

Patient Case #1: 19-Year-Old Male With ADHD
- Craig Chepke, MD, DFAPA, FAPA
- Andrew J. Cutler, MD
Stephen Faraone, PhD, presents the case of a 19-year-old male with ADHD.

EP: 1 . Prevalence of Adult ADHD
Ep: 2 . diagnosis and management of adults adhd compared to children.
EP: 3 . Diagnosing Adults With ADHD Based on Patient Presentation

EP: 4 . Unmet Needs in the Treatment of Adult ADHD

EP: 5 . Efficacy and Safety of Treatment Options Utilized in Adult ADHD
Ep: 6 . future of adult adhd, ep: 7 . patient case #1: 19-year-old male with adhd.

EP: 8 . Patient Case #1: Prompting an ADHD Consultation
Ep: 9 . patient case #1: differentiating between adhd and other psychiatric comorbidities, ep: 10 . patient case #1: co-managing adhd, ep: 11 . patient case #1: dealing with treatment delay in adult adhd, ep: 12 . patient case #2: a 23-year-old patient with adhd, ep: 13 . patient case #2: impressions and challenges in adult adhd, ep: 14 . patient case #2: dealing with comorbidities in adult adhd, ep: 15 . patient case #2: addressing non-adherence and stigma of adult adhd, ep: 16 . patient case #2: importance of an integrative approach in adult adhd, ep: 17 . case 3: 24-year-old patient with adhd, ep: 18 . case 3: treatment goals in adult adhd, ep: 19 . case 3: factors driving treatment selection in adult adhd, ep: 20 . implications of pharmacogenetic testing in adhd, ep: 21 . novel drug delivery systems in adhd and take-home messages.
Stephen Faraone, PhD: That's a good one, yes, I'd like that, it's a very creative one, thank you, thank you. OK, let's move on to the case presentation. This first patient is a 19-year-old male, who presented to his psychiatrist after being referred by his primary care provider, PCP for ADHD consultation, during the interview, he noted he was a sophomore in college and is taking 17 credits. This semester chief complaint includes a lack of ability to focus in class as well as struggling with time management. He complained that every time he's in class, he finds himself thinking about many other responsibilities he must complete at home and feels that he cannot control it. He has had this complaint for the past 6 years, but refused to seek help, because he feared being put on medication. In high school, he was assigned a counselor who taught him behavior techniques such as making a schedule, and going on walks, which he found to be very effective. However, these techniques were less effective once he started college. His symptoms tend to get worse before exams, he often feels very anxious, leading to horrible performance on exams, he claimed that he has been this anxious since he took his LSAT tests. Currently, he is on academic probation, and is not allowed to be part of the Student Work Program, which was his only source of income. The patient has no history of substance abuse, no history of taking any medications for his symptoms, and no history of suicidal thoughts.
Transcript edited for clarity
WHO Addresses Gaps in Mental Health Care Delivery and Quality

Treating ADHD in Children: Concerns, Controversies, Safety Measures

Childhood Physical Health and ADHD Symptoms

ADHD in Older Adults

Longitudinal Study Looks at Risk of Cardiovascular Disease With Long-Term ADHD Medication Use

The Week in Review: May 20-24
2 Commerce Drive Cranbury, NJ 08512
609-716-7777


- Presidential Message
- Nominations/Elections
- Past Presidents
- Member Spotlight
- Fellow List
- Fellowship Nominations
- Current Awardees
- Award Nominations
- SCP Mentoring Program
- SCP Book Club
- Pub Fee & Certificate Purchases
- LEAD Program
- Introduction
- Find a Treatment
- Submit Proposal
- Dissemination and Implementation
- Diversity Resources
- Graduate School Applicants
- Student Resources
- Early Career Resources
- Principles for Training in Evidence-Based Psychology
- Advances in Psychotherapy
- Announcements
- Submit Blog
- Student Blog
- The Clinical Psychologist
- CP:SP Journal
- APA Convention
- SCP Conference
CASE STUDY Jen (attention-deficit/hyperactivity disorder)
Case study details.
Jen is a 29 year-old woman who presents to your clinic in distress. In the interview she fidgets and has a hard time sitting still. She opens up by telling you she is about to be fired from her job. In addition, she tearfully tells you that she is in a major fight with her husband of 1 year because he is ready to have children but she fears that she is “too disorganized to be a good mother.” As you break down some of the processes that have led to her current crises, you learn that she has a hard time with time management and tends to be disorganized. She chronically misplaces everyday objects like her keys and runs late to appointments. Although she wants her work to be perfect, she is prone to making careless mistakes. The struggle for perfection makes starting a new task feel very stressful, leading her to procrastinate starting in the first place. As a consequence, she has recently received a number of warnings from her boss related to missing deadlines for assignments and errors in her work, which has led to her acute fear of being fired. As her performance at work has plummeted and she has grown increasingly anxious and doubting of herself, she has grown more pessimistic about starting a family. You learn that she received extra time for test taking in school as a child but never had any formal neuropsychological testing. With Jen’s permission, you conduct additional structured assessments, including collecting collateral information from her fiancé, and conclude that she has adult ADHD.
- Concentration Difficulties
- Impulsivity
Diagnoses and Related Treatments
1. attention deficit hyperactivity disorder (adults).
Thank you for supporting the Society of Clinical Psychology. To enhance our membership benefits, we are requesting that members fill out their profile in full. This will help the Division to gather appropriate data to provide you with the best benefits. You will be able to access all other areas of the website, once your profile is submitted. Thank you and please feel free to email the Central Office at [email protected] if you have any questions
Attention Deficit Hyperactivity Disorder (ADHD): A Case Study and Exploration of Causes and Interventions
- First Online: 02 March 2019
Cite this chapter

- Bijal Chheda-Varma 5
3360 Accesses
The male to female ratio of ADHD is 4:1. This chapter on ADHD provides a wide perspective on understanding, diagnosis and treatment for ADHD. It relies on a neurodevelopmental perspective of ADHD. Signs and symptoms of ADHD are described through the DSM-V criteria. A case example (K, a patient of mine) is illustrated throughout the chapter to provide context and illustrations, and demonstrates the relative merits of “doing” (i.e. behavioural interventions) compared to cognitive insight, or medication alone. Finally, a discussion of the Cognitive Behavioral Modification Model (CBM) for the treatment of ADHD provides a snapshot of interventions used by clinicians providing psychological help.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Similar content being viewed by others
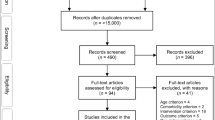
Psychological Treatments in Adult ADHD: A Systematic Review
Attention-Deficit Hyperactivity Disorder

ADHD and Its Therapeutics
Alderson, R. M., Hudec, K. L., Patros, C. H. G., & Kasper, L. J. (2013). Working memory deficits in adults with attention-deficit/hyperactivity disorder (ADHD): An examination of central executive and storage/rehearsal processes. Journal of Abnormal Psychology, 122 (2), 532–541. http://dx.doi.org/10.1037/a0031742 .
Arcia, E., & Conners, C. K. (1998). Gender differences in ADHD? Journal of Developmental and Behavioral Pediatrics, 19 (2), 77–83. http://dx.doi.org/10.1097/00004703-199804000-00002 .
Barkley, R. A. (1990). Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment . New York: Guildford.
Google Scholar
Barkley, R. A. (1997). ADHD and the nature of self-control . New York: Guilford Press.
Barkley, R. A. (2000). Commentary on the multimodal treatment study of children with ADHD. Journal of Abnormal Child Psychology, 28 (6), 595–599. https://doi.org/10.1023/A:1005139300209 .
Article Google Scholar
Barkley, R., Knouse, L., & Murphy, K. Correction to Barkley et al. (2011). Psychological Assessment [serial online]. June 2011; 23 (2), 446. Available from: PsycINFO, Ipswich, MA. Accessed December 11, 2014.
Beck, A. T. (1976). Cognitive therapy and the emotional disorders . New York, NY: International Universities Press.
Brown, T. E. (2005). Attention deficit disorder: The unfocused mind in children and adults . New Haven, CT: Yale University Press.
Brown, T. (2013). A new understanding of ADHD in children and adults . New York: Routledge.
Chacko, A., Kofler, M., & Jarrett, M. (2014). Improving outcomes for youth with ADHD: A conceptual framework for combined neurocognitive and skill-based treatment approaches. Clinical Child and Family Psychology Review . https://doi.org/10.1007/s10567-014-0171-5 .
Chronis, A., Jones, H. A., Raggi, V. L. (2006, August). Evidence-based psychosocial treatments for children and adolescents with attention-deficit/hyperactivity disorder. Clinical Psychology Review, 26 (4), 486–502. ISSN 0272-7358. http://dx.doi.org/10.1016/j.cpr.2006.01.002 .
Curatolo, P., D’Agati, E., & Moavero, R. (2010). The neurobiological basis of ADHD. Italian Journal of Pediatrics, 36 , 79. http://doi.org/10.1186/1824-7288-36-79 . http://www.sciencedirect.com/science/article/pii/S0272735806000031 .
Curtis, D. (2010). ADHD symptom severity following participation in a pilot, 10-week, manualized, family-based behavioral intervention. Child & Family Behavior Therapy, 32 , 231–241. https://doi.org/10.1080/07317107.2010.500526 .
De Young, R. (2014). Using the Stroop effect to test our capacity to direct attention: A tool for navigating urgent transitions. http://www.snre.umich.edu/eplab/demos/st0/stroopdesc.html .
Depue, B. E., Orr, J. M., Smolker, H. R., Naaz, F., & Banich, M. T. (2015). The organization of right prefrontal networks reveals common mechanisms of inhibitory regulation across cognitive, emotional, and motor processes. Cerebral Cortex (New York, NY: 1991), 26 (4), 1634–1646.
D’Onofrio, B. M., Van Hulle, C. A., Waldman, I. D., Rodgers, J. L., Rathouz, P. J., & Lahey, B. B. (2007). Causal inferences regarding prenatal alcohol exposure and childhood externalizing problems. Archives of General Psychiatry, 64, 1296–1304 [PubMed].
DSM-V. (2013). Diagnostic and statistical manual of mental disorders . American Psychological Association.
Eisenberg, D., & Campbell, B. (2009). Social context matters. The evolution of ADHD . http://evolution.binghamton.edu/evos/wp-content/uploads/2012/02/eisenberg-and-campbell-2011-the-evolution-of-ADHD-artice-in-SF-Medicine.pdf .
Gizer, I. R., Ficks, C., & Waldman, I. D. (2009). Hum Genet, 126 , 51. https://doi.org/10.1007/s00439-009-0694-x .
Hinshaw, S. P., & Scheffler, R. M. (2014). The ADHD explosion: Myths, medication, money, and today’s push for performance . New York: Oxford University Press.
Kapalka, G. M. (2008). Efficacy of behavioral contracting with students with ADHD . Boston: American Psychological Association.
Kapalka, G. (2010). Counselling boys and men with ADHD . New York: Routledge, Taylor & Francis Group.
Book Google Scholar
Knouse, L. E., et al. (2008, October). Recent developments in psychosocial treatments for adult ADHD. National Institute of Health, 8 (10), 1537–1548. https://doi.org/10.1586/14737175.8.10.1537 .
Laufer, M., Denhoff, E., & Solomons, G. (1957). Hyperkinetic impulse disorder in children’s behaviour problem. Psychosomatic Medicine, 19, 38–49.
Raggi, V. L., & Chronis, A. M. (2006). Interventions to address the academic impairment of children and adolescents with ADHD. Clinical Child and Family Psychology Review, 9 (2), 85–111. https://doi.org/10.1007/s10567-006-0006-0 .
Ramsay, J. R. (2011). Cognitive behavioural therapy for adult ADHD. Journal of Clinical Outcomes Management, 18 (11), 526–536.
Retz, W., & Retz-Junginger, P. (2014). Prediction of methylphenidate treatment outcome in adults with attention deficit/hyperactivity disorder (ADHD). European Archives of Psychiatry and Clinical Neuroscience . https://doi.org/10.1007/s00406-014-0542-4 .
Safren, S. A., Otto, M. W., Sprich, S., Winett, C. L., Wilens, T. E., & Biederman, J. (2005, July). Cognitive-behavioral therapy for ADHD in medication-treated adults with continued symptoms. Behaviour Research and Therapy, 43 (7), 831–842. ISSN 0005-7967. http://dx.doi.org/10.1016/j.brat.2004.07.001 . http://www.sciencedirect.com/science/article/pii/S0005796704001366 .
Sibley, M. H., Kuriyan, A. B., Evans, S. W., Waxmonsky, J. G., & Smith, B. H. (2014). Pharmacological and psychosocial treatments for adolescents with ADHD: An updated systematic review of the literature. Clinical Psychology Review, 34 (3), 218–232. https://doi.org/10.1016/j.cpr.2014.02.001 .
Simchon, Y., Weizman, A., & Rehavi, M. (2010). The effect of chronic methylphenidate administration on presynaptic dopaminergic parameters in a rat model for ADHD. European Neuropsychopharmacology, 20 (10), 714–720. ISSN 0924-977X. https://doi.org/10.1016/j.euroneuro.2010.04.007 . http://www.sciencedirect.com/science/article/pii/S0924977X10000891 .
Swanson, J. M., & Castellanos, F. X. (2002). Biological bases of ADHD: Neuroanatomy, genetics, and pathophysiology. In P. S. Jensen & J. R. Cooper (Eds.), Attention deficit hyperactivity disorder: State if the science, best practices (pp. 7-1–7-20). Kingston, NJ: Civic Research Institute.
Toplak, M. E., Connors, L., Shuster, J., Knezevic, B., & Parks, S. (2008, June). Review of cognitive, cognitive-behavioral, and neural-based interventions for attention-deficit/hyperactivity disorder (ADHD). Clinical Psychology Review, 28 (5), 801–823. ISSN 0272-7358. http://dx.doi.org/10.1016/j.cpr.2007.10.008 . http://www.sciencedirect.com/science/article/pii/S0272735807001870 .
Wu, J., Xiao, H., Sun, H., Zou, L., & Zhu, L.-Q. (2012). Role of dopamine receptors in ADHD: A systematic meta-analysis. Molecular Neurobiology, 45 , 605–620. https://doi.org/10.1007/s12035-012-8278-5 .
Download references
Author information
Authors and affiliations.
Foundation for Clinical Interventions, London, UK
Bijal Chheda-Varma
You can also search for this author in PubMed Google Scholar
Editor information
Editors and affiliations.
UCL, London, UK
John A. Barry
Norfolk and Suffolk NHS Foundation Trust, Wymondham, UK
Roger Kingerlee
Change, Grow, Live, Dagenham/Southend, Essex, UK
Martin Seager
Community Interest Company, Men’s Minds Matter, London, UK
Luke Sullivan
Rights and permissions
Reprints and permissions
Copyright information
© 2019 The Author(s)
About this chapter
Chheda-Varma, B. (2019). Attention Deficit Hyperactivity Disorder (ADHD): A Case Study and Exploration of Causes and Interventions. In: Barry, J.A., Kingerlee, R., Seager, M., Sullivan, L. (eds) The Palgrave Handbook of Male Psychology and Mental Health. Palgrave Macmillan, Cham. https://doi.org/10.1007/978-3-030-04384-1_15
Download citation
DOI : https://doi.org/10.1007/978-3-030-04384-1_15
Published : 02 March 2019
Publisher Name : Palgrave Macmillan, Cham
Print ISBN : 978-3-030-04383-4
Online ISBN : 978-3-030-04384-1
eBook Packages : Behavioral Science and Psychology Behavioral Science and Psychology (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
A Case Study in Attention-Deficit/Hyperactivity Disorder: An Innovative Neurofeedback-Based Approach
- University of Oviedo

Abstract and Figures

Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations
- Int J Environ Res Publ Health
- Malgorzata Nermend

- Kesra Nermend

- Giada Viviani

- Nerea Aldunate
- Luis J Fuentes

- APPL PSYCHOPHYS BIOF

- Howard Lightstone

- Curr Psychiatr Rep

- J PSYCHIATR RES

- Siyuan Wang

- CLIN NEUROPHYSIOL
- Adam R Clarke

- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Attention deficit/hyperactivity disorder in adults: A case study
Affiliations.
- 1 University of North Dakota, United States of America. Electronic address: [email protected].
- 2 University of North Dakota, United States of America.
- 3 Dana Wiley, MD PA.
- PMID: 35461644
- DOI: 10.1016/j.apnu.2021.12.003
Attention-Deficit/Hyperactivity Disorder (ADHD) is often misdiagnosed or mistreated in adults because it is often thought of as a childhood problem. If a child is diagnosed and treated for the disorder, it often persists into adulthood. In adult ADHD, the symptoms may be comorbid or mimic other conditions making diagnosis and treatment difficult. Adults with ADHD require an in-depth assessment for proper diagnosis and treatment. The presentation and treatment of adults with ADHD can be complex and often requires interdisciplinary care. Mental health and non-mental health providers often overlook the disorder or feel uncomfortable treating adults with ADHD. The purpose of this manuscript is to discuss the diagnosis and management of adults with ADHD.
Keywords: Adult; Attention Deficit/Hyperactivity Disorder; Misuse; Psychoeducation; Stimulant.
Copyright © 2022 Elsevier Inc. All rights reserved.
PubMed Disclaimer
Similar articles
- [Awareness of adult attention-deficit/hyperactivity disorder (ADHD) in Greece]. Pehlivanidis A. Pehlivanidis A. Psychiatriki. 2012 Jun;23 Suppl 1:60-5. Psychiatriki. 2012. PMID: 22796974 Review. Greek, Modern.
- Practical considerations for the evaluation and management of Attention Deficit Hyperactivity Disorder (ADHD) in adults. Weibel S, Menard O, Ionita A, Boumendjel M, Cabelguen C, Kraemer C, Micoulaud-Franchi JA, Bioulac S, Perroud N, Sauvaget A, Carton L, Gachet M, Lopez R. Weibel S, et al. Encephale. 2020 Feb;46(1):30-40. doi: 10.1016/j.encep.2019.06.005. Epub 2019 Oct 11. Encephale. 2020. PMID: 31610922 Review.
- Attention deficit hyperactivity disorder in adults: conceptual and clinical issues. Trollor JN. Trollor JN. Med J Aust. 1999 Oct 18;171(8):421-5. doi: 10.5694/j.1326-5377.1999.tb123723.x. Med J Aust. 1999. PMID: 10590746 Review.
- Health-related quality of life in children and adolescents who have a diagnosis of attention-deficit/hyperactivity disorder. Klassen AF, Miller A, Fine S. Klassen AF, et al. Pediatrics. 2004 Nov;114(5):e541-7. doi: 10.1542/peds.2004-0844. Pediatrics. 2004. PMID: 15520087
- Clinical assessment and treatment of attention deficit hyperactivity disorder in adults. Asherson P. Asherson P. Expert Rev Neurother. 2005 Jul;5(4):525-39. doi: 10.1586/14737175.5.4.525. Expert Rev Neurother. 2005. PMID: 16026236 Review.
- Acoustic and Text Features Analysis for Adult ADHD Screening: A Data-Driven Approach Utilizing DIVA Interview. Li S, Nair R, Naqvi SM. Li S, et al. IEEE J Transl Eng Health Med. 2024 Feb 26;12:359-370. doi: 10.1109/JTEHM.2024.3369764. eCollection 2024. IEEE J Transl Eng Health Med. 2024. PMID: 38606391 Free PMC article.
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- Elsevier Science
- Ovid Technologies, Inc.
- Genetic Alliance
- MedlinePlus Health Information
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

An ADHD diagnosis in adulthood comes with challenges and benefits
For adults, undiagnosed ADHD symptoms can lead to chronic stress and low self-esteem
Vol. 54 No. 2 Print version: page 52
- Perception and Attention

When Terry Matlen, a clinical social worker, was in her 40s, she was diagnosed with ADHD. “My entire life, there was something off,” Matlen said. This included significant anxiety as well as academic and behavioral issues, all of which started at a young age. Although Matlen was initially quite skeptical of her diagnosis, going so far as to seek out a second and third opinion, she eventually came to accept that she had ADHD.
“This makes sense now. I can’t concentrate; I can’t finish projects; my house is a disaster; I can’t get dinner on the table,” Matlen said. “Anxiety doesn’t explain the extent of my disorganization.”
Matlen was diagnosed in the mid-1990s, when many specialists still didn’t understand what ADHD looked like in either girls or adults. Matlen didn’t look like the stereotypical little boy who couldn’t sit still. Although she struggled a lot with her symptoms, which included being unable to pay attention in class or stay organized, no one recognized that the underlying issue was undiagnosed ADHD.
ADHD has three subtypes, which include hyperactive impulsive, primarily inattentive, and combined. With inattentive type, the restlessness is internal. “A lot of kids with inattentive ADHD get overlooked,” said Peter Jaksa, PhD, a psychologist who specializes in treating ADHD. “The behavioral problems get more attention.” For many with inattentive ADHD, they are the ones daydreaming in class rather than paying attention. However, since they aren’t being disruptive, their symptoms can easily go unnoticed.
This is especially true with women and girls, as ADHD is more often diagnosed and treated in males than females, due to differences in how symptoms look ( Skogli, E. W., et al., BMC Psychiatry , Vol. 13, 2013 ). As a number of studies show, untreated ADHD leads to adverse effects on long-term academic performance ( Arnold, L. E., et al., Journal of Attention Disorders , Vol. 24, No. 1, 2015 ). In addition, a number of studies show that those with untreated ADHD fare worse than those with treated ADHD or no ADHD ( Harpin, V., et al., Journal of Attention Disorders , Vol. 20, No. 4, 2013 ).
The process of diagnosing adults
For symptoms to be considered ADHD, they must have started before the age of 12. This makes diagnosing adults more complicated, as the process requires creating a timeline of when symptoms first appeared. In addition to talking with his patient, Jaksa finds that it can be helpful to look at old report cards, where comments such as “Struggles to pay attention during class,” “Often forgets homework at home,” or “Isn’t living up to potential” can help give him a sense of when symptoms started appearing.
“We have a much longer history to look at,” he said. “The best diagnostic indicator for ADHD is not test scores; it’s history.” For the diagnostic process, Jaksa conducts a very structured interview—one that delves into their social, emotional, and academic history. If possible, he interviews a family member who can provide perspective on childhood behaviors.
Jaksa said adults often have comorbidities, such as anxiety and depression. With these comorbidities, untreated ADHD can either cause them or make them worse. “When ADHD is not diagnosed—when it’s not treated effectively—over time, chronic stress and frustration lead to anxiety,” Jaksa said. “This has a very negative impact on self-esteem. It’s very common to see adults with ADHD grow up with a strong sense of underachievement.” Continually hearing messages like “try harder” or “you should be doing better,” can get internalized and lead to anxiety and/or depression, Jaksa said.
In some patients, providers may recognize signs right away, such as tardiness, forgetting valuable personal items, or fidgeting while in the waiting room. Although no one symptom can be definitive, all of this added up can paint a picture of what the symptoms look like, how long they have been going on, and the degree of functional impairment. “My mind is shifting constantly,” said Lisa Green, an oncology nurse who was diagnosed with ADHD in her 40s.
It also helps the diagnosis if there is a family history of ADHD, as it is a highly heritable disorder. For Matlen, the process of seeking a diagnosis for her younger daughter was when she realized that she also had the disorder. “It’s pretty well established that ADHD is about 70% to 80% heritable,” said Eugene Arnold, a professor emeritus at The Ohio State University whose research focuses on ADHD.
Difficulties with diagnosing
One of the challenging aspects of diagnosing an adult is the presence of other comorbidities, some of which can mimic ADHD symptoms. These comorbidities can either be due to a separate disorder or be caused by the ADHD. For many people with ADHD, Matlen included, the lack of early treatment, combined with symptoms of ADHD, can lead to developing mood disorders such as anxiety and depression. If their underlying ADHD is not diagnosed and treated, treatment for their other comorbidities is often ineffective. ( Ginsberg, Y., et al., Primary Care Companion for CNS Disorders , Vol. 16, No. 3, 2014 ). “My anxiety is triggered a lot by being disorganized, by not being prepared, by being constantly overwhelmed,” Matlen said.
There’s also an overlap between ADHD and autism spectrum disorder (ASD). “About half of people with autism also have ADHD,” Arnold said. With ADHD being more common than ASD, the reverse is not true—with a lower proportion of people with ADHD also having ASD.
Jon Stevens, MD, a psychiatrist based in Houston, compares the onset of symptoms as being like layers of an onion: The deepest layer is developmental disorders, such as autism; the second deepest layer is ADHD, for which the symptoms can be observed quite early, followed by mood disorders such as anxiety and depression, which can develop as early as middle or high school. Finally, the outermost layer is schizophrenia and bipolar disorder, which tend to emerge during college years or a little later.
“These conditions, in my experience, develop inside out,” Stevens said. Symptoms of developmental disorders such as autism show up the earliest, while ADHD symptoms will show up a little later. Some of the more noticeable symptoms, such as hyperactivity, parents will start noticing early on, while other symptoms, such as inattentiveness, will start becoming more noticeable once children start school.
Another major difference is the persistence of symptoms. “If you think about anxiety and depression, those disorders and the symptoms that flow from them, tend to be more situational and more cyclic,” said Will Canu, PhD, a professor of psychology at Appalachian State University. With a disorder like ADHD, the symptoms are always there, with the caveat that they can be exacerbated under certain conditions, such as during times of stress or from anxiety or depression.
The effect of Covid -19 on adults with ADHD
The Covid -19 pandemic was particularly hard on those with ADHD because of the disruption in routine. Routines are important for people with ADHD, as they can help with executive functioning issues, such as staying organized and staying on track. However, developing and maintaining these routines is harder, which means that major changes in working and home life have been particularly hard to navigate.
[ Related: Helping adults and children with ADHD in a pandemic world ]
In Stevens’ clinical practice, he has seen patients cope with stress from the pandemic in a number of ways. For adults who were actively receiving treatment, the shift to working from home offered some benefits. “Provided they kept taking their medication, they generally fared well,” he said. “A lot of my patients found [working from home] more helpful, because there were fewer distractions of the water cooler chatter or someone coming to your cubicle.” The big exception was if patients started self-medicating with alcohol or other substances.
Constant upheaval, combined with childcare disruptions, created extremely difficult conditions for women with undiagnosed ADHD and young children, Canu said. In addition to major disruptions in routines, the unpredictability of school and daycare closures has been particularly challenging for parents with young children.
The advantage of diagnosis and treatment
For many patients whose symptoms were overlooked during their early years, diagnosis can be both life changing, and bittersweet. In a 2020 study, researchers compared 444 adults with diagnosed ADHD with 1,055 adults who exhibited symptoms but had no formal diagnosis. After matching for age and gender, those with a diagnosis reported a higher quality of life, which included metrics for work productivity, self-esteem, and functional performance ( Pawaskar, M., et al., Journal of Attention Disorders , Vol. 24, No. 1, 2020 ).
Canu said being diagnosed helps people understand themselves better, which includes gaining perspective on the reasons for some of their struggles. “That can change the way they feel about themselves, which can cascade into a lot of positive things,” Canu said.
Treatments include behavioral strategies for managing their symptoms, for which working with an expert, such as a psychologist who is experienced in treating patients with ADHD, can be invaluable. This includes cognitive behavioral therapy for ADHD, which focuses on managing executive functioning difficulties such as time management, organizational skills, impulse control, and emotional self-regulation.
When necessary, medication can also help manage symptoms. For psychologists who do not have prescribing privileges, this can mean working in concert with integrated care teams, primary-care providers, or psychiatrists. For many patients, their most effective treatment regimen is a combination of behavioral strategies and medication. “With that in place, if it’s effective, they’re able to function better,” Canu said.
In a 2014 study, 250 previously nonmedicated adults who received the ADHD medication methylphenidate for the first time were followed for a full year, with those patients who either couldn’t tolerate or didn’t experience relief in symptoms switched to either an alternate stimulant medication or the nonstimulant medication atomoxetine. Compared with their peers who discontinued medication, those who were still on medication had reduced severity of symptoms ( Fredriksen, M., et al., European Neuropsychopharmacology , Vol. 24, No. 12, 2014 ). “Medication slows me down enough to breathe and to think,” Green said.
Dealing with late-life diagnosis
Receiving a diagnosis as an adult can often bring up some complicated emotions, whether it’s grief over lost opportunities, relief at finally understanding certain struggles, or anger over symptoms having been overlooked for so long. For Matlen, she felt an overwhelming sense of relief. “There was a concrete explanation,” she said.
For others, receiving a diagnosis later in life can lead to regrets about lost opportunities, whether it was failing out of school, struggling to establish a career, or experiencing relationship issues because of their ADHD symptoms going overlooked and untreated. “There is a lot of grief work that needs to be done to help work through the many years of struggling and not knowing why,” Matlen said. However, in her experience, “Once all those parts and pieces are looked at with this new understanding, people really take off, in a good way,” she said. Often, therapy is an important component of thriving after a diagnosis.
For Matlen, in addition to gaining a better understanding of why she was struggling so much, receiving a diagnosis and treatment changed her entire life. It ended up being the missing piece that helped ease her anxiety. Once she had a diagnosis and started treatment, her issues with anxiety started improving in a way that years of therapy and antianxiety medication had never been able to accomplish.
Given how life-changing her diagnosis was, combined with the lack of information and resources available, especially for women, Matlen ultimately made a career switch, combining her own experience of growing up with undiagnosed ADHD with her background as a clinical social worker. She went on to write the books The Queen of Distraction and Survival Tips for Women With AD/HD . She also founded a Facebook group for women with ADHD, which now has over 36,000 members, and she often consults with specialists on the realities of living with ADHD.
Now, almost 30 years after her initial diagnosis, Matlen still hasn’t seen nearly as much progress in the field as she had hoped, especially for girls and women. “I see the same stories even now,” she said.
Further reading
Meta-analysis of cognitive–behavioral treatments for adult ADHD Knouse, L. E., et al., Journal of Consulting and Clinical Psychology , 2017
Association between psychiatric symptoms and executive function in adults with attention deficit hyperactivity disorder Arellano-Virto, P. T., et al., Psychology & Neuroscience , 2021
The ADHD Symptom Infrequency Scale (ASIS): A novel measure designed to detect adult ADHD simulators Courrégé, S. C., et al., Psychological Assessment , 2019
A randomized controlled trial examining CBT for college students with ADHD Anastopoulos, A. D., et al., Journal of Consulting and Clinical Psychology , 2021
Succeeding With Adult ADHD: Daily Strategies to Help You Achieve Your Goals and Manage Your Life Levrini, A., APA LifeTools Series, 2023
Recommended Reading

Related topic
Six things psychologists are talking about.
The APA Monitor on Psychology ® sister e-newsletter offers fresh articles on psychology trends, new research, and more.
Welcome! Thank you for subscribing.
Speaking of Psychology
Subscribe to APA’s audio podcast series highlighting some of the most important and relevant psychological research being conducted today.
Subscribe to Speaking of Psychology and download via:

Contact APA
You may also like.

Faculty and Disclosures
Disclosure of conflicts of interest, disclosure of unlabeled use.

Attention-deficit Hyperactivity Disorder (ADHD): Two Case Studies
- Authors: Authors: Joseph Biederman, MD; Stephen V. Faraone, PhD
- THIS ACTIVITY HAS EXPIRED FOR CREDIT
Target Audience and Goal Statement
This activity has been designed to meet the educational needs of pediatricians, family practitioners, child and adolescent psychiatrists, and general psychiatrists involved in the management of patients with ADHD.
Attention-deficit hyperactivity disorder (ADHD) is a chronic condition that affects 8% to 12% of school-aged children and contributes significantly to academic and social impairment. There is currently broad agreement on evidence-based best practices of ADHD identification and diagnosis, therapeutic approach, and monitoring. However, the increasing rate of diagnosis and treatment in the pediatric population has contributed to the significant public debate and misunderstanding of ADHD. Despite increased awareness, Attention-deficit hyperactivity disorder (ADHD) is a chronic condition that affects 8% to 12% of school-aged children and contributes significantly to academic and social impairment. There is currently broad agreement on evidence-based best practices of ADHD identification and diagnosis, therapeutic approach, and monitoring. However, the increasing rate of diagnosis and treatment in the pediatric population has contributed to the significant public debate and misunderstanding of ADHD. Despite increased awareness, ADHD remains underrecognized and may be undertreated by a factor of 10 to 1 in the US population. In order to educate the public and ensure optimal outcomes for ADHD patients, this continuing education activity has been developed to provide physicians and other healthcare providers with the most current information available on assessing and treating ADHD.
Upon completion of this activity, participants should be able to:
- Discuss the incidence of ADHD in adolescents and adults.
- Identify DSM-IV criteria used to make the diagnosis of ADHD in each age group.
- List important comorbidities of ADHD and identify distinguishing features between ADHD and other psychiatric diagnoses with similar manifestations.
- Describe a pharmacologic approach to ADHD treatment, including treatment goals and choice of medication.
- Enumerate self-management skills to be recommended when coaching ADHD patients on how to get along at school, at work, and at home.
Disclosures
Accreditation statements, for physicians.
This activity has been planned and implemented in accordance with the Essential Areas and Policies of the Accreditation Council for Continuing Medical Education (ACCME). The Postgraduate Institute for Medicine is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians.
The Postgraduate Institute for Medicine designates this educational activity for a maximum of 1.0 Category 1 credit toward the AMA Physician's Recognition Award. Each physician should claim only those credits that he/she actually spent in the activity.
Contact This Provider
For questions regarding the content of this activity, contact the accredited provider for this CME/CE activity noted above. For technical assistance, contact [email protected]
Instructions for Participation and Credit
There are no fees for participating in or receiving credit for this online educational activity. For information on applicability and acceptance of continuing education credit for this activity, please consult your professional licensing board. This activity is designed to be completed within the time designated on the title page; physicians should claim only those credits that reflect the time actually spent in the activity. To successfully earn credit, participants must complete the activity online during the valid credit period that is noted on the title page. Follow these steps to earn CME/CE credit*:
- Read the target audience, learning objectives, and author disclosures.
- Study the educational content online or printed out.
- Online, choose the best answer to each test question. To receive a certificate, you must receive a passing score as designated at the top of the test. In addition, you must complete the Activity Evaluation to provide feedback for future programming.
You may now view or print the certificate from your CME/CE Tracker. You may print the certificate but you cannot alter it. Credits will be tallied in your CME/CE Tracker and archived for 5 years; at any point within this time period you can print out the tally as well as the certificates by accessing "Edit Your Profile" at the top of your Medscape homepage. *The credit that you receive is based on your user profile.
- Policy Statement for Documentation of Attention-Deficit/Hyperactivity Disorder in Adolescents and Adults (Revised). Princeton, NJ: Office of Disability Policy, Educational Testing Service; June 1999.
- American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 4th ed (DSM-IV). Washington, DC: APA, 2000.
- Dulcan MK, Benson RS. AACAP Official Action. Summary of the practice parameters for the assessment and treatment of children, adolescents, and adults with ADHD. J Am Acad Child Adolesc Psychiatry. 1997;36:1311-7.
- Elia J, Ambrosini PJ, Rapoport JL. Treatment of attention-deficit-hyperactivity disorder. N Engl J Med. 1999;340:780-8.
- Wender PH. Pharmacotherapy of attention-deficit/hyperactivity disorder in adults. J Clin Psychiatry. 1998;59 Suppl 7:76-9.
- Wilens TE, Biederman J, Lerner M; et al. Effects of once-daily osmotic-release methylphenidate on blood pressure and heart rate in children with attention-deficit/hyperactivity disorder: results from a one-year follow-up study. J Clin Psychopharmacol. 2004;24:36-41.
- Searight HR, Burke JM, Rottnek F. Adult ADHD: evaluation and treatment in family medicine. Am Fam Physician. 2000;62:2077-86, 2091-2.
- Biederman J, Faraone SV, Monuteaux MC, et al. Growth deficits and attention-deficit/hyperactivity disorder revisited: Impact of gender, development, and treatment. Pediatrics. 2003;111:1010-6.
- Spencer T, Biederman J, Wilens T. Growth deficits in children with attention deficit hyperactivity disorder. Pediatrics. 1998;102:501-6.
- Spencer T, Biederman J, Harding M, et al. Growth deficits in ADHD children revisited: evidence for disorder-associated growth delays? J Am Acad Child Adolesc Psychiatry. 1996;35:1460-9.
- Hechtman L, Greenfield B. Long-term use of stimulants in children with attention deficit hyperactivity disorder: safety, efficacy, and long-term outcome. Paediatr Drugs. 2003;5:787-94.
- Spencer T, Biederman, M, Coffey B, et al. The 4-year course of tic disorders in boys with attention-deficit/hyperactivity disorder. Arch Gen Psychiatry. 1999;56:842-7.
- Biederman J, Faraone SV, Spencer T. Pharmacotherapy of attention-deficit/hyperactivity disorder reduces risk for substance use disorder. Pediatrics. 1999;104:e20.
- Biederman J, Willens TE, Mick E, et al. Does attention-deficit hyperactivity disorder impact the developmental course of drug and alcohol abuse and dependence? Biol Psychiatry. 1998;44:269-73.
- Greene RW, Biederman J, Faraone SV, et al. Adolescent outcome of boys with attention-deficit/hyperactivity disorder and social disability: results from a 4-year longitudinal follow-up study. J Consult Clin Psychol. 1997;65:758-67.
- Wilens TE, Biederman J, Mick E, et al. Attention deficit hyperactivity disorder (ADHD) is associated with early onset substance use disorders. J Nerv Ment Dis. 1997 Aug;185:475-82.
- Clure C, Brady KT, Saladin ME, et al. Attention-deficit/hyperactivity disorder and substance use: symptom pattern and drug choice. Am J Drug Alcohol Abuse. 1999;25:441-8.
- Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit/hyperactivity disorder: a meta-analysis of follow-up studies. Psychological Medicine. In press.
- Kessler RC, Adler L, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: results from the national comorbidity survey replication. Am J Psychiatry. In press.
- Biederman J, Faraone SV, Mick E, et al. Clinical correlates of ADHD in females: findings from a large group of girls ascertained from pediatric and psychiatric referral sources. J Am Acad Child Adolesc Psychiatry. 1999;38:966-75.
- Weiss G, Hechtman L. Adult hyperactive subjects' view of their treatment in childhood and adolescence. In: G. Weiss and L. Hechtman, eds. Hyperactive Children Grown Up: ADHD in Children, Adolescents, and Adulthood, 2nd ed. New York, NY: The Guilford Press; 1993.
- Mannuzza S, Klein RG, Bessler A, et al. Adult outcome of hyperactive boys: educational achievement, occupational rank, and psychiatric status. Arch Gen Psychiatry. 1993;50:565-76.
- Biederman J. Impact of Comorbidity in Adults with ADHD. J Clin Psychiatry. 2004(Suppl 3);65:3-7.
- Murphy K, Barkley RA. Attention deficit hyperactivity disorder adults: comorbidities and adaptive impairments. Compr Psychiatry. 1996;37:393-401.
- Biederman J, Faraone SV, Spencer T, et al. Patterns of psychiatric comorbidity, cognition, and psychosocial functioning in adults with attention deficit hyperactivity disorder. Am J Psychiatry. 1993;150:1792-8.
- Shekim WO, Asarnow RF, Hess E, et al. A clinical and demographic profile of a sample of adults with attention deficit hyperactivity disorder, residual state. Compr Psychiatry. 1990;31:416-25.
- Hornig M. Addressing comorbidity in adults with attention-deficit/hyperactivity disorder. J Clin Psychiatry. 1998;59:769-75.
- Angold A, Costello EJ, Erkanli A. Comorbidity. J Child Psychol Psychiatry. 1999;40:57-87.
- Pliszka SR, Carlson CL, Swanson JM. ADHD With Comorbid Disorders: Clinical Assessment and Management. New York, NY: The Guilford Press; 1999.

Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- PubMed/Medline
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
A case study in attention-deficit/hyperactivity disorder: an innovative neurofeedback-based approach.

1. Introduction
1.1. evaluation of adhd, 1.2. adhd intervention, 2. methodology, 2.1. description of the case, 2.1.1. patient identification, 2.1.2. reason for consultation, 2.1.3. history of the problem, 2.2. proposed evaluation and intervention, 2.2.1. evaluation: brainwave analysis with the miniq instrument, 2.2.2. intervention: neurofeedback protocols, 3.1. brainwave evaluation, 3.2. progression following neurofeedback intervention, 4. discussion, 5. conclusions, author contributions, institutional review board statement, informed consent statement, data availability statement, conflicts of interest.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders , 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [ Google Scholar ]
- Mirsky, A.F. Disorders of attention: A neuropsychological perspective. In Attention, Memory and Executive Function ; Lyon, R.G., Kranesgor, N.A., Eds.; Paul, H. Brookes: Baltimore, MD, USA, 1996; pp. 71–95. [ Google Scholar ]
- Barkley, R.A. Behavioral inhibition, sustained attention, and executive functions: Constructing a unifying theory of ADHD. Psychol. Bull. 1997 , 121 , 65–94. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems , 11th ed.; World Health Organization: Geneva, Switzerland, 2019. [ Google Scholar ]
- Klem, G.H.; Lüders, H.O.; Jasper, H.H.; Elger, C. The ten-twenty electrode system of the International Federation. The International Federation of Clinical Neurophysiology. Electroencephalogr. Clin. Neurophysiol. 1999 , 52 , 3–6. [ Google Scholar ]
- Lubar, J.F. Neurofeedback for the management of attention deficit disorders. In Biofeedback: A Practitioner’s Guide , 3rd ed.; Schwartz, M.S., Andrasik, F., Eds.; Guilford Press: New York, USA, 2003; pp. 409–443. [ Google Scholar ]
- Monastra, V.J.; Lubar, J.F.; Linden, M.; VanDeusen, P.; Green, G.; Wing, W.; Phillips, A.; Fenger, T.N. Assessing attention deficit hyperactivity disorder via quantitative electroencephalography: An initial validation study. Neuropsychology. 1999 , 13 , 424–433. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Martella, D.; Aldunate, N.; Fuentes, L.J.; Sánchez-Pérez, N. Arousal and executive alterations in attention deficit hyperactivity disorder (ADHD). Front. Psychol. 2020 , 11 , 1991. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Rodríguez, C.; González-Castro, P.; Cueli, M.; Areces, D.; González-Pienda, J.A. Attention deficity/hyperactivity disorder (ADHD) diagnosis: An activation-execution model. Front. Psychol. 2016 , 7 , 1406. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Clarke, A.; Barry, R.; McCarthy, R.; Selikowitz, M. Age and sex effects in the EEG: Development of the normal child. Clin. Neurophysiol. 2001 , 112 , 806–814. [ Google Scholar ] [ CrossRef ]
- Clarke, A.R.; Barry, R.J.; Johnstone, S.J.; McCarthy, R.; Selikowitz, M. EEG development in attention deficit hyperactivity disorder: From child to adult. Clin. Neurophysiol. 2019 , 130 , 1256–1262. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kerson, C.; deBeus, R.; Lightstone, H.; Arnold, L.E.; Barterian, J.; Pan, X.; Monastra, V.J. EEG theta/beta ratio calculations differ between various EEG neurofeedback and assessment software packages: Clinical interpretation. Clin. EEG Neurosci. 2020 , 51 , 114–120. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Caye, A.; Swanson, J.M.; Coghill, D.; Rohde, L.A. Treatment strategies for ADHD: An evidence-based guide to select optimal treatment. Mol. Psychiatry 2019 , 24 , 390–408. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Arns, M.; Heinrich, H.; Strehl, U. Evaluation of neurofeedback in ADHD: The long and winding road. Biol. Psychol. 2014 , 95 , 108–115. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Arns, M.; Clark, C.R.; Trullinger, M.; deBeus, R.; Mack, M.; Aniftos, M. Neurofeedback and attention-defcit/hyperactivity-disorder (ADHD) in children: Rating the evidence and proposed guidelines. Appl. Psychophysiol. Biofeedback 2020 , 45 , 39–48. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Cueli, M.; Rodríguez, C.; Cabaleiro, P.; García, T.; González-Castro, P. Differential efficacy of neurofeedback in children with ADHD presentations. J. Clin. Med. 2019 , 8 , 204. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Lubar, J.F.; Shouse, M.N. EEG and behavioral changes in a hyperkinetic child concurrent with training ofthe sensorimotor rhythm (SMR): A preliminary report. Biofeedback Self-Regul. 1976 , 1 , 293–306. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- González-Castro, P.; Cueli, M.; Rodríguez, C.; García, T.; Álvarez, L. Efficacy of neurofeedback versus pharmacological support in subjects with ADHD. Appl. Psychophysiol. Biofeedback 2016 , 41 , 17–25. [ Google Scholar ] [ CrossRef ]
- Lambez, B.; Harwood-Gross, A.; Golumbic, E.Z.; Rassovsky, Y. Non-pharmacological interventions for cognitive difficulties in ADHD: A systematic review and meta-analysis. J. Psychiatry Res. 2020 , 120 , 40–55. [ Google Scholar ] [ CrossRef ]
- Yan, L.; Wang, S.; Yuan, Y.; Zhang, J. Effects of neurofeedback versus methylphenidate for the treatment of ADHD: Systematic review ad meta-analysis of head-to-head trials. Medicine 2019 , 97 , 12623. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Van Doren, J.; Arns, M.; Heinrich, H.; Vollebregt, M.A.; Strehl, U.; Loo, L.K. Sustained effects of neurofeedback in ADHD: A systematic review and meta-analysis. Eur. Child Adolesc. Psychiatry 2019 , 28 , 293–305. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Vivani, G.; Vallesi, A. EEG-neurofeedback and executive function enhancement in healthy adults: A systematic review. Psychophysiology 2021 , 58 , 13874. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Danielson, M.L.; Visser, S.N.; Chronis-Tuscano, A.; DuPaul, G.J. A national description of treatment among United States children and adolescents with attention-deficit/hyperactivity disorder. J. Pediatrics 2018 , 192 , 240–246. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Enriquez-Geppert, S.; Smit, D.; Garcia-Pimenta, M.; Arns, A. Neurofeedback as a treatment intervention in ADHD: Current evidence and practice. Curr. Psychiatry Rep. 2019 , 21 , 46. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Duric, N.S.; Abmus, J.; Elgen, I.B. Self-reported efficacy of neurofeedback treatment in a clinical randomized controlled study of ADHD children and adolescents. Neuropsychiatr. Dis. Treat. 2014 , 10 , 1645–1654. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Sterman, M.B. Epilepsy and its treatment with EEG feedback therapy. Ann. Behav. Med. 1986 , 8 , 21–25. [ Google Scholar ] [ CrossRef ]
- Jarrett, M.A.; Gable, P.A.; Rondon, A.T.; Neal, L.B.; Price, H.F.; Hilton, D.C. An EEG study of children with and without ADHD symptoms: Between-group differences and associations with sluggish cognitive tempo symptoms. J. Atten. Disord. 2017 , 24 , 1002–1010. [ Google Scholar ] [ CrossRef ]
- van Dijk, H.; deBeus, R.; Kerson, C.; Roley-Roberts, M.E.; Monastra, V.J.; Arnold, L.E.; Pan, X.; Arns, M. Different spectral analysis methods for the theta/beta ratio calculate different ratios but do not distinguish ADHD from controls. Appl. Psychophysiol. Biofeedback 2020 , 45 , 165–173. [ Google Scholar ] [ CrossRef ]
- Janssen, T.W.P.; Bink, M.; Weeda, W.D.; Geladé, K.; van Mourik, R.; Maras, A.; Oosterlaan, J. Learning curves of theta/beta neurofeedback in children with ADHD. Eur. Child Adolesc. Psychiatry 2017 , 26 , 573–582. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Doppelmayr, M.; Weber, E. Effects on SMR and theta/beta neurofeedback on reaction times, spatial abilities and creativity. J. Neurother. 2011 , 15 , 115–129. [ Google Scholar ] [ CrossRef ]
- Vernon, D.; Egner, T.; Cooper, N.; Compton, T.; Neilands, C.; Sheri, A.; Gruzelier, J. The effect of training distinct neurofeedback protocols on aspects of cognitive performance. Int. J. Psychophysiol. 2003 , 47 , 75–85. [ Google Scholar ] [ CrossRef ]
- Gevensleben, H.; Holl, B.; Albrecht, B.; Schlamp, D.; Kratz, O.; Studer, P.; Wangler, S.; Rothenberger, A.; Moll, G.H.; Heinrich, H. Distinct EEG effects related to neurofeedback training in children with ADHD: A randomized controlled trial. Int. J. Psychophysiol. 2009 , 74 , 149–157. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Leins, U.; Goth, G.; Hinterberger, T.; Klinger, C.; Rumpf, N.; Strehl, U. Neurofeedback for children with ADHD: A comparison of SCP and theta/beta protocols. Appl. Psychophysiol. Biofeedback 2007 , 32 , 73–88. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Cortese, S.; Ferrin, M.; Brandeis, D.; Holtmann, M.; Aggensteiner, P.; Daley, D.; Santosh, P.; Simonoff, E.; Stevenson, J.; Stringaris, A.; et al. Neurofeedback for attention-deficit/hyperactivity disorder: Meta-Analysis of clinical and neuropsychological outcomes from randomized controlled trials. J. Am. Acad. Child Adolesc. Psychiatry 2016 , 55 , 444–455. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Logemann, H.N.; Lansbergen, M.M.; Van Os, T.W.; Bocker, K.B.; Kenemans, J.L. The effectiveness of EEG-feedback on attention, impulsivity and EEG: A sham feedback controlled study. Neurosci. Lett. 2010 , 479 , 49–53. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Holtmann, M.; Pniewski, B.; Wachtlin, D.; Wörz, S.; Strehl, U. Neurofeedback in children with attention-deficit/hyperactivity disorder (ADHD)–A controlled multicenter study of a non-pharmacological treatment approach. BMC Pediatrics 2014 , 14 , 202. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Su, Y.; Li, H.; Chen, Y.; Fang, F.; Xu, T.; Lu, H.; Xie, L.; Zhuo, J.; Qu, J.; Yang, L.; et al. Remission rate and functional outcomes during a 6-month treatment with osmotic-release oral-system methylphenidate in children with attention-deficit/hyperactivity disorder. J. Clin. Psychopharmacol. 2015 , 35 , 525–534. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Blume, F.; Hudak, J.; Dresler, T.; Ehlis, A.C.; Kühnhausen, J.; Renner, T.J.; Gawrilow, C. NIRS-based neurofeedback training in a virtual reality classroom for children with attention-deficit/hyperactivity disorder: Study protocol for a randomized controlled trial. Trials 2017 , 18 , 41. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
Click here to enlarge figure
| MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
Share and Cite
Cabaleiro, P.; Cueli, M.; Cañamero, L.M.; González-Castro, P. A Case Study in Attention-Deficit/Hyperactivity Disorder: An Innovative Neurofeedback-Based Approach. Int. J. Environ. Res. Public Health 2022 , 19 , 191. https://doi.org/10.3390/ijerph19010191
Cabaleiro P, Cueli M, Cañamero LM, González-Castro P. A Case Study in Attention-Deficit/Hyperactivity Disorder: An Innovative Neurofeedback-Based Approach. International Journal of Environmental Research and Public Health . 2022; 19(1):191. https://doi.org/10.3390/ijerph19010191
Cabaleiro, Paloma, Marisol Cueli, Laura M. Cañamero, and Paloma González-Castro. 2022. "A Case Study in Attention-Deficit/Hyperactivity Disorder: An Innovative Neurofeedback-Based Approach" International Journal of Environmental Research and Public Health 19, no. 1: 191. https://doi.org/10.3390/ijerph19010191
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
0203 326 9160
Childhood ADHD – Luke’s story
Posted on Thursday, 05 April 2018, in Child & Teen ADHD

In the final part of her ADHD series, Dr Sabina Dosani, Child and Adolescent Psychiatrist and Clinical Partner London, introduces Luke, a patient she was able to help with his ADHD.
ADHD is one of the most common diagnoses for children in the UK and it is thought that 1 in 10 children will display some signs. For some children, their ADHD is severe and can have a huge impact on their ability to engage in school and to build and sustain relationships. Left untreated, evidence shows that those with ADHD are more likely to get into car accidents, engage in criminal activity and may struggle to keep a job or maintain relationships.
Luke, aged six, gets into trouble a lot at school. His mother gets called by his teacher three or four times a week for incidents of fighting, kicking and running in corridors. He is unable to finish his work and becomes quickly distracted. At home, he seems unable to sit still for any length of time, has had several falls when climbing trees and needs endless prompts to tidy his toys.
At school, he annoys his classmates by his constant interruptions, however if he has one-to-one attention from a student teacher who happens to be in his class on a placement he is able to settle and finish the work set. His father was said to have been a ‘lively’ child, then a ‘bright underachiever’ who occasionally fell foul of the law.
The school thought a visit to the GP might be a good idea. At the GP surgery, Luke ran and jumped about making animal noises. He swung on the back legs of a chair and took the batteries out of an ophthalmoscope. He was referred to a me for an assessment.
After a careful assessment, which included collecting information from school, questionnaires and observations of Luke, a diagnosis of ADHD was made. Following a discussion of the treatment options, the family decided they did not want any medication.
The first-line treatment for school‑age children and young people with severe ADHD and severe impairment is drug treatment. If the family doesn’t want to try a pharmaceutical, a psychological intervention alone is offered but drug treatment has more benefits and is superior to other treatments for children with severe ADHD.

Luke's mother was asked to list the behaviours that most concern her. She was encouraged to accept others like making noises or climbing as part of Luke’s development as long as it is safe.
Now, when Luke fights, kicks others or takes risks like running into the road he is given “time-out” which isolates him for a short time and allows him and his parents or teacher to calm down. To reduce aggression and impulsivity, Luke is taught to respond verbally rather than physically and channel energy into activities such as sports or energetic percussion playing.
Over time, Luke’s parents have become skilled at picking their battles. Home is more harmonious. They fenced their garden, fitted a childproof gate and cut some branches off a tree preventing him climbing it. His parents are concerned about Luke’s use of bad language. They have been supported to allow verbal responses as a short-term interim. Whilst these might be unacceptable in other children they are preferable to physical aggression.
At school, Luke is less aggressive, has a statement of special educational need and now works well with a classroom assistant. He has been moved to the front of the class, where the teacher can keep a close eye on him, and given one task at a time. He is given special tasks, like taking the register to the school office, so he can leave class without being expected to sit still for long periods.
Through parental training, Luke’s parents have been able to help Luke work with his challenges to better manage them. As Luke grows and develops and as he faces new challenges in life, Luke may need to revisit the efficacy of ADHD medication. His parents now feel a lot more confident in being able to help Luke and he is a happier child and more settled.

Dr Sabina Dosani Consultant Child & Adolescent Psychiatrist
Dr Sabina Dosani is a highly experienced Consultant Psychiatrist currently working for the Anna Freud Centre looking after Children and Adolescents. She has a Bachelor of Medicine and Bachelor of Surgery as well as being a member of the Royal College of Psychiatrists . Dr Dosani also has a certificate in Systemic Practice (Family Therapy).
Related Articles
- The real reason you need to take adult ADHD seriously
- 10 signs your child might have ADHD
- What causes ADHD?
- Why is ADHD in women undiagnosed so often?
- Anxiety & Stress (14)
- Behavioural Issues (5)
- Bipolar Disorder (3)
- Child Autism (14)
- Child & Teen ADHD (7)
- Child & Teen Anxiety (12)
- Child & Teen Depression (3)
- Depression (3)
- Eating Disorders (2)
- Education & Mental Health (2)
- Maternal Health (2)
- Parenting & Families (16)
- Treatments & Therapy (20)
Already a patient?
Sign in to manage your care
Learn more and see openings
Work with us as a clinician?
Sign in to your clinician portal
- Research article
- Open access
- Published: 12 August 2020
Females with ADHD: An expert consensus statement taking a lifespan approach providing guidance for the identification and treatment of attention-deficit/ hyperactivity disorder in girls and women
- Susan Young ORCID: orcid.org/0000-0002-8494-6949 1 , 2 ,
- Nicoletta Adamo 3 , 4 ,
- Bryndís Björk Ásgeirsdóttir 2 ,
- Polly Branney 5 ,
- Michelle Beckett 6 ,
- William Colley 7 ,
- Sally Cubbin 8 ,
- Quinton Deeley 9 , 10 ,
- Emad Farrag 11 ,
- Gisli Gudjonsson 2 , 12 ,
- Peter Hill 13 ,
- Jack Hollingdale 14 ,
- Ozge Kilic 15 ,
- Tony Lloyd 16 ,
- Peter Mason 17 ,
- Eleni Paliokosta 18 ,
- Sri Perecherla 19 ,
- Jane Sedgwick 3 , 20 ,
- Caroline Skirrow 21 , 22 ,
- Kevin Tierney 23 ,
- Kobus van Rensburg 24 &
- Emma Woodhouse 10 , 25
BMC Psychiatry volume 20 , Article number: 404 ( 2020 ) Cite this article
231k Accesses
149 Citations
700 Altmetric
Metrics details
There is evidence to suggest that the broad discrepancy in the ratio of males to females with diagnosed ADHD is due, at least in part, to lack of recognition and/or referral bias in females. Studies suggest that females with ADHD present with differences in their profile of symptoms, comorbidity and associated functioning compared with males. This consensus aims to provide a better understanding of females with ADHD in order to improve recognition and referral. Comprehensive assessment and appropriate treatment is hoped to enhance longer-term clinical outcomes and patient wellbeing for females with ADHD.
The United Kingdom ADHD Partnership hosted a meeting of experts to discuss symptom presentation, triggers for referral, assessment, treatment and multi-agency liaison for females with ADHD across the lifespan.
A consensus was reached offering practical guidance to support medical and mental health practitioners working with females with ADHD. The potential challenges of working with this patient group were identified, as well as specific barriers that may hinder recognition. These included symptomatic differences, gender biases, comorbidities and the compensatory strategies that may mask or overshadow underlying symptoms of ADHD. Furthermore, we determined the broader needs of these patients and considered how multi-agency liaison may provide the support to meet them.
Conclusions
This practical approach based upon expert consensus will inform effective identification, treatment and support of girls and women with ADHD. It is important to move away from the prevalent perspective that ADHD is a behavioural disorder and attend to the more subtle and/or internalised presentation that is common in females. It is essential to adopt a lifespan model of care to support the complex transitions experienced by females that occur in parallel to change in clinical presentation and social circumstances. Treatment with pharmacological and psychological interventions is expected to have a positive impact leading to increased productivity, decreased resource utilization and most importantly, improved long-term outcomes for girls and women.
Peer Review reports
Attention-deficit/hyperactivity disorder (ADHD) is a common neurodevelopmental condition described in diagnostic classification systems (ICD-10, DSM-5 [ 1 , 2 ]). It is characterised by difficulties in two subdomains: inattention, and hyperactivity-impulsivity. Three primary subtypes can be identified: predominantly inattentive, hyperactive-impulsive, and combined presentations. Symptoms persist over time, pervade across situations and cause significant impairment [ 3 ].
ADHD is present in childhood and symptoms tend to decline with increasing age [ 4 ], with consistent reductions documented in hyperactive-impulsive symptoms but more mixed results regarding the decline in inattentive symptoms [ 5 , 6 , 7 ]. This trajectory does not appear to be different in affected males or females [ 6 , 8 ]. A meta-analysis of longitudinal studies published in 2005 showed that up to one-third of childhood cases continued to meet full diagnostic criteria into their 20s, with around 65% continuing to experience impairing symptoms [ 9 ]. More recent studies in large clinical cohorts indicate that persistence of ADHD into adulthood may be much more common. Two studies from child mental health clinics in the UK and the Netherlands have reported persistence in around 80% of children with the combined type presentation into early adulthood [ 10 , 11 ], potentially relating to the high severity of ADHD in this group and the use of more objective ratings [ 12 ]. The proportion meeting full diagnostic criteria for ADHD then continues to decline in adult samples [ 13 ]. Simultaneously, experiences of ADHD symptoms often change over the course of development: hyperactivity may be replaced by feelings of ‘inner restlessness’ and discomfort; inattention may manifest as difficulty completing chores or work-based activities (e.g. filling out forms, remembering appointments, meeting deadlines) [ 1 ].
Psychiatric comorbidity is very common, which may complicate identification and treatment [ 14 ]. In children with ADHD this includes conduct disorder (CD), oppositional defiant disorder (ODD), disruptive mood dysregulation disorder, autism spectrum disorder (ASD), developmental coordination disorder, tic disorders, anxiety and depressive disorders, reading disorders, and learning and language disorders [ 15 , 16 , 17 ]. Comorbid conditions are also extremely common in adults and include ASD, anxiety and depressive disorders, bipolar disorder, eating disorders, obsessive compulsive disorder, substance use disorders, personality disorders, and impulse control disorders [ 18 , 19 ].
Prevalence of ADHD is estimated at 7.1% in children and adolescents [ 20 ], and 2.5-5% in adults [ 4 , 21 ], and around 2.8% in older adults [ 22 ]. Sex differences in the prevalence of ADHD are well documented. Clinical referrals in boys typically exceed those for girls, with ratios ranging from 3-1 to 16-1 [ 23 ]. The discrepancy of ADHD rates in community samples remains significant, although it is less extreme, at around a 3-1 ratio of boys to girls [ 4 ]. Nevertheless the discrepancy in the sex-ratio between clinic and community samples highlights that a large number of girls with ADHD are likely to remain unidentified and untreated, with implications for long-term social, educational and mental health outcomes [ 24 ].
This disparity in prevalence between boys and girls may stem from a variety of potential factors. The contribution of greater genetic vulnerability, endocrine factors, psychosocial contributors, or a propensity to respond negatively to certain early life stressors in boys have been proposed or investigated as potential contributors to sexual dimorphism in prevalence and presentation [ 25 , 26 ]. Whilst in childhood there is a clear male preponderance of ADHD, in adult samples sex differences in prevalence are more modest or absent [ 21 , 27 , 28 , 29 ]. This may be due to a variety of factors, with potential contributions from the greater reliance on self-report in older samples, greater persistence in females alongside increased levels of remission in males, and potentially more common late onset cases in females [ 25 , 26 , 28 ].
Comprehensive views of the aetiology of ADHD incorporate biological, environmental and cultural perspectives and influences [ 25 ]. Substantial genetic influences have been identified in ADHD [ 30 ]. Individuals who have ADHD are more likely to have children, parents and/or siblings with ADHD [ 31 , 32 ]. The ‘female protective effect’ theory suggests that girls and women may need to reach a higher threshold of genetic and environmental exposures for ADHD to be expressed, thereby accounting for the lower prevalence in females and the higher familial transmission rates seen in families where females are affected [ 33 , 34 ]. Research suggests that siblings of affected girls have more ADHD symptoms compared with siblings of affected boys [ 33 , 34 ].
There is increasing recognition that females with ADHD show a somewhat modified set of behaviours, symptoms and comorbidities when compared with males with ADHD; they are less likely to be identified and referred for assessment and thus their needs are less likely to be met. It is unknown how often a diagnosis of ADHD is being missed or misdiagnosed in females, but it has become clear that a better understanding of ADHD in girls and women is needed if we are to improve their longer-term wellbeing and functional and clinical outcomes [ 35 , 36 ].
This report provides a selective review the research literature on ADHD in girls and women, and aims to provide guidance to improve identification, treatment and support for girls and women with ADHD across the lifespan, developed through a multidisciplinary consensus meeting according to the clinical expertise and knowledge among attendees. To support medical and mental health practitioners in their understanding of ADHD in females, we provide consensus guidance on the presentation of ADHD in females and triggers for referral. We establish specific advice regarding the assessment, interventions, and multi-agency liaison needs in girls and women with ADHD.
In line with previous definitions, we use the terms sex to identify a biological category (male/female), and gender to define a social role and cultural-social properties [ 37 ]. However, we acknowledge the complex differences between the sexes that occur independently of ADHD status [ 38 ], and discuss both biological differences and social roles in the current consensus.
The consensus aimed to provide practical guidance to professionals working with girls and women with ADHD, drawing on the scientific literature and the professional experience of the authors. To achieve this aim, professionals specialising in ADHD convened in London on 30th November 2018 for a meeting hosted by the United Kingdom ADHD Partnership (UKAP; www.UKADHD.com ). Meeting attendees included experts in ADHD across a range of mental health professions, including healthcare specialists (nursing; general practice; child, adolescent and adult psychiatry; clinical and forensic psychology; counselling), academic, educational and occupational specialists. Service-users and ADHD charity workers were also represented. Attendees engaged in discussions throughout the day, with the aim of reaching consensus.
The meeting commenced with presentations of preliminary data obtained from (1) an ongoing systematic review on the clinical and psychosocial presentation of females in comparison with males with ADHD (currently being led by SY and OK); and (2) epidemiological research on sex differences in self-reported ADHD symptoms in population based adolescent cohorts. Following a question and answer session, attendees then separated into three breakout groups. Each group was tasked with providing practical solutions relevant to their assigned topic. Discussions were facilitated by group leaders and summarized by note-takers. Following the small-group work, all attendees re-assembled. Group leaders then presented findings to all meeting attendees for another round of discussion and debate, until consensus was reached. Group discussions included the following themes:
1: Identification and assessment of ADHD in females
Presentation in females and what might trigger referral?
Considering sex differences when conducting ADHD assessments
2: Interventions and treatments for ADHD in females
Pharmacological
Non-pharmacological
3: Multi-agency liaison
Educational considerations
Other multi-agency considerations
Taking a lifespan perspective, each theme was explored in relation to specific age groups considered to be associated with pertinent periods for environmental and biological change, and change in clinical needs and presentation. Recommendations that differed between age groups are presented separately.
The consensus group incorporated evidence from a broad range of sources. However, the assessment, pharmacological treatment, and multiagency support features reflect clinical practice and legislature in the United Kingdom (UK), and may differ in other countries.
All consensus proceedings, including group and feedback sessions were video-recorded and transcribed. One note-taker was allocated to each breakout group, and notes were subsequently circulated to each breakout group contributor for review and agreement. All materials were sent to the medical writer, who consolidated the meeting transcription, electronic slide presentations and small-group notes. The lead author worked closely with the medical writer to synthesise the consensus report, which was then circulated to all authors for review and feedback. A final draft was circulated to all authors for agreement and approval.
Results and consensus outcome
Presentation of adhd in females.
Although much of the scientific literature indicates an overlap in the clinical presentation of males and females with ADHD, the available evidence often draws on predominantly male samples [ 39 ] due to the higher prevalence of ADHD in males [ 4 ]. Some sex differences have been reported, which are described below, and briefly summarised in Table 1 .
ADHD symptoms
Research in population-based samples indicates that for both sexes the hyperactive-impulsive type predominates in pre-schoolers, whereas the inattentive-type is the most common presentation from mid-to-late childhood and into adulthood [ 4 , 21 ]. By contrast, clinical studies typically report a greater prevalence of combined-type ADHD [ 5 , 12 , 22 ]. Early meta-analyses of gender effects have found lower severity of hyperactivity-impulsivity [ 40 ], or all ADHD symptoms (inattention, hyperactivity, impulsivity) [ 24 ] in girls than boys, although individual studies show more mixed results [ 8 , 35 , 41 , 42 ].
Inconsistent findings may reflect that clinic referral and diagnosis tends to favour combined subtypes equally across genders, whilst community sampling points to greater prevalence of inattentive type ADHD in girls than in boys [ 43 ]. Hyperactive-impulsive symptoms have been linked to higher clinic ascertainment rates [ 4 ], and may be more commonly seen in boys [ 40 ], with inattention symptoms being less obvious and therefore less likely to be detected. These differences may lead to the perception that females with ADHD are less impaired [ 44 ].
People may experience and respond to the same behaviour of males and females in different ways due to gender-related behavioural expectations [ 42 ]. For example in two studies where teachers were presented with ADHD-like vignettes, when simply varying the child’s name and pronouns used from male to female, boys names were more likely to be referred for additional support [ 45 ] and considered more suitable for treatment [ 46 ]. Parents may also underestimate impairment and severity of hyperactive/impulsive symptoms in girls whilst over-rating these same symptoms in boys [ 47 ]. Compensatory behaviours in girls, such as socially adaptive behaviour, compliance, increased resilience [ 47 ] or coping strategies to mask behaviour [ 48 ] may also contribute to differing perceptions that may in turn prevent referral.
Less is known about the presentation of ADHD in older adults but evidence suggests whilst symptoms tend to decline, ADHD may persist into middle and old age, with a more even male-to-female community prevalence and referral rate with increasing age [ 22 , 49 ].
- Comorbidity
Externalising problems are more prevalent in males with ADHD [ 24 ], manifesting as higher rates of comorbid oppositional defiant disorder (ODD) and conduct disorder (CD) [ 40 ], characterised by rule-breaking behaviour [ 50 , 51 ] and fights in school [ 36 ]. In adulthood, men with ADHD more commonly show antisocial behaviours characteristic of antisocial personality disorder [ 52 , 53 , 54 ]. Whilst these problems are more prevalent in males, they typically remain elevated in individuals with ADHD across both sexes in comparison with the general population. The lower rates of disruptive behavioural problems in females may contribute to lower rates of referral for ADHD assessment and support [ 48 , 55 ].
Compared with males with ADHD, internalising disorders (e.g. emotional problems, anxiety, depression) are more often reported in females [ 24 , 29 , 47 , 51 , 53 , 56 ]. Borderline personality traits in ADHD tend to be associated with women [ 57 ] with hyperactive/impulsive symptoms being associated with self-harming behaviours [ 58 ]. Additionally, women with ADHD have been found to be at higher risk for some adverse outcomes, including greater mental health impairment [ 29 ], severe mental illness (schizophrenia) [ 59 ] and admissions to in-patient psychiatric hospitals in adulthood [ 60 ].
The less overt presentation of ADHD in girls and women may mask the underlying condition due to females not meeting stereotypical expectations of ADHD behaviour. Instead females may be more likely to attract a primary diagnosis of internalising disorders or personality disorders, in turn delaying diagnosis and appropriate treatment [ 45 , 47 , 48 ].
Disordered eating behaviour has been associated with ADHD across both sexes. Whilst individual studies have shown increased disordered eating in girls and women with ADHD [ 53 , 61 ], a meta-analysis of twelve studies identified increased risk of all eating disorder syndromes (bulimia nervosa, anorexia nervosa and binge eating disorder), amongst individuals with ADHD, with similar risk estimates for males and females [ 62 ]. Meta-analysis has also confirmed increased co-occurrence of obesity in children and adults with ADHD [ 63 , 64 ], albeit with no difference between males and females.
Consensus meeting attendees highlighted the co-occurrence of somatic symptoms such as pain and fatigue with ADHD in females, based on clinical observation. There is little available research on sex differences in the prevalence of somatic symptoms such as pain and fatigue in people with ADHD. However, elevated ADHD symptoms have been reported in clinical cohorts with fibromyalgia [ 65 ], and chronic fatigue syndrome [ 66 ].
Young people with ADHD are at greater risk for tobacco and alcohol use in mid adolescence [ 67 ]. In adulthood they are more likely to become smokers [ 68 ], engage in higher rates of substance use [ 69 ] and develop alcohol and drug use disorders [ 70 ]. A prospective follow-up study of a nationwide birth cohort using Danish registry data reported that ADHD increased the risk of all substance use disorder (SUD) outcomes [ 71 ], with comparable risks seen for males and females. Females with ADHD (but without any comorbid conditions) had a higher risk of alcohol and cannabis abuse when compared with males.
Associated features, functional problems and impairments
In both children and adults ADHD is commonly accompanied by emotional lability and emotion dysregulation problems (irritability, low frustration tolerance, mood changes) [ 72 , 73 , 74 ]. Difficulties of this nature may be more common or severe in girls and women [ 30 , 56 , 57 , 58 ] and emotion dysregulation problems are associated with a broad range of impairments in adulthood, including educational, occupational, social, familial, criminal, driving and financial problems [ 75 , 76 ]. In an Icelandic study of ADHD symptoms in university students, poor social functioning best predicted dissatisfaction with life in males, whereas among females the best predictor of life dissatisfaction was poor emotional control [ 77 ].
Cognitive problems are well established in ADHD [ 78 , 79 , 80 ], spanning difficulties with executive dysfunction (such as inhibition, planning, working memory and set shifting) and non-executive cognitive domains (e.g. word reading, reaction times, colour or letter naming, response consistency). However, ADHD may also be associated with general impairments in intellectual functioning, which tends to be more prominent in females [ 24 , 40 ]. Subtle social cognition deficits, including facial and vocal emotion recognition, have also been reported in both males and females with ADHD, with no clear sex-related differences [ 81 ].
A similar level of social impairment has been identified for ADHD males and females [ 24 , 40 , 82 ]. Autistic-like symptoms, including social and communication impairments, are common in both girls and boys with ADHD, and although these present at a higher rate in boys, likely influenced by the higher base incidence of ASD in boys, alongside greater difficulties in detecting ASD in girls [ 16 ]
Children with ADHD are more likely to experience rejection and unpopularity and have fewer friendships than their peers [ 83 ] and social problems can persist into adulthood [ 75 ]. Disruption to relationships with parents, siblings and peers has been reported for females with ADHD [ 84 , 85 ]. Girls with ADHD may apply a range of ineffective strategies to resolve their peer relationship problems [ 86 , 87 ], and experience more bullying than their peers [ 88 ], including physical, social-relational, and cyberbullying victimisation [ 23 , 89 , 90 ], whilst in boys physical victimisation appears to be more common [ 91 ]. Peer victimisation has been associated with reduced self-esteem and self-efficacy, and increased anxiety and depression symptoms in young people with ADHD [ 90 , 91 ]. Adverse outcomes have been associated with interpersonal difficulties in females with ADHD including lower satisfaction with romantic relationships [ 92 ] and lower self esteem [ 48 ].
There is some evidence to suggest that elevated symptoms of ADHD are associated with excessive internet use in children and adolescents [ 93 ], as well as adults [ 94 ], but the causal direction of this association is unclear (i.e. elevated ADHD symptoms could trigger excessive internet use, or excessive internet use could lead to elevated symptoms of ADHD) [ 95 ]. Excessive gaming [ 96 ] has also been reported. It is not clear whether this association is stronger in males or females or if it is equivalent across the sexes [ 93 , 94 , 97 ]. A large web-based survey of adult internet behaviours and psychopathology in Norway found that elevated ADHD symptoms were associated with increased addictive technological behaviours, including social media use and gaming [ 98 ]. Overall however, addictive social media use was more common in women [ 98 ].
Throughout adolescence and the transition into adulthood, there is an increase in risk taking behaviour which may be associated with symptoms of hyperactivity and/or impulsivity [ 48 ]. For example, young people with ADHD become sexually active earlier, have more sexual partners and are more frequently treated for sexually transmitted infections [ 99 ]. Rates of teenage, early or unplanned pregnancies are elevated in girls and women with ADHD [ 100 , 101 , 102 ]. Pregnant women with ADHD are more likely to smoke up to the third trimester, or be obese or underweight [ 102 ].
A review of ADHD and driving reported that adults with a history of ADHD may be more likely to be unsafe or reckless drivers and have more frequent or severe crashes [ 103 ], albeit with no specific examination of sex differences. One study with data from the US National Epidemiologic Survey on Alcohol and Related Conditions, showed that reckless driving was significantly more frequent in men compared with women with ADHD, reflecting the same pattern as seen the general population [ 29 ]. This suggests that reckless driving is likely to be similarly proportionally enhanced in women as in men with ADHD.
Studies specifically reporting driving problems in women with ADHD have shown no significant association between ADHD and driving outcomes [ 68 , 100 , 104 ]. However, results from a prospective follow-up study of a nationwide birth cohort in Danish registers, reported increased mortality rate among individuals with ADHD; when compared with males with ADHD, females with ADHD had an increased mortality rate after controlling for comorbid CD, ODD and SUD [ 104 ]. The excess mortality in ADHD was mainly driven by deaths from unnatural causes, especially accidents. The authors speculate that the gender difference may be driven by females being less likely to be diagnosed and receive treatment than males with the disorder, leading to greater risk of accidental death.
Delinquency and criminality in females with ADHD is more common compared with their non-ADHD peers but less severe or prevalent than reported in males with ADHD [ 85 , 105 , 106 ]. A study examining adult criminal outcomes in children with ADHD, showed males were twice more likely to be convicted than females, but convictions in females occurred at eighteen times the rate seen in the general population [ 106 ]. Prevalence of ADHD in prison populations is estimated at 25%, with no significant differences seen in relation to gender or age [ 107 ].
Triggers for referral
There are multiple potential triggers that may prompt the referral of females for assessment, shown in Table 2 . Some of these triggers are indicative of other associated conditions and it is the clustering of multiple trait-like symptoms that are pervasive and impairing that is informative, rather than state-like symptoms showing situational change. The decision to refer would also be strongly supported if there is a first-degree relative with ADHD.
The stereotype of the ADHD ‘disruptive boy’ [ 47 ] is likely to influence the likelihood of referral and access to diagnosis and treatment. The key message is not to disregard females because they do not present with the externalising behavioural problems, or the disruptive, hard-to-manage presentation (e.g. engaging in boisterous, loud behaviours) commonly associated with males with ADHD. Females with ADHD may be overlooked and/or their symptoms misinterpreted, particularly for those in highly structured environments, receiving a high level of support, and for those who have developed strategies to mask or compensate for their difficulties.
It is important to be mindful that environmental demands (including educational, occupational, financial, familial and social functions and responsibilities) increase in number, scope and complexity with age and level of independence, whilst support resources decline [ 108 ]. Many young peoples’ struggles and impairments become apparent as they lose the family and educational scaffolding that was previously in place. Therefore, young people (both males and females) may be particularly vulnerable at times of transition, when symptoms become exposed. Increased functional demands on transition to secondary school (planning ahead, organising work and juggling assignments) may lead them to feel overwhelmed. This may impact on self-esteem and result in learner anxiety and perfectionism in an attempt to compensate. Periods of transition may therefore unmask unidentified ADHD by exposing or exacerbating symptoms, together with the development of internalising problems leading to increased vulnerability.
These environmental changes often occur at a time when girls undergo changes in their physiological and sexual maturation. There is growing recognition that puberty is a phase of high risk for mental health problems [ 109 ]. The developmental changes that occur during puberty and later in adolescence may lead females with ADHD to be particularly psychologically vulnerable if they are not able to access support.
Difficulty coping with more complex social interactions and resolving interpersonal conflict may also trigger cause for concern. As girls with ADHD move into their teenage years, difficulty maintaining friendships often becomes more marked and they may feel rejected and socially isolated. Some respond with bravado to buffer them from social isolation but a ‘brave face’ is unlikely to prevent them from feeling distressed and developing low mood and anxiety. Dysfunctional coping strategies and the lack of a support network may lead them to express these feelings by self-harming behaviours (e.g. cutting) or changes in eating patterns.
The identification of specific educational or learning problems may also be an important trigger for referral. Children may be diagnosed with specific learning difficulties, such as dyslexia, when a diagnosis of ADHD may be more appropriate. Parents/carers and teachers may note the disparity between educational performance (day-to-day classroom contribution) and achievement (end grades).
Many young people with ADHD do not exceed the mandatory minimum level of schooling, and the problems described above may become even more marked when they enter further education and/or leave home. Research suggests that adolescent school girls with elevated ADHD symptoms make significantly fewer plans for their future than their peers, suggesting that they leave this to chance and opportunistic encounters [ 86 ]. Those who enter the world of work may find that their difficulties evolve into employment impairments and limitations. However, as they mature young people may begin to develop greater awareness of their difficulties, leading to an increase in self-referrals.
For both males and females, a comprehensive assessment should be completed to accurately capture the symptoms of ADHD across multiple settings, their persistence over time and associated functional impairments. High rates of comorbidity are typically present. The assessment process is typically tripartite involving the use of rating scales, a clinical interview and ideally objective information from informants or school reports. Key recommendations for enhancing diagnostic assessment in girls and women are provided in Table 3 .
Rating Scales
Rating scales can obtain perspectives from different informants (e.g. family, teacher, youth worker, occupational health practitioner) in a consistent, quick and easy way. They are not the sole domain of healthcare practitioners and can be applied (with patient consent) by allied professionals, such as social care providers and those working in educational and occupational establishments, to guide whether referral might be merited.
While rating scales are useful aids for clinical assessment and treatment monitoring, findings should be interpreted cautiously if they are used for screening purposes as they are non-specific markers of potential problems [ 110 ]. Rigid adherence to cut-offs may lead to a high proportion of false positives and negatives. There are many rating scales available with varying merits and limitations and some are yet to be updated to reflect revisions to diagnostic criteria. Where possible both informant- and patient-rated scales should be obtained. Rating scales in common use are presented in Table 4 .
Rating scale norms are predominantly from male or mixed samples, which may disadvantage their use in females, although some provide female-specific norms (see Table 4 ). Where female norms are not available, greater emphasis should be placed on collateral information (e.g. parental and school reports). The Nadeau and Quinn checklists may also be used as indication of possible ADHD in girls and women [ 126 , 127 ], providing structured self-enquiry of ADHD symptoms and associated problems, including a range of difficulties such as learning problems, social/interpersonal and behavioural problems.
Since hyperactive and impulsive behaviours tend to decline as patients move into adulthood and impairments associated with inattention are often sustained, it is helpful to re-administer age appropriate scales as young people with ADHD become adults.
The clinical interview
A clinical diagnostic interview, supplemented by a mental state examination, should consider the extent to which the individual’s functioning is age appropriate and obtain examples of how difficulties interfere with functioning and development in home and education/work environments. For children this is usually carried out in the presence of a person close to the child, has known the child for a long time, and is familiar with their developmental history and functioning in different settings (commonly a parent or carer).
Age-appropriate, common co-occurring conditions in females with ADHD should be explored, including ASD, tics, mood disorders, anxiety, and eating disorders. Fibromyalgia, chronic fatigue syndrome, body dysmorphic disorder and gender dysphoria may also be explored as possible co-occurring conditions. The assessor needs to consider what is primary (i.e. occurring alongside and independently to ADHD) and what is secondary (i.e. caused or exacerbated by ADHD). It will help to determine whether the presenting problem is trait-like or episodic in nature. Clinicians should be alert to signs of self-harming behaviours (especially cutting), which typically peak in adolescence and early adulthood [ 128 , 129 ]. Substance and alcohol use disorders should also be assessed in teenagers and adults. Sleep problems are commonly seen in both males and females with ADHD [ 130 , 131 ], and it is important to determine whether this primarily relates to symptoms of ADHD or co-occurring anxiety.
Since heritability of ADHD is high, ranging between 70-80% in both children and adults [ 132 ], it is important to be mindful that informants who are family members may also have ADHD (possibly undiagnosed) which may affect their judgment of ‘typical’ behaviour. The assessor should therefore obtain specific examples of behaviour from the informant and use these to make clinically informed judgments, rather than relying upon the informants’ perception of what is typical or atypical.
Semi-structured clinical diagnostic interviews are helpful as they guide the healthcare practitioner to complete a comprehensive developmental and clinical interview, whilst allowing for individual differences to be considered. For example, symptoms relating to excessive talking, blurting out answers, fidgeting, interrupting and/or intruding on others have been reported as more frequently endorsed by women than men with ADHD [ 53 , 55 ] and may be more sensitive to the presentation in females. Small modifications may help to capture more female-centric behaviour (e.g. ‘excessive talking and giggling’ instead of ‘excessive talking’) [ 133 ]. Commonly used diagnostic interviews are presented in Table 4 . There are three clinical interviews that prompt the assessor to consider the presence of co-existing conditions (which may differ between males and females); ACE, ACE+ [ 134 ] and the DAWBA [ 118 ].
When assessing adults, the clinical interview is usually completed with the affected individual but whenever possible collateral information should also be obtained. This may be from a parent or carer or another close member of the family. If a reliable informant cannot be identified who knew (and can recall) the individual well during their childhood, it may be helpful to obtain information from an informant who currently knows the individual well (e.g. a partner or a close friend who has known them for a significant period time, 5 years or more) in order to supplement self-reported information with a secondary perspective. If available, reports from childhood (for example, school, social service and/or previous clinical reports) are likely to be informative. Importantly, however, it may not be possible to rely on school reports when assessing females, as subtle hyperactive-impulsive symptoms may have been missed by teachers and/or they omit to comment on interpersonal or relationship problems. School reports may comment more on attentional problems (such as daydreaming or lacking in motivation and effort).
Some girls and women with ADHD become competent at camouflaging their struggles with compensatory strategies, which may lead to an underestimation of their underlying problems. Often these strategies have an adaptive or functional purpose, for example, enabling them to remain focused or sustain attention, or to disguise stress and distress. However, not all strategies are helpful. Coping strategies may be less overt, such as avoiding specific events, settings or people, not facing up to problems, spending too much time online or not seeking out help when needed. Teenage and adult females with ADHD may turn to alcohol, cannabis and other substances to manage emotional turmoil, social isolation and rejection. Some may seek to obtain a social network by forming damaging relationships (for example, joining a gang, engaging in promiscuous and unsafe sexual practices, or criminal activities). If there is cause for concern, a risk assessment should be included that enquires into suicidal ideation, the use of illicit drugs, substances and alcohol, antisocial attitudes and behaviours, harm to self and others, bullying and assault, excessive internet use, unsafe sexual practices and exploitation of a sexual, financial or social nature. In some cases, a physical health assessment may be warranted.
With older age and persistent inattentive symptoms, there may be an increasing risk that individuals with ADHD are incorrectly diagnosed with mild cognitive impairment. Self- perceived ADHD symptoms, and in particular inattention, are found to increase with age in diagnosed adults and perceived symptom severity appears to be exacerbated by concurrent depressive symptoms [ 49 ]. It is not uncommon that adults with ADHD are treated for anxiety and/or depression in the first instance. Clinicians should be mindful that those with treatment resistant anxiety and/or depression should be screened for possible undiagnosed ADHD. Indeed, careful examination of developmental history will elucidate whether symptoms are longstanding and have been exacerbated by situational or biological changes, or whether they represent new-onset symptoms that are less indicative of ADHD.
Objective assessments
Whenever possible, the assessor should obtain collateral information from independent sources. This may include direct observations in a specific setting (e.g. in clinic, at home or at school). A wealth of useful information may be obtained from observing a child in school and speaking directly with teachers. When assessing adults, perusal of school, college and/or employment reports (if available) can be helpful.
Tests that assess executive dysfunction may help to determine deficits in higher order processing skills such as task switching, perseveration, planning, sequencing and organising information. Some have been specifically developed for ADHD populations and focus on assessing attention, impulsivity and vigilance in children and adults. Neuropsychological tests such as the Test of Everyday Attention (TEA) / Test of Everyday Attention for Children (TEACh), may be helpful supplements to the diagnostic process. Those most commonly used in clinical practice include the Conners’ Continuous Performance Test, third edition (CPT 3 [age 8+]) [ 135 ] and the QbTest [ 136 ], the latter including a measure of hyperactivity. QbTest scales have normative data specific to each sex (age 6-60) and may therefore be more sensitive to ADHD in females. The assessor should be mindful that an individual with ADHD may perform relatively well on novel tasks, especially those presented as computerised games providing immediate gratification via rapid feedback. Moreover, findings may lack ecological validity and not reflect performance in the ‘real world’. Neuropsychological assessments are not specific markers of ADHD and should only be used to augment clinical decision making and not be used as stand-alone diagnostic tools.
Interventions and Treatments
Prompt identification and treatment of ADHD is recommended, as there is evidence of long-term functional benefits associated with treatment [ 137 , 138 ]. ADHD is typically treated with psychoactive medication, psychoeducation and therapeutic interventions at all ages, and a stronger treatment effect has been reported with multi-modal treatment [ 138 ]. A brief summary of treatment recommendations is presented in Table 5 .
In the context of changes in the presentation of ADHD with development and ageing, regular treatment reviews are advised. These can revisit and optimise current pharmacological and non-pharmacological approaches, or revisit those patients who previously may not have been suitable for specific treatments or who did not show good response.
Pharmacological management
ADHD is commonly treated with psychostimulants, such as methylphenidate and amphetamine. In certain cases, a nonstimulant such as atomoxetine, an extended-release form of guanfacine or clonidine, or bupropion may be prescribed, especially when stimulants are inappropriate or have been unsuccessful. These medications, with the exception of bupropion are recommended by the National Institute of Health and Care Excellence (NICE) guidance [ 139 ]. A systematic review and network meta-analysis recommended methylphenidate for children and adolescents and amphetamines for adults, taking into account both efficacy and safety [ 140 ]. Larger confidence intervals in relation to the tolerability and efficacy of bupropion, clonidine and guanfacine were reported, indicating less conclusive results with regards to the efficacy and tolerability of these oral medications [ 140 ].
Treatment recommendations do not differ by sex and differ only modestly by age (NICE, 2018 [ 139 ]). The overarching opinion in the consensus group was that there are no differences in the medicines used to treat ADHD in girls and boys. Stimulant medications show good efficacy for improving ADHD symptoms in both children [ 141 ] and adults [ 142 ], and response appears comparable in females and males [ 143 , 144 ]. However girls with ADHD tend to be less likely to be prescribed stimulant treatment than boys with ADHD, and are likely to start treatment at an older age [ 145 ].
The potential benefits of treatment must be viewed in the context of lifetime adverse outcomes associated with poorly managed ADHD described previously. Prompt identification and treatment may help to improve longer-term functional, health and mental health outcomes. Reduced rates of comorbidity (including depression, anxiety disorders, and disruptive behaviour disorders) have been noted in stimulant treated ADHD populations [ 146 , 147 ], although the converse effect has also been reported [ 148 ]. Comorbid ADHD is associated with treatment resistant depression [ 149 ] and regular treatment for ADHD may reduce rates of treatment resistance [ 150 ]. Pharmacological treatment of ADHD is also associated with improved educational [ 146 ] and occupational [ 151 ] outcomes, as well reduced rates of criminality [ 152 ]. Pharmacotherapy for ADHD appears to be a protective factor for obesity [ 64 ], and some limited evidence suggests that it may increase efficacy of weight management strategies (reviewed in [ 153 ]). Additionally, there appears to be a benefit of ADHD treatment with regards to substance use disorders. A study of commercial healthcare claims showed reduced emergency department visits related to substance use disorders when patients were prescribed treatment for ADHD [ 154 ].
Whilst pharmacological treatments themselves should not differ by sex, the way in which they are managed and monitored should occur in a sex-sensitive manner. The consensus group observed that prescribers need to consider ADHD presentations and associated problems in females to appropriately target what medication aims to improve. It may be less helpful to strictly adhere to conventional rating scales or focus on behaviour management to identify treatment-related changes. Instead, treatment response may be better captured through individualised targets, such as measures of emotional regulation, participation in education, and academic attainment. In the UK, all government funded schools have attainment ratings for each child, which could be examined by the prescriber prior to commencement of medications and monitored over time in conjunction with prescribing. Girls with emotional regulation difficulties (for whom internalising difficulties are often a key component of their ADHD) could benefit from measuring changes in emotional lability with medication use.
Parents and carers may not be as aware of the benefits of medication in girls, especially those with inattentive presentations in the absence of challenging or disruptive behaviour. Psychoeducation regarding available treatments and what they are targeting, provided for parents and girls with ADHD themselves, may help to ensure engagement in treatment and improve adherence to treatment regimens. Where required, adherence may be improved by using long-acting stimulant medication in place of short-acting medications [ 155 , 156 , 157 ].
In early to late adolescence, recommended treatment regimens in ADHD remain the same as in early childhood, and do not differ between girls and boys. The use of medication should be followed up over time to verify if medications are effective and well tolerated, and to manage the effects of related conditions (e.g. anxiety, depression) if they emerge. Side effects of stimulants need to be considered, particularly the side effect of appetite suppression if eating disorders are a concern [ 158 ].
There is some early evidence to suggest that ADHD medications may differentially affect women depending on progression of their menstrual cycle. Two small studies have shown that hormonal changes during the menstrual cycle (oestrogen and progesterone levels) may impact on the subjective euphoric and stimulating effects of d-amphetamine in healthy women who are not affected by ADHD [ 159 , 160 ]. Changes in subjective ratings of stimulation have also been noted in young women unaffected by ADHD in response to d-amphetamine after application of estradiol patches (commonly used to treat problems associated with menopause) [ 161 ]. Cellular and small neuroimaging studies which show early evidence of a link between dopamine systems (implicated in the aetiology of ADHD) and gonadal hormones (reviewed in 49). In a case study, a woman with ADHD showed positive response to treatment adjustment around the menstrual cycle, which included augmentation with an antidepressant (fluoxetine) during the immediate pre-menstrual period to reduce problems with moodiness, irritability and inattention normally well controlled through stimulant medication alone [ 162 ].
Whilst the evidence above does not support treatment adjustment according to the menstrual cycle, anecdotal clinical accounts were given during the consensus meeting supporting that this approach benefits certain patients. The consensus group noted that this type of regular medication adjustment may be easier to manage for adult women who can take more control of their dosing, rather than adolescent girls who tend to respond better to routine. There were also anecdotal accounts of symptom exacerbation in women during the post-menopausal period. During this time physicians may consider the use of hormone replacement therapy, if deemed beneficial.
As hormonal changes take place during puberty, the postpartum period and the menopause, patients may report changes in their symptoms and re-evaluation of treatment regimens may be helpful. It may be advised that women track their symptoms during these periods to establish patterns which may help support changes to the medication regimen when reviewed by their physician.
There is no evidence to indicate that females in either early, middle or later adulthood should be treated any differently with respect to specific medicines for ADHD symptoms. However, given the complex clinical picture of many adults with ADHD, particularly with regards to the presence of comorbid conditions, prescribers need to be mindful of potential interactions with other drugs. If ADHD treatment improves co-morbid conditions, medication regimens could potentially be simplified.
Women with ADHD are highly likely to suffer from mental illness and SUDs. Clinicians need to be mindful of, and discuss with their patients, the risks around alcohol and drug use whilst on ADHD medications. Affective symptoms (most commonly emotional lability or volatility) associated with ADHD, may be misattributed to depressive disorders. For women with ADHD in whom depressive mood symptoms are apparent but not pervasive, it is advisable to treat the ADHD symptoms first and monitor for improvement. A more consistent low mood may be due to demoralization driven by ADHD and its functional impairments, and may improve with ADHD medication.
Symptoms or problems experienced by women with ADHD may also overlap with those indicating a personality disorder, such as BPD. Careful consideration is required to establish the underlying condition(s). This will have follow-on implications for treatments, which differ significantly between personality disorders and ADHD. Biosocial theory suggests that BPD may arise as a function of the interaction of early vulnerabilities (impulsivity and heightened emotional sensitivity) with the environment [ 163 ]. If ADHD symptomatology may predispose individuals to later personality disorders [ 164 ], it is possible that early detection and appropriate treatment could prevent the later development of these conditions [ 165 ]. However, there is no clear empirical evidence supporting this hypothesis at present [ 109 ].
Historically, prescribing ADHD medication during pregnancy or breastfeeding was not advised due to a lack of evidence for safety and risks of unknown adverse effects to the baby. However, a recently published systematic review and meta-analysis reported that exposure to ADHD medication during pregnancy does not appear to be associated with serious adverse maternal or neonatal outcomes [ 166 ]. Nevertheless, the group were cautious regarding this outcome and considered that until these findings have been robustly replicated, prescribing ADHD medication during pregnancy or breastfeeding should be avoided. There may be situations however where risks of not treating ADHD may outweigh potential risks to the foetus and continued prescribing may be necessary subject to more careful obstetric monitoring. In this case, women with ADHD need to be informed of these risks.
Women may find their ADHD symptoms worsen or become particularly difficult to manage while breastfeeding given additional life pressures that occur in the presence of a new baby. Whilst it may be possible to use short acting stimulant medication, timed around breastfeeding to minimise transfer between mother and child [ 167 ], there is minimal scientific evidence to support this approach, and it would be generally safer to advise the cessation of medications during this period altogether. Where ADHD medication is necessary, then an alternative to breastfeeding is needed to minimise any risk to the baby.
Prescribers should be aware that mothers with ADHD may experience difficulties in managing their own symptoms alongside the increased demands from family life, and these difficulties may be augmented by the presence of ADHD in their own children. They may benefit from more frequent evaluations of ancillary support requirements and/or a careful review of medication dosage.
Non-pharmacological management
A number of meta-analyses of data from child and adolescent samples have shown that non-pharmacological interventions targeting cognitive processes show small to moderate effects on ADHD symptom outcomes when rated by individuals who are close to the treatment setting (often parents), but that effects become attenuated or non-significant when outcomes are obtained from individuals who are blinded to the interventions (often teachers) or adequately controlled active or sham conditions [ 168 , 169 , 170 ]. Research has documented this effect for specific interventions such as cognitive training (for example, training of attention, memory, inhibitory functions) [ 169 ], and neurofeedback [ 170 ] - although more recent research suggests that effects of neurofeedback are more modest rather than absent when assessed by probably blinded evaluators [ 171 ].
Meta-analyses also show potentially more promising outcomes from non-pharmacological interventions that target behaviours and outcomes beyond ADHD symptoms alone in children and adolescents, with ADHD intervention in children producing a moderate effect on parent stress [ 172 ], and organisational skills interventions which resulted improved ratings from both parents and teachers and with modest improvement in academic function [ 173 ]. Behavioural interventions were found to have a moderate positive effects on a range of outcomes including changes in parenting and conduct problems, even when rated by blinded assessors [ 174 ].
Meta analyses also indicate more promising results from cognitive behavioural therapy, and mindfulness interventions on ADHD symptoms in studies with primarily adult samples, albeit without comparisons from blinded raters [ 175 , 176 ]. Benefits of non-pharmacological treatments in adults are also shown to range beyond improvements in ADHD symptoms, as shown in a recent report from a psychological intervention programme in adults with high levels of ADHD symptoms across three municipalities in Denmark. Participant outcomes were compared with matched controls receiving ‘treatment as usual’ drawn from the Danish Registers at 6 and 12 months post-treatment follow-up. The study showed that participation in the programme was associated with increased employment, education rates and reduced use of cash benefits and social services [ 177 ]
The efficacy of a psychological approach varies across the lifespan and the content of treatment should be tailored to meet the individual presentations and needs of individuals with ADHD [ 178 ]. Regular review of how a person is coping may be especially important at times of key transitions. Since the needs of females with ADHD differ considerably as they mature, the goals of treatment are presented across three age ranges: primary age (5-11 years), secondary age (12-18 years) and adulthood (age 18+).
Primary age
ADHD often places a significant psychological, emotional, and economic burden on families as well as the individual; increased stress and discord in the family unit has been reported [ 179 , 180 ]. Where ADHD affects females, it is also more common in their family members [ 33 , 34 ], resulting in bidirectional effects of ADHD in the mother-child relationship. The aim of non-pharmacological interventions therefore is to support individuals with ADHD and their families to develop and/or improve skills and coping strategies. Psychoeducation and psychological interventions directed at both patient and family are needed to achieve this, as they provide the tools to make helpful changes and achieve positive immediate and long-term functional outcomes.
There are two types of parenting intervention that may be offered to parents/carers in this age-group: (1) parent/carer support interventions, where people can meet and share experiences with others, and (2) parent/carer mediated interventions, sometimes referred to as ‘parent training’. The latter is an indirect intervention as the parent/carer is taught to deliver interventions to their child. Ideally both approaches should integrate a psychoeducational component as this is likely to lead to better outcomes.
Psychoeducation and interventions for girls in this age group should include discussion about the difficulties and challenges they will face at home, in school and in social activities - and how they may respond. At school this may relate to difficulty with sustaining attention, organisation, time management, planning activities, prioritising and organising tasks. They may also require generic skills for coping with interpersonal difficulties and/or social events, conflict management, emotional lability, anxiety and feelings of distress. Some girls may need interventions to address discrete problems, including sleep problems [ 131 ], enuresis [ 181 ], bullying [ 89 , 90 ] and repetitive behaviours such as nail biting [ 182 ]. It is important to emphasise that problems may be less overt in females with ADHD compared with boys due to them being less boisterous and hyperactive, yet their struggles with impulse control may manifest in a different way such as blurting out hurtful things to friends and family in anger, or deliberately self-harming behaviours.
Both group and individual sessions working directly with the child may be helpful additions to parent/carer mediated treatments, although individual treatments may be more appropriate for those with severe symptoms, intellectual limitations and/or those who are unable to tolerate group sessions (e.g. due to lack of confidence, poor social communication). Two specific programmes have been developed for young children with cognitive, emotional, social and/or behavioural problems; one for individual delivery [ 183 ] and the other for group delivery [ 184 , 185 ].
Secondary age
As children mature, they are more likely to receive direct interventions without input from their parents or carers. The best mode of psychological treatment is cognitive behavioural therapy (CBT) together with psychoeducation (which can be provided to both patients and parent/carers together or independently). Parents and carers need to be aware of the elevated risk of deliberate self-harming behaviour (e.g. cutting), eating disorders, substance abuse, risk-taking behaviours, and vulnerability to exploitation in teenage girls with ADHD. Thus psychoeducation should include indicators that problems of this nature may be developing.
The focus of treatment in this age group should include information and guidance on the need for adherence to medication. There is evidence that adherence to pharmacotherapy declines in the teenage years, although adherence appears to be modestly better in girls than in boys [ 155 , 157 , 186 ]. These changes have been attributed to adverse effects, sub-optimal response, reduction in parent supervision, increased need for autonomy, and social stigma associated with ADHD diagnosis and taking medication [ 155 , 156 ]. It is important to provide psychoeducation to encourage young people with ADHD to understand and take ownership of their diagnosis and treatment, rather than feeling it has been imposed on them. Those diagnosed with ADHD for the first time in their teenage years are likely to require different intervention strategies to those who have been treated pharmacologically earlier in childhood. For example, psychoeducation should include information on the purposes and benefits of particular medications, as well as strategies around self-management.
Problems presenting in younger childhood often become more marked with age due to increasing academic and social expectations. These are important years in terms of a young person’s education and interventions can help to support executive function (e.g. improving skills to address problems with time management, focus, sustaining attention, organisation and planning) which may in turn support their coping in secondary schooling. Teenage girls may particularly benefit from treatment aimed at improving self-concept and identity. This may be achieved by unpacking the association between ADHD, lack of achievement, poor self-efficacy, lack of self-confidence, poor self-image and low self-esteem.
Aside from addressing core ADHD symptoms and executive deficits, specific interventions should focus on developing skills and coping strategies for co-occurring conditions, such as managing poor emotional regulation, low mood and anxiety, controlling the impulse to deliberately self-harm (including skin picking and cutting), eating for pleasure or restricting food. Additional support for new skills required in teenage years, such as managing money, may also be helpful.
In adolescence, young people develop a strong focus on peer relationships and a tendency towards social conformity [ 187 ]. For teenage girls with ADHD, the desire to develop robust and supportive social networks can be strong, and the rejection and social isolation experienced by many may mean that family support is especially valued [ 87 ]. Simultaneously interpersonal conflict with family members is not uncommon, and girls may engage with dysfunctional social groups and activities in an attempt to gain a sense of ‘belonging’ and to be accepted. Girls with ADHD are at increased risk of being victims of bullying [ 23 , 90 ], and social media may provide additional challenges since it offers a public platform for victimisation.
Behavioural and oppositional problems remain elevated in teenage girls with ADHD in comparison with their peers, albeit not as elevated as in boys with ADHD. Girls with ADHD may attract detentions, suspensions or exclusions from school for their conduct or oppositional behaviour. Their behaviours may be more socially motivated (e.g. spiteful, manipulative, threatening behaviours and/or lashing out at peers) rather than overt aggression. Social skills and interpersonal relationship interventions become salient at this age. These may aim to develop coping strategies to regulate emotions, build confidence, raise self-esteem and manage peer pressure, deal with rejection and manage conflict.
Interventions to address impulsivity and associated risk-taking behaviour may be helpful. These problems may manifest in early onset of sexual behaviour. The desire to be accepted into a peer network may be a motivating factor. Girls with ADHD are more likely to be pressurised into sex or engage in risky sexual behaviour. They are also more vulnerable to sexual exploitation or perceived exhibitionism (including internet grooming, ‘sexting’ and posting inappropriate content [ 188 ]). This may result in disproportionate social stigma for adolescents and young women with ADHD, in the face of violations of social expectations of female sexuality (where promiscuity may enhance male but damage female reputations). As girls become sexually active, the need for contraception should be discussed.
Impulsive behaviour is also associated with substance misuse. The risks around substance use and interactions with ADHD medication, including risks for addiction, need to be discussed.
Considerations around pregnancy, the post-partum period and parenting may also be required, since rates of early pregnancy are higher in girls with ADHD. Early pregnancy, may load additional stress and impairment on young girls with ADHD. The consensus group noted difficulties in young ADHD mothers not only in relation to child discipline and behaviour management, but also in relation to the organisational demands of parenting (for example, ensuring bottles are washed, medical and other appointments are kept, child’s clothes are cleaned).
Both individual and group CBT interventions will be helpful in this age-group, the latter providing the opportunity to meet and talk to others who have similar experiences as well as acquire and rehearse social skills in a contained environment.
Many of the functional problems experienced by women with ADHD in relation to educational, social, and risk-related behaviours are a continuation of those present in their teenage years. In adulthood, psychoeducation and CBT interventions should continue to address core ADHD symptoms, executive dysfunction, comorbid conditions and dysfunctional strategies (e.g. substance abuse, deliberate self-harm). However, specific attention may be required to address the more complex situations adult females may face, e.g. multitasking occupational demands, home management and family/parenting responsibilities. It is important to encourage the patient to identify and focus on their strengths and positive attributes rather than solely on perceived weaknesses and failures.
Interventions need to address the potential for women with ADHD to be vulnerable in terms of their sexual behaviour and relationships, to support their sexual health and safety. Social stigma associated with risky sexual behaviour in women may augment social problems and limit occupational opportunities. In combination with low self-esteem, this may render women with ADHD vulnerable to sexual harassment, exploitation, and/or abusive or inappropriate relationships. The Adult Psychiatric Morbidity household survey conducted in England found that 27% of females who experienced extensive physical and sexual violence had ADHD traits [ 189 ].
The bulk of household, and parental and caring duties are often borne by women [ 190 , 191 , 192 ], reflecting social and cultural constraints and expectations. These may result in increased impairment and anxiety in relation to these roles and duties in women compared with men. The consensus group identified that the demands placed on mothers often differ from those of fathers and that low self-esteem may be related to perceived failure to reach societal expectations. Mothers may lack confidence or experience feelings of guilt over their perceived inadequacy as a parent. Dysfunctional beliefs of this nature may be reinforced if they have a difficult-to-manage child with ADHD and are offered ‘parent training’ interventions. The group acknowledged that the term ‘parent training’ is unhelpful and may be perceived as pejorative.
However, at the same time harsh, lax or negative parenting styles have been identified to be elevated in mothers with ADHD [ 193 ]. Mothers with ADHD may benefit from life skills coaching, guidance and support in parenting, including ancillary support around parenting strategies. This may be particularly helpful for more vulnerable mothers: those that are young, are sole caregivers for their children, and/or are parenting a child with ADHD. Tailored assessments, support plans and social interventions may help to improve outcomes for this vulnerable group.
Women with ADHD may experience problems in the workplace, such as disorganisation, forgetfulness, inattention, accepting constructive criticism and appraisal, and difficulties managing interpersonal relationships with colleagues. This is likely to be exacerbated in the presence of concurrent intellectual dysfunction and/or other comorbidity. For these types of problems, often a group intervention is helpful and cost-effective. However the decision of whether a group or individualised approach is preferable should be based on careful formulation and individual need. Women may also benefit from targeted support in managing feelings of stress and distress, managing and regulating emotions, coping with rejection and/or feelings of isolation, managing interpersonal conflict, assertiveness training, compromise and negotiation steps, which may help to improve their occupational outcomes and their ability to cope with everyday social interactions.
Multi-agency liaison
This section addresses issues that arise at a broader institutional level. Primarily, support for females with ADHD may be improved through the psychoeducation and training of individuals who work within these institutions. Some may act as referral gatekeepers and, as such, they have the potential to support or hinder the referral process and to positively or negatively influence the progress of young people and adults within these institutions. A brief summary of multi-agency liaison recommendations is presented in Table 6 .
Educational considerations and adjustments
ADHD is associated with low educational attainment and academic underachievement [ 99 , 146 , 195 ]. Interventions should focus on supporting attendance and engagement with education to avoid early school leaving, diminished educational attainment, and associated vulnerabilities. Since ADHD is classified as a disability under the UK Equality Act [ 196 ], reasonable adjustments to education provision are mandated (examples may include: additional examination time, academic coaching, rest-breaks during examination, or possibility for part-time study [ 197 ]). Research suggests that simple interventions, including physical adjustments (table set-up, creating a time-out corner), and behaviour management techniques, as well as joint goal setting with primary age children, can help to improve ADHD symptoms, social and emotional functioning, and reduce conduct problems in the classroom [ 198 ]. However, adjustments cannot be put in place unless ADHD is first recognised and diagnosed.
Young people affected by ADHD are at increased risk for repeating grades, dropping out of high school, being suspended or expelled, and failing to obtain school or higher education qualifications [ 85 , 99 , 199 ]. Maintaining strong links with school is key to promoting adolescent health and social development [ 110 ]. Whilst early or unplanned pregnancy is associated with a reduction in educational and occupational opportunities, school achievement problems in adolescent girls with ADHD have also been shown to predate and predict risky sexual behaviour and unplanned pregnancy [ 200 ]. The consensus group noted that exclusion, truancy and school phobia are associated with increased vulnerability of teenage girls with ADHD in relation to later substance misuse, antisocial behaviour, criminality, sexual exploitation and early pregnancy. There is a danger that punitive measures may be harsher for girls who display hyperactive or disruptive symptoms, due to this behaviour constituting a greater violation of social norms and expectations. Excessive punitive measures can lead to loss of engagement with education. Disciplinary problems (e.g. suspensions, verbal or written warnings or expulsions) predict earlier discontinuation of education in boys with ADHD [ 201 ], although disciplinary problems are less commonly reported in girls [ 85 ].
Externalising conditions have a stronger impact on behaviour in class, whilst internalising problems may impact on motivation and ability to engage in education. Girls with ADHD may present as easily distracted, disorganised, overwhelmed and lacking in effort or motivation. Inattention is more highly predictive of educational under-achievement compared with hyperactivity [ 202 , 203 ]. Females who are more likely to have the diagnosis missed or misdiagnosed, may be particularly disadvantaged since treatment with ADHD medication has been found to mediate educational outcome. For example, a large-scale study of cross-sectional and longitudinal data in ~10,000 12-year old twins from the Netherlands Twin Register showed the potential efficacy of treatment on academic outcomes [ 203 ]. Children taking ADHD medication scored significantly higher on an educational achievement test than children with ADHD who did not.
Individuals with ADHD and intellectual impairments, both male and female, present with complex needs that make it harder for them to engage in education. Many young people with ADHD will have associated specific learning difficulties such as dyslexia, dyscalculia and dysgraphia. Presenting problems may be attributed solely to these specific learning difficulties and/or ASD because school staff are more familiar with them and have a more limited knowledge about ADHD. It may be helpful for students (at all levels of education) who have or who are suspected of having specific learning difficulties to be screened for ADHD, since young people with ADHD may also present with difficulties in reading and writing.
It is important that both child and adult educational professionals have an understanding of ADHD in girls and young women, recognise its presentation and associated vulnerabilities, and have access to screening tools. Training should be disseminated broadly across school staff, including teachers and special educational needs coordinators, as well as teaching assistants, school lunch aides, and after-school club staff who are more likely to supervise children during less structured periods of the day or during one-to-one work in classrooms. It is important that key personnel avoid over-simplistic causation when assessing individual needs (e.g. focusing on their family situation) and understanding of the bi-directional nature of ADHD difficulties in terms of family relationships.
All educational staff should be trained in how to screen females for ADHD and how to make onward referrals for treatment, if indicated. School staff should be trained on the importance of early detection, educational needs and interventions and support strategies that can improve educational outcomes. Training sessions should raise awareness of the current bias towards males in the clinical referral process. Teaching staff may not be as aware of the benefits of referral and ADHD treatment in girls [ 45 ], and children with the inattentive subtype [ 204 ]. Addressing gender-specific ADHD issues, and gender expectations and stereotypes may help staff to better identify affected females. If ADHD is suspected, schools may consider adopting sensitive screening tools for ADHD (Table 4 ) or broader mental health problems (e.g. the SDQ [ 116 ]). These tend to be cost-effective, quick and reliable, and can help to identify vulnerable girls and young women. Difficulties can arise in maintaining medication treatment programmes in school and staff should be mindful that children may find this stigmatising, especially those who require short-acting medications to be dispensed at school.
Many of the training needs for educational staff remain the same in secondary as in primary school. However, transition to secondary school is accompanied by increased academic demands, and increased requirement for self-organisation and personal responsibility against a backdrop of navigating a new social environment. Young people with ADHD are likely to find this shift in self-management and responsibility especially challenging. ADHD symptoms may become exacerbated and more noticeable, triggering referral for the first time. Good learning and teaching practices (i.e. not necessarily ADHD specific) may help to mitigate many of the potential issues in the classroom by promoting engagement, increasing on-task behaviour and reducing social friction.
Efforts toward Technology Enhanced Learning or e-Learning, are likely to be especially helpful for young people with ADHD. With the appropriate content and support, these learning resources have the potential to go beyond improving academic outcomes in secondary school by improving psychosocial functioning (e.g. helping young people to acquire skills to manage risks of exploitation, bullying and/or victimisation in the school environment or online via social media and communication platforms). Although further research is required to determine the efficacy of e-learning methods for improving outcomes in ADHD, specific examples of successful application of these technologies have been reported (reviewed in [ 205 ]).
Careers advice should consider the strengths and weaknesses of female students rather than focus solely on current performance, bearing in mind the relative developmental delay, underachievement, immaturity (and sometimes naivety) of young people with ADHD. Research indicates that occupational ‘fit’ can serve to exacerbate or reduce impairments associated with ADHD. For example, some individuals with ADHD show a preference for more stimulating environments, active, hands-on, or busy and fast-paced jobs [ 206 ]. Career planning that incorporates work experience, non-linear progression towards tertiary education and opportunities to re-sit exams or demonstrate potential may be beneficial for those who have struggled to sustain their engagement in a formal school setting.
Guidance for those wishing to embark in further education should take account of the course demands involved (e.g. level of coursework, method of examination). For those who move away from home, transition is further complicated by the many challenges involved in independent living such as financial management, taking responsibility for domestic and occupational arrangements and healthcare. Moving away from home often escalates social demands, with pressure to integrate with people of different ages, cultural backgrounds and interests. It is essential that young people with ADHD make supportive links within the educational organisation (e.g. disability services or student support services) who can support them to access the help to meet their needs, and coordinate with primary health services. This needs to be planned and thought through in advance because a lack of structure and support at this key stage of transition may unveil or amplify ADHD symptoms, together with associated clinical and functional impairments. Adequate support can help young people with ADHD access additional resources. For example, students with ADHD in further or higher education can apply for Disabled Students Allowance ( https://www.gov.uk/disabled-students-allowances-dsas ), which can fund assistive technology (e.g. speech to text software), specialist mentoring (to help with organisational and planning skills) and “academic coaching”.
In general young people with ADHD reach or complete higher education at a later age than their peers [ 201 ]. This can be due to having to repeat years, re-take modules, and obtain extensions for coursework. Many drop out early due to educational or social problems, or early pregnancy. This emphasises the importance for young people having the opportunity to re-access education in later years. However whilst special educational needs support may be available up to age 25 in the UK, women with unrecognised ADHD may experience difficulties in accessing these provisions or meeting eligibility criteria for learning difficulties. Flexible learning systems and support with childcare are helpful initiatives, e.g. in the UK women with children who wish to return to education can obtain childcare support through government initiatives, such as Care to Learn ( https://www.gov.uk/care-to-learn ), and Childcare Grants ( https://www.gov.uk/childcare-grant ).
Occupational considerations and adjustments
In adulthood, ADHD is associated with unemployment or working in unskilled occupations [ 201 ], difficulty maintaining jobs [ 99 , 201 ], and impaired work performance and financial stress [ 207 ]. A longitudinal study following up girls age from eight until age 30, found that women with childhood ADHD were more likely than their peers to have no or few qualifications, be in poorly paid employment, claim benefits, live in temporary or social housing and have a low income [ 68 ].
ADHD qualifies as a disability under the UK Equality Act 2010 [ 196 ], because it can have a substantial and long-term impact on a person’s ability to perform day-to-day activities. This status can afford women with ADHD certain rights, and access to certain services. For women with ADHD commencing employment, additional support may be required regarding the decision to disclose they have a disability. They may need support in understanding the demands of an organisation, the work-role and personnel structure, how to manage interpersonal conflict, and guidance on how to manage their time, plan and prioritise tasks. Diaries, itineraries, lists, reminder notes and similar scaffolding techniques can be adapted to individual needs through a wide range of digital apps currently available at low or no cost.
Women with ADHD may experience particular difficulty returning to work after having children. This is associated with employment penalties linked to educational problems and potentially having left school early with few or no qualifications. Initiatives such as Specialist Employability Support ( https://www.gov.uk/specialist-employability-support ) are available to provide intensive support and training for unemployed people with a disability.
Occupational difficulties may be further compounded by a difficulty managing the effects of persisting ADHD symptoms on job-related and social performance in the workplace, together with the need to balance occupational demands with childcare. Reasonable adjustments in the workplace may be helpfully put in place [ 208 ] but these may only be achieved if women with ADHD elect to disclose they have a disability. This may not be an easy decision as the individual must balance the need to optimise the environment against their fear of social and occupational stigma, the latter including the possibility they may be held back in promotion and/or other career advancement.
On the other hand, disclosing a disability allows for women with ADHD to be treated more favourably under the UK Equality Act 2010 [ 196 ], and benefit from reasonable adjustments that remove barriers in the workplace that would otherwise disadvantage them. Reasonable adjustments are assessed on a case by case basis and extra support for the costs of making reasonable adjustments in the workplace can come from the Access to Work government initiative (see: https://www.gov.uk/access-to-work ). These rights apply to women with ADHD returning to work, taking up employment or becoming diagnosed at any time during their working lives. Employers who fail to comply with this duty would be liable for disability discrimination.
Health and social care
Research suggests an increased involvement of ADHD children with the social care and foster care systems [ 209 , 210 ]. Equipping social care professionals with tools similar to those used in school settings (e.g. the SDQ) may promote a higher level of insight and understanding. Males may be overrepresented in these systems due to high rates of comorbidity with disruptive behavioural problems. Females with ADHD may be more likely to come into contact with social services if they are young single parents struggling with child-care responsibilities; however their underlying ADHD may be unrecognised.
The overrepresentation of developmental disorders in the care population may be the result of a failure in existing services to recognise the specific contribution of these conditions to family breakdown, and an absence of targeted support in such cases. The group recommends that all children at risk of entering the care system should be systematically screened for developmental disorders. Social care professionals may struggle to identify the parenting potential in undiagnosed women with ADHD, and attribute difficulties more to a chaotic lifestyle choice rather than to any underlying disorder. Given the high heritability rates [ 132 ] it is also helpful to consider that other family members may also share symptoms and suffer with associated impairments, when examining family dynamics.
Social and family services will benefit from training so they can provide specific psychoeducational input to support young mothers of ADHD children and young mothers with ADHD. If deemed appropriate, they might refer mothers with ADHD to mental health services for targeted support that aims to develop skills and coping strategies, and to help them manage their own mental health and personal needs and those of their child.
The early sexual activity, promiscuity and higher risk for sexually transmitted diseases in some females with ADHD is likely to increase contact with sexual health clinics. ADHD training should therefore be extended to include service-providers at these clinics in order to raise awareness of the presentation and needs of females with ADHD. For example this may lead to better understanding of the need for additional sexual health education, including digital health education, which in turn may better support these young women and prevent sexual exploitation.
Criminal justice system
Increased rates of delinquent or criminal behaviour may lead to contact with the criminal justice system [ 107 ]. Prevalence of ADHD in incarcerated populations is high, estimated at around one quarter (25.5%) but with no significant differences overall in relation to gender or age. There is however a lower prevalence in adult women than men (22.1% in female adults v. 31.2%, male adults), whereas female youths have a similar prevalence to male youths (30.8% and 29.5%, respectively) [ 107 ]. One study reported that only 18.8% of male adult offenders diagnosed with ADHD in prison had a prior diagnosis of ADHD [ 211 ]. It is likely that this proportion is even lower for females.
Evidence indicates that ADHD treatment is associated with reduced rates of criminality [ 212 ], is tolerated and effective in prison inmates [ 213 ], and improves their quality of life and cognitive function [ 214 ]. This has led to speculation that effective identification and treatment of ADHD may help to reduce reoffending, albeit with reservations surrounding potential for diversion or misuse of medications, treatment adherence, and discontinuity of ADHD treatment after release [ 215 ]. Current best practice recommendations for screening, identifying, treating and supporting ADHD in prisoners and youth offenders are provided in a previous review and consensus report [ 194 ], with particular recommendations for support provided for female offenders.
Females with ADHD are likely to be perceived to deviate substantially from stereotypical expectations of behaviour. The differential diagnosis between BPD and ADHD may be particularly important for females in forensic settings, where a high rate of comorbidity has been reported [ 216 ]. In the criminal justice system, including prison, there may possibly be a more sympathetic approach toward female offenders but, as for males, their ADHD is unlikely to be recognised. The group noted that ADHD is commonly perceived as ‘bad behaviour’ rather than a vulnerability in this setting, perhaps reflecting high rates of critical incidents (verbal and physical aggression, damage to property, self-injury) being reported in prison [ 217 ]. This may be intensified in female offenders with ADHD due to poor understanding of the condition. Further research regarding the interface between the criminal justice system and females with ADHD is needed.
Over 30 years ago, Berry, Shaywitz and Shaywitz warned that girls constitute a ‘silent minority’ in ADHD, with more internalised behaviour making them less likely to be referred for assessment [ 36 ]. This does not appear to have changed. Females with ADHD remain more likely to be unrecognised or mis-identified leading to lower than expected rates of referral, assessment and treatment for ADHD. Whilst this has been attributed to the higher rate of internalised and inattentive only presentation in girls, this omission is remarkable, given that the predominantly inattentive subtype of ADHD has been endorsed by the Diagnostic and Statistical Manual, a key diagnostic tool, for many years.
There are specific barriers that seem to hinder the recognition of ADHD in girls and women. These include symptomatic differences, gender biases due to stereotypical expectations, comorbidities and compensatory functions, which mask or overshadow the effects of ADHD symptoms. There is strong public perception that ADHD is a behavioural disorder that primarily affects males. Hence the challenge is to raise awareness and provide training on the presence and presentation of ADHD in females to agencies that regularly interface with children, young people and adults.
The current health and social care system appears to be better geared toward identifying and treating ADHD presenting alongside behavioural and externalising problems, in particular those that present as overt, disruptive and aggressive in nature, and are more commonly seen in boys and men. It is erroneous to consider that females do not present with hyperactive and impulsive symptoms – they do. However, these are generally less overt and aggressive in nature than the conduct problems displayed by males and instead seem to relate to more social-relational and psychosexual problems and behaviours. Understanding the expression of ADHD in females is the first step towards improving detection, assessment, and treatment, and ultimately enhancing long-term outcomes for girls and women with ADHD.
One of the most consistent topics discussed at the consensus (and across all breakout groups) related to how social-relational and psychosexual problems seem to be more marked in females with ADHD compared with males. Difficulties in managing and maintaining functional interpersonal relationships hinder some girls and women from developing or maintaining a positive social network or accessing peer support. ADHD symptoms and emotional lability seem to be related to dysfunctional coping strategies and dissatisfaction with life [ 77 ]. Lack of planning for the future [ 86 ] may mean that girls and women with ADHD lack constructive activities and occupations in adulthood. These effects may lead to affected girls and women becoming overwhelmed, anxious and low in mood. In turn they may respond by applying dysfunctional coping strategies, such as self-harm and substance use.
Females with ADHD overall have an earlier onset of sexual activity, more sexual partners, and an increased risk of contracting sexually transmitted infections or having an unplanned pregnancy. They are at risk of sexual exploitation, perceived exhibitionism or being considered promiscuous. Social stigma associated with risky sexual behaviour in women may augment social problems, and render affected women vulnerable to being victimised, bullied, harassed, abused, or entering into unhealthy relationships. Young girls with ADHD may become young mothers with ADHD (and possibly also mothers of children with ADHD). This is associated with a further reduction in educational and occupational opportunities. Research is needed to tease out the motivations and causal mechanisms of these behaviours and outcomes in females with ADHD, and if, how and why they may differ from those of males.
Treatment has been reported to moderate the lifetime risks of ADHD for both males and females. The consensus group identified where adjustments to approaches in treatment are needed to better support girls and women with ADHD. This includes more frequent treatment monitoring and psychoeducation at times of personal transition, with a greater focus on functional and emotional aspects of the disorder. The consensus group considered that multi-agency liaison will also be needed to support some girls and women with ADHD. Furthermore, raising awareness of, and providing training about, ADHD in institutions (e.g. educational, social, family, sexual health and criminal justice services) as well as the key healthcare system (primary health, child and adolescent mental health services and adult general psychiatry) will be helpful to improve detection of girls and women with ADHD, increase understanding and reduce stigma.
The consensus highlighted the relative dearth of research on the life-span experience of females with ADHD. Given the higher prevalence of ADHD in males, it would be helpful if studies reporting sex-mixed cohorts segregated data and results by gender. This would be particularly helpful in large clinical or population-based studies, where information on girls with ADHD would otherwise be buried as variance under the predominant male group. Providing sex-segregated results and data for all studies of ADHD (perhaps under supplementary data) would provide information to inform future meta-analyses.
Future research should investigate the presentation and needs of females with ADHD: how they might better be identified and assessed, and how their treatment response should best be evaluated and monitored to effectively improve outcomes. The most recent meta-analyses of gender differences in ADHD symptom presentation and associated features was reported over 15 years ago. An updated meta-analysis including all recent data is now needed. More research is also required to elucidate the interaction of hormones, ADHD symptoms and stimulant medication on functioning during key times of hormonal change (e.g. during the menstrual cycle, pregnancy and the postpartum period, and menopause), to help inform treatment plans. Factors that are associated with hyperactive/impulsive symptoms in females with ADHD and how these differ to males should be investigated further, including sexual behaviours and their motivations in girls and women with ADHD, as well as vulnerabilities to victimisation, physical and sexual assault and cyberbullying.
This consensus will inform effective identification, treatment and support of girls and women with ADHD. To facilitate identification, it is important to move away from the previously predominating ‘disruptive boy’ stereotype of ADHD and understand the more subtle and internalised presentation that predominates in girls and women. In treatment, it is important to consider a lifespan model of care for females with ADHD, which supports the complex and developmentally changing presentation of ADHD in females. Appropriate intervention is expected to have a positive impact on affected girls and women with ADHD, their families, and more broadly on society leading to increased productivity, decreased resource utilization and, most importantly, better outcomes for girls and women.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Abbreviations
ADHD Child Evaluation
Attention-Deficit/Hyperactivity Disorder
Autism Spectrum Disorder
Adult ADHD Self-report Rating Scale
Borderline Personality Disorder
Conners’ Adult Rating Scales
Cognitive Behavioural Therapy
Conners’ Comprehensive Behavior Rating Scales
Conduct Disorder
Conners’ Continuous Performance Test, third edition
Development and Wellbeing Assessment
Diagnostic Interview of Adult ADHD
Diagnostic Interview for ADHD in Adults with Intellectual Disability
Diagnostic and Statistical Manual of Mental Disorders
Education, Health and Care Plan
International Classification of Diseases
Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version
Learning Disability
Oppositional Defiant Disorder
Personalised Education Plan
The Vanderbilt ADHD Rating Scales
Quantified Behavior Test
Strengths and Difficulties Questionnaire
Swanson, Nolan, and Pelham-IV Questionnaire
Substance Use Disorder
United Kingdom of Great Britain and Northern Ireland
United Kingdom ADHD Partnership
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington DC: American Psychiatric Association; 2013.
Book Google Scholar
World Health Organization. International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10): Version 2019. 2019. https://icd.who.int/browse10/2019/en . Accessed 24 Apr 2020.
Google Scholar
Asherson P. ADHD across the lifespan. Medicine (Baltimore). 2016;40:623–7 https://doi.org/10.1016/j.mpmed.2016.08.012 .
Willcutt EG. The Prevalence of DSM-IV Attention-Deficit/Hyperactivity Disorder: A Meta-Analytic Review. Neurotherapeutics. 2012;9:490–9.
PubMed PubMed Central Google Scholar
Larsson H, Dilshad R, Lichtenstein P, Barker ED. Developmental trajectories of DSM-IV symptoms of attention-deficit/ hyperactivity disorder: Genetic effects, family risk and associated psychopathology. J Child Psychol Psychiatry. 2011;52:954–63.
PubMed Google Scholar
Lapalme M, Déry M, Dubé M, Lemieux A. Developmental Course of ADHD Symptoms Based on Multirater Report in Girls and Boys With or Without a Disruptive Behavior Disorder. J Emot Behav Disord. 2018;26:106–18.
Hinshaw SP, Owens EB, Sami N, Fargeon S. Prospective follow-up of girls with attention-deficit/hyperactivity disorder into adolescence: Evidence for continuing cross-domain impairment. J Consult Clin Psychol. 2006;74:489–99.
Monuteaux MC, Mick E, Faraone SV, Biederman J. The influence of sex on the course and psychiatric correlates of ADHD from childhood to adolescence: A longitudinal study. J Child Psychol Psychiatry Allied Discip. 2010;51:233–41.
Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: A meta-analysis of follow-up studies. Psychol Med. 2006;36:159–65.
Cheung CHM, Rijsdijk F, McLoughlin G, Brandeis D, Banaschewsk T, Asherson P, et al. Cognitive and neurophysiological markers of ADHD persistence and remission. Br J Psychiatry. 2016;208:548–55.
van Lieshout M, Luman M, Twisk JWR, van Ewijk H, Groenman AP, Thissen AJAM, et al. A 6-year follow-up of a large European cohort of children with attention-deficit/hyperactivity disorder-combined subtype: outcomes in late adolescence and young adulthood. Eur Child Adolesc Psychiatry. 2016;25:1007–17.
Du Rietz E, Cheung CHM, McLoughlin G, Brandeis D, Banaschewski T, Asherson P, et al. Self-report of ADHD shows limited agreement with objective markers of persistence and remittance. J Psychiatr Res. 2016;82:91–9.
Karam RG, Breda V, Picon FA, Rovaris DL, Victor MM, Salgado CAI, et al. Persistence and remission of ADHD during adulthood: A 7-year clinical follow-up study. Psychol Med. 2015;45:2045–56.
CAS PubMed Google Scholar
Thapar A, Cooper M. Attention Deficit Hyperactivity Disorder. Lancet. 2016;387:1240–50.
Gillberg C, Gillberg IC, Rasmussen P, Kadesjö B, Söderström H, Råstam M, et al. Co-existing disorders in ADHD - Implications for diagnosis and intervention. Eur Child Adolesc Psychiatry, Suppl. 2004;13:80–92.
Young S, Fridman A, Mandy W. Autistic spectrum disorder symptoms in children and adolescents with attention-deficit/ hyperactivity disorder: ameta-analytical review. Psychological Medicine. 2019:1–14 https://doi.org/10.1017/S0033291719002368 .
Mayes SD, Calhoun SL, Waxmonsky JG, Kokotovich C, Baweja R, Lockridge R, et al. Demographic Differences in Disruptive Mood Dysregulation Disorder Symptoms in ADHD, Autism, and General Population Samples. J Atten Disord. 2019;23:849–58.
Sobanski E. Psychiatric comorbidity in adults with attention-deficit/hyperactivity disorder (ADHD). Eur Arch Psychiatry Clin Neurosci. 2006;256(Suppl. 1):26–31.
Kessler R, Adler L, Barkley R, Biederman J, Conner CK, Demler O, et al. The Prevalence and Correlates of Adult ADHD in the United States: Results From the National Comorbidity Survey Replication. Am J Psychiatry. 2006;163:716–23 https://ajp.psychiatryonline.org/doi/abs/10.1176/ajp.2006.163.4.716 .
Thomas R, Sanders S, Doust J, Beller E, Glasziou P. Prevalence of Attention-Deficit/Hyperactivity Disorder: A Systematic Review and Meta-analysis. Pediatrics. 2015;135:e994–1001.
Simon V, Czobor P, Bálint S, Mészáros Á, Bitter I, Meszáros Á, et al. Prevalence and correlates of adult attention-deficit hyperactivity disorder: meta-analysis. Br J Psychiatry. 2009;194:204–11.
Michielsen M, Semeijn E, Comijs HC, Van De Ven P, Beekman ATF, Deeg DJH, et al. Prevalence of attention-deficit hyperactivity disorder in older adults in the Netherlands. Br J Psychiatry. 2012;201:298–305.
Nøvik TS, Hervas A, Ralston SJ, Dalsgaard S, Rodrigues Pereira R, Lorenzo MJ, et al. Influence of gender on attention-deficit/hyperactivity disorder in Europe - ADORE. Eur Child Adolesc Psychiatry. 2006;15(Suppl. 1):1–24.
Gershon J. A Meta-Analytic Review of Gender Differences in ADHD. J Atten Disord. 2002;5:143–54.
Hinshaw SP. Attention Deficit Hyperactivity Disorder (ADHD): Controversy, Developmental Mechanisms, and Multiple Levels of Analysis. Annu Rev Clin Psychol. 2018;14:291–316.
Greven CU, Richards JS, Buitelaar JK. Sex differences in ADHD. In: Banaschewski T, Coghill D, Zuddas A, editors. Oxford Textbook of Attention Deficit Hyperactivity Disorder. Oxford: Oxford University Press; 2018.
De Zwaan M, Gruß B, Müller A, Graap H, Martin A, Glaesmer H, et al. The estimated prevalence and correlates of adult ADHD in a German community sample. Eur Arch Psychiatry Clin Neurosci. 2012;262:79–86.
Moffitt TE, Houts R, Asherson P, Belsky DW, Corcoran DL, Hammerle M, et al. Is adult ADHD a childhood-onset neurodevelopmental disorder? Evidence from a four-decade longitudinal cohort study. Am J Psychiatry. 2015;172:967–77.
Cortese S, Faraone SV, Bernardi S, Wang S, Blanco C. Gender differences in adult attention-deficit/hyperactivity disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). J Clin Psychiatry. 2016;77:e421–8.
Cortese S. The neurobiology and genetics of Attention-Deficit/Hyperactivity Disorder (ADHD): What every clinician should know. Eur J Paediatr Neurol. 2012;16:422–33 https://doi.org/10.1016/j.ejpn.2012.01.009 .
Biederman J, Faraone SV, Monuteaux MC. Impact of exposure to parental attention-deficit hyperactivity disorder on clinical features and dysfunction in the offspring. Psychol Med. 2002;32:817–27.
Banerjee TD, Middleton F, Faraone SV. Environmental risk factors for attention-deficit hyperactivity disorder. Acta Paediatr. 2007;96:1269–74.
Taylor MJ, Lichtenstein P, Larsson H, Anckarsäter H, Greven CU, Ronald A. Is There a Female Protective Effect Against Attention-Deficit/Hyperactivity Disorder? Evidence From Two Representative Twin Samples. J Am Acad Child Adolesc Psychiatry. 2016;55:504–12 e2.
Rhee SH, Waldman ID. Etiology of sex differences in the prevalence of ADHD: An examination of inattention and hyperactivity-impulsivity. Am J Med Genet. 2004;127B:60–4.
Biederman J, Kwon A, Aleardi M, Chouinard VA, Marino T, Cole H, et al. Absence of gender effects on attention deficit hyperactivity disorder: Findings in nonreferred subjects. Am J Psychiatry. 2005;162:1083–9.
Berry CA, Shaywitz JE, Shaywitz B. Girls with attention deficit disorder: a silent minority? A report on behavioral and cognitive characterisitics. Pediatrics. 1985;76:801–9.
Gentile DA. Special Section : Sex or Gender? Technical Commentary A Call for a New Terminological Standard. Psychol Sci. 2012;4:120–2.
Williamson D, Johnston C. Gender differences in adults with attention-deficit/hyperactivity disorder: A narrative review. Clin Psychol Rev. 2015;40:15–27 https://doi.org/10.1016/j.cpr.2015.05.005 .
Gershon J. Gender Differences in ADHD. ADHD Rep. 2016;10:8–16.
Gaub M, Carlson CL. Gender differences in ADHD: A meta-analysis and critical review. J Am Acad Child Adolesc Psychiatry. 1997;36:1036–45 https://doi.org/10.1097/00004583-199708000-00011 .
Newcorn JH, Halperin JM, Jensen PS, Abikoff HB, Arnold LE, Cantwell DP, et al. Symptom profiles in children with ADHD: Effects of comorbidity and gender. J Am Acad Child Adolesc Psychiatry. 2001;40:137–46 https://doi.org/10.1097/00004583-200102000-00008 .
Millenet S, Laucht M, Hohm E, Jennen-Steinmetz C, Hohmann S, Schmidt MH, et al. Sex-specific trajectories of ADHD symptoms from adolescence to young adulthood. Eur Child Adolesc Psychiatry. 2018;27:1067–75 https://doi.org/10.1007/s00787-018-1129-9 .
Mowlem FD, Rosenqvist MA, Martin J, Lichtenstein P, Asherson P, Larsson H. Sex differences in predicting ADHD clinical diagnosis and pharmacological treatment. Eur Child Adolesc Psychiatry. 2019;28:481–9 https://doi.org/10.1007/s00787-018-1211-3 .
Quinn P, Wigal S. Perceptions of girls and ADHD: Results from a national survey. Medscape Gen Med. 2004;6.
Sciutto MJ, Nolfi CJ, Bluhm C. Effects of child gender and symptom type on referrals for ADHD by elementary school teachers. J Emot Behav Disord. 2004;12:247–53.
Pisecco S, Huzinec C, Curtis D. The Effect of Child Characteristics on Teachers’ Acceptability of Classroom-Based Behavioral Strategies and Psychostimulant Medication for the Treatment of ADHD. J Clin Child Psychol. 2001;30:413–21.
Mowlem F, Agnew-Blais J, Taylor E, Asherson P. Do different factors influence whether girls versus boys meet ADHD diagnostic criteria? Sex differences among children with high ADHD symptoms. Psychiatry Res. 2018;2019(272):765–73 https://doi.org/10.1016/j.psychres.2018.12.128 .
Quinn PO, Madhoo M. A review of attention-deficit/hyperactivity disorder in women and girls: uncovering this hidden diagnosis. Prim Care Companion CNS Disord. 2014;16 https://doi.org/10.4088/PCC.13r01596 .
Bramham J, Murphy DGM, Xenitidis K, Asherson P, Hopkin G, Young S. Adults with attention deficit hyperactivity disorder: An investigation of age-related differences in behavioural symptoms, neuropsychological function and co-morbidity. Psychol Med. 2012;42:2225–34.
Abikoff HB, Jensen PS, Arnold LLE, Hoza B, Hechtman L, Pollack S, et al. Observed classroom behavior of children with ADHD: Relationship to gender and comorbidity. J Abnorm Child Psychol. 2002;30:349–59.
Skogli EW, Teicher MH, Andersen PN, Hovik KT, Øie M. ADHD in girls and boys - gender differences in co-existing symptoms and executive function measures. BMC Psychiatry. 2013;13.
Rasmussen K. Untreated ADHD in Adults Are There Sex Differences in Symptoms, Comorbidity, and Impairment? J Atten Disord. 2008;2010:353–60.
Edvinsson D, Lindström E, Bingefors K, Lewander T, Ekselius L. Gender differences of axis I and II comorbidity in subjects diagnosed with attention-deficit hyperactivity disorder as adults. Acta Neuropsychiatr. 2013;25:165–74.
Klein RG, Mannuzza S, Ramos Olazagasti MA, Roizen E, Hutchison JA, Lashua EC, et al. Clinical and functional outcome of childhood attention-deficit/ hyperactivity disorder 33 years later. Arch Gen Psychiatry. 2012;69:1295–303.
Biederman J, Faraone SV, Monuteaux MC, Bober M, Cadogen E. Gender effects on attention-deficit/hyperactivity disorder in adults, revisited. Biol Psychiatry. 2004;55:692–700.
Quinn P. Gender differences in ADHD. In: Buitelaar JK, Kan CC, Asherson P, editors. ADHD in Adults: Characterization, Diagnosis, and Treatment. Cambridge: Cambridge Univeristy Press; 2011.
Stepp SD, Burke JD, Hipwell AE, Loeber R. Trajectories of attention deficit hyperactivity disorder and oppositional defiant disorder symptoms as precursors of borderline personality disorder symptoms in adolescent girls. J Abnorm Child Psychol. 2012;40:7–20.
Hollingdale J, Woodhouse E, Asherson P, Gudjonsson GH, Young S. A Pilot Study Examining ADHD and Behavioural Disturbance in Female Mentally Disordered Offenders. AIMS Public Heal. 2014;1:100–8.
Dalsgaard S, Mortensen PB, Frydenberg M, Maibing CM, Nordentoft M, Thomsen PH. Association between attention-deficit hyperactivity disorder in childhood and schizophrenia later in adulthood. Eur Psychiatry. 2014;29:259–63 https://doi.org/10.1016/j.eurpsy.2013.06.004 .
Dalsgaard S, Mortensen PB, Frydenberg M, Thomsen PH. Conduct problems, gender and adult psychiatric outcome of children with attention-deficit hyperactivity disorder. Br J Psychiatry. 2002;181:416–21.
Brewerton TD, Duncan AE. Associations between Attention Deficit Hyperactivity Disorder and Eating Disorders by Gender: Results from the National Comorbidity Survey Replication. Eur Eat Disord Rev. 2016;24:536–40.
Nazar BP, Bernardes C, Peachey G, Sergeant J, Mattos P, Treasure J. The risk of eating disorders comorbid with attention-deficit/hyperactivity disorder: A systematic review and meta-analysis. Int J Eat Disord. 2016;49:1045–57.
Cortese S, Moreira-Maia CR, St Fleur D, Morcillo-Peñalver C, Rohde LA, Faraone SV. Association between ADHD and obesity: A systematic review and meta-analysis. Am J Psychiatry. 2016;173:34–43.
Kim J, Mutyala B, Agiovlasitis S, Fernhall B. Health behaviors and obesity among US children with attention deficit hyperactivity disorder by gender and medication use. Prev Med (Baltim). 2011;52:218–22 https://doi.org/10.1016/j.ypmed.2011.01.003 .
Reyero F, Ponce G, Rodriguez-Jimenez R, Fernandez-Dapica P, Taboada D, Martin V, et al. High frequency of childhood ADHD history in women with fibromyalgia. Eur Psychiatry. 2011;26:482–3 https://doi.org/10.1016/j.eurpsy.2010.03.012 .
Sáez-Francàs N, Alegre J, Calvo N, Antonio Ramos-Quiroga J, Ruiz E, Hernández-Vara J, et al. Attention-deficit hyperactivity disorder in chronic fatigue syndrome patients. Psychiatry Res. 2012;200:748–53.
Gudjonsson GH, Sigurdsson JF, Sigfusdottir ID, Young S. An epidemiological study of ADHD symptoms among young persons and the relationship with cigarette smoking, alcohol consumption and illicit drug use. J Child Psychol Psychiatry Allied Discip. 2012;53:304–12.
Brassett-Grundy A, Butler NR. Prevalence and adult outcomes of Attention-Deficit/Hyperactivity Disorder: evidence from a 30-year prospective longitudinal study. BG Occas Pap no 2. 2004. /core/documents/download.asp?id=1210&log_stat=1.
Huntley Z, Young S. Alcohol and Substance Use History Among ADHD Adults: The Relationship With Persistent and Remitting Symptoms, Personality, Employment, and History of Service Use. J Atten Disord. 2014;18:82–90.
Charach A, Yeung E, Climans T, Lillie E. Childhood attention-deficit/hyperactivity disorder and future substance use disorders: comparative meta-analyses. J Am Acad Child Adolesc Psychiatry. 2011;50:9–21 https://doi.org/10.1016/j.jaac.2010.09.019 .
Ottosen C, Petersen L, Larsen JT, Dalsgaard S. Gender Differences in Associations between Attention-Deficit/Hyperactivity Disorder and Substance Use Disorder. J Am Acad Child Adolesc Psychiatry. 2016;55:227–34.e4 https://doi.org/10.1016/j.jaac.2015.12.010 .
Shaw P, Stringaris A, Nigg J, Leibenluft E. Emotion Dysregulation in Attention Deficit Hyperactivity Disorder. Am J Psychiatry. 2014;171:276–93.
Corbisiero S, Mörstedt B, Bitto H, Stieglitz R-D. Emotional Dysregulation in Adults With Attention-Deficit/Hyperactivity Disorder-Validity, Predictability, Severity, and Comorbidity. J Clin Psychol. 2017;73:99–112 https://doi.org/10.1002/jclp.22317 .
Faraone SV, Rostain AL, Blader J, Busch B, Childress AC, Connor DF, et al. Practitioner Review: Emotional dysregulation in attention-deficit/hyperactivity disorder – implications for clinical recognition and intervention. J Child Psychol Psychiatry Allied Discip. 2019;60:133–50.
Barkley RA, Fischer M. The unique contribution of emotional impulsiveness to impairment in major life activities in hyperactive children as adults. J Am Acad Child Adolesc Psychiatry. 2010;49:503–13 https://doi.org/10.1016/j.jaac.2010.01.019 .
Skirrow C, Asherson P. Emotional lability, comorbidity and impairment in adults with attention-deficit hyperactivity disorder. J Affect Disord. 2013;147:80–6.
Gudjonsson GH, Sigurdsson JF, Eyjolfsdottir GA, Smari J, Young S. The relationship between satisfaction with life, ADHD symptoms, and associated problems among university students. J Atten Disord. 2009;12:507–15.
Willcutt EG, Doyle AE, Nigg JT, Faraone S, Pennington BF. Validity of the executive function theory of attention-deficit/hyperactivity disorder: a meta-analytic review. Biol Psychiatry. 2005;57:1336–46 https://doi.org/10.1016/j.biopsych.2005.02.006 .
Boonstra AM, Oosterlaan J, Sergeant JA, Buitelaar JK. Executive functioning in adult ADHD: A meta-analytic review. Psychol Med. 2005;35:1097–108.
Rucklidge JJ, Tannock R. Neuropsychological profiles of adolescent with ADHD: Effects of reading difficulties and gender. J Child Psychol Psychiatry Allied Discip. 2002;43:988–1003.
Bora E, Pantelis C. Meta-analysis of social cognition in attention-deficit/hyperactivity disorder (ADHD): Comparison with healthy controls and autistic spectrum disorder. Psychol Med. 2016;46:699–716.
Ros R, Graziano PA. Social Functioning in Children With or At Risk for Attention Deficit/Hyperactivity Disorder: A Meta-Analytic Review. J Clin Child Adolesc Psychol. 2018;47:213–35 https://doi.org/10.1080/15374416.2016.1266644 .
Nijmeijer JS, Minderaa RB, Buitelaar JK, Mulligan A, Hartman CA, Hoekstra PJ. Attention-deficit/hyperactivity disorder and social dysfunctioning. Clin Psychol Rev. 2008;28:692–708.
Greene RW, Biederman J, Faraone SV, Monuteaux MC, Mick E, Dupre EP, et al. Social impairment in girls with ADHD: Patterns, gender comparisons, and correlates. J Am Acad Child Adolesc Psychiatry. 2001;40:704–10.
Babinski DE, Pelham WE, Molina BSG, Gnagy EM, Waschbusch DA, Yu J, et al. Late adolescent and young adult outcomes of girls diagnosed with ADHD in childhood: An exploratory investigation. J Atten Disord. 2011;15:204–14.
Young S, Heptinstall E, Sonuga-Barke EJS, Chadwick O, Taylor E. The adolescent outcome of hyperactive girls: Self-report of psychosocial status. J Child Psychol Psychiatry Allied Discip. 2005;46:255–62.
Young S, Chadwick O, Heptinstall E, Taylor E, Sonuga-Barke EJS. The adolescent outcome of hyperactive girls: Self-reported interpersonal relationships and coping mechanisms. Eur Child Adolesc Psychiatry. 2005;14:245–53.
Holmberg K, Hjern A. Bullying and attention-deficit-hyperactivity disorder in 10-year-olds in a Swedish community. Dev Med Child Neurol. 2008;50:134–8.
Sciberras E, Ohan J, Anderson V. Bullying and peer victimisation in adolescent girls with attention-deficit/hyperactivity disorder. Child Psychiatry Hum Dev. 2012;43:254–70.
Heiman T, Olenik-Shemesh D, Eden S. Cyberbullying involvement among students with ADHD: relation to loneliness, self-efficacy and social support. Eur J Spec Needs Educ. 2015;30:15–29 https://doi.org/10.1080/08856257.2014.943562 .
Becker SP, Mehari KR, Langberg JM, Evans SW. Rates of peer victimization in young adolescents with ADHD and associations with internalizing symptoms and self-esteem. Eur Child Adolesc Psychiatry. 2017;26:201–14.
Bruner MR, Kuryluk AD, Whitton SW. Attention-deficit/hyperactivity disorder symptom levels and romantic relationship quality in college students. J Am Coll Heal. 2015;63:98–108.
Yen JY, Ko CH, Yen CF, Wu HY, Yang MJ. The Comorbid Psychiatric Symptoms of Internet Addiction: Attention Deficit and Hyperactivity Disorder (ADHD), Depression, Social Phobia, and Hostility. J Adolesc Heal. 2007;41:93–8.
Ko C-H, Yen J-Y, Chen C-S, Chen C-C, Yen C-F. Psychiatric Comorbidity of Internet Addiction in College Students: An Interview Study. CNS Spectr. 2008;13:147–53 https://doi.org/10.1017/S1092852900016308 .
Wang B, Yao N, Zhou X, Liu J, Lv Z. The association between attention deficit/hyperactivity disorder and internet addiction: A systematic review and meta-analysis. BMC Psychiatry. 2017;17:1–12.
Yen JY, Liu TL, Wang PW, Chen CS, Yen CF, Ko CH. Association between Internet gaming disorder and adult attention deficit and hyperactivity disorder and their correlates: Impulsivity and hostility. Addict Behav. 2017;64:308–13 https://doi.org/10.1016/j.addbeh.2016.04.024 .
Yen J-Y, Yen C-F, Chen C-S, Tang T-C, Ko C-H. The Association between Adult ADHD Symptoms and Internet Addiction among College Students: The Gender Difference. CyberPsychology Behav. 2009;12:187–91 https://doi.org/10.1089/cpb.2008.0113 .
Andreassen CS, Billieux J, Griffiths MD, Kuss DJ, Demetrovics Z, Mazzoni E, et al. The relationship between addictive use of social media and video games and symptoms of psychiatric disorders: A large-scale cross-sectional study. Psychol Addict Behav. 2016;30:252–62.
Barkley RA, Fischer M, Smallish L, Fletcher K. Young adult outcome of hyperactive children: Adaptive functioning in major life activities. J Am Acad Child Adolesc Psychiatry. 2006;45:192–202 https://doi.org/10.1097/01.chi.0000189134.97436.e2 .
Owens EB, Zalecki C, Gillette P, Hinshaw SP. Girls with Childhood ADHD as Adults: Cross-Domain Outcomes by Diagnostic Persistence. J Consult Clin Psychol. 2017;85:723–36 https://doi.org/10.1037/ccp0000217.Girls .
Lehti V, Niemelö S, Heinze M, Sillanmöki L, Helenius H, Piha J, et al. Childhood predictors of becoming a teenage mother among Finnish girls. Acta Obstet Gynecol Scand. 2012;91:1319–25.
Skoglund C, Kopp Kallner H, Skalkidou A, Wikström A-K, Lundin C, Hesselman S, et al. Association of Attention-Deficit/Hyperactivity Disorder With Teenage Birth Among Women and Girls in Sweden. JAMA Netw Open. 2019;2:e1912463 https://doi.org/10.1001/jamanetworkopen.2019.12463 .
Barkley RA, Cox D. A review of driving risks and impairments associated with attention-deficit/hyperactivity disorder and the effects of stimulant medication on driving performance. J Safety Res. 2007;38:113–28.
Dalsgaard S, Ostergaard SD, Leckman JF, Mortensen PB, Pedersen MG. Mortality in children, adolescents, and adults with attention deficit hyperactivity disorder: A nationwide cohort study. Lancet. 2015;385:2190–6.
Molina BSG, Flory K, Hinshaw SP, Greiner AR, Arnold LE, Swanson JM, et al. Delinquent behavior and emerging substance use in the MTA at 36 months: Prevalence, course, and treatment effects. J Am Acad Child Adolesc Psychiatry. 2007;46:1028–40 https://doi.org/10.1097/chi.0b013e3180686d96 .
Dalsgaard S, Mortensen PB, Frydenberg M, Thomse PH. Long-term criminal outcome of children with attention deficit hyperactivity disorder. Crim Behav Ment Heal. 2013;23:86–98.
Young S, Moss D, Sedgwick O, Fridman M, Hodgkins P. A meta-Analysis of the prevalence of attention deficit hyperactivity disorder in incarcerated populations. Psychol Med. 2015;45:247–58.
Turgay A, Goodman DW, Asherson P, Lasser RA, Babcock TF, Pucci ML, et al. Lifespan Persistence of ADHD: The life transition model and its application. J Clin Psychiatry. 2012;73:192–201.
Patton GC, Viner R. Pubertal transitions in health. Lancet. 2007;369:1130–9.
Taylor A, Deb S, Unwin G. Scales for the identification of adults with attention deficit hyperactivity disorder (ADHD): A systematic review. Res Dev Disabil. 2011;32:924–38 https://doi.org/10.1016/j.ridd.2010.12.036 .
Conners. Comprehensive Behavior Rating Scales (Conners CBRS). North Tonawanda: Multi-Health Systems Inc; 2008.
Swanson JM. The SNAP-IV Teacher and Parent Rating Scale: 90 item. http://www.shared-care.ca/files/Scoring_for_SNAP_IV_Guide_26-item.pdf . Accessed 1 Oct 2019.
Young S. Rate and Rate C Scales, ACE. https://www.psychology-services.uk.com/adhd.htm . Accessed 1 Oct 2019.
Kaufman J, Birmaher B, Axelson D, Perepletchikova F, Brent D, Ryan N. K-SADS-PL Screener (2016). 2016. https://www.kennedykrieger.org/sites/default/files/library/documents/faculty/ksads-dsm-5-screener.pdf . Accessed 1 Oct 2019.
Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N. Schedule for affective disorders and Schizophrenia for schoolage children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36(7):980–8.
Goodman R. The Strengths and Difficulties Questionnaire: : A Research Note. J Child Psychol Psychiatry. 1997;38:581–6 http://www.sdqinfo.com/py/sdqinfo/b3.py?language=Englishqz (UK). Accessed 1 Oct 2019.
Wolraich M, Lambert W, Doffing M, Bickman L, Simmons T, Worley K. Psychometric Properties of the Vanderbilt ADHD Diagnostic Parent Rating Scale in a Referred Population. J Pediatr Psychol. 2003;28:559–86 https://www.nichq.org/sites/default/files/resource-file/NICHQ_Vanderbilt_Assessment_Scales.pdf . Accessed 1 Oct 2019.
Goodman R, Ford T, Richards H, Gatward R, Meltzer H. The Development and Well-Being Assessment: Description and initial validation of an integrated assessement of child and adolescent psychopathology. J Child Psychol Psychiatry Allied Discip. 2000;41:645–55 https://www.dawba.info/py/dawbainfo/b1list.py?language=English .
CAS Google Scholar
Conners C, Erhardt D, Sparrow E. The Conners adult ADHD rating scale. Toronto, Ontario, Canada: Multi-Health Systems Inc.; 1998.
Ustun B, Adler LA, Rudin C, Faraone SV, Spencer TJ, Berglund P, et al. The world health organization adult attention-deficit/hyperactivity disorder self-report screening scale for DSM-5. JAMA Psychiatry. 2017;74:520–6.
Psychology Services Limited. ADHD Child Evaluation: A diagnostic interview of ADHD in children. 2015. http://www.divacenter.eu/Content/Downloads/ACE.pdf . Accessed 16 May 2019.
DIVA Foundation. Young DIVA-5. 2017. http://www.divacenter.eu/DIVA.aspx?id=535&cc=GB . Accessed 16 May 2019.
Young S. Psychology Services Limited. ACE+: A diagnostic interview of ADHD in adults; 2016. p. 1–43. https://www.psychology-services.uk.com/resource-registration.htm?type=resources&id=ACEPLUS_English.pdf . Accessed 10 Jan 2020.
Epstein JN, Johnson DE, Conners CK. Conners’ Adult ADHD Diagnostic Interview for DSM-IV (CAADID). NorthTonawanda: Multi Health Systems; 2001. https://www.mhs.com/MHS-Assessment?prodname=caadhf .
DIVA Foundation. DIVA-5. 2017. http://www.divacenter.eu/DIVA.aspx?id=529&cc=GB . Accessed 16 May 2019.
Nadeau K, Littman E, Quinn P. AD/HD self-rating scale for girls. Advantage Books, LLC; 2015. https://www.researchgate.net/publication/242642028_ADHD_SELF-RATING_SCALE_FOR_GIRLS . Accessed 2 Oct 2019..
Nadeau K, Quinn P. Women’s AD/HD Self-assessment symptom inventory (SASI). In: Nadeau KG, Quinn PO, editors. Understanding Women With AD/HD. MD, USA: Advantage books; 2002. p. 24–43. http://www.merkercounseling.com/ADHDSelfAssessmentWomen.pdf . Accessed 1 Oct 2019.
Hinshaw SP, Owens EB, Zalecki C, Huggins SP, Montenegro-Nevado AJ, Schrodek E, et al. Prospective Follow-up of Girls with Attention-deficit/ Hyperactivity Disorder into Early Adulthood: Continuing Impairment Includes Elevated Risk for Suicide Attempts and Self-Injury. J Consult Clin Psychol. 2012;80:1041–51.
Swanson EN, Owens EB, Hinshaw SP. Pathways to self-harmful behaviors in young women with and without ADHD: A longitudinal examination of mediating factors. J Child Psychol Psychiatry Allied Discip. 2014;55:505–15.
Philipsen A, Hornyak M, Riemann D. Sleep and sleep disorders in adults with attention deficit / hyperactivity disorder. Sleep Med Rev. 2006;10:399–405.
Cortese S, Faraone SV, Konofal E, Lecendreux M. Sleep in Children With Attention-Deficit/Hyperactivity Disorder: Meta-Analysis of Subjective and Objective Studies. J Am Acad Child Adolesc Psychiatry. 2009;48:894–908 https://doi.org/10.1097/CHI.0b013e3181ae09c9 .
Kooij JJS, Bijlenga D, Salerno L, Jaeschke R, Bitter I, Balázs J, et al. Updated European Consensus Statement on diagnosis and treatment of adult ADHD. Eur Psychiatry. 2019;56:14–34 https://doi.org/10.1016/j.eurpsy.2018.11.001 .
Ohan JL, Johnston C. Gender appropriateness of symptom criteria for attention-deficit/ hyperactivity disorder, oppositional-defiant disorder, and conduct disorder. Child Psychiatry Hum Dev. 2005;35:359–81.
Young S. BGaze ACE. https://bgaze.com/en/ace . Accessed 2 Oct 2019.
Conners CK. Conners’ Continuous Performance Test - third edition. Bloomington: Pearson; 2014.
Ulberstad F. QbTest Technical Manual. rev. ed. Stockholm: QbTech AB; 2012.
Shaw M, Hodgkins P, Caci H, Young S, Kahle J, Woods AG, et al. A systematic review and analysis of long-term outcomes in attention deficit hyperactive disorder. BMC Med. 2012;10:1–15 https://doi.org/10.1186/1741-7015-10-99 .
Arnold LE, Hodgkins P, Caci H, Kahle J, Young S. Effect of treatment modality on long-term outcomes in attention-deficit/hyperactivity disorder: A systematic review. PLoS One. 2015;10:1–19.
National Institute for Health and Care Excellence. Attention deficit hyperactivity disorder: diagnosis and management. 2019. https://www.nice.org.uk/guidance/ng87 . Accessed 8 Nov 2019.
Cortese S, Adamo N, Del Giovane C, Mohr-Jensen C, Hayes AJ, Carucci S, et al. Comparative efficacy and tolerability of medications for attention-deficit hyperactivity disorder in children, adolescents, and adults: a systematic review and network meta-analysis. Lancet Psychiatry. 2018;5:727–38 https://doi.org/10.1016/S2215-0366(18)30269-4 .
Dulcan M, Dunne JE, Ayres W, Arnold V, Benson RS, Bernet W, et al. Practice parameters for the assessment and treatment of children, adolescents, and adults with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 1997;36(10 Suppl):85S–121S.
Mészáros Á, Czobor P, Bálint S, Komlósi S, Simon V, Bitter I. Pharmacotherapy of adult attention deficit hyperactivity disorder (ADHD): A meta-analysis. Int J Neuropsychopharmacol. 2009;12:1137–47.
Sharp WS, Walter JM, Marsh WL, Ritchie GF, Hamburger SD, Castellanos FX. ADHD in girls: Clinical comparability of a research sample. J Am Acad Child Adolesc Psychiatry. 1999;38:40–7.
Polanczyk G, Faraone SV, Bau CHD, Victor MM, Becker K, Pelz R, et al. The impact of individual and methodological factors in the variability of response to methylphenidate in ADHD pharmacogenetic studies from four different continents. Am J Med Genet Part B Neuropsychiatr Genet. 2008;147:1419–24.
Dalsgaard S, Leckman JF, Nielsen HS, Simonsen M. Gender and injuries predict stimulant medication use. J Child Adolesc Psychopharmacol. 2014;24:253–9.
CAS PubMed PubMed Central Google Scholar
Biederman J, Monuteaux MC, Spencer T, Wilens TE, Faraone SV. Do stimulants have a protective effect on the development of psychiatric disorders in youth with ADHD? A ten-year follow-up study. Pediatrics. 2009;124:71–8.
Daviss WB, Birmaher B, Diler RS, Mintz J. Does Pharmacotherapy for Attention-Deficit/Hyperactivity Disorder Predict Risk of Later Major Depression? J Child Adolesc Psychopharmacol. 2008;18:257–64 https://doi.org/10.1089/cap.2007.0100 .
Madjar N, Shlosberg D, Leventer-Roberts M, Akriv A, Ghilai A, Hoshen M, et al. Childhood methylphenidate adherence as a predictor of antidepressants use during adolescence. Eur Child Adolesc Psychiatry. 2019; https://doi.org/10.1007/s00787-019-01301-z .
Sternat T, Fotinos K, Fine A, Epstein I, Katzman MA. Low hedonic tone and attention-deficit hyperactivity disorder: Risk factors for treatment resistance in depressed adults. Neuropsychiatr Dis Treat. 2018;14:2379–87.
Chen MH, Pan TL, Hsu JW, Huang KL, Su TP, Li CT, et al. Attention-deficit hyperactivity disorder comorbidity and antidepressant resistance among patients with major depression: A nationwide longitudinal study. Eur Neuropsychopharmacol. 2016;26:1760–7 https://doi.org/10.1016/j.euroneuro.2016.09.369 .
Halmøy A, Fasmer OB, Gillberg C, Haavik J. Occupational Outcome in Adult ADHD: Impact of Symptom Profile, Comorbid Psychiatric Problems, and Treatment. J Atten Disord. 2009;13:175–87.
Dalsgaard S, Nielsen HS, Simonsen M. Consequences of ADHD medication use for children’s outcomes. J Health Econ. 2014;37:137–51 https://doi.org/10.1016/j.jhealeco.2014.05.005 .
Cortese S, Castellanos FX. The relationship between ADHD and obesity: Implications for therapy. Expert Rev Neurother. 2014;14:473–9.
Quinn PD, Chang Z, Hur K, Gibbons RD, Lahey BB, Rickert ME, et al. ADHD medication and substance-related problems. Am J Psychiatry. 2017;174:877–85.
Lachaine J, Beauchemin C, Sasane R, Hodgkins PS. Treatment patterns, adherence, and persistence in ADHD: A Canadian perspective. Postgrad Med. 2012;124:139–48.
Gajria K, Lu M, Sikirica V, Greven P, Zhong Y, Qin P, et al. Adherence, persistence, and medication discontinuation in patients with attention-deficit/hyperactivity disorder - A systematic literature review. Neuropsychiatr Dis Treat. 2014;10:1543–69.
Barner JC, Khoza S, Oladapo A. ADHD medication use, adherence, persistence and cost among Texas Medicaid children. Curr Med Res Opin. 2011;27:13–22.
Graham J, Coghill D. Adverse Effects of Pharmacotherapies for Attention-Deficit Hyperactivity Disorder : Epidemiology. Prevention and Management I. CNS Drugs. 2008;22:213–37.
Justice AJH, de Wit H. Acute effects of d -amphetamine during the follicular and luteal phases of the menstrual cycle in women. Psychopharmacology (Berl). 2002;145:67–75.
White TL, Justice AJH, De Wit H. Differential subjective effects of D-amphetamine by gender, hormone levels and menstrual cycle phase. Pharmacol Biochem Behav. 2002;73:729–41.
Justice AJH, de Wit H. Acute Effects of Estradiol Pretreatment on the Response to d-Amphetamine in Women. Neuroendocrinology. 2000;71:67–75.
Quinn PO. Treating adolescent girls and women with ADHD: Gender-specific issues. J Clin Psychol. 2005;61:579–87.
Crowell SE, Beauchaine TP, Linehan MM. A Biosocial Developmental Model of Borderline Personality: Elaborating and Extending Linehan’s Theory. Psychol Bull. 2009;135:495–510. https://doi.org/10.1037/a0015616 .
Matthies S, Philipsen A. Comorbidity of Personality Disorders and Adult Attention Deficit Hyperactivity Disorder (ADHD)—Review of Recent Findings. Curr Psychiatry Rep. 2016;18:1–7.
Young S, Gudjonsson GH. ADHD symptomatology and its relationship with emotional, social and delinquency problems. Psychol Crime Law. 2006;12:463–71.
Jiang HY, Zhang X, Jiang CM, Fu HB. Maternal and neonatal outcomes after exposure to ADHD medication during pregnancy: A systematic review and meta-analysis. Pharmacoepidemiol Drug Saf. 2019;28:288–95.
Spigset O, Brede WR, Zahlsen K. Excretion of Methylphenidate in Breast Milk Mirtazapine and Breastfeeding : Maternal and. Am J Psychiatry. 2007;2:348.
Sonuga-Barke E, Brandeis D, Cortese S, Daley D, Ferrin M, Holtmann M, et al. Nonpharmacological Interventions for ADHD: Systematic Review and Meta-analysis of Randomized Controlled Trials of Dietary and Psychological Treatments. Am J Psychiatry. 2013;170:275–89 https://doi.org/10.1176/appi.ajp.2012.12070991 .
Cortese S, Ferrin M, Brandeis D, Buitelaar J, Daley D, Dittmann RW, et al. Cognitive training for attention-deficit/hyperactivity disorder: Meta-analysis of clinical and neuropsychological outcomes from randomized controlled trials. J Am Acad Child Adolesc Psychiatry. 2015;54:164–74 https://doi.org/10.1016/j.jaac.2014.12.010 .
Cortese S, Ferrin M, Brandeis D, Holtmann M, Aggensteiner P, Daley D, et al. Neurofeedback for Attention-Deficit/Hyperactivity Disorder: Meta-Analysis of Clinical and Neuropsychological Outcomes From Randomized Controlled Trials. J Am Acad Child Adolesc Psychiatry. 2016;55:444–55.
Riesco-Matías P, Yela-Bernabé JR, Crego A, Sánchez-Zaballos E. What Do Meta-Analyses Have to Say About the Efficacy of Neurofeedback Applied to Children With ADHD? Review of Previous Meta-Analyses and a New Meta-Analysis. J Atten Disord. 2019.
Theule J, Cheung K, Aberdeen K. Children’s ADHD Interventions and Parenting Stress: A Meta-Analysis. J Child Fam Stud. 2018;27:2744–56 https://doi.org/10.1007/s10826-018-1137-x .
Bikic A, Reichow B, McCauley SA, Ibrahim K, Sukhodolsky DG. Meta-analysis of organizational skills interventions for children and adolescents with Attention-Deficit/Hyperactivity Disorder. Clin Psychol Rev. 2017;52:108–23 https://doi.org/10.1016/j.cpr.2016.12.004 .
Daley D, Van Der Oord S, Ferrin M, Danckaerts M, Doepfner M, Cortese S, et al. Behavioral interventions in attention-deficit/hyperactivity disorder: A meta-analysis of randomized controlled trials across multiple outcome domains. J Am Acad Child Adolesc Psychiatry. 2014;53:835–47.e5 https://doi.org/10.1016/j.jaac.2014.05.013 .
Young Z, Moghaddam N, Tickle A. The Efficacy of Cognitive Behavioral Therapy for Adults With ADHD: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J Atten Disord. 2020;24:875–88.
Xue J, Zhang Y, Huang Y, Tusconi M. A meta-analytic investigation of the impact of mindfulness-based interventions on ADHD symptoms. Med (United States). 2019;98:1–10.
Ramboll and the National Board of Social Services Denmark. Better help for young people and adults with ADHD and corresponding difficulties Final evaluation report. 2020. https://www.psychology-services.uk.com/danish-report-on-r-r2-adhd . Accessed 23 Apr 2020.
Young S, Myanthi AJ. Practitioner Review: Non-pharmacological treatments for ADHD: A lifespan approach. J Child Psychol Psychiatry Allied Discip. 2010;51:116–33.
De Ridder A, De Graeve D. Healthcare use, social burden and costs of children with and without ADHD in Flanders. Belgium. Clin Drug Investig. 2006;26:75–90.
Usami M. Functional consequences of attention-deficit hyperactivity disorder on children and their families. Psychiatry Clin Neurosci. 2016;70:303–17.
Shreeram S, He JP, Kalaydjian A, Brothers S, Merikangas KR. Prevalence of enuresis and its association with attention-deficit/ hyperactivity disorder among U.S. children: Results from a nationally representative study. J Am Acad Child Adolesc Psychiatry. 2009;48:35–41.
Ghanizadeh A, Mohammadi MR, Moini R. Comorbidity of Psychiatric Disorders and Parental Psychiatric Disorder of ADHD Children. J Atten Disord. 2008:149–55 https://doi.org/10.1177/1087054708314601 .
Young S, Smith J. Helping Children with ADHD. A CBT Guide for Practitioners, Parents and Teachers. Chichester: Wiley; 2017.
Young S. The STAR Detective Facilitator Manual: A Cognitive Behavioral Group Intervention to Develop Skilled Thinking and Reasoning for Children with Cognitive, Behavioral, Emotional and Social Problems. London: Jessica Kingsley; 2017.
Young S. Becoming a STAR Detective!: Your Detective’s Notebook for Finding Clues to How You Feel. London: Jessica Kingsley; 2017.
Atzori P, Usala T, Carucci S, Danjou F, Zuddas A. Predictive Factors for Persistent Use and Compliance of Immediate-Release Methylphenidate: A 36-Month Naturalistic Study. J Child Adolesc Psychopharmacol. 2009;19:673–81.
Blakemore S-J. Inventing ourselves: the secret life of the teenage brain: Doubleday; 2018.
Dawson AE, Wymbs BT, Evans SW, DuPaul GJ. Exploring how adolescents with ADHD use and interact with technology. J Adolesc. 2019;71:119–37 https://doi.org/10.1016/j.adolescence.2019.01.004 .
McManus S, Meltzer H, Brugha T, Bebbington P, Jenkins R. Adult Psychiatric Morbidity in England 2007: Results of a household survey. Leeds: The NHS Information Centre; 2009.
Treas J, Tai T. Gender Inequality in Housework Across 20 European Nations: Lessons from Gender Stratification Theories. Sex Roles. 2016;74:495–511 https://doi.org/10.1007/s11199-015-0575-9 .
Ferrant G, Pesando LM, Nowacka K. Unpaid Care Work: The missing link in the analysis of gender gaps in labour outcomes. OECD Development Centre. 2014. https://www.oecd.org/dev/development-gender/Unpaid_care_work.pdf . Accessed 15 May 2019.
Age UK. Breaking Point The Social Care Burden on Women. 2019. https://www.ageuk.org.uk/contentassets/c3dac0771e614672b363c5fe7e6f826e/breaking-point-age-uk.pdf . Accessed 15 May 2019.
Park JL, Hudec KL, Johnston C. Parental ADHD symptoms and parenting behaviors: A meta-analytic review. Clin Psychol Rev. 2017;56:25–39 https://doi.org/10.1016/j.cpr.2017.05.003 .
Young S, Gudjonsson G, Chitsabesan P, Colley B, Farrag E, Forrester A, et al. Identification and treatment of offenders with attention-deficit/hyperactivity disorder in the prison population: A practical approach based upon expert consensus. BMC Psychiatry. 2018;18:1–16.
Uchida M, Spencer TJ, Faraone SV, Biederman J. Adult Outcome of ADHD: An Overview of Results From the MGH Longitudinal Family Studies of Pediatrically and Psychiatrically Referred Youth With and Without ADHD of Both Sexes. J Atten Disord. 2018;22:523–34.
House of Lords Select Committee on the Equality Act. The Equality Act 2010: the impact on disabled people: London Station Off; 2016. p. 1–171.
Sedgwick JA. University students with attention deficit hyperactivity disorder (ADHD): A literature review. Ir J Psychol Med. 2018;35:221–35.
Veenman B, Luman M, Hoeksma J, Pieterse K, Oosterlaan J. A Randomized Effectiveness Trial of a Behavioral Teacher Program Targeting ADHD Symptoms. J Atten Disord. 2019;23:293–304.
LeFever GB, Villers MS, Morrow AL, Vaughn ES. Parental perceptions of adverse educational outcomes among children diagnosed and treated for ADHD: A call for improved school/provider collaboration. Psychol Sch. 2002;39:63–71.
Owens EB, Hinshaw SP. Adolescent Mediators of Unplanned Pregnancy among Women with and without Childhood ADHD. J Clin Child Adolesc Psychol. 2020;49:229–38 https://doi.org/10.1080/15374416.2018.1547970 .
Kuriyan AB, Pelham WE, Molina BSGG, Waschbusch DA, Gnagy EM, Sibley MH, et al. Young adult educational and vocational outcomes of children diagnosed with ADHD. J Abnorm Child Psychol. 2013;41:27–41 https://doi.org/10.1007/s10802-012-9658-z .
Polderman TJC, Boomsma DI, Bartels M, Verhulst FC, Huizink AC. A systematic review of prospective studies on attention problems and academic achievement: Review. Acta Psychiatr Scand. 2010;122:271–84.
de Zeeuw EL, van Beijsterveldt CEM, Ehli EA, de Geus EJC, Boomsma DI. Attention Deficit Hyperactivity Disorder Symptoms and Low Educational Achievement: Evidence Supporting A Causal Hypothesis. Behav Genet. 2017;47:278–89.
Moldavsky M, Groenewald C, Owen V, Sayal K. Teachers’ recognition of children with ADHD: Role of subtype and gender. Child Adolesc Ment Health. 2013;18:18–23.
Drigas AS, Ioannidou R-E, Kokkalia G, Lytras MD. ICTs, mobile learning and social media to enhance learning for attention difficulties. J Univers Comput Sci. 2014;20:1499–510.
Lasky AK, Weisner TS, Jensen PS, Hinshaw SP, Hechtman L, Arnold LE, et al. ADHD in context: Young adults’ reports of the impact of occupational environment on the manifestation of ADHD. Soc Sci Med. 2016;161:160–8.
Brook JS, Brook DW, Zhang C, Seltzer N, Finch SJ. Adolescent ADHD and Adult Physical and Mental Health, Work Performance, and Financial Stress. Pediatrics. 2013;131:5–13 https://doi.org/10.1542/peds.2012-1725 .
Adamou M, Arif M, Asherson P, Aw TC, Bolea B, Coghill D, et al. Occupational issues of adults with ADHD. BMC Psychiatry. 2013;13.
Garland AF, Hough RL, McCabe KM, Yeh M, Wood PA, Aarons GA. Prevalence of psychiatric disorders in youths across five sectors of care. J Am Acad Child Adolesc Psychiatry. 2001;40:409–18 https://doi.org/10.1097/00004583-200104000-00009 .
Harman JS, Childs GE, Kelleher KJ. Mental health care utilization and expenditures by children in foster care. Arch Pediatr Adolesc Med. 2000;154:1114–7 https://jamanetwork.com/journals/jamapediatrics/fullarticle/352217 .
Young S, González RA, Fridman M, Hodgkins P, Kim K, Gudjonsson GH. The economic consequences of attention-deficit hyperactivity disorder in the Scottish prison system. BMC Psychiatry. 2018;18:1–11.
Lichtenstein P, Halldner L, Zetterqvist J, Sjölander A, Serlachius E, Fazel S, et al. Medication for attention deficit-hyperactivity disorder and criminality. N Engl J Med. 2012;367:2006–14.
Ginsberg Y, Lindefors N. Methylphenidate treatment of adult male prison inmates with attention-deficit hyperactivity disorder: Randomised double-blind placebo-controlled trial with open-label extension. Br J Psychiatry. 2012;200:68–73.
Ginsberg Y, Hirvikoski T, Grann M, Lindefors N. Long-term functional outcome in adult prison inmates with ADHD receiving OROS-methylphenidate. Eur Arch Psychiatry Clin Neurosci. 2012;262:705–24.
Ginsberg Y, Långström N, Larsson H, Lichtenstein P. ADHD and criminality: Could treatment benefit prisoners with ADHD who are at higher risk of reoffending? Expert Rev Neurother. 2013;13:345–8.
Rösler M, Retz W, Yaqoobi K, Burg E, Retz-Junginger P. Attention deficit/hyperactivity disorder in female offenders: Prevalence, psychiatric comorbidity and psychosocial implications. Eur Arch Psychiatry Clin Neurosci. 2009;259:98–105.
Young S, Gudjonsson GH, Wells J, Asherson P, Theobald D, Oliver B, et al. Attention deficit hyperactivity disorder and critical incidents in a Scottish prison population. Pers Individ Dif. 2009;46:265–9 https://doi.org/10.1016/j.paid.2008.10.003 .
Download references
Acknowledgements
We are grateful to the assistance of Catherine Coles, Alex Nolan and Hannah Stynes who attended the consensus meeting and made notes during the breakout sessions.
The meeting was funded by the UK ADHD Partnership (UKAP), who has been in receipt of unrestricted educational donations from Takeda. Takeda had no influence or involvement in determining the topic and arrangements of the day, the consensus process and outcomes, or writing the final manuscript. Other than reimbursement of travel expenses to attend the meeting, none of the authors received any financial compensation for attending the meeting or writing the manuscript, aside from CS who received funds for medical writing assistance.
Author information
Authors and affiliations.
Psychology Services Limited, PO 1735, Croydon, London, CR9 7AE, UK
Susan Young
Department of Psychology, Reykjavik University, Reykjavik, Iceland
Susan Young, Bryndís Björk Ásgeirsdóttir & Gisli Gudjonsson
Social, Genetic and Developmental Psychiatry Centre, Institute of Psychiatry, Psychology & Neuroscience, Kings College London, London, UK
Nicoletta Adamo & Jane Sedgwick
Service for Complex Autism and Associated Neurodevelopmental Disorders, South London and Maudsley NHS Foundation Trust, Michael Rutter Centre, London, UK
Nicoletta Adamo
Oxford ADHD and Autism Centre, Oxford, UK
Polly Branney
ADHD Action, Harrogate, North Yorkshire, UK
Michelle Beckett
CLC Consultancy, Perth, UK
William Colley
Manor Hospital, Oxford, UK
Sally Cubbin
National Autism Unit, Bethlem Royal Hospital, South London and Maudsley NHS Foundation Trust, Beckenham, UK
Quinton Deeley
Forensic and Neurodevelopmental Sciences, Institute of Psychiatry, Psychology, and Neuroscience, London, UK
Quinton Deeley & Emma Woodhouse
South London & Maudsley NHS Foundation Trust, Maudsley Health, Abu Dhabi, UAE
Emad Farrag
Department of Psychology, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, London, UK
Gisli Gudjonsson
Independent Consultant in Child and Adolescent Psychiatry, Private Practice, London, UK
Michael Rutter Centre, South London and Maudsley Hospital, London, UK
Jack Hollingdale
Koc University, Istanbul, Turkey
ADHD Foundation, Liverpool, UK
ADHD and Psychiatry Services Limited, Liverpool, UK
Peter Mason
Tavistock and Portman NHS Foundation Trust, London, UK
Eleni Paliokosta
St Thomas’ Hospital London, London, UK
Sri Perecherla
Faculty of Nursing, Midwifery & Palliative Care, King’s College London, London, UK
Jane Sedgwick
Cambridge Cognition, Cambridge, UK
Caroline Skirrow
School of Psychological Science, University of Bristol, Bristol, UK
Neuropsychiatry Team, National Specialist CAMHS, South London and Maudsley NHS Foundation Trust, London, UK
Kevin Tierney
Adult ADHD and AS Team & CYP ADHD and ASD Service in Northamptonshire, Northampton, UK
Kobus van Rensburg
Compass, London, UK
Emma Woodhouse
You can also search for this author in PubMed Google Scholar
Contributions
SY was responsible for the planning and scientific input of this consensus statement. All authors (except NA and EF) attended the consensus meeting. CS completed the first draft of the manuscript. It was substantially revised by SY with further input from EF and BC. The second draft was circulated to all authors for comment and endorsement of the consensus. Following further amendments, the final draft was circulated once more and all authors have read and approved the final manuscript.
Corresponding author
Correspondence to Susan Young .

Ethics declarations
Ethics approval and consent to participate.
The current report reflects a review of the research literature on ADHD in girls and women, and a consensus agreement amongst all authors based on this evidence and their clinical experience. As a result, neither consent for participation, nor ethical approval for this work were required.
Consent for publication
Not applicable
Competing interests
In the last 5 years: SY has received honoraria for consultancy and educational talks years from Janssen, HB Pharma and/or Shire. She is author of the ADHD Child Evaluation (ACE) and ACE+ for adults; and lead author of R&R2 for ADHD Youths and Adults. PH has received honoraria for consultancy and educational talks in the last 5 years from Shire, Janssen and Flynn. He has acted as an expert witness for Lilly. PM has received honoraria for consultancy and educational talks from Shire and Flynn. KvR has received honoraria for educational talks from Shire, Lilly, Janssen, Medici and Flynn. In addition SY, PB, WC, PH, PM and EW are affiliated on a full-time basis with consultancy firms/private practices. CS is employed by Cambridge Cognition. JS has received speakers’ honoraria from Shire, is in receipt of an educational grant from the Royal College of Nursing (RCN) Foundation Trust for a contribution towards PhD tuition & conference fees/ costs and is an Executive Committee Member of the UK Adult ADHD Network ( UKAAN.org ). The remaining authors have no disclosures.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Young, S., Adamo, N., Ásgeirsdóttir, B.B. et al. Females with ADHD: An expert consensus statement taking a lifespan approach providing guidance for the identification and treatment of attention-deficit/ hyperactivity disorder in girls and women. BMC Psychiatry 20 , 404 (2020). https://doi.org/10.1186/s12888-020-02707-9
Download citation
Received : 27 January 2020
Accepted : 31 May 2020
Published : 12 August 2020
DOI : https://doi.org/10.1186/s12888-020-02707-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Attention-deficit/hyperactivity disorder (ADHD)
- Identification
- Interventions
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Copyright © 2024 OccupationalTherapy.com - All Rights Reserved
Pediatric Case Study: Child with ADHD
Nicole quint, dr.ot, otr/l.
- Early Intervention and School-Based
To earn CEUs for this article, become a member.
unlimit ed ceu access | $129/year
Attention deficit hyperactivity disorder (adhd).
Hello everyone. Today, we are going to be talking about attention deficit hyperactivity disorder. I consider this to be under the umbrella of "invisible diagnoses." This population has a special place in my heart because it is very easy to misconstrue some of the challenges that they have as intentional and behavior-based, and therefore, sometimes they get a bad rap. Thus, I am always happy to help kids with ADHD.
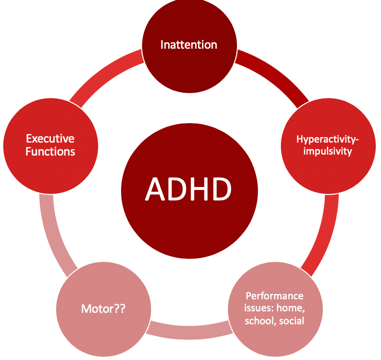
Figure 1. Overview of ADHD.
Individuals with ADHD have a lot of challenges that affect their occupational participation and performance. I think most of us are very comfortable with the idea that inattention, hyperactivity, and impulsivity are the hallmarks, but what sometimes can get lost is the idea that executive functions are very much affected by impulsivity. Motor issues are also often involved with kids with ADHD and are not always considered. In fact, there is a lot of evidence to support that the motor needs of these kids often go unaddressed. Typically, these kids come to us when parents or schools have major concerns about their behavior. Therefore, this tends to be where everyone focuses their attention. Oftentimes, the motor issues then fly under the radar and do not get addressed. The cool thing is that motor interventions can be the means to make some really significant changes for these kids, particularly in the area of executive function. There is a win-win situation when we address the motor issues. Lastly, they tend to also have performance issues not only in their home environment but also in their school and social environments as well.
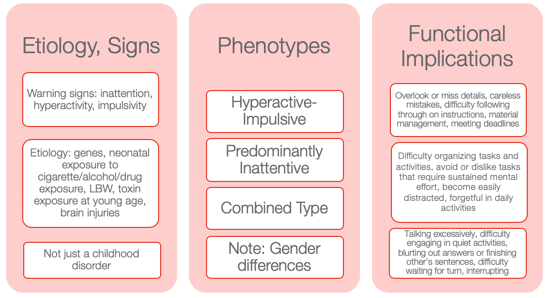
Figure 2. Other information from the NIMH Information Resource Center (2020).
I wanted to provide some information to help you to appreciate how diverse ADHD is. Many might still use ADD when we are talking about the children who have an inattentive type as it seems to make more sense. However, that is not how it is defined in the Diagnostic and Statistical Manual of Mental Disorders (DSM–5).
Etiology and Signs
The etiology and the signs are inattention, hyperactivity, and impulsivity. We also know there is a genetic predisposition to this. Neonatal exposure to cigarettes, alcohol, and drugs can also lead to ADHD. Low birth weight and toxin exposure are some of the environmental elements. ADHD can also be the result of a brain injury. This is not just a childhood disorder, and people do not grow out of it. In fact, the symptoms can actually get worse as life gets harder as one gets older. Adults who have ADHD can have some significant struggles, particularly if they do not know that they have ADHD or if it was never addressed.
There are three phenotypes: hyperactive-impulsive type, predominantly inattentive type, and a combination type. I think the hyperactive-impulsive type is the picture most people have when they think of ADHD. Then, we have the predominantly inattentive type. These are the daydreamers or the individuals that jump from one thought to the next. They have a really hard time staying focused for long. Lastly, there is the combined type. This is where we see both elements of inattention and hyperactivity and/or impulsivity. I think it is really important to also appreciate gender differences. You can see very different types of ADHD in girls versus boys. Boys obviously tend to be of the hyperactive-impulsive type, but even the inattentive type can be a little different. Girls, who have ADHD, tend to be talkative and a little more anxious. They definitely have a different predisposition as opposed to the boys. Thus, it might be the same diagnosis but look very different between the genders.
Functional Implications
Functional implications become extremely important. These are individuals who tend to overlook or miss details. They might make careless mistakes. They have difficulty following through with directions at school. Material management can become very challenging especially dealing with paperwork. They can miss deadlines and have a hard time keeping track of and prioritizing tasks. These are some of the higher-level executive functions. You might also see an avoidance or an expressed dislike of tasks that require a significant amount of sustained mental effort. They might tell you it is too hard, and they might feel very overwhelmed. They become very easily distracted by anything. The use of electronics adds to the issue. They can be forgetful in daily activities, talk excessively, have difficulty engaging in quiet activities, and tend to blurt out answers or finish others' sentences. Often, the perception is they are interrupting and being rude. They may have difficulty waiting for their turn or interrupt during someone else's turn. These are examples of impulsive behaviors. We will talk more about this when we get to executive functions.
Differential Diagnosis Between ADHD and SPD
- A high rate of comorbidity between SMD and ADHD
- ADHD and SMD
- Both at risk for limited participation in many aspects of daily life
- ADHD slightly worse attention scores than SMD
- Tactile, taste/smell, and movement sensitivity, visual-auditory sensitivity; behavioral manifestations of sensory systems
- Exaggerated electrodermal responses to sensory stimulation, thus increased risk of sympathetic “fight or flight” reactions
(Miller et al., 2012; Yochman et al., 2013)
Sometimes, kids who have ADHD also have some sensory issues. You may wonder, "Do they have just ADHD by itself?" This is probably one of the most common questions I get when working with kids with ADHD whether it is from teachers, other therapists, or from parents. Next, we are going to be talking about a child who has straight ADHD. However, for a few minutes, I want to talk about the whole idea of differential diagnosis between ADHD and SPD and how this all fits together. There is a very high comorbidity between sensory modulation disorder and ADHD. When I am referring to sensory modulation disorder, I am using the Lucy Jane Miller nosology. Sensory modulation disorder refers to the over-responsive, under-responsive, and/or craving of sensory input. For both ADHD and sensory modulation disorder, you will see that these diagnoses are both at risk for limited participation. These are kids who will not participate in certain activities because the sensory input is too much or overwhelming for them. ADHD will have slightly worse attention scores than SMD when you complete a formal attention test like the Test of Everyday Attention. However, you will see the same kind of impulsive behaviors.
Those with sensory modulation disorders tend to have difficulty with tactile, taste, smell, and movement sensitivities. You might also see some visual-auditory sensitivity so there are some behavioral manifestations that come of that. They might become stressed related to fears of vestibular or other movement input. They might also dislike certain noises or touch.
They found in the research that sensory modulation dysfunction, not ADHD , will have an exaggerated electrodermal response to sensory stimulation. This means that they have an increased risk of sympathetic activation which is the fight-or-flight, freeze/faint reactions, and meltdowns. When you have a child with meltdowns, you want to investigate if they have sensory modulation dysfunction right away. And, if you have a child with ADHD who does not have a history of meltdowns, that is a really good sign of your initial hypothesis. While this alone does not mean that they do not a sensory modulation dysfunction, chances are that they do not. Additionally, they might have dyspraxia or a discrimination disorder.
This is just a brief summary of how this all comes to play with an ADHD diagnosis and possible comorbidities.
Case Introduction: Jeremy (Age 9, ADHD, Combined Type)
- He lives with his mother and older sister in SFH and goes to his father’s house on the weekend (divorced)
- He is in the 4th grade and has an IEP for OHI
- Strengths: funny, good at math, helps the family to take care of pets, watches WWE with father, loves dogs, likes to play board games (Monopoly, Sorry)
- School concerns: material management, organization, completing tasks or losing work , impulsive, social difficulties (short-lived relationships, fights), “lacks self-control” and “messy”, underperforming and sometimes seems “lost”
- Family concerns: Fights with a sibling, sleep difficulties, messy room, messy notebooks, and backpack, loses things, avoids homework, resists bedtime, difficult to wake in the morning and slow with routine , poor hygiene
- Jeremy’s goal: make friends, be able to find his schoolwork, have good friends, be better at kickball and wrestling
Jeremy is nine, and his diagnosis is ADHD, combined type. I have a feeling Jeremy is probably similar to a lot of the kids you see. I know I have seen a lot of these types of kids. He lives with his mother and older sister in a single-family home and goes to his father's house on the weekend because of a divorce. He is in the fourth grade, is eligible for an IEP because of an OHI (other health impairment), and is eligible for special education services because of his diagnosis of ADHD.
I always like to start with strengths with all kids, especially ADHD because these kids can have a really hard time with confidence and self-esteem. They also get blamed for their behaviors. For his strengths, he is funny, good at math, and he likes to help take care of his pets at home. He likes to watch wrestling, World Wrestling Federation (WWF) with his father, loves dogs, and loves to play board games. He is really good at Monopoly and Sorry.
At school, he had challenges with material management, organization, completing tasks, and not losing work. These last two are highlighted as we are going to focus on that. He is impulsive, and he has social difficulties. His teacher described his relationships as short-lived. He would have a friend, and then all of a sudden, they were not friends anymore. She also reported that he lacked self-control, was messy, and thought he underperformed. And, she felt like he always seemed lost. When they were going through the instructions or going through something, he was always looking at his peer's work or looking confused while he was trying to figure out what was going on.
The family had some concerns about his fighting with a sibling, significant sleep difficulties, a messy room, messy notebooks and backpack, and that he would often lose things. He also avoided his homework and resisted bedtime. As a result, it was very difficult to wake him up in the morning, and he was slow with his AM routine. His mom said that he also had an impulsive way of performing hygiene tasks. For example, he would brush his teeth in two seconds and say he was done. Everything was quick and impulsive. This is very typical for boys with this type of ADHD.
His goals were to make friends and find his school work. He said it was very stressful to always feel like he was losing his school work. He was motivated to do well in school. He did not just want to make friends, but he wanted to have good friends. He also wanted to be better at kickball because that is what the kids played at recess and in PE. He also wanted to be better at wrestling as not only did he like to watch with his dad, but he also liked to wrestle with him.
I want to go back to the highlighted areas in my list: completing tasks, losing work, and difficulty waking in the morning. These are the areas we are going to focus on.
Assessments
Assessments are one of the most challenging things for people because they are often under a time crunch, and the reports are difficult to write up and are time-consuming. However, it is really important with these kids as it gives us a full perspective on where they are having challenges. Knowing that he has "ADHD combined type" does not really tell us about his occupational performance and participation. We want to really get all that information. I like to be pretty thorough, and I will scatter assessments throughout my time with them to try to get a good idea. Again, I really like to check out their motor skills. I have kids that are superstars in sports, but I will still find out that there are some motor problems.
Typically, the motor challenges with ADHD have to do with bilateral coordination, dexterity, and those kinds of things. They might be good at some things, like basketball or baseball, but this does not mean that they are good at fine manipulation. Thus, it is really important to find out where they are. Figure 3 shows a summary of the assessments I did with Jeremy.
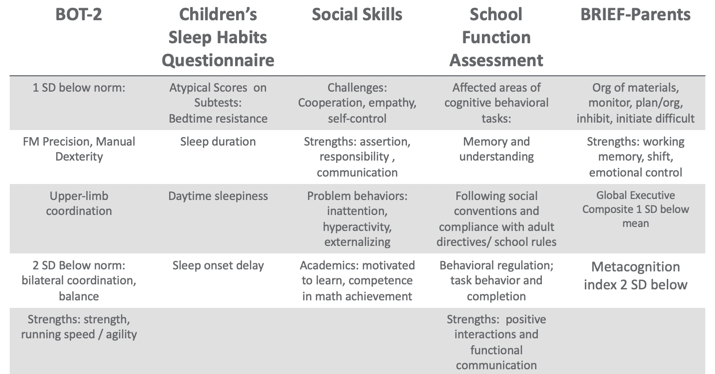
Figure 3. Assessment results.
Using the BOT, I found that Jeremy was one standard deviation below the norm in fine motor, precision, and manual dexterity, which was not surprising. He was two standard deviations below the norm in bilateral coordination and balance. However, his overall strength, running speed, and agility were fine.
There are many great tools out there for sleep including free ones. One of my favorites is the Sleep Habits Questionnaire. It is free online. It is great because it uncovers behaviors regarding going to bed, sleep duration, daytime sleepiness, and sleep onset delay. Many kids with ADHD have an overactive thinking process which then causes a sleep latency problem. It is hard for them to settle their brain and get to sleep. They also might have difficulty with sleep duration and not get enough sleep or good quality of sleep. If their arousal level is still high at night, it' is hard to get them to calm down and want to go to bed, especially if they are very disorganized in their thinking. This questionnaire gives you good information. Our results with Jeremy found that had bedtime resistance, sleep duration, daytime sleepiness, and sleep onset delays that were all atypical scores.
I also did a social skills assessment with him because his goal was to make friends, and school indicated that he had a hard time with solid friendships. I like to have a social-emotional learning perspective, and the more I know about a child's emotional intelligence, the better. We want these kids to be successful in their social interactions because that affects their whole life. With the Social Skills Improvement System (SSIS) Rating Scales, I found challenges with cooperation, empathy, and self-control. His strengths included assertion, responsibility, and communication. Under "problem behaviors", I found inattention, hyperactivity, and some externalizing behaviors. With his diagnosis, this all seems to fit. For academics, he was motivated to learn and had competence in math achievement. We already knew he had strengths in math.
I also did the School Function Assessment. I love this tool. There is one section that is a little dated as it talks about a floppy disk or something, but the other information on there is fantastic. This is especially true if you have kids who have a hard time following rules, social conventions, and material management. You can give it to the teacher, and they can score that. I found that Jeremy had some affected areas with memory and understanding, following social conventions, and compliance with adult directives and school rules. Additionally, he had some behavioral regulation issues, and task behavior and completion were difficult for him. His strengths included positive interactions and functional communication. Communication is strong for him,= which is a good thing.
The BRIEF (Behavior Rating Inventory of Executive Function) is an executive function tool that I did that with his parents. What we found was that the organization of materials, monitoring, planning and organization, inhibition, and initiation were difficult for him. His strengths were his working memory. Additionally, cognitive shifting and emotional control were also strong. However, his global executive composite was one standard deviation below the mean which means that he was low in everything. While it was not devastatingly low, he was below the average in everything. He struggled the most in metacognition, and that was two standard deviations below the norm. Thinking about his own thinking was a struggle for him.
From an observation standpoint, I also got a video from him mom of his AM routine so I could see what that looked like. He was in slow motion, very tired, not wanting to do the routine, and his performance was of low quality, I would put it, writing examples from school, because sometimes you'll see that the handwriting is indicative kind of the brain and the body not matching up, the brain going a little faster than the body. And so I also had a homework video watching him kind of resist homework. And then I did ocular motor testing, checked his tracking, convergence, divergence, and saccades and those kinds of things. Because there is a correlation between having some difficulties with that sometimes. But he actually was fine, and that wasn't a complaint from parents. So I just wanted to make sure it wasn't an issue that we were missing. So that gave me a lot of information.
Research Implications: Assessment
This is information about some of the research implications regarding the assessment process and kind of why I chose the tools that I chose and why I recommend a comprehensive one.
- Motor: Children with parent-reported motor issues received more PT than those with teacher-reported motor issues (risk)/undertreated motor problems in children with ADHD (due to behavioral factors in referral); HW difficulties; higher ADHD and lower motor proficiency scores reported more sleep problems (Papadopoulos et al., 2018)
- Sleep: Sleep deficits negatively affect inhibitory control (Cremone-Caira et al., 2019); Difficulties initiating and maintaining sleep 25-50% in ADHD (Corkum et al., 1998); Prevalence of sleep disorders 84.8 % affecting QoL (Yurumez & Gunay Kilic, 2013)
- EF: Motor skills and EF related (Pan et al., 2015); boys with ADHD have lower EF abilities than typical peers on both performance-based and parent report tools, thus combo is recommended (Sgunibu et al., 2012)
- Social: Children with ADHD 50% lower odds of sports participation than children with asthma with higher incidences of screen time (Tanden et al., 2019); childhood ADHD associated with obesity (Kim et al., 2011); underlying lack of interpersonal empathy (Cordier et al., 2010); Playfulness indicators: ADHD group “typical” with some difficult items but difficulty with basic skills (sharking) (Wilkes-Gillan et al., 2014); seek green outdoor settings at a higher rate (Taylor & Kuo, 2011)
For motor, Papadopoulos and his group (2018) found that there is some difficulty with handwriting. They also reported the higher ADHD and lower motor proficiency scores, the more sleep problems. The fact that Jeremy had sleep problems made me want to look at his motor skills for this reason. This is another interesting one. Children with parent-reported motor issues received more PT than those with teacher-reported motor issues. The fact that we listen to the parents more than the teachers about motor issues is important to consider. Under-treated motor problems in children with ADHD are really due to a behavioral focus so that is why it tends to get missed.
Sleep deficits negatively affect inhibitory control (Cremone-Caira et al., 2019). If we know that these kids have inhibition issues, we need to help them get some sleep. Poor sleep is only reinforcing their challenges and making it worse. They found that there were difficulties initiating and maintaining sleep at a rate of 20 to 50% of kids with ADHD (Corkum et al., 1998). Now, granted, that was 20 years ago, but they have replicated that since. And, if you have a sleep disorder, there is an 84.8% chance that it is negatively affecting your quality of life (Yurumez & Gunay Kilic, 2013).
Motor skills and executive functions are related. If you have some motor difficulties, it is going to influence your executive function ability (Pan et al., 2015). Boys with ADHD have lower executive function ability than typical peers on both performance-based and parent report tools, thus, it is really important that you use a combination of both performance and parent report tools (Sgunibu et al., 2012).
Children with ADHD are 50% less likely to participate in sports than children with asthma (Tanden et al., 2019). I find that amazing. Kids with ADHD also have a higher incidence of screen time usage, and we know that that is always a challenge (Tanden et al., 2019). Childhood ADHD is also associated with obesity. Hence, if you are not doing anything physical and you are sitting there watching your computer or playing video games, and you are impulsive, you are more likely to be obese (Kim et al., 2011). An underlying lack of interpersonal empathy can be something that you often see in ADHD. This affects social abilities and participation and success (Cordier et al., 2010). There are also playfulness indicators. An ADHD group might score as "typical" with some difficult play criteria, but then have more difficulty with basic items (Wilkes-Gillan et al., 2014). Their play may be developmentally out of whack. Again, they might be okay with some high-level types of behaviors, but then when it comes to something simple like taking turns or sharing, they cannot do it. Sometimes we have to go back and practice these rudimentary skills. This might be why they are struggling socially because they are having problems with age-inappropriate items. Lastly, these kids with ADHD really seek green outdoor settings at a higher rate (Taylor & Kuo, 2011). It would be interesting to monitor how outside time might influence their performance on assessments.
EF and Self-Regulation Connection
- Inhibitory control
- Cognitive/mental flexibility
- Working memory
Can these kids self-regulate? When they cannot, it does not work out well for them in school or at home, and it does not work out well in terms of social abilities. When they become adults, they have trouble keeping and maintaining a job. This is the definition of EF.
Some of you might be very familiar with this definition, but it is also quite complicated. This is how we remember information, filter distractions, resist impulses, and sustain attention during an activity that is also goal-directed. While we also adjust our plan as needed to avoid frustration in the process. That is a lot of working parts. Many times, you see people refer to executive functions like an air traffic controller of information and materials. These are the "big 3."
This is how we remember information, filter distractions, resist impulses, and sustain attention during an activity that is goal-directed while adjusting our plan as necessary and avoiding frustration!
Miyake, A., Friedman, N. P., Emerson, M. J., Witzki, A. H., Howerter, A., & Wager, T. D. (2000). The unity and diversity of executive functions and their contributions to complex "frontal lobe" tasks: A latent variable analysis, Cognitive Psychology, 41 , 49-100.
- Impulse Control
- socially acceptable (Olson, 2010)
- Ability to store, update and manipulate /process information over short periods of time (Best & Miller, 2010)
- “Limited-capacity information-processing system” (Roman et al., 2015)
- Verbal, visuospatial, and coordinating central executive
- Ability to think flexibly and shift perspective and approaches easily, critical to learning new ideas (different perspectives)
- Switching between two or more mental sets with each set containing several tasks rules
- Feedback related (unlike inhibition) (Best & Miller, 2010)
All these things are important, but the three basic dimensions are inhibitory control, which develops first around four years of age, cognitive and mental flexibility, and working memory. Mental flexibility is the result of inhibitory control and working memory working together. If you have a problem with inhibition or working memory, or both, you are going to have problems with cognitive flexibility. The flip side of that would be rigidity. It is also being able to shift your thinking in the moment back and forth. The flip side of that would be to be stuck. Working memory is the ability to use your memory functionally. It is very important to know that we only have a very limited amount of memory capacity, and it is all we have. I like to call my working memory my suitcase. You have to make sure you pack the right things in there for the trip that you are going on. If you pack your suitcase for Fiji and you are going to Alaska, you are going to be on the beach with boots and a parka and be miserable. It is really important that we pull in the information that we need. This takes sustained attention. If you cannot sustain your attention, you are not going to capture the right memories. And again, if there are problems with inhibitory control or impulse control, this is going to be challenging. Impulse control is controlling yourself in the moment. If I can string those together, now I have more self-regulation ability. Again, these are the big three: inhibition, working memory, and cognitive flexibility and shifting.
I already explained these, but I want you to appreciate what the research says. Inhibition requires an arbitrary rule to be held in your mind while you are inhibiting one response to produce an alternative response, which is typically the one that is more socially acceptable. Working memory is storing, updating, and manipulating information over short periods of time. It has a limited capacity, and it is verbal and visuospatial. Then, for cognitive shifting and flexibility, there are two pieces to it. It is being open and being able to shift. Here is what is interesting. Cognitive flexibility and shifting respond really well to internal feedback. You can actually start to observe things and gain some insight and make changes. Why that is important is because inhibition does not get better from internal feedback. It only gets better from external feedback. Think about someone you know who interrupts a lot because they are impulsive. They see that they do it and do not change because no one has said anything to them. It requires external feedback for them to say, "Oh, I'm doing it wrong." We do not have this internal mechanism to change our impulsivity. We cannot assume these kids will figure it out and fix it, because they will not. We have to be very stern and to the point and say, "You're doing it wrong. This is why it's wrong and here's what you need to do instead." This is the key. Figure 4 is an executive function cheat sheet.
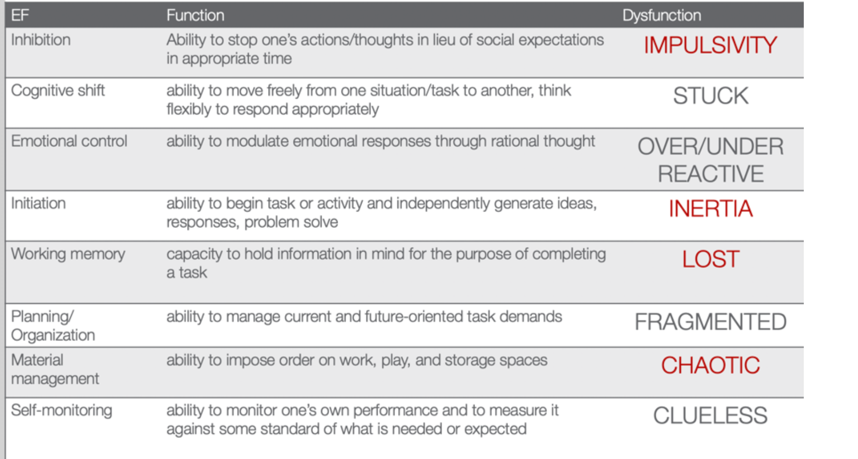
(Cooper-Kahn & Dietzel, 2008)
Figure 4. EF cheat sheet.
This is from Cooper-Kahn and Dietzel (2008). They tell you the executive function, what the function is, and then the end dysfunction. For inhibition, the dysfunction is impulsive. If you cannot cognitively shift, you can get stuck. If you do not have emotional control, you are going to be over or under-reactive. If you cannot initiate a task, you are stuck in inertia. If you do not have a good working memory, you are lost. If you cannot plan and organize, you are fragmented. If you cannot manage your materials, you are chaotic. And then, if you cannot self-monitor, you are clueless. The red ones are those that Jeremy struggled with. He was impulsive, had inertia, was lost, and chaotic. He was also a little fragmented and had a difficult time with organization. However, these four things were his biggest challenges.
Review of Evidence-based Interventions for Case
One of the objectives is to talk about evidence and how we are going to use the evidence to support our intervention. I focused on motor, social, executive functions, and sleep. These are the things that were assessed that also had evidence for different intervention strategies (see Figure 5).
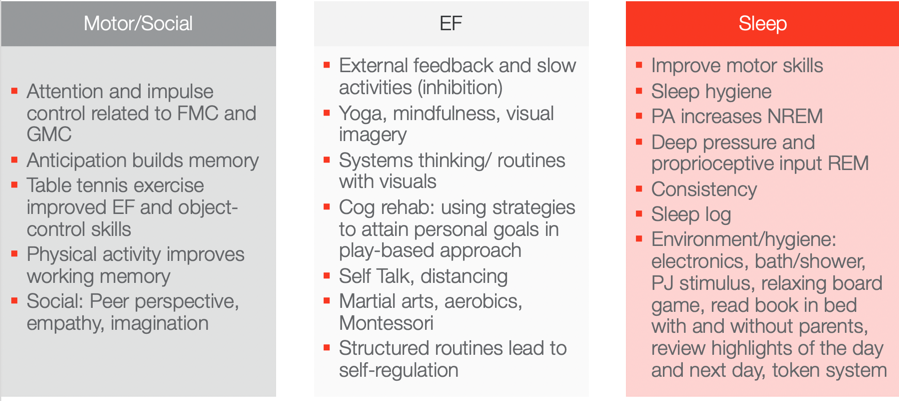
Figure 5. Evidence-based interventions ((Hui Tseng, et al., 2004; Hahn-Markowitz et al., 2016; Washington University, n.d.; Diamond & Lee, 2011; White & Carlson, 2016; Winsler et al., 2009; Marjorek et al., 2004; Kuhn & Floress, 2008; Frike et al, 2006; Keshavarzi et al., 2014).
Motor/Social Categories
Let's look at the motor and social categories. What is really interesting is that attention and impulse control are related to fine motor and gross motor coordination. If we can work on coordination, we can also increase attention and impulse control. This is killing two birds with one stone in Jeremy's case. I do not know who is familiar with Hebbian's law, but it says is that the (brain) cells that fire together wire together. One of the ways to do that is through the concept of anticipation. Anticipation builds memory capacity and will improve working memory. Anticipation is a context, and you can basically put anticipation in anything. With turn-taking, there is anticipation. If there is a competition, there is anticipation among the competitors. If you know you are going to be called on, there is anticipation. If you are playing a game where something might jump out, there is anticipation. These are just a few examples of where you can build in anticipation. If you can add that into your activities, you can build memory capacity. Another study looked at how table tennis exercises improved executive function and object control skills. Table tennis does not require a lot of heavy-duty cardio and it is not a tiring exercise, but it requires a lot of hand-eye coordination and sustained attention. I think this is a really good occupation-based strategy to improve executive function and object control. Physical activity also improves working memory. I have had tons of success with kids doing physical activity both in therapy and at home to improve their working memory. Some of the social strategies that work really for kids, and we will talk about a few in a little bit, is taking a peer's perspective and working on empathy and imagination. These things were really shown to be effective ways to change someone's social success.
Executive Function
For executive function, you have to give them external feedback. You have to tell them when they are being impulsive, and then you have to tell them how to fix it. These are kids who are on a very fast, impulsive temporal context. I talk to them about the hare versus the turtle. I tell them to be more like the turtle. Yoga, mindfulness, and visual imagery are other strategies. Yoga and mindfulness are occupations, and you can incorporate visual imagery into any occupation. They are so effective especially living in a very stressful, fast-paced society. There is self-distancing involved which we know also helps with the social skills for these kids. Systems thinking and routines with visuals are other options. The more visuals we use, the better for these kids. If we can give them visual imagery, it helps. Here is an example of systems thinking. You have family coming over for Thanksgiving dinner. There are 17 people coming and three courses. Each dish takes this long and I need these ingredients for each. Additionally, these dishes all cook at different times so they come out at the right time. This is systems thinking. As a strategy, I gather my recipes and my materials and then put them in order for which ones I have to cook first and for how long. I form a little assembly line of what I am going to do. We can use this type of strategy for kids who struggle with material management and organization. It can be a game-changer. Other ideas include self-talk, martial arts, aerobics, and Montessori. I do not know if anyone has any experience with a Montessori approach. One of the reasons why it is effective is because Montessori uses self-distancing activities. Telling the kids what you want them to do instead of what you do not want them to do really works. It also includes structured routines that lead to self-regulation.
The last section shows that motor skills, as well as sleep hygiene, can improve sleep. Physical activity actually increases non-REM sleep. Deep pressure and proprioceptive can increase REM sleep. A sleep log is actually evidence-based as well. Shortly, I am going to describe a routine that works with kids that is evidence-based. All of these things here you can use as your evidence-based toolkit to work with kids with ADHD.
Case Study Application- Improve ADLs
Top-down analysis.
Jeremy's goal is to have a timely morning routine which involves waking up, dressing, brushing teeth, and packing a backpack. This is a top-down analysis in Figure 6.
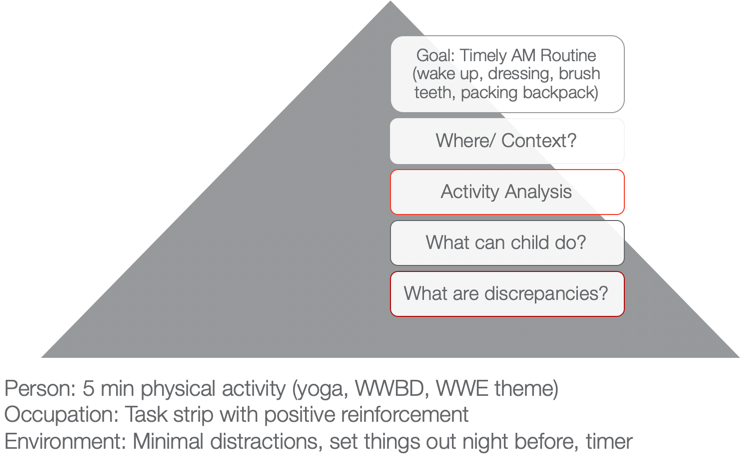
Figure 6. Example of a top-down analysis for ADL routine.
When we use a top-down approach, we are starting with the actual occupation and the goal is to look at where this happens and in what context. I want you to think about where that would happen. In Jeremy's case, it is his bedroom and bathroom. Activity analysis is the bread and butter of OTs. His routine consists of waking up, dressing, brushing his teeth, and packing a backpack. During this analysis, we want to see what he can do and what he cannot do. What are some of your thoughts? Here are some answers from our audience:
- Being aware of time during all tasks/Using a timer. You are seeing a discrepancy between time awareness, time estimation, time monitoring, and time management. I would agree with you that he probably has a hard time all of those.
- Packing the backpack. We know that he is sleepy in the morning and he has a difficult time staying organized. This is especially true if he is half asleep or stressed in the morning.
- Finding his folders. Folders can be elusive sometimes to these kids, so that is a great point. Folders can be found in very strange places.
- Hygiene/organization. Even in hygiene, it is important to make sure that they are organized.
I used a PEO or person-occupation-environment perspective here. We started with some physical activity in the morning to help him to wake up. We did yoga. I asked, "What would Batman do?" He was a big Batman guy. We did some self-distancing by him coming up with strategies for Batman. Or, we used a wresting theme. These activities helped him to be more alert and be able to increase his attention.
We also used a task strip with positive reinforcement to help him see what he needed to do. Visuals can be very helpful for these kids.
Then, we used minimal distractions. We set things out the night before and used that visual so he could match things. We also devised a place where his folders could go. This all might seem trivial, but it really matters for this type of kid. The timer helps as well. You can make it a game.
Activities to Improve ADLs
- Focus on physical activity, motor skills with automaticity and incorporate aspects of yoga to increase sustained attention and memory
- Visual supports and routine with structure
- Self-talk and self-distancing strategies
- Positively reward
To improve ADLs, the key is to focus on physical activity and motor skills with the goal of automaticity. For example, we can incorporate yoga to increase sustained attention and memory. As we talked about earlier, visual supports and structured routines are other great ideas. I cannot emphasize enough the idea of self-talk. This helps with self-regulation and impulsivity on a lower level. The ability to "self-talk" should be pretty solid for kids around the age of seven, but the kids that we are talking about lack this skill. Self-distancing, or having them give strategies to someone other than themselves, is also great. Let them problem-solve and talk it through for someone else, like Batman or John Cena. This way they do not feel like they are picking on themselves or feeling pressured to figure it out for themselves. They are figuring out for someone else, and this strategy is evidence-based. We often forget to positively reward these kids. I like to do something like time with mom and dad, I develop short-term and long-term rewards with mom and dad. For example, Jeremy wanted a wrestling figure for his long term reward. But on a daily basis, he got wrestling bucks and that bought time to wrestle with dad on the weekends.
Case Study Application- Finish a Task with Necessary Supplies
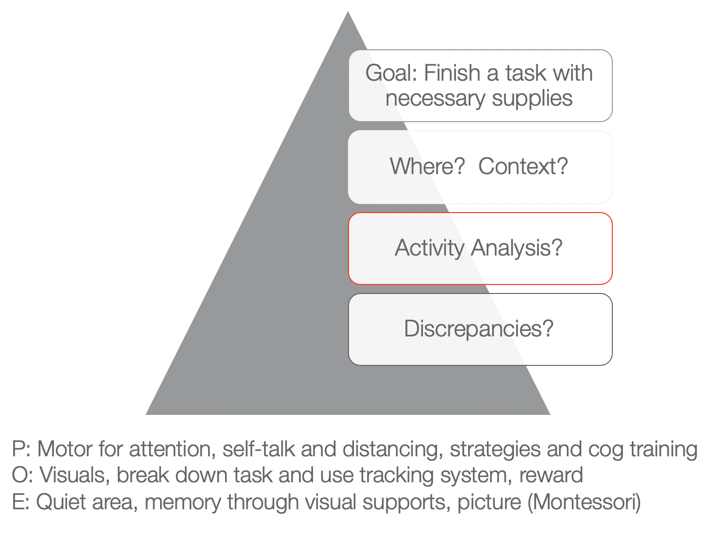
Figure 7. Example of a top-down analysis for finishing a task with necessary supplies.
The next goal is to finish a task with the necessary supplies. You can fill in whatever task that he needed to do like homework, hygiene, or whatever it was with the necessary supplies. Typically, he would start something and then not have all the supplies he needed. He would then run to go get something and then lose track of what he was doing. Activities would not get done and then there would be a mess. We want to know when this would happen and the context. What is required of that activity, and then what can he do versus what he cannot do? Those are the discrepancies.
As I stated a few moments ago, he tends to not have the needed materials. That is the first issue right out of the gate. And because he is impulsive, he starts doing something else. Eventually, he does not finish anything due to a lack of persistence and distractibility. From a personal standpoint, we could work on using motor tasks for increased attention. We know that fine motor and gross motor tasks are going to help. We could also look at using coordination tasks, self-talk, and distancing. Cognitive training is also evidence-based. Can they start to use a checklist or something to create a better strategy?
Then, from an occupation standpoint, again we can use visuals and break down the task. We can also use a tracking system that we are going to go over in just a second.
From an environmental aspect, we can encourage the use of quiet areas to help with sustained attention and better memory. Here we can also use some visual supports or a Montessori approach. "This is what the task is supposed to look like when I am finished." If we have a task, what does the end result look like so that the person knows? And even better, what are the supplies pictured so I know what I have to get first, and then I know what the end result should look like. That is super helpful for someone who is so disorganized when putting materials together.
Activities for Completing Tasks
- Inhibition: Self-talk, slowing down, self-distancing, external feedback
- WM: physical activity
- Attention: physical activity
- Using environmental strategies and visuals to support
- Behavioral: task breakdown, positive reinforcers
- Occupation-based is imperative!
We want to use occupation-based tasks, but we want them to be fun and let the child make a choice. When things are getting easier, we can then move toward less preferred tasks. For example, we do not want to start with homework.
Case Study Application: Social
- Involve a peer or sibling
- Play-based model:
- Capture intrinsic motivations (WWE)
- Empathy focus
- Arrange the environment to foster mutually enjoyable social interaction and imagination
- Teaching social play language and reading expressive body language (can use dogs and their behavior)
- Incorporate parents and coach them so they can coach outside of therapy
(Cordier et al., 2009; Wilkes-Gillan et al., 2016)
There is a play-based model that is evidence-based. They recommend involving a peer or sibling. This play-based model focuses on intrinsic motivation. With Jeremy, we could do wrestling. We could focus on empathy. It is important to arrange the environment so that it is mutually enjoyable. We need to teach social play language and reading expressive body language. The evidence was interesting as it said to use dogs because it could help the child start to read behaviors. Dogs are a little bit easier than people. Jeremy loves dogs so that would work. You could then incorporate parents in order to coach him outside of therapy. They found that to be very successful.
Case Study Application: Sleep
- Turn off electronics 2 hours prior
- Hot bath or shower
- PJs prepped
- Boardgame in room
- Read in bed (parents, then alone
- Highlights with organizer, feelings
- Token reward system
- Flexibility on weekends
- Sleep logs are evidence-based
- Physical activity during day imperative
(Kuhn & Floress, 2008; Fricke et al., 2006)
For sleep, this is the protocol that is highly recommended for these kids. You should turn electronics off two hours prior. Do not shoot the messenger. I know that is really easier said than done. Another protocol is to have the child take a hot bath or shower. They need to have their pajamas prepared. It is a stimulus that can help them progress through the routine. They can do a board game in the room. Another activity is reading in bed. It can start out with the parents reading and then progress to the child reading alone. They can also organize their thoughts and feelings throughout the day. It will help the brain calm down. A token reward system is another great strategy. Make sure to incorporate flexibility on the weekends. It is ok. Sleep logs are evidence-based. And again, physical activity during the day really works.
Systems and Organization
This information is what we already talked about, but I wanted to give you a good resource as well in Figure 8.
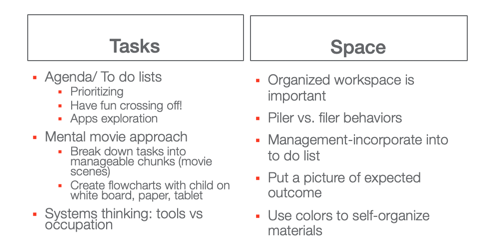
Great resource: https://www.understood.org/~/media/040bfb1894284d019bf78ac01a5f1513.pdf
Figure 8. Systems and organization examples.
I like the idea of a mental movie approach. If they are piler and not a filer, we have to appreciate that and try to use things that can help them. This may be an accordion folder or something like that.
Self-Monitoring: GOAL Attainment Scaling
This is the idea of a Goal Attainment Scale (see Figure 9). It is a strategy to identify changes in academic and social behavior. It creates habits and routines.
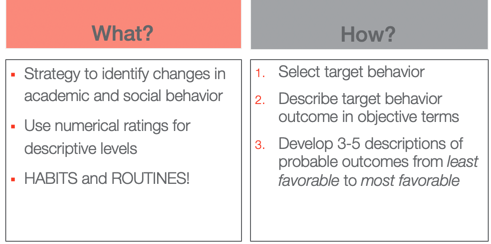
Figure 9. Goal Attainment Scale overview.
The way that you do it is you select the target behavior. You describe that behavior outcome in objective terms and then you develop three to five (I typically use five) descriptions of probable outcomes from least favorable to most favorable.
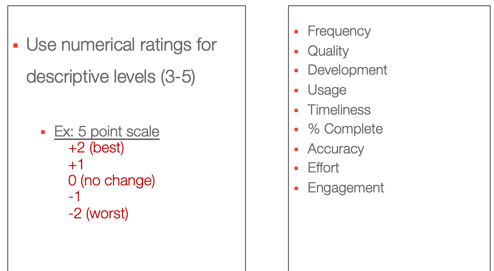
Figure 10. Numerical ratings for the Goal Attainment Scale.
These are some options that you can use, frequency, quality, usage, percent complete.
- Frequency (Never–Sometimes–Very Often–Almost Always–Always)·
- Quality (Poor–Fair–Good–Excellent)·
- Development (Not Present–Emerging–Developing–Accomplished–Exceeding)·
- Usage (Unused–Inappropriate Use–Appropriate Use–Exceptional Use)·
- Timeliness (Late–On-Time–Early)·
- Percent complete (0%–25%–50%–75%–100%)·
- Accuracy (Totally Incorrect–Partially Correct–Totally Correct)·
- Effort (Not Attempted–Minimal Effort–Acceptable Effort–Outstanding Effort)·
- Amount of Support Needed (Totally Dependent–-Extensive Assistance–Some Assistance–Limited Assistance–Independent)·
- Engagement (None–Limited–Acceptable–Exceptional)
This is what the five looks like. You have two choices. You can do a baseline here at zero or the baseline at minus two where that is the worst with no change. Or, you can start at their baseline here at two and only go up. If they cannot handle seeing that they went down, you might choose that option instead. We do not want any negative things causing them anxiety. I have also listed the actual ratings. Here is the example for our friend Jeremy in Figure 11.
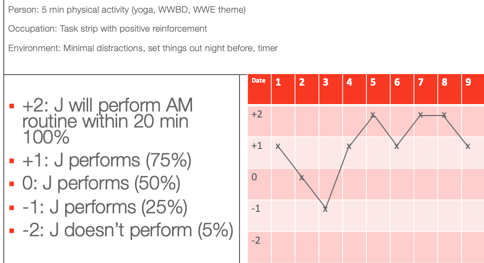
Figure 11. GAS scale example for Jeremy.
He wanted to perform his AM routine within 20 minutes according to his mom. On the first date, he was a +1, which is he did only 75% within 20 minutes. On Day 2, he had 50% of his stuff done within 20 minutes. Day three, he had only 25% done. On four, he was back up to 75%. Day five, he did everything in 20 minutes. Day six, he was back to 75%. And then you see on days seven and eight, he actually met his goal. And on day nine, he almost met his goal. Once you plot the dates you have a graph. This shows change over time and whether or not things are working. You can also do this at home to capture the change in a more specific and sensitive way. On that note, we focused on time.
Thanks for joining me today. I hope you find the information helpful. Feel free to reach out to me if you have any questions.
Best, J. R., & Miller, P. H. (2010). A developmental perspective on executive function. Child Development, 81 (6), 1641-1660.
Cremone-Caira, A., Root, H., Harvey, E. A., McDermott, J. M., & Spencer, R. M. (2019). Effects of sleep extension on inhibitory control in children with ADHD: A pilot study. Journal of Attention Disorders , 1087054719851575.
Corkum, P., Tannock, R., & Moldofsky, H. (1998). Sleep disturbances in children with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 37 , 637-646.
Cordier, R., Bundy, A., Hocking, C., & Einfeld, S. (2010). Empathy in the play of children with attention deficit hyperactivity disorder. OTJR: Occupation, Participation, and Health, 30 (3), 122-132.
Diamond, A. (2012). Activities and programs that improve children’s executive functions. Current Directions in Psychological Science, 21 (5), 335-341.
Levanon-Erez, N., Cohen, M., Traub Bar-Ilan, R., & Maeir, A. (2017). Occupational identity of adolescents with ADHD: A mixed methods study. Scandinavian journal of occupational therapy, 24 (1), 32-40.
Hahn-Markowitz, J., Berger, I., Manor, I., & Maeir, A. (2016). Efficacy of cognitive-functional (Cog-Fun) occupational therapy intervention among children with ADHD: An RCT. Journal of Attention Disorders , 1087054716666955.
Faber Taylor, A., & Kuo, F. E. (2011). Could exposure to everyday green spaces help treat ADHD? Evidence from children's play settings. Applied Psychology: Health and Well‐Being, 3 (3), 281-303.
Fricke L, Mitschke A, Wiater A, Lehmkuhl G. 2006. A new treatment program for children with sleep disorders – concept, practicability, and first empirical results. Prax Kinderpsychol Kinderpsychiatr 55 :141–154.
Keshavarzi, Z., Bajoghli, H., Mohamadi, M. R., Salmanian, M., Kirov, R., Gerber, M., ... & Brand, S. (2014). In a randomized case–control trial with 10-years olds suffering from attention deficit/hyperactivity disorder (ADHD) sleep and psychological functioning improved during a 12-week sleep-training program. The World Journal of Biological Psychiatry, 15 (8), 609-619.
Kuhn BR, Floress MT. (2008). Nonpharmacological interventions for sleep disorders in children. In Ivanenko A, ed. Sleep and psychiatric disorders in children and adolescents . New York, NY: Informa Healthcare USA Inc. pp 261–278.
Majored, M., Tüchelmann, T., & Heusser, P. (2004). Therapeutic Eurythmy—movement therapy for children with attention deficit hyperactivity disorder (ADHD): a pilot study. Complementary therapies in Nursing and Midwifery, 10 (1), 46-53.
Pan, C. Y., Tsai, C. L., Chu, C. H., Sung, M. C., Huang, C. Y., & Ma, W. Y. (2019). Effects of physical exercise intervention on motor skills and executive functions in children with ADHD: A pilot study. Journal of Attention Disorders, 23 (4), 384-397.
Papadopoulos, N., Stavropoulos, V., McGinley, J., Bellgrove, M., Tonge, B., Murphy, A., ... & Rinehart, N. (2019). Moderating effect of motor proficiency on the relationship between ADHD symptoms and sleep problems in children with attention deficit hyperactivity disorder–combined type. Behavioral Sleep Medicine, 17 (5), 646-656.
Tandon, P. S., Sasser, T., Gonzalez, E. S., Whitlock, K. B., Christakis, D. A., & Stein, M. A. (2019). Physical activity, screen time, and sleep in children with ADHD. Journal of Physical Activity and Health, 16 (6), 416-422.
Toplak, M. E., West, R. F., & Stanovich, K. E. (2017). The assessment of executive functions in attention-deficit/hyperactivity disorder: Performance-based measures versus ratings of behavior.
Tseng, M. H., Henderson, A., Chow, S. M., & Yao, G. (2004). Relationship between motor proficiency, attention, impulse, and activity in children with ADHD. Developmental Medicine and Child Neurology, 46 (6), 381-388.
Wilkes-Gillan, S., Bundy, A., Cordier, R., Lincoln, M., & Chen, Y. W. (2016). A randomised controlled trial of a play-based intervention to improve the social play skills of children with attention deficit hyperactivity disorder (ADHD). PLOS one, 11 (8), e0160558
Yürümez, E., & Kılıç, B. G. (2016). Relationship between sleep problems and quality of life in children with ADHD. Journal of Attention Disorders, 20 (1), 34-40.
Quint, N. (2020). Pediatric case study: Child with ADHD. OccupationalTherapy.com, Article 5145 . Retrieved from http://OccupationalTherapy.com

Nicole Quint has been an occupational therapist for over 15 years, currently serving as an Associate Professor in the Occupational Therapy Department at Nova Southeastern University, teaching in both the Masters and Doctoral programs. She provides outpatient pediatric OT services, specializing in children and adolescents with Sensory Processing Disorder and concomitant disorders. She also provides consultation services for schools, professional development, and special education services. She provides continuing education on topics related to SPD, pediatric considerations on the occupation of sleep, occupational therapy and vision, reflective therapist, executive functions, leadership in occupational therapy and social emotional learning.
Related Courses
Evidence-based approaches: a pediatric perspective of the occupation of sleep, course: #6204 level: intermediate 2 hours, pediatric case study: child with oculomotor and perceptual challenges, course: #4536 level: intermediate 1 hour, from meltdowns to an occupation-centered approach for self-regulation and management, course: #6106 level: intermediate 2 hours, course: #4577 level: intermediate 1 hour, motor skill acquisition for optimal occupational performance, course: #3747 level: introductory 1 hour.
Our site uses cookies to improve your experience. By using our site, you agree to our Privacy Policy .

ADHD brains present unique challenges, but the condition is highly treatable − a primary care nurse practitioner with ADHD explains the science
Lecturer of Clinical Pathophysiology and Family Nurse Practitioner, Kennesaw State University
Disclosure statement
Kate Harrington does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
Kennesaw State University provides funding as a member of The Conversation US.
View all partners
“My brain has way too many tabs open.”
“Why can’t I complete tasks?”
“Why do I lose track of time?”
“Why can’t I pay attention?”
These are all things people with attention-deficit/hyperactivity disorder, or ADHD, may ask themselves daily, if not hourly.
As a family nurse practitioner in primary care , I have diagnosed and treated numerous patients with ADHD. I was also diagnosed with it at the age of 21.
Understanding how the wiring differs in a brain with ADHD and what improves functioning is critical to help those struggling because of their brain’s uniqueness.
How brains with ADHD differ
Research has identified multiple differences in how brains with ADHD work .
Put simply, ADHD significantly affects executive function.
Executive functioning is a set of cognitive processes, including planning, prioritizing, impulse control, flexibility, time management and emotional regulation, that help people achieve long-term goals.
These processes occur in the prefrontal cortex – the “personality center” – of the brain.
In addition to the prefrontal cortex, ADHD affects other areas of the brain, including the basal ganglia , an area that regulates communication within the brain, and the cerebellum , which is responsible for movement and balance. All three work together regulating attention, executive function motor activity and impulse control .
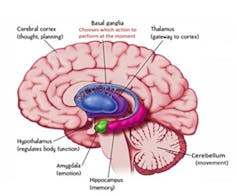
Chemical messengers called neurotransmitters allow brain cells to communicate with each other. Dopamine and norepinephrine are two key neurotransmitters that play critical roles in the executive functioning of the brain .
Dopamine controls motivation, rewards and pleasure . We get a flood of dopamine from pleasurable things such as eating, drinking alcohol, having sex, and receiving affirmations or good grades. That flood also motivates us to repeat the “rewarding” behavior. Norepinephrine is responsible for sustaining attention and helps with executive functioning .
People with ADHD have lower levels of dopamine and norepinephrine in brain regions, including the prefrontal cortex. This leads to difficulty in sustaining cognitive functions such as attention, impulse control and motivation .
Studies show that people with ADHD have more dopamine transporters in the brain . Think of transporters as vacuums that suck dopamine back up into the neuron, making it less available.
As a result, there is less activation by dopamine and norepinephrine in the prefrontal cortex and the mesolimbic pathway , the area that processes rewards and motivation. Less dopamine can drive people to seek out stimulating rewards such as technology, food or drugs.
Researchers have identified at least 27 possible genetic markers that modulate dopamine regulation in the brain .
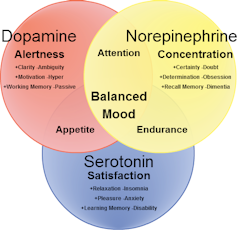
Diagnosing ADHD
Nearly everyone with or without ADHD show some symptoms such as forgetfulness. For instance, when you can’t tolerate sitting in a meeting for one moment longer or you can’t remember why you came into a room.
A true ADHD diagnosis takes into account multiple factors .
If you struggle with ADHD, you have at least five to six symptoms in the inattentive, hyperactive or impulsive categories, such as forgetfulness, trouble sitting still, losing items and getting easily distracted.
For a formal diagnosis, ADHD symptoms need to have been present before the age of 12, something that can be determined in childhood or, as in my case, much later.
Also, ADHD symptoms must negatively affect the person in multiple settings , such as at home, in school or at work – and they can’t be explained away by other conditions, such as thyroid dysfunction, diabetes, sleep deprivation or anemia .
Research shows that girls with ADHD more often display inattentive symptoms along with characteristics not traditionally associated with ADHD, such as shyness, perfectionism and eating disorders . Patients, particularly women and girls , can develop depression or anxiety – or both – because of untreated ADHD. Once ADHD is treated, anxiety and depression symptoms are greatly reduced .
How ADHD medications alter neurotransmitters
The American Academy of Pediatrics provides evidence-based guidelines for the treatment of ADHD in children and teens.
The first U.S. guidelines for the treatment of adult ADHD are expected to be released in fall 2024 .
If patients are 6 or older, stimulant or nonstimulant medications may be used, along with behavioral therapy.
Stimulants are divided into two drug classes: amphetamines, such as Adderall and Vyvanse, and methylphenidates, such as Concerta, Ritalin and Focalin.
Nonstimulants such as Strattera are recommended if patients cannot tolerate or prefer not to take stimulant medications.
Stimulants block the dopamine and norepinephrine transporters , preventing them from depleting those neurotransmitters, so more dopamine is available to activate key areas of the brain.
Amphetamines also increase the release of dopamine and norepinephrine from neurons . These increased levels allow the brain to find challenging tasks, such as doing homework, more rewarding. Because more dopamine is available, the brain’s desire for stimulating rewards decreases.
Methylphenidates are typically the drug of choice for children , while amphetamines are most effective in adults.
Numerous studies have found that stimulants improve ADHD symptoms , patient motivation , parental quality of life and behavioral ratings from teachers. Stimulants decrease anxiety and emotional dysregulation in children . Nonstimulants also improve ADHD symptoms .
Improved outcomes
People with ADHD attempt suicide at twice the rate of people without ADHD . They also have three times the rate of suicidal ideation and six times the rate of completed suicide .
Treating patients with ADHD with stimulant medication, in addition to behavioral therapy, has been shown to decrease suicide attempts , unplanned pregnancies and substance use . One study found that treating children with ADHD with methylphenidate reduced their risk of burn injuries by 57% .
In addition to medication, cognitive behavioral therapy for adults , executive function training , particularly in adolescents , and positive parenting interventions have been shown to be effective for ADHD symptoms. Most researchers agree that behavioral training is most effective when combined with medication .
Positive parenting
Research has found significant improvement in the quality of life for both parents and children when parents participated in positive parenting education . The effect is even more pronounced when combined with medication .
One such model, called the “Nurtured Heart Approach ,” has been used by families , schools , foster care organizations and behavioral health groups , including the New Jersey Children’s System of Care . It emphasizes praise and encouragement, the setting of clear boundaries for acceptable behavior, and teaches children to self-regulate emotions and behaviors.
As a medical provider, I have witnessed such models work wonders in families and classrooms.
Dietary supplements
Multiple studies have demonstrated that children with ADHD have lower levels of vitamin D in their bloodstream.
Having adequate iron in one’s body, stored in the protein ferritin , is important to create dopamine and norepinephrine , the neurotransmitters that are lacking in ADHD. Research has demonstrated that low levels of ferritin cause a disruption in dopamine activity . Children with lower levels are more likely to be diagnosed with ADHD .
For this reason, it’s important for providers to check ferritin levels and not serum iron, which is often used incorrectly to diagnose iron deficiency .
Taking steps forward
If you think your child or you may have ADHD, speak with a health care provider who is familiar with ADHD treatment. For school accommodations, the first place to start is with your provider.
Research is still ongoing, but high intake of processed foods may worsen ADHD symptoms .
Pay attention to sleep; sleep apnea and sleep disordered breathing are common in people with ADHD.
And make sure to get in lots of exercise, because it can improve executive functioning and impulse control while boosting dopamine and norepinephrine levels.
Though overwhelming, I’m happy to say that living with ADHD can be rewarding.
ADHD comes with multiple benefits : We are resilient, unconventional and creative. We have intense energy that, once harnessed, can be used for incredible good.
- Neurotransmitters
- Attention-deficit/hyperactivity disorder (ADHD)
- Prefrontal cortex
- Executive function
- Mesolimbic system
- Impulsivity

Head of School: Engineering, Computer and Mathematical Sciences

Research Fellow in Astrobotany

Educational Designer

Organizational Behaviour – Assistant / Associate Professor (Tenure-Track)

Apply for State Library of Queensland's next round of research opportunities
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Childhood ADHD and Early-Onset Bipolar Disorder Comorbidity: A Case Report
Introduction: Recent research has highlighted an increased rate of co-morbidity between the neurodevelopmental-behavioral disorder of attention deficit hyperactivity disorder (ADHD) and a variety of psychiatric disorders, such as mood disorders or bipolar disorder (BD). The etiology and clinical course of BD are considered to be determined by both genetic and environmental factors, either aggravating or improving. Aim: This follow-up study of an adolescent aimed to clarify the co-morbidity between ADHD and BD. We also discuss the controversies surrounding the two diagnoses in younger populations and describe several aspects of concern regarding diagnosis, differential diagnosis, therapeutic planning/intervention, and prognosis. Methods: Reporting of a two-year follow-up study of a bipolar 15-year-old female patient with a previous diagnosis of ADHD during childhood. Results: Despite the occurrence of major risk factors, such as early onset and positive family history, the patient’s condition rapidly remitted with medication, without relapse and/or rehospitalization during the following two years, due to the stability of her cooperation, and support of a stable and caring familial environment. Early diagnosis of BD and differential diagnoses of ADHD are considered crucial protective factors leading to an appropriate planning of treatment. In addition, parental involvement and empathic attitude towards the patient supported the latter to cooperate and comply with the treatment, enhancing positive outcomes and stability. Conclusions: Research is required into the reliability and validity of diagnostic protocols and criteria for BD in children and adolescents, and also into the development of individualized therapeutic planning.
1. Introduction
Attention deficit hyperactivity disorder (ADHD) is defined in the Diagnostic and Statistical Manual of Mental Disease 5th Edition (DSM-V) as a neurodevelopmental-behavioral disorder, mainly diagnosed in early development and characterized by some stereotypes of behavior presented in several places, such as home and school [ 1 ]. ADHD is the most prevalent neurobehavioral disorder diagnosed in youth, affecting 5–7% of school-aged children globally [ 2 , 3 , 4 , 5 , 6 ]. Recent research has highlighted an increased rate of co-morbidity between ADHD and a variety of psychiatric disorders, such as mood, anxiety, and conduct disorders. Consequently, ADHD is most likely a group of conditions, rather than a single homogeneous clinical entity, characterized by different etiologic and modifying risk factors and different outcomes [ 7 ]. There has been considerable debate about whether this overlap occurred by chance or as an artifact of referral bias, whether the comorbid conditions are secondary to the ADHD, and whether other psychiatric disorders masquerade as attentional problems. Alternatively, each of the ADHD subtypes may occur with its specific comorbidity [ 8 ]. Although a subset of ADHD children also meets the criteria for bipolar disorder (BD), the exact prevalence of this diagnosis in ADHD children is strongly debated. Regardless of its prevalence, this disorder affects a severely impaired group of ADHD children, with high rates of aggression and psychiatric disorders in their families [ 8 ].
There is a growing awareness that the onset of bipolar disorder (BD) often appears during childhood or adolescence, although the typical picture of the symptoms of adolescent mood dysregulation is in many ways dissimilar to the symptomatology of adults [ 9 ].BD is one of the most highly heritable psychiatric illnesses, second only to autism [ 9 ], with lifetime prevalence about 3% globally [ 10 , 11 , 12 , 13 ]. The etiology and clinical course of BD are considered to be determined by genetic and environmental factors [ 13 ]. Current models of etiology consider BD as a primarily genetic illness whose onset and course are influenced by environmental stressors, suggesting that environmental factors may either trigger or prevent the development of a psychiatric disorder [ 13 ]. The available evidence suggests that viral infections during pregnancy and adulthood, maternal smoking, climatic factors, childhood trauma, life events, and low social support might influence the onset and clinical course of BD [ 13 ]. It is worth noting that emotional abuse has the highest prevalence among adverse childhood experiences and that the impact of life events, trauma, and social support on an individual varies across countries and cultures [ 13 ]. Despite ongoing research, there is little conclusive information about the impact of psychosocial stressors on the evolution of early-onset bipolar disorder [ 13 ]. Family studies have shown a high relative risk to first-degree relatives of an individual with BD [ 9 , 14 ]. Twin studies further demonstrate the disorder’s heritability [ 9 , 15 ]. Pediatric BD is associated with various neuropsychological deficits. Attempts have been made to clarify the nature of these deficits, and to determine whether deficits are specific to mood states or whether they remain after symptomatic recovery [ 9 ]. Central findings from several small studies suggest that pediatric BD involves impairment in attention [ 9 , 16 , 17 ], set shifting [ 16 , 18 ], visuospatial memory [ 9 , 16 , 19 ], processing speed and interference control [ 17 ], verbal memory [ 17 , 18 , 20 ], and abstract problem solving or executive function [ 9 , 17 , 21 , 22 , 23 ]. The Performance IQ scores achieved in the Wechsler Intelligence Scale for Children (WISC)by pediatric bipolar patients were reported to be similar to those seen in schizophrenia spectrum disorders, and lower than those in ADHD and unipolar depression [ 9 , 18 , 22 , 24 ].
The frequent occurrence of comorbidity between the two disorders complicates further diagnosis. It is not clear whether comorbidity is explained by overlapping symptoms at the superficial level of operationally defined clinical features or whether it reflects a true overlap in disease entities at the biological level [ 25 , 26 ]. Although co-morbidity is often not assessed correctly because different services may proceed to clinical access differently [ 26 , 27 , 28 ], the patterns of overlap with other disorders can be informative about how clinicians conceptualize disorders [ 26 , 27 , 28 ]. BD and ADHD co-occurrence has been extensively studied by numerous studies. Some researchers concluded that comorbid ADHD/BD is familiarly distinct from other forms of ADHD and may be related to what others have termed as childhood onset BD (characterized by irritability rather than euphoria, a chronic rather than episodic course, and a severe mood dysregulation leading to marked impairment) [ 9 , 29 ]. Retrospective studies in adults have led to similar conclusions, suggesting that ADHD symptoms represent a prodromal or early manifestation of pediatric-onset BD in certain at-risk individuals [ 9 , 30 ]. A prospective study of the rate, risk, and predictors of switching from ADHD to prepubertal and early adolescent bipolar I, showed a higher risk for individuals with ADHD (the cumulative risk of switching from ADHD to bipolar I through the 6-year follow-up was 28.5%, compared to a 2% switching rate for healthy controls) [ 9 , 31 ].
2. Materials and Methods
2.1. design.
We present a two-year follow-up of a bipolar 15-year-old female patient with a previous diagnosis of ADHD during childhood, discussing a number of aspects of concern that emerged during diagnosis and treatment of BD. The study attempts to describe the early-onset form of the BD and to discuss the controversies occurring between the two diagnoses, BD and ADHD, in younger populations.
2.2. Assent and Consent
Decision-making in the framework of child and adolescent psychiatry presents a variety of challenges for children, parents/guardians, and child and adolescent psychiatrists (CAPs) concerning the ethical practice related to standards of care and the obtainment of the patient’s consent. In our clinical and research case, decision-making relies on the concepts of assent and consent by the relatives (Principle IV of the AACAP Code of Ethics, 2014) [ 32 , 33 , 34 , 35 , 36 ]. Parents/guardians and CAPs did not exclude the girl from the decision-making. They recognized that, because of her developmental level, the child might not be capable of according a completely reasoned consent; however, she might be capable of having preferences and communicating them. The importance of her involvement in the decision-making process was also considered a serious factor, recognizing that the girl’s level of participation was lower than that required [ 32 , 33 , 34 , 35 , 36 ]. The patient was given an Informed Assent Form and the parents were given an Informed Consent Form. They both provided their written consent to the content of the documents, after an explanation of the procedure. The patient’s anonymity has been protected.
2.3. Assessment Approach
Acknowledging the difficulty of diagnosing early-onset BD, we followed a comprehensive assessment approach [ 22 , 32 , 33 ] including: (1) a timeline of the child’s development, from birth to the present, showing all prior mood episodes;(2) a semi-structured clinical interview, including co-morbid conditions;(3) a family history genogram to ascertain familial loading;(4) depression and mania rating scales to assess symptom severity and track treatment outcome via administration of the 17-item Hamilton Depression Rating Scale (HAMD-17) [ 37 ] and Young Mania Rating Scale (YMRS) [ 38 ]; (5) global rating scales using multiple informants (parents, teachers) [ 34 ]; and(6) use of mood logs [ 39 ].
3.1. Case Description
A15-year-old female patient with ADHD symptoms for the past six years presented worsening irritability in the last four months. Assessing the patient’s history, interesting data were revealed regarding genetic and environmental factors that might have been related to the development of the psychopathology.
The patient lives with her parents in a small provincial town and is a student in the secondary education. Both patient and parents reported that during her preschool age the family experienced extreme financial instability because both parents were unemployed for a long time, which “led them in despair” after the loss of the child’s paternal grandfather, who was the main supporter of the family. This financial insecurity led the family to change location several times before the girl reached the age of five years old. Parents described this period as very difficult, with tensions, frequent frictions between themselves, and outbursts of anger directed towards the child. The patient recalled traumatic events of her childhood, such as physical and emotional abuse by her parents. We highlight that the trauma history mentioned by the patient was not included in the parents’ reports, although such trauma is supposed to have the highest prevalence among adverse childhood experiences. Both parents, during the assessment, underestimated her descriptions of traumatic events, characterizing them as “rarely occurred” or “insignificant to mention”, emphasizing their absence of empathy.
The girl did not consult any child psychiatry service until the age of nine to ten years old, when she was “suspected” to suffer from attention deficit hyperactivity disorder (ADHD) and treated with methylphenidate, which was discontinued because of a lack of beneficial effects. The girl had no psychiatric history. She had not previously suffered from any physical illnesses, nor used drugs, alcohol, or medication. Her family history was positive via her maternal aunt, who had been diagnosed with recurrent BD since her adolescence.
The patient was admitted to our service after presenting symptoms such as grandiose beliefs, agitation, and distractibility for the previous two days. She did not require sleep, and spent nights thinking about excessive plans, such as becoming a model. The symptomatology rendered her totally unable to take care of her basic needs, such as hygiene and school attendance. There were no recent stressors. The mental status examination revealed a child that was unable to remain seated, was excessively active during the interview, and presented logorrhea, accelerated speech, and flight of thoughts. She expressed countless projects and grandiose beliefs. She was irritable, denying hallucinations and suicidal ideations.
The patient was diagnosed with acute manic episode with no identifiable organic etiology but with a possible biological vulnerability for emotional dysregulation, given the maternal aunt’s BD. ADHD was considered part of the differential diagnosis. However, the clinical presentation—particularly the mental status examination as previously described—clearly corresponded to the severity of a mood disorder. In addition, the manic episode also heightened the prior hypothesis of her biological vulnerability to emotional dysregulation.
The patient was referred to a child psychiatric clinic for treatment. Baseline metabolic tests were negative, including complete blood count, electrolytes, thyroid levels, and urine analysis. A physical evaluation by the pediatrician yielded no significant findings. Electroencephalogram and brain magnetic resonance imaging (MRI) were negative. After no improvement with quetiapine (twice daily dosing totaling 600 mg, p.o.) and sodium valproate (1200 mg daily in divided doses, p.o.) she was also treated with olanzapine (5 mg, p.o.). Medication and the strong presence of nurses and psychoeducators stabilized her condition in fewer than ten days. Hospitalization lasted one month to monitor her symptoms and level of functioning during her progressive return to school. The patient was discharged, with a follow-up by a CAP.
During subsequent weeks, her compliance with medication prevented relapse. This coincided with the stability that occurred in her family environment. Her parents were supportive and showed empathy regarding her fragile emotional state and her preference to internalize her feelings. No pharmacological change was made and, with the presence of the multidisciplinary team, her condition remitted in the following months.
3.2. Diagnosis
The patient as a bipolar family member, from a family with an earlier-onset proband (aunt), was more likely than others to have an early onset [ 9 , 27 ]. In this case, the early onset of BD represents a diagnostic complexity because the prodromal symptoms must be evaluated in the context of an ADHD. Acknowledging the difficulty of diagnosing early-onset BD, we followed a comprehensive assessment approach [ 22 , 40 , 41 ] as mentioned above. The Diagnostic and Statistical Manual of Mental Disorders (fifth edition; DSM-V) spells out the criteria for diagnosing a manic, hypomanic, and major depressive episode. Different combinations of these episodes are required to diagnose BD I versus BD II [ 1 ].
3.3. Symptoms
Semi-structured interviews were used to examine the disorder’s clinical presentation and to provide a particularly helpful description of how symptoms such as euphoria, grandiosity, and hypersexuality manifested differently in childhood and adolescence. For example, a common presentation of grandiosity in childhood is to instruct teachers about how the class should be taught. In adolescence the patient expressed grandiose delusions, such as the achievement of a prominent profession while failing at school. Initially, the main symptoms were increased irritability and core symptoms of ADHD (hyperactivity, distractibility, impulsivity, and restlessness) that persisted for six years. Symptoms that were revealed later included, during the first manic episode: intense energy; distractibility and pressured speech; affective and psychotic symptoms, such as abnormally elevated mood and mixed emotional and psychotic symptoms (ideas of persecution—“I’ve being chased by a black Mercedes”); increased irritability and grandiosity; increased activity; distractibility; impulsivity; and restlessness. Other symptoms revealed later included: risky behaviors, such as substance misuse (alcohol), staying out late, defiance, and aggressivity; decreased need for sleep; and risky sexual misbehavior (masturbating in public places, such as the school hall).
Although the patient expressed no suicidal thoughts, the CAP assessed these symptoms in detail, because other studies highlighted high rates of suicidal ideation among adolescents with BD, which may reveal increased suicidal risk in this particular group of patients and suggest the need for close monitoring [ 17 , 42 ]. During assessment, symptoms such as depression, guilt, self-blame, hopelessness, suicidal ideation, psychomotor retardation, and other depressive-type cognitions, were not reported. Through the developmental history investigation, speech, language, and coordination issues during preschool age were mentioned in agreement with the pre-existing ADHD diagnosis.
3.4. ADHD and BD Comorbidity
Increased rates of symptoms commonly described as part of these syndromes have been reported in children with both ADHD and BD [ 7 , 8 , 22 , 26 ]. Distinguishing BD from ADHD was needed, because symptoms such as hyperactivity and distractibility are criteria for both disorders. Differentiation of BD from ADHD is critical for clinicians because the management of the two is different and also very difficult because some of the symptoms common in mania, such as hyperactivity or distractibility, also occur frequently in ADHD [ 43 ].
3.5. Treatment
Treatment required a multimodal approach that combined pharmacotherapy and psychotherapy [ 22 , 41 ], and the patient and parents’ involvement in the design of the treatment framework was crucial. Medications and adjunctive psychoeducational psychotherapy have a demonstrated efficacy in treating BD, as follows:
3.5.1. Pharmacotherapy
The appropriate medication for the treatment of a BD should be based on patient’s specific factors, such as physical history, previous response (if applicable), and medications prescribed, in addition to family and patient’s preferences, because they affect the treatment’s compliance [ 44 , 45 , 46 , 47 ]. According to the parents’ reports, during the onset of symptoms—six years earlier—the treating physician proposed psychostimulants for ADHD to enhance cognitive capacity, attention, and concentration, although the parents preferred to follow only psychotherapy as a treatment. The combination of the poor cooperation and compliance of the child, with the fear of the parents about the impact and side effects of an early chronic administration of psychostimulants, resulted in the absence of any medication until the present examination.
Acute Manic Episode
When the first manic symptoms appeared, the patient was not yet treated with psychostimulants that could justify the episode as resulting from side effects. For acute manic symptoms mixed with psychosis, initial treatment was combined with a mood stabilizer and an atypical antipsychotic. The dose was increased as rapidly as possible to achieve the lowest therapeutic dose that would produce the desired clinical effect:
- Quetiapine (atypical antipsychotic: twice daily dosing totaling 600 mg, p.o.) appeared to be effective in combination with sodium valproate (mood stabilizer: 750–1500mg daily in divided doses, p.o.) [ 46 , 48 ].
- A good response was also observed in an open-label trial of olanzapine (atypical antipsychotic: p.o., 5 mg trials) administered orally when manic symptoms were exacerbated [ 46 , 49 ].
Relapse Prevention
During her follow-up, mood stabilizing medication halted the rapid shift from high to low moods and back again, and was particularly useful in preventing manic episodes. Antipsychotic medications also acted as mood stabilizers and synergistically decreased episodes that she was experiencing as “a break in reality—an inability to distinguish what’s real from what isn’t”. Olanzapine was used solely for acute treatment, the dosage was reduced and discontinued (tapering over 2 weeks or more) after full remission of symptoms within 3 months. Quetiapine and sodium valproate have been shown to be effective (or probably effective in relapse prevention) and are appropriately continued as long-term treatment is planned (quetiapine: twice daily dosing totaling 400–600 mg, p.o.; and sodium valproate: 750–1000 mg daily in divided doses, p.o.).
Continuous monitoring of body mass index, blood pressure, fasting glucose levels, lipids, serum drug levels, and hepatic and hematological indices took place during the treatment. Once the patient was stabilized on an appropriate dosage of medication, maintenance treatment continued with the goal of relapse prevention. Ongoing monitoring for symptom recurrence, including suicide risk, was important [ 46 , 50 ].
3.5.2. Psychotherapy
Several psychosocial treatments for BD have been shown to be effective in adolescents. Effectiveness is generally measured as longer time to relapse, more time being well, improved functioning, and/or fewer or less severe symptoms/episodes [ 9 ]. These included:
Psycho Education
An approach that involved individual and family teaching to enhance understanding of the disorder (symptoms, classification, etiologies, course, and prognosis). Provided information about medication adherence (classes of medications, alternative therapies, withdrawal syndromes, risks of nonadherence). Developed approaches to detect new episodes (detection of prodromes, warning signs of relapse, relapse prevention planning) and identified illness coping strategies (stress management).
Cognitive-Behavioral Therapy (CBT)
A skills-based individual treatment, which helped the patient recognize and modify the connection between maladaptive thoughts and moods. Structured exercises were applied to identify (thought records, mood diaries, activity scheduling) and modify maladaptive thoughts and behaviors. Focused on automatic negative thoughts, distorted thinking, and maladaptive schema [ 51 ].
Family-Focused Therapy
An approach that involved both the patient and her family and consisted of psychoeducation about BD, and training in communication and problem-solving skills, strengthening the empathic parental attitude [ 52 ].
3.6. Outcomes
A two-year interdisciplinary follow-up and therapeutic intervention gave us the opportunity to assess the comorbidity of the two pathologies. Our patient recovered (defined as eight consecutive weeks with minimal to no symptoms) from her index episode and had no recurrence in the following two years.
4. Discussion
4.1. aspects of concern.
In spite of the precision with which the DSM lays out criteria for diagnosing BD, the clinical presentation of the disorder in children and adolescents is widely debated. Areas of controversy include whether the diagnosis of BD in youth should require clearly demarcated mood episodes and, if so, of what duration, and whether specific hallmark symptoms (euphoria and grandiosity) should be required. The National Institute of Mental Health Research Round table on prepubertal BD (2001) agreed that pediatric BD can be described with “broad” or “narrow” phenotypes [ 9 ]. The narrow phenotype is characterized by recurrent periods of major depression and mania or hypomania fitting the classic definitions of BD I and II, respectively [ 9 ]. The broad phenotype has been variously defined but may involve chronic mood lability/instability rather than discrete mood episodes, and irritability with no euphoria or depression [ 9 ]. Children with the broad phenotype constitute the majority of referrals to clinicians and are characterized by severe irritability, “affective storms,” mood lability, severe temper outbursts, depression, anxiety, hyperactivity, poor concentration, and impulsivity, all with or without clear mood episodes. It is unclear whether broad phenotypes among children are true precursors to full bipolar I disorder in adulthood [ 9 , 53 ].
In our case, comorbidity of BD with ADHD was interesting to study because we had to assess the following details:
- ADHD onset diagnosed under the age of 13 years old, and thus likely to be pre-pubertal, which is in keeping with reports of an earlier onset of BD in youth also suffering from ADHD [ 17 , 54 ]. In contrast, high rates of ADHD are present in children with BD in US studies, with overlap rates from 57% in adolescents to 98% in children [ 17 , 54 , 55 ]. The reported rates of BD in children with ADHD are higher with an onset in childhood than in adolescence [ 17 , 25 ].
- The patient had both conditions even after the remission of overlapping symptoms and continued to meet diagnostic criteria for both conditions, and the predominant mood of mania was irritability rather than euphoria [ 17 , 29 , 56 , 57 ].
- No developmental and global learning difficulties were detected. Conversely, children with ADHD have been found to have more specific developmental and global learning disabilities compared to those with BD. The latter finding is consistent with the well-established literature about the patterns of comorbidity among children with ADHD [ 58 ] and was useful in distinguishing between ADHD and BD [ 17 ].
- In our case study, symptoms such as hyperactivity, distractibility, impulsivity, and restlessness were related to ADHD, as would be expected given that these are core symptoms of the disorder. Additionally, abnormally elevated mood, decreased need for sleep, and psychosis were related to BD. In the literature it is reported that elation and decreased need for sleep may be good symptoms for distinguishing children suffering from BD from those suffering from ADHD [ 9 , 17 , 59 , 60 ]. In our case study, irritability was not useful in the differential diagnosis of BD and ADHD. Irritability as a criterion for BD must be distinguished from irritability as a normal developmental phenomenon and as a common non-specific psychiatric symptom [ 9 ]. Indeed, the nosologic status of irritability in children and adolescents is at the center of the debate about the phenomenology of BD in youth [ 16 , 61 , 62 , 63 ]. Many researchers suggest particular caution is required concerning the use of irritability as a criterion for BD in children and adolescents [ 17 , 64 , 65 , 66 ].
In this clinical case, several aspects of concern about the diagnosis, treatment, and prognosis of BD emerged. Diagnosis of pediatric BD has serious implications for significant short- and long-term morbidities in young people, including poor academic and social performance, psychosocial dysfunction, and increased risk of suicidal behavior [ 7 , 42 , 67 , 68 ]. Accurate differential diagnosis of childhood BD from ADHD is crucial for the appropriate choice of medication and psychosocial interventions [ 17 ]. Moreover, a diagnosis of BD may also lead to treatment with antipsychotics and/or mood stabilizers; both medications may be associated with greater risk of adverse effects in youths [ 17 , 69 ]. Although these treatments have been used increasingly in children, including preschoolers [ 70 ], the risk of excessive pharmacotherapy cannot be understated [ 17 ]. Another aspect of concern is the impact of diagnostic label on a child’s self-conception and emotional life [ 17 ]. Although pharmacotherapy is the mainstay of treatment for BD, medication offers only partial relief for patients. Exclusive treatment with pharmacologic interventions is associated with disappointingly low rates of remission, high rates of recurrence, residual symptoms, and psychosocial impairment. Bipolar-specific therapy is increasingly recommended as an essential component of illness management [ 70 ]. Psychotherapy hastens the recovery from depressive episodes, prevents new mood episodes, and also contributes to the improvement of functioning and quality of life. Given the relatively modest risks associated with psychotherapy (i.e., loss of confidentiality) and robust benefits, psychosocial treatments are considered an important component of BD illness management.
Regarding aspects of concern about the prognosis of BD, long-term follow-up studies illustrate the low recovery rates and high relapse rates associated with the illness. Juveniles have a slower return to euthymia, but a lower relative risk of relapse, and longer time in remission than adult BD patients [ 9 ]. Childhood onset is a predictor less associated with recovery than adolescent onset [ 9 ]. Many studies point out dysfunctions associated with early-onset BD, with negative outcomes including high rates of hospitalization; suicidal behavior; psychosis; reckless behavior; aggression; substance abuse; utilization of psychiatric, medical, and educational services; severe family conflicts; significant caregiver burden; and chronic psychosocial impairment [ 9 , 71 , 72 , 73 , 74 , 75 ]. Some studies make a case for continuity between child- and adult-onset BD based on the similarity of mania symptom distribution between the two, the occurrence of both within the same families, the occurrence of maternal warmth and psychosis as predictors of both outcomes, and the fact that, across the life span and especially in youth, BD usually follows a changeable and sinuous course [ 9 , 26 , 76 ]. Factors such as baseline psychosis and low maternal warmth predict earlier relapse to mania or hypomania [ 9 , 76 ].
4.2. Merits and Limitations
The major contributions of this case report are its emphasis on the narrative aspect (in-depth understanding) and its educational value in helping raise pertinent questions regarding phenomenology, onset, co-morbidity, duration, and management of this important group of disorders [ 77 ]. On the contrary, the major limitations of this case report are the lack generalizability of the results, inability to establish a cause–effect relationship, and the danger of over-interpretation or/and misinterpretation and generalization without justification. In addition, publication bias could be a limiting factor because researchers (or journals in general) favor positive-outcome findings [ 77 , 78 , 79 ]. Retrospective design may be a methodological limitation because case reports are written after the relevant event, i.e., the observation. Thus, retrospectively, the medical record might not contain all of the relevant data and recall bias might prevent us from obtaining the necessary information from the patient, family members, and health professionals [ 77 ].
The clinician (first author) determined that the case report method was the appropriate article type. It is hoped this report can act as a stimulus in the continuing debate regarding the medical case reporting of ADHD and BD comorbidity. The case presentation was conducted by the first author and was cross-checked at every stage by the second and fourth authors to ensure accuracy and validity of data and results, respectively.
5. Conclusions
Despite the occurrence of major risk factors, such as early onset and positive family history, the patient’s condition improved rapidly without any relapse in the subsequent two years. Early and differential diagnoses are considered crucial protective factors for ADHD, leading to an appropriate planning of treatment. In addition, parental involvement and empathic attitude towards the patient supported the latter to cooperate and comply with the treatment, enhancing positive outcomes and stability. Research is required into the reliability and validity of diagnostic protocols and criteria for BD in children and adolescents, and also into the development of individualized therapeutic planning.
Author Contributions
P.T. conceived of the presented idea, performed and developed the case presentation, extracted the main results, composed and revised the report. G.-N.P. corrected, revised and submitted the first and the final draft of the paper. E.B. verified the methods and encouraged P.T. to reshape the extracted results. I.D. supervised the findings of this work. All authors discussed the results and contributed to the final manuscript before the submission. All authors have read and agreed to the published version of the manuscript.
This research received no external funding.
Conflicts of Interest
The authors report no financial or other relationship relevant to the subject of this manuscript.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
- Our Mission
- Related Sites
- Policy Related Centers
- Programming Archive
- Past Programming from CWRU Center for Policy Studies
- Weekly Newsletter
- Location and Parking Directions
- Have a Discussion Suggestion?
- Upcoming Discussions
Shopping cart

College of Arts and Sciences
Public affairs discussion group, why our children struggle in school: going beyond the adhd metaphor.
- June 24, 2024
| |||||||||||















IMAGES
VIDEO
COMMENTS
1.1. Evaluation of ADHD. The current diagnostic criteria for ADHD can be found in the DSM-5 [] and in the International Statistical Classification of Diseases and Related Health Problems, eleventh revision, from the World Health Organization [].Various evaluation instruments are used to identify ADHD, from general assessments via broad scales such as the Wechsler scale, to more specific tests ...
Case Study 1 - JackC. se Study 1 - Jack Jack is a 7 year old male Grade 1 student who lives in Toron. o with his parents. He is the only child to two parents, both of whom have completed post. graduate education. There is an extended family history of Attention Deficit/Hyperactivity Disorder (ADHD), mental health concerns as well as.
OK, let's move on to the case presentation. This first patient is a 19-year-old male, who presented to his psychiatrist after being referred by his primary care provider, PCP for ADHD consultation, during the interview, he noted he was a sophomore in college and is taking 17 credits. This semester chief complaint includes a lack of ability to ...
Case Study Details. Jen is a 29 year-old woman who presents to your clinic in distress. In the interview she fidgets and has a hard time sitting still. She opens up by telling you she is about to be fired from her job. In addition, she tearfully tells you that she is in a major fight with her husband of 1 year because he is ready to have ...
In adult ADHD, the symptoms may be comorbid or mimic other conditions making diagnosis and treatment difficult. Adults with ADHD require an in-depth assessment for proper diagnosis and treatment. The presentation and treatment of adults with ADHD can be complex and often requires interdisciplinary care.
Most of these studies were performed in child and adolescent populations, and as far as we know, only one was conducted in an adult population . Some of the case reports described obsessive-compulsive symptoms as a side effect of MPH treatment in patients with ADHD (12-14, 29-32).
Studies reporting original peer-reviewed qualitative data on the lived experience of adults with ADHD, including mixed-methods studies, were eligible for inclusion. "Adult" was defined as being 18 years of age or older; studies that included adolescent and young adult participants were only included if results were reported separately by age.
Twin, family and adoption studies conducted highlight important generic links to ADHD. Individuals are 60-90% more likely to develop ADHD if there is a familymember who has ADHD (Gizer et al. 2009).Neurotransmitters and genetic coding for specific genes are linked with ADHD traits.
ADHD can result in profound impairments in cognitive and social functioning. For example, impaired short-term memory was higher in college students with ADHD (Dudukovic, Gottshall, Cavanaugh, & Moody, 2014); adults with ADHD are more likely to procrastinate in ... Attention deficit/hyperactivity disorder in adults: A case study ...
The aim of this study was to present the process for detecting a case of ADHD (pre- dominantly inattentive presentation) using the MiniQ test, along with the neurofeedback intervention protocol ...
The presentation and treatment of adults with ADHD can be complex and often requires interdisciplinary care. Mental health and non-mental health providers often overlook the disorder or feel uncomfortable treating adults with ADHD. The purpose of this manuscript is to discuss the diagnosis and management of adults with ADHD.
Despite increased awareness, Attention-deficit hyperactivity disorder (ADHD) is a chronic condition that affects 8% to 12% of school-aged children and contributes significantly to academic and social impairment. There is currently broad agreement on evidence-based best practices of ADHD identification and diagnosis, therapeutic approach, and ...
In a 2020 study, researchers compared 444 adults with diagnosed ADHD with 1,055 adults who exhibited symptoms but had no formal diagnosis. After matching for age and gender, those with a diagnosis reported a higher quality of life, which included metrics for work productivity, self-esteem, and functional performance ( Pawaskar, M., et al ...
Despite increased awareness, Attention-deficit hyperactivity disorder (ADHD) is a chronic condition that affects 8% to 12% of school-aged children and contributes significantly to academic and social impairment. There is currently broad agreement on evidence-based best practices of ADHD identification and diagnosis, therapeutic approach, and ...
This paper presents a case study using monopolar electroencephalogram recording (brain mapping known as MiniQ) for subsequent use in an intervention with neurofeedback for a 10-year-old girl presenting predominantly inattentive ADHD. ... Although this fact may be related to the ADHD profile, in our case study, with 75 neurofeedback sessions, we ...
Clinical case presentation. LB is a 31-year-old divorced woman who presented with complaints of racing thoughts, irritability, worrying, nervousness, labile sleep due to racing thoughts, and inability to remain focused on tasks. ... Impaired early information processing in adult ADHD: A high-density ERP study. BMC Psychiatry, 20 (1) (2020), 10. ...
Characteristics of ADHD seen in children tend to persist into adulthood, but they are often overlooked. This means the prevalence might be higher in adults than reported (Katzman, Bilkey, Chokka, Fallu, & Klassen, 2017). Studies have shown that characteristics seen in children change when individuals enter their late teens or early adulthood.
This thesis presented a case study of a nine year old boy with Attention Deficit Hyperactivity Disorder (hereafter ADHD). ADHD is the current diagnostic label for children presenting with problems in attention, impulse control, and overactivity. These primary characteristics, and the related problems of ADHD
In the final part of her ADHD series, Dr Sabina Dosani, Child and Adolescent Psychiatrist and Clinical Partner London, introduces Luke, a patient she was able to help with his ADHD. ... Case Study. Luke, aged six, gets into trouble a lot at school. His mother gets called by his teacher three or four times a week for incidents of fighting ...
ADHD symptoms. Research in population-based samples indicates that for both sexes the hyperactive-impulsive type predominates in pre-schoolers, whereas the inattentive-type is the most common presentation from mid-to-late childhood and into adulthood [4, 21].By contrast, clinical studies typically report a greater prevalence of combined-type ADHD [5, 12, 22].
A study on ADHD children reported significantly decreased white matter volume, as well as decreased volume in the cortex and caudate nucleus, although it did not reach statistical significance. ... the precise nature of the physiological changes underlying the clinical manifestations of ADHD in each case could be slightly different, affecting ...
Children with ADHD are 50% less likely to participate in sports than children with asthma (Tanden et al., 2019). I find that amazing. Kids with ADHD also have a higher incidence of screen time usage, and we know that that is always a challenge (Tanden et al., 2019). Childhood ADHD is also associated with obesity.
For a formal diagnosis, ADHD symptoms need to have been present before the age of 12, something that can be determined in childhood or, as in my case, much later. Also, ADHD symptoms must ...
Adhd Case Study Essay. 572 Words 3 Pages. Many children battle with functioning and managing Attention-Deficit/ Hyperactivity disorder (ADHD). This single subject research design addressed how the usage of Cognitive-Behavioral Interventions to engage parents, educators, and children can help with the management of ADHD. According to Levine, E ...
In our case study, symptoms such as hyperactivity, distractibility, impulsivity, and restlessness were related to ADHD, as would be expected given that these are core symptoms of the disorder. ... It is hoped this report can act as a stimulus in the continuing debate regarding the medical case reporting of ADHD and BD comorbidity. The case ...
About Our Guest. Arthur Lavin, MD is a retired Pediatrician and Immediate Past Chair of the American Academy of Pediatrics committee charged with drafting policies pertaining to the psychological and social health of America's children. He graduated from Harvard College and earned his MD from Ohio State University. He went on to complete a residency in pediatrics and fellowship in newborn ...
CAMILLA FRANKLIN I-HUMAN CASE STUDY COMPREHENSIVE DIAGNOSIS. 0. ... Add To Wishlist . Trusted by 800,000+ Students; 24/7 Money Back Guarantee; Download is directly available; 12 . 0 . Specifications. Institution. Walden university . Study. NURS-6512 Advanced Health Assessment And Diagnostic Reasoning.
A 2017 study found that about 95 percent of participants who first demonstrated A.D.H.D.-like symptoms at 12 or older did not have the disorder, despite screening positive on symptom checklists ...
Speaking during a listening session Monday, Sangamon County Sheriff Jack Campbell said, "We failed Sonya. We failed Sonya's family and friends."
Li Z. Simulation study of reflective components in primary and secondary school classrooms based on spatial and temporal homogeneity - a case study of Beijing area. MA Thesis, Beijing University of Civil Engineering and Architecture, Beijing, China, 2017. (in Chinese).