Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals More You are viewing from: Google Indexer

You are here
- Volume 14, Issue 5
- How to manage alcohol-related liver disease: A case-based review
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0003-1530-5328 James B Maurice 1 ,
- http://orcid.org/0000-0001-5140-517X Samuel Tribich 2 ,
- Ava Zamani 3 ,
- Jennifer Ryan 4
- 1 Department of Gastroenterology and Hepatology, Southmead Hospital , North Bristol NHS Trust , Bristol , UK
- 2 Department of Hepatology, Royal London Hospital , Barts Health NHS Trust , London , UK
- 3 Hammersmith Hospital , Imperial College Healthcare NHS Trust , London , UK
- 4 Department of Hepatology and Liver Transplantation, Royal Free Hospital , Royal Free London NHS Foundation Trust , London , UK
- Correspondence to Dr James B Maurice, Department of Gastroenterology and Hepatology, Southmead Hospital, North Bristol NHS Trust, Bristol BS10 5NB, UK; james.maurice{at}nbt.nhs.uk
https://doi.org/10.1136/flgastro-2022-102270
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
- alcoholic liver disease
- chronic liver disease
What is already known on this topic
Alcohol-related liver disease (ArLD) is a major cause of morbidity and mortality.
What this study adds
We present a typical case to illustrate current evidence-based investigation and management of a patient with ArLD.
This case-based review aims to concisely support the day-to-day decision making of clinicians looking after patients with ArLD, from risk stratification and fibrosis assessment in the community through to managing decompensated disease, escalation care to critical care and assessment for liver transplantation.
How this study might affect research, practice or policy
We summarise the evolving evidence for the benefit of liver transplantation in alcoholic hepatitis, and ongoing controversies shaping future research in this area.
ArLD is fundamentally a public health problem, and further efforts are required to implement effective policies to reduce consumption and prevent disease.
Introduction
Alcohol is the leading risk factor for premature death in young adults, of which alcohol-related liver disease (ArLD) is a major contributor. 1 The management of ArLD often requires complex decision-making, raising challenges for the clinician and wider multidisciplinary team. This case-based review follows the typical journey of a patient through the progressive stages of the disease process, from early diagnosis and risk stratification in the outpatient clinic through to alcoholic hepatitis and referral for liver transplantation. At each stage, we discuss a practical approach to clinical management and summarise the underlying evidence base.
Case part 1
A 47-year-old man is referred to the general hepatology clinic from his General Practitioner with abnormal liver function tests, ordered in the community following several episodes of non-specific abdominal pain which subsequently resolved. He is now asymptomatic. The referral states that he drinks one bottle of wine each weekday night and more at the weekends. He is on no regular medication, has no other significant medical history and works in construction. On clinical examination, there are a few spider naevi on the chest wall but no other stigmata of liver disease, and his body mass index is 26 kg/m 2 . The blood results show alanine aminotransferase (ALT) 65 IU/L, aspartate aminotransferase (AST) 92 IU/L, alkaline phosphatase (ALP) 100 IU/L, gamma-GT (GGT) 350 IU/L, bilirubin 15 µmol/L, albumin 45 g/L, platelets 256×10 9 /L, internation normalised ratio (INR) 1.0 and creatinine 50 µmol/L. Abdominal ultrasound reveals a mildly enlarged, hyperechoic liver but normal spleen and no ascites.
How can we risk-stratify patients with ArLD in the outpatient clinic?
Early diagnosis and risk stratification of patients enables appropriate selection of patients for follow-up in secondary care, while also providing an opportunity for preventative interventions in those with mild disease. Emergency admissions for hepatic decompensation, where up to 75% of patients present for the first time, represent a late stage of the disease process when 1-year mortality is very high. 2 It is therefore vital to make an early diagnosis of liver disease.
Hepatic fibrosis has been traditionally staged by liver biopsy; however, non-invasive methods of fibrosis staging have an emerging role in ArLD. Transient elastography (TE) has been validated against liver biopsy to accurately stage both advanced fibrosis and cirrhosis, 3–6 and current NICE guidance recommends TE for the diagnosis of cirrhosis in patients with ArLD.
Serological markers of fibrosis such as FIB-4 and AST-Platelet Ratio Index (APRI) have generally not performed well in ArLD, although the enhanced liver fibrosis (ELF) test, measuring direct markers of fibrosis in blood, has an Area Under the Receiver Operator Curve (AUROC) of 0.92 in diagnosing advanced fibrosis using a cut-off value of 10.5. 7
How can we screen for alcohol use disorder and ArLD?
The primary screening tools for alcohol use disorders are the Alcohol Use Disorders Identification Test (AUDIT) or abbreviated AUDIT-C questionnaires. 8 Although clear documentation of the amount of alcohol consumed is important, a diagnosis of alcohol use disorder is more nuanced than volume of alcohol alone, hence the improved sensitivity through use of validated questionnaires. Identifying increasing risk (AUDIT 8–15), higher risk (AUDIT 16–19) or possible dependence (AUDIT≥20) 8 provides an opportunity for targeted brief interventions in those who would most benefit and is a cost-effective method for reducing alcohol intake. 9 Typically only comprising a 5–20 min single interaction, brief interventions offer personalised advice using a motivational and empathetic style of interview ( Box 1 ). If delivered to all new patients registered in primary care, this could save 2500 alcohol-related deaths over 20 years. 10 Patients identified to have alcohol dependence through screening should be referred for specialist treatment.
Typical features of brief interventions
Feedback on the person’s alcohol use and any related harm.
Clarification as to what constitutes low-risk consumption.
Information on the harms associated with risky alcohol use.
Benefits of reducing intake.
Motivational enhancement to support change.
Analysis of high-risk situations for drinking.
Coping strategies and the development of a personal plan to reduce consumption.
Adapted from Public Health England Review: the public health burden of alcohol and the effectiveness and cost-effectiveness of alcohol control policies. An evidence review. 45
Although routine blood tests may be helpful in supporting a diagnosis of ArLD (eg, AST>ALT, increased GGT, macrocytosis), they are of limited value in determining the severity of liver disease before established cirrhosis has developed with impaired liver synthetic function (low albumin, high INR and bilirubin). Individuals drinking at harmful levels should be screened for liver fibrosis with TE. Hepatology referral should be considered in patients with TE 8–16 kPa, particularly in those who continue to drink at harmful levels. Patients with TE≥16 kPa are at high risk of developing complications of cirrhosis, therefore should be followed up in a specialist hepatology clinic and be screened for hepatocellular carcinoma and oesophageal varices. Screening endoscopy for varices should be offered when TE≥20 kPa or platelets≤150×10 9 /L. 11 In the primary care setting, fibrosis screening of individuals drinking at harmful levels may alternatively be done with the ELF test, although this is not uniformly available ( figure 1 ). 12
- Download figure
- Open in new tab
- Download powerpoint
Screening for cirrhosis in individuals drinking at hazardous and harmful levels. ARFI, Acoustic Radiation Force Impulse; AUDIT, Alcohol Use Disorder Identification Test; AUDIT-C, abbreviated Alcohol Use Disorder Identification Test; ELF, enhanced liver fibrosis; GGT, Gamma-GT; HCC, hepatocellular carcinoma; NICE, The National Institute of Health and Care Excellence. Reproduced with permission from Newsome et al . 46
A high-risk population that should be considered for ArLD screening are the patients admitted to hospital acutely with alcohol-related physical harm, such as acute alcohol withdrawal or alcohol-related trauma. These patients should all be referred to alcohol care teams, and in addition to their expertise in delivering brief interventions, tailored detoxification regimens and vital links to local alcohol support services in the community, some hospitals have trained to perform TE and screen for liver fibrosis. This has provided an opportunity to streamline at risk patients into the hepatology services.
Case part 2
The same patient presents on the acute medical take 1 year later with a 2-week history of jaundice and abdominal swelling. Unfortunately, he has continued drinking alcohol. On examination, he is jaundiced with moderate ascites, tender hepatomegaly and subtle asterixis. He is sarcopenic with arm muscle wasting. He has the following blood results: haemoglobin 100 g/L, mean cell volume 107 fL, white cell count 12×10 9 /L, platelets 135×10 9 /L, INR 2.3, sodium 132 mmol/L, potassium 3.0 mmol/L, creatinine 55 µmol/L, urea 2.0 µmol/L, bilirubin 250 µmol/L, ALT 25 IU/L, AST 60 IU/L, ALP 95 IU/L, GGT 200 IU/L, albumin 35 g/L, c-reative protein (CRP) 45 mg/L. A diagnostic paracentesis reveals an ascitic albumin 16 g/L, white cells 90/mm 3 (80% lymphocytes). An X-ray of the chest is normal. Ultrasound liver demonstrates hepatomegaly 17 cm, splenomegaly 15 cm, moderate ascites and a patent portal vein. A clinical diagnosis of alcoholic hepatitis (AH) is made.
What is the role of liver biopsy in the diagnosis of AH?
AH is a clinical syndrome characterised by jaundice and coagulopathy in the context of recent and prolonged heavy alcohol use. Rapid development of jaundice is accompanied by a systemic inflammatory response with constitutional symptoms and low-grade fever, with or without other features of decompensation.
The diagnosis of AH can be made using a standard consensus definition based on clinical and biochemical parameters ( table 1 ), originally established to allow inclusion in clinical trials without the need for a liver biopsy but now generalised to clinical practice. 13 Neither European Association for the Study of Liver Disease (EASL) nor American College of Gastroenterology (ACG) guidelines recommend liver biopsy in patients meeting the criteria for probable AH, 9 10 and these recommendations have been supported by more recent data, showing that liver biopsy rarely changes the diagnosis when clinical criteria are met for AH. 12 However, if diagnostic uncertainty remains, such as atypical biochemical markers, uncertain alcohol use or a suspected alternative cause of liver injury, a liver biopsy should be undertaken to confirm the diagnosis, particularly if planning to administer AH-directed medical therapies. 14
- View inline
Consensus definition for ‘probable’ alcohol hepatitis 13
In those patients in whom a biopsy is undertaken, specific histological features such as degree of neutrophil infiltration, fibrosis stage and presence of megamitochondria can be useful for prognostication using the Alcoholic Hepatitis Histologic Score, which is independently predictive of 90-day mortality. 15 However, the utility of this is significantly limited by interobserver variability between reporting pathologists. 16
Should this patient be treated with steroids?
Once a diagnosis of AH is established, patients should be risk stratified using a validated scoring system. The modified Maddrey’s discriminant function (mDF) is a commonly used score, which defines a cut-off of ≥32 as severe AH; however, this is very sensitive and risks over-treating patients with mild disease. 17 The Glasgow Alcoholic Hepatitis Score (GAHS) and Model for End-Stage Liver Disease (MELD) are better predictors of 28-day and 90-day mortality than mDF 18 19 and are also now included in EASL and ACG guidelines, with severe AH defined as GAHS≥9 or MELD≥21. 20 , 14
The STeroids Or Pentoxifylline for Alcoholic Hepatitis (STOPAH) study is the largest randomised controlled trial to investigate the efficacy of corticosteroids in the treatment of AH. It included 1103 participants with severe AH and the group that received prednisolone only had a small non-significant improvement in 28-day survival (OR 0.72, 95% CI 0.52 to 1.01, p=0.06), a benefit which was lost by 90 days and 1 year. In the multivariate analysis adjusting for baseline variables, prednisolone was associated with improved 28-day survival compared with placebo (OR 0.61, p=0.015), although not at 90 days or 1 year. 21 Further meta-analyses of pooled data have replicated these findings. 22
The EASL and ACG guidelines advise to take steroid treatment with prednisolone 40 mg per day in patients with severe AH, as defined by either the mDF, GAHS or MELD Score. Steroid responsiveness should be assessed using the Lille Score, typically on day 7, although there is data to support earlier application on day 4, 23 with steroids stopped in non-responders (Lille Score≥0.45); responders should complete a 28-day course. It may be possible to predict Lille response using a baseline neutrophil-to-lymphocyte ratio (NLR), with an NLR of 5–8 predictive of a significant reduction in 90-day mortality with corticosteroid treatment, compared with no reduction when NLR is less than 5 or more than 8. 24 Emerging data is further delineating which patients may derive the greatest benefit from corticosteroids 25 ; however, this remains an area of ongoing research.
Infection is a frequent complication of severe AH, contributing significantly to the high mortality rate and associated in particular with an increased 90-day mortality. 26 Corticosteroids are associated with an increased incidence of infection post-treatment compared with placebo (10% vs 6%), 21 and significantly worse 90-day mortality if patients develop infection within the first week of starting steroids. 26 Therefore, particular caution is required prior to starting prednisolone in patients with active sepsis, bearing in mind that patients with cirrhosis may not mount a classic immune response to infection. 26 Biomarkers to predict risk of incident infection on steroids are an area of research interest; baseline NLR of >8 is also associated with increased infection at day 7 of corticosteroid treatment (OR 2.60, p=0.006), but requires further validation. 24
In clinical practice, the commencement of steroids is delayed until infection is excluded, including negative cultures of blood, urine and ascitic fluid. This period also allows for the assessment of the bilirubin trend which, along with risk stratification scoring, helps to inform the decision to start corticosteroids. 27
What are the considerations in managing alcohol withdrawal in patients with advanced liver disease?
Alcohol withdrawal syndrome (AWS) should be assessed using the Clinical Institute Withdrawal Assessment for AlcoholScore, with a symptom-based regimen rather than fixed dosing in order to reduce drug accumulation. 28 Benzodiazepines reduce withdrawal symptoms and the risk of both seizures and delirium tremens and are considered the gold standard for treatment of AWS. Long-acting benzodiazepines such as chlordiazepoxide and diazepam should only be used with caution in patients with cirrhosis and impaired synthetic function due to their unpredictable half-life and significant accumulation in the presence of hepatic dysfunction, where the use of shorter-acting lorazepam or oxazepam may be preferable if available. In addition, benzodiazepines can both precipitate and worsen hepatic encephalopathy and so should be used with care.
Abstinence from alcohol remains the only independent predictor of long-term survival in patients presenting with severe AH 29 and early intervention from an alcohol liaison service during the hospital admission is of fundamental importance.
What is the role of nutrition in the management of AH?
Patients with both AH and cirrhosis are characterised by an almost universal state of malnutrition, sarcopenia and B vitamin deficiency, alongside increased resting energy expenditure and impaired metabolism of carbohydrates, lipids and proteins. 30 Early involvement of the dietetic team is vital to ensure patients with AH meet their nutritional requirements.
Increased caloric intake has been associated with a reduced incidence of infection, improved liver function and quicker resolution of hepatic encephalopathy in multiple randomised trials. 30 A recent large trial reported lower rates of infections and improved 1-month and 6-month mortality in patients with severe AH treated with corticosteroids who received a calorie intake of ≥21.5 kcal/kg/day compared with those who received<21.5 kcal/kg/day, regardless of Lille response or of the mode by which the calories were delivered. 31
EASL and European Society for Clinical Nutrition and Metabolism (ESPEN) guidelines recommend an aim of 35–45 kcal/kg/day and a daily protein intake of 1.2–1.5 g/kg/day, with the oral route as first line and nasogastric feeding advised if oral intake is inadequate. 30 Intravenous thiamine replacement should be given to all patients with a history of alcohol use to reduce the risk of Wernicke’s encephalopathy. Several clinical trials have failed to demonstrate evidence for the use of various specialised dietary formulas and ESPEN recommend using standard nutritional supplements or feed with a high energy density, with a late evening supplement to reduce overnight starvation duration. 30
Case part 3
A full septic screen including blood cultures did not reveal any evidence of sepsis. The patient is managed with nutritional supplements, lactulose 20 mL three times a day and prednisolone 40 mg once daily. At day 7, his blood results are bilirubin 355, INR 3.0, PT 27, Cr 90, albumin 29. Lille Score is 0.60 (>0.45) indicating a poor prognosis, so prednisolone is stopped. Overall 90-day mortality in patients with AH is approximately 30%, increasing to around 45% in patients with a Lille Score>0.45 after 7 days of corticosteroids. 19
Is liver transplantation an option in severe AH?
In Europe, ArLD is the leading indication for liver transplant (LT), but the timing and selection of patients for liver transplantation with ArLD is controversial. A period of abstinence is vital to understand the extent of hepatic recompensation that can occur without the need to undergo LT and to ensure the patient is engaged with the process. However, although pretransplant abstinence is one important predictor of post-LT sobriety, it is not the only factor, and there is data that the risk of relapse is no higher in carefully selected patients transplanted with severe alcoholic hepatitis (SAH) compared with those with alcohol-related cirrhosis under standard selection criteria. 32
Challenging the traditional exclusion of patients with SAH from consideration for LT, a multicentre cohort study in France offered LT to patients with SAH who met specific stringent selection criteria, including non-response to steroid therapy, a first presentation of liver decompensation and a robust social support network. 33 This study showed significantly improved survival in the group offered LT at 2 years (71% vs 23%), a benefit almost entirely gained in the first 6 months. Long-term follow-up data was recently presented, showing overall survival at 1, 5 and 10 years of 83%, 70% and 56%, respectively. Severe alcohol relapse was evident in 10%, similar to other cohorts transplanted for ArLD using standard selection criteria. 34
The largest study in the USA on LT in SAH is a retrospective review of United Network for Organ Sharing data. In 147 patients transplanted with SAH between 2006 and 2017, with no previous decompensation and abstinence of less than 6 months, 1-year and 3-year survival was 94% and 84%, while return to sustained drinking occurred in 10% at 1 year and 17% at 3 years. 35 Interestingly, in a smaller retrospective case-controlled study comparing patients transplanted with SAH with<6 months abstinence (n=46) with a group transplanted for standard ArLD criteria and>6 months abstinence (n=34), the two groups had comparable 1-year survival (97% vs 100%, p=1) and return to harmful drinking after median follow-up of 532 days (17% vs 12%, p=0.5). 32
The only prospective trial of early liver transplantation in SAH was a non-randomised, non-inferiority, controlled trial recently published by the group in France. Over 2 years of follow-up, patients with SAH offered early liver transplant (n=68) had a small but non-significant increased risk of alcohol relapse compared with those transplanted for alcohol-related cirrhosis after ≥6 months of abstinence (n=93, relative risk 1.45, 95% CI 0.82 to 2.60), but also a greater risk of high levels of alcohol intake (RR 4.10, 95% CI 1.56 to 10.75). The 2-year post-transplantation survival was similar between these groups (89.7% and 88.2% respectively, HR 0.87, 95% CI 0.33 to 2.26), whereas the overall 2-year survival of patients with SAH who were not transplanted (n=47) was significantly reduced compared with those who were (28.3% vs 70.6%, HR 0.27, 95% CI 0.16 to 0.47). 36
The landscape of public and medical opinion on offering transplantation for SAH is changing in light of this data. However, concerns remain that predictive models are suboptimal and over 50% of patients with an unfavourable prognosis based on the Lille Score will survive without LT. 37 As such, the UK pilot on LT in SAH failed to recruit any patients over a 3-year period and was closed. 38 The current UK position recommends that if liver insufficiency persists after 3 months of documented alcohol abstinence in individuals with an index presentation of severe AH, consideration should be given to referral for liver transplantation if their psychosocial risk profile is favourable. 37
Case part 4
The patient’s clinical condition deteriorates over the following week. He becomes febrile, an ascitic tap confirms spontaneous bacterial peritonitis (white cells 700 cells/mL, neutrophils>90%) and he develops an oliguric acute kidney injury with haemodynamic instability requiring regular fluid boluses. His liver function remains poor (UK Model for End Stage Liver Disease (UKELD) 68). You call the intensive care unit (ITU) to review the patient, but questions are raised about his suitability for level 3 care.
Should this patient be escalated to critical care?
This patient now requires organ support with inotropes and likely renal replacement therapy. Historically, patients with ArLD have experienced barriers to timely escalation to ITU due to a perceived poor prognosis. Data in the National Confidential Enquiry into Patient Outcome and Death report in 2013 confirmed this practice, showing that 31% of patients deemed to require and be appropriate for escalation of care on independent review of the case notes did not receive such treatment. 39
In the same report, a review by the treating clinicians identified only 7% of cases who were appropriate for escalation but did not receive it. Subjective judgements detrimentally influenced these decisions and led the report to conclude that failure to escalate was due to clinicians having a prior view that it was not appropriate to escalate care in patients with ArLD.’ 39
Over the last 20 years, there has been a significant improvement in survival of patients admitted to ITU with organ failure complicating decompensated chronic liver disease, with mortality falling from 41.0% to 32.5% over this period, despite comparable scores for severity of illness at presentation. Although ArLD was associated with worse survival, improvements were also reported in this group over the same period (50.9% mortality to 41.9%, mean (Acute Physiology and Chronic Health Evaluation (APACHE) II Score 20 vs 19), such that the majority admitted to ITU will survive. 40
However, mortality rates for patients with ArLD and acute-on-chronic liver failure admitted to the ITU remain high, and escalation decisions require careful discussion and shared decision-making between the medical and critical care teams, alongside patients and their families as required. One of the first questions posed by the ITU team may be whether they are a transplant candidate. This is not a straightforward question to answer and may not be the most pertinent issue at this point in the patient’s care: in his case, the immediate answer would be ‘no’ in the UK, for reasons discussed above. But if he survives this admission, maintains abstinence but continues to have a qualifying UKELD Score he may be considered for a transplant assessment in 3 months.
In this instance, the patient’s age and the fact this is a first presentation with hepatic decompensation strongly support escalation at this stage, but the CLIF-ACLF prognostic scoring system can be helpful to add objective data to discussions between the managing team and ICU. While not including some increasingly recognised prognostic factors such as the presence of sarcopenia, the European Foundation for the Study of Chronic Liver Failure Acute-on-chronic Liver Failure (CLIF-C ACLF) Score has nevertheless been validated in a large dataset of patients with decompensated chronic liver disease and organ failure. 41 Days 3–7 on the ITU may be the optimal time to calculate this score, when an accurate assessment on the trajectory and likely outcome can be made. 42 Applying it in this way can support decision-making between the patient’s primary team and the ITU and provide timescales and goals with which to assess the benefits of level 3 care when there is disagreement or uncertainty.
However, even in the setting of treatment escalation it is important to remember that his overall prognosis is poor at this stage and, therefore, early involvement of the palliative care (PC) team should be considered. This can be done in parallel with full active medical care; it is important to bear in mind that PC is not synonymous with ‘end-of-life care’ and they are excellently equipped to optimise symptom control and begin to address wider holistic issues in the care of a patient at high risk of death. As such, early involvement of PC has been shown to improve symptom control and quality of life. 43
Case part 5
After 2 weeks in the ITU and a prolonged inpatient stay, the patient makes sufficient recovery to be discharged home. He continues to have moderate ascites managed with spironolactone and significant liver synthetic dysfunction (UKELD 60). He begins to attend his local alcohol support group and his partner has removed all alcohol from the house to support his abstinence.
When should you refer for transplant assessment?
Although he has made significant progress, this patient remains very unwell and at high risk of further deterioration. His ‘window of opportunity’ for transplant assessment is small. There is no fixed rule on this, but recent guidelines suggest that referral should be considered after 3 months of abstinence, or even sooner if the patient is actively engaged in alcohol cessation support, if there are issues that may complicate the workup assessment, or if the risk of death within 3 months is high. 44 In parallel to referral, every effort should be made to optimise his physical fitness, including dietician input and a graded exercise plan.
The patient maintains abstinence, is referred and successfully receives a life-saving liver transplant. A multidisciplinary team approach is required for patients admitted with decompensated ArLD, in which a dedicated alcohol care team is vital, but preventative measures on a population (eg, minimum unit pricing) and individual (eg, brief interventions and fibrosis stratification) level early in the disease course will have the greatest impact.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
- Griswold MG ,
- Fullman N ,
- Williams R ,
- Aspinall R ,
- Bellis M , et al
- Kettaneh A ,
- Tengher-Barna I , et al
- Pavlov CS ,
- Casazza G ,
- Nikolova D , et al
- Detlefsen S ,
- Sevelsted Møller L , et al
- Lackner C ,
- Bataller R ,
- Burt A , et al
- Madsen BS ,
- Hansen JF , et al
- National Institute for Health and Care Excellence
- Anderson P ,
- Chisholm D ,
- Gillespie D ,
- Ally A , et al
- de Franchis R , Baveno VI Faculty
- Forrest E ,
- Chalasani NP , et al
- Altamirano J ,
- Katoonizadeh A , et al
- Horvath B ,
- Allende D ,
- Xie H , et al
- Forrest EH ,
- Atkinson SR ,
- Richardson P , et al
- Singal AK ,
- Ahn J , et al
- Thursz MR ,
- Richardson P ,
- Allison M , et al
- Chandar AK , et al
- Garcia-Saenz-de-Sicilia M ,
- Altamirano J , et al
- Sinha R , et al
- Baeza N , et al
- Knapp S , et al
- Cabezas J ,
- Mirijello A ,
- D’Angelo C ,
- Ferrulli A , et al
- Labreuche J ,
- Artru F , et al
- Bischoff SC ,
- Dasarathy S , et al
- Deltenre P ,
- Senterre C , et al
- McCaul ME , et al
- Mathurin P ,
- Samuel D , et al
- Dharancy S ,
- Dumortier J , et al
- Platt L , et al
- Moreno C , et al
- Aldersley H ,
- Leithead JA , et al
- Juniper M ,
- Kelly K , et al
- McPhail MJW ,
- Parrott F ,
- Wendon JA , et al
- Pavesi M , et al
- Fernandez J ,
- Garcia E , et al
- Woodland H ,
- Forbes K , et al
- Millson C ,
- Considine A ,
- Cramp ME , et al
- Newsome PN ,
- Davison SM , et al
Twitter @jamesbmaurice
Contributors JBM conceptualised the original article and the case. JBM, ST and AZ drafted the initial version of the manuscript. JBM and ST contributed further editing of various sections. JR provided senior critical review and edited the manuscript. All authors agreed upon the final version.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
Linked Articles
- Highlights from this issue UpFront R Mark Beattie Frontline Gastroenterology 2023; 14 357-358 Published Online First: 07 Aug 2023. doi: 10.1136/flgastro-2023-102519
Read the full text or download the PDF:
Cirrhosis Case Study (45 min)
Watch More! Unlock the full videos with a FREE trial
Included In This Lesson
Study tools.
Access More! View the full outline and transcript with a FREE trial
Mr. Garcia is a 43-year-old male who presented to the ED complaining of nausea and vomiting x 3 days. The nurse notes a large, distended abdomen and yellowing of the patient’s skin and eyes. The patient reports a history of alcoholic cirrhosis.
What initial nursing assessments should be performed?
- Full abdominal assessment, including assessing for ascites
- Heart and lung sounds
- Skin assessment – color, turgor, etc.
- Full set of vital signs
- Neurological assessment
What diagnostic testing do you anticipate for Mr. Garcia?
- LFT’s, CBC, BMP
Mr. Garcia’s vitals are stable, BP 100/58, bowel sounds are active but distant, and the nurse notes a positive fluid wave test on his abdomen. The patient denies itching but is constantly scratching at his chest. He is oriented to person only and his brother at the bedside reports he hasn’t been himself today. He keeps trying to get out of bed
Which finding is most concerning and needs to be reported to the provider? Why?
- Confusion, disorientation – this could indicate hepatic encephalopathy, which could lead to seizures and death if left untreated
What further diagnostic and lab tests should be ordered to determine Mr. Garcia’s priority problems?
- Abdominal X-ray and/or Abdominal ultrasound to visualize liver and whether the distended abdomen is related to ascites or other sources
- Ammonia level to determine if hepatic encephalopathy is the source of Mr. Garcia’s altered mental status.
The provider places orders for the following:
Keep SpO 2 > 92%
Keep HOB > 30 degrees
Insert 2 large bore PIV’s
500 mL NS IV bolus STAT
100 mL/hr NS IV continuous infusion
Hydrocodone/Acetaminophen 5-500 mg 1-2 tabs q4h PRN moderate to severe pain
Diphenhydramine 25 mg PO q8h PRN itching
Ondansetron 4 mg IV q6h PRN nausea
Lactulose 20 mg PO q6h
Mr. Garcia’s LFT’s and Ammonia level are elevated. He is extremely confused and agitated and appears somewhat short of breath. The patient’s current vital signs are as follows:
HR 82 RR 22
BP 94/56 SpO 2 93%
Temp 98.9°F
Which order should be implemented first? Why?
- Insert two large-bore IV’s. The patient requires IV fluids and has other IV meds ordered and will likely need labs drawn. This needs to be a priority.
- You could also say elevate the HOB to 30 degrees or higher, if there was indication that he was lying flat
- His SpO2 is >92%, so no intervention is required there.
- Lactulose should be the next priority intervention – to get the ammonia levels down – but it may take a bit for pharmacy to profile it, send it to the unit, etc.
Which order should be questioned? Why?
- Hydrocodone/Acetaminophen – Acetaminophen can be toxic for patients with liver disease. The way this order is written, this patient could receive anywhere from 3 g – 6 g of Acetaminophen in a 24-hour period. The max for a healthy person is 4 g, but for liver patients, it is 2 g max.
- Either the dose and frequency should be lowered significantly, or the medication should be changed altogether
The order is changed to Fentanyl 25 mcg IV q4h PRN moderate to severe pain. The provider notes somewhat shallow breathing and severe ascites and requests for you to set up for paracentesis. At this time, you express your concern that the patient is extremely confused and agitated and trying to get out of bed. You do not feel that he will be still enough for the procedure. The provider agrees and plans to postpone the paracentesis for now, but orders for you to report any signs of respiratory depression or hypoxia.
Why is Mr. Garcia so confused and agitated?
- His ammonia levels are elevated due to his liver failure – this causes hepatic encephalopathy – damage to the brain cells
- This causes altered mental status, agitation, confusion, and can eventually lead to seizures and death if left untreated
What is the rationale for performing a paracentesis for Mr. Garcia?
- The excess fluid in Mr. Garcia’s belly is compressing his thoracic cavity, causing him to feel short of breath and to only take shallow breaths. Draining this fluid will not only relieve some discomfort, but it can also help improve Mr. Garcia’s breathing
After 6 doses of lactulose, Mr. Garcia is much more calm and cooperative. He is oriented times 2-3 most times. The provider performs the paracentesis and is able to remove 1.5 L of fluid. The patient’s shortness of breath is relieved, and his breathing is less shallow. Ultrasound of the liver showed severe scarring on the liver. Mr. Garcia’s condition continues to improve, and the plan is to discharge him home tomorrow.
What discharge teaching should be included for Mr. Garcia, including nutrition?
- Mr. Garcia should not be eating a high protein diet as this can contribute to the increased ammonia levels and development of hepatic encephalopathy.
- Mr. Garcia should avoid drinking alcohol at all times
- Medication instructions for any new or changed medications
- Especially the importance of taking Lactulose regularly as ordered
- Signs to report to the provider of exacerbation or encephalopathy
View the FULL Outline
When you start a FREE trial you gain access to the full outline as well as:
- SIMCLEX (NCLEX Simulator)
- 6,500+ Practice NCLEX Questions
- 2,000+ HD Videos
- 300+ Nursing Cheatsheets
“Would suggest to all nursing students . . . Guaranteed to ease the stress!”
Nursing Case Studies

This nursing case study course is designed to help nursing students build critical thinking. Each case study was written by experienced nurses with first hand knowledge of the “real-world” disease process. To help you increase your nursing clinical judgement (critical thinking), each unfolding nursing case study includes answers laid out by Blooms Taxonomy to help you see that you are progressing to clinical analysis.We encourage you to read the case study and really through the “critical thinking checks” as this is where the real learning occurs. If you get tripped up by a specific question, no worries, just dig into an associated lesson on the topic and reinforce your understanding. In the end, that is what nursing case studies are all about – growing in your clinical judgement.
Nursing Case Studies Introduction
Cardiac nursing case studies.
- 6 Questions
- 7 Questions
- 5 Questions
- 4 Questions
GI/GU Nursing Case Studies
- 2 Questions
- 8 Questions
Obstetrics Nursing Case Studies
Respiratory nursing case studies.
- 10 Questions
Pediatrics Nursing Case Studies
- 3 Questions
- 12 Questions
Neuro Nursing Case Studies
Mental health nursing case studies.
- 9 Questions
Metabolic/Endocrine Nursing Case Studies
Other nursing case studies.

Citation, DOI, disclosures and case data
At the time the case was submitted for publication Bruno Di Muzio had no recorded disclosures.
Presentation
Previous history of heavy alcoholism.
Patient Data
The liver echotexture appears coarse although the liver surface and hepatic vein walls remain smooth in appearance. There is biphasic flow demonstrated within the main portal vein suggestive of portal hypertension. No other features however of portal hypertension with no upper abdominal masses, flow within the ligamentum teres or splenomegaly. No ascites demonstrated. The hepatic veins were patent. No focal liver lesion. No abnormal biliary dilatation.
The gallbladder was collapsed down. Right upper pole renal cyst. No hydronephrosis bilaterally.
1 case question available
Q: Is the portal vein trace on Doppler normal? show answer
A: No, the flow, although predominantly antegrade, is pulsatile and has biphasic-bidirectional pattern.
Case Discussion
These ultrasound images demonstrate coarsened liver echotexture concerning for cirrhosis and signs of portal hypertension.
The portal vein shows a predominantly antegrade, pulsatile, and biphasic-bidirectional flow. Biphasic flows are commonly seen in patients with tricuspid regurgitation, right-heart cardiac failure, and cirrhosis. In this case, the normal appearances of the hepatic veins and the morphological features of cirrhosis make it the most likely cause for the abnormal portal vein flow.
The portal venous normal waveform should undulate smoothly and must always remain above the baseline.
Case courtesy of Dr Kenny Sim .
2 articles feature images from this case
- Pulsatile portal venous flow
22 public playlists include this case
- 3_114 Liver: Cirrhosis and NASH by RAB Three
- 334433 by Y Tan
- Liver Cases by Zin Min Htun
- UQ Med Yr 3 Hospital practice Orientation week by Craig Hacking ◉ ◈
- abdomen by MD IRFAN ALAM
- UQ Radiology video tutorial: Abdo: Cirrhosis, portal HTN and HCC by Craig Hacking ◉ ◈
- Liver - cirrhosis by Sonam Rosberger
- LIVER by sadrarhami
- Liver Malignant Liver tumor by Hamidou Kourouma
- Vascular ultrasound by Allister Howie
- Abdo - Adult Clinical Conditions - Hepatobiliary by Charlie Handley
- Vascular by Eugene Ng
- Abd Óm by Arnljótur Björn Halldórsson
- Certificate: 3_114 Liver: Cirrhosis and NASH by RAB Three
- Chest by Zin Min Htun
- GD: Hepatobiliary by Gurjeet Dulku
- GK - Abdo - Liver by GLK
- GIT-Liver 2 by Mohamed shweel
- SSS26 by Susheel K
- Hepato case by Nguyen Phu Dang
Promoted articles (advertising)
How to use cases.
You can use Radiopaedia cases in a variety of ways to help you learn and teach.
- Add cases to playlists
- Share cases with the diagnosis hidden
- Use images in presentations
- Use them in multiple choice question
Creating your own cases is easy.
- Case creation learning pathway
ADVERTISEMENT: Supporters see fewer/no ads
By Section:
- Artificial Intelligence
- Classifications
- Imaging Technology
- Interventional Radiology
- Radiography
- Central Nervous System
- Gastrointestinal
- Gynaecology
- Haematology
- Head & Neck
- Hepatobiliary
- Interventional
- Musculoskeletal
- Paediatrics
- Not Applicable
Radiopaedia.org
- Feature Sponsor
- Expert advisers


Liver Cirrhosis Case Study
56 year old Caucasian male with end-stage liver cirrhosis in hospice care, came in for stem cell therapy to help prolong his life. Patient had a history of chronic Hepatitis C, hypertension and diabetes, and did not qualify for liver transplant. Patient had declined steadily over the past year, and over the last month, he had an unintentional weight loss of 30 lbs. He had been struggling with fatigue, weakness, and occasional fever and chills, and also reported of shortness of breath, wheezing, and edema of lower extremities. At the time of treatment, patient presented with an distended abdomen (ascites), with very little energy to even speak.

Pin It on Pinterest
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

CASE STUDY OF PATIENT WITH LIVER CIRRHOSIS

Livercirrhosisisadiseaseinwhichnormaltissueofliverreplacedwithscartissue,livercirrhosisisthe12thleadingcauseofdeathsbydiseaseintheworld.Livercirrhosisiscausedbyanyfactorthatcandamagelivertissues,mostlyfattyliverandchronicliverdiseasesarethemajorcauseoflivercirrhosis. WearepresentingherethecaseofanAsianmanwhowasthevictimoflivercirrhosisthatwascomplicatedbyuntreatedhepatitisc.Hewasexperiencinggeneralizedbodyweakness,brownishtintintheurine,andsuddenweightgainof8-kgswithinaperiodofthreeweeks.Bloodpressurecountwas100/60,pulseratefoundtobe76beats/min,temperature98F,andenlargedumbilical.Laboratorytestsincludingcompletebloodcount,liverfunctiontests,andureatestscameouttobesignificantlyabnormal,complicatingthecase.,ultrasoundreportrevealedthathisliverwasenlarged,urinarybladderpartiallyfilled,umbilicalherniagapereported,ascitespresent(retentionoffluidintheabdomen),Cirrhosisandsplenomegalywerereported.Hisliverwasdamagedandliverfunctioningtestswerenotreturningtonormal,hepatologistrecommendedlivertransplantationasthelastresortforhim. Thereistheneedofgoodclinicalevaluationbyaqualifiedtherapistanduseofappropriateinvestigativestudiestosecurepatientfromsuchacriticalhealthhazard. Keywords:chronicliverdisease,livertransplantation,
Related Papers
Journal of Pharmaceutical Research International
Jaya Khandar
Liver is the second largest organ in human body, more than 5,000 separate bodily functions .including helping blood to clot, cleansing the blood of toxins to converting food into nutrients to control hormone levels, fighting infections and illness, regenerating back after injury and metabolizing cholesterol, glucose, iron and controlling their levels. A 56- years old patient was admitted in AVBRH on date 9/12/2020 in ICU with the chief complaint of abdominal distension, breathlessness on exertion, pedal edema, fever since 8 days. After admitted in hospital all investigation was done including blood test, ECG, fluid cytology, peripheral smear, ultrasonography, etc. All investigation conducted and then final diagnosis confirmed as cirrhosis of liver. Patient was not having any history of communicable disease or any hereditary disease but he has history of hypertension and type II Diabetes mellitus for 12 years. Patient was COVID-19 negative and admitted in intensive care unit. Patient...
The Journal of medical research
Amrendra Yadav
The liver is the multi-functional and vital organ of the body. It is found in the upper abdomen region of the vertebrates. Due to long-term damage, liver stops functioning properly which may lead to cirrhosis. This long-term damage occurred when scar tissue replaces the normal tissue of the liver. This disease develops slowly and has no early symptoms, but when it develops and become worse, then it leads to tiredness, itchiness, weakness, yellow skin, swelling in the lower legs, spider-like blood vessels and an easy bruise on the skin with fluid in the abdomen. The severe complications like bleeding dilated veins in esophagus or stomach, hepatic encephalopathy leading to confusion and unconsciousness and liver cancer may occur in the body. This review article is focusing on the effect of liver damage in the
Asian Australasian Neuro and Health Science Journal (AANHS-J)
Hanun Mahyuddin
Liver cirrhosis is a chronic disease characterized by the presence of fibrosis and regeneration of nodules in the liver, the consequence of which is the development of portal hypertension and liver failure. Usually associated with infectious infectious diseases such as viral hepatitis, alcohol consumption, metabolic syndrome, autoimmune processes, storage diseases, toxic substances and drugs. Major complications include gastrointestinal variceal bleeding, ascites, spontaneous bacterial peritonitis infection, hepatorenal syndrome, hepatic encephalopathy, and hepatocellular carcinoma. A 23-year-old woman comes to the ER, dr. Soegiri Lamongan with complaints of vomiting blood. The patient also complained of black bloody stools. Referred patient from Intan Medika Hospital with the initial complaint of vomiting blood more than 5 times (± equivalent to one medium drinking bottle) four days ago. On examination also found anemic conjunctiva and found splenomegaly. On abdominal ultrasound ex...
Fortune Journals , Umair Akram
Cirrhosis results from chronic liver disease, and is characterized by advanced fibrosis, scarring, and formation of regenerative nodules leading to architectural distortion. The main objective of the study is to find the cirrhosis and its complication, other clinical complications except ACLF and critical illness. This descriptive study was conducted at DHQ hospital, Vehari, Pakistan during June 2022 to January 2023. A comprehensive literature search of the published data was performed in regard with the spectrum, diagnosis, and management of cirrhosis and its complications. Data was also collected from OPD of the hospital record. We include all patients suffering from liver cirrhosis and its complication. It is concluded that patients with cirrhosis have progressive disease and suffer from multiple complications like ascites, HE, variceal bleeding, hepatorenal syndrome, cirrhotic cardiomyopathy, pulmonary syndromes, sarcopenia, frailty, and HCC. The prevention, early diagnosis, treatment, and palliation of these complications are essential in comprehensive clinical care plans.
The Egyptian Journal of Hospital Medicine
ibrahim al rajeh
Clinical Chemistry
Corinne Fantz
Clinical Transplantation
Cyrille Feray
Asian J Pharm Clin Res
Dr Bibhu Prasad Behera
Objective: Efforts can be made to normalize the hematological parameters so that the morbidity and mortality in these patients could be effectively reduced. Methods: This observational study was carried out among 69 cirrhosis patients that fulfills the inclusion and exclusion criteria, attended the medicine outpatient department, and admitted in medicine ward Results: In our study, we had 59 male and 10 female patients with an average age of 49.8±13.19 years. About 92.75% of the patients were alcoholic. Abdominal distension (92.75%) and ascites (84.06%) were the most common presenting complaints. Pallor was present in 42 (60.87%) cases. Splenomegaly was present in 35 (50.72%) cirrhotic patients. Renal dysfunction was present in 23 (33.33%) cases. Sixty-six (95.65%) patients had anemia and 47 (68.12%) patients had thrombocytopenia. Conclusions: From this study, we can conclude that, in cirrhosis of liver patients, various hematological changes are very common which need to be identified and corrected early to reduce morbidity and mortality.
Faridpur Medical College Journal
Shahin Ul Islam
Liver cirrhosis is an important cause of death and disability globally. This cross-sectional study was carried out in Faridpur Medical College Hospital from November 2018 to April 2019 to see the patterns of clinical presentations and associated factors among admitted liver cirrhosis patients. A total of 89 patients were included. Data were collected by detailed history from patients or their relatives followed by thorough physical examination as well as diagnostic evaluation; then those were checked, verified for consistency and edited for result. Among total respondents, the majority were male (69.7%) with a male to female ratio of 1:0.44. Age of patients ranged between 22-106 years with mean age of 52.33 year. The patients predominantly presented with ascites (49.4%), gastrointestinal bleeding (27%), peripheral edema (24.7%), and encephalopathy (21.3%). The in-hospital case fatality rate was 11.2% and the patients presented with decreased urinary output, peripheral edema and ence...
RELATED PAPERS
PabrikKulit PangsitDimsum
Global Journal of Pharmacology
Sharavana Bhava
European Journal of Organic Chemistry
Francesca Martina
Journal of the Korean Institute of Illuminating and Electrical Installation Engineers
Economia & Região
Érica de lima
Comunicação & Sociedade
Claudemir Bertuolo
Abdo mohamed
F. Abachi , Banan Aldewachi
Acta Materialia
Nobuhiro Tsuji
Ismael Possamai
Journal of Applied Pharmaceutical Science
Sheetal Chauhan
Call/WA :0856 0651 6159 | Jual Bunga Sedap Malam Palangkaraya
Agen Bunga Sedap Malam
Applied and Environmental Microbiology
Brent Christner
Water research
Mirjana Stojanovic
Tatiana Engel Gerhardt
San Diego Law Review
Jesus Silva
Indian Journal of Dental Advancements
shwetang goswami
Langenbeck's Archives of Surgery
Zeliha Sert
A.M. Rabasco-Alvarez
Journal of Geography in Higher Education
Kelly Dombroski
Sustainability
Marinko Stojkov
Proceedings of the 5th Universitas Ahmad Dahlan Public Health Conference (UPHEC 2019)
meiske koraag
Corrosion Science
Patrik Schmutz
Future Oncology
Ahmed Shelbaya
See More Documents Like This
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 18 March 2024
- Epidemiology
Routes to diagnosis for hepatocellular carcinoma patients: predictors and associations with treatment and mortality
- Anya Burton ORCID: orcid.org/0000-0002-4416-0538 1 , 2 ,
- Jennifer Wilburn 1 ,
- Robert J. Driver 3 ,
- David Wallace 4 , 5 ,
- Sean McPhail 1 ,
- Tim J. S. Cross ORCID: orcid.org/0000-0003-0625-8726 6 ,
- Ian A. Rowe ORCID: orcid.org/0000-0003-1288-0749 3 &
- Aileen Marshall 7
British Journal of Cancer ( 2024 ) Cite this article
246 Accesses
Metrics details
- Gastrointestinal cancer
Hepatocellular carcinoma (HCC) incidence has increased rapidly, and prognosis remains poor. We aimed to explore predictors of routes to diagnosis (RtD), and outcomes, in HCC cases.
HCC cases diagnosed 2006–2017 were identified from the National Cancer Registration Dataset and linked to Hospital Episode Statistics and the RtD metric. Multivariable logistic regression was used to explore associations between RtD, diagnosis year, 365-day mortality and receipt of potentially curative treatment.
23,555 HCC cases were identified; 36.1% via emergency presentation (EP), 30.2% GP referral (GP), 17.1% outpatient referral, 11.0% two-week wait and 4.6% other/unknown routes. Odds of 365-day mortality was >70% lower via GP or OP routes than EP, and odds of curative treatment 3–4 times higher. Further adjustment for cancer/cirrhosis stage attenuated the associations with curative treatment. People who were older, female, had alcohol-related liver disease, or were more deprived, were at increased risk of an EP. Over time, diagnoses via EP decreased, and via GP increased.
Conclusions
HCC RtD is an important predictor of outcomes. Continuing to reduce EP and increase GP and OP presentations, for example by identifying and regularly monitoring patients at higher risk of HCC, may improve stage at diagnosis and survival.
Similar content being viewed by others

An overview of clinical decision support systems: benefits, risks, and strategies for success
Reed T. Sutton, David Pincock, … Karen I. Kroeker

Deep whole-genome analysis of 494 hepatocellular carcinomas
Lei Chen, Chong Zhang, … Hongyang Wang

Hepatocellular carcinoma
Josep M. Llovet, Robin Kate Kelley, … Richard S. Finn
Introduction
Cancer survival in the UK is improving but remains poor compared to other European [ 1 ] and high income countries [ 2 ]. Improving cancer survival in the UK is a key challenge set out by the Department of Health, the NHS and the Independent Cancer Taskforce [ 3 , 4 , 5 ]. Survival rates vary greatly between cancers [ 1 ]. Primary liver cancer has a particularly poor prognosis compared to many other cancers [ 1 ]. Furthermore, incidence increased over three-fold for hepatocellular carcinoma (HCC), the most common form of liver cancer, between 1997 and 2017 [ 6 ]. HCC diagnosis is strongly associated with liver cirrhosis such that approximately 80% of patients with HCC also have liver cirrhosis. Early detection at a treatable stage improves cancer prognosis [ 7 ]. As such, 6-monthly liver ultrasounds for cancer detections are recommended for people at high risk of HCC [ 8 ].
The route a person takes to their diagnosis of cancer is strongly predictive of 1-year survival [ 9 ]. The Routes to Diagnosis (RtD) metric uses an algorithm to assess information about interactions with health care prior to a cancer diagnosis to assign each patient to a route [ 9 ]. Emergency presentations (via A&E, or emergency GP referral, transfer, consultant outpatient referral, admission or attendance) [ 9 ], have the poorest survival for the majority of cancers ( https://www.cancerdata.nhs.uk/routestodiagnosis/survival ). Conversely, in general, routine and urgent GP referral have the best prognosis. Overall, one in five cancers are diagnosed as an emergency; for HCC it is one in three. Understanding the differences in RtD presentations over time and predictors of RtDs can help us understand the survival gap and indicate ways to address it. Here we aim to explore, in HCC cases for the first time, (1) predictors of RtD, (2) differences in RtD presentations over time, (3) associations with mortality, and (4) associations with receipt of potentially curative treatment.
Registry data
Patient-level data on England residents diagnosed with HCC (defined as 10th edition of the International Classification of Diseases (ICD-10) code C22.0 and the second edition ICD Oncology (ICD-O) morphology code M8170) between 1st January 2006 and 31st December 2017 were extracted from the National Cancer Registration Dataset [ 10 ]. The Registration Dataset uses data from a wide range of sources including hospital activity records, multidisciplinary teams meetings, patient administration systems, pathology reports, molecular test reports and death certificates from the Office for National Statistics. It includes all cases of cancer diagnosed and treated in the National Health Service (NHS) in England (which funds 98–99% of all hospital activity [ 11 ]), as well as some treated privately [ 10 ]. A marker of registration quality is the proportion of cancers identified through death certification alone. In the English National Cancer Registration Database this is less than 1%, indicating that the vast majority of data relevant to a cancer diagnosis is being captured and the cancer registry has very high population completeness [ 10 ].
If a patient had two HCC tumours diagnosed during the study period, only the first tumour was included. Only patients aged 20 or over were included, due to rare aetiologies and subtypes of HCC in young people (47 aged <20 years excluded). HCC diagnoses were based on clinical investigations (imaging) in 60% of cases (as recommended for cirrhotic patients by EASL [ 12 ]), pathology in 35% of cases, and death certificate only or unknown in the remaining 5%. Data extracted included diagnosis date, death date, vital status (alive/dead/emigrated), date of last vital status (follow-up to 02/03/2020), age at diagnosis, gender, ethnicity (broad groups) and Charlson comorbidity score (categorical: no known comorbidities, 1, 2, 3 or more) and index of multiple (IMD) deprivation quintile (depending on year of diagnosis, income domains 2007, 2010, 2015, or 2019 as measured for each lower super output area (administrative areas of approximately 400–1200 households) was used, linked via patient postal address code at diagnosis [ 13 ]). Data on these variables was complete except for 3 people in which a Charlson score had not been derived.
Hospital episode statistics
These data were linked to the Hospital Episode Statistics Admitted Patient Care dataset (HES APC) [ 14 ]. HES data were used to identify cirrhosis status and underlying primary liver disease: cirrhosis status was defined as either compensated, decompensated, or none/unknown based on relevant diagnostic and therapeutic codes, as detailed in Driver et al. [ 15 ] and in the supplementary information. Underlying cause of primary liver disease (PLD) was assigned based on diagnostic codes recorded between five years before and one year after diagnosis. Including diagnostic codes up to one year after diagnosis showed improved PLD identification (supplementary information). The following hierarchy was applied based on relative risk of HCC associated with each PLD to give one primary PLD per patient [ 16 ]: hepatitis C (HCV) > hepatitis B (HBV) > primary biliary cirrhosis (PBC) > autoimmune hepatitis > haemochromatosis > alcohol-related liver disease (ALD) > non-alcoholic fatty liver disease (NAFLD). NAFLD was assigned when a patient had fatty (change of) liver, not elsewhere classified, or cirrhosis combined with obesity or diabetes, without any other PLD. Those with no relevant diagnostic codes were designated as ‘Other/unknown’.
Two sources were used to derive receipt of potentially curative treatment: HES APC records [ 14 ] and the Registration Dataset treatment data [ 10 ]. Treatments given from 60 days before diagnosis until death or 2 years (730 days) after diagnosis were included. Pre-diagnosis treatment was included as HCC may be diagnosed clinically and treated prior to the official registry date of incidence which may take histological tissue as the gold standard for diagnosis and reassign date of diagnosis once tissue is received [ 17 ]. The most definitive HCC treatment a patient received during this time was captured based on the following hierarchy of potentially curable treatments: liver transplant > liver resection > radiofrequency or microwave ablation > irreversible electroporation > percutaneous ethanol injection.
Route to diagnosis
Each HCC case was assigned a route to diagnosis (RtD). Details of methods used to identify and assign these are given in Elliss-Brookes et al. [ 9 ]. In brief, the algorithm interrogates cancer registration data linked to routine data from immediately prior to diagnosis (including HES, Cancer Wait Times, and NHS Screening programme data), and assigns a main RtD category: emergency presentation (EP), general practice (GP) referral, Two Week Wait (TWW, urgent GP referral with a suspicion of cancer), inpatient elective (IP), other outpatient (OP), death certification only (DCO, no data available other than a death certificate flagged by the registry) and Unknown. The methodology was developed using data for all patients with newly diagnosed malignant cancer registered in the English National Cancer Registration system between 2006 and 2008 (739,667 tumours). Since then, the metric has been derived yearly for all cancer new registrations and forms part of the cancer registration dataset.
Patient and public involvement statement
No patients were involved in forming the research question or selecting the outcome measures, nor were they involved in developing the study design. No patients were asked to advise on interpretation or writing up of results. Results will be shared through patient charities, regionally and nationally, including the British Liver Trust and on the NDRS and British Association for the Study of the Liver websites.
Statistical methods
Descriptive.
The distribution of demographic and clinical factors in cases by RtD were described using means and standard deviation (for normally distributed continuous data), medians and IQRs (skewed continuous data) and absolute numbers and percentages (categorical data).
Associations with RtD and differences over time
Associations of the four main HCC routes to diagnosis (EP, OP, TWW and GP) with demographic and clinical variables (year of diagnosis, age, person stated gender, area-based deprivation quintile, ethnicity, Charlson comorbidity score, cirrhosis stage, PLD) were examined using multivariable logistic regression models. Unknown, DCO and IP were not examined due to smaller numbers. Proportions presenting via each route by year of diagnosis, unadjusted, demographic-adjusted (age, gender, ethnicity and deprivation quintile) and fully-adjusted (demographic variables and Charlson comorbidity score, cirrhosis stage, primary liver disease) were calculated.
Association with curative treatment
Associations of RtD with receipt of potentially curative treatment, unadjusted, and adjusted for multiple factors (age, gender, diagnosis year, deprivation quintile, ethnicity, Charlson comorbidity score, cirrhosis stage, and PLD) were assessed using logistic regression to calculate odds ratios (ORs). Those with DCO as the RtD were excluded from these analyses as none received curative treatment ( n = 92). Sensitivity analyses were conducted excluding those that died within 90 days of diagnosis, adjusted for TNM stage (not included in the main model as stage was only available for 27% of cases), and stratified by cirrhosis status, age (< or ≥65years), and PLD.
Those with vital status uncertainty due to discrepancies with recorded date of death (date of death before date of diagnosis ( n = 9), date of death before date of treatment ( n = 15), patient traced alive after date of death ( n = 11)) and those lost to follow up (i.e. emigrated ( n = 50), or with missing vital status ( n = 5), were excluded. Those with DCO as the RtD were also excluded ( n = 92) as there was no variation in survival in this group (date of death and date of diagnosis were the same). This left 23,373 individuals for mortality analysis. Univariable and multivariable logistic regression (adjusted for age, gender, diagnosis year, deprivation quintile, ethnicity, Charlson comorbidity score, cirrhosis status, and PLD) were used to calculate odds of 90-day and 365-day (one-year) mortality from diagnosis date, by RtD. Sensitivity analyses were conducted adjusting for TNM stage, and additionally for receipt of curative treatment, and stratified by cirrhosis status, age (< or ≥ 65years), and PLD.
Model assumptions were checked and met for all analyses performed. Analyses were conducted using Stata version 17.1 StataCorp. 2017. Stata Statistical Software: Release 17 . College Station, TX: StataCorp LLC.
Overall, in England 23,555 HCCs were diagnosed between 2006 and 2017. 36.1% of these presented via an emergency route, 30.2% via GP referral, 17.1% via Outpatient referral and 11.0% via Two Week Wait, 1.3% Inpatient Elective, 0.4% DCO and 3.9% had no data available (‘Unknown’ route) (Table 1 ).
Patient characteristics and routes to diagnosis
The characteristics of cases varied by RtD (Table 1 ). People presenting via IP and OP were younger at diagnosis on average (66.0 and 66.4 years, respectively), and TWW and EP (71.9 and 70.2 years, respectively) older. After adjustment for other characteristics (Table 2 ), the odds of EP and TWW were higher for patients with older age at diagnosis and the odds of GP referral and OP lower. 78.1% of HCC cases were in men, and the proportion varied by RtD. After adjustment, the odds of an EP compared to any other route were 24% higher in women, and of a GP or TWW presentation 11 and 17% lower, respectively. Area-based deprivation was strongly associated with RtD; over 27% of EPs were in people in the most deprived quintile of the population and only 13.8% in the least deprived. A similar pattern was seen for GP and OP presentations, but not for TWW and IP presentations. After adjustment for other characteristics, odds of an EP presentation were 45% higher for those in the most deprived quintile compared to the least. In contrast, odds of OP presentation were 25% lower. The ethnicities of those diagnosed via EP, GP and OP were broadly similar, but a higher proportion of those diagnosed via TWW were white (87.2%), and for those diagnosed via IP a lower proportion were white (77.5%) and a higher proportion (6.7%) black. Ethnicity data was missing for a large proportion of DCOs (57%). After adjustment, there was no strong associations of ethnicity with EP, but odds of GP referral or TWW were highest for white people, and odds of OP were highest for Asian and other ethnicities.
Underlying PLD could be established from HES records in 13,777 (58.5%) cases. The remaining 41.5% either had one of the forms of PLD on our list but no record of a corresponding HES code for it, had a different PLD, or had no PLD. Overall, ALD (20.7% of cases) was the most common PLD, followed by NAFLD (15.1%) and then HCV (13.2%) and this varied by RtD. The odds of an EP presentation were highest for those with ALD compared to other PLDs, after adjustment for other characteristics. In comparison, the odds of a GP referral was higher for PLDs other than ALD. More people presenting via OP had a known PLD than those presenting via other routes. People with AIH, PBC, haemochromatosis, and viral hepatitis were more likely to have an OP presentation than those with ALD, or NAFLD. The odds of TWW presentation was highest in those with NAFLD and with no/unknown PLD.
41.7% of cases had no co-morbidity codes recorded in HES and 29.7% had a score of three or more. Those presenting via TWW or IP had fewest recorded comorbidities (57.2% and 55.9% had none, respectively) and those presenting via OP the most (52.0% had a score of two or more). After adjustment, those with known comorbidities were less likely to present via TWW (OR 0.32 [95%CI 0.28–0.36] in those with a score of ≥3 comorbidities compared to those with no recorded comorbidities), and more likely to present via OP (OR 2.08 [95%CI 1.90–2.28] for ≥3). The highest proportion of patients with decompensated cirrhosis was seen in those presenting via EP (accounting for 39.1% of all EPs). After adjustment, those with decompensated cirrhosis were over 4 times more likely to present via EP than those with compensated cirrhosis (OR 4.21 [95%CI 3.91–4.54]). TWW presentations were less likely to have any recorded cirrhosis. TNM stage was only available for 27.3% of cases. The stage distribution was more favourable in those presenting via GP or OP and least favourable for those presenting via EP.
Routes to diagnosis over time
The proportion presenting via EP reduced between 2006 and 2017 from 42.2% to 31.5% of all cases, and the proportion presenting via GP referral and TWW increased (24.9% to 30.7% and 6.9% to 15.2%, respectively). There was no significant change in the proportion presenting via OP (16.4% to 15.2%). These patterns remained after adjustment for demographic and, additionally, for clinical characteristics of patients (Fig. 1 ).
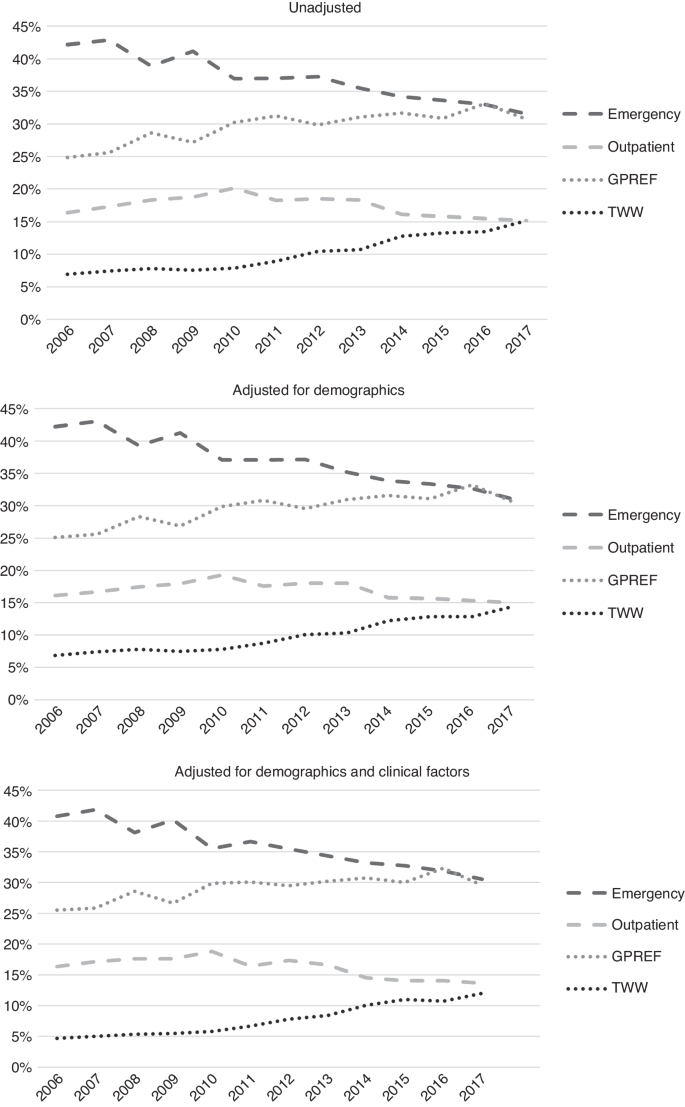
Upper graph: unadjusted. Middle graph: adjusted for demographics. Lower graph: adjusted for demographic and clinical factors.
Associations with mortality
20,671 (87.8%) HCC cases had died by the end of follow-up; median survival was 194 days overall (Table 1 ). Median survival ranged widely from 55 days for diagnoses via EP, to over 400 days for GP and OP (Fig. 2 ). Unadjusted, compared to EPs, those presenting via OP or GP referral had the lowest odds of mortality at 365 days (Table 3 ). In fully adjusted models, associations were only slightly attenuated and those presenting via OP or GP referral continued to have the lowest odds of mortality (OR 0.23 and 0.26, respectively) compared to EP. IP or TWW had intermediate odds (OR 0.37 and 0.42, respectively). In those with stage information, additional adjustment for TNM stage accounted for some of the variation in odds of mortality by RtD and further adjustment for receipt of potentially curative treatment attenuated associations further, but odds of death by 365 days post-diagnosis remained highest for EPs compared to other RtDs.
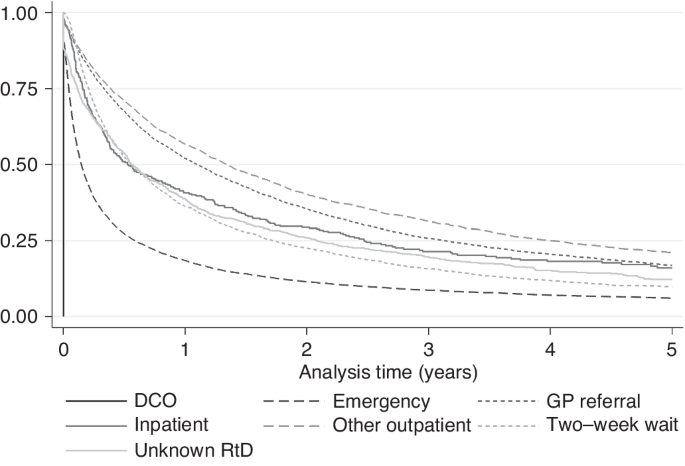
Kaplan–Meier 5-year survival by route to diagnosis.
In the sensitivity analyses (Table 3 ), for people with decompensated cirrhosis, odds of mortality by 365 days were similar for those diagnosed via TWW and EP, and lowest for GP and OP. Odds of 365-day mortality were highest for EPs irrespective of the underlying cause of PLD, although odds were also high for presentations via TWW for people with haemochromatosis and HCV. For those with AIH, PBC or NAFLD, the lowest odds of 365-day mortality were diagnoses via IP or Unknown RtDs, followed by GP and OP. Analyses were repeated with 90-day mortality as the outcome to assess if associations were different for short term mortality (Supplementary Information 5 ). Associations were broadly similar.
Associations of RtD with curative treatment
20.5% of cases received potentially curative treatment overall, which also varied widely by RtD (Table 1 ); from 9.0% for EP to 35.8% for OP. Unadjusted, compared to EP, the odds of curative treatment were almost six times higher for OP (OR 5.94), four times higher for GP and IP (ORs 3.90 and 3.86, respectively) and two times higher for TWW (OR 1.91), and Unknown RtD (OR 1.92) (Table 4 ). In the fully adjusted model, these associations remained but were slightly attenuated (for example, OR for OP was 4.16 compared to EP). In sensitivity analyses, variations in associations were seen. Excluding those that died in the first 90 days after diagnosis attenuated associations substantially, though odds of curative treatment were still 1.8 to 2.3 times higher for presentations via OP, IP, and GP compared to EP. The same attenuation pattern was also seen following additional adjustment for TNM stage. When stratified by cirrhosis stage, large differences in odds of curative treatment by RtD were seen for those with no known cirrhosis (OR range 6.05 for OP to 1.0 for EP (referent)), and compensated cirrhosis (OR range 4.41 for OP to 1.0 for EP). For those with decompensated cirrhosis, odds were highest in those that presented via OP (OR 3.05) and GP (OR 2.20), but those that presented via TWW, IP or unknown RtD all had similar odds to those presenting via EP. Some differences in range of associations were also seen by PLD. For those with haemochromatosis or HBV, odds of curative treatment in those presenting via OP were over six times that of those presenting via EP. For those with NAFLD, odds of curative treatment were 4–5 times higher in those presenting via IP, OP, or GP referral than via EP. For those with other/unknown/no PLD, odds were much higher for OP (OR 6.01) and GP (OR 4.60), compared to EP. An effect modification by age was also seen; those aged over 65 were over five times more likely to receive curative treatment if presentation was via OP than EP, whereas those under 65 were three times more likely.
Route to diagnosis is strongly associated with odds of 90-day and 365-day mortality and inversely associated with receipt of potentially curative treatment in patients diagnosed with HCC. Patients presenting via EP had the poorest prognosis; <10% received curative treatment and median survival was just 55 days. In comparison, of those presenting via OP, over a third received curative treatment, and median survival was nearly10 times higher than for EP diagnoses. After adjustment for demographic and clinical factors, odds of mortality by 365 days was substantially lower for those presenting via GP or OP routes compared to EP, and odds of curative treatment substantially higher. The differences in rates of potentially curative treatment by RtD were influenced by differences in patient age at diagnosis, PLD, cancer and cirrhosis stage at presentation, and early death. Vulnerable patients including older people, women, those with alcohol-related liver disease, and people residing in more deprived areas, were at increased risk of an EP. Fortunately, the proportion of HCC patients presenting as emergencies is decreasing, and those presenting via GP referrals increasing.
Strengths and limitations
This study used a population-based dataset including the vast majority of HCC cases diagnosed and treated in England. The results are therefore representative of and generalisable to the population. 12 years of data were included which allowed examination of differences over time. The sample size was large ( n = 23,555), despite liver cancer being classified as a rare cancer. RtD is a well-established metric derived from linked routinely-collected population-based datasets. We were able to examine associations of RtD with a wide range of factors known to cause variation in mortality available within and derived from the high-quality National Cancer Registration Dataset. We present a novel method for identification of primary liver cancer from HES codes, validated by comparison with PLD from clinical records.
There are limitations. As data was not collected specifically for the purpose of this study, in common with other observation studies based on routine data, some variables that would have been informative were not available in the dataset. In particular, Barcelona liver cancer stage or variables to derive this (TNM stage, Child-Pugh liver function and ECOG performance status) were not available for the majority of cases. Some important liver cancer risk factors such as BMI, smoking and alcohol consumption, or indicators of liver function, were not available. In our study, underlying cause of primary liver cancer, comorbidity score, and cirrhosis stage were inferred from HES codes, which are dependent on hospital admissions and accurate coding practices. PLD and cirrhosis status were not derivable for around 40% of patients, and it was not possible to know if this was true absence of a PLD or just absence of a code. Furthermore, we used data to identify underlying PLD both before and after the diagnosis of HCC. This was done to improve classification recognising that this is an understudied area, but there is the risk of bias through differential misclassification by RtD. Liver surveillance status was unknown. The deprivation measure used was based on area of residence, therefore there may be residual confounding by socioeconomic status. There were insufficient numbers of inpatient presentations to assess associations with this RtD metric. In addition, we were unable to use cause of death to identify cancer-related death due to the propensity to assign deaths in people with HCC as cancer-related although many would have been due to complications of cirrhosis (77% of deaths were attributed to C220 in our cohort).
Comparison with other literature
For all cancers diagnosed 2011 to 2015 combined, screening followed by TWW and then GP referral had the best 12-month net survival, but for liver cancer the other outpatient route had the best survival [ 18 ]. (Note no liver cancers were diagnosed via the screening route as there is not yet a national liver cancer screening programme, although surveillance of at-risk groups is advised). Similar to our study, excess early mortality (the three months after diagnosis) in emergency presentations has previously been reported for colorectal, cervical, breast, lung, and prostate, even after adjustment for age, stage and comorbidity [ 19 ]. A reduction in emergency presentations across all cancers from 2006–2013 was previously reported, of which only one-fifth was explained by change in case mix (age, gender, deprivation and cancer site) [ 20 ]. Our results show change in case-mix had very little influence on these RtD differences over time in those with liver cancer. Similar to our findings for liver cancer, Tataru et al. [ 21 ] found that patients with lung cancer were much less likely to receive surgery if they presented as an emergency. Markar et al. [ 22 ] found that oesophageal and gastric cancer patients that had an emergency diagnosis had poorer prognosis after surgery. Both of these studies, and another large study, including liver cancer, reported female gender, increased age, and higher deprivation to be risk factors for emergency presentations [ 21 , 22 , 23 ].
Interpretation
In order to improve cancer survival in England, the Independent Cancer Taskforce has identified early diagnosis as key [ 4 ]. The high rate of EPs in those with decompensated cirrhosis likely reflects the development of significant symptoms requiring admission (e.g. variceal bleeding/ ascites). The HCC may be diagnosed as part of the investigation of those symptoms. For liver cancer, identifying at-risk patients (i.e. those with asymptomatic compensated cirrhosis or chronic hepatitis B) and closely monitoring them may reduce the number of emergency presentations and improve early diagnosis. Those diagnosed via outpatient routes were most likely to survive for one year after diagnosis and receive potentially curative treatments. People with viral or autoimmune hepatitis, or multimorbidity, were more likely to be diagnosed via OP. These patients would likely have received regular specialist medical care for their chronic liver conditions, which may have led to earlier cancer detection. Similar to OP, patients presenting via GP referral may be interacting regularly with healthcare, thus their more favourable cancer and cirrhosis stage profile at diagnosis. We were unable to assess the impact of surveillance, but 6-monthly liver ultrasounds, with or without serum alpha-fetoprotein testing, have been shown to improve early detection, receipt of curative treatment and survival [ 7 ] and is therefore recommended for people with cirrhosis [ 8 ]. Patients with known cirrhosis undergoing liver surveillance would be most likely to be categorised as OP presentations. Early detection of HCC in patients with NAFLD, the most rapidly increasing cause of HCC [ 24 ], via ultrasound can be challenging [ 25 ]. There is also the challenge of educating patients and clinicians to identify signs and symptoms of HCC, and to increase referrals for diagnostic investigation. A small study in Scotland of GP interactions prior to a cancer diagnosis found not having seen a GP was a strong risk factor of an EP, though 18% of EPs in upper GI cancer cases were missed opportunities (GPs had not adhered to referral guidelines for suspected cancers) [ 26 ]. Of these, over 70% had seen their GP 6 times or more time in the 24 months preceding a diagnosis. A similar proportion occurred while patients were waiting for secondary care appointments.
Rates of liver cancer have been rapidly increasing in the UK and survival is still poor, making liver cancer one of the most rapidly increasing causes of cancer-related death in the UK. Identifying factors associated with treatment and mortality can help identify areas to target to improve early diagnosis and survival. Liver cancer patients are most likely to present via the emergency route to diagnosis, which is strongly associated with higher mortality in the first year after diagnosis and reduced odds of curative treatment, even after adjustment for early mortality and prognostic factors. There was inequality among the cases, where older patients, women and those from more deprived areas are most likely to present as emergencies. The trend toward decreasing emergency presentations and increasing GP referrals needs to continue. Ensuring patients at higher risk of HCC, including those with high BMIs, are identified and regularly monitored, and that both patients and health care professionals are aware of liver cancer risk factors and symptoms, may help increase diagnoses at a curable stage.
Data availability
Access to cancer registration data through NHS England can be granted provided there is a justified purpose for the data release, and that there is an appropriate legal basis with safeguards in place to protect the data. Dependent on the request, ethical approval may be required. The access process is managed by the Data Access Request Service.
De Angelis R, Sant M, Coleman MP, Francisci S, Baili P, Pierannunzio D, et al. Cancer survival in Europe 1999-2007 by country and age: results of EUROCARE–5-a population-based study. Lancet Oncol. 2014;15:23–34.
Article PubMed Google Scholar
Arnold M, Rutherford MJ, Bardot A, Ferlay J, Andersson TM, Myklebust TA, et al. Progress in cancer survival, mortality, and incidence in seven high-income countries 1995-2014 (ICBP SURVMARK-2): a population-based study. Lancet Oncol. 2019;20:1493–1505.
Article PubMed PubMed Central Google Scholar
Department of Health. Improving Outcomes: A Strategy for Cancer. London, England, 2011. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/213785/dh_123394.pdf .
NHS England. Achieving World-Class Cancer Outcomes: A Strategy for England 2015-2020. 2015. https://www.england.nhs.uk/wp-content/uploads/2016/10/cancer-one-year-on.pdf .
The NHS Long Term Plan. 2019. https://www.longtermplan.nhs.uk/wp-content/uploads/2019/08/nhs-long-term-plan-version-1.2.pdf .
Burton A, Tataru D, Driver RJ, Bird TG, Huws D, Wallace D, et al. Primary liver cancer in the UK: Incidence, incidence-based mortality and survival by subtype, sex and nation. JHEP Reports. 2021. https://doi.org/10.1016/j.jhepr.2021.100232 .
Singal AG, Pillai A, Tiro J. Early detection, curative treatment, and survival rates for hepatocellular carcinoma surveillance in patients with cirrhosis: a meta-analysis. PLoS Med. 2014;11:e1001624.
National Institute for Health and Care Excellence. Quality statement 4: Surveillance for hepatocellular carcinoma. Liver Disease. 2017. https://www.nice.org.uk/guidance/qs152 .
Elliss-Brookes L, McPhail S, Ives A, Greenslade M, Shelton J, Hiom S, et al. Routes to diagnosis for cancer - determining the patient journey using multiple routine data sets. Br J Cancer. 2012;107:1220–6.
Article CAS PubMed PubMed Central Google Scholar
Henson KE, Elliss-Brookes L, Coupland VH, Payne E, Vernon S, Rous B. et al. Data Resource Profile: National Cancer Registration Dataset in England. Int J Epidemiol. 2019. https://doi.org/10.1093/ije/dyz076 .
National Audit Office. Healthcare Across the UK: A Comparison of the NHS in England, Scotland, Wales and Northern Ireland. 2012. https://www.nao.org.uk/wp-content/uploads/2012/06/1213192.pdf .
European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J Hepatol. 2018;69:182–236.
Article Google Scholar
McLennan D, Barnes H, Noble M, Davies J, Garratt E. The English Indices of Deprivation 2010. Department for Communities and Local Government; London. 2011.
Herbert A, Wijlaars L, Zylbersztejn A, Cromwell D, Hardelid P. Data Resource Profile: Hospital Episode Statistics Admitted Patient Care (HES APC). Int J Epidemiol. 2017;46:1093–1093i.
Driver RJ, Balachandrakumar V, Burton A, Shearer J, Downing A, Cross T, et al. Validation of an algorithm using inpatient electronic health records to determine the presence and severity of cirrhosis in patients with hepatocellular carcinoma in England: an observational study. BMJ Open. 2019;9:e028571.
Roberts MS, Angus DC, Bryce CL, Valenta Z, Weissfeld L. Survival after liver transplantation in the United States: a disease-specific analysis of the UNOS database. Liver Transpl. 2004;10:886–97.
Tyczynski JE, Parkin DM. Standards and guidelines for cancer registration in Europe. IARC Tech Publ. 2003;40:69–73.
Google Scholar
National Disease Registration Service, NHS England. Survival by Cancer Site and Diagnostic Route. Accessed 2022. https://www.cancerdata.nhs.uk/routestodiagnosis .
McPhail S, Elliss-Brookes L, Shelton J, Ives A, Greenslade M, Vernon S, et al. Emergency presentation of cancer and short-term mortality. Br J Cancer. 2013;109:2027–34.
Herbert A, Winters S, McPhail S, Elliss-Brookes L, Lyratzopoulos G, Abel GA. Population trends in emergency cancer diagnoses: The role of changing patient case-mix. Cancer Epidemiol. 2019;63:101574.
Tataru D, Jack RH, Lind MJ, Moller H, Luchtenborg M. The effect of emergency presentation on surgery and survival in lung cancer patients in England, 2006-2008. Cancer Epidemiol. 2015;39:612–6.
Markar SR, Mackenzie H, Jemal S, Faiz O, Cunningham D, Hanna GB. Emergency Presentation of Esophagogastric Cancer: Predictors and Long-term Prognosis. Ann Surg. 2018;267:711–5.
Abel GA, Shelton J, Johnson S, Elliss-Brookes L, Lyratzopoulos G. Cancer-specific variation in emergency presentation by sex, age and deprivation across 27 common and rarer cancers. Br J Cancer. 2015;112:S129–136.
Huang DQ, El-Serag HB, Loomba R. Global epidemiology of NAFLD-related HCC: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2021;18:223–38.
laz Torres MC, Bodini G, Furnari M, Marabotto E, Zentilin P, Strazzabosco M, et al. Surveillance for Hepatocellular Carcinoma in Patients with Non-Alcoholic Fatty Liver Disease: Universal or Selective? Cancers. 2020;12:1422.
Murchie P, Smith SM, Yule MS, Adam R, Turner ME, Lee AJ, et al. Does emergency presentation of cancer represent poor performance in primary care? Insights from a novel analysis of linked primary and secondary care data. Br J Cancer. 2017;116:1148–58.
Download references
Acknowledgements
This manuscript forms part of the body of work of the HCC-UK BASL/NDRS Partnership. Steering group: Anya Burton, Aileen Marshall, Graeme Alexander, Ian Rowe, Robert J Driver, Vinay Kumar Balachandrakumar, Tim Cross, Katherine Cullen, Tom Bird, Dyfed W Huws, Anna Gavin, Daniela Tataru, Lizz Paley, David Wallace. This work uses data that has been provided by patients and collected by the NHS as part of their care and support. The data are collated, maintained and quality assured by the National Disease Registration Service, which is part of NHS England. The authors would like to thank Peter Jones and Hanhua Liu at NDRS for the help with quality assurance of the analyses.
This work was supported by the British Association for the Study of the Liver who received an unrestricted and unconditional award from BTG International Ltd. BTG had no input into the study design, data collection, analysis or interpretation of the data, writing of the manuscript, review of the manuscript, the decision to submit the manuscript or the writing of this statement.
Author information
Authors and affiliations.
National Disease Registration Service, NHS England, Quarry House, Quarry Hill, Leeds, LS2 7UE, UK
Anya Burton, Jennifer Wilburn & Sean McPhail
Bristol Medical School, Canynge Hall, 39 Whatley Road, Bristol, BS8 2PS, UK
Anya Burton
Leeds Institute for Medical Research at St. James’s, University of Leeds, Leeds, LS9 7TF, UK
Robert J. Driver & Ian A. Rowe
Department of Health Services Research & Policy, London School of Hygiene & Tropical Medicine, 15-17 Tavistock Place, London, WC1H 9SH, UK
David Wallace
Institute of Liver Studies, Kings College Hospital, Denmark Hill, London, SE5 9RS, UK
Liverpool Experimental Cancer Medicine Centre, University of Liverpool, Liverpool, L7 8XP, UK
Tim J. S. Cross
Sheila Sherlock Liver Centre, The Royal Free Hospital, London, NW3 2QG, UK
Aileen Marshall
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the development of the study design, interpretation of the results and critical revision of the manuscript. AB extracted the data, RD conducted the primary liver disease validation work, JW and AB performed the data analyses, and AB drafted the manuscript. All authors read and approved the final submitted version of the manuscript.
Corresponding author
Correspondence to Anya Burton .
Ethics declarations
Competing interests.
All of the authors completed the ICMJE uniform disclosure form; AB declares this work was supported by BTG International Ltd. AM is the chair of HCC UK. TJSC is President elect of the British Association for the Study of the Liver, has shares in AstraZeneca, has given talks for Roche, AstraZeneca, received financial support for educational events from Boston Scientific and Sirtex, works for Roche pharmaceuticals on HCC patient pathways and use of surveillance for HCC, and Roche paid for TJSC’ 2022 attendance at ASCO. IAR reports personal fees from Roche, as well as personal fees from Boehringer Ingelheim outside the submitted work. The other authors declare no competing interests.
Ethics approval and consent to participate
This study was conducted under a special legal instruction to collect patient data without needing informed consent, as part of NHS England. This instruction is granted under section 254 of the Health and Social Care Act 2012.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Burton, A., Wilburn, J., Driver, R.J. et al. Routes to diagnosis for hepatocellular carcinoma patients: predictors and associations with treatment and mortality. Br J Cancer (2024). https://doi.org/10.1038/s41416-024-02645-3
Download citation
Received : 22 June 2023
Revised : 22 February 2024
Accepted : 26 February 2024
Published : 18 March 2024
DOI : https://doi.org/10.1038/s41416-024-02645-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
'That pushed them over the edge': Post pandemic alcohol-related liver disease rises in Arizona
Heather Hann’s skin and eyes started to turn yellow around the time she turned 32. She knew exactly what it was. For the 13 years prior, she was an alcoholic.
“I look like the Simpsons now,” she told Sheila Gallaway, her older sister by almost two years. When her jaundice, a common symptom of liver damage, became too glaring, Heather hid from friends and stopped going to family events. But her drinking did not stop.
“She no longer drank water at some point,” Sheila said. “Heather drank just vodka.”
By 2022, Heather was 35 and looked unrecognizable. Her skin changed from yellowish to grayish and a picture of her urine she sent to Sheila showed it was almost black. She vomited constantly. According to doctors, Heather’s liver was severely scarred.
But still, she could not give up drinking. Sheila said she had simply given up. She believes her sister’s drinking had increased during the 2020 COVID-19 restrictions and worsened her liver problem.
“That was when her skin turned yellow,” she said. “It was that way till 2022 when it got worse.”
Arizona residents drank more than normal in 2020 as COVID-19 lockdowns forced people to stay indoors and working from home became a new normal. But only a few years later, the effect of that drinking is manifesting in high hospitalization rates for liver diseases, especially alcoholic cirrhosis, an Arizona Republic analysis of the state’s hospitalization records shows.
On the morning of May 24, 2022, Sheila received a panicked call that Heather was unresponsive.
Sheila lived just four blocks away. She jumped in her car and sped past a fire department’s ambulance heading to the house in central Phoenix. She arrived to find her mother, who lived with Heather, performing CPR. Sheila took over before the first responders arrived. But Heather would never wake up.
"I knew she had been gone for a while when I took over the CPR," Sheila said.
She had succumbed to alcoholic cirrhosis, a permanent and severe scarring of the liver from chronic alcohol use.
What The Republic found in hospital records
Chronic liver disease or cirrhosis is Arizona’s ninth leading cause of death, according to the Arizona Department of Health Services , but the post-2020 trajectory of the disease is stark.
The Republic analyzed over 5 million hospitalization records from 2016 to 2022 with a focus on diseases that landed people in the hospital.
Across almost all common diseases, hospitalization rates dipped in 2020 due to COVID-19 restrictions. By 2022, hospitalization rates for these diseases — such as stroke, heart disease, diabetes, hypertension and cancer — were either back to pre-COVID, 2019 levels or slightly below them.
However, the numbers moved in a different direction for alcoholic liver disease, especially alcoholic cirrhosis. The hospitalization rate for alcoholic liver disease increased by 5% in 2020 over the previous year. For alcoholic cirrhosis, the increase was 9%.
By 2022, the rate of alcoholic liver disease had increased by 23% over pre-pandemic levels. Hospitalizations for alcoholic cirrhosis shot up 42%.
In contrast, the hospitalization rate for non-alcoholic liver diseases plummeted during the pandemic like the other chronic diseases and has not risen above 2019 levels. Those liver diseases also can be lethal.
The spike in hospitalization rate for alcoholic liver disease — which consists of alcoholic cirrhosis, alcoholic hepatitis and alcoholic fatty liver — is a nationwide trend.
The per capita consumption of alcohol increased during the pandemic more than any time since 1968, according to Dr. Aaron White, the head of the epidemiology and biometry branch at the National Institute on Alcohol Abuse and Alcoholism.
“All of that extra alcohol resulted in extra harm, particularly for people with a history of heavy alcohol use and alcohol use disorder,” he told The Republic.
Deaths from alcohol-related liver disease increased across the country by more than 22% in 2020 over the previous year, according to White.
Arizona ranked 12th nationwide for the death rate for alcohol-related liver diseases in 2019. Two years later, the state was in eighth place at 15.5 age-adjusted deaths per 100,000 people.
Legacy of pandemic drinking is manifesting
One study on alcohol dependency during COVID-19 lockdowns led by William Killgore, a professor of psychiatry at the University of Arizona, found “dramatic increases in harmful alcohol consumption observed over the first six months of the COVID-19 pandemic.”
There are “grave concerns” for the health implications of this, like liver disease, the study said.
The Liver Institute in Tucson, for instance, is seeing this firsthand, according to Dr. Shahid Habib, its medical director.
Alcohol liver disease and fatty liver disease make up the majority of cases the facility is seeing as the volume of cases increased, he said.
Killgore agrees the increase in alcoholic liver diseases is likely related to the rate of alcohol consumption during the pandemic, but he said he could not give a more definitive response as he had not studied the link.
While the pandemic was a tipping point for many people who had chronic liver disease, the damage would likely have started long before 2020, experts told The Republic. The increased consumption during the pandemic put too much pressure on their already damaged livers, they said.
Someone "drinks alcohol every day, like six or seven beers for 20 years, then, all of a sudden during the pandemic, they doubled that. That pushed them over the edge,” said Dr. Frank LoVecchio, the medical director of clinical research at Arizona State University’s College of Health Solutions.
Journey to liver damage for one Phoenix woman
Heather’s autopsy report simply states that she died from complications of chronic ethyl (ETOH) use, a medical term for alcohol use.
Shelia blames Heather's alcoholism on a troubled, long-term relationship. Heather told family members that her boyfriend wouldn't let her seek rehab.
Sheila said Heather was her best friend. Sheila remembers a fun-filled childhood, goofing off with her sister and riding colorful bikes around their Maryvale neighborhood with friends. In their adolescence, they drank normally and nothing beyond what their peers drank, Sheila said.
Heather was a dreamer. She would talk about owning a beautiful house of her own, visiting the beach often and traveling.
Then in high school, she met her boyfriend, with whom she would share an apartment for about 17 years. Heather loved to teach. She became a substitute teacher.
When she became sick from drinking, Sheila would take her to the hospital.
Heather eventually ended her relationship with her boyfriend in November 2021. By that time, she'd already had the jaundice that signaled her advanced liver disease for nearly two years. Then she spiraled.
After she was diagnosed with alcoholic cirrhosis, she was in and out of the hospital in the last months of her life.
According to the Mayo Clinic, alcoholic cirrhosis occurs because the liver repairs itself each time it is injured through excessive drinking or infection. Each time, scar tissues form.
Despite the hospital visits and the dire prognosis of her disease, Heather would not stop drinking. A liver transplant wasn't on the table — she was too far gone for that, Sheila said.
"Heather simply stopped trying," Sheila said. "She knew I would take care of her daughter if she passed."
A family battle with liver disease
For more than a decade, Sheila watched her sister deal with alcoholism while also facing her own battle with alcohol addiction.
In her relationships, things would start out great, and then turn abusive, she said. Alcohol and drugs were forced on her by past partners.
She got to a point where she often needed to drink from the moment she woke up.
“I drank between four to six tall cans of beer every day,” she said. This went on for 15 years.
In 2019, she was diagnosed with alcoholic fatty liver, the first stage of alcoholic liver disease.
Three years later, she watched her sister die from an advanced form of the disease.
She was in and out of sobriety after her fatty liver diagnosis but after Heather died she began heavily drinking again, wracked with guilt about her inability to keep her younger sister alive. That changed in August 2023, and she has stayed sober since.
Despite Sheila's guilt, one expert said Heather would have required tremendous help beyond what her sister could offer to stay clean; alcohol and substance addiction comes with inherent biological predispositions.
Even the prospect of imminent death would not force people with alcohol addiction or other substance abuse disorders to seek help, said Mike Japenga, the program director of Awakening Recovery Center, an addiction center in Tempe.
He said substance use disorder affects how the brain receives emotional reward and suspends the ability to see psychological, social and medical problems caused or exacerbated by a substance.
“Only a small percentage of people are biochemically predisposed towards becoming addicts,” Japenga said. “The vast majority of people who ingest chemicals for the high never pay the price of addiction or death because of this.”
Reach reporter Kunle Falayi at [email protected] or 480-268-1504 .
Risk Factors for Development of Cirrhosis in Chronic Viral Hepatitis B Patients Who Had Persistent Viral Suppression With Antiviral Therapy
Affiliations.
- 1 Division of Gastroenterology, Department of Medicine, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand.
- 2 Ma Har Myaing Hospital, Yangon, Myanmar.
- 3 Division of Academic Affairs, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand.
- 4 Center of Excellence for Innovation and Endoscopy in Gastrointestinal Oncology, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand.
- PMID: 38523735
- PMCID: PMC10956063 (available on 2025-07-01 )
- DOI: 10.1016/j.jceh.2024.101388
Background and aims: Chronic viral hepatitis B (CHB)-infected patients occasionally develop cirrhosis despite having persistent viral suppression with antiviral therapy. We aimed to identify risk factors for developing cirrhosis in hepatitis B virus (HBV)-suppressed patients.
Methods: We conducted a case-control study involving 120 noncirrhotic CHB-infected patients achieving viral suppression with antiviral treatment, with 40 cases developing cirrhosis and 80 age-, sex-, and Fibrosis-4 (FIB-4)-matched controls. Clinical and laboratory data at viral suppression, including body mass index (BMI), comorbidities, pretreatment HBV viral load, HBe antigen status, hepatitis C virus (HCV) and HIV coinfections, liver chemistries, and AST to Platelets Ratio Index (APRI) values, were retrospectively abstracted. Risk factors for cirrhosis post-HBV suppression were identified using Cox proportional hazard analysis.
Results: Case and control groups had similar ages (51.4 ± 9.9 vs. 51.4 ± 10.2 years), proportions of males (80% vs. 80%), and FIB-4 values (1.32 vs. 1.31). The cirrhosis group showed significantly higher BMI (25.1 vs. 22.7, P = 0.01) and more diabetes prevalence (50.0% vs. 26.3%, P = 0.01), while other comorbidities and laboratory parameters were comparable ( P > 0.05). By univariate analysis, BMI >23 kg/m2, diabetes, and APRI >0.7 were significantly associated with cirrhosis, with hazard ratios (HRs) (95%CI) of 2.99 (1.46-6.13), 2.31 (1.23-4.36), and 2.71 (1.05-6.99), P = 0.003, 0.010, and 0.039, respectively. In multivariate analyses adjusted for APRI, BMI>23 kg/m 2 remained significantly associated with cirrhosis (aHR: 2.76, P = 0.006), while diabetes showed borderline significance (aHR: 1.99, P = 0.072).
Conclusions: In HBV-infected patients achieving viral suppression with therapy, a BMI >23 kg/m 2 increases the risk of cirrhosis. Therefore, a comprehensive approach addressing metabolic factors is imperative for preventing disease progression in HBV-infected patients.
Keywords: chronic viral hepatitis B infection; cirrhosis of liver; viral suppression.
© 2024 Indian National Association for Study of the Liver. Published by Elsevier B.V. All rights reserved.

Amyloid beta: Bad for the brain, good for the liver
by Jenna Flogeras | Mar 26, 2024
As a hallmark of Alzheimer’s disease, amyloid beta peptides — fragments of a parent protein called amyloid precursor protein — has a bad rap when it comes to the brain, but researchers in Germany have recently found that this peptide helps keep the liver healthy.
“Amyloid beta serves as a prime example of how an undesirable molecule for the brain turns out to be an important trigger for the normal functioning of the liver,” said Gayane Hrachia Buniatian from the Department of Clinical Pharmacology at the University Hospital of Tübingen, and a lead researcher on a recent study exploring amyloid beta’s effects in the liver.
“In the brain, when overproduced, amyloid beta peptides start to clump together, forming abnormal structures called amyloid plaques,” explained her colleague, Lusine Danielyan, deputy medical director of the same department.
These plaques have been linked to the development of Alzheimer’s disease and other forms of dementia. But the story is different in the liver, whose role is to detoxify the blood. This organ helps clear amyloid beta from the body and also produces amyloid beta itself, with beneficial effects.
“Liver-produced amyloid beta, along with that derived from the bloodstream, help maintain a healthy environment in the liver,” Danielyan stated.
Amyloid beta deficiency and liver disease and cancer
In a previous study, Buniatian, Danielyan, and their colleagues discovered that healthy human and rodent livers were rich in amyloid beta but was depleted in the case of cirrhosis or scarring of the liver resulting from chronic liver disease.
“In cirrhosis, as [liver cells known as] hepatocytes lose their function and die, they stop producing and breaking down amyloid beta,” Danielyan explained.
Motivated by their initial findings, the researchers wondered if amyloid beta’s role in the liver could be leveraged to prevent fibrosis — an earlier stage of cirrhosis — and cancer . “Liver fibrosis can progress to cirrhosis and cancer, underscoring the importance of reducing fibrosis as a potential treatment approach for cancer,” Buniatian stated.
To answer this question, they immunized mice with different amounts of the amyloid beta antibody 3D6 and monitored the changes. “In all three models of amyloid beta deficiency, we observed the upregulation of classical markers of liver fibrosis/cirrhosis,” she said.
They also found that epithelial cells turned into mesenchymal stem cells in mice models and human liver samples where amyloid precursor protein had been knocked out. This transition is known to be a harbinger of cancer.
“When amyloid beta was added to cell cultures or produced in large amounts by mice used as models of Alzheimer’s disease, it reduced the levels of certain proteins associated with fibrosis and cancer,” Buniatian said. “For example, we observed a decrease in the levels of ADAM10 and Adam17, which are markers of fibrosis and cancer, when amyloid beta was present.”
In a mouse model of advanced-stage fibrosis, the drug sacubitril, , commonly used to treat heart failure, had a positive effect. This is because it inhibits neprilysin, an enzyme that degrades amyloid beta.
“When we reduced the breakdown of amyloid beta by inhibiting the powerful amyloid beta-degrading enzyme neprilysin, the levels of other proteins associated with fibrosis and cancer decreased as well,” Buniatian noted.
Implications for Alzheimer’s disease and liver fibrosis
“To our knowledge, this is the first study aiming to explore amyloid beta function in the liver,” Danielyan told us. Although the study sheds a positive light on amyloid beta, many questions remain unanswered.
“For instance, our whole genome analysis of animals with high levels of amyloid beta in their circulating blood and liver hints at the substantial contributions of this peptide to different metabolic pathways, such as lipid metabolism, and the liver’s defense against various injuries, such as oxidative stress,” Danielyan explained.
“We also do not yet know whether and to what extent the transportation of amyloid beta from the blood into the liver contributes to amyloid beta deficiency in the liver,” she added.
The researchers are also interested in studying how the brain responds when the liver fails to effectively process amyloid beta. Given their initial findings, however, Danielyan says that anti-amyloid beta therapies for Alzheimer’s disease should be used with caution.
“Antibodies that avoid depleting amyloid beta levels in the liver would be preferable for Alzheimer’s immunotherapy,” she advised.
To treat liver fibrosis, developing approaches that locally increase amyloid beta levels in the liver without significantly altering its amount in circulating blood and the brain would be ideal. “This can be achieved through liver-targeted drug-, gene-, and cell-based therapies,” Buniatian remarked.
Reference: Gayane Hrachia Buniatian, et al. Consequences of Amyloid-β Deficiency for the Liver , Advanced Science (2024). DOI: 10.1002/advs.202307734

Sign up for our weekly newsletter and receive the latest science news directly to your inbox.
Related posts:

Certain probiotics could help prevent and manage heart disease
Study finds patients with high risk factors for cardiovascular disease may benefit from preemptive use of specific probiotics.

Tiny, self-propelled machines might be key to fighting antimicrobial resistance
Microscopic machines powered by light are a “double threat” to bacteria and could help combat the growing problem of drug resistance.

Decisions, decisions! How neurons connect to shape our choices
A new study cracks the brain’s code on decision-making, uncovering how neurons are wired during the process.

Floating photocatalysts help break down water pollution using light
Sunlight-activated floating photocatalysts offer accessible water purification, vital for remote regions and developing communities.
How a gut-on-a-chip is getting to the bottom of our gut’s microbiome
This artificial gut will allow scientists to gain deeper insights into the biome that exists there and how dysregulation can lead to disease.

Are dietary supplement labels accurate?
A new study finds that prescription generic galantamine and the over-the-counter supplement are not created equal, despite label claims.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Paediatr Child Health
- v.21(3); 2016 Apr

Case 1: A 12-year-old boy with acute liver failure
A previously well 12-year-old boy presented with a four-day history of decreased energy and appetite. On day 3 of this illness, his parents noticed yellowing of his sclera and his urine was “dark” in colour. He was found to have elevated total and conjugated bilirubin, and elevated transaminase and gamma-glutamyl transferase levels, with normal alkaline phosphatase. His albumin level was low, along with an elevated international normalized ratio (INR), which did not respond to intravenous doses of vitamin K. He was found to have a low hemoglobin level, requiring packed red blood cell transfusions, with signs of nonautoimmune hemolytic anemia (low haptoglobin, increased lactate dehydrogenase levels and reticulocyte count, and negative Coomb’s test). There was no pruritus and no fever.
He had no sick contacts or pertinent travel history, no history of ingestion of acetaminophen or other drugs or naturopathic remedies, and no family history of liver disease. Serology for hepatitis A, B and C was negative. His urine toxicology screen was negative, total immunoglobulin G level was normal, and he had negative titres for antinuclear, antismooth muscle and antiliver kidney microsomal antibodies.
His blood and urine cultures were negative, and an abdominal ultrasound revealed no focal liver lesions, a normal biliary tree and patent hepatic veins.
CASE 1 DIAGNOSIS: WILSON DISEASE
The patient continued to deteriorate. By day 5 of his hospitalization, he had developed hepatopulmonary syndrome and encephalopathy, and required mechanical ventilation in the critical care unit. He was placed on the wait list for liver transplantation.
Acute liver failure (ALF) is defined by the presence of biochemical evidence of liver injury, with hepatic-based coagulopathy (INR >2.0 after parenteral replenishment of vitamin K, or INR >1.5 if encephalopathy is present) in the absence of evidence of chronic liver disease ( 1 ). It is an uncommon presentation in the previously well child. In general, symptoms are vague and include anorexia, fatigue and jaundice, while the underlying pathophysiology relates to loss of liver function and its subsequent sequelae (ie, coagulation abnormalities, encephalopathy, hemodynamic instability and renal failure) ( 2 ).
The differential diagnosis for ALF includes infective, toxic, autoimmune, metabolic and vascular causes, and varies according to age. In neonates and infants, gestational alloimmune liver disease, inborn errors of metabolism and hemophagocytic lymphohistiocytosis are the main causes of ALF. In older children, viral infections, drug-induced hepatotoxicity and autoimmune hepatitis are more common. Idiopathic ALF represents up to 50% of most reported cohorts ( 2 ).
Wilson disease (WD) is an autosomal recessive disorder of copper metabolism, affecting approximately one in 30,000 to 40,000 individuals. WD may present as nonspecific elevation of liver enzyme levels, cirrhosis or with ALF. It results from mutations in the ATP7B protein, which functions to incorporate copper into ceruloplasmin – a necessary step for biliary copper excretion. As such, serum ceruloplasmin and copper levels are usually reduced, with simultaneous increases in 24 h urinary copper excretion. The pathological features of WD emerge from copper accumulation in various tissues, especially the liver and brain. Diagnosis is aided by identification of Kayser-Fleischer rings in the eyes and typical features on liver biopsy. ALF due to WD is typically lethal without liver transplantation ( 3 ).
Treatment of WD relies on copper chelation with penicillamine or trientine therapy, low copper diet and use of zinc to reduce copper absorption in the gut. Zinc stimulates metallothionein production in enterocytes of the intestinal tract. Metallothionein is a protein with great affinity for copper and, as such, copper is then excreted when the enterocytes naturally shed into the lumen of the intestinal tract ( 3 ).
This patient presented with classic findings of WD ( 3 ): ALF with only a modest rise in liver enzyme levels and bilirubin accompanying a nonautoimmune hemolytic anemia. His ceruloplasmin level was found to be low (67 mg/L [normal 242 mg/L to 396 mg/L]), and he was started on empirical penicillamine and zinc pending definitive diagnosis from examination of liver tissue for total copper content and from genetic testing for ATP7B mutations. He developed kidney failure and atrial fibrillation, likely related to copper toxicity of the cardiac conducting tissue, which improved with plasmapheresis and albumin dialysis. On day 7 of hospitalization, he received a liver transplant.
Although not found on initial examination, as an outpatient, Kayser-Fleisher rings were seen on slit-lamp examination. A liver specimen obtained during transplant demonstrated elevated liver copper levles (622 μg/g [normal 10 μg/g to 35 μg/g], WD likely if >250 μg/g).
Genetic testing found a p.N1270S variant on chromosome 13, consistent with a mutation in the ATP7B gene, and a known causal factor in the development of WD. This patient’s family was screened for WD and the patient’s eight-year-old brother was found to have a low ceruloplasmin level (39 mg/L [normal 242 mg/L to 396 mg/L]), high urine copper level and screened positive on genetic testing. He has been started on zinc therapy and a low copper diet, and is currently doing well.
Our patient has experienced episodes of acute liver rejection, but is maintained on immunosuppressive therapies.
CLINICAL PEARLS
- New-onset jaundice in children should prompt immediate measurement of INR and, if INR is elevated, emergency referral to an expert centre.
- WD should be suspected in a child presenting with ALF, especially in the context of nonautoimmune hemolytic anemia and a modest rise in liver enzyme levels.
- ALF due to WD is frequently fatal and, therefore, immediate referral for evaluation for liver transplantation is required

VIDEO
COMMENTS
Diffuse liver disease includes etiologies such as the various viral and immune hepatitides, storage diseases, hepatic steatosis, fibrosis, and cirrhosis. 38 Ultrasonography findings are often non-specific in the case of diffuse liver disease, and biopsy is usually required to differentiate between the various etiologies. 38 In cases of acute ...
Presentation of Case. Dr. Nneka N. Ufere (Medicine): A 50-year-old man was admitted to the hospital because of elevated levels of serum aminotransferases, hyperbilirubinemia, anemia, and acute ...
UNFOLDING Reasoning Case Study: STUDENT Cirrhosis History of Present Problem: ... Liver cirrhosis with hepatic encephalopathy and an AKI Admit today - recent admission 6 months ago Hepatic encephalopathy due to advanced liver cirrhosis Hep C +, ETOH use (x25 years), IVDU, liver cirrhosis ...
The first edition of the clinical practice guidelines for liver cirrhosis was published in 2010, and the second edition was published in 2015 by the Japanese Society of Gastroenterology (JSGE). ... improved refractory pruritus with no clinically significant adverse drug reactions in patients with chronic liver disease . A case series study ...
Case Report • 2014 • vol.3 •13-16 CASE STUDY OF PATIENT WITH LIVER CIRRHOSIS Muhammad Rashad, ZubairAhmad, Hassan Ali , shanulqadir , Muhammad umair Faculty of Pharmacy, University of Sargodha. [email protected] Abstract Liver cirrhosis is a disease in which normal tissue of liver replaced with scar tissue, liver cirrhosis is ...
Recently published guidelines by European Association for Studies of Liver (EASL) 3 and European Society for Clinical Nutrition and Metabolism (ESPEN) 13 provide comprehensive overviews of nutrition in cirrhosis. Herein, we provide a case-based practical guide of the causes of malnutrition, assessments tools, daily requirements and dietary ...
This case study examines the physiological nature of alcohol-induced cirrhosis and its pathogenesis, external and internal clinical presentations, and treatment options. Treatments for alcohol-induced cirrhosis include liver transplant for permanent correction as well as varied options to manage symptoms. This case study analyzes alcoholic ...
In patients with compensated cirrhosis, the 10-year probabilities of ascites, hepatic encephalopathy, and gastrointestinal bleeding are 47%, 28%, and 25%, respectively. 6 These are ominous ...
Alcohol-related liver disease (ArLD) is a major cause of morbidity and mortality. Effective management requires multi-disciplinary input at every stage of the disease trajectory. We present a typical case to illustrate current evidence-based investigation and management of a patient with ArLD. This case-based review aims to concisely support the day-to-day decision making of clinicians looking ...
Temp - 37.0 C. Weight 235 lbs. BMI- 33. Alert, oriented to person, place, year and month but not to the day. Sclerae were not icteric. Pulmonary and Cardiovascular exam normal. Abdomen distended with fluid wave, mild tenderness to palpation. No hepatosplenomegaly. 2+ edema to mid-calf / Pedal pulses barely palpable.
Nursing case study for patient with cirrhosis with unfolding questions and answers. Written by ICU nurses. Cirrhosis Case Study (45 min) Watch More! ... 1.5 L of fluid. The patient's shortness of breath is relieved, and his breathing is less shallow. Ultrasound of the liver showed severe scarring on the liver. Mr. Garcia's condition ...
No. 11. CASE STUDY IN CIRRHOSIS OF THE LIVER 1039. Albumin is an abnormal constituent but it was of the urine, sincere wish of both the and was most likely caused by medical renal conges- and nursing staff to try to. tion, which in turn was caused make by him the as liver comfortable and as con-.
Case Report on Cirrhosis of Liver. ... In this retrospective, cross-sectional study, we identified cases of liver cirrhosis admitted between January 2001 to December 2010 and reviewed the medical ...
Case Discussion. These ultrasound images demonstrate coarsened liver echotexture concerning for cirrhosis and signs of portal hypertension. The portal vein shows a predominantly antegrade, pulsatile, and biphasic-bidirectional flow. Biphasic flows are commonly seen in patients with tricuspid regurgitation, right-heart cardiac failure, and ...
The high risk for heavy drinkers found in our meta-analysis of cohort studies is in line with prior research on risk for liver cirrhosis in people with alcohol use disorders.(11, 51, 52) The pooled RRs from case-control studies were much smaller; however, the more recent case-control study corresponds with the risks found in people with alcohol ...
Cirrhosis imposes a substantial health burden on many countries and this burden has increased at the global level since 1990, partly due to population growth and ageing. Although the age-standardised death and DALY rates of cirrhosis decreased from 1990 to 2017, numbers of deaths and DALYs and the proportion of all global deaths due to cirrhosis increased. Despite the availability of effective ...
The hepatologist recommended liver transplantation as the last resort for an Asian man who was the victim of liver cirrhosis that was complicated by untreated hepatitis c. Liver cirrhosis is a disease in which normal tissue of liver replaced with scar tissue, liver cirrhosis is the 12 th leading cause of deaths by disease in the world.Liver cirrhosis is caused by any factor that can damage ...
Liver Cirrhosis Case Study. 56 year old Caucasian male with end-stage liver cirrhosis in hospice care, came in for stem cell therapy to help prolong his life. Patient had a history of chronic Hepatitis C, hypertension and diabetes, and did not qualify for liver transplant. Patient had declined steadily over the past year, and over the last ...
Sixty-six (95.65%) patients had anemia and 47 (68.12%) patients had thrombocytopenia. Conclusions: From this study, we can conclude that, in cirrhosis of liver patients, various hematological changes are very common which need to be identified and corrected early to reduce morbidity and mortality. Download Free PDF.
In our study, underlying cause of primary liver cancer, comorbidity score, and cirrhosis stage were inferred from HES codes, which are dependent on hospital admissions and accurate coding practices.
The hospitalization rate for alcoholic liver disease increased by 5% in 2020 over the previous year. For alcoholic cirrhosis, the increase was 9%. By 2022, the rate of alcoholic liver disease had ...
2. Final Diagnosis :- Cirrhosis of Liver Attending physician :- Informants Obtained From :- Patient (self)& his son B : Chief complain Abdominaldistention since 15-16 days Bilateral pedal swelling since 10-12 days Moderate shortness of breathing since 5-7 days Loss of appetite since 15-16 days C. PresentIllness/Health Status 1.
Background: Refractory ascites affects the prognosis and quality of life in patients with liver cirrhosis. Peritoneovenous shunt (PVS) is a treatment procedure of palliative interventional radiology for refractory ascites. Although it is reportedly associated with serious complications (e.g., heart failure, thrombotic disease), the clinical course of PVS has not been thoroughly evaluated ...
Here, we report the case of a patient presenting with cirrhosis of the liver due to autoimmune hepatitis along with systemic sclerosis. Case presentation A 51-year-old non-obese female with no history of alcoholism was admitted with complaints of gradually progressive abdominal distension and swelling over both lower limbs for the last month.
Background and aims: Chronic viral hepatitis B (CHB)-infected patients occasionally develop cirrhosis despite having persistent viral suppression with antiviral therapy. We aimed to identify risk factors for developing cirrhosis in hepatitis B virus (HBV)-suppressed patients. Methods: We conducted a case-control study involving 120 noncirrhotic CHB-infected patients achieving viral suppression ...
In a previous study, Buniatian, Danielyan, and their colleagues discovered that healthy human and rodent livers were rich in amyloid beta but was depleted in the case of cirrhosis or scarring of the liver resulting from chronic liver disease. "In cirrhosis, as [liver cells known as] hepatocytes lose their function and die, they stop producing ...
Cirrhosis Cirrhosis of the liver is permanent scarring that damages your liver and interferes with its functioning. It can lead to liver failure. Cirrhosis is the result of persistent liver damage over many years. Alcohol and drugs, viruses and metabolic factors are the most common causes (Cleveland Clinic. 2020). • Sluggish Pupil reaction ...
In the past, liver cirrhosis was considered an irreversible phenomenon. However, many experimental data have provided evidence of the reversibility of liver fibrosis. Moreover, multiple clinical studies have also shown regression of fibrosis and reversal of cirrhosis on repeated biopsy samples. As various etiologies are associated with liver ...
This is a biotech to keep an eye on because of the release of results from the phase 2b NAVIGATE study, which is using Belapectin for the prevention of esophageal varices in NASH Cirrhosis. The ...
Acute liver failure (ALF) is defined by the presence of biochemical evidence of liver injury, with hepatic-based coagulopathy (INR >2.0 after parenteral replenishment of vitamin K, or INR >1.5 if encephalopathy is present) in the absence of evidence of chronic liver disease ( 1 ). It is an uncommon presentation in the previously well child.