Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals

Environmental health articles from across Nature Portfolio

Extreme weather threatens informal settlements
Residents of informal settlements suffer from extreme weather due to their precarious living environment. Now, findings show that extreme weather event thresholds do not fully capture the negative impacts experienced by women in Nairobi, Kenya.
- Lauren Broyles
Latest Research and Reviews
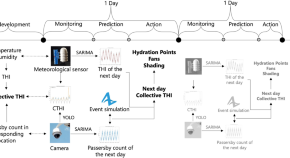
Assessing and forecasting collective urban heat exposure with smart city digital twins
- Dimitris Mavrokapnidis
- John E. Taylor
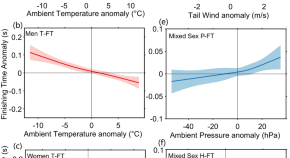
Warming climate is helping human beings run faster, jump higher and throw farther through less dense air
- Shixin Wang
- Toshio Yamagata
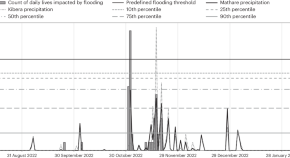
Extreme weather should be defined according to impacts on climate-vulnerable communities
Defining thresholds for extreme weather events is important for adaptation but often ignores impacts on climate-vulnerable communities. This research finds current practices do not capture experiences of women in informal settlements and self-reported impact data could help to address the issue.
- Samantha C. Winter
- Mark R. Winter
- Susan S. Witte
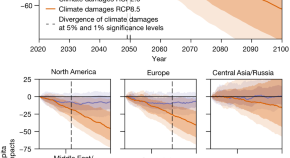
The economic commitment of climate change
Analysis of projected sub-national damages from temperature and precipitation show an income reduction of 19% of the world economy within the next 26 years independent of future emission choices.
- Maximilian Kotz
- Anders Levermann
- Leonie Wenz
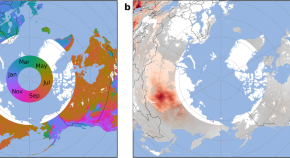
Large transboundary health impact of Arctic wildfire smoke
Large Arctic wildfires have caused around 21,000 excess deaths each year between 2001 and 2020, of which roughly 8000 occurred in countries outside the Arctic Council, suggest Earth model simulations.
- Steve R. Arnold
- Luke Conibear
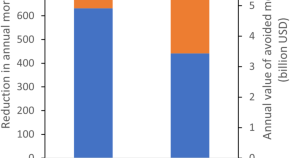
Current inequality and future potential of US urban tree cover for reducing heat-related health impacts
- Robert I. McDonald
- Tanushree Biswas
- Joseph E. Fargione
News and Comment

Ocean salinity
- Lingxiao Yan

Incarcerated people in the United States face deadly and growing heat exposure risk
Carceral facilities have experienced an increase in days with dangerous heat conditions over the past 40 years, particularly at state facilities in the southern and southwestern United States. Indoor temperature regulation is necessary to protect the health of vulnerable incarcerated populations.

China’s response to extreme weather events must be long term

Time to recover
Media attention to the disastrous consequences of this summer’s wildfires has been at a record high. Now the world should wake up to the urgent need to restore burnt sites.

Drought and electricity
Quick links.
- Explore articles by subject
- Guide to authors
- Editorial policies
- Open access
- Published: 23 December 2022
Advancing environmental health sciences through implementation science
- Gila Neta 1 ,
- Lindsey Martin 2 &
- Gwen Collman 3
Environmental Health volume 21 , Article number: 136 ( 2022 ) Cite this article
3729 Accesses
1 Citations
1 Altmetric
Metrics details
Environmental health sciences have identified and characterized a range of environmental exposures and their associated risk for disease, as well as informed the development of interventions, including recommendations, guidelines, and policies for mitigating exposure. However, these interventions only serve to mitigate exposures and prevent disease if they are effectively disseminated, adopted, implemented, and sustained.
Numerous studies have documented the enormous time lag between research and practice, noting that dissemination and implementation are not passive processes but rely on active and intentional strategies. Implementation science seeks to build the knowledge base for understanding strategies to effectively disseminate and implement evidence and evidence-based interventions, and thus, bridge the research-to-practice gap.
Environmental health researchers are well positioned to advance health promotion and disease prevention by incorporating implementation science into their work. This article describes the rationale for and key components of implementation science and articulates opportunities to build upon existing efforts to advance environmental health supported by the National Institute of Environmental Health Sciences and National Institutes of Health broadly.
Peer Review reports
The National Institute of Environmental Health Sciences (NIEHS) seeks to understand “how the environment affects people in order to promote healthier lives.” NIEHS has invested substantially in environmental health research which has enumerated scores of chemicals that may cause disease, elucidated molecular mechanisms for disease initiation and progression, and informed the development of interventions, including recommendations, guidelines, and policies for mitigating exposure. However, these evidence-based interventions, recommendations, guidelines, and policies (hereafter referred to collectively as “interventions”) are only effective at mitigating exposures and preventing disease if they are effectively disseminated, adopted, implemented, and sustained.
Numerous studies have documented the enormous time lag between clinical research and practice. While in healthcare this estimate has hovered around 17 years [ 1 , 2 ], the time lag can be substantially longer for environmental health evidence to result in changes to policy and practice. For example, we continue to see high rates of smoking despite the 1964 Surgeon General Report and effective tobacco control interventions including those which reduce exposure to secondhand smoke in the workplace. Air pollution is another example. Despite significant documentation of mortality associated with air pollution as early as the 1950s [ 3 ], the Clean Air Act wasn’t established until 1970 and air pollution continues to plague many U.S. cities. Even longer lags have been seen with arsenic, which we’ve known is carcinogenic for over a century, yet arsenic levels in the U.S. population continue to be above the U.S. Federal Government’s national health objectives goal as outlined in Healthy People 2020. Other examples include lead and mercury, for which it took decades for the evidence on their health effects to translate to global policy action [ 4 ], and yet millions of children continue to be exposed to high levels of these toxins.
Increasingly researchers have come to appreciate that dissemination and implementation of evidence-based interventions are not passive processes but rely on active and intentional strategies that should be informed by theories, stakeholders, and evidence. Implementation science seeks to build the knowledge base for understanding strategies to effectively disseminate, implement, and sustain evidence and evidence-based interventions, and thus, bridge the research-to-practice gap [ 5 , 6 ]. Given the complex influences and global nature of environmental exposures, environmental health researchers are well positioned to advance disease prevention by integrating implementation science into their work.
In this article, we describe the key components of implementation science and articulate ways that environmental health researchers can build upon existing efforts to advance environmental health through implementation science. NIEHS emphasizes the importance of engaging with affected communities, practitioners, policymakers, and other partners across multiple sectors, and the need to develop and equitably implement effective, evidence-based environmental health interventions to prevent and mitigate harmful exposures and reduce environmental health disparities. Table 1 provides a roadmap for environmental health scientists to consider how implementation science could advance their work in alignment with NIEHS goals. Further, we provide an example of a network of environmental health researchers and implementation scientists collaborating to advance the implementation of clean cookstove interventions to reduce household air pollution and improve population health. We hope this example may serve to drive future research directions and collaborations.
What is implementation science?
Implementation science is the study of methods to promote the adoption and integration of evidence and evidence-based practices, interventions and policies into routine healthcare and community settings to improve health [ 5 , 6 ]. The National Institutes of Health (NIH) issued funding announcements in 2005 to support research on understanding barriers to dissemination and implementation and develop and test strategies to overcome those barriers.
For the purposes of the funding announcements, the NIH makes a distinction between dissemination research and implementation research. Dissemination research is defined as the study of the “targeted distribution of information and intervention materials to a specific public health, clinical practice, or policy audience” [ 5 ]. The intent is to understand how, when, by whom, and under what circumstances evidence and the associated evidence-based interventions can be most effectively communicated and integrated into practice. It accounts for all the stages of dissemination, including the creation, packaging, transmission, and reception of the knowledge and associated interventions. These are steps we often take for granted but that can impact the effectiveness of our dissemination efforts.
Implementation research has been defined as the study of the use of strategies to adopt and integrate evidence-based health interventions into clinical and community settings to improve individual outcomes and benefit population health [ 5 ]. While clinical trials test the effectiveness of interventions to improve health outcomes, implementation research focuses on understanding how those interventions can best be delivered to ensure they have the intended impact on health. Implementation studies develop and test strategies to ensure effective implementation. Rather than focusing on individual health outcomes, implementation studies focus on proximal outcome measures that demonstrate implementation success, such as measures of acceptability, adoption, appropriateness, costs, feasibility, fidelity, penetration, and sustainability [ 12 ]. The goal is to identify a strategy or set of strategies that will maximize effective adoption, implementation and sustainability of an evidence-based intervention, and thus, ultimately improve population health. Additional key components of implementation science are described in the following paragraphs with a guiding example from environmental health on the adoption and use of clean cookstoves to reduce household air pollution. This example comes from the Clean Cooking Implementation Science Network, which was established and funded by the National Institutes of Health in partnership with the Environmental Protection Agency (EPA), Centers for Disease Control and Prevention (CDC), U.S. Agency for International Development (USAID), and the Clean Cooking Alliance. The network consists of environmental health researchers and implementation scientists studying strategies to promote the adoption, use, and scale-up of clean cooking technologies around the globe.
Theories, frameworks, and models
The field of implementation science hinges on theories, frameworks, and models to inform dissemination and implementation processes and help determine the most effective strategies to overcome barriers to dissemination and implementation. These theories, frameworks, and models (hereafter referred to collectively as frameworks) typically recognize the importance of context as well as the multiple levels of influence on dissemination and implementation processes. More than 60 frameworks are used in the field [ 13 ] for a variety of purposes including to inform processes and determinants of implementation, as well as to evaluate implementation success [ 14 ].
Some of the most commonly used frameworks in NIH-funded studies include Everett Rogers’ Diffusion of Innovations [ 15 ] and the Consolidated Framework for Implementation Research [ 16 ], both of which posit that the decision to adopt and successfully implement an intervention is influenced not only by the characteristics of the intervention itself but also by the setting or context in which that intervention is implemented. Further, these frameworks recognize the multiple levels of influence in a given context, from the organizational or community setting to the broader municipality, state, or nation. For example, the decision to adopt and implement a clean cookstove, such as a liquid purified gas (LPG) stove, in a household will be influenced not only by whether that cookstove is relatively simple to use, but also whether the household member(s) can access the gas required to power the stove or have access to technical assistance to use or repair the stove. The decision will also be based on cultural and behavioral factors in the home and community, which often drive adoption and acceptance. These frameworks guide our studies by informing our hypotheses about how interventions work, why they work, and what might impede or support the ability to implement them, which can inform a priori strategies to facilitate implementation.
The selection of frameworks will depend on the research questions and study objectives. In the clean cookstoves example, researchers used the RE-AIM Framework to understand the Reach, Effectiveness, Adoption, Implementation, and Maintenance of clean cookstoves across 11 low- and middle-income countries. This enabled them to identify key gaps in implementation and highlight areas for future efforts.
One important feature of implementation science frameworks is their attentiveness to multi-level factors that influence implementation, including characteristics of 1) the individuals delivering the intervention, 2) the organization in which it is delivered, and 3) the community in which those individuals and organization exist. This is critical for environmental health studies that seek to eliminate health disparities. Understanding contextual factors that influence equitable implementation can help us design and deliver interventions that will mitigate and not exacerbate existing environmental health disparities disproportionately affecting communities of color.
Implementation strategies
Implementation strategies are the focus of implementation science. They are defined as the “methods or techniques used to enhance the adoption, implementation and sustainability of an evidence-based program or practice” [ 17 ]. Most implementation studies seek to develop and test strategies to improve uptake and use of effective interventions. The purpose of these strategies is to improve the aforementioned proximal outcomes, such as the feasibility, adoption, or sustainability of an intervention [ 12 ]. Over 70 strategies have been classified into broad categories [ 17 , 18 ], including evaluative and iterative strategies, interactive assistance, adapting and tailoring to context, developing stakeholder relationships, educating and training, engaging consumers, financial strategies, and strategies to change infrastructure. The selection of a strategy or set of strategies will depend on the implementation barriers being addressed and the implementers being targeted. For example, in efforts to overcome financial barriers for households to use LPG stoves, investigators tested conditional cash transfers as a financial incentive for adoption and use. In seeking to influence policymakers at the municipal, state, or national level for LPG stove distribution, studies might test strategies to develop stakeholder relationships and build buy in. Examples of these types of strategies include identifying champions, informing local opinion leaders, or building coalitions. If a major barrier is the ability to properly use and maintain the stove, studies might focus on strategies to provide interactive assistance, such as facilitation or technical assistance. Ultimately, implementation science seeks to understand which set of strategies work best in a particular context to improve implementation outcomes.
Study designs
Implementation science uses a variety of study designs typically used in other fields, including observational and experimental designs. Study designs that may be less familiar to environmental health researchers but that are commonly used in implementation science include quasi-experimental and effectiveness-implementation hybrid designs, as well as mixed methods designs [ 19 ]. The following paragraphs will review some of these designs in more detail and provide guiding examples.
Experimental designs
One popular experimental design is the stepped wedge design [ 20 ], which is a type of cluster randomized controlled trial (RCT). In the stepped wedge design an intervention is rolled out in multiple places (or clusters) sequentially rather than simultaneously, and comparisons can be made within and between clusters. The advantage of this design is that it is more feasible to focus resources in one place at a time. This can be particularly useful for a clean cookstove intervention trial that seeks to test strategies across multiple community settings but may not have the resources to implement the intervention across all settings at one time.
Quasi-experimental designs
While experimental designs test an intervention through randomization, quasi-experimental designs were developed to test interventions when randomization is not possible. This is often the case when pursuing questions related to mitigation or reduction of exposures to environmental pollutants. These include designs such as interrupted time series [ 21 ], regression discontinuity [ 22 ], and non-equivalent control group [ 23 ]. These designs are particularly useful in environmental health where it may be unethical to withhold an intervention that can prevent or reduce exposure harms. For example, in an interrupted time series (ITS) design everyone receives the intervention and multiple assessments are taken prior to and following the introduction of the intervention. An ITS design could be an appropriate design to study the impact and rollout of a lead abatement program which would be implemented broadly, including all eligible households in a community rather than withholding abatement from some participants. In selecting a study design, careful attention should be paid to the underlying assumptions, advantages, and disadvantages.
Hybrid designs
Effectiveness-implementation hybrid designs are another particularly useful design for environmental health researchers developing interventions. These designs have a dual focus a priori on assessing intervention effectiveness and implementation [ 24 ]. The overall goal is to accelerate the transition from effectiveness studies to implementation studies. There are three types of hybrid designs that vary by the emphasis placed on the aims of the study. At one end of the spectrum, Type 1 designs are primarily focused on studying intervention effectiveness while secondarily collecting information about implementation processes including barriers to implementation. For example, in developing an early warning system for disaster preparedness, researchers can test the effectiveness of the system in its ability to predict and monitor conditions allowing for communities to prepare for and adapt to disasters, while also studying how such a system would be implemented in a particular context (e.g., how would data be accessed, how would the system be run and maintained, how would output reach the affected communities, who would be ensuring these steps take place, etc.) At the other end of the spectrum, Type 3 designs are primarily focused on testing implementation strategies while secondarily collecting information on health outcomes. For example, researchers developed and tested an effective household intervention that increased the appropriate and exclusive use of clean cooking technologies through education, incentivization, and environmental restructuring [ 25 , 26 ]. In a subsequent type 3 hybrid design, researchers could develop and test strategies that will support the ability to scale up the intervention across a range of settings while also assessing the intervention’s effectiveness to increase use of clean cookstoves, for example, through air monitoring to measure reductions in indoor air pollution. Type 2 designs fall in between Type 1 and Type 3 designs, with a dual primary focus of testing effectiveness and testing an implementation strategy. The type of hybrid design selected is dependent on the degree to which effectiveness of an intervention is already well characterized for a particular context. These designs offer an opportunity for environmental health researchers who are focusing on prevention to not only test the effectiveness of their interventions but also understand implementation processes required to deliver the intervention in a variety of settings. Understanding these processes and identifying the appropriate people to implement an intervention are the first steps in understanding factors that influence successful implementation, enabling subsequent implementation studies on strategies to increase the likelihood that these interventions will be effectively delivered in practice.
Mixed methods
Mixed methods designs are the collection and integration of qualitative and quantitative data to help understand processes and context. Where quantitative data can provide a measure of effect, qualitative data can reveal the reasons why and how things work or don’t work. For example, in a clean cookstove study that tests strategies to enhance LPG stove adoption and use, investigators may measure uptake and use by measuring particulate matter levels in household ambient air and may also use direct observation and/or conduct qualitative interviews and focus groups to understand how and why households used or did not use the LPG stoves. Understanding why a strategy to enhance implementation was effective or not allows for an iterative process to modify or adapt an intervention to fit a specific context, or to further refine a set of strategies to enhance implementation.
For environmental health researchers who have historically focused on documenting risks and understanding their causes, implementation science can further expedite efforts that shift the scientific focus towards better understanding how to promote prevention. Through focusing on the how , we can advance disease prevention and improve population health by understanding the most effective strategies that enable us to effectively communicate, integrate, and sustain interventions (including recommendations, guidelines, and policies) in practice. The following section enumerates ways that environmental health researchers can incorporate implementation science into their work at various stages of the translational research pathway, to bridge the gap from research to practice.
Integrating implementation science into environmental health sciences
Many have articulated the translational research pathway from basic discovery to human application to intervention development to implementation and evaluation [ 27 , 28 , 29 ]. However, these earlier models were developed primarily for medical research. More recently, the NIEHS developed the Translational Research Framework ( https://www.niehs.nih.gov/research/programs/translational/framework-details/index.cfm ) which serves as a guide for environmental health scientists to envision how their studies can move along this pathway. Importantly, this framework highlights the development of evidence-based interventions and implementation science playing key roles in this iterative (and not always linear) process [ 30 ]. Figure 1 illustrates the translational research pathway in the context of environmental health research, elaborating on the role of implementation science.
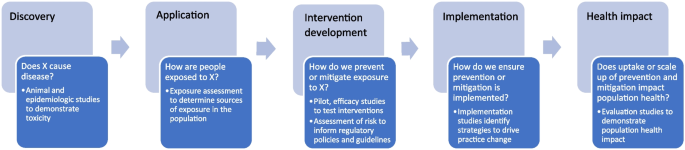
The Translational Pathway of Environmental Health Research from Discovery to Population Health Impact
Much of environmental health research has focused on the first stages of this pathway, from basic discovery to application to intervention development, namely, informing recommendations, guidelines, and regulatory policies, as well as health interventions. For example, environmental health researchers have made substantial progress in basic discovery by identifying and characterizing chemical toxicity through in vitro, in silico, animal, and epidemiologic studies. These discoveries have led to research that focuses on the underlying mechanisms by which these exposures impact biology and pathophysiology and research on understanding how people are exposed to these chemicals across the lifespan in multiple environments. Through exposure assessments, environmental health researchers have elucidated the relevant chemical species and main sources of exposure. This application then leads to science that would inform the development of policies, recommendation, and guidelines, such as risk assessments that would reduce exposures to a safe level in a population. Further, understanding the relevant sources of exposure can inform prevention or mitigation efforts. Thus, interventions can be developed that can prevent or mitigate human exposure to these relevant sources. For example, to reduce exposure to household air pollution, a variety of clean cooking technologies have been developed for households with unreliable access to electricity or gas. However, these clean cookstove technologies are not necessarily being adopted nor used appropriately by households [ 31 ]. Once interventions are developed and tested, implementation studies can inform the most effective strategies to ensure their adoption and appropriate use, and ultimately, how best to scale up these interventions to all populations who can benefit. In the example of cookstoves, the Clean Cooking Implementation Science Network [ 31 ] has studied a range of strategies to promote adoption and appropriate use, including strategies to increase awareness [ 32 ] and financial strategies to incentivize replacement of polluting stoves [ 33 ]. Finally, evaluation studies can assess the health impact of these implementation and scale up efforts [ 34 ].
Implementation science has evolved and developed methods not only to focus on the later stages of the translational research pathway, but also to inform intervention development studies. In studying human application and intervention development, researchers should consider who will be delivering the intervention and how it fits with the ultimate consumer population, and build in tests of training, support, and adherence. For example, effectiveness-implementation hybrid designs, whereby researchers can dually study intervention effectiveness as well as implementation [ 24 ], as described above in the examples of early warning systems and clean cookstoves, can help to speed up the translational research process by integrating implementation studies and intervention development studies. By designing interventions for dissemination and implementation, researchers can increase the likelihood that the outputs of their research will be implemented in practice. For example, the Household Air Pollution Intervention Network Trial is a multi-country trial testing the effectiveness of clean cooking technologies on improving health outcomes [ 35 ] while also studying approaches to improve use of the clean cookstoves [ 36 ].
We have a tremendous opportunity to use implementation science to understand how environmental health evidence is being disseminated, implemented, and sustained, and how best to address the gaps in those processes. Institutes, centers, and offices across the NIH recognize the importance of advancing our understanding of the most effective strategies to integrate evidence-based interventions within community, clinical, and public health systems. Thus, they have issued a set of funding announcements in Dissemination and Implementation Research in Health (PAR-22-105, PAR-22-106, PAR-22-109), which seek to build the knowledge base on how to effectively disseminate, implement, sustain, and scale evidence-based interventions, as described in the previous section. These institutes and centers include several focused on environmental exposures, including NIEHS, National Cancer Institute (NCI), Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institute of Mental Health, National Heart, Lung, and Blood Institute, and Fogarty International Center. At NIEHS, the integration of implementation science is developing throughout the portfolio, including a new initiative on children’s health that supports collaborations between environmental health scientists and implementation scientists ( https://grants.nih.gov/grants/guide/rfa-files/rfa-es-20-001.html ). NIEHS supported scientists are also involved in the NIH-wide RADxUP program which is conducting implementation science related to the uptake of COVID19 testing in communities experiencing health disparities and environmental injustice.
In addition to funding opportunities, NIH supports a range of training opportunities. For example, the NCI hosts the Training Institute in Dissemination and Implementation Research in Cancer (TIDIRC), which provides thorough instruction in conducting dissemination and implementation studies and is now available in open access format ( https://cancercontrol.cancer.gov/IS/training-education/tidirc/openaccess.html ). Additional implementation science resources for environmental health researchers can be found at the NIEHS website ( https://www.niehs.nih.gov/research/supported/translational/implementation/index.cfm ) and the NCI Implementation Science Team website ( https://cancercontrol.cancer.gov/IS/ ).
Conclusions
Environmental health researchers can advance disease prevention not only by informing the development of effective interventions, regulatory policies, and guidelines, but also by ensuring that those interventions, policies, and guidelines are effectively adopted, implemented and sustained. They can do this by incorporating implementation science into their work across the translational research pathway. Namely, environmental health researchers can design interventions that better fit the context in which they are meant to be applied. Further, they can study implementation processes and inform implementation strategies to most effectively implement those interventions. A variety of methods and study designs in implementation science have been described in this paper that can guide environmental health researchers to conduct implementation studies. By fully integrating the concepts, methods, and findings of implementation science into the environmental health research agenda, we can envision a more comprehensive flow from research to practice that maximizes the use of scientific discovery and supports the NIEHS mission of discovering how the environment affects people in order to promote healthier lives.
Balas EA, Boren SA. Managing clinical knowledge for health care improvement. Yearb Med Inform. 2000;1:65–70.
Google Scholar
Morris ZS, Wooding S, Grant J. The answer is 17 years, what is the question: understanding time lags in translational research. J R Soc Med. 2011;104(12):510–20.
Article Google Scholar
Brunekreef B, Holgate ST. Air pollution and health. Lancet. 2002;360(9341):1233–42.
Article CAS Google Scholar
UN. Global sustainable development report: United Nations; 2015.
NIH. Dissemination and Implementation Research in Health Program Announcement (R01 Clinical Trial Optional) 2022 [Available from: https://grants.nih.gov/grants/guide/pa-files/PAR-22-105.html .]
Eccles MP, Mittman BS. Welcome to implementation science. Implement Sci. 2006;1(1):1.
Brownson RC, Kumanyika SK, Kreuter MW, Haire-Joshu D. Implementation science should give higher priority to health equity. Implement Sci. 2021;16(1):28.
Kumar P, Dover RE, Díaz-Valdés Iriarte A, Rao S, Garakani R, Hadingham S, et al. Affordability, accessibility, and awareness in the adoption of liquefied petroleum gas: a case-control study in rural India. Sustainability. 2020;12(11):4790.
Ronzi S, Puzzolo E, Hyseni L, Higgerson J, Stanistreet D, Hugo MNB, et al. Using photovoice methods as a community-based participatory research tool to advance uptake of clean cooking and improve health: the LPG adoption in Cameroon evaluation studies. Soc Sci Med. 2019;228:30–40.
Johnson K, Gustafson D, Ewigman B, Provost L, Roper R. Using rapid-cycle research to reach goals: awareness, assessment, adaptation, acceleration in: quality AfHRa, editor. Bethesda, MD. 2015;2015.
Metz A, Woo B, Loper A. Equitable implementation at work. Stanf Soc Innov Rev. 2021;19(3):A29–31.
Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Admin Pol Ment Health. 2011;38(2):65–76.
Tabak RG, Khoong EC, Chambers DA, Brownson RC. Bridging research and practice: models for dissemination and implementation research. Am J Prev Med. 2012;43(3):337–50.
Nilsen P. Making sense of implementation theories, models and frameworks. Implement Sci. 2015;10:53.
Rogers EM. Diffusion of innovations, vol. xxi. 5th ed. New York: Free Press; 2003. p. 551.
Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50.
Powell BJ, Waltz TJ, Chinman MJ, Damschroder LJ, Smith JL, Matthieu MM, et al. A refined compilation of implementation strategies: results from the expert recommendations for implementing change (ERIC) project. Implement Sci. 2015;10:21.
Waltz TJ, Powell BJ, Matthieu MM, Damschroder LJ, Chinman MJ, Smith JL, et al. Use of concept mapping to characterize relationships among implementation strategies and assess their feasibility and importance: results from the expert recommendations for implementing change (ERIC) study. Implement Sci. 2015;10:109.
Brown CH, Curran G, Palinkas LA, Aarons GA, Wells KB, Jones L, et al. An overview of research and evaluation designs for dissemination and implementation. Annu Rev Public Health. 2017;38:1–22.
Hemming K, Haines TP, Chilton PJ, Girling AJ, Lilford RJ. The stepped wedge cluster randomised trial: rationale, design, analysis, and reporting. BMJ. 2015;350:h391.
Kontopantelis E, Doran T, Springate DA, Buchan I, Reeves D. Regression based quasi-experimental approach when randomisation is not an option: interrupted time series analysis. BMJ . 2015;350:h2750.
Venkataramani AS, Bor J, Jena AB. Regression discontinuity designs in healthcare research. BMJ . 2016;352:i1216.
Krishnan P. A review of the non-equivalent control group post-test-only design. Nurse Res. 2019;26(2):37–40.
Curran GM, Bauer M, Mittman B, Pyne JM, Stetler C. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care. 2012;50(3):217–26.
Thompson LM, Diaz-Artiga A, Weinstein JR, Handley MA. Designing a behavioral intervention using the COM-B model and the theoretical domains framework to promote gas stove use in rural Guatemala: a formative research study. BMC Public Health. 2018;18(1):253.
Williams KN, Thompson LM, Sakas Z, Hengstermann M, Quinn A, Díaz-Artiga A, et al. Designing a comprehensive behaviour change intervention to promote and monitor exclusive use of liquefied petroleum gas stoves for the Household Air Pollution Intervention Network (HAPIN) trial. BMJ Open. 2020;10(9):e037761.
Zerhouni EA. Clinical research at a crossroads: the NIH roadmap. J Investig Med. 2006;54(4):171–3.
Khoury MJ, Gwinn M, Ioannidis JP. The emergence of translational epidemiology: from scientific discovery to population health impact. Am J Epidemiol. 2010;172(5):517–24.
Fort DG, Herr TM, Shaw PL, Gutzman KE, Starren JB. Mapping the evolving definitions of translational research. J Clin Transl Sci. 2017;1(1):60–6.
Pettibone KG, Balshaw DM, Dilworth C, Drew CH, Hall JE, Heacock M, et al. Expanding the concept of translational research: making a place for environmental health sciences. Environ Health Perspect. 2018;126(7):074501.
Rosenthal J, Balakrishnan K, Bruce N, Chambers D, Graham J, Jack D, et al. Implementation science to accelerate clean cooking for public health. Environ Health Perspect. 2017;125(1):A3–a7.
Kumar P, Dhand A, Tabak RG, Brownson RC, Yadama GN. Adoption and sustained use of cleaner cooking fuels in rural India: a case control study protocol to understand household, network, and organizational drivers. Arch Public Health. 2017;75:70.
Harrell BS, Pillarisetti A, Roy S, Ghorpade M, Patil R, Dhongade A, et al. Incentivizing elimination of biomass cooking fuels with a reversible commitment and a spare LPG cylinder. Environ Sci Technol. 2020;54(23):15313–9.
Quinn AK, Bruce N, Puzzolo E, Dickinson K, Sturke R, Jack DW, et al. An analysis of efforts to scale up clean household energy for cooking around the world. Energy for Sustainable Dev. 2018;46:1–10.
Clasen T, Checkley W, Peel JL, Balakrishnan K, McCracken JP, Rosa G, et al. Design and rationale of the HAPIN study: a multicountry randomized controlled trial to assess the effect of liquefied petroleum gas stove and continuous fuel distribution. Environ Health Perspect. 2020;128(4):047008.
Hengstermann M, Díaz-Artiga A, Otzóy-Sucúc R, Laura Maria Ruiz-Aguilar A, Thompson LM, Aravindalochanan V, et al. Developing visual messages to support liquefied petroleum gas use in intervention homes in the household air pollution intervention network (HAPIN) trial in rural Guatemala. Health Educ Behav. 2021;48(5):651–69.
Download references
Acknowledgements
The authors wish to acknowledge David Chambers at the National Cancer Institute for reading the manuscript and providing feedback. Additionally, the authors thank Curt DellaValle at the National Cancer Institute for serving as a sounding board in the development of this commentary.
Open Access funding provided by the National Institutes of Health (NIH). No financial support was provided for this work.
Author information
Authors and affiliations.
Division of Cancer Control and Population Sciences, National Cancer Institute, National Institutes of Health, 9609 Medical Center Drive, Rockville, MD, 20850, USA
Division of Extramural Research and Training, National Institute of Environmental Health Sciences, National Institutes of Health, Research Triangle Park, NC, 27709, USA
Lindsey Martin
Office of Scientific Coordination, Planning and Evaluation (SCOPE), National Institute of Environmental Health Sciences, National Institute of Health, Research Triangle Park, NC, 27709, USA
Gwen Collman
You can also search for this author in PubMed Google Scholar
Contributions
GN conceived of and led the development and writing of the manuscript. LM contributed to the writing of sections of the manuscript, including developing the table. GC provided substantial input on the manuscript and development of the table. All authors contributed to the writing of the manuscript, revising it critically for important intellectual content. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Gila Neta .
Ethics declarations
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Neta, G., Martin, L. & Collman, G. Advancing environmental health sciences through implementation science. Environ Health 21 , 136 (2022). https://doi.org/10.1186/s12940-022-00933-0
Download citation
Received : 17 June 2022
Accepted : 27 October 2022
Published : 23 December 2022
DOI : https://doi.org/10.1186/s12940-022-00933-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Environmental health sciences
- Implementation science
- Translation
- Environmental health
Environmental Health
ISSN: 1476-069X
- General enquiries: [email protected]
Identifying Issues and Priorities in Reporting Back Environmental Health Data
Affiliations.
- 1 HERCULES Exposome Research Center, Rollins School of Public Health, Emory University, Atlanta, GA 30322, USA.
- 2 Institute for the Environment, UNC Superfund Research Program, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA.
- 3 Department of Occupational and Environmental Health, University of Iowa, Iowa City, IA 52246, USA.
- 4 College of Pharmacy & Mountain West Clinical and Translational Research-Infrastructure Network, UNM Health Sciences Center, University of New Mexico, Albuquerque, NM 87131, USA.
- PMID: 32947900
- PMCID: PMC7557638
- DOI: 10.3390/ijerph17186742
Experts recommend reporting environmental exposure results back to research participants and communities, yet environmental health researchers need further guidance to improve the practice of reporting back. We present the results of a workshop developed to identify pertinent issues and areas for action in reporting back environmental health research results. Thirty-five attendees participated, brainstorming responses to the prompt: "What are some specific issues that are relevant to reporting back research results to individuals or the larger community?", and then grouping responses by similarity and rating their importance. Based on a combined theoretical foundation of grounded theory and qualitative content analysis, we used concept mapping to develop a collective understanding of the issues. Visual maps of the participants' responses were created using nonmetric multidimensional scaling and hierarchical cluster analysis. The resulting concept map provided a spatial depiction of five issue areas: Effective Communication Strategies, Community Knowledge and Concerns, Uncertainty, Empowering Action, and Institutional Review and Oversight (listed from highest to lowest rating). Through these efforts, we disentangled the complex issues affecting how and whether environmental health research results are reported back to participants and communities, by identifying five distinct themes to guide recommendations and action. Engaging community partners in the process of reporting back emerged as a unifying global theme, which could improve how researchers report back research results by understanding community context to develop effective communication methods and address uncertainty, the ability to act, and institutional concerns about beneficence and justice.
Keywords: community engagement; concept mapping; environmental health; research report-back.
Publication types
- Research Support, N.I.H., Extramural
- Environmental Exposure* / analysis
- Environmental Health*
- Grounded Theory
- Research Personnel
Grants and funding
- P42ES031007/ES/NIEHS NIH HHS/United States
- 1P50ES026102/ES/NIEHS NIH HHS/United States
- P30 ES019776/ES/NIEHS NIH HHS/United States
- P42 ES031007/ES/NIEHS NIH HHS/United States
- P30 ES005605/ES/NIEHS NIH HHS/United States

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
JavaScript appears to be disabled on this computer. Please click here to see any active alerts .
Health and the Environment

On this page:
- Research on Health Effects from Air Pollution
- Human Health and Climate Change
- Health and Water Research
Research on COVID in the Environment
- Human Health Risk Assessment
- Lead (Pb) Research
How and where are people exposed to potentially harmful pollutants, chemicals, and other contaminants in the environment? What are the health risks from those exposures? And what tools, information, and other resources can EPA researchers provide to advance cleaner air, water, and land for healthier, more sustainable communities? Those are some of the key questions our health researchers and their partners are working to answer.
Below are links to learn more about EPA research on health and the environment.
Research on Health Effects from Air Pollution
Our researchers are leading the effort to advance what is known about the health effects of air pollution . Together with their grantees and partners they are working to better understand the role that poor air quality plays in causing and/or exacerbating conditions such as asthma, cardiovascular events (including heart attacks and strokes) and other detrimental health impacts—especially in children, the elderly, and people living in areas with high levels of air pollution.
Human Health and Climate Change
Our researchers are working to understand the human health implications of the changing climate . The goal is to provide information that can be used to help people make informed decision about how to protect themselves in the face of heat waves and other extreme weather events, and by medical and other health professionals to develop plans and strategies to prevent or minimize public health impacts from climate change.
Health and Water Research
Clean, abundant water is crucial to public health. Our health-related water research supports drinking water standards and other policies that protect people from waterborne illnesses, improves methods to measure human exposure to pathogens and contaminants in drinking water, and prioritizes pathogen groups and information on the health risks of waterborne pathogens.
Our researchers are working to reduce the risk of exposure to SARS-CoV-2 , the virus that causes COVID-19. This research will help states, tribes, local, and territorial governments, including public health agencies, guide homeowners, business owners, and workplace managers to reduce the risk of exposure to SARS-CoV-2.
Human Health Risk Assessment
Our researchers conduct human health risk assessments to estimate the nature and probability of adverse health effects in humans who may be exposed to chemicals in the environment. EPA’s Health and Environmental Risk Assessment Research Program is designed to develop and apply state-of-the-science research to characterize the impacts on human and ecological systems, whether they result from exposure to single, complex, or multiple physical, chemical, or biological stressors.
Lead (Pb) Research
Even though lead (Pb) exposures have dramatically declined in recent decades, they still pose serious risks to public health. Our researchers are conducting research across the environment and at critical life stages to understand and mitigate risks associated with exposure to lead .
- Health Research Home
- Children's Environmental Health Research
- Community Public Health
- Cumulative Impacts Research
- Funding, Resources, & Partnerships
- Health & the Environment
- Health Impact Assessments
Advancing social justice, promoting decent work ILO is a specialized agency of the United Nations
Global Report
Climate change is already having serious impacts on the safety and health of workers in all regions of the world. Workers are among those most exposed to climate change hazards yet frequently have no choice but to continue working, even if conditions are dangerous. Global occupational safety and health (OSH) protections have struggled to keep up with the evolving risks from climate change, resulting in worker mortality and morbidity.
This report presents critical evidence related to the impacts of climate change on OSH, to bring attention to the global health threat workers are currently facing. The report addresses the following key issues:
- Excessive heat
- Ultraviolet (UV) radiation
- Extreme weather events
- Workplace air pollution
- Vector-borne diseases
- Agrochemicals
Additional details
- ISBN: 9789220405079 (web PDF)
- ISBN: 9789220405062 (print)
Related content

OSH and climate change
Climate change creates a ‘cocktail’ of serious health hazards for 70 per cent of the world’s workers

World Day for Safety and Health at Work 2024: The impacts of climate change on occupational safety and health

Overview of the key findings of the report
Report at a glance: Ensuring safety and health at work in a changing climate
- Skip to main content
- Keyboard shortcuts for audio player
130 million Americans routinely breathe unhealthy air, report finds
Alejandra Borunda

Wildfire smoke from Canada caused dangerously unhealthy air quality in New York City and across much of the U.S. in 2023. While air quality has improved greatly in the U.S. in recent decades, wildfire smoke and other climate-influenced problems are endangering that progress. Ed Jones/AFP via Getty Images hide caption
Wildfire smoke from Canada caused dangerously unhealthy air quality in New York City and across much of the U.S. in 2023. While air quality has improved greatly in the U.S. in recent decades, wildfire smoke and other climate-influenced problems are endangering that progress.
Over one-third of Americans, or about 130 million people, routinely breathe in unhealthy air, according to the newest State of the Air report from the American Lung Association (ALA). That number is larger in 2023 than in years past, despite significant long-term and ongoing efforts to clean the nation's air. And climate change, the report says, is making the job harder.
Hotter temperatures lead to more ozone formation and can make the air dustier, too. But the biggest climate-fueled pollution challenge comes from wildfire smoke , which has added vast quantities of dangerous fine particle pollution to the air. Western states like California and Colorado have found that wildfire smoke is counterbalancing long-term, successful efforts to clean up pollution from human-controlled industrial sources , like coal-fired power plants and diesel truck exhaust.
"Wildfires are changing the landscape, literally and figuratively," says Katherine Pruitt, national policy director at the American Lung Association.
Long-term air improvements interrupted in the West
Since the passage of the landmark Clean Air Act in 1970 , the country's air has improved markedly. Measures like adding pollution control to cars, trucks, and fossil-fuel-burning power plants cut down on the amount of fine particles in the air. Those particles can penetrate deep into people's lungs and even cross into the bloodstream, where they contribute to a range of chronic and acute health risks.
Between 1990 and 2020, pollution from those fine particles dropped by about 40% nationwide . The improvements were particularly noticeable in industrial East Coast cities and states.
This year's State of the Air report reiterates that most of the country, most notably the eastern U.S., has gotten cleaner over time as industrial pollution sources have been reined in.
But in the West, 2023 had the most days ever recorded with dangerous or very dangerous air quality, measured by the Air Quality Index. And for the first time in the report's 25-year history, the 25 cities with the worst short-term particle pollution in the country were all in the Western U.S.
"The severity of the pollution is unprecedented," says Pruitt.
The report highlights an increasingly clear challenge, says Susan Anenberg, an air quality expert at George Washington University and a consultant for the EPA. Through regulations over past decades, "we've pretty much addressed the easiest ways of reducing pollution," she says. "So we have catalytic converters on our vehicles, we have diesel particulate filters on our trucks, we have scrubbers on our power plants."
But now, Anenberg says, the challenge is getting harder as human-driven climate change worsens some problems like ozone, a gas that forms near the ground when pollutants and some natural compounds react with sunlight and heat, and wildfire smoke. The easy wins, she says, are gone.
"It just really underscores that we need to do both things at the same time," Anenberg says. "We need to reduce carbon emissions that are causing anthropogenic climate change, and we need to continue to pursue stringent regulations on air pollution emissions."
A soup of unhealthy pollutants
The State of the Air report tracks particle pollution and ozone. Both are harmful to people's health, increasing the risk of respiratory problems like asthma. Fine particle pollution has also been linked to worse heart disease outcomes and even the development of dementia.
Bakersfield, California, has stayed at the top of the report's list for the U.S. city with the worst short-term particle pollution in the country for five years. This time, it also got top billing for year-round particle pollution, too. The region is a major site of oil and gas production as well as agriculture, both of which produce significant local pollution.
"Those industries are the main driver of our economy but also our air pollution," says Jasmin Martinez, an advocate at the Central Valley Air Quality Coalition who has lived most of their life in the San Joaquin Valley, where Bakersfield lies. The area has been heavily polluted for their entire lifetime, despite the federal and state laws mandating local industries to minimize pollution.
They chose to move back home after college even though they were well aware of the dangers. "It's always in the back of my mind, just living here, I may be just losing years of my life," Martinez says.
Air pollution helps hasten t ens or even hundreds of thousands of premature deaths each year in the U.S. alone. It is one of the most profound public health risks in the nation, says Pruitt.
Bangor, Maine, and Honolulu, Hawaii, have some of the cleanest air in the country.
Unequal exposure to dirty air
While air in the U.S. got much cleaner overall after Clean Air Act-related regulations, the improvements were far from uniformly shared. Communities of color and low-income Americans have historically breathed in dirtier air than wealthier or whiter communities , a disparity that continues into 2024, the report says.
About 130 million Americans live in places where particle or ozone pollution exceeds levels the EPA considers healthy. About 70 million of those are people of color.
Pruitt stresses people of color are "more than twice as likely as white people to live in a place that gets failing grades" for short and long-term particle pollution and ozone, she says.

Opportunity for progress?
Late last year, the Environmental Protection Agency announced a long-awaited update to its regulatory standard for PM2.5, or fine particle pollution . The agency lowered the allowable pollution from 12 micrograms per meter cubed of air averaged over a year to 9—a major tightening, says Anenberg.
The tighter standard still far exceeds the World Health Organization's recommendation of 5 micrograms or less.
The American Lung Association used the new standard to calculate dangerous exposures. Applying the new value, they found the number of Americans exposed to unhealthy air rose from about 120 million people counted in the previous report to roughly 130 million.
What that really means, says Pruitt, is that "those people have been breathing unhealthy air for years." They simply weren't counted yet.
Meeting the new standard will take years to achieve, but Pruitt welcomes the rules. Next, she says, she hopes to see similar standard tightening for ozone pollution.
Meanwhile, climate change complicates efforts to clean up the air, says Anenberg. "This report tells us that we need to ramp up our carbon mitigation efforts so that we're slowing the rate of climate change because that climate change is putting more pollution into the air," she says. At the same time, "we need to redouble our efforts to reduce pollution from the sources where it's possible to reduce pollution."
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
Environmental Factor
Your online source for niehs news, niehs-supported research can help people with asthma breathe better.
Recent scientific advances help to identify root causes of and new treatment approaches for asthma, a chronic respiratory disease.
By Janelle Weaver and Caroline Stetler
In recognition of Asthma Awareness Month, Environmental Factor shares the latest discoveries made by NIEHS scientists and grant recipients related to the chronic respiratory disease.
Asthma, which is characterized by coughing, wheezing, chest tightness, and shortness of breath, affects about 25 million people in the United States, including 4.7 million children and adolescents. In 2021, more than 3,500 people across the country died from asthma-related causes.
The following examples of recently published research aim to improve the diagnosis, treatment, and prevention of asthma by better understanding the environment’s role in the disease.

Majority of clinicians do not frequently assess environmental asthma triggers
Environmental assessment and recommendations to patients vary considerably among asthma care providers, according to NIEHS researchers and their collaborators. A higher percentage of specialists assessed asthma triggers at home, school, or work than primary care or advanced practice providers. However, 46%-76% of clinicians, depending on clinician type, reported not assessing triggers almost always during asthma visits. Read the full summary .
Citation : Salo PM, Akinbami LJ, Cloutier MM, Wilkerson JC, Elward KS, Mazurek JM, Diette GB, Mitchell TA, Williams S, Zeldin DC. 2023. Environmental management of asthma in clinical practice: results from the 2012 National Ambulatory Medical Care Survey . J Allergy Clin Immunol Glob 3(1):100192.
Plasma proteomic signatures of adult asthma
A large-scale proteomics study identified more than 100 plasma proteins associated with asthma in adults, according to NIEHS researchers and their collaborators. In addition to validating previous associations, the researchers identified many novel proteins that could inform the development of diagnostic biomarkers and therapeutic targets in asthma management. Read the full summary .
Citation : Smilnak GJ, Lee Y, Chattopadhyay A, Wyss AB, White JD, Sikdar S, Jin J, Grant AJ, Motsinger-Reif AA, Li JL, Lee M, Yu B, London SJ. 2024. Plasma protein signatures of adult asthma . Allergy 79(3):643-655.
Targeting the root cause of asthma
Housing policy may be a tool to reduce childhood asthma disparities, according to recent findings from the NIEHS-funded Mobility Asthma Project . As reported in the Journal of the American Medical Association, children who move to neighborhoods with lower rates of poverty experience significant improvements in asthma symptoms, in part by reducing stress. Read the full article .
Citation : Pollack CE, Roberts LC, Peng RD, Cimbolic P, Judy D, Balcer-Whaley S, Grant T, Rule A, Deluca S, Davis MF, Wright RJ, Keet CA, Matsui EC. 2023. Association of a housing mobility program with childhood asthma symptoms and exacerbations . JAMA 329(19):1671-1681.
Why anti-thromboxane therapies have failed in asthma clinical trials
Thromboxane A2 (TXA2) can dampen the immune response in the allergic lung, which may have important therapeutic consequences, according to NIEHS researchers and their collaborators. In contrast to its acute, pro-inflammatory, and bronchoconstrictive effects, TXA2 also has longer-lasting immunosuppressive effects that attenuate Th2 and Th9 cell differentiation that drives asthma progression. These results help explain the failure of anti-thromboxane therapies and suggest that targeting the TXA2/TP receptor signaling pathway may lead to the development of novel asthma treatments. Read the full summary .
Citation : Li H, Bradbury JA, Edin ML, Gruzdev A, Li H, Graves JP, DeGraff LM, Lih FB, Feng C, Wolf ER, Bortner CD, London SJ, Sparks MA, Coffman TM, Zeldin DC. 2024. TXA2 attenuates allergic lung inflammation through regulation of Th2, Th9 and Treg differentiation . J Clin Invest e165689 [Online 14 Mar 2024].
Community-level characteristics modify childhood asthma risk
Early-life air pollution exposure is associated with increased childhood asthma incidence, with higher risk among minoritized families living in densely populated communities, according to NIEHS-funded researchers. Their results suggest that exposure to fine particulate matter (PM) smaller than 2.5 microns in diameter (PM2.5) and nitrogen dioxide (NO2) may play a role in the development of asthma by early and middle childhood in communities characterized by fewer opportunities and resources and multiple environmental exposures. Read the full article .
Citation : Zanobetti A, Ryan PH, Coull BA, Luttmann-Gibson H, Datta S, Blossom J, Brokamp C, Lothrop N, Miller RL, Beamer PI, Visness CM, Andrews H, Bacharier LB, Hartert T, Johnson CC, Ownby DR, Khurana Hershey GK, Joseph CLM, Mendonça EA, Jackson DJ, Zoratti EM, Wright AL, Martinez FD, Seroogy CM, Ramratnam SK, Calatroni A, Gern JE, Gold DR; ECHO Children’s Respiratory and Environmental Workgroup. 2024. Early-Life exposure to air pollution and childhood asthma cumulative incidence in the ECHO CREW Consortium . JAMA Netw Open 7(2):e240535.
Additional resources to explore
- For resources on the prevention, treatment, and management of asthma, check out the NIH Learn More Breathe Better® program .
- Lower allergen levels in your home by reviewing these tips on the NIEHS asthma webpage .
- Join an asthma study to help scientists understand how bacteria and other factors in the environment affect people who have moderate to severe asthma.
- Learn about new research exploring the asthma-air pollution connection .
- Check out the asthma research portal from the National Institute of Allergy and Infectious Diseases.
(Janelle Weaver, Ph.D., is a contract writer for the NIEHS Office of Communications and Public Liaison. Caroline Stetler is Editor-in-Chief of the Environmental Factor, produced monthly by the NIEHS Office of Communications and Public Liaison.)
Related Articles

NIEHS Women’s Health Awareness event celebrates 10th anniversary

Lisa Rider inducted into Association of American Physicians
Ask the Expert: How does NIEHS research on PFAS affect me?

Community engagement critical to addressing women’s health concerns

Monica Bertagnolli starts as new NIH director
Ad-free. Influence-free. Powered by consumers.
The payment for your account couldn't be processed or you've canceled your account with us.
We don’t recognize that sign in. Your username maybe be your email address. Passwords are 6-20 characters with at least one number and letter.
We still don’t recognize that sign in. Retrieve your username. Reset your password.
Forgot your username or password ?
Don’t have an account?
- Account Settings
- My Benefits
- My Products
- Donate Donate
Save products you love, products you own and much more!
Other Membership Benefits:
Suggested Searches
- Become a Member
Car Ratings & Reviews
2024 Top Picks
Car Buying & Pricing
Which Car Brands Make the Best Vehicles?
Tires, Maintenance & Repair
Car Reliability Guide
Key Topics & News
Listen to the Talking Cars Podcast
Home & Garden
Bed & Bath
Top Picks From CR
Best Mattresses
Lawn & Garden
TOP PICKS FROM CR
Best Lawn Mowers and Tractors
Home Improvement
Home Improvement Essential
Best Wood Stains
Home Safety & Security
HOME SAFETY
Best DIY Home Security Systems
REPAIR OR REPLACE?
What to Do With a Broken Appliance
Small Appliances
Best Small Kitchen Appliances
Laundry & Cleaning
Best Washing Machines
Heating, Cooling & Air
Most Reliable Central Air-Conditioning Systems
Electronics
Home Entertainment
FIND YOUR NEW TV
Home Office
Cheapest Printers for Ink Costs
Smartphones & Wearables
BEST SMARTPHONES
Find the Right Phone for You
Digital Security & Privacy
MEMBER BENEFIT
CR Security Planner
Take Action
How PFAS Can Harm Your Health
Even at low levels, these chemicals have been linked to kidney disease, lowered immunity in kids, and a variety of other health concerns

In recent decades, PFAS exposure has been linked to a growing list of health problems, including immune system suppression, lower birth weight, and increased risk for some cancers. These chemicals are added to many materials to make them resistant to grease, water, and stains, and to add nonstick properties. But their effects on human health and the environment have put their widespread use under increased scrutiny.
In 2022 Consumer Reports tests of more than 100 food packaging products from U.S. restaurants and supermarkets found dangerous PFAS chemicals in many of them , including paper bags for french fries, wrappers for hamburgers, molded fiber salad bowls, and single-use paper plates. ( Recent action by the Food and Drug Administration suggests that such uses may be on the way out.) Previous CR tests found PFAS—per- and polyfluoroalkyl substances—in drinking water and bottled water . We’ve also identified dental flosses that contain these chemicals and found certain PFAS in nonstick cookware that manufacturers said were not present.
- How Humans Are Exposed to PFAS
- PFAS Effects on Health
Are PFAS Replacements Safe?
How people are exposed to pfas.
PFAS are often called “forever chemicals” because they break down extremely slowly, if ever. That persistence, combined with the many products that now contain PFAS, means that there are many ways the chemicals can enter the environment and eventually reach humans, too.
Consider, for example, the production of food packaging with PFAS coating. In Maine, wastewater sludge from mills where such products are produced has reportedly been used to fertilize fields where cattle graze. In 2020 the Maine Department of Agriculture, Conservation, and Forestry tested milk from dairy farms and found levels of one particular PFAS in a sample from a farm that were more than 150 times higher than state regulations permit.
When food packaging contains PFAS, some of those chemicals can migrate into food. Other products, like stain-resistant carpets, can leave PFAS in household dust and air.
And finally, once food packaging or other products containing PFAS are thrown away, PFAS can leach out from landfills or spread from incinerators into the environment, where they can contaminate soil, food, water, and air—just like they can when they’re first produced.
People may then eat food containing the chemicals, drink water that contains them, or even breathe in the chemicals.

On April 10 the Environmental Protection Agency announced the first nationwide limits on PFAS, setting enforceable limits on certain PFAS in drinking water. The agency estimates that these limits—which are far stricter than the nonenforceable levels the agency previously used—will require 6 to 10 percent of water utilities to take action. The EPA says these new limits are the strictest that are feasible but acknowledges that even lower levels may pose health risks .
Learn how to avoid PFAS .
PFAS Are Linked to Many Health Problems
For decades PFAS manufacturers have had information indicating that the chemicals may harm human health, according to reporting from the Environmental Working Group . But for the first 60 or so years that PFAS were in production, many people—including many health experts—thought that potential harms were specific to workers exposed to the chemicals at an industrial scale, not the general public.
Then, in 1998, a West Virginia farmer named Wilbur Tennant started raising concerns about the effects that pollution from a nearby DuPont factory had on his cattle. This helped lead to a class-action lawsuit alleging that this contamination—with the PFAS chemical PFOA, also known as C8—could be affecting about 70,000 people who got water from the same polluted source.
The resulting settlement led to the creation of the C8 science panel , which between 2005 and 2013 assessed links between exposure to PFOA and a number of diseases, and found probable links between PFOA exposure and thyroid disease, higher cholesterol levels, kidney and testicular cancer, ulcerative colitis, and pregnancy-induced hypertension. Other research on various PFAS has found links to metabolic changes in children , as well as liver damage and kidney disease.
There are consistent patterns across these chemicals, and the most consistent pattern is that they’re toxic.
PFAS Pose Health Concerns Even at Low Levels
Calculating the exact level of PFAS exposure that causes harm isn’t straightforward, especially because there are thousands of different PFAS, some more toxic than others. But growing research has shown that health risks can occur even at very low levels. Case in point: The effects from PFAS are present even on the pristine Faroe Islands, a group of 18 small, rocky islands midway between Iceland and Norway.
In 2010 and 2011, Philippe Grandjean, PhD, a professor of environmental medicine at the University of Southern Denmark, studied children in the Faroes to see whether certain chemicals in the environment could dampen the immune system’s response to childhood vaccines. When he saw a study showing that PFAS could affect animal immune systems, he and colleagues decided to see whether PFAS also affected how children responded to the vaccines.
The results were dramatic. “I fell off my chair,” Grandjean says. “It was very clear these compounds were inhibiting the immune system.”
In 2012 Grandjean and colleagues published research showing that higher levels of PFAS in blood samples taken from the children were associated with less effective protection after being vaccinated.
The findings were alarming not just for people in the Faroes. Blood PFAS levels among children in the U.S. are comparable, Grandjean says. Follow-up research in other countries has confirmed this effect and has also shown that children with higher blood levels of PFAS have more infections, he says.
Read our investigation, " ‘Forever Chemicals’ Are Found in Some Milk, Including Organic ."
Manufacturers have stopped producing certain PFAS chemicals in the U.S. as concerns about their impact on health have become more widely known. But they’ve been replaced by newer substances in the same chemical family that have not been as thoroughly studied by independent researchers.
Both the Food and Drug Administration and the American Chemistry Council, which represents PFAS manufacturers, argue that we don’t know for sure that newer PFAS are as unsafe as the ones they are replacing.
But a growing body of research suggests that many do pose risks, says Miriam Rotkin-Ellman, formerly a senior scientist at the Natural Resources Defense Council. A database of research on more than two dozen different PFAS compiled by a group of scientists who have studied the chemicals suggests harmful effects associated with many of them. “There are consistent patterns across these chemicals,” she says, “and the most consistent pattern is that they’re toxic.”
@consumerreports Our tests of 118 food packaging products found PFAS—‘forever chemicals’ linked to a growing list of health problems—in all kinds of food packaging. Learn more at CR.org/pfaspackaging #foodtok #foodsafety ♬ original sound - Consumer Reports
Kevin Loria
Kevin Loria is a senior reporter covering health and science at Consumer Reports. He has been with CR since 2018, covering environmental health, food safety, infectious disease, fitness, and more. Previously, Kevin was a correspondent covering health, science, and the environment at Business Insider. Kevin lives in Washington, D.C., with his wife and children. Follow him on Twitter @kevloria .
Sharing is Nice
We respect your privacy . All email addresses you provide will be used just for sending this story.
Trending in Toxic Chemicals & Substances
A Third of Chocolate Products Are High in Heavy Metals, CR's Tests Find
Lead and Cadmium Could Be in Your Dark Chocolate
How to Get PFAS Out of Your Drinking Water
Best Multipurpose Cleaners
- Open access
- Published: 18 April 2024
Research ethics and artificial intelligence for global health: perspectives from the global forum on bioethics in research
- James Shaw 1 , 13 ,
- Joseph Ali 2 , 3 ,
- Caesar A. Atuire 4 , 5 ,
- Phaik Yeong Cheah 6 ,
- Armando Guio Español 7 ,
- Judy Wawira Gichoya 8 ,
- Adrienne Hunt 9 ,
- Daudi Jjingo 10 ,
- Katherine Littler 9 ,
- Daniela Paolotti 11 &
- Effy Vayena 12
BMC Medical Ethics volume 25 , Article number: 46 ( 2024 ) Cite this article
1214 Accesses
6 Altmetric
Metrics details
The ethical governance of Artificial Intelligence (AI) in health care and public health continues to be an urgent issue for attention in policy, research, and practice. In this paper we report on central themes related to challenges and strategies for promoting ethics in research involving AI in global health, arising from the Global Forum on Bioethics in Research (GFBR), held in Cape Town, South Africa in November 2022.
The GFBR is an annual meeting organized by the World Health Organization and supported by the Wellcome Trust, the US National Institutes of Health, the UK Medical Research Council (MRC) and the South African MRC. The forum aims to bring together ethicists, researchers, policymakers, research ethics committee members and other actors to engage with challenges and opportunities specifically related to research ethics. In 2022 the focus of the GFBR was “Ethics of AI in Global Health Research”. The forum consisted of 6 case study presentations, 16 governance presentations, and a series of small group and large group discussions. A total of 87 participants attended the forum from 31 countries around the world, representing disciplines of bioethics, AI, health policy, health professional practice, research funding, and bioinformatics. In this paper, we highlight central insights arising from GFBR 2022.
We describe the significance of four thematic insights arising from the forum: (1) Appropriateness of building AI, (2) Transferability of AI systems, (3) Accountability for AI decision-making and outcomes, and (4) Individual consent. We then describe eight recommendations for governance leaders to enhance the ethical governance of AI in global health research, addressing issues such as AI impact assessments, environmental values, and fair partnerships.
Conclusions
The 2022 Global Forum on Bioethics in Research illustrated several innovations in ethical governance of AI for global health research, as well as several areas in need of urgent attention internationally. This summary is intended to inform international and domestic efforts to strengthen research ethics and support the evolution of governance leadership to meet the demands of AI in global health research.
Peer Review reports
Introduction
The ethical governance of Artificial Intelligence (AI) in health care and public health continues to be an urgent issue for attention in policy, research, and practice [ 1 , 2 , 3 ]. Beyond the growing number of AI applications being implemented in health care, capabilities of AI models such as Large Language Models (LLMs) expand the potential reach and significance of AI technologies across health-related fields [ 4 , 5 ]. Discussion about effective, ethical governance of AI technologies has spanned a range of governance approaches, including government regulation, organizational decision-making, professional self-regulation, and research ethics review [ 6 , 7 , 8 ]. In this paper, we report on central themes related to challenges and strategies for promoting ethics in research involving AI in global health research, arising from the Global Forum on Bioethics in Research (GFBR), held in Cape Town, South Africa in November 2022. Although applications of AI for research, health care, and public health are diverse and advancing rapidly, the insights generated at the forum remain highly relevant from a global health perspective. After summarizing important context for work in this domain, we highlight categories of ethical issues emphasized at the forum for attention from a research ethics perspective internationally. We then outline strategies proposed for research, innovation, and governance to support more ethical AI for global health.
In this paper, we adopt the definition of AI systems provided by the Organization for Economic Cooperation and Development (OECD) as our starting point. Their definition states that an AI system is “a machine-based system that can, for a given set of human-defined objectives, make predictions, recommendations, or decisions influencing real or virtual environments. AI systems are designed to operate with varying levels of autonomy” [ 9 ]. The conceptualization of an algorithm as helping to constitute an AI system, along with hardware, other elements of software, and a particular context of use, illustrates the wide variety of ways in which AI can be applied. We have found it useful to differentiate applications of AI in research as those classified as “AI systems for discovery” and “AI systems for intervention”. An AI system for discovery is one that is intended to generate new knowledge, for example in drug discovery or public health research in which researchers are seeking potential targets for intervention, innovation, or further research. An AI system for intervention is one that directly contributes to enacting an intervention in a particular context, for example informing decision-making at the point of care or assisting with accuracy in a surgical procedure.
The mandate of the GFBR is to take a broad view of what constitutes research and its regulation in global health, with special attention to bioethics in Low- and Middle- Income Countries. AI as a group of technologies demands such a broad view. AI development for health occurs in a variety of environments, including universities and academic health sciences centers where research ethics review remains an important element of the governance of science and innovation internationally [ 10 , 11 ]. In these settings, research ethics committees (RECs; also known by different names such as Institutional Review Boards or IRBs) make decisions about the ethical appropriateness of projects proposed by researchers and other institutional members, ultimately determining whether a given project is allowed to proceed on ethical grounds [ 12 ].
However, research involving AI for health also takes place in large corporations and smaller scale start-ups, which in some jurisdictions fall outside the scope of research ethics regulation. In the domain of AI, the question of what constitutes research also becomes blurred. For example, is the development of an algorithm itself considered a part of the research process? Or only when that algorithm is tested under the formal constraints of a systematic research methodology? In this paper we take an inclusive view, in which AI development is included in the definition of research activity and within scope for our inquiry, regardless of the setting in which it takes place. This broad perspective characterizes the approach to “research ethics” we take in this paper, extending beyond the work of RECs to include the ethical analysis of the wide range of activities that constitute research as the generation of new knowledge and intervention in the world.
Ethical governance of AI in global health
The ethical governance of AI for global health has been widely discussed in recent years. The World Health Organization (WHO) released its guidelines on ethics and governance of AI for health in 2021, endorsing a set of six ethical principles and exploring the relevance of those principles through a variety of use cases. The WHO guidelines also provided an overview of AI governance, defining governance as covering “a range of steering and rule-making functions of governments and other decision-makers, including international health agencies, for the achievement of national health policy objectives conducive to universal health coverage.” (p. 81) The report usefully provided a series of recommendations related to governance of seven domains pertaining to AI for health: data, benefit sharing, the private sector, the public sector, regulation, policy observatories/model legislation, and global governance. The report acknowledges that much work is yet to be done to advance international cooperation on AI governance, especially related to prioritizing voices from Low- and Middle-Income Countries (LMICs) in global dialogue.
One important point emphasized in the WHO report that reinforces the broader literature on global governance of AI is the distribution of responsibility across a wide range of actors in the AI ecosystem. This is especially important to highlight when focused on research for global health, which is specifically about work that transcends national borders. Alami et al. (2020) discussed the unique risks raised by AI research in global health, ranging from the unavailability of data in many LMICs required to train locally relevant AI models to the capacity of health systems to absorb new AI technologies that demand the use of resources from elsewhere in the system. These observations illustrate the need to identify the unique issues posed by AI research for global health specifically, and the strategies that can be employed by all those implicated in AI governance to promote ethically responsible use of AI in global health research.
RECs and the regulation of research involving AI
RECs represent an important element of the governance of AI for global health research, and thus warrant further commentary as background to our paper. Despite the importance of RECs, foundational questions have been raised about their capabilities to accurately understand and address ethical issues raised by studies involving AI. Rahimzadeh et al. (2023) outlined how RECs in the United States are under-prepared to align with recent federal policy requiring that RECs review data sharing and management plans with attention to the unique ethical issues raised in AI research for health [ 13 ]. Similar research in South Africa identified variability in understanding of existing regulations and ethical issues associated with health-related big data sharing and management among research ethics committee members [ 14 , 15 ]. The effort to address harms accruing to groups or communities as opposed to individuals whose data are included in AI research has also been identified as a unique challenge for RECs [ 16 , 17 ]. Doerr and Meeder (2022) suggested that current regulatory frameworks for research ethics might actually prevent RECs from adequately addressing such issues, as they are deemed out of scope of REC review [ 16 ]. Furthermore, research in the United Kingdom and Canada has suggested that researchers using AI methods for health tend to distinguish between ethical issues and social impact of their research, adopting an overly narrow view of what constitutes ethical issues in their work [ 18 ].
The challenges for RECs in adequately addressing ethical issues in AI research for health care and public health exceed a straightforward survey of ethical considerations. As Ferretti et al. (2021) contend, some capabilities of RECs adequately cover certain issues in AI-based health research, such as the common occurrence of conflicts of interest where researchers who accept funds from commercial technology providers are implicitly incentivized to produce results that align with commercial interests [ 12 ]. However, some features of REC review require reform to adequately meet ethical needs. Ferretti et al. outlined weaknesses of RECs that are longstanding and those that are novel to AI-related projects, proposing a series of directions for development that are regulatory, procedural, and complementary to REC functionality. The work required on a global scale to update the REC function in response to the demands of research involving AI is substantial.
These issues take greater urgency in the context of global health [ 19 ]. Teixeira da Silva (2022) described the global practice of “ethics dumping”, where researchers from high income countries bring ethically contentious practices to RECs in low-income countries as a strategy to gain approval and move projects forward [ 20 ]. Although not yet systematically documented in AI research for health, risk of ethics dumping in AI research is high. Evidence is already emerging of practices of “health data colonialism”, in which AI researchers and developers from large organizations in high-income countries acquire data to build algorithms in LMICs to avoid stricter regulations [ 21 ]. This specific practice is part of a larger collection of practices that characterize health data colonialism, involving the broader exploitation of data and the populations they represent primarily for commercial gain [ 21 , 22 ]. As an additional complication, AI algorithms trained on data from high-income contexts are unlikely to apply in straightforward ways to LMIC settings [ 21 , 23 ]. In the context of global health, there is widespread acknowledgement about the need to not only enhance the knowledge base of REC members about AI-based methods internationally, but to acknowledge the broader shifts required to encourage their capabilities to more fully address these and other ethical issues associated with AI research for health [ 8 ].
Although RECs are an important part of the story of the ethical governance of AI for global health research, they are not the only part. The responsibilities of supra-national entities such as the World Health Organization, national governments, organizational leaders, commercial AI technology providers, health care professionals, and other groups continue to be worked out internationally. In this context of ongoing work, examining issues that demand attention and strategies to address them remains an urgent and valuable task.
The GFBR is an annual meeting organized by the World Health Organization and supported by the Wellcome Trust, the US National Institutes of Health, the UK Medical Research Council (MRC) and the South African MRC. The forum aims to bring together ethicists, researchers, policymakers, REC members and other actors to engage with challenges and opportunities specifically related to research ethics. Each year the GFBR meeting includes a series of case studies and keynotes presented in plenary format to an audience of approximately 100 people who have applied and been competitively selected to attend, along with small-group breakout discussions to advance thinking on related issues. The specific topic of the forum changes each year, with past topics including ethical issues in research with people living with mental health conditions (2021), genome editing (2019), and biobanking/data sharing (2018). The forum is intended to remain grounded in the practical challenges of engaging in research ethics, with special interest in low resource settings from a global health perspective. A post-meeting fellowship scheme is open to all LMIC participants, providing a unique opportunity to apply for funding to further explore and address the ethical challenges that are identified during the meeting.
In 2022, the focus of the GFBR was “Ethics of AI in Global Health Research”. The forum consisted of 6 case study presentations (both short and long form) reporting on specific initiatives related to research ethics and AI for health, and 16 governance presentations (both short and long form) reporting on actual approaches to governing AI in different country settings. A keynote presentation from Professor Effy Vayena addressed the topic of the broader context for AI ethics in a rapidly evolving field. A total of 87 participants attended the forum from 31 countries around the world, representing disciplines of bioethics, AI, health policy, health professional practice, research funding, and bioinformatics. The 2-day forum addressed a wide range of themes. The conference report provides a detailed overview of each of the specific topics addressed while a policy paper outlines the cross-cutting themes (both documents are available at the GFBR website: https://www.gfbr.global/past-meetings/16th-forum-cape-town-south-africa-29-30-november-2022/ ). As opposed to providing a detailed summary in this paper, we aim to briefly highlight central issues raised, solutions proposed, and the challenges facing the research ethics community in the years to come.
In this way, our primary aim in this paper is to present a synthesis of the challenges and opportunities raised at the GFBR meeting and in the planning process, followed by our reflections as a group of authors on their significance for governance leaders in the coming years. We acknowledge that the views represented at the meeting and in our results are a partial representation of the universe of views on this topic; however, the GFBR leadership invested a great deal of resources in convening a deeply diverse and thoughtful group of researchers and practitioners working on themes of bioethics related to AI for global health including those based in LMICs. We contend that it remains rare to convene such a strong group for an extended time and believe that many of the challenges and opportunities raised demand attention for more ethical futures of AI for health. Nonetheless, our results are primarily descriptive and are thus not explicitly grounded in a normative argument. We make effort in the Discussion section to contextualize our results by describing their significance and connecting them to broader efforts to reform global health research and practice.
Uniquely important ethical issues for AI in global health research
Presentations and group dialogue over the course of the forum raised several issues for consideration, and here we describe four overarching themes for the ethical governance of AI in global health research. Brief descriptions of each issue can be found in Table 1 . Reports referred to throughout the paper are available at the GFBR website provided above.
The first overarching thematic issue relates to the appropriateness of building AI technologies in response to health-related challenges in the first place. Case study presentations referred to initiatives where AI technologies were highly appropriate, such as in ear shape biometric identification to more accurately link electronic health care records to individual patients in Zambia (Alinani Simukanga). Although important ethical issues were raised with respect to privacy, trust, and community engagement in this initiative, the AI-based solution was appropriately matched to the challenge of accurately linking electronic records to specific patient identities. In contrast, forum participants raised questions about the appropriateness of an initiative using AI to improve the quality of handwashing practices in an acute care hospital in India (Niyoshi Shah), which led to gaming the algorithm. Overall, participants acknowledged the dangers of techno-solutionism, in which AI researchers and developers treat AI technologies as the most obvious solutions to problems that in actuality demand much more complex strategies to address [ 24 ]. However, forum participants agreed that RECs in different contexts have differing degrees of power to raise issues of the appropriateness of an AI-based intervention.
The second overarching thematic issue related to whether and how AI-based systems transfer from one national health context to another. One central issue raised by a number of case study presentations related to the challenges of validating an algorithm with data collected in a local environment. For example, one case study presentation described a project that would involve the collection of personally identifiable data for sensitive group identities, such as tribe, clan, or religion, in the jurisdictions involved (South Africa, Nigeria, Tanzania, Uganda and the US; Gakii Masunga). Doing so would enable the team to ensure that those groups were adequately represented in the dataset to ensure the resulting algorithm was not biased against specific community groups when deployed in that context. However, some members of these communities might desire to be represented in the dataset, whereas others might not, illustrating the need to balance autonomy and inclusivity. It was also widely recognized that collecting these data is an immense challenge, particularly when historically oppressive practices have led to a low-trust environment for international organizations and the technologies they produce. It is important to note that in some countries such as South Africa and Rwanda, it is illegal to collect information such as race and tribal identities, re-emphasizing the importance for cultural awareness and avoiding “one size fits all” solutions.
The third overarching thematic issue is related to understanding accountabilities for both the impacts of AI technologies and governance decision-making regarding their use. Where global health research involving AI leads to longer-term harms that might fall outside the usual scope of issues considered by a REC, who is to be held accountable, and how? This question was raised as one that requires much further attention, with law being mixed internationally regarding the mechanisms available to hold researchers, innovators, and their institutions accountable over the longer term. However, it was recognized in breakout group discussion that many jurisdictions are developing strong data protection regimes related specifically to international collaboration for research involving health data. For example, Kenya’s Data Protection Act requires that any internationally funded projects have a local principal investigator who will hold accountability for how data are shared and used [ 25 ]. The issue of research partnerships with commercial entities was raised by many participants in the context of accountability, pointing toward the urgent need for clear principles related to strategies for engagement with commercial technology companies in global health research.
The fourth and final overarching thematic issue raised here is that of consent. The issue of consent was framed by the widely shared recognition that models of individual, explicit consent might not produce a supportive environment for AI innovation that relies on the secondary uses of health-related datasets to build AI algorithms. Given this recognition, approaches such as community oversight of health data uses were suggested as a potential solution. However, the details of implementing such community oversight mechanisms require much further attention, particularly given the unique perspectives on health data in different country settings in global health research. Furthermore, some uses of health data do continue to require consent. One case study of South Africa, Nigeria, Kenya, Ethiopia and Uganda suggested that when health data are shared across borders, individual consent remains necessary when data is transferred from certain countries (Nezerith Cengiz). Broader clarity is necessary to support the ethical governance of health data uses for AI in global health research.
Recommendations for ethical governance of AI in global health research
Dialogue at the forum led to a range of suggestions for promoting ethical conduct of AI research for global health, related to the various roles of actors involved in the governance of AI research broadly defined. The strategies are written for actors we refer to as “governance leaders”, those people distributed throughout the AI for global health research ecosystem who are responsible for ensuring the ethical and socially responsible conduct of global health research involving AI (including researchers themselves). These include RECs, government regulators, health care leaders, health professionals, corporate social accountability officers, and others. Enacting these strategies would bolster the ethical governance of AI for global health more generally, enabling multiple actors to fulfill their roles related to governing research and development activities carried out across multiple organizations, including universities, academic health sciences centers, start-ups, and technology corporations. Specific suggestions are summarized in Table 2 .
First, forum participants suggested that governance leaders including RECs, should remain up to date on recent advances in the regulation of AI for health. Regulation of AI for health advances rapidly and takes on different forms in jurisdictions around the world. RECs play an important role in governance, but only a partial role; it was deemed important for RECs to acknowledge how they fit within a broader governance ecosystem in order to more effectively address the issues within their scope. Not only RECs but organizational leaders responsible for procurement, researchers, and commercial actors should all commit to efforts to remain up to date about the relevant approaches to regulating AI for health care and public health in jurisdictions internationally. In this way, governance can more adequately remain up to date with advances in regulation.
Second, forum participants suggested that governance leaders should focus on ethical governance of health data as a basis for ethical global health AI research. Health data are considered the foundation of AI development, being used to train AI algorithms for various uses [ 26 ]. By focusing on ethical governance of health data generation, sharing, and use, multiple actors will help to build an ethical foundation for AI development among global health researchers.
Third, forum participants believed that governance processes should incorporate AI impact assessments where appropriate. An AI impact assessment is the process of evaluating the potential effects, both positive and negative, of implementing an AI algorithm on individuals, society, and various stakeholders, generally over time frames specified in advance of implementation [ 27 ]. Although not all types of AI research in global health would warrant an AI impact assessment, this is especially relevant for those studies aiming to implement an AI system for intervention into health care or public health. Organizations such as RECs can use AI impact assessments to boost understanding of potential harms at the outset of a research project, encouraging researchers to more deeply consider potential harms in the development of their study.
Fourth, forum participants suggested that governance decisions should incorporate the use of environmental impact assessments, or at least the incorporation of environment values when assessing the potential impact of an AI system. An environmental impact assessment involves evaluating and anticipating the potential environmental effects of a proposed project to inform ethical decision-making that supports sustainability [ 28 ]. Although a relatively new consideration in research ethics conversations [ 29 ], the environmental impact of building technologies is a crucial consideration for the public health commitment to environmental sustainability. Governance leaders can use environmental impact assessments to boost understanding of potential environmental harms linked to AI research projects in global health over both the shorter and longer terms.
Fifth, forum participants suggested that governance leaders should require stronger transparency in the development of AI algorithms in global health research. Transparency was considered essential in the design and development of AI algorithms for global health to ensure ethical and accountable decision-making throughout the process. Furthermore, whether and how researchers have considered the unique contexts into which such algorithms may be deployed can be surfaced through stronger transparency, for example in describing what primary considerations were made at the outset of the project and which stakeholders were consulted along the way. Sharing information about data provenance and methods used in AI development will also enhance the trustworthiness of the AI-based research process.
Sixth, forum participants suggested that governance leaders can encourage or require community engagement at various points throughout an AI project. It was considered that engaging patients and communities is crucial in AI algorithm development to ensure that the technology aligns with community needs and values. However, participants acknowledged that this is not a straightforward process. Effective community engagement requires lengthy commitments to meeting with and hearing from diverse communities in a given setting, and demands a particular set of skills in communication and dialogue that are not possessed by all researchers. Encouraging AI researchers to begin this process early and build long-term partnerships with community members is a promising strategy to deepen community engagement in AI research for global health. One notable recommendation was that research funders have an opportunity to incentivize and enable community engagement with funds dedicated to these activities in AI research in global health.
Seventh, forum participants suggested that governance leaders can encourage researchers to build strong, fair partnerships between institutions and individuals across country settings. In a context of longstanding imbalances in geopolitical and economic power, fair partnerships in global health demand a priori commitments to share benefits related to advances in medical technologies, knowledge, and financial gains. Although enforcement of this point might be beyond the remit of RECs, commentary will encourage researchers to consider stronger, fairer partnerships in global health in the longer term.
Eighth, it became evident that it is necessary to explore new forms of regulatory experimentation given the complexity of regulating a technology of this nature. In addition, the health sector has a series of particularities that make it especially complicated to generate rules that have not been previously tested. Several participants highlighted the desire to promote spaces for experimentation such as regulatory sandboxes or innovation hubs in health. These spaces can have several benefits for addressing issues surrounding the regulation of AI in the health sector, such as: (i) increasing the capacities and knowledge of health authorities about this technology; (ii) identifying the major problems surrounding AI regulation in the health sector; (iii) establishing possibilities for exchange and learning with other authorities; (iv) promoting innovation and entrepreneurship in AI in health; and (vi) identifying the need to regulate AI in this sector and update other existing regulations.
Ninth and finally, forum participants believed that the capabilities of governance leaders need to evolve to better incorporate expertise related to AI in ways that make sense within a given jurisdiction. With respect to RECs, for example, it might not make sense for every REC to recruit a member with expertise in AI methods. Rather, it will make more sense in some jurisdictions to consult with members of the scientific community with expertise in AI when research protocols are submitted that demand such expertise. Furthermore, RECs and other approaches to research governance in jurisdictions around the world will need to evolve in order to adopt the suggestions outlined above, developing processes that apply specifically to the ethical governance of research using AI methods in global health.
Research involving the development and implementation of AI technologies continues to grow in global health, posing important challenges for ethical governance of AI in global health research around the world. In this paper we have summarized insights from the 2022 GFBR, focused specifically on issues in research ethics related to AI for global health research. We summarized four thematic challenges for governance related to AI in global health research and nine suggestions arising from presentations and dialogue at the forum. In this brief discussion section, we present an overarching observation about power imbalances that frames efforts to evolve the role of governance in global health research, and then outline two important opportunity areas as the field develops to meet the challenges of AI in global health research.
Dialogue about power is not unfamiliar in global health, especially given recent contributions exploring what it would mean to de-colonize global health research, funding, and practice [ 30 , 31 ]. Discussions of research ethics applied to AI research in global health contexts are deeply infused with power imbalances. The existing context of global health is one in which high-income countries primarily located in the “Global North” charitably invest in projects taking place primarily in the “Global South” while recouping knowledge, financial, and reputational benefits [ 32 ]. With respect to AI development in particular, recent examples of digital colonialism frame dialogue about global partnerships, raising attention to the role of large commercial entities and global financial capitalism in global health research [ 21 , 22 ]. Furthermore, the power of governance organizations such as RECs to intervene in the process of AI research in global health varies widely around the world, depending on the authorities assigned to them by domestic research governance policies. These observations frame the challenges outlined in our paper, highlighting the difficulties associated with making meaningful change in this field.
Despite these overarching challenges of the global health research context, there are clear strategies for progress in this domain. Firstly, AI innovation is rapidly evolving, which means approaches to the governance of AI for health are rapidly evolving too. Such rapid evolution presents an important opportunity for governance leaders to clarify their vision and influence over AI innovation in global health research, boosting the expertise, structure, and functionality required to meet the demands of research involving AI. Secondly, the research ethics community has strong international ties, linked to a global scholarly community that is committed to sharing insights and best practices around the world. This global community can be leveraged to coordinate efforts to produce advances in the capabilities and authorities of governance leaders to meaningfully govern AI research for global health given the challenges summarized in our paper.
Limitations
Our paper includes two specific limitations that we address explicitly here. First, it is still early in the lifetime of the development of applications of AI for use in global health, and as such, the global community has had limited opportunity to learn from experience. For example, there were many fewer case studies, which detail experiences with the actual implementation of an AI technology, submitted to GFBR 2022 for consideration than was expected. In contrast, there were many more governance reports submitted, which detail the processes and outputs of governance processes that anticipate the development and dissemination of AI technologies. This observation represents both a success and a challenge. It is a success that so many groups are engaging in anticipatory governance of AI technologies, exploring evidence of their likely impacts and governing technologies in novel and well-designed ways. It is a challenge that there is little experience to build upon of the successful implementation of AI technologies in ways that have limited harms while promoting innovation. Further experience with AI technologies in global health will contribute to revising and enhancing the challenges and recommendations we have outlined in our paper.
Second, global trends in the politics and economics of AI technologies are evolving rapidly. Although some nations are advancing detailed policy approaches to regulating AI more generally, including for uses in health care and public health, the impacts of corporate investments in AI and political responses related to governance remain to be seen. The excitement around large language models (LLMs) and large multimodal models (LMMs) has drawn deeper attention to the challenges of regulating AI in any general sense, opening dialogue about health sector-specific regulations. The direction of this global dialogue, strongly linked to high-profile corporate actors and multi-national governance institutions, will strongly influence the development of boundaries around what is possible for the ethical governance of AI for global health. We have written this paper at a point when these developments are proceeding rapidly, and as such, we acknowledge that our recommendations will need updating as the broader field evolves.
Ultimately, coordination and collaboration between many stakeholders in the research ethics ecosystem will be necessary to strengthen the ethical governance of AI in global health research. The 2022 GFBR illustrated several innovations in ethical governance of AI for global health research, as well as several areas in need of urgent attention internationally. This summary is intended to inform international and domestic efforts to strengthen research ethics and support the evolution of governance leadership to meet the demands of AI in global health research.
Data availability
All data and materials analyzed to produce this paper are available on the GFBR website: https://www.gfbr.global/past-meetings/16th-forum-cape-town-south-africa-29-30-november-2022/ .
Clark P, Kim J, Aphinyanaphongs Y, Marketing, Food US. Drug Administration Clearance of Artificial Intelligence and Machine Learning Enabled Software in and as Medical devices: a systematic review. JAMA Netw Open. 2023;6(7):e2321792–2321792.
Article Google Scholar
Potnis KC, Ross JS, Aneja S, Gross CP, Richman IB. Artificial intelligence in breast cancer screening: evaluation of FDA device regulation and future recommendations. JAMA Intern Med. 2022;182(12):1306–12.
Siala H, Wang Y. SHIFTing artificial intelligence to be responsible in healthcare: a systematic review. Soc Sci Med. 2022;296:114782.
Yang X, Chen A, PourNejatian N, Shin HC, Smith KE, Parisien C, et al. A large language model for electronic health records. NPJ Digit Med. 2022;5(1):194.
Meskó B, Topol EJ. The imperative for regulatory oversight of large language models (or generative AI) in healthcare. NPJ Digit Med. 2023;6(1):120.
Jobin A, Ienca M, Vayena E. The global landscape of AI ethics guidelines. Nat Mach Intell. 2019;1(9):389–99.
Minssen T, Vayena E, Cohen IG. The challenges for Regulating Medical Use of ChatGPT and other large Language models. JAMA. 2023.
Ho CWL, Malpani R. Scaling up the research ethics framework for healthcare machine learning as global health ethics and governance. Am J Bioeth. 2022;22(5):36–8.
Yeung K. Recommendation of the council on artificial intelligence (OECD). Int Leg Mater. 2020;59(1):27–34.
Maddox TM, Rumsfeld JS, Payne PR. Questions for artificial intelligence in health care. JAMA. 2019;321(1):31–2.
Dzau VJ, Balatbat CA, Ellaissi WF. Revisiting academic health sciences systems a decade later: discovery to health to population to society. Lancet. 2021;398(10318):2300–4.
Ferretti A, Ienca M, Sheehan M, Blasimme A, Dove ES, Farsides B, et al. Ethics review of big data research: what should stay and what should be reformed? BMC Med Ethics. 2021;22(1):1–13.
Rahimzadeh V, Serpico K, Gelinas L. Institutional review boards need new skills to review data sharing and management plans. Nat Med. 2023;1–3.
Kling S, Singh S, Burgess TL, Nair G. The role of an ethics advisory committee in data science research in sub-saharan Africa. South Afr J Sci. 2023;119(5–6):1–3.
Google Scholar
Cengiz N, Kabanda SM, Esterhuizen TM, Moodley K. Exploring perspectives of research ethics committee members on the governance of big data in sub-saharan Africa. South Afr J Sci. 2023;119(5–6):1–9.
Doerr M, Meeder S. Big health data research and group harm: the scope of IRB review. Ethics Hum Res. 2022;44(4):34–8.
Ballantyne A, Stewart C. Big data and public-private partnerships in healthcare and research: the application of an ethics framework for big data in health and research. Asian Bioeth Rev. 2019;11(3):315–26.
Samuel G, Chubb J, Derrick G. Boundaries between research ethics and ethical research use in artificial intelligence health research. J Empir Res Hum Res Ethics. 2021;16(3):325–37.
Murphy K, Di Ruggiero E, Upshur R, Willison DJ, Malhotra N, Cai JC, et al. Artificial intelligence for good health: a scoping review of the ethics literature. BMC Med Ethics. 2021;22(1):1–17.
Teixeira da Silva JA. Handling ethics dumping and neo-colonial research: from the laboratory to the academic literature. J Bioethical Inq. 2022;19(3):433–43.
Ferryman K. The dangers of data colonialism in precision public health. Glob Policy. 2021;12:90–2.
Couldry N, Mejias UA. Data colonialism: rethinking big data’s relation to the contemporary subject. Telev New Media. 2019;20(4):336–49.
Organization WH. Ethics and governance of artificial intelligence for health: WHO guidance. 2021.
Metcalf J, Moss E. Owning ethics: corporate logics, silicon valley, and the institutionalization of ethics. Soc Res Int Q. 2019;86(2):449–76.
Data Protection Act - OFFICE OF THE DATA PROTECTION COMMISSIONER KENYA [Internet]. 2021 [cited 2023 Sep 30]. https://www.odpc.go.ke/dpa-act/ .
Sharon T, Lucivero F. Introduction to the special theme: the expansion of the health data ecosystem–rethinking data ethics and governance. Big Data & Society. Volume 6. London, England: SAGE Publications Sage UK; 2019. p. 2053951719852969.
Reisman D, Schultz J, Crawford K, Whittaker M. Algorithmic impact assessments: a practical Framework for Public Agency. AI Now. 2018.
Morgan RK. Environmental impact assessment: the state of the art. Impact Assess Proj Apprais. 2012;30(1):5–14.
Samuel G, Richie C. Reimagining research ethics to include environmental sustainability: a principled approach, including a case study of data-driven health research. J Med Ethics. 2023;49(6):428–33.
Kwete X, Tang K, Chen L, Ren R, Chen Q, Wu Z, et al. Decolonizing global health: what should be the target of this movement and where does it lead us? Glob Health Res Policy. 2022;7(1):3.
Abimbola S, Asthana S, Montenegro C, Guinto RR, Jumbam DT, Louskieter L, et al. Addressing power asymmetries in global health: imperatives in the wake of the COVID-19 pandemic. PLoS Med. 2021;18(4):e1003604.
Benatar S. Politics, power, poverty and global health: systems and frames. Int J Health Policy Manag. 2016;5(10):599.
Download references
Acknowledgements
We would like to acknowledge the outstanding contributions of the attendees of GFBR 2022 in Cape Town, South Africa. This paper is authored by members of the GFBR 2022 Planning Committee. We would like to acknowledge additional members Tamra Lysaght, National University of Singapore, and Niresh Bhagwandin, South African Medical Research Council, for their input during the planning stages and as reviewers of the applications to attend the Forum.
This work was supported by Wellcome [222525/Z/21/Z], the US National Institutes of Health, the UK Medical Research Council (part of UK Research and Innovation), and the South African Medical Research Council through funding to the Global Forum on Bioethics in Research.
Author information
Authors and affiliations.
Department of Physical Therapy, Temerty Faculty of Medicine, University of Toronto, Toronto, Canada
Berman Institute of Bioethics, Johns Hopkins University, Baltimore, MD, USA
Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD, USA
Department of Philosophy and Classics, University of Ghana, Legon-Accra, Ghana
Caesar A. Atuire
Centre for Tropical Medicine and Global Health, Nuffield Department of Medicine, University of Oxford, Oxford, UK
Mahidol Oxford Tropical Medicine Research Unit, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand
Phaik Yeong Cheah
Berkman Klein Center, Harvard University, Bogotá, Colombia
Armando Guio Español
Department of Radiology and Informatics, Emory University School of Medicine, Atlanta, GA, USA
Judy Wawira Gichoya
Health Ethics & Governance Unit, Research for Health Department, Science Division, World Health Organization, Geneva, Switzerland
Adrienne Hunt & Katherine Littler
African Center of Excellence in Bioinformatics and Data Intensive Science, Infectious Diseases Institute, Makerere University, Kampala, Uganda
Daudi Jjingo
ISI Foundation, Turin, Italy
Daniela Paolotti
Department of Health Sciences and Technology, ETH Zurich, Zürich, Switzerland
Effy Vayena
Joint Centre for Bioethics, Dalla Lana School of Public Health, University of Toronto, Toronto, Canada
You can also search for this author in PubMed Google Scholar
Contributions
JS led the writing, contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. JA contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. CA contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. PYC contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. AE contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. JWG contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. AH contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. DJ contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. KL contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. DP contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. EV contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper.
Corresponding author
Correspondence to James Shaw .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Shaw, J., Ali, J., Atuire, C.A. et al. Research ethics and artificial intelligence for global health: perspectives from the global forum on bioethics in research. BMC Med Ethics 25 , 46 (2024). https://doi.org/10.1186/s12910-024-01044-w
Download citation
Received : 31 October 2023
Accepted : 01 April 2024
Published : 18 April 2024
DOI : https://doi.org/10.1186/s12910-024-01044-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Artificial intelligence
- Machine learning
- Research ethics
- Global health
BMC Medical Ethics
ISSN: 1472-6939
- General enquiries: [email protected]

Health & Environmental Research Online (HERO)
- Learn about HERO
- Search HERO
- Projects in HERO
- Risk Assessment
- Transparency & Integrity
Environmental Pollution in the Moscow Region According to Long-term Roshydromet Monitoring Data
- Published: 02 November 2020
- Volume 45 , pages 523–532, ( 2020 )
Cite this article

- G. M. Chernogaeva 1 , 2 ,
- L. R. Zhuravleva 1 ,
- Yu. A. Malevanov 1 ,
- N. A. Fursov 3 ,
- G. V. Pleshakova 3 &
- T. B. Trifilenkova 3
113 Accesses
Explore all metrics
Long-term Roshydromet monitoring data (2009–2018) on the pollution of the atmosphere, soil, and surface water are considered for the Moscow region (Moscow city within its new boundaries and the Moscow oblast). The air quality in the megacity (Moscow) and in background conditions (Prioksko-Terrasny Reserve) is compared.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Similar content being viewed by others

Air Quality in Russian Cities for 1991–2016

Spatial and temporal look at ten-years air quality of Istanbul city

Author information
Authors and affiliations.
Izrael Institute of Global Climate and Ecology, 107258, Moscow, Russia
G. M. Chernogaeva, L. R. Zhuravleva & Yu. A. Malevanov
Institute of Geography, Russian Academy of Sciences, 119017, Moscow, Russia
G. M. Chernogaeva
Central Administration for Hydrometeorology and Environmental Monitoring, 127055, Moscow, Russia
N. A. Fursov, G. V. Pleshakova & T. B. Trifilenkova
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to G. M. Chernogaeva .
Additional information
Russian Text ©The Author(s), 2020, published in Meteorologiya i Gidrologiya, 2020, No. 8, pp. 9-21.
About this article
Chernogaeva, G.M., Zhuravleva, L.R., Malevanov, Y.A. et al. Environmental Pollution in the Moscow Region According to Long-term Roshydromet Monitoring Data . Russ. Meteorol. Hydrol. 45 , 523–532 (2020). https://doi.org/10.3103/S1068373920080014
Download citation
Received : 06 February 2020
Revised : 06 February 2020
Accepted : 06 February 2020
Published : 02 November 2020
Issue Date : August 2020
DOI : https://doi.org/10.3103/S1068373920080014
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Anthropogenic environmental pollution
- Surface water
- Urbanized areas
- Background conditions
- Find a journal
- Publish with us
- Track your research
New Select Subcommittee Report Recommends EcoHealth Alliance President Debarred and Criminally Investigated, Exposes Failures in NIH Grant Procedures
WASHINGTON — Today, Select Subcommittee on the Coronavirus Pandemic Chairman Brad Wenstrup (R-Ohio) issued an interim staff report titled “ An Evaluation of the Evidence Surrounding EcoHealth Alliance, Inc.’s Research Activities ”. This report details the Select Subcommittee’s comprehensive investigation into the U.S. government’s funding and lack of oversight of gain-of-function research, EcoHealth Alliance (EcoHealth), and the Wuhan Institute of Virology (WIV). The report reveals serious, systemic weaknesses in the National Institute of Allergy and Infectious Diseases (NIAID) and National Institutes of Health’s (NIH) grant procedures and examines how these failures enabled EcoHealth President Dr. Peter Daszak to fund dangerous gain-of-function research in Wuhan, China without sufficient oversight.
Overwhelming primary source documents and credible firsthand testimony gathered throughout the Select Subcommittee’s investigation provide significant evidence that Dr. Daszak repeatedly violated the terms of the NIH grant awarded to EcoHealth. Given Dr. Daszak’s apparent contempt for the American people and disregard for legal reporting requirements the Select Subcommittee recommends the formal debarment of and a criminal investigation into EcoHealth and its President. In addition, as a result of NIH’s inadequate oversight of American taxpayer funds, the Select Subcommittee is also recommending immediate Congressional action to improve grant procedures at NIH and NIAID.
“ EcoHealth Alliance President Dr. Peter Daszak is not a good steward of U.S. taxpayer dollars and should never again receive funding from the U.S. taxpayer. Dr. Daszak and his organization conducted dangerous gain-of-function research at the WIV, willfully violated the terms of a multi-million-dollar NIH grant, and placed U.S. national security at risk. This blatant contempt for the American people is reprehensible. It is imperative to establish higher standards of oversight at the NIH. The Select Subcommittee’s detailed and comprehensive report today holds Dr. Daszak and EcoHealth Alliance accountable and sheds light on severe shortcomings in our public health systems ,” said Chairman Wenstrup .
Key Report Recommendations
- The Select Subcommittee on the Coronavirus Pandemic recommends that EcoHealth Alliance and Dr. Peter Daszak are formally debarred and cut off from receiving any future U.S. taxpayer funding.
- The Select Subcommittee also recommends that the U.S. Department of Justice conduct a formal investigation into Dr. Daszak.
- Further, the Select Subcommittee recommends eight improvements to NIAID and NIH procedures that will improve grant compliance, increase biosafety and biosecurity of high-risk research, and advance transparency and accountability in America’s federal health agencies.
- Evidence obtained by the Select Subcommittee through document requests and transcribed interviews — including with former NIH Director Lawrence Tabak — confirms that EcoHealth facilitated gain-of-function research at the WIV during the fifth year it received funding from the NIH.
- Dr. Daszak, Dr. Fauci, and other health leaders have repeatedly played semantics with the long standing, widely understood definition of “gain-of-function” in order to avoid accountability for funding and facilitating this dangerous research.
- Notably, the NIH removed the longstanding definition of “gain-of-function” from its website on the same day that former NIH Director Tabak reported EcoHealth’s dangerous experiments to Congress.
- EcoHealth Alliance was required to immediately report any gain-of-function experiment that exhibited greater than “one log growth” — meaning a virus was modified to be 10 times more infectious.
- Evidence shows that Dr. Daszak was aware of an experiment conducted with EcoHealth Alliance funding at the Wuhan Institute of Virology that exhibited this potentially dangerous “one log growth” characteristic, yet he failed to report the experiment to NIH.
- EcoHealth was awarded five years of funding by the NIH to conduct research aimed at preventing pandemics. In the fifth year of receiving these funds — which concerningly coincides with the time period immediately preceding the COVID-19 pandemic — EcoHealth failed to submit its annual research update report to NIH before the required deadline.
- NIH finally received the report from EcoHealth in August 2021, nearly two years after the September 2019 deadline.
- Dr. Fauci and former NIH Director Lawrence Tabak testified that Mark Meadows — Chief of Staff to then President Donald Trump — instructed the NIH to terminate EcoHealth’s grant after the Trump Administration discovered significant malfeasance.
- The NIH official in charge of grant compliance testified he was unaware of any problems with either EcoHealth or its grant to the WIV prior to the Trump Administration’s intervention.
- Despite suggestions of political persecution against EcoHealth, NIH leadership supported every compliance action recommended by the Trump Administration after the malfeasance was discovered.
- NIH reinstated EcoHealth’s problematic grant in 2023 — in part because Dr. Daszak claimed to be in possession of virus sequences and samples that had not yet been tested and were previously paid for by the federal government.
- When Dr. Daszak applied for grant reinstatement, he omitted the material fact that the unanalyzed samples and sequences were not in his custody, but instead, are in the custody and control of the WIV.
- The terms of the WIV’s debarment not only prohibit EcoHealth from funding the lab but also prohibit the lab from influencing any activity that is funded by the U.S. taxpayer.
- Since the untested samples remain at the WIV and are used to influence EcoHealth’s research, NIH’s funding of EcoHealth subsequently violates the WIV’s formal debarment.
Read the final report here , excerpts from select transcribed interviews here , and supporting materials here .
Transcribed interviews with Dr. Daszak and other individuals influential to the findings of the report can be found below:
- Dr. Lawrence Tabak
- Dr. Michael Lauer
- Dr. David Morens (Part 1)
- Dr. David Morens (Part 2)
- Dr. Emily Erbelding
- Dr. Erik Stemmy
- Dr. Peter Daszak
- Dr. Ralph Baric

IMAGES
VIDEO
COMMENTS
environmental health. ... Research Open Access 26 Apr 2024 Scientific Reports. Volume: 14, P: 9653. ... Research Open Access 24 Apr 2024 npj Climate and Atmospheric Science. Volume: 7, P: 94 ...
If you are giving a presentation about an environmental health topic or just looking for general information about environmental health research or the institute, this webpage will help. ... NIEHS is pleased to join with other NIH Institutes and Centers to release the first NIH Climate Change and Health Initiative Annual Report. Read about the ...
Abstract. Experts recommend reporting environmental exposure results back to research participants and communities, yet environmental health researchers need further guidance to improve the practice of reporting back. We present the results of a workshop developed to identify pertinent issues and areas for action in reporting back environmental ...
Background: The practice of reporting back individual results to participants in environmental health research has evolved significantly over the past 20 years. Research findings support the potential of report-back to enhance the ethics, quality, and impact of environmental health research. Nonetheless, implementation of environmental health report-back practices is not yet routine ...
The Lancet Commission on pollution and health reported that pollution was responsible for 9 million premature deaths in 2015, making it the world's largest environmental risk factor for disease and premature death. We have now updated this estimate using data from the Global Burden of Diseases, Injuriaes, and Risk Factors Study 2019. We find that pollution remains responsible for approximately ...
Current Environmental Health Reports provides in a systematic manner, the views of experts on the current advances in the environmental health field in a clear and readable form, and by providing reviews which highlight the most important papers recently published from the wealth of original publications. The coverage extends to a broad range ...
Environmental health sciences have identified and characterized a range of environmental exposures and their associated risk for disease, as well as informed the development of interventions, including recommendations, guidelines, and policies for mitigating exposure. However, these interventions only serve to mitigate exposures and prevent disease if they are effectively disseminated, adopted ...
Prenatal Exposure to Nitrate in Drinking Water and Adverse Health Outcomes in the Offspring: a Review of Current Epidemiological Research. Pernille Jul Clemmensen. Jörg Schullehner. Cecilia Høst Ramlau-Hansen. ReviewPaper Open access 16 July 2023 Pages: 250 - 263.
NIEHS Reports. Much of the work carried out by DTT is in support of the National Toxicology Program (NTP), an interagency partnership of the Food and Drug Administration, National Institute for Occupational Safety and Health, and NIEHS. These reports describe innovative toxicology research conducted to better understand the effects of ...
Background: The practice of reporting back individual results to participants in environmental health research has evolved significantly over the past 20 years. Research findings support the potential of report-back to enhance the ethics, quality, and impact of environmental health research. Nonetheless, implementation of environmental health ...
Affiliations 1 HERCULES Exposome Research Center, Rollins School of Public Health, Emory University, Atlanta, GA 30322, USA.; 2 Institute for the Environment, UNC Superfund Research Program, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA.; 3 Department of Occupational and Environmental Health, University of Iowa, Iowa City, IA 52246, USA.
Purpose of Review Data science is an exploding trans-disciplinary field that aims to harness the power of data to gain information or insights on researcher-defined topics of interest. In this paper, we review how data science can help advance environmental health research. Recent Findings We discuss the concepts of computationally scalable handling of big data and the design of efficient ...
Our researchers conduct human health risk assessments to estimate the nature and probability of adverse health effects in humans who may be exposed to chemicals in the environment. EPA's Health and Environmental Risk Assessment Research Program is designed to develop and apply state-of-the-science research to characterize the impacts on human ...
What could the future of environmental health sciences hold, and what steps might be taken now to guide the field's trajectory? To envision a future research enterprise that integrates environmental health sciences, biomedical science, prevention research, and disease-specific research across the continuum from fundamental discovery research through the application of this research to ...
EHP Research Articles. EHP. Research Articles. Research articles report original research results that are relevant to the relationship between the environment and human health, and that make a substantial advance in the field. EHP strongly recommends that authors consult the following reporting guidelines while drafting manuscripts:
ASTHO administered the 2023 Environmental Scan survey to SHOs between April and June 2023. In total, 42 states and Washington, D.C. have at least one plan included in the findings for this section of the report. Maternal, child, and family health is a priority area in 60% of states with a SHIP and/or strategic plan included in the Scan and was ...
Through the NIH Climate Change and Health Initiative launched in 2022, NIH is taking action to expand research funding and support to address these urgent and complex problems. As the climate continues to change, and weather-related events such as floods, hurricanes, wildfires, and heat waves become more extreme, the risk to human health grows ...
RESEARCH LETTERS Research Letters present brief original research reports that make a substantial advance in understanding the relationship between the environment and human health. Manuscripts that exceed the specified limits below for length, tables, or figures should be submitted as Research articles. Research Letters are subject to peer review.
A member of the Louisiana State University (LSU) Superfund Research Program (SRP) Center, Lomnicki spearheads a project focused on contaminants called environmentally persistent free radicals (EPFRs). These contaminants can be found in the air and soil around Superfund sites, especially where hazardous waste is disposed of through burning.
Climate change is already having serious impacts on the safety and health of workers in all regions of the world. Workers are among those most exposed to climate change hazards yet frequently have no choice but to continue working, even if conditions are dangerous. Global occupational safety and health (OSH) protections have struggled to keep up with the evolving risks from climate change ...
Ed Jones/AFP via Getty Images. Over one-third of Americans, or about 130 million people, routinely breathe in unhealthy air, according to the newest State of the Air report from the American Lung ...
Environmental assessment and recommendations to patients vary considerably among asthma care providers, according to NIEHS researchers and their collaborators. A higher percentage of specialists assessed asthma triggers at home, school, or work than primary care or advanced practice providers. However, 46%-76% of clinicians, depending on ...
Kevin Loria is a senior reporter covering health and science at Consumer Reports. He has been with CR since 2018, covering environmental health, food safety, infectious disease, fitness, and more.
The ethical governance of Artificial Intelligence (AI) in health care and public health continues to be an urgent issue for attention in policy, research, and practice. In this paper we report on central themes related to challenges and strategies for promoting ethics in research involving AI in global health, arising from the Global Forum on Bioethics in Research (GFBR), held in Cape Town ...
Health & Environmental Research Online (HERO) ... 5099094 Reference Type. Technical Report Title. Industrywide studies report of walk-through survey of the Kendall Company, U.S. 31, W. North, Franklin, Kentucky 42134 Author(s) Greife, A; Stayner, L Year. 1985 Publisher. National Institute for Occupational Safety and Health Location. Cincinnati ...
5 Report—the report that included the results of research and experiments for June 2018 through May 2019, the time period immediately preceding the outbreak of the COVID-19 pandemic— was due September 30, 2019. However, EcoHealth submitted this report nearly two years later on August 3, 2021.
The present study analyzes the chemical pollution of the atmosphere, precipitation, soil, and surface water in urbanized and background areas of the Moscow region based on long-term Roshydromet monitoring data which are provided in detail in the information materials by the Central Administration for Hydrometeorology and Environmental Monitoring (Central AHEM) and Izrael Institute of Global ...
The report reveals serious, systemic weaknesses in the National Institute of Allergy and Infectious Diseases (NIAID) and National Institutes of Health's (NIH) grant procedures and examines how these failures enabled EcoHealth President Dr. Peter Daszak to fund dangerous gain-of-function research in Wuhan, China without sufficient oversight.
Report-back of environmental health research results is an important foundation of community engagement in research and public support for science. Environmental health research often informs individual, community, organizational, and policy-level action. In this commentary, we have described some of the past experience and research that has ...