- Search Menu
- Advance Articles
- Editor's Choice
- Supplements
- Patient Perspectives
- Methods Corner
- ESC Content Collections
- Author Guidelines
- Instructions for reviewers
- Submission Site
- Open Access Options
- Self-Archiving Policy
- Read & Publish
- About European Journal of Cardiovascular Nursing
- About ACNAP
- About European Society of Cardiology
- ESC Publications
- Editorial Board
- Advertising & Corporate Services
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, why patient journey mapping, how is patient journey mapping conducted, use of technology in patient journey mapping, future implications for patient journey mapping, conclusions, patient journey mapping: emerging methods for understanding and improving patient experiences of health systems and services.
Lemma N Bulto and Ellen Davies Shared first authorship.
Conflict of interest: none declared.
- Article contents
- Figures & tables
- Supplementary Data
Lemma N Bulto, Ellen Davies, Janet Kelly, Jeroen M Hendriks, Patient journey mapping: emerging methods for understanding and improving patient experiences of health systems and services, European Journal of Cardiovascular Nursing , 2024;, zvae012, https://doi.org/10.1093/eurjcn/zvae012
- Permissions Icon Permissions
Patient journey mapping is an emerging field of research that uses various methods to map and report evidence relating to patient experiences and interactions with healthcare providers, services, and systems. This research often involves the development of visual, narrative, and descriptive maps or tables, which describe patient journeys and transitions into, through, and out of health services. This methods corner paper presents an overview of how patient journey mapping has been conducted within the health sector, providing cardiovascular examples. It introduces six key steps for conducting patient journey mapping and describes the opportunities and benefits of using patient journey mapping and future implications of using this approach.
Acquire an understanding of patient journey mapping and the methods and steps employed.
Examine practical and clinical examples in which patient journey mapping has been adopted in cardiac care to explore the perspectives and experiences of patients, family members, and healthcare professionals.
Quality and safety guidelines in healthcare services are increasingly encouraging and mandating engagement of patients, clients, and consumers in partnerships. 1 The aim of many of these partnerships is to consider how health services can be improved, in relation to accessibility, service delivery, discharge, and referral. 2 , 3 Patient journey mapping is a research approach increasingly being adopted to explore these experiences in healthcare. 3
a patient-oriented project that has been undertaken to better understand barriers, facilitators, experiences, interactions with services and/or outcomes for individuals and/or their carers, and family members as they enter, navigate, experience and exit one or more services in a health system by documenting elements of the journey to produce a visual or descriptive map. 3
It is an emerging field with a clear patient-centred focus, as opposed to studies that track patient flow, demand, and movement. As a general principle, patient journey mapping projects will provide evidence of patient perspectives and highlight experiences through the patient and consumer lens.
Patient journey mapping can provide significant insights that enable responsive and context-specific strategies for improving patient healthcare experiences and outcomes to be designed and implemented. 3–6 These improvements can occur at the individual patient, model of care, and/or health system level. As with other emerging methodologies, questions have been raised regarding exactly how patient journey mapping projects can best be designed, conducted, and reported. 3
In this methods paper, we provide an overview of patient journey mapping as an emergent field of research, including reasons that mapping patient journeys might be considered, methods that can be adopted, the principles that can guide patient journey mapping data collection and analysis, and considerations for reporting findings and recognizing the implications of findings. We summarize and draw on five cardiovascular patient journey mapping projects, as examples.
One of the most appealing elements of the patient journey mapping field of research is its focus on illuminating the lived experiences of patients and/or their family members, and the health professionals caring for them, methodically and purposefully. Patient journey mapping has an ability to provide detailed information about patient experiences, gaps in health services, and barriers and facilitators for access to health services. This information can be used independently, or alongside information from larger data sets, to adapt and improve models of care relevant to the population that is being investigated. 3
To date, the most frequent reason for adopting this approach is to inform health service redesign and improvement. 3 , 7 , 8 Other reasons have included: (i) to develop a deeper understanding of a person’s entire journey through health systems; 3 (ii) to identify delays in diagnosis or treatment (often described as bottlenecks); 9 (iii) to identify gaps in care and unmet needs; (iv) to evaluate continuity of care across health services and regions; 10 (v) to understand and evaluate the comprehensiveness of care; 11 (vi) to understand how people are navigating health systems and services; and (vii) to compare patient experiences with practice guidelines and standards of care.
Patient journey mapping approaches frequently use six broad steps that help facilitate the preparation and execution of research projects. These are outlined in the Central illustration . We acknowledge that not all patient journey mapping approaches will follow the order outlined in the Central illustration , but all steps need to be considered at some point throughout each project to ensure that research is undertaken rigorously, appropriately, and in alignment with best practice research principles.
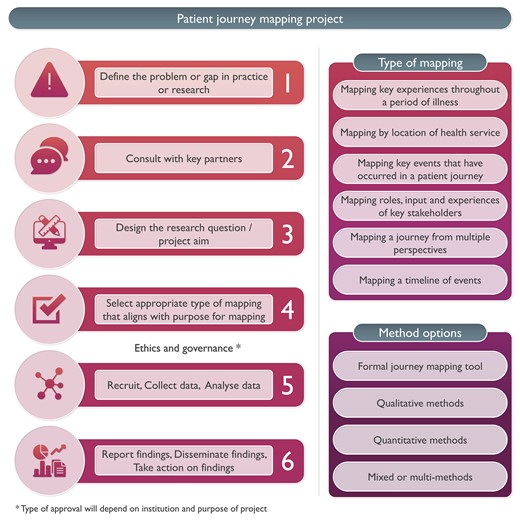
Steps for conducing patient journey mapping.
Five cardiovascular patient journey mapping research examples have been included in Figure 1 , 12–16 to provide specific context and illustrate these six steps. For each of these examples, the problem or gap in practice or research, consultation processes, research question or aim, type of mapping, methods, and reporting of findings have been extracted. Each of these steps is then discussed, using these cardiovascular examples.
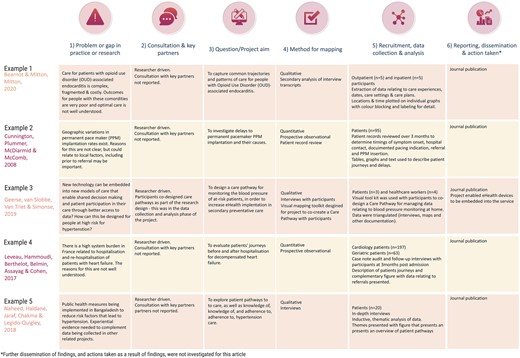
Examples of patient journey mapping projects.
Define the problem or gap in practice or research
Developing an understanding of a problem or gap in practice is essential for facilitating the design and development of quality research projects. In the examples outlined in Figure 1 , it is evident that clinical variation or system gaps have been explored using patient journey mapping. In the first two examples, populations known to have health vulnerabilities were explored—in Example 1, this related to comorbid substance use and physical illness, 13 and in Example 2, this related to geographical location. 13 Broader systems and societal gaps were explored in Examples 4 and 5, respectively, 15 , 16 and in Example 3, a new technologically driven solution for an existing model of care was tested for its ability to improve patient outcomes relating to hypertension. 14
Consultation, engagement, and partnership
Ideally, consultation with heathcare providers and/or patients would occur when the problem or gap in practice or research is being defined. This is a key principle of co-designed research. 17 Numerous existing frameworks for supporting patient involvement in research have been designed and were recently documented and explored in a systematic review by Greenhalgh et al . 18 While none of the five example studies included this step in the initial phase of the project, it is increasingly being undertaken in patient partnership projects internationally (e.g. in renal care). 17 If not in the project conceptualization phase, consultation may occur during the data collection or analysis phase, as demonstrated in Example 3, where a care pathway was co-created with participants. 14 We refer readers to Greenhalgh’s systematic review as a starting point for considering suitable frameworks for engaging participants in consultation, partnership, and co-design of patient journey mapping projects. 18
Design the research question/project aim
Conducting patient journey mapping research requires a thoughtful and systematic approach to adequately capture the complexity of the healthcare experience. First, the research objectives and questions should be clearly defined. Aspects of the patient journey that will be explored need to be identified. Then, a robust approach must be developed, taking into account whether qualitative, quantitative, or mixed methods are more appropriate for the objectives of the study.
For example, in the cardiac examples in Figure 1 , the broad aims included mapping existing pathways through health services where there were known problems 12 , 13 , 15 , 16 and documenting the co-creation of a new care pathway using quantitative, qualitative, or mixed methods. 14
In traditional studies, questions that might be addressed in the area of patient movement in health systems include data collected through the health systems databases, such as ‘What is the length of stay for x population’, or ‘What is the door to balloon time in this hospital?’ In contrast, patient mapping journey studies will approach asking questions about experiences that require data from patients and their family members, e.g. ‘What is the impact on you of your length of stay?’, ‘What was your experience in being assessed and undergoing treatment for your chest pain?’, ‘What was your experience supporting this patient during their cardiac admission and discharge?’
Select appropriate type of mapping
The methods chosen for mapping need to align with the identified purpose for mapping and the aim or question that was designed in Step 3. A range of research methods have been used in patient journey mapping projects involving various qualitative, quantitative, and mixed methods techniques and tools. 4 Some approaches use traditional forms of data collection, such as short-form and long-form patient interviews, focus groups, and direct patient observations. 18 , 19 Other approaches use patient journey mapping tools, designed and used with specific cultural groups, such as First Nations peoples using artwork, paintings, sand trays, and photovoice. 17 , 20 In the cardiovascular examples presented in Figure 1 , both qualitative and quantitative methods have been used, with interviews, patient record reviews, and observational techniques adopted to map patient journeys.
In a recent scoping review investigating patient journey mapping across all health care settings and specialities, six types of patient journey mapping were identified. 3 These included (i) mapping key experiences throughout a period of illness; (ii) mapping by location of health service; (iii) mapping by events that occurred throughout a period of illness; (iv) mapping roles, input, and experiences of key stakeholders throughout patient journeys; (v) mapping a journey from multiple perspectives; and (vi) mapping a timeline of events. 3 Combinations or variations of these may be used in cardiovascular settings in the future, depending on the research question, and the reasons mapping is being undertaken.
Recruit, collect data, and analyse data
The majority of health-focused patient journey mapping projects published to date have recruited <50 participants. 3 Projects with fewer participants tend to be qualitative in nature. In the cardiovascular examples provided in Figure 1 , participant numbers range from 7 14 to 260. 15 The 3 studies with <20 participants were qualitative, 12 , 14 , 16 and the 2 with 95 and 260 participants, respectively, were quantitative. 13 , 15 As seen in these and wider patient journey mapping examples, 3 participants may include patients, relatives, carers, healthcare professionals, or other stakeholders, as required, to meet the study objectives. These different participant perspectives may be analysed within each participant group and/or across the wider cohort to provide insights into experiences, and the contextual factors that shape these experiences.
The approach chosen for data collection and analysis will vary and depends on the research question. What differentiates data analysis in patient journey mapping studies from other qualitative or quantitative studies is the focus on describing, defining, or exploring the journey from a patient’s, rather than a health service, perspective. Dimensions that may, therefore, be highlighted in the analysis include timing of service access, duration of delays to service access, physical location of services relative to a patient’s home, comparison of care received vs. benchmarked care, placing focus on the patient perspective.
The mapping of individual patient journeys may take place during data collection with the use of mapping templates (tables, diagrams, and figures) and/or later in the analysis phase with the use of inductive or deductive analysis, mapping tables, or frameworks. These have been characterized and visually represented in a recent scoping review. 3 Representations of patient journeys can also be constructed through a secondary analysis of previously collected data. In these instances, qualitative data (i.e. interviews and focus group transcripts) have been re-analysed to understand whether a patient journey narrative can be extracted and reported. Undertaking these projects triggers a new research cycle involving the six steps outlined in the Central illustration . The difference in these instances is that the data are already collected for Step 5.
Report findings, disseminate findings, and take action on findings
A standardized, formal reporting guideline for patient journey mapping research does not currently exist. As argued in Davies et al ., 3 a dedicated reporting guide for patient journey mapping would be ill-advised, given the diversity of approaches and methods that have been adopted in this field. Our recommendation is for projects to be reported in accordance with formal guidelines that best align with the research methods that have been adopted. For example, COREQ may be used for patient journey mapping where qualitative methods have been used. 20 STROBE may be used for patient journey mapping where quantitative methods have been used. 21 Whichever methods have been adopted, reporting of projects should be transparent, rigorous, and contain enough detail to the extent that the principles of transparency, trustworthiness, and reproducibility are upheld. 3
Dissemination of research findings needs to include the research, healthcare, and broader communities. Dissemination methods may include academic publications, conference presentations, and communication with relevant stakeholders including healthcare professionals, policymakers, and patient advocacy groups. Based on the findings and identified insights, stakeholders can collaboratively design and implement interventions, programmes, or improvements in healthcare delivery that overcome the identified challenges directly and address and improve the overall patient experience. This cyclical process can hopefully produce research that not only informs but also leads to tangible improvements in healthcare practice and policy.
Patient journey mapping is typically a hands-on process, relying on surveys, interviews, and observational research. The technology that supports this research has, to date, included word processing software, and data analysis packages, such as NVivo, SPSS, and Stata. With the advent of more sophisticated technological tools, such as electronic health records, data analytics programmes, and patient tracking systems, healthcare providers and researchers can potentially use this technology to complement and enhance patient journey mapping research. 19 , 20 , 22 There are existing examples where technology has been harnessed in patient journey. Lee et al . used patient journey mapping to verify disease treatment data from the perspective of the patient, and then the authors developed a mobile prototype that organizes and visualizes personal health information according to the patient-centred journey map. They used a visualization approach for analysing medical information in personal health management and examined the medical information representation of seven mobile health apps that were used by patients and individuals. The apps provide easy access to patient health information; they primarily import data from the hospital database, without the need for patients to create their own medical records and information. 23
In another example, Wauben et al. 19 used radio frequency identification technology (a wireless system that is able to track a patient journey), as a component of their patient journey mapping project, to track surgical day care patients to increase patient flow, reduce wait times, and improve patient and staff satisfaction.
Patient journey mapping has emerged as a valuable research methodology in healthcare, providing a comprehensive and patient-centric approach to understanding the entire spectrum of a patient’s experience within the healthcare system. Future implications of this methodology are promising, particularly for transforming and redesigning healthcare delivery and improving patient outcomes. The impact may be most profound in the following key areas:
Personalized, patient-centred care : The methodology allows healthcare providers to gain deep insights into individual patient experiences. This information can be leveraged to deliver personalized, patient-centric care, based on the needs, values, and preferences of each patient, and aligned with guideline recommendations, healthcare professionals can tailor interventions and treatment plans to optimize patient and clinical outcomes.
Enhanced communication, collaboration, and co-design : Mapping patient interactions with health professionals and journeys within and across health services enables specific gaps in communication and collaboration to be highlighted and potentially informs responsive strategies for improvement. Ideally, these strategies would be co-designed with patients and health professionals, leading to improved care co-ordination and healthcare experience and outcomes.
Patient engagement and empowerment : When patients are invited to share their health journey experiences, and see visual or written representations of their journeys, they may come to understand their own health situation more deeply. Potentially, this may lead to increased health literacy, renewed adherence to treatment plans, and/or self-management of chronic conditions such as cardiovascular disease. Given these benefits, we recommend that patients be provided with the findings of research and quality improvement projects with which they are involved, to close the loop, and to ensure that the findings are appropriately disseminated.
Patient journey mapping is an emerging field of research. Methods used in patient journey mapping projects have varied quite significantly; however, there are common research processes that can be followed to produce high-quality, insightful, and valuable research outputs. Insights gained from patient journey mapping can facilitate the identification of areas for enhancement within healthcare systems and inform the design of patient-centric solutions that prioritize the quality of care and patient outcomes, and patient satisfaction. Using patient journey mapping research can enable healthcare providers to forge stronger patient–provider relationships and co-design improved health service quality, patient experiences, and outcomes.
None declared.
Farmer J , Bigby C , Davis H , Carlisle K , Kenny A , Huysmans R , et al. The state of health services partnering with consumers: evidence from an online survey of Australian health services . BMC Health Serv Res 2018 ; 18 : 628 .
Google Scholar
Kelly J , Dwyer J , Mackean T , O’Donnell K , Willis E . Coproducing Aboriginal patient journey mapping tools for improved quality and coordination of care . Aust J Prim Health 2017 ; 23 : 536 – 542 .
Davies EL , Bulto LN , Walsh A , Pollock D , Langton VM , Laing RE , et al. Reporting and conducting patient journey mapping research in healthcare: a scoping review . J Adv Nurs 2023 ; 79 : 83 – 100 .
Ly S , Runacres F , Poon P . Journey mapping as a novel approach to healthcare: a qualitative mixed methods study in palliative care . BMC Health Serv Res 2021 ; 21 : 915 .
Arias M , Rojas E , Aguirre S , Cornejo F , Munoz-Gama J , Sepúlveda M , et al. Mapping the patient’s journey in healthcare through process mining . Int J Environ Res Public Health 2020 ; 17 : 6586 .
Natale V , Pruette C , Gerohristodoulos K , Scheimann A , Allen L , Kim JM , et al. Journey mapping to improve patient-family experience and teamwork: applying a systems thinking tool to a pediatric ambulatory clinic . Qual Manag Health Care 2023 ; 32 : 61 – 64 .
Cherif E , Martin-Verdier E , Rochette C . Investigating the healthcare pathway through patients’ experience and profiles: implications for breast cancer healthcare providers . BMC Health Serv Res 2020 ; 20 : 735 .
Gilburt H , Drummond C , Sinclair J . Navigating the alcohol treatment pathway: a qualitative study from the service users’ perspective . Alcohol Alcohol 2015 ; 50 : 444 – 450 .
Gichuhi S , Kabiru J , M’Bongo Zindamoyen A , Rono H , Ollando E , Wachira J , et al. Delay along the care-seeking journey of patients with ocular surface squamous neoplasia in Kenya . BMC Health Serv Res 2017 ; 17 : 485 .
Borycki EM , Kushniruk AW , Wagner E , Kletke R . Patient journey mapping: integrating digital technologies into the journey . Knowl Manag E-Learn 2020 ; 12 : 521 – 535 .
Barton E , Freeman T , Baum F , Javanparast S , Lawless A . The feasibility and potential use of case-tracked client journeys in primary healthcare: a pilot study . BMJ Open 2019 ; 9 : e024419 .
Bearnot B , Mitton JA . “You’re always jumping through hoops”: journey mapping the care experiences of individuals with opioid use disorder-associated endocarditis . J Addict Med 2020 ; 14 : 494 – 501 .
Cunnington MS , Plummer CJ , McDiarmid AK , McComb JM . The patient journey from symptom onset to pacemaker implantation . QJM 2008 ; 101 : 955 – 960 .
Geerse C , van Slobbe C , van Triet E , Simonse L . Design of a care pathway for preventive blood pressure monitoring: qualitative study . JMIR Cardio 2019 ; 3 : e13048 .
Laveau F , Hammoudi N , Berthelot E , Belmin J , Assayag P , Cohen A , et al. Patient journey in decompensated heart failure: an analysis in departments of cardiology and geriatrics in the Greater Paris University Hospitals . Arch Cardiovasc Dis 2017 ; 110 : 42 – 50 .
Naheed A , Haldane V , Jafar TH , Chakma N , Legido-Quigley H . Patient pathways and perceptions of treatment, management, and control Bangladesh: a qualitative study . Patient Prefer Adherence 2018 ; 12 : 1437 – 1449 .
Bateman S , Arnold-Chamney M , Jesudason S , Lester R , McDonald S , O’Donnell K , et al. Real ways of working together: co-creating meaningful Aboriginal community consultations to advance kidney care . Aust N Z J Public Health 2022 ; 46 : 614 – 621 .
Greenhalgh T , Hinton L , Finlay T , Macfarlane A , Fahy N , Clyde B , et al. Frameworks for supporting patient and public involvement in research: systematic review and co-design pilot . Health Expect 2019 ; 22 : 785 – 801 .
Wauben LSGL , Guédon ACP , de Korne DF , van den Dobbelsteen JJ . Tracking surgical day care patients using RFID technology . BMJ Innov 2015 ; 1 : 59 – 66 .
Tong A , Sainsbury P , Craig J . Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups . Int J Qual Health Care 2007 ; 19 : 349 – 357 .
von Elm E , Altman DG , Egger M , Pocock SJ , Gøtzsche PC , Vandenbroucke JP , et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies . Lancet 2007 ; 370 (9596): 1453 – 1457 .
Wilson A , Mackean T , Withall L , Willis EM , Pearson O , Hayes C , et al. Protocols for an Aboriginal-led, multi-methods study of the role of Aboriginal and Torres Strait Islander health workers, practitioners and Liaison officers in quality acute health care . J Aust Indigenous HealthInfoNet 2022 ; 3 : 1 – 15 .
Lee B , Lee J , Cho Y , Shin Y , Oh C , Park H , et al. Visualisation of information using patient journey maps for a mobile health application . Appl Sci 2023 ; 13 : 6067 .
Author notes
- cardiovascular system
- health personnel
- health services
- health care systems
- narrative discourse
Email alerts
Related articles in pubmed, citing articles via.
- Recommend to Your Librarian
- Advertising and Corporate Services
- Journals Career Network
Affiliations
- Online ISSN 1873-1953
- Print ISSN 1474-5151
- Copyright © 2024 European Society of Cardiology
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.

Patients’ Lived Experiences During the Transplant and Cellular Therapy Journey pp 9–17 Cite as
Creating a Patient-Centered Case Study
- Jennifer Holl 5 ,
- Lisa Wesinger 6 ,
- Judi Gentes 7 ,
- Carissa Morton 8 &
- Jean Coffey 9
- First Online: 25 August 2023
61 Accesses
Case studies provide an invaluable record of professional clinical practice and have been used in medicine since the late 1800s to describe both traditional and unusual presentations of specific disease pathologies. In medicine, case studies traditionally take a detached, objective approach to outlining the clinical course of a disease and its treatment. In keeping with the holistic approach to patient care found in nursing and using the theoretical foundations established in Jean Watson’s Theory of Human Caring as well as the Relationship-Based Care Model, this research team sought to revolutionize the case study paradigm and deconstruct the traditional case study approach, placing the patient, instead of the provider, at the center of the narrative. This new case study method intercalates the clinicians’ analysis of the case with the patient’s commentary. This chapter outlines the methods and theoretical underpinnings used to create a patient-centered case study and seeks to provide nurses with a creative alternative to the traditional, objective case study approach. Implications for future research include whether using patient-centered case studies, instead of traditional case studies, provide a valuable learning tool to educate nurses.
- Qualitative research
- Phenomenology
- Relationship-based care
This is a preview of subscription content, log in via an institution .
Buying options
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Bergen A, While A. A case for case studies: exploring the use of case study design in community nursing research. J Adv Nurs. 2000;31(4):926–34.
Article CAS PubMed Google Scholar
Benner P. Interpretive phenomenology. Thousand Oaks: Sage Publications; 1994.
Google Scholar
Gary JC, Hudson CE. Reverse engineering: strategy to teach evidence-based practice to online RN-to-BSN students. Nurse Educ. 2016;41(2):83–5.
Article PubMed Google Scholar
Koloroutis M, editor. Relationship-based care: a model for transforming practice. Minneapolis: Creative Health Care Management; 2004.
Luck L, Jackson D, Usher K. Case study: a bridge across the paradigms. Nurs Inq. 2006;13(2):103–9.
Meyer CB. A case in case study methodology. Field Methods. 2001;13:329–52.
Article Google Scholar
Noble H, Smith J. Issues of validity and reliability in qualitative research. Evid Based Nurs. 2015;18(2):34–5. https://doi.org/10.1136/eb-2015-102054 .
Polit DF, Beck CT. Essentials of nursing research: appraising evidence for nursing practice. 8th ed. Philadelphia: Lippincott Williams & Wilkins; 2014.
Smith J, Flowers P, Larkin M. Interpretative phenomenological analysis: theory, method and research. London: Sage; 2013.
Taylor R, Thomas-Gregory A. Case study research. Nurs Stand. 2015;29(41):36–40.
Watson J. Nursing: the philosophy and science of caring. Rev. ed. Boulder: University Press of Colorado; 2008.
Yin RK. Case study research: design and methods. 5th ed. Thousand Oaks: Sage Publications; 2014.
Download references
Author information
Authors and affiliations.
Hematology/Oncology, Dartmouth Health, Lebanon, NH, USA
Jennifer Holl
Transplant and Cellular Therapy, Dartmouth Health, Lebanon, NH, USA
Lisa Wesinger
Oncology/Hematology, Dartmouth Health, Lebanon, NH, USA
Judi Gentes
Dartmouth Health, Dartmouth Cancer Center, St. Johnsbury, VT, USA
Carissa Morton
School of Nursing, University of Connecticut, Storrs, CT, USA
Jean Coffey
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Jean Coffey .
Editor information
Editors and affiliations.
Dartmouth Health, Dartmouth–Hitchcock Medical Center, Lebanon, NH, USA
John M. Hill Jr.
School Nursing, University of Connecticut, Storrs, CT, USA
Thomas Long
Elizabeth B. McGrath
Rights and permissions
Reprints and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter.
Holl, J., Wesinger, L., Gentes, J., Morton, C., Coffey, J. (2023). Creating a Patient-Centered Case Study. In: Coffey, J., Hill Jr., J.M., Long, T., McGrath, E.B. (eds) Patients’ Lived Experiences During the Transplant and Cellular Therapy Journey. Springer, Cham. https://doi.org/10.1007/978-3-031-25602-8_2
Download citation
DOI : https://doi.org/10.1007/978-3-031-25602-8_2
Published : 25 August 2023
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-25601-1
Online ISBN : 978-3-031-25602-8
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 04 December 2019
“Patient Journeys”: improving care by patient involvement
- Matt Bolz-Johnson 1 ,
- Jelena Meek 2 &
- Nicoline Hoogerbrugge 2
European Journal of Human Genetics volume 28 , pages 141–143 ( 2020 ) Cite this article
24k Accesses
18 Citations
25 Altmetric
Metrics details
- Cancer genetics
- Cancer screening
- Cancer therapy
- Health policy
“I will not be ashamed to say ‘ I don’t know’ , nor will I fail to call in my colleagues…”. For centuries this quotation from the Hippocratic oath, has been taken by medical doctors. But what if there are no other healthcare professionals to call in, and the person with the most experience of the disease is sitting right in front of you: ‘ your patient ’.
This scenario is uncomfortably common for patients living with a rare disease when seeking out health care. They are fraught by many hurdles along their health care pathway. From diagnosis to treatment and follow-up, their healthcare pathway is defined by a fog of uncertainties, lack of effective treatments and a multitude of dead-ends. This is the prevailing situation for many because for rare diseases expertise is limited and knowledge is scarce. Currently different initiatives to involve patients in developing clinical guidelines have been taken [ 1 ], however there is no common method that successfully integrates their experience and needs of living with a rare disease into development of healthcare services.
Even though listening to the expertise of a single patient is valuable and important, this will not resolve the uncertainties most rare disease patients are currently facing. To improve care for rare diseases we must draw on all the available knowledge, both from professional experts and patients, in order to improve care for every single patient in the world.
Patient experience and satisfaction have been demonstrated to be the single most important aspect in assessing the quality of healthcare [ 2 ], and has even been shown to be a predictor of survival rates [ 3 ]. Studies have evidenced that patient involvement in the design, evaluation and designation of healthcare services, improves the relevance and quality of the services, as well as improves their ability to meet patient needs [ 4 , 5 , 6 ]. Essentially, to be able to involve patients, the hurdles in communication and initial preconceptions between medical doctors and their patients need to be resolved [ 7 ].
To tackle the current hurdles in complex or rare diseases, European Reference Networks (ERN) have been implemented since March 2017. The goal of these networks is to connect experts across Europe, harnessing their collective experience and expertise, facilitating the knowledge to travel instead of the patient. ERN GENTURIS is the Network leading on genetic tumour risk syndromes (genturis), which are inherited disorders which strongly predispose to the development of tumours [ 8 ]. They share similar challenges: delay in diagnosis, lack of cancer prevention for patients and healthy relatives, and therapeutic. To overcome the hurdles every patient faces, ERN GENTURIS ( www.genturis.eu ) has developed an innovative visual approach for patient input into the Network, to share their expertise and experience: “Patient Journeys” (Fig. 1 ).
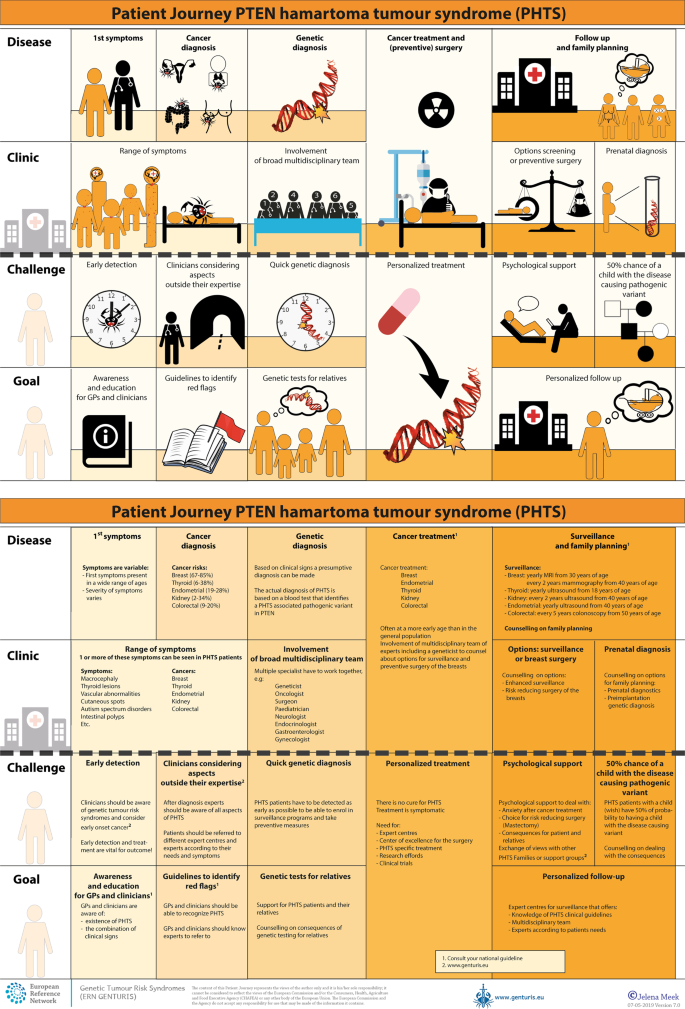
Example of a Patient Journey: PTEN Hamartoma Tumour Syndrome (also called Cowden Syndrome), including legend page ( www.genturis.eu )
The “Patient Journey” seeks to identify the needs that are common for all ‘ genturis syndromes ’, and those that are specific to individual syndromes. To achieve this, patient representatives completed a mapping exercise of the needs of each rare inherited syndrome they represent, across the different stages of the Patient Journey. The “Patient Journey” connects professional expert guidelines—with foreseen medical interventions, screening, treatment—with patient needs –both medical and psychological. Each “Patient Journey” is divided in several stages that are considered inherent to the specific disease. Each stage in the journey is referenced under three levels: clinical presentation, challenges and needs identified by patients, and their goal to improve care. The final Patient Journey is reviewed by both patients and professional experts. By visualizing this in a comprehensive manner, patients and their caregivers are able to discuss the individual needs of the patient, while keeping in mind the expertise of both professional and patient leads. Together they seek to achieve the same goal: improving care for every patient with a genetic tumour risk syndrome.
The Patient Journeys encourage experts to look into national guidelines. In addition, they identify a great need for evidence-based European guidelines, facilitating equal care to all rare patients. ERN GENTURIS has already developed Patient Journeys for the following rare diseases ( www.genturis.eu ):
PTEN hamartoma tumour syndrome (PHTS) (Fig. 1 )
Hereditary breast and ovarian cancer (HBOC)
Lynch syndrome
Neurofibromatosis Type 1
Neurofibromatosis Type 2
Schwannomatosis
A “Patient Journey” is a personal testimony that reflects the needs of patients in two key reference documents—an accessible visual overview, supported by a detailed information matrix. The journey shows in a comprehensive way the goals that are recognized by both patients and clinical experts. Therefore, it can be used by both these parties to explain the clinical pathway: professional experts can explain to newly identified patients how the clinical pathway generally looks like, whereas their patients can identify their specific needs within these pathways. Moreover, the Patient Journeys could serve as a guide for patients who may want to write, in collaboration with local clinicians, diaries of their journeys. Subsequently, these clinical diaries can be discussed with the clinician and patient representatives. Professionals coming across medical obstacles during the patient journey can contact professional experts in the ERN GENTURIS, while patients can contact the expert patient representatives from this ERN ( www.genturis.eu ). Finally, the “Patient Journeys” will be valuable in sharing knowledge with the clinical community as a whole.
Our aim is that medical doctors confronted with rare diseases, by using Patient Journeys, can also rely on the knowledge of the much broader community of expert professionals and expert patients.
Armstrong MJ, Mullins CD, Gronseth GS, Gagliardi AR. Recommendations for patient engagement in guideline development panels: a qualitative focus group study of guideline-naive patients. PloS ONE 2017;12:e0174329.
Article PubMed PubMed Central Google Scholar
Gupta D, Rodeghier M, Lis CG. Patient satisfaction with service quality as a predictor of survival outcomes in breast cancer. Supportive Care Cancer Off J Multinatl Assoc Supportive Care Cancer. 2014;22:129–34.
Google Scholar
Gupta D, Lis CG, Rodeghier M. Can patient experience with service quality predict survival in colorectal cancer? J Healthc Qual Off Publ Natl Assoc Healthc Qual. 2013;35:37–43.
Sharma AE, Knox M, Mleczko VL, Olayiwola JN. The impact of patient advisors on healthcare outcomes: a systematic review. BMC Health Serv Res. 2017;17:693.
Fonhus MS, Dalsbo TK, Johansen M, Fretheim A, Skirbekk H, Flottorp SA. Patient-mediated interventions to improve professional practice. Cochrane Database Syst Rev. 2018;9:Cd012472.
PubMed Google Scholar
Cornman DH, White CM. AHRQ methods for effective health care. Discerning the perception and impact of patients involved in evidence-based practice center key informant interviews. Rockville, MD: Agency for Healthcare Research and Quality (US); 2017.
Chalmers JD, Timothy A, Polverino E, Almagro M, Ruddy T, Powell P, et al. Patient participation in ERS guidelines and research projects: the EMBARC experience. Breathe (Sheff, Engl). 2017;13:194–207.
Article Google Scholar
Vos JR, Giepmans L, Rohl C, Geverink N, Hoogerbrugge N. Boosting care and knowledge about hereditary cancer: european reference network on genetic tumour risk syndromes. Fam Cancer 2019;18:281–4.
Article PubMed Google Scholar
Download references
Acknowledgements
This work is generated within the European Reference Network on Genetic Tumour Risk Syndromes – FPA No. 739547. The authors thank all ERN GENTURIS Members and patient representatives for their work on the Patient Journeys (see www.genturis.eu ).
Author information
Authors and affiliations.
SquareRootThinking and EURORDIS – Rare Diseases Europe, Paris, France
Matt Bolz-Johnson
Human Genetics, Radboud University Medical Center, Nijmegen, The Netherlands
Jelena Meek & Nicoline Hoogerbrugge
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Nicoline Hoogerbrugge .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Bolz-Johnson, M., Meek, J. & Hoogerbrugge, N. “Patient Journeys”: improving care by patient involvement. Eur J Hum Genet 28 , 141–143 (2020). https://doi.org/10.1038/s41431-019-0555-6
Download citation
Received : 07 August 2019
Revised : 04 October 2019
Accepted : 01 November 2019
Published : 04 December 2019
Issue Date : February 2020
DOI : https://doi.org/10.1038/s41431-019-0555-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Care trajectories of surgically treated patients with a prolactinoma: why did they opt for surgery.
- Victoria R. van Trigt
- Ingrid M. Zandbergen
- Nienke R. Biermasz
Pituitary (2023)
Designing rare disease care pathways in the Republic of Ireland: a co-operative model
- E. P. Treacy
Orphanet Journal of Rare Diseases (2022)
Rare disease education in Europe and beyond: time to act
- Birute Tumiene
- Harm Peters
- Gareth Baynam
Development of a patient journey map for people living with cervical dystonia
- Monika Benson
- Alberto Albanese
- Holm Graessner
Der klinische Versorgungspfad zur multiprofessionellen Versorgung seltener Erkrankungen in der Pädiatrie – Ergebnisse aus dem Projekt TRANSLATE-NAMSE
- Daniela Choukair
- Min Ae Lee-Kirsch
- Peter Burgard
Monatsschrift Kinderheilkunde (2022)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Open access
- Published: 31 August 2023
The hospital-to-home care transition experience of home care clients: an exploratory study using patient journey mapping
- Marianne Saragosa 1 , 2 ,
- Sonia Nizzer 2 ,
- Sandra McKay 2 , 3 , 4 , 5 , 6 &
- Kerry Kuluski 7 , 8
BMC Health Services Research volume 23 , Article number: 934 ( 2023 ) Cite this article
1801 Accesses
Metrics details
Care transitions have a significant impact on patient health outcomes and care experience. However, there is limited research on how clients receiving care in the home care sector experience the hospital-to-home transition. An essential strategy for improving client care and experience is through client engagement efforts. The study's aim was to provide insight into the care transition experiences and perspectives of home care clients and caregivers of those receiving home care who experienced a hospital admission and returned to home care services by thematically and illustratively mapping their collective journey.
This study applied a qualitative descriptive exploratory design using a patient journey mapping approach. Home care clients and their caregivers with a recent experience of a hospital discharge back to the community were recruited. A conventional inductive approach to analysis enabled the identification of categories and a collective patient journey map. Follow-up interviews supported the validation of the map.
Seven participants (five clients and two caregivers) participated in 11 interviews. Participants contributed to the production of a collective journey map and the following four categories and themes: (1) Touchpoints as interactions with the health system; Life is changing ; (2) Pain points as barriers in the health system: Sensing nobody is listening and Trying to find a good fit ; (3) Facilitators to positive care transitions: Developing relationships and gaining some continuity and Trying to advocate, and (4) Emotional impact: Having only so much emotional capacity .
Conclusions
The patient journey map enabled a collective illustration of the care transition depicted in touchpoints, pain points, enablers, and feelings experienced by home care recipients and their caregivers. Patient journey mapping offers an opportunity to acknowledge home care clients and their caregivers as critical to quality care delivery across the continuum.
Peer Review reports
In 2021 nearly 921,700 Canadian households reported accessing formal home care [ 1 ]. The general population uses home care services for various needs, such as recovery after hospital discharge, supporting end-of-life care, or managing chronic conditions, disabilities, or mental illnesses. Internationally, variations exist within and between countries in home care organization, policies, and availability of services [ 2 ], and targeted population groups within home care systems [ 3 , 4 ]. With the population aging and citizens living with disability, reliance on the home care system in combination with substantial care by unpaid caregivers enables people to live safely in their own homes. While most home care recipients (hereafter referred to as ‘client’) are 65 years and older, home care services are also provided to adults with long-term disabilities younger than 65 years [ 1 ].
Hospitalization and the period immediately following hospital discharge are particularly critical periods. The Canadian Institute for Health Information reports that 9.3% of patients discharged from the hospital are readmitted within 30 days [ 5 ]. Factors cited as predictors of readmission include hospital length of stay, patient acuity, and comorbidity [ 6 ]. Patient-reported challenges that arise during the hospital-to-home care transition require further exploration.
Understanding patient experience is important and is increasingly recognized as a quality measure, clinical effectiveness, and patient safety [ 7 ]. Patient experience is a multifaceted concept that spans a range of patient health setting/environment experiences, including lived and care experiences, clinical interactions, organizational features of care, and process measures [ 8 ]. Despite more attention on patient experience, it remains understudied in the formal home care sector [ 9 ]. The care transition experience in home care clients also requires more attention [ 10 ]. Client engagement efforts are an important strategy for improving client care and experience. Client engagement describes a partnership of clients, families, and health care professionals working together to improve the client experience [ 11 ]. Previous home care research has reported on client interest in direct care and care planning and less so on broader organizational improvement efforts [ 11 ]. However, through structured processes and engaging with older adults as experts in their lived experiences it is possible for community-dwelling service recipients to be partners in bettering health care services [ 12 ].
Journey mapping is a research approach that evolved from the market research industry to gain insight into how patients navigate and experience complex health services and systems [ 13 , 14 , 15 ]. As a “patient-oriented” activity, patient journey mapping is undertaken to understand the barriers, facilitators, experiences, and interactions with services or providers for those entering, navigating, and exiting a health system by documenting and producing an illustrated map [ 13 ]. Of the existing literature, patient journey mapping has been effectively used to understand the patient experience [ 16 , 17 , 18 ], improve the quality of care [ 7 , 19 ], and for informing health service redesign/improvement [ 13 , 15 , 20 ]. Journey maps go beyond a static view of patients' perspectives by illustrating key moments in a patient’s journey, including important touchpoints, pain points, and the emotions experienced [ 7 , 21 ]. For home care clients, mapping their journey from the hospital to home in a concise and visually compelling story may shed light on the multi-level barriers and challenges that they face, and has the potential to inspire new initiatives that improve the client experience. Using patient journey mapping, this study aimed to understand and characterize the care transition experiences for home care clients and unpaid caregivers after they transition from hospital to home with home care services. The objective of this study is to use patient journey mapping to characterize home care clients and caregivers’ experiences of home care services after transitioning from hospital to home.
Study design and setting
To achieve this aim, we used a qualitative descriptive exploratory design with a patient journey mapping approach. The study involved a large-scale not-for-profit charitable organization providing home care and support services in select Southern Ontario urban regions in Canada. For the purposes of this study, we recruited clients being served by the home care agency within one of the urban regions that provides both in-home personal and nursing care services. The Health Sciences Research Ethics Board of the University of Toronto (REB Human Protocol #31,494) provided ethics approval for this study.
Participants and data collection
We applied a purposeful sampling strategy using pre-determined selection criteria to identify and recruit potential participants. We approached clients if they met the following inclusion criteria: (1) recipient of home care services from the aforementioned organization during the study period; (2) experienced a hospital admission and transitioned back home with home care upon discharge in 2021; (3) living in the community (i.e., private home, retirement home or assisted living setting that offers support services to help maintain independence); (4) aged 18 or older; (5) ability to provide informed consent and communicate verbally; (6) were not receiving palliative care; and (7) the ability to communicate in conversational English. Similarly, caregivers could be involved if they could communicate in English and self-identify as unpaid or privately paid caregivers to a home care client who met the abovementioned inclusion criteria. Unpaid family and friend caregivers and privately paid caregiver supports were required to be working with older adults living independently in their home [ 22 ]. Caregivers were recruited after clients were enrolled in the study using the same targeted measures as clients. We targeted only clients who resumed home care services, given that this enabled us to identify and invite them to participate in the study.
Three recruitment strategies were used including: social media, digital, and mailout. First, the home care organization’s client digital newsletter promoted the study through an electronic post encouraging interested clients to contact the researcher. Second, a master list of clients that were previously admitted to hospital and resumed home care services between January 1, 2021, to November 15, 2021, was generated from the organization’s administrative database. A study invitation letter was sent to potential study participants either electronically or by mail using the master list of clients, depending on the availability of the email address on file, starting with the most recently documented hospital holds in November 2021. In keeping with previous literature on hospital-to-home transitions, the aim was to conduct initial interviews between two and four weeks post-discharge [ 23 ]. A longer timespan between hospital discharge and the first client interview (i.e., > 45 days) could negatively impact clients’ ability to recall events [ 24 ]. Prospective participants contacted the researcher via email or phone to share their interest in the study. Once it was determined that potential participants met the inclusion criteria, they received the consent form for their review by email and provided informed verbal consent prior to data collection.
The study team delineated two distinct data collection phases:
Phase 1: Initial interview : During the initial interview, the first author (MS) verbally collected demographic information and asked questions about the home—hospital—home care trajectory. Using a semi-structured interview guide, interview questions covered topics such as the precipitating factors to the care transition, what worked well and what was missing in terms of services and how care was delivered, and touchpoints with providers and services along the way. Examples of patient journey mapping interview guides were used to develop interview questions [ 13 , 25 , 26 ]. Further, the interview guide was piloted with a client partner with lived experience transitioning from hospital-to-home to ensure the questions were clear and relevant. As themes began to emerge during interviews, the semi-structured interview questions were modified using probing questions to gather more in-depth descriptions of emerging themes.
Phase 2: Follow-up interview : Interviews were analyzed after the first interview and findings from phase 1 were used to create a patient journey map. The same participants were then invited to participate in a follow-up interview to review the journey map [aggregated client-level data], validate its content, suggest changes, and discuss how challenges along their journey could be addressed. If they agreed to participate in the second interview, they received the draft patient journey map through email or mail beforehand.
Data analysis
Three of the initial participants were lost to follow-up resulting in eleven interviews, conducted from April 2022 to August 2022, which were audio recorded and transcribed verbatim. Interviews ranged from 46 to 108 min, with an average length of 52 min. Interview transcripts were analyzed iteratively using content and thematic analysis [ 27 ] to generate a collective patient journey map. We used an inductive 3-phase approach including: preparation (reading data thoroughly, immersion), organizing (open coding, developing a coding scheme, grouping the data), and reporting (generating themes reflected in the patient journey map and a conceptual understanding of the phenomenon) [ 27 ]. Members of the study team (MS, SN) with qualitative research and clinical experience worked together to develop a coding scheme by identifying broad open codes, such as “touch point,” “pain point,” “facilitator,” and “feelings.” The agreed upon coding scheme was used to analyze transcripts and develop a codebook with the broad codes and associated narratives. From this document, we developed the collective patient journey map. Further data grouping occurred, enabling us to identify overarching categories and themes from the clients’ and caregivers’ perspectives.
Strategies to increase the quality of our research process are collectively known as an assessment of trustworthiness and are encapsulated by the following three domains [ 28 , 29 ]. (1) Credibility techniques that were applied involved prolonged engagement with participants across two interviews, assessment of the researcher's own influence on the research process known as reflexivity, and member checking by sharing interpretations during follow-up interviews. (2) Dependability was enhanced by following an analytical plan and having multiple coders. (3) Credibility is grounded in a team of expert researchers in qualitative methods, home care delivery, and patient engagement, who frequently met to discuss the data and emerging insights.
A total of seven participants (five home care clients and two caregivers of individuals receiving home care) completed seven initial interviews, and four completed a follow-up interview for a total of 11 interviews (Table 1 ). Most participants identified as female (n = 5) and were on average 66 years of age (range 44 to 88 years). Caregivers (n = 2) identified as a spouse and a paid private caregiver, with neither providing respite care.
Participants were engaged in the production of a collective journey map (Fig. 1 ). The following four categories and themes emerged as key experiences in participants’ journey transitioning from hospital-to-home: (1) Touchpoints; Life is changing ; (2) Pain points: Sensing nobody is listening and trying to find a good fit ; (3) Facilitators: Developing relationships gaining some continuity, and trying to advocate, and (4) Emotional impact: Having only so much emotional capacity .
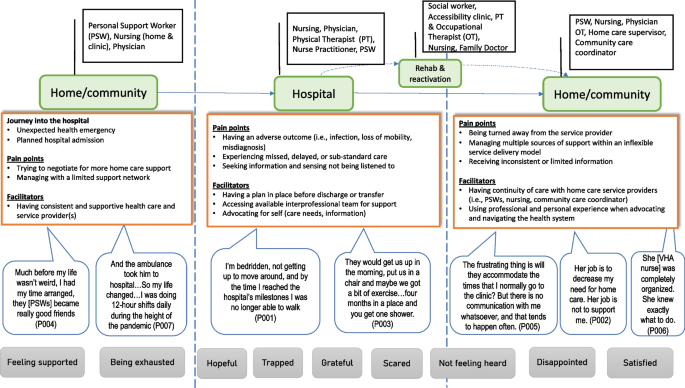
Illustration depicting the collective journey map
Touchpoints as interactions with the health system – Life is changing
Participants described service touchpoints experienced by home care clients as they transitioned from hospital to home. Participant narratives highlight the complexity of the care transitions, including the variety of providers and multiple sectors involved. Participant 6 described:
“ A podiatrist told me the condition of my right foot did not look good and that I should probably go in to emerge and have them do an assessment. I did do that, and I wound up being admitted to the hospital, and within a couple of days, they did a partial amputation on my right foot. Then I was admitted to rehab for a two-week stay .” (P006)
Experiences of health system touchpoints were also described by participant 004 as:
“ After 2 months of Rehab I realized if I had to do long-term care, I could but I didn’t want to, it was that simple if I could get support at home then I would, so the discharge planner started to work on how to get him support and how many times a day we would need it and that’s how we ended up with multiple agencies because we need 4 times a day .” (P004)
While most participants described the hospitalizations as unplanned, acute situations, two individuals had planned surgeries. Regardless of the context for admission, many participants often noted that exacerbations of chronic conditions or an acute episode of illness had a life-altering impact on them or the person they cared for. For this reason, participants left the hospital setting with greater intensity in care needs than before admission. For example, one participant described the significant physical decline in coping with a hospital-acquired infection, while another explicitly noted how life had changed for her and her husband after hospital admission in an increase in touchpoints, mainly because of the pandemic,
“ We have three agencies so our life is really coo-coo compared to then when it was all just one agency and one coordinator and if you needed something special you knew exactly who to call like if you had a dental appointment you knew who to call for extra support on this day, can move this hour to here it was fine, things were more flexible.” (P004)
Pain points as barriers in the health system
Pain points were described as critical moments that hindered quality care transitions from the participants' perspective. Two themes emerged as Sensing nobody is listening and Trying to find a good fit and were discussed as communication and care coordination challenges.
Sensing nobody is listening
Several participants observed that their opinions about their treatment plan went unnoticed by the health care providers. In some cases, not being heard contributed to patient harm, including adverse outcomes and missed or delayed care. The harmful events included losing mobility and continence due to bed restrictions post-surgery, hospital-acquired infection, and a procedure-related incident. Participant 001 described feeling unheard as:
“ It was supposed to be an overnight stay, and then go home, stay overnight, one or two nights, I’ll be fine and ready to go home. It didn't turn out that way because the hospital insisted on reaching a few milestones that my body wasn't ready for, like being able to go to the toilet on my own, instead of relying on a catheter, and that takes a few days, so I’m bedridden, not getting up to move around and not getting any exercise, and by the time I reached the hospital's milestones I was no longer able to walk .” (P001) “After a week he was in the hospital, maybe 10 days after, the doctor said, ‘I want to take out the stitches now.’ And I said, ‘I know [name], and I feel that maybe we could just wait a little bit.’ ‘So no. I'm taking them out. And I'm the doctor. You're not.’ So he took the stitches out and left the room, and then there were loops of small bowel coming out of the hole…So they had to rush him up to the emergency and do another operation. So that delayed everything.” (P007)
Many participants described instances of emotional harm in the case of not receiving clear communication from health care providers and feeling frustrated and unsupported. One participant reported this experience as receiving “different stories” (P002) depending on whom you spoke to, while another individual said fragmented communication between a hospital clinic and a community provider about her leg dressing left her “removed from the situation” noted in the following quote:
“ It's probably almost like being back in high school. That's sometimes how I feel, to be honest, a couple of times I've left there in tears because it's just like nobody is listening to me. Nobody is listening to what I need. And I'm going home, and it's [leg wound] leaking all over my floor and it's frustrating not to have that communication piece. It's just like I'm there, and it doesn't matter what my experience is .” (P005)
Trying to find a good fit
Most participants noted the absence of continuity of care among home care providers as a pain point when they transitioned home from the hospital. This transpired for home care clients who required more home care hours upon discharge, which could no longer be accommodated by one service provider alone. Service coverage by multiple home care agencies had participants trying to find “a good fit” (P002) as they had to coordinate not only fluctuating schedules but different home care workers and communication practices:
“ There's a definite ‘Oh, my God, here we go again, training new people.’ And we've had it throughout the year, something's happened to somebody and they've gone. And then we start with somebody new. We have not been able to get consistent care in the evening since he left. This morning, I just got a call that one of the other—that’s now the fifth agency, believe it or not, is saying they could try and pick it up in the evening and for me to call them and see what we can work out .” (P004)
The changing service providers impacted the clients and caregivers, who often noted that they had to “train” the incoming staff about their or the person they care for personal needs. A new home care provider for some is like “starting from scratch” (P002), which has become more problematic because of COVID-19 and workforce shortages in health care:
“ The agency that was doing my PSW [personal support worker] care could not, at that time, provide me with the service, so I had to start with a new home care agency so the PSWs switched. Again, starting with new people and a new agency and retraining and trying to find a good fit. The biggest barriers have been with the agency and starting from scratch .” (P002)
For one participant, to maintain a consistent PSW and comfort with care, the client chose to remain in her bed for 20 h to accommodate this worker’s schedule and explained her rationale for this decision in the following quote:
“ I stay in bed from 5:00 at night to 1:00 in the afternoon every Thursday, so that kind of sucks, but nobody can do anything about it. I have a PSW coming at different hours every day and if I want the same PSW she is not available until 1 in the afternoon. It's better for me to have the same PSW because it gets exhausting to remind them to do everything .” (P001)
Facilitators to positive care transitions
Facilitators are positive system and client-level factors that helped to support the transition and the adjustment to being home. This theme comprises two sub-themes that consider the importance of relationships and advocacy for quality care transitions.
Developing relationships and gaining some continuity
Many participants described existing relationships with home care providers as tight-knit bonds that strengthened over time. As such, these relationships were central to their care transition journey because the home care providers knew them well, including their baseline functioning, family, and household, and were often a driving force behind changes to the service plan. These longer-term relationships also enabled providers to flag medical inconsistencies among clients. For example, continuity of care in home care nursing resulted in an escalation in care because of a client’s deteriorating symptoms according to one participant,
“ She sent me back to the hospital when I was in A-fib (heart arrhythmia) because she knew what my normal was and she knew that this was not normal .” (P002)
The continuity of care in service providers has also acted as a safety net for other participants who rely on one or more key people to help coordinate and deliver care in the community. One participant described an extensive network of providers: the community care coordinator, a home care supervisor, an interdisciplinary primary care program, and a personal support worker. Collectively, this team has enabled her and her husband to stay at home safely as they age.
“ I have to say that the home care supervisor has been so caring, and she's done everything that you can to get the time that we've been allotted by the care coordinator, and all it did was just reconfirmed to us that we were not going to go into an institution and that we are staying home .” (P003)
Trying to advocate
All the participants reported being an advocate for themselves or the person they care for as a facilitator for a better transition experience. Advocating appeared to express their needs and requests firmly, and when supporting the participants drew from their professional skills or previous care transitions. For example, one participant managed to secure a transfer to an inpatient rehabilitation facility for additional physical therapy. Once she realized that her prior home care agency could not support her service plan, she called the home care supervisor at that agency directly.
“ I think I kind of felt that the squeaky wheel gets the worm, so to be turned away from the home care agency after having been with them for 5 years, it just floored me and scared me. To be told ‘no’ I think that was the social worker that told me, so I had to say to her ‘Hello, can you re-visit that and see if I can get back in? Rather than relying on the social worker, I phoned directly to the home care agency and spoke to my coordinator who used to schedule me. ” (P001)
Advocating for respite care through home care by one caregiver participant did not result in a service change and instead created frustration and tension for this individual. According to this participant, despite phone calls, letter writing, and an in-person meeting with the community care coordinator, their needs went unheard, and an escalation in the advocacy process seemed to be justified in this case noted in the following example,
“ So I feel I walk with integrity, and I feel she [community care coordinator] needs a wake-up call. And I will facilitate that. And it may be 20 pages, but I don't care. I've got nothing to lose. I don't care right now in my life. I will just push and push and push and push, and I'll say, ‘Well, then, I'll go to your ombudsman then. Because if you're not going to cooperate with the care plan and support me with [name’s] care, I want to make sure that everyone in the industry knows it. " (P007)
Emotional impact
The final category of feelings is framed by the theme, Having only so much emotional capacity to illustrate the emotional impact of these care transitions on clients and caregivers.
Having only so much emotional capacity
The participants described a mixture of primarily negative feelings when faced with unexpected challenges related to hospitalization and transition back to the community. When hospitalized, several participants felt “trapped” (P001) and “scared,” and “helpless” (P003) because of their lack of control over their situation. Once discharged from the hospital, certain feelings persisted. For example, one person expressed feeling worried about the availability of care to meet a future need based on prior experiences when,
“ My coordinator is coming out next week and because every 90 days I’m supposed to be assessed and that’s the opportunity to get support, but really her job is to decrease my need for home care…I worry because I'm due for another hospitalization to have that surgery. And I know that I'm going to come home needing more service, and I'm worried I'm not going to get it .” (P002)
In another example, the participant called out feeling “diminished” and “worthless” when their request for an extra hour of personal support for respite went unheeded by the community care coordinator. In turn, this individual felt “taken for granted” rather than validated after many years of providing private caregiving service to a mother-son dyad,
“ So when you've been told three times in a row, ‘You're not going to get that extra hour,’ for me, it diminishes all my 27 years of work. ‘Well, I'm worthless.’ I have to go through those emotions .” (P007)
When participants expressed positive emotions of feeling “respected” and “appreciated,” they described the enabling factors as sensing that the providers were invested in their care and wellbeing, having their questions answered and listened to, and being engaged in critical discussions by the providers. These positive excerpts indicated that these participants perceived quality care being delivered and the presence of an adequate level of support to meet their complex care needs.
“ She [physiatrist] doesn't miss a thing. She is very attentive. Will explain things in detail. When she admitted me to Rehab for the two-week stay, my wife nicknamed her St. Name…Because my wife was at her wit’s end trying to figure out what to do. And, uh the doctor basically took that out of her hands and took over .” (P006)
This study provides an overarching illustration of the patient journey of home care recipients from hospitalization to the return to the community and resumed home care service. The findings offer insights into the touchpoints, pain points, facilitators, and feelings experienced and perceived by these clients regarding their journey. We derived categories and themes from our data that highlighted issues with communication and continuity of care. All participants identified factors that mitigated negative transition experiences, such as relying on long-standing relationships and advocating for themselves. The findings contribute to the focus on the care transition needs of home care clients and the optimization of a more integrated health system.
In many countries worldwide, patients receiving home care services typically live with comorbid conditions, with high functional and cognitive impairment rates [ 30 , 31 , 32 ]. Sinn and colleagues observed that in Ontario, Canada, 7.3% of patients died, 16.6% were hospitalized, and 44.4% visited the emergency department within 90 days of being admitted to home care [ 30 ]. Unsurprisingly, most of the participants in our study had hospitalizations that resulted in significant functional decline and hospital-acquired infection. In this context, individuals leave the hospital with higher medical complexities, and they or their family members receiving home care require additional support to remain in their own homes. Our finding supports previous studies that describe the post-discharge period as a vulnerable time for these patients [ 33 , 34 ]. More specifically, adaptation to life after the hospital is experienced as challenging when health problems compound daily activities such as laundry, meal preparation, and meeting basic needs like toileting [ 33 ].
During their transition journey, participants reported not feeling listened to and having limited information about their treatment and discharge plan while navigating between hospital-to-home. In a few cases, patients experienced harm that could have been prevented including loss of mobility, hospital-acquired infection, functional decline, and emotional damage. Further, adverse health outcomes contributed to delayed discharge from the hospital, resulting in additional usage of health care resources upon return home.
Hospital-based patient harm remains an ongoing issue. In Canada in 2021/22, 5.8% of patients experienced hospital harm during acute hospital admission [ 35 ]. Internationally, the pooled rate of hospital harm is 6% of patients across medical settings [ 36 ]. These findings are consistent with other research on communication failures between patients and health care providers [ 37 ] and the experience and impacts of hospital-based patient harm [ 38 ]. Similar to our findings, patient-provider miscommunication is often identified as a quality and safety concern by patients even without an adverse event [ 37 ]. Participants’ experiences of feeling unheard is detrimental, regardless if negative health outcomes or physical harm is caused.
Participants experienced challenges with the continuity of home care service providers, namely PSWs, once discharged home. The challenge stemmed from workforce constraints that resulted in either the home care organization being unable to resume service or the client needing assistance from multiple agencies to meet higher care demands. As a result of COVID-19, home care agencies faced extreme challenges in providing high-quality, in-home client care, including the adoption of virtual care use. The home care sector also experienced personal protective equipment shortages and staffing constraints caused by COVID-19 infection [ 39 , 40 ]. These issues are compounded by unprecedented home and community care staffing shortages observed in a tripling of staff vacancies—a 331% increase in PSW openings from 2020 to 2021 [ 41 ]. Our findings show that home care clients not only value and desire consistency in home care service providers, but they also make sacrifices to achieve consistency in care. Despite critical issues of delivering continuity of care, there is limited literature exploring challenges of scheduling consistency for PSWs in home care delivery and pressures this causes for delivering high-quality care [ 10 , 42 ]. Other research has detailed the importance of consistent PSWs in building trusting relationships with clients and families and delivering tailored care to match client needs and preferences [ 10 , 43 ]. In our study, patients receiving homecare and their family caregivers described relational continuity with home care providers as an enabler of quality transitions. Participants also discussed continuity of care from home and community care workers prevented harm and contributed to a safety net in the community. The linkage between quality home care and continuity of care in the literature [ 44 ], and broadly speaking, relational continuity in health care has led to more effective and efficient diagnosis and management of health problems and a means of building patient trust [ 45 ]. In our study we found that when established home care services were disrupted by planned or unplanned hospitalizations and homecare was resumed, the disruption in relational continuity was destabilizing for clients and caregivers and may contribute to potential safety issues.
Both client and caregiver participants addressed needing to speak up for themselves when their needs went unmet. Across all participants, they leveraged their professional expertise or previous transition experiences to self-advocate. Advocating is a strategy for patients and families to engage in the care experience meaningfully. By doing so, they can make informed decisions, communicate effectively with providers, and build strong connections with others [ 46 ]. Our findings contributes evidence that confirms other research on advocacy [ 47 ]. Yet, uniquely these authors describe “growth” in families' ability to engage in “assertive advocacy” that allowed for collaborative partnerships rather than mistrust and conflict.
Our study has several important implications. Addressing improved patient-provider communication, the transitions warrant greater attention. Although this is not a novel finding, communication improvements could be considered through an integrated care lens. Opportunities exist in the home and community care sector to identify innovative, evidence-based practices that could enhance the continuity of care. One example is the renewed focus on health care co-production, which includes patients and families as influential members of the health care teams at all levels of service delivery—system, organizational, and one-on-one [ 48 ]. Home care offers ideal conditions for fostering participation in health care co-production, given that relational continuity, interprofessional collaboration, and client desire in the direct care and care planning [ 11 ]. Research findings also revealed that scarcity of resources may have led to clients facing trade-offs in quality of care owing to concerns around consistency in care. This is an important finding as it contributes to our understanding of client-provider partnerships to maintain treatment preference and client safety. Furthermore, our study contributes to the patient journey mapping body of literature in two ways. First, it highlights the complexity of health care navigation experiences from the viewpoint of clients and caregivers, including areas of improvement. There is a clear need to optimize coordination and collaboration within and between sectors. A scoping review identified that interaction and communication between health care providers were key contributors to optimizing home care [ 49 ]. Second, our patient journey mapping approach via interview and follow-up interview provided a mechanism for participants to review and comment on the collective journey map. This could be an opportunity for further co-designing with end-users on targeted action that aligns with the care recipients' needs.
Limitations
Our study has several limitations for consideration. While providing rich narrative data, findings from our study must consider the limitation of generalizing results to other populations and settings. However, our research has the potential value to be transferable whereby readers can discern the extent to which the findings are similar and different to their own situations [ 50 ]. Additionally, the number of participants that self-identified as interested in participating in the study was limited, and therefore the number of participants resulted in a small sample size of seven participants. Although guidelines on adequate sample size for patient journey mapping do not exist, studies commonly cite larger sample sizes as ten or more participants [ 13 ]. In contrast, research using patient journey mapping with large samples of hospital staff reported limitations from not gathering information from the perspectives of those with lived experience [ 51 ]. Participants in this study were homogenous, and a lack of diversity among study participants is a limitation. A more diverse sample such as participants from marginalized communities that do not speak English may provide more diverse experiences and lead to more generalizable findings. For example, research has shown that racism and racialization intersect with other aspects of identity and social determinants of health, including sexism, ageism, and ableism, to name a few [ 52 ]. We also acknowledge the potential for self-selection bias among participants, including those who cannot effectively advocate for a quality care transition and may have been excluded. Despite a homogenous small sample size, our study is strengthened by gathering rich descriptions of the lived experiences of home care clients and their care partners. Another area for improvement is how we captured the care transition journey itself. Participants were asked about the hospital discharge during the 2021 period; however, many also drew on other health care transition experiences, which may have led to a blurring interpretation. This flexible approach supports how patients and caregivers view their care transition experiences – not as discrete events but as a compilation of ongoing, intersecting transitional experiences.
Our study provided insight into the hospital-to-home care transition experiences and perspectives of home care clients and their caregivers by mapping their collective journey. The patient journey map enabled a collective illustration of the care transition depicted in their touchpoints, pain points, feelings, and findings that can help identify potential improvement areas. Patient journey mapping offers an opportunity to demonstrate how care is experienced and acknowledges home care clients and their caregivers as critical partners that need to be involved in care delivery across the continuum.
Availability of data and materials
The dataset analyzed for the current study is not publicly available due to confidentiality guaranteed to the participants. However, data are available from the authors upon reasonable request, conditioned by the REB and participants' permission. If someone wants to request the data from this study, please contact the corresponding author, Marianne Saragosa, [email protected].
Abbreviations
Personal support
Personal support worker
Statistics Canada. Home care use and unmet home care needs in Canada, 2021 2022 [Available from: https://www150.statcan.gc.ca/n1/daily-quotidien/220826/dq220826a-eng.htm .
Genet N, Boerma WG, Kringos DS, Bouman A, Francke AL, Fagerström C, et al. Home care in Europe: a systematic literature review. BMC Health Serv Res. 2011;11:1–14.
Article Google Scholar
Voie KS, Blix BH, Helgesen AK, Larsen TA, Maehre KS. Professional home care providers' conceptualisations of frailty in the context of home care: A focus group study. Int J Older People Nurs. 2023;18(1):1–10.
Article PubMed Google Scholar
van der Roest HG, van Eenoo L, van Lier LI, Onder G, Garms-Homolová V, Smit JH, et al. Development of a novel benchmark method to identify and characterize best practices in home care across six European countries: design, baseline, and rationale of the IBenC project. BMC Health Serv Res. 2019;19:1–11.
Google Scholar
Canadian Institute for Health Information. 2020–2021: Patients urgently readmitted to hospital within 30 days of discharge (Percentage) 2022 [Available from: https://yourhealthsystem.cihi.ca/hsp/inbrief.#!/indicators/006/all-patients-readmitted-to-hospital/;mapC1;mapLevel2;provinceC5001;trend(C1,C5001 );/.
Van Walraven C, Dhalla IA, Bell C, Etchells E, Stiell IG, Zarnke K, et al. Derivation and validation of an index to predict early death or unplanned readmission after discharge from hospital to the community. CMAJ. 2010;182(6):551–7.
Article PubMed PubMed Central Google Scholar
McCarthy S, O’Raghallaigh P, Woodworth S, Lim YL, Kenny LC, Adam F. An integrated patient journey mapping tool for embedding quality in healthcare service reform. J Decis Syst. 2016;25(sup1):354–68.
Wolf PhDC, Jason A. Defining patient experience. Patient Exp J. 2014;1(1):7–19.
Lines LM, Anderson WL, Blackmon BD, Pronier CR, Allen RW, Kenyon AE. Qualitative analysis and conceptual mapping of patient experiences in home health care. Home Health Care Serv Q. 2018;37(1):25–40.
Saragosa M, Jeffs L, Okrainec K, Kuluski K. Towards defining quality in home care for persons living with dementia. PLoS ONE. 2022;17(9): e0274269.
Article CAS PubMed PubMed Central Google Scholar
Kirst M, Elmi A, Ray-Daniels M, Foster J, editors. Client engagement in home and community care services: The client and care coordinator perspective. Healthcare Management Forum; 2016: SAGE Publications Sage CA: Los Angeles, CA.
Hulko W, Mirza N, Seeley L. Older adults’ views on the repositioning of primary and community care. Can J Aging/La Revue Canadienne Du Vieillissement. 2021;40(1):114–26.
Davies EL, Bulto LN, Walsh A, Pollock D, Langton VM, Laing RE, et al. Reporting and conducting patient journey mapping research in healthcare: A scoping review. J Adv Nurs. 2022.
Crosier A, Handford A. Customer journey mapping as an advocacy tool for disabled people: A case study. Soc Mark Q. 2012;18(1):67–76.
Ly S, Runacres F, Poon P. Journey mapping as a novel approach to healthcare: a qualitative mixed methods study in palliative care. BMC Health Serv Res. 2021;21(1):1–9.
Schouten B, Driesen BE, Merten H, Burger BH, Hartjes MG, Nanayakkara PW, et al. Experiences and perspectives of older patients with a return visit to the emergency department within 30 days: patient journey mapping. Eur Geriatr Med. 2021:1–12.
de Ridder EF, Dekkers T, Porsius JT, Kraan G, Melles M. The perioperative patient experience of hand and wrist surgical patients: an exploratory study using patient journey mapping. Patient Exp J. 2018;5(3):97–107.
Ramamoorthi K, Liu R, Fujioka J, Rathod P, Rosart J, Desveaux L, et al. Navigating Virtual Care Services in Ontario Urban Hospitals, Using Patient Journey Mapping. J Patient Exp. 2023;10:23743735231179060.
Fraser S, Mackean T, Grant J, Hunter K, Ryder C, Kelly J, et al. Patient journey mapping to investigate quality and cultural safety in burn care for Aboriginal and Torres Strait Islander children and families–development, application and implications. BMC Health Serv Res. 2022;22(1):1–13.
Kushniruk AW, Borycki EM, Parush A. A case study of patient journey mapping to identify gaps in healthcare: Learning from experience with cancer diagnosis and treatment. Knowledge Manage E Learn. 2020;12(4):405.
Trebble TM, Hansi N, Hydes T, Smith MA, Baker M. Process mapping the patient journey: an introduction. Bmj. 2010;341:394–401.
Carpentier N, Grenier A. Successful linkage between formal and informal care systems: The mobilization of outside help by caregivers of persons with Alzheimer’s disease. Qual Health Res. 2012;22(10):1330–44.
Byrne K, Orange JB, Ward-Griffin C. Care transition experiences of spousal caregivers: from a geriatric rehabilitation unit to home. Qual Health Res. 2011;21(10):1371–87.
Foust JB, Vuckovic N, Henriquez E. Hospital to home health care transition: patient, caregiver, and clinician perspectives. West J Nurs Res. 2012;34(2):194–212.
Hainstock T, Cloutier D, Penning M. From home to ‘home’: Mapping the caregiver journey in the transition from home care into residential care. J Aging Stud. 2017;43:32–9.
Madathil SC, Lopes AJ, Alfred M, editors. Patient Journey Mapping: A Literature Review. IIE Annual Conference Proceedings; 2020: Institute of Industrial and Systems Engineers (IISE).
Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88.
Morse JM. Critical analysis of strategies for determining rigor in qualitative inquiry. Qual Health Res. 2015;25(9):1212–22.
Krefting L. Rigor in qualitative research: The assessment of trustworthiness. Am J Occup Ther. 1991;45(3):214–22.
Article CAS PubMed Google Scholar
Sinn C-LJ, Heckman G, Poss JW, Onder G, Vetrano DL, Hirdes J. A comparison of 3 frailty measures and adverse outcomes in the intake home care population: a retrospective cohort study. CMAJ Open . 2020;8(4):E796-E809.
Schneider J, Algharably EAE, Budnick A, Wenzel A, Dräger D, Kreutz R. High prevalence of multimorbidity and polypharmacy in elderly patients with chronic pain receiving home care are associated with multiple medication-related problems. Front Pharmacol. 2021;12: 686990.
Rijken M, Hujala A, van Ginneken E, Melchiorre MG, Groenewegen P, Schellevis F. Managing multimorbidity: profiles of integrated care approaches targeting people with multiple chronic conditions in Europe. Health Policy. 2018;122(1):44–52.
Hestevik CH, Molin M, Debesay J, Bergland A, Bye A. Older persons’ experiences of adapting to daily life at home after hospital discharge: a qualitative metasummary. BMC Health Serv Res. 2019;19(1):1–13.
Romagnoli KM, Handler SM, Ligons FM, Hochheiser H. Home-care nurses’ perceptions of unmet information needs and communication difficulties of older patients in the immediate post-hospital discharge period. BMJ Qual Saf. 2013;22(4):324–32.
Canadian Institute for Health Information. Patient harm in Canadian hospitals? It does happen. 2022 [cited 2022 December 5]. Available from: https://www.cihi.ca/en/patient-harm-in-canadian-hospitals-it-does-happen .
Panagioti M, Khan K, Keers RN, Abuzour A, Phipps D, Kontopantelis E, et al. Prevalence, severity, and nature of preventable patient harm across medical care settings: systematic review and meta-analysis. bmj. 2019;366:1–11.
Harrison R, Walton M, Manias E, Smith-Merry J, Kelly P, Iedema R, et al. The missing evidence: a systematic review of patients’ experiences of adverse events in health care. Int J Qual Health Care. 2015;27(6):424–42.
Guilcher SJ, Everall AC, Cadel L, Li J, Kuluski K. A qualitative study exploring the lived experiences of deconditioning in hospital in Ontario. Canada BMC Geriatr. 2021;21(1):1–9.
Jones CD, Bowles KH. Emerging challenges and opportunities for home health care in the time of COVID-19. J Am Med Dir Assoc. 2020;21(11):1517–8.
Seshadri S, Concannon C, Woods JA, McCullough KM, Dumyati GK. “It’s like fighting a war with rocks”: Nursing home healthcare workers’ experiences during the COVID-19 pandemic. Infect Control Hosp Epidemiol. 2021;42(8):1020–1.
Ontario Community Support Association. Staffing crisis threatens home and community care sector with 421% increase in vacant RN positions and 331% increase in vacant PSW positions 2022 [Available from: https://www.ocsa.on.ca/staffing-crisis-threatens-home-and-community-care-sector-with-421-increase-in-vacant-rn-positions-and-331-increase-in-vacant-psw-positions .
Breen R, Savundranayagam MY, Orange JB, Kothari A. Quality home care for persons living with dementia: Personal support workers’ perspectives in Ontario, Canada. Health Soc Care Commun. 2022;30(5):e2497–506.
Nizzer S, Ryan S, McKay SM. The little things: Exploring perceptions and experiences of client and family-centred care through photovoice. Patient Exp J. 2020;7(1):31–43.
Aase I, Ree E, Johannessen T, Strømme T, Ullebust B, Holen-Rabbersvik E, et al. Talking about quality: how ‘quality’is conceptualized in nursing homes and homecare. BMC Health Serv Res. 2021;21(1):1–12.
Guthrie B, Wyke S. Access and continuity in UK general practice: a qualitative study of general practitioners’ and patients’ perceptions of when and how they matter. BMC Fam Pract. 2006;7(11):11.
Thomas TH, Murray PJ, Rosenzweig M, Taylor S, Brufsky A, Bender C, Schenker Y. I was never one of those people who just jumped right in for me”: patient perspectives on self-advocacy training for women with advanced cancer. Supportive Care Cancer. 2023;31(1):96.
Walmsley BD, McCormack L. Dementia families: Relinquishing home care to aged care services: Guilt, traumatic loss and growth. Dementia. 2021;20(5):1814–31.
Palumbo R. Contextualizing co-production of health care: a systematic literature review. Int J Pub Sector Mgmt. 2016;29(1):72
Ganann R, Weeres A, Lam A, Chung H, Valaitis R. Optimization of home care nurses in Canada: a scoping review. Health Soc Care Commun. 2019;27(5):e604–21.
Smith B. Generalizability in qualitative research: Misunderstandings, opportunities and recommendations for the sport and exercise sciences. Qualitative Res Sport Exerc Health. 2018;10(1):137–49.
Wolff JC, Maron M, Chou T, Hood E, Sodano S, Cheek S, et al. Experiences of child and adolescent psychiatric patients boarding in the emergency department from staff perspectives: patient journey mapping. Admin Policy Mental Health Mental Health Serv Res. 2023;50(3):417–26.
Hassen N, Lofters A, Michael S, Mall A, Pinto AD, Rackal J. Implementing anti-racism interventions in healthcare settings: a scoping review. Int J Environ Res Public Health. 2021;18(6):2993.
Download references
Acknowledgements
We thank the participants who contributed their time and stories to our study. We would also like to acknowledge the support of Emmelie Mohammed, who assisted with recruitment efforts.
Funding from the CIHR Health System Impact Fellowship (RN447323—460820) generously supported this study.
Author information
Authors and affiliations.
Lunenfeld-Tanenbaum Research Institute, Sinai Health System, 1 Bridgepoint Drive, Toronto, ON, M4M 2B5, Canada
Marianne Saragosa
VHA Home HealthCare, Toronto, ON, Canada
Marianne Saragosa, Sonia Nizzer & Sandra McKay
Department of Physical Therapy, University of Toronto, Toronto, ON, Canada
Sandra McKay
Ted Rogers School of Management, Toronto Metropolitan University, Toronto, ON, Canada
The Institute for Education Research, University Health Network, Toronto, ON, Canada
Michael Garron Hospital, Toronto East Health Network, East York, Toronto, ON, Canada
Trillium Health Partners, Mississauga, ON, Canada
Kerry Kuluski
Institute of Health Policy, Management and Evaluation, University of Toronto, Toronto, ON, Canada
You can also search for this author in PubMed Google Scholar
Contributions
MS, SM, and KK conceived of the study. MS collected and analyzed the data and wrote the draft of the paper. SN analyzed the data and provided comments on the drafts of the paper. MS prepared the illustrative figure. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Marianne Saragosa .
Ethics declarations
Ethics approval and consent to participate.
The Ethical Review Board of the University of Toronto approved this study. All participants signed informed consent forms before participating in the study. All methods were carried out in strict accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Saragosa, M., Nizzer, S., McKay, S. et al. The hospital-to-home care transition experience of home care clients: an exploratory study using patient journey mapping. BMC Health Serv Res 23 , 934 (2023). https://doi.org/10.1186/s12913-023-09899-2
Download citation
Received : 06 January 2023
Accepted : 10 August 2023
Published : 31 August 2023
DOI : https://doi.org/10.1186/s12913-023-09899-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Care transition
- Journey mapping
- Patient experience
- Caregiver experience
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Breast cancer patient experiences through a journey map: A qualitative study
Roles Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Clinical Psychology and Psychobiology Department, Faculty of Psychology, University of Barcelona, Barcelona, Spain
Roles Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing
Affiliation Medical Oncology Department Hospital Universitario Central of Asturias, Oviedo, Spain
Roles Resources, Validation, Writing – review & editing
Affiliation Social Psychology and Quantitative Psychology Department, Faculty of Psychology, University of Barcelona, Barcelona, Spain
Affiliation Medical Oncology Department, Hospital Universitario Clínico San Carlos, Madrid, Spain
Affiliation Medical Oncology Department, Complexo Hospitalario Universitario de Ourense, Ourense, Spain
Affiliation Medical Oncology Department, Hospital Universitario La Paz, Madrid, Spain
Affiliation Medical Oncology Department, Hospital General Universitario de Elche, Elche, Spain
Affiliation Medical Oncology Department, Hospital Universitario Fundación Alcorcón, Madrid, Spain
Roles Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing
- Laura Ciria-Suarez,
- Paula Jiménez-Fonseca,
- María Palacín-Lois,
- Mónica Antoñanzas-Basa,
- Ana Fernández-Montes,
- Aranzazu Manzano-Fernández,
- Beatriz Castelo,
- Elena Asensio-Martínez,
- Susana Hernando-Polo,
- Caterina Calderon

- Published: September 22, 2021
- https://doi.org/10.1371/journal.pone.0257680
- Reader Comments
Registered Report Protocol
21 Dec 2020: Ciria-Suarez L, Jiménez-Fonseca P, Palacín-Lois M, Antoñanzas-Basa M, Férnández-Montes A, et al. (2020) Ascertaining breast cancer patient experiences through a journey map: A qualitative study protocol. PLOS ONE 15(12): e0244355. https://doi.org/10.1371/journal.pone.0244355 View registered report protocol
Breast cancer is one of the most prevalent diseases in women. Prevention and treatments have lowered mortality; nevertheless, the impact of the diagnosis and treatment continue to impact all aspects of patients’ lives (physical, emotional, cognitive, social, and spiritual).
This study seeks to explore the experiences of the different stages women with breast cancer go through by means of a patient journey.
This is a qualitative study in which 21 women with breast cancer or survivors were interviewed. Participants were recruited at 9 large hospitals in Spain and intentional sampling methods were applied. Data were collected using a semi-structured interview that was elaborated with the help of medical oncologists, nurses, and psycho-oncologists. Data were processed by adopting a thematic analysis approach.
The diagnosis and treatment of breast cancer entails a radical change in patients’ day-to-day that linger in the mid-term. Seven stages have been defined that correspond to the different medical processes: diagnosis/unmasking stage, surgery/cleaning out, chemotherapy/loss of identity, radiotherapy/transition to normality, follow-up care/the “new” day-to-day, relapse/starting over, and metastatic/time-limited chronic breast cancer. The most relevant aspects of each are highlighted, as are the various cross-sectional aspects that manifest throughout the entire patient journey.
Conclusions
Comprehending patients’ experiences in depth facilitates the detection of situations of risk and helps to identify key moments when more precise information should be offered. Similarly, preparing the women for the process they must confront and for the sequelae of medical treatments would contribute to decreasing their uncertainty and concern, and to improving their quality-of-life.
Citation: Ciria-Suarez L, Jiménez-Fonseca P, Palacín-Lois M, Antoñanzas-Basa M, Fernández-Montes A, Manzano-Fernández A, et al. (2021) Breast cancer patient experiences through a journey map: A qualitative study. PLoS ONE 16(9): e0257680. https://doi.org/10.1371/journal.pone.0257680
Editor: Erin J. A. Bowles, Kaiser Permanente Washington, UNITED STATES
Received: February 17, 2021; Accepted: September 3, 2021; Published: September 22, 2021
Copyright: © 2021 Ciria-Suarez et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: Relevant anonymized data excerpts from the transcripts are in the main body of the manuscript. They are supported by the supplementary documentation at 10.1371/journal.pone.0244355 .
Funding: This work was funded by the Spanish Society of Medical Oncology (SEOM) in 2018. The sponsor of this research has not participated in the design of research, in writing the report, or in the decision to submit the article for publication.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Breast cancer is the most common cancer and the one that associates the highest mortality rates among Spanish women, with 32,953 new cases estimated to be diagnosed in Spain in 2020 [ 1 ]. Thanks to early diagnosis and therapeutic advances, survival has increased in recent years [ 2 ]. The 5-year survival rate is currently around 85% [ 3 , 4 ].
Though high, this survival rate is achieved at the expense of multiple treatment modalities, such as surgery, chemotherapy, radiotherapy, and hormone therapy, the side effects and sequelae of which can interfere with quality-of-life [ 5 ]. Added to this is the uncertainty surrounding prognosis; likewise, life or existential crises are not uncommon, requiring great effort to adjust and adapt [ 6 ]. This will not only affect the patient psychologically, but will also impact their ability to tolerate treatment and their socio-affective relations [ 7 ].
Several medical tests are performed (ultrasound, mammography, biopsy, CT, etc.) to determine tumor characteristics and extension, and establish prognosis [ 8 ]. Once diagnosed, numerous treatment options exist. Surgery is the treatment of choice for non-advanced breast cancer; chemotherapy, radiotherapy, and hormone therapy are adjuvant treatments with consolidated benefit in diminishing the risk of relapse and improving long-term survival [ 9 ]. Breast cancer treatments prompt changes in a person’s physical appearance, sexuality, and fertility that interfere with their identity, attractiveness, self-esteem, social relationships, and sexual functioning [ 10 ]. Patients also report more fatigue and sleep disturbances [ 11 ]. Treatment side effects, together with prognostic uncertainty cause the woman to suffer negative experiences, such as stress in significant relationships, and emotions, like anxiety, sadness, guilt, and/or fear of death with negative consequences on breast cancer patients’ quality-of-life [ 10 , 12 ]. Once treatment is completed, patients need time to recover their activity, as they report decreased bodily and mental function [ 13 ], fear of relapse [ 14 ], and changes in employment status [ 15 ]. After a time, there is a risk of recurrence influenced by prognostic factors, such as nodal involvement, size, histological grade, hormone receptor status, and treatment of the primary tumor [ 16 ]. Thirty percent (30%) of patients with early breast cancer eventually go on to develop metastases [ 17 ]. There is currently no curative treatment for patients with metastatic breast cancer; consequently, the main objectives are to prolong survival, enhance or maintain quality-of-life, and control symptoms [ 17 , 18 ]. In metastatic stages, women and their families are not only living with uncertainty about the future, the threat of death, and burden of treatment, but also dealing with the existential, social, emotional, and psychological difficulties their situation entails [ 18 , 19 ].
Supporting and accompanying breast cancer patients throughout this process requires a deep understanding of their experiences. To describe the patient’s experiences, including thoughts, emotions, feelings, worries, and concerns, the phrase “patient voice” has been used, which is becoming increasingly common in healthcare [ 20 ]. Insight into this “voice” allows us to delve deeper into the physical, emotional, cognitive, social, and spiritual effects of the patient’s life. This narrative can be portrayed as a “cancer journey", an experiential map of patients’ passage through the different stages of the disease [ 21 ] that captures the path from prevention to early diagnosis, acute care, remission, rehabilitation, possible recurrence, and terminal stages when the disease is incurable and progresses [ 22 ]. The term ‘patient journey’ has been used extensively in the literature [ 23 – 25 ] and is often synonymous with ‘patient pathway’ [ 26 ]. Richter et al. [ 26 ] state that there is no common definition, albeit in some instances the ‘patient journey’ comprises the core concept of the care pathway with greater focus on the individual and their perspective (needs and preferences) and including mechanisms of engagement and empowerment.
While the patient’s role in the course of the disease and in medical decision making is gaining interest, little research has focused on patient experiences [ 27 , 28 ]. Patient-centered care is an essential component of quality care that seeks to improve responsiveness to patients’ needs, values, and predilections and to enhance psychosocial outcomes, such as anxiety, depression, unmet support needs, and quality of life [ 29 ]. Qualitative studies are becoming more and more germane to grasp specific aspects of breast cancer, such as communication [ 27 , 30 ], body image and sexuality [ 31 , 32 ], motherhood [ 33 ], social support [ 34 ], survivors’ reintegration into daily life [ 13 , 15 ], or care for women with incurable, progressive cancer [ 17 ]. Nevertheless, few published studies address the experience of women with breast cancer from diagnosis to follow-up. These include a clinical pathway approach in the United Kingdom in the early 21st century [ 35 ], a breast cancer patient journey in Singapore [ 25 ], a netnography of breast cancer patients in a French specialized forum [ 28 ], a meta-synthesis of Australian women living with breast cancer [ 36 ], and a systematic review blending qualitative studies of the narratives of breast cancer patients from 30 countries [ 37 ]. Sanson-Fisher et al. [ 29 ] concluded that previously published studies had examined limited segments of patients’ experiences of cancer care and emphasized the importance of focusing more on their experiences across multiple components and throughout the continuum of care. Therefore, the aim of this study is to depict the experiences of Spanish breast cancer patients in their journey through all stages of the disease. To the best of our knowledge, there are no studies that examine the experience of women with breast cancer in Spain from diagnosis through treatment to follow-up of survivors and those who suffer a relapse or incurable disease presented as a journey map.
A map of the breast cancer patient’s journey will enable healthcare professionals to learn first-hand about their patients’ personal experiences and needs at each stage of the disease, improve communication and doctor-patient rapport, thereby creating a better, more person-centered environment. Importantly, understanding the transitional phases and having a holistic perspective will allow for a more holistic view of the person. Furthermore, information about the journey can aid in shifting the focus of health care toward those activities most valued by the patient [ 38 ]. This is a valuable and efficient contribution to the relationship between the system, medical team, and patients, as well as to providing resources dedicated to the patient’s needs at any given time, thus improving their quality of life and involving them in all decisions.
Study design and data collection
We conducted a qualitative study to explore the pathway of standard care for women with breast cancer and to develop a schematic map of their journey based on their experiences. A detailed description of the methodology is reported in the published protocol “Ascertaining breast cancer patient experiences through a journey map: A qualitative study protocol” [ 39 ].
An interview guide was created based on breast cancer literature and adapted with the collaboration of two medical oncologists, three nurses (an oncology nurse from the day hospital, a case manager nurse who liaises with the different services and is the ‘named’ point of contact for breast cancer patients for their journey throughout their treatment, and a nurse in charge of explaining postoperative care and treatment), and two psycho-oncologists. The interview covered four main areas. First, sociodemographic and medical information. Second, daily activities, family, and support network. Third, participants were asked about their overall perception of breast cancer and their coping mechanisms. Finally, physical, emotional, cognitive, spiritual, and medical aspects related to diagnosis, treatment, and side effects were probed. Additionally, patients were encouraged to express their thoughts should they want to expand on the subject.
The study was carried out at nine large hospitals located in six geographical areas of Spain. To evaluate the interview process, a pilot test was performed. Interviews were conducted using the interview guide by the principal investigator who had previous experience in qualitative research. Due to the Covid-19 pandemic, all interviews were completed online and video recorded with the consent of the study participants for subsequent transcription. Relevant notes were taken during the interview to document key issues and observations.
Participant selection and recruitment
Inclusion criteria were being female, over 18 years of age, having a diagnosis of histologically-confirmed adenocarcinoma of the breast, and good mental status. To ascertain the reality of women with breast cancer, most of the patients recruited (80%) had been diagnosed in the past 5 years. Patients (20%) were added who had been diagnosed more than 5 years earlier, with the aim of improving the perspective and ascertaining their experience after 5 years.
Medical oncologists and nurses working at the centers helped identify patients who met the inclusion criteria. Participants went to the sites for follow-up between December 2019 and January 2021. Eligible women were informed of the study and invited to participate during an in-person visit by these healthcare professionals. Those who showed interest gave permission to share their contact information (e-mail or telephone number) with the principal investigator, who was the person who conducted all interviews. The principal investigator contacted these women, giving them a more detailed explanation of the study and clarifying any doubts they may have. If the woman agreed to participate, an appointment was made for a videoconference.
A total of 21 women agreed to participate voluntarily in this research. With the objective of accessing several experiences and bolstering the transferability of the findings, selection was controlled with respect to subjects’ stage of cancer, guaranteeing that there would be a proportional number of women with cancer in all stages, as well as with relapses.
Data analysis
The data underwent qualitative content analysis. To assure trustworthiness, analyses were based on the system put forth by Graneheim, and Lundman [ 40 ]. Interviews were transcribed and divided into different content areas; units of meaning were obtained and introduced into each content area; meaning codes were extracted and added; codes were categorized in terms of differences and similarities, and themes were created to link underlying meanings in the categories. All members of the research team (core team, two medical oncologists, three nurses and two psycho-oncologists) reviewed the data and triangulated the outcomes between two sources of data: qualitative data from the interview and non-modifiable information, such as sociodemographic (i.e., age, marital status, having children) and clinical (i.e., cancer stage and surgery type) data. Following this process, we reached saturation of the interview data by the time we had completed 21 interviews.
Ethical considerations
This study was performed in accordance with the ethical standards of the Declaration of Helsinki, and its subsequent amendments. The study was approved by the Research Ethics Committee of University of Barcelona (Institutional Review Board: IRB00003099) and supported by the Bioethics Group of the Spanish Society of Medical Oncology (SEOM) 2018 grant. All participants received a written informed consent form that they signed prior to commencing with the interviews and after receiving information about the study.
Patient baseline characteristics
In total, 21 women with a mean age of 47 years (range, 34 to 61) were interviewed. Most of the study population was married (66.7%), had a college education (66.7%), and had 2 or more children (42.9%). All cancer stages were represented, up to 23.8% tumor recurrence, and most of the primary cancers had been resected (95.2%) (see Table 1 ).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0257680.t001
Description of the breast cancer patient journey
The women diagnosed with breast cancer describe the journey as a process tremendously affected by the different medical stages. Each stage has its own characteristics that condition the experiences, unleashing specific physical, emotional, cognitive, and social processes. Additionally, the patients perceive this entire process as pre-established journey they must undertake to save their life, with its protocols based on the type and stage of cancer.
“ People said to me , ‘What do you think ? ’ and I answered that there was nothing for me to think about because everything is done , I have to go on the journey and follow it and wait to see how it goes” (Patient 6)
Fig 1 displays the various phases of the journey that patients with breast cancer go through; nevertheless, each woman will go through some or others, depending on their type of cancer.
https://doi.org/10.1371/journal.pone.0257680.g001
Throughout the entire patient journey.
Processes of loss and reinterpretation of the new circumstance . What stands out the most in the process these women go through during the diagnosis and treatment of breast cancer is loss; specifically, the loss of health and a reinterpretation of the new circumstance and the new bodily reality. In the most extreme cases, the loss of health emerges with the fear of death that many women report at the time of diagnosis or during treatment, due to the distress generated. The loss of identity seems to be related to the evolutionary (existential) moment in which the woman is; there are patients who report feelings of disability or loss of attractiveness, or fear of not being able to get pregnant in the future, especially the youngest.
I felt a terrifying fear and thought , “You have cancer you tell yourself , you’re going to die tomorrow .” (Patient 6) I feel like after the hysterectomy , as a woman , I no longer have anything , only the physical . Sure , I look great , but I tell myself that it’s just a shell , the shell I inhabit , because as a woman , I only have one breast left . (Patient 6) At that moment , I had to make the decision that I was no longer going to be a mother . (Patient 14)
Personal change . Most of the women report that with the diagnosis of breast cancer, their life stands still and from that point forward, a different journey begins. The sole focus on this journey is the disease and its implications. During all those months, the patients stop working; they focus on their medical treatments, and reflect a lot on their current situation and on life. Most of the participants state, especially those who have already been discharged, that they know themselves better now; they take better care of themselves, and they enjoy their day-to-day and the small moments more, making the most of their time, with more initiatives and fewer trivial complaints.
Clearly , you’re not the same person you were before; I don’t think she’ll ever come back; your mindset changes completely and I have sequelae from all the treatments . (Patient 1) I re-think wasting energy on lost causes; what’s more , I’ve also learnt to say no . If I’m not in the mood to go somewhere , I just say no . (Patient 7) I take much more advantage of the present now , because you realize that things can change on any given day . (Patient 3)
Trust and appreciation for their physician . Most of the interviewees stated that they fully trusted the doctors who care for them, without question or objection to the treatments proposed. They reported that, as they go forward, they discuss the tests and treatments that are going to be performed, as well as possible side effects. Several stated that they are unaware of the stage of their cancer; similarly, most also do not know the benefits expressed in X% of the treatments. A few of the participants claimed that they did talk in detail about the different types of treatments with their oncologists, that they had sought another opinion, and one of them even reported having decided to stop chemotherapy, which was very hard for her, given her physician’s insistence that she continue.
The truth is that the oncologist didn’t say much about percentages; what she told me were the steps that I had to take; I thoroughly trusted her and she gave me a lot of peace of mind . (Patient 5) I told him , “I’m going to do whatever you tell me to . ” It never occurred to me to dispute whatever the oncologist might tell me . I was willing to do whatever was needed . (Patient 8)
Most of the women, at some point during the interview, state that they are grateful for the care they received and that, within the seriousness of their situation, there is a treatment for their condition.
I am super grateful for the treatment I’ve received and with the doctors assigned to me . (Patient 2) I’m very lucky; I’m only on my second line of treatment for metastasis and I’ve got a lot more ahead of me , but I consider myself lucky and I believe things are going very well . (Patient 20)
Role of the woman . We can see that the women adopt a role of care-givers and managers of their surroundings. They worry about the disease negatively affecting the people around them, which is why they make an effort to manage the family’s activity for when they can’t do it and they try to avoid being a physical burden or cause emotional distress to the people around them.
I was very strong ; I made everything easy for people , but making it very easy , doesn’t mean that it was easy for me , but that I made it easy for everyone . (Patient 8) I didn’t want to worry anyone because that’s just the way I am , I push forward and that’s that . (Patient 5)
Support network . In all cases, the family appears to be one of the elements that is most involved in the disease process. Within the family, the partner deserves special mention. The testimonies in this regard reveal a wide spectrum of possibilities that range from the feeling of having had great support to a lack of attention and understanding that, in many situations, causes the relationship to be strained or to end. Friends tend to appear more occasionally.
I can’t complain about my husband; he was up to the challenge , very attentive toward me and he fully understood how I was feeling ; I felt very supported . (Patient 14) We’ve had a period of a lot of arguing; I’ve had to sit down with him and tell him that life had changed for me . (Patient 18) I had a partner I had lived with for five and a half years and he told me , literally , that he looked at me like a little sister , no longer as a woman , and he left me , and that hurt me tremendously . (Patient 6)
On the other hand, many patients commented on the importance of social media, where they have met people in the same situation as them. They report feeling understood and in good company; likewise, they commented on the importance of being able to share their doubts and get to know about other experiences.
It’s a situation that only someone who has gone through can understand; you can have all the good intentions in the world , but if you haven’t gone through it , you can’t even begin to understand . (Patient 8)
Use of complementary treatments . Most patients follow conventional medical treatment. However, many resort to other disciplines that help them improve their quality-of-life, like dietary changes, getting more exercise than usual, visits to a psychologist or physical therapist, or using other integrative therapies, such as acupuncture, yoga, reiki, flowers of Bach, homeopathy, cannabis, or meditation.
I started to read a whole bunch of books to see what I could do to take care of myself in terms of nutrition and exercise ; you consider everything you can do . (Patient 5)

Diagnosis/unmasking.
This phase encompasses the time from when the woman detects some symptom or goes to a check-up until the medical diagnosis is made. For the woman, this is a time of a series of tests and results. We have observed that the procedures, especially the healthcare professionals that deal with the patients, and the timing vary, depending on the medical center where they are being cared for. Emotionally, this is one of the most complicated stages.
Emotional whirlwind . The wait to obtain test results has a huge emotional impact for the women, given that it is a time of great uncertainty and fear.
An entire month with all the anguish of finding out if you have something . (Patient 3) The worst part is waiting 15 days to find out the magnitude of the tragedy , if it’s throughout your entire body or only in your breast; you go through a brutal emotional whirlwind; the wait is horrible because there’s nothing else you can do , so that anguish that you carry inside is dreadful; it was hell for me . (Patient 10)
Additionally, the interviewees described many other emotions that included fear of death, fear of having no time, feeling of unreality, rage, anger, sadness, avoidance, denial…
The first thing I thought was that I was going to die and that I wouldn’t finish watching my children [grow up]; my father had died of lung cancer 25 years ago . (Patient 9) My only aim was to get back to normal , as if there were nothing wrong . (Patient 4) You have a lot of conflicting feelings; you wish this weren’t happening; you want to run away , but you say , “Where am I going to run to ? ” . (Patient 14)
Impact of medical communication . Several women comment that, when given the diagnosis, they dissociate because of the emotional impact and that they don’t listen to all the information that the medical professional is giving them.
I remember that she talked and talked , but I didn’t know what she was saying until she said , “Isabel , you’re going to be cured , okay ?”. (Patient 9)
During the diagnostic testing, the women are highly sensitive to the healthcare professionals’ words and gestures.
I looked at the face of the person who was doing the mammogram and that’s when I started to imagine the worst . (Patient 20) I say to them , “ But , is there a solution to this ? ” , and they say to me , “Don’t worry , I’m sure there is a solution . ” That “sure” is etched in my mind . (Patient 10)
Communication and managing their surroundings . After the diagnosis, the patients feel that they have to tell the people around them about their situation, especially those closest to them, the family. They all agree on how hard it is to share. Normally, the people it’s hardest to tell are their mother and their children. When they do, they try to put the most positive spin on it possible, in an attempt to keep them from worrying.
You no longer think only about yourself , you think , “Good grief , now I’ve got to tell my mother .” It’s hard . (Patient 16) I wanted to tell my kids the way I say things , always trying to look for the upside , and positive , although it was hard , but , anyway , in the end , it went well . When I finished , my husband told me , “You’ve convinced me that it’s no big deal .” (Patient 9) I told my son , “Son , don’t cry , your mom’s going to get over this , this is nothing .” (Patient 1)
During this period, the women contemplate how their situation will affect their surroundings and they try to organize it as much as possible.
I devoted myself to planning everything , to organizing what to do with my daughter , and to thinking about work , too , how I had left things at work . (Patient 4)
Surgery/cleaning out the cancer.
Uncertainty and fear . The participants express that before going into surgery, they are told about the kind of procedure that will be done, but that, depending on what they find and the analysis, it may change. In light of this, they exhibit an enormous feeling of uncertainty and fear. In addition, many voice concern about how the surgery will go.
They tell you conservative surgery , but if we open up and see something we didn’t see on the tests , then everything could change . (Patient 10) Aside from the anesthesia , that I’m terrified of , you spend several hours in surgery and you don’t really know how things will go; when they clean it out , they analyze it , and you go into the operating room and you don’t know what can happen . (Patient 9)
Feeling of loss . Considering that the breast is associated with an intimate, feminine part [of their body], many women experience the operation as a loss. This loss is more acute if the operation is a mastectomy and there is no reconstruction at the same time. The loss also involves a loss of identity, compounded by the side effects of chemotherapy, such as hair loss. The interviewees who had undergone mastectomy say that following surgery, when the bandaging is removed and the scar is revealed, is one of the most critical moments, which is why they express difficulty in managing it and appreciate the caring assistance from the professionals.
It is identification with yourself , you know , it’s what you’ve seen in the mirror , what you think you’re like and , suddenly , you’re no longer like that; there’s an incredible personal crisis because you no longer recognize what you’re seeing . (Patient 11) I closed my eyes and I removed the bandaging and I didn’t dare look … with my eyes , I imagined the worst . (Patient 12)
Acceptance or demand for more aggressive intervention . The patients perceive the surgery as essential to recovering their health, which is why the process is widely accepted. Some patients who demand a more invasive intervention, normally a bilateral mastectomy, do so because that way, they feel safer with respect to a possible relapse, as well as more comfortable esthetically.
If they have to remove my breast , let them take it; what I want is to get better . (Patient 16) They say that I am in full remission , so they only removed the lump , but at first , I said that I wanted my whole [breast] removed ; then they assessed how to do it . (Patient 13) They told me that I had a genetic mutation and more possibilities of developing breast cancer and , since I felt such rejection toward my remaining breast , I decided to get rid of that one , too . (Patient 20)
Chemotherapy/loss of identity.
The chemotherapy phase is one of the phases that affects the women’s lives the most, because of its physical impact and how long it lasts. No differences have been found in how they experience chemotherapy depending on whether it was neoadjuvant or adjuvant.
Negative impact of side effects . Chemotherapy is associated with many side effects that vary from one woman to another. Many indicate that they have suffered physical discomfort, such as fatigue, dysgeusia, pain, nausea and vomiting, mucositis, diarrhea, etc.
One day when I didn’t want to go to bed , I went to bed crying because I had the feeling that I wasn’t going to wake up . That day it was because I felt awful . (Patient 1)
Furthermore, all of the women suffer hair loss, which is one of the most-feared effects. Likewise, their body hair also falls out, especially on their face, and their weight fluctuates. All of these changes lead to a loss of identity that is experienced as taking away from their femininity. It must be remembered that oftentimes, chemotherapy is administered after surgery, further exacerbating this physical change. On top of all that, several women comment having to decide at the beginning of treatment whether to freeze their eggs or not; at that moment, many of them forfeit the possibility of becoming a mother or of becoming a mother again, which also adds to this loss of femininity.
Losing my hair was hard , but when it grew out again , I had an identity crisis . I didn’t recognize myself; people said I was really pretty like that , with my hair so short . I looked at myself in the mirror and I said that I’m not that woman , I can see that that woman is pretty , but it’s just that I don’t recognize myself . That’s not me or , it was like , I looked at myself and I didn’t recognize myself . That’s when I suffered a serious identity crisis , psychologically serious , but also serious because I sobbed because I looked at myself , but it wasn’t me . (Patient 6) Where’s that sexy lady , where is she ?, because you don’t feel good . I didn’t like myself at all . I was several sizes larger and I looked at myself and said , “What a monster . ” I didn’t feel good about myself . (Patient 1)
Many patients say that chemotherapy decreases their libido and dries up their mucous membranes, which is why they prefer not to have sex. For those who live as a couple, this situation can strain the relationship.
Sexually , I just didn’t feel like it , I wasn’t in the mood; not only did I not feel like it , my mucous membranes were dry and , what’s smore , I just couldn’t , I couldn’t , I felt bad for my husband , but he said , “Don’t worry .” (Patient 16)
Finally, some interviewees expressed a feeling of being poisoned by the treatment. These women tend to be highly focused on taking care of their body and have a very natural attitude toward life.
I had to really work my awareness that I was poisoning myself; at night I was at home and I thought that all that red liquid was circulating through my veins … I think I even had nightmares . (Patient 4)
Balance between caring for oneself and caring for others . The patients feel that it is time to take care of themselves, so they prioritize resting when they need it. Moreover, they worry about getting a haircut and, most of the times, they look for turbans and wigs. Some also learn how to put on make-up, which they rate as being very positive. On the other hand, those who have children or another person in their care, try to take care of them as much as they are able.
Around 11 : 00 , I no longer felt good , so I’d go to the armchair to rest and it’s like I had an angel , because I’d wake up a minute before I had to set the table and get lunch for my son who would be coming home from school . (Patient 1) While I was getting chemo , I went with the gadget and I told myself , “I’m going to teach you to apply make-up; for instance , your eyelashes are going to fall out . Make a line like this ” and at that moment when you look in the mirror , and we look like Fester in the Addams family . (Patient 13)
Vulnerability . The women experience great uncertainty and feelings of vulnerability the first times they receive chemotherapy, since they don’t know what side effects they will suffer.
With chemo , I started with a lot of fear and , later on , I became familiar with it little by little until the time comes when you go to the hospital like someone who’s going to pick up a bit of paper . (Patient 9)
In addition, those participants who join a social network or who are more closely tied to the hospital setting, know about the relapses and deaths of people around them diagnosed with breast cancer, which makes them feel highly vulnerable.
There are some people who leave the group because … it’s not like there are a lot of relapses and , geez , I think that it messes with your head . (Patient 13) We were almost always the same people at chemotherapy ; there was one guy who was really yellow who looked terrible and , there was one time when we stopped seeing him and another lady asked and the nurse said that he had died . (Patient 15)
At the same time, given the physical changes, especially those that have to do with body hair, many women feel observed when they leave home.
If I have to go out and take off my scarf because I’m hot or go straight out without any scarf on my head and whoever wants to look… let them ; I think that it’s up to us , the patients , to normalize the situation; unfortunately , there are more and more cases . (Patient 9)
Telling the kids . Since when the chemotherapy stage is going to entail many physical changes, the women look for ways to talk to their children about the treatment. Most of them comment that it is a complicated situation and all of them try to talk to their children in such a way as to protect them as much as possible.
I asked the nurse for help before I started chemotherapy to see if she had any pointers about how to talk about this with the kids and she recommended a story , but when I saw it , I didn’t like it … so , in the end , I decided to do it off the cuff . (Patient 10)
Radiotherapy/transition to normality.
The “last” treatment . When the patient reaches radiotherapy, normally, they have already spent several months undergoing physically aggressive medical procedures, which is why they feel exhausted. There is a physical exhaustion resulting from the previous treatments and made worse by the radiation therapy. Furthermore, many women also report feeling emotionally drained by the entire process. However, this is generally accompanied by joy and relief because they feel that they are in the final stage of treatment.
Emotionally , it’s a marathon that has to end up at some point . (Patient 10) For me , radiotherapy was like a lull in the battle , with a winning mind-set . (Patient 4)
Comparison with chemotherapy . There is a widespread perception that radiotherapy has fewer side effects than chemotherapy, although later, when they receive it, several patients suffer discomfort, above all fatigue and dizziness. Several report that at this point, they are mentally worn out and just want to be done with the process, which is why they have less information than about chemotherapy.
I feel like radiotherapy is unknown , that you think it’s more “light ” and it turns out not to be so light . (Patient 13)
Follow-up care/the “new” day-to-day.
Difficulty in getting back to normal . Once the patients are discharged, many feel that they need some time to recover, that it will be slow, in order to restore a more normalized pace of life. They are still working on their emotional and personal process.
When they tell you that you have cancer , they make it very clear : you have a goal; you have some months of chemo , some months of radio , and when you finish , you say , “And now , what do I do ?”. I say that because now I have to get back to my normal life , but I don’t feel normal . I still don’t feel cured , I’m not 100% . And you’re glad you’ve that you’ve finished it all and you’re alive , but at the same time , you say , “Gosh… this is very odd . ” It was a very strange feeling . (Patient 8)
Most patients report that their quality-of-life has diminished, due to the sequelae from the treatments. Lymphedema is one of the sequelae they name most often, although they also mention other symptoms, like digestive upset, weight issues, eye problems, scar pain, etc. The women who are on hormone therapy also suffer side effects, such as joint and muscle pain.
I have lymphedema and , although I have good mobility , I’m a little bit weak; when I go out for dinner , I generally order fish , because I can’t always cut meat well . (Patient 6)
Several interviewees also express difficulty in their affective-sexual relations. Many of them feel insecure because of all the physical changes; others have sequelae that hinder their relations, and still others are suffering symptoms of early menopause. This can cause problems in the couple and for those who don’t have a partner, suffer many complications when it comes to meeting other people.
I haven’t had sex with my husband for 2 years because , it’s also really complicated to get over; I’ve gone for pelvic physical therapy; I’ve used gels , but nothing works . (Patient 8) It’s taken me many months for me to have a relationship again; it’s been really hard because , even though everyone told me that I looked fine , I didn’t feel fine . My breast cancer had taken away all my attributes as a woman . (Patient 6)
Some women also experience difficulties when it comes to returning to work. Several state that they had been fired when they went back. They also report that when interviewing for a job, it’s complicated for them because they have to explain what happened and they mention the schedule of doctor’s visits that they have. Other women comment that they’ve been given early retirement or disability.
You go to the interview and if you tell them that you’ve had the disease , they look at you like you’re a weirdo . (Patient 13)
Breast reconstruction . How reconstruction is experienced, as well as its timing, are highly contingent upon they type of reconstruction. Each one has its pros and cons, but the opinions collected with respect to the type of reconstruction have been positive.
Although it took 18 months for the entire process to be over , I’m delighted with reconstruction with the expander . (Patient 16)
Some patients state that after the whole process, which has been long and complicated, they prefer not to undergo reconstruction immediately. In these cases, they report having felt a subtle pressure from the outside to undergo reconstruction.
Every time I went for my check-ups , they said , “You’re the only one left [who hasn’t undergone reconstruction]” and in the end , the truth is that I’m really happy because I think I look pretty . (Patient 12)
Check-ups and fear of relapse . Check-ups are one of the times that generate most worry and insecurity. The women remark that, starting a few days before and until they receive the results of the follow-up studies, they are more anxious about the possibility of relapse.
At every check-up my legs start shaking again and my stomach is in knots, although at my last one, everything turned out okay and I’m thrilled. (Patient 6) During the first stage , I did everything I had to do and I got over it , but it’s a lottery . You can do whatever you want , but it’s the luck of the draw and when you start going for check-ups , it’s like going to play Russian roulette . (Patient 8)
Maintenance hormone therapy . Hormone therapy is understood differently depending on age and on the major decision of whether or not to be a mother or to have another child. If the woman does not want to have more children, the treatment is accepted better. The patients who take it also report effects derived from menopause, for instance, joint pain or dry mucous membranes.
I did notice joint pain , but since I exercised , [I felt it] much less than my fellow women , although , for instance , when it comes to getting up from a chair , you get up like an old lady . (Patient 10)
Position of support . Several patients mention that, after discharge, they stay active on social media, they volunteer when they find out about someone or to participate in activities related to breast cancer, with the aim of being able to help other people who are in this situation.
It’s really good to meet other people who are going through the same thing , so , now that I’ve finished , I like it and I always help whenever I can , because I can share what was good for me . (Patient 13)
Relapse/starting over.
Emotional impact . The diagnosis of a relapse is experienced much the same as the initial diagnosis. All of the women report fear, although they also state that they are more familiar with the processes. Other emotions emerge, such as why me, blame, disbelief, etc.
Since they had told me that it wasn’t going to happen again , I believed it , of course , I wanted to believe it and it totally surprised me; I couldn’t stop crying and crying . (Patient 17)
Telling the family again . Patients repeat that telling the family about it again, especially the children and parents, is tough and they try to minimize it in an attempt to protect them emotionally.
On the very same day that I had my mammogram , my mother says that she wants to come a see the kids . We’re in the park , when she arrives , I have to tell her that everything’s fine and when we get home , I tell her everything . My mother’s devastated again and I tell her not to worry , that everything is going to be fine . (Patient 16)
Thinking about whether something could have been done differently . Several women comment that, after their relapse, they think about whether the treatment was enough or there must have been something they could have done to avoid the relapse.
You get furious , because you say , “I wasn’t supposed to get sick , because if , 2 years ago when the first microcalcifications appeared I had had them removed , then I wouldn’t have metastasis , or maybe I would . (Patient 19)
Metastatic breast cancer/time-limited chronic.
Re-interpreting the concept of metastasis . Most of the participants in this stage state that they have had to give new meaning to the word, “metastasis,” since their first perception was directly related to death. In this way, they come to understand that cancer can become chronic, although they now have to take medication and go to the hospital on a regular basis. Nevertheless, they know that their life expectancy may be a few years. The women who are involved in a group point out how hard it is to see their fellow member pass away.
What I now call my “ new normal” consists of lots of visits to the hospital and never going back to work . (Patient18)
They also state that at this stage, they do not identify with the disease generally known socially as “breast cancer”, where there is great emphasis placed on early detection and on their chances of being cured. This causes them to feel more isolated.
These pink ribbon campaigns hurt us because they tend to underscore that everything is going to turn out fine because breast cancer has a very high cure rate; there is huge lack of awareness . (Patient 20)
Physical and emotional discomfort . Most of the women in this stage report side effects from the treatments, although some comment that good quality-of-life can be preserved. On an emotional level, they say that they sometimes feel a certain agony due to not knowing how much longer the treatment will be effective. They live in a state of uncertainty that they try to cope with by focusing on their day-to-day and experience the good times deeply.
When I’m not in pain , I try not to even remember what I have and go out and have fun with my family and live . (Patient 20)
Several women who have children express with regret that they worry about their children enjoying them and remembering them when they were well. They are sad that they won’t be able to grow up in a normal family. Some also comment the impact this diagnosis is having on their partner.
What I don’t want is for them to carry this baggage of having a sick mother . (Patient 18)
A conflict with disability also appears, as many women report their desire to continue working, but feel that they can’t keep up with the pace of work. Additionally, several state that going through the medical board is a strenuous process, given that they look good physically.
It’s hard to deal with , I’m a non-practicing lawyer and I have degrees galore , but I worked the first year and I couldn’t continue . (Patient 21) Every year they call me again for the disability monitoring and they always threaten me . To be honest , the treatment doesn’t make me sick , but I don’t know how long it’s going to be like this . (Patient 19)
Social invisibility . The participants say that they do not have any physical signs of being ill, that they look fine, although they know and feel that inside, they are not well. They say that it is sometimes hard to manage socially, since on occasion, they feel misunderstood and disparaged.
I’m much sicker now , but people think or want to think that I’m fine . When I was doing chemo , it was like wearing a sign that said “cancer . ” (Patient 17)
This study describes the patient journey of women with breast cancer, specifying the different phases with the most relevant aspects of each, as well as the different cross-sectional features they report throughout the entire treatment process.
The results portray breast cancer as a process in which there is a striking feeling of loss of health and self-identity, changes in routines, personal and employment transformation, as well as emotional hardship during and after breast cancer treatment, aspects that are also reported in the literature [ 41 , 42 ]. Earlier studies state that experiencing cancer is highly stressful. It involves a major threat to life or physical integrity, in addition to mental health, interfering with the path, projects, and plans patients have for their life over the short, medium, and, on occasion, long term as well [ 6 ]. Along with reporting adverse physical and psychological impacts, patients also report positive ways in which they have grown psychologically or emotionally from the experience [ 7 , 42 ]. The diagnosis of breast cancer not only impacts the women individually, but also affects their surroundings. As reported in the literature, despite going through a very challenging time, the women struggle to put on a positive face and attempt to conserve the family’s well-being, specifically that of their children [ 7 ]. At the same time, the family is a fundamental source of support and usually provide indispensable support; however, it is not always effective, because family members do not fully understand the stresses involved in living with cancer [ 43 ]. Previous studies also reveal that for some women, their partners are one of their most significant supports; nonetheless, research also suggests that a cancer diagnosis predicts marital breakup more strongly for female survivors than males [ 44 ]. Our results reflect that the women frequently resort to other women in the same situation, possibly because they face significant unmet supportive care needs [ 30 ]. The need for social support may lead patients to seek social support groups consisting of people who are experiencing similar health crises, because such groups allow them to interact with those who best understand their suffering [ 43 ]. Another aspect that appears across the board is the relationship the participants have with the medical team. In this study, we have noted their trust in the medical team and acceptance of the treatments proposed without going into the clinical data of the disease and without needing to know the benefit provided by the treatment. Cancer patients are confronted with a potentially life-threatening [condition], feeling vulnerable, and need to rely heavily on their care providers, expecting the physician to act in their best interests [ 5 ]. Therefore, they need to have a close relationship, as well as comprehensive care [ 30 ]. Patients’ trust in a physician has been associated with a reduction of their fears and anxiety and [increased] satisfaction and adherence to treatment [ 5 , 30 ]. We believe that it would be important to provide patients with accurate information, so as to avoid misunderstandings (such as cancer being synonymous with death, regardless of stage) as several participants in this study have reported, which can lead them to believe that the risk of relapse with and without chemotherapy is much greater than the oncologists estimate [ 45 ]. We believe that in future studies that it would be worthwhile to examine the peculiarities of each kind of patient information with the aim of determining how to break it up and make it both comprehensible and tolerable to promote patients’ well-being.
A breast cancer diagnosis is generally unexpected and practically all patients suffer psychological distress, such as feelings of uncertainty, disbelief, hopelessness, vulnerability, anger, fear, anxiety, and sadness [ 46 , 47 ]. The literature has reported that many women experience peritraumatic distress or dissociation during the medical conversation in which they are given their diagnosis of cancer [ 48 ], which might account for the reactions of the respondents. Given that, when they receive their diagnosis, additional information is generally given to them, such as clinical aspects and preferred treatments. Repeating this information at subsequent appointments could contribute to improving communication with patient, since several participants stated that they found it hard to pay attention to the physician, given the emotional impact. Additionally, breast cancer patients tend to be diagnosed when they are relatively young, and often when they are in the middle furthering their career or raising children [ 12 ]. In spite of everything, the women try to put on as brave a face as they can and focus on maintaining their children’s well-being [ 7 ]. Telling children about their diagnosis is reportedly one of the biggest challenges; parents are usually unsure of how to tell them, because at the same time that they want it to be open and honest and cover their children’s developmental needs, they also want to protect them children [ 49 ].
Once diagnosed, breast cancer patients go through different treatments. The most salient experiences of these phases pertain to the impact of side effects on physical quality-of-life and psychological well-being, which is consistent with the literature [ 11 ]. Moreover, cancer therapy entails physical changes that affect their feminine identity, fertility, self-esteem, sexual functioning, and makes them more vulnerable [ 10 , 50 ]. Women described their inner self as being on an emotional rollercoaster with highs and lows throughout the various phases of treatment [ 7 ]. Given treatment side effects and sequelae, these women are more likely to experience physical symptoms and psychological disorders than patients with other kinds of tumors [ 51 ]. The side effects involve an acute sense of loss of health and quality-of-life, as well as identity and femininity. It would be interesting for future research to explore the therapies used in grief counseling with cancer patients, as understanding and exploring this perspective could comprise an additional clinical aid.
Once the women have completed their treatments, they gradually get back to normal and many contemplate returning to work. However, in line with our results, the literature reveals that even though they want to normalize their lives, female breast cancer survivors feel that they will never return to their baseline status [ 7 ]. A significant number of patients experience difficulties in physical, cognitive, and emotional functioning after their treatment, such as symptoms like lymphedema, fatigue, pain, sleep disorders, cancer-related cognitive impairment, emotional stress, symptoms of depression and anxiety, problems with relationships, reduced sexual identity, fertility problems, and fear of cancer relapse [ 13 , 14 ]. Furthermore, patients with hormone therapy suffer hot flashes, sweats, joint pain, weight gain, decreased libido, and low energy [ 52 ]. A sizeable number of these women also experience changes in employment status which can happen even 5–10 years following diagnosis [ 15 ]. Given that all these changes alter the structure of the woman’s everyday life, personalized care and treatment plans in cancer survivors are highlighted in the literature with extended specialized support being proposed that enables them to make a better psychosocially adjusted transition from treatment to follow-up [ 53 ] and advocating for the patient’s participation in all decisions that affect her during this period [ 54 ]. Further research is needed concerning how to structure the follow-up and support offered to these women during this stage so as to meet their needs and help them adjust to their new reality with the chronic sequelae caused by cancer and its treatment. On the other hand, the personal transformation of the initial stages of the journey are best seen during this phase. The literature shows that women who have had breast cancer report changes in their philosophy of life, such as embarking on a new life path, changing their priorities in life, as well as valuing life in general [ 42 ]. Most of the participants in our study place special emphasis on appreciating life, enjoying it more, and living each day to the fullest. Cancer survivors report being aware of how precarious life is, while also feeling the joy of being alive [ 55 ]. Similarly, they have been found to be more resilient and better able to repair their mood than healthy women [ 56 ].
About 5% of all patients with breast cancer are diagnosed when the disease is metastatic, whereas some 30% have suffered a relapse of an early breast cancer [ 17 ]. We saw that some women suffering a relapse after initial treatment with curative intent tend to wonder if the treatment was sufficient or if they should have done something more to prevent the relapse. Metastatic breast cancer is uncurable, which is why these women’s main psychosocial challenges are not the same as those who are diagnosed in early stages [ 18 ]. Faced with incurability, the women react with shock and fear of imminent death, but this anxiety diminishes once they begin treatment and learn that there are more treatment options [ 17 ]. During this phase, the interviewees reported impaired physical QoL and functioning, being hindered by pain, fatigue, or menopausal symptoms. Emotionally, they report suffering bouts of depression and anxiety, as well as fear because of the spread of their cancer. As for their relational QoL, their children’s welfare is their number one concern, especially for mothers of young children [ 17 , 57 ]. What’s more, these women felt isolated from society in general and, more specifically, from the non-advanced breast cancer community, inasmuch as they feel that nobody understands what they are going through [ 18 ]. A psychosocial approach is especially important in this phase to help these women to continuously adapt to the changes of their individual clinical situation and to the progression of the disease, thereby improving their coping.
Clinical implications
Having first-person information enables us to comprehend in detail the experiences of breast cancer patients, their situation, and emotional state, which favors holistic cancer care for health professionals.
Healthcare professionals should prepare women for a changed life situation, as well as to face prolonged, multimodal treatment (surgery, chemotherapy, hormone therapy, radiotherapy), and to confront physical and psychological sequelae, as well as the fear surrounding an uncertain prognosis. It is important to help them manage their expectations and fears and, to identify and address the issues and concerns that arise at different time points during treatment. The information and support offered should be adjusted to each woman’s individual needs, her life situation, her coping style, and the time and stage of their cancer. This more empathic, understanding outlook can also contribute to improving the physician-patient rapport, promoting communication, understanding, and shared decision-making.
Finally, a comprehensive understanding of the women’s psychosocial support endorses their belonging to groups of women with breast cancer, in which there is a relationship among equals. Further research is needed to specify the type needed so as to decrease both the impact of the death of women in the group, as well as the vast amount of information that they may end up obtaining, without needing it or requesting it.
Limitations
This study was performed with Spanish participants, which is why certain aspects cannot reflect the experiences of breast cancer patients from other countries, given the particularities of both the Spanish healthcare system and Spanish culture. Likewise, the data attained were specific to women with breast cancer, which can scarcely be extrapolated to individuals with other cancers. Moreover, the findings do not reflect men’s experiences with breast cancer and research with this group would enrich the field further. In addition, the age of our participants ranged from 34 to 61 years; hence the results should be interpreted for a middle-aged population and do not reflect the experiences of women diagnosed at very early or very old ages. Finally, we believe that there may be a bias regarding the women who agree to participate, as this group has probably accepted their condition more, as well as having worked on it more.
Despite these limitations, we hope that our findings can contribute to better understanding the experiences of women with breast cancer.
Acknowledgments
The authors are grateful to the investigators of the Neoetic study and the Bioetic Group of the Spanish Society of Medical Oncology (SEOM) for their contribution to this study. We would like to thank all the women who generously shared their experiences with us, the support of HealthyOnco ( www.healthyonco.com ), and Priscilla Chase Duran for editing and translating the manuscript.
- View Article
- Google Scholar
- PubMed/NCBI
Integrated patient journey
Drive better outcomes with multi-layered insights and analytics
One journey, many lenses
Gaining a granular view of the patient journey data is critical to life sciences commercialization in today’s patient-centric world, informing everything from product development to market access and post-launch management.
Unfortunately, patient journey efforts are often conducted in a fragmented fashion, with different teams employing different methodologies and data sources, depriving companies of a more comprehensive view of the barriers and drivers impacting their brands.
At Clarivate, we’re rethinking the way we trace the patient journey touchpoints with the aim of capturing the larger picture, in greater detail, so that our customers can better serve their customers.
“Our previous patient journey work was conducted in typical fashion – qualitative interviews with patients, maybe a quantitative study, but we really needed to understand the emotions patients were experiencing at each stage in order to identify messaging that resonates in order to better support patients and keep them on that journey longer.
Having that voice-of-the-patient lexicon was huge – a lot of what our marketing team puts out now utilizes the language patients are using online, as opposed to the more clinical language encouraged by medical, legal and regulatory. Patients don’t want to read language that they’re not using in the context of their day-to-day.”
- Head of Market Intelligence
- Mid-sized Pharma
How we help
At Clarivate, we examine the patient journey through multiple lenses in order to provide a granular and insights-rich view of the patient journey research:
Clinical journey
- Treatment and referral patterns
- Time to diagnosis
- Sites of care
- Line of therapy progression
Cost Journey
- Impact of cost burden and market access factors on treatment decisions and behaviors
Attitudinal Journey
- What patients are feeling at each stage in the treatment journey
- Connections with patient behaviors such as adoption, adherence, discontinuation and switching
- HCP attitudes
Informational Journey
- Channels, devices and sites sourced for health and medical info
We partner with clients on patient journey analyses to help enhance commercial activities, including:
- Sales force optimization
- Patient engagement
- Physician engagement
- Payer value communication
- Segmentation and targeting
- Adherence and switching management
- Opportunity assessment
Integrated patient journey assessment - a Clarivate solution
At Clarivate, we’re rethinking the way we trace the patient journey with the aim of capturing the larger picture, in greater detail, so that our customers can better serve their customers.
Diverse data sources
The power of the integrated patient journey approach lies in the combination of quantitative and qualitative data sources to reveal key intervention points and opportunities for differentiating products across multiple stakeholder audiences.
- 26 billion claims
- Visibility into 300+ million patients (over 3 years)
- 2+ million healthcare providers
- 98% of 750 U.S. payers, real-time updates
- Hospitals, physician offices, ASCs, pharmacies, long-term care, nursing facilities
Electronic health records
- Visibility into 100+ million patients (over 3 years)
- Diagnoses, diagnostic tests, assessments, vaccines, vitals, Rx
Social data
- Anonymized social conversation data from public social platforms, online communities and message boards
Online behavioral data
- Search data
- Clickstream data
Primary patient journey market research
- 25+ countries
- 25+ specialities
- 50+ therapeutic areas
Secondary patient journey market research
- Public health and demographic data sets
- Formulary coverage
Integrated Patient Journey: One Journey, Many Lenses

Integrated patient journey: Leveraging real world data and analytics to understand patients’ unmet needs

Integrated patient journey assessment – A Clarivate solution

Want to learn more?
Contact us to connect with a specialist on how we can enhance your healthcare patient journey mapping
Speak to our team
Nursing Case Studies with Answers
Explore Nursing Case Studies with Answers and examples in Carepatron's free downloadable PDF. Enhance your nursing knowledge and prepare for exams with practical scenarios.

By Wynona Jugueta on Mar 25, 2024.
Fact Checked by Ericka Pingol.

What is a case study?
A case study in medicine is a detailed report of a patient's experience with a disease, treatment, or condition. It typically includes the patient's medical history, symptoms, diagnostic tests, treatment course, and outcome.
Some key things to know about medical case studies template . First, they delve deep into the specifics of a single case, providing a rich understanding of a particular medical situation.
Medical professionals use case studies to learn about rare diseases, unusual presentations of common conditions, and the decision-making process involved in complex cases.
Case studies can identify exciting areas for further investigation through more rigorous clinical trials. While informative, they can't be used to develop general treatment guidelines because they only focus on a single case.
Overall, medical case studies are valuable tools for medical education and research, offering insights into human health and disease complexities.
Printable Nursing Case Studies with Answers
Download this Nursing Case Studies with Answers to analyze complex clinical situations, identify priority needs, and develop effective care plans tailored to individual patients.
What is in a nursing case study?
A nursing case study is a detailed examination of a patient's health condition, treatment plan, and overall care journey, specifically from the perspective of nursing practice. These case studies are essential components of nursing education and professional development, providing valuable insights into clinical scenarios and patient care experiences.
In a case nursing study template , various elements are typically included to comprehensively understand the patient's situation. First and foremost, the case study outlines the patient's demographic information, including age, gender, medical history, and presenting symptoms. This demographic overview sets the stage for understanding the context in which healthcare interventions occur.
Moreover, nursing case studies often delve into the nursing assessment process, highlighting the initial and ongoing assessments nurses conduct to gather relevant patient health status data. These assessments involve physical examinations, vital sign monitoring, and assessment tools to identify potential health issues and risk factors.
Critical thinking skills are essential in nursing case studies, as they enable nurses to analyze complex clinical situations, identify priority needs, and develop effective care plans tailored to individual patients. Nursing students and experienced nurses use case studies as opportunities to enhance their critical thinking abilities and clinical decision-making processes.
Nursing case studies serve several vital purposes within healthcare education and professional practice, whether they are a primary care physician or a group of nursing students. Let's explore each purpose in detail:
Enhancing clinical reasoning skills
One primary purpose of nursing case studies is to enhance nursing students' and practicing nurses' clinical reasoning skills. By presenting realistic patient scenarios, case studies challenge individuals to analyze clinical data, interpret findings, and develop appropriate nursing interventions. This process promotes critical thinking and problem-solving abilities essential for effective nursing practice.
Applying theoretical knowledge to practice
Nursing case studies provide a bridge between theoretical knowledge and practical application. They allow nursing students to apply concepts learned in the classroom to real-world patient care situations. By engaging with case studies, students can integrate theoretical principles with clinical practice, gaining a deeper understanding of nursing concepts and their relevance to patient care.
Facilitating interdisciplinary collaboration
Another purpose of nursing case studies is to facilitate interdisciplinary collaboration among healthcare professionals. Nurses often collaborate with physicians, specialists, therapists, and other team members in complex patient cases to deliver comprehensive care. Case studies offer opportunities for nurses to explore collaborative decision-making processes, communication strategies, and teamwork dynamics essential for providing quality patient care.
Promoting evidence-based practice
Nursing case studies are crucial in promoting evidence-based practice (EBP) within nursing and healthcare settings. Nurses can make informed decisions about patient care interventions by analyzing patient scenarios and considering current research evidence. Case studies encourage nurses to critically evaluate research findings, clinical guidelines, and best practices to ensure the delivery of safe, effective, and patient-centered care.
Fostering professional development
Engaging with nursing case studies contributes to the ongoing professional development of nurses at all stages of their careers. For nursing students, case studies provide valuable learning experiences that help prepare them for clinical practice. For experienced nurses, case studies offer opportunities to refine clinical skills, stay updated on emerging healthcare trends, and reflect on past experiences to improve future practice.
How to write a nursing case study?
Writing a nursing case study involves several essential steps to ensure accuracy, relevance, and clarity. Let's break down the process into actionable steps:
Step 1: Select a patient case
Begin by selecting a patient case that presents a relevant and compelling healthcare scenario. Consider factors such as the patient's demographic information, medical history, presenting symptoms (e.g., joint stiffness, pain), and healthcare needs (e.g., medication administration, vital signs monitoring). Choose a case that aligns with your learning objectives and offers meaningful analysis and discussion opportunities.
Step 2: Gather relevant data
Collect comprehensive data about the selected patient case, including medical records, test results, nursing assessments, and relevant healthcare documentation. Pay close attention to details such as the patient's current health status, past medical history (e.g., diabetes), treatment plans, and any ongoing concerns or challenges. Utilize assessment tools and techniques to evaluate the patient's condition thoroughly and identify areas of clinical significance.
Step 3: Assess the patient's needs
Based on the gathered data, evaluate the patient's needs, considering physical, emotional, social, and environmental factors. Assess the patient's pain levels, mobility, vital signs, and other relevant health indicators. Identify any potential complications, risks, or areas requiring immediate attention. Consider the patient's preferences, cultural background, and individualized care requirements in your assessment.
Step 4: Formulate nursing diagnoses
Formulate nursing diagnoses that accurately reflect the patient's health needs and priorities based on your assessment findings. Identify actual and potential nursing diagnoses related to the patient's condition, considering factors such as impaired mobility, ineffective pain management, medication adherence issues, and self-care deficits. Ensure your nursing diagnoses are specific, measurable, achievable, relevant, and time-bound (SMART).
Step 5: Develop a care plan
Develop a comprehensive care plan outlining the nursing interventions and strategies to address the patient's identified needs and nursing diagnoses. Prioritize interventions based on the patient's condition, preferences, and care goals. Include evidence-based nursing interventions to promote optimal health outcomes, manage symptoms, prevent complications, and enhance the patient's overall well-being. Collaborate with other healthcare professionals as needed to ensure coordinated care delivery.
Step 6: Implement and evaluate interventions
Implement the nursing interventions outlined in the care plan while closely monitoring the patient's response to treatment. Administer medications, provide patient education, perform nursing procedures, and coordinate care activities to effectively meet the patient's needs. Continuously evaluate the effectiveness of interventions, reassessing the patient's condition and adjusting the care plan as necessary. Document all interventions, observations, and outcomes accurately and comprehensively.
Step 7: Reflect and seek assistance
Reflect on the nursing case study process, considering what worked well, areas for improvement, and lessons learned. Seek assistance from nursing instructors, preceptors, or colleagues if you encounter challenges or have concerns about the patient's care. Collaborate with interdisciplinary team members to address complex patient issues and ensure holistic care delivery. Continuously strive to enhance your nursing practice through ongoing learning and professional development.
Nursing Case Studies with Answers example (sample)
Below is an example of a nursing case study sample created by the Carepatron team. This sample illustrates a structured framework for documenting patient cases, outlining nursing interventions, and providing corresponding answers to guide learners through the analysis process. Feel free to download the PDF and use it as a reference when formulating your own nursing case studies.
Download this free Nursing Case Studies with Answers PDF example here

Why use Carepatron as your nursing software?
Carepatron stands out as a comprehensive and reliable solution for nursing professionals seeking efficient and streamlined workflows in their practice. With a range of features tailored to the needs of nurses and healthcare teams, Carepatron offers unparalleled support and functionality for managing various aspects of patient care.
Nurse scheduling software
One of the key advantages of Carepatron is its nurse scheduling software , which simplifies the process of creating and managing schedules for nursing staff. With intuitive scheduling tools and customizable options, nurses can easily coordinate shifts, manage availability, and ensure adequate staffing levels to meet patient needs effectively.
Telehealth platform
In addition, Carepatron offers a robust telehealth platform that facilitates remote patient monitoring, virtual consultations, and telemedicine services. This feature enables nurses to provide continuity of care beyond traditional healthcare settings, reaching patients in remote areas or those unable to attend in-person appointments.
Clinical documentation software
Furthermore, Carepatron's clinical documentation software streamlines the documentation process, allowing nurses to easily capture patient data, record assessments, and document interventions. The platform supports accurate and efficient documentation practices, ensuring compliance with regulatory standards and promoting continuity of care across healthcare settings.

Commonly asked questions
In clinical terms, a case study is a detailed examination of a patient's medical history, symptoms, diagnosis, treatment, and outcomes, typically used for educational or research purposes.
Case studies are essential in nursing as they provide real-life scenarios for nurses to apply theoretical knowledge, enhance critical thinking skills, and develop practical clinical reasoning and decision-making abilities.
Case studies in nursing education offer benefits such as promoting active learning, encouraging problem-solving skills, facilitating interdisciplinary collaboration, and fostering a deeper understanding of complex healthcare situations.
Related Templates
Popular templates.
Chronic Illnesses List
Access this helpful guide on chronic illnesses you can refer to when working on prevention, diagnosis, and treatment planning.
Therapy Letter for Court
Explore our guide on writing Therapy Letters for Court, offering templates and insights for therapists to support clients' legal cases effectively.
Nursing Nutrition Assessment
Learn about nursing nutrition assessments, including examples and Carepatron's free PDF download to help you understand the process and improve patient care.
Facial Massage Techniques PDF
Unlock the secrets of rejuvenating facial massage techniques with Carepatron's comprehensive PDF guide. Learn how to enhance your skincare routine and achieve a radiant, glowing complexion.
Blood Test for Heart Attack
Learn about the importance of blood tests for detecting heart attacks and download Carepatron's free PDF example for reference. Find crucial information to help you understand the process.
Mental Health Handout
Learn key insights into mental health conditions, warning signs, and resources. Access a free Mental Health Handout today!
Procedure Note Template
Ensure patient identity, consent, anesthesia, vital signs, and complications are documented. Download our accessible Procedure Note Template today!
Nursing Home Report Sheet
Discover a comprehensive guide on creating a Nursing Home Report Sheet. Includes tips, examples, and a free PDF download to streamline healthcare reporting.
Obesity Chart
Explore our free Obesity Chart and example, designed to help practitioners and patients monitor overall health risks associated with obesity.
Charge Nurse Duties Checklist
Take charge with our comprehensive Charge Nurse Duties Checklist. Free PDF download available!
Pre-employment Medical Exam
Ensure job applicants' fitness for duty with our Pre-Employment Medical Exam Template. Comprehensive guide for thorough health assessments.
Medical Clearance Form
Get your health clearance certificate easily with our Medical Clearance Form. Download for free for a streamlined process and hassle-free experience.
Level of Care Assessment
Discover what a Level of Care Assessment entails and access Carepatron's free PDF download with an example to help you better understand the process.
Standard Intake Questionnaire Template
Access a standard intake questionnaire tool to help you enhance the initial touchpoint with patients in their healthcare process.
Patient Workup Template
Optimize patient care with our comprehensive Patient Workup Template. Streamline assessments and treatment plans efficiently.
Stroke Treatment Guidelines
Explore evidence-based Stroke Treatment Guidelines for effective care. Expert recommendations to optimize stroke management.
Counseling Theories Comparison Chart
Explore a tool to differentiate counseling theories and select approaches that can work best for each unique client.
Nursing Registration Form
Learn what a nurse registry entails, its significance to registered nurses, and the application process completed through a Nursing Registration Form.
Physical Therapy Plan of Care
Download Carepatron's free PDF example of a comprehensive Physical Therapy Plan of Care. Learn how to create an effective treatment plan to optimize patient outcomes.
ABA Intake Form
Access a free PDF template of an ABA Intake Form to improve your initial touchpoint in the therapeutic process.
Speech Language Pathology Evaluation Report
Get Carepatron's free PDF download of a Speech Language Pathology Evaluation Report example to track therapy progress and communicate with team members.
Home Remedies for Common Diseases PDF
Explore natural and effective Home Remedies for Common Diseases with our guide, and educate patients and caretakers to manage ailments safely at home.
HIPAA Policy Template
Get a comprehensive HIPAA policy template with examples. Ensure compliance, protect patient privacy, and secure health information. Free PDF download available.
Health Appraisal Form
Download a free Health Appraisal Form for young patients. Streamline your clinical documentation with our PDF template and example.
Consent to Treat Form for Adults
Discover the importance of the Consent to Treat Form for adults with our comprehensive guide and example. Get your free PDF download today!
Nursing Skills Assessment
Know how to evaluate nursing skills and competencies with our comprehensive guide. Includes an example template for a Nursing Skills Assessment. Free PDF download available.
Medical Record Request Form Template
Discover how to streamline medical record requests with our free template & example. Ensure efficient, compliant processing. Download your PDF today.
Personal Training Questionnaire
Access a comprehensive Personal Training Questionnaire to integrate when onboarding new clients to ensure a personalized fitness plan.
Agoraphobia DSM 5 Criteria
Explore a helpful documentation tool to help screen for the symptoms of agoraphobia among clients. Download a free PDF resource here.
Dental Inventory List
Streamline your dental practice's inventory management with our Dental Inventory List & Example, available for free PDF download.
Personal Trainer Intake Form
Discover how to create an effective Personal Trainer Intake Form with our comprehensive guide & free PDF example. Streamline your fitness assessments now.
Healthy Liver Foods List
Explore our Healthy Liver Foods List to support liver health with the right diet. Learn how Carepatron aids healthcare professionals in managing nutrition plans.
Printable Family History Form
Streamline patient intake with our Family History Form template. Capture essential family medical history to enhance patient care and risk assessment.
Portable Medication List
Keep track of your prescription medicines, supplements, and vitamins with our Portable Medication List and take care of your health
Universal Health Form
Learn the importance of a Universal Health Form. Download a free PDF and template to guide parents and guardians when completing the form.
Skin Analysis Form
Need a skin analysis form? Download Carepatron's free PDF template and get an example to help you conduct comprehensive skin analyses effectively.
Family Nursing Care Plan
Discover our Family Nursing Care Plan template, designed to help create comprehensive care plans for families and enhance overall well-being.
Client Questionnaire Template
Efficiently gather medical client information with our concise Client Questionnaire Template designed for healthcare professionals. Download now!
Healthcare Practitioner Form
Get Carepatron's free PDF download of a healthcare practitioner form and an example to streamline administrative tasks. Perfect for healthcare professionals looking to improve efficiency.
MOST Medical Form
Discover the essential guide to the MOST Medical Form, including a comprehensive overview and a free PDF example. Ideal for healthcare professionals and users.
Home Care Form
Optimize your healthcare with our Home Care Form, ensuring streamlined processes and personalized care. Improve efficiency today!
Dental Medical Clearance Form
Learn how a Dental Medical Clearance Form works. Download a free PDF template and sample for your practice.
Blood Test for Depression
Learn about blood tests for depression and download Carepatron's free example in PDF format to understand the process better.
Preparticipation Physical Evaluation Form
Download a free Preparticipation Physical Evaluation Form and an example. Streamline your practice documentation with Carepatron's customizable template.
Foot Stress Fracture Test
Learn how to perform the Foot Stress Fracture Test. Download a free PDF template to document your findings and notes.
ADA Blood Sugar Log
Learn about the ADA Blood Sugar Log and how it helps manage diabetes. Download a free PDF and sample here.
Nursing assessment for pneumonia
Learn the importance of nursing assessments in managing pneumonia. Get a free PDF Nursing Assessment for Pneumonia form here.
Vertigo Test
Assess for vertigo with our comprehensive Vertigo Test. Quick, accurate evaluation for symptoms like dizziness and balance issues.
Circulation Assessment
Learn about the circulatory system, its significance, and how to conduct a comprehensive Circulation Assessment using our free template example.
Vitamin Chart
Discover the importance of vitamins for optimal health with our comprehensive Vitamin Chart. Learn about functions, sources, and dietary recommendations.
Medical Needs Form
Download Carepatron's free PDF example of a Medical Needs Form to help organize and track important medical information for individuals. Keep your medical needs organized with this helpful form.
Conduct Disorder Test
Assessing conduct disorder in individuals is crucial for effective intervention. Download Carepatron's free PDF example of a Conduct Disorder Test and learn how to use it effectively.
Women's Daily Nutritional Requirements Chart
Download Carepatron's free PDF chart outlining women's daily nutritional requirements, including examples of a balanced diet to help you meet your dietary needs effectively.
Maximum Heart Rate Chart
Maximize your fitness routine with our Maximum Heart Rate Chart template. Use it to monitor your heart rate and enhance your workout effectiveness safely!
Immunization Form
Streamline school health compliance with our Immunization Form template, designed to track student vaccinations and ensure a safe learning environment.
Work Physical Form
Enhance workplace safety and compliance with our Work Physical Form template, designed for healthcare professionals to assess employee fitness for work.
Nurse Practitioner Collaborative Agreement Template
Streamline nurse practice collaboration with our template—clear agreements for seamless teamwork in healthcare. Download now!
Orthorexia Test
Assess your relationship with food and well-being with our Orthorexia Test. Download the template now for a balanced approach to nutrition.
Home Health Documentation
Download our free Home Health Documentation template to help you with your document needs. Learn the importance of good home health documentation.
Medical Prior Authorization Form
Learn the importance of prior authorization for your patients. Download a free Medical Prior Authorization Form to simply insurance requests.
Daycare Physical Form
Learn the importance of physical exams for daycare. Download a free Daycare Physical Form to document a child's health records.
Psychology Career Test
Take this test to determine your suitability in the role of a psychologist. Use this template as a self test or with clients considering new occupational roles.
Time Lapse Assessment
Download our Time Lapse Assessments for holistic patient care. Learn how tracking changes over time enhances early intervention and personalized treatment plans.
EMT Practice Scenarios
Discover EMT practice scenarios that can support your emergency staff to refine their skills and knowledge as well as enhance their practical skills.
Inpatient Billing Cheat Sheet
Unlock efficient inpatient billing with our Cheat Sheet. Streamline CPT coding, enhance accuracy, and ensure timely reimbursements. Download now!
Pregnancy Verification Letter
Get your pregnancy confirmed with our Pregnancy Verification Letter. Official proof of pregnancy with physician validation simplified!
Normative Test
Discover the essence of normative testing in a concise guide exploring its principles, significance, and applications.
Hearing Test Frequency
Prioritize your hearing health today! Download our free Hearing Test Frequency example for personalized recommendations on monitoring your auditory well-being.
Pancreas Blood Test
Learn more about the Pancreas Blood Test and obtain a template you can use to request and record the results of this assessment.
Neuro Eye Exam
A neuro eye exam is a comprehensive assessment of the visual system to diagnose and manage neurological conditions. Download Carepatron's neuro eye exam PDF to learn more about it.
Discover how to diagnose and manage Small Intestinal Bacterial Overgrowth with our comprehensive SIBO Test Template, designed for healthcare professionals.
Diagnosis Template
Unlock streamlined diagnosis with our template. Ideal for healthcare pros seeking accurate patient assessments. Download now for comprehensive care.
Medicare Private Contract
Explore Medicare Private Contracts: key agreements for medical practitioners opting out of Medicare, ensuring clarity & compliance.
Chiropractic Business Plan
Our Chiropractic Business Plan guide is designed to help you navigate the competitive landscape, optimize operations, and maximize profitability in your chiropractic practice.
Urgent Care Form
Streamline patient check-in and expedite care with our Urgent Care Form template, designed to efficiently gather vital patient information.
Discover the key aspects of an ENT Exam with our comprehensive template, designed for health professionals to assess ear, nose, and throat health effectively.
Home Safety Assessment
Ensure a safer home environment with our comprehensive Home Safety Assessment. Identify potential hazards and take proactive steps for peace of mind.
Dysphagia Care Plan
Optimize patient outcomes with our free Dysphagia Care Plan template. Streamline care delivery for individuals with swallowing difficulties.
Community Health Improvement Plan
Discover how Community Health Improvement Plans (CHIPs) address community health needs strategically for effective outcomes and better population health.
Assess dysphagia with EAT-10: 10-question tool, which predicts aspiration and risk factors and evaluates swallowing disorders. Streamline care and improve outcomes.
Pediatric Assessment
Learn the essentials of pediatric assessment with Carepatron's free PDF download. Get examples and practical guidance for assessing pediatric patients to enhance your skills and knowledge.
Patient Discharge Form
Access a free Patient Discharge Form for easy clinical documentation. Download the PDF template and example now!
Nutrition SOAP Note
Get our free Nutrition SOAP Notes template now! Optimize your nutrition practice with structured documentation. Download here!
Randot Test
Discover the Randot Test and understand how it evaluates stereopsis, suitable age groups, conditions diagnosed, accuracy, and alternatives.
9-Panel Drug Test
Discover the comprehensive 9-panel drug test that screens 9 substances, including marijuana & cocaine. Learn more!
Caregiver Note Template
Access our comprehensive Caregiver Note Template for organized healthcare documentation. Simplify caregiving with our efficient solution.
South Oaks Gambling Screen
Explore the South Oaks Gambling Screen (SOGS) for identifying gambling disorders. Designed for diagnosing and managing gambling-related issues.
Microblading Consent Form
Discover the essential Microblading Consent Form for healthcare professionals and aestheticians, ensuring informed consent and legal compliance.
Medical Consent Form
Get access to a free Medical Consent Form template. Learn its importance in upholding your patients' rights.
Unlock precise and effective EM coding with our free template. Streamline documentation, select accurate codes, and ensure proper reimbursement. Download now!
Patient Follow Up Template
Streamline patient follow-up with our template. Schedule appointments, update medical history, and ensure continuity of care effortlessly!
Nutrition Care Plan
Developing a nutrition care plan is crucial for individuals to improve their health and well-being. Download Carepatron's free nutrition care plan PDF example here.
Diabetes Teaching Plan
Here's a comprehensive Diabetes Teaching Plan with essential blood sugar management information, diabetes education, and patient outcomes. Download now!
General Survey Nursing
Access Carepatron's free PDF download of a General Survey Nursing example to help you understand and improve your nursing assessment skills.
Emergency Nursing Assessment
Learn about the role of emergency nurses and the importance of conducting assessments. Download a free Emergency Nursing Assessment template today!
Otoscope Examination
Learn how to perform an otoscope examination and see an example with our Carepatron's free PDF download.
Ultrasound Test
Are you looking for examples of ultrasound tests? Download Carepatron's free PDF with sample ultrasound test questions to help you prepare for your upcoming exam.
Private Practice Startup Checklist
Launch your practice quickly using our comprehensive Private Practice Startup Checklist. Download for free!
Gallbladder Physical Exam
Learn about the physical exam for the gallbladder, including techniques and examples. Download Carepatron's free gallbladder physical exam PDF guide for reference.
Refusal Skills Worksheet
Develop assertive communication and decision-making with our Refusal Skills Worksheet. Practice strategies to navigate peer pressure and prioritize well-being.
Join 10,000+ teams using Carepatron to be more productive
CASE REPORT article
Case report: iatrogenic tattoos caused by skin marking pen in a postoperative patient provisionally accepted.

- 1 West China Hospital, Sichuan University, China
- 2 West China Fourth Hospital of Sichuan University, China
The final, formatted version of the article will be published soon.
In this report, a female patient suffering from pigment retention caused by a skin marking pen was elucidated. The patient underwent blepharoplasty 6 months ago and presented with blue-black linear marks at the upper eyelid incision 2 weeks after surgery. Under dermoscopy, scattered pigments were observed to accumulate in the epidermis of the upper eyelid. The patient was diagnosed with iatrogenic tattoo by a surgical marking pen. We chose surgical excision of the skin with the pigmentation. Previous studies have established that the risk of bacterial contamination, contact dermatitis, and allergies may increase with the surgical marking pens, while pigment retention has not yet been mentioned yet. Here, we present a case with a pigment retention in the incision. The selection of the surgical labelling methods and the management of the pigmentation were also addressed. According to our clinical findings, the risk of pigment retention by marking pens needs to be mentioned in the patient's informed consent. Therefore, the practitioner should ensure that the ink is cleaned by the end of each invasive procedure.
Keywords: Surgical complication, Pigmentation and colour, dermatosurgery, Tattoo, iatrogenic accident
Received: 18 Feb 2024; Accepted: 25 Mar 2024.
Copyright: © 2024 Zhao, Wu, Yu and Cao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Dr. Chang Cao, West China Hospital, Sichuan University, Chengdu, China
People also looked at
- Share full article
Advertisement
Supported by
Taxpayers Were Overcharged for Patient Meds. Then Came the Lawyers.
A group of politically connected lawyers teamed up to go after insurers and made millions from one of the largest Medicaid settlements in history.

By Shalina Chatlani
Shalina Chatlani examined the health care system in Mississippi as a part of The Times’s Local Investigations Fellowship .
In 2018, when Mike DeWine was Ohio’s attorney general, he began investigating an obscure corner of the health care industry.
He believed that insurers were inflating prescription drug prices through management companies that operated as middlemen in the drug supply chain. There were concerns that these companies, known as pharmacy benefit managers, or P.B.M.s, were fleecing agencies like Medicaid, the government-run health insurance program for the poor.
Three years later, after Mr. DeWine became governor of Ohio, the state announced an $88 million settlement with one of the nation’s largest insurance companies, Centene.
The case led to a nationwide reckoning for the company, as attorneys general in one state after another followed Ohio’s lead, announcing multimillion-dollar settlements and claiming credit for forcing Centene to reform its billing practices.
On the surface, it appeared that these settlements, which now total nearly $1 billion, were driven by state governments cracking down on a company that had ripped off taxpayers.
But a New York Times investigation, drawing on thousands of pages of court documents, emails and other public records in multiple states, reveals that the case against Centene was conceived and executed by a group of powerful private lawyers who used their political connections to go after millions of dollars in contingency fees.
The lawyers were first hired in Ohio, without competitive bidding. Then, they gathered evidence against Centene of questionable billing practices across the country.
Using information they acquired from Centene and other sources, they negotiated with the company to set the basic framework of an agreement that could be applied in other states. With that in hand, they approached attorneys general in multiple states and made a compelling offer: hire them, at no direct cost to taxpayers, and recoup millions of dollars Centene had already set aside.
So far, the lawyers have been awarded at least $108 million in fees.
The Centene case is just one example in a thriving industry that allows private lawyers to partner with elected attorneys general and temporarily gain powers usually reserved for the government. Under the banner of their state partners, these lawyers sue corporations and help set public policy while collecting millions of dollars in fees, usually based on a percentage of whatever money they recoup. The practice has become standard fare in the oversight of major industries, shifting the work of accountability away from legislators and regulators to the opaque world of private litigation.
Private lawyers do not have to publicly defend the deals they make or prove how aggressively they went after a company accused of wrongdoing. Nearly all their work happens in secret, especially if companies settle before the stage of a lawsuit when evidence is filed with the court.
The lawyers do not even have to disclose who worked on a case or who was paid, so the public may be left unable to monitor potential conflicts of interest even as the lawyers pursue litigation on behalf of the people.
The Centene case was organized by the Mississippi-based law firm Liston & Deas along with at least three other firms, several with close ties to former Gov. Haley Barbour of Mississippi, who was once considered one of the most influential Republican power brokers in the nation.
The lawyers included Paul Hurst, who served as Mr. Barbour’s chief of staff when he was governor and who married into Mr. Barbour’s family, and David H. Nutt, one of the richest men in Mississippi, who amassed a fortune funding state lawsuits against tobacco companies. Cohen Milstein, a huge national law firm with deep experience in contingency work for state attorneys general, was also part of the venture.
Though he is not listed in any government contracts as a lawyer of record, Mr. Barbour himself was a member of the legal team when Liston & Deas vied for the contract in Ohio.
At the time, Mr. Barbour also worked for Centene as a federal lobbyist .
Even now, close to three years after Centene signed its first settlements, no one has fully explained Mr. Barbour’s role in the case for the company. There is no way for the public to know whether he influenced the outcome or to measure whether Centene paid its full share, because the data used to calculate what Centene overcharged remains hidden from the public under provisions designed to protect attorney work product.
Mr. Barbour and other lawyers said that the former governor worked on the case for less than a year when the group was examining several insurance companies, and that he cut ties when Centene emerged as the primary target. Mr. Barbour said he informed Centene and his colleagues about the development and was never involved in negotiations or legal matters. He continued representing Centene as a lobbyist, he said, but his role in the case on behalf of the company was as “more of an observer.”
The lawyers said that Mr. Barbour was never paid for his work and that the settlement was not influenced by Mr. Barbour’s connections to Centene or to the lawyers who remained. They said each state attorney general reviewed Centene’s billing practices when deciding whether to enter a settlement agreement.
Got a confidential news tip?
The New York Times would like to hear from readers who want to share messages and materials with our journalists.
In recent years, P.B.M.s have been widely criticized , including by members of Congress, who have held multiple hearings and proposed legislation. The Centene settlements stand as the most successful attempt to hold a company operating in the industry accountable.
Liston & Deas and its partner law firms uncovered that Centene had arranged discounts with CVS Caremark on certain drugs and then pocketed the savings instead of passing them on to Medicaid. In some states, they revealed that Centene layered on unnecessary management fees that it had not disclosed. Although Centene settled without admitting guilt, the company agreed to be more transparent in how it sets reimbursement rates.
The lawyers noted that they spent several years investigating Centene and negotiating with the company at their own risk, saving states the cost of building a case.
Mr. Nutt, one of the lawyers who pursued the case, said states were happy with the terms of the settlements.
“Almost every one of those states audited to determine if our damage model was fair,” Mr. Nutt said.
“The formula was based on a triple damages model that we developed. And everybody was quite satisfied with it, because it was three times what anybody could have proven in court.”
Hiring Outside Counsel
For most of their history, state attorneys general were largely focused on advising state officials on legal matters and representing local agencies in court.
That changed drastically almost 30 years ago, when states came together to sue tobacco companies and won a $206 billion settlement to cover the cost of medical care related to smoking. The lawsuit helped redefine the role of the attorney general as one of the most powerful positions in state government and a natural place to start a political career.
Through high-profile lawsuits against corporations, an attorney general could directly affect policy and build a reputation as a champion of the people.
But complex litigation against large companies can require years of investigation and legal work, with no guarantee of success. Increasingly, states have turned to private lawyers willing to work on contingency as a way to stretch limited resources.
The rise of contingency fee cases kicked off a new wave of lobbying across the nation. Law firms looking for contracts have poured money into attorney general election campaigns and sponsored conferences at high-priced resorts, where private lawyers mingle with attorneys general and pitch their latest ideas for lawsuits.
Many states have capped how much lawyers can be paid in contingency fees and have increased oversight of private firms working for the government. But there remains concern about undue political influence and potential conflicts of interest.
“In theory, there’s an incentive to have the settlement be as big as possible, and of course that’s great for the state,” said Paul Nolette, a professor at Marquette University who has studied how the role of attorneys general has changed over time.
But in reality, lawyers have an incentive to recover the largest amount of money in the shortest amount of time, which could pressure them to water down settlements and compromise on punitive measures, Dr. Nolette said.
“I think that does raise some questions about how forcefully A.G.s and private attorneys are prosecuting a particular case,” he said.
Several experts said that contingency cases had recouped billions of dollars on behalf of the public and had become a critical way to regulate the behavior of powerful industries and large corporations.
But inviting private lawyers to help set public policy has inherent risks, they said.
Private lawyers may be more likely to have conflicts of interest because they generally represent many businesses and individuals, not just the citizens of a state.
And unlike most attorneys general, private lawyers are not elected officials. They are not generally governed by open records laws or subject to public pressure, as from legislators setting their budgets.
In the Centene case, Mr. Barbour’s associations with both Centene and the private lawyers raise “important questions” about who controlled the case to make sure it was pursued in the best interests of states that settled, said Kathleen Clark, a professor of legal ethics at Washington University in St. Louis.
“Did state A.G.s proactively pursue these cases, or did they passively accept the ‘free money’ or ‘easy money’ of the proposed settlements that the law firms had already negotiated with Centene?” Ms. Clark asked.
Christina Saler, a partner at Cohen Milstein, said Mr. Barbour’s early association with the legal team was not a conflict of interest because Mr. Barbour withdrew from the case before lawyers started investigating Centene.
“After Mr. Barbour’s disassociation, we had no further contact with Mr. Barbour on this matter,” she said.
A Well-Connected Team
Mr. Barbour’s involvement in the Ohio case against P.B.M.s illustrates the potential for favoritism when states hire private lawyers.
Mr. Hurst noted the involvement of Mr. Barbour when seeking the contract in Ohio, according to emails acquired from the Ohio attorney general’s office through a public records request.
In a June 22, 2018, email exchange, just a few days before the state hired Liston & Deas, Mr. Hurst recalled meeting with the attorney general’s staff in Ohio.
Mr. Hurst went on to note that members of his team had worked with Governor Barbour while he was in office and that they all “continue to work together now.”
In an email a week later, an assistant attorney general shared Mr. Barbour’s cell number with Mr. DeWine, saying that Mr. Barbour had shared it so he could “call him about this case anytime.”
Mr. Barbour, who had served two terms as governor of Mississippi, was a former chairman of the Republican Governors Association and a former chairman of the Republican National Committee. Known as a prolific fund-raiser , he was credited with bringing in hundreds of millions of dollars to support Republican candidates across the nation.
In 1991, Mr. Barbour co-founded BGR Group, a lobbying firm that quickly became one of the most influential in Washington.
Mr. Barbour had known Mr. DeWine since he was first elected to the Senate in 1995.
Two decades later, when Mr. DeWine was in the midst of a hard-fought campaign for governor, Mr. Barbour’s close associates solicited him for the legal work on the Centene case. In October 2018, less than three months after Mr. DeWine hired Liston & Deas, he traveled to Washington to visit Mr. Barbour’s lobbying firm for several hours, according to calendar records.
At the time, Mr. Barbour and others at BGR were registered lobbyists for Centene.
Mr. Barbour has never been named in state contracts as one of the private lawyers on the case in Ohio or anywhere else. His involvement has rarely, if ever, been publicly reported.
Ms. Saler, of Cohen Milstein, said there was no need to inform state officials because Mr. Barbour had not been involved in the Centene portion of the case and had exited the venture several years before states hired the lawyers.
At least four law firms were involved in the case in two or more states, according to retainer agreements and financial records showing broadly how settlement funds were disbursed.
According to Max Littman, a former data analyst with HealthPlan Data Solutions, the analytics firm that helped identify Centene’s overcharges in Ohio, one important role for many of the lawyers was to use their connections as they presented the overcharges to various states.
Mr. Littman, who said he worked closely with the legal team, described the dynamic: Liston & Deas, with roots in a deeply red state, would approach Republican attorneys general, and Cohen Milstein, “who were our Democrats,” would focus on Democratic states.
When The Times asked for records showing Liston & Deas’s qualifications to be hired to represent the State of Ohio, the attorney general’s office said no records existed. Cohen Milstein and other law firms had submitted such documentation in the past when seeking contracts in Ohio.
Settling With States
In June 2021, nearly three years after Ohio hired its outside counsel, two states announced the first settlements with Centene on the same day: Ohio would get $88 million, Mississippi $55 million.
After that, Centene settled in one state after another, often with just months between announcements.
In fact, Centene had already set aside $1.1 billion to handle all subsequent cases. The company estimated the amount after early discussions with the private lawyers that did not involve the state attorneys general who would later work with them.
With a settlement in hand and an estimate of how much each state could collect, the private lawyers had a powerful pitch. The team also had the option to file whistle-blower lawsuits, which can advance without a state attorney general’s having to hire outside counsel.
The team pursued whistle-blower lawsuits in Texas, California and Washington.
In Texas, the whistle-blower lawsuit came with a benefit for Attorney General Ken Paxton: Under Texas law , his office is allowed to recoup “reasonable attorney’s fees” for work associated with such cases. It collected nearly $25 million in legal fees on the Centene case while spending just 561 hours on it, financial records show. That comes out to more than $44,000 per hour of work. The Texas attorney general’s office declined to comment.
Ms. Saler said all the state attorneys general decided their own strategies in reaching settlements with Centene based on the best interest of taxpayers in their states.
In states that hired the lawyers on contingency, the attorney general closely reviewed Centene’s billing practices. But no state has revealed whether its own overcharge calculations matched those of the private lawyers.
State officials who hired Liston & Deas and the other firms knew that the lawyers had previously negotiated with Centene. But in a vast majority of states, officials did not explicitly address that fact when talking publicly about the settlements.
In addition, Liston & Deas and most of the states the firm worked for have not revealed exactly how much Centene overcharged for drugs or how settlement amounts were calculated. A few states have offered sparse descriptions, which vary widely.
The New Hampshire attorney general’s office wrote in its settlement announcement that Centene’s activities had a “$2.4 million negative financial impact.” Centene agreed to pay the state nearly 10 times that amount.
The attorney general’s office in Washington, one of the few states where officials agreed to discuss basic details about the settlement with The Times, said the $33 million it recovered amounted to treble damages.
A news release from the California attorney general’s office said the state recovered double its damages, for a total settlement of more than $215 million.
As of last month, Centene had settled in at least 19 states. The Liston & Deas website says Centene will ultimately pay about $1.25 billion to 22 states.
A Sweetheart Deal?
Some observers believe Centene would have faced stricter penalties if the federal government had taken up the case instead of private lawyers hopscotching from one state to the next.
Several experts in health care fraud litigation and whistle-blower cases said the best way to recoup money for taxpayers would have been to file a federal whistle-blower case, similar to what the lawyers did in state court in Texas and California.
A federal case could have triggered the involvement of the Justice Department, which might have investigated Centene more thoroughly. And a federal case probably would have gotten more attention and media coverage, required more transparency and taken longer to complete, the experts said.
Mr. Hurst and other lawyers in the case said they had not filed any type of federal action against Centene.
A spokesperson for the Justice Department confirmed that it had inquired about the P.B.M. and Centene cases in Ohio, but no further federal action was taken. The department declined further comment.
Mary Inman, a lawyer at Whistleblower Partners L.L.P. with decades of experience, said one of the reasons Liston & Deas wound up in state court might have been that its case relied on whistle-blowers the federal government was unlikely to approve.
The whistle-blower in Texas was Mr. Hurst. In California, the whistle-blower was Matthew McDonald, a lawyer at David Nutt & Associates and the son of Bryan McDonald, who worked in Mr. Barbour’s administration when he was governor.
Ms. Inman said whistle-blowers are typically insiders with firsthand knowledge of wrongdoing who share information at some risk to themselves, not lawyers who gain information while on the job.
“It’s very unusual,” Ms. Inman said. “And it’s something that I, as a longtime lawyer in this space, I would not want to do because atmospherically and reputationally it doesn’t look great.”
Mr. Barbour said he believes everyone walked away from the settlements happy — including executives at Centene. As evidence, he cited the company’s stock performance.
“I can’t speak for them, but if I had agreed to pay a big settlement and my stock went up after the first day, I would think it was a pretty good settlement,” Mr. Barbour said.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health

Mapping the Patient’s Journey in Healthcare through Process Mining
Michael arias.
1 Department of Business Computer Science, Universidad de Costa Rica, San Ramón 111-4250, Costa Rica
2 Department of Clinical Laboratories, School of Medicine, Pontificia Universidad Católica de Chile, Santiago 8320000, Chile; [email protected]
Santiago Aguirre
3 Department of Industrial Engineering, School of Engineering, Pontificia Universidad Javeriana, Bogotá 110231, Colombia; oc.ude.anairevaj@erriugas
Felipe Cornejo
4 Department of Computer Science, School of Engineering, Pontificia Universidad Católica de Chile, Santiago 7820436, Chile; lc.cu@ojenrocaf (F.C.); lc.cu@numj (J.M.-G.); lc.cup.gni@socram (M.S.)
Jorge Munoz-Gama
Marcos sepúlveda, daniel capurro.
5 School of Computing and Information Systems, University of Melbourne, Victoria 3010, Australia; ua.ude.bleminu@orrupacd
Nowadays, assessing and improving customer experience has become a priority, and has emerged as a key differentiator for business and organizations worldwide. A customer journey (CJ) is a strategic tool, a map of the steps customers follow when engaging with a company or organization to obtain a product or service. The increase of the need to obtain knowledge about customers’ perceptions and feelings when interacting with participants, touchpoints, and channels through different stages of the customer life cycle. This study aims to describe the application of process mining techniques in healthcare as a tool to asses customer journeys. The appropriateness of the approach presented is illustrated through a case study of a key healthcare process. Results depict how a healthcare process can be mapped through the CJ components, and its analysis can serve to understand and improve the patient’s experience.
1. Introduction
Customer journey mapping (CJM) [ 1 ] is a well-known technique that focuses on assessing how customers interact with a company or organization. This allows the gain of a deeper knowledge about the customers’ perceptions, and becomes an essential tool to improve the overall customer experience (CX). This knowledge can be used to generate competitive advantage and satisfied customers [ 2 ]. Understanding each step required to complete a process (customer paths), and how customers interact with a company’s services throughout that journey are key aspects to assess customer needs, the ability to improve them, and the delivery of great products and services. During a journey, customers can interact with a company through different methods or channels (e.g., on-line, phone call, etc.), go through different stages, and face specific business context factors. Recently, companies in several industries embarked in a transformation to take advantage of the benefits of new digital technologies. This digital transformation may impact key business factors, customer relationships, as well as products, services and processes [ 3 ]. However, a primary limitation is that companies do not have enough knowledge about their customers or how their end-to-end processes look like [ 4 ].
Along with this digital transformation, and the data generated through digital interactions, two novel disciplines have emerged: process science and data science [ 5 ]. Process science combines knowledge from information technologies and management sciences, to run and improve operational processes (e.g., time or cost aspects) based on a model-driven perspective. Within this discipline, Business Process Management (BPM) [ 6 ]—a process-oriented discipline—can be used to enhance organizational processes, aiming to combine different approaches to execute the design, implementation, control, monitoring, and optimization of business processes. Data science seeks to turn data into real value (data-driven approach), by focusing on generating knowledge to improve processes from larger and smaller datasets [ 7 ].
As part of the process science discipline, there is an important data-oriented sub-discipline called process mining (PM), which can be used to enhance companies’ operational processes. The aim of PM is to extract knowledge about process execution from data stored in existing information systems [ 8 ]. This sub-discipline can be understood as a bridge between process science and data science. Process mining has been used in several industries including healthcare [ 9 ] and education [ 10 ], as well as in resource allocation or recommendations for business processes [ 11 ].
In healthcare, there is a particular interest in a correct and efficient execution of both clinical and business processes. However, it is widely known that healthcare processes are often challenging due to their complexity, dynamics, and sometimes owing to their ad-hoc nature and multiplicity of disciplines involved [ 12 ]. Hospitals usually embrace standards to ensure the quality of healthcare processes. As a consequence, the identification of typical and non-typical patient journeys, and the monitoring compliance (process deviations) with hospital policies and standards become a focus of interest. Disciplines such as process mining could be used to support those initiatives and provide valuable insights not only to improve our understanding of clinical processes, but also to influence their execution and efficiency [ 9 ].
In this paper, we use customer journey analysis as a method to map patients’ experience using process mining, which in turn guides the creation of key indicators to improve the patients’ satisfaction, based on multiple identified touchpoints during a specific healthcare process. We conduct a case study in which the CJM has been put into practice in two different scenarios based on an Emergency Room process.
2. Background
2.1. process mining in healthcare.
The provision of quality care to patients is the most relevant aspect in a healthcare process [ 5 ]. Process can either have a positive or negative impact on patient outcomes. Process mining provides the capability to study healthcare processes using data routinely stored in the electronic health records (EHRs). This can provide details about executed activities, their sequence, duration, and resources involved [ 9 ]. Using this information, stakeholders in healthcare environments can analyze and improve clinical processes. The order in which tasks can be performed and its resource allocation can be modified to improve clinical outcomes; clinical processes can be checked against recommended clinical guidelines to ensure adherence to best practices.
Process mining has been applied in several healthcare domains, using different techniques and diverse datasets, and on multiple clinical settings [ 9 ]. Process mining has shown good results in healthcare and its application can potentially be expanded to include additional uses.
2.2. Customer Journey Mapping
Improving the customer’s experience (CX) has become one of the priorities in numerous business contexts and industries [ 13 ]. According to a study by McColl-Kennedy et al. [ 2 ], there are multiple definitions of CX, but the authors highlight the importance of focusing on elements that create value (e.g., resources, activities, context, interactions, customer role), cognitive responses, and discrete emotions at different touchpoints throughout the customer’s interactions.
Customer Journey Mapping (CJM) has gained popularity among researchers and practitioners as a tool to obtain knowledge about customers and to understand better the customer experience. A CJM is a device that allows researchers to attain a deeper comprehension about experiences, the generation of specific metrics, and the understanding of how they interact throughout the different stages required to provide a product or service [ 14 ]. A CJM is a visual representation that shows the sequence of events that emerge during the interaction between a customer and a specific process. For example, in a customer service process, the customer interacts with several touchpoints and through different channels such as creating an on-line request, emailing support documents, receiving an email response, and completing a customer satisfaction survey using a mobile app (see Figure 1 ). Throughout the whole process, the customer engages with each activity (touchpoints), which can help the people involved in the process to understand all different stages in a journey that a customer may undertake.

Example of the sequence of frequent activities in a customer service process.
Primarily, CJMs allow organizations to track customer interactions and to inform decision-making processes on how they could be enriched [ 15 ].
2.3. Components of CJM (Customer Journey Mapping)
In a recent study [ 14 ], the authors conducted a literature review to clarify the most common components of CJM. The main components identified are: customer, journey, mapping, goal, touchpoint, timeline, channel, stage, experience, lens, and multimedia. Those components and their corresponding description are explained in Section 3 .
These components can be used to create a blueprint for a company’s products or services, giving companies a more comprehensive view about their work methods, processes, required information, technology used in their operations, and factors that could emerge in specific domains. These components can serve as an important technique to elicit the evaluation of the experience throughout the journey. They can help to identify less important touchpoints, to reveal what customer actually do, instead of what process’ owners think they do, to assess customer experience, and to promote strategic initiatives, among other uses [ 1 ].
CJM has been applied in multiple domains to improve existing products and services or to create new ones. Uses include mobile services [ 16 ], marketing [ 15 ], and libraries [ 17 ].
There are other process-oriented methods available not only to investigate customers’ interactions but also to assess their experiences based on customer interviews (CIT—Critical Incident Technique) [ 18 ], surveys considering the sequence of the customer touchpoints (SIT—Sequential Incident Technique) [ 19 ], or performing service walkthroughs (STA -Service Transaction Analysis-) [ 20 ]. Nevertheless, all of them involve the collection of new data. CJM using process mining can become a data-driven alternative to efficiently map customer journeys.
3. Process Mining in Healthcare as a Customer Journey Mapping Tool
According with Terragni and Hassani [ 21 ], only few studies have applied process mining in costumer journey analysis, making it an interdisciplinary field with great opportunity to conduct research in this background. Particularly, they proposed a novel approach for applying process mining techniques to web log customer journey analysis. Bernard and Andritsos [ 14 ] were the first authors to propose the application of process mining for a CJM, highlighting the potential of this discipline to analyze customer journeys. The authors proposed a customer journey exploration map using event logs and data analytics [ 22 ] as an opportunity to characterize hundreds or thousands of customer journeys at the same time. Bernard and Andritsos extended their work in [ 23 ], and developed a javascript-based tool that can handle process mining models to create a CJM at different levels of granularity; and additionally, they introduced the use of genetic algorithms to solve the problem of automatically building CJMs from event logs [ 24 ].
Process mining and patient journey has been studied before [ 25 , 26 ], but further studies are needed to fully understand the experience of the patient. Therefore, in this paper we address this research gap. In Section 2.3 , each of the main components of CJM (based on [ 14 ]) has been mentioned. In this section, those components are now mapped to each of their corresponding concepts in the healthcare domain and what they can mean for a process mining perspective as follow.
Customer : as we stated, the customer is the stakeholder who undertakes the journey. Considering the variety of existing healthcare processes and the people involved in their execution, three different customers categories can be identified [ 9 , 27 ]: patients, healthcare professionals, and healthcare administrators.
Journey: a customer journey should contain at least one journey. An event log [ 5 ] can be defined as a set of traces, each encompassing all the events performed in a particular process instance or a case. Journey Maps can be discovered from information stored in event logs. Moreover, a journey can be part of any healthcare process such as inpatient episodes [ 28 ]), outpatient visits, diagnostic test paths, telemedicine paths, and online patient portal paths [ 27 ].
Mapping: Process mining techniques are used in multiple industries, including healthcare, to create process maps [ 29 ]. There are dozens of discovering algorithms that focus on the control-flow perspective supported by distinct process mining tools; such as, ProM [ 30 ] (e.g., Heuristics Miner, and Fuzzy Miner), Disco [ 31 ] (interactive process map) and Celonis [ 32 ] (the flow of most frequent activities known as happy path).
Goal: allows, both organization and customer, to establish a common target to analyze with more detail the customer journey. It obtains the process ’As-Is’ representation, recognizes time constraints, identifies process bottlenecks, performs an organizational analysis (resource perspective), detects process deviations, reduces process complexity, among others, are typical examples of outcomes that can be obtained when applying process mining techniques [ 5 ] to analyze specific customer journey goals. From the healthcare point of view, the clinical outcome is the most relevant goal. These outcomes have a direct impact in changing the patient’s long-term quality of life.
Touchpoint: is a set of interactions (events) where a patient might be involved during the healthcare process (journey). Those interactions may include events such as: diagnose, treat, follow-up, and the application of preventative measures, thus with the intention of improving clinical outcomes [ 9 ].
Timeline: refers to an end-to-end timestamp [ 5 ] registered in order to track when the distinct touchpoints occur and it’s order.
Channel: depicts the method chosen by the customer to participate with the different touchpoints identified previously. Typical examples are: (i) Hospital Information Systems/Process Information Systems [ 33 ]/Electronic Patient Records (EPR) [ 34 ]/Electronic medical records (EMR); (ii) Patient Portal (Medical history, schedule appointments, message their physician, view bills and make payments all online) (iii) ePrescribing (sending prescriptions to pharmacies); among others.
Stage: touchpoints could be grouped into a cluster of activities (defined as stages or phases). Distinct techniques could be used to split the process into “sub-processes”, much like, using the own semantics of the process (decomposition manually), using Passages, applying Single-Entry Single-Exit (SESE) decomposition, or using generic decomposition approaches [ 35 ]. For instance, in a healthcare process, a cluster of “Registration” events or “Treatment Decision” events, as well as “Inpatient” and “outpatient” events could be identified and grouped.
Experience: aims to capture and evaluate stakeholder’s experience (e.g., healthcare professionals and patients) of different services. Positive or negative perceptions can be obtained through several mechanism such as: experts feedback [ 36 ], patients feedback using some of the multiple experience surveys available [ 37 ], quality of life and other patient centered measures (e.g., patient satisfaction, patient perceptions, patient engagement, patient participation, and patient preferences), staff observations, shadowing, video recording [ 38 ]. Using process mining techniques would allow process owners to monitor and analyze identified journeys, and to improve the user experience (e.g., identify Key Performance Indicators (KPIs) and metrics to increase patient satisfaction).
Lens: is a domain’s specific component that can be added and would represent particular elements of the process landscape. Lens might differ across different process scenarios. Some common examples are: environmental factors taking into account during healthcare process execution (e.g., pollution, weather, exposure to ultraviolet radiation), food hygiene, pests and vectors (e.g., mosquitoes), unhealthy housing, and waste management.
Multimedia: similar to other industries, important data can be extracted from different multimedia content that registered how the distinct process touchpoints are executed. Video recording [ 38 ], audio, multicast, and broadcast, are examples of traditional media that can be represented, stored, and transformed into event logs.
4. Case Study
To understand the importance of the application of CJM using process mining, a case study with two distinct scenarios have been carried out for different diagnostics. The first case study is for patients with Pneumonia, and the second case study is for patients with Acute Myocardial Infarction.
4.1. Context and Description
Both cases were conducted using historical data collected in a 500-bed teaching hospital located in Santiago, Chile and the study was approved by the institutional ethics committee (Id: 180504002). The historical data was extracted from the Hospital Information System and the Emergency Department’s Electronic Medical Record. Multiple activities can be executed on both settings (in the clinic or the Emergency Room), therefore the prefix “ER” will be used to differentiate them. Furthermore, it is relevant to mention that the project was reviewed and authorized by the hospital’s local human subject review board.
4.2. Data and Event Log Construction
The data was extracted in CSV format, and encompassed information about clinical episodes that took place between 2 January 2017 and 30 June 2018. The data includes 6715 cases, including 523,521 events executed, and eight main process activities. We found detailed information about patient demographics, clinical episodes, diagnoses, and timestamped process activities.
To create the event log, we considered the following features:
- Episode ID: corresponds to the episode identifier.
- Activity: refers to the phases that involved patient’s interactions with the clinical services.
- Episode diagnosis: patient diagnosis documented by the physician.
- Activity details: further details about the episode diagnosis registered by the physician.
- Timestamp:date of the activity performed.
- Age: patient’s age at the moment of the episode.
- Gender: patient’s gender.
To load the information into the selected process mining tool (see further details in Section 4.3 ), we executed a set of previous steps (see Figure 2 ) to perform a data configuration procedure to generate a proper data model which in turn allows to perform a detailed process analysis.

Steps followed for data processing and process analysis.
After the data was extracted we split it into two CSV files. The first file is identified as the event log that contained the case identifier plus some attributes (“Cases_EventLog”). In this event log the following fields were included: EpisodeID, gender, age, and episode diagnosis. Table 1 shows an extract of the “Cases_EventLog”.
Example of an event log at case identifier level.
The second event log ("Activities_EventLog") contains information about the process activities. We included following fields: EpisodeID, activity, timestamp and activity details. Table 2 shows an extract of the “Activities_EventLog”.
Example of the an event log at activity level.
Third, we uploaded both files into a data pool and, fourth, we created a new data model. This step involved adding the two files mentioned above, establishing the activity table and selecting the following columns: CaseId column (EpisodeID), activity column, and timestamp column. To finish the data model creation step, a entity-relation diagram was created. The EpisodeId was selected as a Foreign key between the source table (“Cases_EventLog”) and the target table (“Activities_EventLog”). Once the data model was created, the data was loaded into the analysis tool. Finally, in our sixth step, we execute the process analysis for both case studies presented in Section 4.4 and Section 4.5 .
4.3. Process Mining Tool
There are several tools that offer distinct techniques and algorithms to perform process mining analysis. For the case studies of this article, the Celonis platform [ 32 ] was selected. Celonis is a leader in Enterprise Performance Acceleration process mining software. This commercial platform has recently been renewed into an Intelligent Business Cloud and now provides a set of features grouped by distinct categories like Business Process Analytics, Action Engine, Event Log Collection, Machine Learning and Artificial Intelligence, and Process Automation, among others. We have chosen this tool mainly due to its capacity to handle complex processes together with the feature of being able to generate the most common path that cases follow—also known as “happy-path”—which not only helps us to identify touchpoints between the patient and the process, but it also visualizes and explores all the variants that have been discovered in the process. In addition, we have decided to take advantage of the process analytics features and capabilities that Celonis offers, in order to generate a set of analytic visualizations which helped us to explore the process in a more interactive way and to create valuable process KPIs regarding the selected episodes as explained below.
4.4. Case Study I: Pneumonia
In this first case study, process mining was used to find the patients’ journey map when they are diagnosed with Pneumonia.
Process Models and Journey Analysis
A process discovery algorithm was used to obtain the model that shows the different touchpoints and the patients’ journey that is presented in Figure 3 . In total there are 12 touchpoints where most of the cases (97 percent) start in the Emergency Room (ER) where laboratory exams, medical images and procedures are performed. Given the nature of the dataset, all patients required hospitalization and presented a median length of stay of 7 days (see Figure 4 ).

Pneumonia patients’ journey map.

Length of stay of patients who were 65 years of age or older.
A variant analysis was used to discover the different paths that patients go through on the healthcare process and their relationship with the length of stay. In the case of pneumonia the most common variant covers 28 percent of the total cases and has six touchpoints as shown in Figure 5 : ER (laboratory, images, medication, procedure) hospitalization and discharge with a medium length of hospitalization stay of 4 days.

Variant analysis for pneumonia patients.
With this analysis we found a relationship between the age, gender, length of stay and complexity of the process model, measured by number of variants. Patients between 65 and 76 years old, most of them men (64 percent) have an average of 12 days of hospital stay with 41 process variants (see Figure 6 ) in comparison, patients between 76 and 87 years old with a majority of woman (59 percent) had an average length of stay of 13 days with 66 process variants (see Figure 7 ), while patients between 87 and 100 years old with a majority of men (54 percent), had the highest average length of stay with 18 days among the three groups analyzed, and 36 process variants (see Figure 8 ). This highlights that older patients require additional touchpoints like medical images, laboratory exams and procedures, which can be translated into different patient journeys. Additionally, we found that the prevalence rate is first higher in the men’s age group of 65–76 with a 64%; then it switches over to the women’s age group of 76–87 with a 59%, and then higher again among the men’s group, this time those between 87 and 100 years old (see Table 3 ).

Length of stay of patients between 65 and 76 years of age.

Length of stay of patients between 76 and 87 years of age.

Length of stay of patients between 87 and 100 years of age.
A comparative summary of different pneumonia groups analyzed.
4.5. Case Study II: Acute Myocardial Infarction (AMI)
In this second case study, process mining was used to find the patients’ journey map when they are diagnosed with an AMI.
In this case the patient’s journey also starts in most of the cases (65 percent) with ER. In comparison with the pneumonia’s journey where most of the exams and medical images are performed in the Emergency Room, in the case of hearth stroke the exams and procedures are performed before or after the procedures that follows hospitalization as Figure 9 shows.

AMI patients’ journey map.
A relationship was found between the hospital length of stay and the number of variants and touchpoints. In cases with length of stay between 1 and 7 days, the number of variants is 50 and the most common path has five touchpoints as seen in Figure 10 .

Variant and short stay for AMI patients.
Cases with lengths of stay longer than 7 days tend to have more variants, in this case 54 and the path that covers 25 percent of observed cases has nine touchpoints it the patients journey ( Figure 11 ).

Variant and extended stay for AMI patients.
4.6. Lead to Key Indicators
A patient’s experience during healthcare is a key aspect of healthcare quality. Developing a visual display that presents how the process is executed and characterizing it according to distinct attributes would help to monitor the process more effectively and enable the implementation of improvement measures. Healthcare organizations should constantly seek to assess the patients’ perception of the services they receive. This dimension was not included in the customer journeys assessed since patient satisfaction was not available in the studied dataset. However, the inclusion of standard patient satisfaction surveys in CJM activities is strongly encouraged. As an example, the HCAHPS (Hospital Consumer Assessment of Healthcare Providers & Systems) survey assesses several dimensions of the patient’s experience [ 39 ]:
- Communication with healthcare professionals;
- Responsiveness of hospital staff;
- Operation of hospital units;
- Cleanliness of hospital facilities;
- Quiet environment;
- Discharge information;
- Amenities provided.
The assessment of those indicators (among others) would help clinicians and administrators to identify where the changes are required, to proactively test them and to assess the impact of those changes, and to determine the most effective ways to improve patient care, operational efficiency, and enhance process outcomes.
5. Discussion
CJM has become an interesting and relevant management technique with a clear set of concepts to understand and describe process paths from the customer point of view. One of the most relevant aspects is the capacity to provide a context for the different variables that affect the customer experience.
The use of process mining to generate customer journey maps has created a powerful analysis tool to understand how processes variants (paths) and touchpoints may affect the customer experience, as well to discover how end-to-end processes look like.
Specifically, in healthcare processes the concepts of CJM can be directly applied, contextualizing them in a much better and detailed way, so as to provide complementary information for the analysis of these processes. Adding complementary information will also allow users to include patients’ feedback to improve and enrich clinical processes. In the same way, it also allow healthcare experts to describe processes, not only using a conceptual process model, but also using real process paths and variants (what customers really do), including more frequent and less frequent touchpoints, analyzing process performance, and identifying process deviations. Based on a more detailed description, it becomes easier to discover process improvement opportunities.
When combining the application of CJM technique and process mining discipline on a real-life case study of a clinical process in a hospital in Santiago, Chile, it has become clear that routinely collected clinical data has the capability to reveal—with great detail— the multiple interactions (touchpoints) that a patient has when visiting the hospital. The CJ maps can be quickly generated from electronic healthcare record data and become a valuable visual tool that allows a detailed analysis on how patients interact during the attention process (end-to-end process), according to specific diagnoses, which may provide important details about the analyzed healthcare processes.
In addition to discovering the process using real-world-data, these methods can help to establish gaps between the expected and the real patient experience. Comparing the two case studies, it was found that the trajectories vary depending on the diagnosis, which serves as a useful input to understand relevant touchpoints and where the process could be improved.
The approach proposed in this article is novel as it is aimed at understanding the interaction between the patient and the emergency department at each touchpoint, using a systematic approach based on CJM. In [ 25 ], the control-flow perspective is analyzed, i.e., in which order patient care is performed in an emergency room. In [ 28 ], it is analyzed how different healthcare professionals interact to care for patients. In this article, these views are complemented, also taking into account the patient’s perspective. In [ 26 ], the customer journey is analyzed in a simplified and ad-hoc way; instead, the approach proposed in this article uses a systematic approach based on CJM techniques.
A key aspect in analyzing healthcare processes and generating key indicators is how the discovered model can be complemented with additional information. In both of our case studies, we were able to add demographic patient data such as age and gender. Adding more information to the study will broaden the possibilities of generating tailored and valuable indicators for each patient type.
One of the challenges that arises when using process mining to understand the CJM is to find the most effective method to measure the patient’s experience in order to link it with specific process paths. Typically, organizations obtain customer feedback by means of surveys, based on samples that lacks of the necessary respond rate to be reliable.
6. Limitations
In our study, we identified some limitations. First, the dataset did not include the outpatient component of the patient’s journey. Having access to the whole care continuum should provide a richer picture of the complete patient journey. Second, patient satisfaction surveys were not available in the included dataset, which limited our ability to assess the association between specific process variants and patient satisfaction. This dimension will be addressed in future work. Finally, in the presented case studies, the Lens and Multimedia components have not been evaluated since the event logs were generated from electronic medical records which only capture the clinical dimensions of the process.
7. Conclusions and Future Work
This article describes how to apply process mining techniques to understand patient journeys in healthcare, providing a new and complementary perspective for understanding and improving patient care. The proposed approach allows to analyze touchpoints in the lights of the patient and to understand the multiple variants or paths that appear in the customer journeys and how they could be related to the patient’s experience. It can be used to deal with complex processes, including those with multiple trajectories. We have been able to conduct a case study where we have applied the CJM technique to a real-life healthcare process, encouraging the creation of healthcare KPIs as an alternative to assess how healthcare units are achieving their goals in order to provide improvements on quality of care.
As future work, we would like to explore the application of additional process mining algorithms and techniques in order to gain knowledge from the control-flow perspective, but also from other process perspectives, such as the organizational perspective, to analyze the experience of a patient at each touchpoint and the interactions with clinical staff. Further, expanded case studies should be carried out, including the complete care continuum, to see the proper use of this vision and adjust the concepts if necessary. The incorporation of patient satisfaction represents a key challenge to work on.
Acknowledgments
We thank Jerome Geyer-Klingeberg and Celonis Academic Alliance for their support and material.
Abbreviations
The following abbreviations are used in this manuscript:
Author Contributions
All authors undertook research, writing and review tasks throughout this study. All authors have read and agreed to the published version of the manuscript.
This research was partially funded by the 16CTTS-66390 grant by the Chilean National Development Agency (CORFO).
Conflicts of Interest
The authors declare no conflict of interest.

IMAGES
VIDEO
COMMENTS
A case study of patient journey mapping to identify gaps in healthcare: Learning from experience with cancer diagnosis and treatment. Knowledge Management & E‐Learning‐An International Journal, 12 (4), 405-418. 10.34105/j.kmel.2020.12.022 [Google Scholar] Lam, M. (2018).
What differentiates data analysis in patient journey mapping studies from other qualitative or quantitative studies is the focus on describing, defining, or exploring the journey from a patient's, rather than a health service, perspective. ... The feasibility and potential use of case-tracked client journeys in primary healthcare: a pilot study.
Figure 1 shows a longitudinal patient journey map for AB, including the sequence of events, patient experience evaluation, and communication patterns. A patient journey map uses quantitative and qualitative data to visualize the patient experience from the patient's perspective ().Patient journey maps can be generated using a variety of techniques (8,9), can be used to identify problems, and ...
In this article the authors discuss a case study of a patient journey involving multiple care organizations, several health professionals and care in both Canada and the United States. By applying patient journey mapping a simplified version of such complexity can be presented in a visual and succinct way, allowing health professionals and ...
The lived experiences of a bone marrow transplant patient and caregiver's journey are embedded within the case study format. Researchers, employing interpretive phenomenology, invited patients and caregivers to share their stories about the bone marrow transplant journey through face-to-face interviews, questionnaires, written narratives, art ...
A "Patient Journey" is a personal testimony that reflects the needs of patients in two key reference documents—an accessible visual overview, supported by a detailed information matrix. The ...
A case study of a patient journey involving multiple care organizations, several health professionals and care in both Canada and the United States is discussed and implications of using patient journey mapping for improving cancer care and healthcare more generally are discussed. Journey mapping methods have a number of practical uses. One of the most promising applications in the area of ...
Purpose To understand how different methodologies of qualitative research are able to capture patient experience of the hospital journey. Methods A qualitative study of orthopaedic patients admitted for hip and knee replacement surgery in a 250-bed university hospital was performed. Eight patients were shadowed from the time they entered the hospital to the time of transfer to rehabilitation ...
The objective of this study is to use patient journey mapping to characterize home care clients and caregivers' experiences of home care services after transitioning from hospital to home. ... A case study of patient journey mapping to identify gaps in healthcare: Learning from experience with cancer diagnosis and treatment. Knowledge Manage ...
Background Healthcare professionals caring for chronically ill patients increasingly want to provide patient-centered care (PCC). By understanding each individual patient journey, they can significantly improve the quality of PCC. A patient journey consists of patient interactions, so-called touchpoints, with healthcare professionals distributed over three periods: pre-service, service, and ...
DOI: 10.3233/SHTI200326 Corpus ID: 219986357; Towards a Lean Process for Patient Journey Mapping - A Case Study in a Large Academic Setting @article{SijmEeken2020TowardsAL, title={Towards a Lean Process for Patient Journey Mapping - A Case Study in a Large Academic Setting}, author={Marieke Sijm-Eeken and Jaqueline Zheng and Linda W. P. Peute}, journal={Studies in health technology and ...
Case Study: Defining the Rare Disease Patient Journey to Support Commercialization of Therapy. May 6, 2022 5/6/22 ... A client specializing in gene therapy for a particular rare disease came to EVERSANA looking to better understand the patient journey identify and target their therapy to patients and healthcare providers. While frequently ...
Background Breast cancer is one of the most prevalent diseases in women. Prevention and treatments have lowered mortality; nevertheless, the impact of the diagnosis and treatment continue to impact all aspects of patients' lives (physical, emotional, cognitive, social, and spiritual). Objective This study seeks to explore the experiences of the different stages women with breast cancer go ...
In this article the authors discuss a case study of a patient journey involving multiple care organizations, several health professionals and care in both Canada and the United States. By applying patient journey mapping a simplified version of such complexity can be presented in a visual and succinct way, allowing health professionals and ...
In this paper a patient-specific case study is presented. It is a personal patient journey that involved a complex set of organizations, information systems and decision-making processes that spanned two countries, multiple healthcare contexts and the use of an array of information sources available to patients on the Internet across the WWW.
Case study: Understanding competitive dynamics at IQGEN-X. India-based IQGEN-X turned to Cortellis Generics Intelligence to aid in its strategic planning and improve ROI. ... "Our previous patient journey work was conducted in typical fashion - qualitative interviews with patients, maybe a quantitative study, but we really needed to ...
A nursing case study is a detailed examination of a patient's health condition, treatment plan, and overall care journey, specifically from the perspective of nursing practice. These case studies are essential components of nursing education and professional development, providing valuable insights into clinical scenarios and patient care ...
In this report, a female patient suffering from pigment retention caused by a skin marking pen was elucidated. The patient underwent blepharoplasty 6 months ago and presented with blue-black linear marks at the upper eyelid incision 2 weeks after surgery. Under dermoscopy, scattered pigments were observed to accumulate in the epidermis of the upper eyelid. The patient was diagnosed with ...
The Centene case is just one example in a thriving industry that allows private lawyers to partner with elected attorneys general and temporarily gain powers usually reserved for the government.
The first case study is for patients with Pneumonia, and the second case study is for patients with Acute Myocardial Infarction. 4.1. Context and Description ... Moon H., Han S.H., Chun J., Hong S.W. A design process for a customer journey map: A case study on mobile services. Hum. Factors Ergon. Manuf. Serv. Ind. 2016; 26:501-514. doi: 10. ...