- Breast Cancer
- Multiple Sclerosis (MS)
- Rheumatoid Arthritis
- Type 2 Diabetes
- Sponsored Topics
- Acid Reflux
- Alzheimer's & Dementia
- Bipolar Disorder
- Crohn's Disease
- Chronic Pain
- Cold & Flu
- Fibromyalgia
- Heart Disease
- High Cholesterol
- Hypertension
- Osteoarthritis
- Skin Disorders and Care
- Sexual Health
- Women's Health
- Mental Well-Being
- Vitamins & Supplements
- Mental Health
- At-Home Testing
- Men’s Health
- Fresh Food Fast
- Diagnosis Diaries
- You’re Not Alone
- Present Tense
- Youth in Focus
- Healthy Harvest
- Through An Artist's Eye
- Future of Health
- Mindful Eating
- Sugar Savvy
- Move Your Body
- Align Your Spine
- Primary Care
- Dermatologists
- Neurologists
- Cardiologists
- Orthopedists
- Weight Management
- Am I Depressed? A Quiz for Teens
- Are You a Workaholic?
- How Well Do You Sleep?
- Health News
- Find a Diet
- Find Healthy Snacks
- Inflammatory Bowel Disease
- Multiple Sclerosis
- Follow us on social media
- Health Conditions

What to Expect from Gender Confirmation Surgery

What is it?
For some, though not all, transgender people, surgery is an important and affirming part of the transition process. It can help alleviate feelings of dysphoria , help align your body with your internal sense of your gender, and make it easier to navigate the world in your gender.
Over the years, the names for these surgeries have evolved. Today, many transgender people prefer to use the term “gender confirmation surgery,” because when we say something like gender “reassignment” or “sex change,” it implies that a person’s gender changes when they have surgery.
As many trans folks have noted, surgery doesn’t change one’s gender — it changes the body in which one experiences that gender.
Here, we break down the different types of surgeries available to transgender people.
Top surgery for people assigned female at birth
During puberty, most folks who were assigned female at birth (AFAB) will develop breast or chest tissue.
Top surgery is a procedure to remove the chest tissue and reconstruct the chest to have more of a masculine appearance.
There are three basic top surgery options for AFAB folks:
Double incision
With this procedure, incisions are typically made at the top and bottom of the pectoral muscle and the chest tissue is removed.
The skin is pulled down and reconnected at the sight of the lower incision.
The nipples are also removed and used to create a graft that has the appearance of a nipple. This method generally results in decreased nipple sensation.
With the Inverted-T and Buttonhole methods, incisions are made around the nipples. This allows them to remain intact and retain sensation.
This procedure may work best for people with medium- to large-sized chests.
Periareolar and keyhole
With the periareolar procedure, one incision is made around the areola, and a larger circular incision is made around that.
The breast tissue is removed, as is the ring of skin between the two incisions.
The skin is then pulled in around the nipple — like a drawstring — and reattached. This leaves the nipple intact.
With the keyhole procedure, there’s only one incision. It goes underneath the nipple, allowing the chest tissue to be removed from there.
These procedures may work best for folks with smaller chests.
Bottom surgery for people assigned female at birth
AFAB folks were, for the most part, born with a vagina and clitoris.
Although testosterone use increases the size of the clitoris, some transmasculine people may wish to have some form of bottom surgery in which the genitals are reconstructed to create a phallus.
Testicular implants may be added, the urethra may be rerouted into the new phallus, and the vagina and other reproductive organs may be removed.
Bottom surgery options for AFAB folks include the following:
Metoidioplasty
The enlarged clitoris is released from the clitoral hood to create a new phallus.
Folks who get this surgery may have their urethra rerouted with a graft from their cheek or the inside of the vaginal wall so they can urinate through the new phallus.
The addition of testicular implants is also possible.
This surgery is only possible for folks who have been on testosterone. It’s a great option for people who want something less invasive than phalloplasty.
Phalloplasty
A graft is taken — typically from the forearm, thigh, or back — and used to create a penis.
Depending on the type of surgery , the urethra may be linked to allow urination through the new penis, and an implant may be installed to allow the penis to become erect.
This surgery is best for people who want a more realistic, average-size penis .
Hysterectomy, oophorectomy, and vaginectomy
AFAB trans people have a number of options when it comes to their reproductive organs. This includes removal of the uterus ( hysterectomy ), removal of one or both ovaries ( oophorectomy ), and removal of the vagina.
Top surgery for folks who were assigned male at birth
For transfeminine people and nonbinary folks who were assigned male at birth (AMAB), the absence of breast tissue can be a source of discomfort or dysphoria.
While hormone therapy can increase the size of the chest, some may wish to have top surgery to increase the size of the breasts, known as breast augmentation.
Breast augmentation
An incision is made along the areola, at the point where the chest and breast tissue meet or under the armpit.
The surgeon then inserts either a custom-sized silicone or saline implant and sutures the incision.
Silicone implants tend to be softer and more realistic. Saline implants are typically less expensive.
This surgery is great for anyone who wants to have a larger chest.
Bottom surgery for people who were assigned male at birth
Most AMAB folks have a penis and testicles. For transfeminine and nonbinary AMAB folks, this may be a source of discomfort which bottom surgery can relieve.
There are three basic bottom surgery options for AMAB folks:
Vaginoplasty
A functioning vagina is created out of existing tissue . The most common method is through penile inversion. The penis is inverted to create a vagina, the tip of the penis becomes a functioning clitoris, and the scrotal skin becomes the labia.
There are variations in which a graft from the intestine is used to create the vaginal wall (to supply more lubrication), or in which the scrotum is inverted to create a vaginal wall.
This surgery may be an option for anyone who wishes to have a functioning vagina.
Orchiectomy and scrotectomy
With these procedures, one or both testicles or the entire scrotum are removed.
Orchiectomy is a relatively inexpensive option in which the testes are removed. This allows your body to create less endogenous testosterone, which can be especially helpful for those on hormone replacement therapy.
Scrotectomy offers similar results, but it isn’t recommended for folks who wish to have a vaginoplasty. Scrotal skin is required for a vaginoplasty.
Things to consider
The increasing availability of gender confirmation surgeries is an incredible mark of progress for the transgender community. However, it’s important to note a few things about gender confirmation surgery and whether it’s the right choice for you.
Surgery isn’t the only aspect of medical transition
Representations of trans people tend to focus on the surgical aspects of transition, especially bottom surgery.
However, hormonal transition is also a valid medical option and can often produce results that alleviate dysphoria.
And, remember, medical transition isn’t necessary unless it’s something you truly want.
Surgery isn’t the same for everyone
One of the biggest things to remember is that not everyone wishes to have gender confirmation surgery, and the results — mental, physical, and emotional — will be different for everyone. Do your research and figure out what the right path is for you.
Surgery doesn’t define your experience or make you more valid
Surgery can be incredibly affirming for those who wish to have it.
But it’s important to remember that gender confirmation surgery simply changes the body in which you experience your gender, not your gender itself.
Your gender is valid, regardless of whether you want to have surgery.
Cost and insurance
Section 1557 of the Affordable Care Act (ACA) prohibits discrimination based on gender identity by any public insurance program or private insurance company receiving federal funding.
This means that if you have Medicare, Medicaid, public school insurance, or a private plan through the ACA marketplace, it’s illegal for you to be discriminated against for being transgender.
Your insurance may cover gender confirmation surgery in order to avoid breaching this non-discrimination clause. However, the law doesn’t require that an insurance company cover any specific procedures, leaving it somewhat open to interpretation.
Recent news from the White House makes it unclear how insurance companies will handle gender confirmation surgeries in the future. But as it currently stands, many people are able to get their surgeries covered by insurance.
If you don’t have insurance or if your insurance won’t cover your surgery, you may need to raise the funds yourself and pay out-of-pocket. Many trans people have used crowdfunding or medical loans to cover their surgeries.
Regardless, these are the prices you can expect to pay for the surgeries we’ve listed here.
- Transmasculine top surgery: Ranges from $3,000 to $11,000, depending on surgery type and surgeon.
- Transmasculine bottom surgery: Starts around $4,000 for metoidioplasty and goes up to $22,000 for phalloplasty.
- Transfeminine top surgery: Ranges from $3,000 to $11,000 , depending on surgeon and location.
- Transfeminine bottom surgery: Starts around $4,000 for orchiectomy and goes up to $20,000 for vaginoplasty.
How to find a provider
Depending on your insurance coverage, you may need to find someone in your network. You can check with your insurance company to see which surgeons are in your network.
If you don’t have insurance or your insurance won’t cover your surgery, you may be able to select a doctor you like based on their work and other factors.
These are a few great resources for finding a provider:
- Metoidioplasty.net
- MTF Surgery
- Topsurgery.net
- Trans HealthCare
- TS Surgery Guide
The bottom line
Gender confirmation surgery certainly isn’t the right choice for everyone.
But for the folks who want — and in fact need — confirmation surgery, it can be an incredible opportunity to help align your body with your internal sense of self.
If gender confirmation surgery is in your future, be sure to do your research to find the right surgeon for you.
KC Clements is a queer, nonbinary writer based in Brooklyn, NY. Their work deals with queer and trans identity, sex and sexuality, health and wellness from a body positive standpoint, and much more. You can keep up with them by visiting their website , or by finding them on Instagram and Twitter .
Last medically reviewed on December 19, 2018
How we reviewed this article:
- Bluebond-Langner R, et al. (2017).Top surgery in transgender men: how far can you push the envelope? DOI: https://journals.lww.com/plasreconsurg/Fulltext/2017/04000/Top_Surgery_in_Transgender_Men___How_Far_Can_You.14.aspx
- Female-to-male price list. (2018). http://www.thetransgendercenter.com/index.php/femaletomale1/ftm-price-list.html
- Frey J, et al. (2016). Asystematic review of metoidioplasty and radial forearm flap phalloplasty infemale-to-male transgender genital reconstruction: is the “ideal” neophallus anachievable goal? DOI: https://dx.doi.org/10.1097%2FGOX.0000000000001131
- Horbach S, et al. (2015). Outcomeof vaginoplasty in male‐to‐female transgenders: a systematic review of surgicaltechniques. DOI: https://doi.org/10.1111/jsm.12868
- Male-to-female price list. (2018). http://www.thetransgendercenter.com/index.php/maletofemale1/mtf-price-list.html
- Metoidioplasty cost. (2018). https://www.realself.com/ftm-metoidioplasty/cost
- MTF breast augmentation cost.(2018). https://www.realself.com/mtf-breast-augmentation/cost
- Section 1557 of the Patient Protectionand Affordable Care Act. (2010). Health and human services. https://www.hhs.gov/civil-rights/for-individuals/section-1557/index.html
- Stojanovic B, et al. (2017).One-stage gender confirmation surgery as a viable surgical procedure forfemale-to-male transsexuals. DOI: https://doi.org/10.1016/j.jsxm.2017.03.256
- Weigert R, et al. (2013). Patientsatisfaction with breasts and psychosocial, sexual, and physical well-beingafter breast augmentation in male-to-female transsexuals. DOI: https://journals.lww.com/plasreconsurg/Abstract/2013/12000/Patient_Satisfaction_with_Breasts_and.9.aspx
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Dec 22, 2018
KC Clements
Prerna Sharma
Dec 19, 2018
Medically Reviewed By
Timothy J. Legg, PhD, PsyD
Share this article
Read this next
What does having a vagina mean? There’s no right or wrong way of having a relationship with your vagina, and yet having or not having one can…
People who are genderqueer often experience their gender as fluid, meaning it can shift and change at any given time. Here's what it might look like…
We created an LGBTQIA+ safer sex guide that understands the true complexity and diversity across gender identities, sexual orientation, attractions…
You may have heard the term “misgendering” before, but what exactly does it mean? Here's what you should know about what pronouns to use and when.
Society typically tells us that there are two sexes, male and female, and that they align with two genders, man and woman. With the increased…
You may have heard the term "deadnaming" before, but what exactly does this mean? Here's what you should know and why it matters.
Cissexism is based on the assumption that all people are cisgender. This is so deeply ingrained in our society, so many people say and do things that…
Words can unconsciously undermine transgender and nonbinary people, so being conscious of our words and their affect is so important.
Many transgender men, transmasculine people, and even some cisgender men pursue facial masculinization surgery to create or enhance certain features.
- Patient Care & Health Information
- Tests & Procedures
- Feminizing surgery
Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation. Bottom surgery can involve removal of the testicles, or removal of the testicles and penis and the creation of a vagina, labia and clitoris. Facial procedures or body-contouring procedures can be used as well.
Not everybody chooses to have feminizing surgery. These surgeries can be expensive, carry risks and complications, and involve follow-up medical care and procedures. Certain surgeries change fertility and sexual sensations. They also may change how you feel about your body.
Your health care team can talk with you about your options and help you weigh the risks and benefits.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Available Sexual Health Solutions at Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
Many people seek feminizing surgery as a step in the process of treating discomfort or distress because their gender identity differs from their sex assigned at birth. The medical term for this is gender dysphoria.
For some people, having feminizing surgery feels like a natural step. It's important to their sense of self. Others choose not to have surgery. All people relate to their bodies differently and should make individual choices that best suit their needs.
Feminizing surgery may include:
- Removal of the testicles alone. This is called orchiectomy.
- Removal of the penis, called penectomy.
- Removal of the testicles.
- Creation of a vagina, called vaginoplasty.
- Creation of a clitoris, called clitoroplasty.
- Creation of labia, called labioplasty.
- Breast surgery. Surgery to increase breast size is called top surgery or breast augmentation. It can be done through implants, the placement of tissue expanders under breast tissue, or the transplantation of fat from other parts of the body into the breast.
- Plastic surgery on the face. This is called facial feminization surgery. It involves plastic surgery techniques in which the jaw, chin, cheeks, forehead, nose, and areas surrounding the eyes, ears or lips are changed to create a more feminine appearance.
- Tummy tuck, called abdominoplasty.
- Buttock lift, called gluteal augmentation.
- Liposuction, a surgical procedure that uses a suction technique to remove fat from specific areas of the body.
- Voice feminizing therapy and surgery. These are techniques used to raise voice pitch.
- Tracheal shave. This surgery reduces the thyroid cartilage, also called the Adam's apple.
- Scalp hair transplant. This procedure removes hair follicles from the back and side of the head and transplants them to balding areas.
- Hair removal. A laser can be used to remove unwanted hair. Another option is electrolysis, a procedure that involves inserting a tiny needle into each hair follicle. The needle emits a pulse of electric current that damages and eventually destroys the follicle.
Your health care provider might advise against these surgeries if you have:
- Significant medical conditions that haven't been addressed.
- Behavioral health conditions that haven't been addressed.
- Any condition that limits your ability to give your informed consent.
Like any other type of major surgery, many types of feminizing surgery pose a risk of bleeding, infection and a reaction to anesthesia. Other complications might include:
- Delayed wound healing
- Fluid buildup beneath the skin, called seroma
- Bruising, also called hematoma
- Changes in skin sensation such as pain that doesn't go away, tingling, reduced sensation or numbness
- Damaged or dead body tissue — a condition known as tissue necrosis — such as in the vagina or labia
- A blood clot in a deep vein, called deep vein thrombosis, or a blood clot in the lung, called pulmonary embolism
- Development of an irregular connection between two body parts, called a fistula, such as between the bladder or bowel into the vagina
- Urinary problems, such as incontinence
- Pelvic floor problems
- Permanent scarring
- Loss of sexual pleasure or function
- Worsening of a behavioral health problem
Certain types of feminizing surgery may limit or end fertility. If you want to have biological children and you're having surgery that involves your reproductive organs, talk to your health care provider before surgery. You may be able to freeze sperm with a technique called sperm cryopreservation.
How you prepare
Before surgery, you meet with your surgeon. Work with a surgeon who is board certified and experienced in the procedures you want. Your surgeon talks with you about your options and the potential results. The surgeon also may provide information on details such as the type of anesthesia that will be used during surgery and the kind of follow-up care that you may need.
Follow your health care team's directions on preparing for your procedures. This may include guidelines on eating and drinking. You may need to make changes in the medicine you take and stop using nicotine, including vaping, smoking and chewing tobacco.
Because feminizing surgery might cause physical changes that cannot be reversed, you must give informed consent after thoroughly discussing:
- Risks and benefits
- Alternatives to surgery
- Expectations and goals
- Social and legal implications
- Potential complications
- Impact on sexual function and fertility
Evaluation for surgery
Before surgery, a health care provider evaluates your health to address any medical conditions that might prevent you from having surgery or that could affect the procedure. This evaluation may be done by a provider with expertise in transgender medicine. The evaluation might include:
- A review of your personal and family medical history
- A physical exam
- A review of your vaccinations
- Screening tests for some conditions and diseases
- Identification and management, if needed, of tobacco use, drug use, alcohol use disorder, HIV or other sexually transmitted infections
- Discussion about birth control, fertility and sexual function
You also may have a behavioral health evaluation by a health care provider with expertise in transgender health. That evaluation might assess:
- Gender identity
- Gender dysphoria
- Mental health concerns
- Sexual health concerns
- The impact of gender identity at work, at school, at home and in social settings
- The role of social transitioning and hormone therapy before surgery
- Risky behaviors, such as substance use or use of unapproved hormone therapy or supplements
- Support from family, friends and caregivers
- Your goals and expectations of treatment
- Care planning and follow-up after surgery
Other considerations
Health insurance coverage for feminizing surgery varies widely. Before you have surgery, check with your insurance provider to see what will be covered.
Before surgery, you might consider talking to others who have had feminizing surgery. If you don't know someone, ask your health care provider about support groups in your area or online resources you can trust. People who have gone through the process may be able to help you set your expectations and offer a point of comparison for your own goals of the surgery.
What you can expect
Facial feminization surgery.
Facial feminization surgery may involve a range of procedures to change facial features, including:
- Moving the hairline to create a smaller forehead
- Enlarging the lips and cheekbones with implants
- Reshaping the jaw and chin
- Undergoing skin-tightening surgery after bone reduction
These surgeries are typically done on an outpatient basis, requiring no hospital stay. Recovery time for most of them is several weeks. Recovering from jaw procedures takes longer.
Tracheal shave
A tracheal shave minimizes the thyroid cartilage, also called the Adam's apple. During this procedure, a small cut is made under the chin, in the shadow of the neck or in a skin fold to conceal the scar. The surgeon then reduces and reshapes the cartilage. This is typically an outpatient procedure, requiring no hospital stay.
Top surgery
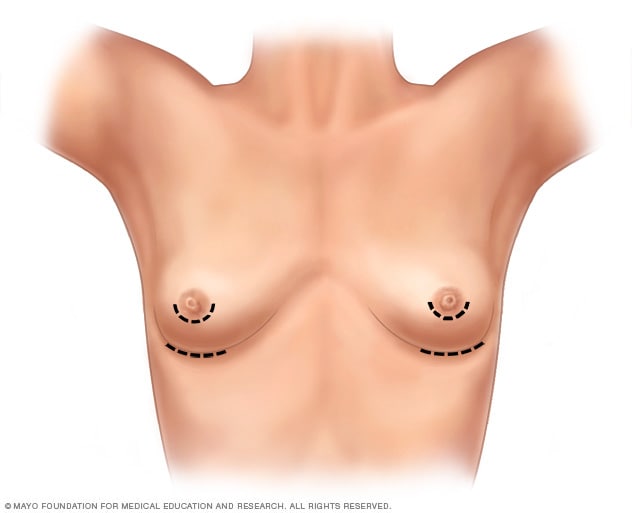
- Breast augmentation incisions
As part of top surgery, the surgeon makes cuts around the areola, near the armpit or in the crease under the breast.
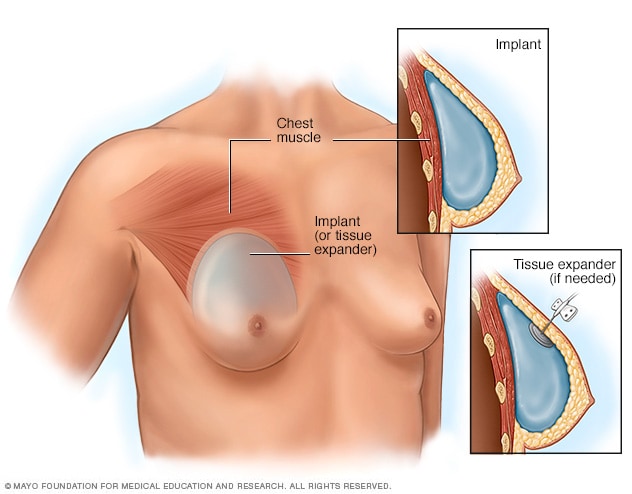
- Placement of breast implants or tissue expanders
During top surgery, the surgeon places the implants under the breast tissue. If feminizing hormones haven't made the breasts large enough, an initial surgery might be needed to have devices called tissue expanders placed in front of the chest muscles.
Hormone therapy with estrogen stimulates breast growth, but many people aren't satisfied with that growth alone. Top surgery is a surgical procedure to increase breast size that may involve implants, fat grafting or both.
During this surgery, a surgeon makes cuts around the areola, near the armpit or in the crease under the breast. Next, silicone or saline implants are placed under the breast tissue. Another option is to transplant fat, muscles or tissue from other parts of the body into the breasts.
If feminizing hormones haven't made the breasts large enough for top surgery, an initial surgery may be needed to place devices called tissue expanders in front of the chest muscles. After that surgery, visits to a health care provider are needed every few weeks to have a small amount of saline injected into the tissue expanders. This slowly stretches the chest skin and other tissues to make room for the implants. When the skin has been stretched enough, another surgery is done to remove the expanders and place the implants.
Genital surgery
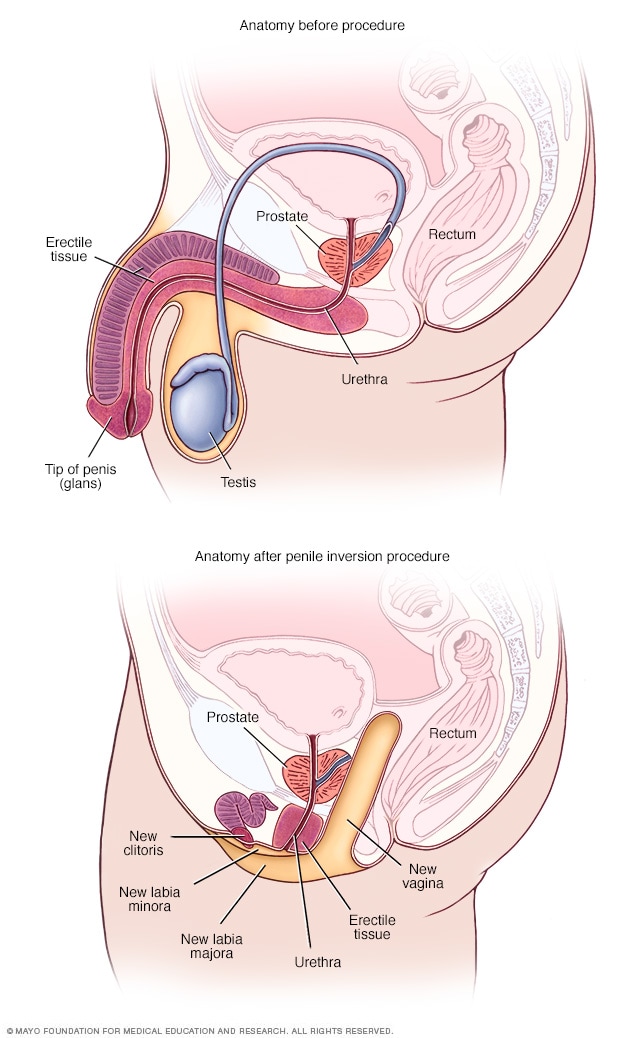
- Anatomy before and after penile inversion
During penile inversion, the surgeon makes a cut in the area between the rectum and the urethra and prostate. This forms a tunnel that becomes the new vagina. The surgeon lines the inside of the tunnel with skin from the scrotum, the penis or both. If there's not enough penile or scrotal skin, the surgeon might take skin from another area of the body and use it for the new vagina as well.
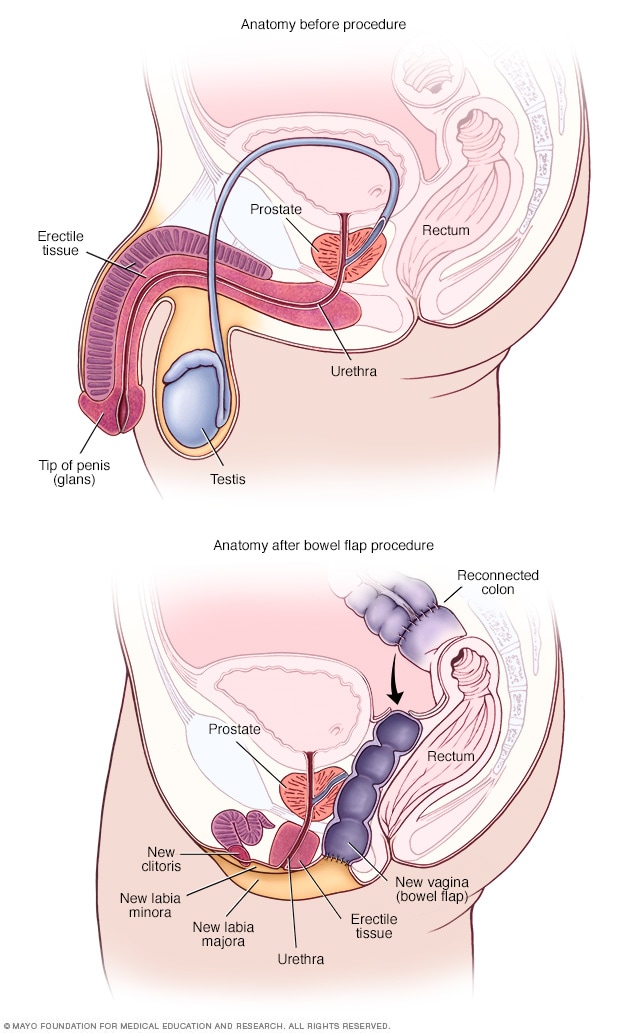
- Anatomy before and after bowel flap procedure
A bowel flap procedure might be done if there's not enough tissue or skin in the penis or scrotum. The surgeon moves a segment of the colon or small bowel to form a new vagina. That segment is called a bowel flap or conduit. The surgeon reconnects the remaining parts of the colon.
Orchiectomy
Orchiectomy is a surgery to remove the testicles. Because testicles produce sperm and the hormone testosterone, an orchiectomy might eliminate the need to use testosterone blockers. It also may lower the amount of estrogen needed to achieve and maintain the appearance you want.
This type of surgery is typically done on an outpatient basis. A local anesthetic may be used, so only the testicular area is numbed. Or the surgery may be done using general anesthesia. This means you are in a sleep-like state during the procedure.
To remove the testicles, a surgeon makes a cut in the scrotum and removes the testicles through the opening. Orchiectomy is typically done as part of the surgery for vaginoplasty. But some people prefer to have it done alone without other genital surgery.
Vaginoplasty
Vaginoplasty is the surgical creation of a vagina. During vaginoplasty, skin from the shaft of the penis and the scrotum is used to create a vaginal canal. This surgical approach is called penile inversion. In some techniques, the skin also is used to create the labia. That procedure is called labiaplasty. To surgically create a clitoris, the tip of the penis and the nerves that supply it are used. This procedure is called a clitoroplasty. In some cases, skin can be taken from another area of the body or tissue from the colon may be used to create the vagina. This approach is called a bowel flap procedure. During vaginoplasty, the testicles are removed if that has not been done previously.
Some surgeons use a technique that requires laser hair removal in the area of the penis and scrotum to provide hair-free tissue for the procedure. That process can take several months. Other techniques don't require hair removal prior to surgery because the hair follicles are destroyed during the procedure.
After vaginoplasty, a tube called a catheter is placed in the urethra to collect urine for several days. You need to be closely watched for about a week after surgery. Recovery can take up to two months. Your health care provider gives you instructions about when you may begin sexual activity with your new vagina.
After surgery, you're given a set of vaginal dilators of increasing sizes. You insert the dilators in your vagina to maintain, lengthen and stretch it. Follow your health care provider's directions on how often to use the dilators. To keep the vagina open, dilation needs to continue long term.
Because the prostate gland isn't removed during surgery, you need to follow age-appropriate recommendations for prostate cancer screening. Following surgery, it is possible to develop urinary symptoms from enlargement of the prostate.
Dilation after gender-affirming surgery
This material is for your education and information only. This content does not replace medical advice, diagnosis and treatment. If you have questions about a medical condition, always talk with your health care provider.
Narrator: Vaginal dilation is important to your recovery and ongoing care. You have to dilate to maintain the size and shape of your vaginal canal and to keep it open.
Jessi: I think for many trans women, including myself, but especially myself, I looked forward to one day having surgery for a long time. So that meant looking up on the internet what the routines would be, what the surgery entailed. So I knew going into it that dilation was going to be a very big part of my routine post-op, but just going forward, permanently.
Narrator: Vaginal dilation is part of your self-care. You will need to do vaginal dilation for the rest of your life.
Alissa (nurse): If you do not do dilation, your vagina may shrink or close. If that happens, these changes might not be able to be reversed.
Narrator: For the first year after surgery, you will dilate many times a day. After the first year, you may only need to dilate once a week. Most people dilate for the rest of their life.
Jessi: The dilation became easier mostly because I healed the scars, the stitches held up a little bit better, and I knew how to do it better. Each transgender woman's vagina is going to be a little bit different based on anatomy, and I grew to learn mine. I understand, you know, what position I needed to put the dilator in, how much force I needed to use, and once I learned how far I needed to put it in and I didn't force it and I didn't worry so much on oh, did I put it in too far, am I not putting it in far enough, and I have all these worries and then I stress out and then my body tenses up. Once I stopped having those thoughts, I relaxed more and it was a lot easier.
Narrator: You will have dilators of different sizes. Your health care provider will determine which sizes are best for you. Dilation will most likely be painful at first. It's important to dilate even if you have pain.
Alissa (nurse): Learning how to relax the muscles and breathe as you dilate will help. If you wish, you can take the pain medication recommended by your health care team before you dilate.
Narrator: Dilation requires time and privacy. Plan ahead so you have a private area at home or at work. Be sure to have your dilators, a mirror, water-based lubricant and towels available. Wash your hands and the dilators with warm soapy water, rinse well and dry on a clean towel. Use a water-based lubricant to moisten the rounded end of the dilators. Water-based lubricants are available over-the-counter. Do not use oil-based lubricants, such as petroleum jelly or baby oil. These can irritate the vagina. Find a comfortable position in bed or elsewhere. Use pillows to support your back and thighs as you lean back to a 45-degree angle. Start your dilation session with the smallest dilator. Hold a mirror in one hand. Use the other hand to find the opening of your vagina. Separate the skin. Relax through your hips, abdomen and pelvic floor. Take slow, deep breaths. Position the rounded end of the dilator with the lubricant at the opening to your vaginal canal. The rounded end should point toward your back. Insert the dilator. Go slowly and gently. Think of its path as a gentle curving swoop. The dilator doesn't go straight in. It follows the natural curve of the vaginal canal. Keep gentle down and inward pressure on the dilator as you insert it. Stop when the dilator's rounded end reaches the end of your vaginal canal. The dilators have dots or markers that measure depth. Hold the dilator in place in your vaginal canal. Use gentle but constant inward pressure for the correct amount of time at the right depth for you. If you're feeling pain, breathe and relax the muscles. When time is up, slowly remove the dilator, then repeat with the other dilators you need to use. Wash the dilators and your hands. If you have increased discharge following dilation, you may want to wear a pad to protect your clothing.
Jessi: I mean, it's such a strange, unfamiliar feeling to dilate and to have a dilator, you know to insert a dilator into your own vagina. Because it's not a pleasurable experience, and it's quite painful at first when you start to dilate. It feels much like a foreign body entering and it doesn't feel familiar and your body kind of wants to get it out of there. It's really tough at the beginning, but if you can get through the first month, couple months, it's going to be a lot easier and it's not going to be so much of an emotional and uncomfortable experience.
Narrator: You need to stay on schedule even when traveling. Bring your dilators with you. If your schedule at work creates challenges, ask your health care team if some of your dilation sessions can be done overnight.
Alissa (nurse): You can't skip days now and do more dilation later. You must do dilation on schedule to keep vaginal depth and width. It is important to dilate even if you have pain. Dilation should cause less pain over time.
Jessi: I hear that from a lot of other women that it's an overwhelming experience. There's lots of emotions that are coming through all at once. But at the end of the day for me, it was a very happy experience. I was glad to have the opportunity because that meant that while I have a vagina now, at the end of the day I had a vagina. Yes, it hurts, and it's not pleasant to dilate, but I have the vagina and it's worth it. It's a long process and it's not going to be easy. But you can do it.
Narrator: If you feel dilation may not be working or you have any questions about dilation, please talk with a member of your health care team.
Research has found that that gender-affirming surgery can have a positive impact on well-being and sexual function. It's important to follow your health care provider's advice for long-term care and follow-up after surgery. Continued care after surgery is associated with good outcomes for long-term health.
Before you have surgery, talk to members of your health care team about what to expect after surgery and the ongoing care you may need.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Feminizing surgery care at Mayo Clinic
- Tangpricha V, et al. Transgender women: Evaluation and management. https://www.uptodate.com/ contents/search. Accessed Aug. 16, 2022.
- Erickson-Schroth L, ed. Surgical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Coleman E, et al. Standards of care for the health of transgender and gender diverse people, version 8. International Journal of Transgender Health. 2022; doi:10.1080/26895269.2022.2100644.
- AskMayoExpert. Gender-affirming procedures (adult). Mayo Clinic; 2022.
- Nahabedian, M. Implant-based breast reconstruction and augmentation. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Erickson-Schroth L, ed. Medical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Ferrando C, et al. Gender-affirming surgery: Male to female. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Doctors & Departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Preparation and Procedures Involved in Gender Affirmation Surgeries
If you or a loved one are considering gender affirmation surgery , you are probably wondering what steps you must go through before the surgery can be done. Let's look at what is required to be a candidate for these surgeries, the potential positive effects and side effects of hormonal therapy, and the types of surgeries that are available.
Gender affirmation surgery, also known as gender confirmation surgery, is performed to align or transition individuals with gender dysphoria to their true gender.
A transgender woman, man, or non-binary person may choose to undergo gender affirmation surgery.
The term "transexual" was previously used by the medical community to describe people who undergo gender affirmation surgery. The term is no longer accepted by many members of the trans community as it is often weaponized as a slur. While some trans people do identify as "transexual", it is best to use the term "transgender" to describe members of this community.
Transitioning
Transitioning may involve:
- Social transitioning : going by different pronouns, changing one’s style, adopting a new name, etc., to affirm one’s gender
- Medical transitioning : taking hormones and/or surgically removing or modifying genitals and reproductive organs
Transgender individuals do not need to undergo medical intervention to have valid identities.
Reasons for Undergoing Surgery
Many transgender people experience a marked incongruence between their gender and their assigned sex at birth. The American Psychiatric Association (APA) has identified this as gender dysphoria.
Gender dysphoria is the distress some trans people feel when their appearance does not reflect their gender. Dysphoria can be the cause of poor mental health or trigger mental illness in transgender people.
For these individuals, social transitioning, hormone therapy, and gender confirmation surgery permit their outside appearance to match their true gender.
Steps Required Before Surgery
In addition to a comprehensive understanding of the procedures, hormones, and other risks involved in gender-affirming surgery, there are other steps that must be accomplished before surgery is performed. These steps are one way the medical community and insurance companies limit access to gender affirmative procedures.
Steps may include:
- Mental health evaluation : A mental health evaluation is required to look for any mental health concerns that could influence an individual’s mental state, and to assess a person’s readiness to undergo the physical and emotional stresses of the transition.
- Clear and consistent documentation of gender dysphoria
- A "real life" test : The individual must take on the role of their gender in everyday activities, both socially and professionally (known as “real-life experience” or “real-life test”).
Firstly, not all transgender experience physical body dysphoria. The “real life” test is also very dangerous to execute, as trans people have to make themselves vulnerable in public to be considered for affirmative procedures. When a trans person does not pass (easily identified as their gender), they can be clocked (found out to be transgender), putting them at risk for violence and discrimination.
Requiring trans people to conduct a “real-life” test despite the ongoing violence out transgender people face is extremely dangerous, especially because some transgender people only want surgery to lower their risk of experiencing transphobic violence.
Hormone Therapy & Transitioning
Hormone therapy involves taking progesterone, estrogen, or testosterone. An individual has to have undergone hormone therapy for a year before having gender affirmation surgery.
The purpose of hormone therapy is to change the physical appearance to reflect gender identity.
Effects of Testosterone
When a trans person begins taking testosterone , changes include both a reduction in assigned female sexual characteristics and an increase in assigned male sexual characteristics.
Bodily changes can include:
- Beard and mustache growth
- Deepening of the voice
- Enlargement of the clitoris
- Increased growth of body hair
- Increased muscle mass and strength
- Increase in the number of red blood cells
- Redistribution of fat from the breasts, hips, and thighs to the abdominal area
- Development of acne, similar to male puberty
- Baldness or localized hair loss, especially at the temples and crown of the head
- Atrophy of the uterus and ovaries, resulting in an inability to have children
Behavioral changes include:
- Aggression
- Increased sex drive
Effects of Estrogen
When a trans person begins taking estrogen , changes include both a reduction in assigned male sexual characteristics and an increase in assigned female characteristics.
Changes to the body can include:
- Breast development
- Loss of erection
- Shrinkage of testicles
- Decreased acne
- Decreased facial and body hair
- Decreased muscle mass and strength
- Softer and smoother skin
- Slowing of balding
- Redistribution of fat from abdomen to the hips, thighs, and buttocks
- Decreased sex drive
- Mood swings
When Are the Hormonal Therapy Effects Noticed?
The feminizing effects of estrogen and the masculinizing effects of testosterone may appear after the first couple of doses, although it may be several years before a person is satisfied with their transition. This is especially true for breast development.
Timeline of Surgical Process
Surgery is delayed until at least one year after the start of hormone therapy and at least two years after a mental health evaluation. Once the surgical procedures begin, the amount of time until completion is variable depending on the number of procedures desired, recovery time, and more.
Transfeminine Surgeries
Transfeminine is an umbrella term inclusive of trans women and non-binary trans people who were assigned male at birth.
Most often, surgeries involved in gender affirmation surgery are broken down into those that occur above the belt (top surgery) and those below the belt (bottom surgery). Not everyone undergoes all of these surgeries, but procedures that may be considered for transfeminine individuals are listed below.
Top surgery includes:
- Breast augmentation
- Facial feminization
- Nose surgery: Rhinoplasty may be done to narrow the nose and refine the tip.
- Eyebrows: A brow lift may be done to feminize the curvature and position of the eyebrows.
- Jaw surgery: The jaw bone may be shaved down.
- Chin reduction: Chin reduction may be performed to soften the chin's angles.
- Cheekbones: Cheekbones may be enhanced, often via collagen injections as well as other plastic surgery techniques.
- Lips: A lip lift may be done.
- Alteration to hairline
- Male pattern hair removal
- Reduction of Adam’s apple
- Voice change surgery
Bottom surgery includes:
- Removal of the penis (penectomy) and scrotum (orchiectomy)
- Creation of a vagina and labia
Transmasculine Surgeries
Transmasculine is an umbrella term inclusive of trans men and non-binary trans people who were assigned female at birth.
Surgery for this group involves top surgery and bottom surgery as well.
Top surgery includes :
- Subcutaneous mastectomy/breast reduction surgery.
- Removal of the uterus and ovaries
- Creation of a penis and scrotum either through metoidioplasty and/or phalloplasty
Complications and Side Effects
Surgery is not without potential risks and complications. Estrogen therapy has been associated with an elevated risk of blood clots ( deep vein thrombosis and pulmonary emboli ) for transfeminine people. There is also the potential of increased risk of breast cancer (even without hormones, breast cancer may develop).
Testosterone use in transmasculine people has been associated with an increase in blood pressure, insulin resistance, and lipid abnormalities, though it's not certain exactly what role these changes play in the development of heart disease.
With surgery, there are surgical risks such as bleeding and infection, as well as side effects of anesthesia . Those who are considering these treatments should have a careful discussion with their doctor about potential risks related to hormone therapy as well as the surgeries.
Cost of Gender Confirmation Surgery
Surgery can be prohibitively expensive for many transgender individuals. Costs including counseling, hormones, electrolysis, and operations can amount to well over $100,000. Transfeminine procedures tend to be more expensive than transmasculine ones. Health insurance sometimes covers a portion of the expenses.
Quality of Life After Surgery
Quality of life appears to improve after gender-affirming surgery for all trans people who medically transition. One 2017 study found that surgical satisfaction ranged from 94% to 100%.
Since there are many steps and sometimes uncomfortable surgeries involved, this number supports the benefits of surgery for those who feel it is their best choice.
A Word From Verywell
Gender affirmation surgery is a lengthy process that begins with counseling and a mental health evaluation to determine if a person can be diagnosed with gender dysphoria.
After this is complete, hormonal treatment is begun with testosterone for transmasculine individuals and estrogen for transfeminine people. Some of the physical and behavioral changes associated with hormonal treatment are listed above.
After hormone therapy has been continued for at least one year, a number of surgical procedures may be considered. These are broken down into "top" procedures and "bottom" procedures.
Surgery is costly, but precise estimates are difficult due to many variables. Finding a surgeon who focuses solely on gender confirmation surgery and has performed many of these procedures is a plus. Speaking to a surgeon's past patients can be a helpful way to gain insight on the physician's practices as well.
For those who follow through with these preparation steps, hormone treatment, and surgeries, studies show quality of life appears to improve. Many people who undergo these procedures express satisfaction with their results.
Bizic MR, Jeftovic M, Pusica S, et al. Gender dysphoria: Bioethical aspects of medical treatment . Biomed Res Int . 2018;2018:9652305. doi:10.1155/2018/9652305
American Psychiatric Association. What is gender dysphoria? . 2016.
The World Professional Association for Transgender Health. Standards of care for the health of transsexual, transgender, and gender-nonconforming people . 2012.
Tomlins L. Prescribing for transgender patients . Aust Prescr . 2019;42(1): 10–13. doi:10.18773/austprescr.2019.003
T'sjoen G, Arcelus J, Gooren L, Klink DT, Tangpricha V. Endocrinology of transgender medicine . Endocr Rev . 2019;40(1):97-117. doi:10.1210/er.2018-00011
Unger CA. Hormone therapy for transgender patients . Transl Androl Urol . 2016;5(6):877-884. doi:10.21037/tau.2016.09.04
Seal LJ. A review of the physical and metabolic effects of cross-sex hormonal therapy in the treatment of gender dysphoria . Ann Clin Biochem . 2016;53(Pt 1):10-20. doi:10.1177/0004563215587763
Schechter LS. Gender confirmation surgery: An update for the primary care provider . Transgend Health . 2016;1(1):32-40. doi:10.1089/trgh.2015.0006
Altman K. Facial feminization surgery: current state of the art . Int J Oral Maxillofac Surg . 2012;41(8):885-94. doi:10.1016/j.ijom.2012.04.024
Therattil PJ, Hazim NY, Cohen WA, Keith JD. Esthetic reduction of the thyroid cartilage: A systematic review of chondrolaryngoplasty . JPRAS Open. 2019;22:27-32. doi:10.1016/j.jpra.2019.07.002
Top H, Balta S. Transsexual mastectomy: Selection of appropriate technique according to breast characteristics . Balkan Med J . 2017;34(2):147-155. doi:10.4274/balkanmedj.2016.0093
Chan W, Drummond A, Kelly M. Deep vein thrombosis in a transgender woman . CMAJ . 2017;189(13):E502-E504. doi:10.1503/cmaj.160408
Streed CG, Harfouch O, Marvel F, Blumenthal RS, Martin SS, Mukherjee M. Cardiovascular disease among transgender adults receiving hormone therapy: A narrative review . Ann Intern Med . 2017;167(4):256-267. doi:10.7326/M17-0577
Hashemi L, Weinreb J, Weimer AK, Weiss RL. Transgender care in the primary care setting: A review of guidelines and literature . Fed Pract . 2018;35(7):30-37.
Van de grift TC, Elaut E, Cerwenka SC, Cohen-kettenis PT, Kreukels BPC. Surgical satisfaction, quality of life, and their association after gender-affirming aurgery: A follow-up atudy . J Sex Marital Ther . 2018;44(2):138-148. doi:10.1080/0092623X.2017.1326190
American Society of Plastic Surgeons. Gender confirmation surgeries .
American Psychological Association. Transgender people, gender identity, and gender expression .
Colebunders B, Brondeel S, D'Arpa S, Hoebeke P, Monstrey S. An update on the surgical treatment for transgender patients . Sex Med Rev . 2017 Jan;5(1):103-109. doi:10.1016/j.sxmr.2016.08.001
IU School of Medicine surgeons perform a variety of gender affirming surgeries at our clinical affiliates for patients over 18 years of age. Our team will work with you to learn your goals and to develop an individualized plan to meet your needs. We currently offer:
chest reconstruction
breast augmentation
orchiectomy
vulvoplasty
vaginoplasty
voice surgery
facial feminization surgery
metoidioplasty
phalloplasty
hysterectomy and oophorectomy
Surgeons work together with other specialists to provide a coordinated, safe approach to medical and surgical care. All of our providers follow the World Professional Association for Transgender Health (WPATH) Standards of Care.
WPATH Standards of Care
Chest Reconstruction
Chest reconstruction is a common top surgery among transgender and non-binary patients who were assigned female at birth (AFAB). A plastic surgeon removes your mammary and fat tissue to create a masculine chest. The nipples are repositioned and resized, if desired.
Your care team will work closely with you to understand your goals and will recommend the best surgical approach to meet your needs. We offer several different types of chest reconstruction procedures, including double incision with nipple grafts, buttonhole and peri-aeriolar incisions (keyhole), using liposuction to help with contouring and prevention of “dogears.” The team will work with you to help pick the right technique at the time of your consultation.
Chest reconstruction surgery requires general anesthesia, and is performed as an outpatient procedure, meaning there is no hospital stay after surgery. After surgery you must wear a compression vest for at least four weeks. Drains are used for peri-aeriolar incision surgery. Foam bolsters are also placed on the chest to protect nipple grafts. The bolsters and/or drains will be removed one week after surgery. Most people are able to resume regular daily activities after one month with no restrictions.
Breast Augmentation
Breast augmentation is usually for transgender women and transfeminine spectrum non-binary people. It is also often called feminizing augmentation mammoplasty. We will give your chest a female appearance by placing implants underneath your natural breast tissue or pectoral muscle. Your care team will discuss the implant type (silicone or saline), size and shape to match your body and your desires during your consultation.
A small incision will be made in the crease underneath each breast or around the nipple. A pocket is made underneath the breast or pectoral muscle to give each breast a natural teardrop shape. Often, an additional incision will need to be made around the nipple to lift the breast and nipple into a more feminine position (mastopexy).
Some patients can benefit from fat grafting from the belly, hips or thighs in conjunction with implant surgery to achieve additional fullness in specific areas of the breast. This procedure is not currently covered by insurance.
Orchiectomy
The gender health team offers this surgery as part of gender affirming care for transfeminine patients. Orchiectomy (testicle removal) requires general anesthesia and is a low-risk, outpatient procedure, meaning there is no hospital stay after surgery.
A small incision is made in the scrotum along the median raphe (line in the midline of the scrotum). This approach does not affect future bottom surgery choices. It is common to see a small amount of bruising and swelling and experience mild discomfort. Rare risks include skin infection and a large bruise (hematoma). The recovery process is brief, and most patients are able to resume work and most daily activities within a few days. In those who do not want any further bottom surgeries, the scrotum can also be removed.
Vulvoplasty
The vulva is the outside part of the vagina. A vulvoplasty is a type of surgery that uses skin and tissue from a penis to create all of the outside parts of a vagina. Vulvoplasty does not create the internal vaginal canal.
The steps of a vulvoplasty are the same as a vaginoplasty. During a vulvoplasty, your provider will:
- create a clitoris out of the glans (head) of the penis
- create a labia minor and labia majora from skin on the penis and scrotum
- create the opening of the urethra so you can urinate
- create the introitus (opening of the vagina)
The only thing that’s different between a full vaginoplasty and a vulvoplasty is the internal part of the vaginal canal. This means you will not be able to insert a penis or toys into your vagina.
Vaginoplasty
Vaginoplasty involves creating a vagina, clitoris, labia majora, and labia minora. The procedure is effective both for people who have and those who have not had orchiectomy in the past. Removal of the testes is required as a part of vaginoplasty.
We perform vaginoplasty under general anesthesia. Most people spend six to seven full days in the hospital after surgery. Recovery from vaginoplasty can take up to three months, and requires intensive post-operative care. It is important to have both someone who can help take care of you after surgery as well as the privacy you need to take care of yourself.
You will need the privacy to dilate at least 30 minutes twice a day. Dilation involves inserting a medical dilator into the vagina. This is important because the vagina will close if people do not dilate.
The gender health team has pioneered an approach using the peritoneal lining, the tissue that lines your abdominal wall and covers most of the organs in your abdomen. The peritoneal lining is hairless and pink. While the peritoneal vaginoplasty does provide moisture, it is not self-lubricating. Patients will still need to use water-based lubricant for intercourse and dilation. This is a new procedure, and we are still gathering data about the procedure's long-term safety and efficacy.
How do I choose between vulvoplasty vs. vaginoplasty?
A vulvoplasty has a much easier recovery. It has a shorter hospital stay and does not require the lifelong maintenance of performing dilations to maintain the vagina.
Some patients know that they’re not interested in having vaginal intercourse. For these patients, a vulvoplasty may be a better choice.
After a vulvoplasty, you can still have orgasms through clitoral stimulation, just like with vaginoplasty. During a vulvoplasty, your surgeon will create a clitoris from the glans or head of the penis.
Metoidioplasty
Metoidioplasty is a procedure for patients who desire a penis. Your surgeon will remove the vagina in those that experience dysphoria from this organ, then release the clitoris from the ligament that holds it in place to lengthen it. Tissue grafting is used to create the penis. The result is a neophallus that can become erect. We are one of the only centers that offer this surgery at the same time as a hysterectomy.
We can perform this procedure with or without extending the urethra to allow urination out of the tip of the penis. The provider can also create a scrotum and insert testicular implants depending on your preference. After metoidioplasty, you will have a three to four day hospital stay. You will go home with a tube in your stomach to help drain your urine, as well as a catheter in the penis. Recovery can take six to eight weeks. Problems with urinary flow are very common, but often resolve on their own.
Phalloplasty
With phalloplasty, a surgeon will create a penis out of skin from somewhere on the body. Faculty at IU School of Medicine currently offer several different techniques. These include the radial forearm flap (RFF) phalloplasty, Anterolateral Thigh (ALT) flap, and Suprapubic.
Phalloplasty can involve several procedures in addition to the creation of a penis. We can close the front pelvic opening (vaginectomy). This often requires a hysterectomy as well.
Urethral lengthening creates a urethra that allows urination from the tip of the penis. Scrotoplasty creates a scrotum. We can perform one or both of these procedures during phalloplasty. Neither is required.
All options for phalloplasty require multiple surgical procedures. Some procedures involve a hospital stay. Some stages of phalloplasty require a hospital stay for up to a week, if not longer.
If you are interested in phalloplasty, we start with a complete consultation. IU School of Medicine providers will discuss the pros and cons of each procedure and help you decide what is right for you. Your care team will be there every step of the way to support you. It is our goal to make sure you feel comfortable and confident with your decision and satisfied with your results.
Hysterectomy and Oophorectomy
Hysterectomy is the removal of the uterus and ovaries. This surgery is part of gender affirming care for transmasculine patients. There is no hospital stay after surgery. Most people recover within two to four weeks. This can be in combination with metoidioplasty or top surgery.
You will have a complete consultation prior to scheduling surgery. At this appointment, your provider will discuss the surgery, review the role of removing the ovaries (oophorectomy) and the route of removing the uterus. For most patients a minimally invasive approach is offered via laparoscopy (making very small incisions on the abdomen).
Should I remove my ovaries?
This is a very personal decision. There is conflicting evidence on the role of the estrogen produced by the ovaries on the risk of heart disease or osteoporosis. Keeping an ovary can mean that you continue to experience cyclic hormonal symptoms, even without a uterus or menstruation.
The ovaries contain eggs for reproduction. Even without a uterus you can still use the eggs for a pregnancy. If you are interested in having children it may be beneficial to keep your ovaries. Your provider will discuss these options in your initial visit and in the surgical planning.
It is likely there is little or no benefit to keeping the ovaries for patients who are not interested in future reproduction and who intend to continue on long term testosterone therapy until at least age 50.
Photographs
Do I need a referral to see a specialist? Learn more here . Explore the Department Directory Learn more about Telehealth Appointments Protect Yourself from West Nile Virus
How to schedule your APPOINTMENT at Denver Health: CURRENT PATIENTS: Login to MyChart to schedule appointments or call 303-436-4949 . NEW PATIENTS: Schedule an appointment online or call 303-436-4949 . NEED CARE? Schedule a Virtual Urgent Care appointment or click here to find an Urgent Care clinic .
MyChart Login
Login to MyChart
MyChart for Mobile
Download the MyChart mobile app for access to your healthcare information. Managing your healthcare has never been more simple. Download for iPhone and Android .
MyChart Sign Up
Learn about MyChart features , and sign up for an account .
Virtual Urgent Care Now Available for Denver Health MyChart Users
Denver Health MyChart users can now have a virtual urgent care visit with one of our expert providers. It’s easy and convenient to get the urgent care you need from the comfort of your home, using your smartphone, tablet or computer.
Click here for more details

- Departments & Services
- Conditions & Treatments
- Our Locations
- Find a Provider
- Pharmacy / Prescriptions
- Pay my bill
- Main Campus (303) 436-6000
- Appointments (303) 436-4949
- Lean Academy 855-888-5326
- Nurseline (303) 739-1211
- Pharmacy (303) 389-1390
- Telehealth (303) 436-4949
Contact LGBTQ Patient Navigator
Hours of operation, vaginoplasty.
Learn more about gender affirmation surgery:
Interested in this surgery?
Please complete the following surgical interest form and submit it to our LGBTQ+ Services team.
Surgical Interest Form
Overview of Vaginoplasty
Vaginoplasty is a gender-affirming, feminizing, lower surgery to create a vagina* and vulva (including mons, labia, clitoris, and urethral opening) and remove the penis, scrotal sac and testes.
What is the procedure for vaginoplasty?
- The scrotum and testes are removed.
- The glans is made into a clitoris.
- Space for the vagina is dissected between the bladder and the rectum.
- Skin from the shaft of the penis* is inverted to create the inner walls of your vagina.
- Extra skin may be taken from the scrotum* to line your vagina. The hair roots on the skin graft will be cauterized.
- The urethra is shortened.
- Vulva are created using scrotal and urethral tissue.
- A temporary urinary catheter is inserted into the bladder.
- A temporary prosthesis/stent is inserted in the vagina.
Do I need to have hair removal before vaginoplasty ?
Hair removal is highly encouraged and recommended prior to penile inversion vaginoplasty (full depth vaginoplasty). The scrotal skin will be used to make the neo vagina. If you do not do hair removal, there will be hair inside the vagina. This can make post operative care more difficult and place you at increased risk for post op infection. The surgeon will not do any hair removal during the surgical procedure. Ask an LGBTQ+ Patient Advocate about resources for hair removal.
** Hair removal is not required for minimal depth vaginoplasty.
Do I need to stop taking hormones before vaginoplasty?
Your surgeon will discuss this with you at your pre-visit.
How long will my hospital stay be?
You will be admitted to the hospital for 3 days following your surgery.
What medications will I be prescribed after surgery?
You will likely receive painkillers and antibiotics to prevent infection. Your surgeon will provide you with a list of medications to avoid for the first month. Do not resume taking hormones until your surgeon has advised you to do so.
What should I expect during the healing process?
- Bleeding during the first 48 hours following surgery
- Itchiness and small shooting electrical sensations as nerve endings heal
- Bruising can spread from your belly to your thighs and takes 3-4 weeks to settle down
- A bit of spraying when you urinate which usually improves over time
- Swelling of your labia which can take up to 6 weeks to resolve
- Brown/yellow vaginal discharge for the first 6-8 weeks
- Your vulva will approach its final appearance at 4 months
- Numbness that will improve over the first few months, and can take up to 18 months to resolve
- Red, dark pink or purple scars that take up to one year to fade
What will my post-operative routine look like?
A urinary catheter will be in place for the first five days after surgery to allow you to pass urine while your urethra heals. Sometimes people still aren’t able to urinate when the catheter comes out, due to swelling around the urethra. This situation can easily be resolved with a second catheter that will remain in place for a week and be removed by your physician when you go home. You’ll be encouraged to drink lots of fluids to prevent urinary tract infections.
A prosthesis/stent will be placed in your vagina during surgery and will remain there for 5 days to make sure the skin grafts stay in place. When it’s removed, you will begin dilating and douching. A vaginal douche is a process of rinsing the vagina by forcing water or another solution into the vagina to flush away vaginal discharge or other contents. You will be given a set of vaginal dilators of different sizes. You’ll use them to maintain vaginal depth and width and promote healing.
Initially, you’ll dilate several times a day and over the first year the amount of time spent dilating will be gradually reduced. After you have completely healed, you will only need to dilate about once a week. The frequency depends on how much penetrative sex you have. For the first two months after surgery, you will take sitz baths. A sitz bath is a way to soak your surgical site to keep it clean. You’ll want to wear thin maxi pads for about one month to manage post-operative bleeding and discharge.
What check-ups will be needed after my hospital stay?
The number of check-ups needed varies from person to person. If possible, see your primary care provider about a week after and then every 2-4 weeks for the first few months. When you visit your surgeon or primary care provider, they should check your surgical sites to make sure there are no infections or wound healing problems. They will ask questions about dilating, bleeding, vaginal discharge, fever, pain and how you are feeling emotionally and physically.
How long will it take for me to get back to my usual activities?
Recovery time varies from person to person, so always follow the advice of your surgeon. Many people begin to feel more comfortable during the second week after their surgery. You’ll need plenty of rest in the first two weeks. It’s common to be back to your usual activities, including work, in six to eight weeks. Some activities, such as driving, heavy lifting, exercise, sex and soaking in hot tubs, may be restricted in the post-operative period. Your surgeon will give you advice about when it is okay to resume these activities. Complete recovery can take up to one year.
What complications are associated with vaginoplasty?
All surgical procedures involve some risks, including negative reactions to anesthesia, blood loss, blood clots and infection. These complications can, in extreme cases, result in death. It’s important to discuss these risks in detail with your surgeon. Your surgical care team will take a wide variety of steps to prevent these problems, detect them if they arise and respond to them appropriately.
They will also inform you about what you can do to minimize your risks. The list below includes some of the complications associated with vaginoplasty in particular. It does not replace a thorough consultation with your surgeon.
This is when blood collects in the surgical site, causing pain, swelling and redness. Smaller hematomas can be drained, but larger ones require removal through surgery.
Abscess Formation
An abscess is a collection of pus. It’s caused by a bacterial infection. It can be treated with antibiotics or drained by the surgeon.
This is when clear fluid accumulates in the surgical site. Small seromas may need to be aspirated, or sucked out, once or more by the surgeon.
Loss of Sensation
You may have small areas of numbness. Your ability to achieve orgasm could decrease. Loss of clitoris is a remote possibility.
Rectovaginal fistula
This is when an abnormal path between the rectum and vagina is created. Surgery would be needed to correct this.
May be correctable with various treatments, including additional surgery.
Injury to the Nerves or Muscles in the Legs
Can lead to numbness or a change of sensation in the skin of the legs. In very rare cases, it can lead to difficulty moving the leg which needs correction through surgery.
Unsatisfactory Size or Shape of the Vagina, Clitoris or Labia
Outcomes that are quite different from what was expected may require surgical revision.
Urological Complications
Examples include:
- fistulas (flow of urine to areas other than urethra opening)
- stenosis (narrowing of the urethra, causing difficulties urinating)
- strictures (blockage of the urethra, causing difficulty urinating).
It is common to have spraying or dribbling when urinating until your swelling settles down. If these problems don’t resolve on their own, they may require additional surgery.
- 0 && newsLoaded" class="" data-id="{044698B9-FA04-4636-994D-47662155601F}" ref="news"> News
- 0 && blogLoaded" class="" data-id="{9AB9C6CB-06BD-4D71-867F-FAB69D88F93C}" ref="blog"> Blog Articles
- 0 && storiesLoaded" class="" data-id="{71E64EA2-1956-4F7C-A67D-579E0BB54378}" ref="stories"> Patient Stories
- Apr 27 Boot Camp for New Dads ®
- May 1 Labor and Delivery Tour for Expectant Families
- May 8 Labor and Delivery Tour for Expectant Families
- May 11 Labor and Delivery Tour for Expectant Families
- The Most Beautiful Trans Models on Instagram (Of the World)
- Dating an Only Child: 10 Things You Should Know
- Boost your Trans Dating Confidence with those simple tips
- Reasons why you should consider dating someone outside of your type
- Meet Thai Transgender Women: The Thailand Trans Dating Guide
- What is CatFishing and 10 Tips on how to spot a Catfish on a Dating Site
- 20 Dating Red Flags You Should Look Out For Early in a Relationship
- 10 Tips on How to Flirt Online to Find Love and Make a Good First Impression

Gender-Affirming Surgery (SRS): Guide to Transgender Surgery
Are you considering plastic surgery or sex reassignment surgery, or just curious about what it entails? You've come to the right place! In this article, we'll explore the basics of SRS, its history, and why it can be a life-changing option for some individuals.
Download the PDF file:
Table of Contents
Definition of SRS
Sex Reassignment Surgery (SRS), also known as gender affirmation surgery or gender-confirming surgery, is a medical procedure that alters an individual's physical characteristics to align with their gender identity. In other words, it's a way to help transgender people feel more comfortable in their bodies.
Brief history of SRS
Did you know that the history of SRS dates back to the early 20th century?
The first recorded procedures were performed in the 1930s, with pioneering work by surgeons like Dr. Magnus Hirschfeld in Germany.
However, it wasn't until the 1950s and 1960s that SRS gained more attention with a follow-up study. Thanks to high-profile cases like Christine Jorgensen , the first widely known person to have the surgery.


Understanding gender dysphoria
Gender dysphoria is a deep and persistent discomfort with one's assigned gender at birth. It can cause significant emotional distress, anxiety, and depression. For some individuals, living with gender dysphoria is unbearable, and that's where SRS comes into the picture.
Why SRS is a viable option for some individuals
Not all trans individuals choose to undergo confirmation surgery (genital surgery), but for those who do, it can provide immense relief from gender dysphoria. By physically transitioning, they can feel more at ease in their bodies and experience improved mental health. It's important to remember that SRS is just one of many steps in an individual's transition journey, and it may not be the right choice for everyone.
Preparing for transgender surgery
So, you're considering bottom surgery or top surgery – what now? There are several steps to take before undergoing the surgery, and we'll discuss each of them below.
Psychological evaluations and counseling
Before surgery, the transgender patient undergoes a psychological evaluation to ensure you fully understand the implications of the surgery and are emotionally prepared for it. Counseling can also help address any concerns or fears you might have about the procedure and the changes it brings.
Physical evaluations and medical clearance
Your overall health plays a significant role in determining your eligibility for SRS. A thorough physical evaluation and medical clearance from your healthcare provider are necessary to ensure you're in good health and able to handle the surgery and recovery process.
Stay tuned for more sections on preparing for SRS, the surgical procedure itself, life after SRS, and the challenges and controversies surrounding it.
Hormone therapy
Before undergoing SRS, many transgender individuals choose to start hormone therapy. This involves taking prescribed hormonal therapy to help bring about physical changes that align with their gender identity. For example, transgender women may take estrogen, while transgender men may take testosterone. Hormone therapy usually begins several months or even years before SRS, and it's essential to work closely with your healthcare provider to ensure you're on the right treatment plan.
Social and legal considerations
Transitioning is not just about the physical changes; it also involves social and legal aspects. Before SRS, it's essential to consider how your transition will affect your relationships, work, and other aspects of your life. You may need to update your name, gender marker, and other documentation, as well as navigate the legal requirements for these changes.
Choosing a surgeon and surgical team
Selecting the right surgeon and surgical team is crucial to ensuring the best possible outcome for your SRS. Look for a surgeon with experience in performing the specific procedure you're seeking and consider factors like their qualifications, success rates, and patient testimonials. Don't be afraid to ask questions and discuss your concerns with potential surgeons to find the best fit for you.
Understanding the risks and benefits
As with any surgery, SRS carries both risks and benefits. Potential complications can include infection, bleeding, and issues with anesthesia. However, many people experience significant improvements in their mental health and overall well-being after undergoing SRS. It's crucial to weigh the risks against the benefits and make an informed decision about whether SRS is the right choice for you.
The Surgical Procedure - Feminization surgery
Now that you have a better understanding of what to expect before SRS, let's dive into the surgical procedure itself.
Types of gender-affirming procedures (MTF and FTM)
Sex Reassignment Surgery can be broken down into two main categories: male-to-female (MTF) and female-to-male (FTM) procedures. MTF (penile, scrotal & urethra) surgeries may include vaginoplasty, breast augmentation, and facial feminization, while FTM (genitalia) surgeries can involve phalloplasty, metoidioplasty, chest reconstruction, and more. The specific procedures you choose will depend on your goals and personal preferences.
Explanation of the surgical process
While the details of each reconstructive procedure will vary, the overall goal is to reshape the body's sexual characteristics to align with the individual's gender identity. Surgeons utilize advanced techniques and specialized knowledge to ensure the best possible outcomes. It's important to discuss your expectations and concerns with your surgeon, so they can provide a clear understanding of what the surgical process will entail.
Risks and potential complications
As mentioned earlier, SRS carries certain risks and potential complications. These can include infection, excessive bleeding, issues with anesthesia, and dissatisfaction with the results. It's essential to be aware of these risks and discuss them with your surgeon to make an informed decision about moving forward with SRS.
Pain management and recovery
Pain management and a smooth recovery are crucial aspects of the SRS process. Your surgical team will help you manage pain with medications and other techniques, and they'll provide guidance on how to care for your surgical site to minimize the risk of complications. Recovery times vary depending on the specific procedure, but it's essential to follow your surgeon's instructions and attend all follow-up appointments to ensure a successful outcome.
In the next sections, we'll explore life after SRS, the challenges and controversies surrounding it, and how to seek support and resources.
Life after Sex Change
Congratulations, you've made it through the surgery! But what comes next? In this section, we'll discuss the postoperative physical and emotional changes you can expect after surgery and provide some tips for managing expectations and seeking support.
Physical and emotional changes
After surgery, you'll likely notice a range of physical changes that align with your gender identity. These changes can be both exciting and challenging to navigate. Emotionally, you may experience a mixture of relief, happiness, and anxiety as you adjust to your new body. It's essential to be patient with yourself and give yourself time to heal and adapt to these changes.
Managing expectations
It's important to have realistic expectations about life after surgery - and keep standards of care in mind. While the surgery can significantly improve your quality of life and alleviate gender dysphoria, it may not solve all of your problems. Keep in mind that everyone's transition journey is unique, and it's essential to focus on your personal growth and self-acceptance as you move forward.
Support and resources
A strong support system is vital during your transition journey. Reach out to friends, family, and other transgender individuals who can provide encouragement and advice. There are also numerous organizations and online communities that offer resources and support for those who have undergone SRS. Some helpful resources include the World Professional Association for Transgender Health (WPATH) , GLAAD (Gay & Lesbian Alliance Against Defamation) , the National Center for Transgender Equality , Trans Lifeline , and Point of Pride . Don't hesitate to seek help when you need it, as these organizations can offer valuable guidance and assistance throughout your journey.
Sexual function and fertility
One common concern among individuals considering SRS is how the surgery will affect their sexual function and fertility. While many people report satisfying sexual experiences after the procedure, it's important to discuss your specific concerns with your surgeon. In terms of fertility, you may want to consider options like sperm or egg preservation before undergoing the procedure if you plan to have biological children in the future.
Legal considerations and documentation
After surgery, you'll need to update your legal documents to reflect your new name and gender, if you haven't already done so. This process varies depending on your location, so be sure to research the specific requirements in your area. Some common documents that may need updating include your driver's license, passport, and birth certificate.
Challenges and Controversies
Sex Reassignment Surgery is not without its challenges and controversies. In this section, we'll explore some of the issues faced by transgender individuals seeking surgery, as well as the broader debates surrounding the procedure.
Religious and cultural attitudes
SRS can be a contentious topic in some religious and cultural communities. It's essential to be aware of the attitudes and beliefs of those around you, as they may impact your support system and access to resources. Remember, your transition journey is personal, and it's crucial to prioritize your well-being and happiness above all else.
Access to healthcare
Unfortunately, access to healthcare, can be limited for transgender individuals due to factors like insurance coverage, geographic location, and provider availability. It's essential to research your options and advocate for your healthcare needs as you navigate the complex world of medical care.
Financial considerations
It can be costly, and not all insurance plans cover the procedure or facial feminization surgery. Be prepared to explore various financing options, such as personal savings, loans, or crowdfunding, to help cover the cost of your surgery.
Transphobia and discrimination
Transgender individuals often face discrimination and transphobia in various aspects of life, from healthcare to employment. It's important to know your rights and seek support from allies and organizations that advocate for transgender rights and well-being.
Debates about medical necessity and ethics
While many medical professionals consider SRS to be a medically necessary treatment for gender dysphoria, some individuals and organizations argue against the procedure on ethical grounds. It's important to be aware of these debates and to stand firm in your conviction that your transition journey is a deeply personal and valid choice.
Conclusion on sex reassignment surgery
In this article, we've covered a wide range of topics related to Sex Reassignment Surgery, from its history and purpose to the challenges faced by those who seek it. As you consider whether SRS is the right choice for you, remember that every individual's journey is unique, and there is no one-size-fits-all approach.
Summary of key points
To recap, we've discussed the definition of SRS, its history, and its role in alleviating gender dysphoria. We've also explored the steps involved in preparing for the surgery, the surgical procedure itself, life after SRS, and the challenges and controversies surrounding the topic.
Encouragement to seek more information
This article is just a starting point for understanding SRS. We encourage you to seek out additional information, talk to medical professionals, and connect with others who have gone through the process. The more you learn, the better equipped you'll be to make informed decisions about your transition journey.
Emphasis on the importance of individual choice and autonomy
Finally, it's crucial to remember that your transition journey is deeply personal and should be guided by your needs, desires, and sense of self. Whether you choose to pursue SRS or not, the most important thing is to prioritize your well-being and happiness. Embrace your unique path and celebrate your authentic self
Frequently Asked Questions about Sex Reassignment Surgery
Embarking on the journey of sex reassignment surgery can feel overwhelming, and it's natural to have questions about the process. In this section, we've gathered some of the most common questions related to SRS and provided clear, friendly answers to help you better understand this life-changing procedure. Whether you're considering SRS for yourself or seeking to support a loved one, we hope these answers will provide valuable insights and guidance.
What is the success rate of SRS?
Success rates for SRS vary depending on the specific procedure, but many people report high levels of satisfaction with their results. It's crucial to choose a skilled and experienced surgeon to improve the chances of a successful outcome.
Can SRS be reversed?
SRS is generally considered irreversible, as it involves the removal or alteration of certain tissues. However, in some cases, revisions or additional surgeries may be possible to address specific concerns or complications.
How long does recovery take after SRS?
Recovery times after SRS can vary, but generally, you can expect a recovery period of several weeks to a few months, depending on the specific procedure. Following your surgeon's instructions and attending follow-up appointments are essential for a successful recovery.
Is SRS covered by insurance?
Insurance coverage for SRS varies depending on the insurance plan and the specific procedure. Some plans cover SRS as a medically necessary treatment, while others may not. It's essential to review your insurance policy and discuss your options with your healthcare provider.
Can someone who is non-binary or genderqueer undergo SRS?
Non-binary or genderqueer individuals may choose to undergo SRS or other gender-affirming procedures based on their personal preferences and goals. It's essential to work with a supportive healthcare team that understands and respects your unique identity and needs.
How can I support a loved one who is considering SRS?
To support a loved one considering SRS, educate yourself about the procedure, listen to their concerns, and offer emotional support. Be there for them throughout the process and connect them with resources and support groups
What are some alternatives to SRS for gender affirmation?
Some alternatives to SRS for gender affirmation include hormone therapy, social transition (such as changing one's name, pronouns, and clothing), and non-surgical procedures like facial feminization surgery or chest binding. Each person's journey is unique, and it's essential to explore various options to find the best path for you.
What is the youngest age someone can undergo SRS?
The youngest age someone can undergo SRS varies depending on the country and specific regulations. In general, most surgeons require patients to be at least 18 years old to provide informed consent. However, some countries or individual surgeons may have different age requirements.
How does SRS affect hormone therapy?
SRS affects hormone therapy by reducing or eliminating the need for certain hormone medications. For example, a trans woman who has had vaginoplasty may no longer need anti-androgens, while a trans man who has had a hysterectomy may require lower doses of testosterone. It's important to work closely with your healthcare provider to adjust your hormone therapy as needed after SRS.
Are there any long-term health risks associated with SRS?
Long-term health risks associated with SRS are generally low, particularly when the surgery is performed by an experienced surgeon. However, potential risks can include infection, scarring, and complications related to anesthesia or surgical technique. It's essential to discuss your specific risks with your surgeon and follow post-operative care instructions to minimize potential complications.
As a proud transgender woman, I'm an award-winning blogger blending my unique life experiences with a Bachelor's degree in Communication. Known for my linguistic expertise and dynamic writing style, I specialize in CBD, SEO, music, technology, and digital marketing sectors.
Related Posts
Medical side of mtf male to female transition: hormone therapy explained, gender identity: understanding various gender identities, hormone replacement therapy (hrt) for trans women.
Type above and press Enter to search. Press Esc to cancel.
Long-term Outcomes After Gender-Affirming Surgery: 40-Year Follow-up Study
Affiliations.
- 1 From the Department of Plastic and Reconstructive Surgery.
- 2 School of Medicine.
- 3 Department of Obstetrics and Gynecology.
- 4 Department of Urology.
- 5 Department of Psychiatry and Neurobehavioral Sciences, University of Virginia, Charlottesville, VA.
- PMID: 36149983
- DOI: 10.1097/SAP.0000000000003233
Background: Gender dysphoria is a condition that often leads to significant patient morbidity and mortality. Although gender-affirming surgery (GAS) has been offered for more than half a century with clear significant short-term improvement in patient well-being, few studies have evaluated the long-term durability of these outcomes.
Methods: Chart review identified 97 patients who were seen for gender dysphoria at a tertiary care center from 1970 to 1990 with comprehensive preoperative evaluations. These evaluations were used to generate a matched follow-up survey regarding their GAS, appearance, and mental/social health for standardized outcome measures. Of 97 patients, 15 agreed to participate in the phone interview and survey. Preoperative and postoperative body congruency score, mental health status, surgical outcomes, and patient satisfaction were compared.
Results: Both transmasculine and transfeminine groups were more satisfied with their body postoperatively with significantly less dysphoria. Body congruency score for chest, body hair, and voice improved significantly in 40 years' postoperative settings, with average scores ranging from 84.2 to 96.2. Body congruency scores for genitals ranged from 67.5 to 79 with free flap phalloplasty showing highest scores. Long-term overall body congruency score was 89.6. Improved mental health outcomes persisted following surgery with significantly reduced suicidal ideation and reported resolution of any mental health comorbidity secondary to gender dysphoria.
Conclusion: Gender-affirming surgery is a durable treatment that improves overall patient well-being. High patient satisfaction, improved dysphoria, and reduced mental health comorbidities persist decades after GAS without any reported patient regret.
Copyright © 2022 Wolters Kluwer Health, Inc. All rights reserved.
- Follow-Up Studies
- Gender Dysphoria* / surgery
- Sex Reassignment Surgery*
- Transgender Persons* / psychology
- Transsexualism* / psychology
- International edition
- Australia edition
- Europe edition

Transgender journey: recovering from surgery
W hen I got the date for my sex reassignment surgery, I wasn't so worried about the operation itself (I'd be asleep, right?) as its aftermath: how I was going to look after myself during the two months it would take to recover? I called my parents and immediately my mother offered to take care of me at the family home. I'd never felt so glad or relieved: the Gender Identity Clinic suggest full-time care for at least the first two weeks, and getting it from my parents (especially my mother, a former district nurse) meant that they would be reassured that I was fine, while I would benefit from rest, relaxation and plenty of home cooking.
The day after my discharge from Charing Cross Hospital, my father drives me back to Horley, Surrey, where I will convalesce in my old bedroom. As he does so, the post-surgical pain increases dramatically. I try to be stoic: it isn't going away for some time, so I decide to get through the journey, sleep and see how I feel in the morning. Much worse, is the answer: the sight and smell of the neovagina instantly confirms that I've contracted an infection.
My father takes me to the nearest Urgent Treatment Centre. The nurse has never encountered my circumstances before, and warns that as the Accident & Emergency unit at East Surrey Hospital may not be able to treat me, I might need to return to Charing Cross. This would mean a long drive back to London in searing heat, two days before the Olympics. I hold back tears as we contact the GIC's nurse specialist, who says that this is not uncommon and can be handled with antibiotics. After inspection by a senior doctor, who says that the bruising above the wound has become infected, I am sent home with new medication.
The following Monday, the addition of new drugs to my painkiller regime completely floors me - and my energy was already low as my body strived to heal itself. I spend the entire afternoon in bed, having slept little at night due to the pain and the pills, which warp my dreams into vivid nightmares for weeks after the operation. My mother and I decide to stop the antibiotics slightly early; from there, my recovery is slow, but steady.
My movement is limited, as lying down hurts far less than sitting, but it does at least provide quiet time to read and watch films. My mother encourages me to go outside, but 10 days after surgery I can barely reach the top of our road. There are sharp pains as nerve endings reconnect; a dull, throbbing ache and an unbearable pushing sensation at the base of the affected area, which stay constant for weeks; and plenty of discharge for the first month. This is alleviated by regular baths, which are pleasant but boring.
To pass the time, I listen to the radio: one afternoon, the DJ plays Joy Division's Love Will Tear Us Apart , which was constantly on my stereo during my alienated youth. As I hear its opening bars, the entire transition, from my childhood gender dysphoria to this pain-filled moment in the house where I grew up, 20 years later, replays itself in my mind, and suddenly I'm in waves of cathartic tears.
"And yet there's still this appeal that we've kept through our lives …"
This feels like a watershed: gradually things improve. Being with my parents changes my relationship not just with them, but my home town. One day a friend visits and I take her on a tour: with just an afternoon and almost incapacitated, I still manage to show her the entire centre twice. My favourite feature is the sign in the bookshop: "Look! Fifty Shades of Grey in stock now." I dread to imagine the letters to the local paper .
Three and a half weeks post-surgery, I take another friend to watch Horley Town play Holmesdale in the FA Cup. We stand behind the goal and when Horley's winger shanks a cross into touch, I'm nearest the ball. Instinctively I run to throw it back. I soon wish I hadn't, remembering that the pain will take weeks if not months to disappear completely.
Mentally, it's a strange time too. At first the discomfort and discharge stop me from forming a positive relationship with my altered body, and my constant urge to be active sits badly with my inability to walk more than a few hundred metres. Further constrained by the need to dilate three times daily, watching the world pass by on Twitter and television, I remind myself that this is temporary: soon, I can put it all behind me.
Coming back to London, I slowly step up my activity, meeting friends in local cafes and testing my pain barrier in going to watch Norwich City start the season at Fulham. Despite City's abject hammering , it feels wonderful to return to one of the mainstays of my social life.
Just as importantly, I start to familiarise myself with my changed body, getting used to the sight of it in the mirror. Then, after several weeks, the dilation stops being painful and becomes pleasurable, at least at times – the discovery of sexual sensation is another huge landmark, and finally I'm excited not just about returning to my pre-surgical normality but about discovering a post-surgical one.
Two months after surgery, I make a final, brief visit to the surgical team at the Clinic, who check my health and administer some silver nitrate to deal with the granulation tissue that has developed during the healing process. Before I leave, I schedule my last appointment with the psychiatric team, where we can address the final question: how do I feel?
- Health & wellbeing
- A transgender journey
- Transgender
Comments (…)
Most viewed.
- FIND A PROVIDER
I'm a Candidate
I'm a Provider
Log In / Sign Up
I'm a candidate
Provider login
I'm a provider
List your practice
FTM Gender Confirmation: Genital Construction
The specifics, the takeaway.
Download the app
As part of a transgender individual’s transition, genital reassignment surgery alters female genitalia into male genitalia.
Written By: Erin Storm, PA-C
Published: October 07, 2021
Last updated: February 18, 2022
- Procedure Overview
- Ideal Candidate
- Side Effects
- Average Cost
thumbs-up Pros
- Can Help Complete A Gender Affirmation Journey
thumbs-down Cons
- Potentially Cost Prohibitive
Invasiveness Score
Invasiveness is graded based on factors such as anesthesia practices, incisions, and recovery notes common to this procedure.
Average Recovery
Application.
Surgical Procedure
$ 50000 - $ 100000
What is a female to male (FTM) gender reassignment surgery?
Female to male (FTM) gender reassignment surgery is also known as sex reassignment surgery (SRS), genital construction, and generally as gender confirmation surgery. These plastic surgery procedures are used by transgender patients to remove and alter female genitalia into traditional male genitalia.
Plastic surgeons will usually perform a hysterectomy and salpingo-oophorectomy to remove the uterus and ovaries. A vaginoplasty or vaginectomy will close the vagina, the erectile tissue of the clitoris is released and with the mons portion of the pubic area a neo-phallus is created (phalloplasty or metoidioplasty). The labia majora then become the scrotum (scrotoplasty), bilateral testicular implants are placed, and finally the urethra is lengthened through the newly created penile tissue.
Typically gender reassignment surgery is performed as a last step in a transgender individuals transition journey. Guidelines on standards of care from The World Professional Association for Transgender Health (WPATH) state candidates must have letters of recommendation from their mental health professional and healthcare provider, have been living full time as a man for one year, and have completed one year of hormonal therapy to be eligible.
Information on facial masculinization surgeries, top surgeries (like a mastectomy), and other female to male gender affirming surgeries as part of a gender transition for transmen can be found in our comprehensive guide to FTM gender affirmation solutions .
What concerns does a FTM gender reassignment surgery treat?
- Transmasculine Bottom Surgery & Genital Construction : Female to male gender reassignment surgery creates male genitalia that are aesthetically authentic and functional.
Who is the ideal candidate for a FTM gender reassignment surgery?
The ideal candidate for FTM gender reassignment surgery is a transgender man seeking to complete his physical embodiment of his gender identity. This reconstructive genital surgery creates functioning male genitalia. FTM gender reassignment surgery is not recommended for those who have not been on hormone therapy for one year, have not been living full time as a man for one year, do not have letters of recommendation from their mental health provider and physician, children under the age of 18, and those with certain chronic medical conditions.
What is the average recovery associated with a FTM gender reassignment surgery?
Most patients experience four to six weeks of recovery time following a FTM gender reassignment surgery. Patients can expect bruising, swelling, and tenderness following the procedure. A urinary catheter is typically used for two to three weeks.
What are the potential side effects of a FTM gender reassignment surgery?
Possible side effects following a FTM gender reassignment surgery include bleeding, swelling, bruising, incision site infection, altered sensation, difficulty urinating due to strictures, difficulty with sexual function, prolonged edema, and complications from anesthesia or the procedure.
What can someone expect from the results of a FTM gender reassignment surgery?
The results of FTM gender reassignment surgery are permanent. This procedure creates functional male genitalia and removes all female genitalia.
What is the average cost of a FTM gender reassignment surgery?
What to expect.
A FTM gender reassignment surgery creates male genitalia. Here is a quick guide for what to expect before, during, and after a FTM gender reassignment surgery:
Before Surgery
- Prophylactic antibiotics or antivirals may be prescribed
- Stop taking blood thinning medications two weeks prior to surgery. Blood thinners may include, Advil, Tylenol, Aspirin, and prescription anticoagulants
- Stop smoking four weeks prior to the procedure and continue cessation for four weeks post op
- No alcohol two days prior to the procedure
- Do not eat or drink six hours before
During Surgery
- General anesthesia
- A hysterectomy, oophorectomy, and vaginoplasty are performed
- The clitoris is released from suspensory ligaments
- The neo-phallus and scrotum are created with existing tissues
- Testicular implants are placed - The urethra is lengthened
Immediately After Surgery
- Swelling, bruising, and tenderness
1 - 30 Days After Treatment & Beyond
- Resume most activities after a few days
- Swelling typically resolves within a few weeks
- Avoid strenuous activity for two to four weeks
- Remove urinary catheter after two to three weeks
Result Notes
- Results are permanent
- Proper aftercare will ensure optimal results
- Any revisions needed are typically not performed until six months after the initial procedure
Gender confirmation surgeries for transgender individuals are an important component of transgender health and in creating an embodied gender identity. Gender reassignment surgery allows transgender men who feel it is a part of their transition to more fully embrace their gender identity.
To learn more about our content creation practices, visit our Editorial Process page .
Source List
AEDIT uses only high-quality sources, including peer-reviewed studies, to support the facts within our articles. Read our editorial process to learn more about how we fact-check and keep our content accurate, reliable, and trustworthy.
- American Society of Plastic Surgeons Gender Confirmation Surgeries plasticsurgery.org
- Karel E Y Claes Chest Surgery for Transgender and Gender Nonconforming Individuals PubMed.gov ; 2018-07-02
Related Procedures

FTM Gender Confirmation Solutions

Adam’s Apple Enhancement

FTM Gender Confirmation: Facial Masculinization

FTM Gender Confirmation: Transmasculine Top & Bottom Surgeries
View all procedures
Learn More About FTM Gender Confirmation: Genital Construction in The AEDITION

Gender Transitioning And Skincare: Taking Care Of Your Changing Face
Side effects of hormone therapy often show up on the skin in the form of acne, pigmentation, and uneven skin texture. Here’s what you need to know about the most common skin concerns and treatment options.

Everything You Need To Know About Clavicle Surgery
Clavicle (a.k.a. collarbone) surgery is growing in popularity among patients seeking to change the length and prominence of the bone, enhance their décolleté, and improve the overall proportion of the body.

Finding The Right Plastic Surgeon, Dermatologist, Or Cosmetic Dentist
When considering a cosmetic procedure, it is so important to find the right doctor for you.
Discover more articles

‘Try on’ aesthetic procedures and instantly visualize possible results with AEDIT and our patented 3D aesthetic simulator.
Find Top Aesthetic Providers Near You
Providers by locations.
- Alpharetta, GA Providers
- Baltimore, MD Providers
- Boston, MA Providers
- Fort Lauderdale, FL Providers
- Glenview, IL Providers
- Lone Tree, CO Providers
- Metairie, LA Providers
- Minneapolis, MN Providers
- More Locations
- New Haven, CT Providers
- Scottsdale, AZ Providers
- Southfield, MI Providers
- Springdale, AR Providers
- Washington, DC Providers
- West Hollywood, CA Providers
Providers by Specialties
- Cosmetic Dentistry Providers
- Cosmetic Dermatology Providers
- Cosmetic Surgery Providers
- Dermatologic Surgery Providers
- Dermatology Providers
- Facial Plastic and Reconstructive Surgery Providers
- General Surgery Providers
- Hair Restoration Surgery Providers
- Head and Neck Surgery Providers
- Medspa Providers
- More Procedures
- Oculoplastic Surgery Providers
- Plastic and Reconstructive Surgery Providers
- Vaginal Rejuvenation Providers
Providers by Procedures
- Acne Scar Treatment Providers
- Acne Treatment Providers
- Birthmark Removal Providers
- Blepharoplasty Providers
- Botox Providers
- Brow Lift Providers
- Buccal Fat Removal (Cheek Reduction) Providers
- Cheek Augmentation (Cheek Implants) Providers
- Cheek Surgery Providers
- Chemical Peels Providers
- Chin Surgery (Mentoplasty) Providers
- Dental Treatments Providers
- Dermabrasion Treatment Providers
- Dermal Fillers & Injectables Providers
- More Specialties
- Alzheimer's & Dementia
- Asthma & Allergies
- Atopic Dermatitis
- Breast Cancer
- Cardiovascular Health
- Environment & Sustainability
- Exercise & Fitness
- Headache & Migraine
- Health Equity
- HIV & AIDS
- Human Biology
- Men's Health
- Mental Health
- Multiple Sclerosis (MS)
- Parkinson's Disease
- Psoriatic Arthritis
- Sexual Health
- Ulcerative Colitis
- Women's Health
- Nutrition & Fitness
- Vitamins & Supplements
- At-Home Testing
- Men’s Health
- Women’s Health
- Latest News
- Medical Myths
- Honest Nutrition
- Through My Eyes
- New Normal Health
- 2023 in medicine
- Why exercise is key to living a long and healthy life
- What do we know about the gut microbiome in IBD?
- My podcast changed me
- Can 'biological race' explain disparities in health?
- Why Parkinson's research is zooming in on the gut
- Health Hubs
- Find a Doctor
- BMI Calculators and Charts
- Blood Pressure Chart: Ranges and Guide
- Breast Cancer: Self-Examination Guide
- Sleep Calculator
- RA Myths vs Facts
- Type 2 Diabetes: Managing Blood Sugar
- Ankylosing Spondylitis Pain: Fact or Fiction
- Our Editorial Process
- Content Integrity
- Conscious Language
- Health Conditions
- Health Products
What transgender men can expect after gender-affirming surgery

Transgender men may choose to have gender-affirming surgery, such as metoidioplasty or phalloplasty. These may provide sensations and functions including erections and urinating standing up.

Gender-affirming procedures require recovery time and may alter people’s experience of sex, use of contraception, and use of protection.
This article discusses how long a trans man should wait to have sex after gender-affirming surgery .
It also looks at what a person can expect during sex after these procedures and other sexual health tips.
When can a person have sex?
Recovery times after surgery can vary for each individual, so it is important that people follow the specific advice of a healthcare team.
If people have undergone a metoidioplasty, they may gradually return to their usual activities in the 6 weeks after surgery.
People may need to avoid or restrict sexual activity, heavy lifting, and exercise during this recovery time. They will need to consult a doctor about when it is safe to have sex.
People who have had a phalloplasty may be able to return to their usual activities 6–8 weeks after surgery. It may take longer than this before people can do certain activities, including sex, heavy lifting, and driving. A doctor will let people know when they can safely have sex.
Penis size and functionality
A metoidioplasty involves cutting the ligaments around the erectile tissue or clitoris. This releases it from the pubis to make it longer. A person can expect an average length of 4–6 centimeters .
People with a metoidioplasty will not ejaculate during orgasm due to the absence of certain structures such as the seminal vesicles and prostate . The urethra may release a clear fluid from the Skene’s glands , though.
For those undergoing a phalloplasty, the size of the penis will depend on their body. Those with less fat will have a penis with less girth compared with those with more fat. However, the typical size will be 5–6 inches after postoperative swelling decreases.
It will not be possible to ejaculate.
A person can also choose the size of the testicular implants with the advice of a healthcare professional.
After both procedures, it is possible to urinate while standing.
What sensations can a person expect?
The sensations a person experiences will depend on the type of surgery.
Metoidioplasty
According to a 2019 article , metoidioplasty does not typically create a penis large enough for penetrative sex. If penetrative sex is important to people, they may choose to have additional phalloplasty.
However, the article states that clitoral lengthening results in postoperative reports of excellent sensation and erection.
Although a metoidioplasty does not create a penis large enough for a penile implant , erections are possible due to the use of clitoral and genital tissues.
People with a metoidioplasty will still experience sexual arousal and orgasm. In a 2014 study , 97 participants who had undergone metoidioplasty reported complete satisfaction with the quality of erection and sensation. There were no reports of any issues with sexual arousal, orgasm, or masturbation.
The study also referred to earlier research in which people reported the following improvements after gender-affirming surgery:
- sexual satisfaction with a partner increased from 50% to 81.9%
- orgasm frequency increased from 45.5% to 77.8%
- frequent sexual arousal increased from 40% to 60.9%
- frequent masturbation increased from 20% to 78.3%
Phalloplasty
According to Johns Hopkins , those opting for a phalloplasty will develop a surgical plan with their healthcare team to decide which procedures they wish to undergo.
Phalloplasty involves:
- creating a penis
- lengthening the urethra
- creating the glans, or tip, of the penis
- creating a scrotum
- removing the vagina
- inserting testicular and erectile implants
The surgeon will use skin from a donor site. A donor site is an area that doctors will take skin, fat, nerves, and blood vessels from to create a penis. Possible donor sites include the arm, leg, or back. If preserving sensation is important to people, a surgeon may suggest a donor site with good nerve innervation.
Nerve quality will differ with each donor site, so people may choose a donor site based on their desired outcome. If sensation is important to people, they may choose the arm as a donor site as this provides the highest availability of nerves.
Nerve “hook up” allows people to have sensation by using nerves from a donor site such as the arm and connecting them to nerves in the pelvis.
There are fewer nerves available in the legs, and if people use the back as a donor site, they are unlikely to have any sensation.
Alongside people’s preferences, doctors also have to consider other factors such as overall health, fat distribution, nerve functionality, and blood flow.
Following stage one of a phalloplasty, nerves may start to regenerate 3 weeks after surgery, but this may take longer for some people. In some cases, sensation may take up to a year or more to return.
If penetrative sex and maintaining an erection are important, people can have an erectile prosthetic. There are usually three stages to a phalloplasty, and during the third stage, a doctor can implant an erectile prosthetic device, which allows people to maintain an erection.
It is possible to have an orgasm after phalloplasty.
Contraception and STIs
Using protective barriers during sex can help prevent people from passing on or contracting sexually transmitted infections (STIs) .
According to the Terence Higgins Trust , people can use an external condom over a penis after metoidioplasty or phalloplasty. People can use a new condom if they are having sex for more than half an hour, with a new partner, or changing between vaginal or frontal sex and anal sex.
Internal condoms are the safest choice for people with a metoidioplasty. If people are taking testosterone , it can reduce fertility but is not an effective contraceptive. If people want to prevent pregnancy, they will need to use condoms consistently or use another contraceptive method such as the:
- coil or IUD
All of these options are safe to use alongside testosterone.
Learn more about sexual health and transgender men here.
During recovery from a metoidioplasty, people may expect the following :
- some bleeding following surgery
- swelling in the genital area for up to 6 weeks post-surgery
- bruising from the abdomen to the thighs, which can last a few weeks
- itching and minor electrical sensations as the nerve endings heal
- numbness around surgical scars, which may last several months
- difficulty urinating when standing for the first weeks after surgery
- scarring in the genital area, which will fade with time
During recovery from a phalloplasty, people may expect the following :
- bleeding that may occur in the first 48 hours following surgery
- swelling in the penis, scrotum, and pubic area for the first 1–4 months
- bruising from the abdomen to thighs may occur in the first few weeks
- itching and minor electrical sensations as nerve endings heal
- numbness in the penis and scrotum, which will go within 18 months of surgery
- scarring from the procedure and donor site
Hygiene and aftercare
People will need to follow any post-surgery hygiene advice from their healthcare team.
After a metoidioplasty, people may need to apply antibiotic ointment to any surgical scars to prevent infection and change gauze dressings following surgery. People will need to follow a doctor’s advice for when they can bathe the genital area after a metoidioplasty.
After a phalloplasty, people can follow a doctor’s advice, which may include :
- covering the skin graft when bathing to keep it dry
- sponge bathing for the first week following surgery
- gently washing the penis with warm, soapy water and patting dry, beginning one week after surgery
- avoiding submerging the genital or donor site in water until a doctor advises it is safe
If people have had a skin graft from the arm, they may be able to get it wet 3 weeks after surgery.
People will also need to attend any checkups following surgery to ensure the healing process is going well.
People will need to follow the advice of their healthcare team for proper healing and to check when they are safe to have sex following a metoidioplasty or phalloplasty.
People can expect to still have sexual arousal, erection, and orgasm after lower gender-affirming surgery. Sensation may depend on the type of surgery people have and surgery recovery times.
Last medically reviewed on September 30, 2021
- Sexual Health / STDs
How we reviewed this article:
- Crane, C. (2016). Phalloplasty and metoidioplasty: Overview and postoperative considerations. https://transcare.ucsf.edu/guidelines/phalloplasty
- Djordjevic, M. L., et al . (2019). Metoidioplasty: Techniques and outcomes. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6626308/
- FAQ: Phalloplasty. (n.d.). https://www.hopkinsmedicine.org/center-transgender-health/services-appointments/faq/phalloplasty#FAQ
- Metoidioplasty. (n.d.). https://healthcare.utah.edu/transgender-health/gender-affirmation-surgery/metoidioplasty.php#metoidioplastyaftersurgery
- Metoidioplasty. (n.d.). http://www.phsa.ca/transcarebc/surgery/gen-affirming/lower-body-surgeries/metoidioplasty
- Phalloplasty guide: How to prepare & what to expect during your recovery. (n.d.). https://healthcare.utah.edu/transgender-health/gender-affirmation-surgery/phalloplasty-recovery.php#howtotakecareofyourpenisscrotumskingraftafteryouleavethehospital
- Phalloplasty. (n.d.). http://www.phsa.ca/transcarebc/surgery/gen-affirming/lower-body-surgeries/phalloplasty
- Safer sex and sexual health for trans masculine people. (n.d.). https://www.tht.org.uk/hiv-and-sexual-health/sexual-health/trans-people/trans-masculine/safer-sex
- Vukadinovic, V., et al . (2014). The role of clitoral anatomy in female to male sex reassignment surgery. https://www.hindawi.com/journals/tswj/2014/437378/
Share this article
Latest news
- Vitamin D may balance gut microbiome to give cancer immunotherapy a boost
- Dietary interventions better than medication for IBS management
- Human brains are getting bigger: Could this lead to lower dementia risk?
- Korean soybean paste shows promise in alleviating menopause symptoms
- Could cutting down calories influence longevity?
Related Coverage
Metoidioplasty is a type of lower surgery to create a penis from the clitoris and other genital tissue. Learn about the different types, the results…
It is important to know about sexual health. Learn more about sexual health for transgender men here.
Transgender men face a number of mental health concerns. Working past personal and societal stigmas may help them access care and find the support…
Sexual dysfunction refers to persistent physical or psychological problems that prevent someone from engaging in sexual activities. Learn more here.
Friday, April 26, 2024
Tax payer funded gender reassignment surgeries prompt questions about military readiness.
- by: Tracy Beanz

Read our latest news on any of these social networks!
Get the latest news delivered daily!
We will send you breaking news right to your inbox
Recent Articles
- Entertainment
- Sports Sports Betting Podcasts Better Planet Vault Mightier Autos Newsletters Unconventional Vantage Experts Voices
- Subscribe for $1
- Sports Betting
- Better Planet
- Newsletters
- Unconventional
Fact Check: Musk Says Trans Study Shows Higher Suicide Rate After Surgery
Since his takeover of Twitter , Elon Musk has not hesitated to engage in sensitive topics on the social media platform.
Having previously courted controversy over gender, the billionaire has entered into multiple conversations about transgender treatment and care.
During one recent exchange on transgender health, Musk quoted a study suggesting that those who had undergone transgender surgery were more likely to die by suicide than the general population.

A tweet by Musk, posted on April 25, 2023, viewed 1.2 million times, claimed that a "comprehensive study in Sweden" showed that "sex-reassigned" persons showed increased suicide.
Musk added: "Death for sex-reassigned persons was higher than for controls of same birth sex, particularly death from suicide. They also had increased risk for suicide attempts and psychiatric inpatient care."
T he association between transgender people and poorer mental health outcomes is documented. Multiple studies have observed association between suicide attempts and people who identify as transgender , with figures ranging from about 20 percent to 40 percent within those populations.
However, the study that Musk cites contains some important details that should be taken into consideration when looking at his claim.
The study, published in 2011, estimated the "mortality, morbidity, and criminal rate after surgical sex reassignment of transsexual persons" of "324 "sex-reassigned persons" in Sweden for 30 years. Each of these participants was matched with 10 population controls matched by birth year and birth sex or "reassigned (final) sex."
Data, which was taken from health and population registers in Sweden, found that those who had their sex "reassigned" were more likely to have died by suicide, made a suicide attempt or been psychiatrically hospitalized.
The paper stated: "This highlights that post surgical transsexuals are a risk group that need long-term psychiatric and somatic follow-up. Even though surgery and hormonal therapy alleviates gender dysphoria, it is apparently not sufficient to remedy the high rates of morbidity and mortality found among transsexual persons.
"Improved care for the transsexual group after the sex reassignment should therefore be considered."
Although a long-term analysis, the findings might reflect only the attitudes toward and lack of support for transgender people from 1973 to 2003. The paper recognizes modern improvements to sex reassignment surgery, hormonal treatments and psychosocial care that "might have improved the outcome" of the transgender case studies.
In keeping with this, other results in the study appear to show that those who had surgery later in the data set had a lower incidence rate of some of the mortality and morbidity outcomes it measured.
For example, the researchers found that there was not a statistically significant higher risk of suicide attempts among those who had reassignment surgery between 1989 and 2003 compared to those who did so between 1973 and 1988. The overall mortality rate was also only significantly higher in the group that had the surgery before 1989.
- Fact Check: Do Democrats plan to "cancel" presidential primary debates?
- Fact Check: Did NYPD bring in 38,000 Officers for Trump arraignment?
- Fact Check: Did Tucker Carlson testify "under oath" that Trump didn't win?
While we cannot conclude without further analysis why the 15-year period in which reassignment surgeries were performed led to these statistical differences, the study notes that it might be explained "by improved health care for transsexual persons during 1990s, along with altered societal attitudes towards persons with different gender expressions."
Historical context is important in assessing health risks as serious and sensitive as suicide, particularly in marginalized groups. It was just over 10 years ago that the American Psychiatric Association revised its Diagnostic and Statistical Manual of Mental Disorders to no longer list being transgender as a mental disorder (after the study Musk cited was published).
It is just one example of the types of changes to attitudes and care that might affect access to and willingness to seek health care, support and treatment, and could have influenced the results here.
These attitudes might also have affected the pool of participants that the researchers were able to recruit. As mentioned, the cases in the study were also based on national database records, not cases identified individually or recruited within the population.
Had a greater number of individuals felt compelled or comfortable to seek surgery during the time period from which data was collected, it might have provided more representative results of what the actual risks of mental illness and suicide were among the wider transgender population.
In any case, while Musk is not necessarily wrong to quote the study—which does provide useful insights into the risk outcomes among those who undergo reassignment surgery—it also neglects to mention the historical context of the data it was based on and the evidence in it that suggests that younger generations experienced improved outcomes.
This month, several transgender groups accused Twitter of censoring language associated with the LGBTQ+ community. Certain words, such as "trans," "LGBT" or "BLM" ( Black Lives Matter ), were said not to appear in the preview pane if sent as a private message, known as a DM, on the platform.
Trans Safety Network, a U.K.-based organization of journalists and data analysts who provide research to decision-makers influencing actions that affect trans people's safety, also looked into the issue.
It found many more words seemed to have been banned from Twitter DMs, including "queer," "sex," "lesbian," "homosexual," "bisexual" and "intersex."
Newsweek reached out to Twitter for comment.

Needs Context.
While Musk did not incorrectly quote the results of the 2011 study, his tweet does not mention that it was based on data from (in some instances) 50 years ago, nor does it mention the improved outcomes among the younger generations in the study.
Although the study Musk mentions provides some interesting insight into transgender-based outcomes, the importance of the historical context from which the data was taken should be carefully considered.
FACT CHECK BY Newsweek's Fact Check team
Uncommon Knowledge
Newsweek is committed to challenging conventional wisdom and finding connections in the search for common ground.
About the writer
To read how Newsweek uses AI as a newsroom tool, Click here.

- Newsweek magazine delivered to your door
- Newsweek Voices: Diverse audio opinions
- Enjoy ad-free browsing on Newsweek.com
- Comment on articles
- Newsweek app updates on-the-go

Top stories
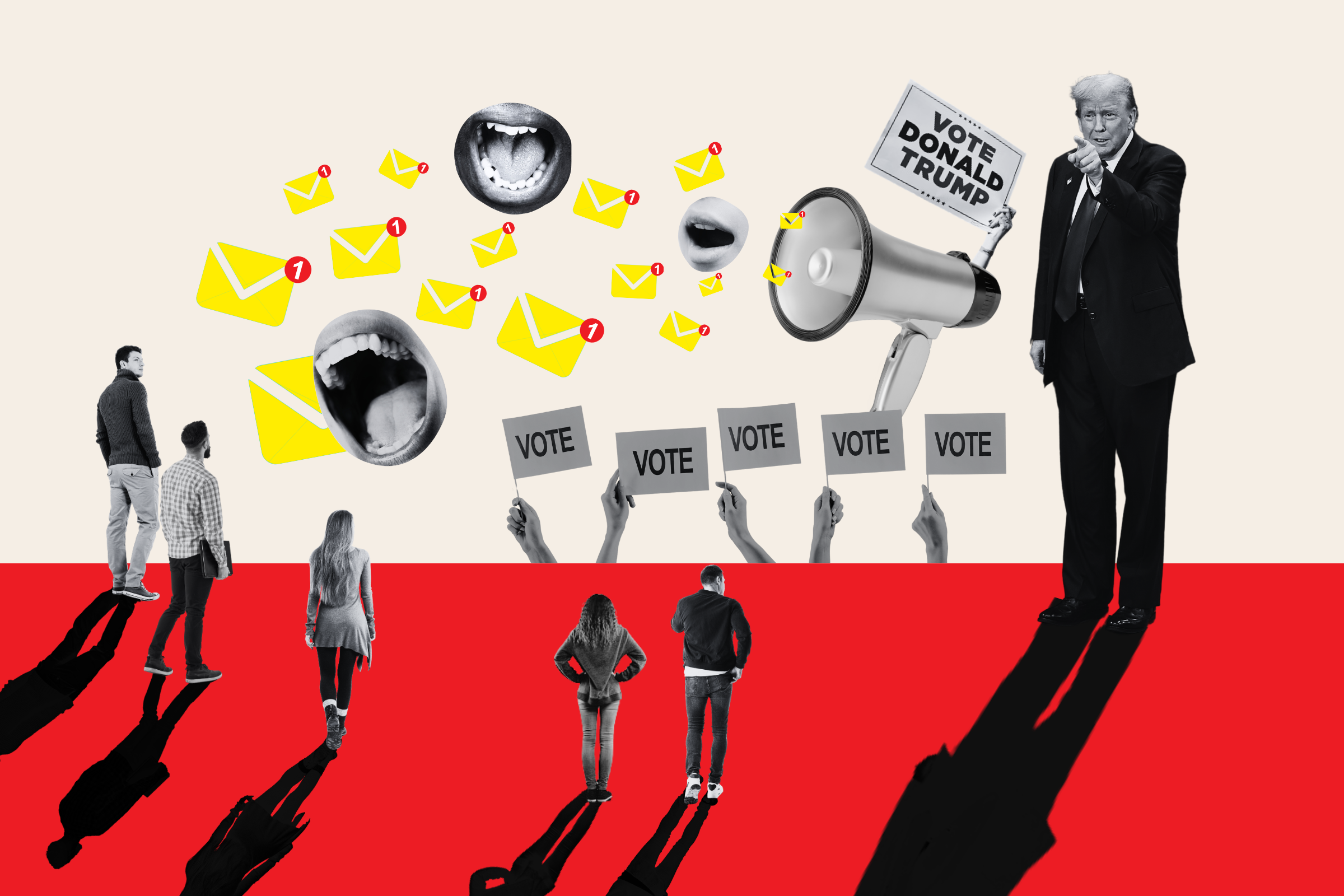
Donald Trump Campaign Accused of Spamming People With Unsolicited Emails

'The Mummy's' Rachel Weisz Reveals the 'Funniest Line' She Ever Had to Say
Brett Kavanaugh's 'Jarring' Supreme Court Remarks Stun Legal Experts

Joe Biden's Polling Turnaround Has One Major Problem


IMAGES
VIDEO
COMMENTS
Sex and sexual health tips for transgender women after gender-affirming surgery. Sex after surgery. Achieving orgasm. Libido. Vaginal depth and lubrication. Aftercare. Contraceptions and STIs ...
Research consistently shows that people who choose gender affirmation surgery experience reduced gender incongruence and improved quality of life. Depending on the procedure, 94% to 100% of people report satisfaction with their surgery results. Gender-affirming surgery provides long-term mental health benefits, too.
Gender affirming surgery can be used to create a vulva and vagina. It involves removing the penis, testicles and scrotum. During a vaginoplasty procedure, tissue in the genital area is rearranged to create a vaginal canal (or opening) and vulva (external genitalia), including the labia. A version of vaginoplasty called vulvoplasty can create a ...
Breast augmentation is often performed as an outpatient procedure but some patients may require one night stay in the hospital. 1 of 7. See before and after photos of patients who have undergone gender-affirming surgeries at Cleveland Clinic, including breast augmentations, facial feminizations, mastectomies and vaginoplasty.
Great care is taken to limit the external scars from a vaginoplasty by locating the incisions appropriately and with meticulous closure. Typical depth is 15 cm (6 inches), with a range of 12-16cm (5-6.5 inches); in comparison, typical vaginal depth in non-transgender females is between 9-12cm (3.5 to 5 inches).
Risks and complications. There are always risks associated with surgery, but vaginoplasty complications are rare. Infections can usually be cleared up with antibiotics. Some immediate postsurgical ...
Recovering from bottom surgery. Three to six days of hospitalization is required, followed by another 7-10 days of close outpatient supervision. After your procedure, expect to refrain from work ...
Request an Appointment. 844-546-5645 Maryland. 855-695-4872 Outside of Maryland. +1-410-502-7683 International. To help provide guidance for those considering gender affirmation surgery, two experts from the Johns Hopkins Center for Transgender Health answer questions about what to expect before and after your surgery.
Today, many transgender people prefer to use the term "gender confirmation surgery," because when we say something like gender "reassignment" or "sex change," it implies that a person ...
The cost of transitioning can often exceed $100,000 in the United States, depending upon the procedures needed. A typical genitoplasty alone averages about $18,000. Rhinoplasty, or a nose job, averaged $5,409 in 2019. Insurance Coverage for Sex Reassignment Surgery.
Overview. Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation.
We perform vaginoplasty under general anesthesia. Most people spend three full days in the hospital after surgery. Recovery from vaginoplasty can take up to three months, and requires intensive post-operative care. Most people spend the first seven to ten days after the procedure in bed, getting up only to go to the bathroom.
Top surgery is surgery that removes or augments breast tissue and reshapes the chest to create a more masculine or feminine appearance for transgender and nonbinary people. Facial gender surgery: While hormone replacement therapy can help achieve gender affirming changes to the face, surgery may help. Facial gender surgery can include a variety ...
Overview. Gender affirmation surgery, also known as gender confirmation surgery, is performed to align or transition individuals with gender dysphoria to their true gender. A transgender woman, man, or non-binary person may choose to undergo gender affirmation surgery. The term "transexual" was previously used by the medical community to ...
Feminizing bottom surgery is a procedure that allows your physical body to match your gender identity. It reconstructs organs in the male reproductive system into parts of a vulva and possibly a vagina. Recovery can take up to several months. Contents Overview Procedure Details Risks / Benefits Recovery and Outlook When To Call the Doctor ...
Gender Affirming Surgery. IU School of Medicine surgeons perform a variety of gender affirming surgeries at our clinical affiliates for patients over 18 years of age. Our team will work with you to learn your goals and to develop an individualized plan to meet your needs. We currently offer:
Please tell your medical provider the words you use to describe your body. Vaginoplasty is a gender-affirming, feminizing, lower surgery (transgender surgery; gender reassignemnt surgery; sex change surgery) to create a vagina and vulva (including mons, labia, clitoris, and urethral opening) and remove the penis, scrotal sac and testes.
Definition of SRS. Sex Reassignment Surgery (SRS), also known as gender affirmation surgery or gender-confirming surgery, is a medical procedure that alters an individual's physical characteristics to align with their gender identity. In other words, it's a way to help transgender people feel more comfortable in their bodies.
Long-term overall body congruency score was 89.6. Improved mental health outcomes persisted following surgery with significantly reduced suicidal ideation and reported resolution of any mental health comorbidity secondary to gender dysphoria. Conclusion: Gender-affirming surgery is a durable treatment that improves overall patient well-being ...
After sex reassignment surgery, Juliet Jacques recuperates at home with her parents. An infection delays her recovery, but eventually pain begins to give way to pleasure
Featured Expert: Fan Liang, M.D. Phalloplasty is surgery for masculinizing gender affirmation. Phalloplasty is a multistaged process that may include a variety of procedures, including: Creating the penis. Lengthening the urethra so you are able to stand to urinate. Creating the tip (glans) of the penis. Creating the scrotum.
A FTM gender reassignment surgery creates male genitalia. Here is a quick guide for what to expect before, during, and after a FTM gender reassignment surgery: Before Surgery. Prophylactic antibiotics or antivirals may be prescribed. Stop taking blood thinning medications two weeks prior to surgery. Blood thinners may include, Advil, Tylenol ...
People can expect to still have sexual arousal, erection, and orgasm after lower gender-affirming surgery. Sensation may depend on the type of surgery people have and surgery recovery times. Last ...
1-5 days in hospital, 6-8 weeks recovery, generally. After that, an ADSM could be deployed, right? Wrong. I decided to go right to the source and watched hundreds of videos of trans people telling their stories after gender reassignment surgery. And I am going to share some of them now. First, here is a doctor who makes many videos on YouTube.
TikTok video from Emma Ellingsen (@emmaellingsen_84): "gender reassignment surgery Q&A (life after, dating, v card etc) Parte 2". Surgery Recovery. original sound - Emma Ellingsen.
The study, published in 2011, estimated the "mortality, morbidity, and criminal rate after surgical sex reassignment of transsexual persons" of "324 "sex-reassigned persons" in Sweden for 30 years.
A pair of stunning transgender women who turned up at an army recruitment office in Thailand and were exempted from service by presenting proof of sex reassignment surgery have caused quite a stir ...
The book claims that it is "easy" to undergo gender reassignment surgery in the US, Aoyama said. But in Japan, paediatric psychiatry does not recommend gender reassignment surgery for minors ...