- Alzheimer's & Dementia
- Asthma & Allergies
- Atopic Dermatitis
- Breast Cancer
- Cardiovascular Health
- Environment & Sustainability
- Exercise & Fitness
- Headache & Migraine
- Health Equity
- HIV & AIDS
- Human Biology
- Men's Health
- Mental Health
- Multiple Sclerosis (MS)
- Parkinson's Disease
- Psoriatic Arthritis
- Sexual Health
- Ulcerative Colitis
- Women's Health
- Nutrition & Fitness
- Vitamins & Supplements
- At-Home Testing
- Men’s Health
- Women’s Health
- Latest News
- Medical Myths
- Honest Nutrition
- Through My Eyes
- New Normal Health
- 2023 in medicine
- Why exercise is key to living a long and healthy life
- What do we know about the gut microbiome in IBD?
- My podcast changed me
- Can 'biological race' explain disparities in health?
- Why Parkinson's research is zooming in on the gut
- Health Hubs
- Find a Doctor
- BMI Calculators and Charts
- Blood Pressure Chart: Ranges and Guide
- Breast Cancer: Self-Examination Guide
- Sleep Calculator
- RA Myths vs Facts
- Type 2 Diabetes: Managing Blood Sugar
- Ankylosing Spondylitis Pain: Fact or Fiction
- Our Editorial Process
- Content Integrity
- Conscious Language
- Health Conditions
- Health Products

Sex and sexual health tips for transgender women after gender-affirming surgery

Lower gender-affirming surgery for trans women will mean they need to wait until the surgical site heals before having sex. Using lubricant and taking additional steps to protect against contracting sexually transmitted infections (STIs) can also help during the healing process.
Three options for lower gender-affirming surgery for transgender women include:
- Orchidectomy : This involves the removal of the testes. It can be a stand-alone procedure or occur during a vaginoplasty.
- Vaginoplasty: This involves removing the penis, testicles, and scrotum and creating a vaginal canal and labia. The surgeon will also create a clitoris using a portion of the glans penis.
- Vulvoplasty: This creates a vulva, including the mons pubis, labia, clitoris, and urethral opening. People may opt for this surgery if they are uninterested in receptive vaginal sex or do not wish to maintain the dilation and aftercare regime necessary after vaginoplasty. People may also refer to this option as a minimal depth vaginoplasty.
This article discusses how long recovery can take and when people can have sex after gender-affirming surgery.
It also looks at what to expect during sex after surgery and tips for hygiene, contraception , and protection from infections.
When can a person have sex after surgery?

According to Johns Hopkins Medicine , people can have receptive intercourse or take part in any sexual activity 12 weeks after a vaginoplasty. Sexual activity before this may lead to delayed wound healing and complications.
After an orchidectomy, it may take 1–2 days for people to become fully mobile again. They may be able to return to work a few days to a week after surgery.
Full recovery from an orchidectomy may take 2–8 weeks . For a few weeks following surgery, people will not be able to carry out certain activities such as driving or heavy lifting. The area of surgery will need to fully heal before people can have sex.
A healthcare professional can advise people when it is safe for them to have sex after gender-affirming surgery.
Will it be possible to achieve orgasm?
Following surgery, it can take time for people to recover and start to experience orgasms.
When people undergo a vulvoplasty, the surgeon forms a clitoris from the head of the penis. This means most people will still be able to experience orgasms through clitoral stimulation.
Johns Hopkins Medicine states that people may experience clitoral sensation after a vaginoplasty, although it can vary for each individual. Nerve regeneration may begin around 3 weeks following surgery, but in some cases, it may take a year or more to regain sensation.
People may experience a shooting or tingling sensation as the nerves regenerate, which should decrease over time.
In a 2017 study , 84 participants had rectosigmoid vaginoplasty. A post-surgery interview found that 79 of the participants had had sexual intercourse, and 72 had experienced orgasm.
Some reported infrequent symptoms, such as pain after sex and vaginal spotting , but these improved within 6 months.
A 2016 study of 22 people who had undergone a vaginoplasty and clitoroplasty found that 86% of participants could experience orgasm after surgery.
In addition, research from 2017 involving 28 transgender women found that pressure and vibration provided the best results for genital sensitivity after gender-affirming surgery.
How will it affect libido?
Transgender women may experience a decrease in sex drive after gender-affirming surgery.
According to a 2020 article , people can stop taking anti- testosterone medication and may experience a decreased sex drive following an orchidectomy.
Hormone replacement therapy may help maintain a regular sex drive.
Vaginal depth and lubrication
Vaginal depth after a vaginoplasty can vary for each person and depend on the amount of skin in the genital area before surgery.
An average vaginal depth after a vaginoplasty is 4–6 inches . For comparison, the average depth of a cisgender female’s vagina measures from 3.5 to 5 inches .
In people who have a rectosigmoid vaginoplasty or colovaginoplasty, the vagina may have more depth.
The University of California, San Francisco Medical Centre notes that the most common vaginoplasty technique uses the penile inversion procedure. This does not create a vaginal mucosa. As a result, the vagina will not self-lubricate, and a person will need to use lubricants to undergo dilation or have penetrative sex.
Another vaginoplasty technique uses the colon or small bowel to line the vagina, which will result in a self-lubricating vagina. However, it is a far less common procedure that may lead to serious and possibly life threatening complications.
When using lubrication, people should use a water or silicone-based lube with latex condoms, as oil-based lubricants can damage latex.
Aftercare and dilation
After a vaginoplasty, people need to use a vaginal dilator to stretch the vaginal canal and keep it open. Following surgery, people may need to dilate twice each day for a minimum of 15 minutes. This helps prevent loss of vaginal depth and width.
A healthcare professional will provide instructions on how to safely and correctly use a dilator. Although people may experience some discomfort when they begin dilating, they should not experience any severe pain.
If people experience pain when dilating, they will need to stop and readjust the dilator and body position. People will also need to use lubrication during dilation.
An orchidectomy can cause testosterone levels to drop. A sudden drop in testosterone may lead to mood swings or low energy following surgery.
To help prevent this, people may want to discuss mild testosterone replacement options with a healthcare professional to allow a more gradual reduction in testosterone.
People may need to use plenty of lubricant to make sex feel more comfortable and prevent any tears. They may also find the rest of the genital area, including the anus, is more tender following surgery.
Contraception and STIs
According to the Terrence Higgins Trust , surgery can increase the risk of contracting STIs , as any unhealed skin can allow infections to pass more easily into the body.
If people have had a vaginoplasty that uses part of the colon, a mucus membrane will line the vagina, making it easier for STIs to pass through.
If people have had a vaginoplasty that uses penile and scrotal skin, the vagina is less susceptible to STIs, but any unhealed skin can still be a risk factor.
Dilation of the vagina can also cause bleeding, so it is important to use a condom for any sex following dilation.
Using a condom during sex can help protect from STIs. People can use an external condom over a penis or sex toy and an internal condom inside a vagina. An internal condom may not suit everyone, as using an internal condom will depend on vaginal depth.
People can also use a dental dam during oral-vaginal sex. Regular testing can help to prevent passing on or contracting STIs from a sexual partner.
If people have not had an orchidectomy or vasectomy, they will need to use contraception for any penetrative sex with a partner who is able to get pregnant and is not using contraception.
If people are taking estrogen or other hormone therapy, these will not provide enough contraceptive protection, so they will need to use other contraceptive methods.
Learn more about sexual health for transgender women here.
Hygiene tips
After a vaginoplasty, it is important to keep the genital area clean and free of infection .
People will need to keep the outside of the vagina dry. It may be useful to place an absorbent pad between the labia to soak up any excess moisture.
Once the genital area is allowed to get wet, people should use soap and water to gently wash the area. It is important to avoid scrubbing or allowing shower spray to reach the surgical site.
Johns Hopkins Medicine states that people will need to douche using a non-fragranced vaginal douche , beginning 8 days after surgery. Depending on how much vaginal discharge people have, douching may be required 1–2 times each week. More frequent douching may be necessary if there is a large amount of discharge.
Following an orchidectomy, people may experience some mild discomfort, bruising, and swelling around the area of surgery. Some bleeding may occur, although this is rare . People may need to apply topical antibiotics to prevent infection.
People will need to speak with a healthcare professional to check when they can bathe the area of surgery following an orchidectomy.
It can take time to heal, recover, and adjust to sex and intimacy after gender-affirming surgery.
If people are experiencing any physical or emotional issues regarding surgery, they can speak with a doctor, a mental health professional, or a sex therapist.
Last medically reviewed on October 27, 2021
- Sexual Health / STDs
How we reviewed this article:
- Can transgender women have orgasms after gender-reassignment surgery? (n.d.). https://issm.info/sexual-health-qa/can-transgender-women-have-orgasms-after-gender-reassignment-surgery
- FAQ: Vaginoplasty. (n.d.). https://www.hopkinsmedicine.org/center-transgender-health/services-appointments/faq/vaginoplasty
- Kim, S-K., et al . (2017). Is rectosigmoid vaginoplasty still useful? https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5300923/
- LeBreton, M., et al. (2016). Genital sensory detection thresholds and patient satisfaction with vaginoplasty in male-to-female transgender women. https://www.jsm.jsexmed.org/article/S1743-6095(16)30859-1/fulltext
- Meltzer, T. (2016). Vaginoplasty procedures, complications and aftercare. https://transcare.ucsf.edu/guidelines/vaginoplasty
- Orchiectomy. (n.d.). https://transcare.ucsf.edu/orchiectomy
- Orchiectomy. (n.d.). https://www.transhub.org.au/orchiectomy
- Orchiectomy. (n.d.). http://www.phsa.ca/transcarebc/surgery/gen-affirming/lower-body-surgeries/orchiectomy#Post--surgery
- Safer sex and sexual health for trans feminine people. (n.d.). https://www.tht.org.uk/hiv-and-sexual-health/sexual-health/trans-people/trans-feminine/safer-sex
- Sigurjónsson, H., et al. (2017). Long-term sensitivity and patient-reported functionality of the neoclitoris after gender reassignment surgery. https://www.jsm.jsexmed.org/article/S1743-6095(16)30857-8/fulltext
- Vaginoplasty / vulvoplasty. (n.d.). https://healthcare.utah.edu/transgender-health/gender-affirmation-surgery/vaginoplasty.php
- van der Sluis, W. B., et al . (2020). Orchiectomy in transgender individuals: A motivation analysis and report of surgical outcomes. https://www.tandfonline.com/doi/full/10.1080/26895269.2020.1749921
Share this article
Latest news
Related coverage.
There is no age limit on when a person can transition. Learn more about how to do so here.
Transgender is a term to refer to those who have a different gender identity than the one assigned to them at birth. Learn more here.
Estrogen hormone therapy can cause physical, sexual, reproductive, and emotional changes. Learn more about how it affects the body here.
Keelee MacPhee, M.D.
Transgender Surgery & Plastic Surgery
TRANSGENDER SURGERY COSMETIC PLASTIC SURGERY BOARD CERTIFIED
MTF Vaginoplasty
In male-to-female sex reassignment, the trans woman may choose to undergo vaginoplasty – the inversion of the penis to create a vagina – as part of her physical transition. This procedure can result in a fully sensate neovagina.
Dr. MacPhee performs this reconstructive procedure by disassembling the penis and utilizing the inverted penile and scrotal skin flap and urethral flap to construct a new vulva, clitoris and vagina. The blood and nerve supplies are preserved to provide sensation, and the urethra is used to create the mucosal part of the vagina that provides additional sensitivity and wetting. The remaining penile and scrotal tissue are used to form the clitoral hood and labia.
The depth and diameter of the neovagina may be limited due the narrowness of the male pelvis. At the time of surgery, a stent is put in place to form vaginal dimensions, and the patient will need to dilate the vagina following surgery, frequently at first and tapering over time. A typical post-op protocol will involve dilating three times a day for 50 minutes each time for the first year. After that, maintenance dilation will be necessary for life. View MTF genital reconstruction results in our Photo Gallery.
Dr. MacPhee also performs orchiectomy, scrotal skin removal and limit-depth vaginoplasty procedures as alternatives to full MTF genital reconstruction .
PHOTO GALLERY

We are grateful for our many patients who are willing to share their experiences and results. Click … Read More >
MEET DR. MACPHEE

A highly skilled Plastic & Reconstructive surgeon in practice for more than 17 years, Dr. Keelee … Read More >
TRANSGENDER SURGERY

Dr. Keelee MacPhee has been performing gender affirming surgery since 2005 and is grateful for the … Read More >
READ OUR BLOG

Tune into our blog for recent news about GRS and the latest trends in cosmetic surgery procedures … Read More >
- About Dr. MacPhee
- Office Environment
- Surgery Hospitals
- Blog / News
- Photo Gallery
- Patient Forms
- Price Transparency
- Referring Therapists
- Referring Physicians

Graphic Medical Content
Content May be Inappropriate for Younger Audiences
Are you over 18 years of age?

- Health Care Home
- Transgender Health Program
- Gender Affirmation Surgery
Vaginoplasty / Vulvoplasty
Wpath standards of care.
- Breast Augmentation
- Facial Feminization Surgery
- Orchiectomy
- Vaginoplasty / Vulvuplasty
Gender affirmation surgery for a transfeminine person is sometimes called bottom surgery. These are three surgeries that can help a patient feel more aligned with their gender identity. They are:
- vaginoplasty,
- vulvoplasty, and
- orchiectomy .
Criteria for Vaginoplasty Vulvoplasty in Transfeminine Patients
- Persistent, well documented gender dysphoria;
- Capacity to make a fully informed decision and to consent for treatment;
- be the age of majority in a given country;
- If significant medical or mental health concerns are present, they must be well controlled;
- 12 continuous months of hormone therapy as appropriate to the patient’s gender goals (unless the patient has a medical contraindication or is otherwise unable or unwilling to take hormones);
- 12 continuous months of living in a gender role that is congruent with their gender identity.
Vaginoplasty
During a vaginoplasty surgery, a surgeon creates both an outer and inner vagina by using skin and tissue from a penis.
- Your surgeon will use skin from the penis and scrotum to build the inner and outer labia of the vagina
- Your surgeon will create a new opening for the urethra (so you can urinate)
- Your surgeon will use tissue from your foreskin to build the new opening of the vagina (also called the introitus).
Vaginoplasty Procedure
During most vaginoplasties, your surgeon will use a skin graft to create a new vaginal canal (the inside wall of the vagina). To do this, your surgeon will take skin from your scrotum and thin it so it works well as a skin graft.
If there’s not enough skin from your scrotum to make your new vagina, then your surgeon can take extra skin from the sides of your abdomen where there won’t be a very noticeable scar.
To make your new vaginal canal, your surgeon will create a space between your rectum and bladder. Once your skin graft is inserted, your surgeon will place gauze or spongy material inside the new vaginal canal for 5 days. The gauze puts pressure on the skin graft so it grows like it should into the surrounding vaginal tissue.
Vaginoplasty & Orgasms
Many transfeminine people wonder if they’ll still be able to have orgasms after having a vaginoplasty.
Your surgeon will use skin from your penis to create a clitoris. This clitoris still has feeling, and most transgender women can have orgasm through clitoral stimulation.
How Long Will I Be in the Hospital After Vaginoplasty?
Patients are in the hospital for 5 days and mostly rest in bed. Resting will help your skin graft grow into the surrounding tissue in your vaginal canal.
Your surgeon will also place a compressive bandage on the outside of your vagina. After the outer and inner bandages are removed, most patients feel fine and can leave the hospital.
When Should I Start to Dilate my Vagina After Vaginoplasty?
Each patient’s situation is different, but we recommend waiting two weeks after your surgery before you start dilating your vagina. Waiting two weeks will let your vagina heal.
Your surgeon will give you vaginal dilators to use at home. You should dilate your vagina two to three times each day for the first six months after your surgery.
Read this instruction sheet on how to dilate your vagina after having a vaginoplasty .
Preparing for Vaginoplasty Surgery
There are several things that patients need to do before having a vaginoplasty.
Pursue hair reduction: The first thing you’ll need to do is have hair removal on your scrotum and lower penile skin. Your vaginoplasty surgeon will use this skin to create your new vaginal canal. If hair were to grow inside your new vagina, it would create hygiene problems.
Quit smoking: If you’re a smoker, it’s very important for you to quit. Smoking, vaping, or using any nicotine products decreases blood flow to the area around your genitals and will make it harder for you to heal after your surgery.
If you’re a recent smoker, we will give you a nicotine urine test to make sure you’ve been able to quit completely. Nicotine takes about a month to wash out of your system before the test results will be negative.
Weight considerations : Keep in mind that patients with a body mass index ( BMI *) greater than 35 are at a higher risk for wound healing problems and complications after surgery. However, we understand that BMI is not a perfect measure of your overall health. We will discuss how your weight may affect you and the potential benefits of losing weight before surgery. If our team decides that weight loss is the best pre-surgical option for you, we will refer you to our weight management program .
For some people, vaginoplasty or vulvoplasty may not be possible because of their body shape and weight.
Physical Therapy for Vaginoplasty
Both before and after having a vaginoplasty, your surgeon will recommend that you start seeing a physical therapist. Physical therapy can help you prepare for this surgery.
Vulvoplasty
The vulva is the outside part of the vagina. A vulvoplasty is a type of surgery that uses skin and tissue from a penis to create all of the outside parts of a vagina (except for the vaginal canal).
The steps of a vulvoplasty are the same as a vaginoplasty. During a vulvoplasty, your surgeon will:
- create a clitoris out of the glans (or head) of the penis,
- create an inner and outer labia from skin on the penis and scrotum,
- create the opening of the urethra so you can urinate, and
- create the introitus (opening of the vagina).
The only thing that’s different between a full vaginoplasty and a vulvoplasty is the internal part of the vaginal canal.
- Vaginoplasty creates a vaginal canal.
- Vulvoplasty creates all the parts of a vagina except for the vaginal canal.
After vulvoplasty, this means you won’t be able to have intercourse or insert a penis into your vagina.
How Do I Choose Between a Vulvoplasty vs. Vaginoplasty?
A vulvoplasty has a much easier recovery. For example, you won’t need to dilate (or stretch) your vagina.
Another reason to consider vulvoplasty instead of vaginoplasty is because of medical problems or complications. One serious complication after vaginoplasty is called rectal injury. In some cases, a rectal injury can create a hole between your rectum and vagina.
But your chances of developing a rectal injury are much lower if you have a vulvoplasty instead of a vaginoplasty.
Sex & Vaginal Intercourse
Some patients know that they’re not interested in having vaginal intercourse. For these patients, a vulvoplasty may be a better choice.
After a vulvoplasty, you can still have orgasms through clitoral stimulation, just like with vaginoplasty. During a vulvoplasty, your surgeon will create a clitoris from the glans or head of the penis.
How Long Will I Be in the Hospital After Vulvoplasty?
Patients usually are in the hospital for 3 days after having a vulvoplasty. Your surgical team will give you a compressive dressing that reduces inflammation (swelling) after your surgery.
Most patients rest in bed while they’re healing since the dressing is uncomfortable to walk with.
After your dressing is removed, you can leave the hospital, usually right at about 3 days.
Find a Surgeon
Post-surgery instructions, vaginal dilation instructions, hear from our patient.
"I definitely feel complete. I feel whole. But that doesn’t describe it… that doesn’t even begin to describe it,” beams Josie Jesse as she sits, finally comfortable, in her new body that reflects who she has always been.
Read Josie Jesse's Story

- Patient Care & Health Information
- Tests & Procedures
- Feminizing surgery
Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation. Bottom surgery can involve removal of the testicles, or removal of the testicles and penis and the creation of a vagina, labia and clitoris. Facial procedures or body-contouring procedures can be used as well.
Not everybody chooses to have feminizing surgery. These surgeries can be expensive, carry risks and complications, and involve follow-up medical care and procedures. Certain surgeries change fertility and sexual sensations. They also may change how you feel about your body.
Your health care team can talk with you about your options and help you weigh the risks and benefits.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Available Sexual Health Solutions at Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
Many people seek feminizing surgery as a step in the process of treating discomfort or distress because their gender identity differs from their sex assigned at birth. The medical term for this is gender dysphoria.
For some people, having feminizing surgery feels like a natural step. It's important to their sense of self. Others choose not to have surgery. All people relate to their bodies differently and should make individual choices that best suit their needs.
Feminizing surgery may include:
- Removal of the testicles alone. This is called orchiectomy.
- Removal of the penis, called penectomy.
- Removal of the testicles.
- Creation of a vagina, called vaginoplasty.
- Creation of a clitoris, called clitoroplasty.
- Creation of labia, called labioplasty.
- Breast surgery. Surgery to increase breast size is called top surgery or breast augmentation. It can be done through implants, the placement of tissue expanders under breast tissue, or the transplantation of fat from other parts of the body into the breast.
- Plastic surgery on the face. This is called facial feminization surgery. It involves plastic surgery techniques in which the jaw, chin, cheeks, forehead, nose, and areas surrounding the eyes, ears or lips are changed to create a more feminine appearance.
- Tummy tuck, called abdominoplasty.
- Buttock lift, called gluteal augmentation.
- Liposuction, a surgical procedure that uses a suction technique to remove fat from specific areas of the body.
- Voice feminizing therapy and surgery. These are techniques used to raise voice pitch.
- Tracheal shave. This surgery reduces the thyroid cartilage, also called the Adam's apple.
- Scalp hair transplant. This procedure removes hair follicles from the back and side of the head and transplants them to balding areas.
- Hair removal. A laser can be used to remove unwanted hair. Another option is electrolysis, a procedure that involves inserting a tiny needle into each hair follicle. The needle emits a pulse of electric current that damages and eventually destroys the follicle.
Your health care provider might advise against these surgeries if you have:
- Significant medical conditions that haven't been addressed.
- Behavioral health conditions that haven't been addressed.
- Any condition that limits your ability to give your informed consent.
Like any other type of major surgery, many types of feminizing surgery pose a risk of bleeding, infection and a reaction to anesthesia. Other complications might include:
- Delayed wound healing
- Fluid buildup beneath the skin, called seroma
- Bruising, also called hematoma
- Changes in skin sensation such as pain that doesn't go away, tingling, reduced sensation or numbness
- Damaged or dead body tissue — a condition known as tissue necrosis — such as in the vagina or labia
- A blood clot in a deep vein, called deep vein thrombosis, or a blood clot in the lung, called pulmonary embolism
- Development of an irregular connection between two body parts, called a fistula, such as between the bladder or bowel into the vagina
- Urinary problems, such as incontinence
- Pelvic floor problems
- Permanent scarring
- Loss of sexual pleasure or function
- Worsening of a behavioral health problem
Certain types of feminizing surgery may limit or end fertility. If you want to have biological children and you're having surgery that involves your reproductive organs, talk to your health care provider before surgery. You may be able to freeze sperm with a technique called sperm cryopreservation.
How you prepare
Before surgery, you meet with your surgeon. Work with a surgeon who is board certified and experienced in the procedures you want. Your surgeon talks with you about your options and the potential results. The surgeon also may provide information on details such as the type of anesthesia that will be used during surgery and the kind of follow-up care that you may need.
Follow your health care team's directions on preparing for your procedures. This may include guidelines on eating and drinking. You may need to make changes in the medicine you take and stop using nicotine, including vaping, smoking and chewing tobacco.
Because feminizing surgery might cause physical changes that cannot be reversed, you must give informed consent after thoroughly discussing:
- Risks and benefits
- Alternatives to surgery
- Expectations and goals
- Social and legal implications
- Potential complications
- Impact on sexual function and fertility
Evaluation for surgery
Before surgery, a health care provider evaluates your health to address any medical conditions that might prevent you from having surgery or that could affect the procedure. This evaluation may be done by a provider with expertise in transgender medicine. The evaluation might include:
- A review of your personal and family medical history
- A physical exam
- A review of your vaccinations
- Screening tests for some conditions and diseases
- Identification and management, if needed, of tobacco use, drug use, alcohol use disorder, HIV or other sexually transmitted infections
- Discussion about birth control, fertility and sexual function
You also may have a behavioral health evaluation by a health care provider with expertise in transgender health. That evaluation might assess:
- Gender identity
- Gender dysphoria
- Mental health concerns
- Sexual health concerns
- The impact of gender identity at work, at school, at home and in social settings
- The role of social transitioning and hormone therapy before surgery
- Risky behaviors, such as substance use or use of unapproved hormone therapy or supplements
- Support from family, friends and caregivers
- Your goals and expectations of treatment
- Care planning and follow-up after surgery
Other considerations
Health insurance coverage for feminizing surgery varies widely. Before you have surgery, check with your insurance provider to see what will be covered.
Before surgery, you might consider talking to others who have had feminizing surgery. If you don't know someone, ask your health care provider about support groups in your area or online resources you can trust. People who have gone through the process may be able to help you set your expectations and offer a point of comparison for your own goals of the surgery.
What you can expect
Facial feminization surgery.
Facial feminization surgery may involve a range of procedures to change facial features, including:
- Moving the hairline to create a smaller forehead
- Enlarging the lips and cheekbones with implants
- Reshaping the jaw and chin
- Undergoing skin-tightening surgery after bone reduction
These surgeries are typically done on an outpatient basis, requiring no hospital stay. Recovery time for most of them is several weeks. Recovering from jaw procedures takes longer.
Tracheal shave
A tracheal shave minimizes the thyroid cartilage, also called the Adam's apple. During this procedure, a small cut is made under the chin, in the shadow of the neck or in a skin fold to conceal the scar. The surgeon then reduces and reshapes the cartilage. This is typically an outpatient procedure, requiring no hospital stay.
Top surgery
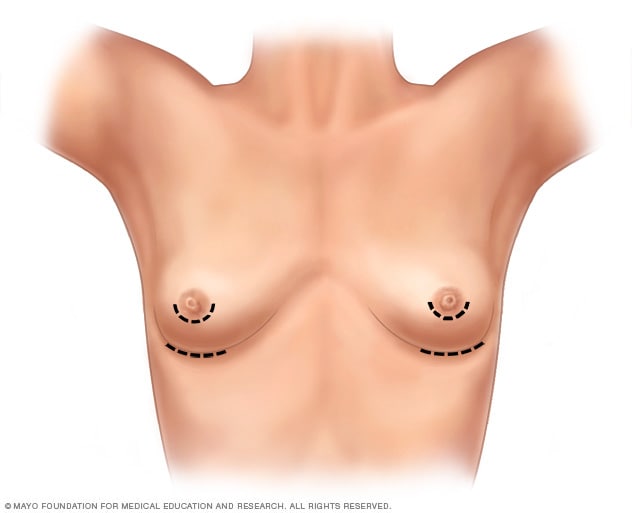
- Breast augmentation incisions
As part of top surgery, the surgeon makes cuts around the areola, near the armpit or in the crease under the breast.
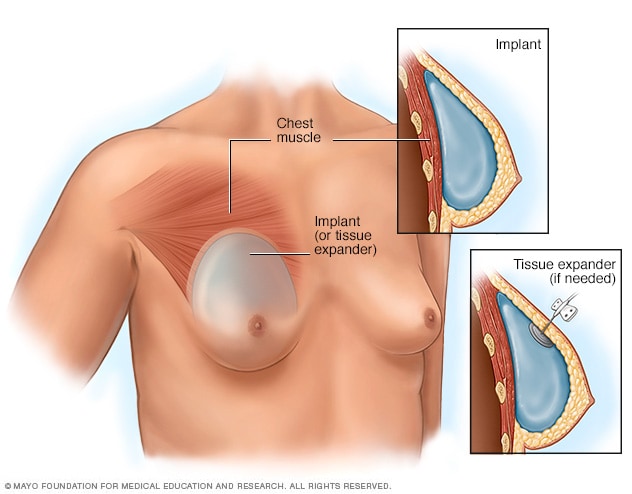
- Placement of breast implants or tissue expanders
During top surgery, the surgeon places the implants under the breast tissue. If feminizing hormones haven't made the breasts large enough, an initial surgery might be needed to have devices called tissue expanders placed in front of the chest muscles.
Hormone therapy with estrogen stimulates breast growth, but many people aren't satisfied with that growth alone. Top surgery is a surgical procedure to increase breast size that may involve implants, fat grafting or both.
During this surgery, a surgeon makes cuts around the areola, near the armpit or in the crease under the breast. Next, silicone or saline implants are placed under the breast tissue. Another option is to transplant fat, muscles or tissue from other parts of the body into the breasts.
If feminizing hormones haven't made the breasts large enough for top surgery, an initial surgery may be needed to place devices called tissue expanders in front of the chest muscles. After that surgery, visits to a health care provider are needed every few weeks to have a small amount of saline injected into the tissue expanders. This slowly stretches the chest skin and other tissues to make room for the implants. When the skin has been stretched enough, another surgery is done to remove the expanders and place the implants.
Genital surgery
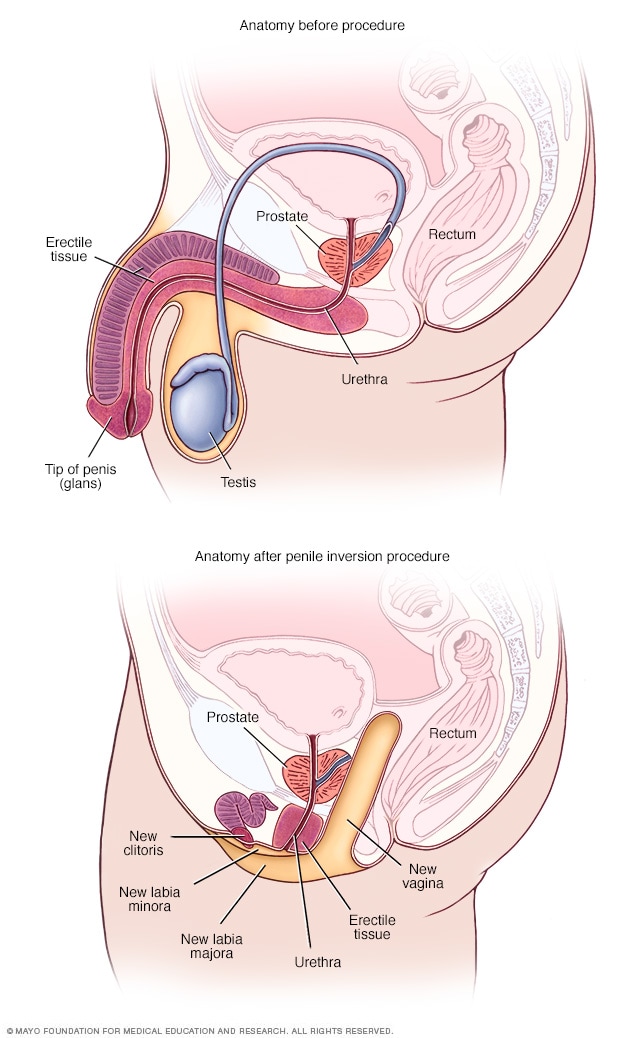
- Anatomy before and after penile inversion
During penile inversion, the surgeon makes a cut in the area between the rectum and the urethra and prostate. This forms a tunnel that becomes the new vagina. The surgeon lines the inside of the tunnel with skin from the scrotum, the penis or both. If there's not enough penile or scrotal skin, the surgeon might take skin from another area of the body and use it for the new vagina as well.
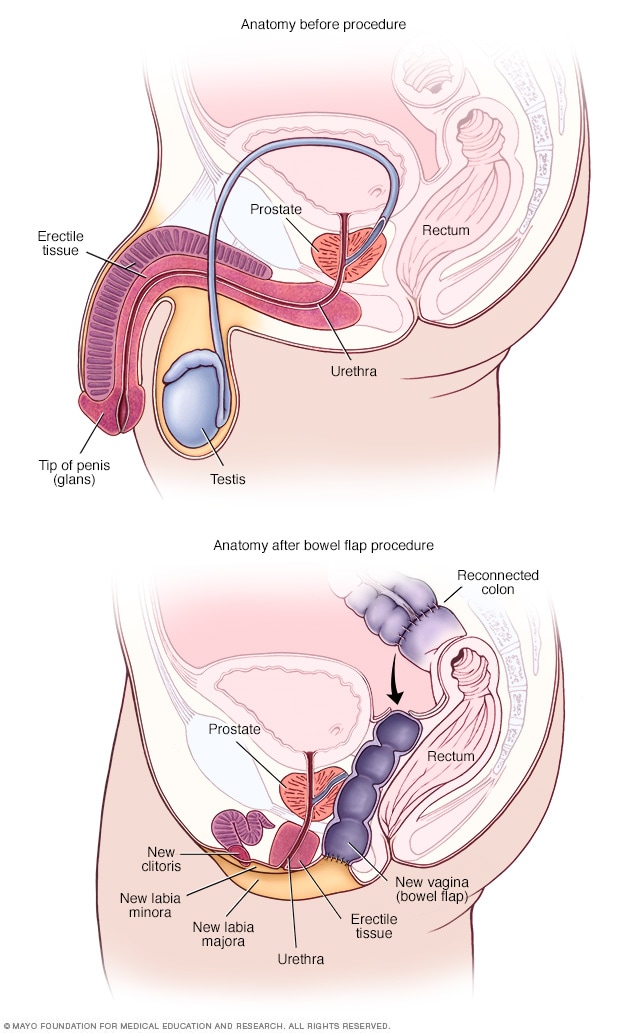
- Anatomy before and after bowel flap procedure
A bowel flap procedure might be done if there's not enough tissue or skin in the penis or scrotum. The surgeon moves a segment of the colon or small bowel to form a new vagina. That segment is called a bowel flap or conduit. The surgeon reconnects the remaining parts of the colon.
Orchiectomy
Orchiectomy is a surgery to remove the testicles. Because testicles produce sperm and the hormone testosterone, an orchiectomy might eliminate the need to use testosterone blockers. It also may lower the amount of estrogen needed to achieve and maintain the appearance you want.
This type of surgery is typically done on an outpatient basis. A local anesthetic may be used, so only the testicular area is numbed. Or the surgery may be done using general anesthesia. This means you are in a sleep-like state during the procedure.
To remove the testicles, a surgeon makes a cut in the scrotum and removes the testicles through the opening. Orchiectomy is typically done as part of the surgery for vaginoplasty. But some people prefer to have it done alone without other genital surgery.
Vaginoplasty
Vaginoplasty is the surgical creation of a vagina. During vaginoplasty, skin from the shaft of the penis and the scrotum is used to create a vaginal canal. This surgical approach is called penile inversion. In some techniques, the skin also is used to create the labia. That procedure is called labiaplasty. To surgically create a clitoris, the tip of the penis and the nerves that supply it are used. This procedure is called a clitoroplasty. In some cases, skin can be taken from another area of the body or tissue from the colon may be used to create the vagina. This approach is called a bowel flap procedure. During vaginoplasty, the testicles are removed if that has not been done previously.
Some surgeons use a technique that requires laser hair removal in the area of the penis and scrotum to provide hair-free tissue for the procedure. That process can take several months. Other techniques don't require hair removal prior to surgery because the hair follicles are destroyed during the procedure.
After vaginoplasty, a tube called a catheter is placed in the urethra to collect urine for several days. You need to be closely watched for about a week after surgery. Recovery can take up to two months. Your health care provider gives you instructions about when you may begin sexual activity with your new vagina.
After surgery, you're given a set of vaginal dilators of increasing sizes. You insert the dilators in your vagina to maintain, lengthen and stretch it. Follow your health care provider's directions on how often to use the dilators. To keep the vagina open, dilation needs to continue long term.
Because the prostate gland isn't removed during surgery, you need to follow age-appropriate recommendations for prostate cancer screening. Following surgery, it is possible to develop urinary symptoms from enlargement of the prostate.
Dilation after gender-affirming surgery
This material is for your education and information only. This content does not replace medical advice, diagnosis and treatment. If you have questions about a medical condition, always talk with your health care provider.
Narrator: Vaginal dilation is important to your recovery and ongoing care. You have to dilate to maintain the size and shape of your vaginal canal and to keep it open.
Jessi: I think for many trans women, including myself, but especially myself, I looked forward to one day having surgery for a long time. So that meant looking up on the internet what the routines would be, what the surgery entailed. So I knew going into it that dilation was going to be a very big part of my routine post-op, but just going forward, permanently.
Narrator: Vaginal dilation is part of your self-care. You will need to do vaginal dilation for the rest of your life.
Alissa (nurse): If you do not do dilation, your vagina may shrink or close. If that happens, these changes might not be able to be reversed.
Narrator: For the first year after surgery, you will dilate many times a day. After the first year, you may only need to dilate once a week. Most people dilate for the rest of their life.
Jessi: The dilation became easier mostly because I healed the scars, the stitches held up a little bit better, and I knew how to do it better. Each transgender woman's vagina is going to be a little bit different based on anatomy, and I grew to learn mine. I understand, you know, what position I needed to put the dilator in, how much force I needed to use, and once I learned how far I needed to put it in and I didn't force it and I didn't worry so much on oh, did I put it in too far, am I not putting it in far enough, and I have all these worries and then I stress out and then my body tenses up. Once I stopped having those thoughts, I relaxed more and it was a lot easier.
Narrator: You will have dilators of different sizes. Your health care provider will determine which sizes are best for you. Dilation will most likely be painful at first. It's important to dilate even if you have pain.
Alissa (nurse): Learning how to relax the muscles and breathe as you dilate will help. If you wish, you can take the pain medication recommended by your health care team before you dilate.
Narrator: Dilation requires time and privacy. Plan ahead so you have a private area at home or at work. Be sure to have your dilators, a mirror, water-based lubricant and towels available. Wash your hands and the dilators with warm soapy water, rinse well and dry on a clean towel. Use a water-based lubricant to moisten the rounded end of the dilators. Water-based lubricants are available over-the-counter. Do not use oil-based lubricants, such as petroleum jelly or baby oil. These can irritate the vagina. Find a comfortable position in bed or elsewhere. Use pillows to support your back and thighs as you lean back to a 45-degree angle. Start your dilation session with the smallest dilator. Hold a mirror in one hand. Use the other hand to find the opening of your vagina. Separate the skin. Relax through your hips, abdomen and pelvic floor. Take slow, deep breaths. Position the rounded end of the dilator with the lubricant at the opening to your vaginal canal. The rounded end should point toward your back. Insert the dilator. Go slowly and gently. Think of its path as a gentle curving swoop. The dilator doesn't go straight in. It follows the natural curve of the vaginal canal. Keep gentle down and inward pressure on the dilator as you insert it. Stop when the dilator's rounded end reaches the end of your vaginal canal. The dilators have dots or markers that measure depth. Hold the dilator in place in your vaginal canal. Use gentle but constant inward pressure for the correct amount of time at the right depth for you. If you're feeling pain, breathe and relax the muscles. When time is up, slowly remove the dilator, then repeat with the other dilators you need to use. Wash the dilators and your hands. If you have increased discharge following dilation, you may want to wear a pad to protect your clothing.
Jessi: I mean, it's such a strange, unfamiliar feeling to dilate and to have a dilator, you know to insert a dilator into your own vagina. Because it's not a pleasurable experience, and it's quite painful at first when you start to dilate. It feels much like a foreign body entering and it doesn't feel familiar and your body kind of wants to get it out of there. It's really tough at the beginning, but if you can get through the first month, couple months, it's going to be a lot easier and it's not going to be so much of an emotional and uncomfortable experience.
Narrator: You need to stay on schedule even when traveling. Bring your dilators with you. If your schedule at work creates challenges, ask your health care team if some of your dilation sessions can be done overnight.
Alissa (nurse): You can't skip days now and do more dilation later. You must do dilation on schedule to keep vaginal depth and width. It is important to dilate even if you have pain. Dilation should cause less pain over time.
Jessi: I hear that from a lot of other women that it's an overwhelming experience. There's lots of emotions that are coming through all at once. But at the end of the day for me, it was a very happy experience. I was glad to have the opportunity because that meant that while I have a vagina now, at the end of the day I had a vagina. Yes, it hurts, and it's not pleasant to dilate, but I have the vagina and it's worth it. It's a long process and it's not going to be easy. But you can do it.
Narrator: If you feel dilation may not be working or you have any questions about dilation, please talk with a member of your health care team.
Research has found that that gender-affirming surgery can have a positive impact on well-being and sexual function. It's important to follow your health care provider's advice for long-term care and follow-up after surgery. Continued care after surgery is associated with good outcomes for long-term health.
Before you have surgery, talk to members of your health care team about what to expect after surgery and the ongoing care you may need.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Feminizing surgery care at Mayo Clinic
- Tangpricha V, et al. Transgender women: Evaluation and management. https://www.uptodate.com/ contents/search. Accessed Aug. 16, 2022.
- Erickson-Schroth L, ed. Surgical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Coleman E, et al. Standards of care for the health of transgender and gender diverse people, version 8. International Journal of Transgender Health. 2022; doi:10.1080/26895269.2022.2100644.
- AskMayoExpert. Gender-affirming procedures (adult). Mayo Clinic; 2022.
- Nahabedian, M. Implant-based breast reconstruction and augmentation. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Erickson-Schroth L, ed. Medical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Ferrando C, et al. Gender-affirming surgery: Male to female. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Doctors & Departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Let’s celebrate our doctors!
Join us in celebrating and honoring Mayo Clinic physicians on March 30th for National Doctor’s Day.
Do I need a referral to see a specialist? Learn more here . Explore the Department Directory Learn more about Telehealth Appointments Protect Yourself from West Nile Virus
How to schedule your APPOINTMENT at Denver Health: CURRENT PATIENTS: Login to MyChart to schedule appointments or call 303-436-4949 . NEW PATIENTS: Schedule an appointment online or call 303-436-4949 . NEED CARE? Schedule a Virtual Urgent Care appointment or click here to find an Urgent Care clinic .
MyChart Login
Login to MyChart
MyChart for Mobile
Download the MyChart mobile app for access to your healthcare information. Managing your healthcare has never been more simple. Download for iPhone and Android .
MyChart Sign Up
Learn about MyChart features , and sign up for an account .
Virtual Urgent Care Now Available for Denver Health MyChart Users
Denver Health MyChart users can now have a virtual urgent care visit with one of our expert providers. It’s easy and convenient to get the urgent care you need from the comfort of your home, using your smartphone, tablet or computer.
Click here for more details

- Departments & Services
- Conditions & Treatments
- Our Locations
- Find a Provider
- Pharmacy / Prescriptions
- Pay my bill
- Main Campus (303) 436-6000
- Appointments (303) 436-4949
- Lean Academy 855-888-5326
- Nurseline (303) 739-1211
- Pharmacy (303) 389-1390
- Telehealth (303) 436-4949
Contact LGBTQ Patient Navigator
Hours of operation, vaginoplasty.
Learn more about gender affirmation surgery:
Interested in this surgery?
Please complete the following surgical interest form and submit it to our LGBTQ+ Services team.
Surgical Interest Form
Overview of Vaginoplasty
Vaginoplasty is a gender-affirming, feminizing, lower surgery to create a vagina* and vulva (including mons, labia, clitoris, and urethral opening) and remove the penis, scrotal sac and testes.
What is the procedure for vaginoplasty?
- The scrotum and testes are removed.
- The glans is made into a clitoris.
- Space for the vagina is dissected between the bladder and the rectum.
- Skin from the shaft of the penis* is inverted to create the inner walls of your vagina.
- Extra skin may be taken from the scrotum* to line your vagina. The hair roots on the skin graft will be cauterized.
- The urethra is shortened.
- Vulva are created using scrotal and urethral tissue.
- A temporary urinary catheter is inserted into the bladder.
- A temporary prosthesis/stent is inserted in the vagina.
Do I need to have hair removal before vaginoplasty ?
Hair removal is highly encouraged and recommended prior to penile inversion vaginoplasty (full depth vaginoplasty). The scrotal skin will be used to make the neo vagina. If you do not do hair removal, there will be hair inside the vagina. This can make post operative care more difficult and place you at increased risk for post op infection. The surgeon will not do any hair removal during the surgical procedure. Ask an LGBTQ+ Patient Advocate about resources for hair removal.
** Hair removal is not required for minimal depth vaginoplasty.
Do I need to stop taking hormones before vaginoplasty?
Your surgeon will discuss this with you at your pre-visit.
How long will my hospital stay be?
You will be admitted to the hospital for 3 days following your surgery.
What medications will I be prescribed after surgery?
You will likely receive painkillers and antibiotics to prevent infection. Your surgeon will provide you with a list of medications to avoid for the first month. Do not resume taking hormones until your surgeon has advised you to do so.
What should I expect during the healing process?
- Bleeding during the first 48 hours following surgery
- Itchiness and small shooting electrical sensations as nerve endings heal
- Bruising can spread from your belly to your thighs and takes 3-4 weeks to settle down
- A bit of spraying when you urinate which usually improves over time
- Swelling of your labia which can take up to 6 weeks to resolve
- Brown/yellow vaginal discharge for the first 6-8 weeks
- Your vulva will approach its final appearance at 4 months
- Numbness that will improve over the first few months, and can take up to 18 months to resolve
- Red, dark pink or purple scars that take up to one year to fade
What will my post-operative routine look like?
A urinary catheter will be in place for the first five days after surgery to allow you to pass urine while your urethra heals. Sometimes people still aren’t able to urinate when the catheter comes out, due to swelling around the urethra. This situation can easily be resolved with a second catheter that will remain in place for a week and be removed by your physician when you go home. You’ll be encouraged to drink lots of fluids to prevent urinary tract infections.
A prosthesis/stent will be placed in your vagina during surgery and will remain there for 5 days to make sure the skin grafts stay in place. When it’s removed, you will begin dilating and douching. A vaginal douche is a process of rinsing the vagina by forcing water or another solution into the vagina to flush away vaginal discharge or other contents. You will be given a set of vaginal dilators of different sizes. You’ll use them to maintain vaginal depth and width and promote healing.
Initially, you’ll dilate several times a day and over the first year the amount of time spent dilating will be gradually reduced. After you have completely healed, you will only need to dilate about once a week. The frequency depends on how much penetrative sex you have. For the first two months after surgery, you will take sitz baths. A sitz bath is a way to soak your surgical site to keep it clean. You’ll want to wear thin maxi pads for about one month to manage post-operative bleeding and discharge.
What check-ups will be needed after my hospital stay?
The number of check-ups needed varies from person to person. If possible, see your primary care provider about a week after and then every 2-4 weeks for the first few months. When you visit your surgeon or primary care provider, they should check your surgical sites to make sure there are no infections or wound healing problems. They will ask questions about dilating, bleeding, vaginal discharge, fever, pain and how you are feeling emotionally and physically.
How long will it take for me to get back to my usual activities?
Recovery time varies from person to person, so always follow the advice of your surgeon. Many people begin to feel more comfortable during the second week after their surgery. You’ll need plenty of rest in the first two weeks. It’s common to be back to your usual activities, including work, in six to eight weeks. Some activities, such as driving, heavy lifting, exercise, sex and soaking in hot tubs, may be restricted in the post-operative period. Your surgeon will give you advice about when it is okay to resume these activities. Complete recovery can take up to one year.
What complications are associated with vaginoplasty?
All surgical procedures involve some risks, including negative reactions to anesthesia, blood loss, blood clots and infection. These complications can, in extreme cases, result in death. It’s important to discuss these risks in detail with your surgeon. Your surgical care team will take a wide variety of steps to prevent these problems, detect them if they arise and respond to them appropriately.
They will also inform you about what you can do to minimize your risks. The list below includes some of the complications associated with vaginoplasty in particular. It does not replace a thorough consultation with your surgeon.
This is when blood collects in the surgical site, causing pain, swelling and redness. Smaller hematomas can be drained, but larger ones require removal through surgery.
Abscess Formation
An abscess is a collection of pus. It’s caused by a bacterial infection. It can be treated with antibiotics or drained by the surgeon.
This is when clear fluid accumulates in the surgical site. Small seromas may need to be aspirated, or sucked out, once or more by the surgeon.
Loss of Sensation
You may have small areas of numbness. Your ability to achieve orgasm could decrease. Loss of clitoris is a remote possibility.
Rectovaginal fistula
This is when an abnormal path between the rectum and vagina is created. Surgery would be needed to correct this.
May be correctable with various treatments, including additional surgery.
Injury to the Nerves or Muscles in the Legs
Can lead to numbness or a change of sensation in the skin of the legs. In very rare cases, it can lead to difficulty moving the leg which needs correction through surgery.
Unsatisfactory Size or Shape of the Vagina, Clitoris or Labia
Outcomes that are quite different from what was expected may require surgical revision.
Urological Complications
Examples include:
- fistulas (flow of urine to areas other than urethra opening)
- stenosis (narrowing of the urethra, causing difficulties urinating)
- strictures (blockage of the urethra, causing difficulty urinating).
It is common to have spraying or dribbling when urinating until your swelling settles down. If these problems don’t resolve on their own, they may require additional surgery.
- 0 && newsLoaded" class="" data-id="{044698B9-FA04-4636-994D-47662155601F}" ref="news"> News
- 0 && blogLoaded" class="" data-id="{9AB9C6CB-06BD-4D71-867F-FAB69D88F93C}" ref="blog"> Blog Articles
- 0 && storiesLoaded" class="" data-id="{71E64EA2-1956-4F7C-A67D-579E0BB54378}" ref="stories"> Patient Stories
- Mar 27 Labor and Delivery Tour for Expectant Families
- Apr 3 Labor and Delivery Tour for Expectant Families
- Apr 6 Boot Camp for New Dads ®
- Apr 10 Labor and Delivery Tour for Expectant Families
Transgender Health Program
- Enter keyword Search
Gender-Affirming Surgery
OHSU surgeons are leaders in gender-diverse care. We provide specialized services tailored to the needs and goals of each patient. We offer:
- Specialists who do hundreds of surgeries a year.
- Plastic surgeons, urologists and other specialists who are leading experts in bottom surgery, top surgery and other gender-affirming options.
- Vocal surgery with a highly trained ear, nose and throat doctor.
- Peer volunteers who can provide support during visits.
- Welcoming care for every patient, every gender and every journey.
Our surgical services
We offer many gender-affirming surgery options for transgender and nonbinary patients, including options within the following types. We also welcome you to request a procedure that isn’t listed on our pages.
Top surgery:
- Gender-affirming mastectomy
- Gender-affirming breast augmentation
Bottom surgery:
- Phalloplasty and metoidioplasty , including vagina-preserving options
- Vaginoplasty and vulvoplasty , including penile-preserving options
Hysterectomy
Nullification surgery, oophorectomy, orchiectomy.
Bottom surgery options also include:
- Scrotectomy
- Scrotoplasty
- Urethroplasty
- Vaginectomy
Additional gender-affirming options:
- Adam’s apple surgery

Vocal surgery
Face and body surgery, preparing for surgery.
Please see our patient guide page to learn about:
- Steps to surgery
- WPATH standards of care
- The letter of support needed for some surgeries
For patients
Request services.
Please fill out an online form:
- I am seeking services for myself.
- I am seeking services for someone else.
Other questions and concerns
Contact us at:
- 503-494-7970
- [email protected]
Refer a patient
- Please complete our Request for Transgender Health Services referral form and fax with relevant medical records to 503-346-6854 .
- Learn more on our For Health Care Professionals page.
At OHSU, our gynecologic surgeon, Dr. Lishiana Shaffer, specializes in hysterectomies (uterus and cervix removal; often combined with oophorectomy, or ovary removal) for gender-diverse patients. She does more than 150 a year.
We also offer a Transgender Gynecology Clinic with a gender-neutral space. Services include surgery. Referrals and appointments are made through the OHSU Center for Women's Health, though the space is not in the center. Call 503-418-4500 to request an appointment.
Some patients choose hysterectomy to:
- More closely align their bodies with their gender identity.
- With ovary removal, to remove a main source of the hormone estrogen.
- To end pain caused by testosterone therapy that shrinks the uterus.
- To end the need for some gynecologic exams, such Pap smears.
Preparation: We usually recommend a year of hormone therapy first, to shrink the uterus. We don’t require a year of social transition.
Most often, we use a minimally invasive laparoscope and small incisions in the belly. We usually recommend removing fallopian tubes as well, to greatly reduce the risk of ovarian cancer.
Most patients spend one night in the hospital. Recovery typically takes about two weeks. You’re encouraged to walk during that time but to avoid heavy lifting or strenuous exercise.
Hysterectomy is usually safe, and we have a low rate of complications. Risks can include blood clots, infection and scar tissue. Because of a possible link between hysterectomy and higher risk of cardiovascular disease, your doctors may recommend regular tests.
Removing the uterus also ends the ability to carry a child. OHSU fertility experts offer options such as egg freezing before treatment, and connecting patients with a surrogacy service.
OHSU offers nullification surgery to create a gender-neutral look in the groin area.
Nullification surgery may include:
- Removing the penis (penectomy)
- Removing the testicles (orchiectomy)
- Reducing or removing the scrotum (scrotectomy)
- Shortening the urethra
- Removing the uterus (hysterectomy)
- Removing the vagina (vaginectomy)
The procedure takes several hours. Patients can expect to spend one to two nights in the hospital. Recovery typically takes six to eight weeks. Patients are asked to limit walking and to stick to light to moderate activity for four weeks. They should wait three months before bicycling or strenuous activity.
Nullification surgery cannot be reversed. Risks can include:
- Changes in sensation
- Dissatisfaction with the final look
- Healing problems
Removing the penis and testicles or the uterus also affects the ability to conceive a child. OHSU fertility experts offer options such as freezing eggs and connecting patients with a surrogacy service.
Having a gynecologic surgeon remove one or both ovaries is often done at the same time as a hysterectomy. We do nearly all these surgeries with a minimally invasive laparoscope and small incisions in the belly.
Most patients spend one night in the hospital and return to their regular routine in about two weeks.
The ovaries produce estrogen, which helps prevent bone loss and the thickening of arteries. After removal, a patient should be monitored long-term for the risk of osteoporosis and cardiovascular disease.
We encourage patients to keep at least one ovary to preserve fertility without egg freezing. This also preserves some hormone production, which can avoid early menopause.
At OHSU, expert urologists do orchiectomies (testicle removal). Patients may choose this option:
- To remove the body’s source of testosterone
- As part of a vaginoplasty or vulvoplasty (surgeries that create a vagina and/or vulva)
- To relieve dysphoria (some patients choose only this surgery)
Removing the testicles usually means a patient can stop taking a testosterone blocker. Patients may also be able to lower estrogen therapy.
The surgeon makes an incision in the scrotum. The testicles and the spermatic cord, which supplies blood, are removed. Scrotal skin is removed only if the patient specifically requests it. The skin is used if the patient plans a vaginoplasty or vulvoplasty.
You will probably go home the same day. Patients can typically resume normal activities in a week or two.
Reducing testosterone production may increase the risk of bone loss and cardiovascular disease, so we recommend regular tests. Without prior fertility treatment, orchiectomy also ends the ability to produce children. Serious risks are uncommon but include bleeding, infection, nerve damage and scarring.
Adam’s apple reduction (laryngochrondoplasty)
Dr. Joshua Schindler, an ear, nose and throat doctor who does Adam’s apple and vocal surgeries, completed his training at Johns Hopkins University.
Laryngochrondoplasty is also known as Adam’s apple reduction or a tracheal shave (though the trachea, or windpipe, is not affected).
A surgeon removes thyroid cartilage at the front of the throat to give your neck a smoother appearance. This procedure can often be combined with facial surgery.
Thin incision: At OHSU, this procedure can be done by an ear, nose and throat doctor (otolaryngologist) with detailed knowledge of the neck’s anatomy. The surgeon uses a thin incision, tucked into a neck line or fold. It can also be done by one of our plastic surgeons, typically with other facial surgery.
In an office or an operating room: Our team can do a laryngochrondoplasty in either setting, which may limit a patient’s out-of-pocket expenses.
OHSU also offers Adams’ apple enhancement surgery.
Many patients find that hormone therapy and speech therapy help them achieve a voice that reflects their identity. For others, vocal surgery can be added to raise the voice’s pitch.
Voice therapy: Patients have voice and communication therapy before we consider vocal surgery. Your surgeon and your speech therapist will assess your voice with tests such as videostroboscopy (allowing us to see how your vocal cords work) and acoustic voice analysis.
Effective surgery: We use a surgery called a Wendler glottoplasty. It’s done through the mouth under general anesthesia. The surgeon creates a small controlled scar between the two vocal cords, shortening them to increase tension and raise pitch. Unlike techniques that can lose effectiveness over time, this surgery offers permanent results.
Hormone therapy can bring out desired traits, but it can’t change the underlying structure or remove hair follicles. Our highly trained surgeons and other specialists offer options. Patients usually go home the same day or spend one night in a private room.
Face options:
- Browlift (done with the forehead)
- Cheek augmentation
- Chin surgery (genioplasty), including reductive, implants or bone-cut options
- Eyelid surgery
- Face-lift, neck lift
- Forehead lengthening
- Forehead reduction, including Type 3 sinus setback and orbital remodeling
- Hairline advancement (done with the forehead)
- Jawline contouring
- Lip lift and/or augmentation
- Lipofilling (transferring fat using liposuction and filling)
- Nose job (rhinoplasty)
Body options:
Hormone treatment may not result in fat distribution consistent with your gender. We offer liposuction and fat grafting to reshape areas of the body.
MTFsurgery .net
- Orchiectomy
- Penile Inversion Vaginoplasty
- Peritoneal Vaginoplasty
- Rectosigmoid Vaginoplasty
- Vulvoplasty
- Non-Binary Bottom Surgery
- Facial Feminization Surgery
- Breast Augmentation
- Breast Augmentation w/ Fat Transfer
- Body Feminization
- What Is Board Certification?
- Getting Surgery In Thailand
- Vaginoplasty Hair Removal
- Follicular Cautery vs. Hair Removal
- Vaginal Stenosis After Vaginoplasty
- Importance of Dilation
- Breast Aug & Surgeon Experience
- Browse All Surgeons
- Orchiectomy Surgeons
- Vaginoplasty Surgeons
- FFS Surgeons
- Breast Augmentation Surgeons
- Body Feminization Surgeons
- MTF Breast Augmentation
- MTF Vaginoplasty
MTF Surgery Procedures » Vulvoplasty
Vulvoplasty: Assessing an Alternative to Vaginoplasty

Vulvoplasty is a suitable surgical solution for patients who:
- Are not interested in receiving penetrative vaginal sex;
- Have concerns about age and recovery;
- Do not want to or are unable to commit to the lifelong regimen of dilation associated with Vaginoplasty;
- Identify as non-binary and feel that Vulvoplasty is more affirming of their gender;
- Have higher risk factors due to: - Previous radical prostatectomy, pelvic radiation, major rectal injury; - Congestive heart failure; - Multiple mental health conditions or limited ability for self-care.
- Have concerns about timing, for example impending loss of health insurance (Vulvoplasty can often be scheduled sooner than Vaginoplasty), hair removal requirements (no pre-operative hair removal required with Vulvoplasty.)
- Lack insurance and are paying out-of-pocket for surgery. (Vulvoplasty costs less than Vaginoplasty.)
For these patients, Vulvoplasty is appropriate and should be offered by the surgeon as an option.
While more studies are needed, Vulvoplasty has been associated with a high rate of satisfaction. A 2018 study reported that 93% of respondents were satisfied with their surgery and with their decision to pursue Vulvoplasty. (Jiang, et al.) In cases where a patient later desires Vaginoplasty, a Vulvoplasty can be converted to full depth Vaginoplasty, using skin grafts or a section of sigmoid colon.
What's in a Name? Vulvoplasty and Zero Depth Vaginoplasty
Vulvoplasty is known by many other names, most notably: Zero Depth Vaginoplasty, Shallow Depth Vaginoplasty, and Limit Depth Vaginoplasty; Cosmetic Vaginoplasty; No Cavity SRS and Partial SRS.
Both providers and patients can agree that the choice of terminology used by surgeons in reference to patients is extremely important, and should be gender affirming as well as culturally sensitive. However, not all surgeons agree on the terminology for Vulvoplasty:
"Gender-affirming vulvoplasty" is the authors preferred term to describe gender-affirming surgery that creates the vulva (including the clitoris, labia majora and labia minora, and female urethral position) without creation of a vaginal canal. We prefer "vulvoplasty" over other terms in common use, such as "zero depth" or "cosmetic" vaginoplasty, as it more accurately reflects the anatomic intent of a surgery for which the goal is to form a vulva without creating a vagina." (Jiang, et al.) "Various terms exist for vaginoplasty without creation of a vaginal canal, including partial vaginoplasty and vulvaplasty. These are technical, anatomic terms that are not part of lay language. The author believes that the use of such terms is purely academic and for patients, creates a false dichotomy. Such terms suggest that a patient is not undergoing creation of a "real vagina," which itself can create dysphoria for patients. "While the term 'zero-depth vaginoplasty' is technically an accurate term for a neovagina without a true canal, the author has moved away from this term and instead now uses 'shallow depth vaginoplasty.' The decision to adopt the term 'shallow-depth' was based on feedback from a small subset of patients who found 'shallow depth' to be a more normalizing term than 'zero depth.'" (Garcia, et al.)
Case Report: Patient Living for Nearly 50 Years as Trans Woman Undergoes Successful Vulvoplasty Surgery In Minnesota
A trans woman who transitioned nearly 50 years ago sought out Gender Confirmation Surgery with goals of removing male genitalia, being able to urinate while sitting and having a sensate clitoris. Three months after healing completely, this patient was happy with results of a sensate neoclitoris and feminine-appearing vulva.
The Growing Trend of Vulvoplasty
While Vaginoplasty is performed much more frequently, Vulvoplasty has become more popular in recent years, with as many as 10% of patients requesting it. (Jiang, et al.) Some surgeons believe that Vulvoplasty should be offered as an option to all patients:
"The author believes that shallow-depth vaginoplasty should always be offered to patients during discussion of surgical options and planning. Doing so helps ensure that patients are provided with a review of all surgical options. A thorough approach such as this is patient centered and affords patients who may not feel the need to have a vaginal canal, or want to expend effort and assume the risks of maintaining a canal, to opt out if they wish. This approach also likely engenders greater mutual respect between patient and surgeon." (Garcia, et al.)
Some surgeons offer Vulvoplasty specifically to patients who have greater risk factors:
"At our institution, we offer vulvoplasty to patients who are at high risk for complications due to social or medical co-morbidities. For those patients, vulvoplasty is a lower-risk alternative. Additionally, despite having no contra-indication to vaginal canal reconstruction, some patients present requesting vulvoplasty." (Jiang, et al.)
It is much more common however for patients to not be offered Vulvoplasty at all in consultation with surgeons. A recent study reported that 86% of patients surveyed had not been offered Vulvoplasty. (Garcia, et al.)
In 15 years of performing MTF Vaginoplasty , Dr. Marci Bowers says that patient requests for Vulvoplasty are "rare" and that she has only completed three in more than 1800 MTF surgeries. "To be fair, this number may be limited by consumers who were previously unaware of [zero depth vaginoplasty]—we did not talk about this as an option unless specifically asked." Furthermore, Dr. Bowers believes :
"A troubling trend of late is that inexperienced surgeons, lacking confidence in their own abilities to perform the difficult and risky portions of the procedure, use fear of complications (and their own inadequacy?) to convince patients to undergo [zero depth vaginoplasty] rather than traditional vaginoplasty. Recently—in a public statement—one surgeon declared that more than 30% of his patients chose [zero depth vaginoplasty]! Absurd! If your surgeon suggests [zero depth vaginoplasty], 'buyer, beware!' Surgeons, lacking confidence, may speak of complications—as they should—but, when the centerpiece of their interaction is framed by a discussion of complications, seek care elsewhere."
When it comes to bottom surgery, decision making is critical. Vulvoplasty is a valid alternative to Vaginoplasty that deserves discussion between patients and surgeons. While it does not include the creation of a vaginal canal, Vulvoplasty results in aesthetically pleasing female genitalia which is entirely gender affirming for some patients. Vulvoplasty is also a good solution for patients with higher risk factors. There is no "one-size-fits-all" way to medically transition and Vulvoplasty is simply another option worthy of consideration for those seeking gender affirming lower surgery.

Surgeons who offer Vulvoplasty:
- Dr. Heidi Wittenberg & Dr. Adam Bonnington - San Francisco CA
- Dr. Dany Hanna - Dallas TX
- Dr. Curtis Crane , Dr. Richard Santucci , Dr. Ashley DeLeon , Dr. Gerhard Mundinger - Austin TX
- Dr. Thomas Satterwhite , Dr. Dev Gurjala - San Francisco CA
- Dr. Michael Safir - Santa Monica CA
- Dr. Jonathan Keith - Livingston NJ
- Dr. Drew Marano - New York NY
- Dr. Ellie Zara Ley - San Francisco CA
- Dr. Praful Ramineni - Washington DC
- Dr. Gabriel Del Corral - Baltimore MD and Washington D.C.
- Dr. Angela Rodriguez - San Francisco CA
- Dr. John Whitehead - Miami FL
- Dr. Toby Meltzer - Scottsdale AZ
- Dr. Nick Esmonde - Portland OR
- Dr. Loren Schechter - Illinois
- Dr. Katherine Gast - Wisconsin
- Dr. Pichet Rodchareon - Thailand
- Dr. Kamol Pansritum - Thailand
- Dr. Daniel Dugi, Dr. Geolani Dy, Dr. Blair Peters - Portland OR
- Dr. Maurice Garcia - Los Angeles CA
- Dr. Gladys Ng - Los Angeles CA
- Dr. Ali Salim - San Francisco CA
- Dr. Christi Butler - San Francisco CA
- Dr. Joseph Pariser - Minneapolis MN
- Dr. James Hotaling, Dr. Jeremy Myers - Salt Lake City UT
- Dr. Christodoulos Kaoutzanis - Aurora CO
- Dr. Sumanas Jordan - Chicago IL
- Dr. Leo Otake - Darien CT
- Dr. Keelee MacPhee - Durham NC
- Dr. Sidhbh Gallagher - Miami FL
- Dr. Pierra Brassard - Montreal, Canada
- Dr. Narendra Kaushik - Delhi, India
- Dr. Chettawut Tulayaphanich - Thailand
References:
Does Depth Matter? Factors Affecting Choice of Vulvoplasty Over Vaginoplasty as Gender-Affirming Genital Surgery for Transgender Women. Jiang D, Witten J, Berli J, Dugi D. J Sex Med. 2018 Jun;15(6):902-906. doi: 10.1016/j.jsxm.2018.03.085. Epub 2018 Apr 26.
Sexual Function After Shallow and Full-Depth Vaginoplasty: Challenges, Clinical Findings, and Treatment Strategies — Urologic Perspectives Maurice M.Garcia, Clinics in Plastic Surgery , Volume 45, Issue 3, July 2018, Pages 437-446.
Gender-Affirming Penile Inversion Vaginoplasty. Salim A, Poh M. Clinics in Plastic Surgery , Volume 45, Issue 3, July 2018, Pages 343-350.
Last updated: 02/06/24

Genital Reconfiguration Surgery
On this page:
Standards of care Vaginoplasty Vulvoplasty Phalloplasty Metoidioplasty Downloads
GRS, or Genital Reconfiguration Surgery, is the name given to several different surgeries that change the shape and function of existing genitals. GRS may occur concurrently to, or after a hysterectomy, orchidectomy, or oophorectomy. Genital surgeries are not available to people under 18 years old.
Genital surgeries have picked up a few different names over the years, with Genital Reconfiguration Surgery simply being the most recent. You may have heard patients refer to it as bottom surgery, lower surgery, Sexual Reassignment Surgery, Gender Reassignment Surgery, a sex change surgery, inning-an-outie, vice versa, or others.
TransHub uses the term Genital Reconfiguration Surgery to be specific that the only thing changing during surgery is physiological, rather than gender. It’s always good to remember that genitals don’t have genders, people do, and you are already the woman, man or non-binary person you’ve always been.
While genital surgery is often seen as the ‘last part’ of gender affirmation, it is just another step along the way of some people’s journeys. There’s no right or wrong way to be or embody your gender, regardless of your surgical status. Not all trans people want, seek or can have surgery, and being trans doesn’t necessitate surgery either. Find out more about that here .
Information and resources to assist clinicians learn more about genital surgeries can be found here .
All surgeries carry some risk, including complications, infection, blood clots, and rarely death. It’s important to ask your surgeon about possible risks and how to avoid them.
WPATH Standards of Care
The Standards of Care - 7th Ed (SoC7) is published by the World Professional Association for Transgender Health (WPATH) and offers guidance to clinicians working with trans patients all over the world, including criteria and recommended referral pathways for those seeking particular medical and surgical interventions.
The SoC7 does not specify an order by which surgeries should occur, if sought at all, and are guidelines, not legislated requirements.
Criteria for metoidioplasty or phalloplasty in FtM patients and for vaginoplasty in MtF patients:
- Persistent, well-documented gender dysphoria;
- Capacity to make a fully informed decision and to consent for treatment;
- Age of majority in a given country;
- If significant medical or mental health concerns are present, they must be well controlled;
- 12 continuous months of hormone therapy as appropriate to the patient’s gender goals (unless hormones are not clinically indicated for the individual).
- 12 continuous months of living in a gender role that is congruent with their gender identity.
Although not an explicit criterion, it is recommended that these patients also have regular visits with a mental health or other medical professional.
WPATH Standards of Care for the Health of Transsexual, Transgender, and Gender-Nonconforming People V7
Vaginoplasty
Vaginoplasty is a procedure to surgically create a vagina and vulva from existing tissue. Depending on the procedure and technique used, the tissue used to create the different parts of the vagina and vulva may be taken from different donor sites. This surgery is generally sought by trans people who were presumed male at birth ( PMAB ), including women and non-binary people.
A vaginal cavity is created, and tissue from the penis, testes, and in some cases lower intestine or other donor sites on the body are shaped to line the vaginal canal. The tissues are also used to create the external vulva including inner and outer labia. Often, what was the head (or glans) of the penis will be used to create the clitoris and surrounding tissue, in order to preserve sensation. The urethra is shortened and repositioned to the required place in the vulva.
The main form of vaginoplasty available today is the ‘ penile inversion ’ method, in which the skin on the outside of the penis is used to create the lining of the vagina. Previously, Sigmoid vaginoplasty was more common, but is used far less today. Surgeons around the world are experimenting with other donor tissue sites such as inner skin layers around the abdomen, and the body of knowledge is constantly growing. Peritoneal Pull-down Vaginoplasty (PPV) is now offered by several Australian surgeons and is gaining in popularity.
Some surgeons require patients to decrease hormones, particularly estrogen, for a period of time in the lead up to, and immediately following, vaginoplasty surgery. For those using estradiol implants, it’s worthwhile trying to time surgery so that blood levels are low when surgery takes place, with the next implant due for insertion after surgery.
Healing from any genital surgery can take quite a while, and it’s important to plan time to rest and recover.
In general, 4 to 8 days in hospital are required after surgery, followed by another 7-10 days of close outpatient supervision. During this time, you will likely have a catheter in place. Rest is then advised for the next 5-6 weeks, and it is recommended that any strenuous activity is avoided up to 8-12 weeks after the procedure. The amount of rest required will vary from patient to patient. No sex, arousal, or sexual contact is advised for at least 3 months after the procedure.
Recovery from a vaginoplasty will also include learning to use a vaginal dilator to help keep the vaginal canal open, as it can take some time for the body to get used to having a new cavity there. Regular dilation is often required for the first year after surgery, and irregular dilation for a period after that.
The specific instructions for your recovery will vary from surgeon to surgeon, and also depend on where and what specific surgical techniques are used.
Vaginoplasty can cost between $8,000 - $30,000 out of pocket in Australia, and sometimes more, depending on the procedures, techniques and surgeon. Some people also choose to travel overseas for vaginoplasty which can increase costs due to travel, accommodation, and other fees. Some private health insurers may cover some of the costs incurred, and further discussion with your prospective insurer may be needed.
For more information about accessing compassionate release of superannuation, go to our Superannuation page.
Vaginoplasty is performed in Australia. The Australian Professional Association for Trans Health hosts a provider list of their members. It includes surgeons in Australia and is available here .
Vaginoplasty is also performed in other countries including Thailand and America, both of which have a number of world-leading surgeons.
Codes for Genital Reconstructive Surgery (click to see full list)
Labiaplasty (also referred to as Cosmetic / Vulvaplasty)
Vulvoplasty
Vulvoplasty, or shallow depth vaginoplasty/zero depth vaginoplasty is an alternative form of GRS to surgically create a vulva from existing tissue, with a shallow or no vagina. Depending on the procedure and technique used, the tissue used to create the different parts of the vagina and vulva may be taken from different donor sites. This surgery is generally sought by trans people who were presumed male at birth ( PMAB ), including women and non-binary people.
The results are similar in outwards appearance to vaginoplasty, but without a vagina present. It is also a less complex form of surgery, and may come with a reduced change of complications for people who are at higher surgical risk.
Tissue from the penis and testes are used to create the external vulva including inner and outer labia. Often, what was the head (or glans) of the penis will be used to create the clitoris and surrounding tissue, in order to preserve sensation. The urethra is shortened and repositioned to the required place in the vulva.
Vulvoplasty costs can vary, depending on the procedures, techniques and surgeon. Some people also choose to travel overseas for vulvoplasty which can increase costs due to travel, accommodation, and other fees. Some private health insurers may cover some of the costs incurred, and further discussion with your prospective insurer may be needed.
Vulvoplasty is performed in Australia. The Australian Professional Association for Trans Health hosts a provider list of their members. It includes surgeons in Australia and is available here . Vulvoplasty is also performed in other countries including Thailand and America, both of which have a number of world-leading surgeons.
Phalloplasty
A phalloplasty is a procedure that surgically creates a penis, or phallus, from existing tissue, often including reconstruction of the urethra so as to allow for standing urination. A phalloplasty procedure may also include a simultaneous hysterectomy, oophorectomy, vaginectomy (to remove or partially remove the vagina) and other surgeries. This surgery is generally sought by trans people who were presumed female at birth ( PFAB ), including men and non-binary people.
The two main forms of phalloplasty are: the arm radial forearm free-flap (RFF) or anterior lateral thigh phalloplasty (ALT). These surgeries may be broken down into as many as three stages, with a period of several months to a year between each stage.
RFF phalloplasty is the most recent development in phalloplasty surgeries. In a free-flap procedure, the blood vessels and nerves in the donor tissue remain intact, and then able to be reattached to allow natural blood flow and sensation. At present, more than one admission is required, as RFF includes 4 operations, over a minimum of 18 months.
ALT phalloplasty is an older phalloplasty surgery that has been around for a while longer, and can result in reduced sensation. In this procedure, the blood vessels and nerves in the donor tissue are separated.
Surgeons will work out an individualised phalloplasty plan with you.
In general, up to two weeks in hospital are required after each surgery, followed by a period of close outpatient supervision. During this time, you will likely have a catheter in place. Rest is then advised for the next 5-6 weeks, and it is recommended that any strenuous activity is avoided up to 8 weeks after the procedure.
Minor complications are quite common, which require consideration for travel and accommodation, as you may need to spend longer than the advised minimum time in the same city as your surgeon.
Full healing, including rediscovery of sexual sensation, can take up to 1-2 years.
The specific instructions for your recovery will vary from surgeon to surgeon, and depending on where and what specific surgical techniques are used.
Phalloplasty can cost between $50,000 - and $80,000 in Australia, depending on the technique and surgeon, and additional costs can be included ie. for anaesthetics. There are also many hidden costs that may come up as part of recovery.
For more information about accessing compassionate release of superannuation, go to our Superannuation page. Private health insurance can also cover costs like hospital admissions and help with rebates.
Phalloplasties are performed in Australia by very few surgeons. In Australia, hysterectomy is always done separate to phalloplasty. The Australian Professional Association for Trans Health hosts a provider list of their members. It includes surgeons in Australia and is available here .
Phalloplasties are also performed in Thailand, the US, UK, and in some European countries.
Metoidioplasty
A metoidioplasty is a procedure that creates a penis, or phallus, from a hormonally-enlarged clitoral shaft. This surgery is generally sought by trans people who were presumed female at birth ( PFAB ), including men and non-binary people.
When a person starts taking testosterone, the clitoral shaft will naturally enlarge. During a metoidioplasty, the existing clitoral shaft will be raised higher up on the body, and have the urethra inserted. The clitorial ligaments will also be detached, which allows the shaft to lengthen and drop into a position similar to a natal penis. A small graft is taken from the inside of the cheek and used as tissue for the urethra. A vaginectomy (removal of vagina) may also be completed at the same time.
While metoidioplasty is often considered to be a single-stage surgery, you may request additional surgeries in order to achieve the desired affirming results.
Healing from any genital surgery can take quite a while, and it’s important to plan time to rest and recover. It is likely that you will be required to rest and take time off of work for at least the first two weeks after the procedure.
Costs for metoidioplasty can vary, depending on the technique and surgeon.
Metoidioplasty is performed in Australia by very few surgeons. The Australian Professional Association for Trans Health hosts a provider list of their members. It includes surgeons in Australia and is available here .
Metoidioplasty is also performed in Thailand, the US, UK, and in some European countries.
Surgical readiness referral - TransHub
10 trans questions to ask a doctor - TransHub [ Plaintext version ]
10 tips for clinicians working with trans & gender diverse people - TransHub [ Plaintext version ]
Gender affirming intake form for doctors - TransHub
Providers list - AusPath
WPATH Standards of Care V7 [PDF]
Australian Standards of Care and Treatment Guidelines for Trans and Gender Diverse Children and Adolescents v1.1 [PDF] - The Royal Children’s Hospital Melbourne
Trans children and medical treatment: the law [PDF] - Inner City Legal Centre
Going overseas for a medical procedure (medical tourism) - SmartTraveller
The Go-To Guide to Gender Surgeons
Find a qualified surgeon for gender-affirming care.
Start Your Search
Find a Surgeon
Search by U.S. State, Procedure and Insurance Search by Country and Procedure Browse the Global Surgeon Maps
The Go-To Guide To Gender Surgeons

Advertisement
Surgical Outcomes and Complications of Genital Gender Affirmation Surgery
- Sexual Orientation and Identity (E Coleman & GN Rider, Section Editors)
- Published: 02 December 2021
- Volume 13 , pages 107–116, ( 2021 )
Cite this article
- Devin M. Melancon 1 ,
- Alice B. Walton 2 ,
- Gerhard Mundinger 3 &
- Cooper Benson 4
234 Accesses
Explore all metrics
Purpose of Review
There is a significant rise in the interest in genital gender affirmation surgery (gGAS), which is increasingly offered and performed throughout the world. While gGAS is not new, the expansion of gGAS is associated with progressive societal acceptance of transgender and gender non-conforming individuals. There is a clear role for gGAS in the management of gender dysphoria, and with the prevalance of gGAS it is important for physicians to be familiar with the altered anatomy and potential complications of gGAS. In this review, we summarize the literature on the outcomes and complications associated with gGAS.
Recent Findings
Fifty-five studies were utilized in this review, encompassing meta-analyses, literature reviews, retrospective primary studies, and case reports.
gGAS is a complex procedure with a variety of techniques that each carry their own strengths and weaknesses. Current gGAS procedures deliver predictable results with high patient satisfaction despite high complication rates for gGAS. Further research is needed to refine gGAS techniques in order to to minimize complication rates and to improve the management of complications when they do occur.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price excludes VAT (USA) Tax calculation will be finalised during checkout.
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

source from author CRB, informed consent obtained for use of photo)

Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Am. Psychiatr. Assoc. Arlington, VA; 2013.
World Professional Association for Transgender Health. Stand. Care Heal. Transsexual, Transgender, Gender-Conforming People [7th Version]. 2012.
Massie JP, Morrison SD, Van Maasdam J, Satterwhite T. Predictors of Patient Satisfaction and Postoperative Complications in Penile Inversion Vaginoplasty. Plast Reconstr Surg United States. 2018;141:911e–21e. This study retrospectively investigates 117 penile-inversion vaginoplasties performed by a single surgeon. This study uniquely reports both postoperative complications and patient-reported outcomes.
Article CAS Google Scholar
Gentile G, Martino A, Nadalin D, Masetti M, Marta BL, Palmisano F, et al. 2020 Penile-scrotal flap vaginoplasty versus inverted penile skin flap expanded with spatulated urethra: A multidisciplinary single-centre analysis. Arch Ital di Urol Androl organo Uff [di] Soc Ital di Ecogr Urol e Nefrol. Italy 92.
Dy GW, Blasdel G, Shakir NA, Bluebond-Langner R, Zhao LC. 2021 Robotic Peritoneal Flap Revision Vaginoplasty in Transgender Women: a Novel Technique for Treating Neovaginal Stenosis. Urology [Internet]. Available from: http://www.ncbi.nlm.nih.gov/pubmed/33823174
Shoureshi P, Dy GW, Dugi D. Neovaginal Canal Dissection in Gender-Affirming Vaginoplasty. J Urol. 2021;205:1110–8.
Article Google Scholar
Scahrdein JN, Zhao LC, Nikolavsky D. Management of Vaginoplasty and Phalloplasty Complications. Urol Clin North Am. 2019;46:605–18. https://doi.org/10.1016/j.ucl.2019.07.012 .
Manrique OJ, Adabi K, Martinez-Jorge J, Ciudad P, Nicoli F, Kiranantawat K. Complications and Patient-Reported Outcomes in Male-to-Female Vaginoplasty-Where We Are Today: A Systematic Review and Meta-Analysis. Ann Plast Surg. 2018;80:684–91.
Ferrando CA. Adverse events associated with gender affirming vaginoplasty surgery. Am J Obstet Gynecol United States. 2020;223:267.e1-267.e6.
Levy JA, Edwards DC, Cutruzzula-Dreher P, McGreen BH, Akanda S, Tarry S, et al. Male-to-Female Gender Reassignment Surgery: An Institutional Analysis of Outcomes, Short-term Complications, and Risk Factors for 240 Patients Undergoing Penile-Inversion Vaginoplasty. Urology United States. 2019;131:228–33. This study is a retrospective study of 240 penile-inversion vaginoplasties performed by a single surgeon. It analyzes outcomes, complications, and risk factors in a large sample size.
Ives GC, Fein LA, Finch L, Sluiter EC, Lane M, Kuzon WM, et al. Evaluation of BMI as a Risk Factor for Complications following Gender-affirming Penile Inversion Vaginoplasty. Plast Reconstr surgery Glob open. 2019;7:e2097.
Mañero Vazquez I, García-Senosiain O, Labanca T, Gómez GE. Aesthetic Refinement in the Creation of the Clitoris, Its Preputial Hood, and Labia Minora in Male-to-Female Transsexual Patients. Ann Plast Surg United States. 2018;81:393–7.
van der Sluis WB, Steensma TD, Timmermans FW, Smit JM, de Haseth K, Özer M, et al. Gender-Confirming Vulvoplasty in Transgender Women in the Netherlands: Incidence, Motivation Analysis, and Surgical Outcomes. J Sex Med. 2020;17:1566–73. https://doi.org/10.1016/j.jsxm.2020.04.007 .
Article PubMed Google Scholar
Cocci A, Rosi F, Frediani D, Rizzo M, Cito G, Trombetta C, et al. 2019 Male-to-Female (MtoF) gender affirming surgery: Modified surgical approach for the glans reconfiguration in the neoclitoris (M-shape neoclitorolabioplasty). Arch Ital di Urol Androl organo Uff [di] Soc Ital di Ecogr Urol e Nefrol. Italy 91.
Cristofari S, Bertrand B, Leuzzi S, Rem K, Rausky J, Revol M, et al. Postoperative complications of male to female sex reassignment surgery: A 10-year French retrospective study. Ann Chir Plast Esthet France. 2019;64:24–32. This study evaluates postoperative complications in 189 patients who underwent feminizing gGAS by a single surgeon.
Dy GW, Jun MS, Blasdel G, Bluebond-Langner R, Zhao LC. Outcomes of Gender Affirming Peritoneal Flap Vaginoplasty Using the Da Vinci Single Port Versus Xi Robotic Systems. Eur Urol [Internet]. European Association of Urology; 2021;79:676–83. Available from: https://doi.org/10.1016/j.eururo.2020.06.040
Buncamper ME, Van Der Sluis WB, Van Der Pas RSD, Özer M, Smit JM, Witte BI, et al. Surgical Outcome after Penile Inversion Vaginoplasty: A Retrospective Study of 475 Transgender Women. Plast Reconstr Surg. 2016;138:999–1007.
Elmer-DeWitt MA, Wood HM, Hull T, Unger CA. Rectoneovaginal Fistula in a Transgender Woman Successfully Repaired Using a Buccal Mucosa Graft. Female Pelvic Med Reconstr Surg United States. 2019;25:e43-4.
Safa B, Lin WC, Salim AM, Deschamps-Braly JC, Poh MM. Current Concepts in Feminizing Gender Surgery. Plast Reconstr Surg. 2019;143:1081e–91e.
Chi AC, Poh MM. 2021 Urological Care for the Transgender Patient. Urol Care Transgender Patient 83–97.
Van Der Sluis WB, Bouman MB, Buncamper ME, Pigot GLS, Mullender MG, Meijerink WJHJ. Clinical characteristics and management of neovaginal fistulas after vaginoplasty in transgender women. Obstet Gynecol. 2016;127:1118–26.
Kavvadias T, Seifert HH, Ebbing J, Garcia DN, Kind AB. Robotic sacrocolpopexy for recurrent vaginal vault prolapse after sex reassignment surgery in a trans-woman. J Obstet Gynaecol J Inst Obstet Gynaecol England. 2019;39:569–70.
Stanojevic DS, Djordjevic ML, Milosevic A, Sansalone S, Slavkovic Z, Ducic S, et al. Sacrospinous Ligament Fixation for Neovaginal Prolapse Prevention in Male-to-Female Surgery. Urology. 2007;70:767–71.
Jacoby A, Maliha S, Granieri MA, Cohen O, Dy GW, Bluebond-Langner R, et al. Robotic Davydov Peritoneal Flap Vaginoplasty for Augmentation of Vaginal Depth in Feminizing Vaginoplasty. J Urol. 2019;201:1171–5.
Amend B, Seibold J, Toomey P, Stenzl A, Sievert KD. Surgical reconstruction for male-to-female sex reassignment. Eur Urol. 2013;64:141–9.
Bizic M, Stojanovic B, Bencic M, Bordás N, Djordjevic M. 2020 Overview on metoidioplasty: variants of the technique. Int J Impot Res. England
Monstrey S, Hoebeke P, Selvaggi G, Ceulemans P, Van Landuyt K, Blondeel P, et al. Penile reconstruction: is the radial forearm flap really the standard technique? Plast Reconstr Surg United States. 2009;124:510–8.
Al-Tamimi M, Pigot GL, Ronkes B, de Haseth KB, van de Grift TC, van Moorselaar RJA, et al. The First Experience of Using the Pedicled Labia Minora Flap for Urethral Lengthening in Transgender Men Undergoing Anterolateral Thigh and Superficial Circumflex Iliac Artery Perforator Flap Phalloplasty: A Multicenter Study on Clinical Outcomes. Urology United States. 2020;138:179–87.
Stojanovic B, Bizic M, Bencic M, Kojovic V, Majstorovic M, Jeftovic M, et al. One-Stage Gender-Confirmation Surgery as a Viable Surgical Procedure for Female-to-Male Transsexuals. J Sex Med Netherlands. 2017;14:741–6.
Meyer R, Daverio PJ, Dequesne J. One-stage phalloplasty in transsexuals. Ann Plast Surg United States. 1986;16:472–9.
Jolly D, Wu CA, Boskey ER, Taghinia AH, Diamond DA, Ganor O. Is Clitoral Release Another Term for Metoidioplasty? A Systematic Review and Meta-Analysis of Metoidioplasty Surgical Technique and Outcomes. Sex Med. 2021;9:100294.
Lin-Brande M, Clennon E, Sajadi KP, Djordjevic ML, Dy GW, Dugi D. Metoidioplasty With Urethral Lengthening: A Stepwise Approach. Urology. United States; 2021. p. 319–22. This study compares outcomes and complications of metoidioplasty with an without urethral lengthening at a single-center.
Kjölhede A, Cornelius F, Huss F, Kratz G. Metoidioplasty and groin flap phalloplasty as two surgical methods for the creation of a neophallus in female-to-male gender-confirming surgery: A retrospective study comprising 123 operated patients. JPRAS open. 2019;22:1–8.
Robinson IS, Blasdel G, Cohen O, Zhao LC, Bluebond-Langner R. Surgical Outcomes Following Gender Affirming Penile Reconstruction: Patient-Reported Outcomes From a Multi-Center, International Survey of 129 Transmasculine Patients. J Sex Med. Netherlands; 2021. This study compares outcomes and complication from phalloplasty, metoidioplasty, and phalloplasty secondary to metoidioplasty at a single-center.
Al-Tamimi M, Pigot GL, van der Sluis WB, van de Grift TC, van Moorselaar RJA, Mullender MG, et al. The Surgical Techniques and Outcomes of Secondary Phalloplasty After Metoidioplasty in Transgender Men: An International, Multi-Center Case Series. J Sex Med Netherlands. 2019;16:1849–59.
Schardein J, Weinberg AC, Zhao LC, Nikolavsky D. 2020 Management of Urethral Complications Following Metoidioplasty and Phalloplasty BT - Gender Confirmation Surgery: Principles and Techniques for an Emerging Field. In: Schechter LS, editor. Cham: Springer International Publishing. p. 201–13.
Ascha M, Massie JP, Morrison SD, Crane CN, Chen ML. Outcomes of Single Stage Phalloplasty by Pedicled Anterolateral Thigh Flap versus Radial Forearm Free Flap in Gender Confirming Surgery. J Urol United States. 2018;199:206–14. This study compares complications of single-stage ALT and single-stage RFFF at a single-center.
Falcone M, Preto M, Timpano M, Ciclamini D, Crosio A, Giacalone F, et al. 2021 The surgical outcomes of radial artery forearm free-flap phalloplasty in transgender men: single-centre experience and systematic review of the current literature. Int J Impot Res. England
Bouman FG. The first step in phalloplasty in female transsexuals. Plast. Reconstr. Surg. United States; 1987. p. 662–4.
Cohen O, Stranix JT, Zhao L, Levine J, Bluebond-Langner R. Use of a Split Pedicled Gracilis Muscle Flap in Robotically Assisted Vaginectomy and Urethral Lengthening for Phalloplasty: A Novel Technique for Female-to-Male Genital Reconstruction. Plast Reconstr Surg United States. 2020;145:1512–5.
Pigot GLS, Al-Tamimi M, Nieuwenhuijzen JA, van der Sluis WB, van Moorselaar RJA, Mullender MG, et al. Genital Gender-Affirming Surgery Without Urethral Lengthening in Transgender Men-A Clinical Follow-Up Study on the Surgical and Urological Outcomes and Patient Satisfaction. J Sex Med Netherlands. 2020;17:2478–87.
Chen W, Cylinder I, Najafian A, Dugi DD 3rd, Berli JU. An Option for Shaft-Only Gender-Affirming Phalloplasty: Vaginal Preservation and Vulvoscrotoplasty. A Technical Description. Plast Reconstr Surg United States. 2021;147:480–3.
Massie JP, Morrison SD, Wilson SC, Crane CN, Chen ML. Phalloplasty with Urethral Lengthening: Addition of a Vascularized Bulbospongiosus Flap from Vaginectomy Reduces Postoperative Urethral Complications. Plast Reconstr Surg United States. 2017;140:551e–8e.
Veerman H, de Rooij FPW, Al-Tamimi M, Ronkes BL, Mullender MG, Bouman BM, et al. Functional Outcomes and Urological Complications after Genital Gender Affirming Surgery with Urethral Lengthening in Transgender Men. J Urol United States. 2020;204:104–9.
Wirthmann AE, Majenka P, Kaufmann MC, Wellenbrock SV, Kasper L, Hüttinger S, et al. Phalloplasty in Female-to-Male Transsexuals by Gottlieb and Levine’s Free Radial Forearm Flap Technique-A Long-Term Single-Center Experience Over More than Two Decades. J Reconstr Microsurg United States. 2018;34:235–41.
Namba Y, Watanabe T, Kimata Y. Flap Combination Phalloplasty in Female-to-Male Transsexuals. J Sex Med Netherlands. 2019;16:934–41.
van der Sluis WB, Smit JM, Pigot GLS, Buncamper ME, Winters HAH, Mullender MG, et al. Double flap phalloplasty in transgender men: Surgical technique and outcome of pedicled anterolateral thigh flap phalloplasty combined with radial forearm free flap urethral reconstruction. Microsurgery. 2017;37:917–23.
Djordjevic ML, Bencic M, Kojovic V, Stojanovic B, Bizic M, Kojic S, et al. Musculocutaneous latissimus dorsi flap for phalloplasty in female to male gender affirmation surgery. World J Urol Germany. 2019;37:631–7.
Terrier M, Morel-Journel N, Carnicelli D, Ruffion A, Terrier J-E, Maucort-Boulch D, et al. 2021 Suprapubic phalloplasty in transmen: surgical results and critical review. Int J Impot Res. England
Falcone M, Timpano M, Oderda M, Cocci A, Morelli G, Preto M, et al. 2020 Suprapubic pedicled phalloplasty in transgender men: a multicentric retrospective cohort analysis. Int J Impot Res. England
Terrier J-É, Courtois F, Ruffion A, Morel JN. Surgical outcomes and patients’ satisfaction with suprapubic phalloplasty. J Sex Med Netherlands. 2014;11:288–98.
Garcia MM, Christopher NA, De Luca F, Spilotros M, Ralph DJ. Overall satisfaction, sexual function, and the durability of neophallus dimensions following staged female to male genital gender confirming surgery: the Institute of Urology, London U.K. experience. Transl Androl Urol. 2014;3:156–62.
PubMed PubMed Central Google Scholar
Küenzlen L, Nasim S, van Neerven S, Kühn S, Burger AE, Sohn M, et al. Multimodal Evaluation of Functional Nerve Regeneration in Transgender Individuals After Phalloplasty With a Free Radial Forearm Flap. J Sex Med Netherlands. 2020;17:1012–24.
D’Arpa S, Claes K, Lumen N, Oieni S, Hoebeke P, Monstrey S. Urethral Reconstruction in Anterolateral Thigh Flap Phalloplasty: A 93-Case Experience. Plast Reconstr Surg United States. 2019;143:382e–92e.
Nolan IT, Kuhner CJ, Dy GW. Demographic and temporal trends in transgender identities and gender confirming surgery. Transl Androl Urol. 2019;8:184–90.
Takamatsu A, Harashina T. Labial ring flap: a new flap for metaidoioplasty in female-to-male transsexuals. J Plast Reconstr Aesthet Surg Netherlands. 2009;62:318–25.
Danker S, Annen AW, Cylinder I, Esmonde NO, Berli JU. Technical Description and Microsurgical Outcomes in Phalloplasty Using the Deep Inferior Epigastric Artery and Locoregional Veins. Plast Reconstr Surg United States. 2020;146:196e–204e.
Download references
Author information
Authors and affiliations.
Louisiana State University School of Medicine, New Orleans, LA, USA
Devin M. Melancon
Tulane University School of Medicine, New Orleans, LA, USA
Alice B. Walton
Department of Plastic Surgery, Louisiana State University Health Sciences Center, New Orleans, LA, USA
Gerhard Mundinger
Department of Urology, Tulane University School of Medicine, 1430 Tulane Avenue, New Orleans, LA, 70112, USA
Cooper Benson
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Cooper Benson .
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Topical Collection on Sexual Orientation and Identity
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (PDF 36 KB)
Supplementary file2 (pdf 48 kb), supplementary file3 (xlsx 28 kb), rights and permissions.
Reprints and permissions
About this article
Melancon, D.M., Walton, A.B., Mundinger, G. et al. Surgical Outcomes and Complications of Genital Gender Affirmation Surgery. Curr Sex Health Rep 13 , 107–116 (2021). https://doi.org/10.1007/s11930-021-00318-3
Download citation
Accepted : 05 October 2021
Published : 02 December 2021
Issue Date : December 2021
DOI : https://doi.org/10.1007/s11930-021-00318-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Genital gender affirmation
- Vulvoplasty
- Vaginoplasty
- Metoidioplasty
- Phalloplasty
- Surgical Outcomes
- Find a journal
- Publish with us
- Track your research
- Accessibility Tools
- Skip to main content
- All You Need To Know About Male To Female Gender Reassignment Surgery

Male to female gender reassignment surgery is an umbrella term referring to a variety of medical procedures that treat gender dysphoria. For transgender women, gender reassignment surgery can have a monumentally positive impact on mental health.
While feminizing hormone therapy helps create female characteristics, many transgender patients opt for surgical procedures as well. There is no right or wrong way to transition. Undergoing any form of male to female gender reassignment surgery is a highly personal decision.
If you’re considering gender reassignment surgery, below you’ll find a guide outlining the most common procedures.
Bottom Surgery
Bottom surgery refers to surgeries that reshape and reconstruct male genitalia into female genitalia. There are three main types of bottom surgery: vaginoplasty, vulvoplasty, and orchiectomy.
Vaginoplasty
During a vaginoplasty, your surgeon builds the inner and outer labia of the vagina by using skin from the penis and scrotum. They also use tissue from your foreskin to build a vaginal opening, create a clitoris with skin from your penis, and create a new urethra so you can urinate.
After a vaginoplasty, you stay in the hospital for about five days. For six months, you will have to dilate your vagina two to three times a day. This means inserting a lubricated dilator into the vaginal canal and holding it there for a set number of minutes.
Vulvoplasty
During a vulvoplasty, your surgeon uses tissue from the penis to create the external parts of the vagina (the clitoris, inner and outer labia, the vaginal opening). The main difference between a vulvoplasty and a vaginoplasty is the lack of vaginal canal. A vulvoplasty does not create a vaginal canal, so you cannot have vaginal intercourse after a vulvoplasty.
After a vulvoplasty, patients usually remain in the hospital for three days.
Orchiectomy
An orchiectomy is a procedure in which the testicles are removed. It is a much simpler procedure than a vaginoplasty or vulvoplasty and can even be done under local anesthesia. It only takes about 20 minutes. One benefit of orchiectomy is that your body will naturally produce less testosterone, so it may make your hormone regiment simpler.
Recovery is usually mild, although you may experience bruising or bleeding for a few days after surgery.
Other Procedures
Many people use the term gender reassignment surgery to talk exclusively about bottom surgery. However, there are many other procedures people undergo during a gender transition.
Facial Feminization Surgery
Facial feminization surgery includes a wide range of procedures that aim to create a more traditionally feminine face. While surgery is highly subjective to individual goals, it often includes reshaping the forehead, lips, cheekbones, jaw, and chin.
Breast Augmentation
While hormonal therapy can stimulate breast development, some transgender women may want to enhance their natural breasts more. Breast augmentation involves increasing breast volume using either fat transplants or implants.
Voice Feminization Surgery
Voice feminization surgery refers to two types of surgeries that raise vocal pitch. Anterior glottic web formation shortens the vocal cords, while cricothyroid approximation fixes cricoid cartilage to thyroid cartilage to lengthen the vocal cords. Both have the potential to create a higher pitch overall.
Tracheal Shave
A tracheal shave reduces the size of the Adam’s apple, often done as part of facial feminization surgery. The surgeon makes a small incision under the chin, folds back the muscles covering the thyroid cartilage, and then stitches up the incision.
Buttock Enhancement
Buttock enhancement refines the shape of the buttocks either through fat grafting or implants. For transgender women, this can help create an hourglass figure.
Frequently Asked Questions
This is a lot of information to parse through, and it’s understandableto have some questions. Below, we’ll cover some of the most common questions people have about female to male gender reassignment surgery.
How do I prepare for surgery?
That depends on the operation. With more intense surgery, like a vaginoplasty, you may need to refrain from eating or drinking before the operation. You may also be asked to make certain lifestyle changes, like quitting smoking or losing weight, prior to undergoing surgery.
However, for surgeries that require local anathesia, preparation will usually be milder. Talk to your surgeon about how to best prepare. Make sure to follow instructions carefully to avoid complications.
How long is the recovery?
Again, this depends on your choice of gender reassignment surgery. For a vaginoplasty or vulvoplasty, you will be in the hospital for a few days. You will also have to see a physical therapist for a number of weeks to ensure you’re healing properly.
However, less invasive procedures usually have shorter recovery times. With a tracheal shave, for example, you’ll just have to eat softer foods for a few days.
How do I find the right surgeon?
In genral, you want to work wtih a board-certified plastic surgeon with experience in the type of surgery you want. You can ask for referals from people in the trans community. You can also find informaton online from the World Professional Association for Transgender Health .
How do you choose between a vaginoplasty and a vulvoplasty?
There are benefits and drawbacks to both procedures, and it comes down to personal choice.
The main difference is that a vaginoplasty creates a vaginal canal, allowing for vaginal sex, while a vulvoplasty does not. Some transgender women may have no interest in vaginal sex, meaning a vulvoplasty makes more sense.
A vulvoplasty also carries a slightly lower risk for medical complications. Plus, the recovery is easier as you will not have to dilate your vagina after surgery.
However, if having vaginal intercourse is important to you, a vaginoplasty may be the better option.
How much does female to male gender reassignment surgery cost?
That depends on the type of operation you get. Costs are high, however, and can range anywhere from $35,000 to $40,000 . The good news is that more and more insurance companies are open to covering gender reassignment surgeries and procedures. Depending on your coverage, you may be able to get some or most of the costs covered.
Can I orgasm afterwards?
Yes! After both a vaginoplasty and a vulvoplasty, you will be able to acheive orgasm via clitoral stimulation.
Undergoing gender reassignment surgery can have myriad benefits for your mental health and overall well-being. However, it’s a major decision that requires careful thought and consideration. Everyone’s needs are different, and there is no right way to transition. It’s about deciding what is right for you and your body.
Ready to get started? Leif Rogers is an Ivy League-educated, board-certified plastic surgeon and a standing member of the American Society of Plastic Surgeons. If you’re interested in gender reassignment surgery, get in touch with his team to schedule a consultation.
Your Path to Perfection begin your radiant transformation
Genital gender-affirming surgery for transgender women
Affiliations.
- 1 Department of Plastic, Reconstructive and Hand Surgery, Amsterdam University Medical Center, Location VUmc, Amsterdam, the Netherlands; Gender Clinic, Bosch en Duin, the Netherlands. Electronic address: [email protected].
- 2 Gender Clinic, Bosch en Duin, the Netherlands; Department of Plastic Surgery, University Medical Centre Groningen, Groningen, the Netherlands.
- 3 Department of Plastic and Reconstructive Surgery, Radboud University Medical Centre, Nijmegen, the Netherlands.
- 4 Department of Plastic, Reconstructive and Hand Surgery, Amsterdam University Medical Center, Location VUmc, Amsterdam, the Netherlands; Gender Clinic, Bosch en Duin, the Netherlands; Amsterdam Public Health (APH) Research Institute, Amsterdam University Medical Center, Location VUmc, Amsterdam, the Netherlands.
- PMID: 36599721
- DOI: 10.1016/j.bpobgyn.2022.102297
Transgender women may opt for genital gender-affirming surgery (gGAS), which comprises bilateral orchiectomy, gender-affirming vulvoplasty, or vaginoplasty. Vaginoplasty is chosen most frequently in this population, penile inversion vaginoplasty being the surgical gold standard. In selected cases, skin graft vaginoplasty, intestinal vaginoplasty, or peritoneal vaginoplasty may be indicated. In this article, we discuss the various types of gGAS for transgender women, (contra)-indications, intraoperative considerations, techniques, surgical outcomes, and postoperative patient-reported outcomes.
Keywords: Gender dysphoria; Orchiectomy; Transgender; Vaginoplasty; Vulvoplasty.
Copyright © 2023 The Authors. Published by Elsevier Ltd.. All rights reserved.
Publication types
- Penis / surgery
- Sex Reassignment Surgery* / methods
- Transgender Persons*
- Transsexualism* / surgery
- Vagina / surgery
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.14(6); 2022 Jun

National Trends in Gender-Affirming Surgical Procedures: A Google Trends Analysis
Emily merrick.
1 Plastic and Reconstructive Surgery, Northwestern University Feinberg School of Medicine, Chicago, USA
Joshua P Weissman
Sumanas w jordan, marco ellis.
Background: There has been a significant increase in the volume of gender-affirming surgical (GAS) procedures over the past decade. The objective of this paper is to use online search data from Google Trends (GT) to describe national search trends for GAS procedures.
Methods: GT was queried for search terms relating to GAS from January 2004 to February 2021. The 19 selected keywords covered a broad range of GAS topics. United States (US) search interest was collected as relative search volumes (RSVs) and then analyzed by geographic region. The number of plastic surgery providers offering GAS and academic surgery centers was collected from the World Professional Association for Transgender Health (WPATH) and Trans- health.com . RSVs were analyzed by metro area to determine the relationship between search demand and personal income. State Medicaid policies for transgender health services were also collected.
Results: All search terms demonstrated a positive increase in RSVs over time except “sex reassignment surgery” and “penectomy”. The Mountain/Pacific and East South Central/West South Central had the greatest search volume for GAS and most providers offering care. The East South Central/West South Central region ranked last for providers offering care, despite the relatively high search interest. This region also had no states with explicit Medicaid policies covering gender-affirming care. Metro areas in the top five for RSV but bottom quartile for per capita personal income were identified.
Conclusions: Online search interest for GAS-related terms has increased. Search interest for GAS has regional variation and did not show a specific pattern with provider availability.
Introduction
Approximately 1.4 million transgender and non-binary (TGNB) adults and 150,000 TGNB adolescents and young adults live in the United States (US) [ 1 ]. Gender-affirming surgery (GAS) has become increasingly performed over the past five years for this growing patient population [ 2 ]. GAS has been shown to improve quality of life among TGNB patients experiencing gender dysphoria [ 3 - 6 ]. Many patients consult internet forums and social media for information regarding GAS [ 7 , 8 ]. El-Hadi et al. found that websites targeted at TGNB patients were the primary source of information for GAS. Furthermore, the authors found that the majority of TGNB individuals had difficulty finding a physician and reported having a lack of access to information [ 3 ].
Search engines such as Google can provide valuable information about healthcare-related search trends. The largest keyword search engine, Google Trends (GT), is a free, accessible tool that allows individuals to analyze geographic and temporal trends as relative search volumes (RSVs) for search terms [ 9 ]. GT is gaining popularity in healthcare-related research [ 10 - 14 ]. As has been done in prior studies, these RSVs can be used as a proxy for both search demand and interest [ 14 - 19 ]. Prior plastic surgery research has utilized GT to predict public interest in various surgical procedures, understand demand for marketing purposes, perceive celebrity influences on procedure interest, and conduct geographical analysis of provider demand [ 14 - 19 ]. A recent study utilizing GT reported increased searches for GAS-related search terms globally [ 19 ].
GT has not been utilized to analyze US interest in GAS. The purpose of this study is to describe US trends in internet searches for GAS-related keywords by region and over time. We hypothesize that there will be discrepancies across various national regions between GT search demand for GAS such that areas with more surgical providers and gender centers will generate higher search interest.
Materials and methods
Data source
GT was used to assess search volumes and trends over time [ 9 , 20 ]. GT evaluates the interest of a specific search term and generates an indicator known as an RSV, which is a score that calculates the relative popularity of a term as a proportion of all Google search terms for a specific geographic region or time frame [ 9 , 20 ]. GT analyses can be customized by search term, geographic location, time period, category (e.g. “Arts and Entertainment”, “Books and Literature”), and type of Google search (e.g. “web search”, “image search”, “news search”). This method provides anonymous, open-source data that controls population size and internet usage. Each data point is divided by the total number of searches of the geography and time point it represents. The resultant numbers are scaled on a range of 0 to 100 based on a topic’s proportion to all searches on all topics within that region or time [ 9 ]. A score of 100 represents the geographic area or time period with the greatest interest for that search term. All other geographic areas and times are assigned numbers that quantify interest relative to the maximum. For example, if area or time X had a search volume of 550 searches and area or time Y had an RSV of 495 searches, GT would record area or time X as having an RSV of 100 (550/550) and area or time Y would have an RSV of 90 (495/550).
Data acquisition
GT search parameters were set to Geographic Location: “United States,” Time Period: “1/1/2004-2/18/2021,” Category: “All Categories,” and Type of Search: “Web Search” to capture all US queries for the designated terms. Specific dates were used to ensure the replicability of the study. The terms used in this analysis were among the core procedure types defined by the World Professional Association for Transgender Health (WPATH) [ 21 ]. The aim was to capture a broad scope of demand for GAS. Researcher and clinical consensus were used for final term selection as determined by the two senior authors who regularly perform GAS. Of note, the authors acknowledge that terminology such as male-to-female (“MTF”), “FTM”, and “gender confirmation surgery” may be considered outdated and/or stigmatizing to some. These terms were included in order to reflect and analyze language that shifts within a wide time frame. The search terms included in this study can be found in Table Table1. 1 . “Male to female/female to male surgery” was counted as one search term as GT does not consider word order and generates the same data for both searches. Terms that did not generate any RSV values from GT were excluded from the analysis. These terms were as follows: “peritoneal flap vaginoplasty”, “Adam’s apple reduction”, “facial masculinization”, “MTF vaginoplasty”, “transmasculine bottom surgery”, and “transfeminine bottom surgery”. Surgical terms that were not specific to gender-affirming procedures such as “vaginoplasty”, “breast augmentation”, and “mastectomy” were excluded. All terms were individually queried via GT and the RSVs were determined for each search term from January 1, 2004 to February 18, 2021.
Terms were selected through the World Professional Association for Transgender Health and clinical consensus between the two senior authors who frequently perform gender affirming procedures. The authors acknowledge that some terms are outdated and stigmatizing but were utilized to reflect the changing language of this wide time frame.
Temporal data
Microsoft Excel (Redmond, WA) was used to conduct a trend line analysis for each search term’s RSV.
Regional data
RSV values were recorded by state for each of the 19 search terms. States were categorized according to regions designated by the American Society of Plastic Surgeons (ASPS) Annual Reports [ 2 ]. Figure Figure1 1 displays the five regions used in the analysis. The top 10 RSVs were recorded for all search terms. The total number of times each region appeared in the top ten RSVs was recorded to compare regional interest in GAS.

To determine the specific region in which each search term was most popular, the top 10 RSVs were examined. The region composed the largest percentage of RSVs for each search term’s top 10 RSVs was deemed to have the greatest regional interest for that term. For search terms where there was insufficient data to report on 10 states, the RSV for all available states was reported. In the event that multiple regions made up equal percentages (e.g., five RSVs were from Region 1 and five RSVs were from Region 2), the region with the larger average RSV for that search term was determined to have the greatest interest.
Metropolitan area based on income data
A metropolitan analysis of RSV for each of our search terms was also conducted for all of our search terms. GT search parameters were set to Geographic Location: “United States,” Time Period: “1/1/2004-2/18/2021,” Categories: “All categories,” and Type of Search: “Web Search.” For each of our search terms, we analyzed any metro area that was in the top five for RSV but bottom quartile according to the US Bureau of Economic Analysis [ 22 ]. Metro areas were then recorded to determine demand trends in low-income areas where care may be less accessible.
Providers and academic medical centers offering GAS data
To quantify the number of plastic surgeon providers in the US offering GAS as of February 2021, the World Professional Association of Transgender Health’s (WPATH) website was utilized. The website lists plastic surgery providers in each state, and the search was subsequently filtered for these providers [ 21 ]. The number of providers listed on this website for each state were determined and the number of providers in each region were calculated. The Trans-Health website was queried for the number of academic medical centers with TGNB surgery programs [ 23 ]. Additional centers were manually added if they were known to have TGNB programs but were not listed on the website. All 154 websites of US medical schools were evaluated for access to a dedicated TGNB surgical program or dedicated GAS section, and fifteen academic medical centers were added to the original list. The number of centers were counted for each state and region.
Medicaid coverage data
As of February 2021, the states that have an explicit policy stating that TGNB health-related services are covered under Medicaid were determined [ 24 ]. We also examined which states had a policy excluding coverage and which states did not have a specific stance. We then calculated the number of states within each region that had each of the aforementioned policies. This was done to determine whether there are associations between a state’s Medicaid status for GAS and its overall search demand for GAS-specific terms.
Trends in interest in the United States from 2004 to 2021
Overall, national trends in search terms for gender affirming surgery revealed “transgender surgery,” “gender reassignment surgery,” “gender affirming surgery,” “gender confirming surgery” “top surgery,” “bottom surgery,” “upper surgery,” “lower surgery,” “male to female/female to male surgery,” “MTF bottom surgery,” “FTM bottom surgery,” “facial feminization surgery,” “metoidioplasty,” “FTM phalloplasty,” “tracheal shave,” “vulvoplasty,”, and “penile skin inversion.” all showed positive increases in RSV from 2004 to 2021. The two terms that showed a decrease in RSV overtime were “sex reassignment surgery” and “penectomy.”
Interest in GAS by region
Based on GT data for all selected search term to identify interest by state and region, 41/159 (25.8%) of the top ten RSV values fell into Region 5 (Mountain/Pacific), 38/159 (23.4%) RSVs fell into Region 4 (East South Central/West South Central), 34/159 (21.4%) of RSVs fell into Region 1 (New England/Middle Atlantic), 25/159 (15.7%) fell into Region 2 (East North Central/West North Central), and 21/159 (13.2%) RSVs fell into Region 3 (South Atlantic) (Figure (Figure2 2 ).

For all 19 search terms, the states with the top ten relative search volumes were listed. The number of times each state was included in the top 10 was noted and added into one of the five regions described by the America Society of Plastic Surgeons.
Based on RSV data for all nineteen search terms, Region 5 (Mountain/Pacific) had the greatest interest for the search terms: “sex reassignment surgery,” “gender reassignment surgery,” “tracheal shave,” “penectomy,” “facial feminization surgery,” “metoidioplasty,” and “penile skin inversion.” Region 4 (East South Central/West South Central) had the greatest interest for the search terms “bottom surgery,” “male to female/female to male surgery,” “vulvoplasty,” “lower surgery.” Region 1 (New England/Middle Atlantic) had the greatest interest for “transgender surgery,” “top surgery,” “FTM phalloplasty.” Region 3 (South Atlantic) had the greatest search interest for “MTF bottom surgery,” “FTM bottom surgery,” and “upper surgery.” Region 2 (East North Central/West North Central) had the greatest interest for the search terms “gender affirming surgery” and “gender confirming surgery.”
Metropolitan data based on income
Metro areas in the top five for RSV but bottom quartile for per capita personal income included: Richmond, Virginia, Las vegas, Nevada, Spartansburg, South Carolina, Grand rapids-Kalamazoo-Battle Creek, MI, Jacksonville, Florida, Columbus, Ohio, Hartford, Connecticut, and Bowling Green Kentucky.
The WPATH website provided 101 plastic surgery providers across the US. A national distribution of these providers can be seen in Figure Figure3. 3 . Region 5 (Mountain/Pacific) has the most providers with 33% of the total. Region 1 (New England/Middle Atlantic) has 26%, Region 2 (East North Central/West North Central) has 19%, Region 3 (South Atlantic) has 14% of the providers. Region 4 (East South Central/West South Central) has the fewest number of providers with nine percent.

Plastic surgeon providers across the United States as listed on the World Professional Association for Transgender Health (WPATH) website.
A total of 46 academic medical centers with TGNB surgery programs or dedicated TGNB surgery sections on their websites were found. A national distribution of these institutions can be seen in Figure Figure4. 4 . Region 1 (New England/Middle Atlantic) had the most institutions with 14 (30%). Region 2 (East North Central/West North Central) followed with 12 institutions (26%). Regions 3 (South Atlantic) and 5 (Mountain/Pacific) had nine (20%) and eight (17%) institutions, respectively. Region 4 (East South Central/West South Central) had the fewest number of institutions with three (7%).

States with academic medical centers with a dedicated transgender and non-binary surgery program or faculty dedicated to providing this type of care - World Professional Association for Transgender Health (WPATH) website.
Of the 22 states and Washington D.C. in which Medicaid programs cover gender affirming care, Region 1 (New England/Middle Atlantic) has the most states with this policy (nine states). Region 5 (Mountain/Pacific) follows with seven states, Region 2 (East North Central/West North Central) has four states, Region 3 (South Atlantic) has three states. Region 4 (East South Central/West South Central) has no states with this explicit policy. Figure Figure5 5 illustrates a national distribution of state policy.

We used GT to describe US search trends for various GAS procedures according to geographic region. As past studies have done, we aimed to use GT search data as a proxy for national interest in GAS [ 14 , 16 - 19 ]. Given the greater number of individuals identifying as TGNB, GAS is becoming an increasingly important component of health care in the US [ 25 - 27 ]. Prior studies have highlighted the rapid increase in demand for GAS [ 25 ]. We found that national search interest related to GAS has increased over time while demonstrating regional variation.
Our results highlight growing US search interest in GAS, as 17 of 19 included search terms had positive increases in RSVs from 2004 to 2021. The only terms that decreased in popularity were “sex reassignment surgery” and “penectomy.” This may be due to a shift in language used by TGNB individuals [ 4 - 7 , 25 - 27 ].
TGNB patients report that the lack of knowledgeable TGNB providers is a large barrier to care [ 27 ]. Using GT to identify areas that lack available providers may be a helpful step in addressing this barrier. Our GT analysis demonstrates that search interest for GAS does not align with areas containing providers or gender centers. This highlights a geographic barrier to accessing care. Our GT regional analysis shows that Region 5 (Mountain/Pacific) and Region 4 (East South Central/West South Central) have higher search demand volume relative to the other three regions. Despite generating relatively high search interest, Region 4 (East and West South Central) ranked last for both the number of providers and academic medical centers offering care. GT can be used to identify high interest, low availability areas where increasing providers may want to be prioritized.
Each region had certain search terms that were more widely used. For example, Region 5 (Mountain/Pacific) had the highest demand for terms such as “tracheal shave”, “penectomy”, and “facial feminization surgery” whereas Region 4 (East South Central/West South Central) had the highest demand for “vulvoplasty”. Variation in search interest for specific terms may indicate potentially popular procedures in certain regions and/or regional differences in language. Providers in these areas can use this knowledge to include popular searches in their internet presence or increase awareness about other available procedures that patients might appreciate but not be exposed to in their region.
Additionally, certain states (Wyoming, Wisconsin, Virginia, Delaware, South Dakota, and Hawaii) did not have top 10 search volumes for any of the selected terms. Of the states that did not appear in the top 10 for RSV volumes, only Wisconsin and Virginia had available providers to perform GAS. These can be targeted as areas where increasing awareness of potential procedures may be of significant value to TGNB individuals. GT can be used to track increased interest, and providers can be recruited to practice in areas of increasing interest.
We identified eight low-income metro areas with significant search interest for GAS procedures. To ensure equitable access to care, providers can be incentivized to practice in these areas. Our results demonstrate that Region 4 (East South Central/West South Central) had the lowest rates of Medicaid coverage and the fewest providers. Increasing coverage may be another means to draw providers to certain areas. Ultimately, regional variations of demand for gender-affirming care are complex and are often the result of local and state legislation, Medicaid coverage, and culture [ 28 ].
There are several limitations to this study. Search volume values can be skewed by population size. A state with a larger population may have a higher absolute search volume but a lower proportion of total search results compared to a state with a smaller population. This limitation is minimized as numbers are taken in the context of RSVs and there are no comparisons made between absolute search volumes. In addition, only search terms with sufficient interest to generate an RSV value were included. The authors also recognize that not every term relating to GAS may have been included in this analysis. Patients may also be searching terms not specifically analyzed in this study or search terms in another language. Additionally, this study is limited in not providing information or outcomes for those actually undergoing GAS: not differentiating between the number of insured versus uninsured patients undergoing GAS, complication rates, or the types of surgeries people are getting. This offers the future-direction of questionnaire-based studies to elucidate this information. The GT algorithm generates RSV values based on a random sample of Google searches, meaning that reproducibility of our exact search is not guaranteed. It is also important to acknowledge that not all patients have internet access. Our sample only represents patients who can search online. Nevertheless, the 2018 United States Census shows that 92% of households in the US own a computer and 85% had an internet subscription [ 29 ]. Although Google has the largest search engine market share (93%), the results of this study are only representative of the demographic that uses the Google search engine users and those who use the internet for healthcare-related information [ 30 ].
Conclusions
This paper reports on the utility of GT in relation to transgender health and GAS. We describe national trends in online search interest based on region, city, and metropolitan area. Our results highlight a strong, growing national interest in GAS. Search interest for GAS has regional variation and did not show a specific pattern with provider availability. By improving our understanding of temporal and geographical search interest, we can identify areas where patients may seek GAS.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
GPs taken out of day job to work in ‘gender dysphoria’ clinics
Family doctors will carry out assessments, recommend hormone treatment and make referrals for reassignment surgery
Family doctors are being put in charge of local NHS gender services, as specialist clinics become overwhelmed.
GPs will carry out assessments, recommend hormone treatment and make referrals for gender reassignment surgery - prompting concern that they will be drawn away from where they are most needed.
Health officials have set up new schemes, deploying GPs to take on work previously done by specialist clinics, as they warn that the current system cannot keep up with demand.
Pressure groups raised concern that responsibility for life-changing decisions was being handed to those with inadequate specialist knowledge, with one likening the pilot schemes to “the Wild West”.
In one pilot scheme, which has just been launched across Sussex, family doctors and nurses will be asked to carry out specialist assessments of adults with concerns around “gender dysphoria”.
Under their new roles GPs will take decisions about whether patients should be prescribed hormone therapy, voice coaching to “feminise” or “masculinise” their voices or be referred for gender reassignment surgery.
Those running the service, which has just begun taking patients, said all staff will be given specialist training from a centre for transgender health care in Nottingham, with which it has been paired.
It is one of five pilot schemes commissioned by NHS England which will mean those aged 17 and over who are considering medical treatment to change gender will receive consultations from GPs and staff working in sexual health services.
The moves come despite a national shortage of GPs, with a shortfall of more than 4,000 family doctors.
GP Louise Irvine , from the Clinical Advisory Network on Sex and Gender , said: “This will take GPs away from where they are desperately needed in general practice, which is suffering from a shortage of GPs. It also suggests the GPs who would staff these services would have a shorter training than the gender specialists, in order to have them available as soon as possible.”
She said giving GPs responsibility for assessment, hormone prescribing and referral for surgery was “the wrong approach” to address shortages of specialists.
“This is not part of core GP training and the training to be a gender specialist should be no less stringent and thorough than for specialist consultants,” she said.
‘Experts of their own experience’
The doctor said GPs were being expected to deliver services without a clear evidence base or rationale.
One NHS pilot scheme staffed by GPs describes itself as “trans and non-binary led” describing trans and non-binary people as “the experts of their own experience”.
In documents seen by The Telegraph, health officials suggest that the controversial shift is necessary because existing specialist clinics cannot cope with demand.
In the past decade, the number of referrals to adult gender dysphoria clinics has risen by 280 per cent, the report by NHS England warns, highlighting average waits of three years for a first appointment, and a risk of harm to those facing such delays.
“Based on waiting times and workforce shortages, there are concerns that the historical gender dysphoria clinic model is not sustainable in its current form,” it says.
“NHS England has established five new pilot services, testing how gender dysphoria healthcare delivered by gender dysphoria clinics could be delivered in other settings, such as primary care and sexual health clinics.”
The document, dated March 2023, warned that 28,000 people are waiting for a first appointment at a gender dysphoria clinic, including 1,100 in Sussex.
A report by Sussex Partnership NHS Foundation Trust, presented to council officials in Brighton and Hove, described how its pilot scheme will have GPs from Sussex as “core members of the clinical team” with nurses, speech and language therapists and psychologists also recruited and trained.
Surgical interventions
“The pilot will provide onward care as appropriate, including making referrals for surgical interventions,” it says, while the service will directly deliver “specialist endocrinology [hormone] services, speech and language/voice coaching and gender-specific psychological support.”
GPs working for the gender service will be asked to provide specialist assessments, and to make recommendations so patients seeking to change gender can be prescribed hormone treatment, such as testosterone or oestrogen.
While each of the five pilot schemes is different, most rely heavily on GPs.
The East of England has created a “GP-led” pilot, while Indigo Gender Service in Greater Manchester is based in primary care, and staffed by GPs, while describing itself as “trans and non-binary led”.
“We know that trans and non-binary people are the experts of their own experience, and that is why this service has been developed by and for trans communities. Our services are trans and non-binary led, with trans and non-binary people guiding and feeding into them at all levels,” the service states. The Cheshire and Merseyside Adult Gender Identity Collaborative is run by primary care and sexual health services. Another scheme, TransPlus, the first integrated Gender, Sexual, Health and HIV service, has been commissioned on a long-term basis, following a pilot phase.
NHS England has said the models may be rolled out more widely, depending on the success of the two-year pilots, which may be extended.
Complex area of healthcare
A spokesman from Sussex Partnership NHS Foundation Trust said: “We are continuing to develop the Sussex Gender Service, which is a pilot service, and are working to ensure the service is staffed by professionals who are highly skilled in this complex area of healthcare. “All vacant posts at the service are now recruited to, and most staff have received initial training. Staff who will form the pilot service continue to receive specialist training and supervision in gender healthcare from the Nottingham Centre for Transgender Healthcare - our link gender identity clinic. Our clinicians will also complete the Royal College of Physicians Gender Identity Healthcare Credentials course.”
Stephanie Davies Arai, founder and director of Transgender Trend, an organisation calling for evidence-based health care, said: “We have great concerns about these pilot clinics - they’re like the Wild West.”
“My concern is that these people are not really clinically qualified to make these diagnoses,” she said, warning of a lack of scrutiny of adult services which take cases from the age of 17.

She raised concerns that some of the schemes gave too much authority to those from the trans community, rather than to those taking an independent view.
“Where you’re getting people with so called ‘lived experience’ running the clinics or being heavily involved in these clinics, and nobody dare say anything against that, that deeply concerns me,” she said.
It comes after the NHS announced that it will no longer prescribe puberty blockers to children, outside of clinical trials, in a landmark decision.
It follows a decision last year to close the Tavistock child gender identity clinic , after a review found that it was “not safe”.
Guidance issued by the British Medical Association in October says that GPs should “understand gender incongruence and the issues involved to ensure quality care is provided”.
However, it says: “We need to balance what can be expected of GPs and the expertise which should rightly remain with specialist services”.
Earlier guidance from the Royal College of GPs stresses that “gender dysphoria and gender identity issues are not part of the GP curriculum or GP speciality training.
“GPs are currently required to refer patients experiencing gender dysphoria to gender identity specialists for further assessment and treatment advice.”
An NHS spokesman said: “While GPs will continue to focus on delivering a record number of routine appointments, a small number of primary care services alongside sexual health clinics will run gender dysphoria clinics, with staff in those services receiving specialist training from the Royal College of Physicians.”
- NHS (National Health Service),
- British Medical Association (BMA)
- Facebook Icon
- WhatsApp Icon

This State Just Outlawed Gender Reassignment Surgery on Children

Republican Gov. Mark Gordon (R-WYo.) signed a series of bills banning gender reassignment surgery on minors. However, he rejected a bill that would have elevated significant barriers to abortion,
On Friday, Gordon signed the “Children gender change prohibition," legislation into law, which bans physicians from performing gender-reassignment procedures on children and administering such medications that would alter their body chemistry.
"I signed SF99 because I support the protections this bill includes for children, however, it is my belief that the government is straying into the personal affairs of families," Gordon said in a statement. "Our legislature needs to sort out its intentions with regard to parental rights. While it inserts governmental prerogative in some places, it affirms parental rights in others."
The law will prohibit any “surgery that sterilizes the child, including castration, vasectomy, hysterectomy, oophorectomy, metoidioplasty, orchiectomy, penectomy, phalloplasty and vaginoplasty."
It will also ban related prescription drugs “that induce transient or permanent infertility," or are considered a “puberty suppression or blocking prescription drugs to stop or delay normal puberty."
Recommended

However, Gordon vetoed the “Regulation of abortions” bill, which would have placed further restrictions on abortions in the state.
The legislation would have "properly regulated surgical abortion clinics in Wyoming," however, the governor noted that the "amendments to the bill complicated its purpose, making it vulnerable to legal challenges."
“It is my opinion that HB148, as amended, had the potential to further delay the resolution of this critical issue for the unborn," Gordon said in the statement. "The potential of starting over on a new course of legal arguments would in my mind be derelict, and would have only sacrificed additional unborn lives in Wyoming."
The bill would have classified abortion clinics as a “ambulatory surgical center.”

Trending on Townhall Videos
- CNN Panelist Warns What Will Happen If Letitia James Seizes Trump's Assets, and It's Not Good for Dems
- Gallagher Is Resigning Early. Here's What's Troubling About the Date He Chose to Exit.
- Bidenomics Sucks, And So Does Joe And All Democrats
- Sen. John Kennedy: Can You Answer These Basic Questions About Climate Change, Please? Activist: Uh...


Wyoming governor signs bill outlawing gender-reassignment procedures on children, vetoes abortion restrictions
Wyoming's Republican Governor Mark Gordon signed into legislation Friday a bill outlawing gender-reassignment procedures on children and vetoed a bill that would have imposed further restrictions on abortion clinics, including required licensure.
SF0099, also titled "Children gender change prohibition," prohibits physicians from performing gender-reassignment procedures on children and administering related medications. The legislation specifically banned "a surgery that sterilizes the child, including castration, vasectomy, hysterectomy, oophorectomy, metoidioplasty, orchiectomy, penectomy, phalloplasty and vaginoplasty."
The legislation continued on to specify that outlawed medications under the legislation included "any of the following prescription drugs that induce transient or permanent infertility," proceeded by a list of medications , including "puberty suppression or blocking prescription drugs to stop or delay normal puberty."
WYOMING JUDGE TO RULE ON ABORTION LAWS, INCLUDING THE FIRST-IN-THE-NATION BAN ON ABORTION PILLS
The bill also outlined various procedures that were exempt from the legislation, such as procedures or treatments performed on a child as a result of "a medically verifiable genetic disorder of sex development." The legislation specified that parental/guardian consent was required.
"I signed SF99 because I support the protections this bill includes for children, however, it is my belief that the government is straying into the personal affairs of families" Gordon said in a statement released. "Our legislature needs to sort out its intentions with regard to parental rights. While it inserts governmental prerogative in some places, it affirms parental rights in others."
READ ON THE FOX NEWS APP
TRUMP SUGGESTS HE WOULD SUPPORT ABORTION BAN AT AROUND 15 WEEKS OF PREGNANCY
Gordon also vetoed HB0148, known as "Regulation of abortions," that would have placed additional restrictions on abortion clinics in the state. The press release noted that the bill would have "properly regulated surgical abortion clinics in Wyoming," but "amendments to the bill complicated its purpose, making it vulnerable to legal challenges."
The legislation would have required a surgical abortion facility in the state to be licensed as "an ambulatory surgical center," and a facility conducting the procedures would need a separate license as well.
NEW STUDY FINDS WOMEN WHO CHOOSE SUPPORTIVE BIRTH SERVICES OVER ABORTION BENEFIT IN TRAGIC FETAL ANOMALY CASES
"It is my opinion that HB148, as amended, had the potential to further delay the resolution of this critical issue for the unborn," Gordon said in the statement. "The potential of starting over on a new course of legal arguments would in my mind be derelict, and would have only sacrificed additional unborn lives in Wyoming."
Abortion is currently legal in Wyoming, pending a court decision challenging the state's abortion laws.
On the national scale, the U.S. Supreme Court is set to hear oral arguments Tuesday about the federal government's approval process of the drug mifepristone, a medication used to terminate pregnancies. A ruling is expected about three months later.
The Supreme Court is currently allowing the FDA to continue regulating the drug while the appeals process plays out. Such regulation includes continued telemedicine prescriptions and retail pharmacy dispensing.
Fox News' Shannon Bream, Bill Mears and The Associated Press contributed to this report.
Original article source: Wyoming governor signs bill outlawing gender-reassignment procedures on children, vetoes abortion restrictions

Bias of United Press International
92% of our members expressed interest in funding our mission.
Become an Angel Investor Now

TRUST, restored. NEWS, balanced. DEMOCRACY, strengthened.

- Balanced News
- Story of the Week
- News Curation Principles
- Newsletters
- Balanced Search
Wyoming governor signs bill banning gender reassignment surgery, care

United Press International
Related Coverage

AllSides Picks

Joan Blades
March 22nd, 2024

March 23rd, 2024

More News about Politics from the Left , Center and Right
From the left, from the center, from the right.


IMAGES
VIDEO
COMMENTS
Gender affirming surgery can be used to create a vulva and vagina. It involves removing the penis, testicles and scrotum. During a vaginoplasty procedure, tissue in the genital area is rearranged to create a vaginal canal (or opening) and vulva (external genitalia), including the labia. A version of vaginoplasty called vulvoplasty can create a ...
When people undergo a vulvoplasty, the surgeon forms a clitoris from the head of the penis. ... Long-term sensitivity and patient-reported functionality of the neoclitoris after gender ...
A vulvoplasty is a gender-affirming surgery that creates a vulva for transgender and nonbinary individuals who are designated male at birth (DMAB). 800.223.2273; ... A vulvoplasty is a major surgery with the potential to help you inhabit your gender more comfortably. As you consider whether or not a vulvoplasty is right for you, find a support ...
In male-to-female sex reassignment, the trans woman may choose to undergo vaginoplasty - the inversion of the penis to create a vagina - as part of her physical transition. This procedure can result in a fully sensate neovagina. Dr. MacPhee performs this reconstructive procedure by disassembling the penis and utilizing the inverted penile ...
The vulva is the outside part of the vagina. A vulvoplasty is a type of surgery that uses skin and tissue from a penis to create all of the outside parts of a vagina (except for the vaginal canal). The steps of a vulvoplasty are the same as a vaginoplasty. During a vulvoplasty, your surgeon will:
Research consistently shows that people who choose gender affirmation surgery experience reduced gender incongruence and improved quality of life. Depending on the procedure, 94% to 100% of people report satisfaction with their surgery results. Gender-affirming surgery provides long-term mental health benefits, too.
Sex reassignment surgery is usually preceded by beginning feminizing hormone therapy. Some surgeries can reduce the need for hormone therapy. ... Vulvoplasty is the process of constructing a neovulva from existing genital tissue. The testicles, scrotum, and penis are removed, and the glans made into a clitoris.
Overview. Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation.
Vaginoplasty is a gender-affirming, feminizing, lower surgery (transgender surgery; gender reassignemnt surgery; sex change surgery) to create a vagina and vulva (including mons, labia, clitoris, and urethral opening) and remove the penis, scrotal sac and testes.
She does more than 150 a year. We also offer a Transgender Gynecology Clinic with a gender-neutral space. Services include surgery. Referrals and appointments are made through the OHSU Center for Women's Health, though the space is not in the center. Call 503-418-4500 to request an appointment.
Community Commitment. Lesbian, Gay, Bisexual and Transgender Health Care. Gender Affirming Surgical Services. Before & After Photos. Appointments 216.445.6308. Request an Appointment. See before and after photos of patients who have undergone gender-affirming surgeries at Cleveland Clinic, including breast augmentations, facial feminizations ...
Salim A, Poh M. Clinics in Plastic Surgery, Volume 45, Issue 3, July 2018, Pages 343-350. Vulvoplasty is a male-to-female gender affirming procedure that removes the penis, scrotum and testicles, creates the labia and clitoris, and re-positions the urethral opening. Unlike Vaginoplasty, Vulvoplasty does not include the creation of the vaginal ...
Note on gender-affirming hormones: Consult your surgeon and hormone prescriber prior to surgery, as your hormone regimen will be altered prior to and post-surgery. Note on fertility: Vulvoplasty is a permanent, irreversible procedure that results in the loss of fertility. Fertility preservation and family planning must be completed prior to ...
You may have heard patients refer to it as bottom surgery, lower surgery, Sexual Reassignment Surgery, Gender Reassignment Surgery, a sex change surgery, inning-an-outie, vice versa, or others. ... Vulvoplasty, or shallow depth vaginoplasty/zero depth vaginoplasty is an alternative form of GRS to surgically create a vulva from existing tissue ...
The Crane Center for Transgender Surgery has announced the launch of a gender-affirming hormone clinic at their transgender wellness center in Austin, Texas. The new clinic offers hormone replacement therapy for transgender and non-binary adults through an informed consent model. Both in-office and telemedicine appointments are available.
A vulvoplasty is a type of surgery that uses skin and tissue from a penis to create the vulva which is all the outside parts of a vagina (except for the vaginal canal). This surgery creates the same look as a full vaginoplasty, however a vagina and vaginal walls are not
Purpose of Review There is a significant rise in the interest in genital gender affirmation surgery (gGAS), which is increasingly offered and performed throughout the world. While gGAS is not new, the expansion of gGAS is associated with progressive societal acceptance of transgender and gender non-conforming individuals. There is a clear role for gGAS in the management of gender dysphoria ...
Conclusions: This is the first study of factors impacting a patient's choice of or a surgeon's recommendation for vulvoplasty over vaginoplasty as gender-affirming genital surgery; it also is the first reported series of patients undergoing vulvoplasty only. Limitations of this study include its retrospective nature, non-validated questions ...
That depends on the type of operation you get. Costs are high, however, and can range anywhere from $35,000 to $40,000 . The good news is that more and more insurance companies are open to covering gender reassignment surgeries and procedures. Depending on your coverage, you may be able to get some or most of the costs covered.
Transgender women may opt for genital gender-affirming surgery (gGAS), which comprises bilateral orchiectomy, gender-affirming vulvoplasty, or vaginoplasty. Vaginoplasty is chosen most frequently in this population, penile inversion vaginoplasty being the surgical gold standard. In selected cases, skin graft vaginoplasty, intestinal ...
Approximately 1.4 million transgender and non-binary (TGNB) adults and 150,000 TGNB adolescents and young adults live in the United States (US) [ 1 ]. Gender-affirming surgery (GAS) has become increasingly performed over the past five years for this growing patient population [ 2 ]. GAS has been shown to improve quality of life among TGNB ...
In sex reassignment surgery, some male-to-female transgender patients receive vulvoplasty without vaginoplasty to reconstruct the exterior of female genitalia. During clitoroplasty, a clitoris is made from the tissue of the glans penis. Labiaplasty can be performed as a discrete surgery, or as a subordinate procedure within a vaginoplasty.
(7) "Genital gender reassignment surgery" means a surgical procedure performed for the purpose of assisting an individual with a physical gender transition including, without limitation, penectomy, orchiectomy, vaginoplasty, clitoroplasty, vulvoplasty, hysterectomy, ophorectomy, reconstruction of the urethra, metoidioplasty or phalloplasty ...
March 23 (UPI) --Wyoming's Republican governor has signed a bill into law banning doctors in that state from performing gender transitioning and gender reassignment procedures for children.Wyoming ...
GPs will carry out assessments, recommend hormone treatment and make referrals for gender reassignment surgery - prompting concern that they will be drawn away from where they are most needed.
French Senators want to ban gender transition treatments for under-18s, after a report described sex reassignment in minors as potentially "one of the greatest ethical scandals in the history of ...
Republican Gov. Mark Gordon (R-WYo.) signed a series of bills banning gender reassignment surgery on minors. However, he rejected a bill that would have elevated significant barriers to abortion ...
Wyoming's Gov. Mark Gordon passed legislation Friday outlawing gender-reassignment procedures on minors in the state and vetoed a separate bill that would have placed additional restrictions on ...
In 2012, former U.S. Vice President Dick Cheney, 71, underwent heart transplant surgery at a hospital in Falls Church, Va. ... Wyoming governor signs bill banning gender reassignment surgery, care.
Wyoming governor signs bill banning gender reassignment surgery, care. Politics. Posted on AllSides March 23rd, 2024. Save for Later . From The Center. Read full story. Politics. United Press International. AllSides Media Bias Rating: Center. agree; disagree; 125387 / 93967.