150 Case Studies: Real Stories Of People Overcoming Struggles of Mental Health
At Tracking Happiness, we’re dedicated to helping others around the world overcome struggles of mental health.
In 2022, we published a survey of 5,521 respondents and found:
- 88% of our respondents experienced mental health issues in the past year.
- 25% of people don’t feel comfortable sharing their struggles with anyone, not even their closest friends.
In order to break the stigma that surrounds mental health struggles, we’re looking to share your stories.

Overcoming struggles
They say that everyone you meet is engaged in a great struggle. No matter how well someone manages to hide it, there’s always something to overcome, a struggle to deal with, an obstacle to climb.
And when someone is engaged in a struggle, that person is looking for others to join him. Because we, as human beings, don’t thrive when we feel alone in facing a struggle.
Let’s throw rocks together
Overcoming your struggles is like defeating an angry giant. You try to throw rocks at it, but how much damage is one little rock gonna do?
Tracking Happiness can become your partner in facing this giant. We are on a mission to share all your stories of overcoming mental health struggles. By doing so, we want to help inspire you to overcome the things that you’re struggling with, while also breaking the stigma of mental health.
Which explains the phrase: “Let’s throw rocks together”.
Let’s throw rocks together, and become better at overcoming our struggles collectively. If you’re interested in becoming a part of this and sharing your story, click this link!
Case studies
May 7, 2024
My Journey From Hitting Rock Bottom to Overcoming Abuse, Addiction, and Eating Disorder
“Then something happened. On about day 3 or 4, the group spoke and I realized that their way of thinking around food, their rituals, and their tendencies, were all the same as the things I would do. It was wild because I thought I had made these things up myself and here I was with a room full of people who did the same things.”
Struggled with: Abuse Bullying Depression Divorce Eating disorder PTSD
Helped by: Self-Care Social support Therapy Treatment
May 2, 2024
How Yoga Became My Lifeline in Navigating Depression and Building Self-Love
“My relationship with myself was pretty broken and I had no self-belief, I had low self-esteem and I resented my family. It was through yoga that I found the truest feeling of comfort, self-compassion, and courage to move forward, grow as a person, and fall back in love with myself and life again.”
Struggled with: Depression Insomnia Stress Suicidal
Helped by: Exercise Meditation Mindfulness Self-Care
April 30, 2024
Finding Clarity After an ADHD Diagnosis and Bettering Myself With CBT and Medication
“Now as I was getting older, I felt I couldn’t trust my own thoughts in the same way as before, and self-doubt would creep in. I would constantly ask myself whether my emotions and thoughts were accurate or not when reacting to social situations. As you can imagine this was a huge challenge and draining emotionally.”
Struggled with: ADHD Autism
Helped by: Medication Social support Therapy
April 25, 2024
How I’m Seeking Moments of Happiness Despite Struggling With Depression
“The diagnosis I longed for finally arrived, but it didn’t bring the expected empowerment. While it sheds light on my struggles, it also serves as a reminder that this is a part of me that won’t simply vanish. Though mental health can be managed, I know it will always leave its mark. The most challenging part is not always pinpointing why I feel the way I do.”
Struggled with: Depression Negative body image
Helped by: Medication Therapy
April 24, 2024
How Boxing and Therapy Help Me Recover My Identity After Extreme Weight Loss
“When my body changed so drastically and rapidly, it broke my sense of self-identity. About a year into my weight loss, I began to experience early dissociation, depersonalization, and dissociative amnesia. I broke into two people. Me of now and her of before.”
Struggled with: Depression Dissociative amnesia
Helped by: Exercise Self-improvement Therapy
April 18, 2024
How Therapy, Medication and Baking Help Me Navigate Depression and OCD
“I was hospitalized for my eating disorder and my depression several times throughout my college career struggling with the will to live… I was desperate to be “normal” but my brain really got in the way of that.”
Struggled with: Anxiety Depression Eating disorder OCD Suicidal
Helped by: Medication Self-improvement Therapy Treatment
April 16, 2024
How I Found My Self-Worth After Battling Chronic Pain, Anxiety and Panic Attacks
“I remember being floored with a horrible throat infection, and I was just crying. I was done suffering, I couldn’t do it anymore, I was really broken down. That was about 2 years ago now, and it shifted something in my brain. Instead of going down the drain – and keeping that negativity going – it suddenly hit me that I’m the only one responsible for how I feel.”
Struggled with: Anxiety Chronic pain Panic attacks Stress
Helped by: Medication Self-Care Self-improvement Therapy
April 11, 2024
How a Mindset Change Helped Me Break Free From Childhood Trauma and Toxicity
“My mother said she wanted to end it in bloodshed and she waited for him to come home from his late-night meeting. She thought better of it when he was late arriving home. She was overwhelmed with thoughts of her in prison and me in foster care. To say that she made the right decision in achieving the goal of a good life is an answer I struggled to answer for many years.”
Struggled with: Abuse Anxiety Childhood CPTSD Depression
Helped by: Mindfulness Reinventing yourself Self-improvement Therapy
April 9, 2024
Healing From Postpartum Depression With Therapy, Friends & Exercise
“I wasn’t sure how to feel better for a while. People talk about ‘getting help’ but that’s a blanket term and unfortunately it’s not a band-aid you can just put on and suddenly be yourself again. It takes time to find the right therapist, medication if that’s what you decide to do, to find a new rhythm with family, and in my case, I really needed friends locally.”
Struggled with: Postpartum depression
Helped by: Exercise Social support Therapy
April 4, 2024
My Journey from Loneliness and Isolation to Creating an Online Haven for Seniors
“When one is home alone, all day, with nothing to do, nobody to speak with, stuck with their thoughts both good and bad, it’s easy to slip back into a depressive state. Feeling unneeded, unwanted, no happiness, no joy, no reason to get out of bed – just suffering with “the blahs”.”
Struggled with: Depression Loneliness
Helped by: Self-improvement Social support

Mental Health Case Study: Understanding Depression through a Real-life Example
Imagine feeling an unrelenting heaviness weighing down on your chest. Every breath becomes a struggle as a cloud of sadness engulfs your every thought. Your energy levels plummet, leaving you physically and emotionally drained. This is the reality for millions of people worldwide who suffer from depression, a complex and debilitating mental health condition.
Understanding depression is crucial in order to provide effective support and treatment for those affected. While textbooks and research papers provide valuable insights, sometimes the best way to truly comprehend the depths of this condition is through real-life case studies. These stories bring depression to life, shedding light on its impact on individuals and society as a whole.
In this article, we will delve into the world of mental health case studies, using a real-life example to explore the intricacies of depression. We will examine the symptoms, prevalence, and consequences of this all-encompassing condition. Furthermore, we will discuss the significance of case studies in mental health research, including their ability to provide detailed information about individual experiences and contribute to the development of treatment strategies.
Through an in-depth analysis of a selected case study, we will gain insight into the journey of an individual facing depression. We will explore their background, symptoms, and initial diagnosis. Additionally, we will examine the various treatment options available and assess the effectiveness of the chosen approach.
By delving into this real-life example, we will not only gain a better understanding of depression as a mental health condition, but we will also uncover valuable lessons that can aid in the treatment and support of those who are affected. So, let us embark on this enlightening journey, using the power of case studies to bring understanding and empathy to those who need it most.
Understanding Depression
Depression is a complex and multifaceted mental health condition that affects millions of people worldwide. To comprehend the impact of depression, it is essential to explore its defining characteristics, prevalence, and consequences on individuals and society as a whole.
Defining depression and its symptoms
Depression is more than just feeling sad or experiencing a low mood. It is a serious mental health disorder characterized by persistent feelings of sadness, hopelessness, and a loss of interest in activities that were once enjoyable. Individuals with depression often experience a range of symptoms that can significantly impact their daily lives. These symptoms include:
1. Persistent feelings of sadness or emptiness. 2. Fatigue and decreased energy levels. 3. Significant changes in appetite and weight. 4. Difficulty concentrating or making decisions. 5. Insomnia or excessive sleep. 6. feelings of guilt, worthlessness, or hopelessness. 7. Loss of interest or pleasure in activities.
Exploring the prevalence of depression worldwide
Depression knows no boundaries and affects individuals from all walks of life. According to the World Health Organization (WHO), an estimated 264 million people globally suffer from depression. This makes depression one of the most common mental health conditions worldwide. Additionally, the WHO highlights that depression is more prevalent among females than males.
The impact of depression is not limited to individuals alone. It also has significant social and economic consequences. Depression can lead to impaired productivity, increased healthcare costs, and strain on relationships, contributing to a significant burden on families, communities, and society at large.
The impact of depression on individuals and society
Depression can have a profound and debilitating impact on individuals’ lives, affecting their physical, emotional, and social well-being. The persistent sadness and loss of interest can lead to difficulties in maintaining relationships, pursuing education or careers, and engaging in daily activities. Furthermore, depression increases the risk of developing other mental health conditions, such as anxiety disorders or substance abuse.
On a societal level, depression poses numerous challenges. The economic burden of depression is significant, with costs associated with treatment, reduced productivity, and premature death. Moreover, the social stigma surrounding mental health can impede individuals from seeking help and accessing appropriate support systems.
Understanding the prevalence and consequences of depression is crucial for policymakers, healthcare professionals, and individuals alike. By recognizing the significant impact depression has on individuals and society, appropriate resources and interventions can be developed to mitigate its effects and improve the overall well-being of those affected.
The Significance of Case Studies in Mental Health Research
Case studies play a vital role in mental health research, providing valuable insights into individual experiences and contributing to the development of effective treatment strategies. Let us explore why case studies are considered invaluable in understanding and addressing mental health conditions.
Why case studies are valuable in mental health research
Case studies offer a unique opportunity to examine mental health conditions within the real-life context of individuals. Unlike large-scale studies that focus on statistical data, case studies provide a detailed examination of specific cases, allowing researchers to delve into the complexities of a particular condition or treatment approach. This micro-level analysis helps researchers gain a deeper understanding of the nuances and intricacies involved.
The role of case studies in providing detailed information about individual experiences
Through case studies, researchers can capture rich narratives and delve into the lived experiences of individuals facing mental health challenges. These stories help to humanize the condition and provide valuable insights that go beyond a list of symptoms or diagnostic criteria. By understanding the unique experiences, thoughts, and emotions of individuals, researchers can develop a more comprehensive understanding of mental health conditions and tailor interventions accordingly.
How case studies contribute to the development of treatment strategies
Case studies form a vital foundation for the development of effective treatment strategies. By examining a specific case in detail, researchers can identify patterns, factors influencing treatment outcomes, and areas where intervention may be particularly effective. Moreover, case studies foster an iterative approach to treatment development—an ongoing cycle of using data and experience to refine and improve interventions.
By examining multiple case studies, researchers can identify common themes and trends, leading to the development of evidence-based guidelines and best practices. This allows healthcare professionals to provide more targeted and personalized support to individuals facing mental health conditions.
Furthermore, case studies can shed light on potential limitations or challenges in existing treatment approaches. By thoroughly analyzing different cases, researchers can identify gaps in current treatments and focus on areas that require further exploration and innovation.
In summary, case studies are a vital component of mental health research, offering detailed insights into the lived experiences of individuals with mental health conditions. They provide a rich understanding of the complexities of these conditions and contribute to the development of effective treatment strategies. By leveraging the power of case studies, researchers can move closer to improving the lives of individuals facing mental health challenges.
Examining a Real-life Case Study of Depression
In order to gain a deeper understanding of depression, let us now turn our attention to a real-life case study. By exploring the journey of an individual navigating through depression, we can gain valuable insights into the complexities and challenges associated with this mental health condition.
Introduction to the selected case study
In this case study, we will focus on Jane, a 32-year-old woman who has been struggling with depression for the past two years. Jane’s case offers a compelling narrative that highlights the various aspects of depression, including its onset, symptoms, and the treatment journey.
Background information on the individual facing depression
Before the onset of depression, Jane led a fulfilling and successful life. She had a promising career, a supportive network of friends and family, and engaged in hobbies that brought her joy. However, a series of life stressors, including a demanding job, a breakup, and the loss of a loved one, began to take a toll on her mental well-being.
Jane’s background highlights a common phenomenon – depression can affect individuals from all walks of life, irrespective of their socio-economic status, age, or external circumstances. It serves as a reminder that no one is immune to mental health challenges.
Presentation of symptoms and initial diagnosis
Jane began noticing a shift in her mood, characterized by persistent feelings of sadness and a lack of interest in activities she once enjoyed. She experienced disruptions in her sleep patterns, appetite changes, and a general sense of hopelessness. Recognizing the severity of her symptoms, Jane sought help from a mental health professional who diagnosed her with major depressive disorder.
Jane’s case exemplifies the varied and complex symptoms associated with depression. While individuals may exhibit overlapping symptoms, the intensity and manifestation of those symptoms can vary greatly, underscoring the importance of personalized and tailored treatment approaches.
By examining this real-life case study of depression, we can gain an empathetic understanding of the challenges faced by individuals experiencing this mental health condition. Through Jane’s journey, we will uncover the treatment options available for depression and analyze the effectiveness of the chosen approach. The case study will allow us to explore the nuances of depression and provide valuable insights into the treatment landscape for this prevalent mental health condition.
The Treatment Journey
When it comes to treating depression, there are various options available, ranging from therapy to medication. In this section, we will provide an overview of the treatment options for depression and analyze the treatment plan implemented in the real-life case study.
Overview of the treatment options available for depression
Treatment for depression typically involves a combination of approaches tailored to the individual’s needs. The two primary treatment modalities for depression are psychotherapy (talk therapy) and medication. Psychotherapy aims to help individuals explore their thoughts, emotions, and behaviors, while medication can help alleviate symptoms by restoring chemical imbalances in the brain.
Common forms of psychotherapy used in the treatment of depression include cognitive-behavioral therapy (CBT), interpersonal therapy (IPT), and psychodynamic therapy. These therapeutic approaches focus on addressing negative thought patterns, improving relationship dynamics, and gaining insight into underlying psychological factors contributing to depression.
In cases where medication is utilized, selective serotonin reuptake inhibitors (SSRIs) are commonly prescribed. These medications help rebalance serotonin levels in the brain, which are often disrupted in individuals with depression. Other classes of antidepressant medications, such as serotonin-norepinephrine reuptake inhibitors (SNRIs) or tricyclic antidepressants (TCAs), may be considered in specific cases.
Exploring the treatment plan implemented in the case study
In Jane’s case, a comprehensive treatment plan was developed with the intention of addressing her specific needs and symptoms. Recognizing the severity of her depression, Jane’s healthcare team recommended a combination of talk therapy and medication.
Jane began attending weekly sessions of cognitive-behavioral therapy (CBT) with a licensed therapist. This form of therapy aimed to help Jane identify and challenge negative thought patterns, develop coping strategies, and cultivate more adaptive behaviors. The therapeutic relationship provided Jane with a safe space to explore and process her emotions, ultimately helping her regain a sense of control over her life.
In conjunction with therapy, Jane’s healthcare provider prescribed an SSRI medication to assist in managing her symptoms. The medication was carefully selected based on Jane’s specific symptoms and medical history, and regular follow-up appointments were scheduled to monitor her response to the medication and adjust the dosage if necessary.
Analyzing the effectiveness of the treatment approach
The effectiveness of treatment for depression varies from person to person, and it often requires a period of trial and adjustment to find the most suitable intervention. In Jane’s case, the combination of cognitive-behavioral therapy and medication proved to be beneficial. Over time, she reported a reduction in her depressive symptoms, an improvement in her overall mood, and increased ability to engage in activities she once enjoyed.
It is important to note that the treatment journey for depression is not always linear, and setbacks and challenges may occur along the way. Each individual responds differently to treatment, and adjustments might be necessary to optimize outcomes. Continuous communication between the individual and their healthcare team is crucial to addressing any concerns, monitoring progress, and adapting the treatment plan as needed.
By analyzing the treatment approach in the real-life case study, we gain insights into the various treatment options available for depression and how they can be tailored to meet individual needs. The combination of psychotherapy and medication offers a holistic approach, addressing both psychological and biological aspects of depression.
The Outcome and Lessons Learned
After undergoing treatment for depression, it is essential to assess the outcome and draw valuable lessons from the case study. In this section, we will discuss the progress made by the individual in the case study, examine the challenges faced during the treatment process, and identify key lessons learned.
Discussing the progress made by the individual in the case study
Throughout the treatment process, Jane experienced significant progress in managing her depression. She reported a reduction in depressive symptoms, improved mood, and a renewed sense of hope and purpose in her life. Jane’s active participation in therapy, combined with the appropriate use of medication, played a crucial role in her progress.
Furthermore, Jane’s support network of family and friends played a significant role in her recovery. Their understanding, empathy, and support provided a solid foundation for her journey towards improved mental well-being. This highlights the importance of social support in the treatment and management of depression.
Examining the challenges faced during the treatment process
Despite the progress made, Jane faced several challenges during her treatment journey. Adhering to the treatment plan consistently proved to be difficult at times, as she encountered setbacks and moments of self-doubt. Additionally, managing the side effects of the medication required careful monitoring and adjustments to find the right balance.
Moreover, the stigma associated with mental health continued to be a challenge for Jane. Overcoming societal misconceptions and seeking help required courage and resilience. The case study underscores the need for increased awareness, education, and advocacy to address the stigma surrounding mental health conditions.
Identifying the key lessons learned from the case study
The case study offers valuable lessons that can inform the treatment and support of individuals with depression:
1. Holistic Approach: The combination of psychotherapy and medication proved to be effective in addressing the psychological and biological aspects of depression. This highlights the need for a holistic and personalized treatment approach.
2. Importance of Support: Having a strong support system can significantly impact an individual’s ability to navigate through depression. Family, friends, and healthcare professionals play a vital role in providing empathy, understanding, and encouragement.
3. Individualized Treatment: Depression manifests differently in each individual, emphasizing the importance of tailoring treatment plans to meet individual needs. Personalized interventions are more likely to lead to positive outcomes.
4. Overcoming Stigma: Addressing the stigma associated with mental health conditions is crucial for individuals to seek timely help and access the support they need. Educating society about mental health is essential to create a more supportive and inclusive environment.
By drawing lessons from this real-life case study, we gain insights that can improve the understanding and treatment of depression. Recognizing the progress made, understanding the challenges faced, and implementing the lessons learned can contribute to more effective interventions and support systems for individuals facing depression.In conclusion, this article has explored the significance of mental health case studies in understanding and addressing depression, focusing on a real-life example. By delving into case studies, we gain a deeper appreciation for the complexities of depression and the profound impact it has on individuals and society.
Through our examination of the selected case study, we have learned valuable lessons about the nature of depression and its treatment. We have seen how the combination of psychotherapy and medication can provide a holistic approach, addressing both psychological and biological factors. Furthermore, the importance of social support and the role of a strong network in an individual’s recovery journey cannot be overstated.
Additionally, we have identified challenges faced during the treatment process, such as adherence to the treatment plan and managing medication side effects. These challenges highlight the need for ongoing monitoring, adjustments, and open communication between individuals and their healthcare providers.
The case study has also emphasized the impact of stigma on individuals seeking help for depression. Addressing societal misconceptions and promoting mental health awareness is essential to create a more supportive environment for those affected by depression and other mental health conditions.
Overall, this article reinforces the significance of case studies in advancing our understanding of mental health conditions and developing effective treatment strategies. Through real-life examples, we gain a more comprehensive and empathetic perspective on depression, enabling us to provide better support and care for individuals facing this mental health challenge.
As we conclude, it is crucial to emphasize the importance of continued research and exploration of mental health case studies. The more we learn from individual experiences, the better equipped we become to address the diverse needs of those affected by mental health conditions. By fostering a culture of understanding, support, and advocacy, we can strive towards a future where individuals with depression receive the care and compassion they deserve.
Similar Posts

Exploring the World of Bipolar Bingo: Understanding the Game and Its Connection to Bipolar Disorder
Imagine a world where a game of chance holds the power to bring solace and support to individuals affected by bipolar disorder. A seemingly unlikely connection, but one that exists nonetheless. Welcome to the world of…

Can Anxiety Disorders be Genetic? Exploring the Hereditary Aspects of Anxiety Disorders
Introduction to Genetic Factors in Anxiety Disorders Understanding anxiety disorders Anxiety disorders are a common mental health condition that affect millions of individuals worldwide. People with anxiety disorders experience overwhelming feelings of fear, worry, and unease…

Understanding the Abbreviations and Acronyms for Bipolar Disorder
Living with bipolar disorder can be a challenging journey. The constant rollercoaster of emotions, the highs and lows, can take a toll on a person’s mental and emotional well-being. But what if there was a way…

The Connection Between Ice Cream and Depression: Can Ice Cream Really Help?
Ice cream has long been hailed as a delightful treat, bringing joy to people of all ages. It is often associated with carefree summer days, laughter, and moments of pure bliss. But what if I told…

Understanding the Relationship Between Bipolar Disorder and PTSD
Imagine living with extreme mood swings that can range from feeling on top of the world one day to plunging into the depths of despair the next. Now add the haunting memories of a traumatic event…

The Connection Between Meth and Bipolar: Understanding the Link and Seeking Treatment
It’s a tangled web of interconnectedness – the world of mental health and substance abuse. One doesn’t often think of them as intertwined, but for those battling bipolar disorder, the link becomes all too clear. And…

Patient Case #1: 27-Year-Old Woman With Bipolar Disorder
- Theresa Cerulli, MD
- Tina Matthews-Hayes, DNP, FNP, PMHNP
Custom Around the Practice Video Series
Experts in psychiatry review the case of a 27-year-old woman who presents for evaluation of a complex depressive disorder.

EP: 1 . Patient Case #1: 27-Year-Old Woman With Bipolar Disorder
Ep: 2 . clinical significance of bipolar disorder, ep: 3 . clinical impressions from patient case #1, ep: 4 . diagnosis of bipolar disorder, ep: 5 . treatment options for bipolar disorder, ep: 6 . patient case #2: 47-year-old man with treatment resistant depression (trd), ep: 7 . patient case #2 continued: novel second-generation antipsychotics, ep: 8 . role of telemedicine in bipolar disorder.
Michael E. Thase, MD : Hello and welcome to this Psychiatric Times™ Around the Practice , “Identification and Management of Bipolar Disorder. ”I’m Michael Thase, professor of psychiatry at the Perelman School of Medicine at the University of Pennsylvania in Philadelphia, Pennsylvania.
Joining me today are: Dr Gustavo Alva, the medical director of ATP Clinical Research in Costa Mesa, California; Dr Theresa Cerulli, the medical director of Cerulli and Associates in North Andover, Massachusetts; and Dr Tina Matthew-Hayes, a dual-certified nurse practitioner at Western PA Behavioral Health Resources in West Mifflin, Pennsylvania.
Today we are going to highlight challenges with identifying bipolar disorder, discuss strategies for optimizing treatment, comment on telehealth utilization, and walk through 2 interesting patient cases. We’ll also involve our audience by using several polling questions, and these results will be shared after the program.
Without further ado, welcome and let’s begin. Here’s our first polling question. What percentage of your patients with bipolar disorder have 1 or more co-occurring psychiatric condition? a. 10%, b. 10%-30%, c. 30%-50%, d. 50%-70%, or e. more than 70%.
Now, here’s our second polling question. What percentage of your referred patients with bipolar disorder were initially misdiagnosed? Would you say a. less than 10%, b. 10%-30%, c. 30%-50%, d. more than 50%, up to 70%, or e. greater than 70%.
We’re going to go ahead to patient case No. 1. This is a 27-year-old woman who’s presented for evaluation of a complex depressive syndrome. She has not benefitted from 2 recent trials of antidepressants—sertraline and escitalopram. This is her third lifetime depressive episode. It began back in the fall, and she described the episode as occurring right “out of the blue.” Further discussion revealed, however, that she had talked with several confidantes about her problems and that she realized she had been disappointed and frustrated for being passed over unfairly for a promotion at work. She had also been saddened by the unusually early death of her favorite aunt.
Now, our patient has a past history of ADHD [attention-deficit/hyperactivity disorder], which was recognized when she was in middle school and for which she took methylphenidate for adolescence and much of her young adult life. As she was wrapping up with college, she decided that this medication sometimes disrupted her sleep and gave her an irritable edge, and decided that she might be better off not taking it. Her medical history was unremarkable. She is taking escitalopram at the time of our initial evaluation, and the dose was just reduced by her PCP [primary care physician]from 20 mg to 10 mg because she subjectively thought the medicine might actually be making her worse.
On the day of her first visit, we get a PHQ-9 [9-item Patient Health Questionnaire]. The score is 16, which is in the moderate depression range. She filled out the MDQ [Mood Disorder Questionnaire] and scored a whopping 10, which is not the highest possible score but it is higher than 95% of people who take this inventory.
At the time of our interview, our patient tells us that her No. 1 symptom is her low mood and her ease to tears. In fact, she was tearful during the interview. She also reports that her normal trouble concentrating, attributable to the ADHD, is actually substantially worse. Additionally, in contrast to her usual diet, she has a tendency to overeat and may have gained as much as 5 kg over the last 4 months. She reports an irregular sleep cycle and tends to have periods of hypersomnolence, especially on the weekends, and then days on end where she might sleep only 4 hours a night despite feeling tired.
Upon examination, her mood is positively reactive, and by that I mean she can lift her spirits in conversation, show some preserved sense of humor, and does not appear as severely depressed as she subjectively describes. Furthermore, she would say that in contrast to other times in her life when she’s been depressed, that she’s actually had no loss of libido, and in fact her libido might even be somewhat increased. Over the last month or so, she’s had several uncharacteristic casual hook-ups.
So the differential diagnosis for this patient included major depressive disorder, recurrent unipolar with mixed features, versus bipolar II disorder, with an antecedent history of ADHD. I think the high MDQ score and recurrent threshold level of mixed symptoms within a diagnosable depressive episode certainly increase the chances that this patient’s illness should be thought of on the bipolar spectrum. Of course, this formulation is strengthened by the fact that she has an early age of onset of recurrent depression, that her current episode, despite having mixed features, has reverse vegetative features as well. We also have the observation that antidepressant therapy has seemed to make her condition worse, not better.
Transcript Edited for Clarity
Dr. Thase is a professor of psychiatry at the Perelman School of Medicine at the University of Pennsylvania in Philadelphia, Pennsylvania.
Dr. Alva is the medical director of ATP Clinical Research in Costa Mesa, California.
Dr. Cerulli is the medical director of Cerulli and Associates in Andover, Massachusetts.
Dr. Tina Matthew-Hayes is a dual certified nurse practitioner at Western PA Behavioral Health Resources in West Mifflin, Pennsylvania.

The 2024 APA Annual Meeting: Sunday, May 5

Blue Light, Depression, and Bipolar Disorder

The Week in Review: April 1-5

Four Myths About Lamotrigine

An Update on Bipolar I Disorder

Bipolar Disorder Research Roundup: March 29, 2024
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

- Research article
- Open access
- Published: 01 April 2021
Three case studies of community behavioral health support from the US Department of Veterans Affairs after disasters
- Tamar Wyte-Lake ORCID: orcid.org/0000-0001-8449-7701 1 , 2 ,
- Susan Schmitz 1 ,
- Reginald J. Kornegay 3 ,
- Felix Acevedo 4 &
- Aram Dobalian 1 , 5
BMC Public Health volume 21 , Article number: 639 ( 2021 ) Cite this article
2341 Accesses
2 Citations
Metrics details
Community disaster resilience is comprised of a multitude of factors, including the capacity of citizens to psychologically recover. There is growing recognition of the need for public health departments to prioritize a communitywide mental health response strategy to facilitate access to behavioral health services and reduce potential psychological impacts. Due to the US Department of Veterans Affairs’ (VA) extensive experience providing trauma-informed behavioral healthcare to its Veterans, and the fact that VA Medical Centers (VAMCs) are located throughout the United States, the VA is well situated to be a key partner in local communities’ response plans. In this study we examined the role the VA can play in a community’s behavioral health response using case studies from three disasters.
This study investigated experiences of VA employees in critical emergency response positions ( N = 17) in communities where disasters occurred between 2017 and 2019. All respondents were interviewed March–July 2019. Data were collected via semi-structured interviews exploring participants’ experiences and knowledge about VA activities provided to communities following the regional disasters. Data were analyzed using thematic and grounded theory coding methods.
Respondents underscored VA’s primary mission after a disaster was to maintain continuity of care to Veterans. The majority also described the VA supporting community recovery. Specifically, three recent events provided key examples of VA’s involvement in disaster behavioral health response. Each event showed VA’s integration into local response structures was facilitated by pre-existing emergency management and clinical relationships as well as prioritization from VA leadership to engage in humanitarian missions. The behavioral health interventions were provided by behavioral health teams integrated into disaster assistance centers and non-VA hospitals, VA mobile units deployed into the community, and VA telehealth services.
Conclusions
Recent disasters have revealed that coordinated efforts between multidisciplinary agencies can strengthen communities’ capacity to respond to mental health needs, thereby fostering resilience. Building relationships with local VAMCs can help expedite how VA can be incorporated into emergency management strategies. In considering the strengths community partners can bring to bear, a coordinated disaster mental health response would benefit from involving VA as a partner during planning.
Peer Review reports
Disaster behavioral health
The current COVID-19 pandemic, while still underway, has already demonstrated the need for psychological interventions to manage the isolation, stress, and trauma stemming from the ongoing disaster [ 1 , 2 , 3 , 4 , 5 ]. While the scale of the event is unprecedented, interest in understanding the psychological consequences of disasters is not unique to the pandemic [ 6 , 7 , 8 , 9 , 10 ]. Generally, studies exploring the impacts of disasters on behavioral health have found increases in psychological distress in the short term, with the potential for some individuals to experience long-term psychiatric disorders such as posttraumatic stress disorder, depression, and anxiety [ 6 , 7 , 8 , 9 , 10 ].
To ameliorate the potential negative health effects to impacted populations, numerous early interventions have been explored [ 7 , 11 , 12 , 13 , 14 ]. Some countries such as the Netherlands and Iceland use federally structured plans to implement disaster behavioral health interventions [ 12 , 15 ]. And countries like New Zealand have invested heavily in developing extensive mental health programs in response to large scale disaster events [ 16 , 17 ]. In the United States, federal entities strive to create resources and guidance on implementing behavioral health services after disaster, however, interventions are generally managed and delivered by state, territory, and local agencies [ 14 , 18 , 19 ]. Often, after federally declared disasters, the US Federal Government additionally provides funding through the Crisis Counseling Assistance and Training Program (CCP) to community behavioral health programs [ 8 , 13 , 20 ]. Yet the structure and content of interventions are left to the discretion of the implementing agency.
Regardless of the services provided, having a plan in place prior to a disaster can facilitate implementation [ 8 , 11 , 12 , 13 , 19 , 21 , 22 ]. Few publications detail the creation of a local disaster behavioral health response plans [ 15 , 18 , 20 ] or describe the process in which interventions were deployed following an incident [ 7 , 10 , 15 , 20 , 23 , 24 ]. Common themes arising in studies exploring disaster behavioral health plans or interventions are the need for interdisciplinary teams and interagency collaboration [ 8 , 12 , 18 , 19 , 20 ] and strong community response [ 16 ].
The United States Department of Veterans Affairs
One interagency partner often overlooked in the United States is the U.S. Department of Veterans Affairs (VA) Veterans Health Administration (VHA). Previous publications on VHA’s participation in collaborative disaster planning and preparedness efforts with local communities identified barriers to its involvement [ 25 , 26 ]. One such barrier is that the community, and sometime even VHA employees, are unaware that VHA is tasked with planning for and acting to support “national, state, and local emergency management, public health, safety and homeland security efforts” [ 9 , 27 ]. This responsibility to contribute to community efforts is called the VA’s Fourth Mission and is in addition to VHA’s duty to ensure continuity of services to veterans after a disaster.
The expertise of VHA’s 322,030 healthcare professionals and support staff who provide a range of services at its 1255 healthcare facilities spread throughout the U.S. and its territories makes VHA a valuable potential partner in disaster response [ 28 ]. In addition to inpatient and ambulatory medical care, VHA provides a variety of reintegration programs including trauma recovery and behavioral health services for Veterans and their families at its facilities and through community-based care at Vet Centers, Mobile Vet Centers, and college and university campuses [ 29 ]. How these services are applied in community response efforts has been detailed in the grey literature [ 28 , 30 , 31 , 32 ].
This study highlights the potential role of local VA facilities in supporting local behavioral health activities after a disaster, and specifically, presents three exemplars of VHA integrating into communities’ disaster behavioral health response and providing behavioral health support to non-Veterans. The three VA facilities and the events they responded to are: (1) VA Pacific Island Healthcare System (VAPIHC), which is based in Honolulu, Hawaii but provides care to Veterans throughout numerous Pacific Islands. On October 24th, 2018, Super Typhoon Yutu made direct landfall on the Mariana Islands, a US Commonwealth with a nascent established VA tele-mental health clinic on the island of Tinian. This was the strongest typhoon ever recorded to strike the area, severely damaging or destroying many buildings and much of the critical infrastructure of Tinian [ 33 ]; (2) Orlando VA Healthcare System, which serves east central Florida, and encompasses 7 counties. On June 12, 2016, a domestic terrorist attack [ 34 ], targeted hate crime, and one of the deadliest mass shootings in the U.S. occurred at a local establishment, Pulse Nightclub. In a matter of hours, 49 people were killed and 53 were wounded before law enforcement breached the building and ended the violence [ 35 ]; and (3) VA Southern Nevada HCS (VASNHCS), located in and providing care throughout Las Vegas, Nevada. On October 1, 2017, the worst mass shooting in modern history took place at the Route 91 Harvest Music Festival on the downtown Las Vegas Strip. A gunman opened fire on a crowd of more than 22,000, killing 58 people and wounding 413 [ 36 ]. These cases provide examples of interagency partnerships and the implementation of collaborative responses for communities developing their own plans to address the behavioral health needs of their citizens during disasters, including the ongoing COVID-19 pandemic.
Study design
The results presented in this paper stem from a larger study broadly examining the role of local VA facilities in responding to regional large-scale disasters. This study used qualitative interview methods to elicit study participants’ experiences during disasters impacting the U.S. between 2016 and 2018 (see Table 1 for the full list of the disasters covered in the study, the impacted US states and territories, and VA entities affiliated with the impacted areas). Findings on disaster behavioral health functions were pulled as a subset of data and analyzed. The VA Greater Los Angeles Healthcare System Institutional Review Board (Los Angeles, California USA) approved this study.
Setting and sample
The full study sample was purposively chosen to represent individuals with emergency response roles critical to coordinating VA’s local response to disasters. Emergency management personnel at various levels of the VA were the first point of contact and, when applicable, identified additional individuals with critical response roles to interview. Additional respondents were recruited independently by the project team These facilities made up the broad recruitment sample. Due to some respondents covering multiple disasters or being deployed to disasters outside their normal service region, not all entities were included in the final sample.
Data collection methods
Data were collected through semi-structured, 60-min telephone interviews between March–August 2019, using an interview guide developed for this study (see Additional file 1 ). Interviews were conducted individually with each respondent and led jointly by at least two of the authors. Interviews explored participants’ experiences and knowledge about VA activities in the community, specifically focusing on how VA networked and coordinated with non-VA community agencies. Interviews were audio-recorded, although one respondent declined to be recorded.
Analysis plan
A total of 17 individuals were interviewed. However, five interviews did not indicate collaborating with non-VA entities and were therefore not included in the analysis. Due to their involvement in multiple disasters, two respondents were interviewed twice. At completion of the interviews, this resulted in 13 interview recordings being transcribed, and one set of interview notes (due to interviewee declining to be recorded), resulting in a total of 14 interviews that were analyzed with Atlas.ti (v.7) using a grounded theory approach. In phase one of analysis, one author reviewed all 14 interviews, using inductive coding to identify emergent themes in the data, and informed by extensive conversations about project findings held by the project team at the conclusion of each interview [ 37 ]. As a product of this process, a significant emergent theme [ 37 ] was the presence of interagency partnerships implementing collaborative responses to address the behavioral health needs of local citizens during disasters. A decision was made by the project team to narrow the focused coding analyses [ 37 ] to the way local VA facilities engaged in a behavioral response within their local community, in response to their respective large-scale disaster events.
In phase two of the analysis, the initial codes identified by SS were reviewed by TWL for consistency and agreement. Codes not deemed consistent to the focus topic were dropped. Additional grounded themes were confirmed by the team and applied to the data set [ 37 ]. Consensus on final codes was achieved, and one code list was finalized. In phase three of the analysis, the final code list was applied across all relevant interviews. The final code list had a focus on behavioral health response, including behavioral health activities, method of delivery, reactions of staff, and types of impacted community populations, but also included an identification of high level themes across all disasters, including VA expertise, integrating into local, established response activities, identification of local needs, and logistical challenges. Authors TWL and SS then independently coded each interview and resolved discrepancies by consensus.
All respondents played a substantial role in VA’s activities following the respective disasters. However, only 12 participants indicated the VAMC they supported collaborated with non-VA partners during the event in question. Included disasters ranged from widespread to geographically contained; weather-related to acts of violence; and direct impact on VA facilities ranged from none to significant. Though not all respondents described intensive engagement with the community following the event, all respondents described the importance of integrating into local, established response activities. This translated into involvement in community-wide drills and planning committees and following the lead of local incident command. Respondents indicated one of the areas where the VA could provide support to the community was in disaster behavioral health relief operations.
Activities described by respondents were often centered around tasks where the VA could reduce the caseload of other community agencies by identifying Veterans obtaining services in the community and meeting their needs regardless if they were previously enrolled in VA benefits. One key activity described by several respondents included outreach into local shelters. As one respondent explained, VA staff at shelters “[distribute] fliers [that] outline that our counselors are experts in trauma, loss, and in readjustment. They also provide referrals to Veterans for a variety of services, including housing and employment. We also offered free counseling for all community members impacted .”
Identifying where shelters were established and receiving authorization to deploy VA assets to those locations required coordination with local authorities. Multiple respondents mentioned connecting with emergency management running relief efforts to describe available VA resources and detail the services available to both Veterans and the community at large. In some of the events explored in this study, the non-VA authorities were unaware of what the VA could offer while others had pre-existing relationships that allowed for more transparent understanding of how the VA could support response efforts. One respondent went on to describe how the disaster that impacted their VAMC led to additional outreach to local jurisdictions and shelter coordinating agencies (e.g., the American Red Cross) to build relationships and understanding specifically of the behavioral health services the VA could deploy, if needed and approved.
Respondents noted there were specific benefits to conducting outreach in locations where other agencies provided services to the people impacted such as shelters and Local Assistance Centers. They noted that VA staff could more easily reach Veterans to enroll them, if eligible, into VA services and offer care to those who usually used non-VA health and mental health facilities, thereby supporting local agencies by reducing potential patient loads elsewhere. Additionally, by positioning resources at a central location, VA could more readily offer community members services as an extension of their work with Veterans. One specific resource identified as useful for Veteran and community support was Mobile Vet Centers, which have the primary goal of providing social work and mental health services to Veterans. In cases where respondents mentioned this resource, they underscored that non-Veteran community members who requested services in the first days after the disaster were never turned away.
Three community profiles
Three disaster events described by respondents distinctly highlighted cases where the VA was deeply involved in the local community’s disaster behavioral health response. Each event showed VA’s integration into local response structures was facilitated by pre-existing emergency management and clinical relationships, as well as prioritization from VA leadership to engage in humanitarian missions to support the community.
Telehealth in Tinian, Mariana Islands
Prior to Super Typhoon Yutu impacting the Mariana Islands, the VA Pacific Island Healthcare System (VAPIHC) established tele-mental health services on the island of Tinian. These services were located at a non-VA owned healthcare clinic using pre-positioned VA telemedicine equipment and coordinated with the clinic director and staff. Typhoon Yutu devastated the island and led to many Tinian healthcare clinic employees losing their homes. The clinic with VA tele-mental health equipment became a temporary housing site for staff as it was undamaged by the storm. The clinic director realized that in addition to sheltering needs, employees also experienced significant trauma. However, there were limited mental health resources on the island. Once VA became aware of the need, it worked with other federal agencies to manage the logistics of implementing services that took advantage of pre-positioned VA resources.
“… it was a relationship that we had with [the US Department of Health and Human Services] (HHS) and a relationship that we had with the folks on Guam and Saipan … we have a lot of relationships going on. So, we knew that we had that telehealth equipment. We also knew that Tinian was … hit pretty hard. And that there was a lot of grief. And so I can’t say how it totally emerged, but there’s so many relationships and there’s so much communication during an emergency.”
Respondents reported it was initially challenging to identify whether VA could provide mental health services in the community and how the services would be funded. Staff at all levels of the VA worked with the Federal Emergency Management Agency (FEMA) and HHS to get official authorization as well as receive federal funding for VAPIHC to provide time limited tele-mental health interventions to clinic staff on Tinian. VAPIHC Tele-mental Health Hub coordinated with the local clinic director to inform employees about available services and utilized technology onsite to provide weekly support groups for 13 health center employees.
Director’s 50 in Orlando, Florida and the pulse nightclub shooting
The Orlando VA Healthcare System (OVAHCS) houses a unique emergency response team “The Director’s 50.” Made up of multi-disciplinary VA healthcare workers, including mental health professionals (i.e. psychologists, psychiatrists, mental health nurses), the Director’s 50 can deploy a team of up to 50 volunteers within 2 hours to areas throughout the region when authorized by the Orlando VAMC Director. As described by one respondent, the mission of the team is,
“to provide an immediate gap fill to an emergency before VA can get its assets organized and into a formal support and response role. So the team is multi-disciplinary and multi-functional with its capabilities, so that it can immediately address the needs of the emergency response until VA can formalize how it’s going to provide their support to the community.”
The Director’s 50 includes interdisciplinary clinical and service support training for all members such as triage and treatment services, mental health intervention, peer counseling, and psychological support to trauma. Through participation in community-wide exercises and drills, the Director’s 50 has built versatile capabilities and strong relationships with local emergency management agencies and area hospitals.
In response to the Pulse Nightclub Shooting, VA Central Office requested OVAHCS to deploy the Director’s 50 to provide VA resources and support the community’s response. The team activated their mass notification system to alert their nearly 100 volunteer members and quickly assembled an initial response team of about 15 clinical, mental health, and support professionals within 1 hour. Respondents noted having internal approval can speed up the process of deploying teams. In general, to distribute VA resources into the community, a federal disaster declaration is required to initiate the Robert T. Stafford Disaster Relief and Emergency Assistance Act or where the HHS Secretary has activated the National Disaster Medical System, both of which grant VA the ability to provide assistance. Therefore, respondents noted a need to balance expectations of leadership to help quickly, while also ensuring VA resources were legally allowed to be used in the response.
One thing that facilitated OVAHCS’s integration into the local response system was a pre-existing relationship with the City of Orlando’s Office of Emergency Management and the Central Florida Medical Disaster Coalition, which facilitated the Director’s 50 integration into the city’s response and allowed them to report to the victim reunification center. The team was tasked.
“to be the initial communication to the family members for those victims that actually passed away. So, 49 victims, our team was assigned to go ahead and be the initial contact to let them know that their loved ones had passed, and to begin the coordination for services, grief counseling and victim advocacy, you know, to help them prepare the initial points of piecing together their lives after being notified of such tragic events.”
Accordingly, the initial multi-disciplinary team narrowed its focus to mainly members with mental health expertise. Over the next 2 weeks, the team worked with the community, helping to manage vigils and gatherings for the public, and continuing grief counseling and mental health support for the whole community, including providing peer behavioral health support to municipal first responders. Since this act of violence targeted people who were Lesbian Gay Bisexual Transgender Queer (LGBTQ) frequenting Pulse Nightclub, not only were relatives of victims or survivors from inside the building affected, but the entire LGBTQ community felt the traumatic impact of the shooting. One respondent described the importance of providing mental health support from multiple community agencies when a disaster of this magnitude occurs,
“And they [the people who were at the shooting] truly needed a place, and this is why we were there for greater than just the 24-48 hours of initially identifying the people who was killed during the shooting, you had everyone that was inside of the club who were seeking a place where they could go and receive the care and support that they needed as well. And obviously, you know, this is something that is an endemic issue with healthcare as a whole, is the access to mental health counseling and services. So VA, as well as some other partnering mental health organizations were able to supply that need right there at the site where they were doing victim notification or victim reunification and family support. We were able to do that.”
One respondent noted a key point to remember about the Director’s 50, “they are all volunteers...And these people will go—you know, 24 hours a day, day in and day out, to execute that mission. And we have to think about team resiliency.” This included caring for team member’s well-being by rotating staff and providing and attending to the mental heath of one another. As described by one respondent,
“Because when it was all said and done, the team was very affected by what they had to do. You know, just imagine hearing—you know, overwhelming grief for every one of the 49 victims’ families that would show up. And the team took that burden on … and I will tell you, to this day, it still affects the people who went and supported that mission. And they really—those who supported that mission have a greater reverence for what we do now, as a team. So you’d never have to ask them to—whether they are going to support anything related to the Director’s 50. That comradery that’s there, they won’t let their own kind of—go into the bowels of despair like that, alone.”
Integrating into community response in Las Vegas, Nevada after the route 91 harvest festival shooting
As a large city with many national and international visitors, respondents described Las Vegas as having a very centralized emergency response structure. Relationships between VA Southern Nevada HCS (VASNHCS) and local response agencies and area hospitals were described as “tightknit” with great working relationships where organizations plan and prepare for disasters together. As one respondent put it,
“what I do know is my community. I know my community partners. I know what they have, what they don’t have, they know what I have, what I don’t have. And that’s what makes us so resilient. That’s community.”
Although located too far away from the Las Vegas Strip to actively receive injured victims when the shooting occurred at the Route 91 Harvest Music Festival, VASNHCS activated its Hospital Incident Command System so it could actively participate in the community’s response and organize efforts. A Multi-Agency Coordination Center (MACC) organized the response activities, and respondents underscored the value of both pre-existing relationships and an understanding of the county’s emergency response structure. As explained by a respondent,
“You can’t wait for your community to ask you. You have to be on the forefront and know what they need. And you only do that by knowing your community. You know, I spent probably as much time in my community as I do in my medical center. A lot of the time, it’s my own time, but again, it builds that relationship that when they’re updating their mass casualty plan, one of the people they’re calling is [me].”
This previous collaboration, as well as being present at the MACC, allowed VASNHCS to identify community needs that it could address.
As news of the shooting spread, VA leadership tasked VASNHCS with deploying staff into the community. However, it was challenging to balance the push from VA to deploy with continuing to respect established local coordination structures. VASNHCS maintained a presence within the Medical Area Surge Command of the MACC to offer resources and expertise, waiting for requests, instead of directly deploying assets outside of the established system.
In the immediate response, VASNHCS assisted with managing fatalities. It offered morgue space to the county and initiated the mass fatality plan to increase morgue capacity. This provided the county and partner hospitals space for victims until they could be processed, and families could claim them. Additionally, VASNHC offered a Psychological First Aid (PFA) team.
Initially, VASNHCS deployed their PFA team to the community’s family reunification center. The team was composed of social workers, psychologists, psychiatrists, administrators (as support staff), canteen services (for water and snacks to sustain clients and staff), and the medical center’s Chief of Staff. As the situation evolved, the MACC received requests from local agencies for psychological assistance and VASNHCS transitioned to directly integrating into area hospitals.
Three Las Vegas hospitals received the bulk of the injured or dead and recognized the need for psychological interventions with their staff. Due to their close relationships with other hospitals, one respondent explained that they were familiar with the Employee Assistance Program (EAP) at these hospitals. The respondent knew it would take time for the EAP to arrive onsite and they would most likely focus on clinical staff involved in directly treating the injured. Therefore, VASNHCS developed a three-pronged approach to complement EAP services at the receiving hospitals. Firstly, the PFA team provided what one respondent called “ trauma therapy ” to hospital staff, regardless whether they worked the night of the shooting. The assistance extended beyond clinical staff to non-clinical departments, such as environmental services/housekeeping, whose staff were also impacted through their response roles.
Respondents reported one of the reasons their response in the hospitals was so successful was that the team was multidisciplinary, allowing staff from different departments to talk to people in similar positions, which was valued by the recipients.
“So for example, we have a nurse that’s trained in trauma, psychological first aid. So they want the nurses at [the hospital with a patient surge], they want to talk to our team. They were still processing. But when we brought our nurse into the ward, they were more than willing to open up to her, because she was one of them. She was part of their tribe. So we try to match our tribe to their tribe, and that’s why we were successful.”
Secondly, the VASNHCS team worked with victims of the shooting, providing PFA and social work services. Thirdly, they integrated with family members of patients at the hospitals and provided them items that they did not otherwise have because they were visitors to Las Vegas. Examples included coordinating free transportation to and from hospitals and hotels, connecting them to local mortuary services, and providing information about how to access services when they returned home.
The PFA team ran for 24 h a day, for 7 days in those three impacted hospitals. To balance VA patient care with the community response mission, VASNHCS staff volunteered shifts outside of their normal work hours. One respondent described the overwhelming desire of VA staff to help their community.
“And while it didn’t impact our staff or our clinics, or our patients, it impacted our community. I think another thing that still amazes me to this day, was the outpour of our staff and what I mean by that is they were coming out of the woodwork to support. We had more volunteers working an eight-hour shift and then coming in [to volunteer] at five o’clock or four o’clock and working to midnight to two in the morning and not go home until four or five in the morning, and then go to work the next day, because we didn’t want to impact our patient care. And they were doing this out of their—you know, because they care. They care about the community, they care about the event, they care about the people. And then at the end of the day, you know, we had more volunteers than we had placements, because we did not want to overwhelm the health systems with all of these VA personnel.”
However, with new volunteers each shift, a key lesson learned was to have a daily team debrief. As people changed daily, a debrief provided key information and a running tally of support being provided to save time and avoid reinventing the wheel identifying contacts or systems already developed.
Another lesson was that preparedness requires ongoing maintenance. The importance of ongoing preparedness was underscored when VASNHCS realized that leading up to the shooting, they had reduced their focus on PFA training. As described by one respondent, “ We noticed that we need that continuous [psychological first aid] training, that we need continuous exercising, and it’s not an easy fit, to send a bunch of people to someone else’s hospital or an area to do that kind of service .” They also realized the first wave of personnel went into community hospitals without basic supplies they needed to provide services, including basic items such as pens, PFA guides, and informational brochures.
Three months following the shooting, the VASNHCS Emergency Manager, working with the Chief of Social Work hosted a lunch for staff who volunteered to thank them for their involvement. During that event, they realized volunteers were not only impacted by the event itself, but also by their time providing support in the community. They therefore created a forum to again gather staff who had deployed at the 6 month and 9 month marks to eat and talk about the impact of the event on the healthcare system and themselves. On the 1 year anniversary, management had a special event for the volunteers,
“we actually had people from the community that we supported coming in and they broke bread with our team and what they did was, they talked about what the impact of the VA Southern Nevada Healthcare System was going into that event, and how we helped them bridge the gap [of mental health support] that was crucial at that time, and how appreciative they were to our cause and our Clark County Office of Emergency Management gave all our staff that responded T-shirts that said Vegas Strong, because they wanted them to know that we—they appreciated the work that we did for them to support our community.”
The need for attention to the psychological well-being of individuals during and after a disaster has been well proven as disasters have been found to be associated with both short and long-term symptoms and disorders [ 6 , 7 , 8 , 9 , 10 , 38 ]. Although in some parts of the world there are federally structured plans to implement disaster behavioral health interventions, in the United States there is a patchwork system that often relies on support and resource allocation from a multitude of agencies [ 8 , 13 , 14 , 18 , 19 , 20 ]. In this study we examined the role the VA can play in a community’s disaster relief effort and highlighted the opportunity for VA to support behavioral health response focusing specifically on case studies from three disasters.
Essential to effective emergency management is an understanding of, and engagement with, available resources in a local community. This is of particular importance when considering complex individual and group needs such as behavioral health support. VA Medical Centers can be seen as challenging partners to work with because they are both a federal entity and a local healthcare facility [ 26 ]. However, in the case of Super Typhoon Yutu, the federal positioning of the VA and its connection with HHS and FEMA facilitated the deployment of VAPIHC virtual resources. The regional respondents who supported the VA disaster mission in Tinian described how preexisting relationships with federal partners facilitated authorization and funding.
Another potential challenge to incorporating the VA into response efforts is that prior to offering services, VA leadership must balance the mission of the agency with community needs, without contradicting the restrictions of the Stafford Act. In all three presented cases, VA’s behavioral health support was not formally included in a city or county response plan, and yet pre-existing relationships between key stakeholders facilitated the provision of VA behavioral health services to support identified community needs. Respondents also described participating in interagency coordinating groups, response trainings, and exercises before the disaster. These activities aided in a deeper understanding of the response structures each partner operated under and encouraged strong rapport between agencies.
Relationships between VA emergency management and local emergency management proved invaluable as VA staff understood that services should not be provided without first engaging local response coordinators. All VA facility leadership and emergency managers are required to be trained in the Incident Command System (ICS) and National Incident Management System (NIMS), which are the coordinating structures all U.S. response agencies work within [ 39 ]. As a health care provider at a national level, VHA falls within the operations section Essential Support Function (ESF) 8: Public Health and Medical Services to support the Department of Health and Human Services [ 40 ]. Local jurisdictions may also connect with VAMCs through ESF 8 representation. For example, the VA has provided significant support to communities impacted by COVID-19. As of July 8, 2020, VA provided more than 330,000 pieces of Personal Protective Equipment (PPE) in support of the Fourth Mission, as well as hand sanitizer, laundry support, test kits and testing support, and webcams for use with existing equipment to state and local facilities. In addition, VA has admitted 279 non-Veterans to VA Medical Centers because of the pandemic [ 27 ]. Much of this coordination was done through ESF 8 coordination at a local or national level.
While respondents did not go into detail about their participation in the emergency management structure, some participants described their VA’s roles within emergency operations as liaisons. Groups such as this could report to either the planning, operations, or command sections within the ICS. Group supervisors would most commonly report to the operations section chief, likely through branch directors, given that the focus of the work would be more on specialized functions as needed for tactical operations. Regardless of where they fit, their presence at emergency operations centers and command posts facilitated communication to allow for VA’s integration into incident action plans. Particularly during the response to mass casualty events in Orlando and Las Vegas, understanding the local response network and then proffering available services was essential to avoid confusion or duplication of activities. By working within the established coordination centers, VA’s efforts were effectively integrated into the greater community behavioral health response and were deployed to points of greatest need. Although a detailed understanding of the integration of VA activities into ICS structures fell outside of the scope of this work, future assessment of the integration of VA representatives into local, state, and/or regional ICS structures could help clarify roles and identify which section liaisons best support (e.g., operations, planning, logistics) [ 40 ].
VA is increasingly strengthening partnerships with agencies that provide behavioral health services to Veterans and their families who use non-VA community-based care [ 41 ]. In each case example, the primary support provided by VA to the community was the provision of behavioral health services in response to an identified need. Respondents described this as being due, in large part, to the recognition of VA’s expertise in trauma and post-trauma treatment, thereby allowing these resources to come to the forefront. While not mentioned by the respondents, an additional value that VA providers add to disaster behavioral health responses is their exposure to and understanding of the unique needs of various populations throughout their communities. In addition to ensuring care is culturally competent to the unique identity of being a Veteran, VA staff must respect the diversity of Veterans themselves. Just like the U.S. population at large, Veterans represent a range of ages, races, genders, sexual orientations, socioeconomic statuses, etc. and mental health services must be considerate of this diversity. The VA recognizes this and offers training to providers to understand and respect their patients’ unique needs [ 42 ]. Working with a variety of populations preposition VA staff to have a deeper understanding of the post-disaster needs of the wider community.
Two of the case examples described in this study especially bring to the forefront the importance of disaster behavioral health response planning and implementation teams understanding unique experiences of community members. Super Typhoon Yutu directly impacted an archipelago housing a majority Asian and/or Pacific Island population. The Pulse Nightclub shooting, while a terrorist event, was a targeted hate crime intended to inflict violence on the LGBTQ community. Disaster behavioral health interventions for these affected groups not only need to take into consideration the importance of cultural competency but also the potential of re-traumatization and distinct population mental health needs.
In the Northern Mariana Islands, while there is a mix of ethnic groups (Filipino, Chamorro, Chinese, Carolinian, Korean, Palauan, etc.), many either identify as or are categorized more broadly as Asian and/or Pacific Islanders. Although there are more than 1.4 million people who are considered Pacific Islanders living the in the U.S., there is a dearth of information on the mental health of this population [ 43 ]. Similarly, the prevalence and incidence rates of mental illness in the Mariana Islands is not well studied [ 44 ]. Some sources attribute this lack of understanding to a disproportionate underuse of mental health services [ 43 ]. However, Asian and Pacific Islanders within the U.S. and those territories affiliated with it often experience transgenerational trauma, discrimination, continued loss from colonization, historical trauma, and mental health stigma which can impact psychological wellbeing and help seeking behavior. Additionally, cultural elements (collectivism, reverence for the past, hierarchical social order, etc.) of this population are important to understand when providing behavioral health services [ 43 , 45 ]. One of the reasons respondents indicated that the VA was asked to provide assistance following Typhoon Yutu was the lack of availability of mental health services in Tinian. The established VA telehealth technology increased accessibility to behavioral practitioners from VAPIHC who most likely were experienced working with Asian and Pacific Island populations since more than 55,000 Veterans who identify as this ethnicity live in Island Areas or Hawaii [ 46 , 47 ].
The Pulse Nightclub Shooting was a terrorist driven hate crime targeting individuals who identified as LGBTQ. Members of this group often experience discrimination, stigma, and trauma throughout their lives. Discrimination and heterocentric health and mental health practices can marginalize this population and impact help seeking behavior [ 48 , 49 ]. This is of particular concern as individuals who are LGBTQ face numerous mental health disparities with a higher likelihood of experiencing depression, anxiety, substance misuse, and suicide attempts. The shooting not only targeted LGBTQ people but it also took place during Latin Pride Night meaning many of the victims and casualties were LGBTQ Latinx. The resulting psychological impacts of the Pulse Nightclub shooting on those directly impacted, people who are LGBTQ Latinx, and individuals in the wider LGBTQ community have been investigated and show experiences of trauma and impacts on perceived safety [ 50 ]. At the time of the shooting, the Orlando VAMC had established relationships with LGBTQ local mental health services and had staff knowledgeable in the needs of this community [ 51 ]. In fact, in the recent past, the VA has increased its efforts to ensure Veterans who are LGBTQ receive the highest quality patient-centered care possible [ 52 ]. Mental health services in particular have bolstered recognition of the complex needs of these Veterans [ 52 ].
All three cases demonstrate innovative ways VA can provide behavioral health support outside of their facilities, i.e., via telehealth capabilities across an ocean and into a healthcare clinic, teams of mobile units reaching directly into the community to support victims, victims’ families, and the community at large, and finally by incorporating PFA teams directly into hospitals to support staff, patients, and patients’ families. This flexibility across sites to address different needs and populations while using varying available infrastructure support, is paramount to any local jurisdiction’s ability to meet on the ground needs following a disaster. It demonstrates the variability between VAMCs and the importance of local disaster behavioral health planning teams to pre-identify resources to assess local capacity. Plans can then be developed that access and deploy the tools/skills of interdisciplinary and interagency teams. Building processes to deploy local health and mental health practitioners can lead to more rapid implementation of interventions and help ensure the diversity of the impacted community is recognized and respected. Additional studies focused on how communities develop disaster behavioral health plans could provide insight into which agencies are involved and how they collaborate. It may also be useful to assess whether and how these plans are implemented to identify best practices.
In addition to the people directly impacted by disasters, respondents underscored the importance of offering support to responders as well. There is growing recognition that health care workers are themselves front-line response workers who may be psychologically impacted when caring for others, leading to a growing emphasis on the importance of selfcare and employee wellbeing [ 39 , 40 , 41 , 42 ]. In all three case studies, behavioral health support was, at least in part, directed toward healthcare workers. In the case of Las Vegas, a respondent highlighted the advantage of having behavioral health support come from individuals who understood the culture of the population they were helping, e.g., nurses supporting nurses. Further, respondents in Las Vegas and Orlando highlighted the importance of supporting deployed behavioral health team members. They detailed actions to maintain staff well-being by having rotating shifts, encouraging peer support, and facilitating gatherings for staff to publicly thank them for their efforts and allow them to address their experiences together as a group. Understanding the needs of healthcare and behavioral health personnel and building support networks into response frameworks can help better sustain and strengthen the overall response process.
A primary limitation of this study is that interviews were conducted up to one and a half years after the disasters described, potentially impacting recall. However, multiple interviewees corroborated the information presented for each of the case studies. Another limitation is that this study focused exclusively on the experiences of VA employees fulfilling mission requirements and their description of instances where VA acted in support of the Fourth Mission. Very few of the respondents directly provided the behavioral health interventions. These perspectives could provide deeper understanding of the interventions themselves as well as the impacts they may have on practitioners. Neither community members nor coalition partners were interviewed in this study. Future research would benefit from both interviewing non-VA participants to explore additional perspectives and gain greater insight on how local jurisdictions experienced collaborating with VA representatives and exploring alternative approaches to mental health units within and outside VA to examine whether and when different approaches may be preferable.
As the largest integrated healthcare system in the United States, VA can play an important role in disaster response across the country. As recognition of VA’s expertise in behavioral health grows, particularly around trauma and post-trauma treatment, VA should be considered a strong potential partner in behavioral health responses. Local VAMC staff are part of the community in which they live and the Veterans they serve are a microcosm of the larger population of the U.S. As the respondents in this study showed, there is a deep desire by VA staff to provide support following a disaster if they are able. Anticipating potential behavioral health concerns, and having a plan to address them, can foster community disaster resilience. While these plans may be different for each jurisdiction, they can be strengthened by identifying and incorporating a range of partners. Having preexisting relationships where VA’s capabilities are known before a disaster occurs can facilitate the rapid deployment of VA resources into identified areas of community need. The case studies presented demonstrate the flexible nature of these resources. By extending knowledge about innovative ways to share behavioral health and other resources in a disaster response, communities and healthcare coalitions can be better prepared to engage collectively and rapidly mobilize essential assets to support the wellbeing of those who need it most.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Crisis Counseling Assistance and Training Program
U.S. Department of Veterans Affairs
Veterans Health Administration
VA Medical Center
VA Pacific Island Healthcare System
VA Southern Nevada HCS
Veterans Health Administration Health Care System
Veterans Integrated Service Network
Office of Emergency Management
US Department of Health and Human Services
Federal Emergency Management Agency
Lesbian Gay Bisexual Transgender Queer
Multi-Agency Coordination Center
Psychological First Aid
Employee Assistance Program
Personal Protective Equipment
Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–20. https://doi.org/10.1016/S0140-6736(20)30460-8 .
Article CAS PubMed PubMed Central Google Scholar
Fiorillo A, Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur Psychiatry. 2020;63(1):e32. https://doi.org/10.1192/j.eurpsy.2020.35 .
Article CAS PubMed Google Scholar
Pfefferbaum B, North CS. Mental health and the COVID-19 pandemic. N Engl J Med. 2020;383(6):510–2. https://doi.org/10.1056/NEJMp2008017 .
Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 2020;33(2):e100213. https://doi.org/10.1136/gpsych-2020-100213 .
Article PubMed PubMed Central Google Scholar
Vigo D, Patten S, Pajer K, Krausz M, Taylor S, Rush B, et al. Mental health of communities during the COVID-19 pandemic. Can J Psychiatr. 2020. https://doi.org/10.1177/0706743720926676 .
Beaglehole B, Mulder RT, Frampton CM, Boden JM, Newton-Howes G, Bell CJ. Psychological distress and psychiatric disorder after natural disasters: systematic review and meta-analysis. Br J Psychiatry. 2018;213(6):716–22. https://doi.org/10.1192/bjp.2018.210 .
Article PubMed Google Scholar
Beinecke R, Raymond A, Cisse M, Renna K, Khan S, Fuller A, et al. The mental health response to the Boston bombing: a three-year review. Int J Ment Health. 2017;46(2):89–124. https://doi.org/10.1080/00207411.2017.1294969 .
Article Google Scholar
Beinecke RH. Addressing the mental health needs of victims and responders to the Boston Marathon bombings. Int J Ment Health. 2014;43(2):17–34. https://doi.org/10.2753/IMH0020-7411430202 .
Dobalian A, Callis R, Davey VJ. Evolution of the Veterans Health Administration’s role in emergency management since September 11, 2001. Disaster Med Public Health Prep. 2011;5(S2):S182–4. https://doi.org/10.1001/dmp.2011.61 .
Heslin KC, Stein JA, Dobalian A, Simon B, Lanto AB, Yano EM, et al. Alcohol problems as a risk factor for postdisaster depressed mood among U.S. veterans. Psychol Addict Behav. 2013;27(1):207–13. https://doi.org/10.1037/a0030637 .
Hobfoll SE, Watson P, Bell CC, Bryant RA, Brymer MJ, Friedman MJ, et al. Five essential elements of immediate and mid-term mass trauma intervention: empirical evidence. Psychiatry. 2007;70(4):283–337. https://doi.org/10.1521/psyc.2007.70.4.283 .
Jacobs J, Oosterbeek M, Tummers LG, Noordegraaf M, Yzermans CJ, Duckers MLA. The organization of post-disaster psychosocial support in the Netherlands: a meta-synthesis. Eur J Psychotraumatol. 2019;10(1):1544024. https://doi.org/10.1080/20008198.2018.1544024 .
North CS, Pfefferbaum B. Mental health response to community disasters: a systematic review. JAMA. 2013;310(5):507–18. https://doi.org/10.1001/jama.2013.107799 .
Watson PJ, Ruzek JI. Academic/state/federal collaborations and the improvement of practices in disaster mental health services and evaluation. Admin Pol Ment Health. 2009;36(3):215–20. https://doi.org/10.1007/s10488-009-0212-4 .
Thordardottir EB, Gudmundsdottir B, Petursdottir G, Valdimarsdottir UA, Hauksdottir A. Psychosocial support after natural disasters in Iceland-implementation and utilization. Int J Disaster Risk Reduction. 2018;27:642–8. https://doi.org/10.1016/j.ijdrr.2017.11.006 .
Fergusson DM, Horwood LJ, Boden JM, Mulder RT. Impact of a major disaster on the mental health of a well-studied cohort. JAMA Psychiatry. 2014;71(9):1025–31. https://doi.org/10.1001/jamapsychiatry.2014.652 .
Gray L, MacDonald C, Mackie B, Paton D, Johnston D, Baker MG. Community responses to communication campaigns for influenza A (H1N1): a focus group study. BMC Public Health. 2012;12(1):1–12.
Compton MT, Cibulas BK, Gard B, Kaslow NJ, Kotwicki RJ, Reissman DB, et al. Incorporating community mental health into local bioterrorism response planning: experiences from the DeKalb County Board of Health. Community Ment Health J. 2005;41(6):647–63. https://doi.org/10.1007/s10597-005-8846-5 .
Pfefferbaum B, Flynn BW, Schonfeld D, Brown LM, Jacobs GA, Dodgen D, et al. The integration of mental and behavioral health into disaster preparedness, response, and recovery. Disaster Med Public Health Prep. 2012;6(1):60–6. https://doi.org/10.1001/dmp.2012.1 .
Elrod CL, Hamblen JL, Norris FH. Challenges in implementing disaster mental health programs: state program directors’ perspectives. Ann Am Acad Pol Soc Sci. 2016;604(1):152–70.
Gil-Rivas V, Kilmer RP. Building community capacity and fostering disaster resilience. J Clin Psychol. 2016;72(12):1318–32. https://doi.org/10.1002/jclp.22281 .
Melmer P, Carlin M, Castater CA, Koganti D, Hurst SD, Tracy BM, et al. Mass casualty shootings and emergency preparedness: a multidisciplinary approach for an unpredictable event. J Multidiscip Healthc. 2019;12:1013–21. https://doi.org/10.2147/JMDH.S219021 .
Naturale A, Lowney LT, Brito CS. Lessons learned from the Boston Marathon bombing victim services program. Clin Soc Work J. 2017;45(2):111–23. https://doi.org/10.1007/s10615-017-0624-7 .
Reifels L, Pietrantoni L, Prati G, Kim Y, Kilpatrick DG, Dyb G, et al. Lessons learned about psychosocial responses to disaster and mass trauma: an international perspective. Eur J Psychotraumatol. 2013;4.
Dobalian A. The US Department of veterans affairs and sustainable health care coalitions. Disaster Med Public Health Prep. 2015;9(6):726–7. https://doi.org/10.1017/dmp.2015.136 .
Schmitz S, Wyte-Lake T, Dobalian A. Facilitators and barriers to preparedness partnerships: a veterans affairs medical center perspective. Disaster Med Public Health Prep. 2018;12(4):431–6. https://doi.org/10.1017/dmp.2017.92 .
VA Fourth Mission Summary [ https://www.va.gov/health/coronavirus/statesupport.asp ].
Office of Public and Intergovernmental Affairs [ https://www.va.gov/opa/pressrel/searchResults.cfm ].
Affairs USDoV: VA Office of mental health and suicide prevention guidebook. 2018.
Google Scholar
Lawrence Q. VA secretary Wilkie: ‘We are the surge force’. In: The coronavirus crisis: NPR. NPR.org ; 2020.
Services UDoHH. HHS, FEMA, DOD and VA continue to provide sustained and critical medical care support for Puerto Rico as part of Trump Administration response to Hurricane Maria. In . HHS.gov News: US Department of Health & Human Services; 2017.
Steinhauer J. The V.A. Prepares to back up a health care system threatened by coronavirus: The New York Times; 2020.
Agency FEM. Super typhoon Yutu: one year later: FEMA; 2019.
Foundation NP: After-action review of the orlando fire department response to the attack at pulse nightclub. 2018.
Investigation FBo: Active shooter incidents in the United States in 2016 an 2017. 2018.
Department LVMP: 1 October after action review. 2018.
Charmaz K, Belgrave LL. Grounded theory: The Blackwell Encyclopedia of Sociology; 2007. https://doi.org/10.1002/9781405165518.wbeosg070 .
Lowe SR, Galea S. The mental health consequences of mass shootings. Trauma Violence Abuse. 2017;18(1):62–82. https://doi.org/10.1177/1524838015591572 .
Department of Veterans Affairs. National incident management system compliance: VHA Directive 0320.12(1): Administration VH. Washington, DC; 2021.
Veterans Health Administration. COVID-19 response plan: Management OoE; 2020.
US Department of Defense DoVA, Department of Health & Human Services. Interagency task force on military and veterans mental health; 2017. p. 1–31.
National Academies of Sciences E, and Medicine, Health and Medicine Division, Board on Health Care Services, Committee to Evaluate the Department of Veterans Affairs Mental Health Services. Evaluation of the Department of Veterans Affairs Mental Health Services: National Academies Press (US); 2018.
Subica AM, Aitaoto N, Link BG, Yamada AM, Henwood BF, Sullivan G. Mental health status, need, and unmet need for mental health services among U.S. Pacific islanders. Psychiatr Serv. 2019;70(7):578–85. https://doi.org/10.1176/appi.ps.201800455 .
Buettner K, Sablan J, Funk M, Arriola, J, Price, S, Sugiura, K, Diminic S, Drew N. WHO profile on mental health in development (WHO proMIND): Commonwealth of the Northern Mariana Islands. Geneva, World Health Organization; 2013. https://apps.who.int/iris/bitstream/handle/10665/85304/9789241505741_eng.pdf;jsessionid=A222F532F705877A650948706A437484 . Accessed 26 Mar 2021.
Mental health in the Asian Americans/Pacific Islander Community [ https://www.amsa.org/2020/09/04/mental-health-in-the-asian-americans-pacific-islander-community/#:~:text=Mental%20Health%20of%20Pacific%20Islanders&text=According%20to%20a%202019%20study%20for%20the%20general%20US%20population ].
Alessi EJ. Acknowledging the impact of social forces on sexual minority clients: introduction to the special issue on clinical practice with LGBTQ populations: Springer; 2013.
Veteran Population [ https://www.va.gov/vetdata/veteran_population.asp ].
Ussher JM. Heterocentric practices in health research and health care: implications for mental health and subjectivity of LGBTQ individuals. Fem Psychol. 2009;19(4):561–7. https://doi.org/10.1177/0959353509342933 .
LGBTQI [ https://www.nami.org/Your-Journey/Identity-and-Cultural-Dimensions/LGBTQI ].
Stults CB, Kupprat SA, Krause KD, Kapadia F, Halkitis PN. Perceptions of safety among LGBTQ people following the 2016 pulse nightclub shooting. Psychol Sex Orientat Gend Divers. 2017;4(3):251–6. https://doi.org/10.1037/sgd0000240 .
Lesbian, Gay, Bisexual and Transgender Veteran Care [ https://www.orlando.va.gov/services/lgbt/index.asp ].
National Academies of Sciences E, and Medicine. Evaluation of the Department of Veterans Affairs Mental Health Services: National Academies of Sciences E, and Medicine; 2018.
Download references
Acknowledgements
Not applicable.
This work was supported by the US Department of Veterans Affairs, Veterans Health Administration, Office of Emergency Management and the Office of Population Health. The views expressed in this presentation are those of the author and do not necessarily reflect the position or policy of the VA or the US government.
Author information
Authors and affiliations.
Department of Veterans Affairs, Veterans Emergency Management Evaluation Center (VEMEC), 16111 Plummer St. MS-152, North Hills, CA, 91343, USA
Tamar Wyte-Lake, Susan Schmitz & Aram Dobalian
Department of Family Medicine, Oregon Health & Science University, 3181 SW Sam Jackson Park Rd, Portland, OR, 97239, USA
Tamar Wyte-Lake
Orlando VA Medical Center, 13800 Veterans Way, Orlando, FL, 32728, USA
Reginald J. Kornegay
VA Southern Nevada Healthcare System, 6900 N. Pecos Road, North Las Vegas, NV, 89086, USA
Felix Acevedo
Division of Health Systems Management and Policy, University of Memphis School of Public Health, Memphis, TN, USA
Aram Dobalian
You can also search for this author in PubMed Google Scholar
Contributions
TWL and SS planned the study, including instrumentation, conducted the data analysis, and wrote the paper. RJK and FA supported the qualitative analysis and contributed to revising the paper. AD helped to plan the study and contributed to revising the manuscript. All authors have read and approved the manuscript.
Corresponding author
Correspondence to Tamar Wyte-Lake .
Ethics declarations
Ethics approval and consent to participate.
The Greater Los Angeles VA Healthcare System Institutional Review Board (Los Angeles, CA USA) approved this study. As the research presented no more than minimal risk of harm to subjects and involved no procedures for which written consent would be normally required outside of the research context, the study received a waiver for documentation of consent from the Institutional Review Board, and verbal, recorded audio consent was approved.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
2017 Disaster Qualitative Study: Collaboration Project Interview Guide. Interview guide utilized during project’s semi-structured interviews.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Wyte-Lake, T., Schmitz, S., Kornegay, R.J. et al. Three case studies of community behavioral health support from the US Department of Veterans Affairs after disasters. BMC Public Health 21 , 639 (2021). https://doi.org/10.1186/s12889-021-10650-x
Download citation
Received : 05 August 2020
Accepted : 18 March 2021
Published : 01 April 2021
DOI : https://doi.org/10.1186/s12889-021-10650-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Emergency preparedness
- Behavioral health; disaster response
- US Department of Veterans Affairs
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
It’s a New Era for Mental Health at Work
- Kelly Greenwood

Research on how the past 18 months have affected U.S. employees — and how companies should respond.
In 2019, employers were just starting to grasp the prevalence of mental health challenges at work, the need to address stigma, and the emerging link to diversity, equity, and inclusion (DEI). One silver lining amid all the disruption and trauma over the last two years is the normalization of these challenges. In a follow-up study of their 2019 Mental Health at Work Report, Mind Share Partners’ 2021 Mental Health at Work Report, the authors offer a rare comparison of the state of mental health, stigma, and work culture in U.S. workplaces before and during the pandemic. They also present a summary of what they learned and their recommendations for what employers need to do to support their employees’ mental health.
When we published our research on workplace mental health in October 2019, we never could have predicted how much our lives would soon be upended by the Covid-19 pandemic. Then the murders of George Floyd and other Black Americans by the police; the rise in violence against Asian Americans and Pacific Islanders (AAPIs); wildfires; political unrest; and other major stressors unfolded in quick succession, compounding the damage to our collective mental health.
- Kelly Greenwood is the Founder and CEO of Mind Share Partners , a national nonprofit changing the culture of workplace mental health so both employees and organizations can thrive. Through movement building , custom training, and strategic advising, it normalizes mental health challenges and promotes sustainable ways of working to create a mentally healthy workforce. Follow her on LinkedIn and subscribe to her monthly newsletter.
- Julia Anas is the chief people officer at Qualtrics, the world’s #1 Experience Management (XM) provider and creator of the XM category. At Qualtrics, she is responsible for building a talented and diverse organization and driving employee development as well as organizational design, talent, and succession planning.
Partner Center
- Specialisations
- Meet the team
- Wellness Program
- Join our talent pool
Posts by Tag
- contract engineering (16)
- contract solutions (10)
- Specialist Recruitment (8)
- technical resourcing (8)
- gig economy (7)
- Recruitment (5)
- job seeker (4)
- Insider (1)
- Resources (1)
The true impact of workplace wellbeing: two case studies
Embedded Expertise, Published: January 29, 2020 - Updated: August 22, 2022
Mental health concerns are a leading cause of workplace absence , and as we see increasing incidents of mental health-related sick days, workplace wellbeing is paramount for both organisational and individual success.
Below I’ve written two real-life stories where bettering the wellbeing of a workplace can have dramatic effects on the individuals and business profitability itself. Hopefully this will inspire you to incorporate a wellness approach into your organisation or team, or take more notice of your own mental health.
Case study one: Michael thought he was fine
Michael* realised he was arguing a lot with his family at home and was becoming increasingly more reactive to situations that probably didn’t warrant it. He wasn’t terribly great at conducting conversations or maintaining relationships with coworkers and this spilled outside of work. Body aches and excessive headaches had also started to culminate: all obvious signs of deep stress that Michael was ignoring.
The thing is, he thought he was actually doing really well and managing his stress levels appropriately and that his behaviour and experiences were quite normal.
But in fact, he was suffering extreme levels of stress . Something he didn’t even comprehend until he connected with a workplace wellbeing expert and he had the opportunity to observe his behaviours.
After one week of dedicated and concentrated awareness on how he was reacting and experiencing situations and noticing stress levels, triggers and emotions as they arose, he started to really notice a difference.
‘After one week of dedicated and concentrated awareness… he started to really notice a difference.’
To mitigate his stress levels and improve his workplace wellbeing and relations, Michael also engaged in visualisations (similar to what athletes do ), particularly with conversations, which creates different pathways in the brain . From here he started acting differently, having better discussions and decisions and was significantly calmer everywhere throughout his life, not just in the workplace.
Case study two: bad behaviour, great worker
Company owner, Rajiv, was experiencing some staff problems that he’d tried to handle but wasn’t seeing any changes. One of his contract managers, Tom, was displaying bad behaviour whenever things would go wrong.
The thing was, it was abundantly clear that what Tom was saying and the problems that he identified were absolutely correct. And the company valued his hard work and how exceptional he was at his job, so there was no desire to terminate his contract early. Which can often be a case for difficult situations in the workplace— many people are too eager to throw the ‘baby out with the bathwater’ so to speak, rather than experiment with some alternative ways of reaching conflict resolution. Or even taking the time to discover what is really going on, stepping away from the ego and its primal behaviour of flight or fight mode.
After supportive discussions with Tom, the wellness team discovered that actually he felt isolated , alone and that he didn’t belong. And, because the mind seeks to confirm our beliefs (through confirmation bias), would create situations and replicate behaviour to further consolidate that belief. He was very caught up in his story that he was an outsider.
A sense of belonging
To further compound this position, Tom was contracted as part of a large project and he felt like he didn’t fit in with the permanent employees, who had established themselves in the internal culture.
Forbes states that, ‘Employees who do not naturally fit into established corporate norms will often times try to assimilate to those norms – or put themselves “on guard” – in order to avoid potential biases or discrimination.’ This can take considerable effort and energy, which could be better spent on a person’s core duties.
A sense of belonging in the workplace contributes greatly to retention and attraction of high-quality candidates, which leads to better productivity, outcomes, creative solutions and more profit. It can also result in 75 per cent fewer sick days and avoid millions of dollars’ worth of lost productivity.
‘A sense of belonging in the workplace contributes greatly to retention and attraction of high quality candidates…’
Fostering this sense of belonging ‘in the workplace makes employees engaged and produce work that is elevated above the ordinary…’.
Once identified, the workplace wellbeing team worked with Tom and Rajiv with proven techniques that involved awareness, cultural changes and compassion and saw rapid improvement within weeks, thanks in part to the commitment of the people involved.
The change was so significant that Rajiv was enthusiastic and hungry to find more ways in which he could change the dynamics to bring out better and better results within his company. The company also extended Tom’s contract when the opportunity became available.

Welcome contract workers too
It can be really easy to forget that contract staff are an integral part of your team, even if they are only on staff for a limited time. And it shouldn’t be a last minute or token effort.
‘… there needs to be a culture and allowance for people to connect as human beings. We shouldn’t need bonding or team leadership days to actually connect with our colleagues and make meaningful relationships ,’ says Dr Michelle Lim, a loneliness researcher and senior lecturer in clinical psychology at Swinburne University.
Incorporating contract workers as genuinely part of the team and treating them as well as you treat all employees will only promote excellent benefits for the business and wider society as a whole and help contribute to preventing distressing issues such as high suicide rates in the engineering industry.
Can you relate in full or in part to these stories? Improve your wellbeing in your workplace today. Discover more about our for our contracting professionals.

*We’ve changed these names to provide privacy and protect the identity of these people.

Nukon is joint venture between the world of optimisation and automation. our parent company, SAGE Automation, is a leader in the operations market, while NUKON has fast established an outstanding reputation in the manufacturing data, intelligence andimprovement area.
This meeting of minds means we can now bridge the gaps between the different silos within our client businesses, bringing visibility, unity and breakthrough improvements right across our clients' businesses.
One Column Text
Enjoyed this post don't forget to share..

Embedded Expertise is a specialist consultancy that matches high calibre technical expertise with the agile clients who need them - fast.
Phone: 1300 050 557 Contact us
SAGE GROUP BRANDS
- SAGE Automation
- Embedded Expertise
QUICK LINKS
- Subscribe to our Newsletter
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
A Multiple Case Study of Mental Health Interventions in Middle Income Countries: Considering the Science of Delivery
Contributed equally to this work with: Sean A. Kidd, Athena Madan, Susmitha Rallabandi, Kwame McKenzie
* E-mail: [email protected]
Affiliations Department of Psychiatry, University of Toronto, Toronto, Ontario, Canada, Toronto Centre for Addiction and Mental Health Toronto, Ontario, Canada
Affiliation Toronto Centre for Addiction and Mental Health Toronto, Ontario, Canada
¶ ‡ These authors also contributed equally to this work.
Affiliation Dalla Lana School of Public Health, University of Toronto, Toronto, Ontario, Canada
Affiliation Ashoka Canada,Toronto, Ontario, Canada
Affiliation BasicNeeds,Bangalore, India
Affiliation Ashoka, Washington D. C., United States of America
- Sean A. Kidd,
- Athena Madan,
- Susmitha Rallabandi,
- Donald C. Cole,
- Elisha Muskat,
- Shoba Raja,
- David Wiljer,
- David Aylward,
- Kwame McKenzie

- Published: March 24, 2016
- https://doi.org/10.1371/journal.pone.0152083
- Reader Comments
In the debate in global mental health about the most effective models for developing and scaling interventions, there have been calls for the development of a more robust literature regarding the "non-specific", science of delivery aspects of interventions that are locally, contextually, and culturally relevant. This study describes a rigorous, exploratory, qualitative examination of the key, non-specific intervention strategies of a diverse group of five internationally-recognized organizations addressing mental illness in middle income countries (MICs). A triangulated approach to inquiry was used with semi-structured interviews conducted with service recipients, service providers and leaders, and key community partners (N = 159). The interview focus was upon processes of implementation and operation. A grounded theory-informed analysis revealed cross cutting themes of: a holistic conceptualization of mental health problems, an intensive application of principles of leverage and creating the social, cultural, and policy “space” within which interventions could be applied and resourced. These findings aligned with key aspects of systems dynamic theory suggesting that it might be a helpful framework in future studies of mental health service implementation in MICs.
Citation: Kidd SA, Madan A, Rallabandi S, Cole DC, Muskat E, Raja S, et al. (2016) A Multiple Case Study of Mental Health Interventions in Middle Income Countries: Considering the Science of Delivery. PLoS ONE 11(3): e0152083. https://doi.org/10.1371/journal.pone.0152083
Editor: Chun-Hsi Huang, University of Connecticut, UNITED STATES
Received: November 19, 2015; Accepted: March 7, 2016; Published: March 24, 2016
Copyright: © 2016 Kidd et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the paper and its Supporting Information files.
Funding: This work was supported by Grand Challenges Canada under grant #0326-04. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: Elisha Muskat and David Aylward were both employees of Ashoka at the time of the study and Shoba Raja was an employee of BasicNeeds at the time of the study. This does not alter the authors' adherence to PLOS ONE policies on sharing data and materials.
Introduction
In a concerted effort to address the large and growing burden of mental illness in low and middle income settings (LMICs), the field of global mental health (GMH) is increasingly focussed upon the application and scaling up of evidence based interventions, with an emphasis upon task shifting [ 1 ]. Considerable controversy attends this emphasis upon standardization and scaling, with randomized trials as the gold standard of evidence [ 2 ]. There is a concern that Western, biomedical conceptualizations of mental illness and treatment can pathologize the individual and that the focus should be on the social determinants of illness. The critique goes further to note that this emphasis does not address non-technical/specific aspects of intervention and important local, contextual and cultural factors. The dialectic in this debate suggests that the greatest impact and ethical rigour in GMH requires a balanced consideration of the benefits of scaled, evidence-based approaches, particularly for severe mental illness while at the same time carefully attending to importance social determinant, cultural and contextual processes [ 2 ].
This debate may partly grow out of an imbalance in the base of evidence. Specifically, a considerable amount of evidence is available regarding assessment tools and protocols for an array of brief interventions for mental illnesses in LMICs [ 3 ]. Such approaches readily lend themselves to conventional clinical research designs. Far less information is available regarding what are variably referred to as the non-technical or non-specific intervention and service process-oriented factors that many would argue are essential to generating substantive impact [ 4 ]. In the broader healthcare arena this has been referred to as the "science of delivery"[ 5 ]. The problem that arises is that the more circumscribed, trial-amenable interventions cannot succeed without attention to the quality of the service processes and contexts in which they are implemented [ 6 ].
Social entrepreneurship is one lens that is available for understanding what will henceforth be referred to as "non-specific" factors such as models of leadership, partnership, and context-relevant conceptualizations of mental illness and intervention [ 7 , 8 ]. Social entrepreneurs have been characterized as change agents who utilize highly flexible approaches to solving social problems that allow them to effectively bridge gaps between multiple sectors and systems [ 9 – 11 ].
Cultivated to a large extent by organizations such as Ashoka [ 12 ] and the Skoll Foundation [ 13 ], social entrepreneurship has emerged as a prominent way of thinking about how complex problems, social and otherwise, are addressed. Health has been regularly connected with social entrepreneurship, with a recent review of 366 case studies finding that health was the primary target in 18% of the cases [ 14 ]. Social entrepreneurship in mental health specifically has had less attention despite its relevance in addressing the complexity of mental illness in under-resourced contexts [ 7 ].
This paper describes a rigorous examination of the key, non-specific or delivery system intervention strategies of a group of internationally recognized organizations addressing mental illness in middle income countries (MICs)—all of which have been identified as leading examples of social entrepreneurship. It is intended to inform the conversation about balance in considering how interventions are best developed and scaled in under-resourced contexts. It is among the first to apply a rigorous research design in this less well-defined domain of service delivery—studying the organization and service delivery models through which interventions are optimally deployed.
Case Identification
This study employed an instrumental, multiple case study design, one in which case study findings are used to inform the understanding of a specific broader issue [ 15 ]. The organizations that were studied were founded by Ashoka Fellows. Ashoka is the organization that is arguably the most prominent, internationally, in employing a social entrepreneurship lens to identify some of the most promising individuals and organizations that address social problems [ 12 ]. While Ashoka’s network by no means represents all social entrepreneurs, it is known for its accuracy in identifying highly effective social entrepreneurial approaches. It uses an intensive Delphi method [ 16 ] to identify potential Fellows and applies a rigorous selection process with a panel review that attends to key domains of social entrepreneurship, impact, and scale or potential for scaling. The Ashoka website at the time of inquiry described the work of 2,663 Fellows and their organizations from over 70 countries. The Fellows working in mental health were identified through (i) a keyword search of the online Ashoka directory using the terms: “mental health”, “mental illness”, “psychiatric”, “addiction”, and “developmental”; and (ii) cross-referencing the list with Ashoka staff familiar with the Fellows working in health to determine if any had been missed. This two-part process revealed 42 Fellows. Detailed descriptions of all 42 Fellows were reviewed by (Cole, Kidd, McKenzie, and Wiljer) at the level of their Ashoka profiles with further inquiry through websites, publications, and with Ashoka staff (e.g., to ensure the organization is still active). A maximum variation sampling strategy was used to identify 5 Fellows and their organizations with which to engage in intensive case studies. Target problem (type of mental health concern), intervention type/approach (service model; scale and reach), target population (by age, rural/urban, socioeconomic status), and geographic location (sociopolitical context past and current; culture) were key dimensions considered in achieving adequate variation, which was an important consideration given the intent to identify broadly applicable themes.
Given the depth of inquiry it was anticipated that 5 case studies would prove adequate to inform the service implementation and process questions that are the focus of this study and to reach saturation in the analysis [ 17 ]. The study was reviewed and approved by the Toronto Centre for Addiction and Mental Health Research Ethics Board. The protocol was also reviewed and approved by the executive leadership and research leads (individuals responsible for research within the organization, ethics review and approval) of each of the participating organizations. None of the organizations approached refused participation and the five that participated were the five originally selected.
Data Collection
Contextual information regarding organization operations and settings were collected through documentation review including websites and annual reports. This review also assisted with tailoring the plan of inquiry for the specific organizations. The primary source of data was semi-structured interviewing with past and present service/organization leadership anddirect service staff with service recipients and key partners (often less aware of implementation and process details) acting as secondary, triangulating sources of information. Key partners included policy makers who had been regular contacts and practitioners associated with partner organizations as identified by case study organization leadership. Service recipients were approached upon the recommendation of staff who assisted with addressing questions of capacity and minimizing intrusiveness in service settings. Leaders and staff had been informed of the intent to connect with stakeholders ranging in degree of supportiveness of their work. Nonetheless, it is possible that some bias might have attended this method of recruitment. The study also included ethnographic observation of activities of the organization (e.g., non-clinical meetings of staff and clients (e.g., in community activities, common spaces), presentations to the public, advocacy activities, etc.) with observations recorded in field notes. The ethnographic component occurred primarily during tours of organization activities by staff as well as interviewers spending time in common spaces. Interviewers were introduced as researchers attempting to develop an understanding about how a given organization worked. Multiple interviews were undertaken with service leaders and their staff, providing opportunities to ask follow up questions as the inquiry and data analysis progressed. Interviews with other stakeholders took place on a single occasion. Interviews were audio-recorded and transcribed verbatim, with translation services used on an as-needed basis, and took place between May, 2014 and March, 2015. Written consent was obtained for interviews with service leaders, staff, and key partners. Verbal consent was obtained from service recipients due to literacy difficulties in the study contexts, and was documented by noting the name, date, and location in which consent was secured. No service recipient was included for whom there was any question of capacity or any other consideration that might affect their understanding of their involvement. Interviews with service recipients were designed to be minimally intrusive, focusing on perceptions about what had been helpful or less helpful in their service experience over time. This verbal consent procedure was approved by the Research Ethics Board. Interviews were conducted by postdoctoral fellows (Madan and Rallabandi) who had no prior relationships or conflicting interests with the organizations of focus.
Specific areas of inquiry included a detailed history tracking the trajectories and turning points in services offered, service structures/models, goals and values, implementation, leveraging support, and relationships with stakeholders and supporters (See S1 Appendix for interview protocols). We undertook an examination of the specific aims and activities of the people involved in the service. Implicit to this line of investigation was a close study of the “theories of action” of the participants–their understanding of how their activities lead to the outcomes that they are seeking to attain. Also examined were their relationships within relevant systems (service, corporate, government, cultural norms)–how they are positioned, how initiatives are achieved or blocked, and the flow of information, people, and resources into and out of the organization from these systems. This attention to the ‘circumstances’, structures, processes, and contexts of the interventions has been previously highlighted as essential in such case studies [ 18 ].
Data Analysis
Following Stake’s model for multiple case study analysis [ 19 ], we analyzed transcripts and field notes using a thematic analysis informed by grounded theory (i.e., employing constant comparison, exploring connections between themes to inform a more theoretical formulation) [ 20 ]. The analysis moved from line-by-line open coding, to the refinement of codes and the development of an overarching thematic framework. Data collection and analysis proceeded simultaneously, allowing for opportunities to refine structure of the findings through increasingly targeted inquiry.
Several steps were taken to maximize rigor in the analysis and to establish the credibility and trustworthiness of the findings. First, there was a very rich set of data in multiple forms that allows for triangulation by source (staff, leaders, partners, observation) and type (field notes, verbal description). Second, participants were engaged in discussion about the emerging categories to support trustworthiness in the analysis. Third, a method of employing multiple coders was undertaken to develop the thematic framework with multiple rounds of review (by Kidd, Madan, and Rallabandi), negotiation of different perspectives, and revision.
Results and Discussion
Participating organizations and individuals.
The five organizations selected for study were BasicNeeds and its sites in Vietnam, and Ghana [ 21 ], the Acid Survivor's Foundation in Bangladesh [ 22 ], the Banyan in Chennai, India [ 23 ], ADVANCE in Egypt [ 24 ], and the Fundacion Colectivo Aqui y Ahora in Colombia [ 25 ] Table 1 . All of these organizations have mental health as a focus (though have a holistic approach that considers physical health, social and cultural domains) and operate where such supports had previously been extremely limited or completely lacking. BasicNeeds is among the largest and most extensively scaled comprehensive interventions to address mental illness globally—with 12 sites and over 600,000 beneficiaries to date. In Ghana and Vietnam, BasicNeeds operates out of several sites, both rural and urban, targeting impoverished people with mental illness. The Acid Survivors Foundation, which is based in Dhaka but has a national reach, provides a diverse set of services from plastic surgery to psychosocial rehabilitation for Bangladeshi people who have survived acid violence. The Banyan provides an intensive array of services for homeless individuals with severe mental illness with the core services studied located in Chennai. ADVANCE in Egypt provides specialized services for children and adolescents with autism spectrum disorders to support improved social integration. ADVANCE operates a stand along education and support centre and provides a range of outreach supports in close connection with schools and parent groups. The Fundacion Colectivo Aqui y Ahora in Colombia addresses youth addictions through a methodology focused upon personal meaning with engagement at family, school, workplace, and public levels. It has a standalone clinic and has outreach activities taking place at a national level in the range of settings noted above. Further details regarding the operations of each of these organizations and the Ashoka Fellows associated with them can be found at the referenced websites or at www.ashoka.org .
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0152083.t001
The total number of individual participants interviewed was 159 with a mean of 31.8 interviews per organization across the 5 case studies. Broken down by type, this included 93 service/organization staff and leadership, 46 community collaborators and members with a range of connections with the organization, 22 individual service recipients and 7 self-help groups with memberships of up to 30 people (for interview details see Table 2 ). These distinctions are somewhat artificial, as in these organizations there are many examples of service recipients becoming staff. Variability in interview and participant times were accounted for by a number of factors including opportunity with respect to time and travel, availability of participants, and sensitivity with respect to some groups of potential participants (e.g., children with autism). Interviews ranged in length from 15 minutes in a single contact (typically community members and recipients) to over 6 hours over multiple contacts (typically with service leaders and staff). Overall, the interview content was rich though in some instances it appeared that histories of conflict and other sociopolitical factors may have influenced the depth of inquiry (e.g., fears of discussing or criticizing systemic barriers in contexts where such talk in the past or present could lead to severe reprisal).
https://doi.org/10.1371/journal.pone.0152083.t002
Overview: Leverage and Space in Which to Work
Despite the considerable diversity across the specific operations and contexts of these organizations, a saturated and coherent theme structure readily emerged in the data analysis. The two cross-cutting thematic elements were leverage and the generation of resources (e.g., social capital) to support the development, capacity, and scaling of the interventions. Here, leverage could be considered the effort to maximize the outputs of every available resource, while applying pressure to aspects of the given complex problem in a manner that results in the maximum amount of change. Concurrently, these organizations ambitiously and persistently created space in which to work—with space being considered the cultivating of public, political, social and cultural resources around the problem. This provided social and fiscal capital and systems in which bureaucracy and policy enabled rather than hindered efforts. These core themes and their subthemes are described in detail below along with full quotes and excerpts that are representative of the data from which they were derived.
Understanding people , treating people equally , being non-judgmental , being down to earth , open minded , balanced between the rational and emotional , a strategic thinker , a good communicator , trustworthy , setting examples by doing things , team building , team spirit , mobilizing people and resources . (Past Executive Director)
This quote concisely encompasses most of the elements that participants considered important in the leadership of these organizations. They were described as individuals with a specific set of skills and values. They are intimately familiar with and intensely, personally invested in the cultures and contexts in which they work.
"Initially , though they were the founders , they didn’t mind doing anything . They have cleaned the bathrooms , they mopped the floors , and they used to cook in the kitchen , they used to clean and wash the clients , they themselves went for rescues , they themselves used to serve food . They have done the maximum from the beginning . They have done so many things from the ground level and that made them to grow higher and earn so much of manpower through the services that they have rendered to the clients ." Direct service staff person
Whether directly affected by mental illness in their families or through a very intensive study of the issues involved through "sitting with, living with" and "supping with" clients, families and communities, this empathetic approach had numerous implications. It was described as leading to an extremely deep understanding of the problem that needs to be addressed, the contexts and dynamics associated with it, and an intense engagement with and knowledge about the relevant stakeholders. This base of knowledge fed into, without exception, an understanding that effective interventions need to be individualized, staged, and multifaceted to address the many interacting needs of clients, families and communities. Furthermore, in the complex systems that surround the mental health problem that they sought to address, such a depth of knowledge and engagement allowed them to better recognize opportunities, resources, and points of leverage.
“So , as parents we got together and we had parents support meeting and we decided that what our children need is beyond what a center can do , we need a total NGO , we need life span services , we need awareness , we need advocacy , we need a lot of other things that’s not there . We also need to train personnel , because the personnel who existed knew maybe about disability but were not specific in their knowledge about autism and sensory issues and so on .” Executive Director and Founder
This depth of understanding was complemented by skill as educators and communicators who "cultivate trust" and "respect" in aligning diverse stakeholders around a clear vision of the problem and its solution–whether person with mental illness, rural villager, senior policy maker or influential public figure. This knowledge and skill in engaging and aligning had clear implications for the core theme of creating space in which to work as access and support across sectors requires this type of alignment.
Leverage, in the form of maximizing everyone’s potential contribution, was evident in their ability to "diagnose the efficiency and hidden talent" of clients, volunteers, and staff. All described working in low-hierarchy environments where everyone was encouraged to explore and extend the limits of their capabilities. In commentary about process over time, while the launch of these endeavours were typically framed as a "passionate outburst" in addressing a human rights issue, over time strategy became much more of an emphasis. For example, one core strategy was to innovate and expand through experimentation ("low cost, low risk experiments") while skillfully advancing large and complex organizations, carefully assessing points of leverage, timing, and maintaining fidelity to the intervention and its values.
Livelihoods
Attention to livelihoods was a pivotal part of this understanding of client needs across interventions. It was discussed as a leveraged part of the mental illness problem for two reasons—one is that mental health interventions are much less effective without attention to livelihoods. Treating mental illness is "secondary to survival", and people fear the costs, financial and otherwise, of engaging in treatment.
“I was 22 years old and had mental illness and nobody understood what was wrong with me and it shamed my parents , I was unmarriageable and a burden to their house .” Service Recipient
Conversely, attending to livelihoods had many advantages—ranging from the direct benefits of being more active to addressing stigma. Working unlocks sources of support from family and communities and through contact with community reduces isolation and social stigma—demonstrating that people with mental illness can contribute and creating opportunities to improve impacts and expand.
“We saw her progress . And that she could do this [broommaking] . It was satisfying seeing her return to find a useful purpose . So she is not forgotten in society . She makes brooms and with that , has money and earnings so that she can buy what she needs to eat . She can go out and participate in community , at pagoda . She is participating in meetings with her brooms—this helps relieve stress and deal with thoughts and be part of community life . The illness is managed/decreased and gradually her health is better .” Family Member
Empowerment
These interventions were described as fundamentally empowering—this is true for staff and volunteers as described above but emphasized to an even greater extent with respect to service recipients. As with the themes above this had clear implications for leverage in interventions and enhancing reach. The use of the term empowerment by the participants in these case studies was very well aligned with the definition of prominent consumer-survivor advocate Dr. Pat Deegan who described a taking back of power "to become sovereign over our own lives and bodies, to reclaim our right to make choices and have access to resources to improve the quality of our lives."([ 26 ], p.11) Grounded in empathetic and rights-oriented approaches, these organizations described very actively seeking out and cultivating the "inner strength" of clients.
"These survivors at the beginning were completely hopeless and helpless … they were not even thinking about surviving . They were thinking about committing suicide . So when the survivors found that someone is understanding them , treating them as real human being , respecting them , respecting their values and their thoughts and helping them to express themselves … that actually helped them more and more . So , when [acid violence survivor] started to talk with other survivors who were receiving treatment in Dhaka medical college hospital , in that way , drop by drop they were also growing ." Service Staff Member
Many benefits of an empowering approach were described. These included the exposure of communities to empowered people with mental illness, which reduced stigma and increased expectations for what they might accomplish in life. This empowering approach also benefited an array of advocacy and fundraising activities—not in the form of narratives of people being "used" to raise funds, but of organizations creating spaces where people could realize their full potential and make a difference.
“ This aspect of their work , the empowerment piece , was described by our participants as one of the most rewarding . It energized , inspired , and is "the heart of the work ." Direct Service Staff Member
Another thread involved the quality and availability of services. Peer support, developed in these contexts of empowerment, was very actively utilized as a leveraged strategy. It was clear in the narratives of peers, those receiving peer support, and staff, that the employment of peers further cultivated messages of hope and empowerment. Peers worked in ways fundamentally grounded in lived experience knowledge about mental illness, along with a deep knowledge of relevant community resources and local cultures. Peers were described as essential to expanding the reach and impact of these organizations.
… ‘We feel this work is better done by us because it is we who are sick and should therefore support each other… Village mobilisers are more familiar with the participants in their community , have a vested interest in the project , have experience of treatment and are aware of the benefits of the project to participants’ lives .” Peer Provider

Directly Engaging and Involving Key Stakeholders
Along with the more obvious financial capital necessary to operate, the participants spent a considerable amount of time discussing how the problem needs to become seen as important and social capital needs to grow around it.
“We formed different advisory groups , the legal advisory group , the prevention advisory group and these people , the experts were helping us in developing strategies and mobilizing resources not just financial but also other resources and in that way , gradually we are making a public opinion against acid violence . I should say that one event which was a kicking point is like in 2002 on International women’s day , we organized men’s rally . That was organized in collaboration with BRAC and the daily newspaper . In the year 2000 they established a forum to help acid survivors . They were also mobilizing resources . In this Men’s March , over 5000 men participated and hundreds of female survivors were leading that March and media , national and international has publicized that issue . So , that created a huge movement in the country .” Organization Senior Staff
These organizations had cultivated relationships with a range of media outlets and created compelling stories about their work and the problems that they were addressing. Along with creating attention and interest among the general public, most were active in the engagement of key stakeholders whether through a media lens (e.g., supportive celebrity advocates) or with others who have influence. This extended as well into the realm of formal education—offering for free highly regarded trainings to government ministries, lawyers, police, and judiciaries on relevant issues and offering helpful practical advice and assistance. This work was further leveraged, through partnerships with and the involvement of lawyers, with the effort to strike down policies that posed barriers and enact helpful policy. Indeed, this active engagement of government was described by some leaders as essential to sustainability and scaling—even a prerequisite to partnership despite the time it can take to develop and the problem of policies being developed but not implemented in practice.
Branding was another key part of these conversations about creating space in which to work. The brand of the organization was established in several ways. They described cultivating an ethos, a set of values, and a distinctly innovative approach that operates in contexts where there would otherwise be little or no service. Respect was garnered through this way of working, as well as through the generation of impacts for large numbers of people who previously might have been considered hopeless by policy makers and the public.
“We’re a very prominent part of the global mental health community . And we have a place there . It’s not a cakewalk—sometimes I get ignored around the table but we are starting to turn that around . People see us as a competent , collaborative presence that is considered an attractive partner to collaborate with .” Organization Senior Staff
Branding was also enhanced through connections from local to global levels with other prominent organizations, and by becoming well-known for their provision of high quality education opportunities to a range of sectors (e.g., government, other service providers, police). The benefits of cultivating such a brand had many advantages, including its feeding into more effective advocacy through access to public and policy forums, improved fundraising ability, and attracting and retaining skilled staff.
Participants also described facing the challenge that, unless they are able to successfully educate, raise awareness, and engage communities and families at a 'grass roots' level, interventions would not be accessed. As one community partner put the problem: "When I go to people's houses, they will let me come in, but I always hear ‘Come in for tea, okay. but don't do that stupid screening, we are fine." It was clear that "knowledge of the population" was crucial to turning this problem around—understanding how to engage diverse communities who may be facing poverty and have low educational backgrounds. This required persistence, but also an understanding of what is important to people—such as the enhancement of the livelihoods. Similar to the ways of engaging clients, the key theme of collaboration and respect were important here as well.
"Strangely , we have faced the least challenges at the community level , particularly the rural communities have been very receptive and I think they are intelligent people … They are receptive because they are intelligent and they know the difference between somebody who is attempting to work with them and genuinely make a difference versus somebody who is exploiting them , somebody who is talking down or condescending . We learn a lot based on what the community tells us , we develop our services . So , some expertise we have , some expertise the community has . So , it is collaborative in that sense and I think they recognize that ." Organization leader
Building collaborations with communities and families was not always described as reaching out—learning from and engaging communities and supporting clients in community based activities and advocacy. A big part of this effort involved inviting people in . This took place in a range of ways.
"We cover five arrays in youth club . It is education , sports , culture , dance and vocation [programming available to the local community who join clients in these activities] . So , in education , we have free tuition classes , spoken English classes and then , in sports we cover indoor and outdoor . Outdoor is cricket , soccer , tennis , volley ball and things like that and indoor carom , chess , running and catching . It’s all simple . This is open for all . So , in indoor games , a lot of boys from youth club come and play with our own men [clients] . They play chess , they play carom and volley ball within our complex . They [local boys] also take our men to the beach and play soccer casually . They wouldn’t have a match but they would just play so that they get to interact also . [Through this approach] we are simultaneously [decreasing] stigma and we are also getting the men [clients] to engage with the community and also community developing in its own way . Staff Member
This inviting of communities in was another leveraged strategy. It was described as reducing stigma, educating the community about the work of the organization and opening doors in a way that helps staff better understand what the community needs, and raises awareness—and by proxy assists with fundraising and volunteerism. This is essential even at the most basic levels–communities came to understand that mental illness is something that the organization can help within a culturally and context relevant way. This was highlighted in the frame of prevention with some noting that too often "people will not come" into treatment or engage supports when prevention might still be possible.
"Here we make four events—art expression , sports day , a conference and a round table seminar … we invite other societies to share in this , to exhibit art , to join us in our events ." Direct Service Staff Member
Finally, there was a strong commitment to volunteers and volunteer development in these organizations. This was highlighted as essential in contexts where financial support was very limited. The purposeful blurring of boundaries between community and the organization was enhanced by volunteers—people who often had histories of helping communities and who by association enhanced the credibility of the organization.
"If the government will not be able to provide these services in the future , we need to provide for our own community to help with problems at a community level . We were invested in improving our communities before this role [with current organization] . We always have been ." Volunteer
Furthermore, volunteers were engaged in the organization culture—the culture of respect "equal say" and growth for everyone involved—again maximizing people's potential contributions.
"I came here to volunteer actually . It wasn’t a decision to study and start work in a very structured way . So , I decided to work like as in art therapy before working with children which was logical as I studied art , so , I can teach them art with children with disability . That’s how it began but as I started work , I found out that I am kind of talented in this field . I know how to deal with them . I love them and all now , the supervisors told me that you can work in this field and you can start to study and just let it be your career . That’s how I started . So , I started to read and to have courses and of course to have training in the organization and now , I have just finished my Master’s in the field . That’s brief of how I started to work in this field ." Direct Service Staff Member and Former Volunteer
Partnership and Scaling
Two other subthemes, framed largely in interviews as being both a part of the process and as outcomes of leveraged ways of working were partnerships and scaling. Partnerships (developed after careful assessment to ensure the proper alignment of values and complementary activities) were emphasized as necessary to the provision of comprehensive services (e.g., plastic surgery for acid violence survivors), leveraging capacity (e.g., mindfulness meditation in Buddhist temples as an acceptable and accessible intervention), and in maintaining identity and focus (e.g., referring people with intellectual disabilities to a partner organization in that specific sector). Close partnership was essential to the scaling activities of all of these organizations—identifying collaborators who had the capacity to successfully implement and sustain the given intervention with fidelity.
More directly, the topic of scaling was very much on the minds of the leaders of these organizations though there was a considerable amount of variability as to the extent to which it had been undertaken.
“Our strategy in scaling up is we set models , we study them , we fine tune them , we develop protocols , then we impact policy and through policy and advocacy , projects are scaled up . So , much of our models or aspects of our models have been incorporated into the mental health policy and urban health mission . That’s one part of scaling up .” Founder
In the context of scaling, the leveraged intervention was described as one that had been intensively examined and tested to identify the basic model—one that might be considered that of a set of " minimum specifications " or core approaches that are effective yet can be adapted to other settings.
“Why do you think the model is so successful ? It’s completely integrated , and flexible according to the local needs . There is no need for rigidity—it suits customs , culture , and universally applicable . It’s been proved in so many different countries . It aids with treatment , sustains livelihoods , and builds capacity . Sustainability is at the core of all its actions .” Senior Staff Person
Leverage and creating space or capacity were further evident in discussions about how scaling is best accomplished and, most critically, the infrastructure needed to effectively support it. As mentioned previously, some of this had to do with the selection of optimal partners and contexts for scaling. Other prominent topics here included a careful assessment of the resources needed to keep the expanded intervention connected and continuously assess fidelity and impact. As this work progressed the focus increasingly was upon "stabilizing" the resulting "alliance of organizations" through a network that supports continued growth, ensuring quality, and keeping people connected.
“We think , the upcoming year we will also form almost 10–15 new groups for survivors . Within a year we will try to organize district level survivor conference where they show their problems , where they interact with government bodies and local authorities . We will give them a platform . That is a two day activity . That will create a district level network and we are trying to train them on basic leadership and fundamental leadership . When they get it , we will form formal network structure at district level and by 2 or 3 years , we have a plan to organize national level conference with all survivors groups , with district committees , with national committees , with the Public Prosecutor and Police . There , they will discuss their problems at national level and all that meetings will be facilitated by survivors .” Staff Member
Points of Divergence and Limited Coverage
As noted previously, there was a great deal of similarity across the case study narratives with a focus upon non-specific aspects of developing and delivering interventions. The differences that did emerge across case studies were primarily ones of emphasis. For example, participants from some organizations spent more time discussing scaling strategies than others. There was some diversity in emphasis with respect to the role of government. While all discussed the importance of engaging government there were differences with respect to what was needed. This ranged from a need for a general approval of operations through to collaboration on policy changes that were key to the effectiveness of the intervention. Further, there were some differences in what was being leveraged from existing community resources. This again ranged from a reduction in barriers such as stigma to points of synergy in intervention (e.g., mindfulness meditation in monasteries). Finally, while inquired about, more detailed and nuanced information about the use of formal research and technology did not emerge beyond a general commentary about utility.
This multiple case study has focussed upon examining the non-specific aspects of internationally-recognized interventions addressing mental illness in MICs through a social entrepreneurship lens. In the past 30 years social entrepreneurship has become an important concept in understanding how to identify and support individuals and organizations that are effective in addressing social problems [ 9 – 11 ]. It grew to a large extent from the need to identify and cultivate sustainable, contextually established and relevant interventions/approaches that have large impacts [ 10 ]. While less commonly employed in the global mental health literature [ 7 ], it is relevant in that it is a framework that focusses on the consideration of how successful approaches to mental health-related problems are developed and applied (i.e., non-specific components).
Herein lies an opportunity to bring the focus to the science of delivery [ 5 ]—the structures (people, resources, and organizations) within which specific, evidence based interventions might best be applied. These structures are complex and are well-addressed through qualitative methods, particularly in this early stage of knowledge generation. Accordingly, this study employed one of the most rigorous research inquiries in this area to date [ 7 ] and focussed upon organizations and people recognized as socially entrepreneurial through Ashoka’s intensive selection and award process [ 10 ].
A coherent model emerged in this study that included interventions underway in multiple MICs. Cutting across a number of themes describing ways of working in mental health were the two themes of leverage and creating space in which to work. It is understandable that these two particular themes arose in this study as the most prominent. Mental illness in most MICs is characterized by severe resource and infrastructure limitations and intense stigma from individual to structural levels. In such settings, and considering the complex nature of mental illness, leverage is necessary to maximize the impact of limited resources—through both obtaining a maximal output of resources and applying them to points in the complex system of mental illness where the least pressure supplies the greatest change. A leveraged approach, however, must be matched by systems and settings that can accommodate it. Effectiveness cannot be achieved if the problem is not seen as important, the service offered is not seen as relevant, and stigmatizing beliefs and policies limit actions and opportunities.
Underlying these themes of leverage and creating space to work were several subthemes. These included leaders who have developed a very deep and nuanced understanding of the mental health problem that they are addressing and the systems within which it occurs. They also are extremely capable in engaging and aligning diverse stakeholders and assessing and maximizing the potential contributions of strategic collaborations, staff, volunteers, community, and service recipients. Key points of leverage in this context included attention to livelihoods through approaches such as social enterprise and the many benefits that attend the empowerment of recipients in a manner that reflects key aspects of recovery-oriented care [ 27 ]. Complementing leverage, creating space in which to work was an effort that involved establishing and marketing a “brand” that is their organization, values, and way of working. This aligned with the key aspects of successful brands highlighted in marketing literatures. Namely that successful brands are distinct (applied in a way and place where other options are not available), are relevant and important, are esteemed by customers and fulfills their promise, is understood and familiar, and is innovative and dynamic to suit changing needs and conditions [ 28 ]. Branding, in these case studies, was greatly enhanced through connections from local to global levels with other prominent organizations and being recognized for the provision of high quality education to a range of sectors (e.g., government, legal system). In synergy with brand development was an intensive effort to generate social capital through strategic partnerships, engagement of the media and influential public figures, engagement of government, and embeddedness in communities.
All of these activities created systems in which a common language for the problem was cultivated, its importance agreed upon, and their organization positioned as having the solution. This was closely attended by efforts to reduce stigma and create policy-enabling environments. This set of subthemes attended both local and scaled initiatives, though the latter involved greater attention to the careful assessment of sites that could successfully support scaling and the infrastructure necessary to develop and sustain scaled operations [ 1 ]. Contributing to the evidence behind social entrepreneurship as a coherent framework, these themes overlap with those of another multiple case study of seven leading organizations operating in impoverished and marginalized contexts, none of which had mental health as a focus [ 29 ]. The areas of overlap included local capacity building that mobilizes existing resources, with an emphasis upon their being “systemic learning” organizations in which continuous cycles of education and contribution by staff and clients is central, and extending impact through alliances.
While helpful in some respects, the lens of social entrepreneurship is problematic due to its breadth and lack of specificity [ 30 ]. Similar to the problems that attend defining “recovery-oriented care”, it encompasses many domains and activities and applies to both individual and group endeavours and characteristics. Perhaps a better way to capture the work of the social entrepreneurs studied here, and the non-specific aspects of their work that are crucial to effectiveness and scaling up, is through a systems dynamic framework. This is highly relevant to the wicked problem nature of mental illness in low resource settings, in which the problem is typically poorly identified, changing, has no definitive solution nor a clear set of possible solutions, is a cause of other problems and a symptom of other problems, and can be explained in numerous ways [ 31 ].
Systems dynamics theory is largely present other fields (e.g., economics) though is increasingly being applied in areas such as public health and sustainable development [ 32 ]. It is premised upon the need to consider wicked or otherwise complex and dynamic problems in holistic, non-linear ways [ 33 ]. It is highly relevant to GMH in that the debate about specific versus non-specific aspects of intervention [ 2 ] is at least to some extent a debate about perceptions of a linear “project” approach being applied rather than a sustained system behaviour framework. Similar to the findings of the present study, system dynamic approaches emphasize the importance of finding leverage points in complex systems where small shifts can produce large amounts of change [ 33 – 35 ]. The participants in this study, whether systematically and/or intuitively, had located important points of leverage and were pushing them in the right direction. Less well-recognized is the premise that leverage in complex systems must often be matched by an “essential complementary activity” just as subsidized low income housing needs to be matched with job creation to achieve the desired impacts [ 33 , 36 ]. In the present study, this was the observation that leveraged approaches were matched by a range of complementary activities designed to create space to operate and build social capital that enables the intervention. This proposition supports the conclusion of Kirmayer and Pederson [ 2 ] that a balanced approach to inquiry and practice of this type will likely have the greatest overall impact in the lives of those suffering from mental illness in low and middle income countries. This work would involve an improved articulation and means of measuring non-specific aspects of intervention within which the more circumscribed and trialed interventions are optimized. Indeed, this is a line of inquiry already in development as models for effective community engagement and social inclusion are being examined as core non-specific aspects of scaled mental health initiatives [ 37 , 38 ]. The findings of the present study contribute to this emerging area of inquiry and implementation science that attends it, albeit with a somewhat broader frame (e.g., consideration of leadership characteristics, engagement with, and conceptualization of the problems faced; facets of social capital generation such as branding).
This study had a number of limitations. These included questions of representativeness beyond the organizations studied, a limited ability to comment upon how certain activities were directly causal of observed benefit, and a lack of an ability to compare these exceptionally successful interventions with those less successful. Considerations of component impact might be complex and require further study. For example, while some approaches to address livelihoods such as social enterprise have been associated with improve mental health and quality of life [ 39 ] and BasicNeeds and its livelihoods emphasis has demonstrated benefit [ 40 ], other models such as microfinance might negatively impact mental health [ 41 ]. Another limitation of the present study was that selection bias in participant recruitment might have been a factor as it is not possible to assess the degree to which past staff, key partner, and service recipient groups were fully representative. Future work, allowing for more fulsome comparison of more and less successful organizations aided through a random recruitment strategy would help to address these shortcomings, though the voluntary consent required by organizations to open themselves up to research scrutiny may always results in some volunteer bias. Also informative would be the examination of how these approaches might best be propagated through sharing information and mentorship—with propagation considering formal scaling, local growth, and sustainability through successorship as founders retire. Lastly, the scope of the interviews limited the ability to examine how specific interventions (e.g., supplying psychotropic medications) might interact with the non-specific elements highlighted in the study.
Conclusions
In sum, this paper suggests the benefit of using social entrepreneurship as a framework for identifying successful efforts and the possible benefit of applying a systems dynamic lens to problems in GMH. It further suggests the potential benefit of matching the evidence base of circumscribed, specific interventions [ 3 ] with an equally rigorous inquiry into the non-specific factors without which those specific interventions cannot be successfully implemented nor sustained. Such work would assist in a stronger ability to identify and support promising organizations and leaders in the field and allow for the testing of methods for enhancing non-specific resources and strategies. This could lead to fewer failed endeavours and improved effectiveness and scaling of interventions. Indeed, as difficult to define as it is, social entrepreneurship in such a program of work provides a framework for considering how these very similar efforts at social capital generation might become better aligned to generate collective impact [ 42 ]. For additional quotes underlying the themes described in this paper please see S2 Appendix .
Supporting Information
S1 appendix. interview protocols..
https://doi.org/10.1371/journal.pone.0152083.s001
S2 Appendix. Thematic Data from which Study Quotes were Selected.
https://doi.org/10.1371/journal.pone.0152083.s002
Acknowledgments
This work was supported by Grand Challenges Canada under grant #0326–04. There are no competing interests related to this work for any of the authors. Appreciation is extended to Ashoka Global and Ashoka Canada.
Author Contributions
Conceived and designed the experiments: SK DC EM SR DW DA KM. Performed the experiments: SK AM SR EM. Analyzed the data: SK AM SR DC EM SR DW KM. Wrote the paper: SK AM SR DC SR DW KM.
- View Article
- PubMed/NCBI
- Google Scholar
- 3. World Health Organization. mhGAP intervention guide for mental, neurological and substance use disorders in non-specialized health settings.[Online].2010. Available: http://www.thehealthwell.info/node/69810 . Accessed 27 August 2015.
- 6. Wampold B. (2010). The research evidence for the common factors models: A historically situated perspective. In Duncan B, Miller S. Wampold B, Hubble M,(eds) The heart and soul of change: Delivering what works in therapy (2nd ed.). Washington, DC: American Psychological Association.
- 10. Bornstein D. How to change the world: Social entrepreneurs and the power of new ideas. New York: Oxford University Press, 2007.
- 12. Available: www.ashoka.org .
- 13. Available: www.skollfoundation.org .
- 15. Stake R. The Art of Case Study Research. Thousand Oaks: Sage, 1995.
- 17. Ritchie J, Lewis J, Elam G. Designing and selecting samples. In: Ritchie J, Lewis J (eds.), Qualitative research practice. A guide for social science students and researchers. Thousand Oaks, CA: Sage, 2003.
- 18. Pawson R. Evidence-Based Policy. Los Angeles, CA: Sage, 2006.
- 19. Stake RE. Multiple case study analysis. New York: Guilford, 2013.
- 20. Charmaz K. Constructing grounded theory. Thousand Oaks, CA: Sage, 2014.
- 21. Available: www.basicneeds.org .
- 22. Available: www.acidsurvivors.org .
- 23. Available: www.thebanyan.org .
- 24. Available: www.advance-society.org .
- 25. Available: www.colectivoaquiyahora.org/ .
- 27. Slade M. 100 ways to support recovery: a guide for mental health professionals. London: Rethink, 2009.
- 36. Forrester J. Urban Dynamics. Portland, OR: Productivity Press, 1969.

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
Part 2 Lucy’s Story
2.4 Lucy case study 3: Mental illness diagnosis
Nicole Graham
Introduction to case study

Lucy has experienced the symptoms of mental illness during her lifespan; however, it was not until her early twenties that she was formally diagnosed with bipolar affective disorder. In the case study below, we explore the symptomology that Lucy experienced in the lead up to and post diagnosis. Lucy needs to consider her mental illness in relation to her work as a Registered Nurse and as she continues to move through the various stages of adulthood.
Learning Objectives
By the end of this case study, you should be able to:
- Identify and consider the symptoms of mental illness.
- Develop an understanding of contributing biopsychosocial stressors that may exacerbate the symptoms of mental illness as experienced by Lucy.
- Critically analyse the professional, ethical, and legal requirements and considerations for a registered health professional living with chronic illness.
Lucy’s small group of friends describe her as energetic and ‘a party person’. Although she sometimes disappears from her social group for periods of time, her friends are not aware that Lucy experiences periods of intense depression. At times Lucy cannot find the energy to get out of bed or even get dressed, sometimes for extended periods. As she gets older, these feelings and moods, as she describes them, get more intense. She loves feeling high on life. This is when she has an abundance of energy, is not worried about what people think of her and often does not need to sleep. These are the times when she feels she can achieve her goals. One of these times is when she decides to become a nurse. She excels at university, loves the intensity of study, practice and the party lifestyle. Emergency Nursing is her calling. The fast pace, the quick turnaround matches her endless energy. The fact that she struggles to stay focused for extended periods of time is something she needs to consider in her nursing career, to ensure it does not impact negatively on her care.
Unfortunately, Lucy has experienced challenges in her career. For example, her manager often comments on her mental illness after she had openly disclosed her diagnosis. It is challenging for her to hear her colleagues speak badly about a person who presents with mental illness. The stigma she hears directed at others challenges her. She is also very aware that it could be her presenting to the Emergency Department when she is unwell and in need of further support. Lucy is constantly worried that her colleagues will read her medical chart and think she is unsafe to practice.
While the symptoms that cause significant distress and disruption to her life began in her late teens, they intensified after she commenced antidepressant medication after the loss of her child. She subsequently ceased taking them due to side effects. These medications particularly impact on her ability to be creative and reduce her libido and energy. By the time she turns 18, she notices more frequent, intense mood swings, often accompanied by intense feelings of anxiety. During her high periods, Lucy enjoys the energy, the feeling of euphoria, the increased desire to exercise, her engagement with people, and being impulsive and creative. Lucas appreciates her increased libido. However, during these periods of high mood, Lucy also has impaired boundaries and is often flirtatious in her behaviour towards both friends and people she doesn’t know. She also increases her spending and has limited sleep. Lucas is often frustrated by this behaviour, leading to fights. On occasion Lucas slaps her and gets into fights with the people she is flirting with. These periods can last days and sometimes weeks, always followed by depressive episodes.
When she is in the low phases of her mood, Lucy experiences an overwhelming sense of hopelessness and emptiness. She is unable to find the energy to get out of bed, shower or take interest in simple daily activities. Lucas gets frustrated and dismisses Lucy’s statements of wanting to end her life as ‘attention seeking’. Lucy often expresses the desire to leave this world when she feels this way. When Lucas seeks support from the local general practitioner, nothing really gets resolved. The GP prescribes the medication; Lucy regains her desire to participate in life; then stops the medication due to side effects which extend to gastrointestinal upsets, on top of the decrease in libido and not feeling like herself. When Lucy is referred to a psychologist, she does not engage for more than one session, saying that she doesn’t like the person and feels they judge her lifestyle. When the psychologist attempts to explore a family history of mental illness, Lucy says no- one in her family has it and dismisses the concept.
The intense ups and downs are briefly interrupted with periods of lower intensity. During these times, Lucy feels worried about various aspects of her life and finds it challenging to let go of her anxious thoughts. There are times when Lucy has symptoms like racing heart, gastrointestinal update and shortness of breath. She spends a great deal of time wanting her life to be better. Her desire to move on from Lucas and to start a new life becomes more intense. Lucy is confident this is not a symptom of depression; it is just that she is unhappy in her relationship. Lucy starts to consider career options, feeling that not working affects her lifestyle, freedom and health. As she explores different options on the internet, Lucy comes across a chat room. Using the chat name ‘Foxy Lady 20’, she develops new friendships. She finds herself talking a lot with a man named Lincoln who lives on the Gold Coast.

After a brief but intense period talking with Lincoln online, Lucy abruptly decides to leave Lucas and her life in Bundaberg to move in with Lincoln. Lincoln, aged 26, 5 years older than Lucy, owns a modest home on the Gold Coast and has stable employment at the local casino. Their relationship progresses quickly and within a month Lincoln has proposed to Lucy. They plan to marry within 12 months.
Lucy is now happy with her life and feels stable. She decides to pursue a degree in nursing at the local university. Lucy enrols and makes many new friends, enjoying the intensity of study and a new social scene. Her fiancé Lincoln also enjoys the social aspects of their relationship. During university examination periods, Lucy experiences strong emotions. At the suggestion of an academic she respects, she makes an appointment with the university counselling service. After the first 3 appointments, Lucy self-discovers, with the support of her counsellor, that she might benefit from a specialist consultation with a psychiatrist. She comes to recognise that her symptoms are not within the normal range experienced by her peers. Lincoln is incredibly supportive and attends the appointments with Lucy, extending on the information she provides. Lucy reveals information about her grandmother, who was considered eccentric, and known for her periods of elevated mood and manic behaviour. The treating psychiatrist suggests Lucy may be living with bipolar affective disorder and encourages her to trial the medication lithium.
Lucy does not enjoy the side effects of decreased energy, nausea and feeling dazed and ceases taking the lithium during the university break period. This causes Lucy to again experience an intense elevation of her mood, accompanied by risk-taking behaviours. Lucy goes out frequently, nightclubbing and being flirtatious with her friends. She becomes aggressive towards a woman who confronts Lucy about her behaviour with her boyfriend in the nightclub. This is the first time Lucy exhibits this type of response, along with very pressured speech, pacing and an inability to calm herself. The police are called. They recommend Lucy gets assessed at the hospital after hearing from Lincoln that she has ceased her medication. Lucy is admitted for a brief period in the acute mental health ward. After stabilising and recommencing lithium, Lucy returns to the care of her psychiatrist in the community. The discharge notes report that Lucy had been previously diagnosed with bipolar disorder, may also be experiencing anxiety related symptoms, and have personality vulnerabilities.
Lucy is in the final year of her university studies when she has a professional experience placement in the emergency ward. Lucy really enjoys the fast pace, as well as the variety of complex presentations. Lucy feels it matches her energy and her desire for frequent change. After she completes her studies, Lucy applies and is successful in obtaining a position at the local hospital. Throughout her initial graduate year, Lucy balances life with a diagnosis of mental illness as well as a program of her own self-care. She finds the roster patterns in particular incredibly challenging and again becomes unwell. She goes through a period of depression and is unable to work. During this period, Lucy experiences an overwhelming sense of hopelessness and considers ending her life. Again, she requires a higher level of engagement from her treating team. Lucy agrees she is not fit to work during this time and has a period of leave without pay to recover. She has disclosed to her manager that she has been diagnosed with a mental illness and later discusses how shift work impacts her sleep and her overall mental wellbeing.
Over time, Lucy develops strategies to maintain wellness. However, she describes her relationship with the Nursing Unit Manager as strained, due to her inability to work night shift as her medical certificate shows. Lucy says she is often reminded of the impact that her set roster has on her colleagues. Lucy also feels unheard and dismissed when she raises workplace concerns, as her manager attributes her feelings to her mental health deteriorating. Lucy has a further period when her mental health deteriorates. However, this time it is due to a change in her medication.
As Lucy and Lincoln have a desire to have a child, Lucy was advised that she cease lithium in favour of lamotrigine, to reduce the risk of harm to the baby. Lucy ceases work during the period when her mental health deteriorates during the initial phase of changing medication. Lucy recommences lithium after she ceases breastfeeding their son at 4 months, with good effect and returns to work.
Case study questions
- Consider the symptoms that Lucy experiences and indicate whether they align with the suggested diagnosis.
- Identify the biopsychosocial contributing factors that could impact mental health and wellness.
- Review and identify the professional disclosure requirements of a Registered Nurse who lives with mental illness in your local area.
- Identify self-care strategies that Lucy or yourself as a health professional could implement to support mental health and wellbeing.
Thinking point
Sometimes people do not agree with a diagnosis of mental illness, which can be incorrectly labelled as ‘denial’ by health professionals. It is possible that the person is unable to perceive or be aware of their illness. This inability of insight is termed anosognosia (Amador, 2023). The cause of anosognosia in simple terms can be due to a non-functioning or impaired part of the frontal lobe of the brain, which may be caused by schizophrenia, bipolar disorder or other diseases such as dementia (Kirsch et al., 2021).
As healthcare workers will likely care for someone who is experiencing anosognosia, it is important to reflect on how you may work with someone who does not have the level of insight you would have hoped. Below is a roleplay activity whereby you can experience what it might be like to communicate with someone experiencing anosognosia. Reflect on your communication skills and identify strategies you could use to improve your therapeutic engagement.
Role play activity – Caring for a person who is experiencing anosognosia
Learning objectives.
- Demonstrate therapeutic engagement with someone who is experiencing mental illness
- Identify effective communication skills
- Reflect on challenges and identify professional learning needs
Resources required
- Suitable location to act out scene.
- One additional person to play the role of service user.
Two people assume role of either service user or clinician. If time permits, switch roles and repeat.
- Lucy has been commenced on lithium carbonate ER for treatment of her bipolar disorder.
- Lucy is attending the health care facility every week, as per the treating psychiatrist’s requests.
- The clinician’s role is to monitor whether Lucy is experiencing any side effects.
Role 1 – Clinician
- Clinician assumes role of health care worker in a health care setting of choice.
- Lucy has presented and your role is to ask Lucy whether she is experiencing any side effects and whether she has noticed any improvements in her mental state.
Role 2 – Lucy who lives with bipolar
- Lucy responds that she does not understand the need for the tablets. She also denies having a mental illness. Lucy says she will do what she is told, but does not think there is anything wrong with her. Lucy thinks she is just an energetic person who at times gets sad, which she describes as ‘perfectly normal.’ Lucy is not experiencing any negative side effects, but says she would like clarification about why the doctor has prescribed this medication.
Post role play debrief
Reflect and discuss your experiences, both as Lucy and as the clinician. Identify and discuss what was effective and what were the challenges.
Identify professional development opportunities and develop a learning plan to achieve your goals.
Additional resources that might be helpful
- Australian Prescriber: Lithium therapy and its interactions
- LEAP Institute: The impact of anosognosia and noncompliance (video)
Key information and links to other resources
Fisher (2022) suggests there are large numbers of health professionals who live with mental illness and recognise the practice value that comes with lived experience. However, the author also notes that as stigma is rife within the health care environment, disclosing mental illness can trigger an enhanced surveillance of the health professional’s practice or impede professional relationships (Fisher, 2022).
It is evident that the case studies derived from Lucy’s life story are complex and holistic care is essential. The biopsychosocial model was first conceptualised in 1977 by George Engel, who suggests it is not only a person’s medical condition, but also psychological and social factors that influence health and wellbeing (Engel,2012).
Below are examples of what you as a health professional could consider in each domain.
- Biological: Age, gender, physical health conditions, drug effects, genetic vulnerabilities
- Psychological: Emotions, thoughts, behaviours, coping skills, values
- Social: Living situation, social environment, work, relationships, finances, education
Developing skills through engaging in reflective practice and professional development is essential. Each person is unique, which requires you as the professional to adapt to their particular circumstances. The resources below can help you develop understanding of both regulatory requirements and the diagnosis Lucy is living with.
Organisations providing information relevant to this case study
- Rethink Mental Illness: Bipolar disorder
- Australian Health Practitioner Regulation Agency (AHPRA): Resources – helping you understand mandatory notifications
- Australian Health Practitioner Regulation Agency (AHPRA): Podcast – Mental health of nurses, midwives and the people they care for
- Black Dog Institute: TEN – The essential network for health professionals
- Borderline Personality Disorder Community
- National Institute of Mental Health (NIMH): Anxiety disorders
Case study 3 summary
In this case study, Lucy’s symptoms of mental illness emerge in her teenage years. Lucy describes periods of intense mood, both elevated and depressed, as well as potential anxiety-related responses. It is not until she develops a therapeutic relationship with a university school-based counsellor that she realises it might be beneficial to engage the services of a psychiatrist. After she is diagnosed with bipolar affective disorder she engages in treatment. Lucy shares her experience of both inpatient and community treatment as well as her professional practice requirements in the context of her mental illness.
Amador, X. (2023). Denial of anosognosia in schizophrenia. Schizophrenia Research , 252 , 242–243. https://doi.org/10.1016/j.schres.2023.01.009
Engel, G. (2012). The need for a new medical model: A challenge for biomedicine. Psychodynamic Psychiatry, 40 (3), 377–396. https://doi.org/10.1521/pdps.2012.40.3.377
Fisher, J. (2023). Who am I? The identity crisis of mental health professionals living with mental illness. Journal of Psychiatric and Mental Health Nursing . Advance online publication. https://doi.org/10.1111/jpm.12930
Kirsch, L. P., Mathys, C., Papadaki, C., Talelli, P., Friston, K., Moro, V., & Fotopoulou, A. (2021). Updating beliefs beyond the here-and-now: The counter-factual self in anosognosia for hemiplegia. Brain Communications , 3 (2), Article fcab098. https://doi.org/10.1093/braincomms/fcab098
Case Studies for Health, Research and Practice in Australia and New Zealand Copyright © 2023 by Nicole Graham is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License , except where otherwise noted.
Share This Book
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
May 1, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
Trial by YouTube: Prejudicial views of mental health labels formed following trial of Johnny Depp and Amber Heard
by University of Surrey

Viewing expert testimony during the court case of Amber Heard and Johnny Depp led to highly prejudicial views of the mental health difficulties of both parties being formed, a new study by students at the University of Surrey reveals. The findings, published in the journal BJPsych Bulletin , suggest these views were considerably more negative than their views about mental illness beforehand.
The 2022 trial was live-streamed globally on YouTube and was viewed more than 1 billion times, making it the most-watched trial in history.
Dr. Oliver Mason, Reader in Psychology at the University of Surrey, said, "This court case is perhaps one of the most memorable of the last decade, with two A-list Hollywood celebrities battling it out for victory.
"Their legal teams sought to undermine both their testimonies with terms such as Borderline and Histrionic Personality Disorder (Heard), Paranoia and Substance Use Disorder (Depp), effectively weaponizing each other's mental health difficulties.
"Given the widespread consumption of this online content, we wanted to assess its impact on perceptions of the reported mental health of Heard and Depp, and of mental health issues in general."
The research team surveyed 38 participants about their attitudes to mental illness both before and after viewing video coverage of expert witness testimony concerning either Heard or Depp.
Participants were then asked to complete the Prejudice Towards People with a Mental Illness (PPMI) scale—a well-known measure that assesses people's feelings of fear/avoidance, authoritarianism, malevolence, and unpredictability towards mental illness.
Participants viewed the trial footage, which was focused on the testimony of mental health experts. The Prejudice towards People with a Mental Illness scale was then repeated concerning Heard or Depp. Researchers identified a statistically marked increase in stigmatizing attitudes towards the mental illness of both Heard and Depp after viewing footage of the trial, which were more negative than participants' previously held views.
Dr. Mason added, "The unmediated availability online of video in which mental health labels were used by experts to discredit testimony, tarnish reputation, and undermine the credibility of both parties is highly concerning.
"Our evidence suggests that this may lead to stigmatizing and prejudicial opinions of the mental health of both parties being formed. It raises the question of whether expert testimony regarding mental health should be widely available in this way for public consumption. There is the clear danger when this happens that prejudicial views of mental health in general are formed."
Explore further
Feedback to editors

Under 4-minute milers' longevity shows that extreme exercise doesn't seem to curb lifespan
7 hours ago

Study shows how night shift work can raise risk of diabetes, obesity
9 hours ago

'Smart' contact lenses could someday enable wireless glaucoma detection
10 hours ago

Low-cost MRI paired with AI produces high-quality results

Navy Growler jet noise over Washington state's Whidbey Island could impact 74,000 people's health
11 hours ago

Human brain map contains never-before-seen details of structure

What makes a public health campaign successful?

High school student helps transform 'crazy idea' into a model that can predict neurotransmitters
12 hours ago

Collaboration uncovers an entirely new COVID-related syndrome

Q&A: Study details how major advances have been implemented in intensive diabetes management
13 hours ago
Related Stories

Stigmatizing content on social media affects perceptions of mental health care, study reveals
Nov 30, 2023

Most homeless Americans are battling mental illness
Apr 17, 2024

Physical ills often plague people with schizophrenia, bipolar
Apr 23, 2024

International Criminal Court judges 'cautious' about using impact of mental health
Nov 27, 2023

Young Britons increasingly face mental illness: study
Feb 26, 2024

Study: Personalized care needed for mental illness and physical health conditions
Apr 4, 2023
Recommended for you

New AI tool uses a small set of interpretable variables to rapidly assess self-harm risk
20 hours ago

Sleep problems as a child may be associated with psychosis in young adults
May 8, 2024

How our knowledge of artists influences our perception of their works

How infections influence our social empathy

Health risks of using cannabis are higher in adolescents than in adults, study finds

More than 321,000 US children lost a parent to drug overdose from 2011 to 2021: Study
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter

Mental Health Awareness Month: After-school program provides sanctuary for teens

Missouri high school freshman Alastor Reynolds said the mental health of his peers is "very not OK."
"I know multiple people and have multiple friends that are struggling right now," he said. "And they just can’t really get the help they need."
But Tyler's House KC in Kansas City, Missouri, is working to make a difference. Alastor said it is a place where he feels safe and feels like he belongs.
The teen wants to inform the surrounding community of the positive impact such places have on teen mental health.
“I mean, high school is a lot,” Alastor said. “There’s a lot of work, there’s a lot of drama, there’s a lot of new things going on.”
When there was no school to keep him busy, he started spending time at Tyler's House.
“I kind of realized it’s so fun here," Alastor said. "Sometimes I'd have a really stressful day and need to relax."

Mental Health
America's Breakdown: Confronting Our Mental Health Crisis (VIDEO)
During his relaxation, he's surrounded by others like Cori Hastings, a former teacher who founded Tyler's House.
“I used to work at a local high school here and was just noticing a lot of students falling through the cracks,” Hastings said. “There was just not enough time to really target the needs of the students.”
The National Alliance on Mental Illness (NAMI) surveyed teens about their mental health , and only half of them said they believe mental health is important to their school.
“We’re just trying to reach them however we need to, with the overall thing being all of this is connection, belonging, and it supports our mental health,” Hastings said.
High schoolers are welcome at Tyler's House on weekdays after school. They can be part of volunteer-led activities or just be in a space where they feel seen and heard.
“It’s a very welcoming environment. I’m very comfortable here," Alastor said. "Not just because I've been here a lot but because the people here, students and volunteers, are easy to talk to, and you can just relate to them with so many other things."

Generation Z finds its voice in conversations about mental health
Alastor said he wishes schools had safe spaces like this. NAMI reported that 2 in 3 teens agree schools should teach what mental health is and how to find treatment.
Scripps News Kansas City's Olivia Acree asked Alastor what he'd do without Tyler's House.
“I don’t really know what I'd do, honestly,” he said.
He encourages teens who feel the same way to stop by.
“If you’re in high school, come to Tyler's House. We would love to have you,” Alastor said.
Most Recent

Judge denies Hunter Biden appeal to dismiss firearms case

New Mexico authorities say Meta is not doing enough to combat child predators

Apple's new iPad ad strikes a chord with creatives. Now the company is apologizing

FDA recalls diabetes care app after glitches resulted in injuries to 224 users

Warnings issued on morel mushroom consumption as foraging season arrives

Number of children losing a parent to drug overdoses surges, study finds

Watch Scripps News
- Research article
- Open access
- Published: 07 May 2024
Floods and cause-specific mortality in the UK: a nested case-control study
- Danijela Gasevic 1 ,
- Zhengyu Yang 1 ,
- Guowei Zhou 2 ,
- Yan Zhang 2 ,
- Jiangning Song 3 ,
- Hong Liu 2 na1 ,
- Shanshan Li 2 na1 &
- Yuming Guo ORCID: orcid.org/0000-0002-1766-6592 2 na1
BMC Medicine volume 22 , Article number: 188 ( 2024 ) Cite this article
13 Accesses
4 Altmetric
Metrics details
Floods are the most frequent weather-related disaster, causing significant health impacts worldwide. Limited studies have examined the long-term consequences of flooding exposure.
Flood data were retrieved from the Dartmouth Flood Observatory and linked with health data from 499,487 UK Biobank participants. To calculate the annual cumulative flooding exposure, we multiplied the duration and severity of each flood event and then summed these values for each year. We conducted a nested case-control analysis to evaluate the long-term effect of flooding exposure on all-cause and cause-specific mortality. Each case was matched with eight controls. Flooding exposure was modelled using a distributed lag non-linear model to capture its nonlinear and lagged effects.
The risk of all-cause mortality increased by 6.7% (odds ratio (OR): 1.067, 95% confidence interval (CI): 1.063–1.071) for every unit increase in flood index after confounders had been controlled for. The mortality risk from neurological and mental diseases was negligible in the current year, but strongest in the lag years 3 and 4. By contrast, the risk of mortality from suicide was the strongest in the current year (OR: 1.018, 95% CI: 1.008–1.028), and attenuated to lag year 5. Participants with higher levels of education and household income had a higher estimated risk of death from most causes whereas the risk of suicide-related mortality was higher among participants who were obese, had lower household income, engaged in less physical activity, were non-moderate alcohol consumers, and those living in more deprived areas.
Conclusions
Long-term exposure to floods is associated with an increased risk of mortality. The health consequences of flooding exposure would vary across different periods after the event, with different profiles of vulnerable populations identified for different causes of death. These findings contribute to a better understanding of the long-term impacts of flooding exposure.
Peer Review reports
Floods are the most frequent type of weather-related disaster, accounting for about 47% of all weather-related disasters from 1995 to 2015 [ 1 , 2 ]. Between 1995 and 2015, more than 2.3 billion people were affected by flood disasters, with over 157 thousand people dying directly as a result of floods [ 3 ]. In recent years, many intense urban flooding events have been recorded in the UK, resulting in loss of lives, damages to personal property and public health infrastructure, and disruption to vital services such as water, communications, energy, and public transport [ 4 , 5 , 6 , 7 , 8 , 9 ]. Approximately 1.9 million people across the UK are at risk of floods, and this number will double as early as the 2050s [ 10 ].
In addition to immediate fatalities due to drowning and acute trauma [ 11 ], floods can also cause short- (lasting days or weeks) or medium-health impacts (several weeks or months), including the spread of water- and vector-borne diseases, such as cholera, typhoid, or malaria; injuries during evacuations and disaster clean-up; and exposure to chemical hazards [ 1 , 12 ]. Non-communicable diseases (e.g. cardiovascular disease, neoplasms, chronic respiratory diseases, and diabetes) which need prolonged treatment and care can be exacerbated after floods due to a disruption in care, treatment, medication, supplies, equipment, and overcrowding in shelters [ 13 , 14 , 15 , 16 , 17 , 18 ]. Mental health issues may arise from stressors caused by floods (e.g. property damage, financial loss, loss of a loved one) and have long-lasting health effects on mortality and morbidity. These long-term health consequences may arise from several pathways, including impairment of the immune system, sleep disturbances, substance abuse, and inadequate self-care [ 19 , 20 , 21 , 22 ].
Despite the severe impacts of floods, there currently is limited epidemiological evidence on the long-term mortality impacts of exposure to floods. To address these gaps in knowledge, we utilized the UK Biobank project, a population-based study with a large sample size, to explore the long-term effects of flooding on mortality. We aimed to estimate the risk of all-cause and seven cause-specific mortality associated with floods and to explore the lag patterns in mortality risk. We also conducted subgroup analyses to identify populations who are potentially more vulnerable to flood-related death.
Study design and study population
We conducted a nested case-control study within a cohort of participants registered with the UK Biobank study. About 0.5 million residents aged between 37 and 73 years were enrolled in the UK Biobank from 2006 to 2010, from 21 assessment centres across England, Wales, and Scotland. The cohort was followed up until the date of death or the study end date (December 31, 2020). We excluded participants lacking longitude and latitude data of residence ( n = 11), participants with missing data on age, sex, and ethnicity ( n = 2775), and those who died in the year of recruitment ( n = 141). A total of 499,487 participants were included (Fig 1 ). All participants in the UK Biobank study provided informed consent. The utilization of the data presented in this paper has been approved by the UK Biobank access committee under UK Biobank application number 55257.
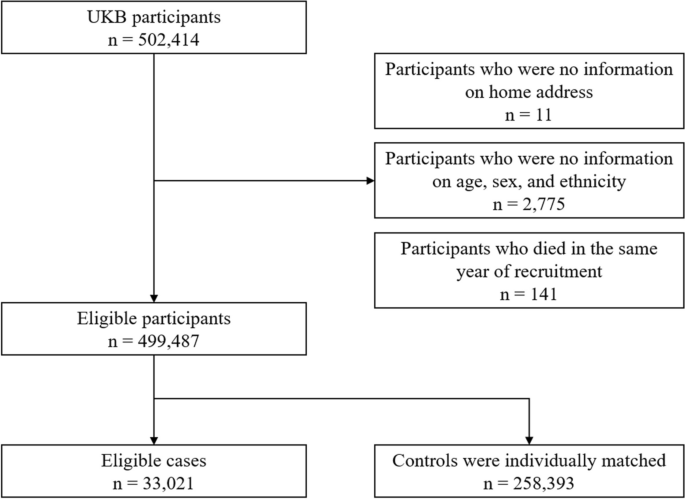
A flow diagram to show participants whose data were used to estimate the association between flooding exposure and mortality
Case-control selection
With the nested case-control design, we matched controls to cases with replacement at the time of the outcome event and assessed exposure retrospectively, from the date of death or end of follow-up. This ensures identical exposure lengths across participants. Using a risk-set sampling method, each case was matched with eight controls randomly selected from study participants who met the matching criteria for age (within 5 years), sex (male and female), and ethnicity (White, Black, Asian or Asian British, mixed, Chinese, and others). The index date for cases corresponded to the date of death; while for controls, it was the date of death of the matched case participant. For twelve case-control sets, eligible controls were less than eight but at least one (Fig 1 ).
Participants were eligible for inclusion as cases for the study if they died during the study period. We defined all-cause mortality and seven cause-specific mortality categories using the International Classification of Diseases, edition 10 (ICD-10), classification as follows: neoplasms, C00–D48; cardiovascular disease, I00–I99; respiratory diseases, J09–J98; digestive disease, K20–K93; neurodegenerative disease, F01–03, G122, G20, G21, G23, G30, G31; mental and behavioural disorders: F00–F90; and suicide: X60–X84, Y10–Y34, Y87.
Flooding exposure
We collected flood data during 2000–2020 from the Dartmouth Flood Observatory (DFO), which is a global catalogue of all flood events with detailed information on start date, end date, centroids, impacted geographic areas, and severities. All documented flood events were sourced from news, government, and instrumental sources and have been validated by satellite observations [ 23 , 24 ]. Participants whose home addresses fall within flood-affected areas were considered as having been exposed to a flood event. To assess the long-term effect of floods, we calculated a cumulative exposure during the study period for each participant. Building on previous research [ 25 , 26 ], we derived the annual cumulative exposure by multiplying the duration and severity of each flood event and summing these values for each year. Our preliminary analyses suggested a weak negative association between flood severity and duration (Pearson coefficient: − 0.03). The severity of each flood event documented in the DFO was classified based on a pre-defined scale, detailed in Additional file 1 : Table S1. For each participant, annual cumulative flooding exposure was calculated using equation ( 1 ):
where \(\mathrm{Flood}\;{\mathrm{index}}_{i,\text{year}=m}\) stands for the cumulative flooding exposure in year \(m\) for participants \(i\) . \({{\text{Duration}}}_{ij}\) and \({{\text{Severity}}}_{ij}\) represent the duration (day) and the severity of the \(j\) th flood event that participant \(i\) experienced in year \(m\) , respectively. If there were no flood events within a given year, a flood index of 0 was recorded.
Meteorological data
We extracted hourly temperature and relative humidity data from the European Centre for Medium-Range Weather Forecasts Reanalysis v5 (ERA-5) reanalysis data set with a spatial resolution of 0.1°×0.1°. We mapped meteorological data to the participant’s geocoded residential address at baseline. Daily meteorological data were calculated by averaging hourly data within each day. Daily temperature and relative humidity were then aggregated into yearly averages.
Baseline data collected by the UK Biobank include demographics, lifestyle factors, socioeconomic status, and anthropometric measurements. We included additional covariates informed by existing literature, beyond those used for matching cases and controls [ 27 , 28 , 29 ]: body mass index (BMI), physical activity, healthy diet score, cigarette smoking, alcohol consumption, educational attainment, average total annual household income before tax, Townsend deprivation index (TDI), overall health rating, and assessment centres. BMI was calculated from objectively measured weight and height as weight over height squared and expressed as kg/m 2 . Physical activity was derived from the International Physical Activity Questionnaire-Short Form (IPAQ-SF) [ 30 ]. Participants were categorized at ‘high’ (≥ 1500 metabolic equivalent (MET)-minutes/week), ‘moderate’ (≥ 600 MET-minutes/week), or ‘low’ levels of physical activity following standardized IPAQ-SF scoring guidance [ 30 ]. Diet score was calculated based on the following dietary factors: vegetable intake ≥ 3 servings/day; fruit intake ≥ 3 servings /day; whole grains ≥ 3 servings/day; refined grains ≤ 1.5 servings/day; fish intake ≥ 2 servings/day; unprocessed red meat intake ≤ 2 servings/week; and processed meat intake ≤ 2 servings/week. Each point was given for each favourable dietary factor, and the suboptimal diet was defined as a diet score < 4. Smoking status was coded into three categories: current, former, and never. Low-risk alcohol consumption was defined as moderate drinking (no more than one drink/day for women and two drinks/day for men; one drink is measured as 8 g ethanol in the UK) on a relatively regular frequency [ 31 ]. Educational attainment was coded in two categories: ‘high’ (college or university degree) or ‘low’ (A/AS levels or equivalent, O levels/GCSEs or equivalent, or none of the above). Annual household income was classified into two groups (< £31,000 and ≥ £31,000). TDI was utilized to define area deprivation level, with participants being classified as either high (TDI above the median) or low [ 32 ]. Self-reported health was categorized as poor, fair, good, and excellent [ 27 ].
Statistical analysis
We performed conditional logistic regression analysis to estimate the risk of mortality associated with per unit increase in flood index. Year-specific flood index was modelled using a distributed lag non-linear model featuring a non-linear exposure-response association and the additional lag-response association, respectively [ 33 , 34 , 35 , 36 ]. The lag-response association refers to how the risk changes over time and provides an estimation of the combined immediate and delayed effects that accumulate throughout the lag period. We first modelled the exposure-response curve with a natural cubic spline with three degrees of freedom. However, the nonlinear analysis indicated an approximately linear relationship (Additional file 1 : Fig. S1). Further, both the Akaike Information Criterion (AIC) and the Bayesian Information Criterion (BIC) favoured the linear model (Additional file 1 : Table S2). Therefore, we applied a linear exposure-response relationship in the formal analysis. The lag-response curve was modelled with a natural cubic spline with three degrees of freedom plus an intercept. The exposure window comprised the 0 to 5 years before the index date. A maximum lag of 5 years was used because the flood-related mortality risk declined to zero by the lag year 5.
Estimates of risk were obtained from the crude model that only included flood (model 1); the multivariate model that additionally controlled for socioeconomic status (education attainment, household income, and deprivation) (model 2); and the full model that additionally adjusted for BMI, physical activity, smoking, alcohol consumption, suboptimal diet, overall health rating, mean temperature, mean relative humidity, and assessment centre which serves as an indicator of the recruitment location for each participant (model 3). All variance inflator factors were less than 1.5, indicating no multicollinearity. Temperature and relative humidity terms were defined as the average annual mean temperature and relative humidity over 6 years (lag 0–5 years) preceding the index date, respectively. Given that the crude model (model 1) did not include any covariates, all participants were retained in the analysis. For models 2 and 3, we excluded participants with any missing data. In sensitivity analyses, we employed multiple imputation to address missing covariate data and assess the robustness of our findings.
We further identified subgroups vulnerable to floods through stratification analyses by age group (≤64 and >65 years), sex, weight status defined according to BMI (≤ 24.9, 25–29.9, ≥ 30), education attainment, household income, physical activity, suboptimal diet, alcohol consumption status, smoking status, and area deprivation level. Results are presented as odds ratios (ORs) and their 95% confidence intervals (95% CIs) per unit increase in flood index. The significance of the difference in results between subgroups was tested using a random-effect meta-regression model.
Sensitivity analysis
We carried out the following sensitivity analyses: (1) Multiple imputation by chained equations was used for the missing values. Five imputed data sets were created, and their results were combined using Rubin’s rules [ 37 ]. (2) Alternative degrees of freedom were used for the lag-response association of flood. (3) Alternative degrees of freedom were used for the non-linear exposure-response relationship of mean temperature and relative humidity. (4) Alternative matching ratios (1:4 and 1:6) were used. (5) Excluding data after 2020 to control for the effect of the COVID-19 pandemic. (6) To capture the variation in flooding impacts within the year preceding mortality, we performed additional analyses with monthly flood index.
Table 1 shows the baseline characteristics of the 33,021 death cases and the 258,393 matched controls. The mean age (± standard deviation (SD)) of participants at study entry was 61.3 (± 6.4) years; 170,549 (58.5%) were male; 281,175 (96.5%) were white. Participants who died were more likely to have a higher BMI and lower household income; were less likely to be university graduates; more likely to smoke; and consumed less fruit and vegetables and more red and processed meat. They were also more likely to rate their overall health as poor and fair. Baseline characteristics of cases and controls with any missing values in covariates are shown in Additional file 1 : Table S3.
The distributions of the flood index and meteorological factors are shown in Table 2 . The annual average flood index across all participants during the study period ranged from 0.0 to 38.3, with a median value of 1.8 (25 th to 75 th percentiles: 0.5 to 3.6). Cases exposed to higher levels of flooding than controls during the 6 years before the end of follow-up (Additional file 1 : Fig. S2). The median annual mean temperature was 10.0 °C (25 th to 75 th percentiles: 9.3°C to 10.7°C) (Table 2 ). The flood index was negatively correlated with mean temperature (Pearson r = − 0.04) but positively correlated with relative humidity (Pearson r = 0.08).
Figure 2 illustrates the estimated cumulative OR of all-cause and cause-specific mortality associated with per unit increase in flood index over lag years 0–5. Per unit increase in flood index was associated with a 9.2% increased risk of all-cause mortality (OR: 1.092, 95% CI: 1.090–1.093) in the crude model. The results remained similar after further adjustment for socio-economic status (OR: 1.090, 95% CI: 1.088–1.091), whereas adjustment for lifestyle factors decreased the strength of the association (OR for fully adjusted model: 1.067, 95% CI: 1.063–1.071). Similar effects were observed for cause-specific mortality after fully adjusting the models, whereby a greater flood index was associated with a greater risk of death from neurodegenerative diseases (OR: 1.068, 95% CI: 1.050–1.087), neoplasm (OR: 1.063, 95% CI: 1.058–1.068), respiratory diseases (OR: 1.062, 95% CI: 1.045–1.080), suicide (OR: 1.052, 95% CI: 1.018–1.088), cardiovascular diseases (OR: 1.051, 95% CI: 1.042–1.059), mental diseases (OR: 1.047, 95% CI: 1.008–1.087), and digestive diseases (OR: 1.031, 95% CI: 1.011–1.052) (Fig. 2, Additional file 1 : Table S4).
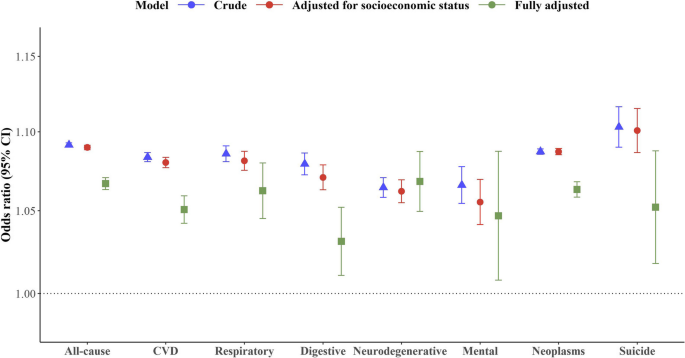
Cumulative odds ratio of all-cause and cause-specific mortality associated with per unit increase in flood index over lag years 0–5. Estimates of risk were obtained from the crude model that only included flood (crude); the multivariate model that additionally controlled for socioeconomic status (education attainment, household income, and deprivation); and the full model that additionally adjusted for BMI, physical activity, smoking, alcohol consumption, suboptimal diet, overall health rating, mean temperature, mean relative humidity, and assessment centre which serves as an indicator of the recruitment location for each participant (fully adjusted). The error bars represent 95% confidence intervals
Figure 3 shows the lag structure in the effects of flooding exposure on all-cause and cause-specific mortality. For all-cause mortality, the magnitude of associations increased from the current year (OR: 1.012, 95% CI: 1.011–1.013) to the lag year 3 (OR: 1.016, 95% CI: 1.015–1.017), and subsequently diminished to zero by lag year 5. For neurodegenerative mortality and mortality due to mental-ill health, the mortality risk was negligible in the current year, but strongest in the lag years 3 and 4. By contrast, the risk of mortality from suicide was the strongest in the current year (OR: 1.018, 95% CI: 1.008–1.028), and attenuated to lag year 5.
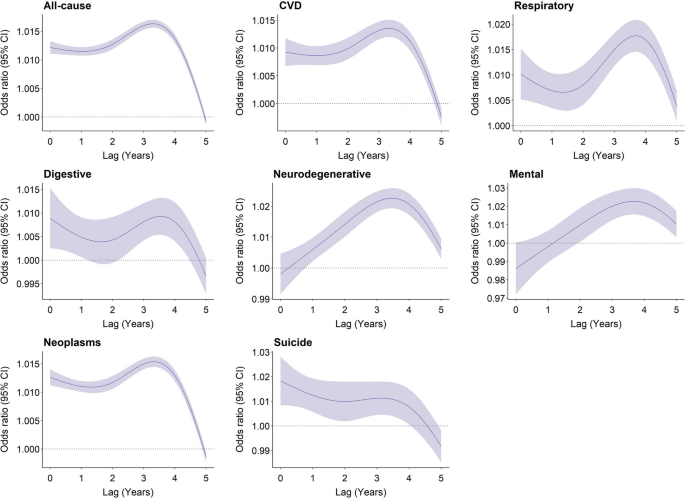
Overall lag structure in effects of flooding exposure on cause-specific mortality. Shaded areas represent 95% confidence intervals for the odds ratio
Subgroup analyses revealed that participants with higher levels of education and household income had a higher estimated risk of death from most causes in association with flooding exposure. Participants aged below 64 and female had a higher estimated risk of death from all-cause mortality, respiratory diseases, and neoplasm, but a lower estimated risk of death from digestive and mental diseases, respectively. The risk of suicide-related mortality in association with flooding exposure was higher among participants who were obese, had lower household income, engaged in less physical activity, were non-moderate alcohol consumers, and had high deprivation levels (Table 3 ).
Our sensitivity analysis suggested that using multiple imputed data did not change study findings (Additional file 1 : Fig. S3). Our results were not dependent on modelling assumptions and remained unaffected by the COVID-19 pandemic (Additional file 1 : Fig. S4–7). Matching ratios of 1:4 and 1:6 revealed a modest increase in the odds ratio for all-cause mortality and neoplasms, while the odds ratio for other causes of death remained unchanged ( Additional file 1 : Fig. S8 ). For all-cause mortality, with per unit increase in monthly flood index, odds ratios over 0–12 months preceding the mortality ranged from 1.005 (95% CI: 1.005–1.006) to 1.018 (95% CI: 1.017–1.018) (Additional file 1 : Table S5).
In this nested case-control study, we observed a significantly increasing risk of mortality associated with floods. The exposure-response curve was linear, with no discernible thresholds. The lag pattern varied across different causes of death. Flooding exposure has a long-lasting impact on neurodegenerative and mental diseases, whereas it has an immediate impact on suicide. Subgroup analyses revealed specific groups of vulnerable populations for flood-related death, which varied according to the cause of death.
Every unit increase in flood index was associated with a 6.7% increase in all-cause mortality risk over the following 6 years. This finding was similar to cause-specific mortality. Although few epidemiological studies have assessed the long-term effect of floods on mortality, our findings are consistent with previous findings of short-term flooding exposure showing increased risk of cholera at lag 0–20 weeks [ 38 ], diarrhoea at lag 0–28 weeks [ 38 ], respiratory infection at lag 3 months [ 39 ], typhoid fever at lag 1 week [ 40 ], malaria at lag 1 year [ 12 ], malnutrition at lag 1 year [ 41 ], and mental disorders at lag 6 months [ 19 ]. One study assessing the effects of flooding on mortality in England and Wales during 1994–2005 suggested a deficit of deaths in the post-flood period [ 42 ]. The inconsistency might result from the underestimation of death number, which can occur when deaths are registered at different places after displacement and a short observation period (one year after flooding exposure) during which the occurrence of death has not been observed. Milojevic et al. reported a slight but non-significant increase in mortality rates following the floods in Bangladesh in the flooded areas compared to non-flooded areas [ 43 ]. The accuracy of their results might be subject to recall bias in exposure assessment, given that exposure to flooding was ascertained from an interview survey four years after the flood event.
The long-term health deterioration resulting from floods could be attributed to mental health disorders driven by financial losses and community or social disruption, especially for those who live in resource-poor countries and communities (e.g. floodplains or non-resistant buildings, lack of warning systems and awareness of flooding hazard) [ 1 , 44 ]. For example, previous studies reported a significant and continued increase in the prevalence of post-traumatic stress disorder (PTSD), stress, anxiety, depression, and even suicide ideation following flooding exposure [ 20 ], which contribute to worse health outcomes. Additionally, among people who were exposed to floods, those who had chronic medical conditions are at higher risk of health deterioration due to potential disruptions in medication and healthcare services. Previous studies have noted that older adults and those receiving long-term care services showed decreased treatment adherence (e.g. interruption of medication and access to physicians) months and even years after the flooding [ 45 , 46 ], which serve to exacerbate or prolong symptoms of existing conditions.
Flooding exposure has a long-lasting impact on neurodegenerative and mental diseases, reaching its peak at 3–4 years post-exposure whereas the highest risk of mortality due to suicide occurs in the year of exposure. This suggests that varying health issues should be given consideration, depending on the stage following flooding exposure. A study in Queensland has noted that direct exposure to flood resulted in an increase in alcohol and tobacco usage half a year after flooding [ 46 ] and use of substances has been associated with an increased risk of suicide attempts in previous studies [ 47 , 48 , 49 , 50 ]. However, social support and compensation coverage have been demonstrated to have had a positive impact on health [ 20 ], which helps reduce the risk of subsequent suicide attempts. By contrast, cognitive decline is more likely to occur 2 years later after natural disasters [ 51 , 52 ], resulting from the new onset of depression and disruption of social contacts (e.g. loss of interactions with neighbours) [ 51 ].
Our findings align with previous studies highlighting the vulnerability of cancer patients to disruptions in healthcare services following natural disasters. While limited evidence suggests an increased risk of disease exacerbation among cancer patients post-disaster, our primary concern is the potential for delays in receiving essential cancer care [ 14 , 18 ]. Natural disasters like floods can severely disrupt healthcare systems, leading to damage to oncology centres, loss of medical records, pharmaceutical shortages, displacement of healthcare workers, and disruptions in pathology specimen handling, all of which can compromise cancer patient care [ 13 , 53 , 54 , 55 , 56 ]. The relocation of cancer patients to temporary shelters can be particularly challenging and distressing, especially for those with clinical instability [ 53 ]. Additionally, initial recovery efforts following natural disasters often prioritize immediate needs such as providing shelter, food, water, and addressing injuries from environmental hazards, infectious diseases, or other acute conditions [ 57 ]. This prioritization of immediate needs may inadvertently overlook the continuity of care required for non-acute medical issues like cancer. Given the individualized and continuous nature of cancer treatment, neoplasms are particularly susceptible to the disruptions caused by natural disasters. Our study demonstrates the association between floods and elevated mortality risks among cancer patients, reinforcing the urgent need to prioritize the needs of cancer patients before, during, and after disasters [ 13 , 58 ].
Profiles of vulnerable populations to flood-related mortality varied across causes of death. Of all factors considered, socio-economic status, which is determined by individual levels of education and income, has been identified as a significant modifier of flood-related mortality impacts. Individuals with higher socioeconomic status tend to have an increased risk of flood-related mortality from chronic diseases (e.g. cardiovascular diseases, respiratory diseases, and neurodegenerative diseases) but decreased risk of flood-related mortality from suicide. Although there is very limited evidence that can elucidate this finding, some insights can be gathered from the following studies. It is reported that people in high socioeconomic groups are more likely to be affected by work-life conflict-induced mental illness due to their higher occupational aspirations but a greater discrepancy between aspirations and reality [ 59 , 60 ]. Flooding exposure may further amplify the disparity between an individual’s aspirations and their actual circumstances, resulting in a negative impact on their mental health. Long-lasting psychological illness has been associated with worse chronic medical conditions [ 61 ].
In our study, we observed that participants with higher BMI and lower physical activity levels exhibited a significantly higher risk of flood-related mortality from suicide, but a comparatively lower risk of all-cause mortality. These associations can be attributed to different factors. On the one hand, individuals in low socio-economic groups, those engaged in minimal physical activity, and non-moderate alcohol drinkers, are at higher risk of developing suicide ideation in a short time following psychological trauma associated with flooding exposure [ 49 , 62 ]. On the other hand, individuals with higher levels of physical activity may be prone to engage in risk-taking behaviours during flooding events, potentially leading to increased mortality rates [ 63 ]. These behaviours could involve actions such as entering floodwaters to cross a river or stream, safeguarding property and families (e.g. through activities like sandbagging homes and clearing drains), and participating in rescuing operations [ 63 ]. Surprisingly, current smokers demonstrated a decreased risk of flood-related mortality from all-cause deaths and neoplasms. We acknowledge that residual confounding, raising from unmeasured factors at follow-up, might contribute to these associations. Nevertheless, it is important to note that our study represents the first report of a higher mortality risk after long-term exposure to floods, highlighting the need for further investigations to validate this finding and explore potential underlying reasons.
Based on our research, flooding exposure is responsible for advancing a substantial number of deaths, with the impact persisting for up to 6 years. Our findings suggest that preventive interventions should be implemented peri- and post-flooding periods to reduce avoidable deaths due to flooding exposure. Following a flooding event, there is an increased risk of suicide within the first year. Therefore, timely provision of coping support and stress management is crucial to avert psychological illness, particularly among individuals in low socio-economic groups, those engaged in less physical activity, and non-moderate alcohol drinkers. In long-term rehabilitation, more resources should be allocated towards addressing the chronic medical conditions of populations that have been exposed to flooding, especially neurological well-being. It is also crucial to pay attention to the high-income population, although further research is needed to elucidate the underlying mechanisms behind their greater mortality risks associated with flooding exposure.
The limitations merit consideration. Our participants were residents in the UK who were more likely to live in less socioeconomically deprived areas, therefore, our results may not be generalizable to a whole population, especially people in low- and middle-income countries. Like most of cohort studies, covariates were collected at enrolment in the biobank. Due to the limited information on behavioural changes after the baseline examinations, we are unable to exclude the effect of behavioural changes on the risk estimates. However, most of the covariates (e.g. socio-economic status) were considered as effect modifiers rather than confounders, therefore, any changes in these factors should not have a substantial impact on our estimates. While the flood index accounts for cumulative exposure, it does not yet capture the potential differential impacts of distinct flood phases (warning, event, post-event) on mortality. Further research with a short-term design would be helpful to investigate the impacts of distinct flood phases. The destructive power of floods can differ based on factors like terrain, altitude, water management, drainage, urbanization, and building design. Therefore, a single severity label for an entire flood event may not fully capture the nuances of varying local experiences. Further research is needed to refine our exposure assessment as more detailed data becomes available. Lastly, it is likely for people to move after flooding exposure, with or without moving back into their homes. We assumed that participants did not move, which may have underestimated the effect of floods if an individual moved from an area with a high risk of flooding to an area with a lower risk of flooding. However, exposure to flooding can still have a long-term impact on them due to potential property damage and financial loss, even if people relocate to areas with a low risk of flooding in the aftermath of the event.
In conclusion, this study provides robust epidemiological evidence for associations of long-term exposure to flooding with increased risk of mortality. The health consequences of flooding exposure can vary across different periods after the event. These findings contribute to a better understanding of the long-term impacts of flooding exposure and can help improve public health practices to reduce the disease burden associated with floods.
Availability of data and materials
Data used in this study are available through registration on the UK Biobank.
Abbreviations
Akaike Information Criterion
Bayesian Information Criterion
Body mass index
Confidence interval
Coronavirus disease 2019
Dartmouth Flood Observatory
European Centre for Medium-Range Weather Forecasts Reanalysis v5
International Classification of Diseases, edition 10
International Physical Activity Questionnaire-Short Form
Metabolic equivalent minutes per week
Post-traumatic stress disorder
Standard deviation
Townsend deprivation index
Lee J, Perera D, Glickman T, Taing LN. Water-related disasters and their health impacts: a global review. Prog Disaster Sci. 2020;8:100123.
Article Google Scholar
Wahlstrom M, Guha-Sapir D. The human cost of weather-related disasters 1995–2015. Geneva: UNISDR. 2015.
Wahlstrom M, Guha-Sapir D. The human cost of natural disasters: a global perspective. Geneva: UNISDR. 2015.
Rubinato M, Nichols A, Peng Y, Zhang JM, Lashford C, Cai YP, et al. Urban and river flooding: Comparison of flood risk management approaches in the UK and China and an assessment of future knowledge needs. Water Sci Eng. 2019;12(4):274–83.
Pitt M. Learning Lessons From the 2007 Floods. An Independent Review by Sir Michael Pitt. Cabinet Office, London. 2008.
Pregnolato M, Ford A, Wilkinson SM, Dawson RJ. The impact of flooding on road transport: A depth-disruption function. Transp Res D Transp Environ. 2017;55:67–81.
Thorne C. Geographies of UK flooding in 2013/4. Geogr J. 2014;180(4):297–309.
Marsh T, Kirby C, Muchan K, Barker L, Henderson E, Hannaford J. The winter floods of 2015/2016 in the UK-a review: UK: NERC/Centre for Ecology and Hydrology; 2016.
Wallemacq P, Below R, McClean D. Economic losses, poverty and disasters: 1998-2017: Geneva: United Nations Office for Disaster Risk Reduction; 2018.
Sayers P, Horritt M, Carr S, Kay A, Mauz J, Lamb R, et al. Third UK Climate Change Risk Assessment (CCRA3): Future flood risk. UK: Research undertaken by Sayers and Partners for the Committee on Climate Change; 2020.
Jonkman SN, Kelman I. An analysis of the causes and circumstances of flood disaster deaths. Disasters. 2005;29(1):75–97.
Article PubMed Google Scholar
Boyce R, Reyes R, Matte M, Ntaro M, Mulogo E, Metlay JP, et al. Severe Flooding and Malaria Transmission in the Western Ugandan Highlands: Implications for Disease Control in an Era of Global Climate Change. J Infect Dis. 2016;214(9):1403–10.
Article PubMed PubMed Central Google Scholar
Man RX, Lack DA, Wyatt CE, Murray V. The effect of natural disasters on cancer care: a systematic review. Lancet Oncol. 2018;19(9):e482–99.
Ryan B, Franklin RC, Burkle FM Jr, Aitken P, Smith E, Watt K, et al. Identifying and Describing the Impact of Cyclone, Storm and Flood Related Disasters on Treatment Management, Care and Exacerbations of Non-communicable Diseases and the Implications for Public Health. PLoS Curr. 2015;7:21–50.
Google Scholar
McKinney N, Houser C, Meyer-Arendt K. Direct and indirect mortality in Florida during the 2004 hurricane season. Int J Biometeorol. 2011;55(4):533–46.
Rath B, Young EA, Harris A, Perrin K, Bronfin DR, Ratarh R, et al. Adverse Respiratory Symptoms and Environmental Exposures Among Children and Adolescents Following Hurricane Katrina. Public Health Rep. 2011;126(6):853–60.
Buajaroen H. Management of health care services for flood victims: The case of the shelter at Nakhon Pathom Rajabhat University Central Thailand. Australas Emerg Nurs. 2013;16(3):116–22.
Loehn B, Pou AM, Nuss DW, Tenney J, McWhorter A, DiLeo M, et al. Factors affecting access to head and neck cancer care after a natural disaster: a post-Hurricane Katrina survey. Head Neck. 2011;33(1):37–44.
Alderman K, Turner LR, Tong S. Assessment of the health impacts of the 2011 summer floods in Brisbane. Disaster Med Public Health Prep. 2013;7(4):380–6.
Zhong S, Yang L, Toloo S, Wang Z, Tong S, Sun X, et al. The long-term physical and psychological health impacts of flooding: A systematic mapping. Sci Total Environ. 2018;626:165–94.
Article CAS PubMed Google Scholar
Trief PM, Ouimette P, Wade M, Shanahan P, Weinstock RS. Post-traumatic stress disorder and diabetes: co-morbidity and outcomes in a male veterans sample. J Behav Med. 2006;29(5):411–8.
Sharpe I, Davison CM. Climate change, climate-related disasters and mental disorder in low- and middle-income countries: a scoping review. BMJ Open. 2021;11(10):e051908.
Carozza DA, Boudreault M. A global flood risk modeling framework built with climate models and machine learning. J Adv Model Earth Syst. 2021;13(4):e2020MS002221.
Yang Z, Huang W, McKenzie JE, Xu R, Yu P, Ye T, et al. Mortality risks associated with floods in 761 communities worldwide: time series study. BMJ. 2023;383:e075081.
Steenland K, Seals R, Klein M, Jinot J, Kahn HD. Risk estimation with epidemiologic data when response attenuates at high-exposure levels. Environ Health Perspect. 2011;119(6):831–7.
White E, Hunt JR, Casso D. Exposure measurement in cohort studies: the challenges of prospective data collection. Epidemiol Rev. 1998;20(1):43–56.
Ganna A, Ingelsson E. 5 year mortality predictors in 498,103 UK Biobank participants: a prospective population-based study. Lancet. 2015;386(9993):533–40.
Wang M, Zhou T, Song Q, Ma H, Hu Y, Heianza Y, et al. Ambient air pollution, healthy diet and vegetable intakes, and mortality: a prospective UK Biobank study. Int J Epidemiol. 2022;51(4):1243–53.
Wang M, Zhou T, Song Y, Li X, Ma H, Hu Y, et al. Joint exposure to various ambient air pollutants and incident heart failure: a prospective analysis in UK Biobank. European heart journal. 2021;42(16):1582–91.
Article CAS PubMed PubMed Central Google Scholar
IPAQ Research Committee. Guidelines for data processing and analysis of the International Physical Activity Questionnaire (IPAQ)-short and long forms. https://www.physio-pedia.com/images/c/c7/Quidelines_for_interpreting_the_IPAQ.pdf (accessed January 20, 2024).
Zhang YB, Chen C, Pan XF, Guo J, Li Y, Franco OH, et al. Associations of healthy lifestyle and socioeconomic status with mortality and incident cardiovascular disease: two prospective cohort studies. BMJ. 2021;373:n604.
Chen H, Cao Y, Ma Y, Xu W, Zong G, Yuan C. Age- and sex-specific modifiable risk factor profiles of dementia: evidence from the UK Biobank. Eur J Epidemiol. 2023;38(1):83–93.
Jung CR, Chung WT, Chen WT, Lee RY, Hwang BF. Long-term exposure to traffic-related air pollution and systemic lupus erythematosus in Taiwan: A cohort study. Sci Total Environ. 2019;668:342–9.
Gasparrini A. Modeling exposure-lag-response associations with distributed lag non-linear models. Stat Med. 2014;33(5):881–99.
Li Y-Z, Huang S-H, Shi S, Chen W-X, Wei Y-F, Zou B-J, et al. Association of long-term particulate matter exposure with all-cause mortality among patients with ovarian cancer: A prospective cohort. Sci Total Environ. 2023;884:163748.
Kriit HK, Andersson EM, Carlsen HK, Andersson N, Ljungman PL, Pershagen G, et al. Using distributed lag non-linear models to estimate exposure lag-response associations between long-term air pollution exposure and incidence of cardiovascular disease. Int J Env Res Pub He. 2022;19(5):2630.
Article CAS Google Scholar
Rubin DB. Multiple imputation for nonresponse in surveys: Canada: Wiley; 2004.
Hashizume M, Wagatsuma Y, Faruque ASG, Hayashi T, Hunter PR, Armstrong B, et al. Factors determining vulnerability to diarrhoea during and after severe floods in Bangladesh. J Water Health. 2008;6(3):323–32.
Saulnier DD, Hanson C, Ir P, Alvesson HM, von Schreeb J. The Effect of Seasonal Floods on Health: Analysis of Six Years of National Health Data and Flood Maps. Int J Env Res Pub He. 2018;15(4):665–77.
Liu ZD, Lao JH, Zhang Y, Liu YY, Zhang J, Wang H, et al. Association between floods and typhoid fever in Yongzhou, China: Effects and vulnerable groups. Environ Res. 2018;167:718–24.
Rodriguez-Llanes JM, Ranjan-Dash S, Mukhopadhyay A, Guha-Sapir D. Flood-Exposure Is Associated with Higher Prevalence of Child Undernutrition in Rural Eastern India. Int J Env Res Pub He. 2016;13(2):210.
Milojevic A, Armstrong B, Kovats S, Butler B, Hayes E, Leonardi G, et al. Long-term effects of flooding on mortality in England and Wales, 1994–2005: controlled interrupted time-series analysis. Environ Health. 2011;10(1):11–9.
Milojevic A, Armstrong B, Hashizume M, McAllister K, Faruque A, Yunus M, et al. Health Effects of Flooding in Rural Bangladesh. Epidemiology. 2012;23(1):107–15.
Ahern M, Kovats RS, Wilkinson P, Few R, Matthies F. Global health impacts of floods: Epidemiologic evidence. Epidemiol Rev. 2005;27:36–46.
Tomio J, Sato H, Mizumura H. Interruption of Medication among Outpatients with Chronic Conditions after a Flood. Prehospital Disaster. 2010;25(1):42–50.
Turner LR, Alderman K, Huang CR, Tong SL. Impact of the 2011 Queensland floods on the use of tobacco, alcohol and medication. Aust Nz J Publ Heal. 2013;37(4):396.
Orri M, Seguin JR, Castellanos-Ryan N, Tremblay RE, Cote SM, Turecki G, et al. A genetically informed study on the association of cannabis, alcohol, and tobacco smoking with suicide attempt. Mol Psychiatr. 2021;26(9):5061–70.
Berlin I, Hakes JK, Hu MC, Covey LS. Tobacco Use and Suicide Attempt: Longitudinal Analysis with Retrospective Reports. Plos One. 2015;10(4):e0122607.
Darvishi N, Farhadi M, Haghtalab T, Poorolajal J. Alcohol-Related Risk of Suicidal Ideation, Suicide Attempt, and Completed Suicide: A Meta-Analysis. Plos One. 2015;10(5):e0126870.
Gobbi G, Atkin T, Zytynski T. Association of Cannabis Use in Adolescence and Risk of Depression, Anxiety, and Suicidality in Young Adulthood: A Systematic Review and Meta-analysis. Jama Psychiat. 2019;76(4):426–34.
Hikichi H, Aida J, Kondo K, Tsuboya T, Matsuyama Y, Subramanian SV, et al. Increased risk of dementia in the aftermath of the 2011 Great East Japan Earthquake and Tsunami. P Natl Acad Sci USA. 2016;113(45):E6911–8.
Akanuma K, Nakamura K, Meguro K, Chiba M, Gutierrez Ubeda SR, Kumai K, et al. Disturbed social recognition and impaired risk judgement in older residents with mild cognitive impairment after the Great East Japan Earthquake of 2011: the Tome Project. Psychogeriatrics. 2016;16(6):349–54.
Morikawa N, Yanagisawa S, Iwasashi H, Tabata T, Abe T, Nakamura R, et al. Cancer patients in the hospital damaged by the Japan earthquake and tsunami. J Clin Oncol. 2012;30(15):e19508-e.
Cancer Ullman K, Disasters Care During Natural. J Natl Cancer I. 2011;103(24):1819–20.
Arrieta MI, Foreman RD, Crook ED, Icenogle ML. Providing Continuity of Care for Chronic Diseases in the Aftermath of Katrina: From Field Experience to Policy Recommendations. Disaster Med Public. 2009;3(3):174–82.
Rosenthal E. How the Cancer Community Fared During Hurricane Sandy's Mid-Atlantic Sweep. Oncology Times. 2012;34(23):8-10.
Prasad AS, Francescutti LH. Natural disasters. International encyclopedia of public health. 2017;5:215-22.
Aitsi-Selmi A, Murray V. Protecting the Health and Well-being of Populations from Disasters: Health and Health Care in The Sendai Framework for Disaster Risk Reduction 2015–2030. Prehospital Disaster. 2016;31(1):74–8.
Cochran DB, Wang EW, Stevenson SJ, Johnson LE, Crews C. Adolescent Occupational Aspirations: Test of Gottfredson’s Theory of Circumscription and Compromise. Career Dev Q. 2011;59(5):412–27.
Kim YM, Cho SI. Socioeconomic status, work-life conflict, and mental health. Am J Ind Med. 2020;63(8):703–12.
Patten SB, Williams JVA, Lavorato DH, Modgill G, Jette N, Eliasziw M. Major depression as a risk factor for chronic disease incidence: longitudinal analyses in a general population cohort. Gen Hosp Psychiat. 2008;30(5):407–13.
Vancampfort D, Hallgren M, Firth J, Rosenbaum S, Schuch FB, Mugisha J, et al. Physical activity and suicidal ideation: A systematic review and meta-analysis. J Affect Disorders. 2018;225:438–48.
Hamilton K, Demant D, Peden AE, Hagger MS. A systematic review of human behaviour in and around floodwater. Int J Disaster Risk Reduction. 2020;47:101561.
Download references
Acknowledgements
We gratefully thank all the participants in the UK Biobank, and everyone involved in planning and conducting the study.
Australian Research Council grant DP210102076
Australian National Health and Medical Research Council grant GNT2000581)
China Scholarship Council grant 202006010044 (YW)
China Scholarship Council grant 202006010043 (BW)
China Scholarship Council grant 201906210065 (PY)
National Health and Medical Research Council grant GNT2009866 (SL)
National Health and. Medical Research Council grant GNT1163693 (YG)
National Health and Medical Research Council grant GNT2008813 (YG)
Author information
Hong Liu, Shanshan Li, and Yuming Guo are co-senior authors.
Authors and Affiliations
School of Public Health and Preventive Medicine, Monash University, Level 2, 553 St Kilda Road, Melbourne, VIC, 3004, Australia
Yao Wu, Danijela Gasevic, Bo Wen, Zhengyu Yang & Pei Yu
Department of Dermatology, Xiangya Hospital, Central South University, Changsha, 410008, Hunan, China
Guowei Zhou, Yan Zhang, Hong Liu, Shanshan Li & Yuming Guo
Department of Biochemistry and Molecular Biology, Monash Biomedicine Discovery Institute, Monash University, Melbourne, VIC, 3800, Australia
Jiangning Song
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization: YG, JS, HL, SL, YW. Methodology: YW, DG. Data collection: BW, ZY, GZ, YZ, ZY
Visualization: YW, BW. Supervision: YG, HL, SL. Writing—original draft: YW. Writing—review and editing: DG, BW, ZY, PY. All authors read and approved the final manuscript.
Authors’ Twitter handles
Yuming Guo: @YumingGuo007
Yao Wu: @Yaoyaowu13
Corresponding author
Correspondence to Yuming Guo .
Ethics declarations
Ethics approval and consent to participate.
UK Biobank has ethical approval from the North West Multi-Centre Research Ethics Committee (reference 16/NW/0274).
Consent for publication
Consent for publication was obtained from all included participants.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:.
Table S1. Definitions of different severities of flood events. Table S2. The Akaike Information Criterion (AIC) and the Bayesian Information Criterion (BIC) of nonlinear and linear models. Table S3. Baseline characteristics of cases and matched controls enrolled in UK Biobank, including missing values. Table S4. Cumulative odds ratios of cause-specific mortality associated with per unit increase in flood index over lag years 0–5. Table S5. Cumulative odds ratios of all-cause mortality associated with per unit increase in monthly flood index over lag month 0–12. Figure S1. Nonlinear curves of the associations between flood index and all-cause and cause-specific mortality. Figure S2. Cumulative flood index of cases and controls during the six years before the date of death or the end of the follow-up. Figure S3. Cumulative odds ratios of all-cause and cause-specific mortality associated with per unit increase in flood index over lag years 0–5 using complete data after multiple imputation. Figure S4. Cumulative odds ratios of all-cause and cause-specific mortality associated with per unit increase in flood index over lag years 0–5 using different degrees of freedom for lag-response association of flood index. Figure S5. Cumulative odds ratios of all-cause and cause-specific mortality associated with per unit increase in flood index over lag years 0–5 using different degrees of freedom for mean temperature. Figure S6. Cumulative odds ratios of all-cause and cause-specific mortality associated with per unit increase in flood index over lag years 0–5 using different degrees of freedom for relative humidity. Figure S7. Cumulative odds ratios of all-cause and cause-specific mortality associated with per unit increase in flood index over lag years 0–5 after excluding deaths after 2020. Figure S8. Cumulative odds ratios of all-cause and cause-specific mortality associated with per unit increase in flood index over lag years 0–5 using different matching ratios.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Wu, Y., Gasevic, D., Wen, B. et al. Floods and cause-specific mortality in the UK: a nested case-control study. BMC Med 22 , 188 (2024). https://doi.org/10.1186/s12916-024-03412-0
Download citation
Received : 27 November 2023
Accepted : 29 April 2024
Published : 07 May 2024
DOI : https://doi.org/10.1186/s12916-024-03412-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Natural disaster
BMC Medicine
ISSN: 1741-7015
- Submission enquiries: [email protected]
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Dr. SooJeong Youn: This case highlights the importance of attending to the intricate, multilevel, systemic factors that affect the mental health experience and clinical presentation of patients ...
150 Case Studies: Real Stories Of People Overcoming Struggles of Mental Health. At Tracking Happiness, we're dedicated to helping others around the world overcome struggles of mental health. In 2022, we published a survey of 5,521 respondents and found: 88% of our respondents experienced mental health issues in the past year.
Introduction to the selected case study. In this case study, we will focus on Jane, a 32-year-old woman who has been struggling with depression for the past two years. Jane's case offers a compelling narrative that highlights the various aspects of depression, including its onset, symptoms, and the treatment journey.
We're going to go ahead to patient case No. 1. This is a 27-year-old woman who's presented for evaluation of a complex depressive syndrome. She has not benefitted from 2 recent trials of antidepressants—sertraline and escitalopram. This is her third lifetime depressive episode.
Her more recent episodes related to her parents' marital problems and her academic/social difficulties at school. She was treated using cognitive-behavioral therapy (CBT). Chafey, M.I.J., Bernal, G., & Rossello, J. (2009). Clinical Case Study: CBT for Depression in A Puerto Rican Adolescent. Challenges and Variability in Treatment Response.
The high prevalence of stress-related and mental health conditions and substance use disorders in the workplace, and the common co-occurrence with other ... employees whose work performance is affected by mental health symptoms.21 See the Case Study Reference Table (p.14) for a listing of case studies developed by other organizations that ...
Disaster behavioral health. The current COVID-19 pandemic, while still underway, has already demonstrated the need for psychological interventions to manage the isolation, stress, and trauma stemming from the ongoing disaster [1,2,3,4,5].While the scale of the event is unprecedented, interest in understanding the psychological consequences of disasters is not unique to the pandemic [6,7,8,9,10].
One Canadian initiative, Gerstein Crisis Centre, stood out as a case study for mental health crisis support rooted in community and human rights. For more than 30 years, this community-based ...
The pilot case study herein underscores the utility and potential of school-based mental health promotion efforts, particularly through InSciEd Out's community-based framework. Targeted improvements in mental health literacy and moderate improvements in help-seeking intentions were accompanied by large decreases in mental health misconceptions.
In a follow-up study of their 2019 Mental Health at Work Report, Mind Share Partners' 2021 Mental Health at Work Report, the authors offer a rare comparison of the state of mental health, stigma ...
Abstract. This collection presents six case studies on the ethics of mental health research, written by scientific researchers and ethicists from around the world. We publish them here as a resource for teachers of research ethics and as a contribution to several ongoing ethical debates. Each consists of a description of a research study that ...
The poor mental health is strongly related to other health and development concern in adolescence people, for example, low self-confident, ... The present case study was undertaken to document mental health vulnerability of school-going adolescent in rural Gujarat. The study reveals that 14% of the study population is vulnerable for mental ...
The true impact of workplace wellbeing: two case studies. Embedded Expertise, Published: January 29, 2020 - Updated: August 22, 2022 Mental health concerns are a leading cause of workplace absence, and as we see increasing incidents of mental health-related sick days, workplace wellbeing is paramount for both organisational and individual success. ...
Impact case studies: mental health services for depression and anxiety. Journal of Health Services Research & Policy 2017 22: 2, 120-125 Share. Share. Social Media; Email; ... Related Articles. Similar Articles: Similar Articles: View all > Specialization and minority health care: hormone therapy for trans people in England
Health has been regularly connected with social entrepreneurship, with a recent review of 366 case studies finding that health was the primary target in 18% of the cases . Social entrepreneurship in mental health specifically has had less attention despite its relevance in addressing the complexity of mental illness in under-resourced contexts ...
National Institute of Mental Health (NIMH): Anxiety disorders; Case study 3 summary. In this case study, Lucy's symptoms of mental illness emerge in her teenage years. Lucy describes periods of intense mood, both elevated and depressed, as well as potential anxiety-related responses. It is not until she develops a therapeutic relationship ...
Kolej Universiti Poly-T ech MARA. ( [email protected]) T el no: 03-92069700 Fax no: 03-92815764. The Malaysian Ministry of Health has aired its concern towards the state of Malaysian ...
In mental health, one of the best-known examples of an influential case report is the story of 19 th century railway worker Phineas Gage . Recorded in 1948, this case report outlines medical observations and care provided by the General Practitioner John Harlow in the hours and days following a terrible railway accident.
NCMHCE Sample Case Study. You are a licensed mental health counselor working in a community agency. Your client self-referred for services because "my mother won't stop bugging me for staying in bed all day. I can't help it. I am in a rut and cannot find a way out.".
Case study details a 27-year-old woman with schizoaffective disorder and fibromyalgia who used high-potency cannabis to alleviate pain but experienced adverse psychiatric effects. A month-long ...
Viewing expert testimony during the court case of Amber Heard and Johnny Depp led to highly prejudicial views of the mental health difficulties of both parties being formed, a new study by ...
A Psychiatric Case Study. College of Nursing, Simmons University. NURS-335AC: Psychiatric and Mental Health Nursing. Professor Jennifer Livesley. March 28, 2022. The Psychiatric Assessment. This patient, an 83 year old white female was admitted on 3/04/2022. She is widowed and has one adult son who was appointed her guardian one month ago.
In addition, many existing systematic studies related to mental health studies have been conducted worldwide. However, only a limited number of studies are integrated with social media and conducted in the context of social science because the available literature heavily focused on medical science . Because social media is a relatively new ...
NAMI reported that 2 in 3 teens agree schools should teach what mental health is and how to find treatment. ... Olive oil could lower risk of dementia-related death, study finds. Chloe Nordquist 5:03 PM, May 06, 2024 . Federal court case could decide if terminal patients may use psilocybin. Vanessa Misciagna 8:33 PM, May 03, 2024 .
Floods are the most frequent weather-related disaster, causing significant health impacts worldwide. Limited studies have examined the long-term consequences of flooding exposure. Flood data were retrieved from the Dartmouth Flood Observatory and linked with health data from 499,487 UK Biobank participants. To calculate the annual cumulative flooding exposure, we multiplied the duration and ...
A multiple case study design requires the selection of cases (i.e., families) who have a similar connection to a phenomenon (i.e., ... At the practice level, all participants in this study noted a lack of training for medical and mental health providers related to working with TGD people. As providers become more aware of, and more TGD youth ...