

Lymph Info Trust
The Lymph Info Trust exists to improve the quality of life of anyone in New Zealand who has a lymphatic condition. We aim to do this through education and raising awareness. We empower New Zealanders who are living with:
- lymphoedema
- lipoedema, and
- phlebolymphoedema.
We provide understandable information, education and resources. We do this to help your understanding of oedema and its treatments.

Swelling (Oedema / Edema)
Oedema is more related to visible symptoms (swelling) and primarily associated with lymphoedema. It may also be known as:
- fluid retention
Symptoms and treatment will vary depending on the cause of the swelling.
Swollen Ankles and Feet During Pregnancy
In late pregnancy, the weight of the uterus can press down on the veins of the pelvis resulting in swollen legs and ankles. This swelling should clear up after giving birth. Even though it is not a cause for concern, please discuss any swelling with your doctor or lead maternity carer (midwife).
Lymphoedema (Chronic Oedema)

Primary Lymphoedema
Primary lymphoedema is congenital. That is, some people are born with this condition. There is a strong link between genetics, family history and hormonal milestones. Symptoms typically develop during the teenage years.
Secondary Lymphoedema
Secondary lymphoedema occurs when the lymphatic system is damaged. The lymphatic system can be damaged as a result of:
- radiation therapy
- infection, or
- a blockage caused by a tumour.

Lipoedema is a condition where fat (lipids) are deposited over the lower part of the body; from the hips to the ankles of both legs, but generally not the waist, nor the feet.
Phlebolymphoedema

Phlebolymphoedema is the accumulation of excess intercellular/interstitial fluid in the legs and feet, resulting from the combined conditions of phlebodoema and lymphoedema.
Phlebogenic oedema is called phleboedema.
Lymphogenic oedema is called lymphoedema.
To put it simply, phleboedema + lymphoedema = phlebolymphoedema.
Phlebolymphoedema is the inevitable failure of the:
- venous circulation system, and This is an interconnected system of veins and sinuses.
- lymphatic circulation system. This is the system that circulates a clear fluid called 'lymph' back into your bloodstream.
Both systems work together to remove used blood from tissue. If one system fails, the other will also fail.
Lymphatic Filiarisis
Lymphatic Filiarisis, also known as Elephantiasis, is a secondary lymphoedema. It is common around the tropical and sub-tropical regions. The cause of Lymphatic Filiarisis is a mosquito-born parasitic worm. This worm is not present in New Zealand. It can affect both men and women, and the symptoms include swelling of the scrotum, legs or breasts.
Medication-Induced Oedema
Some medicines can cause oedema. Talk to your doctor about the possible side effects of any medications you are on. The following medications are known to contribute to oedema.
- Medications with high levels of sodium and sodium bicarbonate, e.g., antibiotics These can cause sodium overload / retention.
- NSAIDs, anti-hypertensives, and anticancer drugs These drugs may exacerbate any pre-existing renal dysfunction in patients and cause oedema.
- Calcium antagonists, insulin, etc These increase vascular permeability and contribute to hyper-permeability.
Disclaimer: Please note, this website does not provide medical advice. It is for informational purposes only and not intended to be a substitute for professional medical advice, diagnosis or treatment. You should always seek the advice of your doctor or other qualified health professional.

Donate via PayPal
You will be redirected to PayPal to make payment.

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 21 October 2021
Primary lymphoedema
- Pascal Brouillard 1 ,
- Marlys H. Witte ORCID: orcid.org/0000-0001-5505-934X 2 ,
- Robert P. Erickson 3 ,
- Robert J. Damstra 4 ,
- Corinne Becker 5 ,
- Isabelle Quéré ORCID: orcid.org/0000-0002-1492-9764 6 &
- Miikka Vikkula ORCID: orcid.org/0000-0002-6236-338X 1 , 7 , 8
Nature Reviews Disease Primers volume 7 , Article number: 77 ( 2021 ) Cite this article
3949 Accesses
45 Citations
52 Altmetric
Metrics details
- Disease genetics
- Vascular diseases
Lymphoedema is the swelling of one or several parts of the body owing to lymph accumulation in the extracellular space. It is often chronic, worsens if untreated, predisposes to infections and causes an important reduction in quality of life. Primary lymphoedema (PLE) is thought to result from abnormal development and/or functioning of the lymphatic system, can present in isolation or as part of a syndrome, and can be present at birth or develop later in life. Mutations in numerous genes involved in the initial formation of lymphatic vessels (including valves) as well as in the growth and expansion of the lymphatic system and associated pathways have been identified in syndromic and non-syndromic forms of PLE. Thus, the current hypothesis is that most cases of PLE have a genetic origin, although a causative mutation is identified in only about one-third of affected individuals. Diagnosis relies on clinical presentation, imaging of the structure and functionality of the lymphatics, and in genetic analyses. Management aims at reducing or preventing swelling by compression therapy (with manual drainage, exercise and compressive garments) and, in carefully selected cases, by various surgical techniques. Individuals with PLE often have a reduced quality of life owing to the psychosocial and lifelong management burden associated with their chronic condition. Improved understanding of the underlying genetic origins of PLE will translate into more accurate diagnosis and prognosis and personalized treatment.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
We are sorry, but there is no personal subscription option available for your country.
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others

The Ehlers–Danlos syndromes

Lower extremity lymphatic function predicted by body mass index: a lymphoscintigraphic study of obesity and lipedema

The impact of obesity on chronic oedema/lymphoedema of the leg – an international multicenter cross-sectional study (LIMPRINT)
Starling, E. H. On the absorption of fluids from the connective tissue spaces. J. Physiol. 19 , 312–326 (1896).
CAS PubMed PubMed Central Google Scholar
Levick, J. R. & Michel, C. C. Microvascular fluid exchange and the revised Starling principle. Cardiovasc. Res. 87 , 198–210 (2010).
CAS PubMed Google Scholar
Quere, I., Nagot, N. & Vikkula, M. Incidence of cellulitis among children with primary lymphedema. N. Engl. J. Med. 378 , 2047–2048 (2018).
PubMed Google Scholar
Moffatt, C. J. et al. Prevalence and risk factors for chronic edema in U.K. community nursing services. Lymphat. Res. Biol. 17 , 147–154 (2019).
PubMed PubMed Central Google Scholar
Moffatt, C. J. et al. Lymphoedema: an underestimated health problem. QJM 96 , 731–738 (2003).
Moffatt, C., Keeley, V. & Quere, I. The concept of chronic edema — a neglected public health issue and an international response: The LIMPRINT Study. Lymphat. Res. Biol. 17 , 121–126 (2019).
Rockson, S. G. & Rivera, K. K. Estimating the population burden of lymphedema. Ann. N. Y. Acad. Sci. 1131 , 147–154 (2008).
Keast, D. H., Despatis, M., Allen, J. O. & Brassard, A. Chronic oedema/lymphoedema: under-recognised and under-treated. Int. Wound J. 12 , 328–333 (2015).
DiSipio, T., Rye, S., Newman, B. & Hayes, S. Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol. 14 , 500–515 (2013).
Mortimer, P. S. & Rockson, S. G. New developments in clinical aspects of lymphatic disease. J. Clin. Invest. 124 , 915–921 (2014).
Rockson, S. G., Keeley, V., Kilbreath, S., Szuba, A. & Towers, A. Cancer-associated secondary lymphoedema. Nat. Rev. Dis. Prim. 5 , 22 (2019). This recent detailed review explores various aspects of secondary lymphoedema, which, in developed countries, mostly results from the treatment of cancer as opposed to infection-related secondary lymphoedema in developing countries.
Mercier, G., Pastor, J., Moffatt, C., Franks, P. & Quere, I. LIMPRINT: health-related quality of life in adult patients with chronic edema. Lymphat. Res. Biol. 17 , 163–167 (2019). This large multicentre study prospectively assessed the health-related quality of life of 1,094 adult patients with chronic oedema and underscored a poor disease-specific and generic health-related quality of life.
Lopez, M., Roberson, M. L., Strassle, P. D. & Ogunleye, A. Epidemiology of lymphedema-related admissions in the United States: 2012–2017. Surg. Oncol. 35 , 249–253 (2020).
Biesecker, L. G. et al. A dyadic approach to the delineation of diagnostic entities in clinical genomics. Am. J. Hum. Genet. 108 , 8–15 (2021).
Gordon, K. et al. Update and audit of the St George’s classification algorithm of primary lymphatic anomalies: a clinical and molecular approach to diagnosis. J. Med. Genet. 57 , 653–659 (2020). This review proposes an updated clinical classification algorithm for primary lymphoedema to assist diagnostic workup and patient management, based on age of onset, areas affected by swelling and associated clinical features, in agreement with the International Society for the Study of Vascular Anomalies 2018 classification.
Nonne, M. & Vier Fälle, V. Elephantiasis congenita hereditarian. Arch. für pathologische anatomie und physiologie und für klinische Med. 125 , 189–196 (1891).
Google Scholar
Milroy, W. F. An undescribed variety of hereditary oedema. N. Y. Med. J. 56 , 505–508 (1892).
Samman, P. D. & White, W. F. The “yellow nail” syndrome. Br. J. Dermatol. 76 , 153–157 (1964).
Meige, H. Distrophie oedemateuse héréditaire. Presse Méd. 6 , 341–343 (1898).
Irrthum, A., Karkkainen, M. J., Devriendt, K., Alitalo, K. & Vikkula, M. Congenital hereditary lymphedema caused by a mutation that inactivates VEGFR3 tyrosine kinase. Am. J. Hum. Genet. 67 , 295–301 (2000).
Karkkainen, M. J. et al. Missense mutations interfere with VEGFR-3 signalling in primary lymphoedema. Nat. Genet. 25 , 153–159 (2000).
Mendola, A. et al. Mutations in the VEGFR3 signaling pathway explain 36% of familial lymphedema. Mol. Syndromol. 4 , 257–266 (2013).
Leppanen, V. M. et al. Characterization of ANGPT2 mutations associated with primary lymphedema. Sci. Transl Med. 12 , eaax8013 (2020). This is the most recent discovery of a novel gene causing primary lymphoedema with functional validation of the mutations in vitro and in a mouse model, underscoring the heterogeneity within genetic causes of PLE .
Iacobas, I. et al. Multidisciplinary guidelines for initial evaluation of complicated lymphatic anomalies-expert opinion consensus. Pediatr. Blood Cancer 67 , e28036 (2020).
Quinn, A. M., Valcarcel, B. N., Makhamreh, M. M., Al-Kouatly, H. B. & Berger, S. I. A systematic review of monogenic etiologies of nonimmune hydrops fetalis. Genet. Med. 23 , 3–12 (2021). This systematic literature review of non-immune hydrops fetalis pinpointed 131 genes with strong evidence for an association with NIHF and 46 genes with emerging evidence, spanning the spectrum of multisystemic syndromes and cardiac, haematological and metabolic disorders.
Smeltzer, D. M., Stickler, G. B. & Schirger, A. Primary lymphedema in children and adolescents: a follow-up study and review. Pediatrics 76 , 206–218 (1985).
Schook, C. C. et al. Primary lymphedema: clinical features and management in 138 pediatric patients. Plast. Reconstr. Surg. 127 , 2419–2431 (2011).
Fastre, E. et al. Splice-site mutations in VEGFC cause loss of function and Nonne-Milroy-like primary lymphedema. Clin. Genet. 94 , 179–181 (2018).
Erickson, R. P. et al. Sex-limited penetrance of lymphedema to females with CELSR1 haploinsufficiency: a second family. Clin. Genet. 96 , 478–482 (2019).
Soo, J. K., Bicanic, T. A., Heenan, S. & Mortimer, P. S. Lymphatic abnormalities demonstrated by lymphoscintigraphy after lower limb cellulitis. Br. J. Dermatol. 158 , 1350–1353 (2008).
Au, A. C. et al. Protein tyrosine phosphatase PTPN14 is a regulator of lymphatic function and choanal development in humans. Am. J. Hum. Genet. 87 , 436–444 (2010).
Hong, S. E. et al. Autosomal recessive lissencephaly with cerebellar hypoplasia is associated with human RELN mutations. Nat. Genet. 26 , 93–96 (2000).
Brice, G. et al. A novel mutation in GJA1 causing oculodentodigital syndrome and primary lymphoedema in a three generation family. Clin. Genet. 84 , 378–381 (2013).
Gumus, E. A rare symptom of a very rare disease: a case report of a oculodentodigital dysplasia with lymphedema. Clin. Dysmorphol. 27 , 91–93 (2018).
Schlogel, M. J. et al. No evidence of locus heterogeneity in familial microcephaly with or without chorioretinopathy, lymphedema, or mental retardation syndrome. Orphanet J. Rare Dis. 10 , 52 (2015).
Commission, E. U. Useful Information on Rare Diseases from EU Perspective . C 151/157–C 151/110 (European Commission 2009).
Park, S. I. et al. Prevalence and epidemiological factors involved in cellulitis in Korean patients with lymphedema. Ann. Rehabil. Med. 40 , 326–333 (2016).
Aslam, A. F., Aslam, A. K., Qamar, M. U. & Levey, R. Primary lymphedema tarda in an 88-year-old African-American male. J. Natl Med. Assoc. 97 , 1031–1035 (2005).
Ibrahim, A. Primary lymphedema tarda. Pan Afr. Med. J. 19 , 16 (2014).
Davey, S. L. et al. The South African multi-disciplinary lymphoedema position statement. Wound Healing South. Afr. 11 , 21–24 (2018).
Julkowska, D. et al. The importance of international collaboration for rare diseases research: a European perspective. Gene Ther. 24 , 562–571 (2017).
Vignes, S. et al. Primary lymphedema French National Diagnosis and Care Protocol (PNDS; Protocole National de Diagnostic et de Soins). Orphanet J. Rare Dis. 16 , 18 (2021).
Nedergaard, M. & Goldman, S. A. Glymphatic failure as a final common pathway to dementia. Science 370 , 50–56 (2020).
Proulx, S. T. Cerebrospinal fluid outflow: a review of the historical and contemporary evidence for arachnoid villi, perineural routes, and dural lymphatics. Cell Mol. Life Sci. 78 , 2429–2457 (2021).
Witte, M. & Bernas, M. in Rutherford’s Vascular Surgery and Endovascular Therapy (eds Sidaway, A. & Perler, B.) Ch. 10, 105–122 (Elsevier, 2019).
Itkin, M. et al. Research priorities in lymphatic interventions: recommendations from a multidisciplinary research consensus panel. J. Vasc. Interv. Radiol. 32 , 762.e1–762.e7 (2021). This document, by a selected panel of experts in lymphatic medicine from the USA, New Zealand and Korea, identified seven priorities for research in the field, including lymphatic decompression in patients with congestive heart failure, detoxification of thoracic duct lymph in acute illness, development of newer agents for lymphatic imaging, characterization of organ-based lymph composition, and development of lymphatic interventions to treat ascites in liver cirrhosis.
Schwartz, F. R. et al. Lymphatic imaging: current noninvasive and invasive techniques. Semin. Intervent. Radiol. 37 , 237–249 (2020).
Kinmonth, J. B. in The Lymphatic: Disease, Lymphography, and Surgery 114–155 (Edward Arnold, 1972).
Witte, M. H. et al. Structure function relationships in the lymphatic system and implications for cancer biology. Cancer Metastasis Rev. 25 , 159–184 (2006).
Földi, M. & Földi, E. in Földi’s Textbook of Lymphology (eds Földi, M. & Földi, E.) Ch. 2, 135–273 (Urban & Fischer Verlag, 2012).
Executive Committee.The diagnosis and treatment of peripheral lymphedema: 2016 consensus document of the international society of lymphology. Lymphology 49 , 170–184 (2016).
Witte, M. H., Dumont, A. E., Cole, W. R., Witte, C. L. & Kintner, K. Lymph circulation in hepatic cirrhosis: effect of portacaval shunt. Ann. Intern. Med. 70 , 303–310 (1969).
Baish, J. W., Netti, P. A. & Jain, R. K. Transmural coupling of fluid flow in microcirculatory network and interstitium in tumors. Microvasc. Res. 53 , 128–141 (1997).
Michel, C. C., Woodcock, T. E. & Curry, F. E. Understanding and extending the Starling principle. Acta Anaesthesiol. Scand. 64 , 1032–1037 (2020).
Lee, B. B. et al. Diagnosis and treatment of primary lymphedema. Consensus document of the International Union of Phlebology (IUP)-2013. Int. Angiol. 32 , 541–574 (2013).
Baluk, P. et al. Functionally specialized junctions between endothelial cells of lymphatic vessels. J. Exp. Med. 204 , 2349–2362 (2007).
Nonomura, K. et al. Mechanically activated ion channel PIEZO1 is required for lymphatic valve formation. Proc. Natl Acad. Sci. USA 115 , 12817–12822 (2018).
Teijeira, A. et al. Lymphatic endothelium forms integrin-engaging 3D structures during DC transit across inflamed lymphatic vessels. J. Invest. Dermatol. 133 , 2276–2285 (2013).
Johnson, L. A. et al. Dendritic cells enter lymph vessels by hyaluronan-mediated docking to the endothelial receptor LYVE-1. Nat. Immunol. 18 , 762–770 (2017).
Executive Committee.The diagnosis and treatment of peripheral lymphedema: 2020 Consensus Document of the International Society of Lymphology. Lymphology 53 , 3–19 (2020). This recent document integrates the broad spectrum of protocols and practices advocated around the world for the diagnosis and treatment of peripheral lymphoedema. It provides a current “Consensus view” of the international community based on various levels of evidence.
Witte, M. H. et al. Phenotypic and genotypic heterogeneity in familial Milroy lymphedema. Lymphology 31 , 145–155 (1998).
Witte, C. L. et al. Advances in imaging of lymph flow disorders. Radiographics 20 , 1697–1719 (2000).
Campisi, C., Boccardo, F., Witte, M. H. & Bernas, M. in Venous and Lymphatic Diseases (eds Dieter, R. S. Jr & Dieter, R. A. III) Ch. 42, 607–629 (McGraw Hill, 2011).
Itkin, M. & Nadolski, G. J. Modern techniques of lymphangiography and interventions: current status and future development. Cardiovasc. Intervent Radiol. 41 , 366–376 (2018).
Sarica, M. et al. Lymphoscintigraphic abnormalities associated with Milroy disease and lymphedema-distichiasis syndrome. Lymphat. Res. Biol. 17 , 610–619 (2019).
Cox, T. C. et al. Imaging of lymphatic dysplasia in Noonan syndrome: case studies and historical atlas. Lymphology 54 , 23–40 (2021).
Kinmonth, J. B. & Wolfe, J. H. Fibrosis in the lymph nodes in primary lymphoedema. Histological and clinical studies in 74 patients with lower-limb oedema. Ann. R. Coll. Surg. Engl. 62 , 344–354 (1980).
Geng, X., Cha, B., Mahamud, M. R. & Srinivasan, R. S. Intraluminal valves: development, function and disease. Dis. Model. Mech. 10 , 1273–1287 (2017).
Gale, N. W. et al. Angiopoietin-2 is required for postnatal angiogenesis and lymphatic patterning, and only the latter role is rescued by Angiopoietin-1. Dev. Cell 3 , 411–423 (2002).
Kriederman, B. M. et al. FOXC2 haploinsufficient mice are a model for human autosomal dominant lymphedema-distichiasis syndrome. Hum. Mol. Genet. 12 , 1179–1185 (2003).
Dellinger, M. T. & Witte, M. H. Lymphangiogenesis, lymphatic systemomics, and cancer: context, advances and unanswered questions. Clin. Exp. Metastasis 35 , 419–424 (2018).
Northup, K. A., Witte, M. H. & Witte, C. L. Syndromic classification of hereditary lymphedema. Lymphology 36 , 162–189 (2003).
Fang, J. et al. Mutations in FOXC2 (MFH-1), a forkhead family transcription factor, are responsible for the hereditary lymphedema-distichiasis syndrome. Am. J. Hum. Genet. 67 , 1382–1388 (2000).
Brouillard, P., Boon, L. & Vikkula, M. Genetics of lymphatic anomalies. J. Clin. Invest. 124 , 898–904 (2014).
Jones, G. E. & Mansour, S. An approach to familial lymphoedema. Clin. Med. 17 , 552–557 (2017).
Michelini, S. et al. Genetic tests in lymphatic vascular malformations and lymphedema. J. Med. Genet. 55 , 222–232 (2018).
Sabin, F. R. On the origin of the lymphatic system from the veins and the development of the lymph hearts and thoracic duct in the pig. Am. J. Anat. https://doi.org/10.1002/aja.1000010310 (1902). The first description on the origin of development of the lymphatic system: generation of lymphatic sacs from the pre-existing venous system.
Article Google Scholar
Hutchinson, G. S. On the development of the jugular lymph sac, of the tributary ulnar lymphatic, and of the thoracic duct from the viewpoint of recent investigations of vertebrate lymphatic ontogeny, together with a consideration of the genetic relations of lymphatic and hemal vascular channels in the embryos of amniotes. Am. J. Anat. 16 , 259–316 (1914).
Schneider, M., Othman-Hassan, K., Christ, B. & Wilting, J. Lymphangioblasts in the avian wing bud. Dev. Dyn. 216 , 311–319 (1999).
Yang, Y. & Oliver, G. Development of the mammalian lymphatic vasculature. J. Clin. Invest. 124 , 888–897 (2014).
Ulvmar, M. H. & Makinen, T. Heterogeneity in the lymphatic vascular system and its origin. Cardiovasc. Res. 111 , 310–321 (2016). This review discusses the heterogeneity observed within the lymphatic system in regard to different organs as well as the functional and molecular specialization of lymphatic endothelial cells and their developmental origin .
Stone, O. A. & Stainier, D. Y. R. Paraxial mesoderm is the major source of lymphatic endothelium. Dev. Cell 50 , 247–255.e3 (2019).
Kaipainen, A. et al. Expression of the fms-like tyrosine kinase 4 gene becomes restricted to lymphatic endothelium during development. Proc. Natl Acad. Sci. USA 92 , 3566–3570 (1995).
Banerji, S. et al. LYVE-1, a new homologue of the CD44 glycoprotein, is a lymph-specific receptor for hyaluronan. J. Cell Biol. 144 , 789–801 (1999).
Breiteneder-Geleff, S. et al. Angiosarcomas express mixed endothelial phenotypes of blood and lymphatic capillaries: podoplanin as a specific marker for lymphatic endothelium. Am. J. Pathol. 154 , 385–394 (1999).
Wigle, J. T. & Oliver, G. Prox1 function is required for the development of the murine lymphatic system. Cell 98 , 769–778 (1999). This article describes a key role for the homeobox gene Prox1 , expressed within some venous endothelial cells that, by budding and sprouting, give rise to the lymphatic system. PROX1 is indicated as a specific and required regulator of the development of the lymphatic system.
Johnson, N. C. et al. Lymphatic endothelial cell identity is reversible and its maintenance requires Prox1 activity. Genes Dev. 22 , 3282–3291 (2008).
Ducoli, L. & Detmar, M. Beyond PROX1: transcriptional, epigenetic, and noncoding RNA regulation of lymphatic identity and function. Dev. Cell 56 , 406–426 (2021).
Harada, K. et al. Identification of targets of Prox1 during in vitro vascular differentiation from embryonic stem cells: functional roles of HoxD8 in lymphangiogenesis. J. Cell Sci. 122 , 3923–3930 (2009).
Frye, M. et al. Matrix stiffness controls lymphatic vessel formation through regulation of a GATA2-dependent transcriptional program. Nat. Commun. 9 , 1511 (2018).
Bowles, J. et al. Control of retinoid levels by CYP26B1 is important for lymphatic vascular development in the mouse embryo. Dev. Biol. 386 , 25–33 (2014).
Morooka, N. et al. Polydom is an extracellular matrix protein involved in lymphatic vessel remodeling. Circ. Res. 120 , 1276–1288 (2017).
Brouillard, P. et al. Loss of ADAMTS3 activity causes Hennekam lymphangiectasia-lymphedema syndrome 3. Hum. Mol. Genet. 26 , 4095–4104 (2017).
Jha, S. K. et al. Efficient activation of the lymphangiogenic growth factor VEGF-C requires the C-terminal domain of VEGF-C and the N-terminal domain of CCBE1. Sci. Rep. 7 , 4916 (2017).
Finegold, D. N. et al. Connexin 47 mutations increase risk for secondary lymphedema following breast cancer treatment. Clin. Cancer Res. 18 , 2382–2390 (2012).
Finegold, D. N. et al. HGF and MET mutations in primary and secondary lymphedema. Lymphat. Res. Biol. 6 , 65–68 (2008).
Choi, D. et al. Piezo1 incorporates mechanical force signals into the genetic program that governs lymphatic valve development and maintenance. JCI Insight 4 , e125068 (2019).
PubMed Central Google Scholar
Alper, S. L. Genetic diseases of PIEZO1 and PIEZO2 dysfunction. Curr. Top. Membr. 79 , 97–134 (2017).
Petrova, T. V. et al. Defective valves and abnormal mural cell recruitment underlie lymphatic vascular failure in lymphedema distichiasis. Nat. Med. 10 , 974–981 (2004).
Lyons, O. et al. Human venous valve disease caused by mutations in FOXC2 and GJC2. J. Exp. Med. 214 , 2437–2452 (2017).
Kazenwadel, J. et al. GATA2 is required for lymphatic vessel valve development and maintenance. J. Clin. Invest. 125 , 2979–2994 (2015).
Welsh, J. D. et al. Hemodynamic regulation of perivalvular endothelial gene expression prevents deep venous thrombosis. J. Clin. Invest. 129 , 5489–5500 (2019).
Tatin, F. et al. Planar cell polarity protein Celsr1 regulates endothelial adherens junctions and directed cell rearrangements during valve morphogenesis. Dev. Cell 26 , 31–44 (2013).
Gonzalez-Garay, M. L. et al. A novel mutation in CELSR1 is associated with hereditary lymphedema. Vasc. Cell 8 , 1 (2016).
Kanady, J. D., Dellinger, M. T., Munger, S. J., Witte, M. H. & Simon, A. M. Connexin37 and Connexin43 deficiencies in mice disrupt lymphatic valve development and result in lymphatic disorders including lymphedema and chylothorax. Dev. Biol. 354 , 253–266 (2011).
Sabine, A. et al. Mechanotransduction, PROX1, and FOXC2 cooperate to control connexin37 and calcineurin during lymphatic-valve formation. Dev. Cell 22 , 430–445 (2012).
Zhang, F., Zarkada, G., Yi, S. & Eichmann, A. Lymphatic endothelial cell junctions: molecular regulation in physiology and diseases. Front. Physiol. 11 , 509 (2020). This recent review highlights the mechanisms governing specialized lymphatic endothelial cell–cell junctions (button and zipper-like states), which are crucial for the maintenance of lymphatic vessel integrity and proper lymphatic functions.
Ferrell, R. E. et al. GJC2 missense mutations cause human lymphedema. Am. J. Hum. Genet. 86 , 943–948 (2010).
Martin-Almedina, S. et al. EPHB4 kinase-inactivating mutations cause autosomal dominant lymphatic-related hydrops fetalis. J. Clin. Invest. 126 , 3080–3088 (2016).
Choi, D. et al. ORAI1 activates proliferation of lymphatic endothelial cells in response to laminar flow through kruppel-like factors 2 and 4. Circ. Res. 120 , 1426–1439 (2017).
Mustacich, D. J. et al. Digenic inheritance of a FOXC2 mutation and two PIEZO1 mutations underlies congenital lymphedema in a multigeneration family. Am. J. Med. (in the press).
Meens, M. J. et al. Cx47 fine-tunes the handling of serum lipids but is dispensable for lymphatic vascular function. PLoS ONE 12 , e0181476 (2017).
Mustacich, D. J., et al. Abnormal lymphatic phenotype in a crispr mouse model of the human lymphedema-causing connexin47 R260C point mutation. Lymphology (in the press).
Boucher, C. A., Sargent, C. A., Ogata, T. & Affara, N. A. Breakpoint analysis of Turner patients with partial Xp deletions: implications for the lymphoedema gene location. J. Med. Genet. 38 , 591–598 (2001).
Ogata, T., Tyler-Smith, C., Purvis-Smith, S. & Turner, G. Chromosomal localisation of a gene(s) for Turner stigmata on Yp. J. Med. Genet. 30 , 918–922 (1993).
Bardi, F. et al. Is there still a role for nuchal translucency measurement in the changing paradigm of first trimester screening? Prenat. Diagn. 40 , 197–205 (2020).
Hsu, L. Y., Shapiro, L. R., Gertner, M., Lieber, E. & Hirschhorn, K. Trisomy 22: a clinical entity. J. Pediatr. 79 , 12–19 (1971).
Rosenfeld, W. et al. Duplication 3q: severe manifestations in an infant with duplication of a short segment of 3q. Am. J. Med. Genet. 10 , 187–192 (1981).
Greenlee, R., Hoyme, H., Witte, M., Crowe, P. & Witte, C. Developmental disorders of the lymphatic system. Lymphology 26 , 156–168 (1993). This article reviews the chromosomal abnormalities and syndromes associated with lymphatic disorders, with a focus on primary lymphoedema.
Unolt, M. et al. Primary lymphedema and other lymphatic anomalies are associated with 22q11.2 deletion syndrome. Eur. J. Med. Genet. 61 , 411–415 (2018).
Bull, L. N. et al. Mapping of the locus for cholestasis-lymphedema syndrome (Aagenaes syndrome) to a 6.6-cM interval on chromosome 15q. Am. J. Hum. Genet. 67 , 994–999 (2000).
Jha, S. K., Rauniyar, K. & Jeltsch, M. Key molecules in lymphatic development, function, and identification. Ann. Anat. 219 , 25–34 (2018).
Baldwin, M. E. et al. Vascular endothelial growth factor D is dispensable for development of the lymphatic system. Mol. Cell Biol. 25 , 2441–2449 (2005).
Benedito, R. et al. Notch-dependent VEGFR3 upregulation allows angiogenesis without VEGF-VEGFR2 signalling. Nature 484 , 110–114 (2012).
Makinen, T. et al. PDZ interaction site in ephrinB2 is required for the remodeling of lymphatic vasculature. Genes Dev. 19 , 397–410 (2005).
Carmeliet, P. & Tessier-Lavigne, M. Common mechanisms of nerve and blood vessel wiring. Nature 436 , 193–200 (2005).
Souma, T. et al. Context-dependent functions of angiopoietin 2 are determined by the endothelial phosphatase VEPTP. Proc. Natl Acad. Sci. USA 115 , 1298–1303 (2018).
Ayadi, A., Suelves, M., Dolle, P. & Wasylyk, B. Net, an Ets ternary complex transcription factor, is expressed in sites of vasculogenesis, angiogenesis, and chondrogenesis during mouse development. Mech. Dev. 102 , 205–208 (2001).
Kajiya, K., Hirakawa, S., Ma, B., Drinnenberg, I. & Detmar, M. Hepatocyte growth factor promotes lymphatic vessel formation and function. EMBO J. 24 , 2885–2895 (2005).
Brouillard, P. et al. Non-hotspot PIK3CA mutations are more frequent in CLOVES than in common or combined lymphatic malformations. Orphanet J. Rare Dis. 16 , 267 (2021).
Schook, C. C. et al. Differential diagnosis of lower extremity enlargement in pediatric patients referred with a diagnosis of lymphedema. Plast. Reconstr. Surg. 127 , 1571–1581 (2011).
Szuba, A., Shin, W. S., Strauss, H. W. & Rockson, S. The third circulation: radionuclide lymphoscintigraphy in the evaluation of lymphedema. J. Nucl. Med. 44 , 43–57 (2003).
Atton, G. et al. The lymphatic phenotype in Turner syndrome: an evaluation of nineteen patients and literature review. Eur. J. Hum. Genet. 23 , 1634–1639 (2015).
Nadarajah, N. et al. A Novel splice-site mutation in VEGFC is associated with congenital primary lymphoedema of Gordon. Int. J. Mol. Sci. 19 , 2259 (2018).
Burnier, P., Niddam, J., Bosc, R., Hersant, B. & Meningaud, J. P. Indocyanine green applications in plastic surgery: a review of the literature. J. Plast. Reconstr. Aesthet. Surg. 70 , 814–827 (2017).
Unno, N. et al. A novel method of measuring human lymphatic pumping using indocyanine green fluorescence lymphography. J. Vasc. Surg. 52 , 946–952 (2010).
Liu, N. F., Yan, Z. X. & Wu, X. F. Classification of lymphatic-system malformations in primary lymphoedema based on MR lymphangiography. Eur. J. Vasc. Endovasc. Surg. 44 , 345–349 (2012).
Biko, D. M. et al. Imaging of central lymphatic abnormalities in Noonan syndrome. Pediatr. Radiol. 49 , 586–592 (2019).
Biko, D. M. et al. Intrahepatic dynamic contrast MR lymphangiography: initial experience with a new technique for the assessment of liver lymphatics. Eur. Radiol. 29 , 5190–5196 (2019).
Dori, Y. Novel lymphatic imaging techniques. Tech. Vasc. Interv. Radiol. 19 , 255–261 (2016).
Kinmonth, J. B., Taylor, G. W., Tracy, G. D. & Marsh, J. D. Primary lymphedema: clinical and lymphangiographic studies of a series of 107 patients in which lower limbs were affected. Br. J. Surg. 45 , 1 (1957).
Rajebi, M. R. et al. Intranodal lymphangiography: feasibility and preliminary experience in children. J. Vasc. Interv. Radiol. 22 , 1300–1305 (2011).
Ho, B., Gordon, K. & Mortimer, P. S. A genetic approach to the classification of primary lymphoedema and lymphatic malformations. Eur. J. Vasc. Endovasc. Surg. 56 , 465–466 (2018).
Dalal, A. et al. Interventions for the prevention of recurrent erysipelas and cellulitis. Cochrane Database Syst. Rev. 6 , CD009758 (2017).
van Karnebeek, C. D. M. et al. The role of the clinician in the multi-omics era: are you ready? J. Inherit. Metab. Dis. 41 , 571–582 (2018).
Damstra, R. J., van Steensel, M. A., Boomsma, J. H., Nelemans, P. & Veraart, J. C. Erysipelas as a sign of subclinical primary lymphoedema: a prospective quantitative scintigraphic study of 40 patients with unilateral erysipelas of the leg. Br. J. Dermatol. 158 , 1210–1215 (2008).
Hayes, S. C. Role of exercise in the prevention and management of lymphedema after breast cancer. Exerc. Sport. Sci. Rev. 38 , 2 (2010).
Hayes, S. C. et al. Exercise for health: a randomized, controlled trial evaluating the impact of a pragmatic, translational exercise intervention on the quality of life, function and treatment-related side effects following breast cancer. Breast Cancer Res. Treat. 137 , 175–186 (2013).
Wirtz, P. & Baumann, F. T. Physical activity, exercise and breast cancer - what is the evidence for rehabilitation, aftercare, and survival? A review. Breast Care 13 , 93–101 (2018).
Dieli-Conwright, C. M. et al. Aerobic and resistance exercise improves physical fitness, bone health, and quality of life in overweight and obese breast cancer survivors: a randomized controlled trial. Breast Cancer Res. 20 , 124 (2018).
Yumuk, V. et al. European guidelines for obesity management in adults. Obes. Facts 8 , 402–424 (2015).
Damstra, R. J. & Halk, A.-B., Dutch Working Group on Lymphoedema.The Dutch lymphoedema guidelines based on the International Classification of Functioning, Disability, and Health and the chronic care model. J. Vasc. Surg. Venous Lymphat. Disord. 5 , 756–765 (2017).
Leysen, L. et al. Risk factors of pain in breast cancer survivors: a systematic review and meta-analysis. Support. Care Cancer 25 , 3607–3643 (2017).
Shahpar, H. et al. Risk factors of lymph edema in breast cancer patients. Int. J. Breast Cancer 2013 , 641818 (2013).
Vieira, R. A. et al. Risk factors for arm lymphedema in a cohort of breast cancer patients followed up for 10 years. Breast Care 11 , 45–50 (2016).
Watt, H., Singh-Grewal, D., Wargon, O. & Adams, S. Paediatric lymphoedema: a retrospective chart review of 86 cases. J. Paediatr. Child. Health 53 , 38–42 (2017).
Badger, C. M., Peacock, J. L. & Mortimer, P. S. A randomized, controlled, parallel-group clinical trial comparing multilayer bandaging followed by hosiery versus hosiery alone in the treatment of patients with lymphedema of the limb. Cancer 88 , 2832–2837 (2000).
O’Donnell, T. F. Jr, Allison, G. M. & Iafrati, M. D. A systematic review of guidelines for lymphedema and the need for contemporary intersocietal guidelines for the management of lymphedema. J. Vasc. Surg. Venous Lymphat. Disord. 8 , 676–684 (2020).
Gloviczki, P. Handbook of Venous Disorders: Guidelines of the American Venous Forum (CRC Press, 2017).
Lymphoedema Framework. Best Practice for the Management of Lymphoedema. International Consensus (MEP Ltd., 2006).
Vreeburg, M. et al. Lymphedema-distichiasis syndrome: a distinct type of primary lymphedema caused by mutations in the FOXC2 gene. Int. J. Dermatol. 47 (Suppl. 1), 52–55 (2008).
Shenoy, V. G., Jawale, S. A., Oak, S. N. & Kulkarni, B. K. Primary lymphedema of the penis: surgical correction by preputial unfurling. Pediatr. Surg. Int. 17 , 169–170 (2001).
Suehiro, K., Morikage, N., Murakami, M., Yamashita, O. & Hamano, K. Primary lymphedema complicated by weeping chylous vesicles in the leg and scrotum: report of a case. Surg. Today 42 , 1100–1103 (2012).
Phillips, J. J. & Gordon, S. J. Conservative management of lymphoedema in children: a systematic review. J. Pediatr. Rehabil. Med. 7 , 361–372 (2014).
Todd, M. Compression in young people living with lymphoedema. Br. J. Nurs. 28 , 908–910 (2019).
Benoughidane, B., Simon, L., Fourgeaud, C. & Vignes, S. Low-stretch bandages to treat primary lower limb lymphoedema: a cohort of 48 children. Br. J. Dermatol. 179 , 1203–1204 (2018).
Vignes, S. & Bellanger, J. Primary intestinal lymphangiectasia (Waldmann’s disease). Orphanet J. Rare Dis. 3 , 5 (2008).
Sarasua, S. M. et al. Clinical and genomic evaluation of 201 patients with Phelan-McDermid syndrome. Hum. Genet. 133 , 847–859 (2014).
Emberger, J. M., Navarro, M., Dejean, M. & Izarn, P. Deaf-mutism, lymphedema of the lower limbs and hematological abnormalities (acute leukemia, cytopenia) with autosomal dominant transmission. J. Genet. Hum. 27 , 237–245 (1979).
Fuchs, S. et al. Vascular endothelial growth factor (VEGF) levels in short, GH treated children: a distinct pattern of VEGF-C in Noonan syndrome. J. Endocrinol. Invest. 38 , 399–406 (2015).
Ostergaard, P. et al. Mutations in GATA2 cause primary lymphedema associated with a predisposition to acute myeloid leukemia (Emberger syndrome). Nat. Genet. 43 , 929–931 (2011).
Wlodarski, M. W., Collin, M. & Horwitz, M. S. GATA2 deficiency and related myeloid neoplasms. Semin. Hematol. 54 , 81–86 (2017).
Rastogi, N. et al. Successful nonmyeloablative allogeneic stem cell transplant in a child with Emberger syndrome and GATA2 mutation. J. Pediatr. Hematol. Oncol. 40 , e383–e388 (2018).
Ramzan, M. et al. Successful myeloablative matched unrelated donor hematopoietic stem cell transplantation in a young girl with GATA2 deficiency and Emberger syndrome. J. Pediatr. Hematol. Oncol. 39 , 230–232 (2017).
Saida, S. et al. Successful reduced-intensity stem cell transplantation for GATA2 deficiency before progression of advanced MDS. Pediatr. Transpl. 20 , 333–336 (2016).
CAS Google Scholar
Lubking, A. et al. Young woman with mild bone marrow dysplasia, GATA2 and ASXL1 mutation treated with allogeneic hematopoietic stem cell transplantation. Leuk. Res. Rep. 4 , 72–75 (2015).
Bishnoi, A. et al. Warty fingers and toes in a child with congenital lymphedema: elephantiasis nostras verrucosa. JAMA Dermatol. 154 , 849–850 (2018).
Perez Botero, J. & Rodriguez, V. Primary lymphedema and viral warts in GATA2 haploinsufficiency. Mayo Clin. Proc. 92 , 482 (2017).
Dorn, J. M. et al. WILD syndrome is GATA2 deficiency: a novel deletion in the GATA2 gene. J. Allergy Clin. Immunol. Pract. 5 , 1149–1152.e1 (2017).
Kreuter, A. et al. A human papillomavirus-associated disease with disseminated warts, depressed cell-mediated immunity, primary lymphedema, and anogenital dysplasia: WILD syndrome. Arch. Dermatol. 144 , 366–372 (2008).
Cusack, C., Fitzgerald, D., Clayton, T. M. & Irvine, A. D. Successful treatment of florid cutaneous warts with intravenous cidofovir in an 11-year-old girl. Pediatr. Dermatol. 25 , 387–389 (2008).
Kreuter, A., Waterboer, T. & Wieland, U. Regression of cutaneous warts in a patient with WILD syndrome following recombinant quadrivalent human papillomavirus vaccination. Arch. Dermatol. 146 , 1196–1197 (2010).
Manevitz-Mendelson, E. et al. Somatic NRAS mutation in patient with generalized lymphatic anomaly. Angiogenesis 21 , 287–298 (2018).
Barclay, S. F. et al. A somatic activating NRAS variant associated with kaposiform lymphangiomatosis. Genet. Med. 21 , 1517–1524 (2019).
Rodriguez-Laguna, L. et al. Somatic activating mutations in PIK3CA cause generalized lymphatic anomaly. J. Exp. Med. 216 , 407–418 (2019).
Foster, J. B. et al. Kaposiform lymphangiomatosis effectively treated with MEK inhibition. EMBO Mol. Med. 12 , e12324 (2020).
Homayun Sepehr, N. et al. KRAS-driven model of Gorham-Stout disease effectively treated with trametinib. JCI Insight https://doi.org/10.1172/jci.insight.149831 (2021).
Article PubMed PubMed Central Google Scholar
Queisser, A., Seront, E., Boon, L. M. & Vikkula, M. Genetic basis and therapies for vascular anomalies. Circ. Res. 129 , 155–173 (2021). This recent review describes the genetic and pathophysiological discoveries in the field of vascular anomalies and the current status of repurposing of cancer drugs for their targeted management (theranostics).
Makinen, T., Boon, L. M., Vikkula, M. & Alitalo, K. Lymphatic malformations: genetics, mechanisms and therapeutic strategies. Circ. Res. 129 , 136–154 (2021). This recent review portrays the numerous discoveries made on the genetic and pathophysiological bases of lymphatic malformations and understanding of the molecular and cellular mechanisms involved. It also illustrates the fast progress made in the repurposing of small molecule inhibitors developed for oncology for the targeted management of lymphatic malformations.
Li, D. et al. ARAF recurrent mutation causes central conducting lymphatic anomaly treatable with a MEK inhibitor. Nat. Med. 25 , 1116–1122 (2019).
Rockson, S. G. et al. Pilot studies demonstrate the potential benefits of antiinflammatory therapy in human lymphedema. JCI Insight 3 , e123775 (2018). This small clinical trial for lymphoedema suggests the utility of anti-inflammatory therapy with ketoprofen for patients with lymphoedema.
Brorson, H., Svensson, H., Norrgren, K. & Thorsson, O. Liposuction reduces arm lymphedema without significantly altering the already impaired lymph transport. Lymphology 31 , 156–172 (1998). This prospective study on 20 patients with arm lymphoedema after breast cancer treatment showed that liposuction combined with controlled compression therapy is efficacious.
Schaverien, M. V., Munnoch, D. A. & Brorson, H. Liposuction treatment of lymphedema. Semin. Plast. Surg. 32 , 42–47 (2018).
Greene, A. K., Sudduth, C. L. & Taghinia, A. Lymphedema (seminars in pediatric surgery). Semin. Pediatr. Surg. 29 , 150972 (2020). This recent report reviews the preventive, compressive and interventional options, including lympho-venous anastomosis, LNT and liposuction, for the management of lymphoedema.
Brorson, H., Ohlin, K., Olsson, G., Svensson, B. & Svensson, H. Controlled compression and liposuction treatment for lower extremity lymphedema. Lymphology 41 , 52–63 (2008).
Greene, A. K., Slavin, S. A. & Borud, L. Treatment of lower extremity lymphedema with suction-assisted lipectomy. Plast. Reconstr. Surg. 118 , 118e–121e (2006).
Hendrickx, A. A., Damstra, R. J., Krijnen, W. P. & van der Schans, C. P. Improvement of limb volumes after bariatric surgery in nine end-stage primary, secondary, and obesity-induced lymphedema patients: a multiple case report. Lymphat. Res. Biol. https://doi.org/10.1089/lrb.2020.0055 (2021).
Article PubMed Google Scholar
Olszewski, W. L. The treatment of lymphedema of the extremities with microsurgical lympho-venous anastomoses. Int. Angiol. 7 , 312–321 (1988).
Yamamoto, T. et al. Indocyanine green lymphography findings in primary leg lymphedema. Eur. J. Vasc. Endovasc. Surg. 49 , 95–102 (2015).
Hara, H. et al. Indication of lymphaticovenous anastomosis for lower limb primary lymphedema. Plast. Reconstr. Surg. 136 , 883–893 (2015).
Maegawa, J., Mikami, T., Yamamoto, Y., Satake, T. & Kobayashi, S. Types of lymphoscintigraphy and indications for lymphaticovenous anastomosis. Microsurgery 30 , 437–442 (2010).
Dermitas, Y., Ozturk, N., Yapici, O. & Topalan, M. Comparison of primary and secondary lower-extremity lymphedema treated with supramicrosurgical lymphaticovenous anastomosis and lymphaticovenous implantation. J. Reconstr. Microsurg. 26 , 137–143 (2010).
Gennaro, P. et al. Ultramicrosurgery: a new approach to treat primary male genital lymphedema. JPRAS Open 20 , 72–80 (2019).
Becker, C. et al. Surgical treatment of congenital lymphedema. Clin. Plast. Surg. 39 , 377–384 (2012).
Vignes, S., Blanchard, M., Yannoutsos, A. & Arrault, M. Complications of autologous lymph-node transplantation for limb lymphoedema. Eur. J. Vasc. Endovasc. Surg. 45 , 516–520 (2013).
Cheng, M. H., Loh, C. Y. Y. & Lin, C. Y. Outcomes of vascularized lymph node transfer and lymphovenous anastomosis for treatment of primary lymphedema. Plast. Reconstr. Surg. Glob. Open 6 , e2056 (2018).
Rychik, J. et al. Evaluation and management of the child and adult with fontan circulation: a scientific statement from the American Heart Association. Circulation https://doi.org/10.1161/CIR.0000000000000696 (2019).
Itkin, M., Pizarro, C., Radtke, W., Spurrier, E. & Rabinowitz, D. A. Lymphatic management in single-ventricle patients. Semin. Thorac. Cardiovasc. Surg. Pediatr. Card. Surg Annu. 23 , 41–47 (2020).
Schumacher, K. R. et al. Fontan-associated protein-losing enteropathy and plastic bronchitis. J. Pediatr. 166 , 970–977 (2015).
Bamezai, S., Aronberg, R. M., Park, J. M. & Gemmete, J. J. Intranodal lymphangiography and interstitial lymphatic embolization to treat chyluria caused by a lymphatic malformation in a pediatric patient. Pediatr. Radiol. 51 , 1762–1765 (2021).
Yamamoto, M. et al. Intranodal lymphatic embolization for chylocolporrhea caused by chylous reflux syndrome in Noonan syndrome. J. Vasc. Interv. Radiol. 30 , 769–772 (2019).
Itkin, M. et al. Protein-losing enteropathy in patients with congenital heart disease. J. Am. Coll. Cardiol. 69 , 2929–2937 (2017).
Okajima, S. et al. Health-related quality of life and associated factors in patients with primary lymphedema. Jpn. J. Nurs. Sci. 10 , 202–211 (2013).
Herberger, K. et al. Quality of life in patients with primary and secondary lymphedema in the community. Wound Repair. Regen. 25 , 466–473 (2017).
Fu, M. R. et al. Psychosocial impact of lymphedema: a systematic review of literature from 2004 to 2011. Psychooncology 22 , 1466–1484 (2013).
Hanson, C. S. et al. Children and adolescents’ experiences of primary lymphoedema: semistructured interview study. Arch. Dis. Child. 103 , 675–682 (2018).
Stucki, G. & Grimby, G. Applying the ICF in medicine. J. Rehabil. Med. 44 (Suppl.), 5–6 (2004).
Hidding, J. T. et al. Measurement properties of instruments for measuring of lymphedema: systematic review. Phys. Ther. 96 , 1965–1981 (2016).
Viehoff, P. B., Hidding, J. T., Heerkens, Y. F., van Ravensberg, C. D. & Neumann, H. A. Coding of meaningful concepts in lymphedema-specific questionnaires with the ICF. Disabil. Rehabil. 35 , 2105–2112 (2013).
Devoogdt, N. et al. Lymphoedema functioning, disability and health questionnaire for lower limb lymphoedema (Lymph-ICF-LL): reliability and validity. Phys. Ther. 94 , 705–721 (2014).
Klernas, P., Johnsson, A., Horstmann, V., Kristjanson, L. J. & Johansson, K. Lymphedema quality of life inventory (LyQLI)-development and investigation of validity and reliability. Qual. Life Res. 24 , 427–439 (2015).
Angst, F., Lehmann, S., Aeschlimann, A., Sandor, P. S. & Wagner, S. Cross-sectional validity and specificity of comprehensive measurement in lymphedema and lipedema of the lower extremity: a comparison of five outcome instruments. Health Qual. Life Outcomes 18 , 245 (2020).
Moffatt, C. J. & Murray, S. G. The experience of children and families with lymphoedema — a journey within a journey. Int. Wound J. 7 , 14–26 (2010).
Moffatt, C. et al. A study to explore the professional conceptualization and challenges of self-management in children and adolescents with lymphedema. Lymphat. Res. Biol. 17 , 221–230 (2019).
Moffatt, C. et al. A study to explore the parental impact and challenges of self-management in children and adolescents suffering with lymphedema. Lymphat. Res. Biol. 17 , 245–252 (2019).
Quere, I. et al. International camps for children with lymphedema and lymphatic anomalies: when education links with psychosocial research. Lymphat. Res. Biol. 19 , 36–40 (2021).
Visser, J., van Geel, M., Cornelissen, A. J. M., van der Hulst, R. & Qiu, S. S. Breast cancer-related lymphedema and genetic predisposition: a systematic review of the literature. Lymphat. Res. Biol. 17 , 288–293 (2019).
Coulie, R. et al. Hypotrichosis-lymphedema-telangiectasia syndrome: Report of ileal atresia associated with a SOX18 de novo pathogenic variant and review of the phenotypic spectrum. Am. J. Med. Genet. A 185 , 2153–2159 (2021).
Kajita, H. et al. Photoacoustic lymphangiography. J. Surg. Oncol. 121 , 48–50 (2020).
Kajita, H. et al. Visualization of lymphatic vessels using photoacoustic imaging. Keio J. Med. https://doi.org/10.2302/kjm.2020-0010-OA (2020).
Shinaoka, A., Yamada, K. & Kimata, Y. in ICG Fluorescence Imaging and Navigation Surgery (eds Kusano, M., Kokudo, N., Toi, M. & Kaibori, M.) 433–442 (Springer 2016).
Hartiala, P. et al. Phase 1 Lymfactin(R) study: short-term safety of combined adenoviral VEGF-C and lymph node transfer treatment for upper extremity lymphedema. J. Plast. Reconstr. Aesthet. Surg. 73 , 1612–1621 (2020).
Heitink, M. V. et al. Lymphedema in Prader-Willi syndrome. Int. J. Dermatol. 47 (Suppl. 1), 42–44 (2008).
Garcia-Cruz, D. et al. Cantu syndrome and lymphoedema. Clin. Dysmorphol. 20 , 32–37 (2011).
Scheuerle, A. E. et al. An additional case of Hennekam lymphangiectasia-lymphedema syndrome caused by loss-of-function mutation in ADAMTS3. Am. J. Med. Genet. A 176 , 2858–2861 (2018).
Alders, M. et al. Mutations in CCBE1 cause generalized lymph vessel dysplasia in humans. Nat. Genet. 41 , 1272–1274 (2009).
Li, D. et al. Pathogenic variant in EPHB4 results in central conducting lymphatic anomaly. Hum. Mol. Genet. 27 , 3233–3245 (2018).
Alders, M. et al. Hennekam syndrome can be caused by FAT4 mutations and be allelic to Van Maldergem syndrome. Hum. Genet. 133 , 1161–1167 (2014).
Doffinger, R. et al. X-linked anhidrotic ectodermal dysplasia with immunodeficiency is caused by impaired NF-kappaB signaling. Nat. Genet. 27 , 277–285 (2001).
Mansour, S. et al. Incontinentia pigmenti in a surviving male is accompanied by hypohidrotic ectodermal dysplasia and recurrent infection. Am. J. Med. Genet. 99 , 172–177 (2001).
Ostergaard, P. et al. Mutations in KIF11 cause autosomal-dominant microcephaly variably associated with congenital lymphedema and chorioretinopathy. Am. J. Hum. Genet. 90 , 356–362 (2012).
Schubbert, S. et al. Germline KRAS mutations cause Noonan syndrome. Nat. Genet. 38 , 331–336 (2006).
Nozawa, A. et al. A somatic activating KRAS variant identified in an affected lesion of a patient with Gorham-Stout disease. J. Hum. Genet. 65 , 995–1001 (2020).
McClelland, J., Burgess, B., Crock, P. & Goel, H. Sotos syndrome: an unusual presentation with intrauterine growth restriction, generalized lymphedema, and intention tremor. Am. J. Med. Genet. A 170A , 1064–1069 (2016).
Foster, A. et al. The phenotype of Sotos syndrome in adulthood: a review of 44 individuals. Am. J. Med. Genet. C. Semin. Med Genet 181 , 502–508 (2019).
Fotiou, E. et al. Novel mutations in PIEZO1 cause an autosomal recessive generalized lymphatic dysplasia with non-immune hydrops fetalis. Nat. Commun. 6 , 8085 (2015).
Lukacs, V. et al. Impaired PIEZO1 function in patients with a novel autosomal recessive congenital lymphatic dysplasia. Nat. Commun. 6 , 8329 (2015).
Yoshida, R., Miyata, M., Nagai, T., Yamazaki, T. & Ogata, T. A 3-bp deletion mutation of PTPN11 in an infant with severe Noonan syndrome including hydrops fetalis and juvenile myelomonocytic leukemia. Am. J. Med. Genet. A 128A , 63–66 (2004).
Croonen, E. A. et al. Prenatal diagnostic testing of the Noonan syndrome genes in fetuses with abnormal ultrasound findings. Eur. J. Hum. Genet. 21 , 936–942 (2013).
Thompson, D. et al. RAF1 variants causing biventricular hypertrophic cardiomyopathy in two preterm infants: further phenotypic delineation and review of literature. Clin. Dysmorphol. 26 , 195–199 (2017).
Burrows, P. E. et al. Lymphatic abnormalities are associated with RASA1 gene mutations in mouse and man. Proc. Natl Acad. Sci. USA 110 , 8621–8626 (2013).
de Wijn, R. S. et al. Phenotypic variability in a family with capillary malformations caused by a mutation in the RASA1 gene. Eur. J. Med. Genet. 55 , 191–195 (2012).
Macmurdo, C. F. et al. RASA1 somatic mutation and variable expressivity in capillary malformation/arteriovenous malformation (CM/AVM) syndrome. Am. J. Med. Genet. A 170 , 1450–1454 (2016).
Gos, M. et al. Contribution of RIT1 mutations to the pathogenesis of Noonan syndrome: four new cases and further evidence of heterogeneity. Am. J. Med. Genet. A 164A , 2310–2316 (2014).
Milosavljevic, D. et al. Two cases of RIT1 associated Noonan syndrome: further delineation of the clinical phenotype and review of the literature. Am. J. Med. Genet. A 170 , 1874–1880 (2016).
Koenighofer, M. et al. Mutations in RIT1 cause Noonan syndrome - additional functional evidence and expanding the clinical phenotype. Clin. Genet. 89 , 359–366 (2016).
Yaoita, M. et al. Spectrum of mutations and genotype-phenotype analysis in Noonan syndrome patients with RIT1 mutations. Hum. Genet. 135 , 209–222 (2016).
Roberts, A. E. et al. Germline gain-of-function mutations in SOS1 cause Noonan syndrome. Nat. Genet. 39 , 70–74 (2007).
Smpokou, P., Tworog-Dube, E., Kucherlapati, R. S. & Roberts, A. E. Medical complications, clinical findings, and educational outcomes in adults with Noonan syndrome. Am. J. Med. Genet. A 158A , 3106–3111 (2012).
Yamamoto, G. L. et al. Rare variants in SOS2 and LZTR1 are associated with Noonan syndrome. J. Med. Genet. 52 , 413–421 (2015).
Cordeddu, V. et al. Activating mutations affecting the Dbl homology domain of SOS2 cause Noonan syndrome. Hum. Mutat. 36 , 1080–1087 (2015).
Lissewski, C. et al. Variants of SOS2 are a rare cause of Noonan syndrome with particular predisposition for lymphatic complications. Eur. J. Hum. Genet. 29 , 51–60 (2021).
Irrthum, A. et al. Mutations in the transcription factor gene SOX18 underlie recessive and dominant forms of hypotrichosis-lymphedema-telangiectasia. Am. J. Hum. Genet. 72 , 1470–1478 (2003).
Shamseldin, H. E. et al. Identification of embryonic lethal genes in humans by autozygosity mapping and exome sequencing in consanguineous families. Genome Biol. 16 , 116 (2015).
Abdelrahman, H. A. et al. A recessive truncating variant in thrombospondin-1 domain containing protein 1 gene THSD1 is the underlying cause of nonimmune hydrops fetalis, congenital cardiac defects, and haemangiomas in four patients from a consanguineous family. Am. J. Med. Genet. A 176 , 1996–2003 (2018).
Prato, G. et al. Congenital segmental lymphedema in tuberous sclerosis complex with associated subependymal giant cell astrocytomas treated with Mammalian target of rapamycin inhibitors. J. Child. Neurol. 29 , NP54–NP57 (2014).
Geffrey, A. L., Shinnick, J. E., Staley, B. A., Boronat, S. & Thiele, E. A. Lymphedema in tuberous sclerosis complex. Am. J. Med. Genet. A 164A , 1438–1442 (2014).
Gordon, K. et al. Mutation in vascular endothelial growth factor-C, a ligand for vascular endothelial growth factor receptor-3, is associated with autosomal dominant Milroy-like primary lymphedema. Circ. Res. 112 , 956–960 (2013).
Balboa-Beltran, E. et al. A novel stop mutation in the vascular endothelial growth factor-C gene (VEGFC) results in Milroy-like disease. J. Med. Genet. 51 , 475–478 (2014).
Mukenge, S. et al. Investigation on the role of biallelic variants in VEGF-C found in a patient affected by Milroy-like lymphedema. Mol. Genet. Genomic Med. 8 , e1389 (2020).
Jones, K. L., Schwarze, U., Adam, M. P., Byers, P. H. & Mefford, H. C. A homozygous B3GAT3 mutation causes a severe syndrome with multiple fractures, expanding the phenotype of linkeropathy syndromes. Am. J. Med. Genet. A 167A , 2691–2696 (2015).
Sekiguchi, K. et al. A transient myelodysplastic/myeloproliferative neoplasm in a patient with cardio-facio-cutaneous syndrome and a germline BRAF mutation. Am. J. Med. Genet. A 161A , 2600–2603 (2013).
Joyce, S. et al. The lymphatic phenotype in Noonan and Cardiofaciocutaneous syndrome. Eur. J. Hum. Genet. 24 , 690–696 (2016).
Hanson, H. L. et al. Germline CBL mutation associated with a noonan-like syndrome with primary lymphedema and teratoma associated with acquired uniparental isodisomy of chromosome 11q23. Am. J. Med. Genet. A 164A , 1003–1009 (2014).
Boone, P. M. et al. Biallelic mutation of FBXL7 suggests a novel form of Hennekam syndrome. Am. J. Med. Genet. A 182 , 189–194 (2020).
Michelini, S. et al. Genetic screening in a large cohort of italian patients affected by primary lymphedema using a next generation sequencing (NGS) Approach. Lymphology 49 , 57–72 (2016).
Kawase, K. et al. Nemaline myopathy with KLHL40 mutation presenting as congenital totally locked-in state. Brain Dev. 37 , 887–890 (2015).
Sparks, T. N. et al. Exome sequencing for prenatal diagnosis in nonimmune hydrops fetalis. N. Engl. J. Med. 383 , 1746–1756 (2020).
Ponti, G. et al. Giant elephantiasis neuromatosa in the setting of neurofibromatosis type 1: a case report. Oncol. Lett. 11 , 3709–3714 (2016).
Michelini, S. et al. Segregation analysis of rare NRP1 and NRP2 variants in families with lymphedema. Genes 11 , 1361 (2020).
CAS PubMed Central Google Scholar
Ricci, M. et al. Review of the function of SEMA3A in lymphatic vessel maturation and its potential as a candidate gene for lymphedema: Analysis of three families with rare causative variants. Lymphology 53 , 63–75 (2020).
Gargano, G. et al. Hydrops fetalis in a preterm newborn heterozygous for the c.4A>G SHOC2 mutation. Am. J. Med. Genet. A 164A , 1015–1020 (2014).
Takenouchi, T. et al. Severe craniosynostosis with Noonan syndrome phenotype associated with SHOC2 mutation: clinical evidence of crosslink between FGFR and RAS signaling pathways. Am. J. Med. Genet. A 164A , 2869–2872 (2014).
Michelini, S. et al. TIE1 as a candidate gene for lymphatic malformations with or without lymphedema. Int. J. Mol. Sci. 21 , 6780 (2020).
Lucas, M. & Andrade, Y. Congenital lymphedema with tuberous sclerosis and clinical Hirschsprung disease. Pediatr. Dermatol. 28 , 194–195 (2011).
Klinner, J. et al. Congenital lymphedema as a rare and first symptom of tuberous sclerosis complex. Gene 753 , 144815 (2020).
Hopman, S. M. et al. PTEN hamartoma tumor syndrome and Gorham-Stout phenomenon. Am. J. Med. Genet. A 158A , 1719–1723 (2012).
Scarcella, A., De Lucia, A., Pasquariello, M. B. & Gambardella, P. Early death in two sisters with Hennekam syndrome. Am. J. Med. Genet. 93 , 181–183 (2000).
Greene, A. K., Grant, F. D. & Slavin, S. A. Lower-extremity lymphedema and elevated body-mass index. N. Engl. J. Med. 366 , 2136–2137 (2012).
Burian, E. A. et al. Cellulitis in chronic oedema of the lower leg: an international cross-sectional study. Br. J. Dermatol. 185 , 110–118 (2021).
World Health Organization. Lymphatic filariasis — managing morbidity and preventing disability — an aide-mémoire for national programme managers . Second edition (WHO, 2021).
Zanten, M. et al. A diagnostic dilemma: aetiological diagnosis of lymphoedema patients at an Indian multidisciplinary meeting. J. Lymphoedema 14 , 43–46 (2019).
Mercier, G. et al. Out-of-pocket payments, vertical equity and unmet medical needs in France: A national multicenter prospective study on lymphedema. PLoS ONE 14 , e0216386 (2019).
Download references
Acknowledgements
M.V.’s laboratories were financially supported by the Fonds de la Recherche Scientifique – FNRS Grants T.0026.14 and T.0247.19, the Fund Generet managed by the King Baudouin Foundation (Grant 2018-J1810250-211305), and by la Région wallonne dans le cadre du financement de l’axe stratégique FRFS-WELBIO (WELBIO-CR-2019C-06). M.V. has also received funding from the MSCA-ITN network V. A. Cure No. 814316 and the Lymphatic Malformation Institute, USA. M.H.W. has received research support from the University of Arizona Health Sciences Translational Imaging Program Projects Stimulus (TIPPS) Award and National Institutes of Health NHLBI R25HL108837 for diverse undergraduate research trainees (Luis Luy, Jasmine Jones, Reginald Myles); she is also Secretary-General, International Society of Lymphology, Tucson, AZ, USA, and Zurich, Switzerland. The authors are grateful to Grace Wagner and Juan Ruiz for programmatic assistance and to Liliana Niculescu for expert secretarial assistance.
Author information
Authors and affiliations.
Human Molecular Genetics, de Duve Institute, University of Louvain, Brussels, Belgium
Pascal Brouillard & Miikka Vikkula
Department of Surgery, Neurosurgery, and Pediatrics, University of Arizona College of Medicine, Tucson, AZ, USA
- Marlys H. Witte
Department of Pediatrics, University of Arizona College of Medicine, Tucson, AZ, USA
Robert P. Erickson
VASCERN PPL European Reference Centre; Department of Dermatology, Phlebology and Lymphology, Nij Smellinghe Hospital, Drachten, Netherlands
Robert J. Damstra
Lymphoedema Center, Clinique Jouvenet, Paris, France
Corinne Becker
Department of Vascular Medicine, Centre de référence des Maladies Lymphatiques et Vasculaires Rares, Inserm IDESP, CHU Montpellier, Université de Montpellier, Montpellier, France
Isabelle Quéré
VASCERN VASCA European Reference Centre; Center for Vascular Anomalies, Division of Plastic Surgery, University Clinics Saint-Luc, University of Louvain, Brussels, Belgium
Miikka Vikkula
Walloon Excellence in Lifesciences and Biotechnology (WELBIO), de Duve Institute, University of Louvain, Brussels, Belgium
You can also search for this author in PubMed Google Scholar
Contributions
Introduction (M.V., P.B., M.H.W. and R.P.E.); Epidemiology (M.V., P.B., M.H.W., R.P.E. and I.Q.); Mechanisms/pathophysiology (M.V., P.B., M.H.W., R.P.E. and I.Q.); Diagnosis, screening and prevention (M.V., P.B., M.H.W., R.P.E., R.J.D., C.B. and I.Q.); Management (M.V., P.B., M.H.W., R.P.E., C.B. and I.Q.); Quality of life (M.V., P.B., M.H.W., R.P.E., R.J.D. and I.Q.); Outlook (M.V., P.B., M.H.W., R.P.E. and I.Q.); Overview of Primer (M.V.).
Corresponding author
Correspondence to Miikka Vikkula .
Ethics declarations
Competing interests.
All authors declare no competing interests.
Additional information
Peer review information.
Nature Reviews Disease Primers thanks M.-H. Cheng, T. Yamamoto and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information, rights and permissions.
Reprints and permissions
About this article
Cite this article.
Brouillard, P., Witte, M.H., Erickson, R.P. et al. Primary lymphoedema. Nat Rev Dis Primers 7 , 77 (2021). https://doi.org/10.1038/s41572-021-00309-7
Download citation
Accepted : 17 September 2021
Published : 21 October 2021
DOI : https://doi.org/10.1038/s41572-021-00309-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Lymphatic vessels in the age of cancer immunotherapy.
- Triantafyllia Karakousi
- Tenny Mudianto
- Amanda W. Lund
Nature Reviews Cancer (2024)
Etiology and treatment of cancer-related secondary lymphedema
- Michael Bernas
- Sara Al-Ghadban
- Margaret L. McNeely
Clinical & Experimental Metastasis (2024)
Evaluation of Primary Lymphedema with Intranodal Lymphangiography
- Charissa Kim
- Jeffrey Weinstein
CardioVascular and Interventional Radiology (2024)
Cancer metastasis through the lymphatic versus blood vessels
- Stanley P. Leong
Advances in photoacoustic imaging aided by nano contrast agents: special focus on role of lymphatic system imaging for cancer theranostics
- Badrinathan Sridharan
- Hae Gyun Lim
Journal of Nanobiotechnology (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Understanding molecular drivers of lymphedema
“We identified a new molecular pathway that identified how mechanical or physical cues can trigger the development of lymphatic valves at the right place and the right time."

Susan Quaggin, SQI Member
Northwestern University scientists led by SQI member Susan Quaggin have uncovered molecular mechanisms underlying lymphatic valve development, a discovery which could prove useful in treating lymphedema, according to a study published in The Journal of Clinical Investigation .
Lymphedema, a chronic condition that causes localized swelling, has no known cure and affects one in 100,000 individuals in the U.S., according to the National Institutes of Health.
In the study, investigators sought to understand how genetic mutations previously associated with lymphedema contribute to the disease, said Quaggin, the chair and Irving S. Cutter Professor of Medicine at Northwestern, who was senior author of the study.
“Lymphedema is a common and debilitating clinical condition,” Quaggin said. “The study was designed to unravel the molecules and pathways responsible for proper development of a functional lymphatic system – disruption of lymphatic development results in lymphedema.”
Previous research has pointed to mutations in the genes PIEZO1 , ANGPT2 and TIE1 as potential culprits responsible for lymphedema.
In the current study, investigators studied mice missing these genes to better understand how a healthy lymphatic system develops and how genetic variations can lead to lymphedema.
By performing RNA sequencing on the mice coupled with cell-based studies, the investigators observed that the activation of PIEZO1 in lymphatic endothelial cells resulted in rapid exocytosis, or the process of vesicles fusing with the plasma membrane and releasing their contents – including the lymphatic growth factor ligand, Angiopoietin-2 – to the outside of the cell.
Investigators also observed that this activation increased signaling in lymphedema-associated genes and caused the cells to export FOXO1, a protein known to repress lymphatic valve formation.
Taken together, the findings provide insight into the genetic regulation of lymphatic function and the molecular pathways involved in lymphedema, Quaggin said.
“We identified a new molecular pathway that identified how mechanical or physical cues can trigger the development of lymphatic valves at the right place and the right time – just at the place where there is likely to be a cue that physical forces require a valve to form,” said Quaggin, who also directs the Feinberg Cardiovascular and Renal Research Institute .
Now, Quaggin and her laboratory will turn their attention to studying this pathway in blood vessel development, she said.
“We are now exploring whether or not this pathway is also true in blood and hybrid vessel development, specifically in development of a unique vessel in the front of the eye known as Schlemm’s canal, which is a lymphatic-like vessel,” Quaggin said. “The reason why it is important to explore the Schlemm’s canal is because of the important role this vessel plays in controlling the pressure in the eye and preventing the development of glaucoma.”
The study was supported by National Cancer Institute grant P30 CA60553 and the National Institutes of Health George M. O’Brien kidney core grant P30 DK114857.
Note: This article was first published by the Feinberg News Center .
Breast Cancer Foundation NZ
- Our Partners
- News & updates
- Medical Professionals
Research & medical
First clinical evaluation of laser treatment for lymphoedema in new zealand.

What is the problem and who is affected?
Lymphoedema causes swelling and hardening of the arm in up to a quarter of breast cancer patients who have multiple lymph nodes removed as part of their breast cancer treatment. Lymphoedema of the arm can also be caused by taxanes, a type of cancer drug, and breast lymphoedema is increasing as more women have breast-conserving surgery (lumpectomy). The discomfort and swelling caused by lymphoedema can be severe, and treatment options are limited.
“In Australia and the USA, laser is seen as a low-cost, safe and effective treatment for breast cancer-related lymphoedema to reduce limb volume and improve function,” said Professor Baxter. “But most studies have been small-scale, and LLLT isn’t established in New Zealand at all. This study is a chance to see how well it works for our patients in our treatment environment.”
What is this research hoping to achieve?
Professor David Baxter and his team will evaluate the potential effectiveness of low level laser therapy (LLLT) for breast cancer-related lymphoedema, its acceptability to patients and therapists, and the feasibility of incorporating the treatment into existing clinical practice within New Zealand’s hospitals.
Pacific peoples’ experiences of cancer and its treatment in Aotearoa: a qualitative study
Characterisation of breast cancer in premenopausal women, identifying transcription factors in metastatic breast cancer.
- Search Hit enter to search
This website may not work correctly because your browser is out of date. Please update your browser .
- Resources and research
- HRC Research Repository
Identification and monitoring of lymphoedema
Back to the HRC-funded research repository
Back to top
Follow the HRC on X
Print this page
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Biology of Lymphedema
Bianca brix, alberto onorato, christian ure, andreas roessler, nandu goswami.
- Author information
- Article notes
- Copyright and License information
Correspondence: [email protected] ; Tel.: +43-316-385-73852
Received 2021 Feb 23; Accepted 2021 Mar 23; Collection date 2021 Apr.
Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/ ).
Simple Summary
Lymphedema is a chronic, debilitating disease of the lymphatic vasculature. Although several reviews focus on the anatomy and physiology of the lymphatic system, this review provides an overview of the lymphatic vasculature and, moreover, of lymphatic system dysfunction and lymphedema. Further, we aim at advancing the knowledge in the area of lymphatic system function and how dysfunction of the lymphatic system—as seen in lymphedema—affects physiological systems, such as the cardiovascular system, and how those might be modulated by lymphedema therapy.
This narrative review portrays the lymphatic system, a poorly understood but important physiological system. While several reviews have been published that are related to the biology of the lymphatic system and lymphedema, the physiological alternations, which arise due to disturbances of this system, and during lymphedema therapy, are poorly understood and, consequently, not widely reported. We present an inclusive collection of evidence from the scientific literature reflecting important developments in lymphedema research over the last few decades. This review aims at advancing the knowledge on the area of lymphatic system function as well as how system dysfunction, as seen in lymphedema, affects physiological systems and how lymphedema therapy modulates these mechanisms. We propose that future studies should aim at investigating, in-detail, aspects that are related to fluid regulation, hemodynamic responses, and endothelial and/or vascular changes due to lymphedema and lymphedema therapy.
Keywords: lymphatic vasculature, lymphedema, complete decongestive therapy, manual lymphatic drainage, cardiovascular system, hemodynamics, fluid shifts, perometry, plasma volume
1. Introduction
The lymphatic system is a vascular network that is more frequently researched in the past years. However, it is still far from being fully understood. This review examines the lymphatic system and lymphedema from a variety of perspectives. Limited knowledge is available regarding how lymphedema as well as lymphedema therapy affect other physiological systems, such as fluid shifts or the cardiovascular system, especially hemodynamic responses and endothelial/vascular (dys-)function. Therefore, this review systematically assesses the possible effects of lymphedema and its therapy on fluid mobilization, hemodynamic parameters at rest, and in response to orthostatic loading, as well as vascular function.
2. Overview of the Lymphatic System
2.1. anatomy.
The lymphatic system includes a variety of structures and so-called lymphoid organs, including the spleen, thymus, and tonsils, all having their specialized role in, e.g., immune function. However, this review focuses on the lymphatic vasculature, which is—compared to the blood vasculature—a unidirectional transport system. It starts at the peripheral capillary beds of the blood vessels and it runs throughout the whole body [ 1 ], organized as vascular tree, and it can be anatomically separated into different sections dependent on the location (distal to central) [ 1 ]: (i) initial lymphatic vessels; (ii) collector lymphatic vessels (pre- and post-nodal); (iii) lymph nodes; and, (iv) lymphatic trunks. For detailed anatomy of the lymphatic system, please see [ 1 , 2 , 3 , 4 , 5 , 6 , 7 ].
2.2. Physiology
In order to fulfil its role in providing fluid and nutrients to the different tissues, blood vessels continuously leak plasma and proteins at the capillary bed / microvasculature into the interstitial space. This mechanism is driven by an imbalance in hydrostatic and osmotic pressure, which is widely known as “Starling equation” [ 8 ]. Approximately eight liters of plasma are filtered each day [ 8 ]. The accumulation of excessive fluid in the interstitial space generates pressure. This is the driving force for fluid to enter into the initial lymphatics via primary valves [ 9 , 10 ]. As the initial lymphatics lie very close to the microvasculature, they serve as entry point for lymphatic fluid [ 1 ].
Two primary forces are responsible for “pushing” lymphatic fluid trough the lymphatic vessels: extrinsic forces, e.g., muscle movement, heart contraction or respiration, as well as intrinsic forces. The anatomical structures of the vasculature, specifically the lymphangions, are of importance in this process. Along with muscle contraction, this enables the vasculature to work as a pump. Lymphatic fluid is pumped from each lymphangion to the next. Structural segments further support this process in the form of unidirectional valves that are made of endothelial cells and connective tissue at each end of the lymphangions. Their main role is to prevent backflow of lymphatic fluid. This is particularly important while standing in an upright position, as the lymph flux must be driven against gravity [ 1 ]. Sequential peristaltic as well as segmented contractions of lymphangions, together with the lymphatic valves, prevent backflow [ 11 , 12 ]. This active, intrinsic pump mechanism plays a crucial role in the regular flow within the lymphatic system [ 13 ]. Neuronal, humoral, and mechanical stimuli (e.g., pressure or shear stress) can enhance fluid flow and optimize lymph function [ 14 ]. Similar to blood vessels, lymphatic vessels also express flow-mediated nitric oxide (NO) production [ 15 ]. Scallan et al. (2013) suggested a potential exchange mechanism between lymphatics and tissues, as atrial and brain natriuretic peptides have shown to modify the permeability of collecting lymphatics [ 16 ]. Lymph fluid consists of immune cells, proteins, lipids, lipoproteins, electrolytes, and bacteria (including potential harmful compounds). Passing through the lymphatic vasculature, lymph fluid is directed through at least one lymph node. There, an adequate immune answer eliminates bacteria and any potentially harmful particles. Thus, blood vessels that are located within the nodes transport different compounds, such as fluid, proteins, and cells [ 1 ]. Additionally, lymphatic fluid is mechanically filtered within lymph nodes. This allows protein-free fluid to pass through the blood–lymph barrier. Therefore, afferent lymph can be concentrated by the reabsorption of water [ 17 ], which leads to a higher protein concentration in post-nodal lymphatic fluid [ 18 ]. From the eight liters of lymphatic fluid that is produced every day, reabsorption processes in the lymph nodes reduce the efferent outcome to about four liters [ 19 ]. Finally, Gannon and Carati (2003) reported the expression of Aquaporin-1 water channels in lymph nodes in an animal model and, thus, suggest that a transcellular transport of water might contribute to protein concentrations [ 4 , 20 ].
2.3. Methods for Assessing Lymphatic Flow
Lymphoscintigraphy is used as a diagnostic tool to image lymphatic vessels. It includes the injection of radioactive colloid particles. The accumulation of those within the lymphatic vasculature and lymph nodes can then be determined. It is used as the gold standard to determine whether tissue swelling occurs due to lymphatic dysfunction [ 21 ]. However, more suitable to show lymphatic flow is the use of near-infrared fluorescence dyes, in particular indocyanine green (ICG). This allows a quantitative analysis of lymph flow [ 22 ]. Another option is magnetic resonance lymphangiography, which is highly suitable for visualizing lymphatic vessels, but scintigraphy is superior in detecting lymph nodes [ 23 , 24 ]. Near infrared fluorescence imaging uses fluorescent dyes to visualize lymphatic vessels. The fluorescent dye indocyanine green is primarily bound to albumin and, due to its large molecular size, it is restricted to the lymphatic vessels. This technique is routinely used in lymphatic-venous anastomosis surgery to find suitable vessels [ 21 ]. Lipidiol has been used as contrast medium in transpedal lymphangiography, as it is retained within the lymphatic vessels when compared to other agents, which tend to diffuse out of the vessels more rapidly [ 25 ]. Further, dynamic contrast-enhanced magnetic resonance lymphangiography (MLR) is a technique that has been used for imaging central conducting lymphatic vessels, using T1-weighted MR images. This method has been applied in imaging as well as treatment planning of lymphatic leaks, thoracic duct, and other lymphatic abnormalities, as well as chyloperitoneum and chylothorax [ 25 , 26 ]. Finally, a novel, innovative tool for the visualization of the lymphatic vasculature is a 3D imaging technique known as a multispectral optoacoustic tomography device (MSOT). This method allows for the precise detection of lymphatic vessels in real-time, utilizing a hand-held device. It has shown to be especially useful in the detection of deep lymphatic vessels that could not be detected via ICG lymphography [ 27 ]. The readers are referred to Polomska et al. (2020) for further details on lymphatic imaging [ 28 ].
Hyaluronic acid (HA), a biogenic macromolecule, is transported into the blood stream solely via the lymphatic vessels [ 29 ]. The level of plasma HA reflects a dynamic balance between delivery to and the bloodstream removal. Therefore, HA has recently been proposed as a novel biomarker in the assessment of lymphatic flow [ 29 , 30 , 31 ]. Previously, increased plasma hyaluronic acid levels have been reported, e.g., during exercise [ 32 ] or post-prandial in healthy subjects [ 33 ]. Roh et al. (2017) showed that the hyaluronic acid levels are increased within the lymphedema tissue in a mouse model [ 30 ]. This was also observed in human lymphedema tissue [ 34 ]. In a pilot study, where we assessed HA levels before and after three weeks of CDT, we could not see changes in plasma HA (as an indicator of lymphatic outflow). These findings raise the question of whether hyaluronan in plasma can serve as a practical lymphatic outflow measure in patients with lymphedema [ 35 ]. Because of its large molecular size, HA molecules may be preserved within the lymphedematous tissue of such patients, possibly leading to the recurrent accumulation of fluid [ 36 ]. It is possible that physical therapy mobilizes fluid from the interstitial space, but without accompanying HA molecules in lymphedema patients. Hyaluronic acid could be resistant to degradation and wash out by application of local physical pressure, as, e.g., during manual lymphatic drainage. Indeed, it has been suggested that recombinant hyaluronidase [ 30 ] or local heat therapy [ 37 ] in mouse models could be effective in breaking down high molecular weight hyaluronic acid.
3. Overview of Lymphedema
Any imbalance in lymphatic fluid generation, transport, outflow, or dysfunctional vessels can lead to lymphedema. Lymphedema is a progressive disease, leading to a massive accumulation of fluid. It usually occurs in the extremities and it is a disabling disease that can arise due lymphatic dysfunction and can display a huge psychological burden [ 38 ]. Independent of the precise etiology, lymphedema is characterized by severe swelling, atrophic skin changes, secondary infections, and localized pain [ 39 ].
3.1. Epidemiology and Etiology
Lymphedema has been reported to often be underestimated or misdiagnosed [ 40 ]. A number of differential diagnosis, such as lipedema or venous diseases, need to be taken into account [ 41 ]. Further, only a limited number of medical doctors specialize in this field. When considering these aspects, patients often find themselves as medical nomads [ 40 ], passing several doctors until a diagnosis is made. Thus, the exact number of patients suffering from lymphedema can only be estimated. These estimates range between 140 Million and up to 300 Million people worldwide [ 38 , 42 , 43 , 44 , 45 ]. Maclellan et al. (2015) found that 25% of 255 patients included were diagnosed with “lymphedema”, although they suffered from different diseases, as e.g., venous stasis (7%), lipedema (6%), or vascular malformations (1%). On average, 7.7 years passed between disease onset and the allocation to a treatment program. About 70% of the patients in this study population were female [ 40 ]. Neuhüttler and Brenner (2006) also showed that females are more likely to develop lymphedemas when compared to males (females:males; 4.6:1) [ 46 ]. The results from a bigger, multi-center investigation that was performed in several countries (France, Turkey, United Kingdom, Canada, and more) are similar: 79% of the patients included were women [ 47 ].
While not yet completely elucidated (precise pathophysiological processes underlying this disorder, its heterogeneity, root cause), it can be differentiated between primary and secondary forms. Primary lymphedema is associated with a strong genetic background (inherited or caused by spontaneous mutation), whereas secondary lymphedema is typically acquired and it evolves e.g. when lymphatic impairment occurs.
3.1.1. Primary Lymphedema
Primary lymphedema is strongly associated with a genetic background in 25–30% of all primary lymphedema patients [ 5 ]. The prevalence is relatively rare, the disease is seen in one from 100.000 individuals [ 42 ]. Typically, this form of lymphedema occurs due to function impairment, which leads to a structural and/or functional dysfunction that negatively influences the drainage abilities [ 48 ]. More than 20 different genes (i.e., VEGFR-3, CCBE1, FOXC2, GATA2, GJC2, PTPN14, SOX18, CCBE1, FAT4, ADAMTS3, FBXL7, GJC2, KIF11, ITGA9, REEKIN, PIEZO1, EPHB4, CALCRL, and CELSR1) have been associated with anomalies in the lymphatic system, leading either to underdeveloped lymphatic structures or poor lymphatic outflow abilities [ 6 , 49 ]. Aspelund et al. (2016) reported that vascular endothelial growth factor-C (VEGF-C) and the endothelial growth factor receptor-3 (VEGFR-3) signaling axis have been found to be involved in around 50% of all primary lymphedema cases [ 50 ]. Another example is lymphedema distichiasis occurring due to mutations in the FOXC2 gene, leading to malformed lymphatic valves [ 51 , 52 ].
Although a genetic background in primary lymphedema has been researched in recent investigations, the disease was historically classified into three groups depending on the age of the patients, when first symptoms occurred [ 43 ]. Different sub-groups were characterized as follows [ 53 ]:
congenital lymphedema: <1 year;
lymphedema praecox: 1–35 years (most common sub-group); and,
lymphedema tarda: <35 years.
The exact numbers of patients suffering from primary lymphedema is not known; however, it is estimated to be up to 10% higher in females when compared with males
3.1.2. Secondary Lymphedema
Secondary lymphedema is the far more common form of lymphedema. The prevalence of the secondary form is estimated at one in 1000 individuals. The average age of patients at diagnosis in secondary lymphedema is between 50–58 years [ 42 ]. When compared to primary lymphedema, secondary lymphedema develops due to tissue damage, vessel obstruction or deranged lymph nodes, and/or lymphatic vessels that were intact before. Therefore, it is acknowledged as an acquired disease. Surgery, trauma, obesity, or infections ( wuchereria bancrofti ) can be the reason for this damage leading to the development of the disease [ 42 , 54 ]. Furthermore, it often occurs following cancer treatment, e.g., radiotherapy or the dissection of lymph nodes [ 42 , 53 ]. Breast cancer related lymphedema (BCRL) is the most common form of secondary lymphedema. The risk of developing lymphedema after breast cancer treatment was reported to be about 15–20% [ 48 ]. A systematic review and meta-analysis of BCRL cases shows an overall incidence of 15.5% after cancer treatment [ 55 ]. Bar Ad et al. (2010) reported that 16% of all patients undergoing treatment with a combination of lymph node resection and radiation therapy developed clinical signs of lymphedema [ 56 ], whereas radiation therapy led to the highest incidences at 31% [ 55 ]. Radiation therapy can lead to the reduction of proliferative potential of the lymphatic tissue, fibrosis of the lymph nodes or to a mechanical insufficiency of the lymphatic vasculature [ 57 ]. Additional co-factors in the development of secondary lymphedema can be congestive heart failure or renal diseases [ 58 ]. It has further been suggested that several genes (e.g. VEGFR2 , VEGFR3 , RORC , GJC2 , and FOXC2 ) are possibly involved in secondary lymphedema developing following breast cancer therapy [ 59 , 60 , 61 ].
3.1.3. Lymphatic Malformations and Chylous Effusions
Lymphatic malformations (LMs) are defined as congenital slow-flow vascular malformations and they are characterized by lesions in the lymphatic vessels, consisting of dilated lymphatic vessels and cystic-like areas that are filled with lymphatic fluid [ 62 , 63 ]. They are typically found in the head and neck area as well as pelvis and axilla. Depending on the appearance, they are categorized as macro-, micro-, and mixed-cystic. LMs can be diagnosed by medical history, physical examination, as well as ultrasound and MRI. Additionally, the lymphatic endothelium marker Poloplanin D2-40 may facilitate diagnosis [ 62 , 63 ]. Masthoff et al. (2018) reported that MSOT may be a promising tool in diagnosing lymphatic malformations, since it has been shown to distinguish other types of vascular malformations [ 64 ].
During surgery, trauma of lymphatic vessels may result in a postoperative leakage of lymphatic fluid. Different kinds of these postoperative lymphatic leakages have been described, e.g., lymphatic ascites, lymphorrhea, chylothorax, chylous ascites, or chylorrhea [ 65 ]. Chylous thoracic or abdominal effusions can, for example, be treated via transinguinal lymphangiography using lipoidol [ 66 ]. Further, thoracic duct embolization (TDE) has shown to be an alternative treatment option for chylous leaks. A high rate of success, together with minimal occurrence of complications, have been reported [ 67 ].
3.2. Clinical Assessment of Lymphedema
Diagnosis of lymphedema can be challenging due to the high variabilities in etiology and underlying mechanism in the development of lymphedema and due to the fact that it is not as easy to be differentiated from other forms of edema. This often leads to lymphedema being underdiagnosed and undertreated. The variable way by which lymphedema is clinically diagnosed and defined is a confounding attribute in the diagnosis process [ 38 , 68 , 69 ]. However, it is important to diagnose and treat lymphedema as soon as possible, as the early detection of the disease is crucial for therapy approaches and outcome, as well as for limiting disease progression. A recent study including 149 patients showed that early detection, along with a simple intervention (which was up to six weeks of self-massage by the patient and usage of a compression garment), can be highly effective in patients at risk of BCRL [ 70 ]. Unfortunately, early stages of lymphedema cannot always be easily differentiated from other causes, leading to edema, as e.g., obesity or venous diseases [ 39 ]. Schook et al. (2011) reported that, in 27% of pediatric patients, other anomalies, such as post-traumatic swellings or lipedema, are mistaken for lymphedema [ 71 ]. Standard diagnostic tools do not usually enable the diagnosis of lymphedema at a subclinical stage.
Although several genes and biomarkers that are associated with lymphedema have been investigated [ 72 , 73 ], up to now most of the diagnoses are performed via clinical history and examination, including aspects that are related to family history and carrying out detailed physical examination involving palpation and skin inspection [ 39 , 74 ]. In the patients’ history, crucial aspects include, e.g., cancer treatment or trauma as well as signs of typical symptoms (swelling, skin changes, and recurrent infections). The Stemmer sign is one of the most reported clinical signs in diagnosing the presence of lymphedema. If it is not possible to pinch a skinfold on the second toe, it is considered positive [ 75 ]. In a study, lymphatic function was tested using lymphoscintigraphy in patients showing a positive Stemmer sign. The results from this study indicated that a positive Stemmer sign is indeed a reliable predictor for lymphedema [ 75 ]. Approximately 15% of the patients show skin changes, such as hyperkeratosis or lymphorrhea [ 71 ]. Other typical symptoms, which are often described by patients is the feeling of heaviness in the affected limb. Together with acute swelling, this is associated with a positive predictive value for the presence of lymphedema [ 73 ].
Especially in early stages, diagnosis of lymphedema can be challenging as changes in limb volume or circumference are not detectable. Tape measurement, water displacement, perometry, and bioelectrical impedance spectroscopy (BIS) are diagnostic tools with good reliability and validity. BIS is the only method that is currently available to detect stage I lymphedema. BIS enables the assessment of whole body composition as well as segmental composition (e.g., of the limbs). This method uses an electrical current to distinguish between total body water, extracellular, and intracellular fluid volumes based on the tissue resistances [ 76 ]. Tape measurement can be highly observer dependent. Therefore, perometry represents a more reliable tool with increased interobserver-reliability [ 77 ]. Imaging techniques (lymphoscintigraphy, lymphangiography, or computer tomography) are used to detect lymphatic flow impairment as an underlying mechanism [ 39 ].

3.3. Therapeutic Options
There is currently no definite cure available for lymphedema. However, various approaches have been investigated and they are currently researched. Ciudad et al. (2019) suggest that the treatment of lymphedema should start as early as possible. The reason for this is that progression of lymphedema into higher stages leads to fibrotic tissue changes and this destruction of possible remaining functional lymphatic vessels [ 78 ]. All of the following therapeutic approaches have a common goal: the reduction of accumulated fluid in the respective body part, by promoting and/or developing alternative pathways from deranged lymphatic structures to tissues where intact lymphatic flow properties can be found [ 79 ]. This serves the overall aim of improving functional status [ 78 ] and preventing disease progression [ 80 ].
3.3.1. Physical Therapy
Physical treatments include massages, lymphatic drainages, the application of different kind of compression garments, and intermittent pneumatic compression [ 81 ]. Natural compression can be simulated by intermitted pneumatic compression devices, which use a sequential airflow to inflate special hoses and, therefore, applying positive pressure on the tissue. A meta-analysis study showed its efficacy in patients that were diagnosed with secondary lymphedema [ 82 ]. It can be applied either alone or in combination with other physical therapies [ 82 ].
Gott et al. (2018) have described a novel therapeutic approach that uses the application of negative pressure (representing a pulling/opening force). While this approach has already been used in the field of wound healing, its use in lymphedema has not yet been fully investigated [ 83 ]. Another form of negative pressure uses kinesiology tapes. These tapes are used to decongest lymphatic fluid that accumulates under the skin. It is additionally recommended to compression bandages, for body parts where compression garments cannot be easily fitted and in cases where bandages could be uncomfortable [ 84 ]. A meta-analysis carried out showed that the quality of life (QoL) is higher in patients under treatment with kinesiological methods. However, the efficacy of this method was not proven in this study [ 84 ]. Davies et al. (2020) reported that the use of kinesiology tapes leads to the reduction of volume. However, they also state that this form of treatment is not superior when compared to other interventions [ 85 ].
Fascia manipulation [ 86 , 87 ], weight loss [ 43 , 88 , 89 , 90 ], heat treatment [ 91 ], or extracorporeal shock wave therapy [ 92 ] and far infrared radiation treatment [ 93 ] have also been used as therapeutical approaches. Currently, these approaches are mainly used in research, and are, therefore, not routinely applied. Further investigations in bigger clinical studies are needed. Please see Tzani et al. (2018) for further details on different physiotherapeutic approaches in lymphedema patients [ 81 ].
3.3.2. Innovative Drugs / Compounds for the Treatment of Lymphedema
Diuretics were believed to have a beneficial effect in some lymphedema patients. However, imbalance of electrolytes and fluid can occur with its usage and, therefore, administration is generally not recommended [ 79 ]. Benzopyrones may positively influence lymphatic fluid absorption by assisting in hydrolyzing proteins and activating the route of lymphatic transport [ 79 ]. However, this has not yet been confirmed in clinical studies. It did not improve limb volume or quality in life in lymphedema patients and, additionally, long-term administration can lead to adverse effects on the liver [ 94 ]. Another compound, Ketoprofen, reduced lymphedema in a mouse model. Ketoprofen is an anti-inflammatory agent [ 95 , 96 ]. Rockson et al. (2018) investigated the effect of anti-inflammatory therapy in an open-labeled and placebo-controlled study. They reported decreases in the thickness of the skin, decreases in the expression of granulocyte-colon-stimulating-factor-1 (GCSF), and changes in the histopathology of lymphedema tissue [ 95 ]. Decreased levels of GCSF, as seen following ketoprofen administration, might have a beneficial effect [ 95 ]. Further investigations are required to confirm these beneficial effects because this was only shown in a pilot study.
T-cells are believed to play a role in the development of lymphedema as they inhibit lymphatic angiogenesis and aid in tissue fibrosis. Therefore, Tacrolimus has been tested as immunosuppressive drug sensitive to CD4 + T-cells in animals [ 97 ]. This compound is also widely used in transplantation medicine in humans [ 98 ]. In terms of lymphedema, applied locally, it was able to prevent the formation of lymphedema, but also showed to be effective once lymphedema was already established. Again, this has only been investigated in animal models and clinical studies are required to confirm these results and provide additional information on the safety of this compound in humans [ 97 ].
Already in the early 1960s, a number of researchers reported the idea of using hyaluronidase treatment in lymphedema and deforming lymphedema stage III [ 99 , 100 , 101 ]. In an animal model of induced lymphedema, Roh et al. (2017) used hyaluronidase, which was injected into the lymphedema tissue. This led to the reduction in the limb with acquired lymphedema. They suggest that lymphangiogenesis is promoted by hyaluronidase and further, HA fragment size is modified by the enzyme. As low molecular weight hyaluronic acid has shown to promote LYVE-1 expression (a player in lymphangiogenesis), it was postulated that regulating HA fragment size might also modulate mechanism of lymphedema [ 30 ]. Therefore, this could potentially be used as a novel therapy in lymphedema patient. This, however, still needs to be confirmed and tested in clinical studies [ 30 ].
Another approach that has been investigated is VEGF-C delivery through gene therapy or injection. Animal studies suggest that VEGF-C delivery enhances lymphangiogenesis as well as the lymphatic pump function via a VEGF receptor 3 dependent mechanism [ 102 ], and it was able to reduce lymphedema [ 103 , 104 ]. A recent report has shown that Lymfactin ® , a combined adenoviral VEGF-C, in combination with lymph node transfer, is well tolerated in a phase I clinical trial including upper limb lymphedema patients [ 105 ].
Further, mesenchymal stem cells showed beneficial effects by differentiating into lymphatic endothelial like cells in several clinical studies [ 44 , 106 , 107 , 108 ]. However, no changes in arm volume were found in a follow up study (up to one year) as well as no significant improvement, being assessed via lymphoscintigraphy post-treatment with adipose-derived stem cells [ 109 ]. Hu et al. (2020) report a new promising approach in secondary lymphedema treatment by using adipose-derived stem cells; however, this still needs to be evaluated in larger clinical studies [ 110 ].
Overall, it appears that drug treatments / medications are not yet able to provide a safe and effective therapy for lymphedema. However, several approaches and compounds being actively used in animal and clinical studies could potentially provide innovative therapy options in the future [ 111 ]. Finally, surgical options are utilized if conservative therapy approaches do not show the expected successful outcomes (see [ 44 , 78 , 112 ]).
3.3.3. Surgical Approaches
More recently, innovative surgical procedures have been investigated in animal models and clinical studies. These are based on different factors, for example, advances in the field of microsurgery as well as novel insights into the lymphatic vasculature itself, and a better understanding of the underlying pathophysiology of lymphedema [ 78 ]. The surgical interventions can be separated into physiological and excisional procedures. Whereas, physiological procedures are aimed at promoting fluid flow properties, either by redirecting the lymphatic flow directly into the venous system or by providing new pathways, excisional procedures involve the removal of affected tissue parts. Table 1 , below, outlines the different surgical approaches in lymphedema.
Surgical approaches applied in lymphedema patients.
Lymphvenous Anastomosis (LVA) and vascularized lymph node transfer (VLNT) are the two most performed surgeries in lymphedema patients. During LVA surgery, a connection between the lymphatic structures and blood vessels is established. Although patients report an improvement in symptoms after LVA, applying compression garments is still required post-surgery. Evidence suggests that LVA is more effective in the upper limbs as compared to the lower extremities [ 78 ]. VLNT is performed in more advanced stages in lymphedema patients in which lymphatic vessels are dysfunctional and/or lymph nodes are not present. A range of donor sites have been described in the literature: Jejunal, gastroepiploic, ileocecal, appendicular, or supraclavicular lymph nodes. Different factors, e.g., prior exposition to radiation, scars, aesthetic appearance, or disease stage, are taken into account when choosing the recipient site [ 112 ]. Two theories on the underlying mechanisms have been suggested [ 78 ]: (1) accumulated fluid in the close area is absorbed by the nodes; and, (2) VEGF-C induced lymph angiogenesis by vascularized lymph nodes LVA and LVNT have both shown promising outcomes in clinical studies in terms of limb volume reduction and reduced episodes of cellulitis. However, no beneficial effect in reducing fibrosis has been observed. Additional future studies are required to evaluate the long-term outcomes of these interventional approaches [ 44 ].
In cases of fibroadipose hypertrophy, as can often be found in chronic lymphedema, suction assisted lipectomy (SAL) can be the surgery of choice. As this procedure shows minor improvement of lymphedema, wearing compression bandages lifelong is necessary in order to not risk recurrence [ 44 ]. Although the overall outcome is very much dependent on the patient and their strict following of the recommendations after surgery, its efficacy in long-term reduction of limb volume has been shown in different studies [ 78 ].
Radical reduction of lymphedema with perforator preservation is a mixture of physiological and excisional surgery, and while some studies show positive and long-term results, it needs outstanding microsurgical abilities, and it has a greater risk of scar forming, risk of contamination, necrosis, and longer operational times when compared to the above-mentioned approaches. It is typically used in advanced stages of lymphedema (stage III) [ 78 ]. The Charles procedure implies the complete removal of the skin and subcutaneous tissue from the impacted area and is performed to minimize excessive thickness and prevent inflammation, particularly in patients with advanced stage severe lymphedema. However, it shows very poor long-term results and is, therefore, obsolete [ 78 ].
4. Complete Decongestive Therapy
Up to date, there is no cure for lymphedema (except obesity induced lymphedema [ 89 , 113 ]). Although several therapeutic options, surgical and non-surgical, have been tested and are currently researched, the therapy of choice is a form of physical therapy that is known as complete/complex decongestive (physio-)therapy (CDT). This form of treatment is not curative for lymphedema, but mainly aims at reducing fluid volume as well as preventing the disease from progression [ 68 ].
4.1. Underlying Principles
CDT is an empirically driven and multicomponent therapy program [ 68 ]. It can generally be separated into two phases. Phase one involves manual lymphatic drainage (MLD), usage of multilayered compression bandages, carrying out physical exercises, and meticulous skin care. The second phase mainly focuses on self-care via elastic sleeves or compression stocks application as well as continuous exercise [ 114 ]. The main components of CDT include:
Manual Lymphatic Drainage (MLD) is performed to enhance lymphatic outflow. Lymph therapists use specific hand movements (rhythmic, flowing or stirring) with a pressure of 30—40 mmHg in a frequency that mimics the intrinsic frequency of the lymphangion (10/min). MLD is started in the area of healthy tissue and then expanded into adjacent areas where the obstructed vessels are located [ 115 , 116 ].
Compression bandages are applied, aiming at increasing interstitial pressure and therefore, to decrease capillary filtration [ 117 ] leading to a decrease in accumulated fluid/volume [ 115 , 116 ].
Physical exercise such as ergometry [ 118 ], aerobic exercise [ 119 ] and/or resistance exercise [ 120 ] as well as associated respiratory movements are believed to assist in increasing lymphatic flow, in reducing swelling and in improving muscle strength as well as quality of life in lymphedema patients [ 82 ].
Skin care and skin restauration [ 121 ].
Psychological support [ 38 ] as the disabling and debilitating characterizations from lymphedema are a huge psychological burden to the patient.
Educational seminars on skin care or nutrition [ 122 ].
4.2. Research into the Effects of Physical Therapy
As described above, the main aim and, therefore, outcome parameter of CDT is the reduction of overall volume and circumference of the affected part of the body, accompanied by improvements of functionality and quality of life. Several studies compare volume and circumference changes before and after different forms of therapy [ 114 , 123 ], with different durations reaching from six days intensive therapy [ 124 ] up to several months of treatment [ 70 , 125 , 126 ]. Water displacement [ 127 ], perometry [ 128 ], and tape measurement of the limb circumference [ 129 ] are the standard methods for these assessments. Apart from the key aspects of CDT (MLD and compression), modified treatments, such as other compression garments or duration and/or composition of therapy, have been investigated [ 91 , 130 , 131 , 132 ]. Overall, there appears to be a lack of existing literature related to the amount of fluid, which is mobilized by CDT, where this fluid is shifted to, and how the body responds to the additional mobilized fluid. Table 2 provides an overview of the effects of lymphedema per se as well as lymphedema therapy, specifically physical therapy, as in complete decongestive treatment: what is known, the knowledge gaps and how they can potentially be addressed.
Overview of lymphedema and lymphedema therapy, current knowledge, knowledge gaps, and how those can potentially be addressed.
4.2.1. Studying Fluid Shifts Caused by Treatment
As described above, the reduction of overall volume and circumference of the affected part of the body, accompanied by improvements of functionality and quality of life, is the main aim and, therefore, outcome parameter of CDT. Questionnaires are mostly used to assess changes in quality of life of the patients [ 114 , 123 ]. Water displacement [ 127 ], perometry [ 128 ] and tape measurement of the limb circumference [ 129 ] are the standard methods for these assessments. Overall, there appears to be a lack of existing literature related to the amount of fluid, which is mobilized by the CDT, where this fluid is shifted to, and how the body responds to, the additional mobilized fluid. Bioelectrical impedance analysis (BIA) or Bioelectrical impedance spectroscopy (BIS) are methods that enable not only the diagnosis of lymphedema, by calculating the ratio between a healthy and affected leg, but distinguishing between extracellular and intracellular fluids [ 133 ]. Using BIS, Pereira de Godoy et al. (2013) determined how much fluid is mobilized following seven days of intensive physical therapy in patients with lower limb lymphedema [ 134 ]. They observed decreases in total water, but increases in intracellular water in the affected limb. They interprete their findings as indicative of fluid mobilization from the affected limb to healthy parts of the body, as they observed increases the total water in the trunk and upper extremities [ 134 ]. A more recent study from the same research group was only partially able to confirm these results, as they found a reduction of intracellular and extracellular water following therapy in the legs and increased levels of intra- and extracellular water, in the trunk and upper limbs [ 124 ]. However, these findings were only assessed prior- and post- physical therapy of seven days. Recently, we tested the hypothesis that fluid mobilization or fluid shifts to different parts of the body induced by CDT will be reflected in plasma volume changes (PVC) and plasma composition. As lymphedema therapy (CDT) mobilizes lymphatic fluid outflow—which means a greater return of lymphatic fluid into the blood circulation—an increase in plasma volume at the level of amount of fluid mobilized from the lymphatic system should be expected. As different equations have been previously used to calculate relative changes in plasma volume, we utilized them in our study. To calculate the relative change in plasma volume, each of these equations uses different blood sample parameters. For example, some equations are based on changes in plasma density [ 135 ], hematocrit [ 136 ], hematocrit and hemoglobin [ 137 ], and both anthropometric data and hematocrit [ 138 ]. While most of these equations calculate relative changes in plasma volume [ 135 , 136 , 137 ], the equation according to Nadler [ 138 ] estimates absolute changes in plasma volume. Changes in plasma volume, especially central hypervolemia, are associated with changes in plasma protein (total protein, albumin, and albumin/globulin ratio), oncotic pressure, electrolyte concentrations (sodium, chloride, and potassium), osmolality, volume regulating hormones, and blood pressure. We observed that fluid shifts occur due to physical therapy and manual lymphatic drainage [ 139 ]. Manual lymphatic drainage affects the limbs and whole-body fluid composition. Fluid shifts due to manual lymphatic drainage are also reflected in plasma volume increases as well as plasma protein increases. All four formulae for plasma volume changes calculations led to similar results. This could be an indirect indicator of the concentration and composition of lymphatic fluid entering into the blood stream through the thoracic duct. Because plasma volume increases due to physical therapy could be associated with compensatory hemodynamic—and volume regulatory hormonal—responses, these aspects should be examined in future studies.
4.2.2. Studying Lymphedema Treatment Effects on Orthostatic Intolerance
Sodium homeostasis has been shown to play an important role in blood pressure regulation [ 5 ]. Animal studies have shown that lymphatic vessels as well as macrophages contribute to both blood pressure control and balance of interstitial fluid [ 140 ]. Sodium is stored in the skin, where it is found bound to proteoglycans without water retention [ 141 ]. Further investigations have shown that VEGF-C and VEGFR-2 also have some role in blood pressure regulation [ 142 ], as the accumulation of sodium together with a higher blood pressure was seen upon inhibition of those [ 5 ]. When patients displaying refractory hypertension symptoms were compared to controls with normal blood pressure levels, higher concentrations of VEGF-C were found in the plasma [ 143 ]. This could be based on the following hypotheses [ 5 ]: the lymphatic system facilitates enhanced interstitial sodium clearance, which is controlled by kidney excretion, and/or that VEGFR-2 mediates the production of endothelial nitric oxide (NO) production and, therefore, vasodilation.
Orthostasis describes an upright posture, as during standing. During an upright posture, the cardiovascular system is affected by gravitational forces, leading to a reduction in blood pressure, as a certain amount of blood is pooled in the lower body. If the cardiovascular system is not able to counteract this blood pressure drop, this can lead to symptoms of fainting, a loss of consciousness, known as syncope, as the mean arterial pressure cannot be stabilized [ 144 , 145 ]. This can be a major problem in people having a history of feeling dizzy when standing up or also in older people. Syncope occurs due to the inability of the cardiovascular system to maintain a certain level of the mean arterial pressure (MAP) during an orthostatic challenge (standing up), which further leads to a critically reduced cerebral blood flow. Hormonal factors [ 146 , 147 ], issues in cerebral autoregulation [ 148 ], dysfunction within the autonomic system [ 149 ], or cardiac problems [ 150 ] are only a few examples of the factors that are involved in the etiology of syncope.
The mechanisms of Falls: Role of Cardio-Postural Interactions and Medications
The supposedly simple task of standing up, the transition from a supine or sitting to a standing position, contributes to approximately 40% of all falls [ 151 ]. While age associated muscle function and structural changes in the muscles (sarcopenia) contributes to falls in the elderly, increasing numbers of falls due to orthostatic hypotension are seen. Deranged motor control has been reported as the most important reason that is involved in this mechanism. Further key factors involved are cardio-postural regulation and cerebral perfusion [ 152 ]. Additionally, medications, such as diuretics or anti-hypertensive therapy, have been known to cause falls [ 153 ]. Therefore, the increased risk of collapse after medication is related to impaired cardio-postural and deranged cerebral perfusion. This also needs to be considered when medications are prescribed for lymphedema patients.
Alteration of Cardio-Postural Interactions during Lymphedema Treatment?
Different external and internal stimuli can affect posture in everyday life and, therefore, imposes a risk of stable standing balance. The ability to detect disturbances in posture and to react accordingly is required to maintain this balance. Age plays an important role here. It has been noted that these abilities are negatively correlated with age, as they deteriorate with higher age, and could, therefore, lead to imbalance and an increased risk of falls [ 154 , 155 , 156 , 157 ]. The higher occurrence of falls because of postural hypotension, together with the loss of postural stability, is of major concern not only in older people, but also in patients. Similar changes in cardio-postural control and blood pressure regulation may also occur in patients with lymphedema due to different fluid volumes in the legs, especially when comparing pre - to post - treatment in these patients.
Esmer et al. (2019) investigated the hemodynamic responses to MLD different body regions. They observed a reduction in systolic blood pressure after MLD in the neck, abdomen, and the lower limbs. Heart rate seemed to decrease after massage in the arms. Diastolic blood pressure showed decreased values after MLD in the neck and legs, but increased after abdominal MLD. Esmer et al. (2019) demonstrated different acute responses of the hemodynamic system, depending on the body part treated by MLD [ 158 ]. However, they only investigated the effects due to MLD on blood pressure, but no cardio postural interaction was assessed during MLD and throughout the several weeks of CDT.
Cardio-postural interaction is a combination of postural sway, electromyography of the legs (EMG), blood pressure (BP), and electrocardiogram (ECG) measurements. This could be investigated by a simple sit-to-stand test [ 159 , 160 ]. Based on this model, we have developed a system to collect, integrate, and analyze these signals to provide an integrated approach of assessing interactions between the cardiovascular and postural control [ 150 , 161 ] during therapy. This blood pressure regulation and cardio-postural responses to orthostatic challenge could differ in patients with lymphedema as compared to healthy controls, due to the amount of fluid, which is mobilized during therapy. Research should be carried out in the future regarding how lymphedema influences cardio-postural interactions.
4.2.3. Vascular/Endothelial (dys-)function
Atherosclerosis is a chronic inflammatory disease, which involves the inner layer of the arterial wall. Plaques are built within the inner lumen of the vessels. These lead to the narrowing of the artery. Atherosclerosis is a disease that develops over several years or decades. Two essential processes are a part of disease development: the recruitment of immune cells and accumulation of cholesterol [ 50 ]. How these two aspects work together in this process is not yet fully elucidated. However, what is known is that the removal of cholesterol from the endothelium of the vessel has been directly linked to the regression of the disease [ 162 ]. A process known as reverse cholesterol transport (RCT) and, further, high-density lipoprotein (HDL) formation, is involved in this removal [ 163 ]. The lymphatic vasculature was only recently associated with the transport of HDL from the interstitial space into the blood stream [ 50 , 164 , 165 ]. In a study by Lim et al. (2013), VEGF-C administration enhanced lymphangiogenesis and further lead to reduced levels of cholesterol through an improvement of RCT. Moreover, in surgically induced lymphedema, a reduction of RCT of about 20% was observed [ 164 ]. Similar to this, a reduction of 77% in RCT was found in a model with no dermal lymphatic structures [ 165 ]. Taking this into account, the lymphatic vessels are reported to be actively involved in lipoprotein metabolism and cholesterol levels in the plasma. Moreover, the lymphatic vasculature is of importance for RCT function [ 5 , 166 , 167 ].
As part of atherosclerosis, endothelial dysfunction can occur, and it is a main predictor of cardiovascular diseases. Endothelial cells are not only the inner layer of the vascular lumen, but they also contribute to blood flow properties and, therefore, blood pressure regulation. Endothelial cells can either release vasoconstrictors, such as endothelin (ET) or platelet-activating factor (PAF), or vasodilators, such as nitric oxide (NO) or prostacyclin (PGI2). Different factors can stimulate further NO production via the endothelial nitric oxide synthase (eNOS) [ 168 ]. One of these important factors is the shear stress on the vessel wall [ 169 ]. During standing up or during exercise, shear stress is increased and it stimulates an increased NO production [ 170 ]. These increased levels of NO result in a flow-mediated dilatation (FMD) in large arteries. Endothelial dysfunction, and in specific NO reduction, is thought to be a driving factor in hypertension pathogenesis [ 171 ], atherosclerosis, and other cardiovascular disorders [ 172 ]. If endothelial dysfunction is detected at an early stage, then it can be reversed via different clinical approaches.
We have previously reported that lymphedema therapy affects endothelial function in lymphedema patients undergoing three weeks of complete decongestive therapy [ 173 ]. Methods for studying endothelial and vascular function are flow-mediated dilatation (FMD), EndoPAT2000, pulse wave velocity (PVW), and retinal imaging. All of these are non-invasive and easy to use also in patients. Flow mediated dilatation (FMD) is an ultrasound-based measurement that can be used to determine brachial artery vascular reactivity after occluding and releasing blood flow [ 174 , 175 ]. Endothelial vasodilator function can be assessed by measuring changes in volume using probes in the fingertips. Arterial stiffness can be investigated by measuring pulse wave velocity (PWV). Blood pressure cuffs are applied at different parts of the body to e.g., determine carotid-femoral (PWVcf) or brachial-ankle pulse wave velocity (PWVba) [ 176 ]. Another innovative and unique opportunity to assess retinal microvasculature changes via retinal fundoscopy. This method can be used to analyze retinal arterioles and venules characteristics from a single picture taken with a fundus camera. Arteriolar-to-venous ratio, vessel diameter, and vessel tortuosity index can be measured [ 177 , 178 , 179 , 180 ].
5. Conclusions and Recommendations
This review summarizes the current knowledge that is related to the lymphatic system and examined the lymphatic system and lymphedema from a variety of perspectives. While several reviews have been published related to the biology of the lymphatic system and lymphedema, the physiological alternations, which arise due to disturbances of this system (e.g., in lymphedema), and during lymphedema therapy, are poorly understood ( Table 2 ). Therefore, there is a need for future investigations aiming at studying in-detail aspects that are related to fluid regulation/mobilization, hemodynamic responses, and endothelial and/or vascular changes and how they are altered in lymphedema as well as due to lymphedema therapy.
Author Contributions
Writing—original draft preparation, B.B., O.S., A.O., C.U., A.R. and N.G.; writing—review and editing, B.B., O.S., A.O., C.U., A.R. and N.G.; funding acquisition, O.S. and N.G. All authors have read and agreed to the published version of the manuscript.
This project was partly funded by the Austrian Scientific & Technological Cooperation (OeAD), grant number: CZ8/2019.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Data availability statement, conflicts of interest.
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
- 1. Breslin J.W., Yang Y., Scallan J.P., Sweat R.S., Adderley S.P., Murfee W.L. Lymphatic Vessel Network Structure and Physiology. Compr. Physiol. 2018;9:207–299. doi: 10.1002/cphy.c180015. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 2. Schmid-Schonbein G.W. Microlymphatics and lymph flow. Physiol. Rev. 1990;70:987–1028. doi: 10.1152/physrev.1990.70.4.987. [ DOI ] [ PubMed ] [ Google Scholar ]
- 3. Moore J.E., Jr., Bertram C.D. Lymphatic System Flows. Annu. Rev. Fluid Mech. 2018;50:459–482. doi: 10.1146/annurev-fluid-122316-045259. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 4. Breslin J.W. Mechanical forces and lymphatic transport. Microvasc. Res. 2014;96:46–54. doi: 10.1016/j.mvr.2014.07.013. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 5. Telinius N., Hjortdal V.E. Role of the lymphatic vasculature in cardiovascular medicine. Heart. 2019;105:1777–1784. doi: 10.1136/heartjnl-2018-314461. [ DOI ] [ PubMed ] [ Google Scholar ]
- 6. Oliver G., Kipnis J., Randolph G.J., Harvey N.L. The Lymphatic Vasculature in the 21st Century: Novel Functional Roles in Homeostasis and Disease. Cell. 2020;182:270–296. doi: 10.1016/j.cell.2020.06.039. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 7. Hsu M.C., Itkin M. Lymphatic Anatomy. Tech. Vasc. Interv. Radiol. 2016;19:247–254. doi: 10.1053/j.tvir.2016.10.003. [ DOI ] [ PubMed ] [ Google Scholar ]
- 8. Levick J.R., Michel C.C. Microvascular fluid exchange and the revised Starling principle. Cardiovasc. Res. 2010;87:198–210. doi: 10.1093/cvr/cvq062. [ DOI ] [ PubMed ] [ Google Scholar ]
- 9. Lynch P.M., Delano F.A., Schmid-Schönbein G.W. The primary valves in the initial lymphatics during inflammation. Lymphat. Res. Biol. 2007;5:3–10. doi: 10.1089/lrb.2007.5102. [ DOI ] [ PubMed ] [ Google Scholar ]
- 10. Trzewik J., Mallipattu S.K., Artmann G.M., Delano F.A., Schmid-Schönbein G.W. Evidence for a second valve system in lymphatics: Endothelial microvalves. FASEB J. 2001;15:1711–1717. doi: 10.1096/fj.01-0067com. [ DOI ] [ PubMed ] [ Google Scholar ]
- 11. Scallan J.P., Zawieja S.D., Castorena-Gonzalez J.A., Davis M.J. Lymphatic pumping: Mechanics, mechanisms and malfunction. J. Physiol. 2016;594:5749–5768. doi: 10.1113/JP272088. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 12. Armenio S., Cetta F., Tanzini G., Guercia C. Spontaneous contractility in the human lymph vessels. Lymphology. 1981;14:173–178. [ PubMed ] [ Google Scholar ]
- 13. Olszewski W.L., Engeset A., Sokolowski J. Lymph flow and protein in the normal male leg during lying, getting up, and walking. Lymphology. 1977;10:178–183. [ PubMed ] [ Google Scholar ]
- 14. Gashev A.A., Davis M.J., Delp M.D., Zawieja D.C. Regional variations of contractile activity in isolated rat lymphatics. Microcirculation. 2004;11:477–492. doi: 10.1080/10739680490476033. [ DOI ] [ PubMed ] [ Google Scholar ]
- 15. Gasheva O.Y., Zawieja D.C., Gashev A.A. Contraction-initiated NO-dependent lymphatic relaxation: A self-regulatory mechanism in rat thoracic duct. J. Physiol. 2006;575:821–832. doi: 10.1113/jphysiol.2006.115212. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 16. Scallan J.P., Davis M.J., Huxley V.H. Permeability and contractile responses of collecting lymphatic vessels elicited by atrial and brain natriuretic peptides. J. Physiol. 2013;591:5071–5081. doi: 10.1113/jphysiol.2013.260042. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 17. Adair T.H., Guyton A.C. Modification of lymph by lymph nodes. III. Effect of increased lymph hydrostatic pressure. Am. J. Physiol. 1985;249:H777–H782. doi: 10.1152/ajpheart.1985.249.4.H777. [ DOI ] [ PubMed ] [ Google Scholar ]
- 18. Hansen K.C., D’Alessandro A., Clement C.C., Santambrogio L. Lymph formation, composition and circulation: A proteomics perspective. Int. Immunol. 2015;27:219–227. doi: 10.1093/intimm/dxv012. [ DOI ] [ PubMed ] [ Google Scholar ]
- 19. Renkin E.M. Some consequences of capillary permeability to macromolecules: Starling’s hypothesis reconsidered. Am. J. Physiol. 1986;250:H706–H710. doi: 10.1152/ajpheart.1986.250.5.H706. [ DOI ] [ PubMed ] [ Google Scholar ]
- 20. Gannon B.J., Carati C.J. Endothelial distribution of the membrane water channel molecule aquaporin-1: Implications for tissue and lymph fluid physiology? Lymphat. Res. Biol. 2003;1:55–66. doi: 10.1089/15396850360495709. [ DOI ] [ PubMed ] [ Google Scholar ]
- 21. Adamczyk L.A., Gordon K., Kholova I., Meijer-Jo rna L.B., Telinius N., Gallagher P.J., van der Wal A.C., Baandrup U. Lymph vessels: The forgotten second circulation in health and disease. Virchows Arch. 2016;469:3–17. doi: 10.1007/s00428-016-1945-6. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 22. Alitalo K. The lymphatic vasculature in disease. Nat. Med. 2011;17:1371–1380. doi: 10.1038/nm.2545. [ DOI ] [ PubMed ] [ Google Scholar ]
- 23. Notohamiprodjo M., Weiss M., Baumeister R.G., Sommer W.H., Helck A., Crispin A., Reiser M.F., Herrmann K.A. MR lymphangiography at 3.0 T: Correlation with lymphoscintigraphy. Radiology. 2012;264:78–87. doi: 10.1148/radiol.12110229. [ DOI ] [ PubMed ] [ Google Scholar ]
- 24. Mazzei F.G., Gentili F., Guerrini S., Cioffi Squitieri N., Guerrieri D., Gennaro P., Scialpi M., Volterrani L., Mazzei M.A. MR Lymphangiography: A Practical Guide to Perform It and a Brief Review of the Literature from a Technical Point of View. BioMed Res. Int. 2017;2017:2598358. doi: 10.1155/2017/2598358. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 25. Pieper C.C., Feisst A., Schild H.H. Contrast-enhanced Interstitial Transpedal MR Lymphangiography for Thoracic Chylous Effusions. Radiology. 2020;295:458–466. doi: 10.1148/radiol.2020191593. [ DOI ] [ PubMed ] [ Google Scholar ]
- 26. Chavhan G.B., Lam C.Z., Greer M.C., Temple M., Amaral J., Grosse-Wortmann L. Magnetic Resonance Lymphangiography. Radiol. Clin. N. Am. 2020;58:693–706. doi: 10.1016/j.rcl.2020.02.002. [ DOI ] [ PubMed ] [ Google Scholar ]
- 27. Giacalone G., Yamamoto T., Belva F., Hayashi A. Bedside 3D Visualization of Lymphatic Vessels with a Handheld Multispectral Optoacoustic Tomography Device. J. Clin. Med. 2020;9:815. doi: 10.3390/jcm9030815. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 28. Polomska A.K., Proulx S.T. Imaging technology of the lymphatic system. Adv. Drug Deliv. Rev. 2020 doi: 10.1016/j.addr.2020.08.013. [ DOI ] [ PubMed ] [ Google Scholar ]
- 29. Rössler A., Fink M., Goswami N., Batzel J.J. Modeling of hyaluronan clearance with application to estimation of lymph flow. Physiol. Meas. 2011;32:1213–1238. doi: 10.1088/0967-3334/32/8/014. [ DOI ] [ PubMed ] [ Google Scholar ]
- 30. Roh K., Cho S., Park J.-h., Yoo B.C., Kim W.-K., Kim S.-k., Park K., Kang H., Ku J.-m., Yeom C.-H., et al. Therapeutic effects of hyaluronidase on acquired lymphedema using a newly developed mouse limb model. Exp. Biol. Med. 2017;242:584–592. doi: 10.1177/1535370216688570. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 31. Rossler A., Hinghofer-Szalkay H. Hyaluronan fragments: An information-carrying system? Horm. Metab. Res. 2003;35:67–68. doi: 10.1055/s-2003-39062. [ DOI ] [ PubMed ] [ Google Scholar ]
- 32. Hinghofer-Szalkay H.G., Mekonen W., Rossler A., Schwaberger G., Lamprecht M., Hofmann P. Post-exercise decrease of plasma hyaluronan: Increased clearance or diminished production? Physiol. Res. 2002;51:139–144. [ PubMed ] [ Google Scholar ]
- 33. Rössler A., László Z., Kvas E., Hinghofer-Szalkay H.G. Plasma hyaluronan concentration: No circadian rhythm but large effect of food intake in humans. Eur. J. Appl. Physiol. Occup. Physiol. 1998;78:573–577. doi: 10.1007/s004210050463. [ DOI ] [ PubMed ] [ Google Scholar ]
- 34. Liu N.-F., Zhang L. Changes of tissue fluid hyaluronan (hyaluronic acid) in peripheral lymphedema. Lymphology. 1998;31:173–179. [ PubMed ] [ Google Scholar ]
- 35. Brix B., Apich G., Rössler A., Walbrodt S., Goswami N. Effects of physical therapy on hyaluronan clearance and volume regulating hormones in lower limb lymphedema patients: A pilot study. Sci. Prog. 2021;104:36850421998485. doi: 10.1177/0036850421998485. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 36. Goswami N., Roessler A., Haditsch B., Hinghofer-Szalkay H., Schneditz D. Paradoxical clearance of hyaluronan fragments during haemodialysis and haemodiafiltration. Nephrol. Dial. Transplant. 2012;27:4420–4422. doi: 10.1093/ndt/gfs266. [ DOI ] [ PubMed ] [ Google Scholar ]
- 37. Liu N.F., Olszewski W. The influence of local hyperthermia on lymphedema and lymphedematous skin of the human leg. Lymphology. 1993;26:28–37. [ PubMed ] [ Google Scholar ]
- 38. Rockson S.G., Rivera K.K. Estimating the population burden of lymphedema. Ann. N. Y. Acad. Sci. 2008;1131:147–154. doi: 10.1196/annals.1413.014. [ DOI ] [ PubMed ] [ Google Scholar ]
- 39. Kayıran O., De La Cruz C., Tane K., Soran A. Lymphedema: From diagnosis to treatment. Turk. J. Surg. 2017;33:51–57. doi: 10.5152/turkjsurg.2017.3870. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 40. Maclellan R.A., Couto R.A., Sullivan J.E., Grant F.D., Slavin S.A., Greene A.K. Management of Primary and Secondary Lymphedema: Analysis of 225 Referrals to a Center. Ann. Plast. Surg. 2015;75:197–200. doi: 10.1097/SAP.0000000000000022. [ DOI ] [ PubMed ] [ Google Scholar ]
- 41. Gasparis A.P., Kim P.S., Dean S.M., Khilnani N.M., Labropoulos N. Diagnostic approach to lower limb edema. Phlebology. 2020;35:650–655. doi: 10.1177/0268355520938283. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 42. Grada A.A., Phillips T.J. Lymphedema: Pathophysiology and clinical manifestations. J. Am. Acad. Dermatol. 2017;77:1009–1020. doi: 10.1016/j.jaad.2017.03.022. [ DOI ] [ PubMed ] [ Google Scholar ]
- 43. Borman P. Lymphedema diagnosis, treatment, and follow-up from the view point of physical medicine and rehabilitation specialists. Turk. J. Phys. Med. Rehabil. 2018;64:179–197. doi: 10.5606/tftrd.2018.3539. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 44. Schaverien M.V., Coroneos C.J. Surgical Treatment of Lymphedema. Plast. Reconstr. Surg. 2019;144:738–758. doi: 10.1097/PRS.0000000000005993. [ DOI ] [ PubMed ] [ Google Scholar ]
- 45. Moffatt C.J., Franks P.J., Doherty D.C., Williams A.F., Badger C., Jeffs E., Bosanquet N., Mortimer P.S. Lymphoedema: An underestimated health problem. Qjm. 2003;96:731–738. doi: 10.1093/qjmed/hcg126. [ DOI ] [ PubMed ] [ Google Scholar ]
- 46. Neuhüttler S., Brenner E. Beitrag zur Epidemiologie des Lymphödems. Phlebologie. 2018;35:181–187. doi: 10.1055/s-0037-1622142. [ DOI ] [ Google Scholar ]
- 47. Keeley V., Franks P., Quere I., Mercier G., Michelini S., Cestari M., Borman P., Hughes A., Clark K., Lisle J., et al. LIMPRINT in Specialist Lymphedema Services in United Kingdom, France, Italy, and Turkey. Lymphat. Res. Biol. 2019;17:141–146. doi: 10.1089/lrb.2019.0021. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 48. Mortimer P.S., Rockson S.G. New developments in clinical aspects of lymphatic disease. J. Clin. Investig. 2014;124:915–921. doi: 10.1172/JCI71608. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 49. Maltese P.E., Michelini S., Ricci M., Maitz S., Fiorentino A., Serrani R., Lazzerotti A., Bruson A., Paolacci S., Benedetti S., et al. Increasing evidence of hereditary lymphedema caused by CELSR1 loss-of-function variants. Am. J. Med. Genet. A. 2019;179:1718–1724. doi: 10.1002/ajmg.a.61269. [ DOI ] [ PubMed ] [ Google Scholar ]
- 50. Aspelund A., Robciuc M.R., Karaman S., Makinen T., Alitalo K. Lymphatic System in Cardiovascular Medicine. Circ. Res. 2016;118:515–530. doi: 10.1161/CIRCRESAHA.115.306544. [ DOI ] [ PubMed ] [ Google Scholar ]
- 51. Brice G., Child A.H., Evans A., Bell R., Mansour S., Burnand K., Sarfarazi M., Jeffery S., Mortimer P. Milroy disease and the VEGFR-3 mutation phenotype. J. Med. Genet. 2005;42:98–102. doi: 10.1136/jmg.2004.024802. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 52. Mellor R.H., Tate N., Stanton A.W., Hubert C., Mäkinen T., Smith A., Burnand K.G., Jeffery S., Levick J.R., Mortimer P.S. Mutations in FOXC2 in humans (lymphoedema distichiasis syndrome) cause lymphatic dysfunction on dependency. J. Vasc. Res. 2011;48:397–407. doi: 10.1159/000323484. [ DOI ] [ PubMed ] [ Google Scholar ]
- 53. Kerchner K., Fleischer A., Yosipovitch G. Lower extremity lymphedema update: Pathophysiology, diagnosis, and treatment guidelines. J. Am. Acad. Dermatol. 2008;59:324–331. doi: 10.1016/j.jaad.2008.04.013. [ DOI ] [ PubMed ] [ Google Scholar ]
- 54. WHO Fact sheet. [(accessed on 4 February 2021)];Lymphatic Filariasis. Available online: https://www.who.int/news-room/fact-sheets/detail/lymphatic-filariasis .
- 55. Cormier J.N., Askew R.L., Mungovan K.S., Xing Y., Ross M.I., Armer J.M. Lymphedema beyond breast cancer: A systematic review and meta-analysis of cancer-related secondary lymphedema. Cancer. 2010;116:5138–5149. doi: 10.1002/cncr.25458. [ DOI ] [ PubMed ] [ Google Scholar ]
- 56. Bar Ad V., Cheville A., Solin L.J., Dutta P., Both S., Harris E.E. Time course of mild arm lymphedema after breast conservation treatment for early-stage breast cancer. Int. J. Radiat. Oncol. Biol. Phys. 2010;76:85–90. doi: 10.1016/j.ijrobp.2009.01.024. [ DOI ] [ PubMed ] [ Google Scholar ]
- 57. Allam O., Park K.E., Chandler L., Mozaffari M.A., Ahmad M., Lu X., Alperovich M. The impact of radiation on lymphedema: A review of the literature. Gland. Surg. 2020;9:596–602. doi: 10.21037/gs.2020.03.20. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 58. Tiwari A. Differential Diagnosis, Investigation, and Current Treatment of Lower Limb Lymphedema. Arch. Surg. 2003;138:152. doi: 10.1001/archsurg.138.2.152. [ DOI ] [ PubMed ] [ Google Scholar ]
- 59. Newman B., Lose F., Kedda M.A., Francois M., Ferguson K., Janda M., Yates P., Spurdle A.B., Hayes S.C. Possible genetic predisposition to lymphedema after breast cancer. Lymphat. Res. Biol. 2012;10:2–13. doi: 10.1089/lrb.2011.0024. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 60. Muambangu J.P., Lukenze Jacques T. Genetic Risk Factors of Secondary Lymphedema in African Breast Cancer Population. J. Oncol. Res. Ther. 2018;4:147. [ Google Scholar ]
- 61. Michelini S., Vettori A., Maltese P.E., Cardone M., Bruson A., Fiorentino A., Cappellino F., Sainato V., Guerri G., Marceddu G., et al. Genetic Screening in a Large Cohort of Italian Patients Affected by Primary Lymphedema Using a Next Generation Sequencing (NGS) Approach. Lymphology. 2016;49:57–72. [ PubMed ] [ Google Scholar ]
- 62. Müller-Wille R., Wildgruber M., Sadick M., Wohlgemuth W.A. Vascular Anomalies (Part II): Interventional Therapy of Peripheral Vascular Malformations. RöFo. 2018;190:927–937. doi: 10.1055/s-0044-101266. [ DOI ] [ PubMed ] [ Google Scholar ]
- 63. Sadick M., Müller-Wille R., Wildgruber M., Wohlgemuth W.A. Vascular Anomalies (Part I): Classification and Diagnostics of Vascular Anomalies. RöFo. 2018;190:825–835. doi: 10.1055/a-0620-8925. [ DOI ] [ PubMed ] [ Google Scholar ]
- 64. Masthoff M., Helfen A., Claussen J., Karlas A., Markwardt N.A., Ntziachristos V., Eisenblätter M., Wildgruber M. Use of Multispectral Optoacoustic Tomography to Diagnose Vascular Malformations. JAMA Dermatol. 2018;154:1457–1462. doi: 10.1001/jamadermatol.2018.3269. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 65. Lv S., Wang Q., Zhao W., Han L., Wang Q., Batchu N., Ulain Q., Zou J., Sun C., Du J., et al. A review of the postoperative lymphatic leakage. Oncotarget. 2017;8:69062–69075. doi: 10.18632/oncotarget.17297. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 66. Pieper C.C., Hur S., Sommer C.M., Nadolski G., Maleux G., Kim J., Itkin M. Back to the Future: Lipiodol in Lymphography-From Diagnostics to Theranostics. Investig. Radiol. 2019;54:600–615. doi: 10.1097/RLI.0000000000000578. [ DOI ] [ PubMed ] [ Google Scholar ]
- 67. Chen E., Itkin M. Thoracic duct embolization for chylous leaks. Semin. Interv. Radiol. 2011;28:63–74. doi: 10.1055/s-0031-1273941. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 68. Rockson S.G. Diagnosis and Management of Lymphatic Vascular Disease. J. Am. Coll. Cardiol. 2008;52:799–806. doi: 10.1016/j.jacc.2008.06.005. [ DOI ] [ PubMed ] [ Google Scholar ]
- 69. Wilting J., Bartkowski R., Baumeister R.G., Földi E., Stöhr S., Strubel G., Schrader K., Traber J. S2k Leitlinie: Diagnostik und Therapie der Lymphödeme. [(accessed on 1 October 2020)]; Available online: https://www.awmf.org/uploads/tx_szleitlinien/058-001l_S2k_Diagnostik_und_Therapie_der_Lymphoedeme_2019-07.pdf .
- 70. Kilgore L.J., Korentager S.S., Hangge A.N., Amin A.L., Balanoff C.R., Larson K.E., Mitchell M.P., Chen J.G., Burgen E., Khan Q.J., et al. Reducing Breast Cancer-Related Lymphedema (BCRL) Through Prospective Surveillance Monitoring Using Bioimpedance Spectroscopy (BIS) and Patient Directed Self-Interventions. Ann. Surg. Oncol. 2018;25:2948–2952. doi: 10.1245/s10434-018-6601-8. [ DOI ] [ PubMed ] [ Google Scholar ]
- 71. Schook C.C., Mulliken J.B., Fishman S.J., Alomari A.I., Grant F.D., Greene A.K. Differential diagnosis of lower extremity enlargement in pediatric patients referred with a diagnosis of lymphedema. Plast. Reconstr. Surg. 2011;127:1571–1581. doi: 10.1097/PRS.0b013e31820a64f3. [ DOI ] [ PubMed ] [ Google Scholar ]
- 72. Lin S., Kim J., Lee M.-J., Roche L., Yang N.L., Tsao P.S., Rockson S.G. Prospective transcriptomic pathway analysis of human lymphatic vascular insufficiency: Identification and validation of a circulating biomarker panel. PLoS ONE. 2012;7:e52021. doi: 10.1371/journal.pone.0052021. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 73. Dixon J.B., Weiler M.J. Bridging the divide between pathogenesis and detection in lymphedema. Semin. Cell Dev. Biol. 2015;38:75–82. doi: 10.1016/j.semcdb.2014.12.003. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 74. Ure C. Diagnosis of lymphedema. Wien. Med. Wochenschr. 2013;163:162–168. doi: 10.1007/s10354-013-0204-6. [ DOI ] [ PubMed ] [ Google Scholar ]
- 75. Goss J.A., Greene A.K. Sensitivity and Specificity of the Stemmer Sign for Lymphedema: A Clinical Lymphoscintigraphic Study. Plast. Reconstr. Surg. Glob. Open. 2019;7:e2295. doi: 10.1097/GOX.0000000000002295. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 76. Hidding J.T., Viehoff P.B., Beurskens C.H., van Laarhoven H.W., Nijhuis-van der Sanden M.W., van der Wees P.J. Measurement Properties of Instruments for Measuring of Lymphedema: Systematic Review. Phys. Ther. 2016;96:1965–1981. doi: 10.2522/ptj.20150412. [ DOI ] [ PubMed ] [ Google Scholar ]
- 77. Sharkey A.R., King S.W., Kuo R.Y., Bickerton S.B., Ramsden A.J., Furniss D. Measuring Limb Volume: Accuracy and Reliability of Tape Measurement Versus Perometer Measurement. Lymphat. Res. Biol. 2018;16:182–186. doi: 10.1089/lrb.2017.0039. [ DOI ] [ PubMed ] [ Google Scholar ]
- 78. Ciudad P., Sabbagh M.D., Agko M., Huang T.C.T., Manrique O.J., L C.R., Reynaga C., Delgado R., Maruccia M., Chen H.C. Surgical Management of Lower Extremity Lymphedema: A Comprehensive Review. Indian J. Plast. Surg. 2019;52:81–92. doi: 10.1055/s-0039-1688537. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 79. Ogawa Y. Recent advances in medical treatment for lymphedema. Ann. Vasc. Dis. 2012;5:139–144. doi: 10.3400/avd.ra.12.00006. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 80. Apich G. Konservative Therapie des Lymphoedems-Lymphologische Rehabilitationsbehandlung. Wien. Med. Wochenschr. 2013;163:169–176. doi: 10.1007/s10354-013-0205-5. [ DOI ] [ PubMed ] [ Google Scholar ]
- 81. Tzani I., Tsichlaki M., Zerva E., Papathanasiou G., Dimakakos E. Physiotherapeutic rehabilitation of lymphedema: State-of-the-art. Lymphology. 2018;51:1–12. [ PubMed ] [ Google Scholar ]
- 82. Dayan J.H., Ly C.L., Kataru R.P., Mehrara B.J. Lymphedema: Pathogenesis and Novel Therapies. Annu. Rev. Med. 2018;69:263–276. doi: 10.1146/annurev-med-060116-022900. [ DOI ] [ PubMed ] [ Google Scholar ]
- 83. Gott F.H., Ly K., Piller N., Mangio A. Negative pressure therapy in the management of lymphoedema. J. Lymphoedema. 2018;13:43–48. [ Google Scholar ]
- 84. Gatt M., Willis S., Leuschner S. A meta-analysis of the effectiveness and safety of kinesiology taping in the management of cancer-related lymphoedema. Eur. J. Cancer Care. 2017;26 doi: 10.1111/ecc.12510. [ DOI ] [ PubMed ] [ Google Scholar ]
- 85. Davies C., Levenhagen K., Ryans K., Perdomo M., Gilchrist L. Interventions for Breast Cancer-Related Lymphedema: Clinical Practice Guideline from the Academy of Oncologic Physical Therapy of APTA. Phys. Ther. 2020;100:1163–1179. doi: 10.1093/ptj/pzaa087. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 86. Stecco A., Stern R., Fantoni I., De Caro R., Stecco C. Fascial Disorders: Implications for Treatment. PM&R. 2016;8:161–168. doi: 10.1016/j.pmrj.2015.06.006. [ DOI ] [ PubMed ] [ Google Scholar ]
- 87. Roman M., Chaudhry H., Bukiet B., Stecco A., Findley T.W. Mathematical analysis of the flow of hyaluronic acid around fascia during manual therapy motions. J. Am. Osteopath Assoc. 2013;113:600–610. doi: 10.7556/jaoa.2013.021. [ DOI ] [ PubMed ] [ Google Scholar ]
- 88. Shaw C., Mortimer P., Judd P.A. A randomized controlled trial of weight reduction as a treatment for breast cancer-related lymphedema. Cancer. 2007;110:1868–1874. doi: 10.1002/cncr.22994. [ DOI ] [ PubMed ] [ Google Scholar ]
- 89. Nitti M.D., Hespe G.E., Kataru R.P., García Nores G.D., Savetsky I.L., Torrisi J.S., Gardenier J.C., Dannenberg A.J., Mehrara B.J. Obesity-induced lymphatic dysfunction is reversible with weight loss. J. Physiol. 2016;594:7073–7087. doi: 10.1113/JP273061. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 90. Kwan M.L., Cohn J.C., Armer J.M., Stewart B.R., Cormier J.N. Exercise in patients with lymphedema: A systematic review of the contemporary literature. J. Cancer Surviv. 2011;5:320–336. doi: 10.1007/s11764-011-0203-9. [ DOI ] [ PubMed ] [ Google Scholar ]
- 91. Mariana V.F., de Fatima G.G., Maria Pde G. The effect of mechanical lymph drainage accompanied with heat on lymphedema. J. Res. Med. Sci. 2011;16:1448–1451. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 92. Bae H., Kim H.J. Clinical outcomes of extracorporeal shock wave therapy in patients with secondary lymphedema: A pilot study. Ann. Rehabil. Med. 2013;37:229–234. doi: 10.5535/arm.2013.37.2.229. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 93. Li K., Zhang Z., Liu N.F., Feng S.Q., Tong Y., Zhang J.F., Constantinides J., Lazzeri D., Grassetti L., Nicoli F., et al. Efficacy and safety of far infrared radiation in lymphedema treatment: Clinical evaluation and laboratory analysis. Lasers Med. Sci. 2017;32:485–494. doi: 10.1007/s10103-016-2135-0. [ DOI ] [ PubMed ] [ Google Scholar ]
- 94. Badger C., Preston N., Seers K., Mortimer P. Benzo-pyrones for reducing and controlling lymphoedema of the limbs. Cochrane Database Syst. Rev. 2004;2:Cd003140. doi: 10.1002/14651858.CD003140.pub2. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 95. Rockson S.G., Tian W., Jiang X., Kuznetsova T., Haddad F., Zampell J., Mehrara B., Sampson J.P., Roche L., Kim J., et al. Pilot studies demonstrate the potential benefits of antiinflammatory therapy in human lymphedema. JCI Insight. 2018;3:e123775. doi: 10.1172/jci.insight.123775. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 96. Nakamura K., Radhakrishnan K., Wong Y.M., Rockson S.G. Anti-inflammatory pharmacotherapy with ketoprofen ameliorates experimental lymphatic vascular insufficiency in mice. PLoS ONE. 2009;4:e8380. doi: 10.1371/journal.pone.0008380. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 97. Gardenier J.C., Kataru R.P., Hespe G.E., Savetsky I.L., Torrisi J.S., Nores G.D., Jowhar D.K., Nitti M.D., Schofield R.C., Carlow D.C., et al. Topical tacrolimus for the treatment of secondary lymphedema. Nat. Commun. 2017;8:14345. doi: 10.1038/ncomms14345. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 98. Schutte-Nutgen K., Tholking G., Suwelack B., Reuter S. Tacrolimus—Pharmacokinetic Considerations for Clinicians. Curr. Drug Metab. 2018;19:342–350. doi: 10.2174/1389200219666180101104159. [ DOI ] [ PubMed ] [ Google Scholar ]
- 99. Schwartz M.S. Use of hyaluronidase by iontophoresis in treatment of lymphedema. AMA Arch. Intern. Med. 1955;95:662–668. doi: 10.1001/archinte.1955.00250110032004. [ DOI ] [ PubMed ] [ Google Scholar ]
- 100. Borelli S. Therapy of elephantiasis with hyaluronidase. Dermatol. Wochenschr. 1959;139:5–8. [ PubMed ] [ Google Scholar ]
- 101. Hochstrasser E., Horvath G. Hyaluronidase therapy of elephantiasis. Borgyogy. Venerol. Sz. 1960;36:201–203. [ PubMed ] [ Google Scholar ]
- 102. Breslin J.W., Gaudreault N., Watson K.D., Reynoso R., Yuan S.Y., Wu M.H. Vascular endothelial growth factor-C stimulates the lymphatic pump by a VEGF receptor-3-dependent mechanism. Am. J. Physiol. Heart Circ. Physiol. 2007;293:H709–H718. doi: 10.1152/ajpheart.00102.2007. [ DOI ] [ PubMed ] [ Google Scholar ]
- 103. Baker A., Kim H., Semple J.L., Dumont D., Shoichet M., Tobbia D., Johnston M. Experimental assessment of pro-lymphangiogenic growth factors in the treatment of post-surgical lymphedema following lymphadenectomy. Breast Cancer Res. 2010;12:R70. doi: 10.1186/bcr2638. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 104. Zhou H., Wang M., Hou C., Jin X., Wu X. Exogenous VEGF-C augments the efficacy of therapeutic lymphangiogenesis induced by allogenic bone marrow stromal cells in a rabbit model of limb secondary lymphedema. Jpn. J. Clin. Oncol. 2011;41:841–846. doi: 10.1093/jjco/hyr055. [ DOI ] [ PubMed ] [ Google Scholar ]
- 105. Hartiala P., Suominen S., Suominen E., Kaartinen I., Kiiski J., Viitanen T., Alitalo K., Saarikko A.M. Phase 1 Lymfactin® Study: Short-term Safety of Combined Adenoviral VEGF-C and Lymph Node Transfer Treatment for Upper Extremity Lymphedema. J. Plast. Reconstr. Aesthet. Surg. 2020;73:1612–1621. doi: 10.1016/j.bjps.2020.05.009. [ DOI ] [ PubMed ] [ Google Scholar ]
- 106. Maldonado G.E., Perez C.A., Covarrubias E.E., Cabriales S.A., Leyva L.A., Perez J.C., Almaguer D.G. Autologous stem cells for the treatment of post-mastectomy lymphedema: A pilot study. Cytotherapy. 2011;13:1249–1255. doi: 10.3109/14653249.2011.594791. [ DOI ] [ PubMed ] [ Google Scholar ]
- 107. Hou C., Wu X., Jin X. Autologous bone marrow stromal cells transplantation for the treatment of secondary arm lymphedema: A prospective controlled study in patients with breast cancer related lymphedema. Jpn. J. Clin. Oncol. 2008;38:670–674. doi: 10.1093/jjco/hyn090. [ DOI ] [ PubMed ] [ Google Scholar ]
- 108. Conrad C., Niess H., Huss R., Huber S., von Luettichau I., Nelson P.J., Ott H.C., Jauch K.W., Bruns C.J. Multipotent mesenchymal stem cells acquire a lymphendothelial phenotype and enhance lymphatic regeneration in vivo. Circulation. 2009;119:281–289. doi: 10.1161/CIRCULATIONAHA.108.793208. [ DOI ] [ PubMed ] [ Google Scholar ]
- 109. Toyserkani N.M., Jensen C.H., Tabatabaeifar S., Jorgensen M.G., Hvidsten S., Simonsen J.A., Andersen D.C., Sheikh S.P., Sorensen J.A. Adipose-derived regenerative cells and fat grafting for treating breast cancer-related lymphedema: Lymphoscintigraphic evaluation with 1 year of follow-up. J. Plast. Reconstr. Aesthet. Surg. 2019;72:71–77. doi: 10.1016/j.bjps.2018.09.007. [ DOI ] [ PubMed ] [ Google Scholar ]
- 110. Hu L.R., Pan J. Adipose-derived stem cell therapy shows promising results for secondary lymphedema. World J. Stem Cells. 2020;12:612–620. doi: 10.4252/wjsc.v12.i7.612. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 111. Rockson S.G. Lymphedema. Vasc. Med. 2016;21:77–81. doi: 10.1177/1358863X15620852. [ DOI ] [ PubMed ] [ Google Scholar ]
- 112. Schaverien M.V., Badash I., Patel K.M., Selber J.C., Cheng M.H. Vascularized Lymph Node Transfer for Lymphedema. Semin. Plast. Surg. 2018;32:28–35. doi: 10.1055/s-0038-1632401. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 113. Kataru R.P., Park H.J., Baik J.E., Li C., Shin J., Mehrara B.J. Regulation of Lymphatic Function in Obesity. Front. Physiol. 2020;11:459. doi: 10.3389/fphys.2020.00459. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 114. Lasinski B.B., McKillip Thrift K., Squire D., Austin M.K., Smith K.M., Wanchai A., Green J.M., Stewart B.R., Cormier J.N., Armer J.M. A systematic review of the evidence for complete decongestive therapy in the treatment of lymphedema from 2004 to 2011. PM&R. 2012;4:580–601. doi: 10.1016/j.pmrj.2012.05.003. [ DOI ] [ PubMed ] [ Google Scholar ]
- 115. Weiss J.M., Spray B.J. The effect of complete decongestive therapy on the quality of life of patients with peripheral lymphedema. Lymphology. 2002;35:46–58. [ PubMed ] [ Google Scholar ]
- 116. Döller W. Lymphologie. Wien. Med. Wochenschr. 2013;163:153–154. doi: 10.1007/s10354-013-0186-4. [ DOI ] [ PubMed ] [ Google Scholar ]
- 117. Ohlin K., Svensson B., Brorson H. Controlled Compression Therapy and Compression Garments. In: Greene A.K., Slavin S.A., Brorson H., editors. Lymphedema: Presentation, Diagnosis, and Treatment. Springer International Publishing; Cham, Switzerland: 2015. pp. 213–225. [ DOI ] [ Google Scholar ]
- 118. Fukushima T., Tsuji T., Sano Y., Miyata C., Kamisako M., Hohri H., Yoshimura C., Asakura M., Okitsu T., Muraoka K., et al. Immediate effects of active exercise with compression therapy on lower-limb lymphedema. Support. Care Cancer. 2017;25:2603–2610. doi: 10.1007/s00520-017-3671-2. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 119. Soriano-Maldonado A., Carrera-Ruiz Á., Díez-Fernández D.M., Esteban-Simón A., Maldonado-Quesada M., Moreno-Poza N., García-Martínez M.D.M., Alcaraz-García C., Vázquez-Sousa R., Moreno-Martos H., et al. Effects of a 12-week resistance and aerobic exercise program on muscular strength and quality of life in breast cancer survivors: Study protocol for the EFICAN randomized controlled trial. Medicine. 2019;98:e17625. doi: 10.1097/MD.0000000000017625. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 120. Baumann F.T., Reike A., Reimer V., Schumann M., Hallek M., Taaffe D.R., Newton R.U., Galvao D.A. Effects of physical exercise on breast cancer-related secondary lymphedema: A systematic review. Breast Cancer Res. Treat. 2018;170:1–13. doi: 10.1007/s10549-018-4725-y. [ DOI ] [ PubMed ] [ Google Scholar ]
- 121. The diagnosis and treatment of peripheral lymphedema: 2013 Consensus Document of the International Society of Lymphology. Lymphology. 2013;46:1–11. [ PubMed ] [ Google Scholar ]
- 122. Douglass J., Graves P., Gordon S. Self-Care for Management of Secondary Lymphedema: A Systematic Review. PLoS Negl. Trop. Dis. 2016;10:e0004740. doi: 10.1371/journal.pntd.0004740. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 123. Bozkurt M., Palmer L.J., Guo Y. Effectiveness of Decongestive Lymphatic Therapy in Patients with Lymphedema Resulting from Breast Cancer Treatment Regardless of Previous Lymphedema Treatment. Breast J. 2017;23:154–158. doi: 10.1111/tbj.12710. [ DOI ] [ PubMed ] [ Google Scholar ]
- 124. Pereira de Godoy J.M., Godoy H., Pereira de Godoy A.C., Marqui T., Guerreiro Godoy M.d.F. Lymphedema and the mobilization of intracellular and extracellular fluids with intensive treatment. Acta Phlebol. 2019;20:57–60. doi: 10.23736/S1593-232X.19.00446-6. [ DOI ] [ Google Scholar ]
- 125. Ancukiewicz M., Russell T.A., Otoole J., Specht M., Singer M., Kelada A., Murphy C.D., Pogachar J., Gioioso V., Patel M., et al. Standardized method for quantification of developing lymphedema in patients treated for breast cancer. Int. J. Radiat. Oncol. Biol. Phys. 2011;79:1436–1443. doi: 10.1016/j.ijrobp.2010.01.001. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 126. Koehler L.A., Mayrovitz H.N. Tissue Dielectric Constant Measures in Women with and without Clinical Trunk Lymphedema Following Breast Cancer Surgery: A 78-Week Longitudinal Study. Phys. Ther. 2020;100:1384–1392. doi: 10.1093/ptj/pzaa080. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 127. Sagen A., Kåresen R., Skaane P., Risberg M.A. Validity for the simplified water displacement instrument to measure arm lymphedema as a result of breast cancer surgery. Arch. Phys. Med. Rehabil. 2009;90:803–809. doi: 10.1016/j.apmr.2008.11.016. [ DOI ] [ PubMed ] [ Google Scholar ]
- 128. Reza C., Nørregaard S., Moffatt C., Karlsmark T. Inter-observer and Intra-observer Variability in Volume Measurements of the Lower Extremity Using Perometer. Lymphat. Res. Biol. 2020;18:416–421. doi: 10.1089/lrb.2019.0063. [ DOI ] [ PubMed ] [ Google Scholar ]
- 129. Tidhar D., Armer J.M., Deutscher D., Shyu C.R., Azuri J., Madsen R. Measurement Issues in Anthropometric Measures of Limb Volume Change in Persons at Risk for and Living with Lymphedema: A Reliability Study. J. Pers. Med. 2015;5:341–353. doi: 10.3390/jpm5040341. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 130. Pereira De Godoy J.M., Gonçalves I.P., Barufi S., Godoy M.F.G. Large reduction in volume with the intensive treatment of lymphedema: Reduction of fluids? Int. J. Angiol. 2012;21:171–174. doi: 10.1055/s-0032-1325167. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 131. De Godoy J.M.P., de Godoy A.C.P., Maria F.G.G. Evolution of Godoy & Godoy manual lymph drainage. Technique with linear Movements. Clin. Pract. 2017;7:1006. doi: 10.4081/cp.2017.1006. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 132. Bertsch T. Evaluation of a novel night-time compression garment: A prospective observational study. Br. J. Community Nurs. 2018;23:535–541. doi: 10.12968/bjcn.2018.23.11.535. [ DOI ] [ PubMed ] [ Google Scholar ]
- 133. Ward L.C. Assessment of lymphedema by bioelectrical impedance spectroscopy. Jpn. J. Nurs. Sci. 2011;8:108. doi: 10.1111/j.1742-7924.2010.00165.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 134. Pereira De Godoy J.M., Franco Brigidio P.A., Salles Cunha S.X., Batigália F., De Fatima Guerreiro Godoy M. Mobilization of fluids in large volumetric reductions during intensive treatment of leg lymphedema. Int. Angiol. 2013;32:479–482. [ PubMed ] [ Google Scholar ]
- 135. Hinghofer-Szalkay H.G., Sauseng-Fellegger G., Greenleaf J.E. Plasma volume with alternative tilting: Effect of fluid ingestion. J. Appl. Physiol. 1995;78:1369–1373. doi: 10.1152/jappl.1995.78.4.1369. [ DOI ] [ PubMed ] [ Google Scholar ]
- 136. Van Beaumont W. Evaluation of hemoconcentration from hematocrit measurements. J. Appl. Physiol. 1972;32:712–713. doi: 10.1152/jappl.1972.32.5.712. [ DOI ] [ PubMed ] [ Google Scholar ]
- 137. Dill D.B., Costill D.L. Calculation of percentage changes in volumes of blood, plasma, and red cells in dehydration. J. Appl. Physiol. 1974;37:247–248. doi: 10.1152/jappl.1974.37.2.247. [ DOI ] [ PubMed ] [ Google Scholar ]
- 138. Nadler S.B., Hidalgo J.H., Bloch T. Prediction of blood volume in normal human adults. Surgery. 1962;51:224–232. [ PubMed ] [ Google Scholar ]
- 139. Brix B., Apich G., Roessler A., Ure C., Schmid-Zalaudek K., Hinghofer-Szalkay H., Goswami N. Fluid Shifts Induced by Physical Therapy in Lower Limb Lymphedema Patients. J. Clin. Med. 2020;9:3678. doi: 10.3390/jcm9113678. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 140. Titze J. Water-free Na+ retention: Interaction with hypertension and tissue hydration. Blood Purif. 2008;26:95–99. doi: 10.1159/000110573. [ DOI ] [ PubMed ] [ Google Scholar ]
- 141. Wiig H., Luft F.C., Titze J.M. The interstitium conducts extrarenal storage of sodium and represents a third compartment essential for extracellular volume and blood pressure homeostasis. Acta Physiol. 2018;222 doi: 10.1111/apha.13006. [ DOI ] [ PubMed ] [ Google Scholar ]
- 142. Titze J., Lang R., Ilies C., Schwind K.H., Kirsch K.A., Dietsch P., Luft F.C., Hilgers K.F. Osmotically inactive skin Na+ storage in rats. Am. J. Physiol. Ren. Physiol. 2003;285:F1108–F1117. doi: 10.1152/ajprenal.00200.2003. [ DOI ] [ PubMed ] [ Google Scholar ]
- 143. Pimenta E., Gaddam K.K., Oparil S., Aban I., Husain S., Dell’Italia L.J., Calhoun D.A. Effects of dietary sodium reduction on blood pressure in subjects with resistant hypertension: Results from a randomized trial. Hypertension. 2009;54:475–481. doi: 10.1161/HYPERTENSIONAHA.109.131235. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 144. Goswami N., Blaber A.P., Hinghofer-Szalkay H., Montani J.P. Orthostatic intolerance in older persons: Etiology and countermeasures. Front. Physiol. 2017;8 doi: 10.3389/fphys.2017.00803. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 145. Goswami N. Falls and fall-prevention in older persons: Geriatrics meets spaceflight! Front. Physiol. 2017;8:603. doi: 10.3389/fphys.2017.00603. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 146. Harrison M.H., Kravik S.E., Geelen G., Keil L., Greenleaf J.E. Blood pressure and plasma renin activity as predictors of orthostatic intolerance. Aviat. Space Environ. Med. 1985;56:1059–1064. [ PubMed ] [ Google Scholar ]
- 147. Hinghofer-Szalkay H. Gravity, the hydrostatic indifference concept and the cardiovascular system. Eur. J. Appl. Physiol. 2011;111:1673–1674. doi: 10.1007/s00421-010-1646-9. [ DOI ] [ PubMed ] [ Google Scholar ]
- 148. Blaber A.P., Goswami N., Bondar R.L., Kassam M.S. Impairment of cerebral blood flow regulation in astronauts with post flight orthostatic intolerance. Stroke. 2011;42:1844–1850. doi: 10.1161/STROKEAHA.110.610576. [ DOI ] [ PubMed ] [ Google Scholar ]
- 149. Putz Z., Németh N., Istenes I., Martos T., Gandhi R.A., Körei A.E., Hermányi Z., Szathmári M., Jermendy G., Tesfaye S., et al. Autonomic dysfunction and circadian blood pressure variations in people with impaired glucose tolerance. Diabet. Med. 2013;30:358–362. doi: 10.1111/dme.12111. [ DOI ] [ PubMed ] [ Google Scholar ]
- 150. Goswami N., Roessler A., Hinghofer-Szalkay H., Montani J.P., Steptoe A. Delaying orthostatic syncope with mental challenge: A pilot study. Physiol. Behav. 2012;106:569–573. doi: 10.1016/j.physbeh.2012.02.022. [ DOI ] [ PubMed ] [ Google Scholar ]
- 151. Rapp K., Becker C., Cameron I.D., König H.H., Büchele G. Epidemiology of falls in residential aged care: Analysis of more than 70,000 falls from residents of bavarian nursing homes. J. Am. Med. Dir. Assoc. 2012;13:187–e181. doi: 10.1016/j.jamda.2011.06.011. [ DOI ] [ PubMed ] [ Google Scholar ]
- 152. Blaber A., Hinghofer-Szalkay H., Goswami N. Blood volume redistribution during hypovolemia. Aviat. Space Environ. Med. 2013;84:59–64. doi: 10.3357/ASEM.3424.2013. [ DOI ] [ PubMed ] [ Google Scholar ]
- 153. Gangavati A., Hajjar I., Quach L., Jones R.N., Kiely D.K., Gagnon P., Lipsitz L.A. Hypertension, orthostatic hypotension, and the risk of falls in a community-dwelling elderly population: The maintenance of balance, independent living, intellect, and zest in the elderly of Boston study. J. Am. Geriatr. Soc. 2011;59:383–389. doi: 10.1111/j.1532-5415.2011.03317.x. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 154. Blaszczyk J.W., Lowe D.L., Hansen P.D. Ranges of postural stability and their changes in the elderly. Gait Posture. 1994;2:11–17. doi: 10.1016/0966-6362(94)90012-4. [ DOI ] [ Google Scholar ]
- 155. Tinetti M.E., Baker D.I., McAvay G., Claus E.B., Garrett P., Gottschalk M., Koch M.L., Trainor K., Horwitz R.I. A multifactorial intervention to reduce the risk of falling among elderly people living in the community. N. Engl. J. Med. 1994;331:821–827. doi: 10.1056/NEJM199409293311301. [ DOI ] [ PubMed ] [ Google Scholar ]
- 156. Mackey D.C., Robinovitch S.N. Mechanisms underlying age-related differences in ability to recover balance with the ankle strategy. Gait Posture. 2006;23:59–68. doi: 10.1016/j.gaitpost.2004.11.009. [ DOI ] [ PubMed ] [ Google Scholar ]
- 157. Hsiao-Wecksler E.T., Robinovitch S.N. The effect of step length on young and elderly women’s ability to recover balance. Clin. Biomech. 2007;22:574–580. doi: 10.1016/j.clinbiomech.2007.01.013. [ DOI ] [ PubMed ] [ Google Scholar ]
- 158. Esmer M., Keser I., Erer D., Kupeli B. Acute Cardiovascular Responses to the Application of Manual Lymphatic Drainage in Different Body Regions. Lymphat. Res. Biol. 2019;17:362–367. doi: 10.1089/lrb.2018.0043. [ DOI ] [ PubMed ] [ Google Scholar ]
- 159. Sachse C., Trozic I., Brix B., Roessler A., Goswami N. Sex differences in cardiovascular responses to orthostatic challenge in healthy older persons: A pilot study. Physiol. Int. 2019;106:236–249. doi: 10.1556/2060.106.2019.16. [ DOI ] [ PubMed ] [ Google Scholar ]
- 160. Trozic I., Platzer D., Fazekas F., Bondarenko A.I., Brix B., Rossler A., Goswami N. Postural hemodynamic parameters in older persons have a seasonal dependency: A pilot study. Z. Gerontol. Geriatr. 2020;53:145–155. doi: 10.1007/s00391-019-01525-3. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 161. Blaber A.P., Landrock C.K., Souvestre P.A. Cardio-postural deconditioning: A model for post-flight orthostatic intolerance. Respir. Physiol. Neurobiol. 2009;169:S21–S25. doi: 10.1016/j.resp.2009.04.007. [ DOI ] [ PubMed ] [ Google Scholar ]
- 162. Small D.M., Bond M.G., Waugh D., Prack M., Sawyer J.K. Physicochemical and histological changes in the arterial wall of nonhuman primates during progression and regression of atherosclerosis. J. Clin. Investig. 1984;73:1590–1605. doi: 10.1172/JCI111366. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 163. Wang X., Rader D.J. Molecular regulation of macrophage reverse cholesterol transport. Curr. Opin. Cardiol. 2007;22:368–372. doi: 10.1097/HCO.0b013e3281ec5113. [ DOI ] [ PubMed ] [ Google Scholar ]
- 164. Lim H.Y., Thiam C.H., Yeo K.P., Bisoendial R., Hii C.S., McGrath K.C., Tan K.W., Heather A., Alexander J.S., Angeli V. Lymphatic vessels are essential for the removal of cholesterol from peripheral tissues by SR-BI-mediated transport of HDL. Cell Metab. 2013;17:671–684. doi: 10.1016/j.cmet.2013.04.002. [ DOI ] [ PubMed ] [ Google Scholar ]
- 165. Randolph G.J., Miller N.E. Lymphatic transport of high-density lipoproteins and chylomicrons. J. Clin. Investig. 2014;124:929–935. doi: 10.1172/JCI71610. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 166. Martel C., Li W., Fulp B., Platt A.M., Gautier E.L., Westerterp M., Bittman R., Tall A.R., Chen S.-H., Thomas M.J., et al. Lymphatic vasculature mediates macrophage reverse cholesterol transport in mice. J. Clin. Investing. 2013;123:1571–1579. doi: 10.1172/JCI63685. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 167. Vuorio T., Nurmi H., Moulton K., Kurkipuro J., Robciuc M.R., Ohman M., Heinonen S.E., Samaranayake H., Heikura T., Alitalo K., et al. Lymphatic vessel insufficiency in hypercholesterolemic mice alters lipoprotein levels and promotes atherogenesis. Arter. Thromb. Vasc. Biol. 2014;34:1162–1170. doi: 10.1161/ATVBAHA.114.302528. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 168. Münzel T., Sinning C., Post F., Warnholtz A., Schulz E. Pathophysiology, diagnosis and prognostic implications of endothelial dysfunction. Ann. Med. 2008;40:180–196. doi: 10.1080/07853890701854702. [ DOI ] [ PubMed ] [ Google Scholar ]
- 169. Levick J.R. An Introduction to Cardiovascular Physiology. 5th ed. Hodder Education; London, UK: 2012. [ Google Scholar ]
- 170. Fleming I. Molecular mechanisms underlying the activation of eNOS. Pflüg. Arch. Eur. J. Physiol. 2010;459:793–806. doi: 10.1007/s00424-009-0767-7. [ DOI ] [ PubMed ] [ Google Scholar ]
- 171. Konukoglu D., Uzun H. Endothelial Dysfunction and Hypertension. Adv. Exp. Med. Biol. 2017;956:511–540. doi: 10.1007/5584_2016_90. [ DOI ] [ PubMed ] [ Google Scholar ]
- 172. Vita J.A. Endothelial function. Circulation. 2011;124:e906–e912. doi: 10.1161/CIRCULATIONAHA.111.078824. [ DOI ] [ PubMed ] [ Google Scholar ]
- 173. Brix B., Apich G., Ure C., Roessler A., Goswami N. Physical therapy affects endothelial function in lymphedema patients. Lymphology. 2020;53:109–117. [ PubMed ] [ Google Scholar ]
- 174. Thijssen D.H., Black M.A., Pyke K.E., Padilla J., Atkinson G., Harris R.A., Parker B., Widlansky M.E., Tschakovsky M.E., Green D.J. Assessment of flow-mediated dilation in humans: A methodological and physiological guideline. American journal of physiology. Heart Circ. Physiol. 2011;300:H2–H12. doi: 10.1152/ajpheart.00471.2010. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 175. Thijssen D.H.J., Bruno R.M., van Mil A., Holder S.M., Faita F., Greyling A., Zock P.L., Taddei S., Deanfield J.E., Luscher T., et al. Expert consensus and evidence-based recommendations for the assessment of flow-mediated dilation in humans. Eur. Heart J. 2019;40:2534–2547. doi: 10.1093/eurheartj/ehz350. [ DOI ] [ PubMed ] [ Google Scholar ]
- 176. Yamashina A., Tomiyama H., Arai T., Hirose K., Koji Y., Hirayama Y., Yamamoto Y., Hori S. Brachial-ankle pulse wave velocity as a marker of atherosclerotic vascular damage and cardiovascular risk. Hypertens. Res. 2003;26:615–622. doi: 10.1291/hypres.26.615. [ DOI ] [ PubMed ] [ Google Scholar ]
- 177. Everson F., De Boever P., Nawrot T.S., Goswami N., Mthethwa M., Webster I., Martens D.S., Mashele N., Charania S., Kamau F., et al. Personal NO(2) and Volatile Organic Compounds Exposure Levels are Associated with Markers of Cardiovascular Risk in Women in the Cape Town Region of South Africa. Int. J. Environ. Res. Public Health. 2019;16:2284. doi: 10.3390/ijerph16132284. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 178. Louwies T., Int Panis L., Alders T., Bonne K., Goswami N., Nawrot T.S., Dendale P., De Boever P. Microvascular reactivity in rehabilitating cardiac patients based on measurements of retinal blood vessel diameters. Microvasc. Res. 2019;124:25–29. doi: 10.1016/j.mvr.2019.02.006. [ DOI ] [ PubMed ] [ Google Scholar ]
- 179. Matušková V., Zeman T., Ewerlingová L., Hlinomazová Z., Souček J., Vlková E., Goswami N., Balcar V.J., Šerý O. An association of neovascular age-related macular degeneration with polymorphisms of CFH, ARMS2, HTRA1 and C3 genes in Czech population. Acta Ophthalmol. 2020;98:e691–e699. doi: 10.1111/aos.14357. [ DOI ] [ PubMed ] [ Google Scholar ]
- 180. Vaes A.W., Spruit M.A., Theunis J., Goswami N., Vanfleteren L.E., Franssen F.M.E., Wouters E.F.M., De Boever P. Looking into the eye of patients with chronic obstructive pulmonary disease: An opportunity for better microvascular profiling of these complex patients. Acta Ophthalmol. 2018;96:539–549. doi: 10.1111/aos.13765. [ DOI ] [ PubMed ] [ Google Scholar ]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
- View on publisher site
- PDF (410.6 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections

- Adolescent and Young Adult Cancer
- Bile Duct Cancer
- Bladder Cancer
- Brain Cancer
- Breast Cancer
- Cervical Cancer
- Childhood Cancer
- Colorectal Cancer
- Endometrial Cancer
- Esophageal Cancer
- Head and Neck Cancer
- Kidney Cancer
- Liver Cancer
- Lung Cancer
- Mouth Cancer
- Mesothelioma
- Multiple Myeloma
- Neuroendocrine Tumors
- Ovarian Cancer
- Pancreatic Cancer
- Prostate Cancer
- Skin Cancer/Melanoma
- Stomach Cancer
- Testicular Cancer
- Throat Cancer
- Thyroid Cancer
- Prevention and Screening
- Diagnosis and Treatment
- Research and Clinical Trials
- Survivorship

Request an appointment at Mayo Clinic

A promising new treatment for lymphedema
Share this:.
By Susan Buckles
Lymphedema is most often associated with cancer treatment, although some cases of lymphedema are congenital. During cancer treatment, lymph nodes may be damaged or removed, and the lymphatic fluid no longer drains. Then lymphedema can develop months or years after cancer treatment.
Research by Antonio Forte, M.D., Ph.D. , a Mayo Clinic plastic surgeon, seeks to better pinpoint who is most likely to benefit from surgery aimed at regenerating a faulty lymphatic system.
"Without surgery, lymphedema gets progressively worse due to accumulation of the lymphatic fluid in tissue and the chronic changes that causes. The upper and lower extremities can feel heavy, and the affected area is more prone to infections. Wounds take longer to heal, and some people lose dexterity to the point that it's hard to put a shoe on," says Dr. Forte.
Surgical options at Mayo Clinic
Mayo Clinic is a leader in surgical options to reverse the damage from lymphedema. Dr. Forte specializes in lymphovenous bypass, a microsurgery done under powerful microscopes that are magnified 20 to 25 times. Through an incision no larger than a paper cut, the surgery connects tiny lymphatic vessels smaller than a strand of hair to tiny veins, creating a type of detour around the damaged area. The new vessel connections restore the body's ability to drain lymphatic fluids.
"When you remove that fluid, we don't know why, but the body is able to reverse these chronic changes in the tissue. In a way, what we're trying to do is reverse the damage that was done by the accumulation of the lymphatic fluid," says Dr. Forte. "It is a regenerative approach because not only do you restore function, but you actually heal the tissues."
Like a ton of bricks
Rebecca, who asked that her last name not be used, was diagnosed with triple-negative breast cancer in 2009. She prayed she'd live long enough to see her two youngest sons graduate college.
The Savannah, Georgia, resident waged a grueling battle that included chemotherapy, mastectomy and lymph node removal. She emerged victorious and was able to not only attend her sons' graduations, but also their weddings. However, a noxious side effect surfaced four years after her cancer treatment. Lymphedema developed in her right arm, causing swelling and fibrous tissue that progressively got harder.
"I felt as if I was dragging a ton of bricks everywhere I went. I could not go away to visit family without being sure I had all materials and compression garments with me. I had to make a checklist to include everything I needed to care for myself anywhere I went," she says.
Occupational therapy, compression wraps and a disciplined exercise regimen helped control her lymphedema, but it never really went away. A devastating reality set in when she realized that no matter how closely she followed medical advice, the lymphedema would not be cured.
9 was the lucky number
By luck, coincidence or maybe even a miracle, Rebecca discovered a new path to treatment while at the ninth green of the Players Championship at TPC Sawgrass in Ponte Vedra Beach, Florida. She and her family had gathered at the ninth green to watch a golfer sink a putt. Rebecca's right hand had swollen during the day.
"I had left my compression glove at home," she says.
She decided to stand in the shade and rest her hand on a tree to see if the swelling would go down. While standing there, with her right hand above her head resting on an ancient live oak tree, a nearby spectator noticed the compression sleeve.
"She said: 'Excuse me. I see you are a lymphedema patient. Did you know that Mayo Clinic offers lymphovenous bypass surgery?' This woman turned out to be a plastic surgery nurse practitioner at Mayo Clinic in Florida. I had not heard about the surgery until our chance meeting," says Rebecca.
Despite her initial apprehension, preparations for surgery started falling in place. Dr. Forte examined her and found the procedure to be a suitable match, and her insurance approved. One year after lymphovenous bypass surgery, Rebecca says the fluid has drained and her right arm is nearly normal.
"I can now feel the bone in my elbow. I hadn't felt that bone in three years," she says. "This surgery has taken a weight, ball and chain and a ton of bricks off my life. Resentment, fear and worry also have been removed. I truly do not have words to express the depth of gratitude and appreciation I have for Dr. Forte and his nurse practitioner. I weep with private tears of joy and relief."
While surgery relieved Rebecca's symptoms, Dr. Forte says there is a chance it might not work the same for others. However, he believes lymphovenous bypass is a safe and low-risk procedure.
"I love the bypass because the morbidity is so low that there's little downside to the procedure. If lymphovenous surgery doesn't relieve fluid buildup, then all you have to heal from is small incisions similar to paper cuts. If it does work, it's life-changing," he says.
By better understanding how each patient responds to the surgery, Dr. Forte hopes to improve the success rate. He also hopes to learn whether a targeted drug or complementary treatment might lead to quicker recovery.
A version of this story originally appeared on the Mayo Clinic Center for Regenerative Medicine blog .
Learn more about lymphedema .
Find a lymphedema clinical trial at Mayo Clinic .
Mayo Clinic's Center for Individualized Medicine is funding research to identify new biomarkers that could predict which patients are most likely to respond to this regenerative surgery.
Related Posts

Mark McNiven, Ph.D., and Tanios Bekaii-Saab, M.D., Mayo Clinic Comprehensive Cancer Center researchers, explain what cancer is, how it develops and why it's challenging to treat.

Findings show extended progression-free survival for people with meningiomas who received a radiopharmaceutical approved for neuroendocrine tumors.

Mayo Clinic study findings reveal a protein that increases glioblastoma malignancy, a new understanding of the tumor's biology, and a potential new treatment strategy.
- What is cancer?
- Advanced cancer
- Bladder cancer
- Blood cancer
- Bone cancer
- Bowel cancer
- Brain tumours
- Breast cancer
- Cervical cancer
- Gynaecological cancers
- Head & neck cancer
- Chemotherapy
- Radiation treatment
- Immunotherapy
- Targeted treatments
- Other therapies
- Clinical trials
- Side effects of treatment
- Making treatment decisions
- Questions to ask
- Your treatment team
- Covid-19 vaccination & cancer
- Coping with waiting
- Emotions and cancer
- Talking about your diagnosis
- Talking to children
- Managing weight
- Eating well with cancer
- Keeping active with cancer
- Medicinal cannabis
- Holidays and special days
- Sex and cancer
- Who is a supporter?
- Understanding your emotions
- Talking to someone with cancer
- Self-care for supporters
- Practical side of supporting
- Healthy eating
- No or less alcohol
- Environmental cancer risks
- Marijuana and cancer risk
- HPV vaccination
- Cancer helpline
- One-on-one support
- Coping with cancer videos
- Psychology and counselling
- Transport to treatment
- Accommodation
- Support Crew
- Connecting you with others
- Relaxation and mindfulness
- Support groups
- Get sorted financially
- Financial assistance
- National Travel Assistance
- Cancer and insurance
- Cancer and your work
- Health professional referral
- A gift in your will
- Donate in memory
- Donate via your pay
- Donate your hair
- Share your story with us
- National Office
- Hawke's Bay
- Central Districts
- Strategic plan
- Equity Charter
- Our history
- Daffodils and Cancer
- Position statements
- Our national submissions
- Our advocacy campaigns
- About Our Research
- National Research Grants 2024
- Māori Cancer Researcher Awards
- Research Strategy
- National Research Grants
- Research Collaboration
- Research History
- Regional Research Grants
- Breast Reconstructive Surgery
- Pharmac Review Panel
- Gift of Compassion
- Mandatory Sunscreen Standard
- Hugo Charitable Trust Donate
- Five unhealthy snacks a day
- COVID-19: Face Mask Safety
- Vaping legislation passes
- Vaping laws welcomed
- One month, one million balls
- Five stories of cancer
- Auckland cancels Daffodil Day
Lymphoedema Lymphoedema
If your lymph nodes are removed or damaged during cancer treatment, you may get lymphoedema.
What is lymphoedema?
Lymphoedema is the swelling of part or parts of the body that occurs when the lymphatic system is not working properly.
The lymphatic system consists of many tiny channels throughout the body called lymph vessels or lymphatics.
Learn more about your lymph nodes and lymphatic system
Lymph nodes (also known as glands) are found throughout the body and are part of the lymphatic system.
The lymphatic system contains a series of lymph vessels (tiny channels under the skin) that carry the lymph fluid through the nodes back to the bloodstream.
Lymph nodes contain white blood cells that help fight infection and diseases, such as cancer.
The number of lymph nodes you have is different for each person.
For example, there can be between 15 to 30 nodes in an armpit. Lymph nodes also vary in size from a pinpoint to the size of a baked bean.
Lymph nodes can swell and become tender when you have an infection. If you develop a swollen lymph node, get it checked by your doctor.
Sometimes, cancer cells spread into the lymph nodes from cancer in another part of the body. It is also possible for cancer to start in a lymph node. This type of cancer is called lymphoma.
Symptoms of lymphoedema
Signs and symptoms of lymphoedema
- changes in feeling (heavy, tight, full, tingling or stiff)
- skin changes (your skin may feel tight, or stretched)
- aching, pain or tension
Having these symptoms does not mean you have lymphoedema, but it is important to get any changes checked.
Ask your treatment team for a referral to a lymphoedema therapist.
What causes lymphoedema?
Lymphoedema can be caused by cancer treatments or the cancer itself.
There is a risk of lymphedema if you have:
- lymph nodes are damaged or removed during surgery
- radiation treatment to the lymph nodes
- cancer cells blocking the flow of lymph fluid
- cancer that is pressing on the lymph vessels blocking the lymph nodes nearby
Lymphoedema occurs close to the part of the body affected by treatment. It can develop weeks, months or years after cancer treatment.
Cancer treatment has changed over the years to help reduce the risk of lymphoedema.
Most people who have surgery or radiation treatment will not get lymphoedema. Your treatment team will be able to explain if you are at risk of lymphoedema.
Treatment of lymphoedema
There is no cure for Lymphoedema. In most cases, it can be controlled with treatment.
Treatment for lymphoedema may include:
- compression
A lymphoedema therapist will help you make an assessment and a treatment plan.
Lymphoedema therapists
These are nurses, physiotherapists or massage therapists who have undertaken specialised training in lymphoedema management.
They can help you with lymphatic drainage massage, fitting compression garments, and tips for living with lymphoedema.
Your treatment team or our nurses will be able to let you know about trained lymphoedema therapists in your area.
Lymphoedema therapists work in public and private practice. If you have medical insurance, the cost may be covered. Check your policy.
Compression garments for lymphoedema
These should be fitted by a lymphoedema therapist or another trained person.
They should be worn according to the therapist’s instructions and cared for according to the manufacturer’s instructions.
Talk to your lymphoedema therapist about suppliers and subsidies that may be available.
Complex Physical Therapy (CPT) for lymphoedema
If your lymphoedema is moderate to severe, your lymphoedema therapist will probably recommend a course of Complex Physical Therapy (CPT).
This can be successful in reducing and controlling swelling, and the earlier it is started in the development of lymphedema, the higher the likelihood of success.
CPT involves daily bandaging and massage for two to three weeks, along with exercise, skincare, dietary advice, and a compression garment fitting.
Looking after your skin with lymphoedema
If you have lymphoedema, looking after your skin well can reduce the risk of infection.
If build-up from lymphoedema sits close to the skin surface, the limb may become infected through cuts, scratches or insect bites.
See your doctor immediately:
- if any pain, redness or heat is present in the affected limb
- you notice any red lines tracking along the limb
- if you feel generally unwell
If you have an infection, you will be given antibiotics. Always follow the instructions of your doctor. If signs and symptoms persist after a course of antibiotics, speak to your doctor. The infection may not have completely cleared.
Some other things to do to look after your skin:
- avoid sunburn - cover up and use 30+ sunscreen when outdoors
- keep skin soft by gently moisturise daily with a non-perfumed cream or oil
- instead of soap try a body wash that won't dry out your skin, for example, QV wash soap alternative or Dove soap
- wear gloves when gardening or doing the dishes
- try to avoid insect bites, cuts and scratches - treat any of these with antiseptic ointment or spray, for example, Savlon or Stingose
- avoid the use of hot water bottles, or ice or heat packs on your affected limb
- avoid spa baths are not recommended
- always wear your compression garment as shown
- for arm lymphoedema, use the unaffected arm for carrying heavy parcels
- check that your work environment is not making your lymphoedema worse, for example, computer set-up, heavy lifting or repetitive movements
- for leg lymphoedema, avoid standing or sitting still for long periods
- Latest advice from The Australian and New Zealand College of Anaesthetists (ANZCA) shows that the arm on the affected side can usually be used safely for medical procedures ANZCA fact sheet
Exercise with lymphoedema
Gentle muscle movement, including deep breathing, increases the flow of lymph fluid. This reduces the risk of fluid building up.
Regular exercise, such as walking and swimming, can be very good. The actions of the muscles will help to move the fluid out of the swollen limb.
Your lymphoedema therapist can help with exercise tips that are best for you.
Being a healthy weight may help reduce your risk of lymphoedema and make it easier to control. Talk to your doctor or dietician if you have concerns about your weight.
Tips for eating with lymphoedema
A balanced diet low in fat and high in fibre is important for people with lymphoedema.
- eat plenty of fresh fruit and vegetables
- drink lots of fluid every day, especially water
- try to maintain the ideal weight for your height and build
- easily digested protein, such as chicken, fish, tofu or low-fat dairy products
Recommended websites
- Australasian Lymphology Association
lymphoedema therapists throughout New Zealand
- Lymph Info Trust

Eating well is important for keeping well, especially when you have cancer.

Keeping active before, during and after cancer treatment is important for your health and wellbeing.

We have free counselling and psychological services for people with cancer and their family/whānau.

A cancer diagnosis and treatment impacts you physically, emotionally and financially. You may be abl…
We know that going through cancer is tough and can raise many questions. You are not alone. We have health professionals to answer your questions and provide the support you need. Get in touch
Did you find the information on this page helpful?
- I found this helpful
- I did not find this helpful
You must enable JavaScript to submit this form
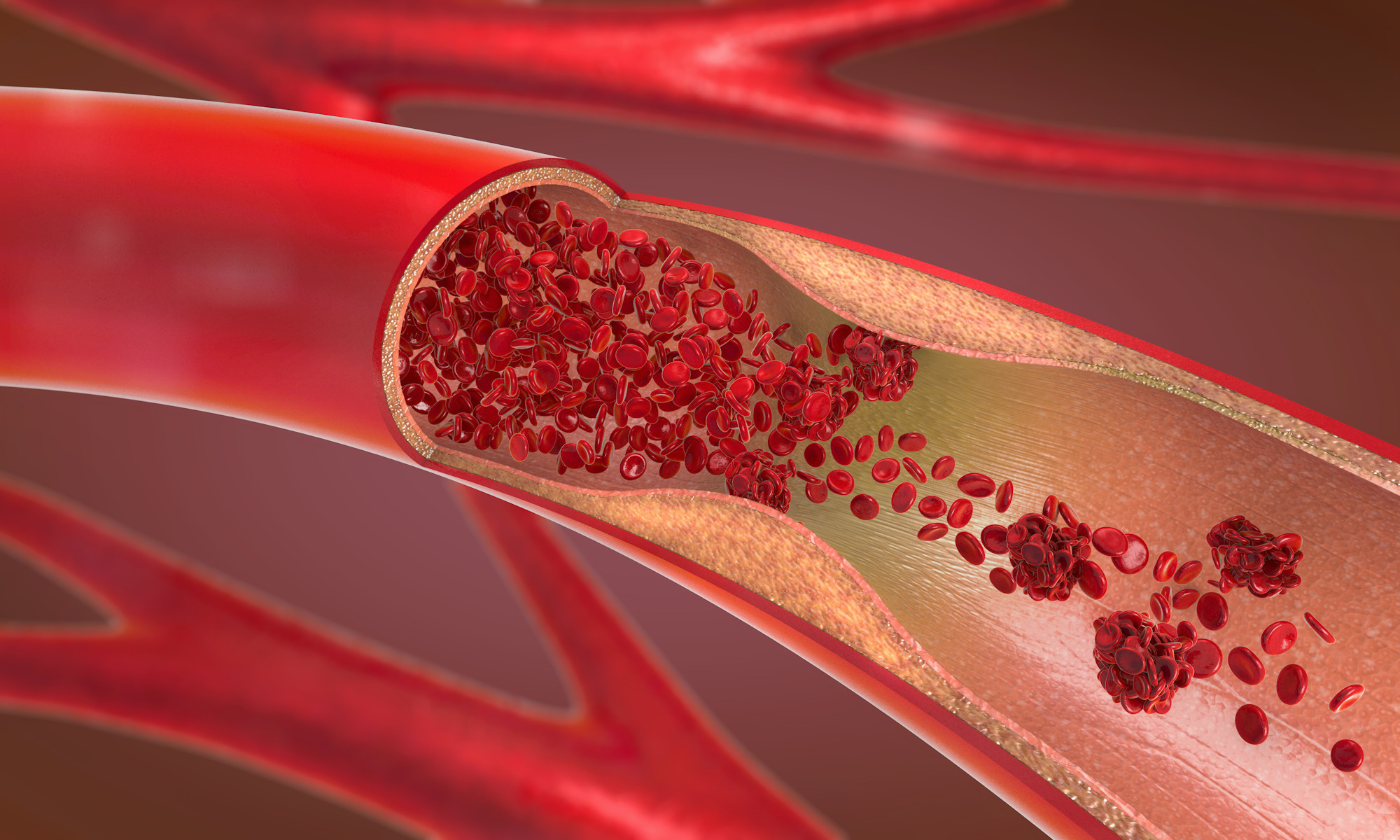
Vascular Society of Aotearoa New Zealand
The Home of Vascular Specialists in Aotearoa New Zealand
Lymphoedema
What is lymphoedema.
Oedema (or Edema) is a collection of fluid, so lymphoedema is a collection of lymph fluid in the body tissues.
Why is it called lymphoedema?
In every person there is a small amount of fluid (lymph) in the body tissues. This is fluid that has left the blood system to provide water and nourishment to the tissues. Normally most of this fluid is collected by a system of drainage tubes, similar to blood vessels, called the lymphatic system. There is a particularly well developed system of lymphatics in the intestines (lacteals) that absorb nutrients after ingested food has been broken down.
The movement of fluid through the lymphatic system is aided by contraction of muscles and there is also a gentle pumping action from the lymphatic vessels themselves. The fluid is filtered through lymph nodes and then eventually drains back to the blood system through a major vein on the left side of the neck. Lymph only flows in one direction towards the blood system and there are tiny valves in the lymphatic channels which aid in this one way flow. There is no circulation of lymph comparable to that in the blood vessel.
Lymph usually moves at about 120 mls/hr and about 2-4 litres of lymph are moved around the body each day. There is great redundancy in the lymphatic system which usually operates at about one tenth of its maximum load. When lymph load is too great, fluid accumulates in tissues rather than draining back into the blood stream and lymphoedema develops.
Why does lymphoedema occur?
Lymphoedema can occur for no apparent reason (Primary lymphoedema) or it can occur as a consequence of another problem (Secondary lymphoedema). Lymphoedema only affects the skin and fatty tissues and not the muscle compartments beneath.
Normal lymphatic vessels can increase the flow of lymph ten times if required. Because of this large reservoir capacity of the lymph system an increase in the formation of lymph fluid on its own does not cause lymphoedema. There must be some abnormality or problem with the lymphatic system itself.
Primary lymphoedema
In primary lymphoedema the lymphatic vessels themselves often appear to be abnormal. They can be very poorly developed (hypoplastic) or not developed at all (aplastic). Tiny valves in the lymphatics may also be faulty. Why this occurs is not entirely clear, but genetic abnormalities have been identified in some patients.
Primary lymphoedema can be divided into two main groups
1. Congenital onset primary lymphoedema
This can be a familial problem such as Milroy’s disease which involves swelling below the knee. It may also be sporadic as in lymphatic malformations, Turner’s syndrome and in other rare syndromes.
2. Post pubertal primary lymphoedema
This can also be a familial condition as in Distichiasis-lymphoedema associated with abnormalities of the eyelashes. It may also be sporadic as in inguinal node sclerosis or yellow-nail syndrome.
Lymphoedema praecox and lymphoedema tarda only refer to the age at which lymphoedema develops. Lymphoedema praecox develops in adolescence and Lymphoedema tarda generally after the age of 35 years. It is not known why normal adults, without known precipitating factors, should develop lymphoedema, but women are affected more commonly.
Secondary lymphoedema
In secondary lymphoedema the accumulation of fluid is because of another problem.
1. Cancer and radiotherapy
After certain types of surgery (breast surgery, node dissection for melanoma) the lymphatics are intentionally removed to reduce the risk of cancer recurrence. As a part of the treatment for some breast cancer or melanoma an axillary clearance may be performed in which all or most of the lymphatic tissue in the armpit is removed (axillary clearance). In melanoma and sometimes in other types of cancer a similar procedure is performed at the top of the leg in the groin (groin clearance). Although in many patients other lymphatics can compensate for the loss of lymphatic tissue, in some patients this is not enough and lymphoedema develops in the arm or the leg. Significant lymphoedema occurs in about 10% (1 in 10) of breast cancer patients. This can also occur after radiotherapy which can damage lymphatic vessels. In patients who have had both surgery and radiotherapy there is an even greater risk of developing lymphoedema. After surgery lymphoedema may not develop immediately. It can develop gradually as the operation site heals by the formation of scar tissue. About one third of the patients who develop lymphoedema will do so more than one year after their breast cancer surgery.
In some patients the development of cancers themselves can lead to lymphoedema. This is because sometimes the tumour cells invade the lymphatic vessels, blocking them.
2. Infection
In tropical countries a tiny worm infection ( filariasis ) in the lymphatics can lead to massive lymphoedema (elephantiasis) of the legs and genital area. The skin also becomes very thickened and with overhanging folds which can resemble the foot of an elephant. This is because the worm is present in the lymphatic vessels and it blocks the flow of lymph fluid. Filariasis is the most common form of secondary lymphoedema worldwide.
Cellulitis is a common soft tissue infection in which the tissues become red, hot, swollen and tender. This typically occurs in the lower leg but can develop anywhere in the body. In severe infections the inflammation can spread to the lymphatics (lymphangitis) and cause damage by leading to scarring around the lymphatics as the inflammatory process resolves. Frequent damage to the lymphatics caused by infection can also lead to swelling because of scarring around the lymphatic channels.
In New Zealand and Australia bites from insects are often blamed for persistent swelling particularly in the legs. The white-tailed spider is frequently blamed, but there is little evidence that this insect is more likely than others to lead to problems. The majority of the problems after an insect bite are probably related to the secondary infection that develops and could develop after any sort of skin break.
What problems can lymphoedema cause?
Swelling – Initially lymphoedema may only cause cosmetic concerns or heaviness and difficulty with some movements. This is because the leg (or arm) that is affected will be swollen and the skin may become slightly shiny. It also contains extra fluid so will feel heavier, because it is heavier. This may be all that happens in some patients.
Cellulitis – the presence of extra tissue fluid causing swelling in the leg can also make the patient more likely to develop infection in the tissues (cellulitis). The lymph fluid itself is very rich in protein and is an ideal fluid for bacterial growth. This can occur even after a minor injury. When this occurs the leg can swell to a greater extent. It will become red, tender and painful and the patient will probably feel generally unwell. This problem can usually be treated effectively with antibiotics, bedrest and elevation of the limb.
Fibrosis – the mere presence of significant amounts of lymph fluid in the tissues over many years can lead to scarring and fibrosis of the tissues. Once infection and inflammation resolve there will inevitably be some residual scar damage to the tissues of the leg leading to slightly more swelling than before. This puts the leg at a slightly greater risk of infection. A vicious cycle can then develop with further infection leading to further swelling and so on. It is important to try and halt this process at an early stage when most of the changes in the leg are at a reversible stage. As well as swelling due to lymphoedema, the skin can become very thickened (hyperkeratosis) and abnormal.
Tumours – very rarely tumours (lymphangiosarcoma) can develop in the chronically inflamed tissues. This is sometimes called Stewart-Treves syndrome.
How is lymphoedema diagnosed?
The diagnosis of lymphoedema is made by your doctor taking a careful medical history and examining the affected areas. This is often sufficient to decide lymphoedema is the likely cause. Lymphoscintigraphy or lymphangiography can sometimes be used to confirm the cause and give further information.
Lymphangiography is a predominantly anatomical test outlining the channels along which lymph drains. It was never widely used because of the difficulties cannulating tiny lymphatic channels and a potential risk of damage to the lymphatic system itself. Radionuclide lymphoscintigraphy was introduced in the 1950s and tells us much more about the function of the lymphatics and how well they are working. This is an easier test to perform and has become the gold standard. In most patients it is not necessary to perform either test.
Gadolinium enhanced magnetic resonance scans (MRI) are also being used in some centres and can produce impressive pictures. This is a very specialised test and few radiologists will have experience of MRI for this indication, but it has much better resolution than lymphoscintigraphy and is likely to be more sensitive and accurate ( Liu et al 2010 ).
Sometimes other tests may be necessary to exclude other conditions. Special scans of the veins may be required to ensure they are working normally.
What treatment is available?
Treatment for lymphoedema needs to be intensive and lifelong. Lymphoedema cannot be cured, but it can be controlled. Benefits can be obtained from the treatments detailed below, but if they are stopped then problems will re-occur. There is debate about whether lymphoedema can be prevented. Breast cancer patients who have undergone surgery to the armpit are usually advised to avoid any procedures, such as having blood taken, from the arm on the same side. They are also advised to avoid insertion of drips and vaccination on the same side as axillary surgery. There is little evidence to support this advice but women with lymphoedema following breast cancer have a need for advice, information and ongoing treatment 3-5 years after their diagnosis ( Girgis 2011 ).
Massage and manual lymphatic drainage (MLD) – Intensive massage by practitioners trained in specific techniques helpful in lymphoedema is the initial treatment of choice, but not always widely available.
This massage is based on creating spaces in the tissues and then massaging fluid into these spaces and away from the limb. To do this the massage needs to start at the part of the limb where it attaches to the trunk where the lymphatics are relatively normal. The lymphoedema therapist then massages fluid away from this area towards the trunk. The massage then works gradually towards the hand or foot. This therapy may need to continue for some weeks until the decrease in swelling is satisfactory. It is time consuming but seems to be one of the most effective treatments.
There are different schools of massage technique each with variations that are thought to produce better results.
Compression hosiery and bandaging- Compression hosiery is crucial in maintaining the benefits produced from massage. Graduated high compression hosiery will prevent swelling re-accumulating once it has been reduced by massage. It is important that hoisery is worn at all times, except at at night. Bandaging is frequently used when swelling is severe. A combination of bandaging and massage can reduce limb size and then compression hosiery is applied.
Patients with lymphoedema usually need to wear the highest compression hosiery available either Class 3 or 4. These can be troublesome to put on, but are very beneficial in reducing swelling. It is frequently necessary to have made to measure stockings as the shape of the swollen limb may make off-the-shelf fitting impossible. Stockings require replacement approximately every 4-6 months, as they begin to lose their compressive effect.
Compression hosiery should not be used if there is significant arterial disease present.
Drugs – there is some evidence that drugs may be helpful, but they have limited value. Paroven may be of some use in some patients and is given at a dose of 3 grams daily. Coumarin has been used previously, but was withdrawn in 1998 as it caused severe liver problems in some patients.
Diuretics or water tablets that promote the passage of more urine are generally ineffective for lymphoedema. Patients will pass more urine but what fluid remains will still gravitate to the affected limb. This is because there is a local problem present leading to lymph retention and it is not due to excess fluid thoughout the whole body.
Surgery – Surgery has a very limited role in patients with lymphoedema. It is hardly ever required and will not be curative. Despite this two main types of operations have been developed. Firstly, in very particular types of patients some form of bypass or drainage procedure may be attempted to drain off the excess lymph fluid from the affected limb. Secondly, in patients with very severely affected limbs debulking operations have been performed to reduce the size of the affected limb by removing excess tissue.
Skin Care and control of infection – it is important to keep the skin in good condition. Regular hygiene particularly in skin creases and between the toes is essential. Anti-fungal powders can be helpful. Simple moisturising creams can be helpful for flaky skin. It is important to take minor wounds seriously and not to allow them to develop into serious problems. Minor infections should be treated aggressively with antibiotics.
Weight loss – many lymphoedema patients are overweight. This situation compounds any existing problems and weight loss is essential to achieve benefits from any other treatments.
Useful links
http://www.lymphoedemanz.org.nz/
http://www.lymphoedema.org.nz/home
http://www.nhs.uk/conditions/lymphoedema/Pages/Introduction.aspx
http://www.lymphnet.org/
http://lymphology.asn.au/new/index.php
http://www.lymphoedema.org/lsn/
http://www.uklymph.com/
http://www.lympho.org/resources.php
http://www.surgical-tutor.org.uk/default-home.htm?system/vascular/lymphoedema.htm~right
www.emedicine.com/med/topic2722.htm
http://www.diseasesdatabase.com/ddb7679.htm
http://en.wikipedia.org/wiki/Lymphedema
Liu N-F, Lu Q, Liu P-A, Wu X-F, Wang B-S. Comparison of radionuclide lymphoscintigraphy and dynamic magnetic resonance lymphangiography for investigating extremity lymphoedema . Br J Surg 2010; 97:359-365. Lee BB, Laredo J. Contemporary role of lymphoscintigraphy: we can no longer afford to ignore! Phlebology 2011; 26: 177-78. Girgis A, Stacey F, Lee T, Black D. Priorities for women with lymphoedema after treatment for breast cancer: population based cohort study Brit Med J 2011; 342: d3442.
Lymphoedema: a study of Otago women treated for breast cancer
Affiliation.
- 1 Otago Polytechnic, Dunedin.
- PMID: 9348900
Lymphoedema, the swollen arm that can follow treatment for breast cancer, is the build up of lymph fluid which is unable to flow normally due to the surgical removal of axillary lymph nodes or the scarring of these nodes from radiotherapy. Previous studies indicate a lack of recognition of preventative measures and treatment of lymphoedema amongst health professionals and women treated for breast cancer. There also appears to be a lack of acknowledgement of the effects that lymphoedema can have on those who develop it. Of 181 women surveyed 68 (38%) reported having developed arm swelling at some stage since their treatment, 56 (31%) of whom met the study criteria for lymphoedema. Of those with lymphoedema 21 (37%) women had not consulted anyone regarding their swollen arm; a further 10 (18%) sought advice, but were offered no treatment. Therefore, in total, 31 (55%) of the women with lymphoedema received no treatment. The remaining 25 (45%) were offered a variety of treatments. In the group of women with lymphoedema, most arm swelling occurred within the first year. For a smaller number, swelling occurred up to 25 years later. Twenty-one percent of those affected, recalled advice about its prevention, compared with 36% in the group who had not experienced lymphoedema. Lifestyles were affected in many ways, with 21 (37.5%) of the women reporting pain of varying intensity and frequency. Other effects were on dress/choice of clothing, household duties, sleep, employment and sports.
Publication types
- Research Support, Non-U.S. Gov't
- Breast Neoplasms / complications
- Breast Neoplasms / therapy*
- Health Surveys
- Lymphedema / etiology*
- Lymphedema / psychology
- New Zealand
- Patient Education as Topic
- Quality of Life
- Surveys and Questionnaires
- View all results
- Close search results
Lymphoedema
Stages of lymphoedema, managing lymphoedema.
- Email this article
- Copy this article's URL
- Lymphoedema is a side effect of breast cancer surgery and treatment
- It is a chronic condition that can be managed by the patient or lymphoedema therapist
- Cording is not associated with lymphoedema and requires separate intervention.
Lymphoedema develops when lymph fluid accumulates in the tissues. Treatment-induced lymphoedema can occur after the lymphatic drainage system is damaged, due to surgery (especially surgery to the axilla) or radiation therapy.
Lymphodema results in swelling of the affected limb (e.g. the arm on the side surgery has taken place). This can be permanent unless managed and it can lead to skin infections and cellulitis.
Symptoms of lymphoedema
The onset of lymphoedema can occur shortly after treatment or years later. It usually develops gradually.
Symptoms include:
- Swelling of the arm, hand, breast or trunk
- The arm or limb might feel heavy, achy or stiff. There may be limited range of movement and jewellery or clothing may feel tighter than usual
- Swelling may be aggravated by heat, overuse or prolonged inactivity. Symptoms may be worse at the end of the day.
Further reading
- Australasian Lymphology Association
- Lymphoedema NZ
Patient support
- Breast Cancer Foundation NZ webinar: Life with lymphoedema
- Patient information on Lymphoedema
- Lymphoedema NZ support groups
- Additional support available to people with lymphoedema
- Contact Breast Cancer Foundation NZ nursing team
Lymphoedema is a progressive, chronic condition. Early intervention can prevent infection, improve range of motion and improve patients’ quality of life. Evidence suggests that early intervention for those at risk of lymphoedema or those who have early lymphoedema leads to better outcomes.
Risk factors for lymphoedema
- The extent of surgery, lymph node removal and radiation therapy
- Skin infections on or near the affected area
- Injury (e.g. sprains, fractures, cuts or wounds) on the affected side
- Obesity and immobility
- Constriction from tight clothes, jewellery or blood pressure tests
- Exposure to excessive heat, including sunburn.
Patients may be advised to limit blood pressure readings, blood tests, injections or IV ports taken on the affected limb.
Treatment for lymphoedema
Lymphoedema therapy in New Zealand is based on the five ‘cornerstones’ of care:
- Light touch massage
- Compression bandages or garments
- Special care of the affected limb or area
- Medical taping.
Was this article helpful?
Suggest an edit.
Would additional content be helpful on this page? Email suggestions and feedback to [email protected] . Thank you.

COMMENTS
Lymphedema is a common, complex, and inexplicably underappreciated human disease. Despite a history of relative neglect by health care providers and by governmental health care agencies, the last decade has seen an explosive growth of insights into, and approaches to, the problem of human lymphedema. The current review highlights the significant advances that have occurred in the investigative ...
Increased investigation has demonstrated the key role of inflammation and resultant fibrosis and adipose deposition leading to the clinical sequelae and associated reduction in quality of life with lymphedema. New imaging techniques including magnetic resonance imaging (MRI), indocyanine green lymphography, and high-frequency ultrasound offer ...
Background: In lymphedema, the accumulation of subcutaneous interstitial fluid is the most characteristic feature. Bioimpedance analysis (BIA) is a promising technique to measure the amount of body components using a noninvasive method. In this study, we determined the clinical significance of BIA parameters in upper limb lymphedema with surgical treatment such as lymphovenous anastomosis or ...
Sponsors. Lymph Info Trust. The Lymph Info Trust wants to improve the quality of life of anyone in NZ with a lymphatic condition through education and raising awareness. We will empower New Zealanders who are living with lymphoedema, lipoedema and phlebolymphoedema. We provide understandable information, education and resources.
This document, by a selected panel of experts in lymphatic medicine from the USA, New Zealand and Korea, identified seven priorities for research in the field, including lymphatic decompression in ...
4 Auckland Bioengineering Institute, The University of Auckland, Auckland, New Zealand. 5 Australian Lymphoedema Education Research and ... from 2008 to 2023 who previously underwent ALND for cancer treatment and did not develop upper extremity cancer-related lymphedema. ALND patients were matched to control patients presenting with cutaneous ...
Regardless, it is clear that less extensive axillary surgery results in less lymphedema, and therefore, surgical research has focused on how to extend SLNB to more patients. ... , 64 as well as with establishment of new lymphaticovenous drainage within these driven by perfusion gradients between the arterial inflow and venous outflow ...
Lymphoedema occurs when the lymphatic system is not working properly due to damaged or removed lymph nodes. For people with cancer, this can be brought about by surgery or radiation although not everyone who has had these treatments will develop the condition. "If you've had treatment on your leg, then it's possible this area may be ...
Northwestern University scientists led by SQI member Susan Quaggin have uncovered molecular mechanisms underlying lymphatic valve development, a discovery which could prove useful in treating lymphedema, according to a study published in The Journal of Clinical Investigation.. Lymphedema, a chronic condition that causes localized swelling, has no known cure and affects one in 100,000 ...
Study identifies potential drug target for lymphedema. The human lymphatic system consists of a vast network of vessels that drain protein-rich fluid in tissues and transport it to lymph nodes ...
Lymphedema has historically been underrated in clinical practice, education, and scholarship to the detriment of many patients with this chronic, debilitating condition. The mechanical insufficiency of the lymphatic system causes the abnormal accumulation of protein-rich fluid in the interstitium, which triggers a cascade of adverse consequences such as fat deposition and fibrosis. As the ...
What is this research hoping to achieve? Professor David Baxter and his team will evaluate the potential effectiveness of low level laser therapy (LLLT) for breast cancer-related lymphoedema, its acceptability to patients and therapists, and the feasibility of incorporating the treatment into existing clinical practice within New Zealand's hospitals.
The importance of the diagnosis of lymphoedema results from the frequent appearance of this problem, particularly after breast cancer treatment. Although the lymphoedema is often underestimated, it causes significant live problems for patients and serious health complications. The aim of the project is to design and develop a device for identification and monitoring of lymphoedematous ...
Simple Summary. Lymphedema is a chronic, debilitating disease of the lymphatic vasculature. Although several reviews focus on the anatomy and physiology of the lymphatic system, this review provides an overview of the lymphatic vasculature and, moreover, of lymphatic system dysfunction and lymphedema. Further, we aim at advancing the knowledge ...
Surgical options at Mayo Clinic. Mayo Clinic is a leader in surgical options to reverse the damage from lymphedema. Dr. Forte specializes in lymphovenous bypass, a microsurgery done under powerful microscopes that are magnified 20 to 25 times. Through an incision no larger than a paper cut, the surgery connects tiny lymphatic vessels smaller ...
Cancer Research. About Our Research; National Research Grants 2024; Māori Cancer Researcher Awards; ... There is a risk of lymphedema if you have: lymph nodes are damaged or removed during surgery; ... Latest advice from The Australian and New Zealand College of Anaesthetists (ANZCA) shows that the arm on the affected side can usually be used ...
Lymphoedema is the swelling of a limb and/or parts of the body caused by the lymphatic system not functioning properly and becoming compromised. The lymphatic system plays an important role in the body's defence against infection by filtering and removing bacteria. The swelling can occur when the normal process of lymph drainage doesn't ...
Significant lymphoedema occurs in about 10% (1 in 10) of breast cancer patients. This can also occur after radiotherapy which can damage lymphatic vessels. In patients who have had both surgery and radiotherapy there is an even greater risk of developing lymphoedema. After surgery lymphoedema may not develop immediately.
Lymphoedema, the swollen arm that can follow treatment for breast cancer, is the build up of lymph fluid which is unable to flow normally due to the surgical removal of axillary lymph nodes or the scarring of these nodes from radiotherapy. Previous studies indicate a lack of recognition of preventative measures and treatment of lymphoedema ...
Lymphoedema. Lymphoedema develops when lymph fluid accumulates in the tissues. Treatment-induced lymphoedema can occur after the lymphatic drainage system is damaged, due to surgery (especially surgery to the axilla) or radiation therapy. Lymphodema results in swelling of the affected limb (e.g. the arm on the side surgery has taken place).
For more information please contact Louise Quertier by calling the Lodge on. (07) 834 2351 or emailing Louise on [email protected]. Rotorua Support Group. Co-ordinator Vanessa Malipaard can be contacted on (07) 348 8211 or 027 350 8843. Healthy Steps: weekly exercise classes in Auckland.
The following links provide further information about lymphoedema. Be aware that websites from other countries may have information that differs from New Zealand recommendations. In the United States the condition is spelled lymphedema. Childhood and teenage lymphoedema (external link) The Lymphoedema Support Network, UK