

Introduction to qualitative nursing research
This type of research can reveal important information that quantitative research can’t.
- Qualitative research is valuable because it approaches a phenomenon, such as a clinical problem, about which little is known by trying to understand its many facets.
- Most qualitative research is emergent, holistic, detailed, and uses many strategies to collect data.
- Qualitative research generates evidence and helps nurses determine patient preferences.
Research 101: Descriptive statistics
Differentiating research, evidence-based practice, and quality improvement
How to appraise quantitative research articles
All nurses are expected to understand and apply evidence to their professional practice. Some of the evidence should be in the form of research, which fills gaps in knowledge, developing and expanding on current understanding. Both quantitative and qualitative research methods inform nursing practice, but quantitative research tends to be more emphasized. In addition, many nurses don’t feel comfortable conducting or evaluating qualitative research. But once you understand qualitative research, you can more easily apply it to your nursing practice.
What is qualitative research?
Defining qualitative research can be challenging. In fact, some authors suggest that providing a simple definition is contrary to the method’s philosophy. Qualitative research approaches a phenomenon, such as a clinical problem, from a place of unknowing and attempts to understand its many facets. This makes qualitative research particularly useful when little is known about a phenomenon because the research helps identify key concepts and constructs. Qualitative research sets the foundation for future quantitative or qualitative research. Qualitative research also can stand alone without quantitative research.
Although qualitative research is diverse, certain characteristics—holism, subjectivity, intersubjectivity, and situated contexts—guide its methodology. This type of research stresses the importance of studying each individual as a holistic system (holism) influenced by surroundings (situated contexts); each person develops his or her own subjective world (subjectivity) that’s influenced by interactions with others (intersubjectivity) and surroundings (situated contexts). Think of it this way: Each person experiences and interprets the world differently based on many factors, including his or her history and interactions. The truth is a composite of realities.
Qualitative research designs
Because qualitative research explores diverse topics and examines phenomena where little is known, designs and methodologies vary. Despite this variation, most qualitative research designs are emergent and holistic. In addition, they require merging data collection strategies and an intensely involved researcher. (See Research design characteristics .)
Although qualitative research designs are emergent, advanced planning and careful consideration should include identifying a phenomenon of interest, selecting a research design, indicating broad data collection strategies and opportunities to enhance study quality, and considering and/or setting aside (bracketing) personal biases, views, and assumptions.
Many qualitative research designs are used in nursing. Most originated in other disciplines, while some claim no link to a particular disciplinary tradition. Designs that aren’t linked to a discipline, such as descriptive designs, may borrow techniques from other methodologies; some authors don’t consider them to be rigorous (high-quality and trustworthy). (See Common qualitative research designs .)
Sampling approaches
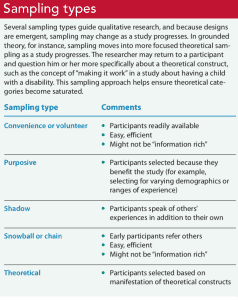
Sampling approaches depend on the qualitative research design selected. However, in general, qualitative samples are small, nonrandom, emergently selected, and intensely studied. Qualitative research sampling is concerned with accurately representing and discovering meaning in experience, rather than generalizability. For this reason, researchers tend to look for participants or informants who are considered “information rich” because they maximize understanding by representing varying demographics and/or ranges of experiences. As a study progresses, researchers look for participants who confirm, challenge, modify, or enrich understanding of the phenomenon of interest. Many authors argue that the concepts and constructs discovered in qualitative research transcend a particular study, however, and find applicability to others. For example, consider a qualitative study about the lived experience of minority nursing faculty and the incivility they endure. The concepts learned in this study may transcend nursing or minority faculty members and also apply to other populations, such as foreign-born students, nurses, or faculty.
Qualitative nursing research can take many forms. The design you choose will depend on the question you’re trying to answer.
A sample size is estimated before a qualitative study begins, but the final sample size depends on the study scope, data quality, sensitivity of the research topic or phenomenon of interest, and researchers’ skills. For example, a study with a narrow scope, skilled researchers, and a nonsensitive topic likely will require a smaller sample. Data saturation frequently is a key consideration in final sample size. When no new insights or information are obtained, data saturation is attained and sampling stops, although researchers may analyze one or two more cases to be certain. (See Sampling types .)
Some controversy exists around the concept of saturation in qualitative nursing research. Thorne argues that saturation is a concept appropriate for grounded theory studies and not other study types. She suggests that “information power” is perhaps more appropriate terminology for qualitative nursing research sampling and sample size.
Data collection and analysis
Researchers are guided by their study design when choosing data collection and analysis methods. Common types of data collection include interviews (unstructured, semistructured, focus groups); observations of people, environments, or contexts; documents; records; artifacts; photographs; or journals. When collecting data, researchers must be mindful of gaining participant trust while also guarding against too much emotional involvement, ensuring comprehensive data collection and analysis, conducting appropriate data management, and engaging in reflexivity.
Data usually are recorded in detailed notes, memos, and audio or visual recordings, which frequently are transcribed verbatim and analyzed manually or using software programs, such as ATLAS.ti, HyperRESEARCH, MAXQDA, or NVivo. Analyzing qualitative data is complex work. Researchers act as reductionists, distilling enormous amounts of data into concise yet rich and valuable knowledge. They code or identify themes, translating abstract ideas into meaningful information. The good news is that qualitative research typically is easy to understand because it’s reported in stories told in everyday language.
Evaluating a qualitative study
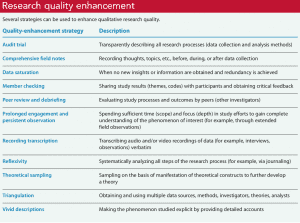
Evaluating qualitative research studies can be challenging. Many terms—rigor, validity, integrity, and trustworthiness—can describe study quality, but in the end you want to know whether the study’s findings accurately and comprehensively represent the phenomenon of interest. Many researchers identify a quality framework when discussing quality-enhancement strategies. Example frameworks include:
- Trustworthiness criteria framework, which enhances credibility, dependability, confirmability, transferability, and authenticity
- Validity in qualitative research framework, which enhances credibility, authenticity, criticality, integrity, explicitness, vividness, creativity, thoroughness, congruence, and sensitivity.
With all frameworks, many strategies can be used to help meet identified criteria and enhance quality. (See Research quality enhancement ). And considering the study as a whole is important to evaluating its quality and rigor. For example, when looking for evidence of rigor, look for a clear and concise report title that describes the research topic and design and an abstract that summarizes key points (background, purpose, methods, results, conclusions).
Application to nursing practice
Qualitative research not only generates evidence but also can help nurses determine patient preferences. Without qualitative research, we can’t truly understand others, including their interpretations, meanings, needs, and wants. Qualitative research isn’t generalizable in the traditional sense, but it helps nurses open their minds to others’ experiences. For example, nurses can protect patient autonomy by understanding them and not reducing them to universal protocols or plans. As Munhall states, “Each person we encounter help[s] us discover what is best for [him or her]. The other person, not us, is truly the expert knower of [him- or herself].” Qualitative nursing research helps us understand the complexity and many facets of a problem and gives us insights as we encourage others’ voices and searches for meaning.
When paired with clinical judgment and other evidence, qualitative research helps us implement evidence-based practice successfully. For example, a phenomenological inquiry into the lived experience of disaster workers might help expose strengths and weaknesses of individuals, populations, and systems, providing areas of focused intervention. Or a phenomenological study of the lived experience of critical-care patients might expose factors (such dark rooms or no visible clocks) that contribute to delirium.
Successful implementation
Qualitative nursing research guides understanding in practice and sets the foundation for future quantitative and qualitative research. Knowing how to conduct and evaluate qualitative research can help nurses implement evidence-based practice successfully.
When evaluating a qualitative study, you should consider it as a whole. The following questions to consider when examining study quality and evidence of rigor are adapted from the Standards for Reporting Qualitative Research.
Jennifer Chicca is a PhD candidate at the Indiana University of Pennsylvania in Indiana, Pennsylvania, and a part-time faculty member at the University of North Carolina Wilmington.
Amankwaa L. Creating protocols for trustworthiness in qualitative research. J Cult Divers. 2016;23(3):121-7.
Cuthbert CA, Moules N. The application of qualitative research findings to oncology nursing practice. Oncol Nurs Forum . 2014;41(6):683-5.
Guba E, Lincoln Y. Competing paradigms in qualitative research . In: Denzin NK, Lincoln YS, eds. Handbook of Qualitative Research. Thousand Oaks, CA: SAGE Publications, Inc.;1994: 105-17.
Lincoln YS, Guba EG. Naturalistic Inquiry . Thousand Oaks, CA: SAGE Publications, Inc.; 1985.
Munhall PL. Nursing Research: A Qualitative Perspective . 5th ed. Sudbury, MA: Jones & Bartlett Learning; 2012.
Nicholls D. Qualitative research. Part 1: Philosophies. Int J Ther Rehabil . 2017;24(1):26-33.
Nicholls D. Qualitative research. Part 2: Methodology. Int J Ther Rehabil . 2017;24(2):71-7.
Nicholls D. Qualitative research. Part 3: Methods. Int J Ther Rehabil . 2017;24(3):114-21.
O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: A synthesis of recommendations. Acad Med . 2014;89(9):1245-51.
Polit DF, Beck CT. Nursing Research: Generating and Assessing Evidence for Nursing Practice . 10th ed. Philadelphia, PA: Wolters Kluwer; 2017.
Thorne S. Saturation in qualitative nursing studies: Untangling the misleading message around saturation in qualitative nursing studies. Nurse Auth Ed. 2020;30(1):5. naepub.com/reporting-research/2020-30-1-5
Whittemore R, Chase SK, Mandle CL. Validity in qualitative research. Qual Health Res . 2001;11(4):522-37.
Williams B. Understanding qualitative research. Am Nurse Today . 2015;10(7):40-2.
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Post Comment

NurseLine Newsletter
- First Name *
- Last Name *
- Hidden Referrer
*By submitting your e-mail, you are opting in to receiving information from Healthcom Media and Affiliates. The details, including your email address/mobile number, may be used to keep you informed about future products and services.
Test Your Knowledge
Recent posts.

Why COVID-19 patients who could most benefit from Paxlovid still aren’t getting it

Human touch

Leadership style matters

My old stethoscope

Nurse referrals to pharmacy

Lived experience

The nurse’s role in advance care planning

High school nurse camp

The transformational role of charge nurses in the post-pandemic era

Health Care Workers Push for Their Own Confidential Mental Health Treatment

Do We Simply Not Care About Old People?

Healthcare’s role in reducing gun violence

Early Release: Nurses and firearm safety

Gun violence: A public health issue

Eating disorders are the most lethal mental health conditions – reconnecting with internal body sensations can help reduce self-harm
- Technical Support
- Find My Rep
You are here
Global Qualitative Nursing Research
Preview this book.
- Description
- Aims and Scope
- Editorial Board
- Abstracting / Indexing
- Submission Guidelines
Journal Highlights
- Indexed in: Emerging Sources Citation Index (ESCI), PubMed Central (PMC) and Scopus
- Publication is subject to payment of an article processing charge (APC)
- Submit here
Global Qualitative Nursing Research (GQNR) is an open access peer reviewed journal focusing on qualitative research in fields relevant to nursing and other health professionals worldwide. Please see the Aims and Scope tab for further information. This journal is a member of the Committee on Publication Ethics (COPE). Submission information Submit your manuscript at https://mc.manuscriptcentral.com/gqn Please see the Submission Guidelines tab for more information on how to submit your article to the journal. Open access article processing charge (APC) information Publication in the journal is subject to payment of an article processing charge (APC). The APC serves to support the journal and ensures that articles are freely accessible online in perpetuity under a Creative Commons licence. Members of the International Institute for Qualitative Methodology are entitled to a 25% discount on the APC. The article processing charge (APC) for this journal is is 2000 USD. Contact Please direct any queries to [email protected] Special Sections Global Qualitative Nursing Research has the following special sections open for submission and publication:
- Methodological Development
- Advancing Theory/Metasynthesis
- Establishing Evidence
- Application to Practice
Translations Authors can publish translated versions of their article alongside the English version. Please see Submission Guidelines Section 6 for more details.
GQNR will publish research articles using qualitative methods and qualitatively-driven mixed-method designs as well as meta-syntheses and articles focused on methodological development. Special sections include Ethics, Methodological Development, Advancing Theory/Metasynthesis, Establishing Evidence, and Application to Practice.
- Clarivate Analytics: Emerging Sources Citation Index (ESCI)
- Directory of Open Access Journals (DOAJ)
- Google Scholar: h-5 index - 11, h-5 median - 13
- PubMed Central (PMC)
Global Qualitative Nursing Research (GQNR) is an international, interdisciplinary, refereed journal focusing on qualitative research in fields relevant to nursing world-wide. The journal specializes in topics related to nursing practice, responses to health, illness, and disability, health promotion, healthcare delivery, and global issues that affect nursing and healthcare. GQNR also welcomes qualitative studies pertinent to nursing that advance knowledge of diversity and systemic biases (e.g., racism), including the intersection of multiple oppressions and social identities, that shape experiences of health and illness, nursing and healthcare, and their implications for health equity. The journal provides a forum for sharing qualitative research from around the world that has international relevance for nursing.
GQNR will publish qualitative methods research, qualitatively-driven mixed-method designs, as well as meta-syntheses and articles focused on methodological developments. Each article accepted by peer review is made freely available online immediately upon publication, is published under a Creative Commons license and will be hosted online in perpetuity. Publication costs of the journal are covered by the collection of article processing charges which are paid by the funder, institution or author of each manuscript upon acceptance. There is no charge for submitting a paper to the journal.
The following author guidelines are designed assist authors with the manuscript preparation and submission process. Please note that manuscripts not conforming to these guidelines may be returned. Only manuscripts of sufficient quality that meet the aims and scope of Global Qualitative Nursing Research will be reviewed.
Sage Publishing disseminates high-quality research and engaged scholarship globally, and we are committed to diversity and inclusion in publishing. We encourage submissions from a diverse range of authors from across all countries and backgrounds.
Manuscript Submission Guidelines: Global Qualitative Nursing Research
- Open Access
- Article processing charge (APC)
- What do we publish? 3.1 Aims & Scope 3.2 Article types 3.3 Writing your paper 3.3.1 Making your article discoverable
- Editorial policies 4.1 Peer review policy 4.2 Authorship 4.3 Acknowledgements 4.4 Writing Assistance 4.5 Funding 4.6 Declaration of conflicting interests 4.7 Research ethics and patient consent 4.8 Clinical trials 4.9 Reporting guidelines 4.10 Diversity: Naming and exploring implications of systematic biases in research 4.11 Sex and gender equity in research
- Publishing policies 5.1 Publication ethics 5.2 Contributor’s publishing agreement
- Preparing your manuscript 6.1 Article format 6.2 Word processing formats 6.3 Writing style 6.4 Artwork, figures and other graphics 6.5 Reference style 6.6 English language editing services 6.7 Publishing translated versions of articles 6.8 Supplementary material
- Submitting your manuscript 7.1 Title, keywords and abstracts 7.2 ORCID 7.3 Information required for completing your submission 7.4 Permissions
- On acceptance and publication 8.1 SAGE Production 8.2 Continuous publication 8.3 Promoting your article
- Further information
1. Open Access
Global Qualitative Nursing Research (GQNR) is an open access, international, peer reviewed journal focusing on qualitative research in field relevant to nursing. GQNR will publish qualitative methods research, qualitatively-driven mixed-method designs, as well as meta-syntheses and articles focused on methodological developments. Each article accepted by peer review is made freely available online immediately upon publication, is published under a Creative Commons license and will be hosted online in perpetuity. Publication costs of the journal are covered by the collection of article processing charges which are paid by the funder, institution or author of each manuscript upon acceptance. There is no charge for submitting a paper to the journal.
For general information on open access at SAGE please visit the Open Access page or view our Open Access FAQs .
Back to top
2. Article processing charge (APC)
If, after peer review, your manuscript is accepted for publication, a one-time article processing charge (APC) is payable. This APC covers the cost of publication and ensures that your article will be freely available online in perpetuity under a Creative Commons license.
As of September 5 2023, the article processing charge (APC) is 2000 USD.
Students are entitled to a 75% discount off the current APC as long as they are the first and corresponding author. Validation is required after submission.
Members of the International Institute for Qualitative Methodology are entitled to a 25% discount on the APC.
Please note that all communication concerning the APC should be conducted with SAGE Publications rather than with GQNR.
3. What do we publish?
Global Qualitative Nursing Research welcomes submissions focusing on qualitative research in fields relevant to nursing and are aligned with the aims and scope of the journal outlined here: https://journals.sagepub.com/aims-scope/GQN .
GQNR is a nursing focused journal and regardless of the topic, if intended for nurses, it should reflect a nursing perspective and/or the contribution that nurses bring to interprofessional ways of delivering care. In addition, we encourage authors to use the language of nursing and nurses versus healthcare professionals, providers, and clinicians when referring to nurses.
GQNR is an international journal so the relevance of manuscripts to the subject field internationally and also its transferability into other care settings, cultures or nursing specialties should be considered.
3.1 Aims & Scope
Before submitting your manuscript to Global Qualitative Nursing Research, please ensure you have read the Aims & Scope.
3.2 Article types
Global Qualitative Nursing Research publishes the following types of articles:
- Single-method qualitative research
- Qualitatively-driven mixed-method research
- Qualitative studies that are part of multiple method projects
- Metasynthesis studies that advance theory
- Scoping reviews of qualitative research
- Qualitative methodological development
- Qualitative study protocols
Guidelines for each article type are included below:
Single method qualitative research : GQNR publishes high quality, methodologically rigorous qualitative research that contributes original findings to areas of international relevance for nursing, midwifery or related fields. The journal welcomes qualitative research papers that are based on various qualitative approaches and forms of data. A full description of the qualitative approach is required including the epistemological underpinnings/methodology and methods, and the analytical lens and strategies used in data analysis, and strategies to support rigor.
Qualitative driven mixed method research : GQNR invites articles about studies in which the main study was qualitative, and the supplementary data collection was either qualitative or quantitative (QUAL qant or QUAL qual designs) (for more information see Morse, 2003 , 2010 , 2016 ). Mixed-method studies are studies in which the data collected for a main study is supplemented with data that were collected using a data collection strategy that is not normally used in the main study. For example, a study using a grounded theory design in which laboratory results are added to qualitative data collected would be called a mixed-method study, but the addition of the same kind of quantitative data in an ethnographic study would not be called a mixed-method study, as ethnographies typically include both qualitative and quantitative data. Articles reporting studies designed using a mixed-method approach must include the data from both the main study and the supplemental component. Articles that describe supplemental data only will not be accepted, as the supplemental data cannot stand on its own; it is only interpretable in the context of the main study. Within the description of the design, the authors must include a statement about why a mixed-method approach was used. In the data collection section of the article, the authors must include an explanation about when and how the data from the main study and the supplemental component were integrated (e.g., Taylor, 2020 ).
Qualitative studies within multiple method research projects : GQNR is interested in receiving articles about qualitative studies that are part of multiple method projects, provided they meet the usual criteria for qualitative studies. Multiple method (multimethod) projects are comprised of a group of complete studies that are linked by one overarching aim. These studies may be qualitative or quantitative, are complete and can each stand alone, with separate but complementary research questions that link the study to the overall aim of the project. We also invite articles reporting the results of all the studies within a multiple method project (that include at least one qualitative study) and a description of how the results of each study contribute to the overarching aim of the project (e.g., Porr et al., 2010 ).
Metasynthesis studies that advance theory : Articles are invited that synthesize and interpret data across qualitative studies using relevant and rigorous approaches and make distinctive contributions to the body of evidence for practice. Articles should include inclusion/exclusion processes congruent with aims of the review; data display approaches that support analysis; evidence of critical reflection on the role played by method, theoretical framework, disciplinary orientation, and local conditions in shaping included studies; interpretations that reflect advances in the field over time; and a conceptually, well-integrated set of new findings that make a substantive contribution to the field that extends beyond individual qualitative studies. Systematic or scoping reviews of qualitative studies that simply summarize commonalities among a collection of qualitative studies will not be considered.
Scoping reviews of qualitative research: GQNR invites high quality, rigorous scoping reviews of qualitative research that are conducted for the purpose of identifying gaps in the current qualitative evidence, investigating how qualitative research has been conducted, and identifying areas that require further qualitative inquiry. A compelling rationale for the scoping review is required. Scoping reviews will only be considered if they clearly make a substantive and constructive contribution to the field and nursing and/or advance our thinking about qualitative methods. Possible contributions of scoping reviews of qualitative research include: advancing our thinking about how qualitative research is conducted on a particular topic/field and contributing to method development, clarifying concepts in the literature by examining relevant qualitative research, and mapping qualitative evidence to inform future research. Scoping reviews must be conducted using rigorous and transparent methods. Scoping reviews that include both qualitative and quantitative research will not be considered.
Methodological development : Articles are invited that focus on qualitative methods that provide insights, advances or innovations that are likely to be of interest to qualitative researchers in fields relevant to nursing world-wide. What the paper adds to existing methodological knowledge must be clearly explained.
Qualitative study protocols : To further the development of qualitative methods, GQNR accepts nationally funded study protocols for qualitative or qualitatively-driven mixed method studies that illustrate novel methodological ideas and/or practices. Student proposals / non-funded / locally-funded studies will not be considered. We encourage the submission of protocol manuscripts at an early stage of the study and prior to completion of data collection. Manuscripts that report work already carried out will not be considered as protocols. The dates of the study must be included in the manuscript and cover letter. Articles describing study protocols should include: background/study justification, explanation and justification of method, sampling/recruitment, data management/analysis plan, ethical considerations, and approach to supporting qualitative rigor. A dissemination plan (publications, data deposition and curation) should be included, as well as a discussion about how the methods will meet study aims. Proof of both ethics approval and funding will be required on submission as supplementary files. The inclusion of copies of interview guides and/or field work plans as supplementary files are encouraged. Reviewers will be instructed to review for clarity and sufficient detail. The intention of peer review is not to alter the study design. Reviewers will be asked to check that the study is scientifically credible (i.e., congruence between methodology and methods, strategies to establish rigor, etc.) and ethically sound in its scope and methods, and that there is sufficient detail to instill confidence that the study will be conducted successfully.
3.3 Writing your paper
The SAGE Author Gateway has some general advice and on how to get published , plus links to further resources.
3.3.1 Making your article discoverable
The title, keywords and abstract are key to ensuring readers find your article through search engines such as Google. For information and guidance on how to make your article more discoverable, visit our Gateway page on How to Help Readers Find Your Article Online.
4. Editorial policies
4.1 Peer review policy
SAGE does not permit the use of author-suggested (recommended) reviewers at any stage of the submission process, be that through the web-based submission system or other communication.
Reviewers should be experts in their fields and should be able to provide an objective assessment of the manuscript. Our policy is that reviewers should not be assigned to a paper if:
- The reviewer is based at the same institution as any of the co-authors.
- The reviewer is based at the funding body of the paper.
- The author has recommended the reviewer.
- The reviewer has provided a personal (e.g. Gmail/Yahoo/Hotmail) email account and an institutional email account cannot be found after performing a basic Google search (name, department and institution).
Following a preliminary triage to eliminate submissions unsuitable for Global Qualitative Nursing Research all papers are sent out for peer review. The cover letter is important. To help the Editor in this preliminary evaluation, please indicate in your letter to the editor why you think the paper is suitable for publication and relevant to the subject field internationally.
The journal’s policy is to have manuscripts reviewed by three expert reviewers. Global Qualitative Nursing Research utilizes a double-anonymized peer review process in which the reviewer and authors’ names and information are withheld from the other. All manuscripts are reviewed as rapidly as possible, while maintaining rigor. Reviewers make comments to the author and recommendations to the Editor-in-Chief who then makes the final decision.
GQNR maintains a transparent review system: once all reviews are received, they are forwarded to the author(s) as well as to ALL reviewers.
Global Qualitative Nursing Research is committed to delivering high quality, fast peer-review for your paper, and as such has partnered with Publons. Publons is a third-party service that seeks to track, verify and give credit for peer review. Reviewers for Global Qualitative Nursing Research can opt in to Publons in order to claim their reviews or have them automatically verified and added to their reviewer profile. Reviewers claiming credit for their review will be associated with the relevant journal, but the article name, reviewer’s decision and the content of their review is not published on the site. For more information visit the Publons website.
The Editor or members of the Editorial Board may occasionally submit their own manuscripts for possible publication in the journal. In these cases, the peer review process will be managed by alternative members of the Board and the submitting Editor/Board member will have no involvement in the decision-making process.
4.2 Authorship
Papers should only be submitted for consideration once consent is given by all contributing authors. Those submitting papers should carefully check that all those whose work contributed to the paper are acknowledged as contributing authors. The list of authors should include all those who can legitimately claim authorship. This is all those who:
- Made a substantial contribution to the concept or design of the work; or acquisition, analysis or interpretation of data,
- Drafted the article or revised it critically for important intellectual content,
- Approved the version to be published,
- Each author should have participated sufficiently in the work to take public responsibility for appropriate portions of the content.
Authors should meet the conditions of all of the points above. Each author should have participated sufficiently in the work to take public responsibility for appropriate portions of the content.
When a large, multicenter group has conducted the work, the group should identify the individuals who accept direct responsibility for the manuscript. These individuals should fully meet the criteria for authorship.
Authors should determine the order of authorship among themselves and should settle any disagreements before submitting their manuscript. Changes in authorship (i.e., order, addition, and deletion of authors) should be discussed and approved by all authors. Any requests for such changes in authorship after initial manuscript submission and before publication should be explained in writing to the editor in a letter or email from all authors.
Acquisition of funding, collection of data, or general supervision of the research group alone does not constitute authorship, although all contributors who do not meet the criteria for authorship should be listed in the Acknowledgments section. Please refer to the International Committee of Medical Journal Editors (ICMJE) authorship guidelines for more information on authorship.
4.3 Acknowledgements
All contributors who do not meet the criteria for authorship should be listed in an Acknowledgements section. Examples of those who might be acknowledged include a person who provided purely technical help, or a department chair who provided only general support.
4.4 Writing assistance
Individuals who provided writing assistance, e.g. from a specialist communications company, do not qualify as authors and so should be included in the Acknowledgements section. Authors must disclose any writing assistance – including the individual’s name, company and level of input – and identify the entity that paid for this assistance. It is not necessary to disclose use of language polishing services.
For manuscripts translated into English from another language, the name and affiliation of the translator may also be included. Except on a separate title page, the names of authors, and/or translators should not appear in manuscripts submitted for review; they are to be added only after the article is accepted for publication.
Please supply any personal acknowledgements separately to the main text to facilitate anonymous peer review.
4.5 Funding
To comply with the guidance for research funders, authors, and publishers issued by the Research Information Network (RIN), Global Qualitative Nursing Research requires all authors to acknowledge their funding in a consistent fashion under a heading “Funding.” Please visit the Funding Acknowledgements page on the SAGE Journal Author Gateway to confirm the format of the acknowledgment text in the event of funding, or state that: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
4.6 Declaration of conflicting interests
It is the policy of Global Qualitative Nursing Research to require a declaration of conflicting interests from all authors enabling a statement to be carried within the paginated pages of all published articles.
Please include your declaration at the end of your manuscript after any acknowledgments and prior to the references, under a heading “Declaration of Conflicting Interests.” If no conflict exists, please state that ‘The Author(s) declare(s) that there is no conflict of interest’. For guidance on conflict of interest statements, please see the ICMJE recommendations here .
When making a declaration the disclosure information must be specific and include any financial relationship that any author of the article has with any sponsoring organization and the for profit interests the organization represents, and with any for-profit product discussed or implied in the text of the article.
Any commercial or financial involvements that might represent an appearance of a conflict of interest need to be additionally disclosed in the covering letter accompanying your article, to assist the Editor in evaluating whether sufficient disclosure has been made within the Declaration of Conflicting Interests provided in the article.
4.7 Research ethics and patient consent
Medical research involving human subjects must be conducted according to the World Medical Association Declaration of Helsinki .
Submitted manuscripts should conform to the ICMJE Recommendations for the Conduct, Reporting, Editing, and Publication of Scholarly Work in Medical Journals .
- All papers reporting animal and/or human studies must state in the methods section that the relevant Ethics Committee or Institutional Review Board provided (or waived) approval. Please ensure that you anonymized the name and institution of the review committee until such time as your article has been accepted. The Editor will request authors to replace the name and add the approval number once the article review has been completed.
- For research articles, authors are also required to state in the methods section whether participants provided informed consent and whether the consent was written or verbal.
Global Qualitative Nursing Research is committed to protecting the identity and confidentiality of research study participants. With the exception of participatory action research (PAR), no information that could potentially allow identification of a participant—or even a specific study site—should be included in a submitted manuscript or, subsequently, in a published article. Study sites, such as hospitals, clinics, or other organizations, should not be named, but instead should be described; for example: “Study participants were recruited from the coronary care unit of a large metropolitan hospital on the eastern seaboard of the United States.”
Do not include participant names in the manuscript. If the use of names is absolutely necessary for reader understanding (this is rarely the case), use pseudonyms. Even when using pseudonyms, it should not be possible for the reader to “track” the comments or behaviors of any participant throughout the manuscript.
Authors who include participant names and/or photos/images in which individuals are identifiable must submit written permission from the participants to do so (no exceptions). Permission to use photographs should contain the following verbiage: “Permission is granted to use, reproduce, and distribute the likeness/photograph(s) in all media (print and electronic) throughout the world in all languages.”
Information on informed consent to report individual cases or case series should be included in the manuscript text. A statement is required regarding whether written informed consent for patient information and images to be published was provided by the patient(s) or a legally authorized representative.
Research participants have a right to privacy that should not be infringed upon without informed consent. Identifying information, including participants' names, initials, or other identifying characteristics, should not be published in written descriptions and photographs unless the information is essential for scientific purposes and the participant (or parent or guardian) gives signed and dated written informed consent for publication (submitted as a separate document when submitting the manuscript). Informed consent for this purpose requires that a participant who is identifiable be shown the manuscript to be published prior to giving consent.
Identifying details should be omitted if they are not essential. Faces in photographs should be obscured. If identifying characteristics are altered to protect anonymity, authors should provide assurance that alterations do not distort scientific meaning.
Please also refer to the ICMJE Recommendations for the Protection of Research Participants .
4.8 Clinical trials
Global Qualitative Nursing Research conforms to the ICMJE requirement that clinical trials are registered in a WHO-approved public trials registry at or before the time of first patient enrolment as a condition of consideration for publication. The trial registry name and URL, and registration number must be included at the end of the abstract.
4.9 Reporting guidelines
The relevant EQUATOR Network reporting guidelines should be followed depending on the type of study. Metasyntheses should include the completed PRISMA 2020 flow chart as a cited figure and the completed PRISMA checklist should be uploaded with your submission as a supplementary file. The EQUATOR wizard can help you identify the appropriate guideline. Other resources can be found at NLM’s Research Reporting Guidelines and Initiatives .
4.10 Diversity: Naming and exploring implications of systemic biases in research
GQNR encourages authors to acknowledge and advance understanding of diversity and systematic biases that shape experiences of health, illness, disability, nursing and healthcare, and their implications for health equity. Diversity includes all aspects of human differences such as socioeconomic status, race, ethnicity, language, nationality, sex, gender identity, sexual orientation, religion, geography, ability, age, and culture.
We invite authors to:
- consider diversity in the design, implementation, and evaluation of research
- name and explore implications of systemic biases (e.g., racism, ageism, ableism, and gender bias) as well as the intersection of multiple oppressions and social identities that shape health
- acknowledge the positionality of the researcher(s) in relation to the study context and its influence on the research process
- use non-stigmatizing, respectful person-first language (e.g., person who used opioids vs. opioid user or addict) or identity-first language (e.g., autistic person, deaf person or person with intellectual disability) keeping in mind what is best for representing study participants
Authors have an opportunity to address issues related to diversity in the background section, explain how diversity was accounted for in the study design, and/or how study findings address or do not address issues of diversity or reveal systemic bias and their implications for health equity.
4.11 Sex and gender equity in research
We encourage authors to follow the ‘ Sex and Gender Equity in Research – SAGER – guidelines ’ and to include sex and gender considerations where relevant. Authors should use the terms sex (biological attribute) and gender (shaped by social and cultural circumstances) carefully in order to avoid confusing both terms. Article titles and/or abstracts should indicate clearly what sex(es) the study applies to. Authors should also describe in the background, whether sex and/or gender differences may be expected; report how sex and/or gender were accounted for in the design of the study; provide disaggregated data by sex and/or gender, where appropriate; and discuss respective results. If a sex and/or gender analysis was not conducted, the rationale should be given in the Discussion. Resources related to integrating sex and gender in health research have been developed by the Canadian Institutes of Health Research. They can be freely accessed here: www.cihr-irsc.gc.ca/e/50833.html
5. Publishing policies
5.1 Publication ethics
SAGE is committed to upholding the integrity of the academic record. We encourage authors to refer to the Committee on Publication Ethics’ International Standards for Authors and view the Publication Ethics page on the SAGE Author Gateway .
5.1.1 Plagiarism
Global Qualitative Nursing Research and SAGE take issues of copyright infringement, plagiarism or other breaches of best practice in publication very seriously. We seek to protect the rights of our authors and we always investigate claims of plagiarism or misuse of published articles. Equally, we seek to protect the reputation of the journal against malpractice. Submitted articles may be checked with duplication-checking software. Where an article, for example, is found to have plagiarized other work or included third-party copyright material without permission or with insufficient acknowledgement, or where the authorship of the article is contested, we reserve the right to take action including, but not limited to: publishing an erratum or corrigendum (correction); retracting the article; taking up the matter with the head of department or dean of the author's institution and/or relevant academic bodies or societies; or taking appropriate legal action.
5.1.2 Duplicate and prior publication
Global Qualitative Nursing Research conforms to the ICMJE recommendations regarding duplicate and prior publications . If material has been previously published, it is not generally acceptable for publication in a SAGE journal. However, there are certain circumstances where previously published material can be considered for publication. Please refer to the guidance on the SAGE Author Gateway or if in doubt, contact the Editor at the address given below.
Duplicate publication is publication of a paper that overlaps substantially with one already published, without clear, visible reference to the previous publication. Prior publication may include release of information in the public domain (e.g., preprints).
When authors submit a manuscript reporting work that has already been reported in large part in a published article or is contained in or closely related to another paper that has been submitted or accepted for publication elsewhere, the letter of submission should clearly say so and the authors should provide copies of the related material to help the editor decide how to handle the submission.
Authors who choose to post their work on a preprint server should choose one that clearly identifies preprints as not peer-reviewed work and includes disclosures of authors’ relationships and activities. It is the author’s responsibility to inform a journal if the work has been previously posted on a preprint server. In addition, it is the author’s (and not journal editor’s) responsibility to ensure that preprints are amended to point readers to subsequent versions, including the final published article.
5.2 Contributor’s publishing agreement
Before publication SAGE requires the author as the rights holder to sign a Journal Contributor’s Publishing Agreement. Global Qualitative Nursing Research publishes manuscripts under Creative Commons licenses . The standard license for the journal is Creative Commons by Attribution Non-Commercial (CC BY-NC), which allows others to re-use the work without permission as long as the work is properly referenced and the use is non-commercial. For more information, you are advised to visit SAGE's OA licenses page .
Alternative license arrangements are available, for example, to meet particular funder mandates, made at the author’s request.
6. Preparing your manuscript
The following guidelines are designed to assist authors with the manuscript preparation and submission process. Manuscripts that do not conform to these guidelines will be returned to the authors without further review. The entire manuscript (including tables, figures, and references) must be prepared according to the Publication Manual of the American Psychological Association (APA Style Manual 7th edition).
6.1 Article format (see previously published articles in GQNR for style)
- Title page: Title should be succinct; list all authors and their affiliation; keywords. Please upload the title page separately from the main document.
- Include a short title (no more than 50 characters) as a header on all pages, including the title page, for the purposes of double-anonymized peer-review.
- Anonymized review: Do not include any author identifying information in your manuscript, including authors’ own citations. Do not include acknowledgements until the article is accepted.
- Abstract: Unstructured, 150-200 words . This should be the first page of the main manuscript, and it should be on its own page.
- Key words: Provide 4-6 keywords to highlight the main concepts and the scope of the manuscript. Please include region/country where the study was conducted as a key word if appropriate. Include key words following the abstract.
- Main manuscript text: GQNR does not have a word or page count limit. Manuscripts should be as tight as possible, preferably less than 30 pages including references . Longer manuscripts, if exceptional, will be considered.
- Ethics: Include a statement of IRB approval and participant consent. Present demographics as a group, not listed as individuals. Do not link quotations to particular individuals unless essential (as in case studies) as this threatens anonymity.
- Results: Rich and descriptive; theoretical; linked to practice if possible.
- Discussion: Link your findings with research and theory in literature, including other geographical areas and qualitative research.
- References: APA 7th Edition format. Use pertinent references only. References should be on a separate page.
6.2 Word processing formats
Accepted formats for the text, tables, and figures of submitted manuscripts are MS Word .doc and .docx files. The text must be double-spaced throughout. Set margins at 1 inch on all sides. Text should be in standard font (e.g., Times New Roman) 12-point. Do not add line numbers to the text; these are added automatically in the Manuscript Central system.
6.3 Writing style
Writing should be scholarly, and the style consistent throughout the manuscript. If there are two or more authors, do not use “I” statements. Use the past tense when writing about things that happened, were said, or were written in the past. Avoid anthropomorphic language; long, complex sentences; and unnecessary information. Voice: Both the abstract and the manuscript should be written in the first-person active voice. Avoid passive language.
6.4 Artwork, figures and other graphics
Include figures, charts, and tables created in MS Word in the main text rather than at the end of the document. However, figures, tables, and other files created outside of Word should be submitted separately. In this instance, please indicate where table and figures should be inserted within manuscript (e.g., INSERT TABLE 1 HERE). If using or adapting any copyrighted (previously published) material see APA for requirements.
6.4.1 Tables
Tables organize relevant, essential data that would be too awkward or too lengthy to include in the text, and should be used only to provide data not already included in the text. For example, grouped participant demographics take less space presented in a descriptive paragraph than they do as a table. Table titles should be concise and descriptive. Multiple tables within the same manuscript should be similar in appearance and design.
6.4.2 Figures
Like tables, figures should be used sparingly, and only when it is necessary to clarify complex relationships or concepts. Mention figure placement in the manuscript text, but submit each figure in a separate document, with the figure number and title on the first page, followed by the figure itself on the second page. Figure titles should be concise and descriptive. Designate placement of each figure within the manuscript by entering (on a separate line between paragraphs) INSERT FIGURE 1 ABOUT HERE. Figure callouts should be placed following the paragraph in which they are first mentioned. Figures supplied in color will appear in color online.
6.4.3 Photographs
Photographs may be included but should have permission to reprint and faces should be concealed using mosaic patches – unless permission has been given by the individual to use their identity. This permission must be forwarded to QHR’s Managing Editor.
TIFF, JPED, or common picture formats accepted. The preferred format for graphs and line art is EPS.
Resolution: Rasterized based files (i.e. with .tiff or .jpeg extension) require a resolution of at least 300 dpi (dots per inch). Line art should be supplied with a minimum resolution of 800 dpi.
Dimension: Check that the artworks supplied match or exceed the dimensions of the journal. Images cannot be scaled up after origination.
6.4.4 Artwork
Participant artwork may be included provided the content is free of any material that could potentially identify the participant who created it (or any persons who might be depicted). Use artwork only with the permission of the participant. All content should be dark enough to facilitate clear visibility online. Artwork supplied in color will appear in color online.
6.5 Reference style
Global Qualitative Nursing Research adheres to the APA 7th edition reference style. You may review this quick reference sheet to ensure your manuscript conforms to this reference style.
To anonymize the manuscript for review, citations for references authored by any author of the submitted manuscript should read only “(Author, year).” References authored by any author of the submitted manuscript should read only “Author. (year).” Do not include the reference title or any other information pertaining to the reference.
6.6 English language editing services
Authors seeking assistance with English language editing, translation, or figure and manuscript formatting to fit the journal’s specifications should consider using SAGE Language Services. Note: Some non-native English authors of accepted articles may be required to have their final manuscript professionally edited by a native-English-speaking editor. Visit SAGE Language Services on our Journal Author Gateway for further information, or contact the journal office at GQNR- [email protected] .
6.7 Publishing translated versions of articles
GQNR encourages authors to submit translated versions of your title, abstract and key words to be published alongside the English version. In addition, GQNR allows translated versions of accepted article to be published along with the English version as a supplementary file. Please follow the instructions in the submission site to ensure your translated version is published. Authors may use the proof of their accepted Article as the basis of the Translation and may use similar formatting and typesetting for the Translation as used in the original Article to create a PDF of the Translation. The Editor will arrange for light review of each Translation prior to publication. The review may be completed by a member of the Editorial Board or other trusted academic reviewer who is fluent in the language of the Translation to review the Translation to confirm there are no material errors in the Translation that result in an inconsistency with the original Article.
As part of GQNR’s commitment to supporting and disseminating qualitative nursing research internationally, selected articles may be subject to translation by GQNR following acceptance and/or publication. Authors will be notified if their article and/or the article title, abstract is selected for translation.
For further questions, please email [email protected]
6.8 Supplementary material
This journal is able to host additional materials online (e.g. datasets, podcasts, videos, images etc.) alongside the full-text of the article. These will be subjected to peer-review alongside the article. For more information please refer to our guidelines on submitting supplementary files, which can be found within SAGE’s Manuscript Submission Guidelines page.
7. Submitting your manuscript
Before submitting your manuscript, please carefully read and adhere to all of the guidelines and instructions provided below, especially the Manuscript Style. Manuscripts not conforming to these guidelines may be returned.
Global Qualitative Nursing Research is hosted on SAGE Track, a web based online submission and peer review system powered by ScholarOne™ Manuscripts. Visit https://mc.manuscriptcentral.com/GQNR to login and submit your article online. Please do not email manuscripts to the journal office.
PLEASE NOTE: If you are in the process of submitting a revision and will need an extension on the submission deadline, please email [email protected] If you choose not to submit a revision, please email [email protected] as soon as possible to notify us of this decision. Until a manuscript is formally withdrawn, it is considered under review at the journal that issued the revision decision.
IMPORTANT: Please check whether you already have an account in the system before trying to create a new one. If you have reviewed or authored for the journal in the past year it is likely that you will have had an account created. For further guidance on submitting your manuscript online please visit ScholarOne Online Help .
All papers must be submitted via the online system. If you seek advice on the submission process, please contact the Publishing Editor.
7.1 Title, keywords and abstract
Please supply a title, an abstract (unstructured, approximately 150 words) and keywords to accompany your article. The title, keywords and abstract are key to ensuring readers find your article online through online search engines such as Google. Please refer to the information and guidance on how best to title your article, write your abstract and select your keywords by visiting the SAGE Journal Author Gateway for guidelines on How to Help Readers Find Your Article Online .
7.2 Information required for completing your submission
Provide full contact details for the corresponding author including email, mailing address and telephone numbers. Academic affiliations are required for all co-authors. These details should be presented separately to the main text of the article to facilitate anonymous peer review.
You will be asked to provide contact details and academic affiliations for all co-authors via the submission system and identify who is to be the corresponding author. These details must match what appears on your manuscript. At this stage please ensure you have included all the required statements and declarations and uploaded any additional supplementary files (including reporting guidelines where relevant).
Please indicate if you are submitting a manuscript for a special collection. Information about open calls for special collections can be found here: https://journals.sagepub.com/gqn/open-special-collections
To facilitate an anonymized review process, no author names, initials, or other identifying information should appear anywhere in the manuscript; however, this information is needed by the Editor. In a “title page” separate from the manuscript, include the following information, in this order:
- Manuscript title
- Author names as they should appear, and in the same order in which they should appear, in the published article
- Affiliation information for each author, to include only the following: (a) thehighest-level institution (e.g., university); (b) the city in which the institution is located; (c) the state or province (if any); and (d)the country [Note: Use “USA” for the United States]
- Name and complete mailing address (including country) of the corresponding author
- Preferred email address of the corresponding author
- A biographical statement for each author, in order. Follow the template below in preparing the bios, and be sure to include all required elements (name, credentials, title or role, affiliation, city, state/province/territory [if any], country):
- Joan L. Bottorff, RN, PhD, FCAHS, FAAN is a professor at the University of British Columbia, Faculty of Health and Social Development, School of Nursing in Kelowna, British Columbia, Canada.
As part of our commitment to ensuring an ethical, transparent and fair peer review process SAGE is a supporting member of ORCID, the Open Researcher and Contributor ID . ORCID provides a unique and persistent digital identifier that distinguishes researchers from every other researcher, even those who share the same name, and, through integration in key research workflows such as manuscript and grant submission, supports automated linkages between researchers and their professional activities, ensuring that their work is recognized.
The collection of ORCID iDs from corresponding authors is now part of the submission process of this journal. If you already have an ORCID iD you will be asked to associate that to your submission during the online submission process. We also strongly encourage all co-authors to link their ORCID ID to their accounts in our online peer review platforms. It takes seconds to do: click the link when prompted, sign into your ORCID account and our systems are automatically updated. Your ORCID iD will become part of your accepted publication’s metadata, making your work attributable to you and only you. Your ORCID iD is published with your article so that fellow researchers reading your work can link to your ORCID profile and from there link to your other publications.
If you do not already have an ORCID iD please follow this link to create one or visit our ORCID homepage to learn more.
7.4 Permissions
Authors are responsible for obtaining permission from copyright holders for reproducing any illustrations, tables, figures or lengthy quotations previously published elsewhere. For further information including guidance on fair dealing for criticism and review, please visit our Frequently Asked Questions on the SAGE Journal Author Gateway . Please do not address permission and copyright questions to the journal office.
8. On acceptance and publication
If your paper is accepted for publication after peer review, you will first be asked to complete the contributor’s publishing agreement. Once your manuscript files have been check for SAGE Production, the corresponding author will be asked to pay the article processing charge (APC) via a payment link. Once the APC has been processed, your article will be prepared for publication and can appear online within an average of 30 days. Please note that no production work will occur on your paper until the APC has been received.
8.1 SAGE Production
Your SAGE Production Editor will keep you informed as to your article’s progress throughout the production process. Proofs will be sent by PDF to the corresponding author and should be returned promptly. Authors are reminded to check their proofs carefully to confirm that all author information, including names, affiliations, sequence and contact details are correct, and that Funding and Conflict of Interest statements, if any, are accurate. Please note that if there are any changes to the author list at this stage all authors will be required to complete and sign a form authorizing the change.
8.2 Online publication
One of the many benefits of publishing your research in an open access journal is the speed to publication. Your article will be published online in a fully citable form with a DOI number as soon as it has completed the production process. At this time it will be completely free to view and download for all.
8.3 Promoting your article
Publication is not the end of the process! You can help disseminate your paper and ensure it is as widely read and cited as possible. The SAGE Author Gateway has numerous resources to help you promote your work. Visit the Promote Your Article page on the Gateway for tips and advice.
9. Further information
Any correspondence, queries or additional requests for information on the Manuscript Submission process should be sent to the Global Qualitative Nursing Research Publishing Editor as follows: Lorianne Sarsfield
Email: [email protected]
- Read Online
- Current Issue
- Email Alert
- Permissions
- Foreign rights
- Reprints and sponsorship
- Advertising
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- Write for Us
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 15, Issue 1
- Qualitative data analysis
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Correspondence to Kate Seers RCN Research Institute, School of Health & Social Studies, University of Warwick, Coventry, CV4 7AL, Warwick, UK; kate.seers{at}warwick.ac.uk
https://doi.org/10.1136/ebnurs.2011.100352
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Good qualitative research uses a systematic and rigorous approach that aims to answer questions concerned with what something is like (such as a patient experience), what people think or feel about something that has happened, and it may address why something has happened as it has. Qualitative data often takes the form of words or text and can include images.
Qualitative research covers a very broad range of philosophical underpinnings and methodological approaches. Each has its own particular way of approaching all stages of the research process, including analysis, and has its own terms and techniques, but there are some common threads that run across most of these approaches. This Research Made Simple piece will focus on some of these common threads in the analysis of qualitative research.
So you have collected all your qualitative data – you may have a pile of interview transcripts, field-notes, documents and notes from observation. The process of analysis is described by Richards and Morse 1 as one of transformation and interpretation.
It is easy to be overwhelmed by the volume of data – novice qualitative researchers are sometimes told not to worry and the themes will emerge from the data. This suggests some sort of epiphany, (which is how it happens sometimes!) but generally it comes from detailed work and reflection on the data and what it is telling you. There is sometimes a fine line between being immersed in the data and drowning in it!
A first step is to sort and organise the data, by coding it in some way. For example, you could read through a transcript, and identify that in one paragraph a patient is talking about two things; first is fear of surgery and second is fear of unrelieved pain. The codes for this paragraph could be ‘fear of surgery’ and ‘fear of pain’. In other areas of the transcript fear may arise again, and perhaps these codes will be merged into a category titled ‘fear’. Other concerns may emerge in this and other transcripts and perhaps best be represented by the theme ‘lack of control’. Themes are thus more abstract concepts, reflecting your interpretation of patterns across your data. So from codes, categories can be formed, and from categories, more encompassing themes are developed to describe the data in a form which summarises it, yet retains the richness, depth and context of the original data. Using quotations to illustrate categories and themes helps keep the analysis firmly grounded in the data. You need to constantly ask yourself ‘what is happening here?’ as you code and move from codes, to categories and themes, making sure you have data to support your decisions. Analysis inevitably involves subjective choices, and it is important to document what you have done and why, so a clear audit trail is provided. The coding example above describes codes inductively coming from the data. Some researchers may use a coding framework derived from, for example, the literature, their research questions or interview prompts, (Ritchie and Spencer 2 ) or a combination of both approaches.
Qualitative data, such as transcripts from an interview, are often routed in the interaction between the participant and the researcher. Reflecting on how you, as a researcher, may have influenced both the data collected and the analysis is an important part of the analysis.
As well as keeping your brain very much in gear, you need to be really organised. You may use highlighting pens and paper to keep track of your analysis, or use qualitative software to manage your data (such as NVivio or Atlas Ti). These programmes help you organise your data – you still have to do all the hard work to analyse it! Whatever you choose, it is important that you can trace your data back from themes to categories to codes. There is nothing more frustrating than looking for that illustrative patient quote, and not being able to find it.
If your qualitative data are part of a mixed methods study, (has both quantitative and qualitative data) careful thought has to be given to how you will analyse and present findings. Refer to O’Caithain et al 3 for more details.
There are many books and papers on qualitative analysis, a very few of which are listed below. 4 , – , 6 Working with someone with qualitative expertise is also invaluable, as you can read about it, but doing it really brings it alive.
- Richards L ,
- Ritchie J ,
- O'Cathain ,
- Bradley EH ,
- Huberman AM
Competing interests None.
Read the full text or download the PDF:
- Open access
- Published: 27 May 2020
How to use and assess qualitative research methods
- Loraine Busetto ORCID: orcid.org/0000-0002-9228-7875 1 ,
- Wolfgang Wick 1 , 2 &
- Christoph Gumbinger 1
Neurological Research and Practice volume 2 , Article number: 14 ( 2020 ) Cite this article
679k Accesses
264 Citations
88 Altmetric
Metrics details
This paper aims to provide an overview of the use and assessment of qualitative research methods in the health sciences. Qualitative research can be defined as the study of the nature of phenomena and is especially appropriate for answering questions of why something is (not) observed, assessing complex multi-component interventions, and focussing on intervention improvement. The most common methods of data collection are document study, (non-) participant observations, semi-structured interviews and focus groups. For data analysis, field-notes and audio-recordings are transcribed into protocols and transcripts, and coded using qualitative data management software. Criteria such as checklists, reflexivity, sampling strategies, piloting, co-coding, member-checking and stakeholder involvement can be used to enhance and assess the quality of the research conducted. Using qualitative in addition to quantitative designs will equip us with better tools to address a greater range of research problems, and to fill in blind spots in current neurological research and practice.
The aim of this paper is to provide an overview of qualitative research methods, including hands-on information on how they can be used, reported and assessed. This article is intended for beginning qualitative researchers in the health sciences as well as experienced quantitative researchers who wish to broaden their understanding of qualitative research.
What is qualitative research?
Qualitative research is defined as “the study of the nature of phenomena”, including “their quality, different manifestations, the context in which they appear or the perspectives from which they can be perceived” , but excluding “their range, frequency and place in an objectively determined chain of cause and effect” [ 1 ]. This formal definition can be complemented with a more pragmatic rule of thumb: qualitative research generally includes data in form of words rather than numbers [ 2 ].
Why conduct qualitative research?
Because some research questions cannot be answered using (only) quantitative methods. For example, one Australian study addressed the issue of why patients from Aboriginal communities often present late or not at all to specialist services offered by tertiary care hospitals. Using qualitative interviews with patients and staff, it found one of the most significant access barriers to be transportation problems, including some towns and communities simply not having a bus service to the hospital [ 3 ]. A quantitative study could have measured the number of patients over time or even looked at possible explanatory factors – but only those previously known or suspected to be of relevance. To discover reasons for observed patterns, especially the invisible or surprising ones, qualitative designs are needed.
While qualitative research is common in other fields, it is still relatively underrepresented in health services research. The latter field is more traditionally rooted in the evidence-based-medicine paradigm, as seen in " research that involves testing the effectiveness of various strategies to achieve changes in clinical practice, preferably applying randomised controlled trial study designs (...) " [ 4 ]. This focus on quantitative research and specifically randomised controlled trials (RCT) is visible in the idea of a hierarchy of research evidence which assumes that some research designs are objectively better than others, and that choosing a "lesser" design is only acceptable when the better ones are not practically or ethically feasible [ 5 , 6 ]. Others, however, argue that an objective hierarchy does not exist, and that, instead, the research design and methods should be chosen to fit the specific research question at hand – "questions before methods" [ 2 , 7 , 8 , 9 ]. This means that even when an RCT is possible, some research problems require a different design that is better suited to addressing them. Arguing in JAMA, Berwick uses the example of rapid response teams in hospitals, which he describes as " a complex, multicomponent intervention – essentially a process of social change" susceptible to a range of different context factors including leadership or organisation history. According to him, "[in] such complex terrain, the RCT is an impoverished way to learn. Critics who use it as a truth standard in this context are incorrect" [ 8 ] . Instead of limiting oneself to RCTs, Berwick recommends embracing a wider range of methods , including qualitative ones, which for "these specific applications, (...) are not compromises in learning how to improve; they are superior" [ 8 ].
Research problems that can be approached particularly well using qualitative methods include assessing complex multi-component interventions or systems (of change), addressing questions beyond “what works”, towards “what works for whom when, how and why”, and focussing on intervention improvement rather than accreditation [ 7 , 9 , 10 , 11 , 12 ]. Using qualitative methods can also help shed light on the “softer” side of medical treatment. For example, while quantitative trials can measure the costs and benefits of neuro-oncological treatment in terms of survival rates or adverse effects, qualitative research can help provide a better understanding of patient or caregiver stress, visibility of illness or out-of-pocket expenses.
How to conduct qualitative research?
Given that qualitative research is characterised by flexibility, openness and responsivity to context, the steps of data collection and analysis are not as separate and consecutive as they tend to be in quantitative research [ 13 , 14 ]. As Fossey puts it : “sampling, data collection, analysis and interpretation are related to each other in a cyclical (iterative) manner, rather than following one after another in a stepwise approach” [ 15 ]. The researcher can make educated decisions with regard to the choice of method, how they are implemented, and to which and how many units they are applied [ 13 ]. As shown in Fig. 1 , this can involve several back-and-forth steps between data collection and analysis where new insights and experiences can lead to adaption and expansion of the original plan. Some insights may also necessitate a revision of the research question and/or the research design as a whole. The process ends when saturation is achieved, i.e. when no relevant new information can be found (see also below: sampling and saturation). For reasons of transparency, it is essential for all decisions as well as the underlying reasoning to be well-documented.
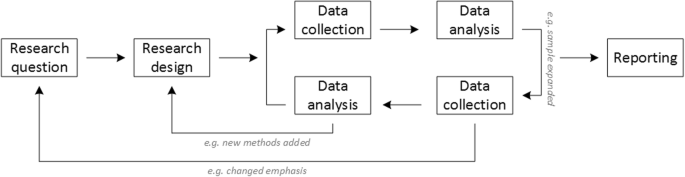
Iterative research process
While it is not always explicitly addressed, qualitative methods reflect a different underlying research paradigm than quantitative research (e.g. constructivism or interpretivism as opposed to positivism). The choice of methods can be based on the respective underlying substantive theory or theoretical framework used by the researcher [ 2 ].
Data collection
The methods of qualitative data collection most commonly used in health research are document study, observations, semi-structured interviews and focus groups [ 1 , 14 , 16 , 17 ].
Document study
Document study (also called document analysis) refers to the review by the researcher of written materials [ 14 ]. These can include personal and non-personal documents such as archives, annual reports, guidelines, policy documents, diaries or letters.
Observations
Observations are particularly useful to gain insights into a certain setting and actual behaviour – as opposed to reported behaviour or opinions [ 13 ]. Qualitative observations can be either participant or non-participant in nature. In participant observations, the observer is part of the observed setting, for example a nurse working in an intensive care unit [ 18 ]. In non-participant observations, the observer is “on the outside looking in”, i.e. present in but not part of the situation, trying not to influence the setting by their presence. Observations can be planned (e.g. for 3 h during the day or night shift) or ad hoc (e.g. as soon as a stroke patient arrives at the emergency room). During the observation, the observer takes notes on everything or certain pre-determined parts of what is happening around them, for example focusing on physician-patient interactions or communication between different professional groups. Written notes can be taken during or after the observations, depending on feasibility (which is usually lower during participant observations) and acceptability (e.g. when the observer is perceived to be judging the observed). Afterwards, these field notes are transcribed into observation protocols. If more than one observer was involved, field notes are taken independently, but notes can be consolidated into one protocol after discussions. Advantages of conducting observations include minimising the distance between the researcher and the researched, the potential discovery of topics that the researcher did not realise were relevant and gaining deeper insights into the real-world dimensions of the research problem at hand [ 18 ].
Semi-structured interviews
Hijmans & Kuyper describe qualitative interviews as “an exchange with an informal character, a conversation with a goal” [ 19 ]. Interviews are used to gain insights into a person’s subjective experiences, opinions and motivations – as opposed to facts or behaviours [ 13 ]. Interviews can be distinguished by the degree to which they are structured (i.e. a questionnaire), open (e.g. free conversation or autobiographical interviews) or semi-structured [ 2 , 13 ]. Semi-structured interviews are characterized by open-ended questions and the use of an interview guide (or topic guide/list) in which the broad areas of interest, sometimes including sub-questions, are defined [ 19 ]. The pre-defined topics in the interview guide can be derived from the literature, previous research or a preliminary method of data collection, e.g. document study or observations. The topic list is usually adapted and improved at the start of the data collection process as the interviewer learns more about the field [ 20 ]. Across interviews the focus on the different (blocks of) questions may differ and some questions may be skipped altogether (e.g. if the interviewee is not able or willing to answer the questions or for concerns about the total length of the interview) [ 20 ]. Qualitative interviews are usually not conducted in written format as it impedes on the interactive component of the method [ 20 ]. In comparison to written surveys, qualitative interviews have the advantage of being interactive and allowing for unexpected topics to emerge and to be taken up by the researcher. This can also help overcome a provider or researcher-centred bias often found in written surveys, which by nature, can only measure what is already known or expected to be of relevance to the researcher. Interviews can be audio- or video-taped; but sometimes it is only feasible or acceptable for the interviewer to take written notes [ 14 , 16 , 20 ].
Focus groups
Focus groups are group interviews to explore participants’ expertise and experiences, including explorations of how and why people behave in certain ways [ 1 ]. Focus groups usually consist of 6–8 people and are led by an experienced moderator following a topic guide or “script” [ 21 ]. They can involve an observer who takes note of the non-verbal aspects of the situation, possibly using an observation guide [ 21 ]. Depending on researchers’ and participants’ preferences, the discussions can be audio- or video-taped and transcribed afterwards [ 21 ]. Focus groups are useful for bringing together homogeneous (to a lesser extent heterogeneous) groups of participants with relevant expertise and experience on a given topic on which they can share detailed information [ 21 ]. Focus groups are a relatively easy, fast and inexpensive method to gain access to information on interactions in a given group, i.e. “the sharing and comparing” among participants [ 21 ]. Disadvantages include less control over the process and a lesser extent to which each individual may participate. Moreover, focus group moderators need experience, as do those tasked with the analysis of the resulting data. Focus groups can be less appropriate for discussing sensitive topics that participants might be reluctant to disclose in a group setting [ 13 ]. Moreover, attention must be paid to the emergence of “groupthink” as well as possible power dynamics within the group, e.g. when patients are awed or intimidated by health professionals.
Choosing the “right” method
As explained above, the school of thought underlying qualitative research assumes no objective hierarchy of evidence and methods. This means that each choice of single or combined methods has to be based on the research question that needs to be answered and a critical assessment with regard to whether or to what extent the chosen method can accomplish this – i.e. the “fit” between question and method [ 14 ]. It is necessary for these decisions to be documented when they are being made, and to be critically discussed when reporting methods and results.
Let us assume that our research aim is to examine the (clinical) processes around acute endovascular treatment (EVT), from the patient’s arrival at the emergency room to recanalization, with the aim to identify possible causes for delay and/or other causes for sub-optimal treatment outcome. As a first step, we could conduct a document study of the relevant standard operating procedures (SOPs) for this phase of care – are they up-to-date and in line with current guidelines? Do they contain any mistakes, irregularities or uncertainties that could cause delays or other problems? Regardless of the answers to these questions, the results have to be interpreted based on what they are: a written outline of what care processes in this hospital should look like. If we want to know what they actually look like in practice, we can conduct observations of the processes described in the SOPs. These results can (and should) be analysed in themselves, but also in comparison to the results of the document analysis, especially as regards relevant discrepancies. Do the SOPs outline specific tests for which no equipment can be observed or tasks to be performed by specialized nurses who are not present during the observation? It might also be possible that the written SOP is outdated, but the actual care provided is in line with current best practice. In order to find out why these discrepancies exist, it can be useful to conduct interviews. Are the physicians simply not aware of the SOPs (because their existence is limited to the hospital’s intranet) or do they actively disagree with them or does the infrastructure make it impossible to provide the care as described? Another rationale for adding interviews is that some situations (or all of their possible variations for different patient groups or the day, night or weekend shift) cannot practically or ethically be observed. In this case, it is possible to ask those involved to report on their actions – being aware that this is not the same as the actual observation. A senior physician’s or hospital manager’s description of certain situations might differ from a nurse’s or junior physician’s one, maybe because they intentionally misrepresent facts or maybe because different aspects of the process are visible or important to them. In some cases, it can also be relevant to consider to whom the interviewee is disclosing this information – someone they trust, someone they are otherwise not connected to, or someone they suspect or are aware of being in a potentially “dangerous” power relationship to them. Lastly, a focus group could be conducted with representatives of the relevant professional groups to explore how and why exactly they provide care around EVT. The discussion might reveal discrepancies (between SOPs and actual care or between different physicians) and motivations to the researchers as well as to the focus group members that they might not have been aware of themselves. For the focus group to deliver relevant information, attention has to be paid to its composition and conduct, for example, to make sure that all participants feel safe to disclose sensitive or potentially problematic information or that the discussion is not dominated by (senior) physicians only. The resulting combination of data collection methods is shown in Fig. 2 .
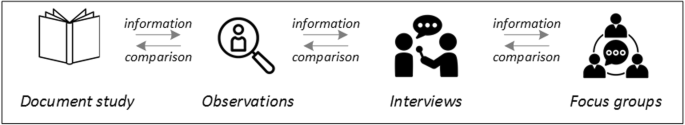
Possible combination of data collection methods
Attributions for icons: “Book” by Serhii Smirnov, “Interview” by Adrien Coquet, FR, “Magnifying Glass” by anggun, ID, “Business communication” by Vectors Market; all from the Noun Project
The combination of multiple data source as described for this example can be referred to as “triangulation”, in which multiple measurements are carried out from different angles to achieve a more comprehensive understanding of the phenomenon under study [ 22 , 23 ].
Data analysis
To analyse the data collected through observations, interviews and focus groups these need to be transcribed into protocols and transcripts (see Fig. 3 ). Interviews and focus groups can be transcribed verbatim , with or without annotations for behaviour (e.g. laughing, crying, pausing) and with or without phonetic transcription of dialects and filler words, depending on what is expected or known to be relevant for the analysis. In the next step, the protocols and transcripts are coded , that is, marked (or tagged, labelled) with one or more short descriptors of the content of a sentence or paragraph [ 2 , 15 , 23 ]. Jansen describes coding as “connecting the raw data with “theoretical” terms” [ 20 ]. In a more practical sense, coding makes raw data sortable. This makes it possible to extract and examine all segments describing, say, a tele-neurology consultation from multiple data sources (e.g. SOPs, emergency room observations, staff and patient interview). In a process of synthesis and abstraction, the codes are then grouped, summarised and/or categorised [ 15 , 20 ]. The end product of the coding or analysis process is a descriptive theory of the behavioural pattern under investigation [ 20 ]. The coding process is performed using qualitative data management software, the most common ones being InVivo, MaxQDA and Atlas.ti. It should be noted that these are data management tools which support the analysis performed by the researcher(s) [ 14 ].
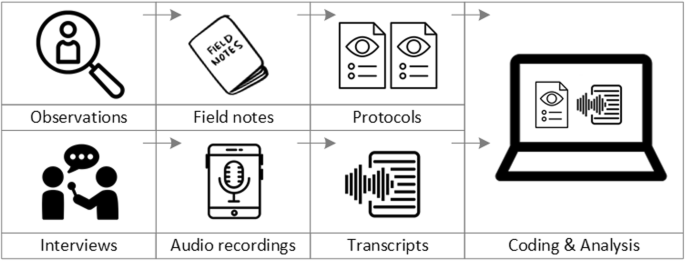
From data collection to data analysis
Attributions for icons: see Fig. 2 , also “Speech to text” by Trevor Dsouza, “Field Notes” by Mike O’Brien, US, “Voice Record” by ProSymbols, US, “Inspection” by Made, AU, and “Cloud” by Graphic Tigers; all from the Noun Project
How to report qualitative research?
Protocols of qualitative research can be published separately and in advance of the study results. However, the aim is not the same as in RCT protocols, i.e. to pre-define and set in stone the research questions and primary or secondary endpoints. Rather, it is a way to describe the research methods in detail, which might not be possible in the results paper given journals’ word limits. Qualitative research papers are usually longer than their quantitative counterparts to allow for deep understanding and so-called “thick description”. In the methods section, the focus is on transparency of the methods used, including why, how and by whom they were implemented in the specific study setting, so as to enable a discussion of whether and how this may have influenced data collection, analysis and interpretation. The results section usually starts with a paragraph outlining the main findings, followed by more detailed descriptions of, for example, the commonalities, discrepancies or exceptions per category [ 20 ]. Here it is important to support main findings by relevant quotations, which may add information, context, emphasis or real-life examples [ 20 , 23 ]. It is subject to debate in the field whether it is relevant to state the exact number or percentage of respondents supporting a certain statement (e.g. “Five interviewees expressed negative feelings towards XYZ”) [ 21 ].
How to combine qualitative with quantitative research?
Qualitative methods can be combined with other methods in multi- or mixed methods designs, which “[employ] two or more different methods [ …] within the same study or research program rather than confining the research to one single method” [ 24 ]. Reasons for combining methods can be diverse, including triangulation for corroboration of findings, complementarity for illustration and clarification of results, expansion to extend the breadth and range of the study, explanation of (unexpected) results generated with one method with the help of another, or offsetting the weakness of one method with the strength of another [ 1 , 17 , 24 , 25 , 26 ]. The resulting designs can be classified according to when, why and how the different quantitative and/or qualitative data strands are combined. The three most common types of mixed method designs are the convergent parallel design , the explanatory sequential design and the exploratory sequential design. The designs with examples are shown in Fig. 4 .
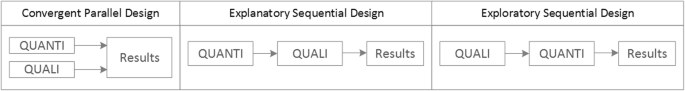
Three common mixed methods designs
In the convergent parallel design, a qualitative study is conducted in parallel to and independently of a quantitative study, and the results of both studies are compared and combined at the stage of interpretation of results. Using the above example of EVT provision, this could entail setting up a quantitative EVT registry to measure process times and patient outcomes in parallel to conducting the qualitative research outlined above, and then comparing results. Amongst other things, this would make it possible to assess whether interview respondents’ subjective impressions of patients receiving good care match modified Rankin Scores at follow-up, or whether observed delays in care provision are exceptions or the rule when compared to door-to-needle times as documented in the registry. In the explanatory sequential design, a quantitative study is carried out first, followed by a qualitative study to help explain the results from the quantitative study. This would be an appropriate design if the registry alone had revealed relevant delays in door-to-needle times and the qualitative study would be used to understand where and why these occurred, and how they could be improved. In the exploratory design, the qualitative study is carried out first and its results help informing and building the quantitative study in the next step [ 26 ]. If the qualitative study around EVT provision had shown a high level of dissatisfaction among the staff members involved, a quantitative questionnaire investigating staff satisfaction could be set up in the next step, informed by the qualitative study on which topics dissatisfaction had been expressed. Amongst other things, the questionnaire design would make it possible to widen the reach of the research to more respondents from different (types of) hospitals, regions, countries or settings, and to conduct sub-group analyses for different professional groups.
How to assess qualitative research?
A variety of assessment criteria and lists have been developed for qualitative research, ranging in their focus and comprehensiveness [ 14 , 17 , 27 ]. However, none of these has been elevated to the “gold standard” in the field. In the following, we therefore focus on a set of commonly used assessment criteria that, from a practical standpoint, a researcher can look for when assessing a qualitative research report or paper.
Assessors should check the authors’ use of and adherence to the relevant reporting checklists (e.g. Standards for Reporting Qualitative Research (SRQR)) to make sure all items that are relevant for this type of research are addressed [ 23 , 28 ]. Discussions of quantitative measures in addition to or instead of these qualitative measures can be a sign of lower quality of the research (paper). Providing and adhering to a checklist for qualitative research contributes to an important quality criterion for qualitative research, namely transparency [ 15 , 17 , 23 ].
Reflexivity
While methodological transparency and complete reporting is relevant for all types of research, some additional criteria must be taken into account for qualitative research. This includes what is called reflexivity, i.e. sensitivity to the relationship between the researcher and the researched, including how contact was established and maintained, or the background and experience of the researcher(s) involved in data collection and analysis. Depending on the research question and population to be researched this can be limited to professional experience, but it may also include gender, age or ethnicity [ 17 , 27 ]. These details are relevant because in qualitative research, as opposed to quantitative research, the researcher as a person cannot be isolated from the research process [ 23 ]. It may influence the conversation when an interviewed patient speaks to an interviewer who is a physician, or when an interviewee is asked to discuss a gynaecological procedure with a male interviewer, and therefore the reader must be made aware of these details [ 19 ].
Sampling and saturation
The aim of qualitative sampling is for all variants of the objects of observation that are deemed relevant for the study to be present in the sample “ to see the issue and its meanings from as many angles as possible” [ 1 , 16 , 19 , 20 , 27 ] , and to ensure “information-richness [ 15 ]. An iterative sampling approach is advised, in which data collection (e.g. five interviews) is followed by data analysis, followed by more data collection to find variants that are lacking in the current sample. This process continues until no new (relevant) information can be found and further sampling becomes redundant – which is called saturation [ 1 , 15 ] . In other words: qualitative data collection finds its end point not a priori , but when the research team determines that saturation has been reached [ 29 , 30 ].
This is also the reason why most qualitative studies use deliberate instead of random sampling strategies. This is generally referred to as “ purposive sampling” , in which researchers pre-define which types of participants or cases they need to include so as to cover all variations that are expected to be of relevance, based on the literature, previous experience or theory (i.e. theoretical sampling) [ 14 , 20 ]. Other types of purposive sampling include (but are not limited to) maximum variation sampling, critical case sampling or extreme or deviant case sampling [ 2 ]. In the above EVT example, a purposive sample could include all relevant professional groups and/or all relevant stakeholders (patients, relatives) and/or all relevant times of observation (day, night and weekend shift).
Assessors of qualitative research should check whether the considerations underlying the sampling strategy were sound and whether or how researchers tried to adapt and improve their strategies in stepwise or cyclical approaches between data collection and analysis to achieve saturation [ 14 ].
Good qualitative research is iterative in nature, i.e. it goes back and forth between data collection and analysis, revising and improving the approach where necessary. One example of this are pilot interviews, where different aspects of the interview (especially the interview guide, but also, for example, the site of the interview or whether the interview can be audio-recorded) are tested with a small number of respondents, evaluated and revised [ 19 ]. In doing so, the interviewer learns which wording or types of questions work best, or which is the best length of an interview with patients who have trouble concentrating for an extended time. Of course, the same reasoning applies to observations or focus groups which can also be piloted.
Ideally, coding should be performed by at least two researchers, especially at the beginning of the coding process when a common approach must be defined, including the establishment of a useful coding list (or tree), and when a common meaning of individual codes must be established [ 23 ]. An initial sub-set or all transcripts can be coded independently by the coders and then compared and consolidated after regular discussions in the research team. This is to make sure that codes are applied consistently to the research data.
Member checking
Member checking, also called respondent validation , refers to the practice of checking back with study respondents to see if the research is in line with their views [ 14 , 27 ]. This can happen after data collection or analysis or when first results are available [ 23 ]. For example, interviewees can be provided with (summaries of) their transcripts and asked whether they believe this to be a complete representation of their views or whether they would like to clarify or elaborate on their responses [ 17 ]. Respondents’ feedback on these issues then becomes part of the data collection and analysis [ 27 ].
Stakeholder involvement
In those niches where qualitative approaches have been able to evolve and grow, a new trend has seen the inclusion of patients and their representatives not only as study participants (i.e. “members”, see above) but as consultants to and active participants in the broader research process [ 31 , 32 , 33 ]. The underlying assumption is that patients and other stakeholders hold unique perspectives and experiences that add value beyond their own single story, making the research more relevant and beneficial to researchers, study participants and (future) patients alike [ 34 , 35 ]. Using the example of patients on or nearing dialysis, a recent scoping review found that 80% of clinical research did not address the top 10 research priorities identified by patients and caregivers [ 32 , 36 ]. In this sense, the involvement of the relevant stakeholders, especially patients and relatives, is increasingly being seen as a quality indicator in and of itself.
How not to assess qualitative research
The above overview does not include certain items that are routine in assessments of quantitative research. What follows is a non-exhaustive, non-representative, experience-based list of the quantitative criteria often applied to the assessment of qualitative research, as well as an explanation of the limited usefulness of these endeavours.
Protocol adherence
Given the openness and flexibility of qualitative research, it should not be assessed by how well it adheres to pre-determined and fixed strategies – in other words: its rigidity. Instead, the assessor should look for signs of adaptation and refinement based on lessons learned from earlier steps in the research process.
Sample size
For the reasons explained above, qualitative research does not require specific sample sizes, nor does it require that the sample size be determined a priori [ 1 , 14 , 27 , 37 , 38 , 39 ]. Sample size can only be a useful quality indicator when related to the research purpose, the chosen methodology and the composition of the sample, i.e. who was included and why.
Randomisation
While some authors argue that randomisation can be used in qualitative research, this is not commonly the case, as neither its feasibility nor its necessity or usefulness has been convincingly established for qualitative research [ 13 , 27 ]. Relevant disadvantages include the negative impact of a too large sample size as well as the possibility (or probability) of selecting “ quiet, uncooperative or inarticulate individuals ” [ 17 ]. Qualitative studies do not use control groups, either.
Interrater reliability, variability and other “objectivity checks”
The concept of “interrater reliability” is sometimes used in qualitative research to assess to which extent the coding approach overlaps between the two co-coders. However, it is not clear what this measure tells us about the quality of the analysis [ 23 ]. This means that these scores can be included in qualitative research reports, preferably with some additional information on what the score means for the analysis, but it is not a requirement. Relatedly, it is not relevant for the quality or “objectivity” of qualitative research to separate those who recruited the study participants and collected and analysed the data. Experiences even show that it might be better to have the same person or team perform all of these tasks [ 20 ]. First, when researchers introduce themselves during recruitment this can enhance trust when the interview takes place days or weeks later with the same researcher. Second, when the audio-recording is transcribed for analysis, the researcher conducting the interviews will usually remember the interviewee and the specific interview situation during data analysis. This might be helpful in providing additional context information for interpretation of data, e.g. on whether something might have been meant as a joke [ 18 ].
Not being quantitative research
Being qualitative research instead of quantitative research should not be used as an assessment criterion if it is used irrespectively of the research problem at hand. Similarly, qualitative research should not be required to be combined with quantitative research per se – unless mixed methods research is judged as inherently better than single-method research. In this case, the same criterion should be applied for quantitative studies without a qualitative component.
The main take-away points of this paper are summarised in Table 1 . We aimed to show that, if conducted well, qualitative research can answer specific research questions that cannot to be adequately answered using (only) quantitative designs. Seeing qualitative and quantitative methods as equal will help us become more aware and critical of the “fit” between the research problem and our chosen methods: I can conduct an RCT to determine the reasons for transportation delays of acute stroke patients – but should I? It also provides us with a greater range of tools to tackle a greater range of research problems more appropriately and successfully, filling in the blind spots on one half of the methodological spectrum to better address the whole complexity of neurological research and practice.
Availability of data and materials
Not applicable.
Abbreviations
Endovascular treatment
Randomised Controlled Trial
Standard Operating Procedure
Standards for Reporting Qualitative Research
Philipsen, H., & Vernooij-Dassen, M. (2007). Kwalitatief onderzoek: nuttig, onmisbaar en uitdagend. In L. PLBJ & H. TCo (Eds.), Kwalitatief onderzoek: Praktische methoden voor de medische praktijk . [Qualitative research: useful, indispensable and challenging. In: Qualitative research: Practical methods for medical practice (pp. 5–12). Houten: Bohn Stafleu van Loghum.
Chapter Google Scholar
Punch, K. F. (2013). Introduction to social research: Quantitative and qualitative approaches . London: Sage.
Kelly, J., Dwyer, J., Willis, E., & Pekarsky, B. (2014). Travelling to the city for hospital care: Access factors in country aboriginal patient journeys. Australian Journal of Rural Health, 22 (3), 109–113.
Article Google Scholar
Nilsen, P., Ståhl, C., Roback, K., & Cairney, P. (2013). Never the twain shall meet? - a comparison of implementation science and policy implementation research. Implementation Science, 8 (1), 1–12.
Howick J, Chalmers I, Glasziou, P., Greenhalgh, T., Heneghan, C., Liberati, A., Moschetti, I., Phillips, B., & Thornton, H. (2011). The 2011 Oxford CEBM evidence levels of evidence (introductory document) . Oxford Center for Evidence Based Medicine. https://www.cebm.net/2011/06/2011-oxford-cebm-levels-evidence-introductory-document/ .
Eakin, J. M. (2016). Educating critical qualitative health researchers in the land of the randomized controlled trial. Qualitative Inquiry, 22 (2), 107–118.
May, A., & Mathijssen, J. (2015). Alternatieven voor RCT bij de evaluatie van effectiviteit van interventies!? Eindrapportage. In Alternatives for RCTs in the evaluation of effectiveness of interventions!? Final report .
Google Scholar
Berwick, D. M. (2008). The science of improvement. Journal of the American Medical Association, 299 (10), 1182–1184.
Article CAS Google Scholar
Christ, T. W. (2014). Scientific-based research and randomized controlled trials, the “gold” standard? Alternative paradigms and mixed methodologies. Qualitative Inquiry, 20 (1), 72–80.
Lamont, T., Barber, N., Jd, P., Fulop, N., Garfield-Birkbeck, S., Lilford, R., Mear, L., Raine, R., & Fitzpatrick, R. (2016). New approaches to evaluating complex health and care systems. BMJ, 352:i154.
Drabble, S. J., & O’Cathain, A. (2015). Moving from Randomized Controlled Trials to Mixed Methods Intervention Evaluation. In S. Hesse-Biber & R. B. Johnson (Eds.), The Oxford Handbook of Multimethod and Mixed Methods Research Inquiry (pp. 406–425). London: Oxford University Press.
Chambers, D. A., Glasgow, R. E., & Stange, K. C. (2013). The dynamic sustainability framework: Addressing the paradox of sustainment amid ongoing change. Implementation Science : IS, 8 , 117.
Hak, T. (2007). Waarnemingsmethoden in kwalitatief onderzoek. In L. PLBJ & H. TCo (Eds.), Kwalitatief onderzoek: Praktische methoden voor de medische praktijk . [Observation methods in qualitative research] (pp. 13–25). Houten: Bohn Stafleu van Loghum.
Russell, C. K., & Gregory, D. M. (2003). Evaluation of qualitative research studies. Evidence Based Nursing, 6 (2), 36–40.
Fossey, E., Harvey, C., McDermott, F., & Davidson, L. (2002). Understanding and evaluating qualitative research. Australian and New Zealand Journal of Psychiatry, 36 , 717–732.
Yanow, D. (2000). Conducting interpretive policy analysis (Vol. 47). Thousand Oaks: Sage University Papers Series on Qualitative Research Methods.
Shenton, A. K. (2004). Strategies for ensuring trustworthiness in qualitative research projects. Education for Information, 22 , 63–75.
van der Geest, S. (2006). Participeren in ziekte en zorg: meer over kwalitatief onderzoek. Huisarts en Wetenschap, 49 (4), 283–287.
Hijmans, E., & Kuyper, M. (2007). Het halfopen interview als onderzoeksmethode. In L. PLBJ & H. TCo (Eds.), Kwalitatief onderzoek: Praktische methoden voor de medische praktijk . [The half-open interview as research method (pp. 43–51). Houten: Bohn Stafleu van Loghum.
Jansen, H. (2007). Systematiek en toepassing van de kwalitatieve survey. In L. PLBJ & H. TCo (Eds.), Kwalitatief onderzoek: Praktische methoden voor de medische praktijk . [Systematics and implementation of the qualitative survey (pp. 27–41). Houten: Bohn Stafleu van Loghum.
Pv, R., & Peremans, L. (2007). Exploreren met focusgroepgesprekken: de ‘stem’ van de groep onder de loep. In L. PLBJ & H. TCo (Eds.), Kwalitatief onderzoek: Praktische methoden voor de medische praktijk . [Exploring with focus group conversations: the “voice” of the group under the magnifying glass (pp. 53–64). Houten: Bohn Stafleu van Loghum.
Carter, N., Bryant-Lukosius, D., DiCenso, A., Blythe, J., & Neville, A. J. (2014). The use of triangulation in qualitative research. Oncology Nursing Forum, 41 (5), 545–547.
Boeije H: Analyseren in kwalitatief onderzoek: Denken en doen, [Analysis in qualitative research: Thinking and doing] vol. Den Haag Boom Lemma uitgevers; 2012.
Hunter, A., & Brewer, J. (2015). Designing Multimethod Research. In S. Hesse-Biber & R. B. Johnson (Eds.), The Oxford Handbook of Multimethod and Mixed Methods Research Inquiry (pp. 185–205). London: Oxford University Press.
Archibald, M. M., Radil, A. I., Zhang, X., & Hanson, W. E. (2015). Current mixed methods practices in qualitative research: A content analysis of leading journals. International Journal of Qualitative Methods, 14 (2), 5–33.
Creswell, J. W., & Plano Clark, V. L. (2011). Choosing a Mixed Methods Design. In Designing and Conducting Mixed Methods Research . Thousand Oaks: SAGE Publications.
Mays, N., & Pope, C. (2000). Assessing quality in qualitative research. BMJ, 320 (7226), 50–52.
O'Brien, B. C., Harris, I. B., Beckman, T. J., Reed, D. A., & Cook, D. A. (2014). Standards for reporting qualitative research: A synthesis of recommendations. Academic Medicine : Journal of the Association of American Medical Colleges, 89 (9), 1245–1251.
Saunders, B., Sim, J., Kingstone, T., Baker, S., Waterfield, J., Bartlam, B., Burroughs, H., & Jinks, C. (2018). Saturation in qualitative research: Exploring its conceptualization and operationalization. Quality and Quantity, 52 (4), 1893–1907.
Moser, A., & Korstjens, I. (2018). Series: Practical guidance to qualitative research. Part 3: Sampling, data collection and analysis. European Journal of General Practice, 24 (1), 9–18.
Marlett, N., Shklarov, S., Marshall, D., Santana, M. J., & Wasylak, T. (2015). Building new roles and relationships in research: A model of patient engagement research. Quality of Life Research : an international journal of quality of life aspects of treatment, care and rehabilitation, 24 (5), 1057–1067.
Demian, M. N., Lam, N. N., Mac-Way, F., Sapir-Pichhadze, R., & Fernandez, N. (2017). Opportunities for engaging patients in kidney research. Canadian Journal of Kidney Health and Disease, 4 , 2054358117703070–2054358117703070.
Noyes, J., McLaughlin, L., Morgan, K., Roberts, A., Stephens, M., Bourne, J., Houlston, M., Houlston, J., Thomas, S., Rhys, R. G., et al. (2019). Designing a co-productive study to overcome known methodological challenges in organ donation research with bereaved family members. Health Expectations . 22(4):824–35.
Piil, K., Jarden, M., & Pii, K. H. (2019). Research agenda for life-threatening cancer. European Journal Cancer Care (Engl), 28 (1), e12935.
Hofmann, D., Ibrahim, F., Rose, D., Scott, D. L., Cope, A., Wykes, T., & Lempp, H. (2015). Expectations of new treatment in rheumatoid arthritis: Developing a patient-generated questionnaire. Health Expectations : an international journal of public participation in health care and health policy, 18 (5), 995–1008.
Jun, M., Manns, B., Laupacis, A., Manns, L., Rehal, B., Crowe, S., & Hemmelgarn, B. R. (2015). Assessing the extent to which current clinical research is consistent with patient priorities: A scoping review using a case study in patients on or nearing dialysis. Canadian Journal of Kidney Health and Disease, 2 , 35.
Elsie Baker, S., & Edwards, R. (2012). How many qualitative interviews is enough? In National Centre for Research Methods Review Paper . National Centre for Research Methods. http://eprints.ncrm.ac.uk/2273/4/how_many_interviews.pdf .
Sandelowski, M. (1995). Sample size in qualitative research. Research in Nursing & Health, 18 (2), 179–183.
Sim, J., Saunders, B., Waterfield, J., & Kingstone, T. (2018). Can sample size in qualitative research be determined a priori? International Journal of Social Research Methodology, 21 (5), 619–634.
Download references
Acknowledgements
no external funding.
Author information
Authors and affiliations.
Department of Neurology, Heidelberg University Hospital, Im Neuenheimer Feld 400, 69120, Heidelberg, Germany
Loraine Busetto, Wolfgang Wick & Christoph Gumbinger
Clinical Cooperation Unit Neuro-Oncology, German Cancer Research Center, Heidelberg, Germany
Wolfgang Wick
You can also search for this author in PubMed Google Scholar
Contributions
LB drafted the manuscript; WW and CG revised the manuscript; all authors approved the final versions.
Corresponding author
Correspondence to Loraine Busetto .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Busetto, L., Wick, W. & Gumbinger, C. How to use and assess qualitative research methods. Neurol. Res. Pract. 2 , 14 (2020). https://doi.org/10.1186/s42466-020-00059-z
Download citation
Received : 30 January 2020
Accepted : 22 April 2020
Published : 27 May 2020
DOI : https://doi.org/10.1186/s42466-020-00059-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Qualitative research
- Mixed methods
- Quality assessment
Neurological Research and Practice
ISSN: 2524-3489
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Open access
- Published: 19 May 2023
Clinical nurse competence and its effect on patient safety culture: a systematic review
- Rasha Abu Zaitoun 1 ,
- Nizar B. Said 2 &
- Lila de Tantillo 3
BMC Nursing volume 22 , Article number: 173 ( 2023 ) Cite this article
8157 Accesses
3 Citations
1 Altmetric
Metrics details
Unsafe health practices are one of the leading causes of disability and even death. Competent nurses are crucial to ensure safe and high-quality healthcare services. The patient safety culture is concerned with internalizing safety beliefs, values, and attitudes, translating them into healthcare practices, and committing to maintaining an error-free health environment. A high level of competence ensures the achievement and compliance with the safety culture goal. This systematic review aims to identify the relationship between the level of nursing competence and the safety culture score and perception among nurses at their workplace.
Four international online databases were searched to find relevant studies published between 2018 and 2022. Peer-reviewed articles using quantitative methods, targeting nursing staff, and written in English were included. After reviewing 117 identified studies, 16 full-text studies were included. The PRISMA 2020 checklist for systematic reviews was used.
Evaluation of the studies indicates safety culture, competency, and perception were assessed using various instruments. Safety culture was generally perceived as positive. No unique and standard tool has been developed to investigate the effect of safety competency on the perception of the safety culture in a standardized way.

Conclusions
Existing research provides evidence of a positive correlation between nursing competence and patient safety score. Future research is recommended to investigate ways to measure the effect of nursing competency level on safety culture in healthcare institutions.
Peer Review reports
Unsafe health practices are highly regarded to cause disability and death. It is estimated that the chance that unsafe practice can cause harm for the patient is 1 in 300 chance [ 1 ]. Nearly 400,000 deaths occur annually in the United States due to several reversible adverse events, such as medication error, infection transmission, and fall events [ 2 ]. In addition, poor quality care can cause death and a global health burden [ 3 ]. Patient safety is a health care discipline that evolved as a result of the increasing sophistication of health care systems and the increasing in adverse outcomes in health-care facilities. Its goal is to avoid and decrease risks, mistakes, and harm to patients while providing health care. Therefore, reliable, safe, equitable, effective, and highly standardized patient-centered care has become the ultimate goal of all health care institutions worldwide [ 4 ]. Besides that, patient safety culture focuses on organizational culture issues related to patient safety, patient safety culture is concerned with internalizing safety beliefs, values, and attitudes, translating them into health care practices and commitment to maintaining an error-free health setting and emphasizing reporting culture [ 5 ].
Competent nurses are key contributors to maintaining safe and effective health care services by integrating knowledge, skills, and attitudes that enable them to adapt to dynamic health environments [ 6 ]. Nurses are often the primary point of contact for patients and are responsible for ensuring that their needs are met. By providing patient-centered care, nurses can help create a culture that prioritizes patient safety. In addition, they can act as advocates for patient safety, promoting a culture of safety within the organization and encouraging others to do the same. Nurses should be given the power to make decisions about patient care and safety, as well as to report any harmful conditions or concerns. They can indeed act as role models for other healthcare professionals, emphasizing the importance of patient safety and providing a good example for others to follow.
Patient safety competencies are a core competency in the continuum of professional development activities that protect patients from unnecessary risks and hazards [ 7 ]. A high level of competence promotes the achievement and compliance with the patient safety goal.
Several studies found that patient safety culture and nurse safety competency are affected by many factors. For example, workplace regulations and climate, nursing fatigue, satisfaction, stress, demographics, type of health institution type, teamwork and learning opportunity, specialty, degree of bedside involvement, and job description are all factors that affect safety culture [ 5 , 8 , 9 , 10 , 11 ].
Any improvement strategies to modulate these factors are unnegotiable. However, a better understanding of nurse competence and patient safety culture is essential to improve safe practice and professional development and minimize adverse events [ 12 ]. Therefore, this systematic review aimed to evaluate the literature concerning the relationship between self-reported competencies and the perception of patient safety among nurses in their workplace. In addition, to understand how related studies evaluated nurses’ core competencies and safety culture.
Study design
The present systematic review was designed and conducted from April 1, 2022, and April 11, 2022, by the electronic search from January 1, 2018, through May 1, 2022. This date period was chosen after agreement between the author to find the (five years) recent evidence regarding the respected review topic. The current systematic review was framed by SPIDER [ 13 ] with nurses as the Sample (S); clinical competence as the Phenomenon of Interest (PI); Design (D) as quantitative or mixed-methods studies; Evaluation (E) as covering assessments of patient safety culture; and Research Type (R) as referring to all types of studies with the exception of case studies and review articles. The protocol was performed based on the guidelines of the Preferred Reporting Items for Systematic Review and Meta-Analyses Protocol (PRISMA-P) [ 14 ].
Search strategy and data sources
Four online databases including MEDLINE (via PubMed), CINHAL (via EBSCOhost), Scopus (via Elsevier), and Embase were searched for published studies that describing the relationship between nurse competencies and patient safety culture. Search terms were developed based on experience and keywords from similar research. The search was structured using Boolean operators (AND, OR) and consisted of MeSH terms and free terms related to nursing, patient safety, competency, and safety culture. The term ‘OR’ was used between keywords or comparable MeSH phrases; meanwhile, the Boolean operator ‘AND’ was used to connect phrases or keywords with different meanings to refine the search (see Appendix A). Relevant studies were identified by two reviewers (R.A. and L.T.) independently, and search algorithm varied according to the specifications of each database. To identify the additional relevant studies being lost in the database search, we checked the references of the selected publications.
Inclusion and exclusion criteria
In this review, studies were included if they are using the quantitative approach mainly; targeting nursing staff; published in English language, and full text available. The exclusion criteria were studies in the form of letters, editorials, essays, case studies, comments or narrative, systematic reviews, and conference abstracts; studies focus on nursing students only; and studies of pre-hospital and ambulatory care.
Study selection and quality assessment
After preliminary selection of studies by the first reviewer (R.A) and their verification by the last reviewer (L.T.) the duplicated studies were excluded. Two reviewers (R.A. and L.T.) independently screened the titles, abstracts and full text of the studies.
The Mixed Methods Appraisal Tool (MMAT) [ 15 ] was used to evaluate the quality of the studies included in this review. With the MMAT, two basic screening questions must be asked first to determine whether or not the quality appraisal for a specific study will be continued. The first question is whether the related qualitative, quantitative, or mixed-methods study has clear research questions or objectives. The second question is whether the method of data collection addresses the research questions or objectives. When these initial screening questions are answered positively, qualitative (QUAL) or quantitative (QUAN) studies can be rated as follows: ‘*’ (25%) for one met criterion, ‘**’ (50%) for two, ‘***’ (75%) for three, or ‘****’ (100%) for the highest quality study. Studies with a rating of ** or higher were considered to be of acceptable quality for this review and were included for further analysis.
Data extraction
Data extraction table included: author(s) and publication year, country, design of study, method of data collection, quality assessment. Measurement Tools for Safety Culture and Nursing Competency and main findings focusing on Patient Safety Competency and the Patient Safety Culture. In this stage two authors (R.Z. and L.T.) independently extracted data from the included studies. In case of disagreement between two reviewers (R.Z. and L.T.), a third reviewer (N.S) was involved to make a final decision.
Data synthesis
An iterative narrative synthesis technique was used for data analysis [ 16 ] to identify key themes from every study that would adequately and accurately reflect the findings about clinical nurse competence and patient safety culture. The narrative synthesis was divided into four stages: (1) identifying a frame of how findings from related studies work, why and for whom; (2) synthesizing themes through an iterative process of comparing and examining findings from the included studies; (3) trying to explore themes’ relationships; and (4) evaluating the synthesis’s robustness.
Results of the search strategy
Through the flow of PRISMA-P, the search process found 1341 potentially relevant studies; initial screening revealed that 6 records were duplicated. After excluding the irrelevant studies by title and abstract review (1217) and applying exclusion criteria (57), reports not retrieved related to access issues (n = 18). Full text screening showed that 27 were not relevant. Finally, 16 studies remained and were included in the analysis (Fig. 1 ).
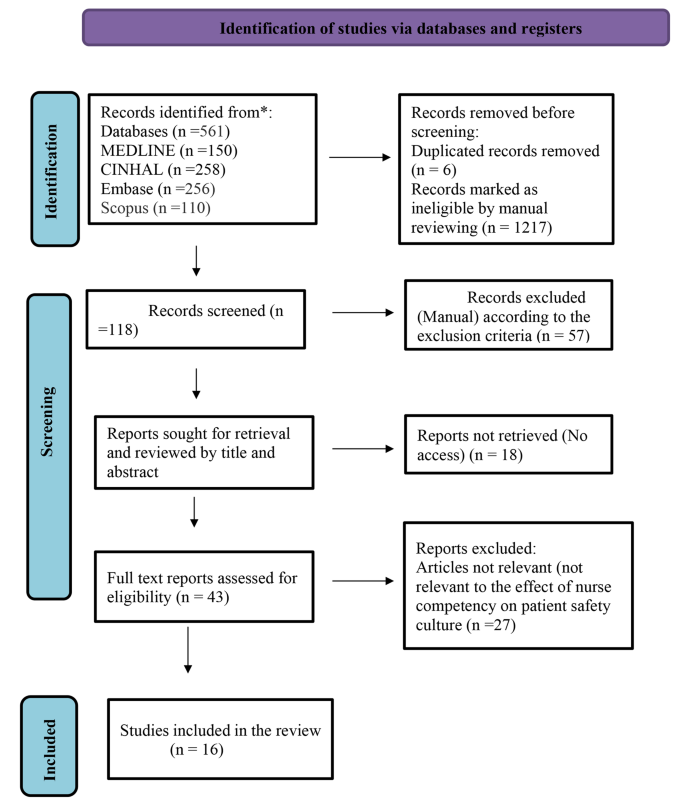
PRISMA flow diagram of the systematic review
The design of the reviewed studies
Of the 16 qualifying studies, 14 were cross-sectional descriptive studies, one applied a quasi-experimental, pretest-posttest design [ 17 ], and one study used a mixed method approach [ 18 ]. Three out of the sixteen studies were conducted in South Korea [ 19 , 20 , 21 ], Canada [ 19 ] Three studies originated from Saudi Arabia [ 9 , 22 , 23 ]. Two studies from Iran [ 24 , 25 ]. In addition, a study was conducted in each Australia [ 26 ], Belgium and Palestine [ 27 ], Brazil [ 28 ], Jordan [ 29 ], Spain [ 18 ], England [ 17 ], and China [ 11 ]. The aforementioned research studies were published from 2019 to 2022 in different journals. Summary of the characteristics of included studies are depicted in Table 1 .
The sampling technique
Given the sampling technique, eight articles used the convenience sampling technique [ 9 , 11 , 19 , 22 , 23 , 25 , 26 , 30 ]. The highest sample size was 2,836 participants in the study by Najjar et al. [ 27 ], while the least was 56 participants in [ 28 ] study.
Methodological quality of included studies
The assessment of the methodological quality of the included studies is presented in Table 2 . After quality assessment, nine studies graded as ‘****’ (100%) and seven studies as ‘***’ (75%) quality using MMAT. Research conducted or published during the COVID-19 outbreak period [ 9 , 11 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 28 , 29 ] received additional review to ensure it met rationale for inclusion and standards for quality, to ensure rigor in response to the substandard work proliferating during this period [ 31 ].
Measurement tools for Safety Culture and nursing competency
The construct concepts of patient safety culture, safety climate, and patient safety competency were operationally measured using various tools or instruments throughout the sixteen studies. Nursing safety competency was measured using the Patient Safety Competency Self-Evaluation Tool, the Health Professional Education in Patient Safety Survey (H-PEPSS) [ 21 ], and the Nurses’ Attitudes and Skills Safety scale, the latest version of NASUS [ 23 ]. Furthermore, AS Alshehry [ 22 ] used the Health Professional Education in Patient Safety Survey (H-PEPSS) to assess safety competency. Halabi et al. [ 9 ] used the short version of Nurse Professional Competence (NPC).The self-reported Patient Safety Competency Nurse Evaluation Scale (PSCNES) was used by Yan et al. [ 11 ].
Three studies applied the Hospital Survey on Patient Safety Culture (HSOPSC) developed by the Agency for Healthcare Research and Quality to measure safety culture [ 21 , 27 , 32 ]. The safety climate was measured using the Safety Attitudes Questionnaire (SAQ) and the Safety Climate Survey (SCS); [ 26 , 28 , 29 ] (Table 2 ).
The patient safety culture
Patient safety culture was mentioned in the title of six studies [ 21 , 23 , 27 , 28 , 32 , 33 ]. There was considerable variation of how this concept was perceived among nurses for example, LM Lousada, FC da Silva Dutra, BV da Silva, NLL de Oliveira, IB Bastos, PF de Vasconcelos and R de Carvalho [ 28 ] in his study found that professionals working in home care services perceived higher scores related to safety culture compared with those working in primary care services. The accredited primary center in Jordan had an average positive response rate in some safety cultures ranging from 58.54 to 75.63% [ 33 ], A total of 32 Iranian teaching hospitals out of 150 reported poor patient safety culture [ 32 ]. On the other hand, and with regard to the safety climate, the study by CJ Connell, S Cooper and R Endacott [ 26 ] revealed that novice-competent nurses in Australian emergency departments rated the safety climate higher than expert nurses in all domains except stress recognition.
Patient safety competency
Six studies examined patient safety competency and several studies connected safety competencies with the domains of safety culture. For example, L Yan, L Yao, Y Li and H Chen [ 11 ] assessed the safety competence scores of Chinese nurses with associate degree and they scored moderate level. A Habibi Soola, M Ajri-Khameslou, A Mirzaei and Z Bahari [ 25 ] found a positive correlation between safety competence and the dimension of team work, psychological safety, leadership, communication, mutual support, situation monitoring, and team structure. JH Han and YS Roh [ 20 ] found that the night shift among emergency nurses in Korean hospitals negatively affected safety competence and was significantly and positively correlated with the number of years of experience in the emergency department and number of reported adverse events by others.
In a medical city in Saudi Arabia, AS Alshehry [ 22 ] studied the correlation between the conflict between nurses and the patient, and safety competencies. The study revealed that nurses were highly competent in effective communication, but they had the lowest competency in ‘working in teams with other health professionals.’ Nurses perceived ‘mistrust of motivations’ and “contradictory communication” got the poorer self-reported safety competency.
The purpose of this study was to provide a systematic review of the literature investigating the relationship between nursing competencies and perception of patient safety among nurses in their workplace. In this systematic review, and after a thorough analysis of the entire manuscript of the retrieved articles, we selected and discussed sixteen articles based on their conformity with the inclusion criteria.
Nurse’ competence refers to the knowledge, skills, and abilities that nurses possess to provide safe and effective care to patients in many fields such as clinical, safety, communication, and leadership. This can include things like knowledge of clinical guidelines, critical thinking skills, and the ability to identify and respond to changes in a patient’s condition, how to manage conflict and communicate with patients and other health care team. A positive patient safety culture is one in which all members of the healthcare team are committed to providing safe care and are empowered to identify and report potential hazards. Research has shown that, specifically, safety nurse competence is positively associated with a positive patient safety culture [ 34 ]. Nurses who are competent in their practice are more likely to be engaged in the safety culture of their organization and more likely to identify and report safety concerns [ 11 ]. Additionally, nurses who possess the knowledge, skills and abilities required to provide safe care are less likely to make errors which can lead to adverse patient outcomes [ 35 ]. Overall, clinical nurse competence is a critical component of a positive patient safety culture, as it helps ensure that nurses are able to provide safe and effective care to patients and promotes engagement and active participation in the safety culture of the organization.
None of the reviewed articles explicitly explored the relationship between clinical or professional nursing competencies and the safety culture dimensions and how they affect each other. Furthermore, studies identified no specific comprehensive tool with high reliability and validity and mostly recommend assessing the relationship between nursing safety competency and the dimensions of safety culture. Rather, the included articles examined patient safety culture, health care safety climate, and other nursing competencies that influenced or affect safety climate independently. Most of the retrieved studies investigated the very specific competencies for nurses which were safety competency and the level of this competency varied among different clinical setting or nationality and range between poor and moderate level and this similar to SM Cho and J Choi [ 36 ] in their study investigated relationship between the three parts of safety competency and domains of patient safety culture among 343 registered nurses in an educational hospital in, South Korea and found that the safety competency was highly correlated with teamwork within units. Teamwork within and across units, supervisor or manager expectations, and each of the three patient safety competencies were strongly associated to attitudes, while teamwork within units and learning were significantly connected to skills. Knowledge was only significantly correlated with organizational learning.
The concentration on assessing and improving Safety competency for nurses instead of more general clinical nurse competence may due to that many health care institutions tend to adopt the principles of patients safety as their institutional goal and so try to improve nursing skills, knowledge and attitude related to patient safety and it would be better to assess the level of nurses’ culture of safety and their safety competency level in order to improve area of weakness or poor practices and reduce adverse events [ 37 , 38 ].
Measurement of patient safety culture
Measuring patient safety culture involves assessing the attitudes, perceptions, and behaviors of healthcare staff related to patient safety in a healthcare organization. There are several tools and survey instruments available to measure patient safety culture. In this review, two self-reported questionnaires were found to have been applied to understand the dimensions and scores of patient safety culture in health institutions. The Safety Attitude Questionnaire (SAQ) [ 28 , 33 ] and the Hospital Survey on Patient Safety Culture (HSOPSC) [ 21 , 23 , 27 , 32 ] were two assessment tools that employed Likert scales. However, in their study, G Alsalem, P Bowie and J Morrison [ 39 ] revealed that five instruments are used to assess the patient safety culture and climate in health institutions. Furthermore, these tools vary in their psychometric properties and scope.
The aforementioned survey instruments assess various aspects of patient safety culture, such as communication, teamwork, error reporting, and leadership. The results of these surveys can be used to identify areas of strength and areas for improvement in the patient safety culture of an organization.
In general, patient safety culture measurement is a continuous activity that should be conducted on a regular basis to assess success and identify areas for improvement. The information gathered through these surveys and other ways may be utilized to design and execute plans to improve the patient safety culture.
The most common study design among the studies was a questionnaire-based descriptive quantitative approach. Using different study designs, such as qualitative research and a variety of data collection methods, could help improve understanding of the safety culture and health care provider perceptions and would be required to address the existing relationship between safety culture and nursing competency [ 40 ].
Measurement of safety nursing competency
Eight of the studies, or 50% of the literature, in this review showed that nurses were more competent in communicating effectively than working in teams with colleagues, and their overall safety culture score was positive. Likewise, LM Zabin, RSA Zaitoun and AA Abdullah [ 41 ] found that both organizational learning and continuous improvement, as well as cooperation within units, received the highest composite frequency of patient safety perception.
In the current findings, the reviewed literature mentioned four self-reported measurement tools for safety competency. Despite that, there was no consensus on the best tool for measuring safety competencies, and the lack of a key self-reported tool for measuring safety culture and linking it to nursing safety competency limited the ability to directly assess the effect of nursing competency on safety culture [ 42 ]. As a result, more research is needed to enrich the literature, improve the understanding of the effect of safety competency on safety culture scores among nurses, and help in providing more appropriate operational definition of safety culture and nursing safety competency [ 43 ].
Although we used broad keywords to search different online databases, the retrieved articles did not specifically discuss the relationship between the dimensions of the safety culture, perception, and competency in nursing safety. Additionally, the lack of a standardized tool to measure the concepts of safety culture and nursing safety competency made it difficult to find a robust number of targeted studies and limited our ability to find specific operational definitions to the concepts of safety culture and nursing safety competency that was used consistently across the literature.
Moreover, using self-reported surveys and relying on convenient sampling eased data collection and provide more objective data for many of the studies in this review. However, there were drawbacks that limited the generalizability and might not cover all aspects of the studies’ content. Therefore, future use of mixed designs with the use of qualitative methods is highly recommended to deepen the study issue and explore the unique relationship between the dimensions of the safety culture and nursing competency that can play a pivotal role in improving safety practices.
This review study recognizes the importance of conducting additional searches and reviews and broadening the scope of keywords used to search online databases to focus on the core of this study. In addition, it is recommended to investigate the effect of nursing competency on perceptions of dimensions of safety culture and to make valid comparisons between demographics and cultures.
More research would provide a better understanding and may have a greater clinical impact and aid in improving and delivering highly effective, safe, and efficient care. Furthermore, the findings would support synchronicity between academic clinical programs and nursing staff safety practices. For example, nursing students receive competency-based training that allows them to live in a safe environment and directly implement the dimension of safety culture [ 44 ].
Limitations
This systematic review study has several limitations. First, we restricted the databases to four primary resources considered suitable for gathering eligible articles for the study purpose. The second is that the delimiters of this review included only articles in English, so some related articles may not have been included. Another limitation that should be highlighted is that we reviewed articles published between 2018 and 2022 to include the most recent data, but this also restricted the number of retrieved studies.
Another potential limitation was that the results of the reviewed studies could not be generalized. The articles were only published in peer-reviewed journals to ensure the high quality of evidence and the reported findings, which omitted many worthwhile studies such as grey and unpublished studies. Additionally, the study designs of the majority of the retrieved papers were descriptive, which restricts the generalizability of their findings and prevents access to many relevant studies. Therefore, it is recommended to conduct further systematic or integrative reviews that might include qualitative and descriptive studies as well as expand the inclusion criteria for other types of literature.
This systematic review draws several conclusions from the sixteen reviewed articles. First, the study showed no specific tool to measure the safety culture and nursing safety competency dimensions. Additionally, no study explicitly discussed the effect of nursing safety competency on safety culture scores among nursing staff. However, most of the studies employed a questionnaire-based descriptive approach. Conducting more research with different study designs such as the experimental, qualitative, and longitudinal approaches may enhance the understanding and assist in constructing a valid and more reliable tool to measure the effect of nursing safety competency on safety culture. Second, rigorous research needed to establish a well-designed competency-based training program to improve safety scores among more diverse demographics and cultures is needed. The findings can motivate administrators to promote safety culture in different health care facilities, as well as increase professional awareness of the factors that impact safety culture and, consequently, patient safety. Finally, the key to improving safety competency for nurses is to create a culture of continuous learning and improvement, where nurses are encouraged and supported to develop their knowledge, skills and abilities in order to provide safe, high-quality care to patients.
Data Availability
All data generated or analyzed during this study are included in this published article. The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Patient safety [ https://www.who.int/news-room/facts-in-pictures/detail/patient-safety ].
Patient Safety Representatives Unite to Implement Global Patient Safety Action Plan. in the United States [ https://blogs.cdc.gov/safehealthcare/patient-safety-action-plan/ ].
Kruk ME, Gage AD, Joseph NT, Danaei G, García-Saisó S, Salomon JA. Mortality due to low-quality health systems in the universal health coverage era: a systematic analysis of amenable deaths in 137 countries. The Lancet. 2018;392(10160):2203–12.
Article Google Scholar
Patient Safety. [ https://www.who.int/news-room/fact-sheets/detail/patient-safety ].
Khoshakhlagh AH, Khatooni E, Akbarzadeh I, Yazdanirad S, Sheidaei A. Analysis of affecting factors on patient safety culture in public and private hospitals in Iran. BMC Health Serv Res. 2019;19(1):1009.
Article PubMed PubMed Central Google Scholar
Fukada M. Nursing competency: definition, structure and development. Yonago acta medica. 2018;61(1):001–7.
Huh A, Shin JH. Person-centered care practice, patient safety competence, and patient safety nursing activities of nurses working in geriatric hospitals. Int J Environ Res Public Health. 2021;18(10):5169. https://doi.org/10.3390/ijerph18105169
Al Ma’mari Q, Sharour LA, Al Omari O. Fatigue, burnout, work environment, workload and perceived patient safety culture among critical care nurses. Br J Nurs. 2020;29(1):28–34.
Article PubMed Google Scholar
Halabi JO, Nilsson J, Lepp M. Professional competence among registered nurses working in hospitals in Saudi Arabia and their experiences of quality of nursing care and patient safety. J Transcult Nurs. 2021;32(4):425–33. https://doi.org/10.1177/1043659621992845
Wang KY, Chou CC, Lai JC. A structural model of total quality management, work values, job satisfaction and patient-safety-culture attitude among nurses. J Nurs Adm Manag. 2019;27(2):225–32.
Yan L, Yao L, Li Y, Chen H. Assessment and analysis of patient safety competency of chinese nurses with associate degrees: a cross-sectional study. Nurs Open. 2021;8(1):395–403. https://doi.org/10.1002/nop2.640
Wami SD, Demssie AF, Wassie MM, Ahmed AN. Patient safety culture and associated factors: a quantitative and qualitative study of healthcare workers’ view in Jimma zone Hospitals, Southwest Ethiopia. BMC Health Serv Res. 2016;16:495.
Cooke A, Smith D, Booth A. Beyond PICO: the SPIDER tool for qualitative evidence synthesis. Qual Health Res. 2012;22(10):1435–43.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906.
Pluye P, Robert E, Cargo M, Bartlett G, O’cathain A, Griffiths F, Boardman F, Gagnon M-P, Rousseau M. Proposal: a mixed methods appraisal tool for systematic mixed studies reviews. Montréal: McGill University. 2011;2:1–8.
Google Scholar
Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, Britten N, Roen K, Duffy S. Guidance on the conduct of narrative synthesis in systematic reviews. Prod ESRC methods programme Version. 2006;1(1):b92.
Letourneau RM, McCurry MK. The effect of transition to Practice Programs on the Self-Assessment of newly licensed registered Nurses’ confidence in Quality and Safety Competency Attainment. Nurs Educ Perspect. 2019;40(3):151–6. https://doi.org/10.1097/01.Nep.0000000000000438
Peñataro-Pintado E, Rodríguez-Higueras E, Llauradó-Serra M, Gómez-Delgado N, Llorens-Ortega R, Díaz-Agea JL. Development and Validation of a Questionnaire of the Perioperative Nursing Competencies in Patient Safety. Int J Environ Res Public Health 2022, 19(5). https://doi.org/10.3390/ijerph19052584
Huh A, Shin JH. Person-Centered Care Practice, Patient Safety Competence, and Patient Safety Nursing Activities of Nurses Working in Geriatric Hospitals. Int J Environ Res Public Health 2021, 18(10).
Han JH, Roh YS. Teamwork, psychological safety, and patient safety competency among emergency nurses. Int Emerg Nurs. 2020;51:100892. https://doi.org/10.1016/j.ienj.2020.100892
Han Y, Kim JS, Seo Y. Cross-sectional study on Patient Safety Culture, Patient Safety Competency, and adverse events. West J Nurs Res. 2020;42(1):32–40. https://doi.org/10.1177/0193945919838990
Alshehry AS. Nurse–patient/relatives conflict and patient safety competence among nurses. INQUIRY: The Journal of Health Care Organization Provision and Financing. 2022;59. https://doi.org/10.1177/00469580221093186
Mahsoon AN, Dolansky M. Safety culture and systems thinking for predicting safety competence and safety performance among registered nurses in Saudi Arabia: a cross-sectional study. J Res Nurs. 2021;26(1–2):19–32.
Kakemam E, Gharaee H, Rajabi MR, Nadernejad M, Khakdel Z, Raeissi P, Kalhor R. Nurses’ perception of patient safety culture and its relationship with adverse events: a national questionnaire survey in Iran. BMC Nurs. 2021;20(1):1–10. https://doi.org/10.1186/s12912-021-00571-w
Habibi Soola A, Ajri-Khameslou M, Mirzaei A, Bahari Z. Predictors of patient safety competency among emergency nurses in Iran: a cross-sectional correlational study. BMC Health Serv Res. 2022;22(1):1–10. https://doi.org/10.1186/s12913-022-07962-y
Connell CJ, Cooper S, Endacott R. Measuring the safety climate in an australian emergency department. Int Emerg Nurs. 2021;58:101048.
Najjar S, Baillien E, Vanhaecht K, Hamdan M, Euwema M, Vleugels A, Sermeus W, Schrooten W, Hellings J, Vlayen A. Similarities and differences in the associations between patient safety culture dimensions and self-reported outcomes in two different cultural settings: a national cross-sectional study in palestinian and belgian hospitals. BMJ Open. 2018;8(7):e021504. https://doi.org/10.1136/bmjopen-2018-021504
Lousada LM, da Silva Dutra FC, da Silva BV, de Oliveira NLL, Bastos IB, de Vasconcelos PF, de Carvalho R. Patient safety culture in primary and home care services. BMC Fam Pract. 2020;21(1):188. https://doi.org/10.1186/s12875-020-01263-1
Khamaiseh A, Al-Twalbeh D, Al-Ajlouni K. Patient safety culture in jordanian primary health-care centres as perceived by nurses: a cross-sectional study. East Mediterr Health J. 2020;26(10):1242–50. https://doi.org/10.26719/emhj.20.044
Son YJ, Lee EK, Ko Y. Association of Working Hours and Patient Safety Competencies with Adverse Nurse Outcomes: A Cross-Sectional Study. Int J Environ Res Public Health 2019, 16(21). https://doi.org/10.3390/ijerph16214083
Bramstedt KA. The carnage of substandard research during the COVID-19 pandemic: a call for quality. J Med Ethics. 2020;46(12):803–7.
Kakemam E, Gharaee H, Rajabi MR, Nadernejad M, Khakdel Z, Raeissi P, Kalhor R. Nurses’ perception of patient safety culture and its relationship with adverse events: a national questionnaire survey in Iran. BMC Nurs. 2021;20(1):60.
Khamaiseh A, Al-Twalbeh D, Al-Ajlouni K: Patient safety culture in Jordanian primary health-care centres as perceived by nurses: a cross-sectional study. East Mediterr Health J. 2020;26(10):1242–1250.
Hwang J-I. What are hospital nurses’ strengths and weaknesses in patient safety competence? Findings from three korean hospitals. Int J Qual Health Care. 2015;27(3):232–8.
Mahsoon AN, Dolansky M: Safety culture and systems thinking for predicting safety competence and safety performance among registered nurses in Saudi Arabia: a cross-sectional study. Journal of Research in Nursing. 2021;26(1–2):19–32.
Cho SM, Choi J. Patient Safety Culture Associated with Patient Safety Competencies among registered nurses. J Nurs Scholarsh. 2018;50(5):549–57.
Rodziewicz TL, Houseman B, Hipskind JE. Medical Error Reduction and Prevention. In: StatPearls . edn. Treasure Island (FL): StatPearls Publishing Copyright © 2022,StatPearls Publishing LLC.; 2022.
Hafezi A, Babaii A, Aghaie B, Abbasinia M. The relationship between patient safety culture and patient safety competency with adverse events: a multicenter cross-sectional study. BMC Nurs. 2022;21(1):292.
Alsalem G, Bowie P, Morrison J. Assessing safety climate in acute hospital settings: a systematic review of the adequacy of the psychometric properties of survey measurement tools. BMC Health Serv Res. 2018;18(1):353.
Alqattan H, Morrison Z, Cleland JA. A narrative synthesis of qualitative studies conducted to assess patient Safety Culture in Hospital settings. Sultan Qaboos Univ Med J. 2019;19(2):e91–8.
Zabin LM, Zaitoun RSA, Abdullah AA. Patient safety culture in Palestine: university hospital nurses’ perspectives. BMC Nurs. 2022;21(1):204.
Arzahan ISN, Ismail Z, Yasin SM. Safety culture, safety climate, and safety performance in healthcare facilities: a systematic review. Saf Sci. 2022;147:105624.
Kalteh HO, Mortazavi SB, Mohammadi E, Salesi M. The relationship between safety culture and safety climate and safety performance: a systematic review. Int J Occup Saf Ergon. 2021;27(1):206–16.
Debourgh GA. Synergy for patient safety and quality: academic and service partnerships to promote effective nurse education and clinical practice. J Prof nursing: official J Am Association Colleges Nurs. 2012;28(1):48–61.
Download references
Acknowledgements
Not applicable.
This work was not supported by research funding.
Author information
Authors and affiliations.
Head of the Continuing Nursing Education, nursing department, An Najah National University Hospital, Nablus, Palestine
Rasha Abu Zaitoun
Department of Nursing and Midwifery, Faculty of Medicine and Health Sciences, An Najah National University, Nablus, Palestine
Nizar B. Said
Keigwin School of Nursing, Jacksonville University, Brooks Rehabilitation College of Healthcare Sciences, 2800 University Boulevard North, Jacksonville, FL, 32211 904.256.8955, USA
Lila de Tantillo
You can also search for this author in PubMed Google Scholar
Contributions
R.A.: Conceptualization, Introduction, Methodology, Analysis and results, Discussion, and Conclusion. L.T.: Conceptualization, Methodology, Analysis, Discussion, and Conclusion.N.S.: Review & Editing. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Rasha Abu Zaitoun .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Zaitoun, R.A., Said, N.B. & de Tantillo, L. Clinical nurse competence and its effect on patient safety culture: a systematic review. BMC Nurs 22 , 173 (2023). https://doi.org/10.1186/s12912-023-01305-w
Download citation
Received : 23 September 2022
Accepted : 15 April 2023
Published : 19 May 2023
DOI : https://doi.org/10.1186/s12912-023-01305-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Patient safety
- Nursing competence
- Safety culture
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
- Open access
- Published: 14 March 2024
Correction: “Because it eases my childbirth plan”: a qualitative study on factors contributing to preferences for caesarean section in Thailand
- Sasitara Nuampa 1 ,
- Ameporn Ratinthorn 1 ,
- Pisake Lumbiganon 2 ,
- Somporn Rungreangkulkij 3 ,
- Nilubon Rujiraprasert 3 ,
- Natthapat Buaboon 4 ,
- Nampet Jampathong 5 ,
- Alexandre Dumont 6 ,
- Claudia Hanson 7 ,
- Myriam de Loenzien 6 ,
- Meghan A. Bohren 8 &
- Ana Pilar Betrán 9
BMC Pregnancy and Childbirth volume 24 , Article number: 202 ( 2024 ) Cite this article
28 Accesses
Metrics details
The Original Article was published on 24 April 2023
Correction : BMC Pregnancy Childbirth 23, 280 (2023)
https://doi.org/10.1186/s12884-023-05576-8 .
Following publication of the original article [ 1 ], the authors reported an error in Ethics approval and consent to participate section.
The current information states “Udon Thani Hospital (UDH REC No 28/2564)” which should be amended to “Udon Thani Hospital (UDH REC No 28/2563). ”
The original article has been corrected.
Nuampa, S., Ratinthorn, A., Lumbiganon, P. et al. “Because it eases my Childbirth Plan”: a qualitative study on factors contributing to preferences for caesarean section in Thailand. BMC Pregnancy Childbirth. 2023;23:280. https://doi.org/10.1186/s12884-023-05576-8
Download references
Author information
Authors and affiliations.
Department of Obstetrics and Gynaecological Nursing, Faculty of Nursing, Mahidol University, Bangkok, Thailand
Sasitara Nuampa & Ameporn Ratinthorn
Department of Obstetrics and Gynaecology, Faculty of Medicine, Khon Kaen University, Khon Kaen, Thailand
Pisake Lumbiganon
Centre for Research and Training on Gender and Women’s Health, Faculty of Nursing, Khon Kaen University, Khon Kaen, Thailand
Somporn Rungreangkulkij & Nilubon Rujiraprasert
Department of Family of Nursing and Midwifery, Faculty of Nursing, Thammasat University, Prathumthani, Thailand
Natthapat Buaboon
Cochrane Thailand, Khon Kaen University, Khon Kaen, Thailand
Nampet Jampathong
Université Paris Cité, IRD, Paris, Ceped, F-75006, Inserm, France
Alexandre Dumont & Myriam de Loenzien
Department of Global Public Health, Karolinska Institutet, Stockholm, Sweden
Claudia Hanson
UNDP/UNFPA/UNICEF/WHO/World Bank Special Program of Research, Development and Research Training in Human Reproduction (HRP), Department of Sexual and Reproductive Health and Research, World Health Organization, Carlton, VIC, Australia
Meghan A. Bohren
Gender and Women’s Health Unit, Centre for Health Equity, School of Population and Global Health, University of Melbourne, Geneva, Switzerland
Ana Pilar Betrán
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Ameporn Ratinthorn .
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The online version of the original article can be found at https://doi.org/10.1186/s12884-023-05576-8 .
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Nuampa, S., Ratinthorn, A., Lumbiganon, P. et al. Correction: “Because it eases my childbirth plan”: a qualitative study on factors contributing to preferences for caesarean section in Thailand. BMC Pregnancy Childbirth 24 , 202 (2024). https://doi.org/10.1186/s12884-024-06379-1
Download citation
Published : 14 March 2024
DOI : https://doi.org/10.1186/s12884-024-06379-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
BMC Pregnancy and Childbirth
ISSN: 1471-2393
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- NCSBN Member Login Submit
Access provided by
Login to your account
If you don't remember your password, you can reset it by entering your email address and clicking the Reset Password button. You will then receive an email that contains a secure link for resetting your password
If the address matches a valid account an email will be sent to __email__ with instructions for resetting your password
Download started.
- PDF [167 KB] PDF [167 KB]
- Add To Online Library Powered By Mendeley
- Add To My Reading List
- Export Citation
- Create Citation Alert
Qualitative Research in Nursing and Health Professions Regulation
- Allison Squires, PhD, RN, FAAN Allison Squires Search for articles by this author
- Caroline Dorsen, PhD, FNP, RN Caroline Dorsen Search for articles by this author
- Credentialing
- government regulation
- professional autonomy
- qualitative research
- • Explain the importance of qualitative research for studies about regulatory issues in nursing.
- • Discuss the core concepts of qualitative research.
- • Describe common methodological challenges researchers can encounter when conducting qualitative research on professional regulatory issues.
- • Identify solutions that can enhance the quality, rigor, and trustworthiness of the findings for regulatory studies.
- Blackman T.
- Google Scholar
- Bradley E.H.
- Devers K.J.
- Scopus (2268)
- Evans-Agnew R.A.
- Boutain D.M.
- Griffith D.M.
- Shelton R.C.
- Scopus (30)
- Waterfield J.
- Holden M.A.
- Ismail K.M.
- Foster N.E.
- Saunders B.
- Kingstone T.
- Scopus (4849)
- Scopus (709)
- Vandermause R.
- Edmundson L.
- Perfetti A.R.
- Yardley S.J.
- Richardson J.C.
A Review of Core Qualitative Research Concepts
- Bochner A.P.
- Scopus (1407)
- Scopus (3242)
- Open table in a new tab
- Patton M.Q.
- Hennink M.M.
- Kaiser B.N.
- Marconi V.C.
- Scopus (1581)
- Vanstone M.
A Note on Cross-language Qualitative Research on Regulatory Issues
- Scopus (135)
- Scopus (386)
- Ziebland S.
- Chiumento A.
- Barbour R.S.
- Poon M.K.-L.
- Scopus (35)
- Lincoln Y.S.
- Gonzalez y Gonzalez E.M.
- Aroztegui Massera C.
- MacKenzie C.A.
- Santos H.P.O.
- Sandelowski M.
- Scopus (98)
- Suurmond J.
- Woudstra A.
- Essink-Bot M.-L.
- Scopus (190)
- Wong J.P.-H.
- Scopus (110)
An Overview of Qualitative Study Designs Appropriate for Regulatory Studies
- Carter S.M.
- Scopus (411)
- Scopus (265)
- Scopus (115)
- Scopus (76)
- Scopus (179)
- Trinidad S.B.
- Scopus (1324)
- van Manen M.
- Willis D.G.
- Sullivan-Bolyai S.
- Scopus (212)
Underutilized Qualitative Designs in Regulatory Research
- Anderson R.A.
- Crabtree B.F.
- Steele D.J.
- McDaniel R.R.
- Scopus (184)
- Carolan C.M.
- Cresswell K.
- Robertson A.
- Morgan S.J.
- Pullon S.R.H.
- Macdonald L.M.
- McKinlay E.M.
- Anderson R.
- Hardwick R.
- Vowinkel J.
- Fletcher A.
- Scopus (158)
- van Belle S.
- van Olmen J.
- Scopus (295)
- Westhorp G.
- Macintyre Latta M.
- Schnellert L.
- Spector-Mersel G.
- Wolgemuth J.R.
Design Dictates the Analytic Approach
- Castro F.G.
- Kellison J.G.
- Scopus (292)
- Scopus (218)
Samples, Sampling, and Saturation
- Malterud K.
- Siersma V.D.
- Guassora A.D.
- MacPhail C.
- Ranganathan M.
- Nelson L.K.
- Norris A.C.
- Farris A.J.
- Babbage D.R.
- Scopus (97)
- Scopus (10126)
Framing Findings
- Scopus (242)
- • Introducing quotes with a single sentence, rather than establishing the context of the quote and how it links to the theme
- • Inserting overly long quotes to represent experiences or the phenomenon
- • Failing to transition between quotes and the next paragraph without an explanatory or transition sentence
- • Choosing quotes that do not represent the theme
- • Inserting too many quotes
- • Separating every quote, regardless of length (35 words or more should be in a separate paragraph), without integrating them into the paragraph for a seamless reading experience.
Choosing Quotes
Managing word count limitations, avoiding discussion pitfalls and the generalizability trap.
- Carminati L.
Conclusions
Ce posttest, instructions, provider accreditation.
- a. Local and national governmental oversight through health professions regulation is needed for professional practice.
- b. Health professions are regulated in order to avoid a risk of harm to the public.
- c. Congress mandates that all professions are regulated.
- d. Both a and b
- a. There are not enough studies to determine the effectiveness of qualitative research yet.
- b. Quantitative research is more critical because it provides both exploratory and explanatory data.
- c. Qualitative research can play a vital role in ensuring that the stakeholder’s voice is represented and their experiences inform the evaluation of regulations and their associated policies.
- d. None of the above
- a. Identification, modification, or abolition
- b. Creation, modification, or elimination
- c. Oversight, enforcement, or evaluation
- d. Creation, development, or destruction
- c. Data saturation
- d. Reliability
- a. Data saturation
- b. Trustworthiness
- a. Termination
- b. Content closure
- c. Conclusion
- d. Data saturation
- a. Rigorous
- b. Trustworthy
- c. Unbiased
- d. Credible
- a. Grounded theory
- b. Phenomenology
- c. Ethnography
- d. Generic qualitative descriptive
- a. The applicability of the results is immediately apparent and translatable into the real world.
- b. The end goal of the study is to generate a theory from the data.
- c. The study must describe the lived experience of a phenomenon.
- d. Generic approaches offer flexibility for studying regulation and regulatory issues.
- 12. Pragmatic qualitative studies _____
- 13. Case studies _____
- 14. Realist evaluations _____
- a. Might work well exploring a state level analysis of a regulatory change
- b. A way to compare contemporary and historical stakeholder perspectives around the legislative process or similar phenomena
- c. Might be useful for studying how new regulations have affected those subject to them during the early phases of implementation
- d. Contributes to the evidence to support or change a regulation
- a. Recruit a sample size that will achieve data saturation.
- b. Aim for a heterogeneous sample.
- c. Plan to achieve a minimum sample size of 8 as a realistic and achievable goal in most cases.
- d. Sample size has no impact on regulatory research.
- a. Long quote
- b. Strong opening sentence
- d. Phenomenon
- a. Representative of participants’ experiences
- b. Improve the trustworthiness of results
- c. Articulately or succinctly explain a phenomenon
- d. All of the above
- a. The discussion section may end up too “thin” because the authors have left no room in the word count for a robust discussion of the findings
- b. The discussion section uses the first paragraph to summarize the findings from the study and how they are unique from the literature
- c. The authors assume the findings are generalizable to the broader population.
- a. They should include all findings, even if the content does not tie back to the original research question.
- b. They can provide useful direction for others seeking to replicate the study in different contexts or with populations affected by the same regulations.
- c. Suggestions for realistic, existing, measurable variables that might be sensitive to the effects of a regulation cannot be useful for a qualitative study focused on regulation.
- d. Qualitative findings can always be applied to other regional, state, national, or international populations.
Evaluation Form (required)
- • Explain the importance of qualitative research for studies about regulatory issues in nursing. 1 2 3 4 5 ___________________________________
- • Discuss the core concepts of qualitative research. 1 2 3 4 5 ___________________________________
- • Describe common methodological challenges researchers can encounter when conducting qualitative research on professional regulatory issues. 1 2 3 4 5 ___________________________________
- • Identify solutions that can enhance the quality, rigor, and trustworthiness of the findings for regulatory studies. 1 2 3 4 5 ___________________________________
- • Were the authors knowledgeable about the subject? 1 2 3 4 5 ___________________________________
- • Were the methods of presentation (text, tables, figures, etc.) effective? 1 2 3 4 5 ___________________________________
- • Was the content relevant to the objectives? 1 2 3 4 5 ___________________________________
- • Was the article useful to you in your work? 1 2 3 4 5 ___________________________________
- • Was there enough time allotted for this activity? 1 2 3 4 5 ___________________________________
- Krefting L.
- Scopus (1932)
Article info
Identification.
DOI: https://doi.org/10.1016/S2155-8256(18)30150-9
ScienceDirect
- View Large Image
- Download Hi-res image
- Download .PPT
Linked Article
- Preview As is standard in scholarly publishing, NCSBN’s Journal of Nursing Regulation (JNR) requires its authors to disclose any potential conflicts of interest (COI). Although COI information has always been collected by our staff in order to support editors’ review of the paper, it was not our standard practice to publish COI statements in each article. In this issue, JNR is retrospectively publishing the COI statements, which were collected with the below papers at submission, in order to make potential COI’s transparent to readers, as well as editors.
Related Articles
- Access for Developing Countries
- Articles & Issues
- Current Issue
- List of Issues
- Supplements
- For Authors
- Guide for Authors
- Author Services
- Permissions
- Researcher Academy
- Submit a Manuscript
- Journal Info
- About the Journal
- Contact Information
- Editorial Board
- New Content Alerts
- Call for Papers
- January & April 2022 Issues
The content on this site is intended for healthcare professionals.
- Privacy Policy
- Terms and Conditions
- Accessibility
- Help & Contact


File(s) under embargo
until file(s) become available
Qualitative Insights on Diverse Impacts of Interprofessional Relationships in Nursing Homes
Degree grantor, degree level, degree name, committee member, thesis type, usage metrics.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Korean Med Sci
- v.37(16); 2022 Apr 25

A Practical Guide to Writing Quantitative and Qualitative Research Questions and Hypotheses in Scholarly Articles
Edward barroga.
1 Department of General Education, Graduate School of Nursing Science, St. Luke’s International University, Tokyo, Japan.
Glafera Janet Matanguihan
2 Department of Biological Sciences, Messiah University, Mechanicsburg, PA, USA.
The development of research questions and the subsequent hypotheses are prerequisites to defining the main research purpose and specific objectives of a study. Consequently, these objectives determine the study design and research outcome. The development of research questions is a process based on knowledge of current trends, cutting-edge studies, and technological advances in the research field. Excellent research questions are focused and require a comprehensive literature search and in-depth understanding of the problem being investigated. Initially, research questions may be written as descriptive questions which could be developed into inferential questions. These questions must be specific and concise to provide a clear foundation for developing hypotheses. Hypotheses are more formal predictions about the research outcomes. These specify the possible results that may or may not be expected regarding the relationship between groups. Thus, research questions and hypotheses clarify the main purpose and specific objectives of the study, which in turn dictate the design of the study, its direction, and outcome. Studies developed from good research questions and hypotheses will have trustworthy outcomes with wide-ranging social and health implications.
INTRODUCTION
Scientific research is usually initiated by posing evidenced-based research questions which are then explicitly restated as hypotheses. 1 , 2 The hypotheses provide directions to guide the study, solutions, explanations, and expected results. 3 , 4 Both research questions and hypotheses are essentially formulated based on conventional theories and real-world processes, which allow the inception of novel studies and the ethical testing of ideas. 5 , 6
It is crucial to have knowledge of both quantitative and qualitative research 2 as both types of research involve writing research questions and hypotheses. 7 However, these crucial elements of research are sometimes overlooked; if not overlooked, then framed without the forethought and meticulous attention it needs. Planning and careful consideration are needed when developing quantitative or qualitative research, particularly when conceptualizing research questions and hypotheses. 4
There is a continuing need to support researchers in the creation of innovative research questions and hypotheses, as well as for journal articles that carefully review these elements. 1 When research questions and hypotheses are not carefully thought of, unethical studies and poor outcomes usually ensue. Carefully formulated research questions and hypotheses define well-founded objectives, which in turn determine the appropriate design, course, and outcome of the study. This article then aims to discuss in detail the various aspects of crafting research questions and hypotheses, with the goal of guiding researchers as they develop their own. Examples from the authors and peer-reviewed scientific articles in the healthcare field are provided to illustrate key points.
DEFINITIONS AND RELATIONSHIP OF RESEARCH QUESTIONS AND HYPOTHESES
A research question is what a study aims to answer after data analysis and interpretation. The answer is written in length in the discussion section of the paper. Thus, the research question gives a preview of the different parts and variables of the study meant to address the problem posed in the research question. 1 An excellent research question clarifies the research writing while facilitating understanding of the research topic, objective, scope, and limitations of the study. 5
On the other hand, a research hypothesis is an educated statement of an expected outcome. This statement is based on background research and current knowledge. 8 , 9 The research hypothesis makes a specific prediction about a new phenomenon 10 or a formal statement on the expected relationship between an independent variable and a dependent variable. 3 , 11 It provides a tentative answer to the research question to be tested or explored. 4
Hypotheses employ reasoning to predict a theory-based outcome. 10 These can also be developed from theories by focusing on components of theories that have not yet been observed. 10 The validity of hypotheses is often based on the testability of the prediction made in a reproducible experiment. 8
Conversely, hypotheses can also be rephrased as research questions. Several hypotheses based on existing theories and knowledge may be needed to answer a research question. Developing ethical research questions and hypotheses creates a research design that has logical relationships among variables. These relationships serve as a solid foundation for the conduct of the study. 4 , 11 Haphazardly constructed research questions can result in poorly formulated hypotheses and improper study designs, leading to unreliable results. Thus, the formulations of relevant research questions and verifiable hypotheses are crucial when beginning research. 12
CHARACTERISTICS OF GOOD RESEARCH QUESTIONS AND HYPOTHESES
Excellent research questions are specific and focused. These integrate collective data and observations to confirm or refute the subsequent hypotheses. Well-constructed hypotheses are based on previous reports and verify the research context. These are realistic, in-depth, sufficiently complex, and reproducible. More importantly, these hypotheses can be addressed and tested. 13
There are several characteristics of well-developed hypotheses. Good hypotheses are 1) empirically testable 7 , 10 , 11 , 13 ; 2) backed by preliminary evidence 9 ; 3) testable by ethical research 7 , 9 ; 4) based on original ideas 9 ; 5) have evidenced-based logical reasoning 10 ; and 6) can be predicted. 11 Good hypotheses can infer ethical and positive implications, indicating the presence of a relationship or effect relevant to the research theme. 7 , 11 These are initially developed from a general theory and branch into specific hypotheses by deductive reasoning. In the absence of a theory to base the hypotheses, inductive reasoning based on specific observations or findings form more general hypotheses. 10
TYPES OF RESEARCH QUESTIONS AND HYPOTHESES
Research questions and hypotheses are developed according to the type of research, which can be broadly classified into quantitative and qualitative research. We provide a summary of the types of research questions and hypotheses under quantitative and qualitative research categories in Table 1 .
Research questions in quantitative research
In quantitative research, research questions inquire about the relationships among variables being investigated and are usually framed at the start of the study. These are precise and typically linked to the subject population, dependent and independent variables, and research design. 1 Research questions may also attempt to describe the behavior of a population in relation to one or more variables, or describe the characteristics of variables to be measured ( descriptive research questions ). 1 , 5 , 14 These questions may also aim to discover differences between groups within the context of an outcome variable ( comparative research questions ), 1 , 5 , 14 or elucidate trends and interactions among variables ( relationship research questions ). 1 , 5 We provide examples of descriptive, comparative, and relationship research questions in quantitative research in Table 2 .
Hypotheses in quantitative research
In quantitative research, hypotheses predict the expected relationships among variables. 15 Relationships among variables that can be predicted include 1) between a single dependent variable and a single independent variable ( simple hypothesis ) or 2) between two or more independent and dependent variables ( complex hypothesis ). 4 , 11 Hypotheses may also specify the expected direction to be followed and imply an intellectual commitment to a particular outcome ( directional hypothesis ) 4 . On the other hand, hypotheses may not predict the exact direction and are used in the absence of a theory, or when findings contradict previous studies ( non-directional hypothesis ). 4 In addition, hypotheses can 1) define interdependency between variables ( associative hypothesis ), 4 2) propose an effect on the dependent variable from manipulation of the independent variable ( causal hypothesis ), 4 3) state a negative relationship between two variables ( null hypothesis ), 4 , 11 , 15 4) replace the working hypothesis if rejected ( alternative hypothesis ), 15 explain the relationship of phenomena to possibly generate a theory ( working hypothesis ), 11 5) involve quantifiable variables that can be tested statistically ( statistical hypothesis ), 11 6) or express a relationship whose interlinks can be verified logically ( logical hypothesis ). 11 We provide examples of simple, complex, directional, non-directional, associative, causal, null, alternative, working, statistical, and logical hypotheses in quantitative research, as well as the definition of quantitative hypothesis-testing research in Table 3 .
Research questions in qualitative research
Unlike research questions in quantitative research, research questions in qualitative research are usually continuously reviewed and reformulated. The central question and associated subquestions are stated more than the hypotheses. 15 The central question broadly explores a complex set of factors surrounding the central phenomenon, aiming to present the varied perspectives of participants. 15
There are varied goals for which qualitative research questions are developed. These questions can function in several ways, such as to 1) identify and describe existing conditions ( contextual research question s); 2) describe a phenomenon ( descriptive research questions ); 3) assess the effectiveness of existing methods, protocols, theories, or procedures ( evaluation research questions ); 4) examine a phenomenon or analyze the reasons or relationships between subjects or phenomena ( explanatory research questions ); or 5) focus on unknown aspects of a particular topic ( exploratory research questions ). 5 In addition, some qualitative research questions provide new ideas for the development of theories and actions ( generative research questions ) or advance specific ideologies of a position ( ideological research questions ). 1 Other qualitative research questions may build on a body of existing literature and become working guidelines ( ethnographic research questions ). Research questions may also be broadly stated without specific reference to the existing literature or a typology of questions ( phenomenological research questions ), may be directed towards generating a theory of some process ( grounded theory questions ), or may address a description of the case and the emerging themes ( qualitative case study questions ). 15 We provide examples of contextual, descriptive, evaluation, explanatory, exploratory, generative, ideological, ethnographic, phenomenological, grounded theory, and qualitative case study research questions in qualitative research in Table 4 , and the definition of qualitative hypothesis-generating research in Table 5 .
Qualitative studies usually pose at least one central research question and several subquestions starting with How or What . These research questions use exploratory verbs such as explore or describe . These also focus on one central phenomenon of interest, and may mention the participants and research site. 15
Hypotheses in qualitative research
Hypotheses in qualitative research are stated in the form of a clear statement concerning the problem to be investigated. Unlike in quantitative research where hypotheses are usually developed to be tested, qualitative research can lead to both hypothesis-testing and hypothesis-generating outcomes. 2 When studies require both quantitative and qualitative research questions, this suggests an integrative process between both research methods wherein a single mixed-methods research question can be developed. 1
FRAMEWORKS FOR DEVELOPING RESEARCH QUESTIONS AND HYPOTHESES
Research questions followed by hypotheses should be developed before the start of the study. 1 , 12 , 14 It is crucial to develop feasible research questions on a topic that is interesting to both the researcher and the scientific community. This can be achieved by a meticulous review of previous and current studies to establish a novel topic. Specific areas are subsequently focused on to generate ethical research questions. The relevance of the research questions is evaluated in terms of clarity of the resulting data, specificity of the methodology, objectivity of the outcome, depth of the research, and impact of the study. 1 , 5 These aspects constitute the FINER criteria (i.e., Feasible, Interesting, Novel, Ethical, and Relevant). 1 Clarity and effectiveness are achieved if research questions meet the FINER criteria. In addition to the FINER criteria, Ratan et al. described focus, complexity, novelty, feasibility, and measurability for evaluating the effectiveness of research questions. 14
The PICOT and PEO frameworks are also used when developing research questions. 1 The following elements are addressed in these frameworks, PICOT: P-population/patients/problem, I-intervention or indicator being studied, C-comparison group, O-outcome of interest, and T-timeframe of the study; PEO: P-population being studied, E-exposure to preexisting conditions, and O-outcome of interest. 1 Research questions are also considered good if these meet the “FINERMAPS” framework: Feasible, Interesting, Novel, Ethical, Relevant, Manageable, Appropriate, Potential value/publishable, and Systematic. 14
As we indicated earlier, research questions and hypotheses that are not carefully formulated result in unethical studies or poor outcomes. To illustrate this, we provide some examples of ambiguous research question and hypotheses that result in unclear and weak research objectives in quantitative research ( Table 6 ) 16 and qualitative research ( Table 7 ) 17 , and how to transform these ambiguous research question(s) and hypothesis(es) into clear and good statements.
a These statements were composed for comparison and illustrative purposes only.
b These statements are direct quotes from Higashihara and Horiuchi. 16
a This statement is a direct quote from Shimoda et al. 17
The other statements were composed for comparison and illustrative purposes only.
CONSTRUCTING RESEARCH QUESTIONS AND HYPOTHESES
To construct effective research questions and hypotheses, it is very important to 1) clarify the background and 2) identify the research problem at the outset of the research, within a specific timeframe. 9 Then, 3) review or conduct preliminary research to collect all available knowledge about the possible research questions by studying theories and previous studies. 18 Afterwards, 4) construct research questions to investigate the research problem. Identify variables to be accessed from the research questions 4 and make operational definitions of constructs from the research problem and questions. Thereafter, 5) construct specific deductive or inductive predictions in the form of hypotheses. 4 Finally, 6) state the study aims . This general flow for constructing effective research questions and hypotheses prior to conducting research is shown in Fig. 1 .

Research questions are used more frequently in qualitative research than objectives or hypotheses. 3 These questions seek to discover, understand, explore or describe experiences by asking “What” or “How.” The questions are open-ended to elicit a description rather than to relate variables or compare groups. The questions are continually reviewed, reformulated, and changed during the qualitative study. 3 Research questions are also used more frequently in survey projects than hypotheses in experiments in quantitative research to compare variables and their relationships.
Hypotheses are constructed based on the variables identified and as an if-then statement, following the template, ‘If a specific action is taken, then a certain outcome is expected.’ At this stage, some ideas regarding expectations from the research to be conducted must be drawn. 18 Then, the variables to be manipulated (independent) and influenced (dependent) are defined. 4 Thereafter, the hypothesis is stated and refined, and reproducible data tailored to the hypothesis are identified, collected, and analyzed. 4 The hypotheses must be testable and specific, 18 and should describe the variables and their relationships, the specific group being studied, and the predicted research outcome. 18 Hypotheses construction involves a testable proposition to be deduced from theory, and independent and dependent variables to be separated and measured separately. 3 Therefore, good hypotheses must be based on good research questions constructed at the start of a study or trial. 12
In summary, research questions are constructed after establishing the background of the study. Hypotheses are then developed based on the research questions. Thus, it is crucial to have excellent research questions to generate superior hypotheses. In turn, these would determine the research objectives and the design of the study, and ultimately, the outcome of the research. 12 Algorithms for building research questions and hypotheses are shown in Fig. 2 for quantitative research and in Fig. 3 for qualitative research.

EXAMPLES OF RESEARCH QUESTIONS FROM PUBLISHED ARTICLES
- EXAMPLE 1. Descriptive research question (quantitative research)
- - Presents research variables to be assessed (distinct phenotypes and subphenotypes)
- “BACKGROUND: Since COVID-19 was identified, its clinical and biological heterogeneity has been recognized. Identifying COVID-19 phenotypes might help guide basic, clinical, and translational research efforts.
- RESEARCH QUESTION: Does the clinical spectrum of patients with COVID-19 contain distinct phenotypes and subphenotypes? ” 19
- EXAMPLE 2. Relationship research question (quantitative research)
- - Shows interactions between dependent variable (static postural control) and independent variable (peripheral visual field loss)
- “Background: Integration of visual, vestibular, and proprioceptive sensations contributes to postural control. People with peripheral visual field loss have serious postural instability. However, the directional specificity of postural stability and sensory reweighting caused by gradual peripheral visual field loss remain unclear.
- Research question: What are the effects of peripheral visual field loss on static postural control ?” 20
- EXAMPLE 3. Comparative research question (quantitative research)
- - Clarifies the difference among groups with an outcome variable (patients enrolled in COMPERA with moderate PH or severe PH in COPD) and another group without the outcome variable (patients with idiopathic pulmonary arterial hypertension (IPAH))
- “BACKGROUND: Pulmonary hypertension (PH) in COPD is a poorly investigated clinical condition.
- RESEARCH QUESTION: Which factors determine the outcome of PH in COPD?
- STUDY DESIGN AND METHODS: We analyzed the characteristics and outcome of patients enrolled in the Comparative, Prospective Registry of Newly Initiated Therapies for Pulmonary Hypertension (COMPERA) with moderate or severe PH in COPD as defined during the 6th PH World Symposium who received medical therapy for PH and compared them with patients with idiopathic pulmonary arterial hypertension (IPAH) .” 21
- EXAMPLE 4. Exploratory research question (qualitative research)
- - Explores areas that have not been fully investigated (perspectives of families and children who receive care in clinic-based child obesity treatment) to have a deeper understanding of the research problem
- “Problem: Interventions for children with obesity lead to only modest improvements in BMI and long-term outcomes, and data are limited on the perspectives of families of children with obesity in clinic-based treatment. This scoping review seeks to answer the question: What is known about the perspectives of families and children who receive care in clinic-based child obesity treatment? This review aims to explore the scope of perspectives reported by families of children with obesity who have received individualized outpatient clinic-based obesity treatment.” 22
- EXAMPLE 5. Relationship research question (quantitative research)
- - Defines interactions between dependent variable (use of ankle strategies) and independent variable (changes in muscle tone)
- “Background: To maintain an upright standing posture against external disturbances, the human body mainly employs two types of postural control strategies: “ankle strategy” and “hip strategy.” While it has been reported that the magnitude of the disturbance alters the use of postural control strategies, it has not been elucidated how the level of muscle tone, one of the crucial parameters of bodily function, determines the use of each strategy. We have previously confirmed using forward dynamics simulations of human musculoskeletal models that an increased muscle tone promotes the use of ankle strategies. The objective of the present study was to experimentally evaluate a hypothesis: an increased muscle tone promotes the use of ankle strategies. Research question: Do changes in the muscle tone affect the use of ankle strategies ?” 23
EXAMPLES OF HYPOTHESES IN PUBLISHED ARTICLES
- EXAMPLE 1. Working hypothesis (quantitative research)
- - A hypothesis that is initially accepted for further research to produce a feasible theory
- “As fever may have benefit in shortening the duration of viral illness, it is plausible to hypothesize that the antipyretic efficacy of ibuprofen may be hindering the benefits of a fever response when taken during the early stages of COVID-19 illness .” 24
- “In conclusion, it is plausible to hypothesize that the antipyretic efficacy of ibuprofen may be hindering the benefits of a fever response . The difference in perceived safety of these agents in COVID-19 illness could be related to the more potent efficacy to reduce fever with ibuprofen compared to acetaminophen. Compelling data on the benefit of fever warrant further research and review to determine when to treat or withhold ibuprofen for early stage fever for COVID-19 and other related viral illnesses .” 24
- EXAMPLE 2. Exploratory hypothesis (qualitative research)
- - Explores particular areas deeper to clarify subjective experience and develop a formal hypothesis potentially testable in a future quantitative approach
- “We hypothesized that when thinking about a past experience of help-seeking, a self distancing prompt would cause increased help-seeking intentions and more favorable help-seeking outcome expectations .” 25
- “Conclusion
- Although a priori hypotheses were not supported, further research is warranted as results indicate the potential for using self-distancing approaches to increasing help-seeking among some people with depressive symptomatology.” 25
- EXAMPLE 3. Hypothesis-generating research to establish a framework for hypothesis testing (qualitative research)
- “We hypothesize that compassionate care is beneficial for patients (better outcomes), healthcare systems and payers (lower costs), and healthcare providers (lower burnout). ” 26
- Compassionomics is the branch of knowledge and scientific study of the effects of compassionate healthcare. Our main hypotheses are that compassionate healthcare is beneficial for (1) patients, by improving clinical outcomes, (2) healthcare systems and payers, by supporting financial sustainability, and (3) HCPs, by lowering burnout and promoting resilience and well-being. The purpose of this paper is to establish a scientific framework for testing the hypotheses above . If these hypotheses are confirmed through rigorous research, compassionomics will belong in the science of evidence-based medicine, with major implications for all healthcare domains.” 26
- EXAMPLE 4. Statistical hypothesis (quantitative research)
- - An assumption is made about the relationship among several population characteristics ( gender differences in sociodemographic and clinical characteristics of adults with ADHD ). Validity is tested by statistical experiment or analysis ( chi-square test, Students t-test, and logistic regression analysis)
- “Our research investigated gender differences in sociodemographic and clinical characteristics of adults with ADHD in a Japanese clinical sample. Due to unique Japanese cultural ideals and expectations of women's behavior that are in opposition to ADHD symptoms, we hypothesized that women with ADHD experience more difficulties and present more dysfunctions than men . We tested the following hypotheses: first, women with ADHD have more comorbidities than men with ADHD; second, women with ADHD experience more social hardships than men, such as having less full-time employment and being more likely to be divorced.” 27
- “Statistical Analysis
- ( text omitted ) Between-gender comparisons were made using the chi-squared test for categorical variables and Students t-test for continuous variables…( text omitted ). A logistic regression analysis was performed for employment status, marital status, and comorbidity to evaluate the independent effects of gender on these dependent variables.” 27
EXAMPLES OF HYPOTHESIS AS WRITTEN IN PUBLISHED ARTICLES IN RELATION TO OTHER PARTS
- EXAMPLE 1. Background, hypotheses, and aims are provided
- “Pregnant women need skilled care during pregnancy and childbirth, but that skilled care is often delayed in some countries …( text omitted ). The focused antenatal care (FANC) model of WHO recommends that nurses provide information or counseling to all pregnant women …( text omitted ). Job aids are visual support materials that provide the right kind of information using graphics and words in a simple and yet effective manner. When nurses are not highly trained or have many work details to attend to, these job aids can serve as a content reminder for the nurses and can be used for educating their patients (Jennings, Yebadokpo, Affo, & Agbogbe, 2010) ( text omitted ). Importantly, additional evidence is needed to confirm how job aids can further improve the quality of ANC counseling by health workers in maternal care …( text omitted )” 28
- “ This has led us to hypothesize that the quality of ANC counseling would be better if supported by job aids. Consequently, a better quality of ANC counseling is expected to produce higher levels of awareness concerning the danger signs of pregnancy and a more favorable impression of the caring behavior of nurses .” 28
- “This study aimed to examine the differences in the responses of pregnant women to a job aid-supported intervention during ANC visit in terms of 1) their understanding of the danger signs of pregnancy and 2) their impression of the caring behaviors of nurses to pregnant women in rural Tanzania.” 28
- EXAMPLE 2. Background, hypotheses, and aims are provided
- “We conducted a two-arm randomized controlled trial (RCT) to evaluate and compare changes in salivary cortisol and oxytocin levels of first-time pregnant women between experimental and control groups. The women in the experimental group touched and held an infant for 30 min (experimental intervention protocol), whereas those in the control group watched a DVD movie of an infant (control intervention protocol). The primary outcome was salivary cortisol level and the secondary outcome was salivary oxytocin level.” 29
- “ We hypothesize that at 30 min after touching and holding an infant, the salivary cortisol level will significantly decrease and the salivary oxytocin level will increase in the experimental group compared with the control group .” 29
- EXAMPLE 3. Background, aim, and hypothesis are provided
- “In countries where the maternal mortality ratio remains high, antenatal education to increase Birth Preparedness and Complication Readiness (BPCR) is considered one of the top priorities [1]. BPCR includes birth plans during the antenatal period, such as the birthplace, birth attendant, transportation, health facility for complications, expenses, and birth materials, as well as family coordination to achieve such birth plans. In Tanzania, although increasing, only about half of all pregnant women attend an antenatal clinic more than four times [4]. Moreover, the information provided during antenatal care (ANC) is insufficient. In the resource-poor settings, antenatal group education is a potential approach because of the limited time for individual counseling at antenatal clinics.” 30
- “This study aimed to evaluate an antenatal group education program among pregnant women and their families with respect to birth-preparedness and maternal and infant outcomes in rural villages of Tanzania.” 30
- “ The study hypothesis was if Tanzanian pregnant women and their families received a family-oriented antenatal group education, they would (1) have a higher level of BPCR, (2) attend antenatal clinic four or more times, (3) give birth in a health facility, (4) have less complications of women at birth, and (5) have less complications and deaths of infants than those who did not receive the education .” 30
Research questions and hypotheses are crucial components to any type of research, whether quantitative or qualitative. These questions should be developed at the very beginning of the study. Excellent research questions lead to superior hypotheses, which, like a compass, set the direction of research, and can often determine the successful conduct of the study. Many research studies have floundered because the development of research questions and subsequent hypotheses was not given the thought and meticulous attention needed. The development of research questions and hypotheses is an iterative process based on extensive knowledge of the literature and insightful grasp of the knowledge gap. Focused, concise, and specific research questions provide a strong foundation for constructing hypotheses which serve as formal predictions about the research outcomes. Research questions and hypotheses are crucial elements of research that should not be overlooked. They should be carefully thought of and constructed when planning research. This avoids unethical studies and poor outcomes by defining well-founded objectives that determine the design, course, and outcome of the study.
Disclosure: The authors have no potential conflicts of interest to disclose.
Author Contributions:
- Conceptualization: Barroga E, Matanguihan GJ.
- Methodology: Barroga E, Matanguihan GJ.
- Writing - original draft: Barroga E, Matanguihan GJ.
- Writing - review & editing: Barroga E, Matanguihan GJ.

IMAGES
VIDEO
COMMENTS
1.1. Background. Research indicates that there is a potential for patients to improve safety (Davis, Jacklin, Sevdalis, & Vincent, 2007; Vincent & Coulter, 2002) and that patients are willing and able to be involved in safety‐related work (Waterman et al., 2006 Wright et al., 2016).However, several barriers to involving patients in improving patient safety has been identified and organized ...
Data analysis. Data collection and inductive thematic analysis took place iteratively [45, 53].The first author coded the data (i.e. observation reports, interview and focus group transcripts), basing the codes on the research question and theoretical notions on nursing role development and distinctions.
Global Qualitative Nursing Research (GQNR) is an open access, peer-reviewed journal focusing on qualitative research in fields relevant to nursing and other health professionals world-wide. Please see the Aims and Scope tab for … | View full journal description. This journal is a member of the Committee on Publication Ethics (COPE).
Nursing interventions can be evaluated qualitatively, as this method enhances the significance of clinical trials and emphasizes the distinctive work and outcomes of nursing care (Sandelowski, 1996 ). However, there are few examples of detailed methodological strategies for doing so (Schumacher et al., 2005 ).
Attempts to shape nursing work have lacked understanding of how nurses contribute to healthcare, with negative consequences. For example, the recent introduction of Nursing Associate roles (Department of Health and Social Care, 2017) in the UK, ostensibly to be a compassionate, patient-facing role and reduce costs, overlooks evidence that replacing registered nurses with other providers leads ...
Healthcare research is a systematic inquiry intended to generate trustworthy evidence about issues in the field of medicine and healthcare. The three principal approaches to health research are the quantitative, the qualitative, and the mixed methods approach. The quantitative research method uses data, which are measures of values and counts ...
Takeaways: Qualitative research is valuable because it approaches a phenomenon, such as a clinical problem, about which little is known by trying to understand its many facets. Most qualitative research is emergent, holistic, detailed, and uses many strategies to collect data. Qualitative research generates evidence and helps nurses determine ...
Abstract This qualitative study aimed to gain an understanding of what it means to live with ischemic heart disease for individuals who perceive health as ... Nursing & Health Sciences ... RESEARCH ARTICLE. The self-management experiences of individuals who perceive health as beyond their control: An interpretive phenomenological study of ...
Global Qualitative Nursing Research (GQNR) is a ground breaking, international, peer-reviewed, open-access journal focusing on qualitative research in fields relevant to nursing world-wide. The journal specializes in topics related to nursing practice, responses to health, illness, and disability, health promotion, healthcare delivery, and global issues that affect nursing and healthcare.
Qualitative research is critical for studies about regulatory issues in nursing and across all health professions. When in-depth stakeholder perspectives are needed, qualitative approaches are often the best methodological choice to ensure their viewpoints and experiences are captured when evaluating the consequences of policy implementation or when informing regulation design.
Therefore, this article aims to address considerations in qualitative research by discussing the purposes of nursing research, exploring basic qualitative approaches, and analyzing ethical principles and trustworthiness specific to qualitative inquiry. 2 PURPOSES OF NURSING RESEARCH. Research is a way to discover information.
Useful terms. Some of the qualitative approaches used in nursing research include grounded theory, phenomenology, ethnography, case study (can lend itself to mixed methods) and narrative analysis. The data collection methods used in qualitative research include in depth interviews, focus groups, observations and stories in the form of diaries ...
Graneheim UH, Lundman B: Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Education Today. 2004, 24: 105-112. 10.1016/j.nedt.2003.10.001. Article CAS PubMed Google Scholar Streubert HJ, Carpenter DR: Qualitative Research in Nursing.
Good qualitative research uses a systematic and rigorous approach that aims to answer questions concerned with what something is like (such as a patient experience), what people think or feel about something that has happened, and it may address why something has happened as it has. Qualitative data often takes the form of words or text and can include images. Qualitative research covers a ...
Introduction. In light of the increasingly complex healthcare setting and system, the collaboration of diverse health professionals has been shown to provide high-quality patient care and maintain healthcare service provision [Citation 1].Interprofessional education (IPE) has emerged as a key component in training future healthcare professionals, emphasizing effective collaboration for patient ...
Qualitative descriptive designs are common in nursing and healthcare research due to their inherent simplicity, flexibility and utility in diverse healthcare contexts. However, the application of descriptive research is sometimes critiqued in terms of scientific rigor. Inconsistency in decision making within the research process coupled with a ...
Qualitative research methods began to appear in nursing in 1960s and 1970s amid cautious and reluctant acceptance. In the 1980s, qualitative health research emerged as a distinctive domain and mode of inquiry. 1 Qualitative research refers to any kind of research that produces findings not arrived at by means of statistical analysis or other means of quantification. 2,3 It uses a naturalistic ...
She is the director of Doctoral of Nursing Science Program. She received her PhD (Nursing) from University of California, San Francisco, USA in 2000. Her area of interest is women's health and quality of maternal and intrapaum care. She has experience in teaching and conducting qualitative research.
Abstract. This paper aims to provide an overview of the use and assessment of qualitative research methods in the health sciences. Qualitative research can be defined as the study of the nature of phenomena and is especially appropriate for answering questions of why something is (not) observed, assessing complex multi-component interventions ...
The first question is whether the related qualitative, quantitative, or mixed-methods study has clear research questions or objectives. ... Journal of Research in Nursing. 2021;26(1-2):19-32. Cho SM, Choi J. Patient Safety Culture Associated with Patient Safety Competencies among registered nurses. J Nurs Scholarsh. 2018;50(5):549-57.
Choosing an appropriate qualitative methodology in nursing research is a researcher's first step before beginning a study. ... Global Challenge Innovations in Nursing Services and Education in the Future Single-Method Research Article. Breastfeeding a Premature Baby During the Covid-19 Pandemic in Perinatology: An Exploration of Mothers ...
As the use of qualitative research methods proliferates throughout health care, and specifically nursing research studies, there is a need for Clinical Nurse Specialists (CNSs) to become informed regarding the potential utility of qualitative research findings in practice. In this column, the questions of what qualitative findings mean, how the ...
Download Citation | On Mar 13, 2024, Preston H Miller and others published Critical care nurse leaders' moral distress: A qualitative descriptive study | Find, read and cite all the research you ...
Centre for Research and Training on Gender and Women's Health, Faculty of Nursing, Khon Kaen University, Khon Kaen, Thailand. Somporn Rungreangkulkij & Nilubon Rujiraprasert. Department of Family of Nursing and Midwifery, Faculty of Nursing, Thammasat University, Prathumthani, Thailand. Natthapat Buaboon
Qualitative research is critical for studies about regulatory issues in nursing and across all health professions. When in-depth stakeholder perspectives are needed, qualitative approaches are often the best methodological choice to ensure their viewpoints and experiences are captured when evaluating the consequences of policy implementation or when informing regulation design.
Background: Preventable nursing home (NH) resident hospitalization remains a critical public health issue. Studies found that improved interprofessional relationships may help reduce preventable resident hospitalizations, yet there is limited research on how different traits of relationships and communication may affect hospitalization decisions. Moreover, understanding perceived changes of ...
INTRODUCTION. Scientific research is usually initiated by posing evidenced-based research questions which are then explicitly restated as hypotheses.1,2 The hypotheses provide directions to guide the study, solutions, explanations, and expected results.3,4 Both research questions and hypotheses are essentially formulated based on conventional theories and real-world processes, which allow the ...
Medical research is either quantitative or qualitative. As a clinical research nurse, you may participate in both. Quantitative studies focus on results that can be empirically measured, such as statistics. Qualitative studies, like case studies, are more holistic and help you better understand a question or issue from all angles.
1. Open Access. Global Qualitative Nursing Research (GQNR) is an open access, international, peer reviewed journal focusing on qualitative research in field relevant to nursing. GQNR will publish qualitative methods research, qualitatively-driven mixed-method designs, as well as meta-syntheses and articles focused on methodological developments.
While many books and articles guide various qualitative research methods and analyses, there is currently no concise resource that explains and differentiates among the most common qualitative approaches. We believe novice qualitative researchers, students planning the design of a qualitative study or taking an introductory qualitative research course, and faculty teaching such courses can ...