

Nursing Concept Map (FREE Template)

Nursing concept maps are dynamic tools with significant value for nurses and especially nursing students starting their educational journey.
In this article, we will learn about concept mapping in nursing and how to apply it to nursing.
Also, we will give a FREE PDF Concept Map Template.
You may also want to check out 15 Attitudes of Critical Thinking in Nursing (Explained W/ Examples)
What is Concept Map?
A concept map also known as a mind map is a visual tool that represents relationships and connections between different concepts or ideas.
It is a graphical representation of information that helps to organize and understand complex topics or subjects.
Concept maps are often used to illustrate how different concepts relate to one another, showing hierarchies, connections, and dependencies.
In a concept map, concepts are represented as nodes or boxes, and the relationships between concepts are depicted using lines or arrows.
The lines connecting the nodes indicate the nature of the relationship, such as “is a part of,” “causes,” “leads to,” “is related to,” and more.
These maps can vary in complexity, from simple diagrams with a few nodes to intricate structures with numerous interconnected concepts.
Concept maps are widely used in education, brainstorming, research, and problem-solving.
They provide a visual representation that helps individuals grasp the bigger picture, understand the connections between ideas, and identify key concepts within a complex system.
Definition of Concept Map
A concept map can be defined as a visual representation that depicts the relationships and connections between various concepts or ideas in a structured and organized manner.
What is a Nursing Concept Map?
In the context of nursing, a concept map is a visual representation that illustrates the relationships between various nursing concepts and their connections within a particular patient’s care or a broader nursing context.
Concept mapping in nursing is a valuable tool for critical thinking , clinical reasoning , and effective communication among healthcare professionals.
Nursing concept maps are used to:
- Organize Information: Nursing concepts such as patient assessment, nursing diagnoses, interventions, and patient outcomes can be organized and displayed visually to help nurses and other healthcare providers better understand the care plan.
- Facilitate Care Planning: Concept maps allow nurses to create a structured plan of care for their patients. This includes identifying nursing diagnoses, selecting appropriate interventions, and predicting potential outcomes.
- Enhance Critical Thinking: Creating a concept map encourages nurses to think critically about the relationships between different aspects of patient care. It helps them identify potential issues, connections, and factors that might impact patient well-being.
- Promote Collaboration: Concept maps can be shared among healthcare professionals, fostering better communication and collaboration among nurses, doctors, therapists, and other team members involved in patient care.
- Improve Patient Education: Concept maps can be simplified and shared with patients to help them understand their medical conditions, treatment plans, and the role of nursing interventions in their care.
- Assist in Decision-Making: Nurses can use concept maps to evaluate different approaches to patient care, considering the potential outcomes of each intervention and selecting the best course of action.
- Document Patient Progress: Over time, nurses can update concept maps to reflect changes in the patient’s condition, modifications to the care plan, and progress toward desired outcomes.
A nursing concept map typically includes components such as nursing diagnoses, patient assessment data, interventions, expected outcomes, and evaluation criteria.
It visually presents the connections between these components, allowing nurses to make informed decisions and provide effective care.
It’s important to note that creating effective concept maps in nursing requires a solid understanding of nursing concepts, patient care processes, and critical thinking skills.
Concept mapping is a dynamic process that evolves as the patient’s condition changes and as the care plan is adjusted based on ongoing assessment and evaluation.
Why Use a Concept Map in Nursing?
Concept mapping is useful in nursing because it can visually represent nonlinear and linear relationships, which aids in the development of critical thinking , analytical skills, and clinical reasoning .
By linking attributes of concepts, concept maps help nurses make meaning of complex ideas, enabling them to visualize information in their own way.
Concept maps offer a way to focus on key concepts and relationships, making them quicker than note-taking and a beneficial tool for care planning, organizing nursing care, and understanding complex concepts.
They bridge existing nursing knowledge with new information and enhance critical thinking . Concept mapping also helps connect theoretical knowledge to clinical practice.
This approach enables nurses to plan care for patients and families effectively while addressing multiple complex problems, ultimately improving clinical reasoning .
What are the Types of Concept Maps?
Concept maps come in various types, each tailored to specific purposes and contexts. Some common types of concept maps include:
Hierarchical Concept Maps:
These show a main concept at the top, with related sub-concepts branching out beneath it, emphasizing relationships and hierarchy.
Spider Concept Maps:
Radiating from a central concept, these maps explore related ideas, making them useful for brainstorming and idea generation.
Flowchart Concept Maps:
Illustrating processes and workflows, they depict sequential steps and decisions in a clear, linear manner.
Systematic Concept Maps:
These demonstrate the components and interactions of a complex system, useful for understanding system dynamics.
Comparative Concept Maps:
Used for analysis, they highlight similarities and differences between concepts, objects, or ideas.
Storyline Concept Maps:
Showing relationships in a narrative format, they’re used for plotting stories, historical events, or case studies.
Venn Diagram Concept Maps:
They display overlapping relationships among sets of concepts, helping to identify commonalities and distinctions.
Although not concept maps per se, mind maps start with a central idea and branch out with associated thoughts, fostering creativity and idea exploration.
Network Concept Maps:
Emphasizing connections without hierarchy, they reveal complex relationships and dependencies.
Tree Concept Maps:
Organizing concepts in a hierarchical tree structure, they’re suitable for classification and categorization.
Cross-Linking Concept Maps:
Linking concepts based on shared attributes, they offer a multidimensional view of relationships.
These diverse types of concept maps cater to different learning styles, communication needs, and information structures, allowing users to select the most suitable format for their specific purposes.
How Do You Create a Nursing Care Plan Concept Map?
Creating a nursing care plan concept map involves visually representing the relationships between various nursing concepts, patient assessment data, nursing diagnoses, interventions, and expected outcomes.
Here’s a step-by-step guide to creating a nursing care plan concept map:
Step 1: choose a patient scenario:.
Select a specific patient scenario or case for which you want to create a nursing care plan concept map.
This could be a patient with a specific medical condition or a set of nursing diagnoses.
Step 2: Gather Patient Data:
Collect relevant patient data, including medical history, physical assessment findings, lab results, and any other information that informs the nursing care plan.
Step 3: Identify Nursing Diagnoses:
Based on the patient data, identify relevant nursing diagnoses. These are clinical judgments about actual or potential health problems that nurses are licensed to treat.
Each nursing diagnosis represents a specific problem or need that requires nursing interventions.
Step 4: Organize Diagnoses Hierarchically:
Place the identified nursing diagnoses at the center of your concept map. Branch out from each diagnosis with lines to represent related concepts such as assessment data, interventions, and expected outcomes.
Step 5: Add Assessment Data:
Connect assessment data relevant to each nursing diagnosis. This could include physical assessment findings, patient history, and any other data that contributes to the identification of the diagnosis.
Step 6: Include Interventions:
Add nursing interventions associated with each nursing diagnosis.
These interventions should be evidence-based and targeted toward addressing the specific patient needs and diagnoses.
Step 7: Predict Expected Outcomes:
Predict the desired outcomes that result from implementing the nursing interventions.
These outcomes should reflect the improvement, stabilization, or prevention of the patient’s health problem.
Step 8: Define Relationships:
Draw lines or arrows to show the relationships between nursing diagnoses, assessment data, interventions, and outcomes.
Use labels to describe the nature of these relationships, such as “supports,” “leads to,” or “addresses.”
Step 9: Evaluate and Refine:
Review your nursing care plan concept map to ensure that the relationships make sense, interventions are appropriate, and outcomes are achievable. Make revisions as needed.
Step 10: Share and Implement:
Share the nursing care plan concept map with other healthcare professionals involved in the patient’s care.
Use it as a guide to communicate the planned interventions and outcomes, and update it as the patient’s condition changes.
Creating a nursing care plan concept map helps you visualize the comprehensive care plan for your patient, ensuring that you consider all relevant aspects of their condition and tailor your interventions accordingly.
Nursing Concept Map Examples
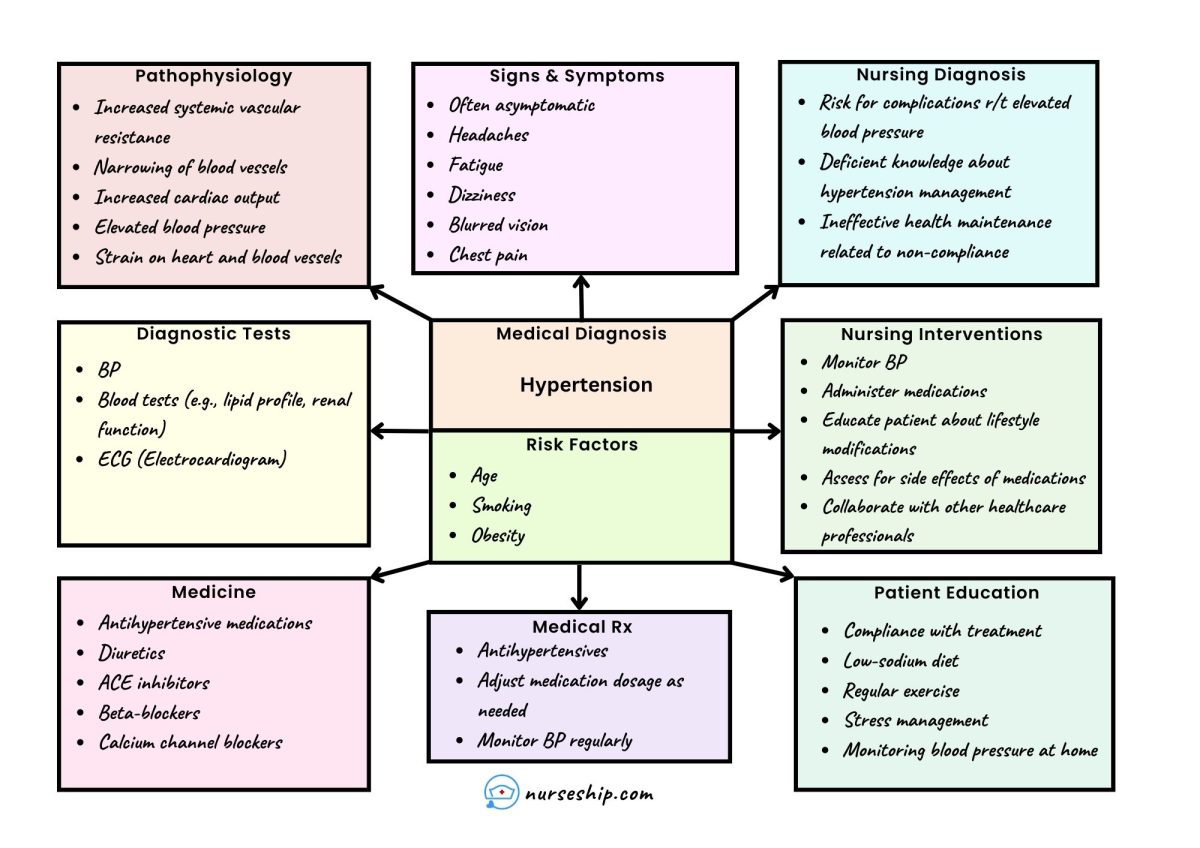
Sample of nursing care plan concept map.
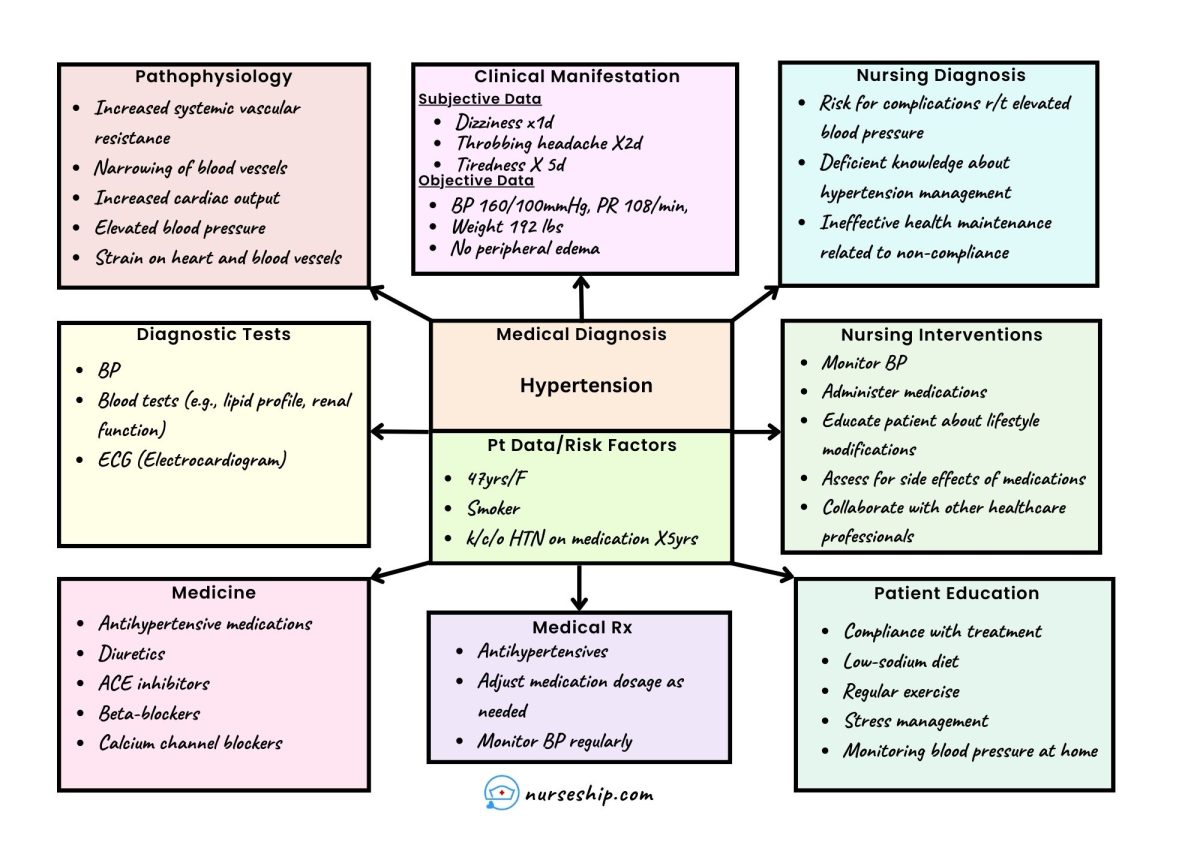
Sample Hypertension Nursing Concept Map
Download FREE Nursing Concept Map Template
- How To Improve Critical Thinking Skills In Nursing? 24 Strategies With Examples
- Clinical Reasoning In Nursing (Explained W/ Example)
- 8 Stages Of The Clinical Reasoning Cycle
- What Are Socratic Questions?
- What is the “5 Whys” Technique?
In conclusion, nursing concept maps offer nursing students an invaluable means to comprehend intricate healthcare concepts, promoting the development of critical thinking and clinical reasoning skills.
By visually representing relationships and care plans, these maps aid students in translating theoretical knowledge into practical patient care scenarios, fostering a holistic approach to nursing education.
Comments are closed.
Medical & Legal Disclaimer
All the contents on this site are for entertainment, informational, educational, and example purposes ONLY. These contents are not intended to be used as a substitute for professional medical advice or practice guidelines. However, we aim to publish precise and current information. By using any content on this website, you agree never to hold us legally liable for damages, harm, loss, or misinformation. Read the privacy policy and terms and conditions.
Privacy Policy
Terms & Conditions
© 2024 nurseship.com. All rights reserved.

This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Critical thinking: what it is and why it counts. 2020. https://tinyurl.com/ybz73bnx (accessed 27 April 2021)
Faculty of Intensive Care Medicine. Curriculum for training for advanced critical care practitioners: syllabus (part III). version 1.1. 2018. https://www.ficm.ac.uk/accps/curriculum (accessed 27 April 2021)
Guerrero AP. Mechanistic case diagramming: a tool for problem-based learning. Acad Med.. 2001; 76:(4)385-9 https://doi.org/10.1097/00001888-200104000-00020
Harasym PH, Tsai TC, Hemmati P. Current trends in developing medical students' critical thinking abilities. Kaohsiung J Med Sci.. 2008; 24:(7)341-55 https://doi.org/10.1016/S1607-551X(08)70131-1
Hayes MM, Chatterjee S, Schwartzstein RM. Critical thinking in critical care: five strategies to improve teaching and learning in the intensive care unit. Ann Am Thorac Soc.. 2017; 14:(4)569-575 https://doi.org/10.1513/AnnalsATS.201612-1009AS
Health Education England. Multi-professional framework for advanced clinical practice in England. 2017. https://www.hee.nhs.uk/sites/default/files/documents/multi-professionalframeworkforadvancedclinicalpracticeinengland.pdf (accessed 27 April 2021)
Health Education England, NHS England/NHS Improvement, Skills for Health. Core capabilities framework for advanced clinical practice (nurses) working in general practice/primary care in England. 2020. https://www.skillsforhealth.org.uk/images/services/cstf/ACP%20Primary%20Care%20Nurse%20Fwk%202020.pdf (accessed 27 April 2021)
Health Education England. Advanced practice mental health curriculum and capabilities framework. 2020. https://www.hee.nhs.uk/sites/default/files/documents/AP-MH%20Curriculum%20and%20Capabilities%20Framework%201.2.pdf (accessed 27 April 2021)
Jacob E, Duffield C, Jacob D. A protocol for the development of a critical thinking assessment tool for nurses using a Delphi technique. J Adv Nurs.. 2017; 73:(8)1982-1988 https://doi.org/10.1111/jan.13306
Kohn MA. Understanding evidence-based diagnosis. Diagnosis (Berl).. 2014; 1:(1)39-42 https://doi.org/10.1515/dx-2013-0003
Clinical reasoning—a guide to improving teaching and practice. 2012. https://www.racgp.org.au/afp/201201/45593
McGee S. Evidence-based physical diagnosis, 4th edn. Philadelphia PA: Elsevier; 2018
Norman GR, Monteiro SD, Sherbino J, Ilgen JS, Schmidt HG, Mamede S. The causes of errors in clinical reasoning: cognitive biases, knowledge deficits, and dual process thinking. Acad Med.. 2017; 92:(1)23-30 https://doi.org/10.1097/ACM.0000000000001421
Papp KK, Huang GC, Lauzon Clabo LM Milestones of critical thinking: a developmental model for medicine and nursing. Acad Med.. 2014; 89:(5)715-20 https://doi.org/10.1097/acm.0000000000000220
Rencic J, Lambert WT, Schuwirth L., Durning SJ. Clinical reasoning performance assessment: using situated cognition theory as a conceptual framework. Diagnosis.. 2020; 7:(3)177-179 https://doi.org/10.1515/dx-2019-0051
Examining critical thinking skills in family medicine residents. 2016. https://www.stfm.org/FamilyMedicine/Vol48Issue2/Ross121
Royal College of Emergency Medicine. Emergency care advanced clinical practitioner—curriculum and assessment, adult and paediatric. version 2.0. 2019. https://tinyurl.com/eps3p37r (accessed 27 April 2021)
Young ME, Thomas A, Lubarsky S. Mapping clinical reasoning literature across the health professions: a scoping review. BMC Med Educ.. 2020; 20 https://doi.org/10.1186/s12909-020-02012-9
Advanced practice: critical thinking and clinical reasoning
Sadie Diamond-Fox
Senior Lecturer in Advanced Critical Care Practice, Northumbria University, Advanced Critical Care Practitioner, Newcastle upon Tyne Hospitals NHS Foundation Trust, and Co-Lead, Advanced Critical/Clinical Care Practitioners Academic Network (ACCPAN)
View articles
Advanced Critical Care Practitioner, South Tees Hospitals NHS Foundation Trust

Clinical reasoning is a multi-faceted and complex construct, the understanding of which has emerged from multiple fields outside of healthcare literature, primarily the psychological and behavioural sciences. The application of clinical reasoning is central to the advanced non-medical practitioner (ANMP) role, as complex patient caseloads with undifferentiated and undiagnosed diseases are now a regular feature in healthcare practice. This article explores some of the key concepts and terminology that have evolved over the last four decades and have led to our modern day understanding of this topic. It also considers how clinical reasoning is vital for improving evidence-based diagnosis and subsequent effective care planning. A comprehensive guide to applying diagnostic reasoning on a body systems basis will be explored later in this series.
The Multi-professional Framework for Advanced Clinical Practice highlights clinical reasoning as one of the core clinical capabilities for advanced clinical practice in England ( Health Education England (HEE), 2017 ). This is also identified in other specialist core capability frameworks and training syllabuses for advanced clinical practitioner (ACP) roles ( Faculty of Intensive Care Medicine, 2018 ; Royal College of Emergency Medicine, 2019 ; HEE, 2020 ; HEE et al, 2020 ).
Rencic et al (2020) defined clinical reasoning as ‘a complex ability, requiring both declarative and procedural knowledge, such as physical examination and communication skills’. A plethora of literature exists surrounding this topic, with a recent systematic review identifying 625 papers, spanning 47 years, across the health professions ( Young et al, 2020 ). A diverse range of terms are used to refer to clinical reasoning within the healthcare literature ( Table 1 ), which can make defining their influence on their use within the clinical practice and educational arenas somewhat challenging.
The concept of clinical reasoning has changed dramatically over the past four decades. What was once thought to be a process-dependent task is now considered to present a more dynamic state of practice, which is affected by ‘complex, non-linear interactions between the clinician, patient, and the environment’ ( Rencic et al, 2020 ).
Cognitive and meta-cognitive processes
As detailed in the table, multiple themes surrounding the cognitive and meta-cognitive processes that underpin clinical reasoning have been identified. Central to these processes is the practice of critical thinking. Much like the definition of clinical reasoning, there is also diversity with regard to definitions and conceptualisation of critical thinking in the healthcare setting. Facione (2020) described critical thinking as ‘purposeful reflective judgement’ that consists of six discrete cognitive skills: analysis, inference, interpretation, explanation, synthesis and self–regulation. Ross et al (2016) identified that critical thinking positively correlates with academic success, professionalism, clinical decision-making, wider reasoning and problem-solving capabilities. Jacob et al (2017) also identified that patient outcomes and safety are directly linked to critical thinking skills.
Harasym et al (2008) listed nine discrete cognitive steps that may be applied to the process of critical thinking, which integrates both cognitive and meta-cognitive processes:
- Gather relevant information
- Formulate clearly defined questions and problems
- Evaluate relevant information
- Utilise and interpret abstract ideas effectively
- Infer well-reasoned conclusions and solutions
- Pilot outcomes against relevant criteria and standards
- Use alternative thought processes if needed
- Consider all assumptions, implications, and practical consequences
- Communicate effectively with others to solve complex problems.
There are a number of widely used strategies to develop critical thinking and evidence-based diagnosis. These include simulated problem-based learning platforms, high-fidelity simulation scenarios, case-based discussion forums, reflective journals as part of continuing professional development (CPD) portfolios and journal clubs.
Dual process theory and cognitive bias in diagnostic reasoning
A lack of understanding of the interrelationship between critical thinking and clinical reasoning can result in cognitive bias, which can in turn lead to diagnostic errors ( Hayes et al, 2017 ). Embedded within our understanding of how diagnostic errors occur is dual process theory—system 1 and system 2 thinking. The characteristics of these are described in Table 2 . Although much of the literature in this area regards dual process theory as a valid representation of clinical reasoning, the exact causes of diagnostic errors remain unclear and require further research ( Norman et al, 2017 ). The most effective way in which to teach critical thinking skills in healthcare education also remains unclear; however, Hayes et al (2017) proposed five strategies, based on well-known educational theory and principles, that they have found to be effective for teaching and learning critical thinking within the ‘high-octane’ and ‘high-stakes’ environment of the intensive care unit ( Table 3 ). This is arguably a setting that does not always present an ideal environment for learning given its fast pace and constant sensory stimulation. However, it may be argued that if a model has proven to be effective in this setting, it could be extrapolated to other busy clinical environments and may even provide a useful aide memoire for self-assessment and reflective practices.
Integrating the clinical reasoning process into the clinical consultation
Linn et al (2012) described the clinical consultation as ‘the practical embodiment of the clinical reasoning process by which data are gathered, considered, challenged and integrated to form a diagnosis that can lead to appropriate management’. The application of the previously mentioned psychological and behavioural science theories is intertwined throughout the clinical consultation via the following discrete processes:
- The clinical history generates an initial hypothesis regarding diagnosis, and said hypothesis is then tested through skilled and specific questioning
- The clinician formulates a primary diagnosis and differential diagnoses in order of likelihood
- Physical examination is carried out, aimed at gathering further data necessary to confirm or refute the hypotheses
- A selection of appropriate investigations, using an evidence-based approach, may be ordered to gather additional data
- The clinician (in partnership with the patient) then implements a targeted and rationalised management plan, based on best-available clinical evidence.
Linn et al (2012) also provided a very useful framework of how the above methods can be applied when teaching consultation with a focus on clinical reasoning (see Table 4 ). This framework may also prove useful to those new to the process of undertaking the clinical consultation process.
Evidence-based diagnosis and diagnostic accuracy
The principles of clinical reasoning are embedded within the practices of formulating an evidence-based diagnosis (EBD). According to Kohn (2014) EBD quantifies the probability of the presence of a disease through the use of diagnostic tests. He described three pertinent questions to consider in this respect:
- ‘How likely is the patient to have a particular disease?’
- ‘How good is this test for the disease in question?’
- ‘Is the test worth performing to guide treatment?’
EBD gives a statistical discriminatory weighting to update the probability of a disease to either support or refute the working and differential diagnoses, which can then determine the appropriate course of further diagnostic testing and treatments.
Diagnostic accuracy refers to how positive or negative findings change the probability of the presence of disease. In order to understand diagnostic accuracy, we must begin to understand the underlying principles and related statistical calculations concerning sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and likelihood ratios.
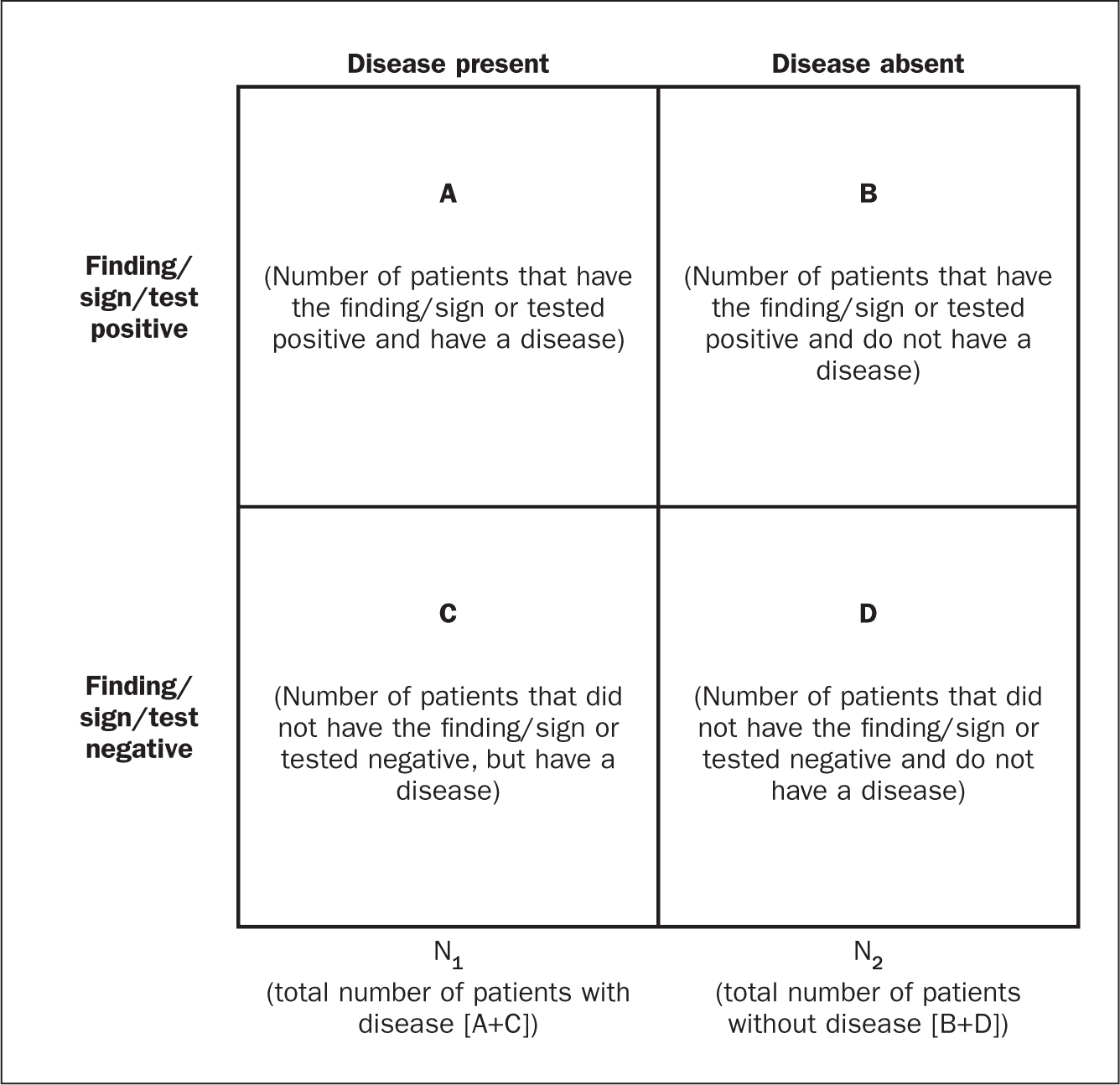
The construction of a two-by-two square (2 x 2) table ( Figure 1 ) allows the calculation of several statistical weightings for pertinent points of the history-taking exercise, a finding/sign on physical examination, or a test result. From this construct we can then determine the aforementioned statistical calculations as follows ( McGee, 2018 ):
- Sensitivity , the proportion of patients with the diagnosis who have the physical sign or a positive test result = A ÷ (A + C)
- Specificity , the proportion of patients without the diagnosis who lack the physical sign or have a negative test result = D ÷ (B + D)
- Positive predictive value , the proportion of patients with disease who have a physical sign divided by the proportion of patients without disease who also have the same sign = A ÷ (A + B)
- Negative predictive value , proportion of patients with disease lacking a physical sign divided by the proportion of patients without disease also lacking the sign = D ÷ (C + D)
- Likelihood ratio , a finding/sign/test results sensitivity divided by the false-positive rate. A test of no value has an LR of 1. Therefore the test would have no impact upon the patient's odds of disease
- Positive likelihood ratio = proportion of patients with disease who have a positive finding/sign/test, divided by proportion of patients without disease who have a positive finding/sign/test OR (A ÷ N1) ÷ (B÷ N2), or sensitivity ÷ (1 – specificity) The more positive an LR (the further above 1), the more the finding/sign/test result raises a patient's probability of disease. Thresholds of ≥ 4 are often considered to be significant when focusing a clinician's interest on the most pertinent positive findings, clinical signs or tests
- Negative likelihood ratio = proportion of patients with disease who have a negative finding/sign/test result, divided by the proportion of patients without disease who have a positive finding/sign/test OR (C ÷ N1) ÷ (D÷N1) or (1 – sensitivity) ÷ specificity The more negative an LR (the closer to 0), the more the finding/sign/test result lowers a patient's probability of disease. Thresholds <0.4 are often considered to be significant when focusing clinician's interest on the most pertinent negative findings, clinical signs or tests.
There are various online statistical calculators that can aid in the above calculations, such as the BMJ Best Practice statistical calculators, which may used as a guide (https://bestpractice.bmj.com/info/toolkit/ebm-toolbox/statistics-calculators/).
Clinical scoring systems
Evidence-based literature supports the practice of determining clinical pretest probability of certain diseases prior to proceeding with a diagnostic test. There are numerous validated pretest clinical scoring systems and clinical prediction tools that can be used in this context and accessed via various online platforms such as MDCalc (https://www.mdcalc.com/#all). Such clinical prediction tools include:
- 4Ts score for heparin-induced thrombocytopenia
- ABCD² score for transient ischaemic attack (TIA)
- CHADS₂ score for atrial fibrillation stroke risk
- Aortic Dissection Detection Risk Score (ADD-RS).
Conclusions
Critical thinking and clinical reasoning are fundamental skills of the advanced non-medical practitioner (ANMP) role. They are complex processes and require an array of underpinning knowledge of not only the clinical sciences, but also psychological and behavioural science theories. There are multiple constructs to guide these processes, not all of which will be suitable for the vast array of specialist areas in which ANMPs practice. There are multiple opportunities throughout the clinical consultation process in which ANMPs can employ the principles of critical thinking and clinical reasoning in order to improve patient outcomes. There are also multiple online toolkits that may be used to guide the ANMP in this complex process.
- Much like consultation and clinical assessment, the process of the application of clinical reasoning was once seen as solely the duty of a doctor, however the advanced non-medical practitioner (ANMP) role crosses those traditional boundaries
- Critical thinking and clinical reasoning are fundamental skills of the ANMP role
- The processes underlying clinical reasoning are complex and require an array of underpinning knowledge of not only the clinical sciences, but also psychological and behavioural science theories
- Through the use of the principles underlying critical thinking and clinical reasoning, there is potential to make a significant contribution to diagnostic accuracy, treatment options and overall patient outcomes
CPD reflective questions
- What assessment instruments exist for the measurement of cognitive bias?
- Think of an example of when cognitive bias may have impacted on your own clinical reasoning and decision making
- What resources exist to aid you in developing into the ‘advanced critical thinker’?
- What resources exist to aid you in understanding the statistical terminology surrounding evidence-based diagnosis?
Teaching Clinical Reasoning and Critical Thinking: From Cognitive Theory to Practical Application
Affiliations.
- 1 Center for Education, Shapiro Institute for Education and Research, Department of Medicine, Beth Israel Deaconess Medical Center and Harvard Medical School, Boston, MA.
- 2 Center for Education, Shapiro Institute for Education and Research, Department of Medicine, Beth Israel Deaconess Medical Center and Harvard Medical School, Boston, MA. Electronic address: [email protected].
- PMID: 32450242
- DOI: 10.1016/j.chest.2020.05.525
Teaching clinical reasoning is challenging, particularly in the time-pressured and complicated environment of the ICU. Clinical reasoning is a complex process in which one identifies and prioritizes pertinent clinical data to develop a hypothesis and a plan to confirm or refute that hypothesis. Clinical reasoning is related to and dependent on critical thinking skills, which are defined as one's capacity to engage in higher cognitive skills such as analysis, synthesis, and self-reflection. This article reviews how an understanding of the cognitive psychological principles that contribute to effective clinical reasoning has led to strategies for teaching clinical reasoning in the ICU. With familiarity with System 1 and System 2 thinking, which represent intuitive vs analytical cognitive processing pathways, respectively, the clinical teacher can use this framework to identify cognitive patterns in clinical reasoning. In addition, the article describes how internal and external factors in the clinical environment can affect students' and trainees' clinical reasoning abilities, as well as their capacity to understand and incorporate strategies for effective critical thinking into their practice. Utilizing applicable cognitive psychological theory, the relevant literature on teaching clinical reasoning is reviewed, and specific strategies to effectively teach clinical reasoning and critical thinking in the ICU and other clinical settings are provided. Definitions, operational descriptions, and justifications for a variety of teaching interventions are discussed, including the "one-minute preceptor" model, the use of concept or mechanism maps, and cognitive de-biasing strategies.
Keywords: clinical reasoning; cognitive bias; critical thinking; education.
Copyright © 2020 American College of Chest Physicians. Published by Elsevier Inc. All rights reserved.
Publication types
- Clinical Reasoning*
- Education, Medical
- Psychological Theory*

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

1.3: Critical Thinking and Clinical Reasoning
- Last updated
- Save as PDF
- Page ID 63335

- Ernstmeyer & Christman (Eds.)
- Chippewa Valley Technical College via OpenRN
Before learning how to use the nursing process, it is important to understand some basic concepts related to critical thinking and nursing practice. Let’s take a deeper look at how nurses think.

Critical Thinking and Clinical Reasoning
Nurses make decisions while providing patient care by using critical thinking and clinical reasoning. Critical thinking is a broad term used in nursing that includes “reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow.” [1] Using critical thinking means that nurses take extra steps to maintain patient safety and don’t just “follow orders.” It also means the accuracy of patient information is validated and plans for caring for patients are based on their needs, current clinical practice, and research.
“Critical thinkers” possess certain attitudes that foster rational thinking. These attitudes are as follows:
- Independence of thought: Thinking on your own
- Fair-mindedness: Treating every viewpoint in an unbiased, unprejudiced way
- Insight into egocentricity and sociocentricity: Thinking of the greater good and not just thinking of yourself. Knowing when you are thinking of yourself (egocentricity) and when you are thinking or acting for the greater good (sociocentricity)
- Intellectual humility: Recognizing your intellectual limitations and abilities
- Nonjudgmental: Using professional ethical standards and not basing your judgments on your own personal or moral standards
- Integrity: Being honest and demonstrating strong moral principles
- Perseverance: Persisting in doing something despite it being difficult
- Confidence: Believing in yourself to complete a task or activity
- Interest in exploring thoughts and feelings: Wanting to explore different ways of knowing
- Curiosity: Asking “why” and wanting to know more
Clinical reasoning is defined as, “A complex cognitive process that uses formal and informal thinking strategies to gather and analyze patient information, evaluate the significance of this information, and weigh alternative actions.” To make sound judgments about patient care, nurses must generate alternatives, weigh them against the evidence, and choose the best course of action. The ability to clinically reason develops over time and is based on knowledge and experience. [3]
The ANA’s Standards of Professional Nursing Practice associated with each component of the nursing process are described below.
Assessment is the first step of the nursing process. The American Nurses Association (ANA) “Assessment” Standard of Practice is defined as, “The registered nurse collects pertinent data and information relative to the health care consumer’s health or the situation.” This includes collecting “pertinent data related to the health and quality of life in a systematic, ongoing manner, with compassion and respect for the wholeness, inherent dignity, worth, and unique attributes of every person, including but not limited to, demographics, environmental and occupational exposures, social determinants of health, health disparities, physical, functional, psychosocial, emotional, cognitive, spiritual/transpersonal, sexual, sociocultural, age-related, environmental, and lifestyle/economic assessments.” [1]
A registered nurse uses a systematic method to collect and analyze patient data. Assessment includes physiological data, as well as psychological, sociocultural, spiritual, economic, and lifestyle data. For example, a nurse’s assessment of a hospitalized patient in pain includes the patient’s response to pain, such as the inability to get out of bed, refusal to eat, withdrawal from family members, or anger directed at hospital staff. Nurses assess patients to gather clues, make generalizations, and diagnose human responses to health conditions and life processes. Patient data is considered either subjective or objective, and it can be collected from multiple sources.
The “Diagnosis” Standard of Practice is defined as, “The registered nurse analyzes the assessment data to determine actual or potential diagnoses, problems, and issues.” [13] A nursing diagnosis is the nurse’s clinical judgment about the client's response to actual or potential health conditions or needs. Nursing diagnoses are the bases for the nurse’s care plan and are different than medical diagnoses.
Outcomes Identification
The “Outcomes Identification” Standard of Practice is defined as, “The registered nurse identifies expected outcomes for a plan individualized to the health care consumer or the situation.” The nurse sets measurable and achievable short- and long-term goals and specific outcomes in collaboration with the patient based on their assessment data and nursing diagnoses.
The “Planning” Standard of Practice is defined as, “The registered nurse develops a collaborative plan encompassing strategies to achieve expected outcomes.” [16] Assessment data, diagnoses, and goals are used to select evidence-based nursing interventions customized to each patient’s needs and concerns. Goals, expected outcomes, and nursing interventions are documented in the patient’s nursing care plan so that nurses, as well as other health professionals, have access to it for continuity of care. [17]
Nursing Care Plans
Creating nursing care plans is a part of the “Planning” step of the nursing process. A nursing care plan is a type of documentation that demonstrates the individualized planning and delivery of nursing care for each specific patient using the nursing process. Registered nurses (RNs) create nursing care plans so that the care provided to the patient across shifts is consistent among health care personnel.
Implementation
The “Implementation” Standard of Practice is defined as, “The nurse implements the identified plan.” Nursing interventions are implemented or delegated with supervision according to the care plan to assure continuity of care across multiple nurses and health professionals caring for the patient. Interventions are also documented in the patient’s electronic medical record as they are completed.
The “Evaluation” Standard of Practice is defined as, “The registered nurse evaluates progress toward attainment of goals and outcomes.” During evaluation, nurses assess the patient and compare the findings against the initial assessment to determine the effectiveness of the interventions and overall nursing care plan. Both the patient’s status and the effectiveness of the nursing care must be continuously evaluated and modified as needed.
Benefits of Using the Nursing Process
Using the nursing process has many benefits for nurses, patients, and other members of the health care team. The benefits of using the nursing process include the following:
- Promotes quality patient care
- Decreases omissions and duplications
- Provides a guide for all staff involved to provide consistent and responsive care
- Encourages collaborative management of a patient’s health care problems
- Improves patient safety
- Improves patient satisfaction
- Identifies a patient’s goals and strategies to attain them
- Increases the likelihood of achieving positive patient outcomes
- Saves time, energy, and frustration by creating a care plan or path to follow
By using these components of the nursing process as a critical thinking model, nurses plan interventions customized to the patient’s needs, plan outcomes and interventions, and determine whether those actions are effective in meeting the patient’s needs. In the remaining sections of this chapter, we will take an in-depth look at each of these components of the nursing process. Using the nursing process and implementing evidence-based practices are referred to as the “science of nursing.” Let’s review concepts related to the “art of nursing” while providing holistic care in a caring manner using the nursing process.
Holistic Nursing Care
The American Nurses Association (ANA) recently updated the definition of nursing as, “Nursing integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence. Nursing is the diagnosis and treatment of human responses and advocacy in the care of individuals, families, groups, communities, and populations in the recognition of the connection of all humanity.”
The ANA further describes nursing is a learned profession built on a core body of knowledge that integrates both the art and science of nursing. The art of nursing is defined as, “Unconditionally accepting the humanity of others, respecting their need for dignity and worth, while providing compassionate, comforting care.”
Nurses care for individuals holistically, including their emotional, spiritual, psychosocial, cultural, and physical needs. They consider problems, issues, and needs that the person experiences as a part of a family and a community as they use the nursing process.
Caring and the Nursing Process
The American Nurses Association (ANA) states, “The act of caring is foundational to the practice of nursing.” Successful use of the nursing process requires the development of a care relationship with the patient. A care relationship is a mutual relationship that requires the development of trust between both parties. This trust is often referred to as the development of rapport and underlies the art of nursing. While establishing a caring relationship, the whole person is assessed, including the individual’s beliefs, values, and attitudes, while also acknowledging the vulnerability and dignity of the patient and family. Assessing and caring for the whole person takes into account the physical, mental, emotional, and spiritual aspects of being a human being. Caring interventions can be demonstrated in simple gestures such as active listening, making eye contact, touching, and verbal reassurances while also respecting and being sensitive to the care recipient’s cultural beliefs and meanings associated with caring behaviors.
- Klenke-Borgmann, L., Cantrell, M. A., & Mariani, B. (2020). Nurse educator’s guide to clinical judgment: A review of conceptualization, measurement, and development. Nursing Education Perspectives, 41 (4), 215-221. ↵
- Powers, L., Pagel, J., & Herron, E. (2020). Nurse preceptors and new graduate success. American Nurse Journal, 15 (7), 37-39. ↵
- “ The Detective ” by paurian is licensed under CC BY 2.0 ↵
- “ In the Quiet Zone… ” by C.O.D. Library is licensed under CC BY-NC-SA 2.0 ↵
- NCSBN. (n.d.). NCSBN clinical judgment model . https://www.ncsbn.org/14798.htm ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- “ The Nursing Process ” by Kim Ernstmeyer at Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- “Patient Image in LTC.JPG” by ARISE project is licensed under CC BY 4.0 ↵
- American Nurses Association. (n.d.). The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process/ ↵
- American Nurses Association. (n.d.). The nursing process . https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process/ ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (3rd ed.). American Nurses Association. ↵
- American Nurses Association. (n.d.) The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process / ↵
- American Nurses Association. (n.d.). The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process / ↵
- Walivaara, B., Savenstedt, S., & Axelsson, K. (2013). Caring relationships in home-based nursing care - registered nurses’ experiences. The Open Journal of Nursing, 7 , 89-95. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3722540/pdf/TONURSJ-7-89.pdf ↵
- “ hospice-1793998_1280.jpg ” by truthseeker08 is licensed under CC0 ↵
- Watson Caring Science Institute. (n.d.). Watson Caring Science Institute. Jean Watson, PHD, RN, AHN-BC, FAAN, (LL-AAN) . https://www.watsoncaringscience.org/jean-bio/ ↵
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Med (Lausanne)
Rethinking clinical decision-making to improve clinical reasoning
Salvatore corrao.
1 Department of Internal Medicine, National Relevance and High Specialization Hospital Trust ARNAS Civico, Palermo, Italy
2 Dipartimento di Promozione della Salute Materno Infantile, Medicina Interna e Specialistica di Eccellenza “G. D’Alessandro” (PROMISE), University of Palermo, Palermo, Italy
Christiano Argano
Associated data.
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Improving clinical reasoning techniques is the right way to facilitate decision-making from prognostic, diagnostic, and therapeutic points of view. However, the process to do that is to fill knowledge gaps by studying and growing experience and knowing some cognitive aspects to raise the awareness of thinking mechanisms to avoid cognitive errors through correct educational training. This article examines clinical approaches and educational gaps in training medical students and young doctors. The authors explore the core elements of clinical reasoning, including metacognition, reasoning errors and cognitive biases, reasoning strategies, and ways to improve decision-making. The article addresses the dual-process theory of thought and the new Default Mode Network (DMN) theory. The reader may consider the article a first-level guide to deepen how to think and not what to think, knowing that this synthesis results from years of study and reasoning in clinical practice and educational settings.
Introduction
Clinical reasoning is based on complex and multifaceted cognitive processes, and the level of cognition is perhaps the most relevant factor that impacts the physician’s clinical reasoning. These topics have inspired considerable interest in the last years ( 1 , 2 ). According to Croskerry ( 3 ) and Croskerry and Norman ( 4 ), over 40 affective and cognitive biases may impact clinical reasoning. In addition, it should not be forgotten that both the processes and the subject matter are complex.
In medicine, there are thousands of known diagnoses, each with different complexity. Moreover, in line with Hammond’s view, a fundamental uncertainty will inevitably fail ( 5 ). Any mistake or failure in the diagnostic process leads to a delayed diagnosis, a misdiagnosis, or a missed diagnosis. The particular context in which a medical decision is made is highly relevant to the reasoning process and outcome ( 6 ).
More recently, there has been renewed interest in diagnostic reasoning, primarily diagnostic errors. Many researchers deepen inside the processes underpinning cognition, developing new universal reasoning and decision-making model: The Dual Process Theory.
This theory has a prompt implementation in medical decision-making and provides a comprehensive framework for understanding the gamma of theoretical approaches taken into consideration previously. This model has critical practical applications for medical decision-making and may be used as a model for teaching decision reasoning. Given this background, this manuscript must be considered a first-level guide to understanding how to think and not what to think, deepening clinical decision-making and providing tools for improving clinical reasoning.
Too much attention to the tip of the iceberg
The New England Journal of Medicine has recently published a fascinating article ( 7 ) in the “Perspective” section, whereon we must all reflect on it. The title is “At baseline” (the basic condition). Dr. Bergl, from the Department of Medicine of the Medical College of Wisconsin (Milwaukee), raised that his trainees no longer wonder about the underlying pathology but are focused solely on solving the acute problem. He wrote that, for many internal medicine teams, the question is not whether but to what extent we should juggle the treatment of critical health problems of patients with care for their coexisting chronic conditions. Doctors are under high pressure to discharge, and then they move patients to the next stage of treatment without questioning the reason that decompensated the clinical condition. Suppose the chronic condition or baseline was not the fundamental goal of our performance. In that case, our juggling is highly inconsistent because we are working on an intermediate outcome curing only the decompensation phase of a disease. Dr. Bergl raises another essential matter. Perhaps equally disturbing, by adopting a collective “base” mentality, we unintentionally create a group of doctors who prioritize productivity rather than developing critical skills and curiosity. We agree that empathy and patience are two other crucial elements in the training process of future internists. Nevertheless, how much do we stimulate all these qualities? Perhaps are not all part of cultural backgrounds necessary for a correct patient approach, the proper clinical reasoning, and balanced communication skills?
On the other hand, a chronic baseline condition is not always the real reason that justifies acute hospitalization. The lack of a careful approach to the baseline and clinical reasoning focused on the patient leads to this superficiality. We are focusing too much on our students’ practical skills and the amount of knowledge to learn. On the other hand, we do not teach how to think and the cognitive mechanisms of clinical reasoning.
Time to rethink the way of thinking and teaching courses
Back in 1910, John Dewey wrote in his book “How We Think” ( 8 ), “The aim of education should be to teach us rather how to think than what to think—rather improve our minds to enable us to think for ourselves than to load the memory with the thoughts of other men.”
Clinical reasoning concerns how to think and make the best decision-making process associated with the clinical practice ( 9 ). The core elements of clinical reasoning ( 10 ) can be summarized in:
- 1. Evidence-based skills,
- 2. Interpretation and use of diagnostic tests,
- 3. Understanding cognitive biases,
- 4. Human factors,
- 5. Metacognition (thinking about thinking), and
- 6. Patient-centered evidence-based medicine.
All these core elements are crucial for the best way of clinical reasoning. Each of them needs a correct learning path to be used in combination with developing the best thinking strategies ( Table 1 ). Reasoning strategies allow us to combine and synthesize diverse data into one or more diagnostic hypotheses, make the complex trade-off between the benefits and risks of tests and treatments, and formulate plans for patient management ( 10 ).
Set of some reasoning strategies (view the text for explanations).
However, among the abovementioned core element of clinical reasoning, two are often missing in the learning paths of students and trainees: metacognition and understanding cognitive biases.
Metacognition
We have to recall cognitive psychology, which investigates human thinking and describes how the human brain has two distinct mental processes that influence reasoning and decision-making. The first form of cognition is an ancient mechanism of thought shared with other animals where speed is more important than accuracy. In this case, thinking is characterized by a fast, intuitive way that uses pattern recognition and automated processes. The second one is a product of evolution, particularly in human beings, indicated by an analytical and hypothetical-deductive slow, controlled, but highly consuming way of thinking. Today, the psychology of thinking calls this idea “the dual-process theory of thought” ( 11 – 14 ). The Nobel Prize in Economic Sciences awardee Daniel Kahneman has extensively studied the dichotomy between the two modes of thought, calling them fast and slow thinking. “System 1” is fast, instinctive, and emotional; “System 2” is slower, more deliberative, and more logical ( 15 ). Different cerebral zones are involved: “System 1” includes the dorsomedial prefrontal cortex, the pregenual medial prefrontal cortex, and the ventromedial prefrontal cortex; “System 2” encompasses the dorsolateral prefrontal cortex. Glucose utilization is massive when System 2 is performing ( 16 ). System 1 is the leading way of thought used. None could live permanently in a deliberate, slow, effortful way. Driving a car, eating, and performing many activities over time become automatic and subconscious.
A recent brilliant review of Gronchi and Giovannelli ( 17 ) explores those things. Typically, when a mental effort is required for tasks requiring attention, every individual is subject to a phenomenon called “ego-depletion.” When forced to do something, each one has fewer cognitive resources available to activate slow thinking and thus is less able to exert self-control ( 18 , 19 ). In the same way, much clinical decision-making becomes intuitive rather than analytical, a phenomenon strongly affected by individual differences ( 20 , 21 ). Experimental evidence by functional magnetic resonance imaging and positron emission tomography studies supports that the “resting state” is spontaneously active during periods of “passivity” ( 22 – 25 ). The brain regions involved include the medial prefrontal cortex, the posterior cingulate cortex, the inferior parietal lobule, the lateral temporal cortex, the dorsal medial prefrontal cortex, and the hippocampal formation ( 26 ). Findings reporting high-metabolic activity in these regions at rest ( 27 ) constituted the first clear evidence of a cohesive default mode in the brain ( 28 ), leading to the widely acknowledged introduction of the Default Mode Network (DMN) concept. The DMN contains the medial prefrontal cortex, the posterior cingulate cortex, the inferior parietal lobule, the lateral temporal cortex, the dorsal medial prefrontal cortex, and the hippocampal formation. Lower activity levels characterize the DMN during goal-directed cognition and higher activity levels when an individual is awake and involved in the mental processes requiring low externally directed attention. All that is the neural basis of spontaneous cognition ( 26 ) that is responsible for thinking using internal representations. This paradigm is growing the idea of stimulus-independent thoughts (SITs), defined by Buckner et al. ( 26 ) as “thoughts about something other than events originating from the environment” that is covert and not directed toward the performance of a specific task. Very recently, the role of the DMN was highlighted in automatic behavior (the rapid selection of a response to a particular and predictable context) ( 29 ), as opposed to controlled decision making, suggesting that the DMN plays a role in the autopilot mode of brain functioning.
In light of these premises, everyone can pause to analyze what he is doing, improving self-control to avoid “ego-depletion.” Thus, one can actively switch between one type of thinking and the other. The ability to make this switch makes the physician more performing. In addition, a physician can be trained to understand the ways of thinking and which type of thinking is engaged in various situations. This way, experience and methodology knowledge can energize Systems 1 and 2 and how they interact, avoiding cognitive errors. Figure 1 summarizes all the concepts abovementioned about the Dual Mode Network and its relationship with the DMN.

Graphical representation of the characteristics of Dual Mode Network, including the relationship between the two systems by Default Mode Network (view the text for explanations).
Emotional intelligence is another crucial factor in boosting clinical reasoning for the best decision-making applied to a single patient. Emotional intelligence recognizes one’s emotions. Those others label different feelings appropriately and use emotional information to guide thinking and behavior, adjust emotions, and create empathy, adapt to environments, and achieve goals ( 30 ). According to the phenomenological account of Fuchs, bodily perception (proprioception) has a crucial role in understanding others ( 31 ). In this sense, the proprioceptive skills of a physician can help his empathic understanding become elementary for empathy and communication with the patient. In line with Fuchs’ view, empathic understanding encompasses a bodily resonance and mediates contextual knowledge about the patient. For medical education, empathy should help to relativize the singular experience, helping to prevent that own position becomes exclusive, bringing oneself out of the center of one’s own perspective.
Reasoning errors and cognitive biases
Errors in reasoning play a significant role in diagnostic errors and may compromise patient safety and quality of care. A recently published review by Norman et al. ( 32 ) examined clinical reasoning errors and how to avoid them. To simplify this complex issue, almost five types of diagnostic errors can be recognized: no-fault errors, system errors, errors due to the knowledge gap, errors due to misinterpretation, and cognitive biases ( 9 ). Apart from the first type of error, which is due to unavoidable errors due to various factors, we want to mention cognitive biases. They may occur at any stage of the reasoning process and may be linked to intuition and analytical systems. The most frequent cognitive biases in medicine are anchoring, confirmation bias, premature closure, search satisficing, posterior probability error, outcome bias, and commission bias ( 33 ). Anchoring is characterized by latching onto a particular aspect at the initial consultation, and then one refuses to change one’s mind about the importance of the later stages of reasoning. Confirmation bias ignores the evidence against an initial diagnosis. Premature closure leads to a misleading diagnosis by stopping the diagnostic process before all the information has been gathered or verified. Search satisficing blinds other additional diagnoses once the first diagnosis is made posterior probability error shortcuts to the usual patient diagnosis for previously recognized clinical presentations. Outcome bias impinges on our desire for a particular outcome that alters our judgment (e.g., a surgeon blaming sepsis on pneumonia rather than an anastomotic leak). Finally, commission bias is the tendency toward action rather than inaction, assuming that only good can come from doing something (rather than “watching and waiting”). These biases are only representative of the other types, and biases often work together. For example, in overconfidence bias (the tendency to believe we know more than we do), too much faith is placed in opinion instead of gathered evidence. This bias can be augmented by the anchoring effect or availability bias (when things are at the forefront of your mind because you have seen several cases recently or have been studying that condition in particular), and finally by commission bias—with disastrous results.
Novice vs. expert approaches
The reasoning strategies used by novices are different from those used by experts ( 34 ). Experts can usually gather beneficial information with highly effective problem-solving strategies. Heuristics are commonly, and most often successfully, used. The expert has a saved bank of illness scripts to compare and contrast the current case using more often type 1 thinking with much better results than the novice. Novices have little experience with their problems, do not have time to build a bank of illness scripts, and have no memories of previous similar cases and actions in such cases. Therefore, their mind search strategies will be weak, slow, and ponderous. Heuristics are poor and more often unsuccessful. They will consider a more comprehensive range of diagnostic possibilities and take longer to select approaches to discriminate among them. A novice needs specific knowledge and specific experience to become an expert. In our opinion, he also needs special training in the different ways of thinking. It is possible to study patterns, per se as well. It is, therefore, likely to guide the growth of knowledge for both fast thinking and slow one.
Moreover, learning by osmosis has traditionally been the method to move the novice toward expert capabilities by gradually gaining experience while observing experts’ reasoning. However, it seems likely that explicit teaching of clinical reasoning could make this process quicker and more effective. In this sense, an increased need for training and clinical knowledge along with the skill to apply the acquired knowledge is necessary. Students should learn disease pathophysiology, treatment concepts, and interdisciplinary team communication developing clinical decision-making through case-series-derived knowledge combining associative and procedural learning processes such as “Vienna Summer School on Oncology” ( 35 ).
Moreover, a refinement of the training of communicative skills is needed. Improving communication skills training for medical students and physicians should be the university’s primary goal. In fact, adequate communication leads to a correct diagnosis with 76% accuracy ( 36 ). The main challenge for students and physicians is the ability to respond to patients’ individual needs in an empathic and appreciated way. In this regard, it should be helpful to apply qualitative studies through the adoption of a semi-structured or structured interview using face-to-face in-depth interviews and e-learning platforms which can foster interdisciplinary learning by developing expertise for the clinical reasoning and decision-making in each area and integrating them. They could be effective tools to develop clinical reasoning and decision-making competencies and acquire effective communication skills to manage the relationship with patient ( 37 – 40 ).
Clinical reasoning ways
Clinical reasoning is complex: it often requires different mental processes operating simultaneously during the same clinical encounter and other procedures for different situations. The dual-process theory describes how humans have two distinct approaches to decision-making ( 41 ). When one uses heuristics, fast-thinking (system 1) is used ( 42 ). However, complex cases need slow analytical thinking or both systems involved ( 15 , 43 , 44 ). Slow thinking can use different ways of reasoning: deductive, hypothetic-deductive, inductive, abductive, probabilistic, rule-based/categorical/deterministic, and causal reasoning ( 9 ). We think that abductive and causal reasoning need further explanation. Abductive reasoning is necessary when no deductive argument (from general assumption to particular conclusion) nor inductive (the opposite of deduction) may be claimed.
In the real world, we often face a situation where we have information and move backward to the likely cause. We ask ourselves, what is the most plausible answer? What theory best explains this information? Abduction is just a process of choosing the hypothesis that would best explain the available evidence. On the other hand, causal reasoning uses knowledge of medical sciences to provide additional diagnostic information. For example, in a patient with dyspnea, if considering heart failure as a casual diagnosis, a raised BNP would be expected, and a dilated vena cava yet. Other diagnostic possibilities must be considered in the absence of these confirmatory findings (e.g., pneumonia). Causal reasoning does not produce hypotheses but is typically used to confirm or refute theories generated using other reasoning strategies.
Hypothesis generation and modification using deduction, induction/abduction, rule-based, causal reasoning, or mental shortcuts (heuristics and rule of thumbs) is the cognitive process for making a diagnosis ( 9 ). Clinicians develop a hypothesis, which may be specific or general, relating a particular situation to knowledge and experience. This process is referred to as generating a differential diagnosis. The process we use to produce a differential diagnosis from memory is unclear. The hypotheses chosen may be based on likelihood but might also reflect the need to rule out the worst-case scenario, even if the probability should always be considered.
Given the complexity of the involved process, there are numerous causes for failure in clinical reasoning. These can occur in any reasoning and at any stage in the process ( 33 ). We must be aware of subconscious errors in our thinking processes. Cognitive biases are subconscious deviations in judgment leading to perceptual distortion, inaccurate assessment, and misleading interpretation. From an evolutionary point of view, they have developed because, often, speed is more important than accuracy. Biases occur due to information processing heuristics, the brain’s limited capacity to process information, social influence, and emotional and moral motivations.
Heuristics are mind shortcuts and are not all bad. They refer to experience-based techniques for decision-making. Sometimes they may lead to cognitive biases (see above). They are also essential for mental processes, expressed by expert intuition that plays a vital role in clinical practice. Intuition is a heuristic that derives from a natural and direct outgrowth of experiences that are unconsciously linked to form patterns. Pattern recognition is just a quick shortcut commonly used by experts. Alternatively, we can create patterns by studying differently and adequately in a notional way that accumulates information. The heuristic that rules out the worst-case scenario is a forcing mind function that commits the clinician to consider the worst possible illness that might explain a particular clinical presentation and take steps to ensure it has been effectively excluded. The heuristic that considers the least probable diagnoses is a helpful approach to uncommon clinical pictures and thinking about and searching for a rare unrecognized condition. Clinical guidelines, scores, and decision rules function as externally constructed heuristics, usually to ensure the best evidence for the diagnosis and treatment of patients.
Hence, heuristics are helpful mind shortcuts, but the exact mechanisms may lead to errors. Fast-and-frugal tree and take-the-best heuristic are two formal models for deciding on the uncertainty domain ( 45 ).
In the recent times, clinicians have faced dramatic changes in the pattern of patients acutely admitted to hospital wards. Patients become older and older with comorbidities, rare diseases are frequent as a whole ( 46 ), new technologies are growing in a logarithmic way, and sustainability of the healthcare system is an increasingly important problem. In addition, uncommon clinical pictures represent a challenge for clinicians ( 47 – 50 ). In our opinion, it is time to claim clinical reasoning as a crucial way to deal with all complex matters. At first, we must ask ourselves if we have lost the teachings of ancient masters. Second, we have to rethink medical school courses and training ones. In this way, cognitive debiasing is needed to become a well-calibrated clinician. Fundamental tools are the comprehensive knowledge of nature and the extent of biases other than studying cognitive processes, including the interaction between fast and slow thinking. Cognitive debiasing requires the development of good mindware and the awareness that one debiasing strategy will not work for all biases. Finally, debiasing is generally a complicated process and requires lifelong maintenance.
We must remember that medicine is an art that operates in the field of science and must be able to cope with uncertainty. Managing uncertainty is the skill we have to develop against an excess of confidence that can lead to error. Sound clinical reasoning is directly linked to patient safety and quality of care.
Data availability statement
Author contributions.
SC and CA drafted the work and revised it critically. Both authors have approved the submission of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
- Open access
- Published: 26 March 2024
The effect of “typical case discussion and scenario simulation” on the critical thinking of midwifery students: Evidence from China
- Yuji Wang 1 na1 ,
- Yijuan Peng 1 na1 &
- Yan Huang 1
BMC Medical Education volume 24 , Article number: 340 ( 2024 ) Cite this article
Metrics details
Assessment ability lies at the core of midwives’ capacity to judge and treat clinical problems effectively. Influenced by the traditional teaching method of “teacher-led and content-based”, that teachers involve imparting a large amount of knowledge to students and students lack active thinking and active practice, the clinical assessment ability of midwifery students in China is mostly at a medium or low level. Improving clinical assessment ability of midwifery students, especially critical thinking, is highly important in practical midwifery education. Therefore, we implemented a new teaching program, “typical case discussion and scenario simulation”, in the Midwifery Health Assessment course. Guided by typical cases, students were organized to actively participate in typical case discussions and to promote active thinking and were encouraged to practice actively through scenario simulation. In this study, we aimed to evaluate the effect of this strategy on the critical thinking ability of midwifery students.
A total of 104 midwifery students in grades 16–19 at the West China School of Nursing, Sichuan University, were included as participants through convenience sampling. All the students completed the Midwifery Health Assessment course in the third year of university. Students in grades 16 and 17 were assigned to the control group, which received routine teaching in the Midwifery Health Assessment, while students in grades 18 and 19 were assigned to the experimental group, for which the “typical case discussion and scenario simulation” teaching mode was employed. The Critical Thinking Disposition Inventory-Chinese Version (CTDI-CV) and Midwifery Health Assessment Course Satisfaction Questionnaire were administered after the intervention.
After the intervention, the critical thinking ability of the experimental group was greater than that of the control group (284.81 ± 27.98 and 300.94 ± 31.67, p = 0.008). Furthermore, the experimental group exhibited higher scores on the four dimensions of Open-Mindedness (40.56 ± 5.60 and 43.59 ± 4.90, p = 0.005), Analyticity (42.83 ± 5.17 and 45.42 ± 5.72, p = 0.020), Systematicity (38.79 ± 4.70 and 41.88 ± 6.11, p = 0.006), and Critical Thinking Self-Confidence (41.35 ± 5.92 and 43.83 ± 5.89, p = 0.039) than did the control group. The course satisfaction exhibited by the experimental group was greater than that exhibited by the control group (84.81 ± 8.49 and 90.19 ± 8.41, p = 0.002).
The “typical case discussion and scenario simulation” class mode can improve the critical thinking ability of midwifery students and enhance their curriculum satisfaction. This approach carries a certain degree of promotional significance in medical education.
Typical case discussion and scenario simulation can improve midwifery students’ critical thinking ability.
Typical case discussion and scenario simulation can enhance students’ learning interest and guide students to learn independently.
Midwifery students were satisfied with the new teaching mode.
Peer Review reports
Maternal and neonatal health are important indicators to measure of the level of development of a country’s economy, culture and health care. The positive impact of quality midwifery education on maternal and newborn health is acknowledged in the publication framework for action strengthening quality midwifery education issued by the World Health Organization (WHO) [ 1 ]. Extensive evidence has shown that skilled midwifery care is crucial for reducing preventable maternal and neonatal mortality [ 2 , 3 , 4 ]. Clinical practice features high requirements for the clinical thinking ability of midwives, which refers to the process by which medical personnel analyze and integrate data with professional medical knowledge in the context of diagnosis and treatment as well as discover and solve problems through logical reasoning [ 5 ]. Critical thinking is a thoughtful process that is purposeful, disciplined, and self-directed and that aims to improve decisions and subsequent actions [ 6 ]. In 1986, the American Association of Colleges of Nursing formulated the “Higher Education Standards for Nursing Specialty”, which emphasize the fact that critical thinking is the primary core competence that nursing graduates should possess [ 7 ]. Many studies have shown that critical thinking can help nurses detect, analyze and solve problems creatively in clinical work and is a key factor in their ability to make correct clinical decisions [ 8 , 9 , 10 ].
However, the traditional teaching method used for midwifery students in China is “teacher-led and content-based”, and it involves efficiently and conveniently imparting a large amount of knowledge to students over a short period. Students have long failed to engage in active thinking and active practice, and the cultivation of critical thinking has long been ignored [ 5 ]. As a result, the critical thinking ability of midwifery students in China is mostly at a medium or low level [ 5 ]. Therefore, it is necessary to develop a new teaching mode to improve the critical thinking ability of midwifery students.
In 2014, Professor Xuexin Zhang of Fudan University, Shanghai, China, proposed a novel teaching method: the divided class mode. The basic idea of this approach is to divide the class time into two parts. The teachers explain the theoretical knowledge in the first lesson, and the students discuss that knowledge in the second lesson. This approach emphasizes the guiding role of teachers and encourages and empowers students to take responsibility for their studies [ 11 ]. Research has shown that the divided class mode can improve students’ enthusiasm and initiative as well as teaching effectiveness [ 12 ].
The problem-originated clinical medical curriculum mode of teaching was first established at McMaster University in Canada in 1965. This model is based on typical clinical cases and a problem-oriented heuristic teaching model [ 13 ]. The process of teaching used in this approach is guided by typical cases with the goal of helping students combine theoretical knowledge and practical skills. This approach can enhance the enthusiasm and initiative of students by establishing an active learning atmosphere. Students are encouraged to discuss and analyze typical cases to promote their ability to digest and absorb theoretical knowledge. Research has shown that the problem-originated clinical medical curriculum teaching mode can enhance students’ confidence and improve their autonomous learning and exploration ability. Scenario simulation teaching can provide students with real scenarios, allowing them to practice and apply their knowledge in a safe environment [ 14 ], which can effectively improve their knowledge and clinical skills and enhance their self-confidence [ 15 , 16 ].
Based on the teaching concept of divided classes, our research team established a new teaching model of “typical case discussion and scenario simulation”. Half of the class time is allocated for students to discuss typical cases and carry out scenario simulations to promote their active thinking and active practice. The Midwifery Health Assessment is the final professional core course that midwifery students must take in our school before clinical practice. All students must complete the course in Grade 3. Teaching this course is important for cultivating the critical thinking and clinical assessment ability of midwifery students. Therefore, our team adopted the new teaching mode of "typical case discussion and scenario simulation" in the teaching of this course. This study explored the teaching mode’s ability to improve the critical thinking ability of midwifery students.
Study design
The study employed a semiexperimental design.
Participants
A convenience sample of 104 third-year midwifery students who were enrolled in the Midwifery Health Assessment course volunteered to participate in this research at a large public university in Sichuan Province from February 2019 to June 2022 (grades 16 to 19). All the students completed the course in the third year of university. Students in grades 16 and 17 were assigned to the control group, which received the traditional teaching mode. Students in grades 18 and 19 were assigned to the experimental group, in which context the “typical case discussion and scenario simulation” class mode was used. The exclusion criteria for midwifery students were as follows: (1) dropped out of school during the study, (2) took continuous leave from school for more than two weeks, or (3) were unable to complete the questionnaire. The elimination criterion for midwifery students was that all the items were answered in the same way. No significant differences in students’ scores in their previous professional courses (Midwifery) were observed between the two groups. Textbooks, teachers, and teaching hours were the same for both groups.
Development of the “typical case discussion and scenario simulation” class mode
This study is based on the implementation of the new century higher education teaching reform project at Sichuan University. With the support of Sichuan University, we first established a “typical case discussion and scenario simulation” class mode team. The author of this paper was the head of the teaching reform project and served as a consultant, and the first author is responsible for supervising the implementation of the project. Second, the teaching team discussed and developed a standard process for the “typical case discussion and scenario simulation” class mode. Third, the entire team received intensive training in the standard process for the “typical case discussion and scenario simulation” class mode.
Implementation of the “typical case discussion and scenario simulation” class mode
Phase i (before class).
Before class, in accordance with the requirements for evaluating different periods of pregnancy, the teacher conceptualized typical cases and then discussed those cases with the teaching team and made any necessary modifications. After the completion of the discussion, the modified cases were released to the students through the class group. To ensure students’ interest, they were guided through the task of discovering and solving relevant problems using an autonomous learning approach.
Phase II (the first week)
Typical case discussion period. The Midwifery Health Assessment course was taught by 5 teachers and covered 5 health assessment periods, namely, the pregnancy preparation, pregnancy, delivery, puerperium and neonatal periods. The health assessment course focused on each period over 2 consecutive teaching weeks, and 2 lessons were taught per week. The first week focused on the discussion of typical cases. In the first lesson, teachers introduced typical cases, taught key knowledge or difficult evaluation content pertaining to the different periods, and explored the relevant knowledge framework. In the second lesson, teachers organized group discussions, case analyses and intergroup communications for the typical cases. They were also responsible for coordinating and encouraging students to participate actively in the discussion. After the discussion, teachers and students reviewed the definitions, treatments and evaluation points associated with the typical cases. The teachers also encouraged students to internalize knowledge by engaging in a process of summary and reflection to achieve the purpose of combining theory with practice.
Phase III (the second week)
Scenario simulation practice period. The second week focused on the scenario simulation practice period. In the first lesson, teachers reviewed the focus of assessment during the different periods and answered students’ questions. In the second lesson, students performed typical case assessment simulations in subgroups. After the simulation, the teachers commented on and summarized the students’ simulation evaluation and reviewed the evaluation points of typical cases to improve the students’ evaluation ability.
The organizational structure and implementation of the “typical case discussion and scenario simulation” class mode showed in Fig. 1 .
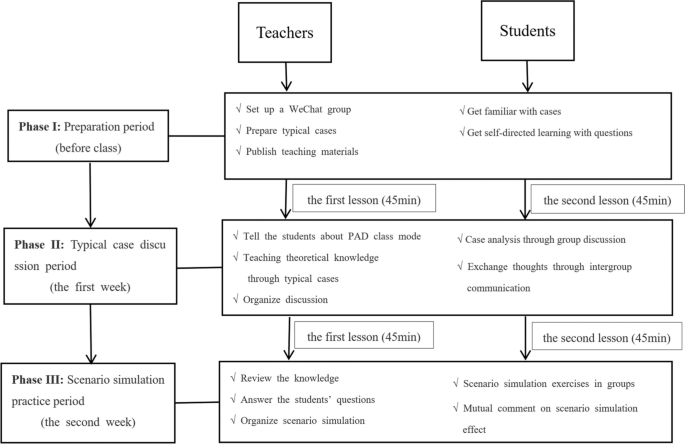
“Typical case discussion and scenario simulation” teaching mode diagram
A demographic questionnaire designed for this purpose was used to collect relevant information from participants, including age, gender, single-child status, family location, experience with typical case discussion or scenario simulation and scores in previous professional courses (Midwifery).
The Critical Thinking Disposition Inventory-Chinese Version (CTDI-CV) was developed by Peng et al. to evaluate the critical thinking ability of midwifery students [ 17 ]. The scale contains 70 items across a total of seven dimensions, namely, open-mindedness, truth-seeking, analytical ability, systematic ability, self-confidence in critical thinking, thirst for knowledge, and cognitive maturity. Each dimension is associated with 10 items, and each item is scored on a 6-point Likert scale, with 1 indicating “extremely agree” and 6 representing “extremely disagree”. The scale includes 30 positive items, which receive scores ranging from “extremely agree” to “extremely disagree” on a scale of 6 to 1, and 40 negative items, which receive scores ranging from “extremely agree” to “extremely disagree” on a scale of 1 to 6. A total score less than 210 indicates negative critical thinking ability, scores between 211 and 279 indicate an unclear meaning, scores of 280 or higher indicate positive critical thinking ability, and scores of 350 or higher indicate strong performance. The score range of each trait is 10–60 points; a score of 30 points or fewer indicates negative trait performance, scores between 31 and 39 points indicate that the trait meaning is incorrect, scores of 40 points or higher indicate positive trait performance, and scores of 50 points or higher indicate extremely positive trait performance. The Cronbach’s α coefficient of the scale was 0.90, thus indicating good content validity and structure. The higher an individual’s score on this measure is, the better that individual’s critical thinking ability.
The evaluation of teaching results was based on a questionnaire used to assess undergraduate course satisfaction, and the researchers deleted and modified items in the questionnaire to suit the context of the “typical case discussion and scenario simulation” teaching mode. Two rounds of discussion were held within the study group to form the final version of the Midwifery Health Assessment satisfaction questionnaire. The questionnaire evaluates the effect of teaching in terms of three dimensions, namely, curriculum content, curriculum teaching and curriculum evaluation. The questionnaire contains 21 items, each of which is scored on a 5-point Likert scale, with 1 indicating “extremely disagree” and 5 representing “extremely agree”. The higher the score is, the better the teaching effect.
Data collection and statistical analysis
We input the survey data into the “Wenjuanxing” platform ( https://www.wjx.cn/ ), which specializes in questionnaire services. At the beginning of the study, an electronic questionnaire was distributed to the students in the control group via student WeChat and QQ groups for data collection. After the intervention, an electronic questionnaire was distributed to the students in the experimental group for data collection in the final class of the Midwifery Health Assessment course. All the data were collected by the first author (Yuji Wang). When students had questions about the survey items, the first author (Yuji Wang) immediately explained the items in detail. To ensure the integrity of the questionnaire, the platform required all the items to be answered before submission.
Statistical Package for Social Sciences Version 26.0 (SPSS 26.0) software was used for data analysis. The Shapiro‒Wilk test was used to test the normality of the data. The measurement data are expressed as the mean ± standard deviation (X ± S), and an independent sample t test was used for comparisons among groups with a normal distribution. The data presented as the number of cases (%), and the chi-square test was performed. A P value < 0.05 indicated that a difference was statistically significant.
Ethical considerations
The study was funded by the New Century Teaching Reform Project of Sichuan University and passed the relevant ethical review. Oral informed consent was obtained from all individual participants in the study.
Characteristics of the participants
A total of 104 third-year midwifery students were enrolled from February 2019 to June 2022, and 98.1% (102/144) of these students completed the survey. Two invalid questionnaires that featured the same answers for each item were eliminated. A total of 100 participants were ultimately included in the analysis. Among the participants, 48 students were assigned to the control group, and 52 students were assigned to the experimental group. The age of the students ranged from 19 to 22 years, and the mean age of the control group was 20.50 years (SD = 0.61). The mean age of the experimental group was 20.63 years (SD = 0.65). Of the 100 students who participated in the study, the majority (96.0%) were women. No significant differences were observed between the intervention and control groups in terms of students’ demographic information (i.e., age, gender, status as an only child, or family location), experience with scenario simulation or typical case discussion and scores in previous Midwifery courses (Table 1 ).
Examining the differences in critical thinking ability between the two groups
The aim of this study was to evaluate the effect of the new teaching mode of “typical case discussion and scenario simulation” on improving the critical thinking ability of midwifery students. Independent sample t tests were used to examine the differences in critical thinking ability between the two groups (Table 2 ). The results showed that the total critical thinking scores obtained by the experimental group were greater than those obtained by the control group (284.81 ± 27.98 and 300.94 ± 31.67, p = 0.008). The differences in four dimensions (Open-Mindedness (40.56 ± 5.60 and 43.59 ± 4.90, p = 0.005), Analyticity (42.83 ± 5.17 and 45.42 ± 5.72, p = 0.020), Systematicity (38.79 ± 4.70 and 41.88 ± 6.11, p = 0.006), and Critical Thinking Self-Confidence (41.35 ± 5.92 and 43.83 ± 5.89, p = 0.039)) were statistically significant.
Examining the differences in curriculum satisfaction between the two groups
To evaluate the effect of the new teaching mode of “the typical case discussion and scenario simulation” on the course satisfaction of midwifery students. Independent sample t tests were used to examine the differences in course satisfaction between the two groups (Table 3 ). The results showed that the curriculum satisfaction of the experimental group was greater than that of the control group (84.81 ± 8.49 and 90.19 ± 8.41, p = 0.002). Independent sample t tests were used to examine the differences in the three dimensions of curriculum satisfaction between the two groups (Table 3 ). The results showed that the average scores of the intervention group on the three dimensions were significantly greater than those of the control group (curricular content: 20.83 ± 1.96 and 22.17 ± 2.23, p = 0.002; curriculum teaching: 34.16 ± 3.89 and 36.59 ± 3.66, p = 0.002; curriculum evaluation: 29.81 ± 3.27 and 31.42 ± 3.19, p = 0.015).
Midwifery is practical and intensive work. To ensure maternal and child safety, midwives must make decisions and take action quickly. Therefore, midwives should have both critical thinking ability and clinical decision-making ability [ 18 ]. In addition, the Australian Nursing and Midwifery Accreditation Council (ANMAC) regulates the educational requirements for the programs required for registration as a midwife. According to these standards, education providers must incorporate learning activities into curricula to encourage the development and application of critical thinking and reflective practice [ 19 ]. Therefore, the challenge of cultivating the critical thinking ability of midwifery students is an urgent problem that must be solved. However, influenced by the traditional teaching method of “teacher-led and content-based”, the critical thinking ability of midwifery students in China is mostly at a medium or low level. In order to improve the critical thinking ability of midwifery students. Our research team has established a new teaching model, the “typical case discussion and scenario simulation” class model. And applied to the midwifery core curriculum Midwifery Health Assessment. This study aimed to investigate the implementation of a novel systematic and structured teaching model for midwifery students and to provide evidence regarding how to improve the critical thinking ability of midwives.
The results showed that the total CTDI-CV score obtained for the experimental group was greater than that obtained for the control group. These findings indicate that the “typical case discussion and scenario simulation” class mode had a positive effect on the cultivation of students’ critical thinking ability, a conclusion which is similar to the findings of Holdsworth et al. [ 20 ], Lapkin et al. [ 21 ] and Demirören M et al. [ 22 ]. We indicate the following reasons that may explain these results.The core aim of the typical case discussion teaching mode is to raise questions based on typical clinical cases and to provide heuristic teaching to students [ 23 ]. This approach emphasizes asking questions based on specific clinical cases, which enables students to engage in targeted learning. Moreover, scenario simulation allows students to attain certain inner experiences and emotions and actively participate in curriculum practice, which can enhance their ability to remember and understand knowledge [ 24 ]. Through the divided class mode, half of the class time was divided into the students. This method emphasizes the guiding role of teachers and encourages and empowers students to assume learning responsibilities. In addition, students can think, communicate and discuss actively [ 22 , 23 ]. Furthermore, this approach created opportunities for students to analyze and consider problems independently and give students sufficient time to internalize and absorb knowledge and deepen their understanding of relevant knowledge, which can increase their confidence in their ability to address such problems and improve their critical thinking ability [ 12 , 25 , 26 ].
In addition, the results showed that except for Truth-Seeking and Systematicity, the other five dimensions were all positive. These findings are similar to the results reported by Atakro et al.. and Sun et al. [ 27 , 28 ]. Through the intervention, the Systematicity scores became positive, suggesting that the new teaching mode can help students deal with problems in an organized and purposeful way. However, Truth-Seeking still did not become positive; this notion focuses on intellectual honesty, i.e., the disposition to be courageous when asking questions and to be honest and objective in the pursuit of knowledge even when the topics under investigation do not support one’s self-interest [ 29 ]. Studies have shown that this factor is related to the traditional teaching mode used [ 30 ]. The traditional teaching mode focuses on knowledge infusion, helps students remember the greatest possible amount of knowledge in a short time, and does not focus on guiding students to seek knowledge with sincerity and objectivity. Therefore, in future educational practice, we should focus on cultivating students’ ability to seek truth and engage in systematization.
Student evaluative feedback is an important way to test the effectiveness teaching mode. Therefore, understanding students’ evaluations of the effects of classroom teaching is key to promoting teaching reform and improving teaching quality. Therefore, we distributed a satisfaction questionnaire pertaining to the midwifery health assessment curriculum, which was based on the “typical case discussion and scenario simulation” class mode, with the goal of investigating curriculum satisfaction in terms of three dimensions (curriculum content, curriculum teaching and curriculum evaluation). The results showed that the satisfaction scores for each dimension increased significantly. This finding suggests that the new teaching method can enrich the teaching content, diversify the teaching mode and improve students’ curriculum evaluations.
In summary, the “typical case discussion and scenario simulation” class mode focuses on typical cases as its main content. Students’ understanding of this content is deepened through group discussion and scenario simulation. The subjectivity of students in curriculum learning should be accounted for. Students can be encouraged to detect, analyze and solve problems with the goal of improving their critical thinking ability. Moreover, this approach can also enhance curriculum satisfaction. It is recommended that these tools should be used continuously in future curriculum teaching.
This study has several limitations. First, the representativeness of the sample may be limited since the participants were recruited from specific universities in China. Second, we used historical controls, which are less effective than simultaneous controlled trials. Third, online self-report surveys are susceptible to response biases, although we included quality control measurements in the process of data collection. Fourth, we did not use the same critical thinking instrument, CTDI-CV, to investigate the critical thinking of the students in the experimental group or the control group before intervention but used professional course grades from the Midwifery for substitution comparison. This may not be a sufficient substitute. However, these comparisons could be helpful since those grades included some sort of evaluation of critical thinking. In light of these limitations, future multicenter simultaneous controlled studies should be conducted. Nonetheless, this study also has several strengths. First, no adjustment of teachers or change in learning materials occurred since the start of the midwifery health assessment, thus ensuring that the experimental and control groups featured the same teaching materials, teachers and teaching hours. In addition, to ensure the quality of the research, the first author of this paper participated in the entirety of the course teaching.
The “typical case discussion and scenario simulation” class mode can improve the critical thinking of midwifery students, which is helpful for ensuring maternal and child safety. Students are highly satisfied with the new teaching mode, and this approach has a certain degree of promotional significance. However, this approach also entails higher requirements for both teachers and students.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
World Health Organisation, Strengthening quality midwifery education for Universal Health Coverage2030,2019, https://www.who.int/maternal_child_adolescent/topics/quality-of-care/midwifery/strengthening-midwifery-education/en/ (accessed 21.01.20).
Akombi BJ, Renzaho AM. Perinatal mortality in Sub-Saharan Africa: a meta-analysis of demographic and health surveys. Ann Glob Health. 2019;85(1):106.
Article Google Scholar
Campbell OM, Graham WJ. Strategies for reducing maternal mortality: getting on with what works. Lancet. 2006;368(9543):1284–99.
Gage AD, Carnes F, Blossom J, Aluvaala J, Amatya A, Mahat K, Malata A, Roder-DeWan S, Twum-Danso N, Yahya T, et al. In low- and middle-income countries, is delivery in high-quality obstetric facilities geographically feasible? Health Aff (Millwood). 2019;38(9):1576–84.
Xing C, Zhou Y, Li M, Wu Q, Zhou Q, Wang Q, Liu X. The effects of CPBL + SBAR teaching mode among the nursing students. Nurse Educ Today. 2021;100:104828.
Carter AG, Creedy DK, Sidebotham M. Critical thinking evaluation in reflective writing: development and testing of Carter assessment of critical thinking in midwifery (Reflection). Midwifery. 2017;54:73–80.
Yeh SL, Lin CT, Wang LH, Lin CC, Ma CT, Han CY. The Outcomes of an Interprofessional simulation program for new graduate nurses. Int J Environ Res Public Health. 2022;19(21):13839.
Chang MJ, Chang YJ, Kuo SH, Yang YH, Chou FH. Relationships between critical thinking ability and nursing competence in clinical nurses. J Clin Nurs. 2011;20(21–22):3224–32.
Shoulders B, Follett C, Eason J. Enhancing critical thinking in clinical practice: implications for critical and acute care nurses. Dimens Crit Care Nurs. 2014;33(4):207–14.
Jalalpour H, Jahani S, Asadizaker M, Sharhani A, Heybar H. The impact of critical thinking training using critical thinking cards on clinical decision-making of CCU nurses. J Family Med Prim Care. 2021;10(10):3650–6.
Xuexin Z. PAD class: a new attempt in university teaching reform. Fudan Educ Forum. 2014;12(5):5–10 [in Chinese].
Google Scholar
Zhai J, Dai L, Peng C, Dong B, Jia Y, Yang C. Application of the presentation-assimilation-discussion class in oral pathology teaching. J Dent Educ. 2022;86(1):4–11.
Colliver JA. Effectiveness of problem-based learning curricula: research and theory. Acad Med. 2000;75(3):259–66.
Bryant K, Aebersold ML, Jeffries PR, Kardong-Edgren S. Innovations in simulation: nursing leaders’ exchange of best practices. Clin Simul Nurs. 2020;41:33-40.e31.
Cicero MX, Whitfill T, Walsh B, Diaz MC, Arteaga G, Scherzer DJ, Goldberg S, Madhok M, Bowen A, Paesano G, et al. 60 seconds to survival: a multisite study of a screen-based simulation to improve prehospital providers disaster triage skills. AEM Educ Train. 2018;2(2):100–6.
Lee J, Lee H, Kim S, Choi M, Ko IS, Bae J, Kim SH. Debriefing methods and learning outcomes in simulation nursing education: a systematic review and meta-analysis. Nurse Educ Today. 2020;87:104345.
Peng G, Wang J, Chen M, Chen H, Bai S, Li J, Li Y, Cai J, Wang L. Yin Validity and reliability of the Chinese critical thinking disposition inventory Chin. J Nurs. 2004;39(09):7–10 [in Chinese].
Papathanasiou IV, Kleisiaris CF, Fradelos EC, Kakou K, Kourkouta L. Critical thinking: the development of an essential skill for nursing students. Acta Inform Med. 2014;22(4):283–6.
Australian Nursing and Midwifery Accreditation Council Midwife accreditation standards, 2014 ANMAC, Canberra. 2014. https://anmac.org.au/document/midwife-accreditation-standards-2014 .
Holdsworth C, Skinner EH, Delany CM. Using simulation pedagogy to teach clinical education skills: a randomized trial. Physiother Theory Pract. 2016;32(4):284–95.
Lapkin S, Fernandez R, Levett-Jones T, Bellchambers H. The effectiveness of using human patient simulation manikins in the teaching of clinical reasoning skills to undergraduate nursing students: a systematic review. JBI Libr Syst Rev. 2010;8(16):661–94.
Demirören M, Turan S, Öztuna D. Medical students’ self-efficacy in problem-based learning and its relationship with self-regulated learning. Med Educ Online. 2016;21:30049.
Spaulding WB, Neufeld VR. Regionalization of medical education at McMaster University. Br Med J. 1973;3(5871):95–8.
Rossler KL, Kimble LP. Capturing readiness to learn and collaboration as explored with an interprofessional simulation scenario: A mixed-methods research study. Nurse Educ Today. 2016;36:348–53.
Yang YL, Luo L, Qian Y, Yang F. Cultivation of undergraduates’ self-regulated learning ability in medical genetics based on PAD class. Yi Chuan. 2020;42(11):1133–9.
Felton A, Wright N. Simulation in mental health nurse education: the development, implementation and evaluation of an educational innovation. Nurse Educ Pract. 2017;26:46–52.
Atakro CA, Armah E, Menlah A, Garti I, Addo SB, Adatara P, Boni GS. Clinical placement experiences by undergraduate nursing students in selected teaching hospitals in Ghana. BMC Nurs. 2019;18:1.
Sun Y, Yin Y, Wang J, Ding Z, Wang D, Zhang Y, Zhang J, Wang Y. Critical thinking abilities among newly graduated nurses: a cross-sectional survey study in China. Nurs Open. 2023;10(3):1383–92.
Wangensteen S, Johansson IS, Björkström ME, Nordström G. Critical thinking dispositions among newly graduated nurses. J Adv Nurs. 2010;66(10):2170–81.
Salsali M, Tajvidi M, Ghiyasvandian S. Critical thinking dispositions of nursing students in Asian and non-Asian countries: a literature review. Glob J Health Sci. 2013;5(6):172–8.
Download references
Acknowledgements
Not applicable.
The study was supported by Sichuan University’s New Century Education and Teaching Reform Project (SCU9316).
Author information
Yuji Wang and Yijuan Peng are co-first authors.
Authors and Affiliations
Department of Nursing, West China Second University Hospital, Sichuan University/West China School of Nursing, Sichuan University/Key Laboratory of Birth Defects and Related Diseases of Women and Children (Sichuan University), No. 20 Third Section, Renmin South Road, Chengdu, Sichuan Province, 610041, China
Yuji Wang, Yijuan Peng & Yan Huang
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Yuji Wang, Yijuan Peng and Yan Huang. The first draft of the manuscript were written by Yuji Wang and Yijuan Peng, and all authors commented on previous versions of the manuscript.
Corresponding author
Correspondence to Yan Huang .
Ethics declarations
Ethics approval and consent to participate.
This study was supported by Sichuan University. And it was approved by the Ethics Review Committee of West China School of Nursing, Sichuan University. As it is a teaching research with no harm to samples, we only obtained oral informed consents from the participants including teachers and midwifery students and it was approved by the Ethics Review Committee of West China School of Nursing, Sichuan University(approval number 2021220). We comfirm that all methods were performed in accordance with the relevant guidelines and regulations in Ethics Approval and Consent to participate in Declarations.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Wang, Y., Peng, Y. & Huang, Y. The effect of “typical case discussion and scenario simulation” on the critical thinking of midwifery students: Evidence from China. BMC Med Educ 24 , 340 (2024). https://doi.org/10.1186/s12909-024-05127-5
Download citation
Received : 19 November 2022
Accepted : 02 February 2024
Published : 26 March 2024
DOI : https://doi.org/10.1186/s12909-024-05127-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical education
- Critical thinking
- Nurse midwives
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Researchers believe map construction is a useful tool that helps students to develop clinical reasoning skills through additional focus on logic, and it probably stimulates the use of thinking skills, such as analysis, interpretation, and evaluation, and finally promotes the development of CT skills .
1. Describe critical thinking (CT), clinical reasoning, and clinical judgment in your own words, based on the descriptions in this chapter. 2. Give at least three reasons why CT skills are essential for stu-dents and nurses. 3. Explain (or map) how the following terms are related to one another: critical thinking, clinical reasoning, clinical ...
Concept maps in nursing education: A historical literature review and research directions. Journal of Nursing Education, 55(11), 631-639. 10.3928/01484834-20161011-05 PMID: 27783817 > Link Google Scholar; Facione N. C., & Facione P. A. (1996). Externalizing the critical thinking in knowledge development and clinical judgment.
Teaching clinical reasoning is challenging, particularly in the time-pressured and complicated environment of the ICU. Clinical reasoning is a complex process in which one identifies and prioritizes pertinent clinical data to develop a hypothesis and a plan to confirm or refute that hypothesis. Clinical reasoning is related to and dependent on critical thinking skills, which are defined as one ...
Concept mapping was introduced as a way to support the nursing student to improve upon critical thinking and clinical reasoning and to identify relationships among the patient's health care problems. The present manuscript features the development and evaluation of the Concepto-Plan (C-P), an innovative, holistic care plan that moves away from ...
Background: Critical thinking, clinical reasoning, and clinical judgment are skills nurses use when caring for clients. However, teaching and evaluation of clinical judgment are challenging for faculty. Problem: Before revising a curriculum, it is necessary to map current practices and determine a framework for revisions. Approach: Faculty mapped critical thinking, clinical reasoning, and ...
Although some authors have argued that critical thinking and clinical reasoning cannot be taught, 35 there is no definitive evidence supporting this claim, ... Collaborative work among learners to create concept/mechanism maps mimics the way a clinical team solves problems. 51, 53, 54 Students are fully engaged, and the creation of the map ...
Clinical reasoning is related to and dependent on critical thinking skills, which are de ned as one's capacity to engage in higher cognitive skills such as analysis, synthesis, and. fi. self-re ection. This article reviews how an understanding of the cognitive psychological prin-. fl.
Concept mapping was introduced as a way to support the nursing student to improve upon critical thinking and clinical reasoning and to identify relationships among the patient's health care problems. The present manuscript features the development and evaluation of the Concepto-Plan (C-P), an innovative, holistic care plan that moves away from ...
Clinical reasoning is a multi-faceted and complex construct, the understanding of which has emerged from multiple fields outside of healthcare literature, primarily the psychological and behavioural sciences. ... Advanced practice: critical thinking and clinical reasoning Br J Nurs. 2021 May 13;30(9):526-532. doi: 10.12968/bjon.2021.30.9.526 ...
The ability to think critically uses reflection, induction, deduction, analysis, challenging assumptions, and evaluation of data and information to guide decisionmaking. 9, 14, 15 Critical reasoning is a process whereby knowledge and experience are applied in considering multiple possibilities to achieve the desired goals, 16 while considering ...
In the context of nursing, a concept map is a visual representation that illustrates the relationships between various nursing concepts and their connections within a particular patient's care or a broader nursing context. Concept mapping in nursing is a valuable tool for critical thinking, clinical reasoning, and effective communication ...
Critical thinking is a broad term used in nursing that includes "reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow.". [1] Certainly, there are many actions that nurses must complete during their shift, but nursing requires adaptation and flexibility to meet emerging patient needs.
Critical Thinking and Clinical Reasoning Map. Admit Date: 11/02/2022 Age: 75 Gender: F Allergies: Iodine Admit Dx: fever, bilateral pneumonia Code Status: full Activity: Diet: regular Vital Signs 0800 1200 1600 T 102 HR 104 RR 26 BP 149/ O2 93. In the event an assessment area below is not appropriate simply put NA in the box Neuro: A & O x 3
As detailed in the table, multiple themes surrounding the cognitive and meta-cognitive processes that underpin clinical reasoning have been identified. Central to these processes is the practice of critical thinking. Much like the definition of clinical reasoning, there is also diversity with regard to definitions and conceptualisation of critical thinking in the healthcare setting.
Clinical reasoning is a complex process in which one identifies and prioritizes pertinent clinical data to develop a hypothesis and a plan to confirm or refute that hypothesis. Clinical reasoning is related to and dependent on critical thinking skills, which are defined as one's capacity to engage in higher cognitive skills such as analysis ...
Critical Thinking and Clinical Reasoning Map. Select the Aggregate(s) for the focus of your Community Health topic: Homelessness. Subpopulation: Homeless. Obesity Subpopulation: Environmental Health Subpopulation: Occupation Health Subpopulation: War Veteran. Rural Subpopulation:
Critical Thinking and Clinical Reasoning. Nurses make decisions while providing patient care by using critical thinking and clinical reasoning. Critical thinking is a broad term used in nursing that includes "reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow." [1] Using critical thinking means that nurses take extra steps to maintain patient safety ...
Critical Thinking and Clinical Reasoning Map Admit Date: 12/27/2021 Age: 74 Gender: F Allergies: xicillin, penicillin, Clotrimazole, Simvastatin, Sulfa Antibiotics Admit Dx: Code Status: Full code Activity: light Diet: Carbohydrate controlled diet Vital Signs 0800 1200 1600 T 96. HR 90 RR 20 BP 166/ O2 97
Improving clinical reasoning techniques is the right way to facilitate decision-making from prognostic, diagnostic, and therapeutic points of view. However, the process to do that is to fill knowledge gaps by studying and growing experience and knowing some cognitive aspects to raise the awareness of thinking mechanisms to avoid cognitive ...
Clinical practice features high requirements for the clinical thinking ability of midwives, which refers to the process by which medical personnel analyze and integrate data with professional medical knowledge in the context of diagnosis and treatment as well as discover and solve problems through logical reasoning . Critical thinking is a ...
Critical Thinking and Clinical Reasoning Map Admit Date: 01/06/2023 Age: 17 months Gender: Male Allergies: No Known Allergies Admit Dx: Failure to thrive Code Status: Full code Activity: ambulate assist Diet: NG/Tube Feedings. Vital Signs 0800 1200 1600. T 36 36. HR 93 RR 27 BP 92/65 N/A O2 100
Name: Edylynn Quijano Clinical Reasoning Map Date 6/9/ Critical Thinking and Clinical Reasoning Map Admit Date: 5/30/22 Age: 56 Gender: Male Allergies: no known Admit Dx: STEMI Code Status: Full Resuscitation Activity: Independnet Diet: Cardiac Vital Signs 0800 1200 1600 T 35 C 35 C 35 C HR 76 75 75 RR 17 17 17 BP 91/47 110/74 113/ O2 94 94 94