You are here
Kidney cancer, table of contents, signs and symptoms, kidney disease and kidney cancer, complications, physical activity, alternative medicine, coping and support, questions for your doctor.
Kidney cancer is a disease that starts in the kidneys. It happens when healthy cells in one or both kidneys grow out of control and form a lump (called a tumor ).
Download the infographic:
- Your Kidneys and Cancer: Infographic
- Your Kidneys and Cancer - Infographic - En Español
In the early stages, most people don’t have signs or symptoms. Kidney cancer is usually found by chance during an abdominal (belly) imaging test for other complaints. As the tumor grows, you may have:
- Blood in the urine
- Pain in the lower back
- A lump in the lower back or side of the waist
- Unexplained weight loss, night sweats, fever, or fatigue
The reason why kidney cells change and become cancerous is not yet known.
We know that people are more likely to develop kidney cancer as they age. However, there are certain risk factors linked to the kidney cancer.

Kidney Cancer Animation Series
Watch these animated videos to learn more about kidney cancer.
Additional Languages:
A risk factor is anything that increases your chance of getting a disease. Some risk factors can be changed (smoking, as an example); but others cannot be changed (your gender or family history). Having a risk factor, or even several risk factors, does not mean you will get kidney cancer, but it may increase your risk.
- Risk factors for kidney cancer include:
- Being overweight (obese)
- High blood pressure
- Gender - about twice as many men as compared to women develop kidney cancer
- Being on dialysis treatment for advanced chronic kidney disease
- Family members with kidney cancer
- Long-term use of a pain-relieving drug called phenacetin
- Certain rare genetic diseases, such as von Hippel-Lindau disease, Birt Hogge Dube syndrome, and others
- History of long-term exposure to asbestos or cadmium
You may be able to lower your risk of developing kidney cancer by avoiding those risk factors that can be controlled. For example, stopping smoking may lower the risk, and controlling body weight and high blood pressure may help as well.
Studies show there is a link between kidney cancer and kidney disease .
Kidney cancer risk
Some studies show that people with kidney disease may have a higher risk for kidney cancer due to:
- Long-term dialysis: Some studies show that people on long-term dialysis have a 5-fold increased risk for kidney cancer. Experts believe this risk is due to kidney disease rather than dialysis.
- Immunosuppressant medicines: Some anti-rejection medicines that must be taken by kidney transplant recipients to prevent rejection can increase your risk for kidney cancer. However, taking your immunosuppressant medicine is important if you have a transplant. Without it, your body will reject your new kidney.
About one-third of the 300,000 kidney cancer survivors in the United States have or will develop kidney disease. [1] , [2]
Kidney disease risk
- Surgery to remove an entire kidney (radical nephrectomy) : Sometimes the entire kidney needs to be removed because the tumor is so large and most of the kidney has been destroyed. Your risk for kidney disease is higher if all (rather than part) of the kidney must be removed due to cancer. However, removing the whole kidney is often better for your survival if the tumor is large or centrally located. If a kidney tumor is small, it is better to undergo an operation to remove the tumor but not the entire kidney (partial nephrectomy). This approach decreases the chance of developing chronic kidney disease and associated problems with heart and blood vessel disease.
- Drugs to slow or stop cancer growth: Drugs that spread throughout the body to treat cancer cells, wherever they may be, are sometimes used to treat advanced kidney cancer. All cancer drugs have some side effects, but some can be toxic to the kidney (called nephrotoxic). The word “nephrotoxic” means it can damage your kidney function.
Remember, not everyone with kidney cancer will get kidney disease. Likewise, not everyone who has kidney disease or a transplant will get kidney cancer. Ask your doctor what you can do to lower your risk.
Sign up for a deeper dive into kidney cancer
Useful animated videos, information on treatments, and other helpful resources on kidney cancer.
General prevention tips
- Don’t smoke
- Maintain a healthy weight
- Find out if you’re exposed to certain toxins at work or at home (such as cadmium, asbestos, and trichloroethylene, which may increase kidney cancer risk)
Take care of your kidneys
People with kidney disease may be at increased risk for kidney cancer:
- Ask your healthcare provider about 2 simple tests to find your kidney score:
- A blood test for kidney function called GFR
- A urine test for kidney damage called ACR
- Avoid prolonged use of non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen
- Manage high blood pressure
- Manage your blood sugar if you have diabetes
Be aware of certain risk factors
- Family history of kidney cancer
- Certain diseases you may have been born with, such as von Hippel-Lindau disease
Renal cell carcinoma
Renal cell carcinoma (RCC) is the most common type of kidney cancer in adults. RCC usually starts in the lining of tiny tubes in the kidney called renal tubules. RCC often stays in the kidney, but it can spread to other parts of the body, most often the bones, lungs, or brain.
Clear cell renal cell carcinoma
Clear cell renal cell carcinoma, also known as ccRCC or conventional renal cell carcinoma , is a the most common form of kidney cancer. Clear cell renal cell carcinoma is named after how the tumor looks under the microscope. The cells in the tumor look clear, like bubbles.
In adults, ccRCC makes up about 80% of all renal cell carcinoma cases. ccRCC is more common in adults than children. Renal cell carcinoma makes up 2% to 6% of childhood and young adult kidney cancer cases."
Rare types of kidney cancer
Rare kidney cancers occur most frequently in children, teenagers, and young adults.
Papillary renal cell carcinoma (PRCC)
- 15% of all renal cell carcinomas
- Tumor(s) located in the kidney tubes
- Type 1 PRCC is more common and grows slowly
- Type 2 PRCC is more aggressive and grows more quickly
Translocation renal cell carcinoma (TRCC)
- Accounts for 1% to 5% of all renal cell carcinomas and 20% of childhood caces
- Tumor(s) located in the kidney
- In children, TRCC usually grows slowly often without any symptoms
- In adults, TRCC tends to be agressive and fast-growing
Benign (non-cancerous) kidney tumors
Benign, or noncancerous kidney tumors grow in size but do not spread to other parts of the body and are not usually life-threatening. Surgical removal is the most common treatment and most tumors do you come back.
Papillary renal adenoma
- The most common benign kidney tumor
- Tumors are small, slow growing, often without any symptoms
- Usually an incidental finding on an imaging test done for a different readon
- Tumors start in the cells of the kidney collecting ducts and tumors can grow in one of both kidneys
- The tumors can grow to a large size about the These tumours can grow quite large, starting at just over an inch (walnut) and growing up to 4 inches (grapefruit)
Angiomyolipoma
- Benign fatty tumors can also be be due to overgrowth of blood vessel and smooth muscle tissue cells
- Tumors are non-cancerous, but they can become very large and destroy surrounding tissue
- Tumors that are over an inch and a half can cause internal bleeding
Complications from kidney cancer may include:
- Kidney failure
- Local spread of the tumor with increasing pain
- Spread of the cancer to lung, liver, and bone
Your doctor will diagnose kidney cancer by reviewing your medical history and doing a physical exam, along with blood and urine tests.
Imaging tests:
- Computed tomography (CT) scans use x-rays to make a complete picture of the kidneys and abdomen (belly). They can be done with or without a contrast dye. Small amounts of radiation are used. The CT scan often shows if a tumor appears cancerous or if it has spread beyond the kidney.
- Magnetic resonance imaging (MRI) scans make a complete picture of the kidneys and abdomen, but without radiation. They can be done with or without a contrast dye called gadolinium that should be avoided in people on dialysis or with very low kidney function.
- Ultrasound uses sound waves to give a complete picture of the kidneys and abdomen without radiation. It may be useful in helping to decide if a mass in the kidneys is a fluid-filled cyst or a solid tumor. This test is done without contrast dye.
A biopsy can be used in special cases, but is typically not recommended. A biopsy requires a very small piece of the kidney to be removed with a needle and then tested for cancer cells.
Who can help
Discuss all your treatment options with your medical team.
Your medical team may include the following specialists:
- Urologist (a surgical doctor who treats the urinary system)
- Oncologist (a doctor who specializes in cancer)
- Radiation oncologist (a doctor who treats cancer with radiation)
- Nephrologist (kidney doctor)
- Oncology nurse
- Social worker
- Other healthcare professionals
Make medical and health-related appointments as soon as possible. You may need several opinions about what treatment choices are best for you.
Once kidney cancer is found, your doctor will run tests to find out if the cancer has spread within the kidney or to other parts of the body. This process is called staging. It is important to know the stage before making a treatment plan. The higher the stage, the more serious the cancer.
The most common treatment for kidney cancer is with surgery to remove all or part of the kidney. However, your treatment will depend on the stage of your disease, your general health, your age, and other factors.
Surgery is most common treatment for kidney cancer—most people with early stage cancer (stages 1, 2, and 3) can be cured with surgery.
Partial nephrectomy
In a partial nephrectomy, the tumor or the part of the kidney with the tumor is removed to leave behind as much of the kidney as possible
Radical nephrectomy
In a radical nephrectomy, the entire kidney is removed. If needed, the surrounding tissues and lymph nodes may also be removed.
Surgical approaches
Ask your doctor about the surgical approach that is best for you:
- Open (traditional surgery with a long incision)
- Laparoscopic (surgery done with a video camera and thin instruments for smaller incisions)
- Robotic (laparoscopic surgery done with the help of a robot)
Nonsurgical options
Thermal ablation
Thermal ablation kills the tumor by burning or freezing and is most often used for small tumors in people who are not good candidates for nephrectomy surgery
Active surveillance
Active surveillance is used if a small tumor is less than 4 centimeters (1.5 inches)
Chemotherapy and radiation
Forms of chemotherapy and radiation used in other forms of cancer are not usually effective treatments for most forms of kidney cancer
Advanced or recurrent kidney cancer treatment
For people with advanced kidney cancer that has spread to other parts of the body, treatment with a drug may be recommended along with surgery, or instead of surgery. Some of these drugs are given to you as a pill that you take by mouth; others are given as an injection. Much progress has been made in recent years, and people with advanced kidney cancer are living much longer than ten years ago.
- Monoclonal antibodies attack a specific part of cancer cells
- Checkpoint inhibitors help the immune system recognize and attack cancer cells
- Vaccines give an overall boost to the immune system
- Anti-angiogenic therapies reduce the blood supply to a tumor to slow or stop its growth
- Targeted therapies directly inhibit the growth of the cancer
It is important to eat well for good nutrition during cancer treatment. Good nutrition means getting enough calories and nutrients to help prevent weight loss and regain strength. Patients who eat well often feel better and have more energy.
Some people find it hard to eat well during treatment. This is because their treatment may cause them to lose their appetite or have side effects like nausea, vomiting or mouth sores, which can make eating difficult. For some people, food tastes different. Others may not feel like eating because they feel uncomfortable or tired.
Complementary and alternative medicine (CAM) is the term for medical products and practices that are not part of standard medical care. Please discuss with your healthcare team any CAM products you are using to make sure they won't affect your treatment plan. These products are not tested for safety, and many can be harmful.
People with cancer may use CAM to:
- Help cope with the side effects of cancer treatments, such as nausea, pain, and fatigue
- Comfort themselves and ease the worries of cancer treatment and related stress
- Feel that they are doing something to help with their own care
- Try to treat or cure their cancer
Mind & Body Therapies
These combine mental focus, breathing, and body movements to help relax the body and mind. Some examples are:
- Meditation: Focused breathing or repetition of words or phrases to quiet the mind
- Biofeedback: Using simple machines, the patient learns how to affect certain body functions that are normally out of one's awareness (such as heart rate)
- Hypnosis: A state of relaxed and focused attention in which a person concentrates on a certain feeling, idea, or suggestion to aid in healing
- Yoga: Systems of stretches and poses, with special attention given to breathing
- Tai Chi: Involves slow, gentle movements with a focus on the breath and concentration
- Imagery: Imagining scenes, pictures, or experiences to help the body heal
- Creative outlets: Interests such as art, music, or dance
Biologically Based Practices
This type of CAM uses things found in nature. Some examples are:
- Vitamins and dietary supplements
- Botanicals, which are plants or parts of plants such as cannibis
- Herbs and spices such as turmeric or cinnamon
- Special foods or diets
Manipulative and Body-Based Practices
These are based on working with one or more parts of the body. Some examples are:
- Massage: The soft tissues of the body are kneaded, rubbed, tapped, and stroked
- Chiropractic therapy: A type of manipulation of the spine, joints, and skeletal system
- Reflexology: Using pressure points in the hands or feet to affect other parts of the body
Biofield Therapy
Biofield therapy, sometimes called energy medicine, involves the belief that the body has energy fields that can be used for healing and wellness. Therapists use pressure or move the body by placing their hands in or through these fields. Some examples are:
- Reiki: Balancing energy either from a distance or by placing hands on or near the patient
- Therapeutic touch: Moving hands over energy fields of the body
Whole Medical Systems
These are healing systems and beliefs that have evolved over time in different cultures and parts of the world. Some examples are:
- Ayurvedic medicine: A system from India in which the goal is to cleanse the body and restore balance to the body, mind, and spirit
- Acupuncture is a common practice in Chinese medicine that involves stimulating certain points on the body to promote health, or to lessen disease symptoms and treatment side effects
- Homeopathy: Uses very small doses of substances to trigger the body to heal itself
- Naturopathic medicine: Uses various methods that help the body naturally heal itself. An example would be herbal treatment
Living with a serious illness is not easy. People with cancer and those who care about them face many problems and challenges. Coping with these problems often is easier when you have helpful information and support from friends and relatives. It also helps many people to meet in support groups to talk about their concerns with others who have or have had cancer. In support groups, patients share what they have learned about dealing with cancer and the effects of treatment.
Keep in mind that each person is different, and the same treatments and ways of dealing with cancer may not work for everyone. Always discuss the advice of friends and family with members of your healthcare team. Many cancer treatment centers have patient navigators who can help you:
- Know the right questions to ask your doctor and healthcare team
- Find more information about your condition and how to decide on the best treatment
- Make appointments and get the resources you need.
This support can reduce the stress of dealing with your care. Speaking with your doctor, healthcare team, and patient navigator about any concerns or questions is essential to getting the right information you need.
Find more information from the following organizations and programs.
National Cancer Institute
800.4.CANCER (800.422.6237) or www.cancer.gov
National Kidney and Urologic Disease Information Clearinghouse (NKUDIC) , a service of the National Institute of Diabetes, Digestive and Kidney Diseases. 800.891.5390 or www.niddk.nih.gov
Kidney Cancer Association www.kidneycancer.org
American Cancer Society 800.227.2345 or www.cancer.org
You and your healthcare provider need to work together. Here are some questions to start the conversation.
- Do I have kidney cancer?
- Has my cancer spread beyond my kidneys?
- Can my kidney cancer be cured?
- What are my treatment options?
- How long will treatment last?
- Are there any risks or side effects associated with my treatment?
- What will my recovery be like?
- How long will it take for me to recover from treatment?
- What are the chances of cancer coming back?
- Should I also see a nephrologist (kidney doctor)?
- Will you be partnering with a nephrologist about my care?
- Should I get a second opinion?
- How much experience do you have treating this kind of cancer?
- Are there any clinical trials I should think about?
[1] What are the Key Statistics about Kidney Cancer. American Cancer Society. 2016; http://www.cancer.org/cancer/kidneycancer/detailedguide/kidney-cancer-adult-key-statistics . Accessed October 20, 2016.
[2] Chang A, Finelli A, Berns JS, Rosner M. Chronic kidney disease in patients with renal cell carcinoma. Adv Chronic Kidney Dis. Jan 2014;21(1):91-95.
Kidney Cancer Infographic
Save this content:
Is this content helpful?
Back to top:
Kidney Cancer: An Overview of Current Therapeutic Approaches
Affiliations.
- 1 Department of Oncology, Sidney Kimmel Comprehensive Cancer Center, Johns Hopkins University School of Medicine, Baltimore, MD 21287, USA; Department of Pathology, Johns Hopkins University School of Medicine, Baltimore, MD 21287, USA; Columbia Center for Translational Immunology, Columbia University Medical Center, 177 Fort Washington Avenue, Suite 6GN-435, New York, NY 10032, USA.
- 2 Columbia Center for Translational Immunology, Columbia University Medical Center, 177 Fort Washington Avenue, Suite 6GN-435, New York, NY 10032, USA; Department of Urology, Herbert Irving Comprehensive Cancer Center, Columbia University Medical Center, 177 Fort Washington Avenue, Suite 6GN-435, New York, NY 10032, USA; Division of Hematology and Oncology, Herbert Irving Comprehensive Cancer Center, Columbia University Medical Center, 177 Fort Washington Avenue, Suite 6GN-435, New York, NY 10032, USA. Electronic address: [email protected].
- PMID: 33008493
- DOI: 10.1016/j.ucl.2020.07.009
The management of metastatic renal cell carcinoma (RCC) has evolved rapidly in recent years with several immunotherapy-based combinations of strategies approved as first-line therapies. Targeted strategies, including systemic antiangiogenesis agents and immune checkpoint blockade, form the basis of a therapeutic approach. With rising rates of recurrence after first-line treatment, it is increasingly important to not only adopt a personalized treatment plan with minimal adverse events but also develop predictive biomarkers for response. This review discusses currently available first-line and second-line therapies in RCC and their pivotal data, with specific focus on ongoing clinical trials in the adjuvant setting, including those involving novel agents.
Keywords: Atezolizumab; Bevacizumab; Clear cell carcinoma; First-line immunotherapy; Kidney cancer; Pembrolizumab; Tyrosine kinase inhibitors.
Copyright © 2020 Elsevier Inc. All rights reserved.
Publication types
- Biological Products / therapeutic use*
- Carcinoma, Renal Cell / drug therapy*
- Carcinoma, Renal Cell / mortality
- Carcinoma, Renal Cell / pathology
- Carcinoma, Renal Cell / surgery
- Clinical Trials, Phase II as Topic
- Combined Modality Therapy
- Drug Therapy, Combination
- Immunotherapy / methods*
- Kidney Neoplasms / drug therapy*
- Kidney Neoplasms / mortality
- Kidney Neoplasms / pathology
- Neoplasm Invasiveness / pathology
- Neoplasm Staging
- Nephrectomy / methods
- Survival Analysis
- Treatment Outcome
- United States
- Biological Products
- Patient Care & Health Information
- Diseases & Conditions
- Kidney cancer
- Kidney cancer FAQs
Urologic oncologist Bradley Leibovich, M.D., answers the most frequently asked questions about kidney cancer.
I'm Dr. Brad Leibovich, a urologic oncologist at Mayo Clinic, and I'm here to answer some questions patients may have about kidney cancer.
Patients diagnosed with kidney cancer often want to know what could they have done differently to prevent this from happening in the first place. In most cases, kidney cancer is completely unrelated to how you've lived your life. And there's really nothing you could have done differently to have prevented this.
Prognosis for kidney cancer depends upon the stage at which the kidney cancer is discovered. For patients with early stage disease, the prognosis is excellent and the expectation is typically that somebody will be cured of their kidney cancer. For later stage disease, thankfully, we have many new treatments. And even if it's not possible to cure a patient, the expectation is we will significantly extend their life.
Patients that have been diagnosed with kidney cancer often want to know if it's necessary to remove the entire kidney. In some cases, the kidney can be preserved and only the tumor needs to be removed. In other cases, it's necessary to remove the entire kidney. Thankfully, most patients have a second kidney and have good enough kidney function with just one kidney, that this is not a problem.
Since most patients have relatively normal kidney function after having a kidney removed, in the majority of circumstances, you do not have to change your lifestyle. Most important is that you have a healthy lifestyle overall. Get good sleep, regular exercise, and have a healthy balanced diet. If you do need to change something about your lifestyle, your doctor will tell you.
Many patients want to know if they need to alter their diet after treatment for kidney cancer. In the majority of circumstances, people have normal enough kidney function that no special diet is required, and people can eat and drink however they did previously.
In my opinion, being the best partner to your medical team means learning as much as you can about your diagnosis and about your options. This will empower you to make the best decisions that are right for you. Never hesitate to ask your medical team any questions or inform them of any concerns you may have. Being informed makes all the difference. Thank you for your time. We wish you well.
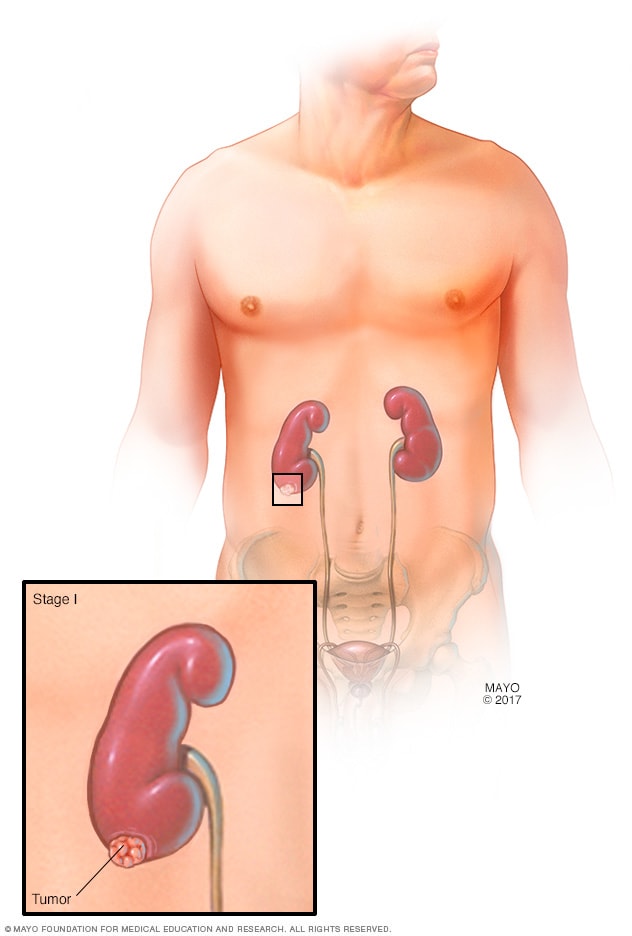
- Stage I kidney tumor
The tumor can be up to 2 3/4 inches (7 centimeters) in diameter. The cancer is only in one kidney and completely contained within it.
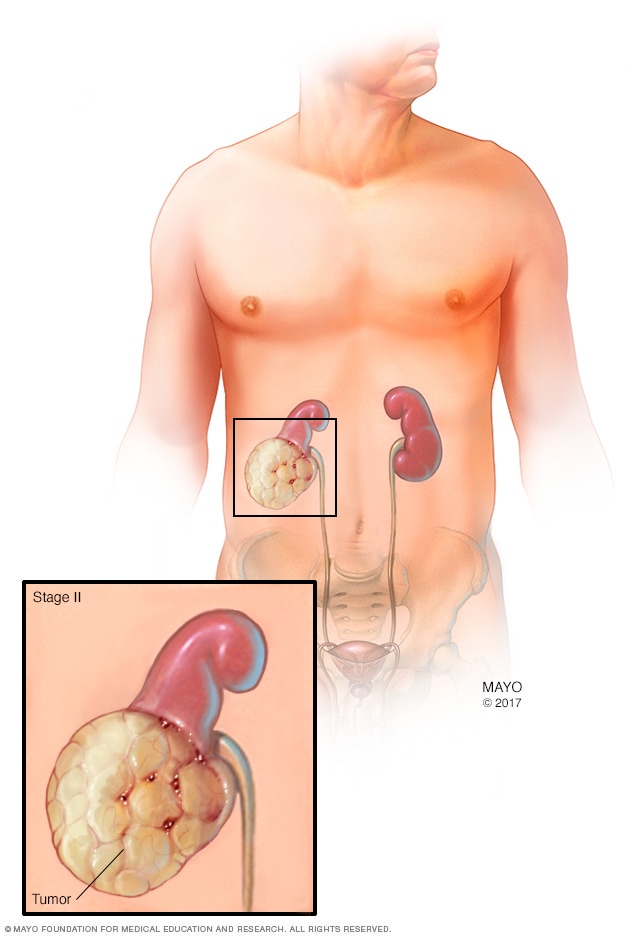
- Stage II kidney tumor
The tumor is larger than 2 3/4 inches (7 centimeters) in diameter, but it's still confined to the kidney.
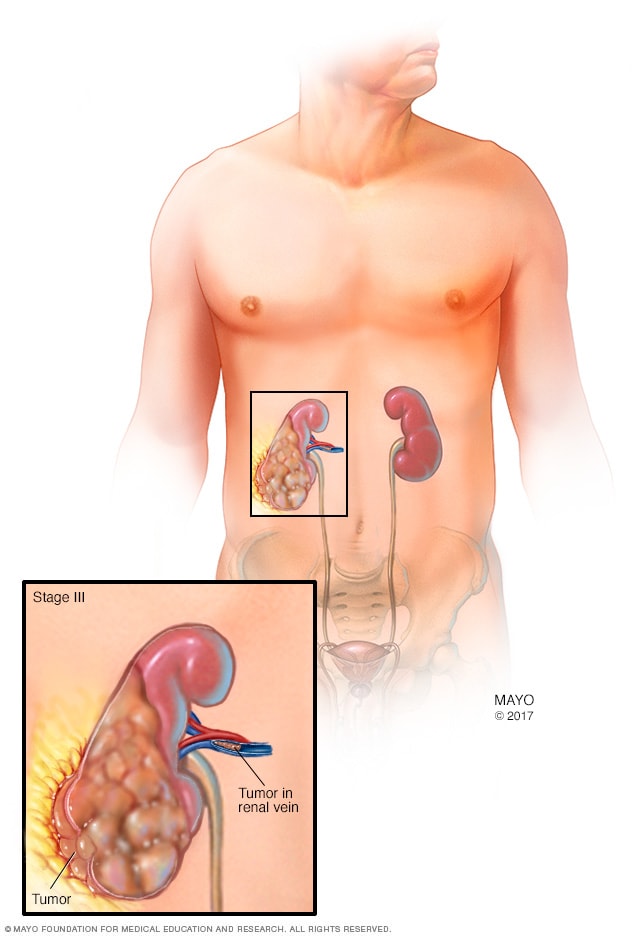
- Stage III kidney tumor
The tumor extends beyond the kidney to the surrounding tissue and may also have spread to nearby lymph nodes.
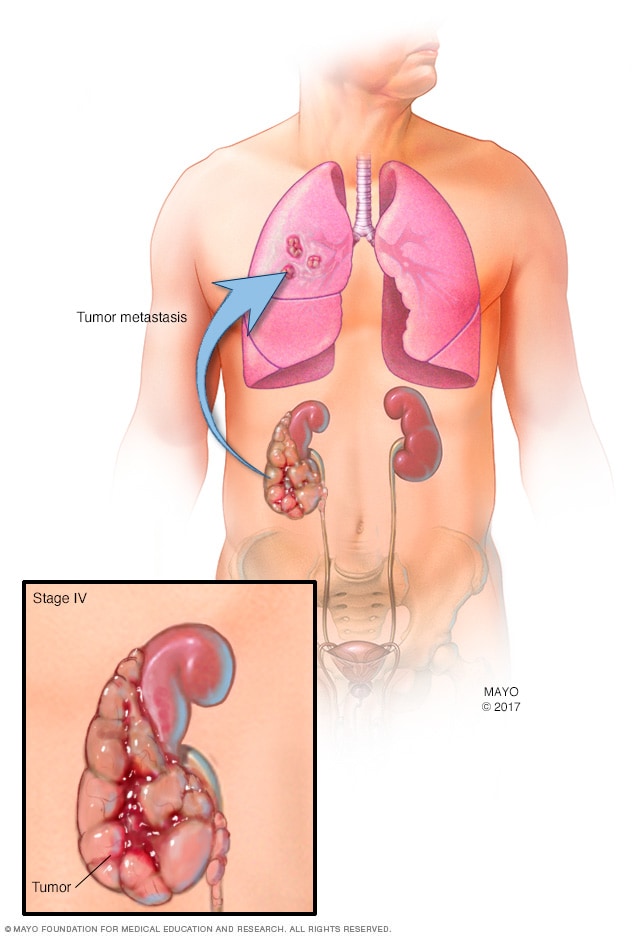
- Stage IV kidney tumor
Cancer spreads outside the kidney, to multiple lymph nodes or to distant parts of the body, such as the bones, liver or lungs.
Tests and procedures used to diagnose kidney cancer include:
- Blood and urine tests. Tests of your blood and your urine may give your doctor clues about what's causing your signs and symptoms.
- Imaging tests. Imaging tests allow your doctor to visualize a kidney tumor or abnormality. Imaging tests might include ultrasound, X-ray, CT or MRI .
- Removing a sample of kidney tissue (biopsy). In some situations, your doctor may recommend a procedure to remove a small sample of cells (biopsy) from a suspicious area of your kidney. The sample is tested in a lab to look for signs of cancer. This procedure isn't always needed.
Kidney cancer staging
Once your doctor identifies a kidney lesion that might be kidney cancer, the next step is to determine the extent (stage) of the cancer. Staging tests for kidney cancer may include additional CT scans or other imaging tests your doctor feels are appropriate.
The stages of kidney cancer are indicated by Roman numerals that range from I to IV, with the lowest stages indicating cancer that is confined to the kidney. By stage IV, the cancer is considered advanced and may have spread to the lymph nodes or to other areas of the body.
More Information
Kidney cancer care at Mayo Clinic
- Computerized tomography (CT) urogram
Kidney cancer treatment usually begins with surgery to remove the cancer. For cancers confined to the kidney, this may be the only treatment needed. If the cancer has spread beyond the kidney, additional treatments may be recommended.
Together, you and your treatment team can discuss your kidney cancer treatment options. The best approach for you may depend on a number of factors, including your general health, the kind of kidney cancer you have, whether the cancer has spread and your preferences for treatment.
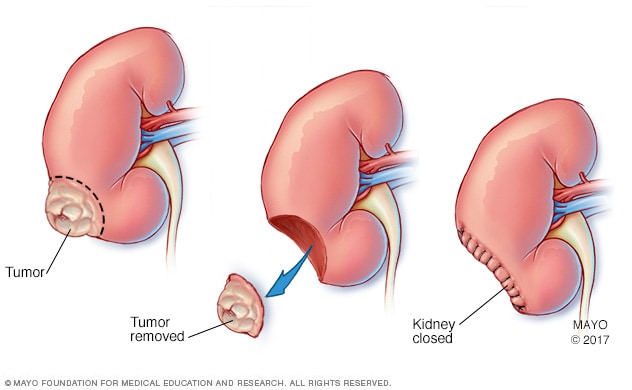
Partial nephrectomy
During a partial nephrectomy, only the cancerous tumor or diseased tissue is removed (center), leaving in place as much healthy kidney tissue as possible. Partial nephrectomy is also called kidney-sparing surgery.
For most kidney cancers, surgery is the initial treatment. The goal of surgery is to remove the cancer while preserving normal kidney function, when possible. Operations used to treat kidney cancer include:
Removing the affected kidney (nephrectomy). A complete (radical) nephrectomy involves removing the entire kidney, a border of healthy tissue and occasionally additional nearby tissues such as the lymph nodes, adrenal gland or other structures.
The surgeon may perform a nephrectomy through a single incision in the abdomen or side (open nephrectomy) or through a series of small incisions in the abdomen (laparoscopic or robotic-assisted laparoscopic nephrectomy).
Removing the tumor from the kidney (partial nephrectomy). Also called kidney-sparing or nephron-sparing surgery, the surgeon removes the cancer and a small margin of healthy tissue that surrounds it rather than the entire kidney. It can be done as an open procedure, or laparoscopically or with robotic assistance.
Kidney-sparing surgery is a common treatment for small kidney cancers and it may be an option if you have only one kidney. When possible, kidney-sparing surgery is generally preferred over a complete nephrectomy to preserve kidney function and reduce the risk of later complications, such as kidney disease and the need for dialysis.
The type of surgery your doctor recommends will be based on your cancer and its stage, as well as your overall health.
Nonsurgical treatments
Small kidney cancers are sometimes destroyed using nonsurgical treatments, such as heat and cold. These procedures may be an option in certain situations, such as in people with other health problems that make surgery risky.
Options may include:
- Treatment to freeze cancer cells (cryoablation). During cryoablation, a special hollow needle is inserted through your skin and into the kidney tumor using ultrasound or other image guidance. Cold gas in the needle is used to freeze the cancer cells.
- Treatment to heat cancer cells (radiofrequency ablation). During radiofrequency ablation, a special probe is inserted through your skin and into the kidney tumor using ultrasound or other imaging to guide placement of the probe. An electrical current is run through the needle and into the cancer cells, causing the cells to heat up or burn.
Treatments for advanced and recurrent kidney cancer
Kidney cancer that comes back after treatment and kidney cancer that spreads to other parts of the body may not be curable. Treatments may help control the cancer and keep you comfortable. In these situations, treatments may include:
- Surgery to remove as much of the kidney cancer as possible. If the cancer can't be removed completely during an operation, surgeons may work to remove as much of the cancer as possible. Surgery may also be used to remove cancer that has spread to another area of the body.
- Targeted therapy. Targeted drug treatments focus on specific abnormalities present within cancer cells. By blocking these abnormalities, targeted drug treatments can cause cancer cells to die. Your doctor may recommend testing your cancer cells to see which targeted drugs may be most likely to be effective.
- Immunotherapy. Immunotherapy uses your immune system to fight cancer. Your body's disease-fighting immune system may not attack your cancer because the cancer cells produce proteins that help them hide from the immune system cells. Immunotherapy works by interfering with that process.
- Radiation therapy. Radiation therapy uses high-powered energy beams from sources such as X-rays and protons to kill cancer cells. Radiation therapy is sometimes used to control or reduce symptoms of kidney cancer that has spread to other areas of the body, such as the bones and brain.
- Clinical trials. Clinical trials are research studies that give you a chance to try the latest innovations in kidney cancer treatment. Some clinical trials assess the safety and effectiveness of potential treatments. Other clinical trials try to find new ways to prevent or detect disease. If you're interested in trying a clinical trial, discuss the benefits and risks with your doctor.
- Ablation therapy
- Biological therapy for cancer
- Nephrectomy (kidney removal)
- Radiation therapy
- Radiofrequency ablation for cancer
- Grateful patient talks about his Mayo Clinic experience
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Alternative medicine
No alternative medicine therapies have been proved to cure kidney cancer. But some integrative treatments can be combined with standard medical therapies to help you cope with side effects of cancer and its treatment, such as distress.
People with cancer often experience distress. If you're distressed, you may have difficulty sleeping and find yourself constantly thinking about your cancer. You may feel angry or sad.
Discuss your feelings with your doctor. Specialists can help you sort through your feelings and help you devise strategies for coping. In some cases, medications may help.
Integrative medicine treatments may also help you feel better, including:
- Art therapy
- Massage therapy
- Music therapy
- Relaxation exercises
- Spirituality
Talk with your doctor if you're interested in these treatment options.
Coping and support
Each person copes with a cancer diagnosis in his or her own way. Once the fear that comes with a diagnosis begins to lessen, you can find ways to help you cope with the daily challenges of cancer treatment and recovery. These coping strategies may help:
- Learn enough about kidney cancer to feel comfortable making treatment decisions. Ask your doctor for details of your diagnosis, such as what type of cancer you have and the stage. This information can help you learn about the treatment options. Good sources of information include the National Cancer Institute and the American Cancer Society.
- Take care of yourself. Take care of yourself during cancer treatment. Eat a healthy diet full of fruits and vegetables, be physically active when you feel up to it, and get enough sleep so that you wake feeling rested each day.
- Take time for yourself. Set aside time for yourself each day. Time spent reading, relaxing or listening to music can help you relieve stress. Write your feelings down in a journal.
- Gather a support network. Your friends and family are concerned about your health, so let them help you when they offer. Let them take care of everyday tasks — running errands, preparing meals and providing transportation — so that you can focus on your recovery. Talking about your feelings with close friends and family also can help you relieve stress and tension.
- Get mental health counseling if needed. If you feel overwhelmed, depressed or so anxious that it's difficult to function, consider getting mental health counseling. Talk with your doctor or someone else from your health care team about getting a referral to a mental health professional, such as a certified social worker, psychologist or psychiatrist.
Preparing for your appointment
Start by making an appointment with your primary care doctor if you have signs or symptoms that worry you. If your doctor suspects you may have kidney cancer, you may be referred to a doctor who specializes in urinary tract diseases and conditions (urologist) or to a doctor who treats cancer (oncologist).
Consider taking a family member or friend along. Sometimes it can be hard to remember all the information provided during an appointment. Someone who accompanies you may remember something that you missed or forgot.
What you can do
At the time you make the appointment, ask if there's anything you need to do in advance, such as restrict your diet. Then make a list of:
- Symptoms you're experiencing, including any that may seem unrelated to the reason for your appointment
- Key personal information, including any major stresses or recent life changes
- All medications (prescription and over-the-counter), vitamins, herbs or other supplements that you're taking
- Questions to ask your doctor
List your questions from most to least important in case time runs out. Some basic questions to ask your doctor include:
- Do I have kidney cancer?
- If so, has my cancer spread beyond my kidney?
- Will I need more tests?
- What are my treatment options?
- What are the potential side effects of each treatment?
- Can my kidney cancer be cured?
- How will cancer treatment affect my daily life?
- Is there one treatment option you feel is best for me?
- I have these other health conditions. How can I best manage them together?
- Should I see a specialist?
- Are there brochures or other printed material that I can have? What websites do you recommend?
Don't hesitate to ask additional questions that may occur to you during your appointment.
What to expect from your doctor
Your doctor is likely to ask you a number of questions. Be ready to answer them so that you'll have time to cover any points you want to focus on. Your doctor may ask:
- When did you first begin experiencing symptoms?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?

- Kidney cancer. National Comprehensive Cancer Network. https://www.nccn.org/professionals/physician_gls/default.aspx. Accessed May 8, 2020.
- Partin AW, et al., eds. Malignant renal tumors. In: Campbell-Walsh-Wein Urology. 12th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 8, 2020.
- Niederhuber JE, et al., eds. Cancer of the kidney. In: Abeloff's Clinical Oncology. 6th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed May 8, 2020.
- Renal cell cancer treatment (PDQ). National Cancer Institute. https://www.cancer.gov/types/kidney/patient/kidney-treatment-pdq. Accessed May 8, 2020.
- Distress management. National Comprehensive Cancer Network. https://www.nccn.org/professionals/physician_gls/default.aspx. Accessed May 8, 2020.
- Alt AL, et al. Survival after complete surgical resection of multiple metastases from renal cell carcinoma. Cancer. 2011; doi:10.1002/cncr.25836.
- Lyon TD, et al. Complete surgical metastasectomy of renal cell carcinoma in the post-cytokine era. The Journal of Urology. 2020; doi:10.1097/JU.0000000000000488.
- Dong H, et al. B7-H1, a third member of the B7 family, co-stimulates T-cell proliferation and interleukin-10 secretion. Nature Medicine. 1999;5:1365.
- Peyronnet B, et al. Impact of hospital volume and surgeon volume on robot-assisted partial nephrectomy outcomes: A multicenter study. BJU International. 2018; doi:10.1111/bju.14175.
- Hsu RCJ, et al. Impact of hospital nephrectomy volume on intermediate- to long-term survival in renal cell carcinoma. BJU International. 2020; doi:10.1111/bju.14848.
- NCCN member institutions. National Comprehensive Cancer Network. https://www.nccn.org/members/network.aspx. Accessed May 20, 2020.
- Locations. Children's Oncology Group. https://www.childrensoncologygroup.org/index.php/locations. Accessed May 20, 2020.
- Kidney Cancer
- What is kidney cancer? An expert explains
Associated Procedures
News from mayo clinic.
- Mayo Clinic Minute: How is kidney cancer treated? March 20, 2023, 02:27 p.m. CDT
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Mayo Clinic Comprehensive Cancer Center
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Mayo Clinic in Rochester, Minnesota, Mayo Clinic in Jacksonville, Florida, and Mayo Clinic in Phoenix/Scottsdale, Arizona, have been recognized among the top Urology and Cancer hospitals in the nation for 2023-2024 by U.S. News & World Report.
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
Renal cancer articles from across Nature Portfolio
Renal cancer refers to all malignancies that occur within the kidney. Subtypes include renal cell carcinoma and Wilms tumours.
Related Subjects
- Renal cell carcinoma
- Wilms tumour
Latest Research and Reviews

Investigating the causal associations between metabolic biomarkers and the risk of kidney cancer
A multiple Mendelian randomization study emphasizes the central role of lactate in kidney tumorigenesis and provides novel insights into possible mechanism how phospholipids could affect kidney tumorigenesis.
- Yaxiong Tang
Targeting STING elicits GSDMD-dependent pyroptosis and boosts anti-tumor immunity in renal cell carcinoma
- Shengpan Wu
- Baojun Wang
The role of RNA-modifying proteins in renal cell carcinoma
- Muna A. Alhammadi
- Khuloud Bajbouj
- Rifat Hamoudi
Prognostic factors of renal cell cancer in elderly patients: a population-based cohort study
- Heini Pajunen
- Thea Veitonmäki
- Teemu Murtola

The integrate profiling of single-cell and spatial transcriptome RNA-seq reveals tumor heterogeneity, therapeutic targets, and prognostic subtypes in ccRCC
- Yanlong Zhang
- Xuefeng Huang
Frontier knowledge and future directions of programmed cell death in clear cell renal cell carcinoma
News and Comment
Pericyte–stem cell crosstalk in ccrcc.
- Susan J. Allison
First-line pembrolizumab plus lenvatinib is effective in non-clear-cell RCC
- Diana Romero
A triple dose of optimism: an initial foray into triplet therapy in metastatic renal cell carcinoma
COSMIC-313 combines all of the approved drugs against actionable targets in renal cell carcinoma into one triplet regimen. Although this approach has greater clinical efficacy than one of the standard-of-care doublet therapies, toxicities can limit adequate drug administration and, thus, we argue that this regimen should not yet be adopted. We also discuss ongoing investigations of other triplet regimens.
- Kathryn E. Beckermann
- Brian I. Rini

PBRM1 loss redirects chromatin remodelling complex to recruit oncogenic factors
The loss of the polybromo-1 (PBRM1) subunit in a class of SWI/SNF chromatin remodelling complexes in clear cell renal cell carcinoma redirects the deficient complexes to aberrant enhancer regions. The catalytic subunit SMARCA4 of the PBRM1-deficient complexes recruits the nuclear factor-κB transcription factor to drive pro-tumorigenic programs.
New combination therapy for advanced-stage RCC
- Peter Sidaway
Patient preferences in the treatment of genitourinary cancers
Several newly approved therapies have substantially altered the treatment paradigm for multiple genitourinary cancers. Considering the existence of numerous possible treatment approaches, understanding which treatment attributes are most valued by each patient is crucial to physicians to recommend a cancer-directed treatment.
- David J. Benjamin
- Arash Rezazadeh Kalebasty
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Shop Online

- Common cancer symptoms
- Facts and figures
- Early detection and screening
- Check for signs of skin cancer
- Diet and exercise
- Smoking and tobacco
- Family history and cancer
- Environmental causes
- Workplace cancer
- Adenocarcinoma
- Anal cancer
- Brain cancer
- Breast cancer
- Breast cancer in men
- Bladder cancer
- Bone cancer
- Bowel cancer
- Cancer of unknown primary
- Cervical cancer
- Children, teens, and young adult cancers
- Head and neck cancers
- Hodgkin lymphoma
Kidney cancer
- Liver cancer
- Lung cancer
- Mesothelioma
- Mouth cancer
- Non-Hodgkin lymphoma
- Non-melanoma skin cancer
- Oesophageal cancer
- Ovarian cancer
- Pancreatic cancer
- Prostate cancer
- Rare cancers
- Secondary bone cancer
- Skin cancer
- Stomach cancer
- Testicular cancer
- Throat cancer
- Thyroid cancer
- Uterine cancer
- Vaginal cancer
- Vulvar cancer
- Tests and scans
- Coping with a cancer diagnosis
- Your guides to best cancer care
- Telling friends and family
- Find a specialist
- Questions to ask your doctor
- Hospital visits for cancer patients and carers
- Telehealth for cancer patients and carers
- Living with cancer
- After cancer treatment
- Chemotherapy

Radiation therapy (radiotherapy)
- Complementary therapies
- Hormone therapy
Immunotherapy
- Clinical trials
Palliative care
Targeted therapy.
- Advanced cancer treatment
- Breast prostheses and reconstruction
- Changes in thinking and memory
- Mouth health
- Neutropenia
- Peripheral neuropathy
- Sexuality and intimacy
- Taste and smell changes
- Downloadable resources
- Cancer Council 13 11 20
- State based service finder
- Support groups
- Transport services
- Wig service
- Cancer support and information centres
- Children, adolescents and young adults
- Cancer and COVID-19
- Information for Aboriginal and Torres Strait Islander people
- Multilingual resources
- Cancer, work and you
- Practical and financial assistance
- Workshops and forums
- Ostomy Service
- Cancer Nurses
- Cancer Council Online Community
- Trusted resources
- Personal cancer stories
- One time donation
- Regular giving
- In memoriam
- In celebration
- Where your money goes
- Workplace Giving
- Upcoming Events and Programs
- Australia's Biggest Morning Tea
- Daffodil Day Appeal
- Relay For Life
- Girls' Night In
- The March Charge
- The Longest Day
- Ponytail Project
- Community fundraising
- Gala Events
- Entertainment books
- Donation tins
- Healthy fundraising
- Men’s Health Pitstop
- Wording for your will
- Shop online
- Find a stockist
- Clothes4Cancer Op Shop
- Clinical Practice Guidelines
- Clinical Guidelines Network
- National Secondary Students' Diet and Activity (NaSSDA) survey
- Research Opportunities, Grants and Scholarships
- Optimal Care Pathways
- Patient resources
- Screening information for GPs
- Informed financial consent
- Inequalities in cancer outcomes
- Caring for Aboriginal and Torres Strait Islander people
- Warning signs of cancer in children
- Online learning
- Australian Cancer Atlas
- Cancer Forum
- Diverse Languages and Cultures
- Conferences and events
- Looking Ahead
- Prevention policy
- Early detection policy
- National cancer care policy
- Clinical practice policy
- Supportive care policy
- Position statements
- Submissions to government
- Consumer engagement
- Media releases
- Our spokespeople
- Media contacts
- Cancer Council Australia
- Cancer Council ACT
- Cancer Council NSW
- Cancer Council NT
- Cancer Council Queensland
- Cancer Council SA
- Cancer Council Tasmania
- Cancer Council Victoria
- Cancer Council WA
- National committees
- Affiliations
- Corporate partnerships
- Endorsed Sun Protection Brands
Types of Cancer
What is kidney cancer.
Kidney cancer is cancer that starts in the cells of the kidney. The most common type of kidney cancer is renal cell carcinoma (RCC), accounting for about 90% of all cases. Usually only one kidney is affected, but in rare cases the cancer may develop in both kidneys.
Other less common types include:
- Urothelial carcinoma (also called transitional cell carcinoma) which can begin in the ureter or renal pelvis where the kidney and ureter meet. It is generally treated like bladder cancer .
- Wilms tumour, which is most common in younger children although it is still rare.
It is estimated that more than 4,600 people were diagnosed with kidney cancer in 2023. The average age at diagnosis is 65 years old.
Kidney cancer is the seventh most commonly diagnosed cancer in Australia, and it is estimated that one in 65 people will be diagnosed by the time they are 85.
Kidney cancer signs and symptoms
In its early stages, kidney cancer often does not produce any symptoms.
Symptoms may include:
blood in the urine or passing urine frequently or during the night, change in urine colour – dark, rusty or brown
pain or a dull ache in the side or lower back that is not due to an injury
a lump in the abdomen
constant tiredness
rapid, unexplained weight loss
fever not caused by a cold or flu.
These symptoms can occur with other illnesses and so they don’t necessarily mean you have kidney cancer. If you have any concerns, contact your doctor.
Causes of kidney cancer
The causes of kidney cancer are not known, but factors that put some people at higher risk are:
smoking – smokers have almost twice the risk of developing kidney cancer as nonsmokers
workplace exposure to chemicals such as arsenic, some metal degreasers or cadmium used in mining, welding, farming and painting
a family history of kidney cancer
being overweight or obese
high blood pressure
having advanced kidney disease
being male - men are more likely to develop kidney cancer.
Diagnosis of kidney cancer
Tests to diagnose kidney cancer include:
Blood and urine tests
These tests do not diagnose kidney cancer but will check your general health and for any signs of a problem in the kidney.
Imaging tests
If kidney cancer is detected, you may have scans to see if the cancer has spread to other parts of your body, such as an ultrasound, chest x-ray, CT scan , MRI , or radioisotope bone scan.
A biopsy removes a tissue sample for examination under a microscope and is a common way to diagnose cancer. However, biopsies are not often needed for kidney cancer before treatment ad imaging scans are good at showing if a kidney tumour is cancer.
If you do have a biopsy, it will be a core needle biopsy where an interventional radiologist will put a hollow needle through the skin to remove a tissue sample.
Treatment for kidney cancer
The main treatment for kidney cancer is surgery , alone or with radiation therapy (radiotherapy) and will depend on the extent of the cancer.
If you are a smoker, your doctors will advise you quit before you start treatment.
A CT scan, bone (radioisotope) scan and chest x-ray are done to determine the extent of the cancer.
The most common staging system used for kidney cancer is the TNM system , which describes the stage of the cancer from stage I to stage IV
Active surveillance
If small tumours are found in your kidney your doctor may recommend active surveillance or observation as it is likely that the tumours will not be aggressive and may not grow in your lifetime. You will have regular ultrasounds or CT scans to monitor the tumours.
A radical nephrectomy (removal of the affected kidney) is the most common type of surgery for renal cell carcinoma.
A partial nephrectomy (removal of part of the kidney) may be an option for people who have a small tumour in one kidney (less than 4cm), people with cancer in both kidneys and those who have only one working kidney.
Radiofrequency ablation
Radiofrequency ablation heats the tumour with high energy waves in order to kill the cancer cells. Your doctor will insert a needle into the tumour and an electrical current is passed into the tumour.
Immunotherapy works to enhance your body's own immune system. Immunotherapy is an option for people with advanced kidney cancer. Cytokines (proteins that activate the immune system) can be given intravenously or orally, and may shrink the cancer.
Targeted therapies may be recommended by your doctor if you have advanced kidney cancer or your cancer is growing quickly. Targeted therapies target specific molecules in cells to block cell growth. Targeted therapy drugs are usually given in the form of tablets or intraveneously.
Tyrosine kinase inhibitors (TKIs) have been trialled in people with advanced kidney cancer and found to cause fewer side effects than chemotherapy drugs.
Radiation therapy may be used if you are not able to have surgery. It may also be used in advanced kidney cancer to shrink tumours and relieve symptoms.
In some cases of kidney cancer, your medical team may talk to you about palliative care . Palliative care aims to improve your quality of life by alleviating symptoms of cancer.
As well as slowing the spread of kidney cancer, palliative treatment can relieve pain and help manage other symptoms. Treatment may include radiotherapy, chemotherapy or other drug therapies.
Treatment Team
- GP (General Practitioner) - looks after your general health and works with your specialists to coordinate treatment.
- Urologist- specialises in the treatment of diseases of the urinary system (male and female) and the male reproductive system
- Nephrologist- diagnoses and treats conditions that cause kidney (renal) failure or impairment.
- Medical oncologist - prescribes and coordinates the course of chemotherapy.
- Radiation oncologist - prescribes and coordinates radiation therapy treatment.
- Radiologist- interprets diagnostic scans (including CT, MRI and PET scans).
- Cancer nurse - assists with treatment and provides information and support throughout your treatment.
- Cancer care coordinators- coordinate your care, liaise with the multidisciplinary team and support you and your family throughout treatment.
- Dietitian - recommends an eating plan to follow while you are in treatment and recovery.
- Other allied health professionals - such as social workers, pharmacists, and counsellors .
Screening for kidney cancer
There is currently no national screening program for kidney cancer available in Australia.
Preventing kidney cancer
Not smoking or quitting smoking. Up to one third of kidney cancers are thought to be due to smoking.
Prognosis for kidney cancer
It is not possible for a doctor to predict the exact course of a disease, as it will depend on each person's individual circumstances. However, your doctor may give you a prognosis, the likely outcome of the disease, based on the type of kidney cancer you have, the test results, the rate of tumour growth, as well as your age, fitness and medical history.
In most cases, the earlier that kidney cancer is diagnosed, the better the prognosis.
- Understanding Kidney Cancer , Cancer Council Australia, © 2020. Last medical review of source booklet: November 2020.
- Australian Institute of Health and Welfare. Cancer data in Australia [Internet]. Canberra: Australian Institute of Health and Welfare, 2023 [cited 2023 Sept 04]. Available from: https://www.aihw.gov.au/reports/cancer/cancer-data-in-australia
This information was last updated September 2023.
Back to all cancer types
Advertisement
Renal cancer: overdiagnosis and overtreatment
- Published: 12 August 2021
- Volume 39 , pages 2821–2823, ( 2021 )
Cite this article
- Giuseppe Rosiello 1 , 2 ,
- Alessandro Larcher 1 , 2 ,
- Francesco Montorsi 1 , 2 &
- Umberto Capitanio 1 , 2
3105 Accesses
12 Citations
Explore all metrics
Avoid common mistakes on your manuscript.
Renal cell carcinoma (RCC) accounts for approximately 4.1% of all new cancers, with a median age at diagnosis of 64 years. In 2020, around 73,750 new cases were expected to be diagnosed in the United States, with an age-adjusted rate of 16.3 cases/100.000 persons [ 1 ]. Worldwide, the incidence of RCC has been rising [ 2 ] due to the widespread use of cross-sectional imaging performed for other reasons (e.g. hypertension, diabetes, etc.) [ 3 ]. As a consequence, a significant increase in incidental detection of renal masses has been observed over time, especially in elderly patients, who are more likely to undergo radiological investigations for other health-related problems [ 4 ]. It is of note that early detection of kidney tumors has been accompanied by a clinical-stage migration toward earlier tumor stages. Specifically, despite locally advanced RCC continues to be diagnosed in a high proportion of patients, with up to 17% harbouring metastatic disease at the time of diagnosis [ 5 ], the rates of cT 1 renal masses increased from 40% in 1992 to roughly 70% in 2015 [ 6 ] Nevertheless, several reports demonstrated a lack of declining mortality rates for localized RCC over time [ 7 ], and the cancer-specific mortality rate of patients harbouring T 1a disease remains below 5% at 5 years. [ 4 ] Such a controversial relationship between increasing detection rates of small renal masses (SRMs), but relatively stable survival outcomes highlights the importance of carefully evaluating and discussing the phenomenon of early detection in RCC, and make the concept of “overdiagnosis” of great importance in this context.
“Overdiagnosis” can be defined as the detection of a renal mass that would not cause any symptoms or clinical progression, if never diagnosed [ 8 ]. Therefore, the overdiagnosis of a small, silent renal mass crashes against our limited ability in determining the nature and the aggressiveness of the incidentally detected mass. Indeed, despite some improvements have been done in the field of nuclear imaging and radiomics [ 9 ], the current technology is limited and still, more than 20% of surgery are done for SRMs, which result totally benign at final pathology.
During the last two decades, the incidence of RCC increased from 9.2 to 12.5 cases per 100.000 persons/year. Notably, over 45% of newly diagnosed RCC have tumor size ≤ 4 cm, and this percentage is on the rise. Based on what was previously stated, it is not surprising that the incidence of T 1a RCC recorded the highest increase over time: + 50% since the beginning of the new millennium. [ 10 ] However, more in-depth analyses of age-specific data are necessary to better understand this phenomenon and its implications in clinical practice. Specifically, despite the incidence rates of SRMs also increased in young adults (from 0.1 to 0.4 cases per 100.000 persons/year), [ 11 ] such estimates are much lower than what was recorded in the general population. [ 2 ] Conversely, data regarding elderly patients are extremely different and deserve particular attention. Indeed, approximately 75% of newly diagnosed RCC are reported in patients over the age of 60. The age-standardised incidence rate in this patient population is as high as 35.0 cases per 100.000 persons/year, and the highest rate is recorded in patients aged ≥ 75 years. [ 2 ] Moreover, the incidence of SRMs is 30-fold higher in ≥ 75 years old than in younger patients. [ 12 ] These data demonstrate the magnitude of the problem, and should not be underestimated but, instead, they should sensitize the urological community about the important implications that they may have, in a global and comprehensive evaluation of the phenomenon. Indeed, the potential consequences of overdiagnosis may be significant and include psychological and behavioural effects of disease labelling, physical harms and side effects of unnecessary tests or treatments, increased financial costs to individuals and wasted resources and opportunity costs to the health system. Last but not least, overdiagnosis may lead to an increased risk of overtreatment.
In RCC, overdiagnosis does not imply invasive detection manoeuvres, as happens for instance in other urological settings (e.g. prostatic biopsy). Therefore, more importantly than overdiagnosis, the most detrimental and dangerous aspect in RCC is the decision after the diagnosis or in other words—the potential “overtreating”. “Overtreatment” is a partially overlapped phenomenon which implies the treatment (and the related consequences) of cancer which wouldn’t have caused any symptom or cancer-related death. Overtreatment comes immediately after our inaccuracy in determining the characteristics of the mass. Even in the case of malignant pathology, the natural history of small low-grade kidney cancer is indolent—in most of the cases—if well balanced with life expectancy, comorbidities and competing risks mortality. Indeed, the majority of overdiagnoses happen in old and comorbid patients, where the balance between pro and cons is completely different relative to the diagnosis of RCC in a middle-aged and healthy patient. While postoperative complications are the most obvious danger resulting from surgical “overtreatment” of patients with SRMs, the decrease in renal function is also well-established [ 13 , 14 ], and the risk resulting from kidney surgery needs to be evaluated, especially in those at higher risk of long-term renal impairment, such as elderly or comorbid patients. Moreover, studies exploring the benefits of nephrectomy in patients older than 75 years with clinically localized cT 1 renal masses demonstrated no superiority of definitive treatment (either partial or radical approach) compared to active surveillance in terms of cancer-specific survival, due to decreased life expectancy in this patient population. In other words, most of these patients would not live long enough to benefit from surgery [ 4 ].
In the current issue of World Journal of Urology, review papers and original articles provide recent data which may limit the effect of overdiagnosis and overtreatment in the kidney cancer setting. Specifically, the natural history of untreated kidney cancer [ 15 ], the importance of frailty and comorbidities for clinical decision making [ 16 , 17 ], the role of contrast-enhanced ultrasound [ 18 ], the novelties in radiomics and biomarkers and the current ongoing active surveillance protocols were summarized and critically analyzed [ 19 , 20 , 21 ].
Motzer RJ, Jonasch E, Agarwal N, Bhayani S, Bro WP, Chang SS et al (2017) Kidney cancer, version 2.2017: clinical practice guidelines in oncology. J Natl Compr Cancer Netw 15:804–834. https://doi.org/10.6004/jnccn.2017.0100
Article Google Scholar
Capitanio U, Bensalah K, Bex A, Boorjian SA, Bray F, Coleman J et al (2019) Epidemiology of renal cell carcinoma. Eur Urol 75:74–84. https://doi.org/10.1016/j.eururo.2018.08.036
Article PubMed Google Scholar
Chow W-H, Dong LM, Devesa SS (2010) Epidemiology and risk factors for kidney cancer. Nat Rev Urol 7:245–257. https://doi.org/10.1038/nrurol.2010.46
Article PubMed PubMed Central Google Scholar
Sun M, Becker A, Tian Z, Roghmann F, Abdollah F, Larouche A et al (2014) Management of localized kidney cancer: calculating cancer-specific mortality and competing risks of death for surgery and nonsurgical management. Eur Urol 65:235–241. https://doi.org/10.1016/j.eururo.2013.03.034
Article CAS PubMed Google Scholar
Capitanio U, Montorsi F (2016) Renal cancer. Lancet 387:894–906. https://doi.org/10.1016/S0140-6736(15)00046-X
Kane CJ, Mallin K, Ritchey J, Cooperberg MR, Carroll PR (2008) Renal cell cancer stage migration: analysis of the national cancer data base. Cancer 113:78–83. https://doi.org/10.1002/cncr.23518
Sun M, Thuret R, Abdollah F, Lughezzani G, Schmitges J, Tian Z et al (2011) Age-adjusted incidence, mortality, and survival rates of stage-specific renal cell carcinoma in North America: a trend analysis. Eur Urol 59:135–141. https://doi.org/10.1016/j.eururo.2010.10.029
Welch HG, Black WC (2010) Overdiagnosis in cancer. J Natl Cancer Inst 102:605–613. https://doi.org/10.1093/jnci/djq099
Leong JY, Wessner CE, Kramer MR, Forsberg F, Halpern EJ, Lyshchik A et al (2020) Superb microvascular imaging improves detection of vascularity in indeterminate renal masses. J Ultrasound Med. https://doi.org/10.1002/jum.15299
Palumbo C, Pecoraro A, Knipper S, Rosiello G, Luzzago S, Deuker M et al (2020) Contemporary age-adjusted incidence and mortality rates of renal cell carcinoma: analysis according to gender, race, stage, grade, and histology. Eur Urol Focus. https://doi.org/10.1016/j.euf.2020.05.003
Palumbo C, Pecoraro A, Rosiello G, Luzzago S, Deuker M, Stolzenbach F et al (2020) Renal cell carcinoma incidence rates and trends in young adults aged 20–39 years. Cancer Epidemiol 67:101762. https://doi.org/10.1016/j.canep.2020.101762
King SC, Pollack LA, Li J, King JB, Master VA (2014) Continued increase in incidence of renal cell carcinoma, especially in young patients and high grade disease: United States 2001 to 2010. J Urol 191:1665–1670. https://doi.org/10.1016/j.juro.2013.12.046
Bhindi B, Lohse CM, Schulte PJ, Mason RJ, Cheville JC, Boorjian SA et al (2019) Predicting renal function outcomes after partial and radical nephrectomy (figure presented). Eur Urol 75:766–772. https://doi.org/10.1016/j.eururo.2018.11.021
Rosiello G, Capitanio U, Larcher A (2019) Acute kidney injury after partial nephrectomy: transient or permanent kidney damage? Impact on long-term renal function. Ann Transl Med 7:S317–S317. https://doi.org/10.21037/atm.2019.09.156
McAlpine K, Finelli A (2021) Natural history of untreated kidney cancer. World J Urol. https://doi.org/10.1007/s00345-020-03578-1
Walach MT, Wunderle MF, Haertel N et al (2021) Frailty predicts outcome of partial nephrectomy and guides treatment decision towards active surveillance and tumor ablation. World J Urol. https://doi.org/10.1007/s00345-020-03556-7
Courcier J, De La Taille A, Lassau N et al (2021) Comorbidity and frailty assessment in renal cell carcinoma patients. World J Urol. https://doi.org/10.1007/s00345-021-03632-6
Bertelli E, Palombella A, Sessa F et al (2021) Contrast-enhanced ultrasound (CEUS) imaging for active surveillance of small renal masses. World J Urol. https://doi.org/10.1007/s00345-021-03589-6
Patel SH, Singla N, Pierorazio PM (2021) Decision-making in active surveillance in kidney cancer: current trends and future urine and tissue markers. World J Urol. https://doi.org/10.1007/s00345-021-03786-3
Rebez G, Pavan N, Mir MC (2021) Available active surveillance follow-up protocols for small renal mass: a systematic review. World J Urol. https://doi.org/10.1007/s00345-020-03581-6
Kuusk T, Neves JB, Tran M et al (2021) Radiomics to better characterize small renal masses. World J Urol. https://doi.org/10.1007/s00345-021-03602-y
Download references
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
Department of Urology, IRCCS San Raffaele Scientific Institute, Via Olgettina 60, 20132 MI, Milan, Lombardia, Italy
Giuseppe Rosiello, Alessandro Larcher, Francesco Montorsi & Umberto Capitanio
Division of Experimental Oncology, URI, Urological Research Institute, IRCCS San Raffaele Scientific Institute, Milan, Italy
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Umberto Capitanio .
Ethics declarations
Conflict of interest.
None to declare.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Rosiello, G., Larcher, A., Montorsi, F. et al. Renal cancer: overdiagnosis and overtreatment. World J Urol 39 , 2821–2823 (2021). https://doi.org/10.1007/s00345-021-03798-z
Download citation
Published : 12 August 2021
Issue Date : August 2021
DOI : https://doi.org/10.1007/s00345-021-03798-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Find a journal
- Publish with us
- Track your research
Kidney Cancer Research Results and Study Updates
See Advances in Kidney Cancer Research for an overview of recent findings and progress, plus ongoing projects supported by NCI.
In a clinical trial, an injectable form of nivolumab (Opdivo) was as effective against kidney cancer as the intravenous form of the drug. Side effects were also similar and treatment time was shorter. Injectable immunotherapies, several experts said, if found to be comparable to IV forms, can be more convenient to receive and accessible to more people.
Stereotactic body radiotherapy was effective in people with localized kidney cancer who weren’t able to have surgery to remove their tumor, a clinical trial has shown. No patients had their cancer start growing or died from cancer over the next 5 years.
FDA has approved belzutifan (Welireg) to treat adults with von Hippel-Lindau disease (VHL) who have tumors of the kidney, brain, nervous system, or pancreas. The drug may help these patients avoid or delay surgery by shrinking their tumors.
Cabozantinib (Cabometyx) is an effective initial treatment for people with metastatic papillary renal cell carcinoma (PRCC), a rare type of kidney cancer. A clinical trial showed the drug was more effective than the current standard treatment.
Results from two studies show that a liquid biopsy that analyzes DNA in blood accurately detected kidney cancer at early and more advanced stages and identified and classified different types of brain tumors.
In two clinical trials, combination treatments that included an immune checkpoint inhibitor and axitinib (Inlyta) led to better outcomes for patients with advanced kidney cancer than treatment with sunitinib (Sutent), the standard initial therapy.
Results from an NCI-sponsored clinical trial may point to an important change in how some children with advanced Wilms tumor, a form of kidney cancer, are treated.
FDA has approved the combination of two immunotherapy drugs, nivolumab (Opdivo) and ipilimumab (Yervoy), as an initial treatment for some patients with advanced kidney cancer. Learn how this approval will affect patient care.
The Food and Drug Administration has approved cabozantinib (Cabometyx®) as an initial treatment for patients with advanced renal cell carcinoma, the most common type of kidney cancer.
Two new studies suggest that a new class of drugs can effectively target a molecular driver of the most common type of kidney cancer.
The FDA has approved two drugs, cabozantinib and lenvatinib, for patients whose advanced kidney cancers have progressed after prior treatment with antiangiogenic therapies.
Results from a recent clinical trial show that post-surgical therapy with two anti-angiogenesis drugs does not improve progression-free survival for patients with kidney cancer and may cause serious side effects.
Researchers with The Cancer Genome Atlas (TCGA) report new findings on papillary renal cell carcinoma and prostate cancer.
We use cookies to enhance our website for you. Proceed if you agree to this policy or learn more about it.
- Essay Database >
- Essay Examples >
- Essays Topics >
- Essay on Urinary System
Free Kidney Cancer Essay Example
Type of paper: Essay
Topic: Urinary System , Kidney , Cancer , Condition , Medicine , Body , Risk , Treatment
Words: 1300
Published: 01/14/2022
ORDER PAPER LIKE THIS
Introduction
Kidney cancer is among the many forms of cancerous conditions that manifest in the human body. Renal cell carcinoma as it is referred in the medical world describes the situation where the kidney cells become malignant. The formation of cancer can take two different forms. One of the forms develops when the kidney cells grow uncontrollably to form large tubules in the kidney thus inhibiting its functions. The other type of cancerous formation occurs when the kidney cells divide at a faster rate forming lumps in the kidneys (Kidneycancer.org 1). Kidney cancer has been prevalent in the United States with the recent statistics indicating that out of the 1.3 million people diagnosed with cancer, 50,000 of them were suffering from kidney cancer. The United States cancer association reports that there exist over 200,000 survivors of kidney cancer living in the United States. Although the doctors do not know the cause of the condition, when detected early, the condition can be treated or managed. The early diagnoses require that the cancerous cells have not undergone metastases, a medical condition that refers to the migration of the malignant cells to other parts of the body (Kidneycancer.org 2). When the kidney of a person develops the malignant condition, the functions of the kidneys are significantly affected. The kidneys are bean shaped organs found on the lower parts of the human abdomen. The kidneys play several physiological processes in the body. One of the critical functions is balancing the concentration of the amount of body salt present in the body fluid by controlling the level of the sodium discharged in urine. The kidney plays a significant role in maintaining the level of the concentration of the minerals in the blood by allowing the exchange of salts and minerals between the blood and the body fluids. The kidney is instrumental I removing waste products in the body through the reverse osmosis and active transport in the body. When the kidney cells are infected with cancer, they are unable to function optimally and the patient can suffer the related conditions due to the accumulation of the waste and toxic products in the blood and the body fluids (Choueiri, Toni, Youjin and Eunyoung 386). When the malignant cells are detected early, the treatment process is easy. However, most of the cancerous cells are detected later in the development process because the patients do not the symptoms that can drive them to asking for screening. The doctors advise that the adult people should go for screening because the signs of the condition are hard to notice. Nonetheless, the causes of the kidney cancer remain a mystery in the medical field. Several studies have been made and are being made in the medical field to evaluate the possible cause of the condition but to date; no study has come to a logical conclusion. The many studies that have been made have provided an insight towards the risk factors of the disease (Choueiri, Toni, Youjin and Eunyoung 388). Risk factors are the conditions that when the human body is exposed to them, puts one at a higher risk of developing the condition. The healthcare researchers have identified several risk factors that put one at a risk of developing the condition. The risk factors vary from living styles, genetic make-up, presence of other diseases, and exposure to radioactive environment to being subjected to some forms of medical treatment. The risk factors that have been identified influence the development of the condition in varying degrees with some having been labeled the most influential to the condition. The most interesting thing about the findings is that the most influential risk factors are health style related, and thus controllable. Genetic make-up has been connected to the increased likelihood of developing kidney cancer. The researchers as among the leading genetic kidney cancer risk factors have identified one of the hereditary disorders referred to as the Von Hippel-Lindau (VHL) condition. The medical researchers have made a tremendous step in the study by isolating the gene that causes the VHL disorder. The step has offered future possibilities for the early diagnosis, management and diagnosis of kidney malignancy (Choueiri, Toni, Youjin and Eunyoung 389). Another genetic disorder linked to the development of kidney cancer is Birt Hogg Dube syndrome. The disorder is mainly characterized by the availability of several bumps appearing on the skin around the nose, ears, forehead, cheeks, and neck. Tuberous sclerosis has also been linked with the development of renal cell carcinoma. However, smoking and obesity pose the most significant threat towards development of the condition (Choueiri, Toni, Youjin and Eunyoung 390). The American Cancer Society reported that over one million fresh cases of the renal cell carcinoma are reported annually in the US. The preference of the condition indicates that the disease manifest twice as much in males than in females. The condition is more prevalent of the older population above 40 years than in the young children and young adults. The report indicates that renal cell carcinoma happens to be the most frequent kind of kidney cancer in the American societies. However, when compared to the other types of cancers, it forms a relatively low percentage constituting of 3% of the cases. When the condition is diagnosed early, surgical treatment is easy done by removing the cancerous cells. However, an early diagnosis is difficult owing to the lack of pronounced symptoms of the disease (Kidneycancer.org 3). The early stages symptoms go unnoticed or are misdiagnosed until they have grown fairly large and have displaced other organs. The displacement of the other organs in most cases is the notable symptom of the disease. The history of the disease indicates that most of the renal tumors are discovered incidentally by ultra sound and x-ray examinations that were not performed for the purpose. 30% of the kidney patients manifest symptoms at the advanced stage of the disease. At the time of the diagnosis, 25% have the cancerous tissue having spread to the other parts of their bodies. At that time, the treatment and management is not as easy as it would have been were the case diagnosed earlier (Kidneycancer.org 4). The most common sign of the condition manifested in most people is painless passing of blood in urine, a condition termed as hematuria. Unfortunately, the blood in urine appears one day and is gone in the next, and can easily be ignored. In addition, the presence o blood in urine could indicate other conditions such as kidney stones. Other signs may include abdominal mass, thickening under the skin, back pain among the persons over forty years, weight loss, and high calcium in blood (Sumpio, Catherine, Knobf, and Sangchoon 287). The condition is tested for its presence using various methods such as computer tomography, magnetic resonance imaging, PET scan, Angiography and biopsy procedures. Other tests include urinalysis and blood tests. Kidney cancer is treated using various methods determined by the grading of the malignant cells. Surgery, chemotherapy, radioactive treatment or a combination of surgery and chemotherapy may be employed in the treatment (Sumpio, Catherine, Knobf, and Sangchoon 292).
Works cited
Choueiri, Toni K., Youjin Je, and Eunyoung Cho. "Analgesic use and the risk of kidney cancer Ameta-analysis of epidemiologic studies." International Journal of Cancer 134.2 (2013): 384-396. Print. Kidneycancer.org. "About Kidney Cancer." Kidney Cancer Association. N.p., 2016. Web. 9 Feb, 2016. Stat Bite Percentage of New Cases of Colorectal Cancer in the United States per 100 000 (2007- 2011)." JNCI Journal of the National Cancer Institute 106.10 (2014): dju342-dju342. Print. Sumpio, Catherine, M. T. Knobf, and Sangchoon Jeon. "Treatment complexity: a description of chemotherapy and supportive care treatment visits in patients with advanced-stage cancer diagnoses." Support Care Cancer 24.1 (2015): 285-293. Print.

Cite this page
Share with friends using:
Removal Request

Finished papers: 1241
This paper is created by writer with
ID 256171354
If you want your paper to be:
Well-researched, fact-checked, and accurate
Original, fresh, based on current data
Eloquently written and immaculately formatted
275 words = 1 page double-spaced

Get your papers done by pros!
Other Pages
Horror argumentative essays, lincoln argumentative essays, maya argumentative essays, networking argumentative essays, coffee argumentative essays, motivation business plans, experience business plans, welfare business plans, entertainment business plans, european union business plans, unix business plans, facebook literature reviews, mandate creative writings, sensitivity creative writings, carbon creative writings, allocation creative writings, gas creative writings, magazine creative writings, course work on divorce, pros and cons of assisted suicide essay, critical thinking on apples 1984 advert, nuisance essay, nirvana and moksha buddhism hinduism and pathways to perfection essay, research paper on data collection and analysis grid, essay on oregon plan raw score, sea based incinerators essay, experiential learning and timely development report, mcdonald swot analysis essay, law the social network movies essay, free course work on potential security weaknesses of aircraft solutions, interview a helping professional essay, sociology review article review example, nonconformist essays, tobias wolff essays, dana gioia essays, hans christian andersen essays, philip sidney essays, burial rites essays, shakers essays, marilyn chin essays, three gorges dam essays, murasaki shikibu essays, make up essays.
Password recovery email has been sent to [email protected]
Use your new password to log in
You are not register!
By clicking Register, you agree to our Terms of Service and that you have read our Privacy Policy .
Now you can download documents directly to your device!
Check your email! An email with your password has already been sent to you! Now you can download documents directly to your device.
or Use the QR code to Save this Paper to Your Phone
The sample is NOT original!
Short on a deadline?
Don't waste time. Get help with 11% off using code - GETWOWED
No, thanks! I'm fine with missing my deadline

- River City Live
- Newsletters
WEATHER ALERT
2 river flood warnings in effect for Brantley and Columbia Counties
Why some kidney cancer patients are living longer.
Ivanhoe Newswire
DALLAS, Tx – Kidney cancer is among the 10 most common cancers in both men and women. About 81,000 people will be diagnosed with it this year.
A decade ago, advanced kidney cancer was a death sentence, but now, new therapies and cutting-edge drugs are helping more people live longer, healthier lives.
“I noticed there was some blood in my urine,” recalled kidney cancer patient Brent Hall.
It’s one of the big red flags when it comes to kidney cancer.
“I used to have a trace of blood in my urine, every physical, but this time there was more than a trace,” said Ralph Auriemma, another kidney cancer patient.
But once a person sees blood in their urine, it means the cancer is probably more advanced.
The most common form of it?
“Renal cell carcinoma is the most common cancer of the kidney,” said Dr. Thomas Hutson, an oncologist at Baylor Scott & White Charles A. Sammons Cancer Center.
Start your morning with our daily forecast, trending news and stories curated by The Morning Show team.
Hutson said treatments include radiation, chemo, and surgery.
“The cancer can be cured, usually, with surgery, but once it has spread beyond the confines of the kidney to other sites of the body or has returned after initial attempts at curing it, then the cancer is generally not felt to be curable,” Hutson explained.
That’s when immunotherapy is used — using antibodies to turn on the body’s immune system to kill the cancer cells, but now a new study shows the effectiveness of using immunotherapies combined with a new generation of oral therapies.
“And for the first time ever, there’s a small group of patients that can actually witness their cancer disappear on X-rays,” Hutson said.
The phase three “CLEAR Study” showed by using a combination of drugs, 95 percent of patients saw no further growth of the tumor and 71% had a significant reduction in the size of it.
“More patients are living with their cancer longer than ever before in history, and our goal is to cure more patients, and I think that’s a realistic expectation over time,” Hutson added.
Smoking is the No. 1 risk factor for kidney cancer. Other risk factors include high blood pressure, obesity, family history and workplace exposure to certain substances.
MORE: Watch the video below for a story of a man who received a pig kidney transplant:
Copyright 2023 by Ivanhoe Newswire - All rights reserved.
Click here to take a moment and familiarize yourself with our Community Guidelines.
Recommended Videos
- Share full article

Sickened by U.S. Nuclear Program, Communities Turn to Congress for Aid
In St. Louis and around the country, people harmed by the drive for an atomic bomb have been shut out of a federal law enacted to help such victims.
Hundreds of thousands of tons of nuclear waste from a St. Louis factory were dumped over decades, seeping into the soil and nearby Coldwater Creek. Credit... Bryan Birks for The New York Times
Supported by

By Catie Edmondson
Catie Edmondson, who covers Congress, surveyed St. Louis’s radioactive contamination from three sites, including the banks of Coldwater Creek.
- April 6, 2024
When Diane Scheig’s father, Bill, came home from work at the Mallinckrodt factory in St. Louis, he would strip down in their garage and hand his clothes to her mother to immediately wash, not daring to contaminate the house with the residue of his labors.
Mr. Scheig, an ironworker who helped build the city’s famous arch, never told their family exactly what he was doing at the plant, where scientists first began processing uranium for the Manhattan Project in 1942. But by the age of 49, he had developed kidney cancer, lost his ability to walk, and died.
Decades later, Diane’s older sister Sheryle, who years earlier had given birth to a baby boy born with a softball-sized tumor in his stomach, died of brain and lung cancer at 54. Her neighbor two doors down died of appendix cancer at 49. So many of her classmates have died of cancer that a large round table covered with their pictures is now a staple of her high school reunions.
“I know for myself, I was thankful when I passed the age of 49,” Ms. Scheig said. “And I was thankful when I passed the age of 54.”
The Mallinckrodt plant processed the uranium that allowed scientists at the University of Chicago to produce the first man-made controlled nuclear reaction, paving the way for the first atomic bomb.
But the factory — and the program it served — left another legacy: A plague of cancer, autoimmune diseases and other mysterious illnesses has ripped through generations of families like Ms. Scheig’s in St. Louis, and other communities across the country that were exposed to the materials used to power the nuclear arms race.
Now Congress is working on legislation that would allow people harmed by the program but so far shut out of a federal law enacted to aid its victims — including in New Mexico, Arizona, Tennessee and Washington state — to receive federal compensation.
A Toxic Legacy

In the 1940s, as workers churned out 50,000 tons of uranium to feed the nation’s nascent atomic arsenal, the factory was also spitting out heaps of nuclear waste.
Over the next several decades, hundreds of thousands of tons of radioactive waste stored in open steel drums were hauled and dumped across the city. The waste seeped into large swaths of soil, including on land that later became ball fields.
And it drained into Coldwater Creek, a tributary that snakes through the metropolitan area for 19 miles through backyards and public parks where children play and catch crayfish. In heavy storms, the creek routinely floods.
There are similar stories across the country, among the Navajo workers in New Mexico and Arizona who were sent into mines with a bucket and a shovel to dig up uranium and were never told about the dangers; the children of workers at uranium processing plants in Tennessee and Washington state; and the downwinders across the Southwest who breathed in the fallout from the mushroom clouds of aboveground tests.
None of those communities qualify for aid under the only federal law to compensate civilians who sustained serious illnesses from the nation’s nuclear weapons program. Passed in 1990, that statute was narrowly constructed to help some uranium miners and a handful of communities who were present for aboveground testing. Claimants, who can include children or grandchildren of those who would have benefited from the program but have since died, receive a one-time payment of $50,000 to $100,000.
The Senate last month passed legislation led by Senator Josh Hawley, Republican of Missouri, and Senator Ben Ray Luján, Democrat of New Mexico, that would update and dramatically expand the law to include thousands of new participants, including Missouri families like the Scheigs.
If Congress does not pass the bill before June, the law will expire altogether, shuttering the fund for those who are currently eligible and cutting off access to cancer screening clinics in neighborhoods that have been hit hard by radioactive exposure and rely on federal money to continue operating.
To read their legislation is to visualize a map of the physical and psychic toll the nation’s nuclear weapons’ legacy has seared into communities across the country, years after the first atomic test at Los Alamos.
“It speaks to the enormity of the burden,” Mr. Hawley, a conservative Republican who is up for re-election this year, said in an interview. “It speaks to the heroism of these people who, for 50-plus years in almost all these cases, have borne the burden themselves. Some of my colleagues complained about the cost. Well, who do they think is bearing the cost now?”
For years, momentum to expand the nuclear compensation program had sputtered along in fits and starts on Capitol Hill, adopted by various lawmakers who inched it forward but were not able to secure a vote in the House or Senate.
But it got a shot in the arm when Mr. Hawley took up the issue, working with Mr. Luján to draft legislation and using his perch on the Armed Services Committee to attach it to the annual defense policy bill.
When the measure was stripped out of the final version of the legislation after Republicans objected to its hefty price tag, which congressional scorekeepers estimated could hit $140 billion, the senators went back to the drawing board. Cutting out expansive new provisions that would have forced the federal government to cover victims’ medical fees, Mr. Hawley and Mr. Luján also added new communities, enticing more senators to support the bill now that it would benefit their states.
When the measure finally got a vote on the Senate floor last month — made possible after some horse-trading between Mr. Hawley and Senator Mitch McConnell, Republican of Kentucky and the minority leader — it passed 69 to 30.
‘Bleeding Through’
St. Louis’s radioactive fate was decided over lunch at the elite Noonday Club in the city’s downtown in 1942, when Arthur Compton, a top administrator of the Manhattan Project and the former head of physics at Washington University met with Edward Mallinckrodt Jr. , a scientist who ran his family’s chemical and pharmaceutical company. Three other companies had already refused Mr. Compton’s request — to begin refining uranium for the development of the bomb. Mr. Mallinckrodt, a longtime friend of Mr. Compton, said yes.
Eight decades later, the consequences of that decision are immediately visible on a drive through St. Louis. Cleanup of the creek is expected to take until 2038, according to The Missouri Independent.
At the site of the old airport, where the first radioactive waste from the plant was stored, workers clad in white Tyvek hazardous materials suits with bright yellow boots can be seen from the highway, digging into the ground behind fences adorned with yellow warning signs and next to rail cars loaded with contaminated soil.
Some miles down is the West Lake landfill , a pit holding thousands of tons of radioactive waste that originated at Mallinckrodt and was illegally dumped in an area now surrounded by chain restaurants, warehouses, and a hospital. By 2010, a growing underground fire about 1,000 feet from the radioactive material was discovered.
Around the same time, Kim Visintine, an engineer-turned-medical professional, began to realize in conversations with friends that the rate at which their families and classmates were falling ill with serious, rare cancers “was just historically way beyond the norm,” she said. Ms. Visintine’s son, Zach, was born with glioblastoma — the most aggressive type of brain tumor — and died at age 6.
She started a Facebook page called “ Coldwater Creek — Just the Facts ” and began mapping reports of serious illnesses linked to radiation, coloring in heavily affected neighborhoods in shades of red. There were soon thousands of examples.
“It just looked like it was bleeding through,” Ms. Visintine said of the red on the maps.
Thumbs Up or Thumbs Down
The illnesses have stretched across the city, and reached deep into family trees.
Carl Chappell’s father, a chemical operator, used to walk to work at the plant in the early 1950s, until he began working at the company’s sprawling Hematite facility , where scientists researched and produced high-enriched nuclear fuel. It was there, in 1956, that his father was exposed to a radiation spill.
“We didn’t know that that was radioactive,” Mr. Chappell recalled in an interview. “All we knew was he was exposed to some toxic chemical spill and hospitalized for a few days or several days down there until he was released to come home.”
Eight years later, his father was diagnosed with renal cancer. Within another eight years, he had died. He was 48.
Decades later, at the age of 40, Mr. Chappell’s son Stephen was diagnosed with a rare kind of mucinous cancer that began in his appendix and spread throughout his abdomen. He died at 44.
For some families, developing cancer feels inevitable. Kay Hake’s father, Marvin, was an engineer at the Mallinckrodt plant and survived bladder, prostate and skin cancer. Her husband, John, who worked as a heavy equipment operator, was among a team of workers dispatched years ago to help clean up toxic waste from another of Mallinckrodt’s uranium plants . Sometimes he was given protective equipment to wear, but other times he was not.
“Every time we get sick, we think it’s probably cancer,” Mr. Hake said in a recent interview over coffee. “Sometimes we’re planning for the future and it’s like, ‘Let’s not plan too far and try to enjoy our lives more.’ Because we don’t know if we’re going to make it.”
“It’s not if it’s going to happen,” Ms. Hake added. “It’s when.”
Christen Commuso, who grew up near the creek and has lobbied extensively for the expansion of the program through her work for the Missouri Coalition for the Environment, has found a small comfort in hoping that the suffering in her family will stop with her.
After Ms. Commuso developed thyroid cancer, doctors removed her thyroid, adrenal gland, gallbladder and eventually her uterus and ovaries. At first, Ms. Commuso said in an interview, she “really mourned the loss of my ability to have my own children.”
“But at the same time, there’s a part of me that feels like well, maybe it was a blessing in disguise,” she added. “Because I didn’t pass something down to a new generation.”
She was in the Senate chamber in March when lawmakers approved the legislation to expand the Radiation Exposure Compensation Act to cover Missourians like her. Just the provision in the existing law to fund screening clinics for survivors would help, she said, because she sometimes skips doctor’s appointments when she cannot afford them.
“I wanted to clap and scream and holler” when it passed, Ms. Commuso said.
But she also found it jarring to see how nonchalant senators were as they voted on her fate — with a customary thumbs up or thumbs down to the Senate clerk.
“To watch people kind of give a thumbs up or a thumbs down on your life — and does your life matter to them? It’s like, what do you have to say and do to convince people that you matter?”
An earlier version of this article misstated the month in which the Senate passed legislation to expand a federal law compensating victims of nuclear waste radiation. The bill was passed last month, not this month.
How we handle corrections
Catie Edmondson covers Congress for The Times. More about Catie Edmondson
Advertisement
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

A Narrative Review of Chronic Kidney Disease in Clinical Practice: Current Challenges and Future Perspectives
1 Diabetes Resource Centre, University Hospital Llandough, Penlan Road, Llandough, Cardiff, CF64 2XX UK
Ruth D. Lewis
2 Health Economics and Outcomes Research Ltd, Cardiff, UK
Angharad R. Morgan
Martin b. whyte.
3 Faculty of Health and Medical Sciences, University of Surrey, Guildford, UK
Wasim Hanif
4 University Hospitals Birmingham NHS Foundation Trust, Birmingham, UK
Stephen C. Bain
5 Diabetes Research Unit, Swansea University Medical School, Swansea, UK
Sarah Davies
6 Woodlands Medical Centre, Cardiff, UK
Umesh Dashora
7 East Sussex Healthcare NHS Trust, Eastbourne, UK
Zaheer Yousef
8 Department of Cardiology, University Hospital of Wales and Cardiff University, Cardiff, UK
Dipesh C. Patel
9 Division of Medicine, Department of Diabetes, University College London, Royal Free Campus, London, UK
W. David Strain
10 Diabetes and Vascular Research Centre, University of Exeter Medical School, Exeter, UK
Chronic kidney disease (CKD) is a complex disease which affects approximately 13% of the world’s population. Over time, CKD can cause renal dysfunction and progression to end-stage kidney disease and cardiovascular disease. Complications associated with CKD may contribute to the acceleration of disease progression and the risk of cardiovascular-related morbidities. Early CKD is asymptomatic, and symptoms only present at later stages when complications of the disease arise, such as a decline in kidney function and the presence of other comorbidities associated with the disease. In advanced stages of the disease, when kidney function is significantly impaired, patients can only be treated with dialysis or a transplant. With limited treatment options available, an increasing prevalence of both the elderly population and comorbidities associated with the disease, the prevalence of CKD is set to rise. This review discusses the current challenges and the unmet patient need in CKD.
Key Summary Points
Introduction.
Chronic kidney disease (CKD) is a complex and multifaceted disease, causing renal dysfunction and progression to end-stage kidney disease (ESKD) and cardiovascular disease. Complications associated with the disease contribute to the acceleration of CKD progression and risk of cardiovascular-related morbidities.
Despite its high prevalence and the clinical and economic burden of its associated complications, disease awareness remains profoundly low. Worldwide, only 6% of the general population and 10% of the high‐risk population are aware of their CKD statuses [ 1 ]. In addition, CKD recognition in primary care settings is also suboptimal, ranging from 6% to 50%, dependent upon primary care specialty, severity of disease, and experience. Awareness of CKD remains low in part because CKD is usually silent until its late stages. However, diagnosis of CKD during the later stages results in fewer opportunities to prevent adverse outcomes. Physician awareness of CKD is critical for the early implementation of evidence-based therapies that can slow progression of renal dysfunction, prevent metabolic complications, and reduce cardiovascular-related outcomes.
Currently CKD is not curable, and management of the disease relies on treatments which prevent CKD progression and cardiovascular disease. Despite available treatments, a residual risk of adverse events and CKD progression remains. This article reviews the challenges associated with CKD and the treatments available for patients, highlighting the unmet need for cardio-renal protection in patients with CKD.
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
CKD Prevalence
CKD is a global health problem. A meta-analysis of observational studies estimating CKD prevalence showed that approximately 13.4% of the world’s population has CKD [ 2 ]. The majority, 79%, were at late stages of the disease (stage 3–5); however, the actual proportion of people with early CKD (stage 1 or 2) is likely to be much higher since early kidney disease is clinically silent [ 3 ].
Prevalence of CKD appears to be growing rapidly both in the UK and in the Western world. Based on the 2012 subnational population projections for England [ 4 ], the number of people with CKD stage 3–5 is projected to exceed 4 million by 2036 [ 5 ]. This rise in CKD prevalence is due to an increased aging population and prevalence of type 2 diabetes (T2DM), obesity, hypertension and cardiovascular disease that contribute to CKD [ 6 – 8 ].
The World Health Organization (WHO) estimated that the annual, global number of deaths caused directly by CKD is 5–10 million [ 9 ]. The presence of CKD advances mortality of comorbidities such as cardiovascular diseases, T2DM, hypertension, and infection with human immunodeficiency virus (HIV), malaria and Covid-19, thereby indirectly adding to CKD mortality [ 9 , 10 ]. A contributing cause of high morbidity and mortality associated with CKD is a lack of awareness of the disease, by both patients and providers [ 11 , 12 ]. Early stages of CKD are clinically silent and patients have no symptoms. Lack of treatment at this stage allows CKD to progress through to advanced stages of the disease, where patients may present complications and/or cardiovascular-related comorbidities, or ESKD. Raising awareness of CKD is therefore paramount to allow for early intervention and reduce the risk of comorbidities and mortality.
Classification of CKD
In order to better manage CKD and provide better care for patients, the classification of CKD was developed by the National Kidney Foundation Kidney Disease Outcomes Quality Initiative [ 13 ] and the international guideline group Kidney Disease Improving Global Outcomes (KDIGO) [ 14 ]. CKD stratification is based upon the estimated glomerular filtration rate (eGFR) and albuminuria.
There are six eGFR categories. An eGFR of less than 60 mL/min per 1.73 m 2 for more than 3 months is indicative of impaired renal function and the severity of kidney damage increases with decreasing eGFR measurements. Patients with early onset of the disease, stage 1–2, have normal to mild decreased levels of eGFR (60 to ≥ 90 mL/min per 1.73 m 2 ). Patients with stage 3a–3b have mild to moderate decreased levels of eGFR (45–59 mL/min per 1.73 m 2 , respectively). Severely decreased levels of eGFR, stage 4–5 (15–29 to < 15 mL/min per 1.73 m 2 , respectively), are indicative of advanced stages of the disease and kidney failure.
Stratification also comprises three categories of albuminuria. Patients with an albumin to creatinine ratio (ACR) of 3 to at most 30 mg/mmol are classified as having microalbuminuria and at moderate risk of adverse outcomes. Those with ACR of greater than 30 mg/mmol are classified as having macroalbuminuria and being severely at risk of developing adverse events [ 15 ]. The eGFR and albuminuria categories independently predict adverse outcomes for patients with CKD, and the combination of both increases this risk further [ 16 ]. The CKD classification system aids clinicians in carrying out accurate assessments of CKD severity and other complications which helps to inform decisions associated with the management and monitoring of patients [ 3 , 17 , 18 ].
Clinical Burden of CKD
CKD is a complex disease, involving both non-modifiable (e.g. older age, family history and ethnicity) and modifiable risk factors (e.g. T2DM, hypertension and dyslipidaemia) which are responsible for the initiation of early CKD, CKD progression (stage 3–5) and ESKD.
In early stages of CKD (stage 1–2), factors such as hypertension, obesity and T2DM can trigger kidney function impairment. This causes glomerular/interstitial damage and results in impaired glomerular filtration, leading to decreased eGFR and increased albuminuria. At this stage, even though clinical symptoms do not present, the presence of additional risk factors, including hypertension, hyperglycaemia, smoking, obesity, dyslipidaemia and cardiovascular disease, may accelerate CKD progression and result in ESKD.
As the disease progresses, the clinical and economic burden of CKD increases (Fig. 1 ) as complications such as CKD mineral bone disorder, anaemia, hypertension and hyperkalaemia may occur and advanced stages of CKD, stage 4–5, ensue. Clinical symptoms, such as fatigue, itching of the skin, bone or joint pain, muscle cramps and swollen ankles, feet or hands, are often present at this stage [ 19 ]. Further deterioration of kidney function causes tubular and glomerular hypertrophy, sclerosis and fibrosis, leading to a significant reduction in eGFR, extreme albuminuria and kidney failure.

A schematic diagram showing the association between CKD progression and clinical and economic burden. Symptoms of CKD typically present during advanced stages of the disease where patients are at increased risk of cardiovascular disease and other comorbidities
Even though CKD progression may lead to kidney failure and renal death, patients with CKD are more likely to die from cardiovascular-related complications before reaching ESKD [ 20 ]. A study using data from a meta-analysis involving 1.4 million individuals found a significant increased risk of cardiovascular-related mortality, even in stage 2 of CKD (eGFR levels < 90 mL/min per 1.73 m 2 ) [ 16 , 21 , 22 ].
As the disease progresses, the risk of cardiovascular disease is markedly increased, such that 50% of patients with late-stage CKD, stage 4–5, have cardiovascular disease. The risk of atrial fibrillation (AF) and acute coronary syndrome (ACS) is doubled in patients with eGFR < 60 mL/min per 1.73 m 2 . AF is associated with a threefold higher risk of progression to ESKD. The incidence of heart failure (HF) is also threefold greater in patients with eGFR < 60 mL/min per 1.73 m 2 compared with > 90 mL/min per 1.73 m 2 and HF is associated with CKD progression, hospitalisation and death [ 23 ].
The increased risk of cardiovascular disease in patients with CKD is due in part to the traditional risk factors associated with cardiovascular disease such as hypertension, T2DM and dyslipidaemia. For instance, a large observational database linked study (Third National Health and Nutrition Examination Survey (NHANES) III) found a strong association between CKD and T2DM combined and an increased risk of mortality [ 24 ]. In this study, the authors observed a 31.1% mortality rate in patients with CKD and diabetes, compared to 11.5% in people with diabetes only. An observational study using both US and UK linked databases showed that the presence of both CKD and T2DM was related to increased risk of major adverse cardiac events (MACE), HF and arrhythmogenic cardiomyopathy (ACM) [ 25 ]. This risk was further elevated in older patients with atherosclerotic cardiovascular disease [ 25 ]. Similarly, the presence of both CKD and T2DM leads to a significant increased risk of all-cause and cardiovascular-related mortality versus T2DM alone [ 24 ].
The direct renal effect on cardiovascular disease is due to generalised inflammatory change, cardiac remodelling, narrowing of the arteries and vascular calcification, both contributing to the acceleration of vascular ageing and atherosclerotic processes, and leading to myocardial infarction, stroke and HF [ 26 ].
Together, these studies highlight the strong relationship which exists between CKD progression, number of comorbidities and heightened risk of cardiovascular disease and cardiovascular-related mortality.
Economic Burden of CKD
In addition to the clinical burden, management of CKD also requires significant healthcare resources and utilisation. In 2009–2010, the estimated cost of CKD to the National Health Service (NHS) in England was £1.45 billion [ 27 ]. Furthermore, in 2016, US Medicare combined expenditure for CKD and ESKD exceeded $114 billion (£86 billion) [ 28 ].
Although estimating the true cost of early CKD is difficult because of the lack of data available for unreported cases, CKD progression is associated with increased healthcare costs [ 29 , 30 ]. A study by Honeycutt et al. combined laboratory data from NHANES with expenditure data from Medicare and found that costs of CKD management increased with disease progression [ 29 ]. Estimated annual medical costs of CKD per person were not significant at stage 1, $1700 at stage 2, $3500 at stage 3 and $12,700 at stage 4.
Healthcare costs associated with early CKD are more likely to be from the sequalae of comorbid disease rather than kidney disease. Hence, patients with CKD stage 1 or 2 are at increased risk of hospitalisation if they also have T2DM (9%), cardiovascular disease (more than twofold), and both cardiovascular disease and T2DM (approximately fourfold) [ 31 ].
ESKD accounts for the largest proportion of CKD management costs. In 2009–2010, 50% of the overall CKD cost to NHS (England) was due to renal replacement therapy (RRT), which accounted for 2% of the CKD population [ 27 ]. The other 50% included renal primary care costs, such as treatment costs for hypertension and tests, consultation costs, non-renal care attributable to CKD and renal secondary care costs. Approximately £174 million was estimated for the annual cost of myocardial infarctions and strokes associated with CKD [ 27 ].
More recently, an economic analysis investigated the burden associated with the management of cardiovascular-related morbidity and mortality in CKD, according to the KDIGO categorisation of both eGFR and albuminuria [ 15 ]. Decreased eGFR levels increased both the risk of adverse clinical outcomes and economic costs, and albuminuria elevated this risk significantly. Furthermore, CKD progression correlated with increased CKD management costs and bed days. Stage 5 CKD (versus stage 1 (or without) CKD) per 1000 patient years was associated with £435,000 in additional costs and 1017 bed days.
The significant economic burden associated with CKD progression and ESKD highlights the importance of optimising CKD management and the unmet need for better treatment options in slowing disease progression in this patient population. Thus, early detection and intervention to slow the progression of the disease has the potential to make substantial savings in healthcare costs.
Current CKD Management Strategies
KDIGO and National Institute for Health and Care Excellence (NICE) have produced detailed guidelines for the evaluation and management of CKD [ 3 , 32 , 33 ]. Both recommend implementing strategies for early diagnosis of the disease in order to reduce the risk of cardiovascular disease, attenuate CKD progression and decrease the incidence of ESKD in this patient population. CKD is a complex disease and thus treatment requires a multifaceted approach utilising both non-pharmacological, e.g. diet and exercise regimes and pharmacological interventions such as antihypertensive and antihyperglycemic drugs [ 34 ]. There has, however, been no significant breakthrough in this area for over 2 decades.
The effect of lifestyle intervention on reducing disease progression is still unclear, although increased physical activity has been shown to slow the rate of eGFR decline [ 35 ] and ESKD progression [ 36 ], improve eGFR levels [ 35 ] and albuminuria [ 37 ], and reduce mortality in patients with CKD [ 35 , 38 – 40 ]. Similarly, diet regimes such as low-protein diet or Mediterranean diet reduce renal function decline and mortality rate in CKD [ 41 , 42 ]. Hence, dietary advice is recommended in accordance with CKD severity to control for daily calorie, salt, potassium, phosphate and protein intake [ 3 , 33 ]. However, patients with consistently elevated serum phosphate levels or metabolic acidosis [low serum bicarbonate levels (< 22 mmol/l)], associated with increased risk of CKD progression and death, may be treated with phosphate binding agents (e.g. aluminium hydroxide and calcium carbonate) or sodium bicarbonate, respectively [ 3 ].
To reduce the risk of cardiovascular disease, KDIGO and NICE recommend active lipid management and blood pressure control [ 33 , 43 , 44 ]. In early CKD stages 1 and 2, statins are recommended for all patients over 50 years of age, whilst in stage 3 and advanced stages of the disease, stage 4–5 (eGFR < 60 mL/min per 1.73 m 2 ), a combination of statins and ezetimibe is advised [ 43 ].
Management of hypertension includes a target blood pressure of less than 140/90 mmHg for patients with CKD and hypertension and less than 130/80 mmHg for patients with CKD and T2DM, and also in patients with albuminuria [ 3 , 32 ], alongside blood pressure lowering therapies and renin–angiotensin–aldosterone system (RAAS) blocking agents, such as angiotensin receptor blockers (ARB) or angiotensin-converting enzyme inhibitors (ACEi). As such, RAAS inhibitors (RAASi) are currently recommended to treat patients with diabetes, hypertension and albuminuria in CKD [ 45 ]. These RAAS blocking agents confer both renal and cardiovascular protection and are recommended as first-line treatment to treat hypertension in patients with CKD [ 34 , 46 ].
The clinical benefits of RAASi have been demonstrated in patients with CKD with and without diabetes [ 47 – 49 ]. These clinical benefits are in addition to their effects on reducing blood pressure and albuminuria, including a reduction in eGFR decline and a decreased risk of ESKD cardiac-related morbidity and all-cause mortality [ 47 – 49 ]. Nevertheless, despite their benefits, RAASi treatment can induce hyperkalaemia, and patients are often advised to reduce RAASi dosage or even discontinue their treatment, which prevents optimum clinical benefits of RAASi therapy being reached. In this instance, combination therapy with potassium binding agents, such as patiromer and sodium zirconium cyclosilicate, may be used alongside RAASi therapy to reduce RAASi-associated hyperkalaemia.
However long-term trials will be required to determine their effect on cardiovascular morbidity and mortality in CKD [ 50 – 52 ]. Despite these therapies being the mainstay of CKD management, there is still a residual risk of CKD progression and an unmet need for new treatments.
Novel/Emerging Treatments for CKD Management
Over the last 2 years, novel therapeutic approaches for CKD management have emerged, with particular attention on mineralocorticoid receptor antagonists (MRAs) and sodium–glucose co-transporter 2 (SGLT2) inhibitors. The clinical effectiveness of finerenone, a selective oral, non-steroidal MRA, has recently been demonstrated to lower risks of CKD progression and cardiovascular events in diabetic kidney disease (DKD) [ 53 ]. Finerenone is under review for approval by the European Medicines Agency (EMA) and US Food and Drug Administration (FDA).
Of these new and emerging therapies, SGTL2i offers the most clinical benefit with both cardiovascular and renal protective effects, independent of glucose lowering. Clinical trials of SGTL2 in T2DM with and without CKD overall showed a 14–31% reduction in cardiovascular endpoints including hospitalisation for HF and MACE and a 34–37% reduction in hard renal-specific clinical endpoints including a sustained reduction in eGFR, progression of albuminuria and progression to ESKD [ 54 – 58 ]. CREDENCE, was a double-blind, multicentre, randomised trial in diabetic patients with albuminuric CKD (eGFR 30 to < 90 mL/min per 1.73 m 2 and ACR ≥ 30 mg/mmol) [ 57 ]. In this trial, canagliflozin reduced the relative risk of the composite of ESKD, doubling of serum creatinine and renal-related mortality by 34%, relative risk of ESKD by 34% and risk of cardiovascular-related morbidity, including myocardial infarction and stroke, and mortality.
The SGTL2i dapagliflozin has proven its effectiveness in slowing CKD progression in addition to reducing cardiovascular risk in early stages of CKD. The DECLARE-TIMI58 trial involved 17,160 diabetic patients with established atherosclerotic cardiovascular disease and early-stage CKD (mean eGFR was 85.2 mL/min per 1.73 m 2 ) and were randomised to receive either dapagliflozin or placebo. Following a median follow-up of 4.2 years, there was a significant reduction in renal composite endpoints with dapagliflozin versus placebo, with a 46% reduction in sustained decline of at least 40% eGFR to less than 60 mL/min per 1.73 m 2 and a reduction in ESKD (defined as dialysis for at least 90 days, kidney transplantation, or confirmed sustained eGFR < 15 mL/min per 1.73 m 2 ) or renal death.
More recently, these cardiovascular and renal protective effects of SGTLT2i have also been demonstrated in a broad range of patients with more advanced stages of CKD (mean eGFR was 43.1 ± 12.4 mL/min per 1.73 m 2 ) without diabetes [ 58 , 59 ]. In the DAPA-CKD trial, many patients were without diabetes, including IgA nephropathy, ischemic/hypertension nephropathy and other glomerulonephritis [ 59 ]. Patients receiving dapagliflozin had a 39% relative risk reduction in the primary composite outcomes of a sustained decline in eGFR of at least 50%, ESKD and renal- or cardiovascular-related mortality and a 31% relative risk reduction of all-cause mortality compared to placebo [ 58 , 60 ]. Safety outcomes from clinical trials of dapagliflozin have also shown similar incidences of adverse events in both placebo and dapagliflozin arms [ 58 , 61 ].
The clinical benefits and safety outcomes from these trials highlight the potential use of SGTL2i in reducing cardiovascular burden and CKD progression in a broad range of CKD aetiologies at early and late stages where there is an unmet need. Currently, SGTL2i class drugs, including canagliflozin, dapagliflozin and empagliflozin, are approved by the US FDA for the treatment of T2DM and, more recently, dapagliflozin and canagliflozin for CKD and DKD respectively [ 62 , 63 ]. In addition, SGTL2i has been recommended for approval in the European Union (EU) by the Committee for Medicinal Products for Human Use (CHMP) of the EMA, for the treatment of CKD in adults with and without T2D [ 64 ]. Hence, there is now a need to raise awareness of the clinical applicability of these drugs in CKD to ensure full utilisation and maximum benefits are met, for both patients and providers.
This narrative review has summarised some of the key challenges associated with CKD. Early stages of the disease are clinically silent which prevents early intervention to slow the progression of the disease and allows progression of CKD and ESKD. At advanced stages of the disease, when clinical symptoms are present, patients with CKD are already at heightened risk of cardiovascular-related morbidity and mortality. Hence, advanced stages of CKD and ESKD are associated with poor outcomes and a significant clinical and economic burden.
At present, there are no treatments to cure CKD; as such, strategies for CKD management have been developed to target the modifiable risk factors in order to reduce cardiovascular disease morbidity in patients with CKD and slow the progression of CKD to ESKD. However, despite available treatment options, residual risk of adverse events and CKD progression remain; hence, an unmet need exists in CKD treatment. SGTL2i have the potential to fill this gap, with recent evidence from clinical trials showing a reduction in cardiovascular and renal adverse endpoints in a broad range of patients with CKD.
Acknowledgements
This manuscript was supported by a grant from AstraZeneca UK Ltd. in respect of medical writing and publication costs (the journal’s Rapid Service and Open Access Fees). AstraZeneca has not influenced the content of the publication, and has reviewed this document for factual accuracy only.
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authors’ Contributions
All authors have been involved in design of this review. Marc Evans, Ruth D. Lewis, and Angharad R. Morgan produced the primary manuscript. All authors have contributed to the drafting and revision of the manuscript and have approved the final version for publication. Marc Evans is responsible for the integrity of the work as a whole.
Disclosures
Marc Evans reports honoraria from AstraZeneca, Novo Nordisk, Takeda and NAPP, and research support from Novo Nordisk outside the submitted work. Ruth D. Lewis and Angharad R Morgan are employees of Health Economics and Outcomes Research Ltd., Cardiff, UK who received fees from AstraZeneca in relation to this study. Martin B. Whyte reports investigator-led research grants from Sanofi, Eli Lilly and AstraZeneca and personal fees from AstraZeneca, Boehringer Ingelheim and MSD outside the submitted work. Wasim Hanif reports grants and personal fees from AstraZeneca, grants and personal fees from Boerhinger Inglhiem, grants and personal fees from NAPP, from MSD, outside the submitted work. Stephen C. Bain reports personal fees and other from Abbott, personal fees and other from AstraZeneca, personal fees and other from Boehringer Ingelheim, personal fees and other from Eli Lilly, personal fees and other from Merck Sharp & Dohme, personal fees and other from Novo Nordisk, personal fees and other from Sanofi-aventis, other from Cardiff University, other from Doctors.net, other from Elsevier, other from Onmedica, other from Omnia-Med, other from Medscape, other from All-Wales Medicines Strategy Group, other from National Institute for Health and Care Excellence (NICE) UK, and other from Glycosmedia, outside the submitted work. PAK reports personal fees for lecturing from AstraZeneca, Boehringer Inglhiem, NAPP, MundiPharma and Novo Nordisk outside the submitted work. Sarah Davies has received honorarium from AstraZeneca, Boehringer Ingelheim, Lilly, Novo Nordisk, Takeda, MSD, NAPP, Bayer and Roche for attending and participating in educational events and advisory boards, outside the submitted work. Umesh Dashora reports personal fees from AstraZeneca, NAPP, Sanofi, Boehringer Inglhiem, Lilly and Novo Nordisk, outside the submitted work. Zaheer Yousef reports personal fees from AstraZeneca, personal fees from Lilly, personal fees from Boehringer Ingelheim and personal fees from Novartis outside the submitted work. Dipesh C. Patel reports personal fees from AstraZeneca, personal fees from Boehringer Ingelheim, personal fees from Eli Lilly, non-financial support from NAPP, personal fees from Novo Nordisk, personal fees from MSD, personal fees and non-financial support from Sanofi outside the submitted work. In addition, DCP is an executive committee member of the Association of British Clinical Diabetologists and member of the CaReMe UK group. W. David Strain holds research grants from Bayer, Novo Nordisk and Novartis and has received speaker honoraria from AstraZeneca, Bayer, Bristol-Myers Squibb, Merck, NAPP, Novartis, Novo Nordisk and Takeda. WDS is supported by the NIHR Exeter Clinical Research Facility and the NIHR Collaboration for Leadership in Applied Health Research and Care (CLAHRC) for the South West Peninsula.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.

IMAGES
VIDEO
COMMENTS
1. Introduction. Kidney cancer is the 15th most common cancer worldwide, with a significantly higher incidence in developed countries .And the incidence is projected to rise in coming years , .In Europe, kidney cancer was responsible for >50 000 deaths in 2018 , .Early detection and screening have been identified as priorities for kidney cancer research , .
In the early stages, most people don't have signs or symptoms. Kidney cancer is usually found by chance during an abdominal (belly) imaging test for other complaints. As the tumor grows, you may have: Blood in the urine. Pain in the lower back. A lump in the lower back or side of the waist.
Kidney cancer, also known as renal cancer, is a group of cancers that starts in the kidney. [4] Symptoms may include blood in the urine, a lump in the abdomen, or back pain. [1] [2] [3] Fever, weight loss, and tiredness may also occur. [1] [2] [3] Complications can include spread to the lungs or brain. [6]
Symptoms. Kidney cancer usually doesn't have signs or symptoms in its early stages. In time, signs and symptoms may develop, including: Blood in your urine, which may appear pink, red or cola colored. Pain in your back or side that doesn't go away. Loss of appetite.
Essay On Kidney Cancer. 1221 Words 5 Pages. Kidney cancer Kidney cancer, also called as renal cancer is a disorder in which the kidney cells grow out of control, thus becoming malignant and forming a tumor. These are initially formed in the lining of the tubules of the kidney. This type of kidney cancer is called Renal Cell Carcinoma.
Age and Sex. Incidence rates of kidney cancer increase steadily with age, with a peak of incidence at approximately age 75 years. 4,5 Worldwide, approximately one half of all cases are diagnosed before age 65 years. 2 The incidence of kidney cancer is two-fold higher in men compared with women. 6 This pattern has been reported repeatedly over time, across countries, and by age groups, and has ...
Abstract. The management of metastatic renal cell carcinoma (RCC) has evolved rapidly in recent years with several immunotherapy-based combinations of strategies approved as first-line therapies. Targeted strategies, including systemic antiangiogenesis agents and immune checkpoint blockade, form the basis of a therapeutic approach.
Renal cell carcinoma. Renal cell carcinoma (RCC), also known as renal cell cancer or renal cell adenocarcinoma, is the most common type of kidney cancer. About 9 out of 10 kidney cancers are renal cell carcinomas. Although RCC usually grows as a single tumor within a kidney, sometimes there are 2 or more tumors in one kidney or even tumors in ...
3. Cancer therapy can have both a negative and positive impact on patient outcome because of the adverse effects on renal function. Kidney diseases in patients with cancer are associated with higher morbidity and mortality; in particular, for patients requiring renal replacement therapy because of acute kidney injury.
In Europe, mortality from renal cell carcinoma peaked at 4·8 per 100 000 in 1990-94 and had declined to 4·1 per 100 000 (−13%) in 2000-04. 5. In the USA, 5-year relative survival rates at diagnosis increased from 50% in 1975-77 to 57% in 1987-89, and reached 73% in 2003-09. 3.
Stage IV kidney tumor Enlarge image. Tests and procedures used to diagnose kidney cancer include: Blood and urine tests. Tests of your blood and your urine may give your doctor clues about what's causing your signs and symptoms. Imaging tests. Imaging tests allow your doctor to visualize a kidney tumor or abnormality.
Renal cancer articles from across Nature Portfolio. Renal cancer refers to all malignancies that occur within the kidney. Subtypes include renal cell carcinoma and Wilms tumours. Renal cell carcinoma.
Kidney Cancer Essay. Decent Essays. 2558 Words. 11 Pages. Open Document. Pathophysiology: Your kidneys are two bean-shaped organs, each about the size of your fist. They're located behind your abdominal organs, one on each side of your spine. Like other major organs in the body, the kidneys can sometimes develop cancer.
Kidney Cancer is a Metabolic Disease. Marston Linehan provided an overview on the genetic basis of kidney cancer and noted that there are currently at least twelve well studied genes known to cause kidney cancer: VHL, MET, FLCN, fumarate hydratase, succinate dehydrogenase B, succinate dehydrogenase D, TFE3, TFEB, MITF, TSC1, TSC2 and PTEN.Each of these genes is involved in the cell's ability ...
Kidney cancer signs and symptoms. In its early stages, kidney cancer often does not produce any symptoms. Symptoms may include: blood in the urine or passing urine frequently or during the night, change in urine colour - dark, rusty or brown. pain or a dull ache in the side or lower back that is not due to an injury.
Renal cancer: overdiagnosis and overtreatment. Renal cell carcinoma (RCC) accounts for approximately 4.1% of all new cancers, with a median age at diagnosis of 64 years. In 2020, around 73,750 new cases were expected to be diagnosed in the United States, with an age-adjusted rate of 16.3 cases/100.000 persons [ 1 ].
See Advances in Kidney Cancer Research for an overview of recent findings and progress, plus ongoing projects supported by NCI. In a clinical trial, an injectable form of nivolumab (Opdivo) was as effective against kidney cancer as the intravenous form of the drug. Side effects were also similar and treatment time was shorter.
Introduction. Kidney cancer is among the many forms of cancerous conditions that manifest in the human body. Renal cell carcinoma as it is referred in the medical world describes the situation where the kidney cells become malignant. The formation of cancer can take two different forms. One of the forms develops when the kidney cells grow ...
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers. ... Kidney cancer is the 13th most common malignancy worldwide, and its incidence is increasing every year. Renal cell carcinomas (RCC) are a heterogeneous group of kidney tumors, composed of ...
The most common type of cancer arising in the kidney is renal cell carcinoma (aka hypernephroma or Grawitz tumor), making up more than 9 out of 10 renal cancers in adults. Other types include transitional cell carcinomas of the renal pelvis, which behave like bladder cancers. Renal sarcoma is another rare tumor of the kidney. This review will focus mainly on renal cell carcinoma (RCC), which ...
Kidney cancer is among the 10 most common cancers in both men and women. About 81,000 people will be diagnosed with it this year. A decade ago, advanced kidney cancer was a death sentence, but now ...
RESULTS Distribution of cases and deaths by world region and cancer types. Figure 2 presents the distribution of new cases and deaths according to world region for both sexes combined and for men and women separately. For both sexes combined, there were an estimated 20.0 million new cases worldwide (19.96 million including NMSC and 18.73 million excluding NMSC) and 9.7 million cancer deaths (9 ...
The International Agency for Research on Cancer has classified the consumption of heat-processed meat as a direct human carcinogen and the consumption of red meat as a probable carcinogen. Mutagenic and carcinogenic compounds present in meat dishes include, among others, polycyclic aromatic hydrocarbons (PAHs) and heterocyclic aromatic amines (HAAs). These compounds can cause the development ...
Renal medullary carcinoma (rmc) is a rare and aggressive cancer of the kidney that primarily affects adolescents and young adults with sickle cell trait (sct). It was first described by Davis et al. in 1995 1.
But by the age of 49, he had developed kidney cancer, lost his ability to walk, and died. ... Guest Essays; Letters; Sunday Opinion; Opinion Video; Arts. Today's Arts; Art & Design; Books;
The Biology of Cancer. Cancer is a disease that begins with genetic and epigenetic alterations occurring in specific cells, some of which can spread and migrate to other tissues. 4 Although the biological processes affected in carcinogenesis and the evolution of neoplasms are many and widely different, we will focus on 4 aspects that are particularly relevant in tumor biology: genomic and ...
Chronic kidney disease (CKD) is a complex disease which affects approximately 13% of the world's population. Over time, CKD can cause renal dysfunction and progression to end-stage kidney disease and cardiovascular disease. Complications associated with CKD may contribute to the acceleration of disease progression and the risk of ...