- Election 2024
- Entertainment
- Newsletters
- Photography
- Personal Finance
- AP Buyline Personal Finance
- Press Releases
- Israel-Hamas War
- Russia-Ukraine War
- Global elections
- Asia Pacific
- Latin America
- Middle East
- March Madness
- AP Top 25 Poll
- Movie reviews
- Book reviews
- Personal finance
- Financial Markets
- Business Highlights
- Financial wellness
- Artificial Intelligence
- Social Media

Trans kids’ treatment can start younger, new guidelines say

This photo provided by Laura Short shows Eli Bundy on April 15, 2022 at Deception Pass in Washington. In South Carolina, where a proposed law would ban transgender treatments for kids under age 18, Eli Bundy hopes to get breast removal surgery next year before college. Bundy, 18, who identifies as nonbinary, supports updated guidance from an international transgender health group that recommends lower ages for some treatments. (Laura Short via AP)
FILE - Dr. David Klein, right, an Air Force Major and chief of adolescent medicine at Fort Belvoir Community Hospital, listens as Amanda Brewer, left, speaks with her daughter, Jenn Brewer, 13, as the teenager has blood drawn during a monthly appointment for monitoring her treatment at the hospital in Fort Belvoir, Va., on Sept. 7, 2016. Brewer is transitioning from male to female. (AP Photo/Jacquelyn Martin, File)
- Copy Link copied

A leading transgender health association has lowered its recommended minimum age for starting gender transition treatment, including sex hormones and surgeries.
The World Professional Association for Transgender Health said hormones could be started at age 14, two years earlier than the group’s previous advice, and some surgeries done at age 15 or 17, a year or so earlier than previous guidance. The group acknowledged potential risks but said it is unethical and harmful to withhold early treatment.
The association provided The Associated Press with an advance copy of its update ahead of publication in a medical journal, expected later this year. The international group promotes evidence-based standards of care and includes more than 3,000 doctors, social scientists and others involved in transgender health issues.
The update is based on expert opinion and a review of scientific evidence on the benefits and harms of transgender medical treatment in teens whose gender identity doesn’t match the sex they were assigned at birth, the group said. Such evidence is limited but has grown in the last decade, the group said, with studies suggesting the treatments can improve psychological well-being and reduce suicidal behavior.
Starting treatment earlier allows transgender teens to experience physical puberty changes around the same time as other teens, said Dr. Eli Coleman, chair of the group’s standards of care and director of the University of Minnesota Medical School’s human sexuality program.
But he stressed that age is just one factor to be weighed. Emotional maturity, parents’ consent, longstanding gender discomfort and a careful psychological evaluation are among the others.
“Certainly there are adolescents that do not have the emotional or cognitive maturity to make an informed decision,” he said. “That is why we recommend a careful multidisciplinary assessment.”
The updated guidelines include recommendations for treatment in adults, but the teen guidance is bound to get more attention. It comes amid a surge in kids referred to clinics offering transgender medical treatment , along with new efforts to prevent or restrict the treatment.
Many experts say more kids are seeking such treatment because gender-questioning children are more aware of their medical options and facing less stigma.
Critics, including some from within the transgender treatment community, say some clinics are too quick to offer irreversible treatment to kids who would otherwise outgrow their gender-questioning.
Psychologist Erica Anderson resigned her post as a board member of the World Professional Association for Transgender Health last year after voicing concerns about “sloppy” treatment given to kids without adequate counseling.
She is still a group member and supports the updated guidelines, which emphasize comprehensive assessments before treatment. But she says dozens of families have told her that doesn’t always happen.
“They tell me horror stories. They tell me, ‘Our child had 20 minutes with the doctor’” before being offered hormones, she said. “The parents leave with their hair on fire.’’
Estimates on the number of transgender youth and adults worldwide vary, partly because of different definitions. The association’s new guidelines say data from mostly Western countries suggest a range of between a fraction of a percent in adults to up to 8% in kids.
Anderson said she’s heard recent estimates suggesting the rate in kids is as high as 1 in 5 — which she strongly disputes. That number likely reflects gender-questioning kids who aren’t good candidates for lifelong medical treatment or permanent physical changes, she said.
Still, Anderson said she condemns politicians who want to punish parents for allowing their kids to receive transgender treatment and those who say treatment should be banned for those under age 18.
“That’s just absolutely cruel,’’ she said.
Dr. Marci Bowers, the transgender health group’s president-elect, also has raised concerns about hasty treatment, but she acknowledged the frustration of people who have been “forced to jump through arbitrary hoops and barriers to treatment by gatekeepers ... and subjected to scrutiny that is not applied to another medical diagnosis.’’
Gabe Poulos, 22, had breast removal surgery at age 16 and has been on sex hormones for seven years. The Asheville, North Carolina, resident struggled miserably with gender discomfort before his treatment.
Poulos said he’s glad he was able to get treatment at a young age.
“Transitioning under the roof with your parents so they can go through it with you, that’s really beneficial,’’ he said. “I’m so much happier now.’’
In South Carolina, where a proposed law would ban transgender treatments for kids under age 18, Eli Bundy has been waiting to get breast removal surgery since age 15. Now 18, Bundy just graduated from high school and is planning to have surgery before college.
Bundy, who identifies as nonbinary, supports easing limits on transgender medical care for kids.
“Those decisions are best made by patients and patient families and medical professionals,’’ they said. “It definitely makes sense for there to be fewer restrictions, because then kids and physicians can figure it out together.’’
Dr. Julia Mason, an Oregon pediatrician who has raised concerns about the increasing numbers of youngsters who are getting transgender treatment, said too many in the field are jumping the gun. She argues there isn’t strong evidence in favor of transgender medical treatment for kids.
“In medicine ... the treatment has to be proven safe and effective before we can start recommending it,’’ Mason said.
Experts say the most rigorous research — studies comparing treated kids with outcomes in untreated kids — would be unethical and psychologically harmful to the untreated group.
The new guidelines include starting medication called puberty blockers in the early stages of puberty, which for girls is around ages 8 to 13 and typically two years later for boys. That’s no change from the group’s previous guidance. The drugs delay puberty and give kids time to decide about additional treatment; their effects end when the medication is stopped.
The blockers can weaken bones, and starting them too young in children assigned males at birth might impair sexual function in adulthood, although long-term evidence is lacking.
The update also recommends:
—Sex hormones — estrogen or testosterone — starting at age 14. This is often lifelong treatment. Long-term risks may include infertility and weight gain, along with strokes in trans women and high blood pressure in trans men, the guidelines say.
—Breast removal for trans boys at age 15. Previous guidance suggested this could be done at least a year after hormones, around age 17, although a specific minimum ag wasn’t listed.
—Most genital surgeries starting at age 17, including womb and testicle removal, a year earlier than previous guidance.
The Endocrine Society, another group that offers guidance on transgender treatment, generally recommends starting a year or two later, although it recently moved to start updating its own guidelines. The American Academy of Pediatrics and the American Medical Association support allowing kids to seek transgender medical treatment, but they don’t offer age-specific guidance.
Dr. Joel Frader, a Northwestern University a pediatrician and medical ethicist who advises a gender treatment program at Chicago’s Lurie Children’s Hospital, said guidelines should rely on psychological readiness, not age.
Frader said brain science shows that kids are able to make logical decisions by around age 14, but they’re prone to risk-taking and they take into account long-term consequences of their actions only when they’re much older.
Coleen Williams, a psychologist at Boston Children’s Hospital’s Gender Multispecialty Service, said treatment decisions there are collaborative and individualized.
“Medical intervention in any realm is not a one-size-fits-all option,” Williams said.
Follow AP Medical Writer Lindsey Tanner at @LindseyTanner.
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Department of Science Education. The AP is solely responsible for all content.


Young Children Do Not Receive Medical Gender Transition Treatment
By Kate Yandell
Posted on May 22, 2023
SciCheck Digest
Families seeking information from a health care provider about a young child’s gender identity may have their questions answered or receive counseling. Some posts share a misleading claim that toddlers are being “transitioned.” To be clear, prepubescent children are not offered transition surgery or drugs.
Some children identify with a gender that does not match their sex assigned at birth. These children are referred to as transgender, gender-diverse or gender-expansive. Doctors will listen to children and their family members, offer information, and in some cases connect them with mental health care, if needed.
But for children who have not yet started puberty, there are no recommended drugs, surgeries or other gender-transition treatments.
Recent social media posts shared the misleading claim that medical institutions in North Carolina are “transitioning toddlers,” which they called an “experimental treatment.” The posts referenced a blog post published by the Education First Alliance, a conservative nonprofit in North Carolina that says many schools are engaging in “ideological indoctrination” of children and need to be reformed.

The group has advocated the passage of a North Carolina bill to restrict medical gender-transition treatment before age 18. There are now 18 states that have taken action to restrict medical transition treatments for minors .
A widely shared article from the Epoch Times citing the blog post bore the false headline: “‘Transgender’ Toddlers as Young as 2 Undergoing Mutilation/Sterilization by NC Medical System, Journalist Alleges.” The Epoch Times has a history of publishing misleading or false claims. The article on transgender toddlers then disappeared from the website, and the Epoch Times published a new article clarifying that young children are not receiving hormone blockers, cross-sex hormones or surgery.
Representatives from all three North Carolina institutions referenced in the social media posts told us via emailed statements that they do not offer surgeries or other transition treatments to toddlers.
East Carolina University, May 5: ECU Health does not offer gender affirming surgery to minors nor does the health system offer gender affirming transition care to toddlers.
ECU Health elaborated that it does not offer puberty blockers and only offers hormone therapy after puberty “in limited cases,” as recommended in national guidelines and with parental or guardian consent. It also said that it offers interdisciplinary gender-affirming primary care for LGBTQ+ patients, including access to services such as mental health care, nutrition and social work.
“These primary care services are available to any LGBTQ+ patient who needs care. ECU Health does not provide gender-related care to patients 2 to 4 years old or any toddler period,” ECU said.
University of North Carolina, May 12: To be clear: UNC Health does not offer any gender-transitioning care for toddlers. We do not perform any gender care surgical procedures or medical interventions on toddlers. Also, we are not conducting any gender care research or clinical trials involving children. If a toddler’s parent(s) has concerns or questions about their child’s gender, a primary care provider would certainly listen to them, but would never recommend gender treatment for a toddler. Gender surgery can be performed on anyone 18 years old or older .
Duke Health, May 12: Duke Health has provided high-quality, compassionate, and evidence-based gender care to both adolescents and adults for many years. Care decisions are made by patients, families and their providers and are both age-appropriate and adherent to national and international guidelines. Under these professional guidelines and in accordance with accepted medical standards, hormone therapies are explicitly not provided to children prior to puberty and gender-affirming surgeries are, except in exceedingly rare circumstances, only performed after age 18.
Duke and UNC both called the claims that they offer gender-transition care to toddlers false, and ECU referred to the “intentional spreading of dangerous misinformation online.”
Nor do other medical institutions offer gender-affirming drug treatment or surgery to toddlers, clinical psychologist Christy Olezeski , director of the Yale Pediatric Gender Program, told us, although some may offer support to families of young children or connect them with mental health care.
The Education First Alliance post also states that a doctor “can see a 2-year-old girl play with a toy truck, and then begin treatment for gender dysphoria.” But simply playing with a certain toy would not meet the criteria for a diagnosis of gender dysphoria, according to the medical diagnostic manual used by health professionals.
“With all kids, we want them to feel comfortable and confident in who they are. We want them to feel comfortable and confident in how they like to express themselves. We want them to be safe,” Olezeski said. “So all of these tenets are taken into consideration when providing care for children. There is no medical care that happens prior to puberty.”
Medical Transition Starts During Adolescence or Later
The Education First Alliance blog post does not clearly state what it means when it says North Carolina institutions are “transitioning toddlers.” It refers to treatment and hormone therapy without clarifying the age at which it is offered.
Only in the final section of the piece does it include a quote from a doctor correctly stating that children are not offered surgery or drugs before puberty.
To spell out the reality of the situation: The North Carolina institutions are not providing surgeries or hormone therapy to prepubescent children, nor is this standard practice in any part of the country.
Programs and physicians will have different policies, but widely referenced guidance from the World Professional Association for Transgender Health and the Endocrine Society lays out recommended care at different ages.
Drugs that suppress puberty are the first medical treatment that may be offered to a transgender minor, the guidelines say. Children may be offered drugs to suppress puberty beginning when breast buds appear or testicles increase to a certain volume, typically happening between ages 8 to 13 or 9 to 14, respectively.
Generally, someone may start gender-affirming hormone therapy in early adolescence or later, the American Academy for Pediatrics explains . The Endocrine Society says that adolescents typically have the mental capacity to participate in making an informed decision about gender-affirming hormone therapy by age 16.
Older adolescents who want flat chests may sometimes be able to get surgery to remove their breasts, also known as top surgery, Olezeski said. They sometimes desire to do this before college. Guidelines do not offer a specific age during adolescence when this type of surgery may be appropriate. Instead, they explain how a care team can assess adolescents on a case-by-case basis.
A previous version of the WPATH guidelines did not recommend genital surgery until adulthood, but the most recent version, published in September 2022, is less specific about an age limit. Rather, it explains various criteria to determine whether someone who desires surgery should be offered it, including a person’s emotional and cognitive maturity level and whether they have been on hormone therapy for at least a year.
The Endocrine Society similarly offers criteria for when someone might be ready for genital surgery, but specifies that surgeries involving removing the testicles, ovaries or uterus should not happen before age 18.
“Typically any sort of genital-affirming surgeries still are happening at 18 or later,” Olezeski said.
There are no comprehensive statistics on the number of gender-affirming surgeries performed in the U.S., but according to an insurance claims analysis from Reuters and Komodo Health Inc., 776 minors with a diagnosis of gender dysphoria had breast removal surgeries and 56 had genital surgeries from 2019 to 2021.
Research Shows Benefits of Affirming Gender Identity
Young children do not get medical transition treatment, but they do have feelings about their gender and can benefit from support from those around them. “Children start to have a sense of their own gender identity between the ages of 2 1/2 to 3 years old,” Olezeski said.
Programs vary in what age groups they serve, she said, but some do support families of preschool-aged children by answering questions or providing mental health care.
Transgender children are at increased risk of some mental health problems, including anxiety and depression. According to the WPATH guidelines, affirming a child’s gender through day-to-day changes — also known as social transition — may have a positive impact on a child’s mental health. Social transition “may look different for every individual,” Olezeski said. Changes could include going by a different name or pronouns or altering one’s attire or hair style.

Two studies of socially transitioned children — including one with kids as young as 3 — have found minimal or no difference in anxiety and depression compared with non-transgender siblings or other children of similar ages.
“Research substantiates that children who are prepubertal and assert an identity of [transgender and gender diverse] know their gender as clearly and as consistently as their developmentally equivalent peers who identify as cisgender and benefit from the same level of social acceptance,” the AAP guidelines say, adding that differences in how children identify and express their gender are normal.
Social transitions largely take place outside of medical institutions, led by the child and supported by their family members and others around them. However, a family with questions about their child’s gender or social transition may be able to get information from their pediatrician or another medical provider, Olezeski said.
Although not available everywhere, specialized programs may be particularly prepared to offer care to a gender-diverse child and their family, she said. A child may get a referral to one of these programs from a pediatrician, another specialty physician, a mental health care professional or their school, or a parent may seek out one of these programs.
“We have created a space where parents can come with their youth when they’re young to ask questions about how to best support their child: what to do if they have questions, how to get support, what do we know about the best research in terms of how to allow kids space to explore their identity, to explore how they like to express themselves, and then if they do identify as trans or nonbinary, how to support the parents and the youth in that,” Olezeski said of specialized programs. Parents benefit from the support, and then the children also benefit from support from their parents.
WPATH says that the child should be the one to initiate a social transition by expressing a “strong desire or need” for it after consistently articulating an identity that does not match their sex assigned at birth. A health care provider can then help the family explore benefits and risks. A child simply playing with certain toys, dressing a certain way or enjoying certain activities is not a sign they would benefit from a social transition, the guidelines state.
Previously, assertions children made about their gender were seen as “possibly true” and support was often withheld until an age when identity was believed to become fixed, the AAP guidelines explain. But “more robust and current research suggests that, rather than focusing on who a child will become, valuing them for who they are, even at a young age, fosters secure attachment and resilience, not only for the child but also for the whole family,” the guidelines say.
Mental Health Care Benefits
A gender-diverse child or their family members may benefit from a referral to a psychologist or other mental health professional. However, being transgender or gender-diverse is not in itself a mental health disorder, according to the American Psychological Association , WPATH and other expert groups . These organizations also note that people who are transgender or gender-diverse do not all experience mental health problems or distress about their gender.
Psychological therapy is not meant to change a child’s gender identity, the WPATH guidelines say .
The form of therapy a child or a family might receive will depend on their particular needs, Olezeski said. For instance, a young child might receive play-based therapy, since play is how children “work out different things in their life,” she said. A parent might work on strategies to better support their child.
One mental health diagnosis that some gender-diverse people may receive is gender dysphoria . There is disagreement about how useful such a diagnosis is, and receiving such a diagnosis does not necessarily mean someone will decide to undergo a transition, whether social or medical.
UNC Health told us in an email that a gender dysphoria diagnosis “is rarely used” for children.
Very few gender-expansive kids have dysphoria, the spokesperson said. “ Gender expansion in childhood is not Gender Dysphoria ,” UNC added, attributing the explanation to psychiatric staff (emphasis is UNC’s). “The psychiatric team’s goal is to provide good mental health care and manage safety—this means trying to protect against abuse and bullying and to support families.”
Social media posts incorrectly claim that toddlers are being diagnosed with gender dysphoria based on what toys they play with. One post said : “Three medical schools in North Carolina are diagnosing TODDLERS who play with stereotypically opposite gender toys as having GENDER DYSPHORIA and are beginning to transition them!!”
There are separate criteria for diagnosing gender dysphoria in adults and adolescents versus children, according to the Diagnostic and Statistical Manual of Mental Disorders. For children to receive this diagnosis, they must meet six of eight criteria for a six-month period and experience “clinically significant distress” or impairment in functioning, according to the diagnostic manual.
A “strong preference for the toys, games or activities stereotypically used or engaged in by the other gender” is one criterion, but children must also meet other criteria, and expressing a strong desire to be another gender or insisting that they are another gender is required.
“People liking to play with different things or liking to wear a diverse set of clothes does not mean that somebody has gender dysphoria,” Olezeski said. “That just means that kids have a breadth of things that they can play with and ways that they can act and things that they can wear . ”
Editor’s note: SciCheck’s articles providing accurate health information and correcting health misinformation are made possible by a grant from the Robert Wood Johnson Foundation. The foundation has no control over FactCheck.org’s editorial decisions, and the views expressed in our articles do not necessarily reflect the views of the foundation.
Rafferty, Jason. “ Gender-Diverse & Transgender Children .” HealthyChildren.org. Updated 8 Jun 2022.
Coleman, E. et al. “ Standards of Care for the Health of Transgender and Gender Diverse People, Version 8 .” International Journal of Transgender Health. 15 Sep 2022.
Rachmuth, Sloan. “ Transgender Toddlers Treated at Duke, UNC, and ECU .” Education First Alliance. 1 May 2023.
North Carolina General Assembly. “ Senate Bill 639, Youth Health Protection Act .” (as introduced 5 Apr 2023).
Putka, Sophie et al. “ These States Have Banned Youth Gender-Affirming Care .” Medpage Today. Updated 17 May 2023.
Davis, Elliott Jr. “ States That Have Restricted Gender-Affirming Care for Trans Youth in 2023 .” U.S. News & World Report. Updated 17 May 2023.
Montgomery, David and Goodman, J. David. “ Texas Legislature Bans Transgender Medical Care for Children .” New York Times. 17 May 2023.
Ji, Sayer. ‘ Transgender’ Toddlers as Young as 2 Undergoing Mutilation/Sterilization by NC Medical System, Journalist Alleges .” Epoch Times. Internet Archive, Wayback Machine. Archived 6 May 2023.
McDonald, Jessica. “ COVID-19 Vaccines Reduce, Not Increase, Risk of Stillbirth .” FactCheck.org. 9 Nov 2022.
Jaramillo, Catalina. “ Posts Distort Questionable Study on COVID-19 Vaccination and EMS Calls .” FactCheck.org. 15 June 2022.
Spencer, Saranac Hale. “ Social Media Posts Misrepresent FDA’s COVID-19 Vaccine Safety Research .” FactCheck.org. 23 Dec 2022.
Jaramillo, Catalina. “ WHO ‘Pandemic Treaty’ Draft Reaffirms Nations’ Sovereignty to Dictate Health Policy .” FactCheck.org. 2 Mar 2023.
McCormick Sanchez, Darlene. “ IN-DEPTH: North Carolina Medical Schools See Children as Young as Toddlers for Gender Dysphoria .” The Epoch Times. 8 May 2023.
ECU health spokesperson. Emails with FactCheck.org. 12 May 2023 and 19 May 2023.
UNC Health spokesperson. Emails with FactCheck.org. 12 May 2023 and 19 May 2023.
Duke Health spokesperson. Email with FactCheck.org. 12 May 2023.
Olezeski, Christy. Interview with FactCheck.org. 16 May 2023.
Hembree, Wylie C. et al. “ Endocrine Treatment of Gender-Dysphoric/Gender-Incongruent Persons: An Endocrine Society Clinical Practice Guideline .” The Journal of Clinical Endocrinology and Metabolism. 1 Nov 2017.
Emmanuel, Mickey and Bokor, Brooke R. “ Tanner Stages .” StatPearls. Updated 11 Dec 2022.
Rafferty, Jason et al. “ Ensuring Comprehensive Care and Support for Transgender and Gender-Diverse Children and Adolescents .” Pediatrics. 17 Sep 2018.
Coleman, E. et al. “ Standards of Care for the Health of Transsexual, Transgender, and Gender-Nonconforming People, Version 7 .” International Journal of Transgenderism. 27 Aug 2012.
Durwood, Lily et al. “ Mental Health and Self-Worth in Socially Transitioned Transgender Youth .” Journal of the American Academy of Child and Adolescent Psychiatry. 27 Nov 2016.
Olson, Kristina R. et al. “ Mental Health of Transgender Children Who Are Supported in Their Identities .” Pediatrics. 26 Feb 2016.
“ Answers to Your Questions about Transgender People, Gender Identity, and Gender Expression .” American Psychological Association website. 9 Mar 2023.
“ What is Gender Dysphoria ?” American Psychiatric Association website. Updated Aug 2022.
Vanessa Marie | Truth Seeker (indivisible.mama). “ Three medical schools in North Carolina are diagnosing TODDLERS who play with stereotypically opposite gender toys as having GENDER DYSPHORIA and are beginning to transition them!! … ” Instagram. 7 May 2023.
- Patient Care & Health Information
- Tests & Procedures
- Feminizing hormone therapy
Feminizing hormone therapy typically is used by transgender women and nonbinary people to produce physical changes in the body that are caused by female hormones during puberty. Those changes are called secondary sex characteristics. This hormone therapy helps better align the body with a person's gender identity. Feminizing hormone therapy also is called gender-affirming hormone therapy.
Feminizing hormone therapy involves taking medicine to block the action of the hormone testosterone. It also includes taking the hormone estrogen. Estrogen lowers the amount of testosterone the body makes. It also triggers the development of feminine secondary sex characteristics. Feminizing hormone therapy can be done alone or along with feminizing surgery.
Not everybody chooses to have feminizing hormone therapy. It can affect fertility and sexual function, and it might lead to health problems. Talk with your health care provider about the risks and benefits for you.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Available Sexual Health Solutions at Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
Feminizing hormone therapy is used to change the body's hormone levels. Those hormone changes trigger physical changes that help better align the body with a person's gender identity.
In some cases, people seeking feminizing hormone therapy experience discomfort or distress because their gender identity differs from their sex assigned at birth or from their sex-related physical characteristics. This condition is called gender dysphoria.
Feminizing hormone therapy can:
- Improve psychological and social well-being.
- Ease psychological and emotional distress related to gender.
- Improve satisfaction with sex.
- Improve quality of life.
Your health care provider might advise against feminizing hormone therapy if you:
- Have a hormone-sensitive cancer, such as prostate cancer.
- Have problems with blood clots, such as when a blood clot forms in a deep vein, a condition called deep vein thrombosis, or a there's a blockage in one of the pulmonary arteries of the lungs, called a pulmonary embolism.
- Have significant medical conditions that haven't been addressed.
- Have behavioral health conditions that haven't been addressed.
- Have a condition that limits your ability to give your informed consent.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
Stay Informed with LGBTQ+ health content.
Receive trusted health information and answers to your questions about sexual orientation, gender identity, transition, self-expression, and LGBTQ+ health topics. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing to our LGBTQ+ newsletter.
You will receive the first newsletter in your inbox shortly. This will include exclusive health content about the LGBTQ+ community from Mayo Clinic.
If you don't receive our email within 5 minutes, check your SPAM folder, then contact us at [email protected] .
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Research has found that feminizing hormone therapy can be safe and effective when delivered by a health care provider with expertise in transgender care. Talk to your health care provider about questions or concerns you have regarding the changes that will happen in your body as a result of feminizing hormone therapy.
Complications can include:
- Blood clots in a deep vein or in the lungs
- Heart problems
- High levels of triglycerides, a type of fat, in the blood
- High levels of potassium in the blood
- High levels of the hormone prolactin in the blood
- Nipple discharge
- Weight gain
- Infertility
- High blood pressure
- Type 2 diabetes
Evidence suggests that people who take feminizing hormone therapy may have an increased risk of breast cancer when compared to cisgender men — men whose gender identity aligns with societal norms related to their sex assigned at birth. But the risk is not greater than that of cisgender women.
To minimize risk, the goal for people taking feminizing hormone therapy is to keep hormone levels in the range that's typical for cisgender women.
Feminizing hormone therapy might limit your fertility. If possible, it's best to make decisions about fertility before starting treatment. The risk of permanent infertility increases with long-term use of hormones. That is particularly true for those who start hormone therapy before puberty begins. Even after stopping hormone therapy, your testicles might not recover enough to ensure conception without infertility treatment.
If you want to have biological children, talk to your health care provider about freezing your sperm before you start feminizing hormone therapy. That procedure is called sperm cryopreservation.
How you prepare
Before you start feminizing hormone therapy, your health care provider assesses your health. This helps address any medical conditions that might affect your treatment. The evaluation may include:
- A review of your personal and family medical history.
- A physical exam.
- A review of your vaccinations.
- Screening tests for some conditions and diseases.
- Identification and management, if needed, of tobacco use, drug use, alcohol use disorder, HIV or other sexually transmitted infections.
- Discussion about sperm freezing and fertility.
You also might have a behavioral health evaluation by a provider with expertise in transgender health. The evaluation may assess:
- Gender identity.
- Gender dysphoria.
- Mental health concerns.
- Sexual health concerns.
- The impact of gender identity at work, at school, at home and in social settings.
- Risky behaviors, such as substance use or use of unapproved silicone injections, hormone therapy or supplements.
- Support from family, friends and caregivers.
- Your goals and expectations of treatment.
- Care planning and follow-up care.
People younger than age 18, along with a parent or guardian, should see a medical care provider and a behavioral health provider with expertise in pediatric transgender health to discuss the risks and benefits of hormone therapy and gender transitioning in that age group.
What you can expect
You should start feminizing hormone therapy only after you've had a discussion of the risks and benefits as well as treatment alternatives with a health care provider who has expertise in transgender care. Make sure you understand what will happen and get answers to any questions you may have before you begin hormone therapy.
Feminizing hormone therapy typically begins by taking the medicine spironolactone (Aldactone). It blocks male sex hormone receptors — also called androgen receptors. This lowers the amount of testosterone the body makes.
About 4 to 8 weeks after you start taking spironolactone, you begin taking estrogen. This also lowers the amount of testosterone the body makes. And it triggers physical changes in the body that are caused by female hormones during puberty.
Estrogen can be taken several ways. They include a pill and a shot. There also are several forms of estrogen that are applied to the skin, including a cream, gel, spray and patch.
It is best not to take estrogen as a pill if you have a personal or family history of blood clots in a deep vein or in the lungs, a condition called venous thrombosis.
Another choice for feminizing hormone therapy is to take gonadotropin-releasing hormone (Gn-RH) analogs. They lower the amount of testosterone your body makes and might allow you to take lower doses of estrogen without the use of spironolactone. The disadvantage is that Gn-RH analogs usually are more expensive.
After you begin feminizing hormone therapy, you'll notice the following changes in your body over time:
- Fewer erections and a decrease in ejaculation. This will begin 1 to 3 months after treatment starts. The full effect will happen within 3 to 6 months.
- Less interest in sex. This also is called decreased libido. It will begin 1 to 3 months after you start treatment. You'll see the full effect within 1 to 2 years.
- Slower scalp hair loss. This will begin 1 to 3 months after treatment begins. The full effect will happen within 1 to 2 years.
- Breast development. This begins 3 to 6 months after treatment starts. The full effect happens within 2 to 3 years.
- Softer, less oily skin. This will begin 3 to 6 months after treatment starts. That's also when the full effect will happen.
- Smaller testicles. This also is called testicular atrophy. It begins 3 to 6 months after the start of treatment. You'll see the full effect within 2 to 3 years.
- Less muscle mass. This will begin 3 to 6 months after treatment starts. You'll see the full effect within 1 to 2 years.
- More body fat. This will begin 3 to 6 months after treatment starts. The full effect will happen within 2 to 5 years.
- Less facial and body hair growth. This will begin 6 to 12 months after treatment starts. The full effect happens within three years.
Some of the physical changes caused by feminizing hormone therapy can be reversed if you stop taking it. Others, such as breast development, cannot be reversed.
While on feminizing hormone therapy, you meet regularly with your health care provider to:
- Keep track of your physical changes.
- Monitor your hormone levels. Over time, your hormone dose may need to change to ensure you are taking the lowest dose necessary to get the physical effects that you want.
- Have blood tests to check for changes in your cholesterol, blood sugar, blood count, liver enzymes and electrolytes that could be caused by hormone therapy.
- Monitor your behavioral health.
You also need routine preventive care. Depending on your situation, this may include:
- Breast cancer screening. This should be done according to breast cancer screening recommendations for cisgender women your age.
- Prostate cancer screening. This should be done according to prostate cancer screening recommendations for cisgender men your age.
- Monitoring bone health. You should have bone density assessment according to the recommendations for cisgender women your age. You may need to take calcium and vitamin D supplements for bone health.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Feminizing hormone therapy care at Mayo Clinic
- Tangpricha V, et al. Transgender women: Evaluation and management. https://www.uptodate.com/contents/search. Accessed Oct. 10, 2022.
- Erickson-Schroth L, ed. Medical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Oct. 10, 2022.
- Coleman E, et al. Standards of care for the health of transgender and gender diverse people, version 8. International Journal of Transgender Health. 2022; doi:10.1080/26895269.2022.2100644.
- AskMayoExpert. Gender-affirming hormone therapy (adult). Mayo Clinic; 2022.
- Nippoldt TB (expert opinion). Mayo Clinic. Sept. 29, 2022.
- Gender dysphoria
- Doctors & Departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Let’s celebrate our doctors!
Join us in celebrating and honoring Mayo Clinic physicians on March 30th for National Doctor’s Day.
May 12, 2022
What the Science on Gender-Affirming Care for Transgender Kids Really Shows
Laws that ban gender-affirming treatment ignore the wealth of research demonstrating its benefits for trans people’s health
By Heather Boerner

As attacks against transgender kids increase in the U.S., Minnesotans hold a rally at the state’s capitol in Saint Paul in March 2022 to support trans kids in Minnesota and Texas and around the country.
Michael Siluk/UCG/Universal Images Group via Getty Images
Editor’s Note (3/30/23): This article from May 2022 is being republished to highlight the ways that ongoing anti-trans legislation is harmful and unscientific.
For the first 40 years of their life, Texas resident Kelly Fleming spent a portion of most years in a deep depression. As an adult, Fleming—who uses they/them pronouns and who asked to use a pseudonym to protect their safety—would shave their face in the shower with the lights off so neither they nor their wife would have to confront the reality of their body.
What Fleming was experiencing, although they did not know it at the time, was gender dysphoria : the acute and chronic distress of living in a body that does not reflect one’s gender and the desire to have bodily characteristics of that gender. While in therapy, Fleming discovered research linking access to gender-affirming hormone therapy with reduced depression in transgender people. They started a very low dose of estradiol, and the depression episodes became shorter, less frequent and less intense. Now they look at their body with joy.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing . By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
So when Fleming sees what authorities in Texas , Alabama , Florida and other states are doing to bar transgender teens and children from receiving gender-affirming medical care, it infuriates them. And they are worried for their children, ages 12 and 14, both of whom are agender—a identity on the transgender spectrum that is neither masculine nor feminine.
“I’m just so excited to see them being able to present themselves in a way that makes them happy,” Fleming says. “They are living their best life regardless of what others think, and that’s a privilege that I did not get to have as a younger person.”
Laws Based on “Completely Wrong” Information
Currently more than a dozen state legislatures or administrations are considering—or have already passed—laws banning health care for transgender young people. On April 20 the Florida Department of Health issued guidance to withhold such gender-affirming care. This includes social gender transitioning—acknowledging that a young person is trans, using their correct pronouns and name, and supporting their desire to live publicly as the gender of their experience rather than their sex assigned at birth. This comes nearly two months after Texas Governor Greg Abbott issued an order for the Texas Department of Family and Protective Services to investigate for child abuse parents who allow their transgender preteens and teenagers to receive medical care. Alabama recently passed SB 184 , which would make it a felony to provide gender-affirming medical care to transgender minors. In Alabama, a “minor” is defined as anyone 19 or younger.
If such laws go ahead, 58,200 teens in the U.S. could lose access to or never receive gender-affirming care, according to the Williams Institute at the University of California, Los Angeles. A decade of research shows such treatment reduces depression, suicidality and other devastating consequences of trans preteens and teens being forced to undergo puberty in the sex they were assigned at birth).
The bills are based on “information that’s completely wrong,” says Michelle Forcier, a pediatrician and professor of pediatrics at Brown University. Forcier literally helped write the book on how to provide evidence-based gender care to young people. She is also an assistant dean of admissions at the Warren Alpert Medical School of Brown University. Those laws “are absolutely, absolutely incorrect” about the science of gender-affirming care for young people, she says. “[Inaccurate information] is there to create drama. It’s there to make people take a side.”
The truth is that data from more than a dozen studies of more than 30,000 transgender and gender-diverse young people consistently show that access to gender-affirming care is associated with better mental health outcomes—and that lack of access to such care is associated with higher rates of suicidality, depression and self-harming behavior. (Gender diversity refers to the extent to which a person’s gendered behaviors, appearance and identities are culturally incongruent with the sex they were assigned at birth. Gender-diverse people can identify along the transgender spectrum, but not all do.) Major medical organizations, including the American Academy of Pediatrics (AAP) , the American Academy of Child and Adolescent Psychiatry , the Endocrine Society , the American Medical Association , the American Psychological Association and the American Psychiatric Association , have published policy statements and guidelines on how to provide age-appropriate gender-affirming care. All of those medical societies find such care to be evidence-based and medically necessary.
AAP and Endocrine Society guidelines call for developmentally appropriate care, and that means no puberty blockers or hormones until young people are already undergoing puberty for their sex assigned at birth. For one thing, “there are no hormonal differences among prepubertal children,” says Joshua Safer, executive director of the Mount Sinai Center for Transgender Medicine and Surgery in New York City and co-author of the Endocrine Society’s guidelines. Those guidelines provide the option of gonadotropin-releasing hormone analogues (GnRHas), which block the release of sex hormones, once young people are already into the second of five puberty stages—marked by breast budding and pubic hair. These are offered only if a teen is not ready to make decisions about puberty. Access to gender-affirming hormones and potential access to gender-affirming surgery is available at age 16—and then, in the case of transmasculine youth, only mastectomy, also known as top surgery. The Endocrine Society does not recommend genital surgery for minors.
Before puberty, gender-affirming care is about supporting the process of gender development rather than directing children through a specific course of gender transition or maintenance of cisgender presentation, says Jason Rafferty, co-author of AAP’s policy statement on gender-affirming care and a pediatrician and psychiatrist at Hasbro Children’s Hospital in Rhode Island. “The current research suggests that, rather than predicting or preventing who a child might become, it’s better to value them for who they are now—even at a young age,” Rafferty says.
A Safe Environment to Explore Gender
A 2021 systematic review of 44 peer-reviewed studies found that parent connectedness, measured by a six-question scale asking about such things as how safe young people feel confiding in their guardians or how cared for they feel in the family, is associated with greater resilience among teens and young adults who are transgender or gender-diverse. Rafferty says he sees his role with regard to prepubertal children as offering a safe environment for the child to explore their gender and for parents to ask questions. “The gender-affirming approach is not some railroad of people to hormones and surgery,” Safer says. “It is talking and watching and being conservative.”
Only once children are older, and if the incongruence between the sex assigned to them at birth and their experienced gender has persisted, does discussion of medical transition occur. First a gender therapist has to diagnose the young person with gender dysphoria .
After a gender dysphoria diagnosis—and only if earlier conversations suggest that hormones are indicated—guidelines call for discussion of fertility, puberty suppression and hormones. Puberty-suppressing medications have been used for decades for cisgender children who start puberty early, but they are not meant to be used indefinitely. The Endocrine Society guidelines recommend a maximum of two years on GnRHa therapy to allow more time for children to form their gender identity before undergoing puberty for their sex assigned at birth, the effects of which are irreversible.
“[Puberty blockers] are part of the process of ‘do no harm,’” Forcier says, referencing a popular phrase that describes the Hippocratic Oath, which many physicians recite a version of before they begin to practice.
Hormone blocker treatment may have side effects. A 2015 longitudinal observational cohort study of 34 transgender young people found that, by the time the participants were 22 years old, trans women experienced a decrease in bone mineral density. A 2020 study of puberty suppression in gender-diverse and transgender young people found that those who started puberty blockers in early puberty had lower bone mineral density before the start of treatment than the public at large. This suggests, the authors wrote, that GnRHa use may not be the cause of low bone mineral density for these young people. Instead they found that lack of exercise was a primary factor in low bone-mineral density, especially among transgender girls.
Other side effects of GnRHa therapy include weight gain, hot flashes and mood swings. But studies have found that these side effects—and puberty delay itself—are reversible , Safer says.
Gender-affirming hormone therapy often involves taking an androgen blocker (a chemical that blocks the release of testosterone and other androgenic hormones) and estrogen in transfeminine teens, and testosterone supplementation in transmasculine teens. Such hormones may be associated with some physiological changes for adult transgender people. For instance, transfeminine people taking estrogen see their so-called “good” cholesterol increase. By contrast, transmasculine people taking testosterone see their good cholesterol decrease. Some studies have hinted at effects on bone mineral density, but these are complicated and also depend on personal, family history, exercise, and many other factors in addition to hormones.”
And while some critics point to decade-old study and older studies suggesting very few young people persist in transgender identity into late adolescence and adulthood, Forcier says the data are “misleading and not accurate.” A recent review detailed methodological problems with some of these studies . New research in 17,151 people who had ever socially transitioned found that 86.9 percent persisted in their gender identity. Of the 2,242 people who reported that they reverted to living as the gender associated with the sex they were assigned at birth, just 15.9 percent said they did so because of internal factors such as questioning their experienced gender but also because of fear, mental health issues and suicide attempts. The rest reported the cause was social, economic and familial stigma and discrimination. A third reported that they ceased living openly as a trans person because doing so was “just too hard for me.”
The Harms of Denying Care
Data suggest the effects of denying that care are worse than whatever side effects result from delaying sex-assigned-at-birth puberty. And medical society guidelines conclude that the benefits of gender-affirming care outweigh the risks. Without gender-affirming hormone therapy, cisgender hormones take over, forcing body changes that can be permanent and distressing.
A 2020 study of 300 gender-incongruent young people found that mental distress—including self-harm, suicidal thoughts and depression— increased as the children were made to proceed with puberty according to their assigned sex. By the time 184 older teens (with a median age of 16) reached the stage in which transgender boys began their periods and grew breasts and transgender girls’ voice dropped and facial hair began to appear, 46 percent had been diagnosed with depression, 40 percent had self-harmed, 52 percent had considered suicide, and 17 percent had attempted it—rates significantly higher than those of gender-incongruent children who were a median of 13.9 years old or of cisgender kids their own age.
Conversely, access to gender-affirming hormones in adolescence appears to have a protective effect. In one study, researchers followed 104 teens and young adults for a year and asked them about their depression, anxiety and suicidality at the time they started receiving hormones or puberty blockers and again at the three-month, six-month and one-year mark. At the beginning of the study, which was published in JAMA Network Open in February 2022, more than half of the respondents reported moderate to severe depression, half reported moderate to severe anxiety, and 43.3 percent reported thoughts of self-harm or suicide in the past two weeks.
But when the researchers analyzed the results based on the kind of gender-affirming care the teens had received, they found that those who had access to puberty blockers or gender-affirming hormones were 60 percent less likely to experience moderate to severe depression. And those with access to the medical treatments were 73 percent less likely to contemplate self-harm or suicide.
“Delays in prescribing puberty blockers and hormones may in fact worsen mental health symptoms for trans youth,” says Diana Tordoff, an epidemiology graduate student at the University of Washington and co-author of the study.
That effect may be lifelong. A 2022 study of more than 21,000 transgender adults showed that just 41 percent of adults who wanted hormone therapy received it, and just 2.3 percent had access to it in adolescence. When researchers looked at rates of suicidal thinking over the past year in these same adults, they found that access to hormone therapy in early adolescence was associated with a 60 percent reduction in suicidality in the past year and that access in late adolescence was associated with a 50 percent reduction.
For Fleming’s kids in Texas, gender-affirming hormones are not currently part of the discussion; not all trans people desire hormones or surgery to feel affirmed in their gender. But Fleming is already looking at jobs in other states to protect their children’s access to such care, should they change their mind. “Getting your body closer to the gender [you] identify with—that is what helps the dysphoria,” Fleming says. “And not giving people the opportunity to do that, making it harder for them to do that, is what has made the suicide rate among transgender people so high. We just—trans people are just trying to survive.”
IF YOU NEED HELP If you or someone you know is struggling or having thoughts of suicide, help is available. Call the National Suicide Prevention Lifeline at 1-800-273-8255 (TALK), use the online Lifeline Chat or contact the Crisis Text Line by texting TALK to 741741.
- Public Health
Gender Transition Medications and Surgeries for Children in the U.S.
Key takeaways.
The U.S. currently has the most permissive laws surrounding transgender treatments for children compared to peer Western and Northern European nations.
Only 12–27% of children with gender dysphoria—a condition where one’s perceived gender identity differs from their biological sex—carry it into adulthood, yet many children in the U.S. are still eligible for irreversible therapies and surgeries.
Many puberty blockers given to children are prescribed for off-label (unapproved) use and can have dangerous side effects, including lowered bone density, stunted growth, and permanent infertility. There is limited research on the long-term effects of transgender interventions on children and little evidence of mental health benefits.
Policymakers should adopt policies to protect children from potentially harmful and irreversible sex reassignment surgeries and medications.
Executive Summary:
Rates of transgenderism in children have rapidly increased in recent years in the U.S., which has sparked discussions between parents, schools, policymakers, and medical professionals alike over how to discuss and treat the issue. On one end of the spectrum, activist groups and a vocal subset of the medical establishment have promoted what is euphemistically known as “gender-affirming care,” whereby children with transgender inclinations are being encouraged to undertake potentially irreversible surgical and hormonal interventions with unknown long-term consequences. The interventions range from preventing normal pubertal development to surgical procedures removing healthy breast tissue and genitalia. Recognizing the potential for significant harm, and with over 300,000 youths between the ages of 13–17 in the U.S. now identifying as transgender, some states are setting policies designed to protect children from such irreversible treatments made at a critical time in their physical, mental, and emotional development ( Herman, Flores, & O’Neil, 2022 ).
By castigating those who disagree with these procedures as “transphobic,” the people calling for the immediate normalization of these surgeries and treatments have dismissed valid concerns. Many important questions have arisen based on emerging evidence from systematic reviews, whistleblowers, detransitioners, and findings of a new clinical phenomenon of rapid onset of the condition in adolescence rather than early childhood. The fervor of the argument for “gender-affirming care” is not matched by any strength of evidence establishing that such treatments are either safe or effective for promoting long-term well-being. On the contrary, Americans have significant reasons to be instead concerned about the effects of such radical interventions undertaken on children.
Indeed, the American people recognize the riskiness of such treatments on children, with most registered voters believing that “gender-affirming care” for children should be illegal. Moreover, around 85% of children with gender dysphoria do not carry this condition into adolescence—making the notion of using permanent treatments to address temporary conditions quite troubling ( Hembree et al., 2017 ). Nevertheless, many medical professionals in the U.S. are using an “affirm-early/affirm-often” approach when it comes to dealing with children who have gender dysphoria, and they often recommend puberty blockers, cross-sex hormones, and/or sex-change surgeries.
Though other nations have shied away from such an approach in recent years, a recent review of eligibility criteria for sex-reassignment surgery found that children in the U.S. have access to the procedure at younger ages than minors in Western and Northern Europe ( Do No Harm, 2023a ). The same holds true with the prescription of puberty blockers and cross-sex hormones. Today, some states in the U.S. have more permissive laws than Western and Northern European nations. Not only is there little evidence that some of these “treatments” do anything to benefit the mental health of a child, but studies have shown mounting evidence that transgender drugs and surgical procedures have negative side effects for children. Moreover, many of the drugs prescribed to children for such procedures are prescribed for unapproved use.
A contrasting approach to the prevailing “gender-affirming” philosophy of interventions does exist. It can be described as the “first, do no harm” model, which holds that the risks of medical and surgical interventions outweigh the benefits, and states that doctors should focus on other options, such as exploratory psychotherapy, while ensuring strong mental and social support ( Schwartz, 2021 ; SEGM, 2021a ). The non-profit “Do No Harm,” which consists of numerous physicians and healthcare professionals, has started an education campaign to protect minors from gender ideology and has, like other non-profit groups, concluded that it is appropriate for state lawmakers to now intervene ( Do No Harm, 2023a ; Do No Harm, 2023b ; Do No Harm, 2023c ; Brown & Stathatos, 2022 ). The Society for Evidence Based Gender Medicine (SEGM) has also highlighted the lack of quality evidence and recommended that the medical community urgently address concerns with current practices while endorsing the approach to “first, do no harm” ( SEGM, 2023 ; SEGM, 2021b ). Policymakers in the U.S. should consider all of this data and adopt policies that protect children from potentially harmful and irreversible procedures.
This report builds upon the foundation set by Do No Harm and SEGM by compiling knowledge from a diversified set of resources to understand the history and diagnosis of gender dysphoria, explore different treatment models for the condition, and investigate how other countries approach the issue relative to how it is dealt with in the U.S. Finally, this report reviews how the American people perceive this issue and then outlines state actions to protect children.
Section One: Defining Gender Dysphoria and Understanding the Role of the Diagnostic and Statistical Manual of Mental Disorders
To fully understand pediatric gender medicine, it is critical to start with the diagnostic history of gender dysphoria and the evolution of the primary tool used by clinicians to make the diagnosis. Originally published in 1952 by the American Psychiatric Association (APA), the Diagnostic and Statistical Manual of Mental Disorders (DSM) is considered the “go-to” reference for the characterization and diagnosis of mental disorders in the U.S. and much of the world ( Kawa & Giordano, 2012 ).
The DSM is translated into over 20 languages and is the leading mental disorder diagnostic resource, exerting heavy influence in the field of psychiatry and across society over the last 70 years ( Kawa & Giordano, 2012 ). This resource is used by clinicians, researchers, policymakers, courts, and insurance companies alike. The DSM is now on volume five, with each edition reflecting a change of definitions and inclusions intended to represent current medical thinking—some with significant impact. As an example, between DSM-II to DSM-III, the number of mental disorder categories rose from 182 to 265, partly due to a shift from considering mental disorders as psychological states to considering them discrete disease categories based on symptoms—a shift one source noted as “an attempt to ‘re-medicalize’ American psychiatry” ( Kawa & Giordano, 2012 ). The most recent version, DSM-5 (the version updated its notation from Roman numerals to numbers), included nearly 300 mental disorders and took 14 years of planning and preparation to publish ( Suris et al. 2016 ).
It was not until DSM-III (1980) that any term related to gender dysphoria was included. The term used in the DSM-III was “transsexualism,” and then was later changed to “gender identity disorder in adults and adolescents” in the DSM-IV released in 1994. In 2013, the DSM-5 was released and again changed the term to “gender dysphoria” ( APA, 2017 ). Given the above history regarding the DSM, it is also important to note that the symptom-based disease categorization of the DSM-III led to an increase in psychopharmacological interventions.
The revised text version of the DSM-5, the DSM-5-TR, was published in 2022. This edition included significant updates, notably the direction to use “culturally-sensitive language,” such as changing “desired gender” to “experienced gender” and changing “cross-sex medical procedure” to “gender-affirming medical treatment” ( APA, 2022a ).
The DSM-5-TR definition of gender dysphoria in adolescents and adults is as follows:
“ … a marked incongruence between one’s experienced/expressed gender and their assigned gender, lasting at least 6 months, as manifested by at least two of the following:
A marked incongruence between one’s experienced/expressed gender and primary and/or secondary sex characteristics (or in young adolescents, the anticipated secondary sex characteristics)
A strong desire to be rid of one’s primary and/or secondary sex characteristics because of a marked incongruence with one’s experienced/expressed gender (or in young adolescents, a desire to prevent the development of the anticipated secondary sex characteristics)
A strong desire for the primary and/or secondary sex characteristics of the other gender
A strong desire to be of the other gender (or some alternative gender different from one’s assigned gender)
A strong desire to be treated as the other gender (or some alternative gender different from one’s assigned gender)
A strong conviction that one has the typical feelings and reactions of the other gender (or some alternative gender different from one’s assigned gender),”
( APA, 2022b ).
Additionally, the DSM-5-TR definition of gender dysphoria in children is as follows:
“ … a marked incongruence between one’s experienced/expressed gender and assigned gender, lasting at least 6 months, as manifested by at least six of the following (one of which must be the first criterion):
A strong desire to be of the other gender or an insistence that one is the other gender (or some alternative gender different from one’s assigned gender)
In boys (assigned gender), a strong preference for cross-dressing or simulating female attire; or in girls (assigned gender), a strong preference for wearing only typical masculine clothing and a strong resistance to the wearing of typical feminine clothing
A strong preference for cross-gender roles in make-believe play or fantasy play
A strong preference for the toys, games or activities stereotypically used or engaged in by the other gender
A strong preference for playmates of the other gender
In boys (assigned gender), a strong rejection of typically masculine toys, games, and activities and a strong avoidance of rough-and-tumble play; or in girls (assigned gender), a strong rejection of typically feminine toys, games, and activities
A strong dislike of one’s sexual anatomy
A strong desire for the physical sex characteristics that match one’s experienced gender,”
Notably, the diagnostic criteria for both include association of the condition with clinically significant distress or impairment in social, occupational, or other important areas of functioning ( APA, 2022b ).
Because of the millions of lives impacted by the DSM, researchers have raised concerns about potential political and financial biases of authors contributing to the clinical reference book. The Society for Humanistic Psychology has been a leader in elevating concerns over the DSM-5 and was critical in launching a petition of over 15,000 concerned mental health professionals and groups from around the world ( Kamens, Elkins, & Robbins, 2017 ). Topping the list of their concerns is a conflict of interest among the authors. Many DSM panel members have direct financial ties to the pharmaceutical industry, and several of the disorders call for pharmacological treatment as the first-line intervention ( Cosgrove & Krimsky, 2012 ).
It is also worth noting that the DSM-5-TR included other considerable “cultural changes.” Published in 2022 as a text revision to the latest DSM-5, the DSM-5-TR changed (among other things) the term “race/racial” to “racialized” to underscore that race is a social construct ( Blanchfield, 2022 ). It also changed “Latino/Latina” to “Latinx” to promote gender equality and discontinued the use of “minority” and “non-White” to avoid creating a social hierarchy ( Blanchfield, 2022 ).
The DSM-5 was designed to include cultural, racial, and gender considerations. As a part of their review and rationale for updating the DSM-5, “a DSM-5 Culture and Gender Study Group was appointed to provide guidelines for the work group literature reviews and data analyses that served as the empirical rationale for draft changes” to ensure that cultural factors were included in revisions ( Regier et al. 2013 ). Although these considerations were included in the DMS-5, updates were made in the DSM-5-TR in “response to concerns that race, ethnoracial differences, racism and discrimination be handled appropriately” ( APA, 2022c ). The strategies used to address these concerns were 1) a 19-person review committee on cultural issues and 2) a 10-person Ethnoracial Equity and Inclusion Work Group made up of practitioners from diverse backgrounds ( APA, 2022c ). Given that the DSM is the mental disorder diagnostic tool used in much of the world, it is critical to note the changes that have been made in response to social, cultural, and political pressures rather than a change in medical data and scientific evidence.
Section Two: The Treatment of Gender Dysphoria
Today, U.S. government agencies and many medical professional groups have signaled their support for these types of treatments. Under the Biden Administration, the U.S. Department of Health and Human Services states that for children, “early gender-affirming care is crucial to overall health and well-being” ( HHS Office of Population Affairs, n.d.). Many medical professionals in the U.S. accept an “affirm-only/affirm-early” approach to gender transition, which strives to implement interventions (including hormonal or surgical) to help a child better align with his or her “gender identity” ( Do No Harm, 2023a ). Though surgery and hormonal treatments are permanent, evidence indicates that about 85% of cases of children with gender dysphoria do not persist into adolescence ( Hembree et al., 2017 ). Nevertheless, the American Academy of Pediatrics (AAP) embraces the approach of early medical intervention for children and adolescents ( Rafferty et al., 2018 ).
Along with the AAP, multiple medical professional guidelines explain that the appropriate treatment of gender dysphoria in children and adolescents should be used in a “gender-affirmative care model” (GACM) and may include:
Psychotherapy;
Hormone or Puberty Blockers;
Cross-Sex Hormone Therapy; and/or
Sex Reassignment Surgery
The GACM allows youth to progress through some or all interventions depending on timing and pubertal maturity ( Brown & Stathatos, 2022 ; Rafferty et al., 2018 ). Psychotherapy has an important distinction; it has a primary role in another model of care known as “first, do no harm” ( Rafferty et al., 2018 ; Schwartz, 2021 ). In this model, medical and surgical interventions are considered to carry greater risk than benefit for youth, a position well summarized by psychologist David Schwartz, Ph.D.:
… in the treatment of children and adolescents, no matter what the diagnosis, encouraging mastectomy, ovariectomy, uterine extirpation, penile disablement, tracheal shave, the prescription of hormones which are out of line with the genetic make-up of the child, or puberty blockers, are all clinical practices which run an unacceptably high risk of doing harm ( SEGM, 2021 ).
Many of the puberty blockers and cross-sex hormone therapies used to treat gender dysphoria in children are prescribed off-label (for a purpose not approved by the U.S. Food and Drug Administration (FDA)). Therefore, they can pose a greater risk, including the risk of unknown long-term effects, to the children who receive them. In 2021, the Texas Attorney General launched an investigation into two pharmaceutical companies for allegedly advertising and promoting the off-label use of puberty blockers without disclosing any of their risks ( Attorney General of Texas, 2021 ). In 2022, the FDA also issued a new warning for commonly used puberty blockers, including “recommendations to monitor patients taking GnRH agonists for signs and symptoms of pseudotumor cerebri, including headache, papilledema, blurred or loss of vision, diplopia, pain behind the eye or pain with eye movement, tinnitus, dizziness and nausea” ( FDA, 2022 ). Despite these facts, a growing number of children are being prescribed these drugs for unapproved uses.
There are significant side effects and limited research on the long-term impacts and efficacy of various treatments used in a GACM of gender dysphoria in children. Patients and parents are advised that the use of puberty blockers in children may be associated with lower bone density, stunted growth, fertility issues, and underdevelopment of genital tissue ( Mayo Clinic, 2022 ; St. Louis Children’s Hospital, n.d.; Brown & Stathatos, 2022 ). Moreover, a study conducted in England demonstrated similar negative side effects, such as lowered bone density and stunted growth, without showing a change in the psychological well-being of the children studied ( Carmichael et al., 2021, p. 18 ; Brown & Stathatos, 2022 ). Cross-sex hormones prescribed to children also demonstrated a plethora of side effects, including blood clots in veins and permanent infertility ( CDC, n.d .; NHS England, 2016, p. 8 ; Brown & Stathatos, 2022 ). Importantly, cross-sex hormones can result in the development of secondary sex characteristics such as the development of breasts in male-to-female patients and deepening of the voice in female-to-male patients that, though desired at the time, are irreversible ( NHS England, 2020b ; Brown & Stathatos, 2022 ). Moreover, the neurocognitive effects of pubertal suppression are unknown. International experts are in consensus about the need to assess long-term effects and have stated that: “Taken as a whole, the existing knowledge about puberty and the brain raises the possibility that suppressing sex hormone production during this period could alter neurodevelopment in complex ways—not all of which may be beneficial” ( Chen et al. 2020 ).
Proponents of a GACM frequently claim that it is the only way to improve mental health and reduce suicide risk in youth. However, a 40-year cohort study from Sweden on transsexual individuals undergoing sex-reassignment surgery—one of the most comprehensive long-term studies available—found that high suicide risk persisted after surgical procedures at a rate 19.1 times higher than the general population ( Dhejne et al., 2011 ). Another Swedish population study with one of the largest cohorts established to date evaluated (in a corrected analysis from the original publication) mental health outcomes among transgender individuals who received surgical interventions and those who did not and found “no advantage of surgery in relation to subsequent mood or anxiety disorder-related health care visits or prescriptions or hospitalizations following suicide attempts” ( Branstrom, & Pachankis, 2019 ; Kalin, 2020 ).
Treatment protocols for gender dysphoria often follow the guidelines of the World Professional Association for Transgender Health (WPATH), the Endocrine Society (an international medical professional association), and the American Association of Pediatrics (AAP). However, a recent review article from the Manhattan Institute outlined significant flaws with the recommendations from each organization based on the evidence available in the academic literature and from best practices in other countries ( Sapir, 2022 ). Notably, the AAP position paper, which supported early affirmation and treatment of gender dysphoria in childhood, was fact-checked by psychologist James Cantor, Ph.D., of the Toronto Sexuality Center. Dr. Cantor found that the AAP position paper omitted information regarding the low frequency of gender dysphoria persisting from childhood to adolescence ( Cantor, 2020 ). He also found that the AAP paper, when rejecting “watchful waiting,” misrepresented citations regarding the approach that aims to put pharmacologic or surgical intervention on hold while the patient receives other supportive care and counseling ( Cantor, 2020 ).
Additionally, the Endocrine Society’s “clinical practice guideline” from 2017 assesses the quality of evidence for each of its recommendations ( Hembree et al., 2017 ). All six recommendations specifically related to treatment for adolescents found only a “low” or “very low” quality of evidence ( Hembree et al., 2017 ). One recommendation (2.5) that is listed as a weak recommendation with a very low quality of evidence is particularly concerning:
We recognize that there may be compelling reasons to initiate sex hormone treatment prior to the age of 16 years in some adolescents with GD [gender dysphoria] / gender incongruence, even though there are minimal published studies of gender-affirming hormone treatments administered before age 13.5 to 14 years. As with the care of adolescents 16 years of age, we recommend that an expert multidisciplinary team of medical and MHPs [mental health providers] manage this treatment ( Hembree et al., 2017 ).
The WPATH guidelines rely heavily on the experience of a specific Dutch protocol, but there are many methodological concerns with how conclusions are supported and how they apply to the current clinical reality ( Coleman et al., 2022 ; Sapir, 2022 ). A recent review of the Dutch protocol methodology outlines the following three primary concerns:
(1) subject selection assured that only the most successful cases were included in the results; (2) the finding that “resolution of gender dysphoria” was due to the reversal of the questionnaire employed; (3) concomitant psychotherapy made it impossible to separate the effects of this intervention from those of hormones and surgery ( Abbruzzese, Levine, & Mason, 2023).
Importantly, there have been challenges replicating the Dutch protocol results largely due to concerns of significant selection bias ( Abbruzzese, Levine, & Mason, 2023) . This fact and the forthcoming discussion about the changing demographics of youth gender dysphoria in the U.S. lend credence to the position that the Dutch protocol cannot adequately justify the current practice patterns in America.
Further, political biases exist within WPATH and appear to be reflected in their guidelines. Dr. Bowers, a transgender woman and world-renowned gender surgeon who is on the board of WPATH, was asked if the organization had been welcoming to a wide variety of doctors’ viewpoints. In response, Dr. Bowers said: “There are definitely people who are trying to keep out anyone who doesn’t absolutely buy the party line that everything should be affirming and that there’s no room for dissent” ( Shrier, 2021, para. 12 ; Brown & Stathatos, 2022 ). A second doctor on the board of WPATH, Dr. Erica Anderson, submitted a co-authored op-ed to the New York Times expressing concerns that transgender children were receiving reckless healthcare and that WPATH was recommending puberty blockers too early in puberty, but the Times declined to publish her piece ( Shrier, 2021, para. 6, 7, & 50 ; Brown & Stathatos, 2022 ). The piece, which was titled “The mental health establishment is failing trans kids: Gender-exploratory therapy is a key step. Why aren’t therapists providing it?” was later published in the Washington Post ( Edwards-Leeper & Anderson, 2021 ). It was co-authored with another clinical psychologist and member of the WPATH, Dr. Laura Edwards-Leeper, with the core message that rushed medical treatment without proper evaluation and therapy puts children at risk ( Edwards-Leeper & Anderson, 2021 ).
In addition to the Do No Harm group, other groups of medical professionals have alternative views on the ideal way to proceed in this area. SEGM is a group made up of over 100 clinicians and researchers from a range of disciplines who are concerned about the quality of evidence being used to recommend medical and surgical interventions as first-line treatment for young patients with gender dysphoria ( SEGM, n.d.(b) ). They offer an alternative clinical position based on their expertise and review of the current evidence:
SEGM firmly believes that medical decisions must remain between patient and clinicians, without political interference. However, we also believe that it is incumbent on US medical societies to urgently examine the evidence base for hormonal and surgical interventions for youth using rigorous systematic research methods. Given the results of the recent systematic evidence review conducted by NICE, which concluded that the evidence of benefits of these interventions is of very low certainty and the risk/benefit profile is unclear, SEGM believes that exploratory psychotherapy should be first-line treatment for gender dysphoric people age 25 and under ( SEGM, n.d.(a) ).
Section Three: A Comparison: Trends in the U.S. vs. Other Nations on the Treatment of Gender Dysphoria in Children and Adolescents
A recent study estimated that nearly 1.6 million people ages 13+ identified as transgender in the U.S. and denoted a generational shift because rates of transgenderism in children are growing at a much faster rate than in adults ( Herman, Flores, & O’Neil, 2022 ). In fact, now nearly 20% of people who identify as transgender are aged 13–17, meaning around 300,000 children are now identifying as transgender ( Herman, Flores, & O’Neil, 2022 ). For added perspective, one must consider that nearly 20% of all people who identify as transgender in the U.S. are children 13–17, yet that age range only makes up 8% of the U.S. population ( Herman, Flores, & O’Neil, 2022 ). Additionally, the number of children known to be on puberty blockers or cross-sex hormones in the U.S. more than doubled in just four years—from 2,394 in 2017 to 5,063 in 2021 ( Do No Harm, 2023a ; Terhune, Respaut, & Conlin, 2022 ). Furthermore, one study found that more than 120,000 children in the U.S. were diagnosed with gender dysphoria during the same four-year period ( Respaut & Terhune, 2022 ). Experts and researchers in the field are concerned with rates in a specific sub-group—adolescent girls—and have called for a greater understanding of “rapid onset gender dysphoria” as a distinct clinical phenomenon ( Sinai, 2022 ).
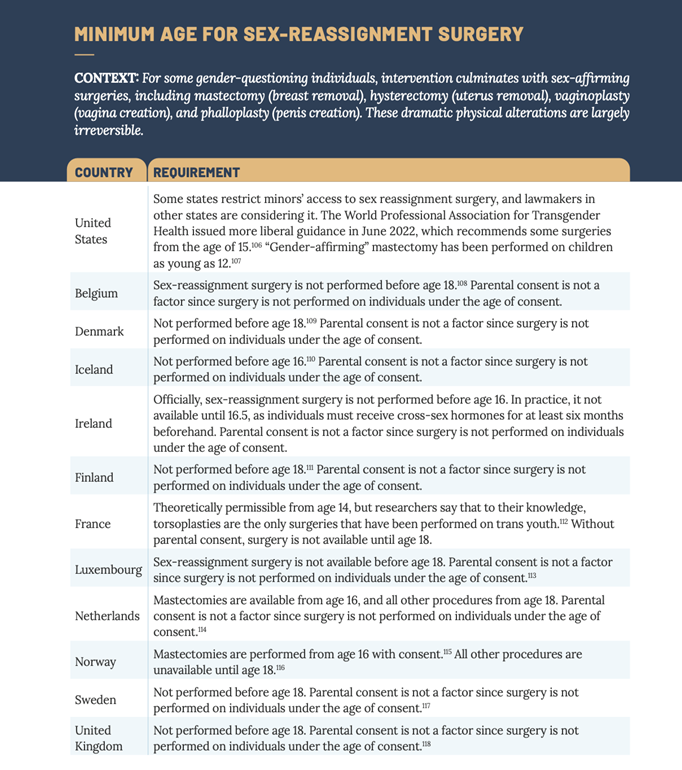
As noted above, the medical community in the U.S. has opted to broadly take an “affirm-early/affirm-often” approach when it comes to treating gender dysphoria in children. By labeling the full spectrum of interventions used to transition youth—from social to puberty-blocking to cross-sex hormones and to surgery—as “affirming,” many have tried to categorize all other treatments into a binary category of “non-affirming.” In doing so, they have framed it as harmful, thereby limiting valid alternatives such as psychotherapy ( D’Angelo et al., 2020 ). More than 60 pediatric gender clinics and more than 300 clinics that provide hormonal interventions to children in the U.S. now exist ( Do No Harm, 2023a , p. 12). When measured against other Western and Northern European countries, the U.S. has the most clinics providing treatment for the gender transition of children and the most permissive laws regarding the legal and medical gender transition of children ( Do No Harm, 2023a , p. 3 & p. 12). Below is a chart from Do No Harm that outlines the laws regarding sex-assignment surgery in the U.S. in comparison to the laws in Western and Northern European nations:
This data clearly demonstrate that the U.S. allows doctors to perform sex-reassignment surgery on children at a younger age than most comparable nations (12 years old in some cases in the U.S.) ( Do No Harm, 2023a , p. 11). Most Western and European nations protect minor children from sex-reassignment surgeries by requiring patients to reach age 18 ( Do No Harm, 2023a , p. 11). The U.S. is in a similar position regarding puberty blockers for children, which clinical guidelines do not recommend until puberty ( Do No Harm, 2023a , p. 9). Nevertheless, many U.S. physicians are prescribing puberty blockers as early as 8 years old (reportedly at the earliest sign of puberty), and, in some states, parental consent for these drugs is not needed. ( Do No Harm, 2023a , p. 9). In Oregon, children 15 and over do not need parental consent, and taxpayers pay for puberty blockers for children through Medicaid ( Do No Harm, 2023a , p. 9). This practice appears to be an outlier in comparison to many other countries where puberty blockers are typically not given until children reach a specific stage of puberty (Tanner Stage II) or until they reach the age of 12 ( Do No Harm, 2023a , p. 9).
The use of cross-sex hormones is likewise another area where some states in the U.S. have more permissive policies than many other countries in the world ( Do No Harm, 2023a , p. 10). Cross-sex hormones have been given to some children in the U.S. under 13 years old (state laws vary on this), and Oregon again has the most permissive laws for this treatment ( Do No Harm, 2023a , p. 10). It now allows for these drugs to be used at the age of 15 without consent and with taxpayer funding ( Do No Harm, 2023a , p. 10). In contrast, the vast majority of other countries examined in the Do No Harm report do not allow for these hormones until age 16 ( Do No Harm, 2023a , p. 10).
In recent years, the path of the U.S. has diverged significantly from the path of other countries. While the U.S. has continued to loosen protocols around puberty blockers, cross-sex hormones, and sex-reassignment surgeries, other countries have begun tightening their protocols and shifting away from the “affirm-early/affirm-often” approach based on emerging evidence from thorough and systematic evidence reviews. In June 2020, Finland recommended psychosocial support to treat gender dysphoria in minors ( Council for Choice in Health Care in Finland, 2020 ). If youth go on to experience severe and persistent gender-related anxiety, they can then be referred to centralized research clinics on gender identity where hormonal treatment through a research protocol is considered on a case-by-case basis only if strict criteria are met ( Council for Choice in Health Care in Finland, 2020 ). Importantly, the Finnish guidelines do not allow surgical treatments stating that they “are not part of the treatment methods for dysphoria caused by gender-related conflicts in minors” ( Council for Choice in Health Care in Finland, 2020 ). Also in 2020, the Tavistock Gender Identity Development Service of England released a study stating that children receiving puberty blockers for gender dysphoria experienced little to no change in their psychological well-being ( Barnes & Cohen, 2020 ; Carmichael et al., 2021 ; Brown & Stathatos, 2022 ). A study completed by England’s National Institute for Health and Care Excellence (NICE) in October 2020 found the studies evaluating the use of puberty blockers to have “very low certainty” in the “critical outcomes of gender dysphoria and mental health” ( NICE, 2020 a p. 45; Brown & Stathatos, 2022 ). In 2022, the Swedish National Board of Health and Welfare updated its recommendations for the care of children and adolescents with gender dysphoria assessing that “the risks of puberty blockers and gender-affirming treatment are likely to outweigh the expected benefits of these treatments” and cautions the healthcare system regarding their use (National Board of Health and Welfare, 2022 p. 3 ; Brown & Stathatos, 2022 ).
In addition to systematic reviews, emerging evidence in the academic literature and in mainstream news about the experience of “detransitioners” is leading to more questions than answers. Detransitioners are defined as those individuals who revert back to living as their biological sex after transitioning, and many medical professionals and the general public are now asking more questions about the care these children and adolescents receive. In a key study of 100 detransitioners, more than half (55%) did not have an adequate evaluation from a doctor or mental health professional before starting to transition, and just one in four (24%) told their clinician they had detransitioned ( Littman, 2021 ).
The U.S. has clearly taken a radical stance regarding the treatment of gender dysphoria in children, while other countries are simultaneously questioning the data and evidence that support the use of hormone therapy and puberty blockers in children. Given the irreversible nature of these treatments, emerging evidence that high numbers of people regret undergoing them as minor children, and rising international awareness that an “affirm-only/affirm-early” approach may be causing inadvertent harm, medical policymakers in the U.S. should strongly consider adopting a more cautious approach.
Section Four: The Position of the American People on “Gender-Affirming Care”
A series of national polls from Scott Rasmussen throughout 2022 demonstrates that the plurality of Americans surveyed does not align with the medical community’s current recommendations. The findings may be largely based on a common-sense approach and informed by other societal norms to protect children from potentially damaging and irreversible decisions until they reach adulthood. Current examples are the legal drinking age of 21 years old, voluntary military participation at 18 years old, and informed parental consent for all aspects of daily life—from field trip permission slips to major medical interventions.
Scott Rasmussen National Survey of Registered Voters
October 25–27, 2022
When given a choice between two candidates for Congress, 56% of registered voters responded that they would vote for the candidate who said it should be illegal to provide surgery to help children transition from one gender to another. 25% of registered voters responded that they would vote for the candidate who said it would be immoral to restrict surgery that helps children transition from one gender to another.
October 18–20, 2022
72% of registered voters do not believe schools should teach children that they can change their gender.
59% of registered voters believe it should be against the law to provide “gender-affirming care” to children, which involves puberty blockers or surgery to help transition a boy to a girl or a girl to a boy.
56% of registered voters believe conducting gender-transition surgery on children is a form of child abuse.
73% of registered voters either strongly or somewhat disagree with people who advocate that children should be allowed to receive “gender-affirming care,” including puberty blockers and surgery, without the permission of their parents.
60% of registered voters believe it is a form of child abuse when a teacher or school encourages students to change their gender identity.
Scott Rasmussen National Survey of Registered Voters
July 12–13, 2022
When asked, “Should a child under 18 be encouraged to explore and define his or her own gender identity, or should he or she be encouraged to accept the gender that aligns with his or her biological sex?” 49% said a child should accept the gender that aligns with his or her biological sex. 32% said a child should define his or her own gender identity, and 19% were not sure.
March 10–12, 2022
When asked, “Some people advocate “gender-affirming care” which involves surgery to alter a person’s physical and sexual characteristics to match their gender identity, which can be used to transition a boy to a girl or a girl to a boy. Should it be against the law to perform such a surgery on young children?” 63% of registered voters said “yes.”
66% of registered voters said it should be against the law to perform such a surgery on anyone under 18.
Section Five: State Actions to Protect Children
The regulation of medical care is under the purview of states, and states have started to take action to protect children. The combination of concerning safety evidence and international trends outlined above supports the need for restrictions on medical and surgical gender transition interventions in children and adolescents. One option states can take is to delegate this responsibility to the state medical board, which could evaluate all the evidence and provide guidance to enact restrictions. Florida implemented this approach in 2022—first with guidance from the Department of Health in April and then with a report from the Agency for Health Care Administration in June ( FL DOH, 2022a , FL ACHA, 2022 ). These releases were immediately followed by a letter from the Surgeon General to Members of the Board asking them to review the evidence and guidance to establish a standard of care for “these complex and irreversible procedures” ( FL DOH 2022b ). The Florida Board of Medicine voted in November 2022 to ban the hormonal and surgical treatment of gender dysphoria in children (Izaguirre, 2022). This approach is a policy lever to preserve the delegative nature of the nuanced medical decision-making to medical experts. However, as seen in the COVID-19 pandemic, state medical boards do not always make evidence-based decisions when providing guidance, which indicates a need for additional policy options for state lawmakers ( Tahir, 2022 ).
In 2021, Arkansas became the first state to pass such restrictions into law with the Save Adolescents from Experimentation (SAFE) Act ( HB 1570, 2021 ; Bryan, 2021 ; Brown & Stathatos, 2022 ). The American Civil Liberties Union (ACLU) quickly filed suit resulting in a preliminary injunction on the restrictions, and the case is currently awaiting a decision in the 8th Circuit Court of Appeals ( ACLU, n.d. ). At least 18 other states are considering similar actions, and Utah became the first state to enact legislation to protect children in 2023 ( Associated Press, 2023 ).
After recently blowing the whistle on The Washington University Transgender Center at St. Louis Children’s Hospital, Jamie Reed began cooperating with the Missouri Attorney General to investigate the center. Following four years of working as a case manager in the clinic, she stated “… I could no longer participate in what was happening there. By the time I departed, I was certain that the way the American medical system is treating these patients is the opposite of the promise we make to ‘do no harm.’ Instead, we are permanently harming the vulnerable patients in our care” ( Reed, 2023 ). Now, Ms. Reed is working with Missouri Attorney General Andrew Bailey, who has launched a multi-agency investigation into the St. Louis Transgender Center on February 9, 2023, for harming hundreds of children ( MO Attorney General’s Office, 2023 ). The investigation is based on Ms. Reed’s sworn affidavit signed on February 7, 2023 ( MO Attorney General’s Office, 2023 ). Missouri is one of several states considering legislative action this session that would create more than one mechanism to resolve the disturbing issues raised by Ms. Reed. Though this is largely a state issue, Ms. Reed, who is self-described as “politically left of Bernie Sanders,” believes there should be a national moratorium on these interventions for children and adolescents until the American people know more ( Reed, 2023 ).
Another high-profile story on youth sex-reassignment surgeries at Vanderbilt University Medical Center (VUMC) led Tennessee Governor Bill Lee to call for an investigation of the pediatric transgender clinic in September 2022 ( Kruesi, 2022a ). VUMC subsequently paused the surgeries in October of 2022 to review their practices ( Kruesi, 2022b ). Tennessee lawmakers in both chambers have prioritized legislation this session that protects children by banning gender transition interventions for minors—Senate Bill 1 has already passed, and House Bill 1 is expected to pass imminently ( Brown, 2023 ).
Although critics argue that these state policies limit necessary medical care and risk the mental health of transgender youth, all should understand that the restrictions on gender transition interventions do not limit the mental health and supportive treatments available for vulnerable children and adolescents. Instead, the policies seek to increase the “first, do no harm” principle of healthcare and protect children from an area of uncertain science with emerging evidence that is rapidly changing international best practices. Indeed, an evidence review completed for the National Health Service in England found that “any potential benefits of gender-affirming hormones must be weighed against the largely unknown long-term safety profile of these treatments in children and adolescents with gender dysphoria,” ( NICE, 2020 b, p. 14).
National policymakers and, specifically, public health officials would be wise to both listen to Ms. Reed and follow the example of Florida Surgeon General Dr. Ladapo in independently gathering data and taking action to ensure the safety of America’s children.
Conclusion
The U.S. is an outlier among peer European nations in its “affirm-early/affirm-often” approach to medical and surgical interventions for gender dysphoria in children. The low-quality evidence of the current clinical practice guidelines and the unknown long-term consequences merit additional safety measures for children. State policymakers can implement solutions through their medical boards, through legal action, and in their 2023 legislative sessions, while the medical community should more broadly adopt a “first, do no harm” model when treating children with gender dysphoria.
Works Cited
Abbruzzese E, Levine Stephen B, Mason Julia W. (2023, January 2). The Myth of “Reliable Research” in Pediatric Gender Medicine: A critical evaluation of the Dutch Studies—and research that has followed. Journal of Sex & Marital Therapy 0:0, pages 1-27. https://doi.org/10.1080/0092623X.2022.2150346
American Psychiatric Association. (2022a). Gender Dysphoria. Retrieved February 6, 2023, from https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/DSM/DSM-5-TR/APA-DSM5TR-GenderDysphoria.pdf
American Psychiatric Association. Turban, J. (Phys. Rev.). (2022b, August). What is Gender Dysphoria? Retrieved February 6, 2023, from https://www.psychiatry.org/patients-families/gender-dysphoria/what-is-gender-dysphoria
American Psychiatric Association. (2022c). Attention to Culture, Racism, and Discrimination in DSM-5-TR. Retrieved February 9, 2023, from https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/DSM/DSM-5-TR/APA-DSM5TR-AttentiontoCultureRacismandDiscrimination.pdf
American Psychiatric Association. Yarbrough, E., Kidd, J., & Parekh, R. (Phys. Rev.). (2017, November). Gender Dysphoria Diagnosis. Retrieved February 6, 2023, from https://www.psychiatry.org/psychiatrists/diversity/education/transgender-and-gender-nonconforming-patients/gender-dysphoria-diagnosis
Associated Press. (2023, January 29). Utah’s governor has signed a bill banning gender-affirming care for transgender youth. NPR. Retrieved February 6, 2023, from https://www.npr.org/2023/01/29/1152388859/utah-ban-gender-affirming-care-transgender-youth
Barnes, H., & Cohen, D. (2020, December 11). Tavistock puberty blocker study published after nine years. BBC News. https://www.bbc.com/news/uk-55282113
Blanchfield, T. (2022, July 27). What to know about the DSM-5-TR. Verywell Mind. Retrieved February 3, 2023, from https://www.verywellmind.com/what-to-know-dsm-5-tr-changes-5521765
Branstrom Richard, & Pachankis John E (2019, October 4). Reduction in Mental Health Treatment Utilization Among Transgender Individuals After Gender-Affirming Surgeries: A Total Population Study. The American Journal of Psychiatry. https://doi.org/10.1176/appi.ajp.2019.19010080
Brown M. (2023, February 13). Youth gender-transition ban passes Tennessee Senate as legal fight looms. USA Today. Retrieved February 18, 2023, from https://www.usatoday.com/story/news/nation/2023/02/13/trans-youth-medical-ban-passes-tennessee-senate/11251617002/
Bryan, M. (2021, April 6). Arkansas lawmakers ban youth transgender treatment and surgeries, overriding governor’s veto. USA Today.
https://www.usatoday.com/story/news/nation/2021/04/06/arkansas-transgender-surgeries-billlegislature-overrides-gov-asa-hutchinson/7112107002/
Cantor J. M. (2020). Transgender and Gender Diverse Children and Adolescents: Fact-Checking of AAP Policy. Journal of sex & marital therapy, 46(4), 307–313. https://doi.org/10.1080/0092623X.2019.1698481
Carmichael, P., Butler, G., Masic, U., Cole, T. J., De Stavola, B. L., Davidson, S., Skageberg, E. M., Khadr, S., & Viner, R. (2021). Short-term outcomes of pubertal suppression in a selected cohort of 12 to 15 year old young people with persistent gender dysphoria in the UK. PLOS One, 16(2), 1–26. https://pubmed.ncbi.nlm.nih.gov/33529227/
Centers for Disease Control and Prevention. (n.d.). What is venous thromboembolism? Retrieved January 10, 2022, from https://www.cdc.gov/ncbddd/dvt/facts.html
Chen D. et al. (2020, December 11). Consensus Parameter: Research Methodologies to Evaluate Neurodevelopmental Effects of Pubertal Suppression in Transgender Youth. Transgender Health. Dec 2020.246-257. http://doi.org/10.1089/trgh.2020.0006
Coleman E. et al. (2022, September 15). Standards of Care for the Health of Transgender and Gender Diverse People, Version 8. International Journal of Transgender Health, 23:sup1, S1-S259, https://doi.org/10.1080/26895269.2022.2100644
Cosgrove, L., & Krimsky, S. (2012). A comparison of DSM-IV and DSM-5 panel members’ financial associations with industry: a pernicious problem persists. PLoS medicine, 9(3), e1001190. https://doi.org/10.1371/journal.pmed.1001190
Council for Choices in Health Care in Finland. (2020, June 16). Medical treatments for gender dysphoria that reduces functional capacity in transgender people – recommendation. Palveluvalikoima. Retrieved February 6, 2023, from https://palveluvalikoima.fi/documents/1237350/22895008/Summary_minors_en.pdf/aaf9a6e7-b970-9de9-165c-abedfae46f2e/Summary_minors_en.pdf
D’Angelo R., Syrulnik E., Ayad S. et al. One Size Does Not Fit All: In Support of Psychotherapy for Gender Dysphoria. Arch Sex Behav 50, 7–16 (2021). https://doi.org/10.1007/s10508-020-01844-2
Dhejne C., Lichtenstein P., Boman M., Johansson ALV., Langstrom N., Landen M., et al. (2011) Long-Term Follow-Up of Transsexual Persons Undergoing Sex Reassignment Surgery: Cohort Study in Sweden. PLoS ONE 6(2): e16885. https://doi:10.1371/journal.pone.0016885
Do No Harm. (2023a). Reassigned. Retrieved February 6, 2023, from https://donoharmmedicine.org/research/2023/reassigned/
Do No Harm. (2023b, January 28). Do No Harm Launches Nationwide Campaign to Protect Minors from Gender Ideology. Retrieved February 6, 2023, from https://donoharmmedicine.org/2023/01/26/do-no-harm-launches-nationwide-campaign-to-protect-minors-from-gender-ideology/
Do No Harm. Prepared by Cooper & Kirk, PLLC, Thompson DH, Barnes BW, & Ramer JD. (2023c). White Paper: The Justice for Adolescent and Child Transitioners Act. Retrieved February 6, 2023, from https://donoharmmedicine.org/wp-content/uploads/2023/01/DNH_Report_JUSTWhitePaper_v5.pdf
Edwards-Leeper L. & Anderson E. (2021, November 24). The mental health establishment is failing trans kids. Washington Post. https://www.washingtonpost.com/outlook/2021/11/24/trans-kids-therapy-psychologist/
Florida Department of Health. (2022a, April 20). Treatment of Gender Dysphoria for Children and Adolescents. https://www.floridahealth.gov/_documents/newsroom/press-releases/2022/04/20220420-gender-dysphoria-guidance.pdf
Florida Department of Health. (2022b, June 2). Florida Board of Medicine Letter from Surgeon General Ladapo. https://www.documentcloud.org/documents/22050967-board-letter
Florida Agency for Health Care Administration (2o22, June). Florida Medicaid Generally Accepted Professional Medical Standards Determination on the Treatment of Gender Dysphoria. https://ahca.myflorida.com/letkidsbekids/docs/AHCA_GAPMS_June_2022_Report.pdf
Food and Drug Administration. (2022, July 1). Risk of pseudotumor cerebri added to labeling for gonadotropin-releasing hormone agonists. U.S. Department of Health and Human Services. https://www.fda.gov/media/159663/download
H.B.1570, (2021). Biennium, 2021 Re. Sess. (Ark. 2021) https://www.arkleg.state.ar.us/Acts/FTPDocument?path=%2FACTS%2F2021R%2FPublic%2F&file=626.pdf&ddBienniumSession=2021%2F2021R
Health and Human Services. (2022, March). Gender-affirming care and young people. Office of Population Affairs. Office of the Assistant Secretary for Health. U.S. Department of Health and Human Services. Retrieved February 6, 2023, from https://opa.hhs.gov/sites/default/files/2022-03/gender-affirming-care-young-people-march-2022.pdf
Hembree, W. C., Cohen-Kettenis, P. T., Gooren, L., Hannema, S. E., Meyer, W. J., Murad, M. H., Rosenthal, S. M., Safer, J. D., Tangpricha, V., & T’Sjoen, G. G. (2017). Endocrine treatment of gender-dsyphoric/gender-incongruent persons: An Endocrine Society clinical practice guideline. The Journal of Clinical Endocrinology & Metabolism, 11(1), 3869–3903. https://doi.org/10.1210/jc.2017-01658
Herman, J. L., Flores, A. R., & O’Neill, K. K. (2022, September 27). How many adults and youth identify as transgender in the United States? Williams Institute. Retrieved February 6, 2023, from https://williamsinstitute.law.ucla.edu/publications/trans-adults-united-states/
Izaguirre A. (2022, November 4). Florida to ban transgender health care treatments for minors. The Associated Press. Retrieved February 18, 2023 from https://apnews.com/article/ron-desantis-health-business-florida-government-and-politics-78e417a184718de8b9e71ff32efbc77f
Kamens S. R., Elkins D. N., & Robbins B. D. (2017). Open Letter to the DSM-5. Journal of Humanistic Psychology, 57(6), 675–687. https://doi.org/10.1177/0022167817698261
Kawa S., & Giordano J. (2012). A brief historicity of the Diagnostic and Statistical Manual of Mental Disorders: issues and implications for the future of psychiatric canon and practice. Philosophy, ethics, and humanities in medicine, 7(2). https://doi.org/10.1186/1747-5341-7-2
Kalin N.H. (2020, August 1). Reassessing Mental Health Treatment Utilization Reduction in Transgender Individuals After Gender-Affirming Surgeries: A Comment by the Editor on the Process. The American Journal of Psychiatry. https://doi.org/10.1176/appi.ajp.2020.20060803
Kruesi K. (2022a, September 21). Social media posts spark calls to Investigate Tenn.’s VUMC. The Associated Press. Retrieved February 18, 2023, from https://apnews.com/article/health-social-media-tennessee-nashville-730906b47882692645463fe9546a8695
Kruesi,K. (2022b, October 7). Vanderbilt to review gender-affirming surgeries for minors. The Associated Press. Retrieved February 18, 202,3 from https://apnews.com/article/health-business-tennessee-nashville-vanderbilt-university-6deb93f7dea92f1b2082c39f72b59766
Littman L. (2021, October 19). Individuals Treated for Gender Dysphoria with Medical and/or Surgical Transition Who Subsequently Detransitioned: A Survey of 100 Detransitioners. Arch Sex Behav 50, 3353–3369 (2021). https://doi.org/10.1007/s10508-021-02163-w
Mayo Clinic. (2022, February 19). Pubertal blockers for transgender and gender-diverse youth. Retrieved February 9, 2023, from https://www.mayoclinic.org/diseases-conditions/gender-dysphoria/in-depth/pubertal-blockers/art-20459075
National Board of Health and Welfare. (2022, December). Care of children and adolescents with gender dysphoria: Summary of national guidelines. https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/kunskapsstod/2023-1-8330.pdf
National Health Service England. (2016). Clinical commissioning policy: Prescribing of cross-sex hormones as part of the Gender Identity Development Service for children and adolescents. https://www.england.nhs.uk/wp-content/uploads/2018/07/Prescribing-of-cross-sex-hormones-as-part-of-the-gender-identity-development-service-for-children-and-adolesce.pdf
National Health Service England. (2020b). Gender dysphoria: treatment. https://www.nhs.uk/conditions/gender-dysphoria/treatment/
National Institute for Health and Care Excellence. (2020a, October). Evidence review: Gonadotrophin releasing hormone analogues for children and adolescents with gender dysphoria Retrieved February 9, 2023, from https://cass.independent-review.uk/wp-content/uploads/2022/09/20220726_Evidence-review_GnRH-analogues_For-upload_Final.pdf
National Institute for Health and Care Excellence. (2020b, October). Evidence review: Gender-affirming hormones for children and adolescents with gender dysphoria. Retrieved February 9, 2023, from https://cass.independent-review.uk/wp-content/uploads/2022/09/20220726_Evidence-review_Gender-affirming-hormones_For-upload_Final.pdf
Rafferty J., Yogman M., Baum R., Gambon T. B., Lavin A., Mattson G., Wissow L. S., Breuner C., Alderman E. M., Grubb L. K., Powers M. E., Upadhya K., Wallace S. B., Hunt L., Gearhart A. T., Harris C., Lowe K. M., Rodgers C. T., & Sherer I. M. (2018). Ensuring comprehensive care and support for transgender and gender-diverse children and adolescents. Pediatrics, 142(4). https://doi.org/10.1542/peds.2018-2162
Reed J. (2023, February 9). I Thought I Was Saving Trans Kids. Now I’m Blowing the Whistle. The Free Press. https://www.thefp.com/p/i-thought-i-was-saving-trans-kids
Regier D.A., Kuhl E.A., Kupfer D.J. (2013, June 4). The DSM-5: Classification and criteria changes. World Psychiatry. 2013;12:92-98. https://doi.org/10.1002/wps.20050
Respaut R., & Terhune C. (2022, October 6). Number of transgender children seeking treatment surges in the U.S. Reuters. Retrieved February 6, 2023, from https://www.reuters.com/article/usa-transyouth-data/number-of-transgender-children-seeking-treatment-surges-in-u-s-idUKL1N3142UU
Sapir L. (2022). ‘Trust the Experts’ Is Not Enough: U.S. Medical Groups Get the Science Wrong on Pediatric ‘Gender Affirming’ Care. Manhattan Institute. Retrieved February 6, 2023, from https://media4.manhattan-institute.org/sites/default/files/how-to-respond-to-medical-authorities_claiming_gender_affirming_care_safe.pdf
Schwartz D. (2021). Clinical and ethical considerations in the treatment of gender dysphoric children and adolescents: When doing less is helping more. Journal of Infant, Child, and Adolescent Psychotherapy, 20(4), 439–449. https://doi.org/10.1080/15289168.2021.1997344
Shrier A. (2021, October 4). Top trans doctors blow the whistle on ‘sloppy’ care. The Free Press. https://www.thefp.com/p/top-trans-doctors-blow-the-whistle
Sinai J. (2022, June). Rapid onset gender dysphoria as a distinct clinical phenomenon. The Journal of Pediatrics,Volume 245, P250. https://doi.org/10.1016/j.jpeds.2022.03.005
Society for Evidence Gender Based Medicine. (n.d.). About Us. Retrieved February 6, 2023, from https://segm.org/about_us
Society for Evidence Gender Based Medicine. (2023, January 11). The Dutch Studies and The Myth of Reliable Research in Pediatric Gender Medicine. Retrieved February 6, 2023, from https://segm.org/Dutch-studies-critically-flawed
Society for Evidence Gender Based Medicine. (2021a, May 28). “Gender-affirming” Hormones and Surgeries for Gender-Dysphoric US Youth. Retrieved February 6, 2023, from https://segm.org/ease_of_obtaining_hormones_surgeries_GD_US
Society for Evidence Based Gender Medicine. (2021b, December 8). Psychotherapy for children and adolescents with gender dysphoria. Retrieved February 6, 2023, from https://segm.org/Psychotherapy_for_Gender_Dysphoric_Youth
St. Louis Children’s Hospital. (n.d.). Puberty Blockers. Retrieved January 10, 2022, from https://www.stlouischildrens.org/conditions-treatments/transgender-center/puberty-blockers
Surís A., Holliday R., & North C. S. (2016). The Evolution of the Classification of Psychiatric Disorders. Behavioral sciences (Basel, Switzerland), 6(1), 5. https://doi.org/10.3390/bs6010005
Tahir D. (2022, February 1). Medical boards get pushback as they try to punish doctors for Covid misinformation. Politico. https://www.politico.com/news/2022/02/01/covid-misinfo-docs-vaccines-00003383
Terhune C., Respaut R., & Conlin M. (2022, October 6). As more transgender children seek medical care, families confront many unknowns. Reuters. Retrieved February 9, 2023, from https://www.reuters.com/investigates/special-report/usa-transyouth-care/
Texas Attorney General. (2021, December 13). AG Paxton to Investigate Promotion of Puberty Blockers in Children. Retrieved February 6, 2023, from https://www.texasattorneygeneral.gov/news/releases/ag-paxton-investigate-promotion-puberty-blockers-children
Similar Articles
Diagnosing and treating what ails the cdc, 5 steps toward a fresh approach to health care reform, fentanyl a lethal enemy to u.s., let’s fight it that way, join the movement.
- Opt into receiving SMS text messages from AFPI
- Introduction
- Conclusions
- Article Information
Error bars represent 95% CIs. GAS indicates gender-affirming surgery.
Percentages are based on the number of procedures divided by number of patients; thus, as some patients underwent multiple procedures the total may be greater than 100%. Error bars represent 95% CIs.
eTable. ICD-10 and CPT Codes of Gender-Affirming Surgery
eFigure. Percentage of Patients With Codes for Gender Identity Disorder Who Underwent GAS
Data Sharing Statement
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Wright JD , Chen L , Suzuki Y , Matsuo K , Hershman DL. National Estimates of Gender-Affirming Surgery in the US. JAMA Netw Open. 2023;6(8):e2330348. doi:10.1001/jamanetworkopen.2023.30348
Manage citations:
© 2024
- Permissions
National Estimates of Gender-Affirming Surgery in the US
- 1 Department of Obstetrics and Gynecology, Columbia University College of Physicians and Surgeons, New York, New York
- 2 Department of Obstetrics and Gynecology, University of Southern California, Los Angeles
Question What are the temporal trends in gender-affirming surgery (GAS) in the US?
Findings In this cohort study of 48 019 patients, GAS increased significantly, nearly tripling from 2016 to 2019. Breast and chest surgery was the most common class of procedures performed overall; genital reconstructive procedures were more common among older individuals.
Meaning These findings suggest that there will be a greater need for clinicians knowledgeable in the care of transgender individuals with the requisite expertise to perform gender-affirming procedures.
Importance While changes in federal and state laws mandating coverage of gender-affirming surgery (GAS) may have led to an increase in the number of annual cases, comprehensive data describing trends in both inpatient and outpatient procedures are limited.
Objective To examine trends in inpatient and outpatient GAS procedures in the US and to explore the temporal trends in the types of GAS performed across age groups.
Design, Setting, and Participants This cohort study includes data from 2016 to 2020 in the Nationwide Ambulatory Surgery Sample and the National Inpatient Sample. Patients with diagnosis codes for gender identity disorder, transsexualism, or a personal history of sex reassignment were identified, and the performance of GAS, including breast and chest procedures, genital reconstructive procedures, and other facial and cosmetic surgical procedures, were identified.
Main Outcome Measures Weighted estimates of the annual number of inpatient and outpatient procedures performed and the distribution of each class of procedure overall and by age were analyzed.
Results A total of 48 019 patients who underwent GAS were identified, including 25 099 (52.3%) who were aged 19 to 30 years. The most common procedures were breast and chest procedures, which occurred in 27 187 patients (56.6%), followed by genital reconstruction (16 872 [35.1%]) and other facial and cosmetic procedures (6669 [13.9%]). The absolute number of GAS procedures rose from 4552 in 2016 to a peak of 13 011 in 2019 and then declined slightly to 12 818 in 2020. Overall, 25 099 patients (52.3%) were aged 19 to 30 years, 10 476 (21.8%) were aged 31 to 40, and 3678 (7.7%) were aged12 to 18 years. When stratified by the type of procedure performed, breast and chest procedures made up a greater percentage of the surgical interventions in younger patients, while genital surgical procedures were greater in older patients.
Conclusions and Relevance Performance of GAS has increased substantially in the US. Breast and chest surgery was the most common group of procedures performed. The number of genital surgical procedures performed increased with increasing age.
Gender dysphoria is characterized as an incongruence between an individual’s experienced or expressed gender and the gender that was assigned at birth. 1 Transgender individuals may pursue multiple treatments, including behavioral therapy, hormonal therapy, and gender-affirming surgery (GAS). 2 GAS encompasses a variety of procedures that align an individual patient’s gender identity with their physical appearance. 2 - 4
While numerous surgical interventions can be considered GAS, the procedures have been broadly classified as breast and chest surgical procedures, facial and cosmetic interventions, and genital reconstructive surgery. 2 , 4 Prior studies 2 - 7 have shown that GAS is associated with improved quality of life, high rates of satisfaction, and a reduction in gender dysphoria. Furthermore, some studies have reported that GAS is associated with decreased depression and anxiety. 8 Lastly, the procedures appear to be associated with acceptable morbidity and reasonable rates of perioperative complications. 2 , 4
Given the benefits of GAS, the performance of GAS in the US has increased over time. 9 The increase in GAS is likely due in part to federal and state laws requiring coverage of transition-related care, although actual insurance coverage of specific procedures is variable. 10 , 11 While prior work has shown that the use of inpatient GAS has increased, national estimates of inpatient and outpatient GAS are lacking. 9 This is important as many GAS procedures occur in ambulatory settings. We performed a population-based analysis to examine trends in GAS in the US and explored the temporal trends in the types of GAS performed across age groups.
To capture both inpatient and outpatient surgical procedures, we used data from the Nationwide Ambulatory Surgery Sample (NASS) and the National Inpatient Sample (NIS). NASS is an ambulatory surgery database and captures major ambulatory surgical procedures at nearly 2800 hospital-owned facilities from up to 35 states, approximating a 63% to 67% stratified sample of hospital-owned facilities. NIS comprehensively captures approximately 20% of inpatient hospital encounters from all community hospitals across 48 states participating in the Healthcare Cost and Utilization Project (HCUP), covering more than 97% of the US population. Both NIS and NASS contain weights that can be used to produce US population estimates. 12 , 13 Informed consent was waived because data sources contain deidentified data, and the study was deemed exempt by the Columbia University institutional review board. This cohort study followed the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline.
We selected patients of all ages with an International Statistical Classification of Diseases and Related Health Problems, Tenth Revision ( ICD-10 ) diagnosis codes for gender identity disorder or transsexualism ( ICD-10 F64) or a personal history of sex reassignment ( ICD-10 Z87.890) from 2016 to 2020 (eTable in Supplement 1 ). We first examined all hospital (NIS) and ambulatory surgical (NASS) encounters for patients with these codes and then analyzed encounters for GAS within this cohort. GAS was identified using ICD-10 procedure codes and Common Procedural Terminology codes and classified as breast and chest procedures, genital reconstructive procedures, and other facial and cosmetic surgical procedures. 2 , 4 Breast and chest surgical procedures encompassed breast reconstruction, mammoplasty and mastopexy, or nipple reconstruction. Genital reconstructive procedures included any surgical intervention of the male or female genital tract. Other facial and cosmetic procedures included cosmetic facial procedures and other cosmetic procedures including hair removal or transplantation, liposuction, and collagen injections (eTable in Supplement 1 ). Patients might have undergone procedures from multiple different surgical groups. We measured the total number of procedures and the distribution of procedures within each procedural group.
Within the data sets, sex was based on patient self-report. The sex of patients in NIS who underwent inpatient surgery was classified as either male, female, missing, or inconsistent. The inconsistent classification denoted patients who underwent a procedure that was not consistent with the sex recorded on their medical record. Similar to prior analyses, patients in NIS with a sex variable not compatible with the procedure performed were classified as having undergone genital reconstructive surgery (GAS not otherwise specified). 9
Clinical variables in the analysis included patient clinical and demographic factors and hospital characteristics. Demographic characteristics included age at the time of surgery (12 to 18 years, 19 to 30 years, 31 to 40 years, 41 to 50 years, 51 to 60 years, 61 to 70 years, and older than 70 years), year of the procedure (2016-2020), and primary insurance coverage (private, Medicare, Medicaid, self-pay, and other). Race and ethnicity were only reported in NIS and were classified as White, Black, Hispanic and other. Race and ethnicity were considered in this study because prior studies have shown an association between race and GAS. The income status captured national quartiles of median household income based of a patient’s zip code and was recorded as less than 25% (low), 26% to 50% (medium-low), 51% to 75% (medium-high), and 76% or more (high). The Elixhauser Comorbidity Index was estimated for each patient based on the codes for common medical comorbidities and weighted for a final score. 14 Patients were classified as 0, 1, 2, or 3 or more. We separately reported coding for HIV and AIDS; substance abuse, including alcohol and drug abuse; and recorded mental health diagnoses, including depression and psychoses. Hospital characteristics included a composite of teaching status and location (rural, urban teaching, and urban nonteaching) and hospital region (Northeast, Midwest, South, and West). Hospital bed sizes were classified as small, medium, and large. The cutoffs were less than 100 (small), 100 to 299 (medium), and 300 or more (large) short-term acute care beds of the facilities from NASS and were varied based on region, urban-rural designation, and teaching status of the hospital from NIS. 8 Patients with missing data were classified as the unknown group and were included in the analysis.
National estimates of the number of GAS procedures among all hospital encounters for patients with gender identity disorder were derived using discharge or encounter weight provided by the databases. 15 The clinical and demographic characteristics of the patients undergoing GAS were reported descriptively. The number of encounters for gender identity disorder, the percentage of GAS procedures among those encounters, and the absolute number of each procedure performed over time were estimated. The difference by age group was examined and tested using Rao-Scott χ 2 test. All hypothesis tests were 2-sided, and P < .05 was considered statistically significant. All analyses were conducted using SAS version 9.4 (SAS Institute Inc).
A total of 48 019 patients who underwent GAS were identified ( Table 1 ). Overall, 25 099 patients (52.3%) were aged 19 to 30 years, 10 476 (21.8%) were aged 31 to 40, and 3678 (7.7%) were aged 12 to 18 years. Private insurance coverage was most common in 29 064 patients (60.5%), while 12 127 (25.3%) were Medicaid recipients. Depression was reported in 7192 patients (15.0%). Most patients (42 467 [88.4%]) were treated at urban, teaching hospitals, and there was a disproportionate number of patients in the West (22 037 [45.9%]) and Northeast (12 396 [25.8%]). Within the cohort, 31 668 patients (65.9%) underwent 1 procedure while 13 415 (27.9%) underwent 2 procedures, and the remainder underwent multiple procedures concurrently ( Table 1 ).
The overall number of health system encounters for gender identity disorder rose from 13 855 in 2016 to 38 470 in 2020. Among encounters with a billing code for gender identity disorder, there was a consistent rise in the percentage that were for GAS from 4552 (32.9%) in 2016 to 13 011 (37.1%) in 2019, followed by a decline to 12 818 (33.3%) in 2020 ( Figure 1 and eFigure in Supplement 1 ). Among patients undergoing ambulatory surgical procedures, 37 394 (80.3%) of the surgical procedures included gender-affirming surgical procedures. For those with hospital admissions with gender identity disorder, 10 625 (11.8%) of admissions were for GAS.
Breast and chest procedures were most common and were performed for 27 187 patients (56.6%). Genital reconstruction was performed for 16 872 patients (35.1%), and other facial and cosmetic procedures for 6669 patients (13.9%) ( Table 2 ). The most common individual procedure was breast reconstruction in 21 244 (44.2%), while the most common genital reconstructive procedure was hysterectomy (4489 [9.3%]), followed by orchiectomy (3425 [7.1%]), and vaginoplasty (3381 [7.0%]). Among patients who underwent other facial and cosmetic procedures, liposuction (2945 [6.1%]) was most common, followed by rhinoplasty (2446 [5.1%]) and facial feminizing surgery and chin augmentation (1874 [3.9%]).
The absolute number of GAS procedures rose from 4552 in 2016 to a peak of 13 011 in 2019 and then declined slightly to 12 818 in 2020 ( Figure 1 ). Similar trends were noted for breast and chest surgical procedures as well as genital surgery, while the rate of other facial and cosmetic procedures increased consistently from 2016 to 2020. The distribution of the individual procedures performed in each class were largely similar across the years of analysis ( Table 3 ).
When stratified by age, patients 19 to 30 years had the greatest number of procedures, 25 099 ( Figure 2 ). There were 10 476 procedures performed in those aged 31 to 40 years and 4359 in those aged 41 to 50 years. Among patients younger than 19 years, 3678 GAS procedures were performed. GAS was less common in those cohorts older than 50 years. Overall, the greatest number of breast and chest surgical procedures, genital surgical procedures, and facial and other cosmetic surgical procedures were performed in patients aged 19 to 30 years.
When stratified by the type of procedure performed, breast and chest procedures made up the greatest percentage of the surgical interventions in younger patients while genital surgical procedures were greater in older patients ( Figure 2 ). Additionally, 3215 patients (87.4%) aged 12 to 18 years underwent GAS and had breast or chest procedures. This decreased to 16 067 patients (64.0%) in those aged 19 to 30 years, 4918 (46.9%) in those aged 31 to 40 years, and 1650 (37.9%) in patients aged 41 to 50 years ( P < .001). In contrast, 405 patients (11.0%) aged 12 to 18 years underwent genital surgery. The percentage of patients who underwent genital surgery rose sequentially to 4423 (42.2%) in those aged 31 to 40 years, 1546 (52.3%) in those aged 51 to 60 years, and 742 (58.4%) in those aged 61 to 70 years ( P < .001). The percentage of patients who underwent facial and other cosmetic surgical procedures rose with age from 9.5% in those aged 12 to 18 years to 20.6% in those aged 51 to 60 years, then gradually declined ( P < .001). Figure 2 displays the absolute number of procedure classes performed by year stratified by age. The greatest magnitude of the decline in 2020 was in younger patients and for breast and chest procedures.
These findings suggest that the number of GAS procedures performed in the US has increased dramatically, nearly tripling from 2016 to 2019. Breast and chest surgery is the most common class of procedure performed while patients are most likely to undergo surgery between the ages of 19 and 30 years. The number of genital surgical procedures performed increased with increasing age.
Consistent with prior studies, we identified a remarkable increase in the number of GAS procedures performed over time. 9 , 16 A prior study examining national estimates of inpatient GAS procedures noted that the absolute number of procedures performed nearly doubled between 2000 to 2005 and from 2006 to 2011. In our analysis, the number of GAS procedures nearly tripled from 2016 to 2020. 9 , 17 Not unexpectedly, a large number of the procedures we captured were performed in the ambulatory setting, highlighting the need to capture both inpatient and outpatient procedures when analyzing data on trends. Like many prior studies, we noted a decrease in the number of procedures performed in 2020, likely reflective of the COVID-19 pandemic. 18 However, the decline in the number of procedures performed between 2019 and 2020 was relatively modest, particularly as these procedures are largely elective.
Analysis of procedure-specific trends by age revealed a number of important findings. First, GAS procedures were most common in patients aged 19 to 30 years. This is in line with prior work that demonstrated that most patients first experience gender dysphoria at a young age, with approximately three-quarters of patients reporting gender dysphoria by age 7 years. These patients subsequently lived for a mean of 23 years for transgender men and 27 years for transgender women before beginning gender transition treatments. 19 Our findings were also notable that GAS procedures were relatively uncommon in patients aged 18 years or younger. In our cohort, fewer than 1200 patients in this age group underwent GAS, even in the highest volume years. GAS in adolescents has been the focus of intense debate and led to legislative initiatives to limit access to these procedures in adolescents in several states. 20 , 21
Second, there was a marked difference in the distribution of procedures in the different age groups. Breast and chest procedures were more common in younger patients, while genital surgery was more frequent in older individuals. In our cohort of individuals aged 19 to 30 years, breast and chest procedures were twice as common as genital procedures. Genital surgery gradually increased with advancing age, and these procedures became the most common in patients older than 40 years. A prior study of patients with commercial insurance who underwent GAS noted that the mean age for mastectomy was 28 years, significantly lower than for hysterectomy at age 31 years, vaginoplasty at age 40 years, and orchiectomy at age 37 years. 16 These trends likely reflect the increased complexity of genital surgery compared with breast and chest surgery as well as the definitive nature of removal of the reproductive organs.
This study has limitations. First, there may be under-capture of both transgender individuals and GAS procedures. In both data sets analyzed, gender is based on self-report. NIS specifically makes notation of procedures that are considered inconsistent with a patient’s reported gender (eg, a male patient who underwent oophorectomy). Similar to prior work, we assumed that patients with a code for gender identity disorder or transsexualism along with a surgical procedure classified as inconsistent underwent GAS. 9 Second, we captured procedures commonly reported as GAS procedures; however, it is possible that some of these procedures were performed for other underlying indications or diseases rather than solely for gender affirmation. Third, our trends showed a significant increase in procedures through 2019, with a decline in 2020. The decline in services in 2020 is likely related to COVID-19 service alterations. Additionally, while we comprehensively captured inpatient and ambulatory surgical procedures in large, nationwide data sets, undoubtedly, a small number of procedures were performed in other settings; thus, our estimates may underrepresent the actual number of procedures performed each year in the US.
These data have important implications in providing an understanding of the use of services that can help inform care for transgender populations. The rapid rise in the performance of GAS suggests that there will be a greater need for clinicians knowledgeable in the care of transgender individuals and with the requisite expertise to perform GAS procedures. However, numerous reports have described the political considerations and challenges in the delivery of transgender care. 22 Despite many medical societies recognizing the necessity of gender-affirming care, several states have enacted legislation or policies that restrict gender-affirming care and services, particularly in adolescence. 20 , 21 These regulations are barriers for patients who seek gender-affirming care and provide legal and ethical challenges for clinicians. As the use of GAS increases, delivering equitable gender-affirming care in this complex landscape will remain a public health challenge.
Accepted for Publication: July 15, 2023.
Published: August 23, 2023. doi:10.1001/jamanetworkopen.2023.30348
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2023 Wright JD et al. JAMA Network Open .
Corresponding Author: Jason D. Wright, MD, Division of Gynecologic Oncology, Department of Obstetrics and Gynecology, Columbia University College of Physicians and Surgeons, 161 Fort Washington Ave, 4th Floor, New York, NY 10032 ( [email protected] ).
Author Contributions: Dr Wright had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Wright, Chen.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Wright.
Critical review of the manuscript for important intellectual content: All authors.
Statistical analysis: Wright, Chen.
Administrative, technical, or material support: Wright, Suzuki.
Conflict of Interest Disclosures: Dr Wright reported receiving grants from Merck and personal fees from UpToDate outside the submitted work. No other disclosures were reported.
Data Sharing Statement: See Supplement 2 .
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
What Is Gender-Affirming Hormone Therapy?
- How to Get Started
- Masculinizing Therapy
- Feminizing Therapy
- What to Expect
- Access to Treatment
Gender-affirming hormone therapy helps transgender and other gender-nonconforming people align their bodies with their gender identity . Not all transgender (trans) people are interested in hormone therapy. However, many transgender people, particularly binary transgender people, turn to hormones to affirm their gender.
Gender-affirming hormone therapy is comprised of masculizing hormone therapy used in trans men and feminizing hormone therapy used in trans women.
This article describes the goals of gender-affirming hormone therapy, how the treatment is administered, and the different types of hormones used. It also explains what to expect when undergoing gender-affirming hormone therapy and the possible risks.
Verywell / Brianna Gilmartin
Definitions
The term "gender affirmation" is preferred over "gender confirmation" because a transgender person does not need to confirm their gender to anyone. The word "confirm" suggests proof, while "affirm" means to assert strongly.

Who Is Gender-Affirming Hormone Therapy For?
Gender-affirming hormone therapy is the primary medical treatment sought by transgender people. It allows their secondary sex characteristics to be more aligned with their individual gender identity.
Gender-affirming hormone therapy comes in two types:
- Masculinizing hormone therapy used to develop typically male sex characteristics
- Feminizing hormone therapy used to develop typically female sex characteristics
Hormone therapy can be used on its own for people who have no interest in pursuing gender-affirming surgery . It can also be used in advance of surgery (usually for six months to one year) to improve the outcomes of surgery, such as breast augmentation.
According to the National Transgender Discrimination Survey, 95% of transgender people and 49% of non-binary people were interested in hormone therapy.
Hormone Therapy vs. Puberty Blockers
Puberty blockers are used to delay the onset of puberty in young, gender-diverse people prior to the start of hormone therapy. They are considered to be a distinct but complementary component of gender-affirmation therapy.
How to Get Started
Gender affirmation is a process in which hormones only play a part. It typically starts with social gender affirmation in which you alter your appearance, wardrobe, and manner of grooming while updating your name, pronouns, and legal documentation.
Medical gender affirmation is typically the next step in which you work with a healthcare provider to identify your personal goals and which type of types of treatments are needed to achieve those goals.
Hormone therapy is typically overseen by a specialist in the endocrine (hormonal) system called an endocrinologist . Other healthcare providers trained in gender-affirming medical care may be equally qualified to administer treatment.
Depending on state law and other factors, healthcare providers may be able to dispense treatment on the same day. No letter from a mental health provider may be needed. Call Planned Parenthood or your local LGBTI organization to learn about the laws in your state.
To receive authorization for insurance coverage, many insurers require a diagnosis of gender dysphoria . To do so, a therapist or mental health professional must confirm that there is a mismatch between a person's expressed or experienced gender and the gender they were assigned at birth for a period of at least six months.
How to Choose the Right Provider
Not every endocrinologist is equally well-suited to administer gender-affirming hormone therapy. Those who have undergone a comprehensive, multidisciplinary gender-affirmation training program are generally preferred.
Do not hesitate to ask about a healthcare provider's experience and qualifications in administering gender-affirming care.
Masculinizing Hormone Therapy
Masculinizing hormone therapy uses various types of testosterone to promote masculinizing changes in both binary and non-binary individuals. Testosterone is most often given as an injection, but other formations are available, including pills and creams.
There has been growing interest in the use of subcutaneous pellets for testosterone treatment, as they only need to be inserted two to four times a year. However, they are not always available or covered by insurance.
Changes that can be induced by masculinizing hormone therapy include:
- Facial and body hair growth
- Increased muscle mass
- Lowering of the pitch of the voice
- Increased sex drive
- Growth of the glans clitoris
- Interruption of menstruation
- Vaginal dryness
- Facial and body fat redistribution
- Sweat- and odor-pattern changes
- Hairline recession; possibly male pattern baldness
- Possible changes in emotions or interests
Masculinizing hormone therapy cannot reverse all of the changes associated with female puberty. If transmasculine individuals have experienced breast growth that makes them uncomfortable, they may need to address that with binding or top surgery .
Testosterone will also not significantly increase height unless it is started reasonably early. Finally, testosterone should not be considered an effective form of contraception, even if menses have stopped.
Feminizing Hormone Therapy
Feminizing hormone therapy uses a combination of estrogen and a testosterone blocker. The testosterone blocker is needed because testosterone has stronger effects on the body than estrogen.
The blocker most commonly used in the United States is spironolactone , a medication also used for heart disease. The medication used as a puberty blocker, called Supprelin LA (histerline), can also be used to block testosterone.
Various forms of estrogen can be used for feminizing hormone therapy. In general, injectable or topical forms are preferred as they tend to have fewer side effects than oral estrogens. However, some trans women prefer oral estrogens.
Changes that can be induced by feminizing hormone therapy include:
- Breast growth
- Softening of the skin
- Fat redistribution
- Reduction in face and body hair (but not elimination)
- Reduced hair loss/balding
- Muscle-mass reduction
- Decrease in erectile function
- Testicular size reduction
Estrogen cannot reverse all changes associated with having undergone testosterone-driven puberty. It cannot eliminate facial or body hair or reverse shoulder width, jaw size, vocal pitch, or facial structure. Many of these can be addressed with aesthetic or surgical treatments.
What to Expect During Treatment
Some hormones used for gender-affirming hormone therapy are self-administered or given by someone you know. Others need to be administered by a healthcare provider.
Thereafter, regular follow-ups are needed to evaluate the effects of treatment and possible side effects. Most healthcare providers recommend visiting every 3 months for the first year and every 6 to 12 months thereafter.
Effects of Therapy
It can take three to five years for your body to show the full effects of gender-affirming hormone therapy. Some changes can occur within the first six months, such as the development of larger breasts. Others, like changes in facial structure, can take years.
In addition to physical changes, hormone therapy can cause emotional changes. If you are sexually active, it may improve sexual satisfaction as well as your overall sense of well-being. Hormone therapy can also help to ease the stress associated with gender dysphoria.
If you discontinue therapy, some changes may be reversible. Others like changes in bone structure may be permanent.
Possible Risks
As beneficial as gender-affirming hormone therapy can be, it also carries certain risks depending on which hormone you are taking.
Possible risks of feminizing hormone therapy include:
- High blood pressure
- Blood clots
- Heart disease
- Type 2 diabetes
- Weight gain
- Infertility
- Breast and prostate cancer
Risks of masculinizing hormone therapy:
- Male pattern baldness
- High cholesterol
- Pelvic pain
- Sleep apnea
- Interfertility
Access to Gender-Affirming Hormone Therapy
Until relatively recently, access to gender-affirming hormone therapy was largely managed through gatekeeping models that required gender-diverse people to undergo a psychological assessment before they could access hormone treatment.
However, there has been a growing movement toward the use of an informed consent model to better reflect access to other types of medical care. This change has been reflected in the standards of care for transgender health produced by the World Professional Association of Transgender Health (WPATH).
Gender-affirming hormone therapy is considered to be a medically necessary treatment for gender dysphoria. It should be covered by most insurers in the United States after legal changes that occurred as part of the passage of the Affordable Care Act.
However, state laws vary substantially in terms of transgender protections, and some states do allow policies to exclude various aspects of transgender health care, including gender-affirming hormone therapy.
Access to hormone therapy can be prohibitively expensive for many people if they need to pay out of pocket, which may lead some people to try to get these medications from friends or other unlicensed sources.
In addition, individuals who are involved with carceral systems such as immigrant detention may be denied access to hormones. This can have significant negative physical and psychological effects.
Gender-affirming hormone therapy is the primary form of treatment for transgender people. Masculizing hormone therapy involving testosterone is used to develop secondary male sex characteristics like larger muscles. Feminizing hormone therapy involving estrogen and a testosterone blocker is used to develop secondary female sex characteristics like breasts.
Some masculinizing and feminizing effects can occur within months, while others may take years. If you stop treatment, many of the effects will reverse while some will be permanent. Regular follow-up care is needed to avoid potential side effects and long-term complications.
Gardner I, Safer JD. Progress on the road to better medical care for transgender patients . Curr Opin Endocrinol Diabetes Obesity . 2013 20(6):553-8. doi:10.1097/01.med.0000436188.95351.4d
James SE, Herman JL, Rankin S, Keisling M, Mottet M, Anafi M. The Report of the 2015 U.S. Transgender Survey . Washington, DC: National Center for Transgender Equality. 2016.
Planned Parenthood. Gender-affirming hormone therapy: what to expect on your first visit and beyond .
Boskey ER, Taghinia AH, Ganor O. Association of surgical risk with exogenous hormone use in transgender patients: A systematic review . JAMA Surg . 2019;154(2):159-169. doi:10.1001/jamasurg.2018.4598
Almazan AN, Benson TA, Boskey ER, Ganor O. Associations between transgender exclusion prohibitions and insurance coverage of gender-affirming surgery. LGBT Health . 2020;7(5). doi:10.1089/lgbt.2019.0212
White Hughto JM, Reisner SL. A systematic review of the effects of hormone therapy on psychological functioning and quality of life in transgender individuals . Transgender Health . 2016;1(1),21–31. doi:10.1089/trgh.2015.0008
Cavanaugh T, Hopwood R, Lambert C. Informed consent in the medical care of transgender and gender-nonconforming patients . AMA Journal of Ethics . 2016;18(11),1147–1155. doi:10.1001/journalofethics.2016.18.11.sect1-161
World Professional Association for Transgender Health. Standards of Care for the Health of Transsexual, Transgender, and Gender Nonconforming People (7th Version) . WPATH. 2011.
By Elizabeth Boskey, PhD Elizabeth Boskey, PhD, MPH, CHES, is a social worker, adjunct lecturer, and expert writer in the field of sexually transmitted diseases.
New Law Impacting Gender Transition Health Care for Minors
By Kirsten Leloudis
House Bill 808- referred to as Session Law (S.L.) 2023-111 now that it has become law- prohibits the initiation of gender transition health care for transgender minors who were not already actively receiving gender transition health care as of August 1, 2023. The law also creates new penalties for medical professionals who provide gender transition health care to minors, establishes immunity for medical professionals and health care entities that decline to provide such care, and prohibits the use of certain State funds for gender transition health care provided to minors. S.L. 2023-111 was passed after a legislative override of the Governor’s veto and has various effective dates, some of which are retroactive to July 1 or August 1, 2023.
Restriction on Providing Gender Transition Health Care to Minors
The new law prohibits “medical professionals” from delivering three types of gender transition health care to minors: performing “surgical gender transition procedures” and prescribing, providing, or dispensing “puberty-blocking drugs” or “cross-sex hormones.”
Who Is a Minor?
The law defines a minor as any person under age 18. There is no distinction between an emancipated and unemancipated minor; age is the determinative factor.
Who Is a Medical Professional?
For the purpose of this new law, “medical professional” means anyone licensed to practice medicine or to prescribe or dispense drugs under G.S. 90 . This includes physicians, nurse practitioners, physician assistants, pharmacists, and pharmacy technicians. The law clarifies that licensed mental health professionals are not prohibited from treating minors when that treatment is within the scope of the professional’s practice and does not constitute performance of a surgical gender transition procedure or the prescribing, providing, or dispensing of puberty blocking drugs or cross-sex hormones.
The Three Types of Gender Transition Health Care
The law defines a “surgical gender transition procedure” as “[a]ny surgical service, including, without limitation, genital gender reassignment surgery and non-genital reassignment surgery, physician’s services, and inpatient and outpatient hospital services related to gender transition, that seeks to do any of the following for the purpose of effecting a gender transition: (a) Alter or remove physical or anatomical characteristics or features that are typical for the individual’s biological sex. (b) Instill or create physiological or anatomical characteristics that resemble a sex different from the individual’s biological sex.” The terms “ genital gender reassignment surgery ” and “ non-genital reassignment surgery ” also have their own definitions, each of which lists specific procedures that cannot be performed on a minor “for the purpose of assisting an individual with a gender transition.”
“Puberty-blocking drugs” are defined under the new law as “[g]onadotropin releasing hormone analogues or other synthetic drugs used in biological males to stop luteinizing hormone secretion and therefore testosterone secretion, or synthetic drugs used in biological females which stop the production of estrogens and progesterone, when used to delay or suppress pubertal development in children for the purpose of assisting an individual with a gender transition.” Gonadotropin releasing hormone (GnRH) is made in the pituitary gland of the brain in people of all sexes. When GnRH is released from the brain, it tells parts of the body to make certain sex hormones: testicles will respond by producing testosterone and ovaries will make estrogen and progesterone. GnRH is typically low in children until puberty, when the body begins to make more GnRH. This triggers the production of sex hormones- testosterone, estrogen, progesterone- and causes the development of secondary sex characteristics (for example, facial hair or breast development). GnRH analogues can be given to a patient to eventually reduce the pituitary gland’s own production of GnRH, which pauses puberty and the further development of secondary sex characteristics. More information about GnRH and its uses in gender transition health care can be found on the Mayo Clinic’s website .
The law defines “cross-sex hormones” as “[s]upraphysiologic doses of testosterone or other androgens to members of the female biological sex or supraphysiologic doses of estrogen or synthetic compounds with estrogenic activity to members of the male biological sex when used for the purpose of assisting an individual with a gender transition.” The term “ supraphysiologic ” means an amount that is greater than what is normally present in the body. While GnRH analogues can be administered to prevent the further development of secondary sex characteristics, hormones like estrogen and testosterone can be given to prompt the development of certain secondary sex characteristics.
Exception: Gender Transition Health Care Started Before August 1, 2023
The law creates an exception for minors who began receiving gender transition health care prior to August 1, 2023. Specifically, the law allows a medical professional to continue or complete a course of treatment that involves a surgical gender transition procedure or administration of puberty-blocking drugs or cross-sex hormones if three conditions are met. First, the course of treatment must have started before August 1, 2023, and the minor’s care must have been “active” as of August 1, 2023. The law does not include a definition of “active” care. Second, the medical professional must find, in their reasonable medical judgement, that it is in the best interest of the minor to continue or complete the course of treatment. Third, the minor’s parent or guardian must consent to continuation or completion of the treatment.
Exception: Treatment for Certain Health Conditions
The law clarifies that a medical professional may provide a minor with certain types of care, including care that meets the law’s definitions of genital gender reassignment surgery or non-genital gender reassignment surgery, when the minor’s parent or guardian gives informed consent and the care is meant to treat certain health conditions described in the law. This could include, for example, performing breast reduction surgery on a female patient to alleviate a physical health condition.
New Penalties for Medical Professionals and Their Employers
Loss of Licensure
If a medical professional provides care to a minor in violation of the new law, the medical professional’s actions will be considered unprofessional conduct and the medical professional’s license to practice will be revoked. As explained earlier in this blog post, “medical professional” means anyone licensed to practice medicine or to prescribe or dispense drugs under G.S. 90 and includes physicians, nurse practitioners, physician assistants, pharmacists, and pharmacy technicians. The loss of licensure provision takes effect (retroactively) on August 1, 2023. It is not yet clear what this may mean for medical professionals who provided gender transition health care to minors between August 1 and August 16, 2023, when S.L. 2023-111 was passed into law. It is possible that the legislature could amend this and other effective dates in S.L. 2023-111 through later legislation.
Liability and Civil Remedies
The law also establishes civil remedies for an injury (any physical, psychological, emotional, or physiological harm) that a minor suffers as a result of a surgical gender transition procedure, puberty-blocking drugs, or cross-sex hormones. These remedies include declaratory or injunctive relief, compensatory damages, punitive damages, attorneys’ fees, court costs, and any other appropriate relief. A minor can sue and seek these remedies against two parties: the medical professional who provided gender transition health care to the minor and the entity that employed or contracted with the medical professional. Medical professionals and the entities that employ or contract with them are prohibited from contractually waiving either party’s liability under the new law. The law creates liability for injuries that result from even the lawful provision of gender transition health care to a minor. For example, a minor who began gender transition health care before August 1, 2023, could sue a medical professional who lawfully continued providing that gender transition health care if the care later resulted in physical, psychological, emotional, or physiological harm to the minor.
The minor (or a parent or guardian on the minor’s behalf) has a limited timeframe to file a lawsuit against a medical professional or the employing/contracting entity under the new law. This limited timeframe is called a “statute of limitations” or “SOL.” The SOL for claims brought under this new law is the latter of 25 years from when the minor turns 18 (which would be when the minor reaches age 43) or within 4 years of discovering both the injury and the causal relationship between the injury and the gender transition health care that was provided. Typically, under G.S. 143-299 , when a State government department, agency, or institution is the party being sued, the person alleging harm only has three years from when the harm accrued to bring their claim against the State. S.L. 2023-111 creates an exception to this rule and says that the longer SOL described in the new law applies to claims made against State government, too. Additionally, G.S. 90-21.19(a) , which limits the noneconomic damages (money) that can be awarded in a medical malpractice case, does not apply to claims brought under the new law. The section of S.L. 2023-111 that establishes liability for medical professionals and their employers and contracting entities takes effect (retroactively) on July 1, 2023.
Immunity for Not Providing Gender Transition Health Care
Under the new law, no medical professional or an entity that employs or contracts with a medical professional can be required to perform a surgical gender transition procedure or to prescribe, provide, or dispense puberty-blocking drugs or cross-sex hormones. Furthermore, hospitals and health care institutions cannot be required to participate in or allow the use of their facilities by a medical professional providing gender transition health care, regardless of whether the medical professional is an employee or contractor or if the medical professional has admitting privileges for the hospital or health care institution. Medical professionals, entities that employ or contract with medical professionals, hospitals, and other health care institutions cannot be held civilly, criminally, or administratively liable for declining to provide or be involved in providing gender transition health care to minors. The section of S.L. 2023-111 that establishes these liability protections went into effect (retroactively) on August 1, 2023.
Limits on Use of State Funds
The new law prohibits the use of State funds, “directly or indirectly,” for the performance of or “in furtherance of” surgical gender transition procedures or the provision of puberty-blocking drugs or cross-sex hormones to a minor. The law does not define what it means to use State funds “in furtherance of” gender transition health care. Additionally, State funds cannot be used to administer any governmental health plan or government-offered insurance plan that covers surgical gender transition procedures, puberty-blocking drugs, or cross-sex hormones for minors. This means that a family enrolled in Medicaid, for example, cannot use the Medicaid program to help cover the costs of gender transition health care for a minor in the family. The provision of S.L. 2023-111 that bars the use of State funds for gender transition health care went into effect (retroactively) on August 1, 2023.
The law carves out the State Health Plan for Teachers and State Employees (hereinafter, the “State Health Plan”) from the prohibition against using State funds for gender transition health care. The State Health Plan provides coverage to an estimated 750,000 teachers, state employees, retirees, and their dependents across North Carolina. The carve out for the State Health Plan is likely due to a recent order issued in Kadel v. Folwell, No. 1:19CV272, 2022 WL 1046313 (M.D.N.C. Apr. 7, 2022) that enjoined the State Health Plan from not providing coverage for certain types of gender transition health care. The Session Law notes that the ban on using State funds for gender transition health care will apply to the State Health Plan after 30 days if the injunction in Kadel v. Folwell is vacated, overturned, or no longer in force.
Frequently Asked Questions
What if a minor wants to start gender transition health care after August 1, 2023, and the minor’s parent or guardian consents to the care?
The law does not create an exception for situations where a minor’s parent or guardian gives consent for the minor to have a surgical gender transition procedure or receive puberty-blocking drugs or cross-sex hormones. Therefore, gender transition health care cannot be initiated for a minor after August 1, 2023 even if the minor’s parent or guardian consents to the care.
Does the new law mean that minors cannot receive certain surgeries, puberty-blocking drugs, or hormones as treatment that is not “for the purpose of assisting an individual with a gender transition?”
No. The law only restricts the performance of a surgical gender transition procedure on a minor or the prescribing, providing, or dispensing of puberty-blocking drugs or cross-sex hormones to a minor when the purpose of that health care is to assist an individual with a gender transition.
For example, GnRH analogues are used to treat various health conditions, including precocious puberty , which occurs when a child begins puberty too early. Because the law defines “puberty-blocking drugs” to only include situations where the drugs are used “for the purpose of assisting an individual with a gender transition,” the law should not limit the provision of GnRH analogues as treatment for precocious puberty in minors.

Coates’ Canons NC Local Government Law
All rights reserved. This blog post is published and posted online by the School of Government to address issues of interest to government officials. This blog post is for educational and informational use and may be used for those purposes without permission by providing acknowledgment of its source. Use of this blog post for commercial purposes is prohibited. To browse a complete catalog of School of Government publications, please visit the School’s website at www.sog.unc.edu or contact the Bookstore, School of Government, CB# 3330 Knapp-Sanders Building, UNC Chapel Hill, Chapel Hill, NC 27599-3330; e-mail [email protected]; telephone 919.966.4119; or fax 919.962.2707.

Wyoming governor signs bill outlawing gender-reassignment procedures on children, vetoes abortion restrictions
Wyoming's Republican Governor Mark Gordon signed into legislation Friday a bill outlawing gender-reassignment procedures on children and vetoed a bill that would have imposed further restrictions on abortion clinics, including required licensure.
SF0099, also titled "Children gender change prohibition," prohibits physicians from performing gender-reassignment procedures on children and administering related medications. The legislation specifically banned "a surgery that sterilizes the child, including castration, vasectomy, hysterectomy, oophorectomy, metoidioplasty, orchiectomy, penectomy, phalloplasty and vaginoplasty."
The legislation continued on to specify that outlawed medications under the legislation included "any of the following prescription drugs that induce transient or permanent infertility," proceeded by a list of medications , including "puberty suppression or blocking prescription drugs to stop or delay normal puberty."
WYOMING JUDGE TO RULE ON ABORTION LAWS, INCLUDING THE FIRST-IN-THE-NATION BAN ON ABORTION PILLS
The bill also outlined various procedures that were exempt from the legislation, such as procedures or treatments performed on a child as a result of "a medically verifiable genetic disorder of sex development." The legislation specified that parental/guardian consent was required.
"I signed SF99 because I support the protections this bill includes for children, however, it is my belief that the government is straying into the personal affairs of families" Gordon said in a statement released. "Our legislature needs to sort out its intentions with regard to parental rights. While it inserts governmental prerogative in some places, it affirms parental rights in others."
READ ON THE FOX NEWS APP
TRUMP SUGGESTS HE WOULD SUPPORT ABORTION BAN AT AROUND 15 WEEKS OF PREGNANCY
Gordon also vetoed HB0148, known as "Regulation of abortions," that would have placed additional restrictions on abortion clinics in the state. The press release noted that the bill would have "properly regulated surgical abortion clinics in Wyoming," but "amendments to the bill complicated its purpose, making it vulnerable to legal challenges."
The legislation would have required a surgical abortion facility in the state to be licensed as "an ambulatory surgical center," and a facility conducting the procedures would need a separate license as well.
NEW STUDY FINDS WOMEN WHO CHOOSE SUPPORTIVE BIRTH SERVICES OVER ABORTION BENEFIT IN TRAGIC FETAL ANOMALY CASES
"It is my opinion that HB148, as amended, had the potential to further delay the resolution of this critical issue for the unborn," Gordon said in the statement. "The potential of starting over on a new course of legal arguments would in my mind be derelict, and would have only sacrificed additional unborn lives in Wyoming."
Abortion is currently legal in Wyoming, pending a court decision challenging the state's abortion laws.
On the national scale, the U.S. Supreme Court is set to hear oral arguments Tuesday about the federal government's approval process of the drug mifepristone, a medication used to terminate pregnancies. A ruling is expected about three months later.
The Supreme Court is currently allowing the FDA to continue regulating the drug while the appeals process plays out. Such regulation includes continued telemedicine prescriptions and retail pharmacy dispensing.
Fox News' Shannon Bream, Bill Mears and The Associated Press contributed to this report.
Original article source: Wyoming governor signs bill outlawing gender-reassignment procedures on children, vetoes abortion restrictions

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Oestrogen and anti-androgen therapy for transgender women
Vin tangpricha.
Division of Endocrinology, Metabolism and Lipids, Department of Medicine, Emory University School of Medicine and Atlanta VA Medical Center, Atlanta, GA, USA
Prof Martin den Heijer
Department of Endocrinology and Center of Expertise on Gender Dysphoria, VU University Medical Center, Amsterdam, Netherlands
Transgender women experience lifelong gender dysphoria due to a gender assignment at birth that is incongruent with their gender identity. They often seek hormone therapy, with or without surgery, to improve their gender dysphoria and to better align their physical and psychological features with a more feminine gender role. Some of the desired physical changes from oestrogen and anti-androgen therapy include decreased body and facial hair, decreased muscle mass, breast growth, and redistribution of fat. Overall the risks of treatment are low, but include thromboembolism, the risk of which depends on the dose and route of oestrogen administration. Other associated conditions commonly seen in transgender women include increased risks of depression and osteoporosis. The risk of hormone-sensitive cancer seems to be low in transgender women, with no increased risk of breast cancer compared with women and no increase in prostate cancer when compared with men. The evidence base for the care of transgender women is limited by the paucity of high-quality research, and long-term longitudinal studies are needed to inform future guidelines.
Introduction
Transgender and gender-non-conforming people often seek hormone therapy, with or without surgery, to change their physical appearance to match their reaffirmed gender, and to alleviate the stress and discomfort associated with living in the incongruent gender. 1 The uneasy feeling of living in an incongruent gender role is termed gender dysphoria. Transgender women, also referred to as transwomen or male-to-female transsexuals, are born with male genitalia and are typically assigned a male gender at birth. Gender dysphoria often presents in childhood. However, children often cannot articulate their discomfort or do not have a supportive family environment to seek medical attention, and thus present to health-care providers with gender dysophoria later in adulthood. Gender dysphoria can also present in adulthood without a clear start in childhood.
The prevalence of gender dysphoria or non-conforming gender identity is a topic of ongoing investigation. The precise number of transgender women estimated in a given population depends on the definition used. One early study in the Netherlands defined all patients who were treated with hormones and underwent surgery as transgender, 2 and the investigators reported the prevalence of transgender women to be one in 11 900 people. A study from Ireland defined a transgender woman as a person assigned male gender at birth who is receiving oestrogen therapy, 3 showing a similar prevalence of one in 10 154 people. Investigators of one of the largest cohort studies in the USA, which used US Veterans Health Administration data, reported a slightly higher prevalence of 3·29 in 10 000 people, based on codes in the ninth revision of the International Statistical Classification of Diseases used to charge for transgender services. 4 Unfortunately, because of limitations of the study design, the researchers were unable to comment on whether these people were all transgender women; however, the veteran population tends to be predominantly men. In a 2016 systematic review of 29 studies, 5 the prevalence of transgender women was roughly 5–20 per 100 000 when diagnostic codes or requests for medical treatment were used, or as high as 521 per 100 000 people if based on self-identification.
Hormonal therapy with gonadotropin-releasing hormone agonists can be started in early puberty (Tanner stage 2–3) to avoid the development of secondary sex characteristics in some individuals who have had appropriate mental health assessment, with the caveat that future fertility could be compromised. Oestrogen therapy follows treatment with gonadotropin-releasing hormone agonists in children, or can be combined with other testosterone-lowering drugs in adults. Several published guidelines exist to aid clinicians in the assessment, diagnosis, and medical treatment of adult transgender individuals. The World Professional Association for Transgender Health (WPATH) publishes comprehensive guidelines for health professionals that address all aspects of health care for gender-nonconforming people. 1 The Endocrine Society publishes clinical practice guidelines that address the initiation and monitoring of hormone therapy for transgender children and adults. 6 Other guidelines exist, including a clinical practice guideline published by the Royal College of Psychiatrists in the UK. 7
In this Review, we provide an overview of the published literature on oestrogen and anti-androgen therapy in adult transgender women (ie, after puberty). The focus will be on the established treatment regimens, reported potential adverse events, long-term care and monitoring, and areas of uncertainty in the care of transgender women.
Oestrogen and anti-androgen therapy
An important goal for transgender women is to live as a woman in society and to have—as far as possible—a body that appears female (ie, to undergo feminisation). Secondary sex characteristics are formed under the influence of sex hormones, so an important factor in the male-to-female transition is to change the balance between oestrogens and androgens (ie, cross-sex hormone treatment). Important physical features in feminisation are breast growth, female body composition (ie, more adipose tissue on the hips and less in the abdominal region), and softer skin. Additionally, sex hormones affect the brain to change mood and have an effect on libido ( figure ).

Effects of oestrogen and anti-androgen therapy in transgender women
Supplementation with oestrogens lowers testosterone concentrations because of negative feedback on the hypothalamic–pituitary–gonadal axis. With the initiation of oestrogen therapy alone, testosterone concentrations decrease into the low-normal range for a man (200–300 ng/dL [6·9–10·4 nmol/L]), but are still above the normal range for a woman (<75 ng/dL [<2·6 nmol/L]). 8 Most patients will require the addition of an anti-androgen medication to further inhibit testosterone production or to block the androgen receptor. Anti-androgen treatments such as spironolactone (in doses up to 400 mg daily) and cyproterone (in doses up to 100 mg daily) are effective adjunctive therapies, given in addition to oestrogen to lower testosterone concentrations into the female range. 9 – 12 Spironolactone is better known as an aldosterone antagonist, but it also has antagonistic effects on the androgen receptor and can act as an oestrogen receptor agonist. 13 Spironolactone could induce hyperkalaemia, especially in patients with impaired renal function. Prior and colleagues 8 showed that the addition of spironolactone to oestrogen therapy is often necessary to lower testosterone values to the female range. In this study, high-dose oestrogen plus medroxyprogesterone led to a mean testosterone concentration of 169 ng/dL (5·9 nmol/L; SD 193 ng/dL [6·7 nmol/L]), whereas adding spironolactone to this regimen led to a mean testosterone concentration of 87 ng/dL (3 nmol/L; SD 111 ng/dL [3·8 nmol/L]).
Several other drugs can be used to lower testosterone including cyproterone and gonadotropin-releasing hormone agonists such as goserelin. Results of studies by Toorians and colleagues 10 and Gava and colleagues 11 showed that cyproterone, in combination with oestradiol, reduced testosterone to less than 30 ng/dL (1 nmol/L). However, there are no head-to-head studies that establish the superiority of one testosterone-lowering drug over another. Additionally, choices for one drug or another are primarily based on local regulations and reimbursement principles. Cyproterone seems to have a stronger anti-androgenic action than spiro nolactone, 14 but depression is a potential side-effect. 15 Cyproterone has anti-androgenic effects through antagonising the androgen receptor, but also has anti-gonadotropic effects. The gonadotropin-releasing hormone analogues such as leuprolide, histrelin, or goserelin work by reducing the secretion of luteinising hormone and follicle-stimulating hormone, which leads to decreased stimulation of testicular testosterone production. In 2016, the results of a small retrospective study showed similar anti-androgenic effects of both cyproterone and the gonadotropin-releasing hormone agonist leuprolide. 11 Gonadotropin-releasing hormone analogues have relatively few effects other than lowering gonadal hormone concentrations. Gonadotropin-releasing hormone agonists are commonly prescribed in adolescents with gender dysphoria as a puberty blocker, to block the onset of puberty, but they might be used also in adult patients who have adverse drug reactions to anti-androgen therapy with spironolactone or cyproterone. The occurrence of (multiple) meningiomas has been reported in association with longer-term use (ie, use over several years) of cyproterone at doses of 25 mg daily or higher. 16 – 19 As a result, in the UK, gonadotropin-releasing hormone agonists are prescribed as the only androgen-lowering agents used in conjunction with oestrogens in the treatment of transgender women in National Health Service gender identity clinics. 20
Some patients request progesterone for enhanced breast growth. However, there have not been any well designed studies to assess the effectiveness of progesterone to improve breast development. Results of studies of progesterone combined with oestrogen in postmenopausal cis-gender women—ie, women who are not transgender—suggest that progesterone combined with oestrogen might be associated with an increased risk of cardiovascular disease. 21 In fact, in a population-based study of premenopausal cis-gender women, taking oral contraceptives including progesterone with or without oestrogen was associated with increased risk of thromboembolism. 22
Finasteride has been used in transgender women as an anti-androgen. 23 This drug is a 5-α reductase inhibitor and might increase testosterone concentration by blocking synthesis of dihydrotestosterone from testosterone. However, this drug is not recommended as a first-line treatment because such drugs might lead to worsened depression. 24
Treatment regimens and guidelines
WPATH and the Endocrine Society have released evidence-based guidelines for the treatment of transgender women ( table 1 ). 1 , 6 Both guidelines suggest that cross-sex hormone treatment be initiated in adults with well documented gender dysphoria and who are able to provide informed consent for treatment. 1 , 6 Furthermore, the guidelines recommend assessment of medical and mental health issues that can be exacerbated by hormone therapy before initiation of cross-sex hormone treatment. 1 , 6
Recommendations from the Endocrine Society’s clinical practice guidelines 6
The hormonal regimens used for transgender women are not standardised across the world ( table 2 ), partly because of regional differences in the availability of oestrogen and testosterone-lowering preparations, as well as cost considerations and differences in practices between countries and centres. 25 For example, in some European countries (Belgium, Germany, Italy, Netherlands, and Norway) common regimens include oral oestradiol combined with cyproterone (50 mg daily). 26 In the UK, oral oestradiol is combined with gonadotropin-releasing hormone agonists. 7 In the USA, all forms of oestradiol are available (parenteral, oral, and patches or gels) and are combined with spironolactone. Conjugated oestrogens and synthetic oestrogens such as ethinylestradiol are not recommended because physicians are unable to monitor their concentrations in the blood, and because of the potential of these drugs to increase the risk of thromboembolism compared with other oestrogens. 27 Because gonadotropin-releasing hormone agonists more effectively suppress endogenous sex steroids than other testosterone-lowering drugs, and could be associated with fewer short-term side-effects, the combination of oral oestradiol and gonadotropin-releasing hormone agonists might be regarded as the superior regimen; however, there are no published long-term studies apart from a small retrospective study in 40 patients, the results of which showed the equivalent effectiveness of cyproterone and leuprolide. 11 Furthermore, the use of gonadotropin-releasing hormone agonists is limited in many countries because of their cost, which is greater than 1000 per year per patient in Europe, with even higher prices in the USA.
Oestrogen and anti-androgen preparations for transgender women
Some formulations are not available in certain countries.
Concentrations of oestradiol and testosterone should be monitored every 3–6 months in the first 2 years of therapy, then annually to ensure that they are in the physiological range for a woman, and especially to ensure that oestradiol concentrations do not exceed peak levels (<400 pg/mL [13·9 nmol/L]) seen in women. 6 The precise concentration of oestradiol that results in adequate feminisation with the lowest risk of complications is not known. 28 For transgender women taking spironolactone, it is advisable to measure serum potassium concentrations every 3–4 months in the first 2 years, then annually, since the potassium concentrations could increase during spironolactone therapy. 6 After gonadectomy, testosterone concentrations drop to nearly zero—only a small amount is still produced by the adrenal glands—and thus, after surgery, anti-androgens can be discontinued. Serum testosterone can be measured within a month after surgery to confirm that testosterone concentrations are low (ie, <50 pg/mL [1·7 nmol/L]) and that testosterone-lowering medications are not needed. It is important to keep the dose of oestrogen at a level that not only maintains sex characteristics and relieves gender dysphoria, but is also adequate to prevent osteoporosis, hot flashes, and mood disorders. 29
We recommend that hormones be prescribed under medical supervision to allow monitoring of hormone levels and screening for potential adverse events. However, many transgender women have inadequate access to health-care providers who have experience with transgender medicine. 30 Other barriers to care include the financial costs of medical care, discrimination against transgender patients, and other socioeconomic and cultural barriers . 31 As a result, up to 50% of transgender women might self-medicate with hormones before seeking the advice of a physician . 15 , 32 , 33 Transgender women who self-prescribe often have a poor understanding of potential side-effects and safe doses of oestrogens, and can report inadequate breast growth. 40 Although less is known about transgender women who self-medicate with cross-hormone therapy, oestrogen and anti-androgen treatment taken under medical supervision seems to be associated with few adverse events. 42
Expected time course and physical changes
The Endocrine Society guidelines for endocrine treatment of transsexual people presents an overview of the feminising physical effects of cross-sex hormone treatment in transgender women, most of which start within a few months and progress for 2–3 years. 6 However, there is a shortage of high-quality evidence about the precise time course and effect-modifiers of these feminising effects, which is partly because these changes cannot be easily measured. Clinically, the most compelling effects of cross-sex hormone treatment are softening of the skin, mood changes, a decrease in libido and erections, fat redistribution at the hips, and growth of breast tissue. Results of studies that focused on bodyweight and composition indicate an increase in bodyweight of 1–3 kg per year, with an increase in fat mass (2–4 kg) and a decrease in lean body mass (2–4 kg) after 1 year of cross-sex hormone treatment. 9 , 12 , 36 The fat mass increases are apparent as both visceral and subcutaneous fat depots. 37 , 38
An important issue for many transgender women is breast development. But despite its importance, only a few low-quality studies have been done to investigate the effect of cross-sex hormone therapy on this outcome. 39 Breast development starts within 2–3 months after initiation of combined oestrogen and anti-androgen treatment, and takes up to 2 years to complete. In a longitudinal study by Meyer and colleagues, 34 breast hemi-circumference increased by 14 cm after 3 years of oestrogen therapy. The response to oestrogen can vary from individual to individual. Up to two-thirds of transgender women are unsatisfied with their breast development and apply for breast augmentation surgery . 40 No evidence exists that the addition of progesterone improves breast development. 39 Cross-sex hormone treatment has also been reported to lead to softening of the skin and feminine hair growth, but systematic studies have not been done. 35 , 41
Comorbidities and pitfalls
Although cross-sex hormone treatment is now regarded as fairly safe when taken under medical supervision, several associated comorbid conditions can occur with hormone therapy. 42 Since oestrogen and testosterone-lowering drugs are often taken in combination and the specific drugs used vary by country and region, it can be difficult to attribute comorbid conditions specifically to oestrogen or testosterone-lowering drugs.
Thromboembolic disease
Oestrogen use is associated with an increased risk of venous thrombosis, as has been reported in many studies of oral contraceptives and postmenopausal hormonal replacement in women. 43 The risk of venous thrombosis in the general population of non-transgender women and men who are not taking oestrogen ranges from one to two events annually per 1000 individuals; incidence increases with age. 44 Bell and colleagues 45 reported the remaining lifetime risk of thromboembolism to be 8·1% (95% CI 7·1–8·7) in a cohort of non-transgender, middle-aged adults (aged 45–64 years) living in the USA. Oestrogen is believed to be the key component in the causation of venous thrombosis, which might be modified by the route of administration of oestrogen or whether it is taken with progestogens. 46
The lifetime risk of venous thrombosis in transgender women has been reported to range between 1% and 5%. However, many of the studies were small and very short in follow-up time. 47 Furthermore, many venous thrombotic events are likely to be under-reported. Data from early studies in transgender women in the Netherlands suggested a high lifetime prevalence (about 5% over a mean of 10 years of follow-up) of thromboembolic disease. 48 However, subsequent studies indicate that the risk of thromboembolic disease is much lower, and that the cause of the increased risk of thromboembolic disease in the earlier cohort was due to the use of ethinylestradiol. 49 Indeed, reports from several European centres have suggested that the lifetime risk of thromboembolism is very low (about 1%). 9 , 50 , 51 In one study from Belgium, the investigators reported that three of 50 transgender women had a thromboembolic event. 52 In a retrospective chart review of 165 transgender women, the prevalence of thromboembolism was 1·2%, and was more frequent with the use of conjugated oestrogens, compared with other oestrogen preparations. 40
The risks of thromboembolism can also be modified by the route of drug administration. A meta-analysis and systematic review of oestrogen replacement therapies in cis-gender women showed that oral oestrogen, but not transdermal oestrogens, increased the risk of venous thromboembolism. 53 A transgender clinic in Amsterdam, Netherlands, noted a 50% reduction in risk of venous thromboembolism after recommending that all trans-gender women older than 40 years change from oral to transdermal oestrogen. 48 Additionally, Ott and colleagues 50 identified no cases of venous thromboembolism 162 transgender women treated with transdermal oestrogen and followed up for a mean of 5 years, lending support to the belief that transdermal preparations could be less thrombogenic than oral oestrogen.
Although the lifetime risk of thromboembolic disease seems to be low in patients followed up in multispecialty gender clinics, providers should inform patients about the potential risk of thromboembolic disease due to oestrogen treatment, and which factors modify this risk. Modifiers in transgender women include the oestrogen preparation used (ethinylestradiol or conjugated oestrogens vs 17–β oestradiol), dosing method (oral vs transdermal), age (older than 50 years is associated with increased risk), obesity (body-mass index >27), 54 and postoperative state (with prophylaxis for deep venous thrombosis vs without). 27 We believe that transgender women who continue to smoke should be switched to transdermal oestrogens, although there are few data to suggest that this reduces risk of thromboembolism.
Osteoporosis
Cross-sex hormone treatment with oestrogens should be protective of bone density, since oestrogens are the major sex steroid hormone that prevents bone loss in both men and women. 55 Low bone density is common after gonadectomy if oestrogen is not prescribed at adequate doses to prevent oestrogen concentrations from dropping into a menopausal range. 56 Some study findings suggest that low bone density can be present initially in transgender women. Up to 16% of transgender women have T-scores less than –2·5 at the hip or spine bones at initial presentation, indicating that osteoporosis might occur even before initiation of oestrogen treatment, and can be present in transgender women in their 20s or 30s. 57 , 58 The cause of low bone density in transgender women before the initiation of cross-sex hormone treatment is unclear. Potential causative factors might include poor nutrition and vitamin D status, and low levels of physical activity and exercise. 48 Although there are no established guidelines about when bone mineral density testing should be done, it might be prudent to check an initial screening dual energy x-ray absorptiometry after age 40 years if risk factors are present, or if there is a personal history of fracture. Despite reports of low bone density occurring in transgender women, there are very few reports of fragility fractures occurring in transgender women. 59
Liver disease
Liver disease was a concern in initial cohort studies, wherein abnormal liver function tests were reported to occur in up to 15% of transgender women . 60 However, it was subsequently determined that the cause of the abnormal findings was not the use of oestrogen; rather the liver function abnormalities identified were secondary to alcohol misuse or viral hepatitis. 48 In a longitudinal cohort study of transgender women in Europe, roughly 5% of study participants had transient increases in liver enzyme concentrations to greater than twice the normal range, but values returned to the normal range after 12 months. 36 Another study conducted in the USA found that measurements of aspartate aminotransferase and alanine aminotransferase in transgender women did not differ from either the male or female reference range. 61 These data suggest that oestradiol might not be hepatotoxic, as previously believed on the basis of data from earlier cohort studies. 60 The alterations in liver function tests reported in earlier studies might have been due to the older age of the early Dutch cohort compared with recent cohorts, differences in alcohol intake, and the formulation of oestrogen treatment used. The risk of oestrogen therapy with respect to liver function remains an area of uncertainty, and the Endocrine Society guidelines recommend periodic measurement of liver function tests.
Lipid abnormalities
Treatment of postmenopausal women with oestrogen, with or without progesterone, has been associated with an increase in triglycerides and HDL cholesterol and a decrease in total and LDL cholesterol. 62 , 63 In premenopausal women, oral contraceptive pills containing oestrogen and progesterone also seem to be associated with increased total cholesterol, triglyceride, and HDL cholesterol concentrations. 64 Results of one of the largest studies examining the effect of oestrogen (given as conjugated equine oestrogen, 0·625 mg daily) and progesterone compared with placebo, in postmenopausal women, showed increases in HDL cholesterol and triglycerides, and decreases in LDL and total cholesterol. 62
Specific to transgender women, data from several longitudinal cohort studies 15 , 38 , 65 suggest that oestrogen (with or without progesterone) increases triglyceride concentrations. In a meta-analysis of 23 studies including 3231 transgender women, Maraka and colleagues 66 reported that oral oestrogen increased serum triglyceride concentrations by about 30 mg/dL (0·34 nmol/L) after 24 months from initiation of oestrogen therapy, with no changes in other lipid parameters, including HDL and LDL cholesterol. However, the oestrogen regimens included in this meta-analysis included different anti-androgen preparations including cyproterone, gonadotropin-releasing hormone agonists, and spironolactone, making it difficult to attribute the changes in lipids caused by oestrogen treatment alone. Only 14 of 1073 transgender women were reported to have had a myocardial infarction in this meta-analysis. It is difficult to interpret whether this represents an increased risk of myocardial infarction without a control group of transgender women who are not being treated with oestrogen therapy. Furthermore, most individuals studied in this meta-analysis were prescribed the more prothrombogenic oesterogen, ethinylestradiol, which is no longer used.
Mental health and depression
The prevalence of psychiatric and mood disturbances is high among transgender people. 67 Several reports suggest that cross-sex hormone treatment improves quality of life and depressive mood symptoms. 68 – 71 In a systematic review and meta-analysis of 28 studies including more than 1800 transgender people (with about 1100 transgender women), hormone treatment, with or without surgery, improved gender dysphoria and quality of life in 80% (95% CI 72–88; 16 studies; I 3=78%) of patients. 72 However, suicide rates remain high in transgender people after hormone therapy, with or without gender reaffirming surgery. 73 – 76 Blosnich and colleagues 73 reported that the crude rate of suicide among transgender military veterans was 82 per 100 000 person-years, which is higher than the rates in non-transgender veterans and the US population, but similar to suicide rates seen in veterans with depression, schizophrenia, and substance misuse. 77 , 78 It is important that clinicians screen for signs of depression and suicidal ideation at each visit, and to refer patients for counselling and psychiatric treatment when needed.
Breast cancer
Several reports have suggested an increased risk of breast cancer in transgender women. 79 In one of the largest cohorts of transgender women and transgender men, the overall prevalence of breast cancer was 20·0 per 100 000 patient-years of cross-sex hormone treatment. 80 For transgender women specifically, the standardised incidence ratio was 0·7 (95% CI 0·03–5·57) compared with natal women, but 33·3 (21·89–45·17) compared with biological men. 81 There are no clear guidelines for when mammogram screening for breast cancer should start. In the absence of any evidence, in our opinion, it could be reasonable to start mammogram screening in transgender women at the same age recommended for cis-gender women, or earlier if known risk factors are present, such as a family history of breast cancer. 81
Prostate cancer
Since castration—either surgical or medical—is the primary treatment in prostate cancer, it might be expected that the incidence of prostate cancer is low in transgender women. Indeed, reports of prostate cancer have been limited to a few case reports. 82 In a review of more than 1000 transgender women followed up by the Amsterdam clinic, only one case of prostate cancer was discovered. 83 On the basis of the low overall prevalence of prostate cancer, these authors suggest screening for prostate cancer only after age 50 years.
Special considerations
Gender-reaffirming surgery.
Cross-sex hormone treatment affects secondary sex characteristics of transgender women, making them more feminine in appearance; however, it has little effect on the primary sex organs except to cause some testicular atrophy. 6 Therefore, many transgender women will seek gender reaffirming surgeries to remove the testes and to create a neovagina. 84 Breast development under cross-sex hormone treatment can often be unsatisfactory and thus many transgender women might choose to have breast augmentation surgery. 85 In transgender women who initiate cross-sex hormone treatment after puberty, secondary male sex characteristics might require surgery such as chondrolaryngoplasty (the so-called tracheal shave) for a prominent larynx or facial feminisation for frontal bossing. 86 , 87 Laryngoplasty can also be done to change the pitch of the voice. 88 Before laryngoplasty, transgender women can benefit from undergoing voice assessment, conditioning, and therapy by a voice and communication professional. 89
There is debate about whether cross-sex hormone treatment, particularly oestrogen, should be interrupted before surgical procedures given the potential thromboembolic risk of oestrogen (and possibly of anti-androgens). Many centres advise transgender women to cease oestrogen use at least 2–4 weeks before any major surgery and do not re-initiate oestrogen treatment until the postoperative patient is fully ambulatory. 25 It is important that transgender women undergo postoperative prophylaxis for deep vein thrombosis. 25 Furthermore, transgender women should reduce the risk of postoperative deep vein thrombosis before surgery by modifying lifestyle factors as bodyweight, smoking, and drug misuse, which can affect the outcome of surgery and the risk of complications. 90 This recommendation is especially true for plastic surgery procedures in which microcirculation is involved.
Cross-sex hormone treatment in transgender women reduces sperm quantity and quality, and eventually results in irreversible infertility, even after cross-sex hormone treatment is stopped. 91 The time course, doses of oestrogen and testosterone-lowering drugs, and risk factors that lead to irreversible infertility are not known. Many transgender women desire the opportunity to have their own biological children in the future, and seek cryopreservation of their sperm. 92 Results of a case series of 29 transgender women showed a high rate of abnormalities in sperm characteristics, even before the initiation of oestrogen therapy, including oligo-azoospermia (27%, eight of 29), teratozoospermia (31%, nine of 29), and asthenozoospermia (31%, nine of 29). 93 Why sperm characteristics are altered in transgender women even before initiation of hormone therapy is not clear. Because cross-sex hormone treatment can reduce sperm number and quality, it is important to discuss fertility issues before the start of hormonal treatment. 1 , 94 Transgender women should be offered sperm banking before the initiation of cross-sex hormone treatment, since it is more difficult to retrieve sperm after cross-sex hormone treatment has been initiated. 1 There are no published longitudinal data for the effect of hormone therapy on sperm quality and the time course over which sperm quality is permanently altered. Physicians should also remind transgender women that cross-sex hormone treatment is not an effective contraceptive.
Concentrations of sex hormones vary with age. Whereas sex hormone concentrations increase during puberty in both sexes, there is a difference between men and women in the decline of circulating sex hormones. In men, there is a gradual decline of circulating testosterone, whereas in women there is a sudden decrease in circulating oestrogen after menopause. There is compelling evidence in cis-women that an earlier start of menopause is associated with an increased risk of osteoporosis and cardiovascular disease, whereas a later start is associated with an increased risk of uterine and breast cancer. 95 Results of the Women’s Health Initiative study 21 , 96 , 97 showed that hormone replacement therapy (oestrogen plus progestogen [medroxyprogesterone]) increased the incidence of breast cancer, coronary heart disease, and ischaemic stroke. The increased risk of breast cancer and coronary heart disease was not seen in women receiving oestrogen alone, without progestogens. 98
Data from transgender women at older ages (>50 years) are completely absent, and it is difficult to attempt to apply the existing evidence from natal women to transgender women because of physiological differences; for example, transgender women do not have a uterus, and breast cancer might have a different histopathology. So, although there are no compelling data about whether or not to stop oestrogen treatment in transgender women at age 50 years, the Women’s Health Initiative study provides evidence that full oestrogen replacement in late menopause might not be safe. In our opinion, it seems prudent to discuss with the patient the possibility of gradually tapering their oestrogen dose at an advanced age, as is done in some transgender health clinics (eg, in the Netherlands). 29 This topic is an important area of uncertainty that should be addressed in future research.
Conclusions
Transgender women seek treatments to better align their gender identity with their physical characteristics. Endocrine treatment remains a key component of care for transgender women. Although no randomised trials are available, hormonal and surgical treatment has been shown in several cohort studies to lead to a clear improvement in psychological wellbeing and quality of life. Health-care providers should understand that there is a wide spectrum of gender non-conforming conditions and that hormonal therapy is only one aspect of medical care. Health professionals should be aware of the WPATH standards of care and the Endocrine Society guidelines, both of which provide guidance on how to initiate and monitor hormone treatment. The recommendations are based on the currently available published evidence; however, most of the available evidence comes from low-quality studies. It might be difficult to conduct randomised controlled studies with sufficient power to answer specific questions related to transgender women. Results of large cohort studies have shown that, generally, when oestrogens are taken under medical supervision, the risks of adverse events are low. 42 The establishment of large, long-term cohort studies from different regions of the world, where different hormone regimens are used in clinical practice, will help advance our understanding and determine whether hormone therapy is associated with any long-term health risks. 99 For now, key treatment goals are to avoid supraphysiological dosing of oestrogen and to reduce modifiable risks associated with oestrogen therapy.
Search strategy and selection criteria
We searched PubMed using the keywords: “transgender”, “transsexual”, “trans*” AND “estrogen” OR “anti-androgen” OR “GnRH”, up to June 1, 2016. We also reviewed the guidelines published by the World Professional Association for Transgender Health, the Endocrine Society, and the Royal College of Psychiatrists, and consulted relevant references from these publications. We only included articles published in English. We largely focused on publications from the past 5 years, but we also cite some older studies, as well as a few key review articles that cover particular topics in detail.
Acknowledgments
We are partly supported by the National Center for Advancing Translational Sciences of the US National Institutes of Health (NIH; award number UL1TR000454). The content of this Review is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. We thank Walter Pierre Bouman from the Nottingham Centre for Gender Dysphoria (Nottingham, UK) for his critical review of this manuscript.
Contributors
Declaration of interests
We declare no competing interests.
Contributor Information
Vin Tangpricha, Division of Endocrinology, Metabolism and Lipids, Department of Medicine, Emory University School of Medicine and Atlanta VA Medical Center, Atlanta, GA, USA.
Prof Martin den Heijer, Department of Endocrinology and Center of Expertise on Gender Dysphoria, VU University Medical Center, Amsterdam, Netherlands.

IMAGES
VIDEO
COMMENTS
Published 6:00 AM PDT, June 15, 2022. A leading transgender health association has lowered its recommended minimum age for starting gender transition treatment, including sex hormones and surgeries. The World Professional Association for Transgender Health said hormones could be started at age 14, two years earlier than the group's previous ...
Puberty blockers can be used to delay the changes of puberty in transgender and gender-diverse youth who have started puberty. The medicines most often used for this purpose are called gonadotropin-releasing hormone (GnRH) analogues. Here's a summary of their possible benefits, side effects and long-term effects.
Transwomen (921 men to female) were more frequent than transmen (719 female to male). Transwomen's treatments were based in antiandrogens, estrogens, new drugs, and sex reassignment surgery, meanwhile transmen's surgeries were based in the administration of several forms of testosterone and sex reassignment.
ECU Health does not provide gender-related care to patients 2 to 4 years old or any toddler period," ECU said. University of North Carolina, May 12: To be clear: UNC Health does not offer any ...
Feminizing hormone therapy also is called gender-affirming hormone therapy. Feminizing hormone therapy involves taking medicine to block the action of the hormone testosterone. It also includes taking the hormone estrogen. Estrogen lowers the amount of testosterone the body makes. It also triggers the development of feminine secondary sex ...
Access to gender-affirming hormones and potential access to gender-affirming surgery is available at age 16—and then, in the case of transmasculine youth, only mastectomy, also known as top surgery.
Drug Interactions. There are no documented drug-drug interactions among estrogen, the various androgen blockers, and testosterone with anesthesia medications. ... Patient-reported complications and functional outcomes of male-to-female sex reassignment surgery. Arch Sex Behav. 2006; 35:717-727. [Google Scholar] 44. Chan W, Drummond A, Kelly ...
Feminizing hormone therapy, also known as transfeminine hormone therapy, is hormone therapy and sex reassignment therapy to change the secondary sex characteristics of transgender people from masculine or androgynous to feminine. It is a common type of transgender hormone therapy (another being masculinizing hormone therapy) and is used to treat transgender women and non-binary transfeminine ...
59% of registered voters believe it should be against the law to provide "gender-affirming care" to children, which involves puberty blockers or surgery to help transition a boy to a girl or a girl to a boy. 56% of registered voters believe conducting gender-transition surgery on children is a form of child abuse.
The standard premium for Medicare Part B in 2020 is $144.60 each month, and there is a $198 annual deductible cost. After a person pays the deductible, Medicare pays 80% of the allowable costs ...
Gender-affirming care is a model of care which includes a spectrum of "social, psychological, behavioral or medical (including hormonal treatment or surgery) interventions designed to support ...
Spironolactone is one of the most common medications used to suppress endogenous testosterone in trans female patients. ... study on sexual function and mood in female-to-male transsexuals during testosterone administration and after sex reassignment surgery. J Sex Marital Ther 2013; 39:321-35. 10.1080/0092623X.2012.736920 [Google Scholar] 19. ...
His confidence in this new approach is the result of nearly three decades of expertise and innovation in SRS and urogenital reconstructive surgery, which includes 600 male-to-female vaginoplasties, 900 female-to-male metoidioplasties, 300 female-to-male phalloplasties, and the co-development of a penile disassembly technique for epispadias repair.
The most common procedures were breast and chest procedures, which occurred in 27 187 patients (56.6%), followed by genital reconstruction (16 872 [35.1%]) and other facial and cosmetic procedures (6669 [13.9%]). The absolute number of GAS procedures rose from 4552 in 2016 to a peak of 13 011 in 2019 and then declined slightly to 12 818 in 2020.
Sex and sexual health tips for transgender women after gender-affirming surgery. Sex after surgery. Achieving orgasm. Libido. Vaginal depth and lubrication. Aftercare. Contraceptions and STIs ...
Gender-affirming hormone therapy is the primary medical treatment sought by transgender people. It allows their secondary sex characteristics to be more aligned with their individual gender identity. Gender-affirming hormone therapy comes in two types: Masculinizing hormone therapy used to develop typically male sex characteristics.
Unlike the other 18 states, Arizona, which prohibits gender-affirming surgeries for most minors, does not place restrictions on other gender-affirming care such as hormone treatments or puberty ...
The new law prohibits the use of State funds, "directly or indirectly," for the performance of or "in furtherance of" surgical gender transition procedures or the provision of puberty-blocking drugs or cross-sex hormones to a minor. The law does not define what it means to use State funds "in furtherance of" gender transition health ...
With the onset of puberty, transgender persons typically experience significant psychological distress (gender dysphoria) and consequently seek gender-affirming—or gender reassignment—treatment ( e4 ). With 9% to 11% and 1.5% to 2%, the rates of suicide attempts ( 3) and committed suicides ( 4 ), respectively, are increased among people ...
Neutering children is all the rage in Western democracies, or it was. A few weeks ago, the UK banned the public health service from allowing gender transition drugs (and therefore surgeries) on minors, following a four-year study that showed the practice had no mental health benefit or made matters worse. This announcement came on the … "Change Surgery for Minors Could be 'Greatest ...
French Senators want to ban gender transition treatments for under-18s, after a report described sex reassignment in minors as potentially "one of the greatest ethical scandals in the history of ...
Wyoming governor signs bill banning gender reassignment surgery, care. Story by Simon Druker. • 13m • 2 min read. Wyoming's Republican governor has signed a bill into law banning doctors in ...
A flyer promoted by several bands says that the Graveyard Gallery in Murfreesboro is hosting the concert on March 31, and using it to raise money for a group that provides gender reassignment surgery. The shooting occurred on March 27, 2023, at the Christian school in Nashville, less than an hour away.
Gender dysphoria, earlier known as gender identity disorder, describes a heterogeneous group of individuals having the desire to possess secondary sexual characteristics of the opposite sex and possessing varying degrees of dissatisfaction regarding their anatomical gender . Gender reassignment surgery (GRS) has proven to be a revolutionary ...
Wyoming's Gov. Mark Gordon passed legislation Friday outlawing gender-reassignment procedures on minors in the state and vetoed a separate bill that would have placed additional restrictions on ...
Wyoming just became the 24th state banning physicians from performing gender transitioning and gender reassignment procedures for children. The law, recently signed by Republican Governor Mark ...
Introduction. Transgender and gender-non-conforming people often seek hormone therapy, with or without surgery, to change their physical appearance to match their reaffirmed gender, and to alleviate the stress and discomfort associated with living in the incongruent gender. 1 The uneasy feeling of living in an incongruent gender role is termed gender dysphoria.
63 likes, 16 comments - officiallytraceymartin on March 18, 2024: "Comparing a tattoo to gender reassignment surgery and puberty blocking drugs. Insane!"