genetics—key points:
There were associations between genetic factors and depression; for example:
- The brain-derived neurotrophic factor (BDNF) plays an important role in depression
- Links exist between major histocompatibility complex region genes, as well as various gene polymorphisms and depression
- Single nucleotide polymorphisms (SNPs) of genes involved in the tryptophan catabolites pathway are of interest in relation to depression
A number of genetic-related factors, genomic regions, polymorphisms, and other related aspects have been examined with respect to depression [ 61 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 , 109 , 110 , 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 , 119 , 120 , 121 , 122 , 123 , 124 , 125 , 126 , 127 , 128 , 129 , 130 , 131 , 132 , 133 , 134 , 135 , 136 , 137 , 138 , 139 , 140 ]. The influence of BDNF in relation to depression has been amply studied [ 117 , 118 , 141 , 142 , 143 ]. Research has shown associations between depression and BDNF (as well as candidate SNPs of the BDNF gene, polymorphisms of the BDNF gene, and the interaction of these polymorphisms with other determinants, such as stress) [ 129 , 144 , 145 ]. Specific findings have been reported: for example, a study reported a link between the BDNF rs6265 allele (A) and major depressive disorder [ 117 ].
Other research focused on major histocompatibility complex region genes, endocannabinoid receptor gene polymorphisms, as well as tissue-specific genes and gene co-expression networks and their links to depression [ 99 , 110 , 112 ]. The SNPs of genes involved in the tryptophan catabolites pathway have also been of interest when studying the pathogenesis of depression.
The results from genetics studies are compelling; however, the findings remain mixed. One study indicated no support for depression candidate gene findings [ 122 ]. Another study found no association between specific polymorphisms and major depressive disorder [ 132 ]. As such, further research using larger samples is needed to corroborate the statistically significant associations reported in the literature.
3.1.3. Microbiome
Studies on the microbiome—key points:
- The gut bacteria and the brain communicate via both direct and indirect pathways called the gut-microbiota-brain axis (the bidirectional communication networks between the central nervous system and the gastrointestinal tract; this axis plays an important role in maintaining homeostasis).
- A disordered microbiome can lead to inflammation, which can then lead to depression
- There are possible links between the gut microbiome, host liver metabolism, brain inflammation, and depression
The common themes of this review have focused on the microbiome/microbiota or gut metabolome [ 146 , 147 , 148 , 149 , 150 , 151 , 152 , 153 , 154 , 155 , 156 , 157 , 158 , 159 , 160 , 161 ], the microbiota-gut-brain axis, and related factors [ 152 , 162 , 163 , 164 , 165 , 166 , 167 ]. When there is an imbalance in the intestinal bacteria, this can interfere with emotional regulation and contribute to harmful inflammatory processes and mood disorders [ 148 , 151 , 153 , 155 , 157 ]. Rodent research has shown that there may be a bidirectional association between the gut microbiota and depression: a disordered gut microbiota can play a role in the onset of this mental health problem, but, at the same time, the existence of stress and depression may also lead to a lower level of richness and diversity in the microbiome [ 158 ].
Research has also attempted to disentangle the links between the gut microbiome, host liver metabolism, brain inflammation, and depression, as well as the role of the ratio of lactobacillus to clostridium [ 152 ]. The literature has also examined the links between medication, such as antibiotics, and mood and behaviour, with the findings showing that antibiotics may be related to depression [ 159 , 168 ]. The links between the microbiome and depression are complex, and further studies are needed to determine the underpinning causal mechanisms.
3.1.4. Inflammation
Studies on inflammation—key points:
- Pro-inflammatory cytokines are linked to depression
- Pro-inflammatory cytokines, such as the tumour necrosis factor (TNF)-alpha, may play an important role
- Different methods of measurement are used, making the comparison of findings across studies difficult
Inflammation has been a theme in this literature review [ 60 , 161 , 164 , 169 , 170 , 171 , 172 , 173 , 174 , 175 , 176 , 177 , 178 , 179 , 180 , 181 , 182 , 183 , 184 ]. The findings show that raised levels of inflammation (because of factors such as pro-inflammatory cytokines) have been associated with depression [ 60 , 161 , 174 , 175 , 178 ]. For example, pro-inflammatory cytokines, such as tumour necrosis factor (TNF)-alpha, have been linked to depression [ 185 ]. Various determinants, such as early life stress, have also been linked to systemic inflammation, and this can increase the risk for depression [ 186 ].
Nevertheless, not everyone with elevated inflammation develops depression; therefore, this is just one route out of many linked to pathogenesis. Despite the compelling evidence reported with respect to inflammation, it is difficult to compare the findings across studies because of different methods used to assess depression and its risk factors.
3.1.5. Stress and HPA Axis Dysfunction
Studies on stress and HPA axis dysfunction—key points:
- Stress is linked to the release of proinflammatory factors
- The dysregulation of the HPA axis is linked to depression
- Determinants are interlinked in a complex web of causation
Stress was studied in various forms in rodent populations and humans [ 144 , 145 , 155 , 174 , 176 , 180 , 185 , 186 , 187 , 188 , 189 , 190 , 191 , 192 , 193 , 194 , 195 , 196 , 197 , 198 , 199 , 200 , 201 , 202 , 203 , 204 , 205 , 206 , 207 , 208 , 209 , 210 , 211 ].
Although this section has some overlap with others (as is to be expected because all of these determinants and body systems are interlinked), a number of studies have focused on the impact of stress on mental health. Stress has been mentioned in the literature as a risk factor of poor mental health and has emerged as an important determinant of depression. The effects of this variable are wide-ranging, and a short discussion is warranted.
Stress has been linked to the release of inflammatory factors, as well as the development of depression [ 204 ]. When the stress is high or lasts for a long period of time, this may negatively impact the brain. Chronic stress can impact the dendrites and synapses of various neurons, and may be implicated in the pathway leading to major depressive disorder [ 114 ]. As a review by Uchida et al. indicates, stress may be associated with the “dysregulation of neuronal and synaptic plasticity” [ 114 ]. Even in rodent studies, stress has a negative impact: chronic and unpredictable stress (and other forms of tension or stress) have been linked to unusual behaviour and depression symptoms [ 114 ].
The depression process and related brain changes, however, have also been linked to the hyperactivity or dysregulation of the HPA axis [ 127 , 130 , 131 , 182 , 212 ]. One review indicates that a potential underpinning mechanism of depression relates to “HPA axis abnormalities involved in chronic stress” [ 213 ]. There is a complex relationship between the HPA axis, glucocorticoid receptors, epigenetic mechanisms, and psychiatric sequelae [ 130 , 212 ].
In terms of the relationship between the HPA axis and stress and their influence on depression, the diathesis–stress model offers an explanation: it could be that early stress plays a role in the hyperactivation of the HPA axis, thus creating a predisposition “towards a maladaptive reaction to stress”. When this predisposition then meets an acute stressor, depression may ensue; thus, in line with the diathesis–stress model, a pre-existing vulnerability and stressor can create fertile ground for a mood disorder [ 213 ]. An integrated review by Dean and Keshavan [ 213 ] suggests that HPA axis hyperactivity is, in turn, related to other determinants, such as early deprivation and insecure early attachment; this again shows the complex web of causation between the different determinants.
3.1.6. Kynurenine Pathway
Studies on the kynurenine pathway—key points:
- The kynurenine pathway is linked to depression
- Indolamine 2,3-dioxegenase (IDO) polymorphisms are linked to postpartum depression
The kynurenine pathway was another theme that emerged in this review [ 120 , 178 , 181 , 184 , 214 , 215 , 216 , 217 , 218 , 219 , 220 , 221 ]. The kynurenine pathway has been implicated not only in general depressed mood (inflammation-induced depression) [ 184 , 214 , 219 ] but also postpartum depression [ 120 ]. When the kynurenine metabolism pathway is activated, this results in metabolites, which are neurotoxic.
A review by Jeon et al. notes a link between the impairment of the kynurenine pathway and inflammation-induced depression (triggered by treatment for various physical diseases, such as malignancy). The authors note that this could represent an important opportunity for immunopharmacology [ 214 ]. Another review by Danzer et al. suggests links between the inflammation-induced activation of indolamine 2,3-dioxegenase (the enzyme that converts tryptophan to kynurenine), the kynurenine metabolism pathway, and depression, and also remarks about the “opportunities for treatment of inflammation-induced depression” [ 184 ].
3.1.7. Cognition
Studies on cognition and the brain—key points:
- Cognitive decline and cognitive deficits are linked to increased depression risk
- Cognitive reserve is important in the disability/depression relationship
- Family history of cognitive impairment is linked to depression
A number of studies have focused on the theme of cognition and the brain. The results show that factors, such as low cognitive ability/function, cognitive vulnerability, cognitive impairment or deficits, subjective cognitive decline, regression of dendritic branching and hippocampal atrophy/death of hippocampal cells, impaired neuroplasticity, and neurogenesis-related aspects, have been linked to depression [ 131 , 212 , 222 , 223 , 224 , 225 , 226 , 227 , 228 , 229 , 230 , 231 , 232 , 233 , 234 , 235 , 236 , 237 , 238 , 239 ]. The cognitive reserve appears to act as a moderator and can magnify the impact of certain determinants on poor mental health. For example, in a study in which participants with multiple sclerosis also had low cognitive reserve, disability was shown to increase the risk for depression [ 63 ]. Cognitive deficits can be both causal and resultant in depression. A study on individuals attending outpatient stroke clinics showed that lower scores in cognition were related to depression; thus, cognitive impairment appears to be associated with depressive symptomatology [ 226 ]. Further, Halahakoon et al. [ 222 ] note a meta-analysis [ 240 ] that shows that a family history of cognitive impairment (in first degree relatives) is also linked to depression.
In addition to cognitive deficits, low-level cognitive ability [ 231 ] and cognitive vulnerability [ 232 ] have also been linked to depression. While cognitive impairment may be implicated in the pathogenesis of depressive symptoms [ 222 ], negative information processing biases are also important; according to the ‘cognitive neuropsychological’ model of depression, negative affective biases play a central part in the development of depression [ 222 , 241 ]. Nevertheless, the evidence on this topic is mixed and further work is needed to determine the underpinning mechanisms between these states.
3.2. Psychological Factors
Studies on psychological factors—key points:
- There are many affective risk factors linked to depression
- Determinants of depression include negative self-concept, sensitivity to rejection, neuroticism, rumination, negative emotionality, and others
A number of studies have been undertaken on the psychological factors linked to depression (including mastery, self-esteem, optimism, negative self-image, current or past mental health conditions, and various other aspects, including neuroticism, brooding, conflict, negative thinking, insight, cognitive fusion, emotional clarity, rumination, dysfunctional attitudes, interpretation bias, and attachment style) [ 66 , 128 , 140 , 205 , 210 , 228 , 235 , 242 , 243 , 244 , 245 , 246 , 247 , 248 , 249 , 250 , 251 , 252 , 253 , 254 , 255 , 256 , 257 , 258 , 259 , 260 , 261 , 262 , 263 , 264 , 265 , 266 , 267 , 268 , 269 , 270 , 271 , 272 , 273 , 274 , 275 , 276 , 277 , 278 , 279 , 280 , 281 , 282 , 283 , 284 , 285 , 286 , 287 , 288 , 289 , 290 ]. Determinants related to this condition include low self-esteem and shame, among other factors [ 269 , 270 , 275 , 278 ]. Several emotional states and traits, such as neuroticism [ 235 , 260 , 271 , 278 ], negative self-concept (with self-perceptions of worthlessness and uselessness), and negative interpretation or attention biases have been linked to depression [ 261 , 271 , 282 , 283 , 286 ]. Moreover, low emotional clarity has been associated with depression [ 267 ]. When it comes to the severity of the disorder, it appears that meta-emotions (“emotions that occur in response to other emotions (e.g., guilt about anger)” [ 268 ]) have a role to play in depression [ 268 ].
A determinant that has received much attention in mental health research concerns rumination. Rumination has been presented as a mediator but also as a risk factor for depression [ 57 , 210 , 259 ]. When studied as a risk factor, it appears that the relationship of rumination with depression is mediated by variables that include limited problem-solving ability and insufficient social support [ 259 ]. However, rumination also appears to act as a mediator: for example, this variable (particularly brooding rumination) lies on the causal pathway between poor attention control and depression [ 265 ]. This shows that determinants may present in several forms: as moderators or mediators, risk factors or outcomes, and this is why disentangling the relationships between the various factors linked to depression is a complex task.
The psychological determinants are commonly researched variables in the mental health literature. A wide range of factors have been linked to depression, such as the aforementioned determinants, but also: (low) optimism levels, maladaptive coping (such as avoidance), body image issues, and maladaptive perfectionism, among others [ 269 , 270 , 272 , 273 , 275 , 276 , 279 , 285 , 286 ]. Various mechanisms have been proposed to explain the way these determinants increase the risk for depression. One of the underpinning mechanisms linking the determinants and depression concerns coping. For example, positive fantasy engagement, cognitive biases, or personality dispositions may lead to emotion-focused coping, such as brooding, and subsequently increase the risk for depression [ 272 , 284 , 287 ]. Knowing the causal mechanisms linking the determinants to outcomes provides insight for the development of targeted interventions.
3.3. Social Determinants
Studies on social determinants—key points:
- Social determinants are the conditions in the environments where people are born, live, learn, work, play, etc.; these influence (mental) health [ 291 ]
- There are many social determinants linked to depression, such as sociodemographics, social support, adverse childhood experiences
- Determinants can be at the individual, social network, community, and societal levels
Studies also focused on the social determinants of (mental) health; these are the conditions in which people are born, live, learn, work, play, and age, and have a significant influence on wellbeing [ 291 ]. Factors such as age, social or socioeconomic status, social support, financial strain and deprivation, food insecurity, education, employment status, living arrangements, marital status, race, childhood conflict and bullying, violent crime exposure, abuse, discrimination, (self)-stigma, ethnicity and migrant status, working conditions, adverse or significant life events, illiteracy or health literacy, environmental events, job strain, and the built environment have been linked to depression, among others [ 52 , 133 , 235 , 236 , 239 , 252 , 269 , 280 , 292 , 293 , 294 , 295 , 296 , 297 , 298 , 299 , 300 , 301 , 302 , 303 , 304 , 305 , 306 , 307 , 308 , 309 , 310 , 311 , 312 , 313 , 314 , 315 , 316 , 317 , 318 , 319 , 320 , 321 , 322 , 323 , 324 , 325 , 326 , 327 , 328 , 329 , 330 , 331 , 332 , 333 , 334 , 335 , 336 , 337 , 338 , 339 , 340 , 341 , 342 , 343 , 344 , 345 , 346 , 347 , 348 , 349 , 350 , 351 , 352 , 353 , 354 , 355 , 356 , 357 , 358 , 359 , 360 , 361 , 362 , 363 , 364 , 365 , 366 , 367 , 368 , 369 , 370 , 371 ]. Social support and cohesion, as well as structural social capital, have also been identified as determinants [ 140 , 228 , 239 , 269 , 293 , 372 , 373 , 374 , 375 , 376 , 377 , 378 , 379 ]. In a study, part of the findings showed that low levels of education have been shown to be linked to post-stroke depression (but not severe or clinical depression outcomes) [ 299 ]. A study within a systematic review indicated that having only primary education was associated with a higher risk of depression compared to having secondary or higher education (although another study contrasted this finding) [ 296 ]. Various studies on socioeconomic status-related factors have been undertaken [ 239 , 297 ]; the research has shown that a low level of education is linked to depression [ 297 ]. Low income is also related to depressive disorders [ 312 ]. By contrast, high levels of education and income are protective [ 335 ].
A group of determinants touched upon by several studies included adverse childhood or early life experiences: ex. conflict with parents, early exposure to traumatic life events, bullying and childhood trauma were found to increase the risk of depression (ex. through pathways, such as inflammation, interaction effects, or cognitive biases) [ 161 , 182 , 258 , 358 , 362 , 380 ].
Gender-related factors were also found to play an important role with respect to mental health [ 235 , 381 , 382 , 383 , 384 , 385 ]. Gender inequalities can start early on in the lifecourse, and women were found to be twice as likely to have depression as men. Gender-related factors were linked to cognitive biases, resilience and vulnerabilities [ 362 , 384 ].
Determinants can impact mental health outcomes through underpinning mechanisms. For example, harmful determinants can influence the uptake of risk behaviours. Risk behaviours, such as sedentary behaviour, substance abuse and smoking/nicotine exposure, have been linked to depression [ 226 , 335 , 355 , 385 , 386 , 387 , 388 , 389 , 390 , 391 , 392 , 393 , 394 , 395 , 396 , 397 , 398 , 399 , 400 , 401 ]. Harmful determinants can also have an impact on diet. Indeed, dietary aspects and diet components (ex. vitamin D, folate, selenium intake, iron, vitamin B12, vitamin K, fiber intake, zinc) as well as diet-related inflammatory potential have been linked to depression outcomes [ 161 , 208 , 236 , 312 , 396 , 402 , 403 , 404 , 405 , 406 , 407 , 408 , 409 , 410 , 411 , 412 , 413 , 414 , 415 , 416 , 417 , 418 , 419 , 420 , 421 , 422 , 423 , 424 , 425 , 426 , 427 , 428 ]. A poor diet has been linked to depression through mechanisms such as inflammation [ 428 ].
Again, it is difficult to constrict diet to the ‘social determinants of health’ category as it also relates to inflammation (biological determinants) and could even stand alone as its own category. Nevertheless, all of these factors are interlinked and influence one another in a complex web of causation, as mentioned elsewhere in the paper.
Supplementary Figure S1 contains a representation of key determinants acting at various levels: the individual, social network, community, and societal levels. The determinants have an influence on risk behaviours, and this, in turn, can affect the mood (i.e., depression), body processes (ex. can increase inflammation), and may negatively influence brain structure and function.
3.4. Others
Studies on ‘other’ determinants—key points:
- A number of factors are related to depression
- These may not be as easily categorized as the other determinants in this paper
A number of factors arose in this review that were related to depression; it was difficult to place these under a specific heading above, so this ‘other’ category was created. A number of these could be sorted under the ‘social determinants of depression’ category. For example, being exposed to deprivation, hardship, or adversity may increase the risk for air pollution exposure and nighttime shift work, among others, and the latter determinants have been found to increase the risk for depression. Air pollution could also be regarded as an ecologic-level (environmental) determinant of mental health.
Nevertheless, we have decided to leave these factors in a separate category (because their categorization may not be as immediately clear-cut as others), and these factors include: low-level light [ 429 ], weight cycling [ 430 ], water contaminants [ 431 ], trade [ 432 ], air pollution [ 433 , 434 ], program-level variables (ex. feedback and learning experience) [ 435 ], TV viewing [ 436 ], falls [ 437 ], various other biological factors [ 116 , 136 , 141 , 151 , 164 , 182 , 363 , 364 , 438 , 439 , 440 , 441 , 442 , 443 , 444 , 445 , 446 , 447 , 448 , 449 , 450 , 451 , 452 , 453 , 454 , 455 , 456 , 457 , 458 , 459 , 460 , 461 , 462 , 463 , 464 , 465 , 466 , 467 , 468 , 469 ], mobile phone use [ 470 ], ultrasound chronic exposure [ 471 ], nighttime shift work [ 472 ], work accidents [ 473 ], therapy enrollment [ 226 ], and exposure to light at night [ 474 ].
4. Cross-Cutting Themes
4.1. lifecourse perspective.
Studies on the lifecourse perspective—key points:
- Early life has an importance on mental health
- Stress has been linked to depression
- In old age, the decline in social capital is important
Trajectories and life events are important when it comes to the lifecourse perspective. Research has touched on the influence of prenatal or early life stress on an individual’s mental health trajectory [ 164 , 199 , 475 ]. Severe stress that occurs in the form of early-life trauma has also been associated with depressive symptoms [ 362 , 380 ]. It may be that some individuals exposed to trauma develop thoughts of personal failure, which then serve as a catalyst of depression [ 380 ].
At the other end of the life trajectory—old age—specific determinants have been linked to an increased risk for depression. Older people are at a heightened risk of losing their social networks, and structural social capital has been identified as important in relation to depression in old age [ 293 ].
4.2. Gene–Environment Interactions
Studies on gene–environment interactions—key points:
- The environment and genetics interact to increase the risk of depression
- The etiology of depression is multifactorial
- Adolescence is a time of vulnerability
A number of studies have touched on gene–environment interactions [ 72 , 77 , 82 , 119 , 381 , 476 , 477 , 478 , 479 , 480 , 481 ]. The interactions between genetic factors and determinants, such as negative life events (ex. relationship and social difficulties, serious illness, unemployment and financial crises) and stressors (ex. death of spouse, minor violations of law, neighbourhood socioeconomic status) have been studied in relation to depression [ 82 , 135 , 298 , 449 , 481 ]. A study reported an interaction of significant life events with functional variation in the serotonin-transporter-linked polymorphic region (5-HTTLPR) allele type (in the context of multiple sclerosis) and linked this to depression [ 361 ], while another reported an interaction between stress and 5-HTTLPR in relation to depression [ 480 ]. Other research reported that the genetic variation of HPA-axis genes has moderating effects on the relationship between stressors and depression [ 198 ]. Another study showed that early-life stress interacts with gene variants to increase the risk for depression [ 77 ].
Adolescence is a time of vulnerability [ 111 , 480 ]. Perceived parental support has been found to interact with genes (GABRR1, GABRR2), and this appears to be associated with depressive symptoms in adolescence [ 480 ]. It is important to pay special attention to critical periods in the lifecourse so that adequate support is provided to those who are most vulnerable.
The etiology of depression is multifactorial, and it is worthwhile to examine the interaction between multiple factors, such as epigenetic, genetic, and environmental factors, in order to truly understand this mental health condition. Finally, taking into account critical periods of life when assessing gene–environment interactions is important for developing targeted interventions.
5. Discussion
Depression is one of the most common mental health conditions, and, if left untreated, it can increase the risk for substance abuse, anxiety disorders, and suicide. In the past 20 years, a large number of studies on the risk and protective factors of depression have been undertaken in various fields, such as genetics, neurology, immunology, and epidemiology. However, there are limitations associated with the extant evidence base. The previous syntheses on depression are limited in scope and focus exclusively on social or biological factors, population sub-groups, or examine depression as a comorbidity (rather than an independent disorder). The research on the determinants and causal pathways of depression is fragmentated and heterogeneous, and this has not helped to stimulate progress when it comes to the prevention and intervention of this condition—specifically unravelling the complexity of the determinants related to this condition and thus refining the prevention and intervention methods.
The scope of this paper was to bring together the heterogeneous, vast, and fragmented literature on depression and paint a picture of the key factors that contribute to this condition. The findings from this review show that there are important themes when it comes to the determinants of depression, such as: the microbiome, dysregulation of the HPA axis, inflammatory reactions, the kynurenine pathway, as well as psychological and social factors. It may be that physical factors are proximal determinants of depression, which, in turn, are acted on by more distal social factors, such as deprivation, environmental events, and social capital.
The Marmot Report [ 291 ], the World Health Organization [ 482 ], and Compton et al. [ 483 ] highlight that the most disadvantaged segments of society are suffering (the socioeconomic context is important), and this inequality in resources has translated to inequality in mental health outcomes [ 483 ]. To tackle the issue of egalitarianism and restore equality in the health between the groups, the social determinants need to be addressed [ 483 ]. A wide range of determinants of mental health have been identified in the literature: age, gender, ethnicity, family upbringing and early attachment patterns, social support, access to food, water and proper nutrition, and community factors. People spiral downwards because of individual- and societal-level circumstances; therefore, these circumstances along with the interactions between the determinants need to be considered.
Another important theme in the mental health literature is the lifecourse perspective. This shows that the timing of events has significance when it comes to mental health. Early life is a critical period during the lifespan at which cognitive processes develop. Exposure to harmful determinants, such as stress, during this period can place an individual on a trajectory of depression in adulthood or later life. When an individual is exposed to harmful determinants during critical periods and is also genetically predisposed to depression, the risk for the disorder can be compounded. This is why aspects such as the lifecourse perspective and gene–environment interactions need to be taken into account. Insight into this can also help to refine targeted interventions.
A number of interventions for depression have been developed or recommended, addressing, for example, the physical factors described here and lifestyle modifications. Interventions targeting various factors, such as education and socioeconomic status, are needed to help prevent and reduce the burden of depression. Further research on the efficacy of various interventions is needed. Additional studies are also needed on each of the themes described in this paper, for example: the biological factors related to postpartum depression [ 134 ], and further work is needed on depression outcomes, such as chronic, recurrent depression [ 452 ]. Previous literature has shown that chronic stress (associated with depression) is also linked to glucocorticoid receptor resistance, as well as problems with the regulation of the inflammatory response [ 484 ]. Further work is needed on this and the underpinning mechanisms between the determinants and outcomes. This review highlighted the myriad ways of measuring depression and its determinants [ 66 , 85 , 281 , 298 , 451 , 485 ]. Thus, the standardization of the measurements of the outcomes (ex. a gold standard for measuring depression) and determinants is essential; this can facilitate comparisons of findings across studies.
5.1. Strengths
This paper has important strengths. It brings together the wide literature on depression and helps to bridge disciplines in relation to one of the most common mental health problems. We identified, selected, and extracted data from studies, and provided concise summaries.
5.2. Limitations
The limitations of the review include missing potentially important studies; however, this is a weakness that cannot be avoided by literature reviews. Nevertheless, the aim of the review was not to identify each study that has been conducted on the risk and protective factors of depression (which a single review is unable to capture) but rather to gain insight into the breadth of literature on this topic, highlight key biological, psychological, and social determinants, and shed light on important themes, such as the lifecourse perspective and gene–environment interactions.
6. Conclusions
We have reviewed the determinants of depression and recognize that there are a multitude of risk and protective factors at the individual and wider ecologic levels. These determinants are interlinked and influence one another. We have attempted to describe the wide literature on this topic, and we have brought to light major factors that are of public mental health significance. This review may be used as an evidence base by those in public health, clinical practice, and research.
This paper discusses key areas in depression research; however, an exhaustive discussion of all the risk factors and determinants linked to depression and their mechanisms is not possible in one journal article—which, by its very nature, a single paper cannot do. We have brought to light overarching factors linked to depression and a workable conceptual framework that may guide clinical and public health practice; however, we encourage other researchers to continue to expand on this timely and relevant work—particularly as depression is a top priority on the policy agenda now.
Acknowledgments
Thank you to Isla Kuhn for the help with the Medline, Scopus, and PsycInfo database searches.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/brainsci11121633/s1 , Figure S1: Conceptual framework: Determinants of depression, Table S1: Data charting—A selection of determinants from the literature.
Appendix A.1. Search Strategy
Search: ((((((((((((((((“Gene-Environment Interaction”[Majr]) OR (“Genetics”[Mesh])) OR (“Genome-Wide Association Study”[Majr])) OR (“Microbiota”[Mesh] OR “Gastrointestinal Microbiome”[Mesh])) OR (“Neurogenic Inflammation”[Mesh])) OR (“genetic determinant”)) OR (“gut-brain-axis”)) OR (“Kynurenine”[Majr])) OR (“Cognition”[Mesh])) OR (“Neuronal Plasticity”[Majr])) OR (“Neurogenesis”[Mesh])) OR (“Genes”[Mesh])) OR (“Neurology”[Majr])) OR (“Social Determinants of Health”[Majr])) OR (“Glucocorticoids”[Mesh])) OR (“Tryptophan”[Mesh])) AND (“Depression”[Mesh] OR “Depressive Disorder”[Mesh]) Filters: from 2017—2020.
Ovid MEDLINE(R) and Epub Ahead of Print, In-Process, In-Data-Review & Other Non-Indexed Citations, Daily and Versions(R)
- exp *Depression/
- exp *Depressive Disorder/
- exp *”Social Determinants of Health”/
- exp *Tryptophan/
- exp *Glucocorticoids/
- exp *Neurology/
- exp *Genes/
- exp *Neurogenesis/
- exp *Neuronal Plasticity/
- exp *Kynurenine/
- exp *Genetics/
- exp *Neurogenic Inflammation/
- exp *Gastrointestinal Microbiome/
- exp *Genome-Wide Association Study/
- exp *Gene-Environment Interaction/
- exp *Depression/et [Etiology]
- exp *Depressive Disorder/et
- or/4-16 637368
- limit 22 to yr = “2017–Current”
- “cause* of depression”.mp.
- “cause* of depression”.ti.
- (cause adj3 (depression or depressive)).ti.
- (caus* adj3 (depression or depressive)).ti.
Appendix A.2. PsycInfo
(TITLE ( depression OR “ Depressive Disorder ”) AND TITLE (“ Social Determinants of Health ” OR tryptophan OR glucocorticoids OR neurology OR genes OR neurogenesis OR “ Neuronal Plasticity ” OR kynurenine OR genetics OR “ Neurogenic Inflammation ” OR “ Gastrointestinal Microbiome ” OR “ Genome-Wide Association Study ” OR “ Gene-Environment Interaction ” OR aetiology OR etiology )) OR TITLE ( cause* W/3 ( depression OR depressive )).
Author Contributions
O.R. was responsible for the design of the study and methodology undertaken. Despite P.T.’s involvement in YPMH, he had no role in the design of the study; P.T. was responsible for the conceptualization of the study. Validation was conducted by O.R. and J.F.M. Formal analysis (data charting) was undertaken by O.R. O.R. and P.T. were involved in the investigation, resource acquisition, and data presentation. The original draft preparation was undertaken by O.R. The writing was conducted by O.R., with review and editing by P.T. and J.F.M. Funding acquisition was undertaken by O.R. and P.T. All authors have read and agreed to the published version of the manuscript.
This research was funded by The William Templeton Foundation for Young People’s Mental Health, Cambridge Philosophical Society, and the Aviva Foundation.
Conflicts of Interest
The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.

- Latest news
- UCL in the media
- Services for media
- Student news
- Tell us your story

Analysis: Depression is probably not caused by a chemical imbalance in the brain – new study
20 July 2022
Writing in The Conversation, Professor Joanna Moncrieff and Dr Mark Horowitz (both UCL Psychiatry) report on their new research showing no clear evidence that serotonin levels or serotonin activity are responsible for depression.

For three decades, people have been deluged with information suggesting that depression is caused by a “chemical imbalance” in the brain – namely an imbalance of a brain chemical called serotonin. However, our latest research review shows that the evidence does not support it.
Although first proposed in the 1960s, the serotonin theory of depression started to be widely promoted by the pharmaceutical industry in the 1990s in association with its efforts to market a new range of antidepressants, known as selective serotonin-reuptake inhibitors or SSRIs. The idea was also endorsed by official institutions such as the American Psychiatric Association, which still tells the public that “differences in certain chemicals in the brain may contribute to symptoms of depression”.
Countless doctors have repeated the message all over the world, in their private surgeries and in the media. People accepted what they were told. And many started taking antidepressants because they believed they had something wrong with their brain that required an antidepressant to put right. In the period of this marketing push, antidepressant use climbed dramatically, and they are now prescribed to one in six of the adult population in England, for example.
For a long time, certain academics, including some leading psychiatrists, have suggested that there is no satisfactory evidence to support the idea that depression is a result of abnormally low or inactive serotonin. Others continue to endorse the theory. Until now, however, there has been no comprehensive review of the research on serotonin and depression that could enable firm conclusions either way.
At first sight, the fact that SSRI-type antidepressants act on the serotonin system appears to support the serotonin theory of depression. SSRIs temporarily increase the availability of serotonin in the brain, but this does not necessarily imply that depression is caused by the opposite of this effect.
There are other explanations for antidepressants’ effects. In fact, drug trials show that antidepressants are barely distinguishable from a placebo (dummy pill) when it comes to treating depression. Also, antidepressants appear to have a generalised emotion-numbing effect which may influence people’s moods, although we do not know how this effect is produced or much about it.
There has been extensive research on the serotonin system since the 1990s, but it has not been collected systematically before. We conducted an “umbrella” review that involved systematically identifying and collating existing overviews of the evidence from each of the main areas of research into serotonin and depression. Although there have been systematic reviews of individual areas in the past, none have combined the evidence from all the different areas taking this approach.
One area of research we included was research comparing levels of serotonin and its breakdown products in the blood or brain fluid. Overall, this research did not show a difference between people with depression and those without depression.
Another area of research has focused on serotonin receptors, which are proteins on the ends of the nerves that serotonin links up with and which can transmit or inhibit serotonin’s effects. Research on the most commonly investigated serotonin receptor suggested either no difference between people with depression and people without depression, or that serotonin activity was actually increased in people with depression – the opposite of the serotonin theory’s prediction.
Research on the serotonin “transporter”, that is the protein which helps to terminate the effect of serotonin (this is the protein that SSRIs act on), also suggested that, if anything, there was increased serotonin activity in people with depression. However, these findings may be explained by the fact that many participants in these studies had used or were currently using antidepressants.
We also looked at research that explored whether depression can be induced in volunteers by artificially lowering levels of serotonin. Two systematic reviews from 2006 and 2007 and a sample of the ten most recent studies (at the time the current research was conducted) found that lowering serotonin did not produce depression in hundreds of healthy volunteers. One of the reviews showed very weak evidence of an effect in a small subgroup of people with a family history of depression, but this only involved 75 participants.
Very large studies involving tens of thousands of patients looked at gene variation, including the gene that has the instructions for making the serotonin transporter. They found no difference in the frequency of varieties of this gene between people with depression and healthy controls.
Although a famous early study found a relationship between the serotonin transporter gene and stressful life events, larger, more comprehensive studies suggest no such relationship exists. Stressful life events in themselves, however, exerted a strong effect on people’s subsequent risk of developing depression.
Some of the studies in our overview that included people who were taking or had previously taken antidepressants showed evidence that antidepressants may actually lower the concentration or activity of serotonin.
The serotonin theory of depression has been one of the most influential and extensively researched biological theories of the origins of depression. Our study shows that this view is not supported by scientific evidence. It also calls into question the basis for the use of antidepressants.
Most antidepressants now in use are presumed to act via their effects on serotonin. Some also affect the brain chemical noradrenaline. But experts agree that the evidence for the involvement of noradrenaline in depression is weaker than that for serotonin.
There is no other accepted pharmacological mechanism for how antidepressants might affect depression. If antidepressants exert their effects as placebos, or by numbing emotions, then it is not clear that they do more good than harm.
Although viewing depression as a biological disorder may seem like it would reduce stigma, in fact, research has shown the opposite, and also that people who believe their own depression is due to a chemical imbalance are more pessimistic about their chances of recovery.
It is important that people know that the idea that depression results from a “chemical imbalance” is hypothetical. And we do not understand what temporarily elevating serotonin or other biochemical changes produced by antidepressants do to the brain. We conclude that it is impossible to say that taking SSRI antidepressants is worthwhile, or even completely safe. People need all this information to make informed decisions about whether or not to take antidepressants.
This article originally appeared in The Conversation on 20 July 2022.
- Article in The Conversation
- Article in The Conversation (Spanish)
- Professor Joanna Moncrieff's academic profile
- Dr Mark Horowitz's academic profile
- UCL Division of Psychiatry
- UCL Faculty of Brain Sciences
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2023 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
What's the Latest in Depression Treatment?
Theodora Blanchfield is an Associate Marriage and Family Therapist and mental health writer using her experiences to help others. She holds a master's degree in clinical psychology from Antioch University and is a board member of Still I Run, a non-profit for runners raising mental health awareness. Theodora has been published on sites including Women's Health, Bustle, Healthline, and more and quoted in sites including the New York Times, Shape, and Marie Claire.
:max_bytes(150000):strip_icc():format(webp)/theodorablanchfieldamft-50c6fe570e584649b5dbc17eb08b5bbf.jpg)
Steven Gans, MD is board-certified in psychiatry and is an active supervisor, teacher, and mentor at Massachusetts General Hospital.
:max_bytes(150000):strip_icc():format(webp)/steven-gans-1000-51582b7f23b6462f8713961deb74959f.jpg)
Psychedelics and Ketamine
- Other Fast-Acting Treatments
- What's on the Horizon
If it’s felt to you like we’re at an inflection point with mental health, you’re not wrong.
Depression rates, which were already on the rise before the pandemic, appear to be higher than ever. One estimate from the World Health Organization (WHO) puts the global increase of people diagnosed with major depressive disorder (MDD) at a more than 25% rate from 2019 to 2020—and this doesn’t even include people who reported feelings of depression but didn’t meet the full criteria for a diagnosis.
Though actual suicide rates were steady or even down in some countries, the same WHO report estimates that in the US, the incidence of suicidal thoughts went up from about 18% to around 30% in 2020 during pandemic stay-at-home orders.
The good news: there’s currently more innovation in mental health treatment than there’s been since the 1980s when selective serotonin uptake inhibitors (SSRIs) were originally introduced. Many of these new treatments work more quickly than those SSRIs, which can sometimes take up to four to six weeks to work.
“It’s a time of hope for many people who haven’t been helped by current treatments,” says Jeffrey Borenstein, MD , who serves as President & CEO of the Brain & Behavior Research Foundation, which funds mental health research grants.
10% of Americans will have multiple depressive episodes in their lives—but nearly half of those people have treatment-resistant depression . This means an estimated 16 million Americans will try one or more treatments for depression without achieving remission.
With this combination of factors, it’s more crucial than ever to find treatments that are effective and work quickly. Read on to learn more about the new depression treatments that are currently being used, ones that are being researched, and where future research might lead.
It’s a time of hope for many people who haven’t been helped by current treatments.
History of Depression Treatment
In order to understand current and future depression treatment, it’s important to know where we’ve come from to get to where we are today—and some of the conventional wisdom we may be in the process of overturning.
The Monoamine Hypothesis
The first antidepressant, Ipronizaid, was discovered by accident when it was given to patients with tuberculosis. The patients showed a marked improvement in mood. This monoamine oxidase inhibitor (MAOI) works by preventing the body’s monoamine oxidase enzyme from breaking down dopamine , serotonin , and norepinephrine in the brain.
These three neurotransmitters, collectively known as monoamines because of their similar chemical structures, are responsible for key processes in the brain including learning, emotion, and memory.
The idea that the depletion of these neurotransmitters is what leads to depression is known as the monoamine hypothesis. Tricyclic antidepressants and SSRIs have also been thought to have their impact based on this theory.
The Development of TCAs and SSRIs
Tricyclic antidepressants (TCAs) were developed following the introduction of MAOIs in the 1950s. They work by inhibiting the absorption of serotonin and norepinephrine, and blocking acetylcholine, another neurotransmitter.
With the development of MAOIs and TCAs in the 1950s and 1960s, there was a significant lack of research on other types of antidepressants—until Prozac (fluoxetine) was introduced in 1987.
This was the first SSRI—that is, the first antidepressant to work exclusively on blocking the reabsorption of serotonin. Increasing serotonin levels is thought to regulate mood. Additionally, SSRIs carry far fewer side effects than the earlier MAOIs/TCAs—though they are not without side effects.
Even newer classes of antidepressants, such as selective serotonin-norepinephrine reuptake inhibitors (SNRIs) and atypical antidepressants, still were thought to work based on the monoamine hypothesis.
Newer theories believe that the monoamine hypothesis of low levels of dopamine, serotonin, and norepinephrine "causing" depression, and depression being "cured" by increasing these neurotransmitters, oversimplifies the complexity of the neurochemistry of depression.
The Neuroplasticity Hypothesis
More modern theories look at the role of stress in depression and at the neuroplasticity hypothesis. Stress is linked to both an increased risk of major depressive episodes and treatment resistance .
It is thought that chronic stress leads to dysregulation in the hypothalmic-pituitary-adrenocortical (HPA) axis, which controls reactions to stress as well as mood and emotion, among other things. This dysregulation causes impairment in the hippocampus, which controls memory and emotion.
This leads to the neuroplasticity hypothesis of depression. Put simply, neuroplasticity is the brain’s ability to adapt and change to signals both within and outside of the body.
Those with depression show significantly lower levels of neuroplasticity and a decreased ability to adapt to stress.
Looking at depression through the neuroplasticity theory broadens the focus from how a medication might affect someone’s brain from looking beyond just levels of neurotransmitters to looking at how well the neurons are communicating with each other at various parts of the process to create neuroplasticity.
BDNF and Glutamate May Be the Future of Depression Treatment
This neuroplasticity theory involves other systems and chemicals within the brain, and two major areas that are receiving particular focus right now in depression treatment are brain-derived neurotrophic factor (BDNF) and glutamate.
BDNF is a chemical in the brain that is associated with cell growth and cell death, and it is thought that lower levels of BDNF lead to lower levels of neuroplasticity, so it is an area that is receiving attention in development of depression treatment.
Glutamate is an “excitatory” neurotransmitter , meaning it is a messenger that stimulates nerve cells to be ready to receive information. It also helps nerve cells better communicate with each other.
It’s being looked at in depression treatment because optimal glutamate functioning may help facilitate, increasing neuroplasticity, so targeting the glutamate system via new treatments such as ketamine or psychedelics may help symptoms.
Timeline of Depression Research History
- 1958: The first antidepressants, Iproniazid (MAOI) and Imipramamine (TCA)
- 1961 MAOIs: Nardil and Partite
- 1961-1980: tricyclic antidepressants—Elavil, Norpramin, Sinequan, Vivactil, Pamelor, Surmontil, Ludiomil
- 1987: Prozac, the first SSRI
- 1991-1998: SSRIs Zoloft, Paxil, Celexa; SNRIs Effexor and Serzone
Psychedelics are currently having a moment in both scientific circles and mainstream media due to their potential for rapid, significant, and long-lasting reduction in symptoms of depression.
A 2016 study of cancer patients found that just a single treatment of psilocybin (magic mushrooms) led to immediate reduction in measures of depression that were then seen to last up to six months, with nearly 80% of study participants still reporting antidepressant effect. Even in a follow-up study five years later, a majority of the study subjects still reported reduced symptoms of depression.
It’s believed that a combination of the drug's biological effects on the brain as well as the spiritual and mystical experience contribute to the high levels of effectiveness. The experience may give people relief from more existential aspects of depression.
With that said, it so far has only been studied in very controlled clinical environments so it’s not yet known how it might work in the “real world,” and a solid framework has not yet been established on how to do this safely. Despite this, the state of Oregon and the cities of Santa Cruz and Oakland, California, among other locale, have decriminalized the use of psilocybin for therapeutic use.
Already, venture capital has been flowing into the psilocybin “market,” with investors eager to capitalize on the promise of its healing powers before it has even been widely legalized or approved by the FDA for treatment of depression. It is estimated that by 2027, psychedelics will be a multibillion dollar industry.
Psilocybin has already been granted FDA Breakthrough Therapy designation , which means that drugs which show a significant amount of improvement over traditional therapies in treating serious illnesses can be reviewed and approved on an expedited timeline.
However, some safety concerns do exist. In addition to physical side effects, some patients experienced an increase in suicidal behaviors and ideations. Research is also being done on how to remove the hallucinogenic properties of these drugs.
MDMA, also known as ecstasy or Molly in its street forms, has also been granted FDA “breakthrough therapy” status after Phase 2 clinical trials where a whopping 67% of people in the trial—who entered with severe PTSD—no longer qualified for a PTSD diagnosis.
Although clinical research for MDMA for depression has not gotten as far as MDMA for PTSD, MDMA does show promise for treating major depressive disorder—and more than 50% of adults who have a diagnosis of PTSD also have a diagnosis of MDD.
MDMA works by rapidly releasing and increasing levels of serotonin and dopamine in the brain.
MDMA, it is theorized, is so helpful in PTSD because it helps people recall negative memories with the brain's fear response being better regulated. This may lead to greater self-compassion and stay with these memories safely in therapy without getting overwhelmed.
Of all of the “psychedelic” treatments out there, ketamine is currently the only one that is legal for treatment in all 50 states. (Experts cannot agree on whether it is a true psychedelic or not, though it does cause dissociative effects.)
Ketamine was first synthesized in the 1960s as an anesthetic and early observations showed that ketamine might work similarly to antidepressants. It wasn’t until the 1990s that ketamine would be studied in earnest to treat depression, with the first randomized controlled study showing promise of ketamine as an antidepressant being released in 2000.
Spravato (esketamine) was approved in 2019 via Fast Track status with the FDA, and it is currently administered as a nose spray that must be consumed under the monitoring of a doctor for safety reasons.
Esketamine specifies a particular type of ketamine molecule that is thought to be more potent at the NMDA glutamate receptor. IV ketamine uses a different part of the molecule and is currently used off-label for depression. It has demonstrated a more significant overall response rate than intranasal ketamine, but is more complicated to use.
Ketamine has received such wide attention for several reasons: first of all, it targets a completely different set of neurotransmitters in the brain than previously studied depression treatments and often begins working within hours. It also may quickly reduce suicidal ideation in some cases.
As other treatments target the monoamine system (see above), ketamine is thought to create a surge of glutamate neurotransmission in the brain.
The fact that ketamine can work so quickly on refractory depression has the potential to be a game changer for depression.
However, more research is needed to figure out how to optimally use this agent, as well as to develop agents like ketamine that don't carry the dissociative side effects and are potentially easier and safer for wide use.
Although ketamine is generally well-tolerated, it does have a number of side effects at the time of administration, such as nausea, dizziness, feeling woozy, spacey, numb, and having sensory distortions—though these side effects typically subside quickly.
Arketamine, which uses a different part of the molecule, is currently being studied as well, as it lasts longer and has fewer side effects, including less dissociative side effects. The FDA has given approval for investigational new drug clearance to study how it will work with other medications.
Other Fast-Acting Treatments
Beyond the psychedelic space, there are several other new depression treatments that are rapid-acting, including a new protocol for TMS therapy as well as a new oral antidepressant.
“The fact that there’s these new treatments [and] that [they can] work so rapidly is something we very much need,” says Borenstein. “One of the benefits is that they’re rapidly acting to treat suicidal acts and risk, and that has the potential to be a game changer in psychiatry."
One of these treatments is the oral antidepressant Auvelity , approved by the FDA in August 2022. Auvelity may work within a week and targets the glutamate system, similarly to ketamine.
The medication is a combination of buproprion (the active ingredient in Wellbutrin) and dextromethorphan (commonly found in cough syrup). Its approval may open the door for a new class of medications that work to increase glutamate.
Although transcranial magnetic stimulation (TMS) was first approved by the FDA in 2008, newer versions of the TMS protocol are found to bring results in less than a week, compared to six weeks in the older version of the protocol.
TMS therapy involves using magnetic pulses on the head to treat depression. The pulses are targeted to the area of the brain implicated in depression and they work to activate these regions. One of the major areas stimulated is the prefrontal cortex, an area of the brain associated with regulating mood.
According to some research, it has been shown to benefit somewhere between 50-60% of those who have not adequately responded to one or more antidepressant treatments.
Typically, TMS treatment takes six weeks of once-daily sessions, a major time commitment. With this Stanford accelerated intelligent neuromodulation therapy (SAINT) protocol, developed at Stanford, people receive 10 treatments per day for five days.
Moreover, according to the Stanford study, nearly 80% of people no longer met criteria for depression, meaning their symptoms were back in the “normal” range. In the “regular” treatment, only about half the people treated improve, with only a third meeting “remission.”
“The patients had remission of depression after a few days, which is tremendous,” says Borenstein.
One of the theories behind SAINT is that people who weren’t receiving a high enough frequency and density of stimulation.
Some key differences in the SAINT protocol:
- treating people multiple sessions per day with optimally spaced intervals
- applying higher levels of stimulation (1800 pulses vs 600)
- precision targeting through FMRI scans that helped the researchers find the precise location in each participants brain where the stimulation would occur
The protocol was approved in September 2022 and is expected to launch in 2023.
What's on the Horizon
In Borenstein’s role helming the Brain & Behavior Research Foundation, he has a birds-eye view of innovation going on in mental health research, as the foundation is the nation’s largest private funder of mental health grants.
A few other possible treatment areas he’s excited about:
Optogenetics : This is a way to use light and genetic tools to control the activity of certain neurons. These techniques have been used to map connections in the brain, but there is hope that someday this technique with be able to positively impact specific cellular pathways in depression.
Stem Cells: A theory is currently being studied that stem cells may decrease depression by helping create more neurons that can form more connections in the brain. Current research includes investigating if there are new molecules that can activate stem cells to act in this antidepressant way.
World Health Organization. Mental Health and COVID-19: Early evidence of the pandemic’s impact: Scientific brief.
Barchas JD, Altemus M. Monoamine hypotheses of mood disorders . Basic Neurochemistry: Molecular, Cellular and Medical Aspects 6th edition .
Varghese FP, Brown ES. The Hypothalamic-Pituitary-Adrenal Axis in Major Depressive Disorder: A Brief Primer for Primary Care Physicians . Prim Care Companion J Clin Psychiatry . 2001;3(4):151-155. doi:10.4088/pcc.v03n0401
Filatova EV, Shadrina MI, Slominsky PA. Major depression: one brain, one disease, one set of intertwined processes . Cells. 2021;10(6):1283. doi:10.3390/cells10061283
Ross S, Bossis A, Guss J, et al. Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: a randomized controlled trial . J Psychopharmacol. 2016;30(12):1165-1180. doi:10.1177/0269881116675512
Agin-Liebes GI, Malone T, Yalch MM, et al. Long-term follow-up of psilocybin-assisted psychotherapy for psychiatric and existential distress in patients with life-threatening cance r. J Psychopharmacol. 2020;34(2):155-166. doi:10.1177/0269881119897615
Ross S, Bossis A, Guss J, et al. Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: a randomized controlled tria l. J Psychopharmacol. 2016;30(12):1165-1180. doi: 10.1177/0269881116675512
Psilocybin treatment for major depression effective for up to a year for most patients, study shows . Johns Hopkins Medicine Newsroom.
COMPASS Pathways announces positive topline results from groundbreaking phase IIb trial of investigational COMP360 psilocybin therapy for treatment-resistant depression | Compass Pathways.
Remmel A. Psychedelic drugs without the trip? This sensor could help seek them out. Nature. doi:10.1038/d41586-021-01156-y
Mitchell JM, Bogenschutz M, Lilienstein A, et al. MDMA-assisted therapy for severe PTSD: a randomized, double-blind, placebo-controlled phase 3 study. Nat Med. 2021;27(6):1025-1033. doi: 10.1038/s41591-021-01336-3
Inouye A, Wolfgang A. 3,4-methylenedioxymethamphetamine (Mdma)-assisted therapy in hawaii: a brief review. Cureus. 14(6):e26402. doi: 10.7759/cureus.26402
Sofia RD, Harakal JJ. Evaluation of ketamine HCl for anti-depressant activity . Arch Int Pharmacodyn Ther. 1975;214(1):68-74.
Berman RM, Cappiello A, Anand A, et al. Antidepressant effects of ketamine in depressed patients . Biological Psychiatry. 2000;47(4):351-354. DOI: 10.1016/s0006-3223(99)00230-9
Abbar M, Demattei C, El-Hage W, et al. Ketamine for the acute treatment of severe suicidal ideation: double blind, randomised placebo controlled trial . BMJ. 2022;376. DOI: 10.1136/bmj-2021-067194
Wei Y, Chang L, Hashimoto K. Molecular mechanisms underlying the antidepressant actions of arketamine: beyond the NMDA receptor . Mol Psychiatry. 2022;27(1):559-573. DOI: 10.1038/s41380-021-01121-1
MD APS. Transcranial magnetic stimulation (Tms): Hope for stubborn depression . Harvard Health.
Cole EJ, Stimpson KH, Bentzley BS, et al. Stanford accelerated intelligent neuromodulation therapy for treatment-resistant depression . AJP. 2020;177(8):716-726.
Optogenetics: A revolutionary approach for the study of depression . Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2021;106:110094. DOI: 10.1016/j.pnpbp.2020.110094
F; MLCMDAGT. Depression and adult neurogenesis: Positive effects of the antidepressant fluoxetine and of physical exercise. Brain research bulletin. DOI: 10.1016/j.brainresbull.2018.09.002
By Theodora Blanchfield, AMFT Theodora Blanchfield is an Associate Marriage and Family Therapist and mental health writer using her experiences to help others. She holds a master's degree in clinical psychology from Antioch University and is a board member of Still I Run, a non-profit for runners raising mental health awareness. Theodora has been published on sites including Women's Health, Bustle, Healthline, and more and quoted in sites including the New York Times, Shape, and Marie Claire.
Articles on Depression
Displaying 1 - 20 of 735 articles.

Young people are getting unhappier – a lack of childhood freedom and independence may be partly to blame
Fiorentina Sterkaj , University of East London
Rich people, bribes and depression – study finds link between corruption and mental health among Ghanaian students
Stephen Baffour Adjei ; Frederick Anyan , Norwegian University of Science and Technology ; Johnny Andoh-Arthur , University of Ghana , and Sylvia Charity Akotia , University of Ghana
Measuring emotional ‘emptiness’ could help manage this potentially life-threatening experience
Shona Joyce Herron , UCL

Elon Musk says ketamine can get you out of a ‘negative frame of mind’. What does the research say?
Julaine Allan , Charles Sturt University

Half of Australians in aged care have depression. Psychological therapy could help
Tanya Davison , Swinburne University of Technology and Sunil Bhar , Swinburne University of Technology


Running or yoga can help beat depression, research shows – even if exercise is the last thing you feel like
Michael Noetel , The University of Queensland

Why are so many Australians taking antidepressants?
Jon Jureidini , University of Adelaide

Women take more antidepressants after divorce than men but that doesn’t mean they’re more depressed
Raquel Peel , RMIT University

Millions of Australians have a chronic illness. So why aren’t employers accommodating them?
Peter Ghin , The University of Melbourne and Susan Ainsworth , The University of Melbourne

Van Gogh’s final months were his most productive
Frances Fowle , The University of Edinburgh

Why you may feel depressed and anxious when you’re ill – and how to cope with it
Julie Lasselin , Stockholm University

I research the therapeutic qualities of writing about art – here are three steps for trying it yourself
Patrick Wright , The Open University

Stressed out? Why mindfulness and meditation help us cope with the world
Lucy Draper-Clarke , University of the Witwatersrand

The Douglas-Bell Canada Brain Bank: a goldmine for research on brain diseases
Naguib Mechawar , McGill University

For many who are suffering with prolonged grief, the holidays can be a time to reflect and find meaning in loss
Mandy Doria , University of Colorado Anschutz Medical Campus

Matthew Perry died of ‘acute effects of ketamine’ – what you need to know about the drug
Philip Crilly , Kingston University

Is it OK to take antidepressants while pregnant?
Alka Kothari , The University of Queensland
Hope brings happiness, builds grit and gives life meaning. Here’s how to cultivate it
Tharina Guse , University of Pretoria

AI can already diagnose depression better than a doctor and tell you which treatment is best
Sarah Hellewell , Curtin University

Could visiting a museum be the secret to a healthy life?
Emma Dupuy , Université de Montréal
Related Topics
- Antidepressants
- Coronavirus
- Mental health
- Mental illness
Top contributors
Professor of Psychiatry, Monash University
Professor and Personal Chair, Swansea University
Associate Professor of Psychiatry, Wayne State University
Professor of Psychology, San Diego State University
Scientia Professor, UNSW Sydney
Professor of Clinical Neuropsychology, University of Cambridge
Director School of Medicine and Psychology, Australian National University
Professor of Health Sciences, Simon Fraser University
Head of the Department of Psychiatry, The University of Melbourne
Honorary Clinical Research Fellow in Psychiatry, UCL
Professor of Psychiatry, UNSW & Black Dog Institute, UNSW Sydney
Professor of Critical and Social Psychiatry, UCL
Clinical Psychologist and Professor in the Department of Psychology and Neuroscience, Dalhousie University
Associate Professor of Family Medicine, Charles R. Drew University of Medicine and Science
Postdoctoral Research Associate, Cognitive Neuroscience, University of Cambridge
- X (Twitter)
- Unfollow topic Follow topic

Depression and Serotonin: What the New Review Actually Says
Using but not overusing the evidence presented in this controversial study..
Posted July 26, 2022 | Reviewed by Abigail Fagan
- What Is Depression?
- Find a therapist to overcome depression
- A new published review finds no evidence that low serotonin levels cause depression.
- The authors use their data to refute the "chemical imbalance" hypothesis of depression, which is an old and imprecise term.
- Despite the claims of some, the study does not disprove that biological factors are irrelevant to depression.
- The dominant model of depression for decades has been one that recognizes the importance of biological, psychological, and social factors.
Some quite strong feelings and very broad conclusions have come following the recent publication of a review study published in the reputable journal Molecular Psychiatry that found little evidence that low levels of the brain neurotransmitter serotonin are related to the development of depression . The study has received strong media coverage and has spurred intense exchanges on social media . Some see the study as a scientific earthquake and total vindication for those who have been skeptical of the “biological” theory of depression from the start, while others view it as the penultimate dead horse beating that has absolutely no bearing on current practices for understanding or treating depression, now the world’s #1 cause for disability.
The study is what is called an “umbrella” review, which means that no new data are presented and the authors are reviewing and summarizing studies that themselves reviewed and summarized individual research studies. They focus on studies that have used various lines of investigation to link depression with low serotonin levels. This includes research (in people only) that compare levels of serotonin in the blood or cerebrospinal fluid between people who are depressed and not-depressed, studies of how well certain protein receptors are able to bind serotonin when depressed, and studies examining the role of a single but very famous gene , the serotonin transporter. The bottom line is that they find little to no evidence from the types of studies they examined that low serotonin levels or activity play a significant role in the development of depression.
These kinds of studies often put people to sleep, but in this case the reaction has been intense and personal. Much of this has to do with the authors pulling in the term “chemical imbalance” as implications of their work. This poorly-chosen term is actually one of psychiatry’s creation and now it’s being thrown back in our face imbued with even broader meaning.
While originally employed as a shortcut term for the monoamine hypothesis (briefly, the idea that some kind of deficiency in a few brain neurotransmitters, including serotonin, was a key contributor to depression), it was quickly incorporated by the pharmaceutical industry as a catch phrase for marketing purposes to depict depression as a biological illness requiring biological treatments.
The monoamine hypothesis faded as a dominant model with further research and was supplanted decades ago by the “biopsychosocial” model of psychiatric disorders which continues to prevail today. Nevertheless, the old chemical imbalance lingo remains a lightening rod to critics of psychiatry. More recently, the term has begun to be the punching bag for people who don’t believe that biological factors (also a squishy term) of any sort play a role in causing depression.
Unfortunately, the current review makes little distinction between the narrower serotonin deficit theory of depression they actually address and this ever expanding but still ill-defined “chemical imbalance” view of mental illness. This has predictably pushed the door wide open for those who want to take this review as proof that neurobiology doesn’t matter at all when it comes to depression, a claim which isn’t supported by this review or wider research whatsoever.
There is some middle ground here. While many of us in psychiatry are a little embarrassed by what now looks like some over simplistic and naïve ideas about the development of depression, there’s no denying that many of these individual studies supporting a straightforward role of serotonin and depression created quite a lot of enthusiasm in their day among the psychiatric community when first published.
These notions were then imparted to students and patients in an attempt to explain what depression was. I remember some of my own Powerpoint slides I previously used in teaching related to a very influential study that the onset of depression was related to the combination of having a particular version of the serotonin transporter gene combined with the presence of an adverse environment. There’s also no denying that selected studies supporting serotonin’s role were heavily leveraged by the pharmaceutical industry to market more antidepressants . For most of us, however, the attractiveness of these simple theories wasn’t in their advertising value but in their ability to help patients see their struggles as something that wasn’t their fault at a time when feelings of guilt and worthlessness were already sky high. Overall, then, this study is an uncomfortable reminder that we did indeed learn and repeat ideas that today look a little foolish.
At the same time, it is important not to let people take this extremely limited study to wild and sweeping conclusions and to prevent the portrayal of the psychiatric community in archaic and stereotypical forms. Depression experts have well moved on from the low serotonin theory years if not decades ago, and although they could have announced this shift better, there certainly is no organized effort to suppress this information. Over two years ago I published a post here on Psychology Today called The Rise and Fall of the Depression Gene which cited some of the same research as this review. Personally, I don’t think I’ve used the term “chemical imbalance” to explain depression in 20 years and current textbooks and information sources provide much more nuance and balance (and vagueness) when describing the origin of depression. Yes, you can still hear people occasionally drop the chemical imbalance term when trying to turn complicated processes into quick soundbites, but that’s a long way from it being an organized and accepted theory promoted by the proverbial psychiatry establishment.

The review also has a number of real problems, which is a little ironic for a study which is one of the few not to have a “limitations” section as part of the manuscript. I’ll blame the editorial staff of the journal for that one, as well as for letting the authors use studies that examine simple depression versus controls differences in serotonin levels to conclude that serotonin, let alone all biological factors, have no role in depression at all.
Reading this study, one would never know that there are animal studies, neuroimaging studies, twin and adoption studies, inflammation research, and many other lines of evidence suggesting that depression is a very complex condition that people can arrive at from multiple pathways. Interestingly, if you look directly at some of the source studies for this review, you will see some of this evidence. For example, the meta-analysis by Ogawa cited in the review did indeed find no evidence of a link between serotonin and depression but did find evidence of a link between dopamine and depression. This statement should not be interpreted as a pitch to trade one overly simplistic view of depression for another but to point out the hazards of making conclusions that far overstep your data.
Another poor choice in this review is that while the authors don’t quite tell readers to stop taking antidepressants, they walk right up to that edge with their claim that the old chemical imbalance theory is one of the primary justifications for why people take them (rather than something like wanting to feel better). This, in my view, is careless and problematic for people who take antidepressants and for those who care for them. Just as many rightly point out that the fact that antidepressants' help shouldn’t be used as evidence of a serotonin deficit in depression, the lack of a clear serotonin deficit in depression shouldn’t be used as evidence to abandon the use of these important medications, any more than (as been said previously) a lack of an “acetaminophen deficit” should be used as evidence not to use Tylenol when you have a headache. Admittedly, we don’t know very well how antidepressants work, but for millions of people, they do.
In the end, it seems best to welcome this study for what it does say while being quite clear about what it doesn’t. Depression is complicated. Different people get there from different paths and find their way out through different means. Ascribing all depression as due to low serotonin, or poor diet , or trauma , or smartphones, or poverty will just end with a study like this.
Moncrieff J, Cooper RE, Stockmann T, et al. The serotonin theory of depression: A systematic umbrella review of the evidence. Mol Psychiatry. 2022; Jul 20. doi: 10.1038/s41380-022-01661-0. Online ahead of print.
Ogawa S, Tsuchimine S, Kunugi H. Cerebrospinal fluid monoamine metabolite concentrations in depressive disorder: A meta-analysis of historic evidence. J Psychiatr Res. 2018; 105:137–46.

David Rettew, M.D. , is a child and adolescent psychiatrist and faculty at the Oregon Health and Science University.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Teletherapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Health Topics
- Brochures and Fact Sheets
- Help for Mental Illnesses
- Clinical Trials
What is depression?
Depression (also known as major depression, major depressive disorder, or clinical depression) is a common but serious mood disorder. It causes severe symptoms that affect how a person feels, thinks, and handles daily activities, such as sleeping, eating, or working.
To be diagnosed with depression, the symptoms must be present for at least 2 weeks.
There are different types of depression, some of which develop due to specific circumstances.
- Major depression includes symptoms of depressed mood or loss of interest, most of the time for at least 2 weeks, that interfere with daily activities.
- Persistent depressive disorder (also called dysthymia or dysthymic disorder) consists of less severe symptoms of depression that last much longer, usually for at least 2 years.
- Perinatal depression is depression that occurs during pregnancy or after childbirth. Depression that begins during pregnancy is prenatal depression, and depression that begins after the baby is born is postpartum depression.
- Seasonal affective disorder is depression that comes and goes with the seasons, with symptoms typically starting in the late fall or early winter and going away during the spring and summer.
- Depression with symptoms of psychosis is a severe form of depression in which a person experiences psychosis symptoms, such as delusions (disturbing, false fixed beliefs) or hallucinations (hearing or seeing things others do not hear or see).
People with bipolar disorder (formerly called manic depression or manic-depressive illness) also experience depressive episodes, during which they feel sad, indifferent, or hopeless, combined with a very low activity level. But a person with bipolar disorder also experiences manic (or less severe hypomanic) episodes, or unusually elevated moods, in which they might feel very happy, irritable, or “up,” with a marked increase in activity level.
Other depressive disorders found in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5-TR) include disruptive mood dysregulation disorder (diagnosed in children and adolescents) and premenstrual dysphoric disorder (that affects women around the time of their period).
Who gets depression?
Depression can affect people of all ages, races, ethnicities, and genders.
Women are diagnosed with depression more often than men, but men can also be depressed. Because men may be less likely to recognize, talk about, and seek help for their feelings or emotional problems, they are at greater risk of their depression symptoms being undiagnosed or undertreated.
Studies also show higher rates of depression and an increased risk for the disorder among members of the LGBTQI+ community.
What are the signs and symptoms of depression?
If you have been experiencing some of the following signs and symptoms, most of the day, nearly every day, for at least 2 weeks, you may have depression:
- Persistent sad, anxious, or “empty” mood
- Feelings of hopelessness or pessimism
- Feelings of irritability, frustration, or restlessness
- Feelings of guilt, worthlessness, or helplessness
- Loss of interest or pleasure in hobbies and activities
- Fatigue, lack of energy, or feeling slowed down
- Difficulty concentrating, remembering, or making decisions
- Difficulty sleeping, waking too early in the morning, or oversleeping
- Changes in appetite or unplanned weight changes
- Physical aches or pains, headaches, cramps, or digestive problems without a clear physical cause that do not go away with treatment
- Thoughts of death or suicide or suicide attempts
Not everyone who is depressed experiences all these symptoms. Some people experience only a few symptoms, while others experience many. Symptoms associated with depression interfere with day-to-day functioning and cause significant distress for the person experiencing them.
Depression can also involve other changes in mood or behavior that include:
- Increased anger or irritability
- Feeling restless or on edge
- Becoming withdrawn, negative, or detached
- Increased engagement in high-risk activities
- Greater impulsivity
- Increased use of alcohol or drugs
- Isolating from family and friends
- Inability to meet the responsibilities of work and family or ignoring other important roles
- Problems with sexual desire and performance
Depression can look different in men and women. Although people of all genders can feel depressed, how they express those symptoms and the behaviors they use to cope with them may differ. For example, men (as well as women) may show symptoms other than sadness, instead seeming angry or irritable. And although increased use of alcohol or drugs can be a sign of depression in anyone, men are more likely to use these substances as a coping strategy.
In some cases, mental health symptoms appear as physical problems (for example, a racing heart, tightened chest, ongoing headaches, or digestive issues). Men are often more likely to see a health care provider about these physical symptoms than their emotional ones.
Because depression tends to make people think more negatively about themselves and the world, some people may also have thoughts of suicide or self-harm.
Several persistent symptoms, in addition to low mood, are required for a diagnosis of depression, but people with only a few symptoms may benefit from treatment. The severity and frequency of symptoms and how long they last will vary depending on the person, the illness, and the stage of the illness.
If you experience signs or symptoms of depression and they persist or do not go away, talk to a health care provider. If you see signs or symptoms of depression in someone you know, encourage them to seek help from a mental health professional.
If you or someone you know is struggling or having thoughts of suicide, call or text the 988 Suicide and Crisis Lifeline at 988 or chat at 988lifeline.org . In life-threatening situations, call 911 .
What are the risk factors for depression?
Depression is one of the most common mental disorders in the United States . Research suggests that genetic, biological, environmental, and psychological factors play a role in depression.
Risk factors for depression can include:
- Personal or family history of depression
- Major negative life changes, trauma, or stress
Depression can happen at any age, but it often begins in adulthood. Depression is now recognized as occurring in children and adolescents, although children may express more irritability or anxiety than sadness. Many chronic mood and anxiety disorders in adults begin as high levels of anxiety in childhood.
Depression, especially in midlife or older age, can co-occur with other serious medical illnesses, such as diabetes, cancer, heart disease, chronic pain, and Parkinson’s disease. These conditions are often worse when depression is present, and research suggests that people with depression and other medical illnesses tend to have more severe symptoms of both illnesses. The Centers for Disease Control and Prevention (CDC) has also recognized that having certain mental disorders, including depression and schizophrenia, can make people more likely to get severely ill from COVID-19.
Sometimes a physical health problem, such as thyroid disease, or medications taken for an illness cause side effects that contribute to depression. A health care provider experienced in treating these complicated illnesses can help determine the best treatment strategy.
How is depression treated?
Depression, even the most severe cases, can be treated. The earlier treatment begins, the more effective it is. Depression is usually treated with psychotherapy , medication , or a combination of the two.
Some people experience treatment-resistant depression, which occurs when a person does not get better after trying at least two antidepressant medications. If treatments like psychotherapy and medication do not reduce depressive symptoms or the need for rapid relief from symptoms is urgent, brain stimulation therapy may be an option to explore.
Quick tip : No two people are affected the same way by depression, and there is no "one-size-fits-all" treatment. Finding the treatment that works best for you may take trial and error.
Psychotherapies
Several types of psychotherapy (also called talk therapy or counseling) can help people with depression by teaching them new ways of thinking and behaving and helping them change habits that contribute to depression. Evidence-based approaches to treating depression include cognitive-behavioral therapy (CBT) and interpersonal therapy (IPT). Learn more about psychotherapy .
The growth of telehealth for mental health services , which offers an alternative to in-person therapy, has made it easier and more convenient for people to access care in some cases. For people who may have been hesitant to look for mental health care in the past, virtual mental health care might be an easier option.
Medications
Antidepressants are medications commonly used to treat depression. They work by changing how the brain produces or uses certain chemicals involved in mood or stress. You may need to try several different antidepressants before finding the one that improves your symptoms and has manageable side effects. A medication that has helped you or a close family member in the past will often be considered first.
Antidepressants take time—usually 4–8 weeks—to work, and problems with sleep, appetite, and concentration often improve before mood lifts. It is important to give a medication a chance to work before deciding whether it’s right for you. Learn more about mental health medications .
New medications, such as intranasal esketamine , can have rapidly acting antidepressant effects, especially for people with treatment-resistant depression. Esketamine is a medication approved by the U.S. Food and Drug Administration (FDA) for treatment-resistant depression. Delivered as a nasal spray in a doctor’s office, clinic, or hospital, it acts rapidly, typically within a couple of hours, to relieve depression symptoms. People who use esketamine will usually continue taking an oral antidepressant to maintain the improvement in their symptoms.
Another option for treatment-resistant depression is to take an antidepressant alongside a different type of medication that may make it more effective, such as an antipsychotic or anticonvulsant medication. Further research is needed to identify the role of these newer medications in routine practice.
If you begin taking an antidepressant, do not stop taking it without talking to a health care provider . Sometimes people taking antidepressants feel better and stop taking the medications on their own, and their depression symptoms return. When you and a health care provider have decided it is time to stop a medication, usually after a course of 9–12 months, the provider will help you slowly and safely decrease your dose. Abruptly stopping a medication can cause withdrawal symptoms.
Note : In some cases, children, teenagers, and young adults under 25 years may experience an increase in suicidal thoughts or behavior when taking antidepressants, especially in the first few weeks after starting or when the dose is changed. The FDA advises that patients of all ages taking antidepressants be watched closely, especially during the first few weeks of treatment.
If you are considering taking an antidepressant and are pregnant, planning to become pregnant, or breastfeeding, talk to a health care provider about any health risks to you or your unborn or nursing child and how to weigh those risks against the benefits of available treatment options.
To find the latest information about antidepressants, talk to a health care provider and visit the FDA website .
Brain stimulation therapies
If psychotherapy and medication do not reduce symptoms of depression, brain stimulation therapy may be an option to explore. There are now several types of brain stimulation therapy, some of which have been authorized by the FDA to treat depression. Other brain stimulation therapies are experimental and still being investigated for mental disorders like depression.
Although brain stimulation therapies are less frequently used than psychotherapy and medication, they can play an important role in treating mental disorders in people who do not respond to other treatments. These therapies are used for most mental disorders only after psychotherapy and medication have been tried and usually continue to be used alongside these treatments.
Brain stimulation therapies act by activating or inhibiting the brain with electricity. The electricity is given directly through electrodes implanted in the brain or indirectly through electrodes placed on the scalp. The electricity can also be induced by applying magnetic fields to the head.
The brain stimulation therapies with the largest bodies of evidence include:
- Electroconvulsive therapy (ECT)
- Repetitive transcranial magnetic stimulation (rTMS)
- Vagus nerve stimulation (VNS)
- Magnetic seizure therapy (MST)
- Deep brain stimulation (DBS)
ECT and rTMS are the most widely used brain stimulation therapies, with ECT having the longest history of use. The other therapies are newer and, in some cases, still considered experimental. Other brain stimulation therapies may also hold promise for treating specific mental disorders.
ECT, rTMS, and VNS have authorization from the FDA to treat severe, treatment-resistant depression. They can be effective for people who have not been able to feel better with other treatments; people for whom medications cannot be used safely; and in severe cases where a rapid response is needed, such as when a person is catatonic, suicidal, or malnourished.
Additional types of brain stimulation therapy are being investigated for treating depression and other mental disorders. Talk to a health care provider and make sure you understand the potential benefits and risks before undergoing brain stimulation therapy. Learn more about these brain stimulation therapies .
Natural products
The FDA has not approved any natural products for treating depression. Although research is ongoing and findings are inconsistent, some people use natural products, including vitamin D and the herbal dietary supplement St. John’s wort, for depression. However, these products can come with risks. For instance, dietary supplements and natural products can limit the effectiveness of some medications or interact in dangerous or even life-threatening ways with them.
Do not use vitamin D, St. John’s wort, or other dietary supplements or natural products without talking to a health care provider. Rigorous studies must be conducted to test whether these and other natural products are safe and effective.
Daily morning light therapy is a common treatment choice for people with seasonal affective disorder (SAD). Light therapy devices are much brighter than ordinary indoor lighting and considered safe, except for people with certain eye diseases or taking medications that increase sensitivity to sunlight. As with all interventions for depression, evaluation, treatment, and follow-up by a health care provider are strongly recommended. Research into the potential role of light therapy in treating non-seasonal depression is ongoing.
How can I find help for depression?
A primary care provider is a good place to start if you’re looking for help. They can refer you to a qualified mental health professional, such as a psychologist, psychiatrist, or clinical social worker, who can help you figure out next steps. Find tips for talking with a health care provider about your mental health.
You can learn more about getting help on the NIMH website. You can also learn about finding support and locating mental health services in your area on the Substance Abuse and Mental Health Services Administration (SAMHSA) website.
Once you enter treatment, you should gradually start to feel better. Here are some other things you can do outside of treatment that may help you or a loved one feel better:
- Try to get physical activity. Just 30 minutes a day of walking can boost your mood.
- Try to maintain a regular bedtime and wake-up time.
- Eat regular, healthy meals.
- Break up large tasks into small ones; do what you can as you can. Decide what must get done and what can wait.
- Try to connect with people. Talk with people you trust about how you are feeling.
- Delay making important decisions, such as getting married or divorced, or changing jobs until you feel better. Discuss decisions with people who know you well.
- Avoid using alcohol, nicotine, or drugs, including medications not prescribed for you.
How can I find a clinical trial for depression?
Clinical trials are research studies that look at new ways to prevent, detect, or treat diseases and conditions, including depression. The goal of a clinical trial is to determine if a new test or treatment works and is safe. Although people may benefit from being part of a clinical trial, they should know that the primary purpose is to gain new scientific knowledge so that others can be better helped in the future.
Researchers at NIMH and around the country conduct many studies with people with and without depression. We have new and better treatment options today because of what clinical trials have uncovered. Talk to a health care provider about clinical trials, their benefits and risks, and whether one is right for you.
To learn more or find a study, visit:
- Clinical Trials – Information for Participants : Information about clinical trials, why people might take part in a clinical trial, and what people might experience during a clinical trial
- Clinicaltrials.gov: Current Studies on Depression : List of clinical trials funded by the National Institutes of Health (NIH) being conducted across the country
- Join a Study: Depression—Adults : List of studies currently recruiting adults with depression being conducted on the NIH campus in Bethesda, MD
- Join a Study: Depression—Children : List of studies currently recruiting children with depression being conducted on the NIH campus in Bethesda, MD
- Join a Study: Perimenopause-Related Mood Disorders : List of studies on perimenopause-related mood disorders being conducted on the NIH campus in Bethesda, MD
- Join a Study: Postpartum Depression : List of studies on postpartum depression being conducted on the NIH campus in Bethesda, MD
Where can I learn more about depression?
Free brochures and shareable resources.
- Chronic Illness and Mental Health: Recognizing and Treating Depression : This brochure provides information about depression for people living with chronic illnesses, including children and adolescents. It discusses signs and symptoms, risk factors, and treatment options.
- Depression : This brochure provides information about depression, including different types of depression, signs and symptoms, how it is diagnosed, treatment options, and how to find help for yourself or a loved one.
- Depression in Women: 4 Things to Know : This fact sheet provides information about depression in women, including signs and symptoms, types of depression unique to women, and how to get help.
- Perinatal Depression : This brochure provides information about perinatal depression, including how it differs from “baby blues,” causes, signs and symptoms, treatment options, and how to find help for yourself or a loved one.
- Seasonal Affective Disorder : This fact sheet provides information about seasonal affective disorder, including signs and symptoms, how it is diagnosed, causes, and treatment options.
- Seasonal Affective Disorder (SAD): More Than the Winter Blues : This infographic provides information about how to recognize the symptoms of SAD and what to do to get help.
- Teen Depression: More Than Just Moodiness : This fact sheet is for teens and young adults and provides information about how to recognize the symptoms of depression and what to do to get help.
- Digital Shareables on Depression : These digital resources, including graphics and messages, can be used to spread the word about depression and help promote depression awareness and education in your community.
Federal resources
- Depression (MedlinePlus - also en español )
- Moms’ Mental Health Matters: Depression and Anxiety Around Pregnancy ( Eunice Kennedy Shriver National Institute of Child Health and Human Development)
Research and statistics
- Journal Articles : This webpage provides articles and abstracts on depression from MEDLINE/PubMed (National Library of Medicine).
- Statistics: Major Depression : This webpage provides the statistics currently available on the prevalence and treatment of depression among people in the United States.
- Depression Mental Health Minute : Take a mental health minute to watch this video on depression.
- NIMH Experts Discuss the Menopause Transition and Depression : Learn about the signs and symptoms, treatments, and latest research on depression during menopause.
- NIMH Expert Discusses Seasonal Affective Disorder : Learn about the signs and symptoms, treatments, and latest research on seasonal affective disorder.
- Discover NIMH: Personalized and Targeted Brain Stimulation Therapies : Watch this video describing repetitive transcranial magnetic stimulation and electroconvulsive therapy for treatment-resistant depression. Brain stimulation therapies can be effective treatments for people with depression and other mental disorders. NIMH supports studies exploring how to make brain stimulation therapies more personalized while reducing side effects.
- Discover NIMH: Drug Discovery and Development : One of the most exciting breakthroughs from research funded by NIMH is the development of a fast-acting medication for treatment-resistant depression based on ketamine. This video shares the story of how ketamine infusions meaningfully changed the life of a participant in an NIMH clinical trial.
- Mental Health Matters Podcast: Depression: The Case for Ketamine : Dr. Carlos Zarate Jr. discusses esketamine—the medication he helped discover—for treatment-resistant depression. The podcast covers the history behind the development of esketamine, how it can help with depression, and what the future holds for this innovative line of clinical research.
Last Reviewed: March 2024
Unless otherwise specified, the information on our website and in our publications is in the public domain and may be reused or copied without permission. However, you may not reuse or copy images. Please cite the National Institute of Mental Health as the source. Read our copyright policy to learn more about our guidelines for reusing NIMH content.
- Latest Latest
- The West The West
- Sports Sports
- Opinion Opinion
- Magazine Magazine
Study says depression not caused by chemical imbalance, raising questions about antidepressants
University college london research says depression is not a serotonin imbalance and drugs that target it may not be the answer.

By Lois M. Collins
Millions of Americans take antidepressants, but a new study suggests the theory underpinning their use may be entirely wrong. Research from the University College London raises doubt that chemical imbalance in the brain is responsible for depression .
A major review of previous studies on serotonin’s role in depression, just published in the journal Molecular Psychiatry, concluded that serotonin level — the target of antidepressants — is not responsible for depression.
The researchers found “no support for the hypothesis that depression is caused by lowered serotonin activity or concentrations.”
They found stronger evidence that stressful life events can lead to depression.
The question is, do antidepressants help, and if so, how? If not, could they be doing harm?
Experts are divided and the study has drawn some pushback.
“Some of the studies in our overview that included people who were taking or had previously taken antidepressants showed evidence that antidepressants may actually lower the concentration or activity of serotonin,” according to an article in The Conversation by the study’s authors, Joanna Moncrieff, professor of psychiatry, and Mark Horowitz, clinical research fellow in psychiatry, both of University College London.
“Most antidepressants are selective serotonin reuptake inhibitors, which were originally said to work by correcting abnormally low serotonin levels. There is no other accepted pharmacological mechanism by which antidepressants affect the symptoms of depression,” the researchers said in a news release .
The research suggests depression is not biochemical and questions how, given that, a biochemical solution would work. Horowitz and Moncrieff also question whether that kind of treatment, which acts on brain chemistry, does more harm than good.
“Our view is that patients should not be told that depression is caused by low serotonin or by a chemical imbalance, and they should not be led to believe that antidepressants work by targeting these unproven abnormalities. We do not understand what antidepressants are doing to the brain exactly, and giving people this sort of misinformation prevents them from making an informed decision about whether to take antidepressants or not,” Moncrieff said.
Targeting serotonin
The “chemical imbalance” theory has dominated the thinking about depression for several decades, according to the researchers.
“It is always difficult to prove a negative, but I think we can safely say that after a vast amount of research conducted over several decades, there is no convincing evidence that depression is caused by serotonin abnormalities, particularly by lower levels or reduced activity of serotonin,” Moncrieff said.
In the United States between 2015 and 2018, 13.9% of adults took antidepressants for depression, according to the National Center for Health Statistics in the Centers for Disease Control and Prevention.
As many as 1 in 6 adults in England are now prescribed antidepressants every year, according to the study.
“I had been taught that depression was caused by low serotonin in my psychiatry training and had even taught this to students in my own lectures. Being involved in this research was eye-opening and feels like everything I thought I knew has been flipped upside down,” said Horowitz in background material.
As Mike McRae wrote for ScienceAlert , “This doesn’t necessarily mean serotonin-based treatments aren’t working on some other mechanism we don’t yet understand. And no one should consider ditching their meds without consulting their doctors. But given so many people are relying on these drugs, it is important to figure out what’s really going on.”
Study nuts and bolts
In all, studies in the review included tens of thousands of participants. Among the serotonin mechanisms studied and the findings:
- No difference was seen between people with depression and healthy control subjects in levels of serotonin and breakdown products in the blood or brain fluids.
- In studies of serotonin receptors and the serotonin transporter protein most antidepressants target, they found “weak and inconsistent evidence” suggesting higher levels of serotonin activity in those who are depressed. They believe that was caused by use of antidepressants.
- Studies that lowered serotonin levels in hundreds of healthy volunteers did not produce depression. The researchers saw “very weak evidence” in a small 75-person subgroup of people with a family history of depression. A study after that was inconclusive.
- No evidence of variation in the serotonin transporter gene was found between those with depression and healthy control subjects.
On the other hand, stressful life events had a “strong effect” on the risk of becoming depressed. And the more one experienced stress or trauma, the greater the likelihood of depression.
“A famous early study found a relationship between stressful events, the type of serotonin transporter gene a person had and the chance of depression. But larger, more comprehensive studies suggest this was a false finding,” the release said.
In the piece from The Conversation , Moncrieff and Horowitz wrote, “It is important that people know that the idea that depression results from a ‘chemical imbalance’ is hypothetical. And we do not understand what temporarily elevating serotonin or other biochemical changes produced by antidepressants do to the brain. We conclude that it is impossible to say that taking SSRI antidepressants is worthwhile, or even completely safe.”
Public perception
Surveys suggest as many as 90% of people believe depression is caused by low serotonin or chemical imbalance. There’s evidence believing that creates a “pessimistic outlook on the likelihood of recovery” and the hope of managing depression without medical help, the study said.
Doubts about brain chemistry’s role in depression have been around a while.
“If you’re among those who are hearing all of this for the first time, the hypothesis has been on shaky ground practically since it took off in the 1990s, with study after study failing to support the idea,” wrote ScienceAlert’s McRae . He noted the Moncrieff and Horowitz limited their research to high-quality, peer-evaluated studies.
“Just 17 studies made the cut, which included a genetic association study, another umbrella review, and a dozen systematic reviews and meta-analyses,” he wrote.
The impact is huge, given most people will have diagnosable levels of anxiety or depression at some point, the researchers said.
The researchers also said one large meta-analysis found people using antidepressants had less serotonin in their blood, which could mean that antidepressants designed to raise levels of serotonin may do the opposite over time.
The researchers note they didn’t look at the efficacy of antidepressants. Their hope, they said, is that more research and treatment will focus on helping people manage stressful or traumatic events, “such as with psychotherapy, alongside other practices such as exercise or mindfulness, or addressing underlying contributors such as poverty, stress and loneliness.”
Some experts disagree
The research has attracted some pushback.
The Guardian quoted Dr. Michael Bloomfield, a consultant psychiatrist and principal clinical research fellow at University College London, who was not involved in the study: “Many of us know that taking paracetamol can be helpful for headaches, and I don’t think anyone believes that headaches are caused by not enough paracetamol in the brain. The same logic applies to depression and medicines used to treat depression.”
He added, “There is consistent evidence that antidepressant medicines can be helpful in the treatment of depression and can be life-saving.”
Johan Lundberg at the Karolinska Institute in Sweden told New Scientist that one limitation of the study is failure to distinguish between those with long-term depression and those having episodes of depression, because their state during the study could be different in terms of serotonin. “It is key to separately analyze data from studies that examine the same patients when ill and when in remission, to have optimal conditions to examine the hypothesis,” he said.
The same article quoted a spokesperson for the Royal College of Psychiatrists who was talking about treatment guidelines from public health officials in England, who said antidepressants are an effective treatment for depression and some other physical and mental health conditions.
The spokesperson noted that “antidepressants will vary in effectiveness for different people, and the reasons for this are complex. We would not recommend for anyone to stop taking their antidepressants based on this review, and encourage anyone with concerns about their medication to contact their (family doctor).”
Teen stress may raise risk of postpartum depression in adults
In a new study, a Johns Hopkins Medicine-led research team reports that social stress during adolescence in female mice later results in prolonged elevation of the hormone cortisol after they give birth. The researchers say this corresponds to the equivalent hormonal changes in postpartum women who were exposed to adverse early life experiences -- suggesting that early life stress may underlie a pathophysiological exacerbation of postpartum depression (PPD).
The team's findings, first published online Apr. 11, 2024, in Nature Mental Health , also suggest that current drug treatments for PPD in people may, in some cases, be less effective at targeting the relevant chemical imbalances in the brain, and that alternative methods may be more beneficial.
According to previous studies, an estimated one-third of psychiatric conditions fail to respond to current therapies, and "PPD is difficult to treat," says study senior author Akira Sawa, M.D., Ph.D., director of the Johns Hopkins Schizophrenia Center and professor of psychiatry, neuroscience, biomedical engineering, genetic medicine and pharmacology at the Johns Hopkins University School of Medicine. "The new study results add to evidence that patients with PPD are not all the same, and more individualized diagnosis and treatment -- a precision medicine approach -- is needed."
PPD, states the federal government's Office on Women's Health, is estimated to occur in 7% to 20% of all women, most commonly within six weeks of giving birth. Symptoms include feelings of sadness, anxiety, and fatigue, and can make it difficult to complete basic self-care tasks and care for the new baby.
The current first-line treatment for PPD is the use of a class of anti-depressant pills called selective serotonin reuptake inhibitors (SSRIs), but these are only effective in approximately half of all patients. SSRIs boost the effects of the natural brain chemical serotonin, one of many hormone-like substances that help control mood. Some patients also are treated with IV infusions of a different class of drugs that target GABAA, a brain chemical linked to nerve hyperactivity.
However, the calming infusions are costly (more than $30,000 for a single course of one such drug) and often require hospitalization. They are generally reserved for the most severe and resistant cases of PPD.
In the new study, the Johns Hopkins-led research team aimed to build on evidence that adverse life events may affect the likelihood and severity of PPD. Previous studies have shown that PPD is more prevalent in teens, and in urban populations.
Working with mice, the researchers first created four test groups: unstressed virgins, stressed virgins, unstressed mothers and stressed mothers. The stressed mice were subjected to social isolation in their adolescence, and all groups were tested for stress. At seven days postpartum, the stressed mothers showed decreased mobility and a decrease in sugar preference, both of which are considered markers for depression. This persisted for at least three weeks after delivery.
As the second and most critical step, the researchers tested plasma levels of several hormones and found the level of cortisol was increased in mothers both with and without adverse early life experiences. However, cortisol levels in unstressed mothers decreased to normal levels after delivery, while the levels in mothers with adverse early life experiences remained high for one to three weeks after birth. This finding, Sawa says, suggests a correlation between prolonged post-delivery elevation of cortisol and behavioral changes in postpartum mice who experienced social isolation in adolescence.
If these findings translate to humans, it could mean that a different kind of antidepressant, a glucocorticoid receptor (GR) antagonist, which blocks the effects of elevated cortisol, could be a novel treatment option for PPD. Mifepristone may be one such drug.
"Unfortunately, everyone knows someone who has suffered or currently suffers from PPD, and it has such a huge impact on both mother and baby," says Sawa. "The alternative line of treatment suggested by the mouse study -- where the findings are consistent with those from our observational study in humans -- might enable mothers to be treated at home and avoid separation from their babies, and target a different mechanism for depression that may be specific to PPD."
Plans are underway, Sawa says, to collect precise data on cortisol levels in people with PPD to determine if GR antagonists would be more beneficial than current treatments for some, and later, to conduct clinical trials with alternatives to SSRIs.
Along with Sawa, members of the study team from Johns Hopkins Medicine are Sedona Lockhart, Jennifer Payne, Gary Wand, Daniel Wood and Kun Yang. Team members from the University of Alabama at Birmingham Heersink School of Medicine are study lead author Minae Niwa, Adeel Ahmed, Shin-ichi Kano, Kyohei Kin and Jose Francis-Oliveira.
Funding for this research was provided by National Institutes of Health grants MH-092443, MH-094268, K99MH-094408, MH-105660, MH-107730, DA-040127, and MH-116869; the Brain and Behavior Research Foundation (formerly the National Alliance for Research on Schizophrenia and Depression); and other sources.
- Mental Health Research
- Teen Health
- Personalized Medicine
- Alternative Medicine
- Mental Health
- Adolescence
- Pituitary gland
- Growth hormone deficiency
- Stress (medicine)
- House mouse
- Double blind
- Menstrual cycle
Story Source:
Materials provided by Johns Hopkins Medicine . Note: Content may be edited for style and length.
Journal Reference :
- Minae Niwa, Sedona Lockhart, Daniel J. Wood, Kun Yang, Jose Francis-Oliveira, Kyohei Kin, Adeel Ahmed, Gary S. Wand, Shin-ichi Kano, Jennifer L. Payne, Akira Sawa. Prolonged HPA axis dysregulation in postpartum depression associated with adverse early life experiences: a cross-species translational study . Nature Mental Health , 2024; DOI: 10.1038/s44220-024-00217-1
Cite This Page :
Explore More
- How 3D Printers Can Give Robots a Soft Touch
- Combo of Multiple Health Stressors Harming Bees
- Methane Emission On a Cold Brown Dwarf
- Remarkable Memories of Mountain Chickadees
- Predicting Future Marine Extinctions
- Drain On Economy Due to Climate Change
- 'Tube Map' Around Planets and Moons
- 'Bizarre' Evolutionary Pattern: Homo Lineage
- Largest Known Marine Reptile
- Neolithic Humans Lived in Lava Tube Caves
Trending Topics
Strange & offbeat.
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
April 16, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
Study suggests adolescent stress may raise risk of postpartum depression in adults
by Johns Hopkins University

In a new study, a Johns Hopkins Medicine-led research team reports that social stress during adolescence in female mice later results in prolonged elevation of the hormone cortisol after they give birth. The researchers say this corresponds to the equivalent hormonal changes in postpartum women who were exposed to adverse early life experiences—suggesting that early life stress may underlie a pathophysiological exacerbation of postpartum depression (PPD).
The team's findings, published in Nature Mental Health , also suggest that current drug treatments for PPD in people may, in some cases, be less effective at targeting the relevant chemical imbalances in the brain, and that alternative methods may be more beneficial.
According to previous studies, an estimated one-third of psychiatric conditions fail to respond to current therapies, and "PPD is difficult to treat," says study senior author Akira Sawa, M.D., Ph.D., director of the Johns Hopkins Schizophrenia Center and professor of psychiatry, neuroscience, biomedical engineering, genetic medicine and pharmacology at the Johns Hopkins University School of Medicine. "The new study results add to evidence that patients with PPD are not all the same, and more individualized diagnosis and treatment—a precision medicine approach—is needed."
PPD, states the federal government's Office on Women's Health, is estimated to occur in 7% to 20% of all women, most commonly within six weeks of giving birth. Symptoms include feelings of sadness, anxiety, and fatigue, and can make it difficult to complete basic self-care tasks and care for the new baby.
The current first-line treatment for PPD is the use of a class of anti-depressant pills called selective serotonin reuptake inhibitors (SSRIs), but these are only effective in approximately half of all patients. SSRIs boost the effects of the natural brain chemical serotonin, one of many hormone-like substances that help control mood. Some patients also are treated with IV infusions of a different class of drugs that target GABAA, a brain chemical linked to nerve hyperactivity.
However, the calming infusions are costly (more than $30,000 for a single course of one such drug) and often require hospitalization. They are generally reserved for the most severe and resistant cases of PPD.
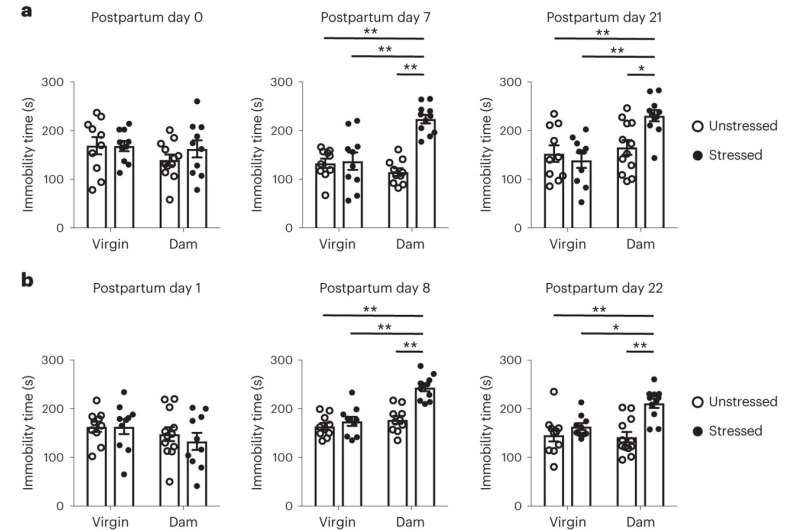
In the new study, the Johns Hopkins-led research team aimed to build on evidence that adverse life events may affect the likelihood and severity of PPD. Previous studies have shown that PPD is more prevalent in teens, and in urban populations.
Working with mice, the researchers first created four test groups: unstressed virgins, stressed virgins, unstressed mothers and stressed mothers. The stressed mice were subjected to social isolation in their adolescence, and all groups were tested for stress. At seven days postpartum, the stressed mothers showed decreased mobility and a decrease in sugar preference, both of which are considered markers for depression. This persisted for at least three weeks after delivery.
As the second and most critical step, the researchers tested plasma levels of several hormones and found the level of cortisol was increased in mothers both with and without adverse early life experiences. However, cortisol levels in unstressed mothers decreased to normal levels after delivery, while the levels in mothers with adverse early life experiences remained high for one to three weeks after birth. This finding, Sawa says, suggests a correlation between prolonged post-delivery elevation of cortisol and behavioral changes in postpartum mice who experienced social isolation in adolescence.
If these findings translate to humans, it could mean that a different kind of antidepressant, a glucocorticoid receptor (GR) antagonist, which blocks the effects of elevated cortisol, could be a novel treatment option for PPD. Mifepristone may be one such drug.
"Unfortunately, everyone knows someone who has suffered or currently suffers from PPD, and it has such a huge impact on both mother and baby," says Sawa. "The alternative line of treatment suggested by the mouse study—where the findings are consistent with those from our observational study in humans—might enable mothers to be treated at home and avoid separation from their babies, and target a different mechanism for depression that may be specific to PPD."
Plans are underway, Sawa says, to collect precise data on cortisol levels in people with PPD to determine if GR antagonists would be more beneficial than current treatments for some, and later, to conduct clinical trials with alternatives to SSRIs.
Explore further
Feedback to editors

Researchers discover new therapeutic target for non-small cell lung cancer
9 hours ago

Immune cells carry a long-lasting 'memory' of early-life pain
10 hours ago

Cannabis legalization and rising sales have not contributed to increase in substance abuse, study finds

No negative impact from prolonged eye patching on child's development or family stress levels

COVID-19 booster immunity lasts much longer than primary series alone, study shows

Study finds that human neuron signals flow in one direction
11 hours ago

A common pathway in the brain that enables addictive drugs to hijack natural reward processing identified
12 hours ago

Scientists identify airway cells that sense aspirated water and acid reflux

Environment may influence metacognitive abilities more than genetics

Contracting RSV before age two can cause long-term lung changes and impairment
Related stories.

Study finds esketamine injection just after childbirth reduces depression in new mothers
Apr 10, 2024

Potential link between high maternal cortisol, unpredicted birth complications
Jan 31, 2024

Altered cortisol cycle in pregnant women with depressive symptoms may affect gestation process
Feb 1, 2024

Antidepressant use, infection during pregnancy linked to neurodevelopmental disorders
Dec 20, 2022

Pregnancy stress may shape baby brain
Nov 24, 2020
Hair cortisol levels predict which mothers are more likely to suffer postpartum depression
Nov 14, 2017
Recommended for you

Molecular atlas shows how the growth factor erythropoietin affects neurons
16 hours ago

Scientists uncover 95 regions of the genome linked to PTSD
21 hours ago

Accelerated aging biology in the placenta found to contribute to a rare form of pregnancy-related heart failure
Apr 17, 2024

Dialogue between brain regions: How memories guide us to rewards

Understanding the brain mechanisms behind emotion processing bias in treatment-resistant depression
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter

IMAGES
COMMENTS
A new type of magnetic brain stimulation brought rapid remission to almost 80% of participants with severe depression in a study conducted at the Stanford University School of Medicine. The treatment, known as Stanford accelerated intelligent neuromodulation therapy (SAINT) or simply Stanford neuromodulation therapy, is an intensive, individualized form of transcranial magnetic stimulation.
Depression is common, costly, debilitating, and associated with increased risk of suicide. It is one of the leading global public health problems. Although existing available pharmacological treatments can be effective, their onset of action can take up to 6 weeks, side-effects are common, and recovery can require treatment with multiple different agents. Although psychosocial interventions ...
The discovery, outlined Thursday in the journal Science, improves understanding of the biological causes of major depression and could accelerate efforts to develop new, faster-acting medications ...
Latest Research and Reviews Psychological flexibility as a mechanism of change in psilocybin-assisted therapy for major depression: results from an exploratory placebo-controlled trial Jordan ...
Scientists at Stanford Medicine conducted a study describing a new category of depression — labeled the cognitive biotype — which accounts for 27% of depressed patients and is not effectively treated by commonly prescribed antidepressants.. Cognitive tasks showed that these patients have difficulty with the ability to plan ahead, display self-control, sustain focus despite distractions and ...
The idea that depression is the result of abnormalities in brain chemicals, particularly serotonin (5-hydroxytryptamine or 5-HT), has been influential for decades, and provides an important ...
A new study led by Stanford Medicine researchers is the first to reveal how magnetic stimulation treats severe depression: ... the NIMH Biobehavioral Research Awards for Innovative New Scientists award (grant R01 5R01MH122754-02), Charles R. Schwab, the David and Amanda Chao Fund II, the Amy Roth PhD Fund, the Neuromodulation Research Fund, the ...
Read the latest research findings and in-depth information on clinical depression and stress in adults, teens, and children. Expand your understanding of the symptoms and available treatment for ...
R. McShaneN Engl J Med 2023;389:1333-1334. Depression can become self-perpetuating as occupational, relationship, and social losses accrue. Sustained remission is achieved in less than half of ...
The current speed of progress in depression research is simply remarkable. We have therefore been able to create a second special issue of Molecular Psychiatry, 2020, focused on depression, with ...
Research on the development of new antidepressants should explore several mechanisms of action on several types of receptors: ... and somatic approaches. Research on depression pharmacotherapy continues to examine new molecules implicated in gamma-aminobutyric acid regulation and glutamate transmission. Also, efforts to personalize and simplify ...
Imagining virtual reality as a simple tool to treat depression. Sarah C. P. Williams April 11, 2024. Some of the 17 million Americans afflicted with major depressive disorder each year may soon receive a surprising new prescription from their clinician: Have fun on a virtual reality device. Engaging in activities that make you feel good may ...
Analysis of published papers around the world from 2009 to 2019 in depressive disorder. A The total number of papers [from a search of the Web of Science database (search strategy: TI = (depression$) or ts = ("major depressive disorder$")) and py = (2009-2019), Articles)].B The top 10 countries publishing on the topic.C Comparison of papers in China and the USA.
Depression: The Latest Research. If you're one of more than 17 million adults or 3.2 million teens in the United States with major depression, you may know that treatment often falls short. The ...
FDA approval of the postpartum depression treatment brexanolone represents the final phase of a bench-to-bedside journey for this drug — a journey that began in the NIMH Intramural Research Program. NIMH experts are available to provide information on postpartum depression and the importance of, and the science underlying, this new drug.
Rodent research has shown that there may be a bidirectional association between the gut microbiota and depression: a disordered gut microbiota can play a role in the onset of this mental health problem, but, at the same time, the existence of stress and depression may also lead to a lower level of richness and diversity in the microbiome .
GAINESVILLE, Fla. — A noninvasive brain stimulation treatment improved depression and anxiety symptoms among older adults in a new University of Florida College of Public Health and Health Professions -led study. Improvements in depression and anxiety symptoms were greatest among patients who reported higher symptom levels before treatment.
Overall, this research did not show a difference between people with depression and those without depression. Another area of research has focused on serotonin receptors, which are proteins on the ends of the nerves that serotonin links up with and which can transmit or inhibit serotonin's effects.
Stem Cells: A theory is currently being studied that stem cells may decrease depression by helping create more neurons that can form more connections in the brain. Current research includes investigating if there are new molecules that can activate stem cells to act in this antidepressant way. 20 Sources.
Running or yoga can help beat depression, research shows - even if exercise is the last thing you feel like. Michael Noetel, The University of Queensland. Our new study shows you may be able to ...
A new published review finds no evidence that low serotonin levels cause depression. The authors use their data to refute the "chemical imbalance" hypothesis of depression, which is an old and ...
Depression is a serious medical illness that involves the brain. It's more than just a feeling of being "down in the dumps" or "blue" for a few days. If you are one of the more than 20 million ...
Depression (also known as major depression, major depressive disorder, or clinical depression) is a common but serious mood disorder. It causes severe symptoms that affect how a person feels, thinks, and handles daily activities, such as sleeping, eating, or working. To be diagnosed with depression, the symptoms must be present for at least 2 ...
Depressive disorder (also known as depression) is a common mental disorder. It involves a depressed mood or loss of pleasure or interest in activities for long periods of time. Depression is different from regular mood changes and feelings about everyday life. It can affect all aspects of life, including relationships with family, friends and ...
Millions of Americans take antidepressants, but a new study suggests the theory underpinning their use may be entirely wrong. Research from the University College London raises doubt that chemical imbalance in the brain is responsible for depression.. A major review of previous studies on serotonin's role in depression, just published in the journal Molecular Psychiatry, concluded that ...
In a new study, a Johns Hopkins Medicine-led research team reports that social stress during adolescence in female mice later results in prolonged elevation of the hormone cortisol after they give ...
Desperate to help record numbers of children suffering anxiety and depression, state and local governments are testing new interventions to get to the root of the crisis — even if they don't ...
New research published last month in JAMA Open Network suggests that familiar scents can improve symptoms in people with depressive disorders. That's because individuals who suffer from depression ...
In a new study, a Johns Hopkins Medicine-led research team reports that social stress during adolescence in female mice later results in prolonged elevation of the hormone cortisol after they give ...
Research has shown that most individuals can help preserve their health and mobility as they age by adopting or continuing healthy habits and lifestyle choices. Read on to learn about 10 common misconceptions related to aging and older adults. 1. Are depression and loneliness normal in older adults?