
No evidence that depression is caused by low serotonin levels, finds comprehensive review
After decades of study, there remains no clear evidence that serotonin levels or serotonin activity are responsible for depression, according to a major review of prior research led by UCL scientists.
The new umbrella review -- an overview of existing meta-analyses and systematic reviews -- published in Molecular Psychiatry , suggests that depression is not likely caused by a chemical imbalance, and calls into question what antidepressants do. Most antidepressants are selective serotonin reuptake inhibitors (SSRIs), which were originally said to work by correcting abnormally low serotonin levels. There is no other accepted pharmacological mechanism by which antidepressants affect the symptoms of depression.
Lead author Professor Joanna Moncrieff, a Professor of Psychiatry at UCL and a consultant psychiatrist at North East London NHS Foundation Trust (NELFT), said: "It is always difficult to prove a negative, but I think we can safely say that after a vast amount of research conducted over several decades, there is no convincing evidence that depression is caused by serotonin abnormalities, particularly by lower levels or reduced activity of serotonin.
"The popularity of the 'chemical imbalance' theory of depression has coincided with a huge increase in the use of antidepressants. Prescriptions for antidepressants have risen dramatically since the 1990s, with one in six adults in England and 2% of teenagers now being prescribed an antidepressant in a given year.
"Many people take antidepressants because they have been led to believe their depression has a biochemical cause, but this new research suggests this belief is not grounded in evidence."
The umbrella review aimed to capture all relevant studies that have been published in the most important fields of research on serotonin and depression. The studies included in the review involved tens of thousands of participants.
Research that compared levels of serotonin and its breakdown products in the blood or brain fluids did not find a difference between people diagnosed with depression and healthy control (comparison) participants.
Research on serotonin receptors and the serotonin transporter, the protein targeted by most antidepressants, found weak and inconsistent evidence suggestive of higher levels of serotonin activity in people with depression. However, the researchers say the findings are likely explained by the use of antidepressants among people diagnosed with depression, since such effects were not reliably ruled out.
The authors also looked at studies where serotonin levels were artificially lowered in hundreds of people by depriving their diets of the amino acid required to make serotonin. These studies have been cited as demonstrating that a serotonin deficiency is linked to depression. A meta-analysis conducted in 2007 and a sample of recent studies found that lowering serotonin in this way did not produce depression in hundreds of healthy volunteers, however. There was very weak evidence in a small subgroup of people with a family history of depression, but this only involved 75 participants, and more recent evidence was inconclusive.
Very large studies involving tens of thousands of patients looked at gene variation, including the gene for the serotonin transporter. They found no difference in these genes between people with depression and healthy controls. These studies also looked at the effects of stressful life events and found that these exerted a strong effect on people's risk of becoming depressed -- the more stressful life events a person had experienced, the more likely they were to be depressed. A famous early study found a relationship between stressful events, the type of serotonin transporter gene a person had and the chance of depression. But larger, more comprehensive studies suggest this was a false finding.
These findings together led the authors to conclude that there is "no support for the hypothesis that depression is caused by lowered serotonin activity or concentrations."
The researchers say their findings are important as studies show that as many as 85-90% of the public believes that depression is caused by low serotonin or a chemical imbalance. A growing number of scientists and professional bodies are recognising the chemical imbalance framing as an over-simplification. There is also evidence that believing that low mood is caused by a chemical imbalance leads people to have a pessimistic outlook on the likelihood of recovery, and the possibility of managing moods without medical help. This is important because most people will meet criteria for anxiety or depression at some point in their lives.
The authors also found evidence from a large meta-analysis that people who used antidepressants had lower levels of serotonin in their blood. They concluded that some evidence was consistent with the possibility that long-term antidepressant use reduces serotonin concentrations. The researchers say this may imply that the increase in serotonin that some antidepressants produce in the short term could lead to compensatory changes in the brain that produce the opposite effect in the long term.
While the study did not review the efficacy of antidepressants, the authors encourage further research and advice into treatments that might focus instead on managing stressful or traumatic events in people's lives, such as with psychotherapy, alongside other practices such as exercise or mindfulness, or addressing underlying contributors such as poverty, stress and loneliness.
Professor Moncrieff said: "Our view is that patients should not be told that depression is caused by low serotonin or by a chemical imbalance, and they should not be led to believe that antidepressants work by targeting these unproven abnormalities. We do not understand what antidepressants are doing to the brain exactly, and giving people this sort of misinformation prevents them from making an informed decision about whether to take antidepressants or not."
Co-author Dr Mark Horowitz, a training psychiatrist and Clinical Research Fellow in Psychiatry at UCL and NELFT, said: "I had been taught that depression was caused by low serotonin in my psychiatry training and had even taught this to students in my own lectures. Being involved in this research was eye-opening and feels like everything I thought I knew has been flipped upside down.
"One interesting aspect in the studies we examined was how strong an effect adverse life events played in depression, suggesting low mood is a response to people's lives and cannot be boiled down to a simple chemical equation."
Professor Moncrieff added: "Thousands of people suffer from side effects of antidepressants, including the severe withdrawal effects that can occur when people try to stop them, yet prescription rates continue to rise. We believe this situation has been driven partly by the false belief that depression is due to a chemical imbalance. It is high time to inform the public that this belief is not grounded in science."
The researchers caution that anyone considering withdrawing from antidepressants should seek the advice of a health professional, given the risk of adverse effects following withdrawal. Professor Moncrieff and Dr Horowitz are conducting ongoing research into how best to gradually stop taking antidepressants.
- Mental Health
- Disorders and Syndromes
- Intelligence
- Neurotransmitter
- Methamphetamine
- Bipolar disorder
- Psychometrics
- Clinical depression
- Confirmation bias
Story Source:
Materials provided by University College London . Note: Content may be edited for style and length.
Journal Reference :
- Joanna Moncrieff, Ruth E. Cooper, Tom Stockmann, Simone Amendola, Michael P. Hengartner, Mark A. Horowitz. The serotonin theory of depression: a systematic umbrella review of the evidence . Molecular Psychiatry , 2022; DOI: 10.1038/s41380-022-01661-0
Cite This Page :
Explore More
- Mice Given Mouse-Rat Brains Can Smell Again
- New Circuit Boards Can Be Repeatedly Recycled
- Collisions of Neutron Stars and Black Holes
- Advance in Heart Regenerative Therapy
- Bioluminescence in Animals 540 Million Years Ago
- Profound Link Between Diet and Brain Health
- Loneliness Runs Deep Among Parents
- Food in Sight? The Liver Is Ready!
- Acid Reflux Drugs and Risk of Migraine
- Do Cells Have a Hidden Communication System?
Trending Topics
Strange & offbeat.

Depression is probably not caused by a chemical imbalance in the brain – new study
Senior Clinical Lecturer, Critical and Social Psychiatry, UCL
Clinical Research Fellow in Psychiatry, UCL
Disclosure statement
Joanna Moncrieff is a co-investigator on a National Institute of Health Research funded study exploring methods of antidepressant discontinuation. She is co-chair person of the Critical Psychiatry Network, an informal and unfunded group of psychiatrists and an unpaid board member of the voluntary group, the Council for Evidence-based Psychiatry.
Mark Horowitz is co-founder of a company aiming to help people safely stop unnecessary antidepressants in Canada. He is an (unpaid) associate of the International Institute of Psychiatric Drug Withdrawal (IIPDW) and a member of the Critical Psychiatry Network.
University College London provides funding as a founding partner of The Conversation UK.
View all partners
- Bahasa Indonesia
For three decades, people have been deluged with information suggesting that depression is caused by a “chemical imbalance” in the brain – namely an imbalance of a brain chemical called serotonin. However, our latest research review shows that the evidence does not support it.
You can listen to more articles from The Conversation, narrated by Noa, here .
Although first proposed in the 1960s , the serotonin theory of depression started to be widely promoted by the pharmaceutical industry in the 1990s in association with its efforts to market a new range of antidepressants, known as selective serotonin-reuptake inhibitors or SSRIs. The idea was also endorsed by official institutions such as the American Psychiatric Association, which still tells the public that “differences in certain chemicals in the brain may contribute to symptoms of depression”.
Countless doctors have repeated the message all over the world, in their private surgeries and in the media. People accepted what they were told. And many started taking antidepressants because they believed they had something wrong with their brain that required an antidepressant to put right. In the period of this marketing push, antidepressant use climbed dramatically, and they are now prescribed to one in six of the adult population in England , for example.
For a long time, certain academics , including some leading psychiatrists , have suggested that there is no satisfactory evidence to support the idea that depression is a result of abnormally low or inactive serotonin. Others continue to endorse the theory . Until now, however, there has been no comprehensive review of the research on serotonin and depression that could enable firm conclusions either way.
At first sight, the fact that SSRI-type antidepressants act on the serotonin system appears to support the serotonin theory of depression. SSRIs temporarily increase the availability of serotonin in the brain, but this does not necessarily imply that depression is caused by the opposite of this effect.
There are other explanations for antidepressants’ effects. In fact, drug trials show that antidepressants are barely distinguishable from a placebo (dummy pill) when it comes to treating depression. Also, antidepressants appear to have a generalised emotion-numbing effect which may influence people’s moods, although we do not know how this effect is produced or much about it.

First comprehensive review
There has been extensive research on the serotonin system since the 1990s, but it has not been collected systematically before. We conducted an “umbrella” review that involved systematically identifying and collating existing overviews of the evidence from each of the main areas of research into serotonin and depression. Although there have been systematic reviews of individual areas in the past, none have combined the evidence from all the different areas taking this approach.
One area of research we included was research comparing levels of serotonin and its breakdown products in the blood or brain fluid. Overall, this research did not show a difference between people with depression and those without depression.
Another area of research has focused on serotonin receptors , which are proteins on the ends of the nerves that serotonin links up with and which can transmit or inhibit serotonin’s effects. Research on the most commonly investigated serotonin receptor suggested either no difference between people with depression and people without depression, or that serotonin activity was actually increased in people with depression – the opposite of the serotonin theory’s prediction.
Research on the serotonin “transporter” , that is the protein which helps to terminate the effect of serotonin (this is the protein that SSRIs act on), also suggested that, if anything, there was increased serotonin activity in people with depression. However, these findings may be explained by the fact that many participants in these studies had used or were currently using antidepressants.
We also looked at research that explored whether depression can be induced in volunteers by artificially lowering levels of serotonin . Two systematic reviews from 2006 and 2007 and a sample of the ten most recent studies (at the time the current research was conducted) found that lowering serotonin did not produce depression in hundreds of healthy volunteers. One of the reviews showed very weak evidence of an effect in a small subgroup of people with a family history of depression, but this only involved 75 participants.
Very large studies involving tens of thousands of patients looked at gene variation, including the gene that has the instructions for making the serotonin transporter . They found no difference in the frequency of varieties of this gene between people with depression and healthy controls.
Although a famous early study found a relationship between the serotonin transporter gene and stressful life events, larger, more comprehensive studies suggest no such relationship exists. Stressful life events in themselves, however, exerted a strong effect on people’s subsequent risk of developing depression.
Some of the studies in our overview that included people who were taking or had previously taken antidepressants showed evidence that antidepressants may actually lower the concentration or activity of serotonin.
Not supported by the evidence
The serotonin theory of depression has been one of the most influential and extensively researched biological theories of the origins of depression. Our study shows that this view is not supported by scientific evidence. It also calls into question the basis for the use of antidepressants.
Most antidepressants now in use are presumed to act via their effects on serotonin. Some also affect the brain chemical noradrenaline. But experts agree that the evidence for the involvement of noradrenaline in depression is weaker than that for serotonin .
There is no other accepted pharmacological mechanism for how antidepressants might affect depression. If antidepressants exert their effects as placebos, or by numbing emotions, then it is not clear that they do more good than harm.
Although viewing depression as a biological disorder may seem like it would reduce stigma, in fact, research has shown the opposite , and also that people who believe their own depression is due to a chemical imbalance are more pessimistic about their chances of recovery.
It is important that people know that the idea that depression results from a “chemical imbalance” is hypothetical. And we do not understand what temporarily elevating serotonin or other biochemical changes produced by antidepressants do to the brain. We conclude that it is impossible to say that taking SSRI antidepressants is worthwhile, or even completely safe.
If you’re taking antidepressants, it’s very important you don’t stop doing so without speaking to your doctor first. But people need all this information to make informed decisions about whether or not to take these drugs.
- SSRI antidepressants

Executive Dean, Faculty of Health

Regional Engagement Officer - Shepparton

Lecturer/Senior Lecturer, Earth System Science (School of Science)

Sydney Horizon Educators (Identified)

Deputy Social Media Producer
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Systematic Review
- Open access
- Published: 20 July 2022
The serotonin theory of depression: a systematic umbrella review of the evidence
- Joanna Moncrieff 1 , 2 ,
- Ruth E. Cooper 3 ,
- Tom Stockmann 4 ,
- Simone Amendola 5 ,
- Michael P. Hengartner 6 &
- Mark A. Horowitz 1 , 2
Molecular Psychiatry volume 28 , pages 3243–3256 ( 2023 ) Cite this article
1.26m Accesses
233 Citations
9425 Altmetric
Metrics details
- Diagnostic markers
The serotonin hypothesis of depression is still influential. We aimed to synthesise and evaluate evidence on whether depression is associated with lowered serotonin concentration or activity in a systematic umbrella review of the principal relevant areas of research. PubMed, EMBASE and PsycINFO were searched using terms appropriate to each area of research, from their inception until December 2020. Systematic reviews, meta-analyses and large data-set analyses in the following areas were identified: serotonin and serotonin metabolite, 5-HIAA, concentrations in body fluids; serotonin 5-HT 1A receptor binding; serotonin transporter (SERT) levels measured by imaging or at post-mortem; tryptophan depletion studies; SERT gene associations and SERT gene-environment interactions. Studies of depression associated with physical conditions and specific subtypes of depression (e.g. bipolar depression) were excluded. Two independent reviewers extracted the data and assessed the quality of included studies using the AMSTAR-2, an adapted AMSTAR-2, or the STREGA for a large genetic study. The certainty of study results was assessed using a modified version of the GRADE. We did not synthesise results of individual meta-analyses because they included overlapping studies. The review was registered with PROSPERO (CRD42020207203). 17 studies were included: 12 systematic reviews and meta-analyses, 1 collaborative meta-analysis, 1 meta-analysis of large cohort studies, 1 systematic review and narrative synthesis, 1 genetic association study and 1 umbrella review. Quality of reviews was variable with some genetic studies of high quality. Two meta-analyses of overlapping studies examining the serotonin metabolite, 5-HIAA, showed no association with depression (largest n = 1002). One meta-analysis of cohort studies of plasma serotonin showed no relationship with depression, and evidence that lowered serotonin concentration was associated with antidepressant use ( n = 1869). Two meta-analyses of overlapping studies examining the 5-HT 1A receptor (largest n = 561), and three meta-analyses of overlapping studies examining SERT binding (largest n = 1845) showed weak and inconsistent evidence of reduced binding in some areas, which would be consistent with increased synaptic availability of serotonin in people with depression, if this was the original, causal abnormaly. However, effects of prior antidepressant use were not reliably excluded. One meta-analysis of tryptophan depletion studies found no effect in most healthy volunteers ( n = 566), but weak evidence of an effect in those with a family history of depression ( n = 75). Another systematic review ( n = 342) and a sample of ten subsequent studies ( n = 407) found no effect in volunteers. No systematic review of tryptophan depletion studies has been performed since 2007. The two largest and highest quality studies of the SERT gene, one genetic association study ( n = 115,257) and one collaborative meta-analysis ( n = 43,165), revealed no evidence of an association with depression, or of an interaction between genotype, stress and depression. The main areas of serotonin research provide no consistent evidence of there being an association between serotonin and depression, and no support for the hypothesis that depression is caused by lowered serotonin activity or concentrations. Some evidence was consistent with the possibility that long-term antidepressant use reduces serotonin concentration.
Similar content being viewed by others

Genetic contributions to brain serotonin transporter levels in healthy adults
The kynurenine pathway in major depressive disorder, bipolar disorder, and schizophrenia: a meta-analysis of 101 studies

The complex clinical response to selective serotonin reuptake inhibitors in depression: a network perspective
Introduction.
The idea that depression is the result of abnormalities in brain chemicals, particularly serotonin (5-hydroxytryptamine or 5-HT), has been influential for decades, and provides an important justification for the use of antidepressants. A link between lowered serotonin and depression was first suggested in the 1960s [ 1 ], and widely publicised from the 1990s with the advent of the Selective Serotonin Reuptake Inhibitor (SSRI) antidepressants [ 2 , 3 , 4 ]. Although it has been questioned more recently [ 5 , 6 ], the serotonin theory of depression remains influential, with principal English language textbooks still giving it qualified support [ 7 , 8 ], leading researchers endorsing it [ 9 , 10 , 11 ], and much empirical research based on it [ 11 , 12 , 13 , 14 ]. Surveys suggest that 80% or more of the general public now believe it is established that depression is caused by a ‘chemical imbalance’ [ 15 , 16 ]. Many general practitioners also subscribe to this view [ 17 ] and popular websites commonly cite the theory [ 18 ].
It is often assumed that the effects of antidepressants demonstrate that depression must be at least partially caused by a brain-based chemical abnormality, and that the apparent efficacy of SSRIs shows that serotonin is implicated. Other explanations for the effects of antidepressants have been put forward, however, including the idea that they work via an amplified placebo effect or through their ability to restrict or blunt emotions in general [ 19 , 20 ].
Despite the fact that the serotonin theory of depression has been so influential, no comprehensive review has yet synthesised the relevant evidence. We conducted an ‘umbrella’ review of the principal areas of relevant research, following the model of a similar review examining prospective biomarkers of major depressive disorder [ 21 ]. We sought to establish whether the current evidence supports a role for serotonin in the aetiology of depression, and specifically whether depression is associated with indications of lowered serotonin concentrations or activity.
Search strategy and selection criteria
The present umbrella review was reported in accordance with the 2009 PRISMA statement [ 22 ]. The protocol was registered with PROSPERO in December 2020 (registration number CRD42020207203) ( https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=207203 ). This was subsequently updated to reflect our decision to modify the quality rating system for some studies to more appropriately appraise their quality, and to include a modified GRADE to assess the overall certainty of the findings in each category of the umbrella review.
In order to cover the different areas and to manage the large volume of research that has been conducted on the serotonin system, we conducted an ‘umbrella’ review. Umbrella reviews survey existing systematic reviews and meta-analyses relevant to a research question and represent one of the highest levels of evidence synthesis available [ 23 ]. Although they are traditionally restricted to systematic reviews and meta-analyses, we aimed to identify the best evidence available. Therefore, we also included some large studies that combined data from individual studies but did not employ conventional systematic review methods, and one large genetic study. The latter used nationwide databases to capture more individuals than entire meta-analyses, so is likely to provide even more reliable evidence than syntheses of individual studies.
We first conducted a scoping review to identify areas of research consistently held to provide support for the serotonin hypothesis of depression. Six areas were identified, addressing the following questions: (1) Serotonin and the serotonin metabolite 5-HIAA–whether there are lower levels of serotonin and 5-HIAA in body fluids in depression; (2) Receptors - whether serotonin receptor levels are altered in people with depression; (3) The serotonin transporter (SERT) - whether there are higher levels of the serotonin transporter in people with depression (which would lower synaptic levels of serotonin); (4) Depletion studies - whether tryptophan depletion (which lowers available serotonin) can induce depression; (5) SERT gene – whether there are higher levels of the serotonin transporter gene in people with depression; (6) Whether there is an interaction between the SERT gene and stress in depression.
We searched for systematic reviews, meta-analyses, and large database studies in these six areas in PubMed, EMBASE and PsycINFO using the Healthcare Databases Advanced Search tool provided by Health Education England and NICE (National Institute for Health and Care Excellence). Searches were conducted until December 2020.
We used the following terms in all searches: (depress* OR affective OR mood) AND (systematic OR meta-analysis), and limited searches to title and abstract, since not doing so produced numerous irrelevant hits. In addition, we used terms specific to each area of research (full details are provided in Table S1 , Supplement). We also searched citations and consulted with experts.
Inclusion criteria were designed to identify the best available evidence in each research area and consisted of:
Research synthesis including systematic reviews, meta-analysis, umbrella reviews, individual patient meta-analysis and large dataset analysis.
Studies that involve people with depressive disorders or, for experimental studies (tryptophan depletion), those in which mood symptoms are measured as an outcome.
Studies of experimental procedures (tryptophan depletion) involving a sham or control condition.
Studies published in full in peer reviewed literature.
Where more than five systematic reviews or large analyses exist, the most recent five are included.
Exclusion criteria consisted of:
Animal studies.
Studies exclusively concerned with depression in physical conditions (e.g. post stroke or Parkinson’s disease) or exclusively focusing on specific subtypes of depression such as postpartum depression, depression in children, or depression in bipolar disorder.
No language or date restrictions were applied. In areas in which no systematic review or meta-analysis had been done within the last 10 years, we also selected the ten most recent studies at the time of searching (December 2020) for illustration of more recent findings. We performed this search using the same search string for this domain, without restricting it to systematic reviews and meta-analyses.
Data analysis
Each member of the team was allocated one to three domains of serotonin research to search and screen for eligible studies using abstract and full text review. In case of uncertainty, the entire team discussed eligibility to reach consensus.
For included studies, data were extracted by two reviewers working independently, and disagreement was resolved by consensus. Authors of papers were contacted for clarification when data was missing or unclear.
We extracted summary effects, confidence intervals and measures of statistical significance where these were reported, and, where relevant, we extracted data on heterogeneity. For summary effects in the non-genetic studies, preference was given to the extraction and reporting of effect sizes. Mean differences were converted to effect sizes where appropriate data were available.
We did not perform a meta-analysis of the individual meta-analyses in each area because they included overlapping studies [ 24 ]. All extracted data is presented in Table 1 . Sensitivity analyses were reported where they had substantial bearing on interpretation of findings.
The quality rating of systematic reviews and meta-analyses was assessed using AMSTAR-2 (A MeaSurement Tool to Assess systematic Reviews) [ 25 ]. For two studies that did not employ conventional systematic review methods [ 26 , 27 ] we used a modified version of the AMSTAR-2 (see Table S3 ). For the genetic association study based on a large database analysis we used the STREGA assessment (STrengthening the REporting of Genetic Association Studies) (Table S4 ) [ 28 ]. Each study was rated independently by at least two authors. We report ratings of individual items on the relevant measure, and the percentage of items that were adequately addressed by each study (Table 1 , with further detail in Tables S3 and S4 ).
Alongside quality ratings, two team members (JM, MAH) rated the certainty of the results of each study using a modified version of the GRADE guidelines [ 29 ]. Following the approach of Kennis et al. [ 21 ], we devised six criteria relevant to the included studies: whether a unified analysis was conducted on original data; whether confounding by antidepressant use was adequately addressed; whether outcomes were pre-specified; whether results were consistent or heterogeneity was adequately addressed if present; whether there was a likelihood of publication bias; and sample size. The importance of confounding by effects of current or past antidepressant use has been highlighted in several studies [ 30 , 31 ]. The results of each study were scored 1 or 0 according to whether they fulfilled each criteria, and based on these ratings an overall judgement was made about the certainty of evidence across studies in each of the six areas of research examined. The certainty of each study was based on an algorithm that prioritised sample size and uniform analysis using original data (explained more fully in the supplementary material), following suggestions that these are the key aspects of reliability [ 27 , 32 ]. An assessment of the overall certainty of each domain of research examining the role of serotonin was determined by consensus of at least two authors and a direction of effect indicated.
Search results and quality rating
Searching identified 361 publications across the 6 different areas of research, among which seventeen studies fulfilled inclusion criteria (see Fig. 1 and Table S1 for details of the selection process). Included studies, their characteristics and results are shown in Table 1 . As no systematic review or meta-analysis had been performed within the last 10 years on serotonin depletion, we also identified the 10 latest studies for illustration of more recent research findings (Table 2 ).
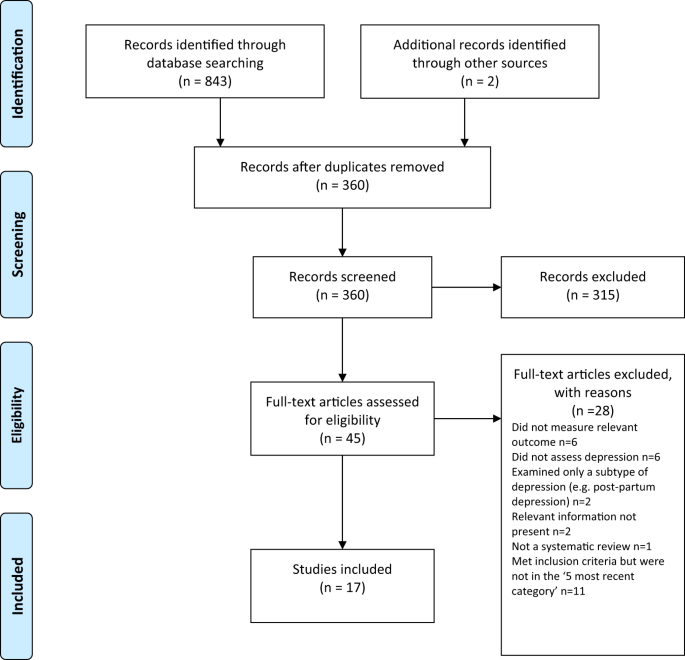
Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) flow diagramme.
Quality ratings are summarised in Table 1 and reported in detail in Tables S2 – S3 . The majority (11/17) of systematic reviews and meta-analyses satisfied less than 50% of criteria. Only 31% adequately assessed risk of bias in individual studies (a further 44% partially assessed this), and only 50% adequately accounted for risk of bias when interpreting the results of the review. One collaborative meta-analysis of genetic studies was considered to be of high quality due to the inclusion of several measures to ensure consistency and reliability [ 27 ]. The large genetic analysis of the effect of SERT polymorphisms on depression, satisfied 88% of the STREGA quality criteria [ 32 ].
Serotonin and 5-HIAA
Serotonin can be measured in blood, plasma, urine and CSF, but it is rapidly metabolised to 5-hydroxyindoleacetic acid (5-HIAA). CSF is thought to be the ideal resource for the study of biomarkers of putative brain diseases, since it is in contact with brain interstitial fluid [ 33 ]. However, collecting CSF samples is invasive and carries some risk, hence large-scale studies are scarce.
Three studies fulfilled inclusion criteria (Table 1 ). One meta-analysis of three large observational cohort studies of post-menopausal women, revealed lower levels of plasma 5-HT in women with depression, which did not, however, reach statistical significance of p < 0.05 after adjusting for multiple comparisons. Sensitivity analyses revealed that antidepressants were strongly associated with lower serotonin levels independently of depression.
Two meta-analyses of a total of 19 studies of 5-HIAA in CSF (seven studies were included in both) found no evidence of an association between 5-HIAA concentrations and depression.
Fourteen different serotonin receptors have been identified, with most research on depression focusing on the 5-HT 1A receptor [ 11 , 34 ]. Since the functions of other 5-HT receptors and their relationship to depression have not been well characterised, we restricted our analysis to data on 5-HT 1A receptors [ 11 , 34 ]. 5-HT 1A receptors, known as auto-receptors, inhibit the release of serotonin pre-synaptically [ 35 ], therefore, if depression is the result of reduced serotonin activity caused by abnormalities in the 5-HT 1A receptor, people with depression would be expected to show increased activity of 5-HT 1A receptors compared to those without [ 36 ].
Two meta-analyses satisfied inclusion criteria, involving five of the same studies [ 37 , 38 ] (see Table 1 ). The majority of results across the two analyses suggested either no difference in 5-HT 1A receptors between people with depression and controls, or a lower level of these inhibitory receptors, which would imply higher concentrations or activity of serotonin in people with depression. Both meta-analyses were based on studies that predominantly involved patients who were taking or had recently taken (within 1–3 weeks of scanning) antidepressants or other types of psychiatric medication, and both sets of authors commented on the possible influence of prior or current medication on findings. In addition, one analysis was of very low quality [ 37 ], including not reporting on the numbers involved in each analysis and using one-sided p-values, and one was strongly influenced by three studies and publication bias was present [ 38 ].
The serotonin transporter (SERT)
The serotonin transporter protein (SERT) transports serotonin out of the synapse, thereby lowering the availability of serotonin in the synapse [ 39 , 40 ]. Animals with an inactivated gene for SERT have higher levels of extra-cellular serotonin in the brain than normal [ 41 , 42 , 43 ] and SSRIs are thought to work by inhibiting the action of SERT, and thus increasing levels of serotonin in the synaptic cleft [ 44 ]. Although changes in SERT may be a marker for other abnormalities, if depression is caused by low serotonin availability or activity, and if SERT is the origin of that deficit, then the amount or activity of SERT would be expected to be higher in people with depression compared to those without [ 40 ]. SERT binding potential is an index of the concentration of the serotonin transporter protein and SERT concentrations can also be measured post-mortem.
Three overlapping meta-analyses based on a total of 40 individual studies fulfilled inclusion criteria (See Table 1 ) [ 37 , 39 , 45 ]. Overall, the data indicated possible reductions in SERT binding in some brain areas, although areas in which effects were detected were not consistent across the reviews. In addition, effects of antidepressants and other medication cannot be ruled out, since most included studies mainly or exclusively involved people who had a history of taking antidepressants or other psychiatric medications. Only one meta-analysis tested effects of antidepressants, and although results were not influenced by the percentage of drug-naïve patients in each study, numbers were small so it is unlikely that medication-related effects would have been reliably detected [ 45 ]. All three reviews cited evidence from animal studies that antidepressant treatment reduces SERT [ 46 , 47 , 48 ]. None of the analyses corrected for multiple testing, and one review was of very low quality [ 37 ]. If the results do represent a positive finding that is independent of medication, they would suggest that depression is associated with higher concentrations or activity of serotonin.
Depletion studies
Tryptophan depletion using dietary means or chemicals, such as parachlorophenylalanine (PCPA), is thought to reduce serotonin levels. Since PCPA is potentially toxic, reversible tryptophan depletion using an amino acid drink that lacks tryptophan is the most commonly used method and is thought to affect serotonin within 5–7 h of ingestion. Questions remain, however, about whether either method reliably reduces brain serotonin, and about other effects including changes in brain nitrous oxide, cerebrovascular changes, reduced BDNF and amino acid imbalances that may be produced by the manipulations and might explain observed effects independent of possible changes in serotonin activity [ 49 ].
One meta-analysis and one systematic review fulfilled inclusion criteria (see Table 1 ). Data from studies involving volunteers mostly showed no effect, including a meta-analysis of parallel group studies [ 50 ]. In a small meta-analysis of within-subject studies involving 75 people with a positive family history, a minor effect was found, with people given the active depletion showing a larger decrease in mood than those who had a sham procedure [ 50 ]. Across both reviews, studies involving people diagnosed with depression showed slightly greater mood reduction following tryptophan depletion than sham treatment overall, but most participants had taken or were taking antidepressants and participant numbers were small [ 50 , 51 ].
Since these research syntheses were conducted more than 10 years ago, we searched for a systematic sample of ten recently published studies (Table 2 ). Eight studies conducted with healthy volunteers showed no effects of tryptophan depletion on mood, including the only two parallel group studies. One study presented effects in people with and without a family history of depression, and no differences were apparent in either group [ 52 ]. Two cross-over studies involving people with depression and current or recent use of antidepressants showed no convincing effects of a depletion drink [ 53 , 54 ], although one study is reported as positive mainly due to finding an improvement in mood in the group given the sham drink [ 54 ].
SERT gene and gene-stress interactions
A possible link between depression and the repeat length polymorphism in the promoter region of the SERT gene (5-HTTLPR), specifically the presence of the short repeats version, which causes lower SERT mRNA expression, has been proposed [ 55 ]. Interestingly, lower levels of SERT would produce higher levels of synaptic serotonin. However, more recently, this hypothesis has been superseded by a focus on the interaction effect between this polymorphism, depression and stress, with the idea that the short version of the polymorphism may only give rise to depression in the presence of stressful life events [ 55 , 56 ]. Unlike other areas of serotonin research, numerous systematic reviews and meta-analyses of genetic studies have been conducted, and most recently a very large analysis based on a sample from two genetic databanks. Details of the five most recent studies that have addressed the association between the SERT gene and depression, and the interaction effect are detailed in Table 1 .
Although some earlier meta-analyses of case-control studies showed a statistically significant association between the 5-HTTLPR and depression in some ethnic groups [ 57 , 58 ], two recent large, high quality studies did not find an association between the SERT gene polymorphism and depression [ 27 , 32 ]. These two studies consist of by far the largest and most comprehensive study to date [ 32 ] and a high-quality meta-analysis that involved a consistent re-analysis of primary data across all conducted studies, including previously unpublished data, and other comprehensive quality checks [ 27 , 59 ] (see Table 1 ).
Similarly, early studies based on tens of thousands of participants suggested a statistically significant interaction between the SERT gene, forms of stress or maltreatment and depression [ 60 , 61 , 62 ], with a small odds ratio in the only study that reported this (1.18, 95% CI 1.09 to 1.28) [ 62 ]. However, the two recent large, high-quality studies did not find an interaction between the SERT gene and stress in depression (Border et al [ 32 ] and Culverhouse et al.) [ 27 ] (see Table 1 ).
Overall results
Table 3 presents the modified GRADE ratings for each study and the overall rating of the strength of evidence in each area. Areas of research that provided moderate or high certainty of evidence such as the studies of plasma serotonin and metabolites and the genetic and gene-stress interaction studies all showed no association between markers of serotonin activity and depression. Some other areas suggested findings consistent with increased serotonin activity, but evidence was of very low certainty, mainly due to small sample sizes and possible residual confounding by current or past antidepressant use. One area - the tryptophan depletion studies - showed very low certainty evidence of lowered serotonin activity or availability in a subgroup of volunteers with a family history of depression. This evidence was considered very low certainty as it derived from a subgroup of within-subject studies, numbers were small, and there was no information on medication use, which may have influenced results. Subsequent research has not confirmed an effect with numerous negative studies in volunteers.
Our comprehensive review of the major strands of research on serotonin shows there is no convincing evidence that depression is associated with, or caused by, lower serotonin concentrations or activity. Most studies found no evidence of reduced serotonin activity in people with depression compared to people without, and methods to reduce serotonin availability using tryptophan depletion do not consistently lower mood in volunteers. High quality, well-powered genetic studies effectively exclude an association between genotypes related to the serotonin system and depression, including a proposed interaction with stress. Weak evidence from some studies of serotonin 5-HT 1A receptors and levels of SERT points towards a possible association between increased serotonin activity and depression. However, these results are likely to be influenced by prior use of antidepressants and its effects on the serotonin system [ 30 , 31 ]. The effects of tryptophan depletion in some cross-over studies involving people with depression may also be mediated by antidepressants, although these are not consistently found [ 63 ].
The chemical imbalance theory of depression is still put forward by professionals [ 17 ], and the serotonin theory, in particular, has formed the basis of a considerable research effort over the last few decades [ 14 ]. The general public widely believes that depression has been convincingly demonstrated to be the result of serotonin or other chemical abnormalities [ 15 , 16 ], and this belief shapes how people understand their moods, leading to a pessimistic outlook on the outcome of depression and negative expectancies about the possibility of self-regulation of mood [ 64 , 65 , 66 ]. The idea that depression is the result of a chemical imbalance also influences decisions about whether to take or continue antidepressant medication and may discourage people from discontinuing treatment, potentially leading to lifelong dependence on these drugs [ 67 , 68 ].
As with all research synthesis, the findings of this umbrella review are dependent on the quality of the included studies, and susceptible to their limitations. Most of the included studies were rated as low quality on the AMSTAR-2, but the GRADE approach suggested some findings were reasonably robust. Most of the non-genetic studies did not reliably exclude the potential effects of previous antidepressant use and were based on relatively small numbers of participants. The genetic studies, in particular, illustrate the importance of methodological rigour and sample size. Whereas some earlier, lower quality, mostly smaller studies produced marginally positive findings, these were not confirmed in better-conducted, larger and more recent studies [ 27 , 32 ]. The identification of depression and assessment of confounders and interaction effects were limited by the data available in the original studies on which the included reviews and meta-analyses were based. Common methods such as the categorisation of continuous measures and application of linear models to non-linear data may have led to over-estimation or under-estimation of effects [ 69 , 70 ], including the interaction between stress and the SERT gene. The latest systematic review of tryptophan depletion studies was conducted in 2007, and there has been considerable research produced since then. Hence, we provided a snapshot of the most recent evidence at the time of writing, but this area requires an up to date, comprehensive data synthesis. However, the recent studies were consistent with the earlier meta-analysis with little evidence for an effect of tryptophan depletion on mood.
Although umbrella reviews typically restrict themselves to systematic reviews and meta-analyses, we aimed to provide the most comprehensive possible overview. Therefore, we chose to include meta-analyses that did not involve a systematic review and a large genetic association study on the premise that these studies contribute important data on the question of whether the serotonin hypothesis of depression is supported. As a result, the AMSTAR-2 quality rating scale, designed to evaluate the quality of conventional systematic reviews, was not easily applicable to all studies and had to be modified or replaced in some cases.
One study in this review found that antidepressant use was associated with a reduction of plasma serotonin [ 26 ], and it is possible that the evidence for reductions in SERT density and 5-HT 1A receptors in some of the included imaging study reviews may reflect compensatory adaptations to serotonin-lowering effects of prior antidepressant use. Authors of one meta-analysis also highlighted evidence of 5-HIAA levels being reduced after long-term antidepressant treatment [ 71 ]. These findings suggest that in the long-term antidepressants might produce compensatory changes [ 72 ] that are opposite to their acute effects [ 73 , 74 ]. Lowered serotonin availability has also been demonstrated in animal studies following prolonged antidepressant administration [ 75 ]. Further research is required to clarify the effects of different drugs on neurochemical systems, including the serotonin system, especially during and after long-term use, as well as the physical and psychological consequences of such effects.
This review suggests that the huge research effort based on the serotonin hypothesis has not produced convincing evidence of a biochemical basis to depression. This is consistent with research on many other biological markers [ 21 ]. We suggest it is time to acknowledge that the serotonin theory of depression is not empirically substantiated.
Data availability
All extracted data is available in the paper and supplementary materials. Further information about the decision-making for each rating for categories of the AMSTAR-2 and STREGA are available on request.
Coppen A. The biochemistry of affective disorders. Br J Psychiatry. 1967;113:1237–64.
CAS PubMed Google Scholar
American Psychiatric Association. What Is Psychiatry? 2021. https://www.psychiatry.org/patients-families/what-is-psychiatry-menu .
GlaxoSmithKline. Paxil XR. 2009. www.Paxilcr.com (site no longer available). Last accessed 27th Jan 2009.
Eli Lilly. Prozac - How it works. 2006. www.prozac.com/how_prozac/how_it_works.jsp?reqNavId=2.2 . (site no longer available). Last accessed 10th Feb 2006.
Healy D. Serotonin and depression. BMJ: Br Med J. 2015;350:h1771.
Google Scholar
Pies R. Psychiatry’s New Brain-Mind and the Legend of the “Chemical Imbalance.” 2011. https://www.psychiatrictimes.com/view/psychiatrys-new-brain-mind-and-legend-chemical-imbalance . Accessed March 2, 2021.
Geddes JR, Andreasen NC, Goodwin GM. New Oxford Textbook of Psychiatry. Oxford, UK: Oxford University Press; 2020.
Sadock BJ, Sadock VA, Ruiz P. Kaplan & Sadock’s Comprehensive Textbook of Psychiatry. 10th Editi. Lippincott Williams & Wilkins (LWW); 2017.
Cowen PJ, Browning M. What has serotonin to do with depression? World Psychiatry. 2015;14:158–60.
PubMed PubMed Central Google Scholar
Harmer CJ, Duman RS, Cowen PJ. How do antidepressants work? New perspectives for refining future treatment approaches. Lancet Psychiatry. 2017;4:409–18.
Yohn CN, Gergues MM, Samuels BA. The role of 5-HT receptors in depression. Mol Brain. 2017;10:28.
Hahn A, Haeusler D, Kraus C, Höflich AS, Kranz GS, Baldinger P, et al. Attenuated serotonin transporter association between dorsal raphe and ventral striatum in major depression. Hum Brain Mapp. 2014;35:3857–66.
Amidfar M, Colic L, Kim MWAY-K. Biomarkers of major depression related to serotonin receptors. Curr Psychiatry Rev. 2018;14:239–44.
CAS Google Scholar
Albert PR, Benkelfat C, Descarries L. The neurobiology of depression—revisiting the serotonin hypothesis. I. Cellular and molecular mechanisms. Philos Trans R Soc Lond B Biol Sci. 2012;367:2378–81.
CAS PubMed PubMed Central Google Scholar
Pilkington PD, Reavley NJ, Jorm AF. The Australian public’s beliefs about the causes of depression: associated factors and changes over 16 years. J Affect Disord. 2013;150:356–62.
PubMed Google Scholar
Pescosolido BA, Martin JK, Long JS, Medina TR, Phelan JC, Link BG. A disease like any other? A decade of change in public reactions to schizophrenia, depression, and alcohol dependence. Am J Psychiatry. 2010;167:1321–30.
Read J, Renton J, Harrop C, Geekie J, Dowrick C. A survey of UK general practitioners about depression, antidepressants and withdrawal: implementing the 2019 Public Health England report. Therapeutic Advances in. Psychopharmacology. 2020;10:204512532095012.
Demasi M, Gøtzsche PC. Presentation of benefits and harms of antidepressants on websites: A cross-sectional study. Int J Risk Saf Med. 2020;31:53–65.
Jakobsen JC, Gluud C, Kirsch I. Should antidepressants be used for major depressive disorder? BMJ Evidence-Based. Medicine. 2020;25:130–130.
Moncrieff J, Cohen D. Do antidepressants cure or create abnormal brain states? PLoS Med. 2006;3:e240.
Kennis M, Gerritsen L, van Dalen M, Williams A, Cuijpers P, Bockting C. Prospective biomarkers of major depressive disorder: a systematic review and meta-analysis. Mol Psychiatry. 2020;25:321–38.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
Fusar-Poli P, Radua J. Ten simple rules for conducting umbrella reviews. Evid Based Ment Health. 2018;21:95–100.
Pollock M, Fernandes RM, Becker LA, Pieper D, Hartling L. Chapter V: Overviews of Reviews. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al., editors. Cochrane Handbook for Systematic Reviews of Interventions version 6.2,. version 6.Cochrane; 2021.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
Huang T, Balasubramanian R, Yao Y, Clish CB, Shadyab AH, Liu B, et al. Associations of depression status with plasma levels of candidate lipid and amino acid metabolites: a meta-analysis of individual data from three independent samples of US postmenopausal women. Mol Psychiatry. 2020;2020. https://doi.org/10.1038/s41380-020-00870-9 .
Culverhouse RC, Saccone NL, Horton AC, Ma Y, Anstey KJ, Banaschewski T, et al. Collaborative meta-analysis finds no evidence of a strong interaction between stress and 5-HTTLPR genotype contributing to the development of depression. Mol Psychiatry. 2018;23:133–42.
Little J, Higgins JPT, Ioannidis JPA, Moher D, Gagnon F, von Elm E, et al. STrengthening the REporting of Genetic Association Studies (STREGA)— An Extension of the STROBE Statement. PLoS Med. 2009;6:e1000022.
Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck-Ytter Y, Schünemann HJ. What is quality of evidence and why is it important to clinicians? BMJ. 2008;336:995–8.
Yoon HS, Hattori K, Ogawa S, Sasayama D, Ota M, Teraishi T, et al. Relationships of cerebrospinal fluid monoamine metabolite levels with clinical variables in major depressive disorder. J Clin Psychiatry. 2017;78:e947–56.
Kugaya A, Seneca NM, Snyder PJ, Williams SA, Malison RT, Baldwin RM, et al. Changes in human in vivo serotonin and dopamine transporter availabilities during chronic antidepressant administration. Neuropsychopharmacology. 2003;28:413–20.
Border R, Johnson EC, Evans LM, Smolen A, Berley N, Sullivan PF, et al. No support for historical candidate gene or candidate gene-by-interaction hypotheses for major depression across multiple large samples. Am J Psychiatry. 2019;176:376–87.
Ogawa S, Tsuchimine S, Kunugi H. Cerebrospinal fluid monoamine metabolite concentrations in depressive disorder: A meta-analysis of historic evidence. J Psychiatr Res. 2018;105:137–46.
Nautiyal KM, Hen R. Serotonin receptors in depression: from A to B. F1000Res. 2017;6:123.
Rojas PS, Neira D, Muñoz M, Lavandero S, Fiedler JL. Serotonin (5‐HT) regulates neurite outgrowth through 5‐HT1A and 5‐HT7 receptors in cultured hippocampal neurons. J Neurosci Res. 2014;92:1000–9.
Kaufman J, DeLorenzo C, Choudhury S, Parsey RV. The 5-HT1A receptor in Major Depressive Disorder. Eur Neuropsychopharmacol. 2016;26:397–410.
Nikolaus S, Müller H-W, Hautzel H. Different patterns of 5-HT receptor and transporter dysfunction in neuropsychiatric disorders – a comparative analysis of in vivo imaging findings. Rev Neurosci. 2016;27:27–59.
Wang L, Zhou C, Zhu D, Wang X, Fang L, Zhong J, et al. Serotonin-1A receptor alterations in depression: A meta-analysis of molecular imaging studies. BMC Psychiatry. 2016;16:1–9.
Kambeitz JP, Howes OD. The serotonin transporter in depression: Meta-analysis of in vivo and post mortem findings and implications for understanding and treating depression. J Affect Disord. 2015;186:358–66.
Meyer JH. Imaging the serotonin transporter during major depressive disorder and antidepressant treatment. J Psychiatry Neurosci. 2007;32:86–102.
Mathews TA, Fedele DE, Coppelli FM, Avila AM, Murphy DL, Andrews AM. Gene dose-dependent alterations in extraneuronal serotonin but not dopamine in mice with reduced serotonin transporter expression. J Neurosci Methods. 2004;140:169–81.
Shen H-W, Hagino Y, Kobayashi H, Shinohara-Tanaka K, Ikeda K, Yamamoto H, et al. Regional differences in extracellular dopamine and serotonin assessed by in vivo microdialysis in mice lacking dopamine and/or serotonin transporters. Neuropsychopharmacology. 2004;29:1790–9.
Hagino Y, Takamatsu Y, Yamamoto H, Iwamura T, Murphy DL, Uhl GR, et al. Effects of MDMA on extracellular dopamine and serotonin levels in mice lacking dopamine and/or serotonin transporters. Curr Neuropharmacol. 2011;9:91–5.
Zhou Z, Zhen J, Karpowich NK, Law CJ, Reith MEA, Wang D-N. Antidepressant specificity of serotonin transporter suggested by three LeuT-SSRI structures. Nat Struct Mol Biol. 2009;16:652–7.
Gryglewski G, Lanzenberger R, Kranz GS, Cumming P. Meta-analysis of molecular imaging of serotonin transporters in major depression. J Cereb Blood Flow Metab. 2014;34:1096–103.
Benmansour S, Owens WA, Cecchi M, Morilak DA, Frazer A. Serotonin clearance in vivo is altered to a greater extent by antidepressant-induced downregulation of the serotonin transporter than by acute blockade of this transporter. J Neurosci. 2002;22:6766–72.
Benmansour S, Cecchi M, Morilak DA, Gerhardt GA, Javors MA, Gould GG, et al. Effects of chronic antidepressant treatments on serotonin transporter function, density, and mRNA level. J Neurosci. 1999;19:10494–501.
Horschitz S, Hummerich R, Schloss P. Down-regulation of the rat serotonin transporter upon exposure to a selective serotonin reuptake inhibitor. Neuroreport. 2001;12:2181–4.
Young SN. Acute tryptophan depletion in humans: a review of theoretical, practical and ethical aspects. J Psychiatry Neurosci. 2013;38:294–305.
Ruhe HG, Mason NS, Schene AH. Mood is indirectly related to serotonin, norepinephrine and dopamine levels in humans: a meta-analysis of monoamine depletion studies. Mol Psychiatry. 2007;12:331–59.
Fusar-Poli P, Allen P, McGuire P, Placentino A, Cortesi M, Perez J. Neuroimaging and electrophysiological studies of the effects of acute tryptophan depletion: A systematic review of the literature. Psychopharmacology. 2006;188:131–43.
Hogenelst K, Schoevers RA, Kema IP, Sweep FCGJ, aan het Rot M. Empathic accuracy and oxytocin after tryptophan depletion in adults at risk for depression. Psychopharmacology. 2016;233:111–20.
Weinstein JJ, Rogers BP, Taylor WD, Boyd BD, Cowan RL, Shelton KM, et al. Effects of acute tryptophan depletion on raphé functional connectivity in depression. Psychiatry Res. 2015;234:164–71.
Moreno FA, Erickson RP, Garriock HA, Gelernter J, Mintz J, Oas-Terpstra J, et al. Association study of genotype by depressive response during tryptophan depletion in subjects recovered from major depression. Mol. Neuropsychiatry. 2015;1:165–74.
Munafò MR. The serotonin transporter gene and depression. Depress Anxiety. 2012;29:915–7.
Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science 2003;301:386–9.
ADS CAS PubMed Google Scholar
Kiyohara C, Yoshimasu K. Association between major depressive disorder and a functional polymorphism of the 5-hydroxytryptamine (serotonin) transporter gene: A meta-analysis. Psychiatr Genet. 2010;20:49–58.
Oo KZ, Aung YK, Jenkins MA, Win AK. Associations of 5HTTLPR polymorphism with major depressive disorder and alcohol dependence: A systematic review and meta-analysis. Aust N. Z J Psychiatry. 2016;50:842–57.
Culverhouse RC, Bowes L, Breslau N, Nurnberger JI, Burmeister M, Fergusson DM, et al. Protocol for a collaborative meta-analysis of 5-HTTLPR, stress, and depression. BMC Psychiatry. 2013;13:1–12.
Karg K, Burmeister M, Shedden K, Sen S. The serotonin transporter promoter variant (5-HTTLPR), stress, and depression meta-analysis revisited. Arch Gen Psychiatry. 2011;68:444.
Sharpley CF, Palanisamy SKA, Glyde NS, Dillingham PW, Agnew LL. An update on the interaction between the serotonin transporter promoter variant (5-HTTLPR), stress and depression, plus an exploration of non-confirming findings. Behav Brain Res. 2014;273:89–105.
Bleys D, Luyten P, Soenens B, Claes S. Gene-environment interactions between stress and 5-HTTLPR in depression: A meta-analytic update. J Affect Disord. 2018;226:339–45.
Delgado PL. Monoamine depletion studies: implications for antidepressant discontinuation syndrome. J Clin Psychiatry. 2006;67:22–26.
Kemp JJ, Lickel JJ, Deacon BJ. Effects of a chemical imbalance causal explanation on individuals’ perceptions of their depressive symptoms. Behav Res Ther. 2014;56:47–52.
Lebowitz MS, Ahn W-K, Nolen-Hoeksema S. Fixable or fate? Perceptions of the biology of depression. J Consult Clin Psychol. 2013;81:518.
Zimmermann M, Papa A. Causal explanations of depression and treatment credibility in adults with untreated depression: Examining attribution theory. Psychol Psychother. 2020;93:537–54.
Maund E, Dewar-Haggart R, Williams S, Bowers H, Geraghty AWA, Leydon G, et al. Barriers and facilitators to discontinuing antidepressant use: A systematic review and thematic synthesis. J Affect Disord. 2019;245:38–62.
Eveleigh R, Speckens A, van Weel C, Oude Voshaar R, Lucassen P. Patients’ attitudes to discontinuing not-indicated long-term antidepressant use: barriers and facilitators. Therapeutic Advances in. Psychopharmacology. 2019;9:204512531987234.
Harrell FE Jr. Regression Modeling Strategies: With Applications to Linear Models, Logistic and Ordinal Regression, and Survival Analysis. Springer, Cham; 2015.
Schafer JL, Kang J. Average causal effects from nonrandomized studies: a practical guide and simulated example. Psychol Methods. 2008;13:279–313.
Pech J, Forman J, Kessing LV, Knorr U. Poor evidence for putative abnormalities in cerebrospinal fluid neurotransmitters in patients with depression versus healthy non-psychiatric individuals: A systematic review and meta-analyses of 23 studies. J Affect Disord. 2018;240:6–16.
Fava GA. May antidepressant drugs worsen the conditions they are supposed to treat? The clinical foundations of the oppositional model of tolerance. Therapeutic Adv Psychopharmacol. 2020;10:2045125320970325.
Kitaichi Y, Inoue T, Nakagawa S, Boku S, Kakuta A, Izumi T, et al. Sertraline increases extracellular levels not only of serotonin, but also of dopamine in the nucleus accumbens and striatum of rats. Eur J Pharm. 2010;647:90–6.
Gartside SE, Umbers V, Hajós M, Sharp T. Interaction between a selective 5‐HT1Areceptor antagonist and an SSRI in vivo: effects on 5‐HT cell firing and extracellular 5‐HT. Br J Pharmacol. 1995;115:1064–70.
Bosker FJ, Tanke MAC, Jongsma ME, Cremers TIFH, Jagtman E, Pietersen CY, et al. Biochemical and behavioral effects of long-term citalopram administration and discontinuation in rats: role of serotonin synthesis. Neurochem Int. 2010;57:948–57.
Download references
There was no specific funding for this review. MAH is supported by a Clinical Research Fellowship from North East London NHS Foundation Trust (NELFT). This funder had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Author information
Authors and affiliations.
Division of Psychiatry, University College London, London, UK
Joanna Moncrieff & Mark A. Horowitz
Research and Development Department, Goodmayes Hospital, North East London NHS Foundation Trust, Essex, UK
Faculty of Education, Health and Human Sciences, University of Greenwich, London, UK
Ruth E. Cooper
Psychiatry-UK, Cornwall, UK
Tom Stockmann
Department of Dynamic and Clinical Psychology, and Health Studies, Faculty of Medicine and Psychology, Sapienza University of Rome, Rome, Italy
Simone Amendola
Department of Applied Psychology, Zurich University of Applied Sciences, Zurich, Switzerland
Michael P. Hengartner
You can also search for this author in PubMed Google Scholar
Contributions
JM conceived the idea for the study. JM, MAH, MPH, TS and SA designed the study. JM, MAH, MPH, TS, and SA screened articles and abstracted data. JM drafted the first version of the manuscript. JM, MAH, MPH, TS, SA, and REC contributed to the manuscript’s revision and interpretation of findings. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Corresponding author
Correspondence to Joanna Moncrieff .
Ethics declarations
Competing interests.
All authors have completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author). SA declares no conflicts of interest. MAH reports being co-founder of a company in April 2022, aiming to help people safely stop antidepressants in Canada. MPH reports royalties from Palgrave Macmillan, London, UK for his book published in December, 2021, called “Evidence-biased Antidepressant Prescription.” JM receives royalties for books about psychiatric drugs, reports grants from the National Institute of Health Research outside the submitted work, that she is co-chairperson of the Critical Psychiatry Network (an informal group of psychiatrists) and a board member of the unfunded organisation, the Council for Evidence-based Psychiatry. Both are unpaid positions. TS is co-chairperson of the Critical Psychiatry Network. RC is an unpaid board member of the International Institute for Psychiatric Drug Withdrawal.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary tables, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Moncrieff, J., Cooper, R.E., Stockmann, T. et al. The serotonin theory of depression: a systematic umbrella review of the evidence. Mol Psychiatry 28 , 3243–3256 (2023). https://doi.org/10.1038/s41380-022-01661-0
Download citation
Received : 21 June 2021
Revised : 31 May 2022
Accepted : 07 June 2022
Published : 20 July 2022
Issue Date : August 2023
DOI : https://doi.org/10.1038/s41380-022-01661-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
The involvement of serotonin in major depression: nescience in disguise.
- Danilo Arnone
- Catherine J. Harmer
Molecular Psychiatry (2024)
Serotonin effects on human iPSC-derived neural cell functions: from mitochondria to depression
- Iseline Cardon
- Sonja Grobecker
- Christian H. Wetzel
Neither serotonin disorder is at the core of depression nor dopamine at the core of schizophrenia; still these are biologically based mental disorders
- Konstantinos N. Fountoulakis
- Eva Maria Tsapakis
The impact of adult neurogenesis on affective functions: of mice and men
- Mariana Alonso
- Anne-Cécile Petit
- Pierre-Marie Lledo
Biallelic variants identified in 36 Pakistani families and trios with autism spectrum disorder
- Ricardo Harripaul
- John B. Vincent
Scientific Reports (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
July 20, 2022
Depression is probably not caused by a chemical imbalance in the brain, says new study
by Joanna Moncrieff and Mark Horowitz, The Conversation

For three decades, people have been deluged with information suggesting that depression is caused by a "chemical imbalance" in the brain—namely an imbalance of a brain chemical called serotonin. However, our latest research review shows that the evidence does not support it.
Although first proposed in the 1960s , the serotonin theory of depression started to be widely promoted by the pharmaceutical industry in the 1990s in association with its efforts to market a new range of antidepressants, known as selective serotonin-reuptake inhibitors or SSRIs. The idea was also endorsed by official institutions such as the American Psychiatric Association, which still tells the public that "differences in certain chemicals in the brain may contribute to symptoms of depression."
Countless doctors have repeated the message all over the world, in their private surgeries and in the media. People accepted what they were told. And many started taking antidepressants because they believed they had something wrong with their brain that required an antidepressant to put right. In the period of this marketing push, antidepressant use climbed dramatically, and they are now prescribed to one in six of the adult population in England , for example.
For a long time, certain academics , including some leading psychiatrists , have suggested that there is no satisfactory evidence to support the idea that depression is a result of abnormally low or inactive serotonin. Others continue to endorse the theory . Until now, however, there has been no comprehensive review of the research on serotonin and depression that could enable firm conclusions either way.
At first sight, the fact that SSRI-type antidepressants act on the serotonin system appears to support the serotonin theory of depression. SSRIs temporarily increase the availability of serotonin in the brain, but this does not necessarily imply that depression is caused by the opposite of this effect.
There are other explanations for antidepressants' effects. In fact, drug trials show that antidepressants are barely distinguishable from a placebo (dummy pill) when it comes to treating depression. Also, antidepressants appear to have a generalized emotion-numbing effect which may influence people's moods, although we do not know how this effect is produced or much about it.
First comprehensive review
There has been extensive research on the serotonin system since the 1990s, but it has not been collected systematically before. We conducted an "umbrella" review that involved systematically identifying and collating existing overviews of the evidence from each of the main areas of research into serotonin and depression. Although there have been systematic reviews of individual areas in the past, none have combined the evidence from all the different areas taking this approach.
One area of research we included was research comparing levels of serotonin and its breakdown products in the blood or brain fluid. Overall, this research did not show a difference between people with depression and those without depression.
Another area of research has focused on serotonin receptors , which are proteins on the ends of the nerves that serotonin links up with and which can transmit or inhibit serotonin's effects. Research on the most commonly investigated serotonin receptor suggested either no difference between people with depression and people without depression, or that serotonin activity was actually increased in people with depression—the opposite of the serotonin theory's prediction.
Research on the serotonin "transporter" , that is the protein which helps to terminate the effect of serotonin (this is the protein that SSRIs act on), also suggested that, if anything, there was increased serotonin activity in people with depression. However, these findings may be explained by the fact that many participants in these studies had used or were currently using antidepressants.
We also looked at research that explored whether depression can be induced in volunteers by artificially lowering levels of serotonin . Two systematic reviews from 2006 and 2007 and a sample of the ten most recent studies (at the time the current research was conducted) found that lowering serotonin did not produce depression in hundreds of healthy volunteers. One of the reviews showed very weak evidence of an effect in a small subgroup of people with a family history of depression, but this only involved 75 participants.
Very large studies involving tens of thousands of patients looked at gene variation , including the gene that has the instructions for making the serotonin transporter . They found no difference in the frequency of varieties of this gene between people with depression and healthy controls.
Although a famous early study found a relationship between the serotonin transporter gene and stressful life events , larger, more comprehensive studies suggest no such relationship exists. Stressful life events in themselves, however, exerted a strong effect on people's subsequent risk of developing depression.
Some of the studies in our overview that included people who were taking or had previously taken antidepressants showed evidence that antidepressants may actually lower the concentration or activity of serotonin.
Not supported by the evidence
The serotonin theory of depression has been one of the most influential and extensively researched biological theories of the origins of depression. Our study shows that this view is not supported by scientific evidence. It also calls into question the basis for the use of antidepressants.
Most antidepressants now in use are presumed to act via their effects on serotonin. Some also affect the brain chemical noradrenaline. But experts agree that the evidence for the involvement of noradrenaline in depression is weaker than that for serotonin .
There is no other accepted pharmacological mechanism for how antidepressants might affect depression. If antidepressants exert their effects as placebos, or by numbing emotions, then it is not clear that they do more good than harm.
Although viewing depression as a biological disorder may seem like it would reduce stigma, in fact, research has shown the opposite, and also that people who believe their own depression is due to a chemical imbalance are more pessimistic about their chances of recovery.
It is important that people know that the idea that depression results from a "chemical imbalance" is hypothetical. And we do not understand what temporarily elevating serotonin or other biochemical changes produced by antidepressants do to the brain. We conclude that it is impossible to say that taking SSRI antidepressants is worthwhile, or even completely safe. People need all this information to make informed decisions about whether or not to take antidepressants.
Explore further
Feedback to editors

Study in Haiti suggests early-onset heart failure is prevalent form of heart disease in low-income countries
38 minutes ago

AI algorithms can determine how well newborns nurse, study shows

Kaposi sarcoma discovery and mouse model could facilitate drug development

Immune cell interaction study unlocks novel treatment targets for chikungunya virus

New method rapidly reveals how protein modifications power T cells

Protein responsible for genetic inflammatory disease identified
3 hours ago

Brain function of older adults catching up with younger generations, finds study

Stem cells improve memory, reduce inflammation in Alzheimer's mouse brains

Laws requiring doctors to report a dementia diagnosis to the DMV may backfire

Researchers explore new cell target for cystic fibrosis treatment
4 hours ago
Related Stories

No evidence that depression is caused by low serotonin levels, finds comprehensive review
Jul 20, 2022

Serotonin transporters increase when depression fades, study shows
May 10, 2021

The effect of taking antidepressants during pregnancy
Dec 16, 2019

New drug can ease the side effects of medication against severe depression
Mar 20, 2020

Common antidepressants won't raise risk for bleeding strokes, shows new study
Feb 26, 2021

Study focuses on atomic structure of the serotonin transporter bound to SSRIs
Jan 29, 2018
Recommended for you

Study suggests that stevia is the most brain-compatible sugar substitute
5 hours ago

Nature's nudge: Study shows green views lead to healthier food choices

After 25 years, researchers uncover genetic cause of rare neurological disease
12 hours ago

Researchers look at genetic clues to depression in more than 14,000 people
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2023 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
The Evidence Is In: Depression Might Not Be Linked to Low Serotonin After All
Claire Gillespie is a freelance writer specializing in mental health. She’s written for The Washington Post, Vice, Health, Women’s Health, SELF, The Huffington Post, and many more.
:max_bytes(150000):strip_icc():format(webp)/Claire_Gillespie_headshot-649830869f1e4a4ca8979b90a304ffa0.jpg)
Karen Cilli is a fact-checker for Verywell Mind. She has an extensive background in research, with 33 years of experience as a reference librarian and educator.
:max_bytes(150000):strip_icc():format(webp)/IMG_20180323_155727-dd779be58f484850bd9352fa78b81eb0.jpeg)
blackCAT / Getty Images
Key Takeaways
- The so-called "serotonin theory" claims that the activity or levels of serotonin in the brain are responsible for depression.
- A major review of prior research says there is no convincing evidence to support this theory.
- Many people take antidepressants because they've been led to believe in a biochemical cause for depression, but this review calls into question what antidepressants actually do.
A new review of prior research on depression is causing a stir in the medical community. Led by University College London (UCL), scientists found no clear evidence that serotonin levels or serotonin activity are responsible for depression.
Published in Molecular Psychiatry, the findings come after decades of scrutinizing existing meta-analyses and systematic reviews. Researchers suggest that depression is not likely caused by a chemical imbalance in the brain, and challenge the role of antidepressants as the first line of treatment.
“For decades people have been given the impression that the idea that depression is caused by low serotonin is an established scientific fact,” says lead author Professor Joanna Moncrieff, a Professor of Psychiatry at UCL.
This idea or hypothesis was the original justification for the use of modern antidepressants (selective serotonin reuptake inhibitors, known as SSRIs ) and the pharmaceutical industry heavily promoted it in the 1990s and 2000s, Moncrieff explains. “Many scientists have known that the evidence to support it was weak and contradictory but because no one had done a systematic overview of the evidence before, it was difficult to say whether it was or wasn’t true,” she adds.
Keeping It in Perspective
While the results of this study are certainly significant, it doesn't negate the effectiveness of antidepressants for many people, nor does it mean you should stop taking them. More research is needed in addition to expanded education around alternative methods for managing depression.
A Closer Look at the Review
The studies involved in the review included tens of thousands of participants and adopted several different approaches to the relationship between serotonin and depression.
Research comparing levels of serotonin and its breakdown products in the blood or brain fluids did not find a difference between people diagnosed with depression and healthy control (comparison) participants.
Joanna Moncrieff
The current study allows us to come to a proper evidence-based verdict on the serotonin theory of depression, which we believe is important for the scientific community and for the general public.
The team also analyzed studies involving hundreds of participants whose serotonin levels were artificially lowered by withdrawing the amino acid required to make serotonin from their diets. A 2007 meta-analysis and a sample of recent studies found that this method of reducing serotonin levels didn’t cause depression in healthy participants, discrediting a link between serotonin deficiency and the condition.
Several large studies looked at gene variation, including the serotonin transporter gene, but they identified no difference in the genes of people with depression and healthy controls.
Many studies considered how stressful life events impact the risk of depression and found that people who had experienced more stressful life events were more likely to have depression.
“The current study allows us to come to a proper evidence-based verdict on the serotonin theory of depression, which we believe is important for the scientific community and for the general public,” Moncrieff says.
What Does This Mean for Depression Care?
The bottom line is that we can't say for certain that antidepressants work in the way that most people have been led to believe, says Moncrieff. "That is, they do not correct an underlying serotonin deficiency or abnormality, because the latter has not been demonstrated," she explains.
Aron Tendler, MD, C.BSM, BrainsWay Chief Medical Officer, says that while the recent review challenges the serotonin theory, it doesn't challenge the efficacy of mental health treatment .
Aron Tendler, MD, C.BSM
This review reminds all scientists to be humble and focus on the data rather than the theory.
"Many psychiatrists and neuroscientists suspected that serotonin theory was invalid from the NIMH-funded Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study, which was completed in 2004, or even before that," Dr. Tendler says.
He points out that this is why there are different classes of antidepressants that work on other neurotransmitters, plus other treatments such as psychotherapy, transcranial magnetic stimulation, and electroconvulsive therapy .
"This review reminds all scientists to be humble and focus on the data rather than the theory," Dr. Tendler adds.
A New Understanding of Depression?
Moncrieff hopes that rather than throw yet more money at trying to find the ever elusive chemical origins of depression , the medical community will accept that depression is not a biological state but an emotional reaction to difficult life circumstances and past experiences.
"There is strong evidence that adverse life events, such as divorce, poverty, debt, loneliness, child abuse, unemployment, etc, make people more vulnerable to depression," Moncrieff says. "What this means is that we should stop seeing depression as a medical condition and view it as a human reaction. Of course the brain is involved in depression, as it is involved in all our moods and actions. But that does not mean that we can find the origin of depression in the brain, or even a part of its origin."
Mental health treatment that is tailored to each individual is key, Moncrieff says, because every case involves a different set of difficult circumstances.
"Things like exercise and psychological therapy may have some general use and have shown to be effective," she adds.
What This Means For You
If you're taking antidepressants and thinking twice about whether you should be, don't stop them suddenly. Seek advice from your doctor, and if you do decide to stop make sure you do it with medical supervision and support, and reduce your dose very slowly.
Moncrieff J, Cooper RE, Stockmann T, Amendola S, Hengartner MP, Horowitz MA. The serotonin theory of depression: A systematic umbrella review of the evidence . Mol Psychiatry . 2022. doi:10.1038/s41380-022-01661-0
Sinyor M, Schaffer A, Levitt A. The sequenced treatment alternatives to relieve depression (STAR*D) trial: A review . Can J Psychiatry . 2010;55(3):126-135. doi:10.1177/070674371005500303
By Claire Gillespie Claire Gillespie is a freelance writer specializing in mental health. She’s written for The Washington Post, Vice, Health, Women’s Health, SELF, The Huffington Post, and many more.
Advertisement

No link between depression and serotonin, finds major analysis
A review of 17 previous studies finds no evidence for a link between depression and low serotonin levels, which SSRI antidepressants focus on – though not everyone is convinced by the findings
By Sarah Wild
20 July 2022

Polarised light micrograph of crystals of serotonin, which is a neurotransmitter in the brain
MICHAEL W. DAVIDSON/SCIENCE PHOTO LIBRARY
There may be no link between serotonin levels and depression , according to an analysis of 17 studies. This raises questions about antidepressants that focus on this brain-signalling molecule, say the authors of the analysis. Not everyone is convinced by the findings, though.
The serotonin hypothesis, which dates from the 1960s, says that a chemical imbalance in the brain, including low levels of serotonin, also known as 5-hydroxytryptamine or 5-HT, leads to depression. We now think various biological, psychological and environmental factors play a role, but the most popular antidepressants, known as selective serotonin reuptake inhibitors (SSRIs), increase the availability of serotonin in the brain.
Now, Joanna Moncrieff at University College London and her colleagues have done an “umbrella analysis” of 17 systematic reviews and studies, which together included hundreds of thousands of people with and without depression.
It is difficult to directly measure real-time serotonin levels in the brain, so the 17 studies looked at depression and proxies for serotonin, such as the molecules in cerebral fluid that serotonin breaks down into; the levels of serotonin receptors and how active they are; or whether there are more genes for serotonin transporters – which remove serotonin – in people with depression.
Fresh ideas about the causes of depression are bringing new treatments
Moncrieff’s team found that there was no evidence that low serotonin activity or amounts cause depression.
“The implication of our paper is that we do not know what [SSRI] antidepressants are doing,” says Moncrieff. One possibility is that they are working through a placebo effect, she says.
However, Johan Lundberg at the Karolinska Institute in Sweden says a limitation of the analysis is that it didn’t distinguish between people who had ongoing depression and those who have episodes of depression, whose state at the time they were assessed could affect the functioning of their serotonin systems. “It is key to separately analyse data from studies that examine the same patients when ill and when in remission, to have optimal conditions to examine the hypothesis,” he says.
Why spending time near water gives us a powerful mental health boost
Moncrieff says the review was dependent on the studies that had already been done, none of which highlighted any difference between people who were experiencing symptoms of depression or had a history of it.
“It must be recognised that 5-HT is likely only one contributor to depression,” says Paul Albert at the University of Ottawa in Canada. “Given the large placebo effect in treatment of depression, it is likely that the contribution of other systems, including dopamine that is implicated in placebo effect, may be greater than that of 5-HT.”
“Antidepressants are an effective, NICE-recommended treatment for depression that can also be prescribed for a range of physical and mental health conditions,” a spokesperson for the Royal College of Psychiatrists told the Science Media Centre in the UK, referring to treatment guidelines from the National Institute for Health and Care Excellence (NICE) in England. “Antidepressants will vary in effectiveness for different people, and the reasons for this are complex. We would not recommend for anyone to stop taking their antidepressants based on this review, and encourage anyone with concerns about their medication to contact their [family doctor].”
Molecular Psychiatry DOI: 10.1038/s41380-022-01661-0
Need a listening ear? UK Samaritans : 116123; US National Suicide Prevention Lifeline : 1 800 273 8255; hotlines in other countries.
Sign up to our free Health Check newsletter that gives you the health, diet and fitness news you can trust, every Saturday
Sign up to our weekly newsletter
Receive a weekly dose of discovery in your inbox! We'll also keep you up to date with New Scientist events and special offers.
More from New Scientist
Explore the latest news, articles and features
Drugs used to treat ADHD and depression may ease Alzheimer's symptoms
The mental tricks you can use in your lifelong pursuit of happiness.
Subscriber-only
Doctors are hypnotising people before surgery to help reduce anxiety
Popular articles.
Trending New Scientist articles
Subscribe or renew today
Every print subscription comes with full digital access
Science News
A chemical imbalance doesn’t explain depression. so what does.
The causes of depression are much more complex than the serotonin hypothesis suggests

Understanding depression means not only studying the brain and body, but also a host of outside factors that influence people’s health, researchers argue.
PETER STRAIN
Share this:
By Laura Sanders
February 12, 2023 at 7:00 am
You’d be forgiven for thinking that depression has a simple explanation.
The same mantra — that the mood disorder comes from a chemical imbalance in the brain — is repeated in doctors’ offices, medical textbooks and pharmaceutical advertisements. Those ads tell us that depression can be eased by tweaking the chemicals that are off-kilter in the brain. The only problem — and it’s a big one — is that this explanation isn’t true.
The phrase “chemical imbalance” is too vague to be true or false; it doesn’t mean much of anything when it comes to the brain and all its complexity. Serotonin, the chemical messenger often tied to depression, is not the one key thing that explains depression. The same goes for other brain chemicals.
The hard truth is that despite decades of sophisticated research, we still don’t understand what depression is. There are no clear descriptions of it, and no obvious signs of it in the brain or blood.
The reasons we’re in this position are as complex as the disease itself. Commonly used measures of depression, created decades ago, neglect some important symptoms and overemphasize others, particularly among certain groups of people. Even if depression could be measured perfectly, the disorder exists amid myriad levels of complexity, from biological confluences of minuscule molecules in the brain all the way out to the influences of the world at large. Countless combinations of genetics, personality, history and life circumstances may all conspire to create the disorder in any one person. No wonder the science is stuck.
It’s easy to see why a simple “chemical imbalance” explanation holds appeal, even if it’s false, says Awais Aftab, a psychiatrist at Case Western Reserve University in Cleveland. What causes depression is nuanced, he says — “not something that can easily be captured in a slogan or buzzword.”
So here, up front, is your fair warning: There will be no satisfying wrap-up at the end of this story. You will not come away with a scientific explanation for depression, because one does not exist. But there is a way forward for depression researchers, Aftab says. It requires grappling with nuances, complexity and imperfect data.
Those hard examinations are under way. “There’s been some really interesting and exciting scientific and philosophical work,” Aftab says. That forward motion, however slow, gives him hope and may ultimately benefit the millions of people around the world weighed down by depression.
How is depression measured?
Many people who feel depressed go into a doctor’s office and get assessed with a checklist. “Yes” to trouble sleeping, “yes” to weight loss and “yes” to a depressed mood would all yield points that get tallied into a cumulative score. A high enough score may get someone a diagnosis. The process seems straightforward. But it’s not. “Even basic issues regarding measurement of depression are actually still quite open for debate,” Aftab says.
That’s why there are dozens of methods to assess depression, including the standard description set by the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders , or DSM-5. This manual is meant to standardize categories of illness.
Variety in measurement is a real problem for the field and points to the lack of understanding of the disease itself, says Eiko Fried, a clinical psychologist at Leiden University in the Netherlands. Current ways of measuring depression “leave you with a really impoverished, tiny look,” Fried says.
Scales can miss important symptoms, leaving people out. “Mental pain,” for instance, was described by patients with depression and their caregivers as an important feature of the illness , researchers reported in 2020 in Lancet Psychiatry . Yet the term doesn’t show up on standard depression measurements.
One reason for the trouble is that the experience of depression is, by its nature, deeply personal, says clinical psychologist Ioana Alina Cristea of the University of Pavia in Italy. Individual patient complaints are often the best tool for diagnosing the disorder, she says. “We can never let these elements of subjectivity go.”
In the middle of the 20th century, depression was diagnosed through subjective conversation and psychoanalysis, and considered by some to be an illness of the soul. In 1960, psychiatrist Max Hamilton attempted to course-correct toward objectivity. Working at the University of Leeds in England, he published a depression scale. Today, that scale, known by its acronyms HAM-D or HRSD, is one of the most widely used depression screening tools, often used in studies measuring depression and evaluating the promise of possible treatments.
Who is depressed?
According to data from 2020, an estimated 21 million adults in the United States have had a major depressive episode in the last year, putting the overall prevalence at 8.4 percent. Rates are notably higher among females, people ages 18 to 25 and people who reported belonging to two or more races. But the widely varied scales used to diagnose depression may not accurately capture the true rates among some populations.
Portion of U.S. adults who have had a major depressive episode in the last year

“It’s a great scheme for a scale that was made in 1960,” Fried says. Since the HRSD was published, “we have put a man on the moon, invented the internet and created powerful computers small enough to fit in people’s pockets,” Fried and his colleagues wrote in April in Nature Reviews Psychology . Yet this 60-year-old tool remains a gold standard.
Hamilton developed his scale by observing patients who had already been diagnosed with depression. They exhibited symptoms such as weight loss and slowed speech. But those mixtures of symptoms don’t apply to everyone with depression, nor do they capture nuance in symptoms.
To spot these nuances, Fried looked at 52 depression symptoms across seven different scales for depression, including Hamilton’s scale. On average, each symptom appeared in three of the seven scales. A whopping 40 percent of the symptoms appeared in only one scale, Fried reported in 2017 in the Journal of Affective Disorders . The only specific symptom common to all seven scales? “Sad mood.”
In a study that examined depression symptoms reported by 3,703 people, Fried and Randolph Nesse, an evolutionary psychiatrist at the University of Michigan Medical School in Ann Arbor, found 1,030 unique symptom profiles . Roughly 14 percent of participants had combinations of symptoms that were not shared with anyone else, the researchers reported in 2015 in the Journal of Affective Disorders .
Before reliable thermometers, the concept of temperature was murky. How do you understand the science of hot and cold without the tools to measure it? “You don’t,” Fried says. “You make a terrible measurement, and you have a terrible theory of what it is.” Depression presents a similar challenge, he says. Without good measurements, how can you possibly diagnose depression, determine whether symptoms get better with treatments or even prevent it in the first place?
Depression differs by gender, race and culture
The story gets murkier when considering who these depression scales were made for. Symptoms differ among groups of people, making the diagnosis even less relevant for certain groups.
Depression symptoms measured by seven scales
Seven common rating tools for depression measure a wide variety of symptoms. When researchers reviewed the 52 symptoms measured by these scales, only one specific symptom appeared in all seven — sad mood.

Behavioral researcher Leslie Adams of Johns Hopkins Bloomberg School of Public Health studies depression in Black men. “It’s clear that [depression] is negatively impacting their work lives, social lives and relationships. But they’re not being diagnosed at the same rate” as other groups, she says. For instance, white people have a lifetime risk of major depression disorder of almost 18 percent; Black people’s lifetime risk is 10.4 percent , researchers reported in 2007 in JAMA Psychiatry . This discrepancy led Adams to ask: “Could there be a problem with diagnostic tools?”
Turns out, there is. Black men with depression have several characteristics that common scales miss , such as feelings of internal conflict, not communicating with others and feeling the burdens of societal pressure, Adams and colleagues reported in 2021 in BMC Public Health . A lot of depression measurements are based on questions that don’t capture these symptoms, Adams says. “ ‘Are you very sad?’ ‘Are you crying?’ Some people do not emote in the same way,” she says. “You may be missing things.”
American Indian women living in the Southeast United States also experience symptoms that aren’t adequately caught by the scales, Adams and her team found in a separate study. These women also reported experiences that do not necessarily signal depression for them but generally do for wider populations.
On common scales, “there are some items that really do not capture the experience of depression for these groups,” Adams says. For instance, a common question asks how well someone agrees with the sentence: “I felt everything I did was an effort.” That “can mean a lot of things, and it’s not necessarily tied to depression,” Adams says. The same goes for items such as, “People dislike me.” A person of color faced with racism and marginalization might agree with that, regardless of depression, she says.
Our ways to measure depression capture only a tiny slice of the big picture. The same can be said about our understanding of what’s happening in the brain.
The flawed serotonin hypothesis
Serotonin came into the spotlight in part because of the serendipitous discovery of drugs that affected serotonin receptors, called selective serotonin reuptake inhibitors, or SSRIs. After getting its start in the late 1960s, the “serotonin hypothesis” flourished in the late ’90s, as advertisers ran commercials that told viewers that SSRIs fixed the serotonin deficit that can accompany depression. These messages changed the way people talked and thought about depression. Having a simple biological explanation helped some people and their doctors, in part by easing the shame some people felt for not being able to snap out of it on their own. It gave doctors ways to talk with people about the mood disorder.
But it was a simplified picture. A recent review of evidence, published in July in Molecular Psychiatry , finds no consistent data supporting the idea that low serotonin causes depression. Some headlines declared that the study was a grand takedown of the serotonin hypothesis. To depression researchers, the findings weren’t a surprise. Many had already realized this simple description wasn’t helpful.
There’s plenty of data suggesting that serotonin, and other chemical messengers such as dopamine and norepinephrine, are somehow involved in depression, including a study by neuropharmacologist Gitte Moos Knudsen of the University of Copenhagen. She and colleagues recently found that 17 people who were in the midst of a depressive episode released, on average, less serotonin in certain brain areas than 20 people who weren’t depressed. The study is small, but it’s one of the first to look at serotonin release in living human brains of people with depression.
But Knudsen cautions that those results, published in October in Biological Psychiatry , don’t mean that depression is fully caused by low serotonin levels. “It’s easy to defer to simple explanations,” she says.
SSRIs essentially form a molecular blockade, stopping serotonin from being reabsorbed into nerve cells and keeping the levels high between the cells. Those high levels are thought to influence nerve cell activity in ways that help people feel better.
Because the drugs can ease symptoms in about half of people with depression, it seemed to make sense that depression was caused by problems with serotonin. But just because a treatment works by doing something doesn’t mean the disease works in the opposite way. That’s backward logic , psychiatrist Nassir Ghaemi of Tufts University School of Medicine in Boston wrote in October in a Psychology Today essay. Aspirin can ease a headache, but a headache isn’t caused by low aspirin.
“We think we have a much more nuanced picture of what depression is today,” Knudsen says. The trouble is figuring out the many details. “We need to be honest with patients, to say that we don’t know everything about this,” she says.
The brain contains seven distinct classes of receptors that sense serotonin. That’s not even accounting for sensors for other messengers such as dopamine and norepinephrine. And these receptors sit on a wide variety of nerve cells, some that send signals when they sense serotonin, some that dampen signals. And serotonin, dopamine and norepinephrine are just a few of dozens of chemicals that carry information throughout a multitude of interconnected brain circuits. This complexity is so great that it renders the phrase “chemical imbalance” meaningless.
Overly simple claims — low serotonin causes depression, or low serotonin isn’t involved — serve only to keep us stymied, Aftab says. “[It] just keeps up that unhelpful binary.”
How treatment helps depression patients
A large study called STAR*D enrolled more than 4,000 people with depression across the United States and offered a window into how well treatment works. In the study, volunteers who didn’t respond to one treatment were switched to a second and so on. At each step, the portion of people in remission increased, though gains were smaller for later steps.
Depression remission rate with treatments

Depression research can’t ignore the world
In the 1990s, Aftab says, depression researchers got intensely focused on the brain. “They were trying to find the broken part of the brain that causes depression.” That limited view “really hurt depression research,” Aftab says. In the last 10 years or so, “there’s a general recognition that that sort of mind-set is not going to give us the answers.”
Reducing depression to specific problems of biology in the brain didn’t work, Cristea says. “If you were a doctor 10 years ago, the dream was that the neuroscience would give us the markers. We would look at the markers and say, ‘OK. You [get] this drug. You, this kind of therapy.’ But it hasn’t happened.” Part of that, she says, is because depression is an “existentially complicated disorder” that’s tough to simplify, quantify and study in a lab.
Our friendships, our loves, our setbacks and our stress can all influence our health. Take a recent study of first-year doctors in the United States. The more these doctors worked, the higher the rate of depression , scientists reported in October in the New England Journal of Medicine . Similar trends exist for caregivers of people with dementia and health care workers who kept emergency departments open during the COVID-19 pandemic. Their high-stress experiences may have prompted depression in some way.
“Depression is linked to the state of the world — and there is no denying it,” Aftab says.
What depression scales don’t ask
In a concept mapping study, descriptions of depression symptoms provided by Black men and key individuals supporting Black men’s health, including Black women and doctors, were clustered into six categories: physical states, emotional states, diminished drive, communication with others, internal conflict and social pressures. Communication with others and internal conflict were each asked about in only one of three commonly used depression assessments studied. Social pressures weren’t reflected in any of the three assessments.
Reflected in three assessments
Physical states: Descriptions in this category included high blood pressure, self-harm or suicidal behavior, binge eating, insomnia, heart palpitations and weight loss and/or gain.
Emotional states: Descriptions in this category included not being able to “get up and go,” a lack of motivation, anger, fatigue, hopelessness, frustration, worry, bursts of crying, low self-esteem, feeling stuck and feeling out of control.
Diminished drive: This category included descriptions of an untidy appearance, the inability to complete tasks and life goals, not being able to provide for family and excessive substance use, such as marijuana, cigarettes and alcohol.
Reflected in one assessment
Communication with others: Descriptions in this category included not being able to communicate properly, including ignoring emails and phone calls, isolation from others, withdrawal from everyday activities, volatile behavior toward others, blunted emotional expression and difficulty maintaining romantic relationships.
Internal conflict: This category included having a pessimistic outlook, feeling guilty, feeling unqualified, feeling attacked or defensive, feeling helpless in the face of aging, and a heightened sense of fear or dread.
Not reflected in the assessments
Social pressures: Descriptions in this category included not being able to keep up appearances, fear of unknown consequences of today’s political environment, adherence to cultural norms of success and power, a lack of work/life balance, seeking happiness through accumulated materials and increased attendance at religious institutions.
Today’s research on depression ought to be more pluralistic, Adams says. “There are so many factors at play that we can’t just rest on one solution,” she says. Research from neuroscience and genetics has helped identify brain circuits, chemical messengers, cell types, molecules and genes that all may be involved in the disorder. But researchers aren’t satisfied with that. “There is other evidence that remains unexplored,” Adams says. “With our neuroscience advances, there should be similar advances in public health and psychiatric work.”
That’s happening. For her part, Adams and colleagues have just begun a study looking at moment-to-moment stressors in the lives of Black adolescents, ages 12 to 18, as measured by cell phone questionnaires. Responses, she hopes, will yield clues about depression and risk of suicide.
Other researchers are trying to fit together all of these different ways of seeing the problem. Fried, for example, is developing new concepts of depression that acknowledge the interacting systems. You tug on one aspect of it — using an antidepressant for instance, or changing sleep patterns — and see how the rest of the system reacts.
Approaches like these recognize the complexity of the problem and aim to figure out ways to handle it. We will never have a simple explanation for depression; we are now learning that one cannot possibly exist. That may sound like cold comfort to people in depression’s grip. But seeing the challenge with clear eyes may be the thing that moves us forward.
What you think you know about depression is probably wrong
We’ve all heard that depression is caused by a chemical imbalance in the brain, but science shows that the truth is much more complex.
What is the serotonin hypothesis of depression?
The serotonin hypothesis says that depression is caused by not enough of a chemical messenger called serotonin in the brain. A related idea is that brain chemicals are out of balance.
Why did it become popular?
Drugs called SSRIs were advertised as ways to treat depression by fixing the serotonin deficit. These drugs ease symptoms for roughly half of people with depression.
Why is the serotonin hypothesis of depression wrong?
It is too simple a picture. There are no clear descriptions of depression, and no obvious signs of it in the brain or blood. All sorts of factors influence depression, ranging from a myriad of minuscule molecules in the brain to events in a person’s life.
What factors need to be considered when studying depression?
Symptoms of depression vary widely from person to person, and common depression scales can miss important symptoms. Signs of depression also vary among different groups of people, and can be influenced by race, gender and culture. What’s more, our friendships, our loves, our setbacks and our stress can all influence our mental health.
More Stories from Science News on Health & Medicine

Irregular bone marrow cells may increase heart disease risk

Traces of bird flu are showing up in cow milk. Here’s what to know

Malaria parasites can evade rapid tests, threatening eradication goals

Rat cells grew in mice brains, and helped sniff out cookies

Pelvic exams at hospitals require written consent, new U.S. guidelines say

A new U.S. tool maps where heat will be dangerous for your health

Aimee Grant investigates the needs of autistic people

These windpipe cells trigger coughs to keep water out of the lungs
Subscribers, enter your e-mail address for full access to the Science News archives and digital editions.
Not a subscriber? Become one now .

- April 24, 2024 | Scientists Turn to Venus in the Search for Alien Life
- April 24, 2024 | NASA Astronauts Enter Quarantine As Boeing Starliner Test Flight Approaches
- April 23, 2024 | Peeking Inside Protons: Supercomputers Reveal Quark Secrets
- April 23, 2024 | A Cheaper and More Sustainable Lithium Battery: How LiDFOB Could Change Everything
- April 23, 2024 | Rewiring Reality: Stanford Unveils the Brain’s Fault Lines in Psychosis
Scientists Find No Evidence That Depression Is Caused by “Chemical Imbalance” or Low Serotonin Levels
By University College London July 25, 2022
Despite the popularity of the ‘chemical imbalance’ theory of depression, scientists say there is no clear evidence that serotonin levels or serotonin activity cause depression.
A comprehensive review by University College London scientists challenges the widely-held belief that depression is caused by a serotonin imbalance. The research, encompassing numerous studies and tens of thousands of participants, found no clear evidence supporting this theory and suggested that long-term antidepressant use might actually lower serotonin levels. The researchers advocate for further investigation into alternative depression treatments, beyond the conventional use of antidepressants.
After decades of research, there remains no clear evidence that serotonin levels or serotonin activity are responsible for depression, according to a comprehensive review of prior research led by University College London (UCL) scientists.
The major new umbrella review – an overview of existing meta-analyses and systematic reviews – was published on July 20 in the journal Molecular Psychiatry . It suggests that depression is not likely caused by a chemical imbalance, and calls into question what antidepressant medications do. This is because most antidepressants are selective serotonin reuptake inhibitors (SSRIs), which were originally said to function by correcting abnormally low serotonin levels. In fact, there is no other accepted pharmacological mechanism by which antidepressants affect the symptoms of depression.
Lead author Professor Joanna Moncrieff, a Professor of Psychiatry at UCL and a consultant psychiatrist at North East London NHS Foundation Trust (NELFT), said: “It is always difficult to prove a negative, but I think we can safely say that after a vast amount of research conducted over several decades, there is no convincing evidence that depression is caused by serotonin abnormalities, particularly by lower levels or reduced activity of serotonin.
“The popularity of the ‘chemical imbalance’ theory of depression has coincided with a huge increase in the use of antidepressants. Prescriptions for antidepressants have risen dramatically since the 1990s, with one in six adults in England and 2% of teenagers now being prescribed an antidepressant in a given year.
“Many people take antidepressants because they have been led to believe their depression has a biochemical cause, but this new research suggests this belief is not grounded in evidence.”
This comprehensive umbrella review aimed to capture all relevant studies that have been published in the most important fields of research on serotonin and depression. The research included in the review involved tens of thousands of participants.
Studies that compared levels of serotonin and its breakdown products in the blood or brain fluids did not find any notable differences between people diagnosed with depression and healthy control (comparison) participants.
Weak and inconsistent evidence suggestive of higher levels of serotonin activity in people with depression was found by studies on serotonin receptors and the serotonin transporter, the protein targeted by most antidepressants. However, the scientists say the findings are likely explained by the use of antidepressants among people diagnosed with depression, since such effects were not reliably ruled out.
The researchers also investigated studies where serotonin levels were artificially lowered in hundreds of people by depriving their diets of the amino acid required to make serotonin. These studies have been cited as demonstrating that a serotonin deficiency is linked to depression. However, a meta-analysis conducted in 2007 and a sample of recent studies found that lowering serotonin in this way did not produce depression in hundreds of healthy volunteers. Very weak evidence was found in a small subgroup of people with a family history of depression, but this only involved 75 participants, and more recent evidence was inconclusive.
Some very large studies involving tens of thousands of patients looked at gene variation, including the gene for the serotonin transporter. No difference in these genes between people with depression and healthy controls were found. These studies also looked at the effects of stressful life events and found that these exerted a strong effect on people’s risk of becoming depressed – the more stressful life events a person had experienced, the more likely they were to be depressed. A famous early study found a relationship between stressful events, the type of serotonin transporter gene a person had, and the chance of depression. But larger, more comprehensive studies suggest this was a false finding.
These findings together led the researchers to conclude that there is “no support for the hypothesis that depression is caused by lowered serotonin activity or concentrations.”
The authors say their findings are important as studies show that as many as 85-90% of the public believes that depression is caused by low serotonin or a chemical imbalance. A growing number of scientists and professional bodies are recognizing the chemical imbalance framing as an over-simplification. There is also evidence that believing that low mood is caused by a chemical imbalance leads people to have a pessimistic outlook on the likelihood of recovery, and the possibility of managing moods without medical help. This is important because most people will meet criteria for anxiety or depression at some point in their lives.
The scientists also found evidence from a large meta-analysis that people who used antidepressants had lower levels of serotonin in their blood. They concluded that some evidence was consistent with the possibility that long-term antidepressant use reduces serotonin concentrations. The researchers say this may imply that the increase in serotonin that some antidepressants produce in the short term could lead to compensatory changes in the brain that produce the opposite effect in the long term.
While the study did not review the efficacy of antidepressants, the authors encourage further research and advice into treatments that might focus instead on managing stressful or traumatic events in people’s lives, such as with psychotherapy, alongside other practices such as exercise or mindfulness, or addressing underlying contributors such as poverty, stress, and loneliness.
Professor Moncrieff said: “Our view is that patients should not be told that depression is caused by low serotonin or by a chemical imbalance, and they should not be led to believe that antidepressants work by targeting these unproven abnormalities. We do not understand what antidepressants are doing to the brain exactly, and giving people this sort of misinformation prevents them from making an informed decision about whether to take antidepressants or not.”
Co-author Dr. Mark Horowitz, a training psychiatrist and Clinical Research Fellow in Psychiatry at UCL and NELFT, said: “I had been taught that depression was caused by low serotonin in my psychiatry training and had even taught this to students in my own lectures. Being involved in this research was eye-opening and feels like everything I thought I knew has been flipped upside down.
“One interesting aspect in the studies we examined was how strong an effect adverse life events played in depression, suggesting low mood is a response to people’s lives and cannot be boiled down to a simple chemical equation.”
Professor Moncrieff added: “Thousands of people suffer from side effects of antidepressants, including the severe withdrawal effects that can occur when people try to stop them, yet prescription rates continue to rise. We believe this situation has been driven partly by the false belief that depression is due to a chemical imbalance. It is high time to inform the public that this belief is not grounded in science.”
The authors caution that anyone considering withdrawing from antidepressants should seek the advice of a health professional, given the risk of adverse effects following withdrawal. Professor Moncrieff and Dr. Horowitz are conducting ongoing research into how best to gradually stop taking antidepressants.
Reference: “The serotonin theory of depression: a systematic umbrella review of the evidence” by Joanna Moncrieff, Ruth E. Cooper, Tom Stockmann, Simone Amendola, Michael P. Hengartner and Mark A. Horowitz, 20 July 2022, Molecular Psychiatry . DOI: 10.1038/s41380-022-01661-0
More on SciTechDaily

Serotonin Deficiency Directly Linked With Depression in Groundbreaking Study

Decoding Serotonin: From Molecular to Whole-Brain Scale Effects
Columbia Researchers Uncover Dangerous Connection Between Serotonin and Heart Valve Disease

Scientists Find Neurochemicals – Dopamine and Serotonin – Have Unexpectedly Profound Roles in the Human Brain

SSRI Antidepressants (Zoloft/Sertraline) May Reduce Anxiety More Than Depressive Symptoms

Good and Bad Feelings for Brain Stem Serotonin Could Lead to New Treatments for Addiction and Depression

Antidepressant Use During Pregnancy Has Increased Risks
Nasa, noaa scientists: earth’s energy imbalance has doubled, 20 comments on "scientists find no evidence that depression is caused by “chemical imbalance” or low serotonin levels".
This study is incorrect. They are relying on results from studies that try to reduce the level of serotonin in the brain. These studies do not find increased depression. But, that is because the method they are using to try and reduce serotonin, reducing tryptophan in the participants diet, has never been shown to significantly change the serotonin level. I corrected my post-stroke depression with an over the counter supplement. See my video: https://youtu.be/LXKAfX5DNcI
You sound like you get paid to post thiis.
The book “Listening To Prozac” by Peter D Kramer (June 1993) came to a similar conclusion, if I understood it and remember it correctly (I read it just after publication). He said that his patients given Prozac did not show signs of their depression dissipating. Rather, he saw their personality types change from “introverted” to “extroverted”. Then they started talking about how they got new friends at work, started going out with them to have fun; or became otherwise involved in some “extra-curricular” activity. Only then, after many months of living this new “extroverted” life, did they show signs of their depression dissipating. He concluded that it was our (modern industrial) society that shuns “introverts” and glorifies “extroverts,” as opposed to the “tribal” societies that we evolved in, that require the “quiet stay-at-home” type to keep the hearth burning and the lamp in the window lit – but a tribe includes them and all tribal members in all tribal activities by default, whereas modern society’s “tribes” do not. He said he would keep prescribing the pills because many of his patients did see improvement; it just wasn’t what the “textbooks” said it was. In my humble opinion of observations of friends (back when we were teen-agers and in our early 20s and 30s) given antidepressants, I had to concur with Dr. Kramer. I saw them change. But I would say for the worst. (would they? THAT is the real question!) They became more cold-hearted. Many warnings have been issued about antidepressants possibly causing aggressive or even violent behavior in teens; (? and suicide too, if I remember correctly ?). This is what I saw. My friends became more aggressive in general. Not outright mean or violent. My opinion is that, yes, these drugs do “switch” personality types (introverted to extroverted). But the truth still remains that they suffered high levels of “trauma or stress” in their early life. In my imagination, I see a violent or otherwise threatening person (all my friends mentioned here were males, and I would also hypothesize that the aggressive person in their life was also male) in their everyday life – likely a parent figure – who was also very extroverted themselves. The friends given the antidepressant pills, switched to extroverted, simply patterned their behavior and personality, like we all do, on the influential adults in their childhood. The kids who get suicidal from A.D. pills simply are rejecting their own personality’s “expression of extrovertness” – they don’t want to be or feel like the person who abused them, and they only see one way out. IDK. Just a guess.
QUOTE from article: Co-author Dr. Mark Horowitz, a training psychiatrist and Clinical Research Fellow in Psychiatry at UCL and NELFT, said: “I had been taught that depression was caused by low serotonin in my psychiatry training and had even taught this to students in my own lectures. Being involved in this research was eye-opening and feels like everything I thought I knew has been flipped upside down.”
That’s because pharmaceutical companies are the biggest industry in the world – I forget if it is by 10 or 100 times bigger than the next biggest: the “defense” (offensive weapons) industry; and they pay the universities big big big $$$$$$ to teach a specific science of medicine that keeps them in profits, and ignores the science behind real treatments for depression; for instance see “The Infinite Mind” by Valerie V. Hunt – a treatment that cures patients in ONE treatment with long-term results.
The reviews of this book are lame. They do not talk about the real contents of what she found in her research and the multi-million dollar work with the NIMH. The Wikipedia article on her is watered down also. They don’t want you to know! Antidepressants hit the market big-time about the same time as her research hit its pinnacle. It is the single most important book on psychology and cognitive science and health and being HUMAN and ALIVE that I’ve ever read.
If its not chemical imbalance then what is it and why is it that depressed people feel better after taking antidepressants? If there is no knowledge on how antidepressants work, how can you counter it without knowing how it works in the first place?
Placebo effect.
If there is no knowledge on how antidepressants work, how can we say they are working?
Here’s an idea (and I am not a professional or something). Maybe the cause of depression is indeed not a chemical imbalance, but rather adverse life events. But maybe using SSRIs (that increase levels of serotonin more than the normal person) helps to overcome this state of mind. People without depression are satisfied with the normal level, because they have nothing to overcome. In short, depression is not caused by serotonin deficiency, but high levels of serotonin help to cope with it.
When I was on antidepressants, they made me feel like I didn’t care. And that I didn’t care that I didn’t care. I didn’t care about how my apartment looked, how I looked. I didn’t care about anything. Sometimes I didn’t know what I was doing. I finally decided to go off when the doctor was going to go over the maximum amount. I reduced the drug I was on by titrating down the amount I was taking. When I got off the drug, it was like waking up. I started walking. Changed my diet. I realized I had been no different than someone who was an addict thinking that the way out of my problems was through a pill. I will never take another antidepressant.
People can debate (comments above) the role of serotonin but are doing so in an evidence vacuum and without reference to underlying cause.
The big elephant in the room is that depression is a symptom, not a disease. There are many pathologies, deficiencies, toxicities, stresses etc that can cause it, and THAT needs to be the diagnosis. Depression is therefore a bogus diagnosis: like ALL psychiatric diagnoses it lacks any objective defining measure. This is like diagnosing an achy head as a disease called “headache”, which tells the sufferer NOTHING.
For instance, if you can’t pay your bills, you don’t need prozac, you need money. If your marriage is crap you need a divorce. If you have a depleted diet you will be low in B vitamins and that can and will manifest as depression etc. If you rely on stimulants you’ll be forever battling a state of comedown.
Don’t get me started on gut flora, antibiotic use and other drug side-effects.
One thing is sure, “SSRI deficiency” is unequivocally NOT the cause of depression.
@Forem Lapsiwala. 100 percent agree, antidepressants do work. If they didn’t, they wouldn’t be prescribed
@Allanor it all depends what we mean by “they work”. Lots of things can make you feel better, but without any relation to the cause of the problem. Many come with a significant downside. The more we can narrow our outcome measures, the more things we will find that “work”, but so what?
But there is only one thing that can ever address the root cause of a problem – and that is addressing the root cause of the problem! EVEN SUPPOSING chemical imbalance really is THE unique disease process for all depression (which is simplistic to the point of ridiculous), there is still the question of WHY!!!
“They work” is a fairly vacuous statement I’m afraid and advances our understanding not one jot.
I think that depression could be a neurological disorder brought about by the loss of neurological stimulation from a degree a person is used to down to a lesser degree, coupled with the brain chemicals released when an individual believes that the return of such a degree and similarity of stimulation can or will be experienced anytime soon is unlikely if not impossible. But this is just a wild guess, probably crazy.
Depressing experiences lead to depressed mood. Who knew?
I’m glad that the truth about the “chemical imbalance” theory has finally gone mainstream. The truth is, there has never been even decent evidence that depressed people had low serotonin levels. The idea was convincingly disproven way back in the mid-80s. The main reason people believe this is pharmaceutical industry advertising, supported by the psychiatric industry.
Antidepressants do seems to have a positive effect for some people, but that has also been massively overstated. See Irving Kirsch’s work.
Maybe it’s time to go back and look at those “stressful events” that actually DO seem to have a high correlation with depression? But who can make enormous profits by actually helping people cope with and control their lives?
I’m reading into these comments a bit of a false dichotomy between mind/experience and chemical imbalance, like it has to be one or the other.
Think more broadly, people. The brain is an organ, it has certain needs. At medical school they tell us that basically means glucose and oxygen. Well, 2/10, must try harder.
Everything medical is chemical – why? Because that is what the chemical industry decided when it took over the American Universities in 1919.
You don’t have to look very far to find plenty of people who have broken out of depression. I’m one of them. A bit like or cancer, when you actually do beat it, nobody seems to want to ask you how. But they all have an opinion on it nevertheless.
I’ll throw you a teaser. The performance of an organ depends on its environment, and that is a huge subject. But suffice to say the problems do not begin with the affected organ, they begin elsewhere. I could run a university course on this, but who would pay me?
Correlation and causation are 2 different things.
Saying that depression is simply a reflection of life issues/stress is a way-oversimplification; just as much as suggesting a lack of appropriate serotonin levels is the root cause. I, along with my identical twin brother were born premature; I was incubated for 3 weeks (being deprived of food compared to my brother led me to be 3.12lbs vs his 5.8lbs) while he was sent home. I firmly believe my depression has a physical cause, whether due to lack of brain development (I have learning difficulties) or not being held as much due to the incubation. From day one, my brother smiled in every picture while I didn’t. At age 5 I told my mom I wanted to kill myself. SAME nurture/environment, a bit different nature (for those 3 weeks). I have ALWAYS been depressed; my brother? Never. The jury is still out. If talk therapy, mindfulness exercise, etc. doesn’t work, yet an SSRI does (not to mention NDRIs and others not so much as mentioned) then who are we to deprive someone of that option? I have tried EVERY conceivable thing out there and I’ve spent way more than $500,000 over 35 years of my own money (basically all my extra income goes to find a treatment/solution) to no avail. Now I am looking at seeing if psilocybin or ayahuasca/dmt may help. For people who have never experienced depression (NOT sadness) over a long period of time, they have no clue of what they say, particularly with claims that depression is a choice, or that meditation, strict diet of x,y,z or Jesus is all you need, is grossly disrespectful, trivializing and just plain ignorant. I pray each day to find a treatment for myself and all others in the same boat. Also, depression (again, NOT sadness which people quickly conflate it with) is just as much a physical feeling as it is a mental/emotional one. It physically HURTS.
The first comment by “David” sounds like a post paid for by BP.
Depression is a complex issue, but consider this.
(Scenario 1) Person A hits Person B, but B is told they can’t hit A back. Lifetime pattern.
(Scenario 2) Same as (1) except B hits A back and A never hits B ever again.
(Scenario 3) Same as (1) but a resolution is reached and A never hits B again, maybe they have become friends.
(Scenario 4) Same as (1), but B has the ability to avoid A from now on and heal from trauma.
Unhealed wounds and unresolved issues are definitely causes for depression. The more you heal from trauma, the more intolerable traumatic people and situations become for you.
And let’s just talk about the huge elephant in the room. The greatest predictor of mental health or mental illness in a person’s life is how the person was treated by their MOTHER in the most vulnerable earliest years of life within the mother-child dyad. Same is true for personality disorders in adulthood.
Sure, biology plays role too.
Chemical imbalance was fabricated supposedly so public accept this. I think it just another money scheme.
True Trauma does cause a person to withdraw and creates many issues that cause depression . No adequate sleep. Binge eating. No adequate nutrition. Exercise is been blinked off the radar in public schools. Now we have not only depression , but also diabetes.
The vicious circle of drugs
It took me 5 years to stop an anti depressant that did nothing I was lied to. A pharmacist told me the truth. An ugly truth about anti depressants. They ruin your heart over time. Cause weight gain. A host of problems .
Bravo to the researchers, at last real science in our mental health community! Sadly this is not new news. I learned this truth 25 years ago when I was in a deep clinical depression with constant thoughts of suicide! At that point I was on antidepressants, anti-anxiety and sleeping pills for insomnia. I suffered for 4 years, sadly so did my two young children and my marriage. I went to doctors, therapist, psychologist, physiatrist anyone that said they can help me! I was fist diagnosed with clinical depression, anxiety, panic attacks, OCD and mood swings. After 4 years I was worse eventually diagnosed with “treatment resistant depression” that’s when I wanted to die! If you ever want to stripe someone of all hope label them with that! By the grace of God I found a psychologist who knew what he was talking about and helped many people before me! I followed what he taught and did the healing work! I’ve been depression free, anxiety free, panic attack free, OCD free and no more mood swings aka bipolar for over 25 years! I am here to say and shout from the mountain tops depression is NOT a chemical imbalance it is a symptom of unresolved emotions from emotionally charged events aka traumas from adverse childhood experiences! As soon as I began to process and heal the traumas my mental health was forever transformed! Trauma is the unprocessed unexpressed emotions left behind from an emotional charged event. The memories will always be there but the negative emotional charge will not! A little disclaimer I do believe in depression from Traumatic Brain Injuries. Anything can happen with an injured brain. I also follow Dr Daniel Amen and believe in his work but not everyone with depression has had a brain injury.
The lack of knowledge, not knowing I can heal my traumas to cure depression almost took my life. Knowledge is truly power so I will share 2 great books to read…How to get what you want and want what you have by Dr. John Gray. This is the book that saved and transformed my life! Self therapy is real! Do the work and take back your life! This next book opened my eyes to why I suffered for 4 years and the truth about Psychiatry and the DSM …CRACKED why psychiatry is doing more harm than good by Dr. James Davies both are a must read!
This study is very exciting. I have shared it on all my social medias, my clients and anyone that needs to hear it! I pray it gets traction and changes how depression is cured!
To Ryan that posted on August 8, 2022 I would look for a hypnotherapist that can do timeline therapy but take you back when you were in your mothers womb. What you wrote caught my attention. As a hypnotherapist I would focus on healing in utero trauma! It is very powerful. Good luck!
“The performance of an organ depends on its environment.” – Jamie James commentator from the thread. I resonate with this statement. Nature versus Nurture. Seems to me that there are humans that are good for our nervous system and those who are injurious to our nervous system. Trauma, according to Emma McAdam, an LMFT and youtube creator of Therapy in a Nutshell, says that trauma is a mental injury, not a mental illness. My subjective opinion about depression is, as long as we live with trauma brain we will have depression. Trauma brain can be healed (neuroplasticity), but it takes a lot of inner work via therapy, mentorship, self-compassion, facing those who’ve caused harm to us, etc. It can take a long time. Maybe facing our trauma head-on will, in the long run, help release the depression locked inside our bodies. I am a person of faith and I cling to John 8:32 (NLT) “And you will know the truth, and the truth will set you free.” Best to all who are in the inner war for peace and freedom.
Leave a comment Cancel reply
Email address is optional. If provided, your email will not be published or shared.
Save my name, email, and website in this browser for the next time I comment.

- Latest news
- UCL in the media
- Services for media
- Student news
- Tell us your story

No evidence that depression is caused by low serotonin levels, finds comprehensive review
20 July 2022
After decades of study, there remains no clear evidence that serotonin levels or serotonin activity are responsible for depression, according to a major review of prior research led by UCL scientists.

The new umbrella review – an overview of existing meta-analyses and systematic reviews – published in Molecular Psychiatry , suggests that depression is not likely caused by a chemical imbalance, and calls into question what antidepressants do. Most antidepressants are selective serotonin reuptake inhibitors (SSRIs), which were originally said to work by correcting abnormally low serotonin levels. There is no other accepted pharmacological mechanism by which antidepressants affect the symptoms of depression.
Lead author Professor Joanna Moncrieff, a Professor of Psychiatry at UCL and a consultant psychiatrist at North East London NHS Foundation Trust (NELFT), said: “It is always difficult to prove a negative, but I think we can safely say that after a vast amount of research conducted over several decades, there is no convincing evidence that depression is caused by serotonin abnormalities, particularly by lower levels or reduced activity of serotonin.
“The popularity of the ‘chemical imbalance’ theory of depression has coincided with a huge increase in the use of antidepressants. Prescriptions for antidepressants have risen dramatically since the 1990s, with one in six adults in England and 2% of teenagers now being prescribed an antidepressant in a given year.
“Many people take antidepressants because they have been led to believe their depression has a biochemical cause, but this new research suggests this belief is not grounded in evidence.”
The umbrella review aimed to capture all relevant studies that have been published in the most important fields of research on serotonin and depression. The studies included in the review involved tens of thousands of participants.
Research that compared levels of serotonin and its breakdown products in the blood or brain fluids did not find a difference between people diagnosed with depression and healthy control (comparison) participants.
Research on serotonin receptors and the serotonin transporter, the protein targeted by most antidepressants, found weak and inconsistent evidence suggestive of higher levels of serotonin activity in people with depression. However, the researchers say the findings are likely explained by the use of antidepressants among people diagnosed with depression, since such effects were not reliably ruled out.
The authors also looked at studies where serotonin levels were artificially lowered in hundreds of people by depriving their diets of the amino acid required to make serotonin. These studies have been cited as demonstrating that a serotonin deficiency is linked to depression. A meta-analysis conducted in 2007 and a sample of recent studies found that lowering serotonin in this way did not produce depression in hundreds of healthy volunteers, however. There was very weak evidence in a small subgroup of people with a family history of depression, but this only involved 75 participants, and more recent evidence was inconclusive.
Very large studies involving tens of thousands of patients looked at gene variation, including the gene for the serotonin transporter. They found no difference in these genes between people with depression and healthy controls. These studies also looked at the effects of stressful life events and found that these exerted a strong effect on people’s risk of becoming depressed – the more stressful life events a person had experienced, the more likely they were to be depressed. A famous early study found a relationship between stressful events, the type of serotonin transporter gene a person had and the chance of depression. But larger, more comprehensive studies suggest this was a false finding.
These findings together led the authors to conclude that there is “no support for the hypothesis that depression is caused by lowered serotonin activity or concentrations.”
The researchers say their findings are important as studies show that as many as 85-90% of the public believes that depression is caused by low serotonin or a chemical imbalance. A growing number of scientists and professional bodies are recognising the chemical imbalance framing as an over-simplification.* There is also evidence that believing that low mood is caused by a chemical imbalance leads people to have a pessimistic outlook on the likelihood of recovery, and the possibility of managing moods without medical help. This is important because most people will meet criteria for anxiety or depression at some point in their lives.
The authors also found evidence from a large meta-analysis that people who used antidepressants had lower levels of serotonin in their blood. They concluded that some evidence was consistent with the possibility that long-term antidepressant use reduces serotonin concentrations. The researchers say this may imply that the increase in serotonin that some antidepressants produce in the short term could lead to compensatory changes in the brain that produce the opposite effect in the long term.
While the study did not review the efficacy of antidepressants, the authors encourage further research and advice into treatments that might focus instead on managing stressful or traumatic events in people’s lives, such as with psychotherapy, alongside other practices such as exercise or mindfulness, or addressing underlying contributors such as poverty, stress and loneliness.
Professor Moncrieff said: “Our view is that patients should not be told that depression is caused by low serotonin or by a chemical imbalance, and they should not be led to believe that antidepressants work by targeting these unproven abnormalities. We do not understand what antidepressants are doing to the brain exactly, and giving people this sort of misinformation prevents them from making an informed decision about whether to take antidepressants or not.”
Co-author Dr Mark Horowitz, a training psychiatrist and Clinical Research Fellow in Psychiatry at UCL and NELFT, said: “I had been taught that depression was caused by low serotonin in my psychiatry training and had even taught this to students in my own lectures. Being involved in this research was eye-opening and feels like everything I thought I knew has been flipped upside down.
“One interesting aspect in the studies we examined was how strong an effect adverse life events played in depression, suggesting low mood is a response to people’s lives and cannot be boiled down to a simple chemical equation.”
Professor Moncrieff added: “Thousands of people suffer from side effects of antidepressants, including the severe withdrawal effects that can occur when people try to stop them, yet prescription rates continue to rise. We believe this situation has been driven partly by the false belief that depression is due to a chemical imbalance. It is high time to inform the public that this belief is not grounded in science.”
The researchers caution that anyone considering withdrawing from antidepressants should seek the advice of a health professional, given the risk of adverse effects following withdrawal. Professor Moncrieff and Dr Horowitz are conducting ongoing research into how best to gradually stop taking antidepressants .
- Research paper in Molecular Psychiatry
- Professor Joanna Moncrieff’s academic profile
- UCL Psychiatry
- * For example, the Royal College of Psychiatrists removed all reference to ‘chemical imbalances’ from their website in recent years. They now say in official statements that “the original idea that antidepressants ‘correct a chemical imbalance in the brain’ is an over-simplification.”
- Media coverage
- Source: iLexx on iStock
Media contact
tel: +44 20 7679 9222
E: chris.lane [at] ucl.ac.uk
- Latest Latest
- The West The West
- Sports Sports
- Opinion Opinion
- Magazine Magazine
Study says depression not caused by chemical imbalance, raising questions about antidepressants
University college london research says depression is not a serotonin imbalance and drugs that target it may not be the answer.

By Lois M. Collins
Millions of Americans take antidepressants, but a new study suggests the theory underpinning their use may be entirely wrong. Research from the University College London raises doubt that chemical imbalance in the brain is responsible for depression .
A major review of previous studies on serotonin’s role in depression, just published in the journal Molecular Psychiatry, concluded that serotonin level — the target of antidepressants — is not responsible for depression.
The researchers found “no support for the hypothesis that depression is caused by lowered serotonin activity or concentrations.”
They found stronger evidence that stressful life events can lead to depression.
The question is, do antidepressants help, and if so, how? If not, could they be doing harm?
Experts are divided and the study has drawn some pushback.
“Some of the studies in our overview that included people who were taking or had previously taken antidepressants showed evidence that antidepressants may actually lower the concentration or activity of serotonin,” according to an article in The Conversation by the study’s authors, Joanna Moncrieff, professor of psychiatry, and Mark Horowitz, clinical research fellow in psychiatry, both of University College London.
“Most antidepressants are selective serotonin reuptake inhibitors, which were originally said to work by correcting abnormally low serotonin levels. There is no other accepted pharmacological mechanism by which antidepressants affect the symptoms of depression,” the researchers said in a news release .
The research suggests depression is not biochemical and questions how, given that, a biochemical solution would work. Horowitz and Moncrieff also question whether that kind of treatment, which acts on brain chemistry, does more harm than good.
“Our view is that patients should not be told that depression is caused by low serotonin or by a chemical imbalance, and they should not be led to believe that antidepressants work by targeting these unproven abnormalities. We do not understand what antidepressants are doing to the brain exactly, and giving people this sort of misinformation prevents them from making an informed decision about whether to take antidepressants or not,” Moncrieff said.
Targeting serotonin
The “chemical imbalance” theory has dominated the thinking about depression for several decades, according to the researchers.
“It is always difficult to prove a negative, but I think we can safely say that after a vast amount of research conducted over several decades, there is no convincing evidence that depression is caused by serotonin abnormalities, particularly by lower levels or reduced activity of serotonin,” Moncrieff said.
In the United States between 2015 and 2018, 13.9% of adults took antidepressants for depression, according to the National Center for Health Statistics in the Centers for Disease Control and Prevention.
As many as 1 in 6 adults in England are now prescribed antidepressants every year, according to the study.
“I had been taught that depression was caused by low serotonin in my psychiatry training and had even taught this to students in my own lectures. Being involved in this research was eye-opening and feels like everything I thought I knew has been flipped upside down,” said Horowitz in background material.
As Mike McRae wrote for ScienceAlert , “This doesn’t necessarily mean serotonin-based treatments aren’t working on some other mechanism we don’t yet understand. And no one should consider ditching their meds without consulting their doctors. But given so many people are relying on these drugs, it is important to figure out what’s really going on.”
Study nuts and bolts
In all, studies in the review included tens of thousands of participants. Among the serotonin mechanisms studied and the findings:
- No difference was seen between people with depression and healthy control subjects in levels of serotonin and breakdown products in the blood or brain fluids.
- In studies of serotonin receptors and the serotonin transporter protein most antidepressants target, they found “weak and inconsistent evidence” suggesting higher levels of serotonin activity in those who are depressed. They believe that was caused by use of antidepressants.
- Studies that lowered serotonin levels in hundreds of healthy volunteers did not produce depression. The researchers saw “very weak evidence” in a small 75-person subgroup of people with a family history of depression. A study after that was inconclusive.
- No evidence of variation in the serotonin transporter gene was found between those with depression and healthy control subjects.
On the other hand, stressful life events had a “strong effect” on the risk of becoming depressed. And the more one experienced stress or trauma, the greater the likelihood of depression.
“A famous early study found a relationship between stressful events, the type of serotonin transporter gene a person had and the chance of depression. But larger, more comprehensive studies suggest this was a false finding,” the release said.
In the piece from The Conversation , Moncrieff and Horowitz wrote, “It is important that people know that the idea that depression results from a ‘chemical imbalance’ is hypothetical. And we do not understand what temporarily elevating serotonin or other biochemical changes produced by antidepressants do to the brain. We conclude that it is impossible to say that taking SSRI antidepressants is worthwhile, or even completely safe.”
Public perception
Surveys suggest as many as 90% of people believe depression is caused by low serotonin or chemical imbalance. There’s evidence believing that creates a “pessimistic outlook on the likelihood of recovery” and the hope of managing depression without medical help, the study said.
Doubts about brain chemistry’s role in depression have been around a while.
“If you’re among those who are hearing all of this for the first time, the hypothesis has been on shaky ground practically since it took off in the 1990s, with study after study failing to support the idea,” wrote ScienceAlert’s McRae . He noted the Moncrieff and Horowitz limited their research to high-quality, peer-evaluated studies.
“Just 17 studies made the cut, which included a genetic association study, another umbrella review, and a dozen systematic reviews and meta-analyses,” he wrote.
The impact is huge, given most people will have diagnosable levels of anxiety or depression at some point, the researchers said.
The researchers also said one large meta-analysis found people using antidepressants had less serotonin in their blood, which could mean that antidepressants designed to raise levels of serotonin may do the opposite over time.
The researchers note they didn’t look at the efficacy of antidepressants. Their hope, they said, is that more research and treatment will focus on helping people manage stressful or traumatic events, “such as with psychotherapy, alongside other practices such as exercise or mindfulness, or addressing underlying contributors such as poverty, stress and loneliness.”
Some experts disagree
The research has attracted some pushback.
The Guardian quoted Dr. Michael Bloomfield, a consultant psychiatrist and principal clinical research fellow at University College London, who was not involved in the study: “Many of us know that taking paracetamol can be helpful for headaches, and I don’t think anyone believes that headaches are caused by not enough paracetamol in the brain. The same logic applies to depression and medicines used to treat depression.”
He added, “There is consistent evidence that antidepressant medicines can be helpful in the treatment of depression and can be life-saving.”
Johan Lundberg at the Karolinska Institute in Sweden told New Scientist that one limitation of the study is failure to distinguish between those with long-term depression and those having episodes of depression, because their state during the study could be different in terms of serotonin. “It is key to separately analyze data from studies that examine the same patients when ill and when in remission, to have optimal conditions to examine the hypothesis,” he said.
The same article quoted a spokesperson for the Royal College of Psychiatrists who was talking about treatment guidelines from public health officials in England, who said antidepressants are an effective treatment for depression and some other physical and mental health conditions.
The spokesperson noted that “antidepressants will vary in effectiveness for different people, and the reasons for this are complex. We would not recommend for anyone to stop taking their antidepressants based on this review, and encourage anyone with concerns about their medication to contact their (family doctor).”
Depression is ‘not caused by chemical imbalance’
Major review suggests low serotonin levels are not a factor and the condition is more likely to be linked to stressful life events
Depression is not a chemical imbalance in the brain and scientists have no idea how antidepressants work, a review by University College London has concluded.
Although one in six adults in England are currently prescribed antidepressants – most of which act by maintaining serotonin levels – the new analysis suggests depression is not actually caused by low levels of serotonin.
Instead, depression may be more strongly equated with negative life events which lower mood, the review found.
Since the 1990s, antidepressant use has grown alongside the theory that the drugs establish correct levels of chemicals in the brain but researchers say that is unfounded.
“I think we can safely say that after a vast amount of research conducted over several decades, there is no convincing evidence that depression is caused by serotonin abnormalities, particularly by lower levels or reduced activity of serotonin,” said lead author Joanna Moncrieff, a professor of psychiatry at UCL.
“Many people take antidepressants because they have been led to believe their depression has a biochemical cause, but this research suggests this belief is not grounded in evidence.”
Important for mood and sleep
Most antidepressants are selective serotonin re-uptake inhibitors (SSRIs) which prevent the loss of a chemical that carries messages between nerve cells in the brain, and is important for mood and sleep.
For the new review, researchers looked again at studies into serotonin and depression and found no difference in levels between thousands of people diagnosed with the condition and healthy control participants.
The authors also looked at studies where serotonin levels were artificially lowered in hundreds of people by depriving their diets of the amino acid required to make serotonin, and found that it did not make them depressed.
People with variations in the gene governing the transportation of serotonin also showed no difference in depression levels.
In contrast, stressful life events were found to exert a strong effect on people’s risk of becoming depressed – the more stressful life events a person had experienced, the more likely they were to be depressed.
The researchers say their findings are important as studies show that as many as 85 to 90 per cent of the public believes that depression is caused by low serotonin or a chemical imbalance.
There is also evidence that believing that low mood is caused by a chemical imbalance leads people to have a pessimistic outlook on the likelihood of recovery, and the possibility of managing moods without medical help .
Co-author Dr Mark Horowitz, a training psychiatrist and clinical research fellow in psychiatry at UCL said: “I had been taught that depression was caused by low serotonin in my psychiatry training and had even taught this to students in my own lectures.
“Being involved in this research was eye-opening and feels like everything I thought I knew has been flipped upside down.
“One interesting aspect in the studies we examined was how strong an effect adverse life events played in depression, suggesting low mood is a response to people’s lives and cannot be boiled down to a simple chemical equation .”
A different route
The researchers say that patients should not be told depression is caused by a chemical imbalance, or informed that the SSRIs can correct the problem. Although it is clear the antidepressants can work, they must be doing so through a different route, the paper concludes.
Commenting on the research, experts warned people against stopping their medication .
The Royal College of Psychiatrists said: “Antidepressants will vary in effectiveness for different people, and the reasons for this are complex, which is why it’s important that patient care is based on each individual’s needs and reviewed regularly.
“Continued research into treatments for depression is important to help us better understand how medications work as well as their effectiveness. Medication should be available for anyone who needs it.
"We would not recommend for anyone to stop taking their antidepressants based on this review, and encourage anyone with concerns about their medication to contact their GP.”
Prof Allan Young, director at the Centre for Affective Disorders at King’s College London, said: “The elephant in the room is the good evidence of the efficacy and acceptability of serotonergic antidepressants.
“The use of these medicines is based on clinical trial evidence which informs their use for patients. This review does not change that.”
The review was published in the journal Molecular Psychiatry.
Depression should not be tackled as if it is a single disorder
Dr Michael Bloomfield, consultant psychiatrist at University College London
Up to one in seven of us will experience depression during our lives. Different people experience different symptoms of depression. While many people experience a mild episode, depression remains a leading global cause of morbidity. Sadly, depression can be potentially life-threatening for some due to an increased risk of suicide. Existing treatments, including several types of antidepressant medicines and psychotherapies (talking therapies), are effective, safe, and not addictive. However, beneficial treatment effects can take weeks to build up and each treatment does not work for everyone. It is therefore essential that we can understand what happens in our brains when we experience depression so that treatments can be improved and targeted.
In the middle of the 20th century, the theory that depression was caused by a chemical imbalance in serotonin represented a really important step forward in the history of medicine. Since then there’s been a huge of amount of research which tells us that the brain’s serotonin system plays very important roles in how our brains process emotions. As depression involves changes in how our brains process emotions, changes in the serotonin system are likely to be important in the development and/or treatment of depression.
The findings from this review are not surprising. Depression has numerous symptom patterns such that two people with depression can have seemingly opposite types of symptoms. For example, some sleep more when they are depressed while others suffer from insomnia. As such, having met scientists and psychiatrists from all over the world, I have yet to meet a colleague who thinks that all cases of depression are caused by a simple “chemical imbalance” in serotonin. Indeed, the serotonin system is complex. What remains likely is that changes in the serotonin system are contributing to certain symptoms in certain people. The challenge with this review is that it isn’t able to address this point because it has grouped together depression as if it is a single disorder which, from a biological perspective, does not make sense.
There is consistent evidence that antidepressant medicines can be helpful in the treatment of depression and even life-saving. This latest paper does not change this. Patients must have access to treatments for depression. Many of us know that taking paracetamol can be helpful for headaches and no one believes that headaches are caused by not enough paracetamol in the brain. The same logic applies to depression and medicines used in its treatment. All medicines can have side-effects and suddenly stopping any treatment can be potentially harmful. Anyone taking a medicine for depression who is thinking of stopping treatment should discuss this with their doctor first.
- Depression,
- Mental health,
- Health news
- Facebook Icon
- WhatsApp Icon
Applications for 2024 Columbia Summer Session programs are now open!
Faculty - August 12, 2022
Is Depression Really Caused by a Chemical Imbalance?
- Bioethics CPA
- Bioethics Executive Education
By Celine Leroudier
A surprising new study published in the journal Molecular Psychiatry recently asserted that “there is no scientific evidence to support the idea that depression is caused by an imbalance of serotonin in the brain.” The researchers further says that, despite that lack of evidence, the public widely believes that low serotonin or chemical imbalances cause depression—and “people are being prescribed antidepressants in huge quantities.”
In an interview with online biotech magazine NEO.LIFE , however, Columbia Bioethics Program Director Dr. Robert Klitzman disagrees with the study’s conclusion: “Psychiatrists use the term ‘chemical imbalance’ as a metaphor so the public can understand it. It is more accurate to say, rather than an ‘imbalance,’ that something chemical is going on in the brains of people with depression.”
Klitzman continues by examining the study’s focus on serotonin levels in the bloodstream. If depression is caused by low levels of serotonin in the brain, does it follow that correspondingly low levels of this neurochemical would be found in the bloodstream? “I would argue that depression may be caused by low serotonin levels in the microscopic spaces or synapses between neurons in various parts of the brain, but that such low levels might not necessarily be found in the bloodstream,” said Klitzman.
Learn more about Columbia’s M.S. in Bioethics program.
Related News
Congestion pricing is nearly here it is indeed ironic that democratic new jersey governor phil murphy, republican representative nicole malliotakis from staten island, and democratic representative josh gottheimer from new jersey all share intense opposition to congestion pricing south of 60th street in manhattan. faculty australia's war on elon musk listen to technology management program director alexis wichowski interviewed on australia's abc radio national about elon musk accusing australian prime minister anthony albanese of censorship. faculty environmental sustainability and consumption the best way to achieve environmental sustainability is to develop a circular economy with services and products that have the least possible impact on the environment. attacking consumption is futile and a waste of effort. all news footer social links.
203 Lewisohn Hall 2970 Broadway, MC 4119 New York, NY, 10027
© Copyright 2019 Columbia University School of Professional Studies. Privacy Policy
- International edition
- Australia edition
- Europe edition

Little evidence that chemical imbalance causes depression, UCL scientists find
Researchers question use of antidepressants, prescribed to one in six UK adults
Scientists have called into question the widespread use of antidepressants after a major review found “no clear evidence” that low serotonin levels are responsible for depression.
Prescriptions for antidepressants have risen dramatically since the 1990s, with one in six adults and 2% of teenagers in England now being prescribed them. Millions more people around the world regularly use antidepressants.
“Many people take antidepressants because they have been led to believe their depression has a biochemical cause, but this new research suggests this belief is not grounded in evidence,” said the study’s lead author, Joanna Moncrieff, a professor of psychiatry at University College London and consultant psychiatrist at North East London NHS foundation trust.
“It is always difficult to prove a negative, but I think we can safely say that after a vast amount of research conducted over several decades, there is no convincing evidence that depression is caused by serotonin abnormalities, particularly by lower levels or reduced activity of serotonin.
“Thousands of people suffer from side-effects of antidepressants, including the severe withdrawal effects that can occur when people try to stop them, yet prescription rates continue to rise. We believe this situation has been driven partly by the false belief that depression is due to a chemical imbalance. It is high time to inform the public that this belief is not grounded in science.”
The new review of existing studies found that depression is not likely to be caused by a chemical imbalance and said people should be made aware of other options for treating it.
However, other experts, including from the Royal College of Psychiatrists, questioned the findings and urged people not to stop taking their medication in light of the study, arguing that antidepressants remained effective.
In the new analysis, researchers said 85% to 90% of the public believed depression was caused by low serotonin or a chemical imbalance.
Most antidepressants are selective serotonin reuptake inhibitors (SSRIs), originally said to work by correcting abnormally low serotonin levels.
The review, published in the journal Molecular Psychiatry , looked at studies examining serotonin and depression involving tens of thousands of people. One of the findings was that research comparing levels of serotonin and its breakdown products in the blood or brain fluids did not discover any difference between people diagnosed with depression and healthy people.
The authors also looked at studies where serotonin levels were artificially lowered in hundreds of people and concluded that lowering serotonin in this way did not produce depression in hundreds of healthy volunteers.
Other studies looked at the effects of stressful life events and found that the more stressful life events a person had experienced, the more likely they were to be depressed, showing the importance of external events.
According to the research, there is also evidence from other studies that antidepressants may actually induce low serotonin in the long term.
“Our view is that patients should not be told that depression is caused by low serotonin or by a chemical imbalance, and they should not be led to believe that antidepressants work by targeting these unproven abnormalities,” said Moncrieff.
“We do not understand what antidepressants are doing to the brain exactly, and giving people this sort of misinformation prevents them from making an informed decision about whether to take antidepressants or not.”
A spokesperson for the Royal College of Psychiatrists said: “Antidepressants are an effective, Nice-recommended treatment for depression that can also be prescribed for a range of physical and mental health conditions. We would not recommend for anyone to stop taking their antidepressants based on this review, and encourage anyone with concerns about their medication to contact their GP.”
Dr Michael Bloomfield, a consultant psychiatrist and principal clinical research fellow at University College London, who was not involved in the study, said: “Many of us know that taking paracetamol can be helpful for headaches, and I don’t think anyone believes that headaches are caused by not enough paracetamol in the brain. The same logic applies to depression and medicines used to treat depression.
“There is consistent evidence that antidepressant medicines can be helpful in the treatment of depression and can be life-saving.”
- Mental health
- UCL (University College London)
Most viewed
'No convincing evidence' depression caused by low serotonin levels
Doctors have insisted antidepressants are effective and urged people not to stop taking their medication.
Wednesday 20 July 2022 03:16, UK

Many antidepressants might not be treating the condition, because they are being used to correct a cause of depression that does not actually exist, new research has suggested.
A new review of existing studies concludes that the "chemical imbalance" theory of depression, in particular low levels of serotonin, does not stand up to scrutiny.
Serotonin is a chemical transmitter that appears to play a role in governing mood and emotions.
Most antidepressants are selective serotonin reuptake inhibitors (SSRIs), and were originally said to work by correcting abnormally low serotonin levels.
However the umbrella study, carried out by researchers at University College London (UCL) and published in Molecular Psychiatry, suggests that depression is not likely caused by a chemical imbalance, and calls into question what antidepressants do.
The number of people in England taking antidepressants has been rising, according to NHS figures, with 8.3 million patients receiving them in 2021/22, a 6% rise on the previous year when the figure was 7.9 million.
The UCL team said 85% to 90% of the public believes that depression is caused by low serotonin or a chemical imbalance, however this does not appear to be the case and patients should be made aware of other options for treating depression .
More on Depression

Exercise even better than anti-depressants at treating depression, study finds

Hallucinogen found in magic mushrooms can reduce depression, study finds

Outdoor swimming to treat depression to be trialled as alternative to drugs
Related Topics:
The lead author of the review, Joanna Moncrieff, professor of psychiatry at UCL, said: "It is always difficult to prove a negative, but I think we can safely say that after a vast amount of research conducted over several decades, there is no convincing evidence that depression is caused by serotonin abnormalities, particularly by lower levels or reduced activity of serotonin.
"The popularity of the 'chemical imbalance' theory of depression has coincided with a huge increase in the use of antidepressants...
"Thousands of people suffer from side-effects of antidepressants, including the severe withdrawal effects that can occur when people try to stop them, yet prescription rates continue to rise.
"We believe this situation has been driven partly by the false belief that depression is due to a chemical imbalance.
"It is high time to inform the public that this belief is not grounded in science."
Read more: Sharp increase in number of anti-anxiety drug prescriptions, study finds
Please use Chrome browser for a more accessible video player

However the Royal College of Psychiatrists said patients should continue to take the medication they had been prescribed.
A spokesman said: "Medication should be available for anyone who needs it. We would not recommend for anyone to stop taking their antidepressants based on this review, and encourage anyone with concerns about their medication to contact their GP."
Professor Allan Young, director of the Centre for Affective Disorders at the Institute of Psychiatry, said of the new study: "The (undiscussed) elephant in the room is the good evidence of the efficacy and acceptability of serotonergic antidepressants.
"The use of these medicines is based on clinical trial evidence which informs their use for patients.
"This review does not change that."
Related Topics
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
Nih research matters.
April 23, 2024
Research in Context: Treating depression
Finding better approaches.
While effective treatments for major depression are available, there is still room for improvement. This special Research in Context feature explores the development of more effective ways to treat depression, including personalized treatment approaches and both old and new drugs.

Everyone has a bad day sometimes. People experience various types of stress in the course of everyday life. These stressors can cause sadness, anxiety, hopelessness, frustration, or guilt. You may not enjoy the activities you usually do. These feelings tend to be only temporary. Once circumstances change, and the source of stress goes away, your mood usually improves. But sometimes, these feelings don’t go away. When these feelings stick around for at least two weeks and interfere with your daily activities, it’s called major depression, or clinical depression.
In 2021, 8.3% of U.S. adults experienced major depression. That’s about 21 million people. Among adolescents, the prevalence was much greater—more than 20%. Major depression can bring decreased energy, difficulty thinking straight, sleep problems, loss of appetite, and even physical pain. People with major depression may become unable to meet their responsibilities at work or home. Depression can also lead people to use alcohol or drugs or engage in high-risk activities. In the most extreme cases, depression can drive people to self-harm or even suicide.
The good news is that effective treatments are available. But current treatments have limitations. That’s why NIH-funded researchers have been working to develop more effective ways to treat depression. These include finding ways to predict whether certain treatments will help a given patient. They're also trying to develop more effective drugs or, in some cases, find new uses for existing drugs.
Finding the right treatments
The most common treatments for depression include psychotherapy, medications, or a combination. Mild depression may be treated with psychotherapy. Moderate to severe depression often requires the addition of medication.
Several types of psychotherapy have been shown to help relieve depression symptoms. For example, cognitive behavioral therapy helps people to recognize harmful ways of thinking and teaches them how to change these. Some researchers are working to develop new therapies to enhance people’s positive emotions. But good psychotherapy can be hard to access due to the cost, scheduling difficulties, or lack of available providers. The recent growth of telehealth services for mental health has improved access in some cases.
There are many antidepressant drugs on the market. Different drugs will work best on different patients. But it can be challenging to predict which drugs will work for a given patient. And it can take anywhere from 6 to 12 weeks to know whether a drug is working. Finding an effective drug can involve a long period of trial and error, with no guarantee of results.
If depression doesn’t improve with psychotherapy or medications, brain stimulation therapies could be used. Electroconvulsive therapy, or ECT, uses electrodes to send electric current into the brain. A newer technique, transcranial magnetic stimulation (TMS), stimulates the brain using magnetic fields. These treatments must be administered by specially trained health professionals.
“A lot of patients, they kind of muddle along, treatment after treatment, with little idea whether something’s going to work,” says psychiatric researcher Dr. Amit Etkin.
One reason it’s difficult to know which antidepressant medications will work is that there are likely different biological mechanisms that can cause depression. Two people with similar symptoms may both be diagnosed with depression, but the causes of their symptoms could be different. As NIH depression researcher Dr. Carlos Zarate explains, “we believe that there’s not one depression, but hundreds of depressions.”
Depression may be due to many factors. Genetics can put certain people at risk for depression. Stressful situations, physical health conditions, and medications may contribute. And depression can also be part of a more complicated mental disorder, such as bipolar disorder. All of these can affect which treatment would be best to use.
Etkin has been developing methods to distinguish patients with different types of depression based on measurable biological features, or biomarkers. The idea is that different types of patients would respond differently to various treatments. Etkin calls this approach “precision psychiatry.”
One such type of biomarker is electrical activity in the brain. A technique called electroencephalography, or EEG, measures electrical activity using electrodes placed on the scalp. When Etkin was at Stanford University, he led a research team that developed a machine-learning algorithm to predict treatment response based on EEG signals. The team applied the algorithm to data from a clinical trial of the antidepressant sertraline (Zoloft) involving more than 300 people.

EEG data for the participants were collected at the outset. Participants were then randomly assigned to take either sertraline or an inactive placebo for eight weeks. The team found a specific set of signals that predicted the participants’ responses to sertraline. The same neural “signature” also predicted which patients with depression responded to medication in a separate group.
Etkin’s team also examined this neural signature in a set of patients who were treated with TMS and psychotherapy. People who were predicted to respond less to sertraline had a greater response to the TMS/psychotherapy combination.
Etkin continues to develop methods for personalized depression treatment through his company, Alto Neuroscience. He notes that EEG has the advantage of being low-cost and accessible; data can even be collected in a patient’s home. That’s important for being able to get personalized treatments to the large number of people they could help. He’s also working on developing antidepressant drugs targeted to specific EEG profiles. Candidate drugs are in clinical trials now.
“It’s not like a pie-in-the-sky future thing, 20-30 years from now,” Etkin explains. “This is something that could be in people's hands within the next five years.”
New tricks for old drugs
While some researchers focus on matching patients with their optimal treatments, others aim to find treatments that can work for many different patients. It turns out that some drugs we’ve known about for decades might be very effective antidepressants, but we didn’t recognize their antidepressant properties until recently.
One such drug is ketamine. Ketamine has been used as an anesthetic for more than 50 years. Around the turn of this century, researchers started to discover its potential as an antidepressant. Zarate and others have found that, unlike traditional antidepressants that can take weeks to take effect, ketamine can improve depression in as little as one day. And a single dose can have an effect for a week or more. In 2019, the FDA approved a form of ketamine for treating depression that is resistant to other treatments.
But ketamine has drawbacks of its own. It’s a dissociative drug, meaning that it can make people feel disconnected from their body and environment. It also has the potential for addiction and misuse. For these reasons, it’s a controlled substance and can only be administered in a doctor’s office or clinic.
Another class of drugs being studied as possible antidepressants are psychedelics. These include lysergic acid diethylamide (LSD) and psilocybin, the active ingredient in magic mushrooms. These drugs can temporarily alter a person’s mood, thoughts, and perceptions of reality. Some have historically been used for religious rituals, but they are also used recreationally.
In clinical studies, psychedelics are typically administered in combination with psychotherapy. This includes several preparatory sessions with a therapist in the weeks before getting the drug, and several sessions in the weeks following to help people process their experiences. The drugs are administered in a controlled setting.
Dr. Stephen Ross, co-director of the New York University Langone Health Center for Psychedelic Medicine, describes a typical session: “It takes place in a living room-like setting. The person is prepared, and they state their intention. They take the drug, they lie supine, they put on eye shades and preselected music, and two therapists monitor them.” Sessions last for as long as the acute effects of the drug last, which is typically several hours. This is a healthcare-intensive intervention given the time and personnel needed.
In 2016, Ross led a clinical trial examining whether psilocybin-assisted therapy could reduce depression and anxiety in people with cancer. According to Ross, as many as 40% of people with cancer have clinically significant anxiety and depression. The study showed that a single psilocybin session led to substantial reductions in anxiety and depression compared with a placebo. These reductions were evident as soon as one day after psilocybin administration. Six months later, 60-80% of participants still had reduced depression and anxiety.
Psychedelic drugs frequently trigger mystical experiences in the people who take them. “People can feel a sense…that their consciousness is part of a greater consciousness or that all energy is one,” Ross explains. “People can have an experience that for them feels more ‘real’ than regular reality. They can feel transported to a different dimension of reality.”
About three out of four participants in Ross’s study said it was among the most meaningful experiences of their lives. And the degree of mystical experience correlated with the drug’s therapeutic effect. A long-term follow-up study found that the effects of the treatment continued more than four years later.
If these results seem too good to be true, Ross is quick to point out that it was a small study, with only 29 participants, although similar studies from other groups have yielded similar results. Psychedelics haven’t yet been shown to be effective in a large, controlled clinical trial. Ross is now conducting a trial with 200 people to see if the results of his earlier study pan out in this larger group. For now, though, psychedelics remain experimental drugs—approved for testing, but not for routine medical use.
Unlike ketamine, psychedelics aren’t considered addictive. But they, too, carry risks, which certain conditions may increase. Psychedelics can cause cardiovascular complications. They can cause psychosis in people who are predisposed to it. In uncontrolled settings, they have the risk of causing anxiety, confusion, and paranoia—a so-called “bad trip”—that can lead the person taking the drug to harm themself or others. This is why psychedelic-assisted therapy takes place in such tightly controlled settings. That increases the cost and complexity of the therapy, which may prevent many people from having access to it.
Better, safer drugs
Despite the promise of ketamine or psychedelics, their drawbacks have led some researchers to look for drugs that work like them but with fewer side effects.
Depression is thought to be caused by the loss of connections between nerve cells, or neurons, in certain regions of the brain. Ketamine and psychedelics both promote the brain’s ability to repair these connections, a quality called plasticity. If we could understand how these drugs encourage plasticity, we might be able to design drugs that can do so without the side effects.

Dr. David Olson at the University of California, Davis studies how psychedelics work at the cellular and molecular levels. The drugs appear to promote plasticity by binding to a receptor in cells called the 5-hydroxytryptamine 2A receptor (5-HT2AR). But many other compounds also bind 5-HT2AR without promoting plasticity. In a recent NIH-funded study, Olson showed that 5-HT2AR can be found both inside and on the surface of the cell. Only compounds that bound to the receptor inside the cells promoted plasticity. This suggests that a drug has to be able to get into the cell to promote plasticity.
Moreover, not all drugs that bind 5-HT2AR have psychedelic effects. Olson’s team has developed a molecular sensor, called psychLight, that can identify which compounds that bind 5-HT2AR have psychedelic effects. Using psychLight, they identified compounds that are not psychedelic but still have rapid and long-lasting antidepressant effects in animal models. He’s founded a company, Delix Therapeutics, to further develop drugs that promote plasticity.
Meanwhile, Zarate and his colleagues have been investigating a compound related to ketamine called hydroxynorketamine (HNK). Ketamine is converted to HNK in the body, and this process appears to be required for ketamine’s antidepressant effects. Administering HNK directly produced antidepressant-like effects in mice. At the same time, it did not cause the dissociative side effects and addiction caused by ketamine. Zarate’s team has already completed phase I trials of HNK in people showing that it’s safe. Phase II trials to find out whether it’s effective are scheduled to begin soon.
“What [ketamine and psychedelics] are doing for the field is they’re helping us realize that it is possible to move toward a repair model versus a symptom mitigation model,” Olson says. Unlike existing antidepressants, which just relieve the symptoms of depression, these drugs appear to fix the underlying causes. That’s likely why they work faster and produce longer-lasting effects. This research is bringing us closer to having safer antidepressants that only need to be taken once in a while, instead of every day.
—by Brian Doctrow, Ph.D.
Related Links
- How Psychedelic Drugs May Help with Depression
- Biosensor Advances Drug Discovery
- Neural Signature Predicts Antidepressant Response
- How Ketamine Relieves Symptoms of Depression
- Protein Structure Reveals How LSD Affects the Brain
- Predicting The Usefulness of Antidepressants
- Depression Screening and Treatment in Adults
- Serotonin Transporter Structure Revealed
- Placebo Effect in Depression Treatment
- When Sadness Lingers: Understanding and Treating Depression
- Psychedelic and Dissociative Drugs
References: An electroencephalographic signature predicts antidepressant response in major depression. Wu W, Zhang Y, Jiang J, Lucas MV, Fonzo GA, Rolle CE, Cooper C, Chin-Fatt C, Krepel N, Cornelssen CA, Wright R, Toll RT, Trivedi HM, Monuszko K, Caudle TL, Sarhadi K, Jha MK, Trombello JM, Deckersbach T, Adams P, McGrath PJ, Weissman MM, Fava M, Pizzagalli DA, Arns M, Trivedi MH, Etkin A. Nat Biotechnol. 2020 Feb 10. doi: 10.1038/s41587-019-0397-3. Epub 2020 Feb 10. PMID: 32042166. Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: a randomized controlled trial. Ross S, Bossis A, Guss J, Agin-Liebes G, Malone T, Cohen B, Mennenga SE, Belser A, Kalliontzi K, Babb J, Su Z, Corby P, Schmidt BL. J Psychopharmacol . 2016 Dec;30(12):1165-1180. doi: 10.1177/0269881116675512. PMID: 27909164. Long-term follow-up of psilocybin-assisted psychotherapy for psychiatric and existential distress in patients with life-threatening cancer. Agin-Liebes GI, Malone T, Yalch MM, Mennenga SE, Ponté KL, Guss J, Bossis AP, Grigsby J, Fischer S, Ross S. J Psychopharmacol . 2020 Feb;34(2):155-166. doi: 10.1177/0269881119897615. Epub 2020 Jan 9. PMID: 31916890. Psychedelics promote neuroplasticity through the activation of intracellular 5-HT2A receptors. Vargas MV, Dunlap LE, Dong C, Carter SJ, Tombari RJ, Jami SA, Cameron LP, Patel SD, Hennessey JJ, Saeger HN, McCorvy JD, Gray JA, Tian L, Olson DE. Science . 2023 Feb 17;379(6633):700-706. doi: 10.1126/science.adf0435. Epub 2023 Feb 16. PMID: 36795823. Psychedelic-inspired drug discovery using an engineered biosensor. Dong C, Ly C, Dunlap LE, Vargas MV, Sun J, Hwang IW, Azinfar A, Oh WC, Wetsel WC, Olson DE, Tian L. Cell . 2021 Apr 8: S0092-8674(21)00374-3. doi: 10.1016/j.cell.2021.03.043. Epub 2021 Apr 28. PMID: 33915107. NMDAR inhibition-independent antidepressant actions of ketamine metabolites. Zanos P, Moaddel R, Morris PJ, Georgiou P, Fischell J, Elmer GI, Alkondon M, Yuan P, Pribut HJ, Singh NS, Dossou KS, Fang Y, Huang XP, Mayo CL, Wainer IW, Albuquerque EX, Thompson SM, Thomas CJ, Zarate CA Jr, Gould TD. Nature . 2016 May 26;533(7604):481-6. doi: 10.1038/nature17998. Epub 2016 May 4. PMID: 27144355.
Connect with Us
- More Social Media from NIH

Mental Health Stigma
How medical psychiatry may worsen mental-health stigma, challenging the received wisdom about mental health..
Posted April 25, 2024 | Reviewed by Gary Drevitch
- Seeing mental illness as having a biological cause tends to make stigma worse, not better.
- Trauma-based explanations of mental illness do not seem to have these negative effects.
- We should reconsider public messaging about mental health in light of these findings.

In the 1980s and 90s, an emerging theory was that mental disorders like depression , bipolar disorder , or schizophrenia were due to faulty brain chemicals, and ultimately, faulty genes.
This message was popularized by books like Nancy Andreasen’s 1985 The Broken Brain , Solomon Snyder’s 1986 Drugs and the Brain , and Jon Franklin’s 1987 Molecules of the Mind .
In this view, schizophrenia was due to dopamine imbalances. Depression involved serotonin imbalances. Bipolar disorder involved lithium imbalances. And drugs like Prozac worked by reversing these imbalances.
While simplistic versions of many of these theories were disproven , the “chemical imbalance” metaphor still has a powerful grip on the professional and public imagination .
Journalists, doctors, and activists thought that this messaging would help end stigma by showing that you’re not to blame for your mental health problems, any more than you’re to blame for breast cancer.
New research, however, is calling this received wisdom into question. This research is showing that medical framings of mental health problems actually make some kinds of stigma worse , not better.
Challenging the Received Wisdom
Over the last decade, a group of psychologists have investigated new questions about mental health stigma .
For example, if I think that your mental illness is caused by your brain or your genes, how does that affect my desire to interact with you? This is known as the desire for social distance .
Similarly, if I think that your mental illness is caused by your brain or your genes, how does that affect my belief that you will recover? This is known as prognostic optimism .
The upshot of this research is that biological explanations of mental illnesses have their own dangers. They tend to increase people’s desire for social distance . If I think your mental illness is caused by your brain or genes, I’m more likely to see you as potentially dangerous and unpredictable, and to want to keep my distance from you. They also decrease prognostic optimism: If I see your mental illness as having a biological cause, I have less hope that you’re going to recover.
On the plus side, these mindsets do reduce the perception of blame: If I think your schizophrenia or depression is caused by your genes, I’m less likely to blame you for it.
One of the most troubling findings in this new research is that, by several measures, stigma towards schizophrenia has actually gotten worse over the last 30 years, not better. This may be related to the greater acceptance of the medical paradigm.
Making Stigma Worse?
Research carried out last year, while confirming those main findings, raised new puzzles of its own. This research was led by sociologist Marta Elliott of the University of Nevada, Reno and published in August, 2023 in Psychiatric Services [1]. Elliott sought to better understand what happens when conditions like schizophrenia, depression, or addiction are presented as having a genetic, versus an environmental, cause. Her team also wanted to know what happens when we combine different sorts of explanations, such as biological and environmental ones.
As they put it, “to our knowledge, this study is the first of its kind to manipulate multiple attributions and treatability and to test their independent and interactive effects on stigma with a large sample representative of the U.S. adult population.”
To this end, they recruited over 1,600 participants and presented various hypothetical scenarios to them (“vignettes”). In one vignette, a man consults a physician and is told his mental disorder is genetic. In another, he is told his mental disorder is caused by trauma. In yet another, he is told his mental disorder is caused by both genes and trauma.
The participants were then asked questions, such as how willing they would be to spend an evening socializing with the man or making friends with him.
Predictably, biological explanations increase the desire for social distance, regardless of which mental illness is in question. The desire for social distance was far stronger for schizophrenia and addiction than for depression.

New Puzzles
Elliott's research, however, raised two new puzzles. First, she found no negative impact on public stigma when mental illness was presented as caused by life trauma. If I see your depression as the result of, say, profound grief , I’m just as likely to want to socialize with you or be friends with you. Knowing that your mental health problems stem from negative life events seems to have a powerful humanizing influence on how people think about those who suffer from mental illnesses.
Second, when offered an explanation that combined life trauma with genetics , participants’ desire for social distance increased almost as much as it did when the biological account was presented alone. It’s as if the “genetic” part of the explanation cancels out the humanizing impact of the traumatic event.
It seems to me that one possible explanation for these findings is that if I see your mental illness as a meaningful response to the problems of life, I’m less likely to see it as defining your very identity .
The authors note that these results may have implications for how psychiatrists and other mental health professionals, as well as the media, discuss mental illness: “Portraying mental illness in exclusively genetic terms may perpetuate stigma, encourage discrimination , and harm the mental health of people living with psychiatric diagnoses.”
As psychologists Eleanor Longden and John Read put the point, when it comes to mental illness, it may be time to start seeing “ people with problems ” rather than “patients with illnesses.”
Elliott, M., Ragsdale, J. M., and LaMotte, M. E. 2024. Causal Explanations, Treatability, and Mental Illness Stigma: Experimental Study. Psychiatric Services 75: 131-138. DOI: 10.1176/appi.ps.20230169

Justin Garson, Ph.D., is a philosopher and author of Madness: A Philosophical Exploration (Oxford, 2022) and The Biological Mind: A Philosophical Introduction, Second Edition (Routledge, 2022).
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience

IMAGES
VIDEO
COMMENTS
Source: vdnhieu/Pixabay. The idea that depression is caused by chemical imbalance in the brain—specifically lower serotonin levels—and can therefore be treated effectively with drugs that ...
For three decades, people have been deluged with information suggesting that depression is caused by a "chemical imbalance" in the brain - namely an imbalance of a brain chemical called serotonin. However, our latest research review shows that the evidence does not support it.
The new umbrella review -- an overview of existing meta-analyses and systematic reviews -- published in Molecular Psychiatry, suggests that depression is not likely caused by a chemical imbalance ...
The origins of speculations that mood disorders arise from a chemical imbalance in the brain can be traced back further, to the mid-20th century, when a monoamine neurotransmitter called noradrenaline was proposed to be out of whack in people with depression. Serotonin - that other famous monoamine - was also viewed with suspicion, leading ...
A new published review finds no evidence that low serotonin levels cause depression. The authors use their data to refute the "chemical imbalance" hypothesis of depression, which is an old and ...
Depression is probably not caused by a chemical imbalance in the brain - new study Published: July 20, 2022 1:12am EDT • Updated: July 21, 2022 6:32am EDT Joanna Moncrieff , Mark Horowitz , UCL
The chemical imbalance theory of depression is still put forward by professionals , and the serotonin theory, in particular, has formed the basis of a considerable research effort over the last ...
For three decades, people have been deluged with information suggesting that depression is caused by a "chemical imbalance" in the brain—namely an imbalance of a brain chemical called serotonin.
Published in Molecular Psychiatry, the findings come after decades of scrutinizing existing meta-analyses and systematic reviews. Researchers suggest that depression is not likely caused by a chemical imbalance in the brain, and challenge the role of antidepressants as the first line of treatment. "For decades people have been given the ...
The serotonin hypothesis, which dates from the 1960s, says that a chemical imbalance in the brain, including low levels of serotonin, also known as 5-hydroxytryptamine or 5-HT, leads to depression.
Serotonin genes aren't linked to depression. Other branches of research led to the overall conclusion of no link but were not as strong. They sometimes left open questions to further research ...
The phrase "chemical imbalance" is too vague to be true or false; it doesn't mean much of anything when it comes to the brain and all its complexity. Serotonin, the chemical messenger often ...
Surveys indicate that more than 80% of the public blames a "chemical imbalance" in the brain. That idea is widespread in pop psychology and cited in research papers and medical textbooks . Listening to Prozac , a book that describes the life-changing value of treating depression with medications that aim to correct this imbalance, spent ...
Maybe the cause of depression is indeed not a chemical imbalance, but rather adverse life events. But maybe using SSRIs (that increase levels of serotonin more than the normal person) helps to overcome this state of mind. ... New Research Reveals That Human Brains Are Getting Larger . April 22, 2024. Astronomers Discover 49 New Galaxies in ...
The new umbrella review - an overview of existing meta-analyses and systematic reviews - published in Molecular Psychiatry, suggests that depression is not likely caused by a chemical imbalance, and calls into question what antidepressants do. Most antidepressants are selective serotonin reuptake inhibitors (SSRIs), which were originally ...
Public perception. Surveys suggest as many as 90% of people believe depression is caused by low serotonin or chemical imbalance. There's evidence believing that creates a "pessimistic outlook on the likelihood of recovery" and the hope of managing depression without medical help, the study said. Doubts about brain chemistry's role in ...
Source: The Conversation. For three decades, people have been deluged with information suggesting that depression is caused by a "chemical imbalance" in the brain - namely an imbalance of a brain chemical called serotonin. However, our latest research review shows that the evidence does not support it. Although first proposed in the 1960s ...
Sarah Knapton, Science Editor 20 July 2022 • 6:00am. Depression is not a chemical imbalance in the brain and scientists have no idea how antidepressants work, a review by University College ...
By Celine Leroudier. A surprising new study published in the journal Molecular Psychiatry recently asserted that "there is no scientific evidence to support the idea that depression is caused by an imbalance of serotonin in the brain." The researchers further says that, despite that lack of evidence, the public widely believes that low serotonin or chemical imbalances cause depression ...
In the new analysis, researchers said 85% to 90% of the public believed depression was caused by low serotonin or a chemical imbalance. Most antidepressants are selective serotonin reuptake ...
A new review of existing studies concludes that the "chemical imbalance" theory of depression, in particular low levels of serotonin, does not stand up to scrutiny. Serotonin is a chemical ...
A recent review study is pushing back against long-held views in medicine that depression is caused by a serotonin imbalance in the brain. Researchers from University College London conducted an ...
Unlike existing antidepressants, which just relieve the symptoms of depression, these drugs appear to fix the underlying causes. That's likely why they work faster and produce longer-lasting effects. This research is bringing us closer to having safer antidepressants that only need to be taken once in a while, instead of every day.
In the 1980s and 90s, an emerging theory was that mental disorders like depression, bipolar disorder, or schizophrenia were due to faulty brain chemicals, and ultimately, faulty genes. This ...