
Substance and Non-Substance Related Addictions pp 205–209 Cite as

Drug Policy
- Olaniyi Olayinka 2
- First Online: 03 January 2022
996 Accesses
Drug policies play a role in protecting the public’s health and reducing drug-related crimes at the local, national, and international levels. This chapter mainly focuses on key drug control treaties and policies, providing a brief historical context on how some of the policies were established. The goal is to present the reader with a general overview of international drug policies and how they might apply to drug control nationally.
This is a preview of subscription content, log in via an institution .
Buying options
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Degenhardt L, Hall W. Extent of illicit drug use and dependence, and their contribution to the global burden of disease. Lancet. 2012;379(9810):55–70.
Article Google Scholar
United Nations Office on Drugs and Crime. World Drug Report 2018. 2018. Available from: https://www.unodc.org/wdr2018/prelaunch/WDR18_Booklet_1_EXSUM.pdf .
Crowley R, Kirschner N, Dunn AS, Bornstein SS. Health and public policy to facilitate effective prevention and treatment of substance use disorders involving illicit and prescription drugs: an American College of Physicians position paper. Ann Intern Med. 2017;166(10):733–6.
Ammerman S, Ryan S, Adelman WP, Abuse CS. The impact of marijuana policies on youth: clinical, research, and legal update. Pediatrics. 2015;peds:2014–4147.
Google Scholar
MacGregor S, Singleton N, Trautmann F. Towards good governance in drug policy: evidence, stakeholders and politics. Int J Drug Policy. 2014;25(5):931–4.
Sweileh WM, Zyoud SH, Al-Jabi SW, Sawalha AF. Substance use disorders in Arab countries: research activity and bibliometric analysis. Subst Abuse Treat Prev Policy. 2014;9:33.
United Nations. The international drug control conventions. Vienna 2013. Available from: http://www.unodc.org/documents/commissions/CND/Int_Drug_Control_Conventions/Ebook/The_International_Drug_Control_Conventions_E.pdf .
Cooper HL, Linton S, Kelley ME, Ross Z, Wolfe ME, Chen Y-T, et al. Racialized risk environments in a large sample of people who inject drugs in the United States. Int J Drug Policy. 2016;27:43–55.
Pauly B. Harm reduction through a social justice lens. Int J Drug Policy. 2008;19(1):4–10.
World Health Organization. Guidance on the WHO review of psychoactive substances for international control. 2010. Available from: http://www.who.int/medicines/areas/quality_safety/GLS_WHORev_PsychoactSubst_IntC_2010.pdf .
United Nations. United Nations treaty collection. 2018. Available from: https://treaties.un.org/pages/viewdetails.aspx?src=treaty&mtdsg_no=vi-16&chapter=6&lang=en .
Beletsky L, Davis CS. Today’s fentanyl crisis: Prohibition’s Iron Law, revisited. Int J Drug Policy. 2017;46:156–9.
Cooper HL. War on drugs policing and police brutality. Subst Use Misuse. 2015;50(8–9):1188–94.
Astorga L, Shirk DA. Drug trafficking organizations and counter-drug strategies in the US-Mexican context. 2010.
BBC News. Canada becomes second country to legalise recreational cannabis. 2018. Available from: https://www.bbc.com/news/world-us-canada-45806255 .
Hetzer H, Walsh J. Pioneering cannabis regulation in Uruguay. NACLA Rep Am. 2014;47(2):33–5.
Volkow ND, Baler RD, Compton WM, Weiss SR. Adverse health effects of marijuana use. N Engl J Med. 2014;370(23):2219–27.
Wilkinson ST, Yarnell S, Radhakrishnan R, Ball SA, D’Souza DC. Marijuana legalization: impact on physicians and public health. Annu Rev Med. 2016;67:453–66.
Watson TM, Erickson PG. Cannabis legalization in Canada: how might ‘strict’ regulation impact youth? Taylor & Francis; 2018.
World Health Organization. Cannabis and cannabis resin. 2014. Available from: http://www.who.int/medicines/areas/quality_safety/8_2_Cannabis.pdf .
Kolodny A, Courtwright DT, Hwang CS, Kreiner P, Eadie JL, Clark TW, et al. The prescription opioid and heroin crisis: a public health approach to an epidemic of addiction. Annu Rev Public Health. 2015;36:559–74.
Volkow ND, Frieden TR, Hyde PS, Cha SS. Medication-assisted therapies—tackling the opioid-overdose epidemic. N Engl J Med. 2014;370(22):2063–6.
Download references
Author information
Authors and affiliations.
Department of Psychiatry and Behavioral Sciences, Interfaith Medical Center, Brooklyn, NY, USA
Olaniyi Olayinka
You can also search for this author in PubMed Google Scholar
Editor information
Editors and affiliations.
Department of Psychiatry New Jersey Medical School, Rutgers University, Newark, NJ, USA
Evaristo Akerele
Rights and permissions
Reprints and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter.
Olayinka, O. (2022). Drug Policy. In: Akerele, E. (eds) Substance and Non-Substance Related Addictions. Springer, Cham. https://doi.org/10.1007/978-3-030-84834-7_18
Download citation
DOI : https://doi.org/10.1007/978-3-030-84834-7_18
Published : 03 January 2022
Publisher Name : Springer, Cham
Print ISBN : 978-3-030-84833-0
Online ISBN : 978-3-030-84834-7
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
- Introduction
- Conclusions
- Article Information
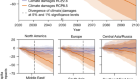
Figure shows the cumulative number of opioid-related state policies implemented, with Medicaid expansion included as a control (A), the number of enacted state policies as of 2018 (B), and the transition rate of the state policies (C). PDMP indicates prescription drug monitoring program.
The error bars represent the 95% CIs, and the shaded backgrounds represent positive (orange) and negative (blue) associations. The solid horizontal line represents the estimated mean effect size across all quarterly effect sizes from random-effects meta-analysis models. Quarters are a period of three months. MAT indicates medication-assisted treatment; open circle, 95% CIs overlap with 0; OUD, opioid use disorder; solid circle, 95% CIs do not overlap with 0.
The error bars represent the 95% CIs, and the shaded backgrounds represent positive (orange) and negative (blue) associations. Open circles indicate that 95% CIs overlap with 0; solid circle, 95% CIs do not overlap with 0.
eAppendix 1. Introduction to Optum Database
eAppendix 2. State Policies
eAppendix 3. Application of Panel Matching Under the Parallel Trends Assumption
eTable 1. Population Coverage of the Optum Database by State
eTable 2. International Classification of Diseases (ICD), Ninth and Tenth Revision Codes to Identify Opioid Use Disorder (OUD) and Overdose Diagnosis (OD)
eTable 3. Characteristics of the Study Samples From the Optum Database
eTable 4. Summary Statistics for Six Indicators Across Medicare Beneficiary Status
eTable 5. Overdose Death Counts Across Different Causes of Death
eTable 6. Mandatory PDMP Implementation Dates
eTable 7. State Policy Implementation Dates
eTable 8. The Meta-Analysis of Quarterly Effects of State Policy Implementation on Indicators of Prescription Opioid Misuse and Opioid Overdose From a Commercially Insured Population
eTable 9. The Meta-Analysis of Quarterly Effects of State Policy Implementation on Overdose Deaths
eFigure 1. Illustration of Parallel Trends Assumption Under the Difference-in-Difference Framework: The Impact of Mandatory PDMPs on All Overdose Deaths
eFigure 2. Pre-Post Trends for Six Outcomes From a Commercially Insured Population Across Six Policies
eFigure 3. Pre-Post Trends for Different Types of Drug-Related Deaths Across Six Policies
eFigure 4. Trends for Major Outcomes
eFigure 5. The Association of State Policy Implementation With Indicators of Prescription Opioid Misuse and Opioid Overdose From a Commercially Insured Population
eFigure 6. The Association of State Policy Implementation With Different Types of Drug Overdose Deaths
eTable 10. Regression Tables for Effects of State Policies on All Outcomes With 95% Confidence Intervals
eReferences
- Error in the Supplement JAMA Network Open Correction March 10, 2021
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Lee B , Zhao W , Yang K , Ahn Y , Perry BL. Systematic Evaluation of State Policy Interventions Targeting the US Opioid Epidemic, 2007-2018. JAMA Netw Open. 2021;4(2):e2036687. doi:10.1001/jamanetworkopen.2020.36687
Manage citations:
© 2024
- Permissions
Systematic Evaluation of State Policy Interventions Targeting the US Opioid Epidemic, 2007-2018
- 1 Department of Sociology, Indiana University-Bloomington, Bloomington
- 2 Luddy School of Informatics, Computing, and Engineering, Indiana University-Bloomington, Bloomington
- 3 Network Science Institute, Department of Sociology, Indiana University-Bloomington, Bloomington
- Correction Error in the Supplement JAMA Network Open
Question Are US state drug policies associated with variation in opioid misuse, opioid use disorder, and drug overdose mortality?
Findings In this cross-sectional study of state-level drug overdose mortality data and claims data from 23 million commercially insured patients in the US between 2007 and 2018, state policies were associated with a reduction in known indicators of prescription opioid misuse as well as deaths from prescription opioid overdose and increases in diagnosis of opioid use disorder, overdose, and drug overdose mortality from illicit drugs.
Meaning Although existing state-level drug policies have been associated with a decrease in the misuse of prescription opioids, these policies may have had the unintended consequence of motivating those with opioid use disorders to switch to alternative illicit substances, inducing higher overdose mortality.
Importance In response to the increase in opioid overdose deaths in the United States, many states recently have implemented supply-controlling and harm-reduction policy measures. To date, an updated policy evaluation that considers the full policy landscape has not been conducted.
Objective To evaluate 6 US state-level drug policies to ascertain whether they are associated with a reduction in indicators of prescription opioid abuse, the prevalence of opioid use disorder and overdose, the prescription of medication-assisted treatment (MAT), and drug overdose deaths.
Design, Setting, and Participants This cross-sectional study used drug overdose mortality data from 50 states obtained from the National Vital Statistics System and claims data from 23 million commercially insured patients in the US between 2007 and 2018. Difference-in-differences analysis using panel matching was conducted to evaluate the prevalence of indicators of prescription opioid abuse, opioid use disorder and overdose diagnosis, the prescription of MAT, and drug overdose deaths before and after implementation of 6 state-level policies targeting the opioid epidemic. A random-effects meta-analysis model was used to summarize associations over time for each policy and outcome pair. The data analysis was conducted July 12, 2020.
Exposures State-level drug policy changes to address the increase of opioid-related overdose deaths included prescription drug monitoring program (PDMP) access, mandatory PDMPs, pain clinic laws, prescription limit laws, naloxone access laws, and Good Samaritan laws.
Main Outcomes and Measures The outcomes of interests were quarterly state-level mortality from drug overdoses, known indicators for prescription opioid abuse and doctor shopping, MAT, and prevalence of drug overdose and opioid use disorder.
Results This cross-sectional study of drug overdose mortality data and insurance claims data from 23 million commercially insured patients (12 582 378 female patients [55.1%]; mean [SD] age, 45.9 [19.9] years) in the US between 2007 and 2018 found that mandatory PDMPs were associated with decreases in the proportion of patients taking opioids (−0.729%; 95% CI, −1.011% to −0.447%), with overlapping opioid claims (−0.027%; 95% CI, −0.038% to −0.017%), with daily morphine milligram equivalent greater than 90 (−0.095%; 95% CI, −0.150% to −0.041%), and who engaged in drug seeking (−0.002%; 95% CI, −0.003% to −0.001%). The proportion of patients receiving MAT increased after the enactment of mandatory PDMPs (0.015%; 95% CI, 0.002% to 0.028%), pain clinic laws (0.013%, 95% CI, 0.005%-0.021%), and prescription limit laws (0.034%, 95% CI, 0.020% to 0.049%). Mandatory PDMPs were associated with a decrease in the number of overdose deaths due to natural opioids (−518.5 [95% CI, −728.5 to −308.5] per 300 million people) and methadone (−122.7 [95% CI, −207.5 to −37.8] per 300 million people). Prescription drug monitoring program access policies showed similar results, although these policies were also associated with increases in overdose deaths due to synthetic opioids (380.3 [95% CI, 149.6-610.8] per 300 million people) and cocaine (103.7 [95% CI, 28.0-179.5] per 300 million people). Except for the negative association between prescription limit laws and synthetic opioid deaths (−723.9 [95% CI, −1419.7 to −28.1] per 300 million people), other policies were associated with increasing overdose deaths, especially those attributed to non–prescription opioids such as synthetic opioids and heroin. This includes a positive association between naloxone access laws and the number of deaths attributed to synthetic opioids (1338.2 [95% CI, 662.5 to 2014.0] per 300 million people).
Conclusions and Relevance Although this study found that existing state policies were associated with reduced misuse of prescription opioids, they may have the unintended consequence of motivating those with opioid use disorders to access the illicit drug market, potentially increasing overdose mortality. This finding suggests that there is no easy policy solution to reverse the epidemic of opioid dependence and mortality in the US.
The current opioid epidemic in the US has its historical roots in the movement during the 1990s to address undertreated chronic pain. In response, opioid-producing pharmaceutical companies engaged in aggressive marketing and prescribers overcorrected, relying on powerful opioid analgesics to treat acute and minor pain in addition to chronic and severe pain. Subsequently, the widespread use of opioid analgesic agents created demand for long-term and non-medical use of prescription and illicit opioids. 1 , 2 To address the growing opioid epidemic, policy makers have focused largely on controlling the prescription and use of opioid analgesics through the implementation of supply-side drug policies. These include prescription drug monitoring programs (PDMPs), pain clinic laws, and prescription limit laws to reduce inappropriate prescribing behavior. In tandem, policy measures to reduce harms and barriers associated with treating and reporting drug overdose, including naloxone access laws and Good Samaritan laws, have been introduced.
Previous studies have provided mixed evidence on the impact that these state policies have had on opioid misuse, nonfatal overdose, and opioid mortality. For example, some research indicates that access to a PDMP, which allows prescribers to review patients’ prescription histories, substantially reduces prescription of opioids by 6 percentage points and oxycodone distribution by 8 percentage points. 3 , 4 In contrast, other studies have found that PDMP access is ineffective 5 - 7 or is only effective if a review of patient records is mandatory. 8 , 9 Other types of policies such as naloxone access and pain clinic laws have reported contradictory evidence. 10 - 12 For example, naloxone access laws were estimated by 1 study to reduce opioid-related fatal overdose by 0.387 per 100 000 people in 3 or more years after adoption, 10 whereas another study reported that there were no significant changes in mean opioid-related mortality but a 14% increase in the Midwest after the implementation of naloxone access laws. 11
A likely explanation for the conflicting evidence on opioid policy outcomes is methodological limitations of existing work. First, discrepant findings may be attributable to differences in data coverage, such as variation in the states and time periods included in analyses. 13 , 14 This sample selection issue makes it difficult to compare and synthesize existing evidence. Second, there is disagreement about how to operationalize and model the timing of policy implementation. 15 Third, the most common modeling approach, the 2-way fixed-effects model in difference-in-differences analysis (ie, controlling for both state and period indicators) has an important limitation: likely violation of the parallel trends assumption. 16 , 17 Because many states enacted new policies after 2013, it is urgent to conduct an updated assessment of the impact of state opioid policy using more recent data.
Herein, we present the most comprehensive study to date on state policies that target the US opioid epidemic, focusing on the consequences of policies for both prescription opioid misuse and overdose mortality. Are state drug policies significantly associated with variations in opioid misuse, opioid use disorder, and drug overdose mortality? To answer this question, we use panel matching to implement a rigorous difference-in-differences approach in conjunction with extensive data coverage that includes observations through 2018 (2007–2018; across 50 states). We also assemble and refine the policy timing data across the 6 most widely studied policies; to our knowledge, these data have never before been investigated in tandem.
This analysis draws on medical and pharmacy claims data from the Optum Clinformatics Data Mart Database (2007-2018) and a publicly available mortality data set from the National Center for Health Statistics (NCHS). The Optum database is a large deidentified database from a national private insurance provider 18 - 20 that includes medical and prescription claims for the full population of patients ever prescribed any controlled substance between 2007 and 2018 (approximately 23 million). eAppendix 1 and eTable 1 in the Supplement include a description of the Optum database and the population coverage by state. Excluded from the study were patients with cancer and those receiving palliative care because they are expected to be outliers with respect to (medically necessary) opioid consumption. We measured all indicators at the patient level and aggregated them to the level of state of residence. We obtained state-level overdose mortality data from the NCHS Multiple Cause of Death file from 1999 to 2018. In addition, we obtained data on several confounders (ie, the proportion of female individuals; those aged <40 years, 40-60 years, and >60 years; White, Black, Asian, and Hispanic individuals, and individuals of other races [American Indian, Pacific Islander, and multiple racial categories except for Hispanic]; those who were unemployed; those living below the poverty line; the state population; and state implementation of Medicaid expansion) from current population surveys. We aggregated individual-level data to quarterly state-level data using the provided survey weights. Herein we report results across quarterly units because we find that these units generate more precise estimates. This study was approved by the institutional review board at Indiana University, and the requirement for informed consent was waived because deidentified data were used. We followed the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline.
We used an extensive set of prescription opioid outcomes. First, we measured the proportion of patients who received any opioid during a given period (ie, quarter). Second, using the subset of patients who received any opioid between 2007 and 2018, we computed 5 additional measures. The International Classification of Diseases, Ninth Revision ( ICD-9 ) and International Statistical Classification of Diseases and Related Health Problems, Tenth Revision ( ICD-10 ) codes were used to identify opioid use disorder and overdose diagnosis (eTable 2 in the Supplement ) and measure the proportion of patients with the disorder or overdose diagnosis. We also calculated the proportion of patients who received opioid doses higher than the maximum daily morphine milligram equivalent (MME) of 90, which was generated by enumerating daily MME (Strength per Unit × [Number of Units/Days Supply] × MME Conversion Factor) 21 of all opioid prescriptions over time for each patient.
In addition, we measured the traditional doctor-shopping indicator (ie, the proportion of patients who visit ≥4 unique doctors and ≥4 unique pharmacies for opioids within 90 days) 22 and the proportion of patients with overlapping opioid prescriptions. We also examined opioid treatment, which was defined as the proportion of patients who were prescribed any medication-assisted treatment (MAT) drug that includes buprenorphine, buprenorphine/naloxone, buprenorphine hydrochloride and naltrexone. 23 We excluded methadone from the MAT drug list because it is often used as an opioid analgesic when prescribed by primary care physicians and other physicians for purposes other than substance use treatment, although results were similar when methadone was included in the list. Across all measures, we used the number of total enrollees, excluding those with cancer and those receiving palliative care in each state and year-quarter as denominators. eTable 3 in the Supplement details the basic characteristics of the analytic sample. eTable 4 in the Supplement includes summary statistics for the 6 indicators across patients with the Medicare low-income subsidy, Medicare beneficiaries, and patients without Medicare.
We used ICD-10 codes to identify overdose mortality and to differentiate the cause of death. Deaths with drug overdose as the underlying cause were first identified using codes X40-X44 (unintentional), X60-X64 (suicide), X85 (homicide), and Y10-Y14 (undetermined intent). Of those codes, drug-related deaths were further identified based on codes T40.0-T40.6, including those for heroin (T40.1), natural and semisynthetic opioids (T40.2), methadone (T40.3), synthetic opioids excluding methadone (T40.4), cocaine (T40.5), and other unspecified drugs (T40.6). We included opioid and nonopioid overdose-inducing drugs because of the high incidence of polysubstance use among those with opioid use disorder. 24 , 25 We repeated our query through the Centers for Disease Control and Prevention’s CDC Wonder online database across different causes of death ( ICD-10 codes T40.1-T40.6) between 1999 and 2018 except for 1 month, and then subtracted the total number of deaths excluding each month from the total number of deaths across 2007 to 2018 (a total of 144 queries) to identify the number of deaths each month. This method can was used to recover the monthly death counts (eTable 5 in the Supplement includes the annual counts across different causes of deaths).
We compiled a data set on 6 opioid-related policies with 2 broad objectives: to control the supply of prescription opioids or reduce harms and barriers to medical assistance for overdose. eTables 6 and 7 in the Supplement show the exact year and month of all policy implementation dates by state. The opioid-related policies include (1) PDMP access laws that provide access to the PDMP, an electronic database that tracks controlled substance prescriptions in a state; (2) mandatory PDMPs that require prescribers under certain circumstances to access the PDMP database prior to prescribing opioids; (3) prescription limit laws that impose limitations on the number of days that medical professionals dispense opioids for acute pain; (4) pain clinic laws that regulate the operation of pain clinics; (5) Good Samaritan laws that provide immunity or other legal protection for those who call for help during overdose events; and (6) naloxone access laws that provide civil or criminal immunity to licensed health care clinicians or lay responders for administration of opioid antagonists, such as naloxone hydrochloride, to reverse overdose. eAppendix 2 in the Supplement describes the information collection process for these state policies. Based on the dates of these policies, we defined treatment indicators , which were assigned a value of 1 if the law was active in a given quarter, otherwise a value of 0 was assigned. In addition, we created a separate indicator for state implementation of Medicaid expansion that we obtained from the Kaiser Family Foundation to control for its potential impact on the statistical inferences.
To ascertain whether state policy altered the prevalence of opioid abuse and misuse indicators, we used a difference-in-differences approach. A state was considered to be a treated case if the policy had been changed at a specified time , otherwise it was considered to be an untreated case. The goal was to compare the outcomes of interest for a state under the new policy regime at a specific time with the outcome under the old policy regime if the policy was not enacted at the same time. The key challenge was to find a suitable control case for the treated case. The difference-in-differences approach imputed the change of outcomes in the control case as a comparison case for the change of outcomes in the treatment case under the parallel trends assumption (ie, potential outcomes have a parallel time trend for the treatment and control groups). Namely, the difference of outcomes between the treated case and the control case before the policy change would stay the same after the change in the absence of treatment.
To mitigate potential violations of the parallel trends assumption, we used panel matching to construct a matched data set to make trends of pretreatment outcomes parallel across control and treatment cases in addition to other observed confounders (ie, the proportion of female individuals; individuals aged <40 years, 40-60 years, and >60 years; individuals of White, Black, Asian, and Hispanic race and those of other races [American Indian, Pacific Islander, and multiple racial categories except for Hispanic], unemployed individuals, those living below the poverty line, as well as the state population and state implementation of Medicaid expansion) through covariate-balancing propensity scores (CBPS). eAppendix 3 in the Supplement describes the application of panel matching.
We used the PanelMatch package in R, version 4.0.1 (R Foundation for Statistical Computing), 26 to estimate the effect sizes of the temporal associations between policies and leading outcomes of interest for each quarter for 3 years (ie, up to 12 quarters). We used the metafor package in R 27 for the random-effects meta-analysis model to summarize temporal associations for each policy and outcome pair (eAppendix 3 in the Supplement ). We present uncertainty associated with effect sizes using 95% CIs to shift focus away from the null hypothesis testing toward showing the full range of effect sizes, we define an association as negative if the mean effect across all quarters is negative and a positive association if the mean effect is positive. In addition, associations are defined as significant if their 95% CIs do not overlap with zero. The data analysis was conducted July 12, 2020. All codes and data to replicate analyses are available at https://dataverse.harvard.edu/dataverse/bk .
This cross-sectional study includes data on drug overdose mortality from the Optum Clinformatics Data Mart database and insurance claims data from the NCHS for 23 million commercially insured patients in 50 states between 2007 and 2018. Of these patients, 12 582 378 (55.1%) were women, and the mean (SD) age was 45.9 (19.9) years. Figure 1 depicts the cumulative count of opioid-related policies implemented by 50 states from 2007 to 2018. The monthly count of opioid policies started to increase substantially after 2012 to 2013. The implementation of Good Samaritan and naloxone access laws have been the largest contributor to the overall increase in policy adoption since 2013. In the first quarter of 2018, states adopted a mean of 4.1 policies, and 22 states adopted all but 1 policy. Access to PDMPs was implemented first by most states followed by the implementation of Good Samaritan and naloxone access laws, whereas mandatory PDMP and prescription limit laws were implemented in later periods. In 2014, Medicaid expansion laws were enacted in approximately half of the states, which may have biased the impact of other state drug policies. We accounted for this issue by controlling for an indicator of Medicaid expansion in the statistical models.
The rate of overdose deaths as well as the diagnosis of overdose and opioid use disorder increased as states implemented more policies (eFigure 4 in the Supplement ), although indicators of opioid misuse and “doctor shopping” declined. For example, states without any of 6 policies exhibited a lower proportion of patients with overdose and opioid use disorder (0.14%) and a higher proportion of patients with a daily MME of 90 or higher (2.54%) vs states with all 6 policies (0.95% and 2.01%, respectively). Associations between mandatory PDMP and naloxone access law on 3 indicators from the commercially insured population are presented in Figure 2 . eFigure 5 in the Supplement shows the consequences of implementation of all 6 policies for all 6 indicators. Figure 2 summarizes the temporal associations for each policy and outcome pair; the effect sizes with 95% CIs are presented with shaded panel backgrounds if the 95% CIs did not overlap with 0 effects (in eTable 8 in the Supplement ).
First, supply-controlling policies were associated with reduction in 4 known prescription opioid misuse indicators: the proportion of patients who take opioids, have overlapping claims, receive higher opioid doses (daily MME ≥90), and visit multiple providers and pharmacies. For example, a mandatory PDMP was associated with a reduction of 0.729% (95% CI, −1.011% to −0.447%) in the proportion of patients taking opioids, those with overlapping opioid claims (−0.027%; 95% CI, −0.038% to −0.017%), those with a daily MME of 90 or higher (−0.095%; 95% CI, −0.150% to −0.041%), and in those who engaged in drug seeking behavior (−0.002%; 95% CI, −0.003% to −0.001%. In contrast, PDMP access was associated with a 0.17% (95% CI, 0.07%-0.26%) increase in the proportion of patients taking opioids and a 0.04% (95% CI, 0.007%-0.075%) increase in patients with a daily MME of 90 or higher. Second, the harm-reduction policies (ie, Good Samaritan laws and naloxone access laws) were associated with modest increases in the proportion of patients with overdose (0.014%; 95% CI, 0.002%-0.027%) and opioid use disorder (0.05%; 95% CI, 0.03%-0.07%). Third, the proportion of patients receiving MAT drugs increased following the implementation of supply-controlling policies, including mandatory PDMP (0.015%; 95% CI, 0.002%-0.028%), pain clinic laws (0.013%; 95% CI, 0.005%-0.021%), and prescription limit laws (0.034%; 95% CI, 0.020%-0.049%). Methadone as MAT produces similar results, including for pain clinic laws (0.024%; 95% CI, 0.009% to 0.039%) and prescription limit laws (0.014%, 95% CI, 0.003% to 0.025%). In general, the policy effect sizes became larger when estimating later outcomes, suggesting that the policy implementation does not produce immediate changes, but rather takes time to be effective (ie, a policy response lag).
Figure 3 shows the rate of drug overdose mortality after enactment of mandatory PDMPs and naloxone access laws. eFigure 6 in the Supplement shows the rate of drug overdose mortality after enactment of all 6 policies, and eTable 9 in the Supplement shows the temporal associations for overall drug overdose deaths and deaths from specific opioids (eg, natural, synthetic, heroin). First, all overdose deaths increased following the implementation of naloxone access laws (1344.3 [95% CI, 627.1-2061.6] per 300 million people), especially deaths attributable to heroin (280.3 per 300 million people), synthetic opioids (1338.2 [95% CI, 662.5-2014.0] per 300 million people), and cocaine (557.6 [95% CI, 328.3-787.0] per 300 million people). Good Samaritan laws were also associated with increases in overall overdose deaths (403.7 [95% CI, 172.7-634.8] per 300 million people). Second, mandatory PDMPs were associated with a reduction of overdose deaths from natural opioids (−518.5 [95% CI, −728.5 to −308.5] per 300 million people) and methadone (−122.7 [95% CI, −207.5 to −37.8] per 300 million people), although the effect size was smaller than those of harm-reduction policies. Prescription drug monitoring program access policies showed similar results, although these policies were also associated with increases in overdose deaths from synthetic opioids (380.3 [95% CI, 149.6-610.8] per 300 million people) and cocaine (103.7 [95% CI, 28.0-179.5] per 300 million people). The implementation of pain clinic laws was associated with an increase in the number of overdose deaths from heroin (336.3 [95% CI, 79.5-593.0] per 300 million people) and cocaine (97.3 [95% CI, 23.9-170.8] per 300 million people). As an exception, having a prescription limit law was associated with a decrease in overdose deaths from synthetic opioids (−723.9 [95% CI, −1419.7 to −28.1] per 300 million people). In line with the results from analysis of 6 policies using medical claims data, we found a substantial policy response lag. All effect sizes from 0 to 12 quarters across 12 outcomes and 6 policies are presented in eTable 10 in the Supplement .
Recent trends in the US opioid epidemic present a paradox: opioid overdose mortality has continued to increase despite declines in opioid prescriptions since 2012. 28 , 29 The opioid paradox may arise from the success—not failure—of state interventions to control opioid prescriptions. This finding is supported by a comprehensive assessment of multiple opioid policies on a range of outcomes, including opioid misuse and overdose mortality with extensive data coverage. We found that supply-controlling policies were associated with a reduction in the amount of prescription opioid misuse and the number of overdose deaths attributable to natural opioids as well as an increase in the number of patients receiving MAT drugs. In tandem, the significant increase of overdose deaths from synthetic opioids, heroin, and cocaine after the enactment of PDMP access, pain clinic laws, and naloxone access laws suggests that current drug policies may have the unintended consequence of motivating opioid users to switch to illicit drugs. An important implication of our findings is that there is no easy policy solution to reverse the epidemic of opioid dependence and mortality in the US. Hence, to resolve the opioid paradox, it is imperative to design policies to address the fundamental causes of overdose deaths (eg, lack of economic opportunity, persistent physical, and mental pain) and enhance treatment for drug dependence and overdose rather than focusing on opioid analgesic agents as the cause of harm. 2 , 30
Prescription drug monitoring programs are the most widely studied policy responses to the opioid epidemic. Previous research on their impact indicates that providing access to PDMPs is not associated with significant improvement, but PDMPs have reduced prescription opioid misuse when accessing the databases was required for physicians. 8 , 22 , 31 The present study found that mandatory PDMPs also reduced opioid misuse in a commercially insured population. In addition, we found that prescription limit laws and pain clinic laws were associated with a reduction in opioid abuse and an increase in the proportion of patients receiving MAT drugs. A study found that these laws as designed significantly reduce the length of initial prescription, although they also increase the likelihood of new (ie, first time) opioid use and the strength of initial prescription. 32 In addition, pain clinic laws have been associated with modest decreases in opioid prescribing in Florida and Texas. 33 , 34 The results of the present study are broadly consistent with those of other studies.
This extensive analysis may settle some of the contradictory findings in the literature and contributes to the previous research on opioid policy outcomes. Previous research on naloxone access and Good Samaritan laws has yielded inconsistent results. Namely, the enactment of naloxone access laws has been associated with substantial reductions in a fatal overdose but increased nonfatal overdoses. 10 , 12 These results, however, have been contradicted by other studies that suggested that expansion of naloxone access laws leads to more opioid-related emergency department visits and thefts without any substantial reductions in opioid mortality. 11 , 35 Likewise, previous research has suggested that Good Samaritan laws are not associated with heroin-related mortality, but substantially reduce mortality from other opioids. 12 The situation is similar to studies examining the association between PDMPs and overdose mortality. 6 , 7 , 13 , 14 Differences between our results and those of previous studies may be explained by our rigorous and extensive analytic approach, which uses panel matching for difference-in-differences analysis to mitigate the violation of the parallel trends assumption and the use of more recent data while simultaneously examining temporal associations. Given that most state policies were enacted after 2013, the present study used data through 2018 to provide the most up-to-date evidence on the opioid policy landscape.
We believe that our findings on the role of harm reduction policies in accelerating drug overdose deaths, especially those attributable to synthetic opioids and heroin, have important implications. Good Samaritan laws are designed to remove the threat of liability for people who call for emergency assistance in the event of a drug overdose. It is theoretically possible that provision of immunity may lead to greater reporting of overdose events in the absence of actual increases, although it is less likely to explain the increase of overdose deaths after the enactment of a Good Samaritan law. Naloxone laws provide civil immunity to licensed health care professionals or lay responders for opioid antagonist administration. Although expanded access to naloxone can reverse an opioid overdose and save lives, we found that naloxone access laws were associated with a substantial increase rather than a decrease in overdose deaths, especially deaths from illicit drugs. It is possible that the prospect of getting access to overdose-reversing treatment may instead induce moral hazards by encouraging people to use opioids and other drugs in riskier ways than they would have without the safety net of naloxone. 11 Although naloxone access laws were estimated to increase naloxone dispensing, 36 a recent study found that only 2135 of 138 108 high-risk patients (1.5%) in the US were prescribed naloxone in 2016. 37 This finding suggests that policies designed to dramatically improve treatment for overdose are needed.
Several important limitations of this study are worth noting. First, a difference-in-differences approach through panel matching cannot account for spillover effects between states and between policies. 26 Although we believe that considering multiple types of drug policies simultaneously is important, teasing out the association between a single policy and outcome from those of other policies is difficult because of correlated policy responses. Likewise, because prior research suggests that states’ adoption of Medicaid expansion has led to an increase in opioid overdose-related mortality 38 but a decrease in opioid-related hospital use, 39 we accounted for this factor by adjusting for Medicaid expansion in the modeling framework. However, identifying policy consequences on outcomes while controlling for the adoption of Medicaid expansion may produce underestimates or overestimates given the policy response lag and overlaps among different policy responses. Future research may consider, for example, sequence analysis or other clustering methods combined with the difference-in-differences approach to examine the impact of correlated policy responses.
Second, because we draw on data from a commercially insured population, these findings may not extend to other populations or to those individuals with insurance who pay cash for opioid prescriptions. Opioid misuse and overdose rates are higher among Medicare beneficiaries in our patient population with a low-income subsidy (eTable 4 in the Supplement ), which suggests that this analysis may be missing a substantial proportion of the population at risk for opioid problems. Although the results on opioid misuse are consistent with those of an earlier report on mandatory PDMPs up to 2013 using a Medicare part D sample, 8 future research is needed to ascertain whether the findings of the present analysis can be generalized to other patient populations. Third, there are potential limitations of using ICD-10 codes to identify fatal overdose owing to inaccuracy and incompleteness of death classification. 40 In addition, the transition of overdose coding from ICD-9 to ICD-10 may have contributed to the increase in overdose cases after October of 2015. 41 Because systematic misreporting on fatal and nonfatal overdoses may induce bias in our estimates, it is crucial to examine and account for factors that affect the identification of overdose deaths in future work.
The cause of opioid dependence is multifactorial, rooted in complex interactions between social, psychological, biological, and genetic factors. 42 Heightened demand for diverted and illicit drugs might arise from limiting the supply of prescription opioids under certain conditions. 43 These unintended consequences may occur if the fundamental causes of demand for opioids are not addressed and if the ability to reverse overdose is expanded without increasing treatment of opioid overdose. We believe that policy goals should be shifted from easy solutions (eg, dose reduction) to more difficult fundamental ones, focusing on improving social conditions that create demand for opioids and other illicit drugs. 2
Accepted for Publication: December 19, 2020.
Published: February 12, 2021. doi:10.1001/jamanetworkopen.2020.36687
Correction: This article was corrected on March 10, 2021, to fix errors in the data reported in eTable 4 in the Supplement.
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2021 Lee B et al. JAMA Network Open .
Corresponding Author: Brea L. Perry, PhD, Department of Sociology, Indiana University-Bloomington, 1020 E Kirkwood Ave, 767 Ballantine Hall, Bloomington, IN 47405 ( [email protected] ).
Author Contributions : Drs Lee and Perry had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Lee, Perry.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Lee.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Lee.
Obtained funding: Perry.
Administrative, technical, or material support: Lee, Zhao, Yang, Ahn.
Supervision: Lee, Ahn.
Conflict of Interest Disclosures: None reported.
Funding/Support: This research was funded by the National Institute on Drug Abuse (R01 DA039928; Dr Perry), and an Indiana University Addictions Grand Challenge Grant (Dr Perry).
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Additional Contributions: We would like to thank the information technology team at the Indiana University Network Science Institute for their technical support. The team received no compensation, other than the usual salary, for contributions to this work.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts

People & Community

Research & Impact

Career Services

Working Papers
0 results found.
Publications about Drug Policy
Do citizens know whether their state has decriminalized marijuana a test of the perceptual assumpti.
, Rosalie Liccardo Pacula, Jamie F. Chriqui, Katherine M. Harris , Peter H. Reuter
Working Paper: GSPP08-011 (April 2008)
Deterrence theory proposes that legal compliance is influenced by the anticipated risk of legal sanctions. This implies that changes in law will produce corresponding changes in behavior, but the marijuana decriminalization literature finds only fragmentary support for this prediction. But few studies have directly assessed the accuracy of citizens' perceptions of legal sanctions. The heterogeneity in state statutory penalties for marijuana possession across the United States provides an opportunity to examine this issue. Using national survey data, we find that the percentages who believe they could be jailed for marijuana possession are quite similar in both states that have removed those penalties and those that have not. Our results help to clarify why statistical studies have found inconsistent support for an effect of decriminalization on marijuana possession.
Drug Use and Drug Policy in a Prohibition Regime
, Karin D. Martin
Working Paper: GSPP08-008 (April 2008)
Prohibition makes some drug use and drug selling a crime by statute, but licit drugs like alcohol are also associated with criminality in myriad ways. Within a prohibition regime, it is difficult but important to distinguish a drug's "intrinsic" psychopharmacological harms from the harms created or exacerbated by prohibition and its enforcement. Rather than debating the merits of legalization (see MacCoun & Reuter, 2001), we evaluate current epidemiological patterns and mainstream policy instruments within the US prohibition regime, but we go beyond the standard criterion of prevalence reduction by considering harm reduction and quantity reduction as well. We close by speculating about some emerging challenges, including the "thizzle" scene and the future of performance enhancing drugs.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- 15 April 2024
- Correction 22 April 2024
Revealed: the ten research papers that policy documents cite most
- Dalmeet Singh Chawla 0
Dalmeet Singh Chawla is a freelance science journalist based in London.
You can also search for this author in PubMed Google Scholar
Policymakers often work behind closed doors — but the documents they produce offer clues about the research that influences them. Credit: Stefan Rousseau/Getty
When David Autor co-wrote a paper on how computerization affects job skill demands more than 20 years ago, a journal took 18 months to consider it — only to reject it after review. He went on to submit it to The Quarterly Journal of Economics , which eventually published the work 1 in November 2003.
Autor’s paper is now the third most cited in policy documents worldwide, according to an analysis of data provided exclusively to Nature . It has accumulated around 1,100 citations in policy documents, show figures from the London-based firm Overton (see ‘The most-cited papers in policy’), which maintains a database of more than 12 million policy documents, think-tank papers, white papers and guidelines.
“I thought it was destined to be quite an obscure paper,” recalls Autor, a public-policy scholar and economist at the Massachusetts Institute of Technology in Cambridge. “I’m excited that a lot of people are citing it.”
The most-cited papers in policy
Economics papers dominate the top ten papers that policy documents reference most.
Data from Overton as of 15 April 2024
The top ten most cited papers in policy documents are dominated by economics research; the number one most referenced study has around 1,300 citations. When economics studies are excluded, a 1997 Nature paper 2 about Earth’s ecosystem services and natural capital is second on the list, with more than 900 policy citations. The paper has also garnered more than 32,000 references from other studies, according to Google Scholar. Other highly cited non-economics studies include works on planetary boundaries, sustainable foods and the future of employment (see ‘Most-cited papers — excluding economics research’).
These lists provide insight into the types of research that politicians pay attention to, but policy citations don’t necessarily imply impact or influence, and Overton’s database has a bias towards documents published in English.
Interdisciplinary impact
Overton usually charges a licence fee to access its citation data. But last year, the firm worked with the publisher Sage to release a free web-based tool , based in Thousand Oaks, California, that allows any researcher to find out how many times policy documents have cited their papers or mention their names. Overton and Sage said they created the tool, called Sage Policy Profiles, to help researchers to demonstrate the impact or influence their work might be having on policy. This can be useful for researchers during promotion or tenure interviews and in grant applications.
Autor thinks his study stands out because his paper was different from what other economists were writing at the time. It suggested that ‘middle-skill’ work, typically done in offices or factories by people who haven’t attended university, was going to be largely automated, leaving workers with either highly skilled jobs or manual work. “It has stood the test of time,” he says, “and it got people to focus on what I think is the right problem.” That topic is just as relevant today, Autor says, especially with the rise of artificial intelligence.
Most-cited papers — excluding economics research
When economics studies are excluded, the research papers that policy documents most commonly reference cover topics including climate change and nutrition.
Walter Willett, an epidemiologist and food scientist at the Harvard T.H. Chan School of Public Health in Boston, Massachusetts, thinks that interdisciplinary teams are most likely to gain a lot of policy citations. He co-authored a paper on the list of most cited non-economics studies: a 2019 work 3 that was part of a Lancet commission to investigate how to feed the global population a healthy and environmentally sustainable diet by 2050 and has accumulated more than 600 policy citations.
“I think it had an impact because it was clearly a multidisciplinary effort,” says Willett. The work was co-authored by 37 scientists from 17 countries. The team included researchers from disciplines including food science, health metrics, climate change, ecology and evolution and bioethics. “None of us could have done this on our own. It really did require working with people outside our fields.”
Sverker Sörlin, an environmental historian at the KTH Royal Institute of Technology in Stockholm, agrees that papers with a diverse set of authors often attract more policy citations. “It’s the combined effect that is often the key to getting more influence,” he says.

Has your research influenced policy? Use this free tool to check
Sörlin co-authored two papers in the list of top ten non-economics papers. One of those is a 2015 Science paper 4 on planetary boundaries — a concept defining the environmental limits in which humanity can develop and thrive — which has attracted more than 750 policy citations. Sörlin thinks one reason it has been popular is that it’s a sequel to a 2009 Nature paper 5 he co-authored on the same topic, which has been cited by policy documents 575 times.
Although policy citations don’t necessarily imply influence, Willett has seen evidence that his paper is prompting changes in policy. He points to Denmark as an example, noting that the nation is reformatting its dietary guidelines in line with the study’s recommendations. “I certainly can’t say that this document is the only thing that’s changing their guidelines,” he says. But “this gave it the support and credibility that allowed them to go forward”.
Broad brush
Peter Gluckman, who was the chief science adviser to the prime minister of New Zealand between 2009 and 2018, is not surprised by the lists. He expects policymakers to refer to broad-brush papers rather than those reporting on incremental advances in a field.
Gluckman, a paediatrician and biomedical scientist at the University of Auckland in New Zealand, notes that it’s important to consider the context in which papers are being cited, because studies reporting controversial findings sometimes attract many citations. He also warns that the list is probably not comprehensive: many policy papers are not easily accessible to tools such as Overton, which uses text mining to compile data, and so will not be included in the database.

The top 100 papers
“The thing that worries me most is the age of the papers that are involved,” Gluckman says. “Does that tell us something about just the way the analysis is done or that relatively few papers get heavily used in policymaking?”
Gluckman says it’s strange that some recent work on climate change, food security, social cohesion and similar areas hasn’t made it to the non-economics list. “Maybe it’s just because they’re not being referred to,” he says, or perhaps that work is cited, in turn, in the broad-scope papers that are most heavily referenced in policy documents.
As for Sage Policy Profiles, Gluckman says it’s always useful to get an idea of which studies are attracting attention from policymakers, but he notes that studies often take years to influence policy. “Yet the average academic is trying to make a claim here and now that their current work is having an impact,” he adds. “So there’s a disconnect there.”
Willett thinks policy citations are probably more important than scholarly citations in other papers. “In the end, we don’t want this to just sit on an academic shelf.”
doi: https://doi.org/10.1038/d41586-024-00660-1
Updates & Corrections
Correction 22 April 2024 : The original version of this story credited Sage, rather than Overton, as the source of the policy papers’ citation data. Sage’s location has also been updated.
Autor, D. H., Levy, F. & Murnane, R. J. Q. J. Econ. 118 , 1279–1333 (2003).
Article Google Scholar
Costanza, R. et al. Nature 387 , 253–260 (1997).
Willett, W. et al. Lancet 393 , 447–492 (2019).
Article PubMed Google Scholar
Steffen, W. et al. Science 347 , 1259855 (2015).
Rockström, J. et al. Nature 461 , 472–475 (2009).
Download references
Reprints and permissions
Related Articles

Will AI accelerate or delay the race to net-zero emissions?
Comment 22 APR 24

We must protect the global plastics treaty from corporate interference
World View 17 APR 24

UN plastics treaty: don’t let lobbyists drown out researchers
Editorial 17 APR 24

CERN’s impact goes way beyond tiny particles
Spotlight 17 APR 24
The economic commitment of climate change
Article 17 APR 24

Last-mile delivery increases vaccine uptake in Sierra Leone
Article 13 MAR 24
Postdoctoral Associate- Artificial Intelligence
Houston, Texas (US)
Baylor College of Medicine (BCM)
Postdoctoral Research Fellow
Looking for postdoctoral fellowship candidates to advance genomic research in the study of lung diseases at Brigham and Women's Hospital and HMS.
Boston, Massachusetts
Brigham and Women's Hospital (BWH)
Position Opening for Principal Investigator GIBH
We aim to foster cutting-edge scientific and technological advancements in the field of molecular tissue biology at the single-cell level.
Guangzhou, Guangdong, China
Guangzhou Institutes of Biomedicine and Health(GIBH), Chinese Academy of Sciences
PostDoc grant- 3D histopathology image analysis
Join a global pharmaceutical company as a Postdoctoral researcher and advance 3D histopathology image analysis! Apply with your proposals today.
Biberach an der Riß, Baden-Württemberg (DE)
Boehringer Ingelheim International GmbH
Postdoctoral Position
We are seeking highly motivated and skilled candidates for postdoctoral fellow positions
Boston, Massachusetts (US)
Boston Children's Hospital (BCH)
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
This website uses cookies to improve your user experience. By continuing to use the site, you are accepting our use of cookies. Read the ACS privacy policy.
- ACS Publications
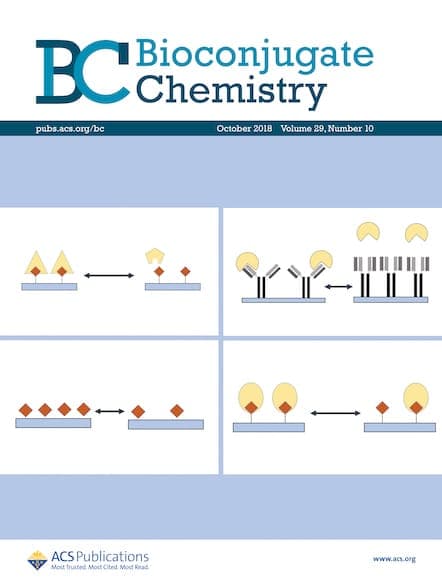
Call for Papers: Brain Targeted Drug Delivery
- Apr 19, 2024
This Special Issue will focus on the latest research in brain targeted drug delivery. Submit your manuscript by June 30, 2024.
The prevalence of central nervous diseases poses significant challenges to society, particularly with the global aging population. While various potential chemical agents, antibodies, and genes have been developed for the treatment of these diseases, the effectiveness of these treatments is greatly hindered by the presence of the blood-brain barrier.
We are pleased to announce that the American Chemical Society journal Bioconjugate Chemistry will publish a Special Issue titled “Brain Targeted Drug Delivery.” With this issue we aim to bring together researchers from different disciplines to share their knowledge and expertise in brain targeted drug delivery.
We welcome topics including, but not limited to:
- Novel approaches to overcome the blood-brain barrier
- Intranasal delivery methods for efficient drug transport to the brain
- Innovative drug delivery strategies for a variety of central nervous system diseases
- Emerging combinations of therapies for the treatment of glioma and Alzheimer’s disease

Guest Editors
Dr. Huile Gao Sichuan University, China
Dr. Zhiqing Pang Fudan University, China
Dr. Yang Liu Sun Yat-Sen University, China
Dr. Jia Li Macquarie University, Australia
How to Submit
- Log in to the ACS Paragon Plus submission site.
- Choose Bioconjugate Chemistry as your journal.
- Select your manuscript type.
- Under “Special Issue Selection” choose “ Brain Targeted Drug Delivery .”
Please see Bioconjugate Chemistry ’s Author Guidelines for more information on submission requirements. The deadline for submissions is June 30, 2024 .
Open Access
There are diverse open access options for publications in American Chemical Society journals. Please visit our Open Science Resource Center for more information.
Stay Connected
Want the latest stories delivered to your inbox each month, bioconjugate chemistry.
More than 1 in 4 deaths among young people in Canada were opioid-related in 2021, study finds
Nationally, annual number of opioid overdose deaths surged from 3,007 to 6,222 over three years.

Social Sharing
Opioid-related deaths doubled in Canada between 2019 and the end of 2021, with Manitoba, Saskatchewan and Alberta experiencing a dramatic jump, mostly among men in their 20s and 30s, says a new study that calls for targeted harm-reduction policies.
Researchers from the University of Toronto analyzed accidental opioid-related deaths between Jan. 1, 2019 and Dec. 31, 2021 in those provinces as well as British Columbia, Ontario, Quebec, New Brunswick and Nova Scotia, and the Northwest Territories.
Manitoba saw the sharpest rise in overdose deaths for those aged 30 to 39 — reaching 500 deaths per million population, more than five times the 89 deaths per million population recorded at the beginning of the study period.
In Saskatchewan, the death toll for that age group nearly tripled to 424 per million, up from 146 per million, while Alberta's rate spiked more than 2.5 times to 729 fatalities per million, up from 272 per million. Ontario's death rate reached 384, up from 210 per million.
B.C., which has been the epicentre of the overdose crisis, recorded 229 deaths per million for that age group in 2019, climbing to 394 in 2020. All data for 2021 from that province's coroners service was not yet available when researchers completed their work based on information collected by the Public Health Agency of Canada.

Push to better understand the long-term harms of opioid use
Nationally, the annual number of opioid overdose deaths surged from 3,007 to 6,222 over the three-year study period, which researchers note coincided with pandemic public health measures that reduced access to harm reduction programs and imposed border restrictions that may have increased the toxicity of the drug supply.
"In addition, for many, the pandemic exacerbated feelings of anxiety, uncertainty and loneliness, contributing to increased substance use globally," they said.
The study was published Monday in the Canadian Medical Association Journal .
Senior author Tara Gomes said one in four deaths involved people in their 20s and 30s. More than 70 per cent of the overall deaths were among men.
A spokesperson with the coroners service in B.C. said 78 per cent of people that fatally overdosed in that province between 2019 and the end of 2021 were men.
Devastating impacts
The sharp surge in fatal overdoses — especially among young adults on the Prairies — suggests provinces must act quickly, said Gomes, an epidemiologist who called for more harm-reduction services including supervised consumption sites.
"Being slow and not being as nimble as we would like to be in our responses can have really devastating impacts," said Gomes, also lead principal investigator of the Ontario Drug Policy Research Network.

Response to opioid crisis must be multipronged, says drug policy expert
Bernadette Smith, Manitoba's minister of housing, addiction, homelessness and mental health, said the province plans to open its first supervised consumption site in Winnipeg next year and will also offer drug-testing machines so people can check if their illicit substances are toxic.
"We came out of a previous government that didn't take a harm-reduction approach, unfortunately," said the New Democrat, whose party defeated the Progressive Conservatives last fall.
'They wouldn't have enough beds'
"We're working with front-line organizations because they have not been listened to or worked with for the last seven years in our province, which has been a real problem," Smith said.
Manitoba plans to train family doctors to treat addiction with medications including Suboxone and methadone, said Smith, noting the physicians typically refer patients to detox for care.

"We're creating a model so that folks aren't having to go to a bunch of different places to get different services," said Smith.
She declined to say whether Manitobans will have access to a prescribed safer supply of drugs.
Tanya Hornbuckle of Edmonton said her son Joel Wolstenholme was 30 when he died in 2022. He became addicted to illicit substances at about age 14, starting with cannabis before shifting to methamphetamine, cocaine and other drugs that were increasingly laced with fentanyl.
He also battled a mental illness, but getting help for both that issue and addiction in a single service was challenging, Hornbuckle said.
Wolstenholme tried multiple times to detox, but there were never enough beds at a clinic where people had to line up at 8 a.m., she said.
"It would happen over and over and then he would call me. I went and stood in line or I drove him there and waited with him in the lineup. They wouldn't have enough beds."
Her son's anxieties and addiction worsened when pandemic restrictions prevented her from entering an emergency room with him because he did not trust staff, Hornbuckle said.
On Feb. 6, 2022, Hornbuckle went to her son's home so they could cook together. She found him dead.
- 8 years and 14,000 deaths later, B.C.'s drug emergency rages on
- Why staff at an Ontario cottage country restaurant took naloxone training
The Alberta government's strategy of focusing more on recovery and abstinence-based treatment than harm reduction, mental health and housing is the wrong approach, said Hornbuckle, noting that for a time her son slept in parks and abandoned houses after losing his vehicle and apartment to addiction.
Rebecca Haines-Saah, an associate professor of community health services at the University of Calgary, called the deaths of young people from overdose a tragedy, and said many more suffer from brain injury due to toxic substances.

Halifax doctor calls for safer opioid access
"Obviously, we have the incorrect response. We do not have the approach and services available to keep people alive," said Haines-Saah, who also called for more harm-reduction services.
"We don't have a full-scale public health response that is required. We don't have any plans to fund anything that relates to what we would call harm reduction."
Much of the current approach to addiction excludes a large number of recreational drug users, said Gomes. She said between a third and half of the deaths in Ontario involved people without an opioid use disorder diagnosis.
"So, focusing on [residential treatment] alone is something that really concerns me because we really need to make sure that we have different options for different people."
Canadian Press health coverage receives support through a partnership with the Canadian Medical Association. CP is solely responsible for this content.
Related Stories
Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
- Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:
Partisan divides over K-12 education in 8 charts

K-12 education is shaping up to be a key issue in the 2024 election cycle. Several prominent Republican leaders, including GOP presidential candidates, have sought to limit discussion of gender identity and race in schools , while the Biden administration has called for expanded protections for transgender students . The coronavirus pandemic also brought out partisan divides on many issues related to K-12 schools .
Today, the public is sharply divided along partisan lines on topics ranging from what should be taught in schools to how much influence parents should have over the curriculum. Here are eight charts that highlight partisan differences over K-12 education, based on recent surveys by Pew Research Center and external data.
Pew Research Center conducted this analysis to provide a snapshot of partisan divides in K-12 education in the run-up to the 2024 election. The analysis is based on data from various Center surveys and analyses conducted from 2021 to 2023, as well as survey data from Education Next, a research journal about education policy. Links to the methodology and questions for each survey or analysis can be found in the text of this analysis.
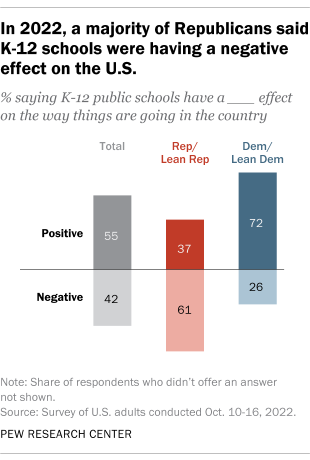
Most Democrats say K-12 schools are having a positive effect on the country , but a majority of Republicans say schools are having a negative effect, according to a Pew Research Center survey from October 2022. About seven-in-ten Democrats and Democratic-leaning independents (72%) said K-12 public schools were having a positive effect on the way things were going in the United States. About six-in-ten Republicans and GOP leaners (61%) said K-12 schools were having a negative effect.
About six-in-ten Democrats (62%) have a favorable opinion of the U.S. Department of Education , while a similar share of Republicans (65%) see it negatively, according to a March 2023 survey by the Center. Democrats and Republicans were more divided over the Department of Education than most of the other 15 federal departments and agencies the Center asked about.
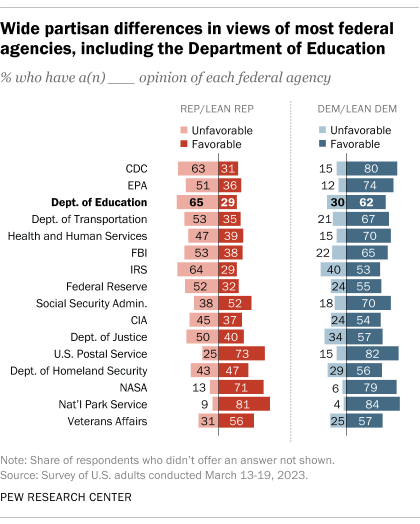
In May 2023, after the survey was conducted, Republican lawmakers scrutinized the Department of Education’s priorities during a House Committee on Education and the Workforce hearing. The lawmakers pressed U.S. Secretary of Education Miguel Cardona on topics including transgender students’ participation in sports and how race-related concepts are taught in schools, while Democratic lawmakers focused on school shootings.
Partisan opinions of K-12 principals have become more divided. In a December 2021 Center survey, about three-quarters of Democrats (76%) expressed a great deal or fair amount of confidence in K-12 principals to act in the best interests of the public. A much smaller share of Republicans (52%) said the same. And nearly half of Republicans (47%) had not too much or no confidence at all in principals, compared with about a quarter of Democrats (24%).
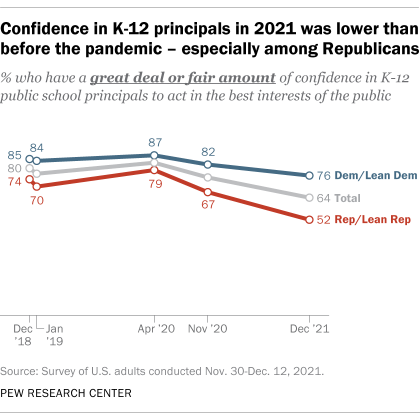
This divide grew between April 2020 and December 2021. While confidence in K-12 principals declined significantly among people in both parties during that span, it fell by 27 percentage points among Republicans, compared with an 11-point decline among Democrats.
Democrats are much more likely than Republicans to say teachers’ unions are having a positive effect on schools. In a May 2022 survey by Education Next , 60% of Democrats said this, compared with 22% of Republicans. Meanwhile, 53% of Republicans and 17% of Democrats said that teachers’ unions were having a negative effect on schools. (In this survey, too, Democrats and Republicans include independents who lean toward each party.)
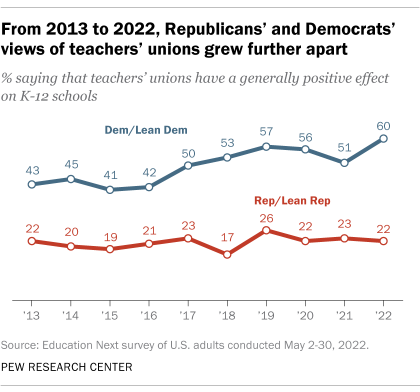
The 38-point difference between Democrats and Republicans on this question was the widest since Education Next first asked it in 2013. However, the gap has exceeded 30 points in four of the last five years for which data is available.
Republican and Democratic parents differ over how much influence they think governments, school boards and others should have on what K-12 schools teach. About half of Republican parents of K-12 students (52%) said in a fall 2022 Center survey that the federal government has too much influence on what their local public schools are teaching, compared with two-in-ten Democratic parents. Republican K-12 parents were also significantly more likely than their Democratic counterparts to say their state government (41% vs. 28%) and their local school board (30% vs. 17%) have too much influence.
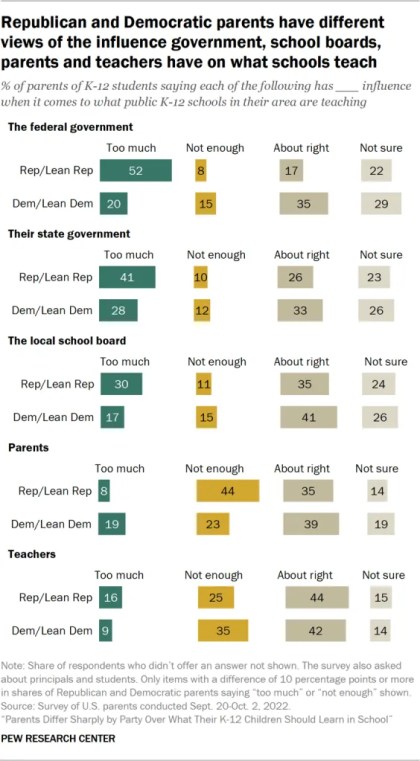
On the other hand, more than four-in-ten Republican parents (44%) said parents themselves don’t have enough influence on what their local K-12 schools teach, compared with roughly a quarter of Democratic parents (23%). A larger share of Democratic parents – about a third (35%) – said teachers don’t have enough influence on what their local schools teach, compared with a quarter of Republican parents who held this view.
Republican and Democratic parents don’t agree on what their children should learn in school about certain topics. Take slavery, for example: While about nine-in-ten parents of K-12 students overall agreed in the fall 2022 survey that their children should learn about it in school, they differed by party over the specifics. About two-thirds of Republican K-12 parents said they would prefer that their children learn that slavery is part of American history but does not affect the position of Black people in American society today. On the other hand, 70% of Democratic parents said they would prefer for their children to learn that the legacy of slavery still affects the position of Black people in American society today.
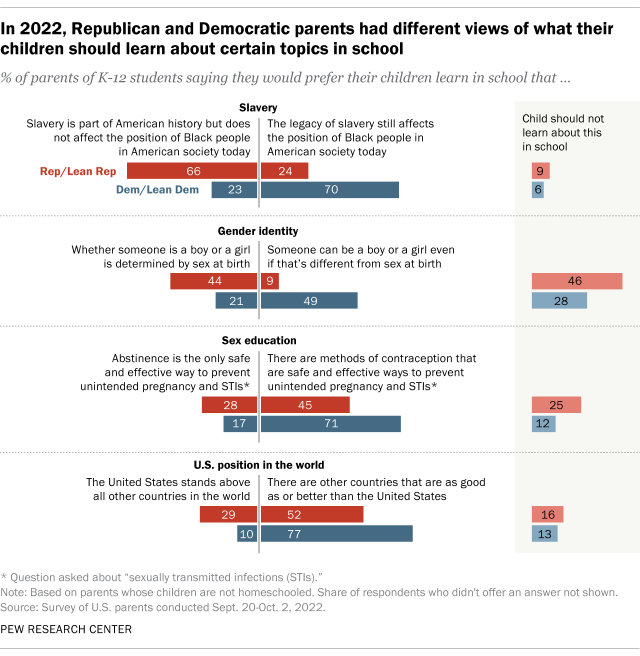
Parents are also divided along partisan lines on the topics of gender identity, sex education and America’s position relative to other countries. Notably, 46% of Republican K-12 parents said their children should not learn about gender identity at all in school, compared with 28% of Democratic parents. Those shares were much larger than the shares of Republican and Democratic parents who said that their children should not learn about the other two topics in school.
Many Republican parents see a place for religion in public schools , whereas a majority of Democratic parents do not. About six-in-ten Republican parents of K-12 students (59%) said in the same survey that public school teachers should be allowed to lead students in Christian prayers, including 29% who said this should be the case even if prayers from other religions are not offered. In contrast, 63% of Democratic parents said that public school teachers should not be allowed to lead students in any type of prayers.
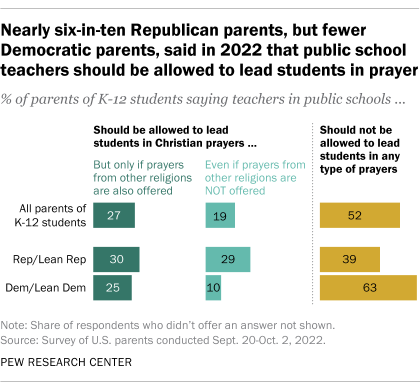
In June 2022, before the Center conducted the survey, the Supreme Court ruled in favor of a football coach at a public high school who had prayed with players at midfield after games. More recently, Texas lawmakers introduced several bills in the 2023 legislative session that would expand the role of religion in K-12 public schools in the state. Those proposals included a bill that would require the Ten Commandments to be displayed in every classroom, a bill that would allow schools to replace guidance counselors with chaplains, and a bill that would allow districts to mandate time during the school day for staff and students to pray and study religious materials.
Mentions of diversity, social-emotional learning and related topics in school mission statements are more common in Democratic areas than in Republican areas. K-12 mission statements from public schools in areas where the majority of residents voted Democratic in the 2020 general election are at least twice as likely as those in Republican-voting areas to include the words “diversity,” “equity” or “inclusion,” according to an April 2023 Pew Research Center analysis .
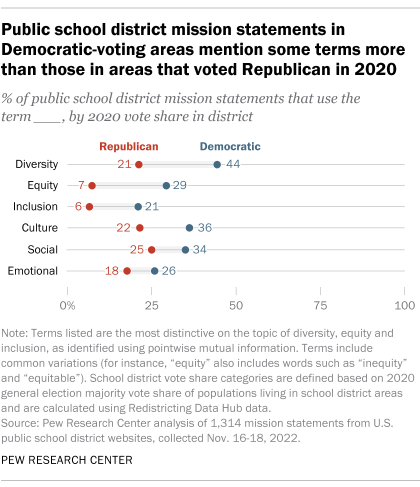
Also, about a third of mission statements in Democratic-voting areas (34%) use the word “social,” compared with a quarter of those in Republican-voting areas, and a similar gap exists for the word “emotional.” Like diversity, equity and inclusion, social-emotional learning is a contentious issue between Democrats and Republicans, even though most K-12 parents think it’s important for their children’s schools to teach these skills . Supporters argue that social-emotional learning helps address mental health needs and student well-being, but some critics consider it emotional manipulation and want it banned.
In contrast, there are broad similarities in school mission statements outside of these hot-button topics. Similar shares of mission statements in Democratic and Republican areas mention students’ future readiness, parent and community involvement, and providing a safe and healthy educational environment for students.
- Education & Politics
- Partisanship & Issues
- Politics & Policy
About 1 in 4 U.S. teachers say their school went into a gun-related lockdown in the last school year
About half of americans say public k-12 education is going in the wrong direction, what public k-12 teachers want americans to know about teaching, what’s it like to be a teacher in america today, race and lgbtq issues in k-12 schools, most popular.
1615 L St. NW, Suite 800 Washington, DC 20036 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Age & Generations
- Coronavirus (COVID-19)
- Economy & Work
- Family & Relationships
- Gender & LGBTQ
- Immigration & Migration
- International Affairs
- Internet & Technology
- Methodological Research
- News Habits & Media
- Non-U.S. Governments
- Other Topics
- Race & Ethnicity
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
Copyright 2024 Pew Research Center
Terms & Conditions
Privacy Policy
Cookie Settings
Reprints, Permissions & Use Policy
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

The Changing Opioid Crisis: development, challenges and opportunities
Nora d. volkow.
1 National Institute on Drug Abuse, Bethesda, MD 20892
Carlos Blanco
The current opioid epidemic is one of the most severe public health crisis in US history. Responding to it has been difficult due to its rapidly changing nature and the severity of its associated outcomes. This review examines the origin and evolution of the crisis, the pharmacological properties of opioids, the neurobiology of opioid use and opioid use disorder (OUD), medications for opioid use disorder (MOUD), and existing and promising approaches to prevention. The results of the review indicate that the opioid epidemic is a complex, evolving phenomenon that involves neurobiological vulnerabilities and social determinants of health. Successfully addressing the epidemic will require advances in basic science, development of more acceptable and effective treatments, and implementation of public health approaches, including prevention. The advances achieved in addressing the current crisis should also serve to advance the science and treatment of other substance use disorders.
Origins and Evolution of the Crisis
The current opioid epidemic is one of the most severe public health crisis in US history. Providing an effective response has been difficult because of its changing nature, geographic and demographic diversity, multiplicity of its causes, and the severity of adverse outcomes associated with opioid use and opioid use disorder (OUD). Furthermore, opioid analgesics, which fueled the origins of the opioid epidemic, are therapeutically beneficial when used properly. This, compounds the difficulties of regulating their availability because they cannot be banned, in contrast with illicit drugs. While earlier phases (i.e., first wave) of the crisis were predominantly driven by non-medical use and addiction to prescription opioid analgesics, heroin (second wave) and subsequently illicit synthetic opioids (third wave) have become progressively important as the crisis progressed and more recently there is emerging evidence of increasing fatalities associated with the combination of psychostimulant drugs with opioids (fourth wave). These changes explain why despite the decreases in the number of opioid prescription dispensed, the number of opioid fatalities has continued to rise unabated. 1 Although the opioid crisis is often seen through the prism of fatal overdoses, its most dramatic manifestation, the misuse of opioids and OUD also lead to death, disease and suffering from many other causes with devastating medical, social and economic consequences. 2 - 5
Like most complex problems, the opioid crisis has multiple roots, 5 including changing social and economic conditions, limited availability of safe and effective analgesics, insufficient treatment capacity for OUD and legal approaches that criminalize OUD rather than fostering treatment. The two major driving factors of the crisis, however, were the steady increase in the rate of opioid prescriptions, particularly in the early stages of the crisis, and the decrease in price and the increase in availability of heroin and synthetic opioids.
Increases in the rate of opioid prescribing followed the identification of undertreatment of pain in the 1990s as an important clinical problem 6 and the mistaken belief, based on anecdotal evidence, that patients in pain were not at risk for OUD. 7 Although less than 10% of individuals to whom opioids are prescribed develop OUD, 8 large increases in the rates of opioid prescriptions inevitably led to more individuals being exposed to opioids and subsequent increases in OUD prevalence. More importantly, increased availability of opioids generated an enormous surplus of medication that was diverted for non-medical use. 9 From 1991 to 2013, the prevalence of non-medical use of prescription opioids in the US more than doubled, from 1.5% to 4.1%, and the prevalence of prescription OUD tripled, from 0.3% to 0.9%. 10 , 11 At the same time, the severity of nonmedical use, as measured by the frequency of use, also increased among nonmedical users. 12
A second major factor in the crisis was the increased accessibility and purity of heroin coupled with reduced price partly due to increases in the efficiency of its distribution channels, which led to increases in heroin use and heroin use disorder. From 2001-2002 and 2012-2013 the prevalence of lifetime heroin use in the US increased from 0.33% to 1.6% and the lifetime prevalence of heroin use disorder increased from 0.21% to 0.69%. 13 , 14 There is controversy regarding whether efforts to decrease use of prescription opioids led to increases in heroin use and use disorder. Although individuals who use prescription opioids are more likely than those who don’t to use heroin, only 3%-5% of individuals who used prescription drugs non-medically in the previous year also reported using heroin during the same year. 15 Furthermore, increases in heroin use among nonmedical prescription opioids users preceded the development of policies to address misuse of prescription opioids. Thus, it may be the case that efforts to improve prescription of opioids have played a more limited role in the increases in heroin use than that ascribed to them. 16
A more recent entrant has been fentanyl and other very potent synthetic fentanyl analogues. From 2010 to 2017, deaths from fentanyl and other synthetic opioids increased nearly ten -fold, from around 3,000 (14.3% of opioid-related deaths) to over 28,466 (59.8%). 17 , 18 Synthetic opioids are now almost twice as commonly involved in overdose deaths as prescription opioids or heroin. 17 The low production costs of fentanyl and its potency (50- fold compared to heroin) make it an attractive option to mix (“lace”) with heroin and illicit manufactured prescription opioids. 19 At present, it is not known how many users actively seek fentanyl, but regardless of intent, heroin users are being exposed to fentanyl or other analogues without realizing it, increasing their risk of overdosing. Overdoses from fentanyl by itself or combined with heroin appear to be harder to reverse with naloxone than overdoses due to prescription opioids or pure heroin, contributing to the lethality of fentanyl or drugs laced with it. The reasons for the decreased efficacy of naloxone for reversing fentanyl overdoses are unclear and might reflect, its very high potency at the mu opioid receptor (MOR), its very fast pharmacokinetics (entering the brain very rapidly minimizing time for intervention), longer duration of its respiratory depressing effects (that might explain re-narcotization after a temporary reversal of an overdose by naloxone) and/or an additive effects when fentanyl is combined with other drugs including heroin. 20
Pharmacological properties of opioids
In addition to their effect on MOR, opioid drugs also bind to kappa- (KOR) and delta-opioid (DOR) receptors, although their affinity, intrinsic efficacy, pharmacokinetics and bioavailability vary by drug. In particular opioid drugs with fast uptake into the brain and full agonist effects at MOR such as heroin and fentanyl are particularly rewarding. 20 A strategy for developing opioid medications with lower abuse liability entails opioids formulations with slower entry into the brain and/or formulations that cannot be injected, since this is the route of administration that results in the faster rate of drug uptake in brain. The intrinsic efficacy of full agonist drugs such as heroin and fentanyl leads to greater rewarding effects than for partial agonists such as buprenorphine. Additionally, the rate of clearance of opioid drugs from the brain determines their duration of action and the severity of withdrawal symptoms upon their discontinuation. For that reason, heroin is associated with a much more severe withdrawal than a drug such as buprenorphine, which clears the brain more slowly. Opioids drugs with longer half-lives, slower clearance rates and slower brain uptake are favored for the treatment of OUD. By binding to MOR they decrease craving and prevent the emergence of withdrawal symptoms. Methadone enters the brain rapidly, which is why it is given orally when used for OUD treatment, for this will slow its entry into the brain. Also while it is a full MOR agonist, it has agonist effects at galanin receptors, which are co-expressed with MOR in brain reward regions antagonizing them, and thus reducing methadone’s rewarding effects. 31
The positive (increase reward) and negative (avoid pain) reinforcing effects of opioids, trigger learned associations between the receipt of the drug and these experiences resulting in conditioning. In parallel, the repeated administration of opioids triggers physiological adaptations that result in tolerance and in physical dependence. Tolerance necessitates increasing opioid doses in order to achieve the same levels of analgesia and when misusing them increasing the doses or shifting to more potent opioids such as fentanyl in order to experience their rewarding effects. The development of tolerance does not occur at the same rate for the various pharmacological effects of opioids. In general, tolerance to the analgesic and hedonic effects develops faster than to respiratory depression, whereas tolerance to constipation might never develop. 32 This explains why increases in dose to maintain analgesia (or reward) or doses injected to get high can markedly increase the risk of overdose.
Physical dependence to opioids also occurs rapidly and is responsible for the emergence of withdrawal symptoms when opioids are abruptly discontinued, which creates a negative reinforcement mechanism that can contribute to the maintenance of opioid use. The severity of withdrawal symptoms varies as a function of the opioid drug used; greater for higher potency short acting opioids than for longer lasting opioids as well as the chronicity of exposure. The symptoms from acute withdrawal usually resolve within days and are rarely lethal, but are extremely uncomfortable and are a powerful trigger for relapse in those with an OUD and for continued opioid use among those being treated with opioid analgesics. The risk of withdrawal is minimized or prevented by tapering opioids gradually.
Repeated use of opioids often results in physical dependence as a result of multiple neuroadaptations including desensitization and internalization of the MOR, impaired MOR signaling with intracellular effectors, and adaptations in glial signaling and in neuropeptide systems that interact with MOR-sensitive neurons, among others 33 , 34 . In contrast to physical dependence, OUD develops only in a minority of individuals exposed to opioids. It is characterized by a pattern of maladaptive opioid use that leads to clinically significant impairment or distress and is manifested as intense craving for opioids, erosion of inhibitory control over efforts to refrain from using them, persistent thinking about procuring the drug, and impaired control over opioid use. Because of their repeated opioid use, those with OUD also suffer from physical dependence and tolerance, unless they have undergone supervised medical withdrawal (formerly known as detoxification) in which case they can have OUD without having physical dependence or tolerance. This is clinically relevant in that patients undergoing medically supervised withdrawal without subsequent treatment for OUD are at an extremely high risk of relapse and of overdosing since they crave the drug as intensely as prior to their withdrawal but have lost their tolerance to the opioids. The behavioral manifestations of OUD are associated with structural and functional changes in the brain’s reward, executive control, emotion and interoceptive circuits. 58 , 59
Biological factors contributing to OUD
In addition to the environmental contributions to the crisis, multiple biological factors modulate an individuals’ vulnerability for opioid use, non-medical use and OUD, including genetic predisposition, brain development, mental illness and social factors.
Studies of genetic epidemiology indicate that genes contribute about 50% of the vulnerability to SUD, including OUD. Yet identifying specific genetic variants for increased OUD risk has been difficult, which is likely to reflect in part the fact that OUD, like other psychiatric disorders is a polygenic disease. Genes influence brain development and function of brain circuits and neurotransmitter systems that mediate the reactivity to the environment including drug responses. Furthermore, genes can intervene at different stages of OUD development, including propensity to use (i.e. genes that modulate personality traits) risk of transition from use to OUD (i.e. gene involved in conditioning and neuroplasticity), and vulnerability to relapse (i.e. genes that modulate severity of withdrawal symptoms, sensitivity to stress or other potential triggers). Because OUD often co-occurs with other psychiatric disorders, genes that increase the risk for those co-occurring disorders can also indirectly increase OUD risk. The effects of genes are also moderated by environmental influences.
Despite these complexities, studies have been able to identify genes that appear to contribute to OUD risk ( Table 1 ). For example, OPRM1 the gene that encodes for MOR has been implicated in increased vulnerability to OUD. 35 Similarly, converging evidence of genome-wide association, neuroimaging and rodent studies support a role in OUD for CNIH3, a gene that encodes for the Cornichon Family AMPA Receptor Auxiliary Protein that regulates trafficking and gating properties of AMPA receptors. 36 Preliminary results also suggest that the BDNF Val(66) Met genotype, which has been associated with neurobehavioral deficits, may promote drug-seeking in individuals with OUD. 37
Genes associated with increased vulnerability to opioid use disorder
Other genes, though not directly linked to OUD, relate to risk factors, such as personality traits, or brain regions implicated in the circuitry of addiction. For example, polymorphisms associated with low activity in MAOA , the gene for monoamine oxidase A, have been linked to a predisposition to externalizing behaviors and disorders that is moderated by environmental exposures. 38 , 39 Similarly, the catecholamine-O-methyltransferase (COMT) gene variant V(108/158)M, leads to greater dopamine degradation and impaired modulation of prefrontal cortex 40 , and has been associated with increased amygdalar reactivity 41 and with disrupted modulation of cortical and striatal activation during anticipation or receipt of a reward. 42 , 43 Numerous animal and human studies have also demonstrated the role of dopamine receptors in reward related behaviors, 44 - 46 but to date, no study has directly linked any dopamine-related gene to the risk of OUD.
Genes whose product influence synaptic plasticity can also contribute to OUD risk, such as Homer proteins, which regulate the level and activity of glutamate receptors, 47 and matrix metalloproteinase 9 (MMP-9), which in animal models increases motivation for drug-seeking. 48 , 49 Genes that influence response to stress by modulating the glucocorticoid receptor’s affinity for cortisol such as the FKBP5 chaperone protein 50 may also increase risk of OUD.
Brain Development
Drug experimentation is commonly initiated during adolescence and the risk to addiction is increased with early drug use. The greater vulnerability of adolescents to drug use and experimentation is driven by multiple factors including genetics that are associated with the developmental trajectories of the human brain. At the same time the social environments during childhood will influence brain development in ways that can increase its vulnerability to drugs or provide with resilience. Notably, the development of the human brain has a greater sensitivity to environmental factor during the first than second decades of life whereas genes influence brain development throughout the first and second decades. 51 This explain why social stressors are particularly harmful during early childhood. However while it is heuristically useful to distinguish environmental from genetic factors, it is likely that it is their interactions that ultimately determine how the brain will develop.
A better characterization of human neurodevelopment has allowed us to start to understand the role of the environment at critical moments of brain development and how differences in the rate of development of neuronal circuits influence vulnerability for drug use. For example, during adolescence reward and emotion circuits develop faster than those related to executive function, creating an imbalance between systems that favor experimentation, reward-seeking and drug use and systems underpinning self-regulation. Early exposure to drugs of abuse may further impair the development of the prefrontal cortex, decreasing self-regulating capabilities and increasing the long-term risk for SUD. 52
Several brain imaging studies have started or will soon start to generate data to inform the development of the brain and the influence of substance use in this development. The Adolescent Brain Cognitive Development Study (ABCD) is a longitudinal study of children 9-10 years old who will be assessed with brain imaging, genotyping, and deep phenotyping and followed for 10 years. It recently completed the baseline assessment of 11,875 children and has started to provide valuable data on normal variability in brain development and its influence by environmental factors. 53 The Baby Connectome Project is a four-year study of children from birth through five years of age, intended to provide a better understanding of how the brain develops from infancy through early childhood and the factors that contribute to healthy brain development. 54 It will help characterize human brain connectivity and map patterns of structural and functional connectivity to important behavioral skills. Additional biological (e.g., genetic markers) and environmental measures (e.g., family demographics) will be collected and examined to provide a more comprehensive picture of the factors that affect brain development. Finally, the planned HEALthy Brain and Child Development (HBCD) study aims to prospectively follow 7,500 infants through childhood (e.g., age 9-10) to assess structural and functional brain development as well as cognitive, behavioral, social, and emotional development and the long-term impacts of pre/postnatal drug (expected oversampling for opioid prenatal exposures) and adverse environmental exposures on brain and behavioral health and risk for substance use and mental disorders.
Social determinants
Epigenetics are implicated in the persistent neuroplastic changes associated with exposure to environmental factors that increase vulnerability to addiction such as social stressors or drug exposures. 55 For example, the environment’s ability to shape the circuits of emotion, particularly those impacted during critical periods of prenatal, postnatal, and adolescent brain development, 56 taps heavily on epigenetic mechanisms. 46 , 57 Studies have also started to assess the effects of social stressors on the development of the human brain, and these studies are relevant for understanding why social stressors increase the risk for SUD and other psychiatric disorders. Studies evaluating the effects of social deprivation during infancy and early childhood have reported delayed maturation that results in impaired brain connectivity, which could underlie increased impulsivity in these children. 58 Fortunately, preliminary studies suggest that interventions that provide social support may help reverse some of these impairments. 59 Nevertheless, stressful events at any age can increase vulnerability to opioid use and OUD.
Though the developing brain is the most sensitive to adverse social environments, these can also negatively influence the adult brain in ways that increase the vulnerability to drugs use and addiction. This is apparent in the current opioid epidemic and the other “deaths of despair” (overdoses, suicide and alcohol-driven cirrhosis) that have prominently affected adult white Americans from economically impoverished environments. There is a scarcity of research on the effects of adverse social environments on adult brain function. 60 , 61
Neurocircuitry of addiction
Reward circuitry.
Although much remains to be learned, our growing knowledge of the brain’s reward circuitry (originating in the dopamine neurons in the ventral tegmental area projecting to the nucleus accumbens, ventral prefrontal cortex and amygdala) and its changes have been fundamental for understanding drug taking and addiction. Reward (more precisely, reinforcement) can be defined as any event that increases the probability of repeating the action. Animal 62 , 63 and human studies consistently indicate that drugs release dopamine (DA) in the nucleus accumbens (NAc), which is fundamental to their rewarding effects. Additionally, increases in endogenous opioids and cannabinoids are also associated with the rewarding effects of various drugs. 64 , 65 It is thought that the rapid release of DA and its binding to D 1 receptors (D1R) in the ventral (location of NAc) and dorsal striatum, which stimulates cyclic AMP (cAMP) signaling is associated with euphoria and pleasure (so-called “high”) and triggers conditioning (learned association between the drug effects and situation where it occurred). By contrast, stimulation of D 2 receptors (D2R), which inhibit cAMP signaling, does not appear to be associated with rewarding effects per se but blocks the aversive effects when D2R-expressing medium spiny neurons (D2R-MSN) are not inhibited by DA. 66 Individuals with SUD often have decreased baseline DA release in the striatum (including in nucleus accumbens) and experience an attenuated DA increase and less intense reward from drug use (i.e., tolerance), which is interpreted to reflect a hypofunction of their reward circuit. It is unknown to what extent this hypofunction reflects a predisposition of the individual versus consequences from chronic drug exposures.
With repeated drug use, conditioning strengthens and drives the motivation to procure the drug reinforcers. Exposure to conditioned stimuli (referred to as cues) by themselves triggers firing of DA neurons and DA release, energizing the motivation to obtain the drug. When previously neutral stimuli become conditioned to the drug they acquire incentive salience, becoming desirable 67 . Conditioning and the associated DA increases in the striatum are hypothesized to underlie the intense desire for drugs that addicted individuals experience upon exposure to environments or situations where they have taken drugs that frequently leads them to relapse.
The drug-induced stimulation of D1R signaling involved with conditioning triggers synaptic changes in N-methyl-D-aspartate (NMDA) and α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptors that enhance glutamatergic signaling in the affected synapses. 68 , 69 At the circuit levels these neuroplastic changes strengthen striatal- pallidal-thalamo-cortical loops that include the ventral and the dorsal striatum, resulting in habit formation 70 and compulsive response for drugs. As SUD progresses, a prominent hypothesis is that these circuits become increasingly sensitized to drug-cues, environmental stressors or negative emotional states, which can then more readily trigger compulsive drug consumption. In more advanced stages, substance use behaviors are more driven by a growing importance of dorsal striatum and habits and a decreasing role of positive drug reward. In parallel, as drug-procuring and taking becomes increasingly salient in the addicted individual, non-drug related activities become less motivating and rewarding. 71 , 72
Although DA and glutamate remain central to our understanding of the reward circuits, these circuits are also modulated by γ-aminobutyric acid (GABA), serotonin, acetylcholine, and the endogenous opioid and cannabinoid systems. Similarly, it is important to realize that, like any other, the reward circuit (as well as the executive control circuit) interact and overlap with circuitry involved in the perception of internal bodily states or interoception (including primary sensory cortex, insula, anterior cingulate cortex and precuneus), homeostasis (hypothalamus), stress (amygdala, hypothalamus, and habenula), salience attribution (orbitofrontal cortex) and learning and memory (amygdala, hippocampus and dorsal striatum) and that the interplay with these circuits modulates the responses to rewards and to conditioned cues ( Figure 1 ). 73

The circuitry of opioid use disorder (reprinted with permission from: George O, Koob GF. Control of craving by the prefrontal cortex. Proc Natl Acad Sci U S A. 2013 Mar 12;110(11):4165-4166
Emotion Circuitry
Although positive reinforcers play a major role in the initial phases of drug taking and the development of OUD, in more advance stages negative emotional experiences such as withdrawal symptoms, craving and enhanced sensitivity to stress become increasingly important and drive drug taking. The increased role of negative reinforcement in drug taking (as a means to escape the negative emotional state) is a considerable barrier to abstinence and a formidable obstacle to successful treatment.
The negative emotional state can be understood as enhancement of processes that are the inverse of those involved in reward (i.e., “anti-reward processes”) 74 that are derived from neuroadaptions to drug-induced stimulation. 62 In the case of opioids most of the physical manifestations of withdrawal, which emerge with drug discontinuation are caused by decreased MOR-triggered intracellular signaling and by enhanced autonomic reactivity. 75 Early signs of withdrawal, appearing generally in the first 8-36 hours of heroin discontinuation include mydriasis, piloerection, muscle twitching, lacrimation, rhinorrhea, diaphoresis, yawning, restlessness, myalgia, abdominal pain, nausea/vomiting, tremor and insomnia. Individuals with fully developed opioid withdrawal can also experience tachycardia, tachypnea, hypertension or hypotension, dehydration, hyperglycemia, fever, anorexia and diarrhea.
In addition to these physiological manifestations, opioid withdrawal is often associated with neuropsychological symptoms that include, irritability, emotional pain, dysphoria, insomnia and subjective distress that can last several months. The subjective aspects of the negative emotional state are associated with disrupted dopaminergic, serotonergic, noradrenergic, glutamatergic, GABAergic neurotransmission in reward and emotion networks (including NAc). 67 Stress-related neurotransmitters, such as CRF, norepinephrine, and dynorphin, are also recruited in the extended amygdala and contribute to the distress and increased irritability often present in withdrawal and protracted abstinence. 76 The lateral habenula, which decreases DA neuronal firing in VTA when expected rewards do not materialize 77 - 79 and is a target of serotonin neurons from the dorsal raphe that modulate mood, also plays a crucial role in triggering and maintaining negative emotional states. 80 Similarly, the insula, which is reciprocally connected to several limbic regions and to the default mode network (DMN) has an interoceptive function that integrates autonomic and visceral information with emotion and motivation 81 , plays a key role in the self-awareness of negative emotional states and of craving. 82 - 84
Executive Control Circuitry
Impairments in executive function (including self-regulation), which can precede as a vulnerability factor for SUD or develop secondary to chronic drug exposures, are important contributors to impulsive and compulsive drug taking. 67
During withdrawal the emergence of the preoccupation/anticipation phase along with mounting craving for the drug results from the interplay of two opposing systems: a Go and a Stop system. The Go system includes most of the circuitry described in the two previous sections, which underlies the hedonic, habitual and emotional aversive aspects that leads to continued drug taking. 85 , 86 The Stop system seeks to control the incentive value of choices, regulate habitual behavior, maintain goal-directed behavior and suppress affective responses to negative emotional signals. 87 - 89 In this framework, the Stop system seeks to inhibit signals generated by the Go system.
The Stop system involves a widely distributed and complex prefrontal cortex–subcortical circuitry. It is mediated through glutamatergic projections from prefrontal cortex to the caudate and ventral striatum to modulate the striatal-pallidal-thalamocortical direct (D 1 receptor-mediated) and indirect (D 2 receptor-mediated) pathways, and to modulate the mesocortical dopamine neurons in the ventral tegmental area, which exert control over DA release in the prefrontal cortex. 73 Deficits in prefrontal cortex in individuals with SUD are associated in impairments in executive function that can interfere with decision making, self-regulation, inhibitory control, and working memory. 90 Reduced activity in the prefrontal cortex (including dorsolateral prefrontal cortex, anterior cingulate gyrus, and medial orbitofrontal cortex) is also associated with downregulation of D2R in the striatum, 91 - 93 and disrupted GABAergic activity in striatum and prefrontal cortex. 94 , 95
The orbital frontal cortex, anterior cingulate cortex and dorsolateral prefrontal cortex are involved with incentive salience, emotional regulation, and decision making, respectively. Deficits in striatal D2R-mediated DA signaling, which modulates them, may underlie the enhanced motivational value of drugs and the loss of control over drug intake in SUD. 96 Furthermore, because dysfunction of the orbital frontal cortex and the anterior cingulate cortex are associated with compulsive behaviors and impulsivity, 97 DA’s impaired modulation of these regions may contribute to compulsive and impulsive drug taking in SUD. 96
Several pathways can encode signals that increase the risk of relapse with exposure to cues, which can activate the ventral prefrontal cortex, including ventral anterior cingulate, and medial and lateral orbitofrontal cortices. 98 - 101 Cue-induced reinstatement involves glutamatergic projections from the prefrontal cortex, basolateral amygdala, and ventral subiculum to the NAc, and DA projections to the basolateral amygdala and dorsal striatum. 102 - 104
In contrast to cue-induced relapse, stress-induced reinstatement depends on the activation of both CRF and norepinephrine in parts of the extended amygdala (i.e., central nucleus of the amygdala and bed nucleus of the stria terminalis) and the VTA. 105 Protracted abstinence, mostly described for alcohol, appears to involve overactive glutamatergic and CRF systems. 106 , 107 A third pathway to relapse is through interoceptive stimuli related to the insula 82 - 84 and its activation during craving has been associated with relapse. 108
Pharmacological treatment of opioids
A range of pharmacological treatments exists to treat different components of OUD. Information on these medications was recently reviewed by the U.S. Substance Abuse and Mental Health Administration 109 and by the National Academy of Medicine. 110
Medically supervised withdrawal (formerly referred to as detoxification) is the gradual taper of opioid agonist medications (methadone or buprenorphine) guided by a clinician to alleviate withdrawal symptoms. The use of α 2 -agonists such as lofexidine (recently approved by the FDA for the treatment of opioid withdrawal) or clonidine can also help attenuate symptoms of withdrawal, 111 though subsequent initiation of medications for OUD (MOUD) is required to prevent relapse into drug taking. Indeed, medically supervised withdrawal is not recommended as an isolated strategy, as most patients without subsequent MOUD initiation relapse shortly thereafter 112 - 114 and are at increased risk for overdosing due to the loss of tolerance. 115 Medically supervised withdrawal is required, though, for patients starting naltrexone, as described in the next section.
Maintenance
Ongoing outpatient treatment with MOUD leads to better retention and outcomes for OUD 116 and reduced risk of HIV and HCV infection and overdose death. 117 - 121 At present, MOUD constitutes the standard of care for most patients with OUD. There are three FDA-approved MOUD: methadone, buprenorphine and naltrexone. In deciding on a specific medication the clinician should evaluate the patient’s responses to prior MOUD treatment, tolerance to opioids and patient preferences. Patients, in turn, should be informed of the efficacy, risks, benefits and relative advantages of each of these medications.
Methadone has been available the longest and has the largest evidence of efficacy. 119 , 121 Higher doses of methadone are associated with better retention in treatment, less heroin use during treatment and lower withdrawal symptoms, until around 100 mg/day, after which the reliability of evidence is lower. 122 Because methadone is a full MOR agonist, it has no ceiling effect. It can lead to overdoses if it is used at doses above the patient’s tolerance or combined with other central nervous depressants such as alcohol, benzodiazepines or other opioids. To minimize the risk of intoxication or overdose, methadone should be started at low doses and increased gradually with daily monitoring over several weeks. An important barrier to the use of methadone, particularly in rural settings is that, with a few exceptions, in the US methadone has to be administered in a licensed opioid treatment programs (methadone clinics) and cannot be prescribed by office-based clinicians.
The use of buprenorphine 123 , 124 has certain advantages over methadone, which explains its growing use for OUD treatment. First, although it can still be lethal when combined with other central nervous depressant substances, as a partial agonist, buprenorphine has lower lethality than methadone. 124 Second, its antagonist effects at the KOR may contribute to its efficacy for OUD. 125 , 126 Its KOR antagonist properties may also have antidepressant effects, which could help improve the depressive symptoms that are common in OUD. Buprenorphine is also an agonist at the nociceptin receptor, which is also implicated on its therapeutic benefits. To deter the injection of buprenorphine, which would enhance its rewarding effects, it is often prescribed in a formulation that includes naloxone, a short-acting opioid antagonist that has poor bioavailability when sublingually administered, but blocks buprenorphine effects if injected. Currently, in the US, prescribers of buprenorphine for the treatment of OUD need to obtain a waiver from the Drug Enforcement Administration (DEA) after completing an 8-hour training.
Extended-release (XR) formulations of buprenorphine have been developed to improve patient adherence. Although, 6-months buprenorphine implants were shown to be as effective as low-dose sublingual buprenorphine, 127 its benefits are restricted to patients who respond to low doses of buprenorphine (8mg). In 2017, the FDA approved a 1-month XR buprenorphine injection for patients with OUD who have been treated with sublingual buprenorphine for at least one week. Another 1-month and a 1-week XR buprenorphine are currently under FDA review. It would be important to know whether those new formulations can increase treatment retention.
The third FDA-approved MOUD is naltrexone, which is a MOR antagonist that can be prescribed by clinicians in outpatient practice. The efficacy of its immediate release formulation was limited by poor adherence, but the development of a monthly extended release formulation (XR-NTX) significantly improved outcomes. 128 - 131 It has been particularly useful in justice system settings reluctant to use agonist therapies, 130 although there is need to assess whether it would be superior to XR-buprenorphine in those settings. Naltrexone is also a KOR antagonist, and while its affinity is lower than that for MOR, a recent brain imaging study reported KOR occupancies > 80% in patients with alcohol use disorder treated with naltrexone. 132 Antagonism of KOR by naltrexone could contribute to the mood improvements reported in OUD patients treated with naltrexone. 133 A potential barrier for the use of XR-NTX is the need for medically supervised withdrawal. Patients cannot use short-acting opioids for at least 7 days and long-acting opioids for 10-14 days preceding induction onto naltrexone to avoid triggering a withdrawal syndrome. A rapid taper consisting of a single day of buprenorphine followed by ascending doses of oral naltrexone along with clonidine and other adjunctive medications (e.g., clonazepam and prochlorperazine) may allow for faster induction protocols for XR-NTX, 131 but requires further study before it can be recommended as standard strategy.
At present, limited data are available regarding the comparative effectiveness of MOUD or about which patients will respond better to each medication. 109 A Cochrane review concluded that flexible-dose methadone leads to greater retention than sublingual buprenorphine, 119 but whether the same results would hold when compared with XR-buprenorphine is unknown. There are currently no published Cochrane reviews of XR-NTX versus buprenorphine, but two studies 134 , 135 have suggested that patients who can be inducted onto XR-NTX have similar outcomes to those treated with sublingual buprenorphine. However, in one of those studies 134 a substantial proportion of patients were unable to complete XR-NTX induction, mostly due to early relapse, leading to superior outcomes for the buprenorphine group in the intent-to-treat analysis.
As knowledge about MOUDs continues to grow, three priority areas need to be addressed. First, studies suggest that longer time in treatment is associated with better outcomes and that the risk of relapse greatly increases after medication discontinuation, yet rates of MOUD discontinuation in the first 6 months of treatment remain very high. Thus, there is a need to improve retention in MOUD treatment. It is also important to know which patients, when and under what circumstances can safely discontinue MOUD.
Second, current evidence indicates that counseling or psychotherapy do not increase retention in buprenorphine treatment or improve abstinence rates 116 , 136 - 139 and that methadone treatment 140 and buprenorphine without concomitant counseling is vastly superior to no treatment. 141 It is important to determine whether the potential benefits of concurrent psychotherapy outweigh the barrier to treatment created by requiring provision of psychotherapy when delivering buprenorphine treatment (such counseling is at present not required for XR-NTX). This was highlighted in the recent report of the National Academy of Medicine , which emphasized that lack of behavioral treatment support is not a reason for withholding MOUD. 110 Nevertheless, evidence-based behavioral interventions can be useful in engaging some patients with OUD in treatment, retaining them in treatment, improving outcomes, and helping them achieve recovery . 142 More research is needed to determine which behavioral interventions provided in conjunction with MOUD are most helpful for which patients, including evidence on the effectiveness peer support. There is also a need to develop models of care that better attract and retain patients in care and can overcome the barriers posed by the limited availability of well-trained clinicians. The use of technology-based approaches (i.e Telehealth, mHealth) may be a promising avenue to achieve these goals.
Third, research is needed to evaluate whether residential or inpatient treatment is superior to outpatient treatment for initiating MOUD. This question is important to evaluate the optimal allocation of resources for the treatment of OUD.
Preventing Opioid-Related Overdoses
Despite national and local efforts, the number of opioid-related overdoses continue to increase, highlighting the need of clinicians to educate patients and their families about the risk of overdose and how to respond to it. Several medication- and patient-related factors increase the risk of overdose. 143 Patient-related factors include: 1) Age above 65 years; 2) respiratory problems; 3) long-term opioid use; 4) substance use disorder (including alcohol use disorder); 5) comorbid mood disorders and/or suicidality; 6) use after a period of abstinence (e.g. following medically supervised withdrawal or incarceration); 7) prior overdose. Medication-related factors include: 1) Daily dose above 100 morphine milligram equivalents; 2) use of higher doses than prescribed (or than usually consumed, in the case of illicit opioids); 3) combination with fentanyl, other high-potency opioids or other substances, such as alcohol or benzodiazepines.
The acute treatment of overdose is administration of naloxone. For many years naloxone, which required injection, could only be administered by health care providers, but the availability of an auto-injectable naloxone device and a naloxone spray now allow laypersons to administer naloxone to revert overdoses. 144 , 145 Nevertheless, increasing the availability of naloxone to ensure that it can reach those who need it on short notice remains a challenge, as there is considerable variability in the availability of naloxone by locality. 146 A 2019 analysis concluded that making naloxone available without prescription (“over the counter”) would substantially increase its availability. 147
In most cases a single dose of naloxone is sufficient to reverse the overdose. However, when high doses or high potency opioids such as fentanyl are used more than one dose is necessary to restore or maintain spontaneous breathing. 148 Furthermore, the fast pharmacokinetics of fentanyl can result in abrupt respiratory depression, which in some instances does not provide sufficient time to administer naloxone. It is believed that the duration of the respiratory depression from fentanyl or other analogues is longer than the duration of its reversal from naloxone. Moreover, thoracic rigidity associated with serotonergic effects from some of the opioids drugs might also interfere with overdose reversals. Naloxone can also fail to reverse overdoses in which opioids are combined with other CNS depressants, such as alcohol or benzodiazepines. First-responders to an overdose should stay with patients until emergency medical services arrive and transport them to an emergency room for a more systematic evaluation. Reversal of the overdose generally triggers an acute withdrawal syndrome, 111 which can lead patients to leave medical supervision to seek opioids for relieving withdrawal. Upon reversal of an overdose OUD patients should be linked to OUD treatment otherwise their risk of overdosing again is very high. The emergency room offers unique opportunities to start patients on MOUD if they can be linked with ongoing services. 149 Nevertheless, more research is needed to improve the management of patients immediately after reversal of an overdose, to retain them under care and to initiate effective MOUD.
Because of the urgency of the crisis, most efforts to date have emphasized treatment approaches. There is growing recognition, however, of the need to develop effective preventive interventions for OUD. 1 , 5 , 150 Initial preventive approaches in the US focused on improving prescription practices for opioid analgesics and increasing the availability of naloxone to prevent overdoses. The growing role of heroin, fentanyl and other synthetic opioids in the opioid crisis, 1 , 16 , 151 has required broadening the scope of preventive interventions. There are no evidence-based primary and secondary prevention for OUD for adults or for youth transitioning into adulthood, but several approaches appear as promising directions.
One approach would be to adapt existing interventions that have been successful for youth. Evidence-supported prevention interventions delivered in community or school settings have shown effectiveness at reducing substance use and other related problem behaviors, including middle-school interventions that have specifically demonstrated an impact on reducing prescription opioid misuse. 152 However, whether those interventions would work in adults is unknown. An obvious difficulty in adapting these interventions is the lack of a setting similar to school where adults could be easily reached.
A second direction would be the development of conceptual frameworks that articulate the relationship among risk factors for OUD to help guide which interventions might be most effective given the prevalence of the risk factors, how they relate to other relevant risk factors and how modifiable the risk factors are. These models could help examine how risk factors present at birth (e.g., family history of substance use disorders) or childhood (e.g., adverse childhood events) can increase the likelihood of risk factors in adolescence (e.g., early onset of psychiatric disorders, low educational achievement), which in turn increase the risk of OUD in adulthood. 153 Simulations could help identify which interventions might be most promising at the full population level or for subgroups with specific constellations of risk factors, as well as to identify potential unintended consequences of those interventions.
A third approach would be to increase the focus on populations at risk that can be accessed for screening and treatment. Those include, for example, individuals who receive regular health care and those in the justice system. Improved management of opioid prescriptions and of treatment of OUD for pregnant women is also a high priority, as it could benefit the mother and simultaneously decrease the risk of neonatal abstinence syndrome (NAS) in newborns by decreasing their in-utero exposure to opioids.
Even with wider use of non-opioid analgesics or use of non-pharmacological approaches, opioids will continue to be necessary for the treatment of many patients with severe pain. Efforts to prevent the development of opioid misuse and OUD can be started in clinical settings. This includes assessment of risk of OUD before opioids are prescribed, periodic assessment of the need for opioid use, and use of urine testing to rule out illicit use of other substances. There is evidence that prescribing lower doses/fewer pills in the emergency room/post-surgery is associated with lower rates of long-term use and possibly OUD. There is also a need to assess each patient for licit and illicit use of other substances, particularly benzodiazepines and alcohol, which can increase the lethality of opioids by potentiating their depressing respiratory effects. Individuals who misuse opioids or develop OUD should be treated by their primary physicians if they have the necessary expertise and support or otherwise be referred to an addiction specialist.
Prevention approaches should also consider supply approaches. The most common sources of diverted opioid analgesics are friends or relatives who were legitimately prescribed opioids. 154 As with any other medication, it is important to educate patients who receive legitimate prescriptions about the health hazards they create for others when they give them their medications. Similarly, it is important to educate patients about the health risks they incur when they take medications (including opioids) that were not prescribed to them. Use of Prescription Drug Monitoring Programs (PDMPs) can help reduce doctor shopping and overdoses, but their use to date is inconsistent. This may be due in part to the voluntary nature of the programs in many states, delays in updating the information, restrictions in data sharing across jurisdictions and the need to access them through a separate computer from the one used to access electronic health records. 150 Approaches that could help decreased the availability of heroin and fentanyl, traditionally in the purview of law enforcement primarily, would also advance prevention, but their development and implementation are challenging in the face of the evolving nature of the epidemic.
Research Gaps and Translational Opportunities
Basic science.
In addition to making progress in clinical and public health approaches, there is a need to advance fundamental science that can provide the foundations of more effective interventions for the current crisis and provide the basis to combat future ones. For example, there is a need to better understand the genes implicated in individual differences in vulnerability to the stages and sequelae along the OUD trajectory, including the development of tolerance, physical dependence, addiction, hyperalgesia, and respiratory depression for they could help identify new medication targets and in the future could serve as biomarkers to predict risk for side effects. Animal models could be used to identify the functions of the relevant genetic variants, epigenetic modifications, and gene networks.
Similarly, technological advances, such as those emerging from the BRAIN initiative could be leveraged to gain a deeper knowledge of endogenous opioids and to identify the consequences of exogenous opioid administration on the endogenous opioid systems and the cells and circuits they modulate across a trajectory of opioid use, ranging from acute administration, tolerance, physical dependence, addiction, and recovery to relapse. This could include studying profile changes in the transcriptome and methylome of opioid-synthesizing neurons, imaging the intracellular signaling cascades following opioid receptor activation (and how those cascades change across the trajectory of opioid use) and using quantitative brain-wide optical imaging combined with computational pipelines for cellular registration to provide unbiased documentation of the stereotyped distributions of cellular activity and cell-types engaged by opioids under different conditions. Post-mortem brains could be used to identify human-specific genes and their proteins, as has been done in the study of other psychiatric disorders. Use of post-mortem brains would enable the discovery and integration of genomic, epigenomic, proteomic, metabolomic, and non-coding RNA features across many brain regions and cell types that distinguish individuals with vulnerabilities to OUD and opioid-induced respiratory depression. This knowledge could be combined to validate findings in animal models (i.e., does the animal model recapitulate the human brain biology?) and to reverse translate from human to test a hypothesis in rodents.
A systematic investigation of developmental trajectories of the human brain is relevant for our understanding of the mechanism through which adverse child experiences as well as drug exposures during fetal development increase risk for drug use and other mental illnesses. To address this question, the HEALthy Brain and Child Development (HBCD) Study, which is part of the HEAL Initiative from the National Institutes of Health, 155 will establish a large cohort of pregnant women from regions of the country significantly affected by the opioid crisis, and follow them and their children for at least 10 years. The study will help better understand typical brain development, beginning in the prenatal period through early childhood, including variability in development and how it contributes to cognitive, behavioral, social, and emotional function.
New Medications
Despite the existence of effective medications for the treatment of OUD, current rates of engagement and retention in treatment suggest that new medications and devices are needed. The introduction of more acceptable and effective medications is crucial to improve the outcomes of individuals with OUD. In turn, improved outcomes could lead to changes in societal attitudes towards OUD, with broader acceptance of OUD as a treatable brain disorder and lower stigmatization of those suffering from it. Because the circuitry and neurotransmitters of the different phases of OUD only partially overlap, several complementary approaches may be necessary to treat the whole spectrum of severity from sporadic to chronic use, withdrawal and relapse.
To help speed the development of novel pharmacotherapies (i.e., excluding already known mechanisms) NIDA recently created a list of medication development priorities based on data from published literature and internal studies with the most direct relevance to OUD. 156 This list, which is not exclusive did not prioritize any of the 10 proposed mechanisms and included: 1) orexin-1 or 1/2 antagonists; 2) Kappa opioid antagonists; 3) GABA-B agonists; 4) Muscarinic M 5 antagonists; 5) AMPA antagonists; 6) nociception opioid peptide receptors/opioid receptor like agonists or antagonists; 7) mGluR2/3 agonists; 8) Ghrelin antagonists; 9) Dopamine D 3 partial agonists; and, 10) Cannabinoid CB-1 antagonists.
In addition to medications that target specific receptors, the development of allosteric modulators of those receptors is also a high priority. Negative allosteric modulators (NAMs) and positive allosteric modulators (PAMs) may provide more physiologically relevant effects compared with agonists and antagonists acting on the same receptor, which may ultimately result in improved clinical outcomes. 157 The development of opioids that selectively activate MOR G-protein intracellular pathways (“biased agonists”) may lead to medication with potent analgesic properties but with lower risk of respiratory depression and addictive liability, which would contribute to decrease the incidence and prevalence of OUD. 158 Other potential directions could include epigenetic, micro RNA and neuroimmune targets.
Better training of health professionals
Despite the severity of the dual crises of chronic pain and OUD, very few medical schools offer adequate training in pain management, and still fewer offer even one course in addiction. Furthermore, surprisingly little is known about how best to train physicians and other health professionals on the management of OUD including the use of medications. 159 There is also evidence that many individuals trained to provide MOUD do not provide that treatment. Some national organizations offer a combination of didactics, supervision and mentoring to provide training beyond residency, 159 and the new subspecialty of addiction medicine is likely to further increase the availability of well-trained professionals that can treat individuals with OUD. However, broader changes, including combating stigma, enhancing institutional support and increasing reimbursement rates may be necessary to increase rates of treatment among those trained to provide it. Increasing the number of addiction treatment and prevention programs, particularly in low-resource communities is also essential.
The opioid crisis is a complex, evolving phenomenon. It involves neurobiological vulnerabilities and social determinants of health. Successfully addressing the crisis will require advances in basic science, development of more effective treatments, and public health approaches to implement current and emerging knowledge. We hope that this review will alert clinicians and researchers about the current approaches to the crisis and suggest opportunities for future research and for practice improvement. The advances achieved in addressing the current crisis should also serve to expand the science and treatment of other substance use disorders.
Acknowledgments:
The views and opinions expressed in this report are those of the authors and should not be construed to represent the views of any of the sponsoring organizations, agencies or the US government.
Conflict of Interest : The authors have no competing financial interests in relation to the work described in this manuscript.

IMAGES
COMMENTS
Given these issues, this paper distinguishes between supply reduction, management of market harms, treatment, other interventions with dependent users, and prevention. ... As a result, foundations have played a major role in drug policy research. The Robert Wood Johnson Foundation remains the largest source of nongovernment support for ...
Gstrein (2018), in a scoping review of social construction and ideation research in drug policy, defines drug policy as "government policy that addresses issues arising from the use of illicit drugs, with a particular focus on health outcomes" (Gstrein, 2018, p. 76). We use "drug policy research" here to refer to this domain but also ...
The International Journal of Drug Policy provides a forum for the dissemination of current research, reviews, debate, and critical analysis on drug use and drug policy in a global context. It seeks to publish material on the social, political, legal, and health contexts of psychoactive substance use, both licit and illicit.The journal is particularly concerned to explore the effects of drug ...
Julie Netherland is the director of the Office of Academic Engagement for the Drug Policy Alliance. In that role, she advances drug policy reform by supporting scholars in doing advocacy, convening experts from a range of disciplines to inform the field, and strengthening DPA's use of research and scholarship in developing and advancing its policy positions.
Expanding access to the overdose reversal drug naloxone, mandating prescriber enrollment and use of prescription monitoring programs, expanding access to pharmacotherapy (e.g., buprenorphine, naltrexone) and psychosocial treatment for individuals with opioid use disorder, and augmenting syringe exchange programs have also attracted significant policy attention and are therefore worthy of ...
Comparative drug policy analysis (CPA) is alive and well, and the emergence of robust alternatives to strict prohibition provides exciting research opportunities. As a multidisciplinary practice, however, CPA faces several methodological challenges. This commentary builds on a recent review of CPA by Ritter and colleagues to argue that the ...
Editorial. This issue of the International Journal on Drug Policy highlights a wide breadth of topics related to the worldwide production in and trade of illicit drugs. From a methodological standpoint, this collection of articles covers two key thematic areas: the qualitative characterization of aspects of the drug trade and/or drug policy in a given region, and the measurement of drug ...
Background and aims. Policy responses to illegal drugs are in a state of flux across the globe, with growing momentum towards alternatives to strict prohibitive models, from depenalisation to legal regulation (Stevens et al., 2019).Much research attention in this area has been given to those countries at the forefront of such policy reforms or is dominated by experiences of 'Western ...
This paper provides a nonpartisan primer on drug use and drug policy in the United States. It aims to bring those new to drug policy up to speed and provide ideas to researchers and potential research funders about how they could make strong contributions to the field.
Abstract. Drug policies play a role in protecting the public's health and reducing drug-related crimes at the local, national, and international levels. This chapter mainly focuses on key drug control treaties and policies, providing a brief historical context on how some of the policies were established. The goal is to present the reader ...
Research Handbook on Int ernational Drug P olicy. Blaine Stothar d. Drugs and Alcohol T oday, GB. [email protected]. This volume is part of the response to the 2016 UN Gener al Assembly ...
The most recent estimate puts the economic cost of illegal drug use under current policies in the United States at $193 billion in 2007 (National Drug Intelligence Center, 2011).3 Costs were classified into three categories: crime ($61 bil-lion), health ($11 billion), and productivity ($120 billion).
Background. The United States (U.S.) continues to experience an epidemic of drug-related harm. Nearly 107,000 people in the U.S. died of a drug overdose in 2021, the highest number ever recorded (National Center for Health Statistics, 2022).Rates of injection-related endocarditis and soft tissue infections are also at or near all-time highs (Barocas et al., 2021; Schranz, Fleischauer, Chu, Wu ...
This review summarizes extant literature on the effect of drug policy liberalization on crime, traffic safety, law enforcement, and racial disparities. ... A Review of the Literature (December 5, 2022). Ohio State Legal Studies Research Paper No. 746, Drug Enforcement and Policy Center, December 2022, Available at SSRN: https://ssrn.com ...
Key Points. Question Are US state drug policies associated with variation in opioid misuse, opioid use disorder, and drug overdose mortality?. Findings In this cross-sectional study of state-level drug overdose mortality data and claims data from 23 million commercially insured patients in the US between 2007 and 2018, state policies were associated with a reduction in known indicators of ...
COMMUNITY DRIVEN DRUG POLICY RESEARCH FEBRUARY 2023 In Spring 2022, Drug Policy Alliance, Urban Survivors Union, and the Network of Drug Researchers with Lived Experience co-hosted a four-part virtual series "Beyond participatory-based research: Innovations in community driven drug policy research." The sessions were designed to encourage
ONDCP 2021 The Biden-Harris Administration's Statement of Drug Policy Priorities for Year One . 5 • Support research on the clinical effectiveness of emerging harm reduction practices in real ...
This paper places America's "war on drugs" in perspective in order to develop a new metaphor for control of drug misuse. A brief and focused history of America's experience with substance use and substance use policy over the past several hundred years provides background and a framework to compare the current Pharmacological Revolution with America's Nineteenth Century Industrial Revolution.
The RAND Drug Policy Research Center has published an Occasional Paper offering a concise, accessible, objective view of where the United States has been, now stands, and might go in the future in its long "war on drugs.". The authors assess the success of drug policies to date and review possible reasons why they have not been more successful.
We used a blended values approach combining Moral Foundations Theory (Haidt and Joseph, 2004; Haidt and Graham, 2007) and MacCoun and Reuter's (2001) four philosophical positions that underpin the drug policy. This paper asks, what values do people who use drugs hold surrounding drug use and drug policy, and what factors predict these values?
Prohibition makes some drug use and drug selling a crime by statute, but licit drugs like alcohol are also associated with criminality in myriad ways. Within a prohibition regime, it is difficult but important to distinguish a drug's "intrinsic" psychopharmacological harms from the harms created or exacerbated by prohibition and its enforcement.
The top ten most cited papers in policy documents are dominated by economics research; the number one most referenced study has around 1,300 citations. When economics studies are excluded, a 1997 ...
Call for Papers: Brain Targeted Drug Delivery. This Special Issue will focus on the latest research in brain targeted drug delivery. Submit your manuscript by June 30, 2024. The prevalence of central nervous diseases poses significant challenges to society, particularly with the global aging population.
A lcohol and other drug policy research has emerged as a public health interest over the past 75 years, encouraged and supported by many research studies that appeared in the Journal of Studies on Alcohol and Drugs (JSAD) and related journals. A critical summary of what is currently known, an examination of the implications of current alcohol and other drug policies, and promising directions ...
Premature deaths related to opioids doubled between 2019 and 2021 across Canada, with more than 1 in 4 deaths among young adults aged 20-39 years attributable to opioids, new research suggests.
But while the story of Makena's rise and fall may be well known, one aspect of the drug's legacy has gone untold. A widely cited study that supported Makena's approval mixed up the names of ...
Pew Research Center conducted this analysis to provide a snapshot of partisan divides in K-12 education in the run-up to the 2024 election. The analysis is based on data from various Center surveys and analyses conducted from 2021 to 2023, as well as survey data from Education Next, a research journal about education policy.
Abstract. The current opioid epidemic is one of the most severe public health crisis in US history. Responding to it has been difficult due to its rapidly changing nature and the severity of its associated outcomes. This review examines the origin and evolution of the crisis, the pharmacological properties of opioids, the neurobiology of opioid ...