

Gender-affirming surgical care in British Columbia
ABSTRACT: A variety of gender-affirming surgical procedures are available to transgender and gender-diverse individuals in BC. Care throughout the entire surgical journey is shared by a multidisciplinary team of surgical specialists and allied health care providers. Upper body gender-affirming surgeries include breast construction, chest construction with subcutaneous mastectomy and male chest contouring, and gender-affirming breast reduction. Lower body gender-affirming surgeries include orchiectomy, vaginoplasty, penectomy, metoidioplasty, phalloplasty, hysterectomy, and bilateral salpingo-oophorectomy. Surgeons are encouraged to follow the World Professional Association for Transgender Health criteria for patient eligibility for these surgeries. All these procedures have associated risks, and all are covered by British Columbia’s Medical Services Plan. Some complementary procedures are funded by Trans Care BC. In addition, facial and neck procedures such as facial feminization, tracheal shaving, and voice surgery may be performed. However, the World Professional Association for Transgender Health does not specify eligibility criteria for these procedures, and they are not currently covered by MSP. Surgeons and physicians should take an individualized approach to providing gender-affirming patient care in order to maximize surgical outcomes and prioritize specific harm-reduction strategies.
Being able to access medically necessary gender-affirming surgeries close to home with the support of a multidisciplinary medical team can maximize the health and well-being of transgender and gender-diverse people.
The goal of gender-affirming surgical care is to maximize the health and well-being of transgender and gender-diverse individuals.[ 1 ] While not all these individuals seek surgical interventions as part of their journey, many find surgery an important and key component of their transition. In September 2019, the Gender Surgery Program BC, located within Vancouver Coastal Health, became Western Canada’s first and only centre to perform lower body gender-affirming surgeries for transgender and gender-diverse individuals. The multidisciplinary team of surgical specialists and allied health care providers provide shared care throughout the entire surgical journey. This program builds upon the existing gender-affirming surgical services offered throughout the province to provide patients with access to safe surgical care close to home. In addition to the Gender Surgery Program BC, Trans Care BC has established a network of transgender-inclusive surgical providers throughout the province and within all health authorities who offer upper body surgery, orchiectomy, and hysterectomy.[ 2 ]
In BC, gender-affirming surgical care largely follows the direction and guidance of the World Professional Association for Transgender Health (WPATH). Current guidelines for surgical standards of care are summarized in the Table .[ 1 ] Not all transition services are currently covered by the provincial Medical Services Plan; procedures that are considered an insured service for transgender individuals are listed in the Table . In addition, an individual’s gender identity is often not binary and may exist along the gender spectrum. As a result, patients may seek some surgical interventions and not others as part of their journey. The following procedures are broadly classified based on anatomic location. Each procedure is an individual choice that may aid a patient to move along the gender spectrum.
Chest and breast procedures
Breast construction (augmentation mammoplasty).
In BC, augmentation mammoplasty is considered to be medically necessary for transgender women who have insufficient breast tissue growth following 18 months of feminizing hormone therapy.[ 3 , 4 ] Prosthetic implants are the mainstay for enhancing the size and symmetry of the chest. Criteria for MSP coverage include insufficient breast growth (less than an AA cup size) or asymmetrical growth of more than 1.5 cup sizes following 18 months of continuous hormone therapy. Women can also be considered for augmentation mammoplasty if hormone therapy is medically contraindicated and they have a less than an AA breast cup [ Table ].
Specific complications with augmentation mammoplasty are rare but include capsular contracture (scar tissue formation around the implant); implant migration, rupture, or exposure; altered sensation; and anaplastic large cell lymphoma.[ 5-7 ] Surgeons in BC are encouraged to follow the WPATH guidelines for patient inclusion criteria [ Table ].
Chest construction with subcutaneous mastectomy and male chest contouring
A subcutaneous mastectomy with male chest contouring involves the removal or reduction of breast tissue and skin to construct a flatter, more sculpted masculine chest. It can be performed with or without nipple and areola resizing and repositioning.[ 8 ] Chest binding, often used by transgender men, may lead to the loss of skin elasticity; therefore, significant excess skin may need to be removed to create a more aesthetically appealing chest.[ 3 ] This surgery can be an important step for transgender men and nonbinary individuals who feel more comfortable with a flat chest or who restrict their activities and social engagement due to body and binder discomfort.[ 3 ] Subcutaneous mastectomy and chest contouring is covered by MSP, and a centralized wait list is managed by Trans Care BC.[ 3 ] Complications specific to this surgery include hematoma or seroma, loss of nipple grafts due to necrosis, change in nipple or areolar sensation, asymmetry or contour abnormalities requiring secondary revisions, and visible scarring.[ 3 , 8 ] Surgeons are encouraged to follow the WPATH guidelines for patient inclusion criteria [ Table ].
Gender-affirming breast reduction
Gender-affirming breast reduction uses surgical principles to reduce chest tissue volume and nipple size. Many nonbinary patients seek breast reduction to feel more affirmed, reduce the need for chest binders, and facilitate clothing choices. This procedure uses similar incision patterns to a standard breast reduction. It is covered by MSP, regardless of chest volume.
Genital procedures
Orchiectomy.
Orchiectomy involves the removal of the testes and spermatic cord to prevent testicular hormone (i.e., testosterone) and sperm production. This procedure reduces the required dose of feminizing hormones and the need for androgen-blocking medications.[ 4 ] Based on patient goals, orchiectomy can be completed independently (with or without scrotectomy) or combined with penile inversion vaginoplasty. Orchiectomy results in permanent sterilization; therefore, sperm banking is suggested for individuals who are interested in future fertility. This procedure is performed in BC and is covered by MSP. Surgeons are encouraged to follow the WPATH guidelines for patient inclusion criteria [ Table ].
Vaginoplasty
Vaginoplasty is the surgical creation of a vaginal cavity and external vulva (consisting of an anatomic clitoral complex and labial complex). The preferred surgical technique is the penile inversion vaginoplasty, which uses the penile and/or scrotal tissue to create the neovagina.[ 3 ] In revision cases or for patients with a technically challenging anatomy, a pedicled colosigmoid transplant or peritoneal vaginoplasty can be offered as an alternative.[ 3 ] Orchiectomy can be completed prior to or during the vaginoplasty procedure. Permanent hair removal of tissue used for vaginal cavity construction is required to avoid hair growth within the vaginal lining. Perineal and scrotal electrolysis for hair removal is funded by Trans Care BC. Vaginal dilation is required postoperatively to maintain the depth and width of the vaginal cavity. Educational sessions are provided postoperatively, and dilators are funded by Trans Care BC. Pelvic floor physiotherapy preoperatively and postoperatively is thought to enhance the surgical outcomes for vaginoplasty patients. Surgical risks include urethral stricture, vaginal stenosis, partial or complete inversion flap loss, hypergranulation tissue, vaginal prolapse, cosmetic dissatisfaction, reduced erogenous sensation, vesicovaginal or rectovaginal fistula, pelvic pain, and postoperative voiding dysfunction.[ 2 , 6 ] Penile inversion vaginoplasty completed in BC is covered by MSP. Surgeons at the Gender Surgery Program BC who offer this procedure follow the WPATH guidelines for patient inclusion criteria [ Table ].
Minimal depth vaginoplasty
Minimal depth vaginoplasty, also referred to as vulvoplasty, is similar to vaginoplasty but a vaginal canal is not created. Instead, a shallow vaginal depression is created when constructing the external genital structures.[ 2 , 5 ] This procedure may be preferred in medically complex patients or individuals who do not wish to have a vaginal cavity. Minimal depth vaginoplasty has the same inclusion criteria and similar complication profile as vaginoplasty (but less risk of stenosis and fistula).
Penectomy involves removal of the penis. While more commonly performed as part of a penile inversion vaginoplasty, some individuals may choose penectomy as a stand-alone procedure.
Metoidioplasty
Metoidioplasty involves the creation of masculine genitalia from existing clitoral and labial tissues. This begins with hormonal enlargement of the clitoris (virilization), followed by surgical release of its attachment ligaments to create a phallus that is 4 to 6 cm long, and removal of the vagina. The labia majora are mobilized to create the scrotum.[ 3 ] Testis implants and reduction of residual labial tissue adjacent to the penis are completed approximately 6 months after the initial procedure. While metoidioplasty extends the urethra externally, standing urination cannot always be ensured due to differences in patient anatomy.[ 2 ] Moreover, it is unlikely that individuals undergoing metoidioplasty will be able to engage in penetrative intercourse because the surgery does not permit internal placement of an erectile device.[ 3 ] Compared to phalloplasty, metoidioplasty is considered a less invasive procedure, and is preferred by transgender and nonbinary individuals whose priorities are maintaining erogenous sensation over neophallus size, and avoiding additional scarring from distant donor sites.[ 3 ] This procedure is covered by MSP. Complications include urethral strictures and fistula, superficial wound infection or hematoma, breakdown of the vaginectomy closure, and persistent vaginal tissue.[ 9 ] Surgeons at the Gender Surgery Program BC who offer this procedure follow the WPATH guidelines for patient inclusion criteria [ Table ].
Phalloplasty
Phalloplasty is a lengthy, multiphase surgery performed to construct a neophallus. This procedure is the most complete genitoperineal transformation for transmasculine individuals, since it most closely approximates the appearance, size, and function of a cisgender phallus. It employs one of two techniques to create the neophallus from the patient’s skin: pedicled flaps (from regional areas, typically the anterolateral thigh, groin, or abdomen) or free flaps (tissue from a remote location, such as the forearm).[ 3 ] Many of these donor sites can contain nerves that can be coapted to the clitoral nerve in order to maintain sensation. The gold standard for phallic reconstruction uses the radial forearm free flap.[ 3 ] Permanent hair removal of the tissue used to reconstruct the penile urethra is required to avoid urinary blockage, stone formation, and urinary tract infection. Donor site hair removal for the urethra is covered by MSP. Similar to metoidioplasty, the testosterone-enlarged clitoris is released, and the labia majora are used to create the scrotum. If desired, testicular implants and semi-rigid or inflatable erectile implants may be inserted during follow-up procedures. Phalloplasty is often completed in transgender and gender-diverse individuals who prioritize a cisgender-appearing neophallus, the ability to urinate while standing, and the capacity for penetrative intercourse.[ 5 ] Potential drawbacks of this procedure include the visible forearm scar at the donor site, the multistage nature of the procedure, the prolonged operative time, and the high complication rates. This procedure is covered by MSP. Phalloplasty has a total complication rate of up to 80%, which comprises mostly urethral issues. Common complications include urinary stricture, stenoses and fistula, partial/total flap (neophallus) necrosis, and donor-site morbidities.[ 10 , 11 ] Surgeons at the Gender Surgery Program BC who offer this procedure follow the WPATH guidelines for patient inclusion criteria [ Table ].
Facial and neck procedures
Facial feminization.
Facial feminization procedures usually focus on altering prominent facial angles of the cheeks (enhancing the malar region), forehead (smoothing of supraorbital bossing), nose (adjusting the glabellar angle), and jaw (reducing the gonial angle), and making adjustments to the hairline and areas surrounding the eyes, ears, and lips.[ 3 ] WPATH does not specify eligibility criteria for facial feminization surgery, and the procedures are not currently covered by MSP.
Thyroid chondroplasty (tracheal shave)
Thyroid chondroplasty involves reducing or reshaping the laryngeal prominence of the thyroid cartilage. The procedure is done under general anesthetic, or local anesthetic with sedation through an incision across a naturally occurring neck skin crease.[ 3 ] WPATH does not specify eligibility criteria for tracheal shaving, and the procedure is not currently covered by MSP.
Voice surgery
Voice surgery is used to raise vocal pitch because feminizing hormone intervention does not affect the adult voice (unlike testosterone, which deepens vocal pitch). The stigma associated with transitioning patients who have a deep voice can cause extreme distress. Various surgical techniques can be employed to raise the vocal pitch, including shortening the vocal cords, increasing the tension across vocal cords, or reducing vibrating vocal cords, in addition to vocal therapy.[ 3 ] Currently, these procedures are not covered by MSP, and only a limited number of surgeons in Canada offer voice surgery. WPATH states that for maximum benefit, the patient should consult with a voice and communication specialist preoperatively and postoperatively.[ 1 ]
Other procedures
Hysterectomy and bilateral salpingo-oophorectomy.
Hysterectomy (removal of the uterus) can be completed independently or with oophorectomy (removal of the ovaries) and salpingectomy (removal of a fallopian tube). Complete hysterectomy (removal of the uterus and cervix) is required if the individual is considering future metoidioplasty or phalloplasty. Oophorectomy and salpingectomy can be completed prior to further lower body gender-affirming surgery but are not required. If the individual is considering future fertility, egg harvesting may be considered prior to oophorectomy. Complications specific to this surgery include damage to surrounding tissues, including ureters, bladder, small bowel, rectum, and blood vessels.[ 5 ] For patients who are seeking either a metoidioplasty or phalloplasty, it is recommended that a hysterectomy be completed 4 to 6 months prior to other lower body gender-affirming surgery to reduce the complications of the vaginectomy component of the procedure. Hysterectomy with or without bilateral salpingo-oophorectomy is covered by MSP. Surgeons are encouraged to follow the WPATH guidelines for patient inclusion criteria [ Table ].
Although the evidence-based guidelines for the WPATH Standards of Care should be met, clinical departures can arise based on a patient’s unique anatomical, social, or psychological situation. Individualized surgical consultation can provide educational information that helps guide patients in their decision-making and surgical planning process. Experienced health professionals should take an individualized approach to patient care in order to prioritize specific harm-reduction strategies and maximize surgical outcomes.[ 1 ]
Competing interests
None declared.
This article has been peer reviewed.
1. Coleman E, Bockting W, Botzer M, et al. Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7. Int J Transgend 2012;13:165-232.
2. Trans Care BC. Gender-affirming surgeries. Provincial Health Services Authority. 2019. Accessed 1 September 2021. www.phsa.ca/transcarebc/surgery/gen-affirming .
3. Schechter LS. Surgical management of the transgender patient. Philadelphia: Elsevier; 2016. p. 35-230.
4. Trans Care BC. Gender-affirming care for trans, Two-Spirit, and gender diverse patients in BC: A primary care toolkit. Provincial Health Services Authority. 2021. Accessed 1 September 2021. www.phsa.ca/transcarebc/Documents/HealthProf/Primary-Care-Toolkit.pdf .
5. Rainbow Health Ontario. Transition-related surgeries summary sheets. Sherbourne Health Centre. 2017. Accessed 1 September 2021. www.rainbowhealthontario.ca/resource-library/trs-surgical-summary-sheets .
6. Lawrence AA. Patient-reported complications and functional outcomes of male-to-female sex reassignment surgery. Arch Sex Behav 2006;35:717-727.
7. Health Canada. Summary safety review—breast implants. 27 May 2019 [updated 29 May 2019]. Accessed 1 September 2021. http://hpr-rps.hres.ca/reg-content/summary-safety-review-detail.php?lang=en&linkID=SSR00223 .
8. Monstrey S, Selvaggi G, Ceulemans P, et al. Chest-wall contouring surgery in female-to-male transsexuals: A new algorithm. Plast Reconstr Surg 2008;121:849-859.
9. Dy GW, Granieri MA, Fu BC, et al. Presenting complications to a reconstructive urologist after masculinizing genital reconstructive surgery. Urology 2019;132:202-206.
10. Morrison SD, Chen ML, Crane CN. An overview of female-to-male gender-confirming surgery. Nat Rev Urol 2017;14:486-500.
11. Morrison SD, Shakir A, Vyas KS, et al. Phalloplasty: A review of techniques and outcomes. Plast Reconstr Surg 2016;138:594-615.
Mx Kumar is a medical student at the University of British Columbia. Mx Bertin is a clinical research coordinator for the Gender Surgery Program BC. Mx Croy is a registered nurse working at the Gender Surgery Program BC. Dr Genoway is a clinical instructor in the Department of Surgery, University of British Columbia, and an active medical staff with Vancouver Coastal Health. Dr Kavanagh is a clinical assistant professor in the Department of Urologic Sciences, University of British Columbia, and an active medical staff with Vancouver Coastal Health.
- Submit a Letter
- CREATE CITATION
Sahil Kumar, MSc, Elise Bertin, BSc, Ray Croy, BSN, RN, Krista Genoway, MD, FRCSC, Alex Kavanagh, MD, FRCSC. Gender-affirming surgical care in British Columbia. BCMJ, Vol. 64, No. 1, January, February, 2022, Page(s) 26-29 - Clinical Articles .
Above is the information needed to cite this article in your paper or presentation. The International Committee of Medical Journal Editors (ICMJE) recommends the following citation style, which is the now nearly universally accepted citation style for scientific papers: Halpern SD, Ubel PA, Caplan AL, Marion DW, Palmer AM, Schiding JK, et al. Solid-organ transplantation in HIV-infected patients. N Engl J Med. 2002;347:284-7.
About the ICMJE and citation styles
The ICMJE is small group of editors of general medical journals who first met informally in Vancouver, British Columbia, in 1978 to establish guidelines for the format of manuscripts submitted to their journals. The group became known as the Vancouver Group. Its requirements for manuscripts, including formats for bibliographic references developed by the U.S. National Library of Medicine (NLM), were first published in 1979. The Vancouver Group expanded and evolved into the International Committee of Medical Journal Editors (ICMJE), which meets annually. The ICMJE created the Recommendations for the Conduct, Reporting, Editing, and Publication of Scholarly Work in Medical Journals to help authors and editors create and distribute accurate, clear, easily accessible reports of biomedical studies.
An alternate version of ICMJE style is to additionally list the month an issue number, but since most journals use continuous pagination, the shorter form provides sufficient information to locate the reference. The NLM now lists all authors.
BCMJ standard citation style is a slight modification of the ICMJE/NLM style, as follows:
- Only the first three authors are listed, followed by "et al."
- There is no period after the journal name.
- Page numbers are not abbreviated.
For more information on the ICMJE Recommendations for the Conduct, Reporting, Editing, and Publication of Scholarly Work in Medical Journals, visit www.icmje.org
BCMJ Guidelines for Authors
Leave a reply, more stories.
Informed consent for gender-questioning youth seeking gender-affirmative care is a complex issue
- Skip to main content
- Skip to main navigation
- Skip to site search
- Skip to side bar
- Skip to footer
BC Gov News
- News Archive
- Live Webcast
- Office of the Premier
- Agriculture and Food
- Attorney General
- Children and Family Development
- Citizens' Services
- Education and Child Care
- Emergency Management and Climate Readiness
- Energy, Mines and Low Carbon Innovation
- Environment and Climate Change Strategy
- Indigenous Relations and Reconciliation
- Intergovernmental Relations Secretariat
- Jobs, Economic Development and Innovation
- Mental Health and Addictions
- Municipal Affairs
- Post-Secondary Education and Future Skills
- Public Safety and Solicitor General
- Social Development and Poverty Reduction
- Tourism, Arts, Culture and Sport
- Transportation and Infrastructure
- Water, Land and Resource Stewardship
B.C.’s first detox services for Indigenous youth coming to Island

B.C. acts to protect kids, school staff from disruptive protests
More from the premier.
- Factsheets & Opinion Editorials
- Search News
- Premier's Bio
Province strengthens drought preparedness

B.C. vineyards, orchards receive help to replant for changing climate
More from this ministry.
- Minister's Bio
New legislation aims to remove systemic barriers for Indigenous, racialized people

Expanded eligibility, new supports available for current, former youth in care

New position expedites progress on Indigenous child welfare
Governments of canada and british columbia working together to bring high-speed internet to more than 7,500 households.

Michael McEvoy to serve as interim information and privacy commissioner
Safer, larger victoria high opens.

B.C. takes action with new wildfire training and education centre, first of its kind in North America

Upgrades to wastewater infrastructure coming to Comox Valley
Bc hydro issues call for new clean electricity to power b.c.’s future.

New legislation ensures B.C. benefits from clean, affordable electricity
Park additions boost outdoor recreation, strengthen ecosystem protection, reducing emissions for a cleaner future for british columbians, budget 2024: taking action for people, families in b.c..

Climate action tax credit helps people with everyday costs
Wildfire-damaged wood recovery underway in b.c., launch of spring covid-19 vaccine boosters marks end of respiratory illness season, province takes more actions to strengthen primary care for people, b.c. builders can now use mass timber in taller buildings.

SAFER improved, top-up benefit coming for people on rental assistance
New legislation will eliminate discriminatory barriers for first nations.

Engagement results released on proposed legislative amendments to First Nations land ownership
Throne speech lays out vision of a stronger b.c. that works better for people.

Province honours people providing extraordinary community service
Research support helps fight metabolism diseases.

Minister’s statement on March Labour Force Survey results
Minimum wage increases to $17.40 an hour on june 1.

Minister’s and parliamentary secretary’s statement on Construction and Skilled Trades Month
Minister’s statement on lives lost to poisoned drugs in february, expanding multi-language support, services for newcomers, construction underway on cowichan sportsplex field house, new legislation recognizes work of first nations post-secondary institutes.

TradeUpBC builds, enhances tradespeoples’ skills
New digital platform improves response, safety for people in crisis in port moody.

New legislation paves the way for police reform
Budget 2024 supports improvements to treatment, recovery services.

Changes aim to help people out of poverty
Engagement launched for canadians of south asian heritages museum.

Historic water bomber destined for wildfire aviation exhibit
Province, yvr work together to support good jobs, fight pollution.

Airport improvements support services, growth for communities
Province supports new weir to keep cowichan river flowing.

Province strengthens flood defences, protecting people, communities
B.c. brings gender-affirming surgery for trans people closer to home.

Honourable Adrian Dix
Minister of Health and Minister responsible for Francophone Affairs
Email: [email protected]
News Release
Media contacts, ministry of health, vincent chou, matt kieltyka.
- Visit Ministry Website
Featured Topics
- Coronavirus (COVID-19)
- Health & Drug Coverage
- Accessing Health Care
- Health Forms
- Office of the Provincial Health Officer
- Office of Indigenous Health
Featured Services
- Medical Services Plan
- HealthLink BC
- Vital Statistics
- Health Care Complaints

Transgender people in British Columbia will soon have access to publicly funded gender-affirming lower surgeries within the province, as British Columbia becomes the first province in western Canada to offer these procedures next year.
“The trans community has advocated over a number of years for improved access to care, including access to complex lower surgeries within B.C.,” said Adrian Dix, Minister of Health. “For those seeking lower surgery, people were required to travel to Montreal or to the U.S., resulting in additional medical risks associated with travelling long distance after surgery and in receiving followup care if there were complications.”
Reconstructive gender-affirming surgeries will be available within Vancouver Coastal Health starting in 2019. In addition, trans people throughout the province now have improved access to publicly funded gender-affirming chest and breast surgeries. A total of 14 surgeons will provide these surgeries in Burnaby, Kamloops, Kelowna, Port Moody, Prince George, Vancouver and Victoria.
Previously, to receive publicly funded gender-affirming breast augmentation or chest construction procedures, people had to travel to Vancouver or Victoria. For those seeking lower surgery, people were required to travel to Montreal or out of the country.
“We are proud to be the first province in western Canada to provide these surgeries,” said Dix. “While B.C. funded these surgeries, they weren’t being delivered close to home and support systems, and that is what we are changing now. This is about bringing care closer to home and offering an enhanced, more efficient, cost-effective solution.”
The number of people travelling out of the province for lower surgeries has been steadily increasing each year with approximately 100 people going outside of B.C. annually for care. Over 200 chest and breast surgeries are expected to take place throughout B.C. in the coming year.
This expanded access to gender-affirming surgery is part of the Province’s new B.C. Surgical and Diagnostic Imaging Strategy, which is supported with ongoing targeted funding of $75 million from the Ministry of Health in 2018-19, and increasing to $100 million in 2019-20.
Lorraine Grieves, director, Trans Care BC –
“With increased access to physicians, surgeons and other medical experts who are knowledgeable about health care for trans people, we have seen an increase in demand for gender-affirming surgeries. When we were planning the Trans Care BC program, we heard from trans communities that training more surgeons and establishing a surgical program for lower surgeries in B.C. was crucial to improving access to this care. It’s very rewarding to know that after years of planning and collaboration, people will soon be able to receive gender-affirming surgeries closer to their home communities and support systems.”
Gwen Haworth, trans educator –
“Having personally travelled out of province to access similar care, this is a significant step forward in improving the patient journey for British Columbians requiring these procedures. Offering services closer to home reduces additional stress, uncertainties and expenses for individuals and their families. It’s reassuring to know that we will have improved access to experienced care providers throughout the entire process, within our home province.”
Quick Facts:
- Around 1% of the population identifies as trans, an umbrella term that describes a wide range of people whose gender differs from their assigned sex at birth. In B.C., an estimated 46,000 people identify as trans or gender diverse. Only a few of these people will access medical or surgical services to support their gender affirmation.
- Between 2014 and 2018, the number of gender-affirming chest and breast surgeries performed annually has more than tripled, from 56 to 178.
- Between 2014 and 2018, the number of annual referrals for chest and breast surgeries has doubled, from 179 to 376.
- Effective Nov. 1, 2018, people who do not identify as male or female have the choice to display an X as a third option in the gender field of their driver’s licence, identity card, birth certificate and BC Services Card.
Learn More:
To learn more about Trans Care BC, visit: www.phsa.ca/transcarebc
Related Articles
Premier’s, minister’s, provincial health officer’s statements on the eighth anniversary of toxic-drug public-health emergency.

Connect with the Ministry
View the Ministry's latest photos on Flickr.
Watch the Ministry's latest videos on YouTube.
Acknowledgment
The B.C. Public Service acknowledges the territories of First Nations around B.C. and is grateful to carry out our work on these lands. We acknowledge the rights, interests, priorities, and concerns of all Indigenous Peoples - First Nations, Métis, and Inuit - respecting and acknowledging their distinct cultures, histories, rights, laws, and governments.
Connect with Us:
- Newsletters
- Accessibility
- Today »

- City & Culture
- Food & Drink
- Film & TV
- Best Of Vancouver
- Sex & Romance
Did I make a mistake? A transgender woman's journey of transition
Vancouver’s Carolynn Dimmer shares the questions she faced before—and after—gender reassignment surgery
Did I make a mistake? Am I doing the right thing? Is this the path for me? These are questions we usually ask and, if not, should be asking ourselves. Gender transition is not for the faint of heart. Early in my transition from male to female, I gave little thought to those questions. I was very busy buying new clothes, coming out to family and friends, and getting ready to return to work after a lengthy absence.
I was working on name changes, birth records. I was preoccupied early in my transition. There was a lot of ground to cover if I was to come out and be my true self. Endless doctors’ appointments. Sometimes I felt as though I should have had a tube from my arm connected directly to the blood lab. I had more blood drawn from me in my first year of transition than I had in my entire life, and I was under the microscope of psychiatrists, every move scrutinized. Should I sit in the blue chair in the doctor’s office? Should I sit in the pink chair? I felt like I was under constant surveillance, and worried my male side would pop out. It didn’t. I did a very good job at covering the male side of who I was. After a few years of this—the real life test—I received a letter saying that I was eligible for and had met all the criteria to move forward and have gender reassignment surgery. To say I was happy would have been a gross understatement. There it was in my hot little hands, the brass ring! The letter I had been working toward for the last four years.
For a brief moment, I hesitated to pick up the phone to book my surgery date. I read and re-read the letter countless times. Then it went into my file, and I didn’t look at it again for at least three months. Those three or so months were when the questioning began. I tried approaching people in my support system. Each of their answers was almost scripted: “Well, if you have any doubts then you’re not really trans!” I thought to myself that “You’re not really trans” was an odd thing to say. My question was still not being addressed. I had a new brass ring to reach for. “Is there anyone who has any doubts or second thoughts?”
One would think this would be a very easy question to have answered. It was my experience that it was the hardest question that I ever asked to find an answer for. It would appear that by the time I reached that stage in my transition, the medical community felt I was ready to move onto the next stage—surgery. I was supposed to be ready to take the final plunge into the mystery of becoming a woman. Hard as I looked for one person to say, “Yes, I had doubts; yes, I was terrified; and yes, I questioned if I made a mistake,” I never found them. That one person never appeared.
I knew they were out there. They didn’t speak. Now I had a new question. Why weren’t they coming forth with their experience? Shortly after I pulled the letter from my file again, I made the call to the surgeon and booked my flight. I was very excited to be on my way to have this correction taken care of, but that one question still haunted me. What haunted me even more was where were the ones that had gone before me, that were supposed to help guide me through this rocky period. It wasn’t long after I had returned home from the surgery that I found the answers I was looking for. I found where most brothers and sisters had gone; I found the answers to those nagging questions. The real work began upon my return home. The rigid schedule of dilating, the inability to get to the bathroom without assistance, the blood, the pain. I’ll never forget the pain. My hips and halfway up my stomach were yellow and black from the bruising. The simplest act of trying to watch television became agony. The deed had been done; there really was no turning back. I couldn’t go home now .
I was now in this surgically created wonderland that I called my female body, laying awake at night still asking, “Did I make the right choice?” Right choice or not, this was where I was! Life carried on seemingly uneventfully, get-well cards came, flowers arrived, people phoned. It was almost like I had celebrity status, but that was short-lived. Then again I was alone with my thoughts. That one nagging question rang through my head. Did I make a mistake? I felt a bit depressed so I made a couple of phone calls trying to find a counsellor to speak with. Oddly no-one would accept me. I called my old shrink and he said, “Our work was finished. I was only there to help you until you had surgery. You’ll need to find another doctor.” The hunt began for another psychiatrist. I thought it would be easy, but it was not. Depression by this time had taken deep root; eventually I was diagnosed with chronic depression. What followed was not at all what I had expected. I stopped going outside, I quit playing softball, I closed my kickboxing gym. I became a recluse, subjugated in my own home by no one other than myself. My depression deepened. My rigid schedule of postsurgical care went out the window. Then another nail struck into my coffin of depression! My surgical area had grown shut!
I had less than two inches of depth. I was horrified. What had become of that soulful, full-of-life woman that I had known at the beginning of my transition? Where did she go? How could I get her back? The question of whether or not I had made a mistake was secondary at this stage; my priority now was to find the real Carolynn again. This was a daunting task to say the least. I was lucky enough to have been referred to a doctor by a dear friend of mine. He saw me, and I would love to say that we got off to a great start. We didn’t. He called me obese and said I needed to exercise. I didn’t see him again for at least a year. When I finally did return to see him, I was a complete train wreck. I had put on 40 to 50 pounds, and I was depressed. I still had the problem of the surgical area having grown closed. After some time with this doctor, things started to look a little better. Over the next few years things began to change. I felt my old self returning, I re-opened my kickboxing school, and started to socialize again. Then my doctor threw this at me one day in a session. He said, “Carolynn, you know you can go for a surgery revision and get that fixed.” My jaw hit the floor. I was in shock. I thought it was a one-time shot, and if, like me, you screwed it up—well, you were screwed forever after.
I felt this little fire of hope begin to burn in me again. I had purpose in my life again. This time, I wasn’t going to screw it up! I jumped through all the hoops, made all the phone calls, and reattached the tube from my arm to the blood lab. Honestly, I felt happiness shine again in my life. Finally, the day came for me to head off and have my surgery revision. I remember arriving at the recovery house and seeing another group of me’s from six or seven years ago. They were all driven. They were all happy and they all had no clue what was going to happen after.
Not from a place of ego, but rather a place of a caring sister, I took it upon myself to inform the other guests that this was not my first time. I had to go around and return their jaws to the closed position. I became very close with two of the girls there. One very young woman was maybe 17 and there with her mother, and another was my own age and all the way from the U.K. They listened intently as I told them my story and the pitfalls to be aware of. My young friend even went so far as to take notes. Our surgery days came and went. We all returned to the places we respectfully called home. A few days later, I got a phone call from my friend in the U.K. She was in tears and panicking, saying, “I don’t know what I have done.” We talked for what seemed like hours until she said she was feeling better. It’s been some time since I have heard from her. As for my young teenage friend, I got a call from her mother on several different occasions telling me what her daughter was not doing, and how she was feeling depressed. Considering myself somewhat of a hip person, I started to text my young friend. We worked out some things via texting and email. My life continued fairly normally. I was again into my routine of dilating and postsurgical care. Only this time I had a new-found appreciation for what I had been given, and the question had finally been answered.
Did I make a mistake? The answer is No! I did not make a mistake. Do I have regrets? Yes, of course, I have regrets. I do not feel I would be classified as human if I didn’t. Do I miss my old self? Sometimes. The question of whether or not I made a mistake at this stage is irrelevant. The more pressing and more important question is, am I able to be happy living as I am? At time of writing, I have an afternoon appointment coming up with a personal trainer at the gym. Later this evening, I’m going out for dinner with some friends and there is this very handsome man I met who asked me on a date.
The answer is, yes, I am happy and can live this way. The question I had chased and tried to have answered was the wrong question. After a few years of wrestling with it, the question “Did I make a mistake?” became irrelevant. The question I should have been asking myself all along is, “Can I be happy after I have made these final choices?” People have surgery everyday. Most don’t ask themselves, “Did I make a mistake?” If my own personal experience is of any use to anyone, then ask yourself the right questions first. Don’t ask “Did I make a mistake?” or “Am I doing the right thing?” Ask yourself, “Can I live happily once these decisions have been made?” That question is far easier to answer than the others.

33 Comments
Biblebeltatheist.
Feb 25, 2013 at 12:35pm
Thank you for sharing this deeply personal story. I wish more trans persons would share their experiences - good and bad. It would be much easier to understand what you folks go through if more would speak up about their real-life experiences instead of telling the world to "go educate yourself".
Vespa chick
Feb 25, 2013 at 1:15pm
Sharing your story is such a personal gift for those in or out of the LGBTQ community, the gift is "self-exploration" ... I as a peer support worker hold such value to personal stories whether they relate to my own experience in Mental Health or not ... relating those experience are the riches in life ! ... Thank you
Feb 25, 2013 at 2:04pm
Thank you so much for telling your story. I am a trans man who is experiencing much the same and have not started my medical transition because of it so thank you for speaking up and out.
Katrina Payne
Feb 25, 2013 at 2:56pm
You sound like the sort of person that had issues with members of the transgender community that generally drive me 100% completely nuts.
This is why I generally do not bother talking with most transgenders (which might have been why I wasn't there to answer).
There is the all too common attitude that having enough surgery to look like a Barbie Doll will cure all their problems in life. Most "transgender" discussions are more around what parts to chop off, rather than, "hey, women have stuff to deal with that most men do not", and stuff that generally seems at home in feminism groups. If you are switching your gender station (in your case, lowering your station) there is stupid social situations to deal with.
Yet in the group it is all, "bigger boobs will solve all my problems", "remove my man jaw" (never mind a lot of cisgender women live fine with so called man jaws) and a bunch of other bullshit that got you into your current place.
It really doesn't help that me and Summer really never seem able to see eye to eye on anything. So I go off and do what I usually do: get most of my help from cisgendered women I know.
Which is why I get people thinking I am not really transgender, I just say I am for attention... or that I am post op, or a bunch of other statements about my general level of passing.
On a related note: I am trying to think of a valid reason to get the surgery. Something that is not hateful to women (a woman is only her vagina, nothing else), something that doesn't seem frivolous(because I totally can) and something that doesn't seem spiteful (will I still have people liking me without my trap parts?).
Feb 25, 2013 at 4:38pm
Thank you. I am the mother of an almost eight year old girl who will have the same choices to make sometime down the road. I'm going to save this article for her. Thank you.
Feb 25, 2013 at 5:30pm
thanks for being brave and telling your story. who would not take the time to think carefully about the sanity of such a major decision?
Deanna Paladina
Feb 25, 2013 at 6:49pm
Thank you for your story. I'm glad you had your revision, and I'm glad you've come to terms, and found your true self after your 'trials', if I may use that word.
Also, thank you for helping others, in so many ways. You are an exceptional person, and an excellent role model.
Thanks you again, and be blessed. :-)
Feb 25, 2013 at 6:59pm
I have met several people who were not ready to have surgery when they had it. Some of these people had their surgeries scheduled based on when their health care system would pay for it - NOT when they were ready to have it. If you have ANY doubts at all about ANYTHING then you are NOT ready to have surgery!!
I had surgery over two years ago when I was 50-years old. I simply could not get on that operating table fast enough! I had very little pain after surgery and have had no problems. My surgery day will always be the GREATEST day of my life and I cherish every second of the time I spent in Montreal! Today everything functions perfectly and I am a normal, legal woman -- and I couldn't be happier!!!
My point is that while there ARE a few people who may have "jumped the gun" and had surgery before they were ready to do so, the vast majority of people who have surgery are very happy and have NO regrets at all. I know MANY people who have had surgery and have never met a single person who regretted they did. I can honestly tell you that GRS saved my life!
Maggie Cochrane
Feb 25, 2013 at 8:25pm
As one of my closest friends I am honored, proud and humbled by your journey. Your honesty, humor and "ginger ways" ;-) have helped in a very big way to erase my judgements and replace them with respect and love... Thank you beautiful!!!!
Feb 25, 2013 at 9:22pm
i am in the middle of transitioning it has been a long journey for me 40 years. now i know where my Journey is going i had questions i am glad i asked them . my friends and partner never left my side my family have been good . My work place has also stuck by me, i have met some real friends in the transgender community, so in my case i have gained friends and not lost any. i am so happy i have made the right choice in my life for once .if there is any Questions people want to ask because they are not sure where they are at i am always available. this is just a little of my story
POPULAR ON STRAIGHT.COM
Sex work is a community like any other, corduroy pie co’s graham marceau is opening a new restaurant in surrey, legendary punk drummer jon card has died, with those left behind praising his talent and humanity, once-vegetarian eatery heirloom officially shutters, blames closure on “deborah”, province forces narrow lounge to shut for a week, raising questions that have long remained unanswered, katie pruitt doesn’t need anyone to pray for them, pne 2024 summer nights concerts includes brad paisley and charlotte cardin, lee’s donuts is opening in steveston village, vancouver vaisakhi festival returns this weekend, what’s in your fridge: legacy, the producer, more on straight.com, confessions, 30 year amortizations aka sign life away..
Okay, so the government prints a ton of money, things shoot up way above any real affordability...
Happy Day Cafe on Kingsway
You were sitting by yourself & you ordered a few Curry Fish Balls and a few deep-fried Spring...
- ONLINE/VIRTUAL
- CLASSIFIEDS
- BEST OF VANCOUVER
- GOLDEN PLATES
FEATURED GUIDES
Georgia straight guide to the 34th annual dancing on the edge festival, indigenous stories, education: upgrade your skills for a dramatically new world.
Find a Surgeon
Search by U.S. State, Procedure and Insurance Search by Country and Procedure Browse the Global Surgeon Maps
Home » Surgeon News
Canada Finally Has Nation-Wide Funding For Gender-Affirming Surgeries

With last week’s announcement from the Government of Nunavut confirming that the territory will pay for mental health services and transition treatments for transgender and non-binary residents, Canada will now have nation-wide funding available for gender-affirming surgeries. Nunavut’s Health Department is partnering with GrS Montréal to provide the surgeries.
Health care in Canada is delivered by the provinces and territories and funding for gender-affirming surgeries varies depending on where a person lives. This patchwork of coverage has resulted in barriers to accessing care that have disproportionately affected people living in Canada’s territories in the North, which includes Yukon, Northwest Territories and Nunavut. While expansion of surgery funding in Canadian provinces has continually progressed over the last decade, comprehensive coverage has only been established in the territories over the past three years.
Nation-wide coverage is obviously a very positive development but advocacy is still needed to continue the work of dismantling barriers for Canadians to access surgical care. Current challenges include:
Getting coverage across the country for Facial Feminization , Breast Augmentation and Male Chest Contouring , procedures that are excluded from funding policies in some jurisdictions.
Surgeons who practice gender-affirming genital surgery are only located in Montreal, Toronto and Vancouver. This means that many transgender and non-binary Canadians need to travel great distances to access surgeons for primary surgeries, follow-ups and specialized care for complications, incurring significant expenses that aren’t universally covered or subsidized.
Wait times are a problem that is not unique to gender-affirming surgical care in Canada but with few experts performing these surgeries patients can wait up to three years just for a consultation with a surgeon.
With the Government of Nunavut’s funding commitment, the goal of nation-wide coverage for gender-affirming surgery in Canada has been achieved. Improvements to provincial and territorial funding policies are still needed but this is a milestone to be celebrated.
Review Funding Policies by Province and Territory:
- British Columbia
- New Brunswick
- Newfoundland and Labrador
- Nova Scotia
- Ontario – PDF
- Prince Edward Island
- Saskatchewan – PDF
- Northwest Territories – PDF
- Nunavut – News article: GN transgender, non-binary health services a positive step
- Yukon – News article: Yukon’s new gender-affirming care policy is most comprehensive in Canada
- CSPS Executive
- Why Choose a Plastic Surgeon?
- Testimonials
- Locate a Surgeon
- Choosing a Plastic Surgeon
- Birth Conditions
- Breast Reconstruction
- Breast Reduction
- Burn Reconstruction
- Hand Surgery
- Skin Cancer
- Body & Wound
- Blepharoplasty (Eyelid Lift)
- Body Contouring
- Breast Augmentation
- Breast Lift
- Liposuction
- Rhinoplasty (Nose Job)
- Soft Tissue Fillers
- Skin Resurfacing
- Laser Hair and Tattoo Removal
- Moles, Cysts and Skin Blemishes
- Apply to be a Member
- Registration
- Scientific Program
- Scientific Award Winners
- Call for Abstracts
- Abstract Reviewer Login
- Code of Ethics
- Training Programs
- Young Surgeons
- Fellowships
- International Meetings
- Canadian Wait Times Alliance
- Plastic Surgery Education Network
- Lifetime Achievement Award
- Clinical or Outcomes Research Grant
- Philanthropic donations
- Global Surgery Map
- Global Surgery Map Submissions
Gender-Affirming Surgery
- Members only
- Past Scientific Programs
- Practice Opportunities
- Women Plastic Surgeons of Canada
- President’s Medal
- Board of Directors
- Visiting Professor Funding
- Humanitarian Missions
Plastic surgeons provide gender-affirming surgeries for the treatment of gender dysphoria with the aim of helping a person physically actualize their internal sense of self. The goals of these procedures are therefore patient specific and can vary beyond the gender binary.
Gender-affirming surgeries can be grouped into four main domains: facial, chest, body and genital procedures. Talking to your plastic surgeon about your individual transition will help direct which surgery options are best for you. Below are some commonly performed procedures, however, all patients should discuss both variations and the spectrum of options with their surgeon individually to make sure their chosen procedures match their individual needs and goals.
Please click here ( https://www.wpath.org/publications/soc ) for information from the World Professional Association of Transgender Health (WPATH) on information on preparing for Gender-affirming surgery.
Facial Gender-Affirming Surgery
Facial procedures can either masculinize or feminize the appearance of the face.
To enhance a feminine appearance, both bony anatomy and soft tissue augmentation can be done. Hairline lowering, forehead shortening and forehead contouring are typically done in a combination to achieve an overall feminine appearance of the upper face. Alterations to the middle face include rhinoplasty and upper lip lifts. Fat grafting can also be used to create fuller and softer cheeks. For the lower face, the jawline can be softened and reduced with mandible contouring. Finally, the thyroid cartilage can be reduced to feminize the appearance of the “Adam’s apple” and voice procedures can be used to increased vocal pitch.
Due to the effects of gender-affirming hormones therapy (testosterone) on the skin and facial hair growth, facial masculinization surgery is much less common. Some examples of surgical procedures include facial implants for augmentation of the jawline or chin.
Gender-Affirming Chest Surgery
Gender-affirming mastectomy is the most commonly performed gender-affirming surgical procedure, often referred to as “top surgery”. The most frequently performed technique is the “double incision with free nipple graft” where the breast tissue and excess skin is removed in addition to removing, re-sizing, re-shaping and replacing the nipples as free grafts. Some patients choose not to keep their nipples. Alternative techniques exist when minimal skin removal is needed. Additionally, chest reduction surgery is an option for patients who wish to keep some of their breast tissue.
Breast augmentation is available for patients who aim to increase their breast size. A minimum of 12 months of gender-affirming hormone therapy with estrogen should take place prior to considering or evaluating an individual for breast augmentation. Usually, silicone implants are used. Your surgeon will discuss variation in scar placement techniques.
Genital Gender-Affirming Surgery
For individuals assigned male at birth, options for orchiectomy (testicle removal) in isolation or in combination with vulvar procedures can be done for gender affirmation. Vulvar procedures include either a vulvoplasty or a vaginoplasty. Vulvoplasty refers to creation of an external vulva without a vaginal canal while vaginoplasty similarly creates the external genitalia in addition to a vaginal canal capable of receptive penetrative intercourse. The preoperative preparation for these surgeries varies and may influence your choice of treatment. Vaginoplasty typically requires extensive pre-operative hair removal and a post-operative dilation regimen.
Genital gender-affirming surgery for individual’s with assigned female at birth anatomy falls into two main categories: metoidioplasty and phalloplasty. In both categories the main differentiating factor between the various surgical options is the desire to stand to urinate. While metoidioplasty is done using only pre-existing genital tissue, phalloplasty requires tissue to be transferred from somewhere else on the body to construct the penis. Phalloplasty surgery is often done over multiple stages meaning more than one surgery is required to obtain a functioning phallus capable of standing urination. Many variations of phalloplasty exist. The traditional phalloplasty includes urethral lengthening with the goal of standing urination. Other variations of phalloplasty, referred to as “shaft-only” phalloplasty are increasingly performed. Shaft-only phalloplasty refers to the creation of a phallus without lengthening the uretha. Options in addition to a shaft only phalloplasty include vaginectomy, perineal urostomy, clitoral burial and scrotoplasty, depending on patient goals and individual preference.
Gender-Affirming Body Contouring
Gender-affirming body contouring includes liposuction or fat grating to change the distribution of adipose tissue in the body. Liposuction is done to help narrow the hips and alter the shape of the body. Conversely fat grafting can help augment the buttock and hips to accentuate curves.
Breast Reconstruction Awareness Day - BRA-Day
BRA Day is an initiative designed to promote education, awareness and access for women who may wish to consider post-mastectomy breast reconstruction.
Only physicians who are certified in Plastic Surgery are Plastic Surgeons. There is no foolproof way to choose a Plastic Surgeon or to guarantee your results. However, there are a few basics, which can help you to decide.
Medical Professionals
The Canadian Society of Plastic Surgeons comprises nearly 500 Plastic Surgeons and is focused on sharing knowledge and expertise, improving quality of care, and advancing the practice of plastic surgery in Canada.
- 2021 CSPS Conference Archives
- Global Outreach
- History of the CSPS
- Reconstructive Procedures
- Aesthetic Procedures
- President’s Medal
- Membership Application
- Pay Member Dues
- Annual Meeting
- Information for Plastic Surgeons
- Continuing Professional Development
- Dr. Kimit Rai Family Scholarship
- Privacy Policy
Mailing Address
Street address.
- Contactez-nous
- Politique de confidentialité
B.C. teenager free to move forward with gender-affirming surgery after mother's lawsuit tossed
Court finds disapproving mother 'misled' the court, notes law on issue is already settled in b.c..
Social Sharing
A teenager in B.C. is free to move forward with his gender-affirming chest reconstruction surgery after a Supreme Court justice tossed his mother's attempt to stop the procedure, finding she made "egregious misstatements" while fighting an issue that's already been settled in court.
Lawyers for the teenager, who turns 18 this spring, said he was "relieved" to hear the justice had ruled in his favour.
"Our client is hopeful he can get on with his life ... and get back to being a teenager," read an emailed statement from lawyers Adrienne Smith and Claire Hunter on Monday.
"Our client wishes to keep the details of his private life private, however he wanted to give this comment today so that other trans youth might not be so anxious that an unsupportive parent could unduly interfere in their health-care choices."
The CBC is not identifying the teenager, identified in court documents as Y.Z., or his parents in order to protect the teenager's privacy.
Issue of consent already settled in B.C.
The teenager, who was assigned female at birth, was originally supposed to have his chest reconstruction surgery on Nov. 6. It was cancelled after his mother won an urgent, ex parte court order to stop the procedure with 24 hours to spare.
The mother sued the teenager's doctor and plastic surgeon, demanding they stop treating her child without her permission until the courts had a chance to rule on the issue of consent. Y.Z. applied to have the lawsuit thrown out on Nov. 16, arguing it was an abuse of process.
The mother's ex parte order — a court order granted quickly without giving notice to the respondents — was supposed to buy the court time to argue the issue of a young person's ability to consent to their own health care.
- 'You are beautiful': How this transgender teen found the courage to transition
- Transgender teen on why 'deadnaming' Elliot Page is harmful
What the mother failed to tell the court, according to Monday's judgment, was that that debate was conclusively settled in B.C.'s highest court last year — meaning the judge who granted the procedure-blocking order in November did so without realizing the key issue of consent had already been resolved.
"It was not properly explained to this court that a similar case has recently been decided," Justice Diane Cheryl MacDonald wrote in Monday's judgment.
"There is clearly a broader public debate regarding whether gender-affirming surgery is in the best interest of youth. In B.C., that debate has been resolved in favour of surgery."
Besides leaving out the legal precedent, MacDonald said, the mother also withheld important personal information from the court.
MacDonald said the mother presented the case as though she was Y.Z.'s sole guardian with "unconstrained guardianship rights." In fact, she shares joint custody with the teen's father, who was identified as W.X.
The mother did not mention W.X. at all in her application, or the fact that he supports their child's transition and believes he is "mature enough to make his own health-care decisions."
Court order from 2006
Critically, the court noted, a family court order issued in 2006, after the teenager's parents separated, said mother and father have to "follow the directions of the mutually agreed upon health-care provider" if there is ever a dispute about the child's health care.
Y.Z.'s doctors and social worker support his transition.
MacDonald said the mother made "egregious misstatements" in failing to mention those facts.
The mother responded to the omissions by saying she had filed her original application "on short notice" in "an emergency situation" with days left before the November surgery date.
Applications for urgent ex parte orders in B.C. courtrooms require "full and frank disclosure of all material facts." Failing to disclose all of those relevant facts was grounds for dismissal in the mother's case — even before considering the issue of precedent.
The case was dismissed as an abuse of process.
"Based on my above concerns, and the lack of legal and factual basis to support the orders sought, Y.Z. has satisfied his burden to strike the claim because it is certain to fail," read the judgment.
ABOUT THE AUTHOR
Senior Writer
Rhianna Schmunk is a senior writer for CBC News based in Vancouver. Over a decade in journalism, she has reported on subjects including criminal justice, civil litigation and climate change. You can send story tips to [email protected].
- Send confidential story tips with SecureDrop
- Follow Rhianna on X
Related Stories
- Top stories from British Columbia
- Patient hopes Canada will introduce regulations for psychotherapy with 'magic mushrooms'
- Dawson Creek mayor says it's 'disappointing' that city councillor travelled abroad
- Coroner's inquest called into death of 20-year-old Hudson Brooks, shot 9 times by police
What Surgeons Need to Know About Gender Confirmation Surgery When Providing Care for Transgender Individuals: A Review
Affiliations.
- 1 Division of Plastic Surgery, Department of General Surgery, Oregon Health & Science University, Portland.
- 2 Department of Psychiatry, University of British Columbia, Vancouver, British Columbia, Canada.
- 3 private practice, San Francisco, California.
- 4 Division of Endocrinology, Metabolism, and Lipids, Department of Medicine, Emory University School of Medicine and the Atlanta Veterans Affairs Medical Center, Atlanta, Georgia.
- 5 private practice, Evanston, Illinois.
- 6 Department of Family Medicine, Northshore University Healthsystem, Lincolnwood, Illinois.
- 7 Division of Endocrinology, Department of Medicine, Boston University School of Medicine, Boston, Massachusetts.
- 8 Department of Public Health, San Francisco, California.
- 9 Department of Plastic Surgery, University Hospital Gent, Gent, Belgium.
- 10 University Plastic Surgery, Morton Grove, Illinois.
- PMID: 28196182
- DOI: 10.1001/jamasurg.2016.5549
Importance: In 2014, the US Department of Health and Human Services decided that its 1981 exclusion of transsexual surgical treatments from Medicare coverage was based on outdated, incomplete, and biased science and did not reflect current evidence or standards of care, and the exclusion was therefore lifted. As a direct result of this decision, surgeons nationwide are seeing an increase in consultations for surgical therapy to help transgender and gender-nonconforming individuals. Although some clinicians may have the technical training for such surgical procedures, in many cases, they may not have a full understanding of the complex and comprehensive care required to provide optimal health care for transgender individuals.
Observations: Gender confirmation surgery is a developing field in the United States and other areas of the world. The World Professional Association for Transgender Health started a global education initiative intended to provide surgeons and other health care professionals with the necessary background knowledge to understand and treat this patient population. This article provides an overview of best practices as set forth in the seventh edition of the Standards of Care for the Health of Transsexual, Transgender, and Gender Nonconforming People by the World Professional Association for Transgender Health, including mental health, endocrinology, and surgery for trans women and trans men.
Conclusions and relevance: Experts in each aspect of transgender health have summarized the content of the global education initiative in this article. It provides valuable information to surgeons of all disciplines and other health care professionals to help guide the treatment and management of transgender individuals.
Publication types
- Sex Reassignment Surgery*
- Transsexualism / psychology
- Transsexualism / therapy*
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Anaesthesiol Intensive Ther
- v.53(4); 2021 Oct
- PMC10165989

Gender reassignment surgery – a narrative overview of anaesthetic considerations and implications
Priyanka mishra.
1 Department of Anaesthesia, All India Institute of Medical Sciences, Rishikesh, India
Amborish Nath
2 Department of Burns and Plastic Surgery, AIIMS Rishikesh, India
Ashutosh Kaushal
3 Department of Anaesthesia, AIIMS Bhopal, India
Rakesh Kain
4 Department of Burns and Plastic Surgery, VMMC Safdarjung Hospital, India
The twenty-first century, with its transforming ideology and rising acceptance, is witnessing an increased number of transgender people applying for gender reassignment surgery (GRS). The procedure of GRS is a lengthy and complex one involving the active collaboration of multiple disciplines including psychology, psychiatry, family medicine, plastic surgery, endocrinology, otolaryngology, urology, gynaecology, maxillofacial surgery, and anaesthesiology. The considerable paucity of literature regarding the management of patients presenting for GRS places health care providers at a disadvantage. It is imperative to cautiously regard the specific medical, emotional, social, and economic concerns regarding these patients. Health care providers need to be trained well to deal empathetically with such patients. The present literature about GRS deals mainly with the surgeon’s perspective, while the anaesthetist’s approach remains hazy. This is because GRS imposes the need for anaesthesiologists to search for better and more efficient modes of anaesthesia so as to improve prognosis and minimize the associated morbidity. Anaesthetists should understand the associated psychological aspects and effects of hormone therapy while performing an extensive and informative pre-operative evaluation to formulate an effective strategy. Providing the optimal modes for anaesthesia and keeping a cautious watch for complications along with timely intervention in the advent of the same comprise the approach for high-quality anaesthetic care. This review aims to provide a detailed overview of significant considerations and competent peri-operative outcomes in patients presenting for GRS.
The right to gender identity is one that amounts to contouring an individual’s personality. The present hour calls for an understanding of the meaning that the term transgender holds. It needs to be recognized that sex and gender although often used interchangeably are quite distinct. Sex refers to the physical characteristics (e.g. reproductive organs, chromosomes, hormones) employed to assign people to be female, male, or intersex. However, gender is more of a social construct, sprouting from cultural expectations that shape an individual’s external appearance and conduct [ 1 ]. Gender identity disorders have been frowned upon throughout their existence, making their treatment quite controversial. Gender dysphoria, earlier known as gender identity disorder, describes a heterogeneous group of individuals having the desire to possess secondary sexual characteristics of the opposite sex and possessing varying degrees of dissatisfaction regarding their anatomical gender [ 2 ]. Gender reassignment surgery (GRS) has proven to be a revolutionary intervention for patients with gender dysphoria, hence playing a pivotal role in alleviating their psychological discomfort. GRS is a multidisciplinary endeavour requiring a collaborative effort of psychology, psychiatry, family medicine, plastic surgery, endocrinology, otolaryngology, urology, gynaecology, maxillofacial surgery, and, last but not least, anaesthesiology.
Though GRS is becoming popular and more acceptable, there is still a relative lack of awareness of the process and its associated challenges amongst healthcare professionals. GRS has been performed with various approaches, single and multiple settings, hence imposing the need for anaesthetists to search for better and more efficient modes of anaesthesia to improve prognosis and minimize the associated morbidity. Just as surgeons develop areas of specialization to better care for their patients, anaesthesiologists have specialized in out- and inpatient surgery, both cosmetic and reconstructive.
The vanishing stigma, increasing demographic and acceptance of transgender and gender non-binary (TGNB) individuals calls for the field of medicine to catch up too. Hence, it is only discerning to expect that in coming times, they will present more frequently in general surgical settings and as they do, we would be well prepared to provide them high-quality peri-operative care. The ardent need to review this topic is rooted in the acknowledgement that although there are articles discussing the surgical and peri-operative outlooks of this procedure, there is scarce literature about the role, considerations, and strategies for anaesthesia in these procedures. This substantial shortfall in the published literature regarding the holistic concerns of GRS demands further strategies to be explored. We have discussed the anaesthetist strategy governed by consideration of the psychological aspects, effects of hormone therapy, optimal modes for anaesthesia and cautious watch for complications along with timely intervention for handling the same for providing high-quality anaesthetic care. In this article, we aim to analyse, understand, and formulate an approach for the entire procedure from an anaesthesiologist’s perspective.
RESEARCH METHODS
For this review, we retrieved data by a systematic literature search carried out in the research databases including PubMed, EMBASE, and Google Scholar. We included review articles, original studies, and case reports in our search.
History and current scenario
Dr Alan L. Hart, a TB specialist in the US, became one of the first female-to-male transgender persons who underwent gonadectomy and hysterectomy for his gender dysphoria in 1917 [ 3 ]. According to the 2018 census, nearly 0.6% of adults in the United States, or 1.5 million individuals, make up the transgender community. The estimated transgender population worldwide in the 2018 census ranged between 1% and 2% of the total population, which is nearly 900 million people. The American Society for Plastic Surgeons (ASPS) has reported an expeditious rise in GRS of up to 155% within the span of 2016 to 2017 [ 4 ]. With the legalization of transgender in most of the countries throughout the globe, the curve of GRS surgery is probably going to run further upslope.
OVERVIEW OF THE PROCEDURE
As already described, GRS requires a multidisciplinary approach. To begin with, the guidelines for the Recommendation of GRS indicate that the patient should be physically and psychologically prepared for surgery and should have a clear perception of the interventions to be performed along with the risks and possible complications [ 5 ]. Preparation for GRS is a multistage process that includes an elaborate psychological and wellbeing assessment of the patient. This may take nearly 12 months for complete psychosocial preparation of the patient to deal with the transition. Psychological evaluation is then followed by feminizing or masculinizing hormone replacement therapy (HRT) prescribed by a consulting endocrinologist. There should be documented “real-life experience in the desired role” for at least a whole year [ 5 ]. GRS ensues at the end of this process. The algorithm for the entire procedure is summarized in Figure 1 .

Algorithm for the procedure of gender reassignment surgery
INITIAL EVALUATION
What is required is having an elaborate understanding and assessment of the patient’s psychological, medical, legal, and social concerns. In developing countries, a substantial proportion of this relates to social and psychological aspects. The mental wellbeing assessment aims at evaluating and treating the mental health issues, offering suggestions with peer support with or without family therapy, assessing the gender expression level and the readiness of the patient for fully or partially reversible and irreversible interventions [ 6 ]. A reassuring and sensitive attitude towards the patient affirming that they would receive the best available care without any judgment aids in alleviating their anxiety and concerns. A holistic approach to assessment involves the multidisciplinary effort of various medical teams.
ANAESTHETIC PLAN OF CARE
Pre-operative assessment.
Apart from the routine preoperative assessment as for any other surgery, here we need to address specific history, examination, and investigations. The aim should be at the optimization of the patient care through risk reduction and informed consent [ 7 ]. It also caters to efficiently preparing the patient for surgery and anaesthesia while encouraging their compliance and participation.
- The biological sex and current gender identity of the patient should be noted.
- In the absence of specific gender assignment, measurements and calculations with gender specificity become tricky, e.g. ideal body weight, target-controlled propofol infusion using Schneider mode [ 8 ].
- Medical concerns.
- Patient’s preferred form of address (i.e., title, name, pronouns).
- History of use of anti-depressants, anti-anxiety, and other psychotropic drugs should be derived.
- Higher risk of tobacco, substance abuse, and sexually transmitted diseases (STDs) should be taken into consideration [ 9 ]. The prevalence of HIV was found to be 8.2% in the Indian transgender community as compared to 0.31% national HIV prevalence in India [ 10 ].
- History of multiple silicone injections can cue towards the existence of granulomatous disease, pneumonitis, organ failure, and infection [ 11 , 12 ].
- Masculinizing or feminizing therapy with a detailed description of drugs.
- Duration of therapy.
- Should be done with due respect to the privacy and dignity of the patient while maintaining professionalism.
- A chaperone of the gender of the patient’s choice should be present during physical examination.
- Should include assessment of any restrictive lung disease (common in female-to-male [FTM] chronic chest binders) [ 8 ].
- Most of the parameters should be evaluated as per the patient’s biological sex.
- However, for patients who have received HRT for more than six months, it has been suggested to compare the laboratory values to their cis-counterparts rather than their biological sex [ 13 ].
- There is still limited evidence regarding interpretations in different stages of gender transition.
Investigations to evaluate effects of HRT:
- complete lipid profile to screen for dyslipidaemias;
- liver function assessment to screen for any liver dysfunction;
- complete coagulation profile;
- screening for thromboembolism, breast and endometrial malignancy [ 15 , 16 ].
- Recognition and management of depression, anxiety, and regret.
- Advice on quitting smoking and explanation of its implications.
- Discontinuation of HRT for nearly 2-4 weeks before surgery in consultation with the endocrinologist and surgeon, keeping in consideration that prolonged withdrawal of hormones may culminate in the reversal of desirable effects [ 17 ].
- Considering the use of low-dose aspirin along HRT to reduce the risk of thromboembolism.
- Patients should be well informed regarding the overall cost, duration of hospitalization, surgical and anaesthetic options, complications, and post-operative care, and consent should be obtained.
Anaesthetic implications and concerns of HRT
It is not only relevant but imperative for an anaes-thesiologist to be aware of the various effects of HRT as it can guide the formulation of an efficient plan for anaesthesia. The various medications given in feminizing hormonal therapy include gonadotropin-releasing hormone agonists such as leuprolide and goserelin, spironolactone (androgen blockers), oral, parenteral or transdermal oestrogens and 5-α-reductase inhibitors such as finasteride. These medications can pose a higher risk of endocrine (e.g., diabetes) and cardiovascular (e.g., hypertension, venous thromboembolism [VTE]) implications. Testosterone therapy has been associated with derangements in liver function, which in turn complicate the drug metabolism. These risks are higher in the patients receiving oral formulations, hence necessitating the discontinuation of HRT for a few weeks prior to the surgery [ 16 ]. However, the withdrawal of hormone therapy can potentially make these patients more emotional, with rapid mood swings. This in turn can pose certain challenges for the anaesthetist in patient handling in the perioperative window ( Table 1 ). Incidence of postoperative delirium and post-operative nausea and vomiting (PONV) has also been found to be higher in patients on HRT. Some cases have revealed the occurrence of migraines in patients on anti-androgens. It is important to remember that in many cases these patients require lifelong administration of HRT unless curtailed by severe adverse effects.
Anaesthetic implications and concerns of hormone replacement therapy
Intra-operative considerations
The intra-operative care of these patients is distinctive as it needs the discernment of special anatomical, psychological, physiological, and pharmacological issues as numerated in Figure 2 . An anaesthesiologist needs to pay close attention to the following considerations:

Intra-operative considerations of gender reassignment surgery
- There should be clear instructions to the peri-operative team to maintain minimum traffic within the operating room (OR), particularly when the surgery involves exposure of the chest and/or genital regions.
- The patient’s preferred pronouns should be known and used at all times by the peri-operative staff when addressing the patient and any unnecessary questions should be discouraged.
Modes of anaesthesia
CSE – combined spinal-epidural, GA – general anaesthesia, LA – local anaesthesia, PNB – peripheral nerve block, PONV – post-operative nausea and vomiting, PACU – post-anaesthesia care unit, HRT – hormone replacement therapy.
- Transfer and positioning of the transgender patients who have undergone external body contouring procedures can be challenging and needs to be done with utmost caution.
- FTM transgenders may be using chest wraps and breast binders that need to be removed beforehand. Though there is still insufficient literature on the topic, chronic use of these tight chest binders can pose the risk of a restrictive respiratory pattern [ 14 ].
- Interestingly, even the most routine procedure of urinary catheterization can get tricky and challenging in the patients who have already had GRS concerning the urethra done, e.g. metoidioplasty with urethral lengthening, phalloplasty, or vaginoplasty.
- Patients who have recently had various facial aesthetic procedures such as rhinoplasty or jaw reconstruction may pose a challenge during bag and mask ventilation and should be handled with care and caution.
- Patients who have had previous voice pitch altering surgery such as chondroplasty or laryngoplasty may present as a difficult airway scenario as they pose the risk of tracheal stenosis or perforation, vocal cord damage, and dysphagia. Hence, a difficult airway cart should be kept ready [ 22 ].
- It needs to be taken into consideration that transgender women suffer from higher rates of HIV infection and might be on anti-retroviral therapy (ART). The various sedatives, anxiolytics, hypnotics, and antibiotics may present significant interactions with antiretroviral agents and result in altered drug metabolism [ 23 ].
- As these patients have been off steroid therapy for few weeks, they might experience steroid withdrawal syndrome. This can be prevented by administering a steroid bolus of 100-200 mg hydrocortisone intra-operatively.
- An anaesthetist needs to be vigilant for elevated intraoperative risks due to the possible existing respiratory, renal, cardiovascular, and hepatic compromise of the patient.
- VTE is a major perioperative concern due to the use of HRT medications and needs to be looked out for and relevant preventive interventions should be adopted. Cautious haemodynamic monitoring needs to be done for the early identification and management of this dreaded complication. Intraoperative prophylaxis should be provided with subcutaneous heparin and graded compression devices.
- Higher incidence of stroke has been linked to greater erythropoietin production and haematocrit and hence increased blood viscosity, attributed to parenteral testosterone therapy. Therefore, adequate hydration should be maintained for the patient [ 24 ].
- Considering the extensive nature of surgery, efficient pain control is imperative.
COMPLICATIONS
GRS presents with its arena of complications to be looked out for and dealt with. Amongst them, certain complications demand the anaesthesiologist’s ardent attention ( Table 3 ). These patients may be suffering from anaemia owing to the multiple and prolonged operations they undergo over some time. This needs to be taken care of by adopting appropriate pre-operative optimizing and perioperative blood loss reducing strategies. Two of the dreaded complications that the patients on oestrogen therapy should be monitored for are pulmonary embolism (PE) and deep vein thrombosis (DVT) [ 25 ]. These haematological events are attributed to peri-operative immobility, but due to the thrombotic effects of transgender HRT, there is a considerably higher risk of the same in these patients. The range of occurrence of VTE in transgender women on oestrogen therapy is from 0% to 6% [ 26 ]. The hypercoagulable state resulting due to HRT medications (both male-to-female and FTM) can precipitate cerebrovascular accidents and myocardial infarction and also aggravate any pre-existing coronary disease. This in turn warrants maintenance of adequate hydration at all times along with utmost care during all the phases of anaesthesia, supplemented by cautious intra-operative monitoring.
Complications in gender reassignment surgery, associated risk factors and preventive measures
The extensive wound surface, adverse effects of steroid therapy, and repeated surgery make these patients more susceptible to various infections, necrotizing fasciitis, and septicaemia [ 27 ]. The various other surgical complications include gastrointestinal events (e.g., rectal injury and rectovaginal fistula) and urinary tract complications (e.g., urethral stricture, fistula, and incontinence). Some unspecific events such as inguinal hernia, compartment syndrome, and asymmetry can also be witnessed after the surgery.
POSTOPERATIVE CONSIDERATIONS
The challenges continue after the completion of surgery, as the post-operative period in these patients has its concerns of postoperative pain, anxiety, depression, withdrawal, and at times regret [ 28 ]. Amongst the other parts of a detailed handover to the post-operative care team, one of the most important is validation of the patient’s preferred pronoun and name to avoid any unnecessary and repeated questioning [ 8 ]. It should be ensured that there is a multi-pronged approach with optimal analgesic strategies to manage post-operative pain. This can include epidural anaesthesia, intravenous analgesics, peripheral nerve blocks, parenteral therapy, and patient-controlled analgesia (PCA). There should be a collaborative approach to tend to the patient’s mental health, as well as social and spiritual needs. Canner et al . [ 29 ] reported that transgender patients require a higher level of care, highlighting the significance of formal training of health care providers for best practices to encourage and achieve a respectful and holistic approach towards anaesthesia delivery. Early implementation of social work and community support in the postoperative period plays a major part to smoothen the process of discharge while assisting the transition to patient recovery.
IMPORTANCE OF TEAMWORK AND COLLABORATION
As already mentioned, the complex procedure of gender reassignment involves a multidisciplinary effort of psychology, psychiatry, family medicine, plastic surgery, endocrinology, otolaryngology, urology, gynaecology, maxillofacial surgery, and anaesthesia. Evaluation by mental health professionals for eligibility criteria is a precondition for GRS as it can be a physically, emotionally, financially, and socially overwhelming procedure. The plastic surgeons, otolaryngologists, urologists and all other contributing surgeons need to have clear and competent participation in this long-term therapy. The surgeon and endocrinologist should also collaborate in optimizing HRT withdrawal and restart in the peri-operative period. The current state of affairs is still lacking such a closed loop inter-disciplinary approach. Hence, an efficient and especially dedicated team can help in achieving the ultimate goal of quality management to harness favourable outcomes for the patient.
CONCLUSIONS
Various parts of the world still suffer through an under-representation of the transgender community which stays confined to the margins of society. However, there is no denying the fact that with the changing tide and rising acceptability of transgender persons, the field of medicine is going to be presented with an increased proportion of these patients. The specific emotional, physiological, and pharmacological concerns coupled with the collaborative interplay of multiple disciplines make this class of patients a challenging lot. It is the attitude, preparedness and prudence of the medical team that can bring about a favourable outcome. Proper training of various health care professionals appears imperative here to empathetically handle and efficiently treat these patients. We would not be wrong in believing that the quality care provided before, during and after surgery has a substantial impact on patient outcomes after GRS. This simultaneously deserves acknowledgement of the fact that extensive studies and evidence are needed to understand and define better strategies for perioperative care in patients presenting for GRS.
ACKNOWLEDGEMENTS
Financial support and sponsorship, conflict of interest.
Hundreds of trans teens under 18 have had breasts removed in Canada, new data show
Concerns have been raised about mastectomies in teens when uncertainties exist about long-term health effects and the possibility of regret
You can save this article by registering for free here . Or sign-in if you have an account.
Article content
As tensions rise over the medical care of trans children, a new analysis shows hundreds of adolescents in Canada have undergone female-to-male “top surgery” — double mastectomies — over the past five years.
Hospitalizations and day surgery visits for bilateral mastectomies for gender reassignment surgery have risen sharply, from 536 in 2018-19, to 985 in fiscal 2022-23, according to data compiled for National Post by the Canadian Institute for Health Information.
Enjoy the latest local, national and international news.
- Exclusive articles by Conrad Black, Barbara Kay, Rex Murphy and others. Plus, special edition NP Platformed and First Reading newsletters and virtual events.
- Unlimited online access to National Post and 15 news sites with one account.
- National Post ePaper, an electronic replica of the print edition to view on any device, share and comment on.
- Daily puzzles including the New York Times Crossword.
- Support local journalism.
Create an account or sign in to continue with your reading experience.
- Access articles from across Canada with one account.
- Share your thoughts and join the conversation in the comments.
- Enjoy additional articles per month.
- Get email updates from your favourite authors.
Don't have an account? Create Account
Of the 4,071 visits in total involving gender-affirming mastectomies or breast reductions reported since 2018, 602 involved youth 18 and under.
Of those, 303 involved teens 17 and younger. The youngest age was 14.
The numbers tell only part of the story. The CIHI data exclude Quebec hospitals as well as surgeries performed in private clinics like the McLean Clinic in Mississauga, which describes its surgeons as “industry pioneers” for top surgery — mastectomies and breast reductions in those assigned female at birth, and breast augmentation for those born male transitioning to female.
One specialist in transgender health issues said that, when applying for OHIP funding for people seeking top surgery, “50 to 70 per cent will go to McLean.”
Female-to-male chest surgery involves removing the breasts to achieve a flatter, more masculinized torso, to better align the person’s physical body with their gender identity and reduce gender dysphoria, defined as the persistent distress that can accompany the incongruence between the gender one identifies with and one’s gender at birth.
Get a dash of perspective along with the trending news of the day in a very readable format.
- There was an error, please provide a valid email address.
By signing up you consent to receive the above newsletter from Postmedia Network Inc.
A welcome email is on its way. If you don't see it, please check your junk folder.
The next issue of NP Posted will soon be in your inbox.
We encountered an issue signing you up. Please try again
If this was just about ... kids being allowed to wear what they want and say what they want and be called whatever name they want and it stopped there, who would care?
But concerns have been raised about intervening with permanent, body-altering surgeries in adolescents when uncertainties exist about the long-term health effects, the possibility of regret and whether their trans identity will be lifelong.
Last week thousands gathered in cities across the country for duelling protests over gender policies in schools. Earlier this month delegates to the federal Conservative party’s policy convention voted 69 per cent in favour of prohibiting “life altering medicinal or surgical interventions” on minors under 18 to treat gender confusion or dysphoria.
Sweden, the world’s first country to authorize legal gender transitions in 1972, last year began limiting mastectomies for teenage girls to research settings. “The uncertain state of knowledge calls for caution,” the head of Sweden’s National Board of Health and Welfare said in a statement reported by AFP.
Public coverage for the surgeries varies from province to province. Most cover the cost of the mastectomy itself, but not several thousand dollars or more in extra add on fees for “chest contouring,” liposuction procedures to give the body a more sculpted, masculine look.
The rise in surgeries reflects a dramatic shift in the sex ratio of children and teens being referred to specialized gender identity clinics across the country, from once predominantly young boys to children born female.
One study involving 174 trans and non-binary children and teens referred to 10 gender identity clinics in Canada found 34 per cent of those assigned female at birth were referred for top surgery. Most were 15 or 16 at the time of referral.
Ontario’s Health Ministry declined to respond when asked the number of OHIP approvals for gender-affirming mastectomies in the most recent year available, including the proportion in youth. The McLean Clinic said its surgeons were unable to accommodate a request for an interview.
According to CIHI, of the 536 hospital visits for transgender reassignment mastectomies in 2018-19, 76, or 14 per cent, involved 18-year-olds and younger.
That age group accounted for 18 per cent of visits for mastectomies (174 out of 991) reported in fiscal 2021-22, and 14 per cent of visits (135 out of 985) in 2022-23.
The percentage dipped last year as hospitals grappled with pandemic-driven surgical backlogs. “But the private clinics just kept churning them through,” said one doctor familiar with trans medicine who requested anonymity fearing professional repercussions.
“The fact that you can’t get the numbers from private clinics…. It’s very cloak-and-dagger,” the doctor said. “They’re still billing OHIP. That’s tax dollars. That should be publicly accessible information. We need to see these numbers and ask questions,” the doctor said.
“If this was just about the schools, and just about kids being allowed to wear what they want and say what they want and be called whatever name they want and it stopped there, who would care? But medicine got involved.”
For a double mastectomy, typically two incisions are made on the bottom border of the pectoral muscle or chest area, according to the McLean Clinic’s website. “The skin is then lifted to surgically remove the breast tissue underneath.” The nipples are removed, re-sized and repositioned by grafting “to suit the new masculine appearance of the chest.”
It’s a day-surgery procedure performed under general anesthesia that takes approximately two hours. Complications can include bruising, wound infections and scarring. People lose nipple sensation as well as the ability to breastfeed should they become pregnant.
The uncertain state of knowledge calls for caution
Major medical groups like the American Academy of Pediatrics have strongly endorsed a gender-affirming approach to care to promote “optimal physical, mental and social wellbeing.” Eligibility for gender-affirmative surgeries in teens should be determined on a case-by-case basis, the AAP said in a 2018 policy statement the organization recently reaffirmed, while at the same time calling for a review of the evidence to develop an “expanded set of guidance.”
The growth in referrals to specialized clinics could be due to greater awareness and social acceptance, and the teaching of gender identity in school, experts said. But it’s not clear why it’s concentrated in children and teens born female.
Denying or holding back access to gender-affirming care “can have negative consequences for some youth,” SickKids in Toronto said in a statement. “Decisions for care should be made by youth, their families and their health-care providers, who are best-positioned to support them.”
Trans teens are known to be at higher risk of harassment and cyberbullying, wrote the authors of a recent review on the surgical and ethical considerations of gender affirming surgery in teens. Early access to surgery may reduce the bullying, they said, or help facilitate “age-appropriate romantic and sexual development in adolescents who may otherwise be prevented from engaging in these activities due to gender dysphoria.”
But the evidence is largely anecdotal, they said. The handful of published studies on surgery in minors involved relatively short follow-up periods.
“What we do know is that regret does take place, and it does take place later on in life,” said one trans medicine specialist, who also agreed to speak on the condition of anonymity for fear of being labelled “transphobic.”
“If we know that people can come to this realization that maybe this may have not been the best decision for them, if that takes place after five years or 10 years, we don’t have all the information to allow patients to make an informed decision.”
For such a permanent decision as the removal of healthy breasts, “I’m always looking at the why, and because that hasn’t been answered yet, that’s what leads to my ambivalence,” the specialist said.
“What all this says to me is that we need to be much more thoughtful in our approach and in our assessments.”
National Post
Our website is the place for the latest breaking news, exclusive scoops, longreads and provocative commentary. Please bookmark nationalpost.com and sign up for our daily newsletter, Posted, here .
Postmedia is committed to maintaining a lively but civil forum for discussion. Please keep comments relevant and respectful. Comments may take up to an hour to appear on the site. You will receive an email if there is a reply to your comment, an update to a thread you follow or if a user you follow comments. Visit our Community Guidelines for more information.
Bill Maher roasts Canada, calls the country a 'cautionary tale' of what the U.S. could be
Jesse kline: israel, u.s. should seize opportunity to destroy iran's nuclear program, young canadians squeezed by housing turn away from justin trudeau.
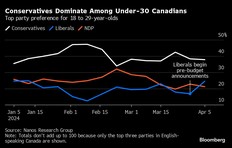
Julia Malott: The CRA's 'bare trust' fiasco serves as a lesson for lawmakers
Why is montreal a stolen car export hub, lululemon has a new bag and it’s trending.
The Parent Backpack is water-repellent, ultra-organized and not just for families
Beauty Buzz: Biotherm Blue Peptides Uplift Firming Day Cream, Virtue Hydrating Healing Hair Oil, and Dr. Hauschka Regenerating Intensive Eye Serum
Beauty Buzz: Three buzzed-about beauty products we tried this week
Advertisement 2 Story continues below This advertisement has not loaded yet, but your article continues below.
How to clean and season cast iron pans
A step-by-step guide on the best way to take care of your pan so it lasts for generations (because it really can)
The best online deals in the Canadian retail space right now
Casper, Shopbop, Best Buy and Sephora, to name a few
5 spring sunglasses guaranteed to elevate your eyewear game
Trends! Colours! Shapes! Price points!
This website uses cookies to personalize your content (including ads), and allows us to analyze our traffic. Read more about cookies here . By continuing to use our site, you agree to our Terms of Service and Privacy Policy .
You've reached the 20 article limit.
You can manage saved articles in your account.
and save up to 100 articles!
Looks like you've reached your saved article limit!
You can manage your saved articles in your account and clicking the X located at the bottom right of the article.
Vancouver Sun ePaper
Ontario court confirms right to surgery for non-binary resident, dismisses ohip appeal, notes surgery is listed, sharon kirkey.
Ontario has been ordered to pay for surgery for a resident who is seeking to have a vagina constructed while leaving their penis intact.
Denying the procedure would infringe on the person's Charter-protected right to security of the person, an Ontario court said in its ruling.
The unanimous decision by a three-member panel of judges of Ontario's Divisional Court could expand access to a novel “bottom surgery” for people who identify as non-binary, meaning neither fully male nor fully female.
The Ontario resident, identified in court documents as K.S., has been locked in a legal battle with the Ontario Health Insurance Plan since 2022, when OHIP denied a funding request to have a penile preserving vaginoplasty performed at a clinic in Austin, Texas.
The surgery, which is not available anywhere in Canada, involves creating a vaginal canal, or opening, without removing the penis.
K.S. was born male but identifies as female dominant and uses a feminine name.
OHIP denied her request for funding, arguing that the procedure is not included on its list of sex-reassignment procedures, and is therefore not an insured service.
K.S. appealed OHIP'S decision to Ontario's Health Services Appeal and Review Board, arguing that forcing her to have her penis removed would invalidate her identity and be akin to an illegal act of conversion therapy.
She also worried about the risk of complications and urinary incontinence from the urological rerouting, and the risk of orgasm dysfunction.
She argued the procedure she is seeking abroad is like standard vaginoplasties performed in Ontario, but without the additional procedure, namely, the penectomy.
The appeal board overturned OHIP'S decision, ruling that a vaginoplasty is among the genital surgeries listed for public coverage and need not inherently include removal of the penis. The board therefore ruled the procedure eligible for public funding.
OHIP appealed the board's decision to the Divisional Court, arguing the review board erred in finding a penis-sparing vaginoplasty is specifically listed as an insured service, and that it failed to consider that the unorthodox procedure is an experimental procedure in Ontario, and, therefore, not eligible for funding.
Just because vaginoplasty is listed as an insured service doesn't mean any type of vaginoplasty qualifies, OHIP argued in court.
The court disagreed. Vaginoplasty and penectomy are listed as discrete, separate services on Ontario's list of surgeries eligible for funding, the court said. “The fact that most people who have a vaginoplasty have it done in a way that also involves a penectomy” doesn't change the provision.
If the province had intended for only one type of vaginoplasty to be insured (vaginoplasty with penis removal) it should have drafted the list differently, the court said.
The court said the appeal board's conclusion was also consistent with the World Professional Association for Transgender Health (WPATH) standards of care — influential guidelines that received a scathing review this week by a massive British report into genderaffirming care.
The WPATH standards, which are referenced in OHIP'S schedule of benefits, “expressly refer to vaginoplasty without penectomy as a surgical option for some non-binary people,” Justice Breese Davies wrote in the court ruling.
While the court said it didn't need to address Charter arguments, if there was any ambiguity concerning what should or should not be covered, the review board's interpretation was also consistent with Charter values of equality and security of the person, the court added.
“The Charter-protected right to security of the person safeguards individual dignity and autonomy,” Davies wrote. Requiring a transgender or non-binary person born male “to remove their penis to receive state funding for a vaginoplasty would be inconsistent with the values of equality and security of the person.”
“Such an interpretation would force transgender, non-binary people like K.S. to choose between having a surgery (penectomy) they do not want, and which does not align with their gender expression, to get state funding on the one hand, and not having gender-affirming surgery at all on the other,” Davies wrote.
“Such a choice would reinforce their disadvantaged position and would not promote their dignity and autonomy.”
OHIP'S appeal was dismissed, and the province ordered to pay K.S. $20,000 to cover legal costs.
“This is a significant win for the transgender and non-binary communities,” K.S.'S lawyer, John Mcintyre, told CTV News Toronto.
2024-04-13T07:00:00.0000000Z
https://epaper.vancouversun.com/article/282724821968379

IMAGES
VIDEO
COMMENTS
Gender Surgery Clinic at Gordon and Leslie Diamond Health Care Centre. 2775 Laurel Street, 7th floor, Station 4A. Vancouver, BC V5Z 1M9. See directions on Google Maps. (604) 875-5060. See more details.
2775 Laurel Street, 7th floor, Station 4A Vancouver, BC V5Z 1M9. [email protected]. (604) 875-5060. Fax: (604) 875-5075. The Gender Surgery Program B.C., including the Gender Surgery Clinic, opened at Vancouver General Hospital (VGH) in September 2019, making the Gender Surgery Program B.C. Western Canada's only program performing ...
Dr. Genoway is a board-certified plastic and reconstructive surgeon in Vancouver, Canada. Dr. Genoway started performing gender-affirming Breast Augmentation and Top Surgery in 2016, followed by Vaginoplasty and Phalloplasty when the Gender Surgery Program B.C. launched in September, 2019.
Vancouver Coastal Health is committed to delivering exceptional care to 1.25 million people, including the First Nations, Métis and Inuit, within the traditional territories of the Heiltsuk, Kitasoo-Xai'xais, Lil'wat, Musqueam, N'Quatqua, Nuxalk, Samahquam, shíshálh, Skatin, Squamish, Tla'amin, Tsleil-Waututh, Wuikinuxv, and Xa ...
The Ministry of Health says a gender surgery clinic will be opening at Vancouver General Hospital by the end of September, meaning patients no longer have to fly to a private clinic in Montreal ...
In September 2019, the Gender Surgery Program BC, located within Vancouver Coastal Health, became Western Canada's first and only centre to perform lower body gender-affirming surgeries for transgender and gender-diverse individuals. ... Patient-reported complications and functional outcomes of male-to-female sex reassignment surgery. Arch ...
Complete your surgery at the most appropriate care facility in Vancouver. As part of your recovery and post-operation care, you will attend follow-up appointments at the Gender ... British Columbians still have the option to pursue their surgery at Gender Reassignment Surgery (GRS) Montreal. When medically necessary, patients may access out-of ...
Reconstructive gender-affirming surgeries will be available within Vancouver Coastal Health starting in 2019. In addition, trans people throughout the province now have improved access to publicly funded gender-affirming chest and breast surgeries. A total of 14 surgeons will provide these surgeries in Burnaby, Kamloops, Kelowna, Port Moody ...
Gender-affirming surgeries change primary or secondary sex characteristics so that they correspond with one's gender identity. Many trans and gender diverse people are happy with their bodies, or find comfort with their bodies through non-surgical means. Only you can decide whether surgery is right for you . Research shows that gender ...
Finding her way: Five years after gender-reassignment surgery Tamara Loyer helps other trans women. In 2015, Tamara Loyer was living in social housing, panhandling, and struggling with gender ...
WPATH SOC-8: Changes to gender-affirming surgery in B.C. In February 2023, several pathway and practice changes, in line with the WPATH SOC-8, were implemented in B.C. ... Statement regarding the delivery of gender-affirming care for youth in B.C. The Provincial Health Services Authority (PHSA), including BC Children's Hospital (BCCH) and ...
and supported before, during, and after your surgery. See Trans Care BC's website to learn more about what to expect during a Surgical Readiness Assessment and other frequently asked questions. In BC, publicly-funded gender-affirming vaginoplasty or vulvoplasty surgery is usually done at GSP BC (Vancouver) or GRS Montreal. Once
Carolynn Dimmer is a 43-year-old transgender woman who had gender reassignment surgery in 2007. Living in the West End of Vancouver, Dimmer has a black belt and teaches self-defense to others in ...
We offer surgery care planning, referrals and system navigation even for patients who are not interested or ready to proceed with hormone initiation. For questions about the referral requirements for the surgery you are interested in, please contact one of our team members at (604) 331-8901 or [email protected].
With the Government of Nunavut's funding commitment, the goal of nation-wide coverage for gender-affirming surgery in Canada has been achieved. Improvements to provincial and territorial funding policies are still needed but this is a milestone to be celebrated. Review Funding Policies by Province and Territory: With Nunavut's announcement ...
The Gender Clinic supports the needs of transgender and gender-questioning youth up until their 17th birthday with puberty blockers and/or gender-affirming hormones. Who we are. In 1998, our clinic began seeing transgender and gender-diverse children, youth, and their families, and we now have one of the busiest clinics in North America.
Gender-affirming mastectomy is the most commonly performed gender-affirming surgical procedure, often referred to as "top surgery". The most frequently performed technique is the "double incision with free nipple graft" where the breast tissue and excess skin is removed in addition to removing, re-sizing, re-shaping and replacing the ...
A teenager in B.C. is free to move forward with his gender-affirming chest reconstruction surgery after a Supreme Court justice tossed his mother's attempt to stop the procedure, finding she made ...
Also in 2019, British Columbia began offering its trans residents access to bottom surgeries at the Vancouver General Hospital. ... "Toronto's Women's College Hospital launches new program for gender-reassignment surgery," Kelly Grant, Globe and Mail, June 17, 2019
Observations: Gender confirmation surgery is a developing field in the United States and other areas of the world. The World Professional Association for Transgender Health started a global education initiative intended to provide surgeons and other health care professionals with the necessary background knowledge to understand and treat this ...
Gender-affirming surgery involves additional planning, and we encourage you to think ahead in your surgical journey. The following are general considerations to plan for as you prepare for surgery. ... Vancouver Coastal Health is committed to delivering exceptional care to 1.25 million people, including the First Nations, Métis and Inuit ...
Gender dysphoria, earlier known as gender identity disorder, describes a heterogeneous group of individuals having the desire to possess secondary sexual characteristics of the opposite sex and possessing varying degrees of dissatisfaction regarding their anatomical gender . Gender reassignment surgery (GRS) has proven to be a revolutionary ...
According to CIHI, of the 536 hospital visits for transgender reassignment mastectomies in 2018-19, 76, or 14 per cent, involved 18-year-olds and younger. That age group accounted for 18 per cent ...
The surgery, which is not available anywhere in Canada, involves creating a vaginal canal, or opening, without removing the penis. K.S. was born male but identifies as female dominant and uses a feminine name. OHIP denied her request for funding, arguing that the procedure is not included on its list of sex-reassignment procedures, and is ...
The Vatican has issued a strong warning against "gender theory" and said that any gender-affirming surgery risks threatening "the unique dignity" of a person, in a new document signed off ...