- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board

Sonography: How a Sonogram Test Works and What It Shows
How to prepare for the test and how the results can help diagnose conditions
Before the Test
During the test, interpreting the results, frequently asked questions.
Sonography is a diagnostic medical test that uses high-frequency sound waves, or ultrasound waves, to create images of tissues, glands, organs, and blood or fluid flow within the body. This test is also referred to as an ultrasound or sonogram.
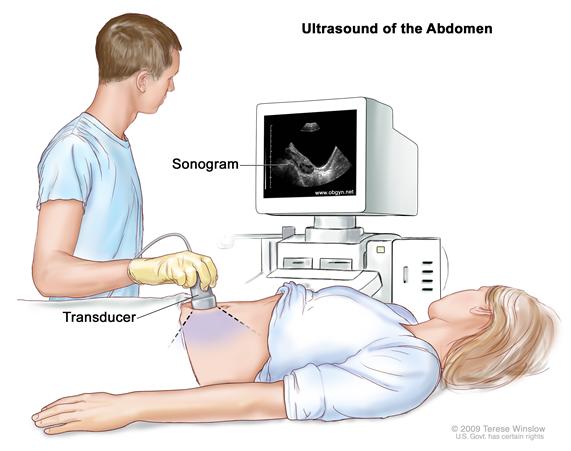
Sonography uses a device called a transducer on the surface of the skin to send ultrasound waves and listen for an echo. A computer translates the ultrasound waves into an image. A trained technician can see, measure, and identify structures in the image. A healthcare provider then reads the images to help diagnose the issue or problem at hand.
This article explains the purpose and limitations of sonography. To demystify the test, this article also explains what to expect before and during the test.
Verywell / Emily Roberts
Purpose of the Test
A sonogram captures a live image of what's going on inside the body. It functions like a camera that takes pictures of body parts or processes in real time.
Sonography is useful for evaluating the size, shape, and density of tissues to help diagnose certain medical conditions. Traditionally, ultrasound imaging is great for looking into the abdomen without having to cut it open.
Abdominal ultrasound is often used to diagnose:
- Gallbladder disease or gallstones
- Kidney stones or kidney disease
- Liver disease
- Appendicitis
- Ovarian cysts
- Ectopic pregnancy
- Uterine growths or fibroids and other conditions
A sonogram is most commonly used to monitor the development of the uterus and fetus during pregnancy. It can also be used to evaluate glands, breast lumps , joint conditions , bone disease , testicular lumps , or to guide needles during biopsies.
Sonography can also recognize blood or fluid flow that moves toward or away from the transducer. It uses color overlays on the image to show the direction of the flow. Very hard and dense tissues or empty spaces, such as organs filled with gas, do not conduct ultrasound waves and therefore cannot be viewed on a sonogram.
Physicians often order a sonogram before moving on to imaging technologies that have more potential for complications. Computerized tomography (CT) , for example, exposes you to significant levels of radiation.
Magnetic resonance imaging (MRI) uses an extremely strong magnet to capture an image. The strength of an MRI magnet can limit its use in patients with metal or devices in their bodies, such as some pacemakers .
What Is the Difference Between Ultrasound and Sonography?
Ultrasound and sonogram are slightly different terms used to refer to the same procedure. Ultrasound imaging, based on sound waves, describes the process itself. The sonogram is the image that an ultrasound generates.
Precautions and Risks
A sonogram is a noninvasive imaging test that has no known complications. Ultrasound waves are thought to be harmless.
While the energy of the ultrasound waves could potentially irritate or disrupt tissues with prolonged exposure, the computer modulates the power of the sound. Also, a trained technician uses techniques to minimize exposure times and angles, making sonography the safest of all imaging tests.
Healthcare providers order sonography as a first-line test, usually together with blood tests. Make sure you ask your provider if you should follow any special instructions before your sonogram.
In an emergency setting, sonography will typically be performed right away. For a test on a future date, find out if you should or should not eat or drink anything before the test. The answer may change depending on the purpose of the test.
For example, healthcare providers often ask patients to fast (not eat or drink) for six hours before an abdominal ultrasound to look at the gallbladder. But they may tell you to drink several glasses of water and not urinate before a sonogram of the bladder.
A sonogram usually doesn’t take longer than 30 minutes. In most cases, it’s important to arrive about 15 minutes before the test to fill out forms and possibly answer other questions. If the test requires that you drink fluids to fill your bladder, you might need to drink water before the test.
Once the technician acquires all the pictures, they will check with the radiologist (a healthcare provider trained to read images) to make sure no other views are required. Medical protocols call for the radiologist to interpret the images from a sonogram before sending a report to the healthcare provider. The provider then shares the results with the patient.
Sonography is done at most imaging centers, hospitals, and some obstetrics offices. The sonography machine looks a bit like a computer with a microphone attached—almost like a Karaoke machine. Usually, the sonography machine is rolled right up to the bedside.
What to Wear
Wear something comfortable and easy to remove to your sonogram appointment. In most cases, you will have to expose only the skin that the technician needs access to. An abdominal ultrasound, for example, can be done while you wear pants and a shirt. You'll just have to pull your shirt up and away to expose your abdomen.
In the case of a transvaginal sonogram, you'll have to undress below the waist, including removing underwear.
Cost and Health Insurance
Sonography is a relatively inexpensive imaging test. It is covered by most insurance policies and might require pre-authorization, depending on the reason the healthcare provider ordered it in the first place.
A 3D or 4D sonogram is an elective test that some expectant parents get during pregnancy. The 3D image shows a three-dimensional rendering of the baby; 4D refers to an animated video rendering of the baby in utero, captured over time. These are known as entertainment tests and are not covered by most health insurance policies.
Is a Sonogram Safe for a Baby When You're Pregnant?
The Food and Drug Administration says ultrasound imaging has an excellent safety record and does not pose the same risks as other imaging tests (like X-rays). It is considered safe for use during pregnancy, but imaging for non-medical purposes is discouraged by the American College of Obstetricians and Gynecologists (ACOG).
In many cases, a sonogram is over before you know it. Here's what you can expect:
Throughout the Test
A sonogram is conducted by a single technician right at the bedside. The technician will ask you to undress enough to expose the area where the test will be performed and to lie down on the bed.
The technician will coat the transducer with conductive gel, which feels like lubricant jelly. If possible, depending on the tools and supplies available, the gel will be warm. Then the technician will slide the transducer over the skin, sometimes with firm pressure. Occasionally, the pressure can cause mild discomfort.
Using the transducer to point to areas of interest, the technician will use the computer to capture images and might use a mouse to drag lines across the screen. The lines help measure size, like a virtual yardstick. You should be able to watch the entire procedure and even ask questions throughout the procedure.
When the sonogram is over, the technician will usually provide a towel to wipe off the conductive gel. Once the technician confirms that all the necessary images have been captured, you will be free to get dressed. There are no special instructions or side effects to manage.
It often takes a radiologist only a few minutes to interpret a sonogram. Typically, sonogram results are sent to the healthcare provider to share with a patient. So if you don't hear from your provider within the promised time frame, be sure to follow up.
If necessary, you can also request a copy of the radiologist's report and a disc containing the original images. For many expectant parents, this makes the entire trip worthwhile.
A sonogram is used to evaluate, diagnose, and treat a wide range of medical conditions, from lumps to kidney stones. Its most common usage, by far, is to check the development of a fetus and hear its heartbeat during pregnancy.
The live image that a sonogram captures is a painless procedure as well as a quick one. In many cases, a sonogram takes no more than 30 minutes from start to finish.
Follow your provider's instructions on whether you should eat or drink before the test, wear comfortable clothing, and the test will probably be over before you have a chance to fully relax.
A Word From Verywell
Sonography is one of the most noninvasive diagnostic medical tests available. It is a safe option for patients who need to know what is going on inside their bodies. If images are necessary, ask your healthcare provider if ultrasound is an option for you.
Most sonographers complete a two-year degree in an accredited sonography training program. Additionally, they may complete the American Registry for Diagnostic Medical Sonography (ARDMS) certification exams.
No. Radiology professionals use imaging that relies on radiation, while sonography is a technology based on sound waves. Sonographers use this ultrasound imagery, with the opportunity to specialize in specific areas like breast ultrasound or diagnostic cardiac ultrasound.
Tomizawa M, Shinozaki F, Hasegawa R, et al. Abdominal ultrasonography for patients with abdominal pain as a first-line diagnostic imaging modality . Exp Ther Med . 2017;13(5):1932-1936. doi:10.3892/etm.2017.4209.
American Pregnancy Association. Ultrasound: Sonogram .
U.S. Food and Drug Administration. Ultrasound imaging.
Whitson MR, Mayo PH. Ultrasonography in the emergency department. Critical Care . 2016;20:227. doi:10.1186/s13054-016-1399-x.
American College of Obstetricians and Gynecologists. Ultrasound in Pregnancy .
American Registry for Diagnostic Medical Sonography. How to Become a Sonographer .
Yeo, L. and Romero, R. (2016), Intelligent navigation to improve obstetrical sonography. Ultrasound Obstet Gynecol, 47: 403-409. doi:10.1002/uog.12562.
By Rod Brouhard, EMT-P Rod Brouhard is an emergency medical technician paramedic (EMT-P), journalist, educator, and advocate for emergency medical service providers and patients.
- Patient Care & Health Information
- Tests & Procedures
Diagnostic ultrasound, also called sonography or diagnostic medical sonography, is an imaging method that uses sound waves to produce images of structures within your body. The images can provide valuable information for diagnosing and directing treatment for a variety of diseases and conditions.
Most ultrasound examinations are done using an ultrasound device outside your body, though some involve placing a small device inside your body.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Assortment of Products for Daily Living from Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
Ultrasound is used for many reasons, including to:
- View the uterus and ovaries during pregnancy and monitor the developing baby's health
- Diagnose gallbladder disease
- Evaluate blood flow
- Guide a needle for biopsy or tumor treatment
- Examine a breast lump
- Check the thyroid gland
- Find genital and prostate problems
- Assess joint inflammation (synovitis)
- Evaluate metabolic bone disease
More Information
- Abdominal aortic aneurysm
- Acute kidney failure
- Acute liver failure
- Acute lymphocytic leukemia
- Adenomyosis
- Adult Still disease
- Alcoholic hepatitis
- Ambiguous genitalia
- Anal cancer
- Appendicitis
- Arteriosclerosis / atherosclerosis
- Arteriovenous fistula
- Atelectasis
- Autonomic neuropathy
- Bladder stones
- Blood in urine (hematuria)
- Breast cancer
- Breast pain
- Carotid artery disease
- Cerebral palsy
- Cholestasis of pregnancy
- Chronic exertional compartment syndrome
- Chronic kidney disease
- Cleft lip and cleft palate
- Congenital adrenal hyperplasia
- Conjoined twins
- Deep vein thrombosis (DVT)
- Double uterus
- Down syndrome
- Ductal carcinoma in situ (DCIS)
- Endometrial cancer
- Endometriosis
- Enlarged breasts in men (gynecomastia)
- Enlarged liver
- Epididymitis
- Erectile dysfunction
- Eye melanoma
- Fibroadenoma
- Fibrocystic breasts
- Galactorrhea
- Ganglion cyst
- Glomerulonephritis
- Growth plate fractures
- Hamstring injury
- High blood pressure in children
- Hurthle cell cancer
- Incompetent cervix
- Infant reflux
- Inflammatory breast cancer
- Intussusception
- Invasive lobular carcinoma
- Iron deficiency anemia
- Ischemic colitis
- Kidney cancer
- Knee bursitis
- Liver cancer
- Liver disease
- Liver hemangioma
- Male breast cancer
- Mammary duct ectasia
- Median arcuate ligament syndrome (MALS)
- Menstrual cramps
- Miscarriage
- Morning sickness
- Morton's neuroma
- Multisystem inflammatory syndrome in children (MIS-C)
- Muscle strains
- Muscular dystrophy
- Myelofibrosis
- Neuroblastoma
- Nonalcoholic fatty liver disease
- Osteoporosis
- Ovarian cancer
- Ovarian cysts
- Painful intercourse (dyspareunia)
- Pancreatic cancer
- Patellar tendinitis
- Pelvic inflammatory disease (PID)
- Peripheral artery disease (PAD)
- Peyronie disease
- Placenta previa
- Placental abruption
- Polycystic kidney disease
- Polymyalgia rheumatica
- Post-vasectomy pain syndrome
- Precocious puberty
- Premature birth
- Preterm labor
- Prostate cancer
- Pulmonary embolism
- Pyloric stenosis
- Recurrent breast cancer
- Residual limb pain
- Retinal detachment
- Retinoblastoma
- Rotator cuff injury
- Sacral dimple
- Sacroiliitis
- Scrotal masses
- Secondary hypertension
- Solitary rectal ulcer syndrome
- Spermatocele
- Spina bifida
- Swollen knee
- Takayasu's arteritis
- Tapeworm infection
- Testicular cancer
- Thrombophlebitis
- Thyroid cancer
- Thyroid nodules
- Torn meniscus
- Toxic hepatitis
- Toxoplasmosis
- Tricuspid atresia
- Tuberous sclerosis
- Uterine fibroids
- Uterine prolapse
- Wilms tumor
- Zollinger-Ellison syndrome
Diagnostic ultrasound is a safe procedure that uses low-power sound waves. There are no known risks.
Ultrasound is a valuable tool, but it has limitations. Sound waves don't travel well through air or bone, so ultrasound isn't effective at imaging body parts that have gas in them or are hidden by bone, such as the lungs or head. Ultrasound may also be unable to see objects that are located very deep in the human body. To view these areas, your health care provider may order other imaging tests, such as CT or MRI scans or X-rays.
How you prepare
Most ultrasound exams require no preparation. However, there are a few exceptions:
- For some scans, such as a gallbladder ultrasound, your care provider may ask that you not eat or drink for a certain period of time before the exam.
- Others, such as a pelvic ultrasound, may require a full bladder. Your doctor will let you know how much water you need to drink before the exam. Do not urinate until the exam is done.
- Young children may need additional preparation. When scheduling an ultrasound for yourself or your child, ask your doctor if there are any specific instructions you'll need to follow.
Clothing and personal items
Wear loose clothing to your ultrasound appointment. You may be asked to remove jewelry during your ultrasound, so it's a good idea to leave any valuables at home.
What you can expect
Before the procedure.
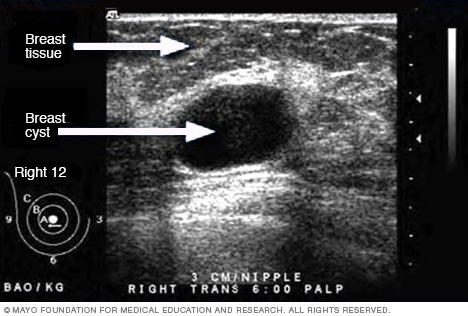
- Ultrasound of breast cyst
This ultrasound shows a breast cyst.
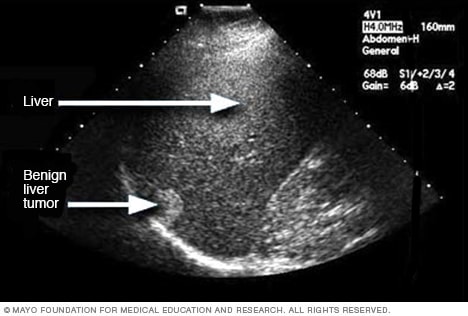
- Liver ultrasound
An ultrasound uses sound waves to make an image. This ultrasound shows a liver tumor that isn't cancer, called benign.

- Ultrasound of gallstones
This ultrasound shows gallstones in the gallbladder.
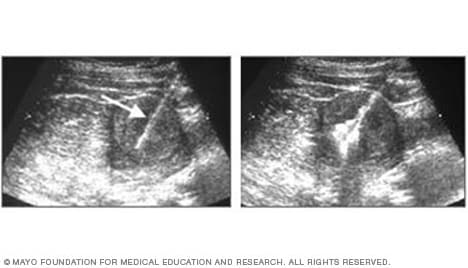
- Ultrasound of needle-guided procedure
These images show how ultrasound can help guide a needle into a tumor (left), where material is injected (right) to destroy tumor cells.
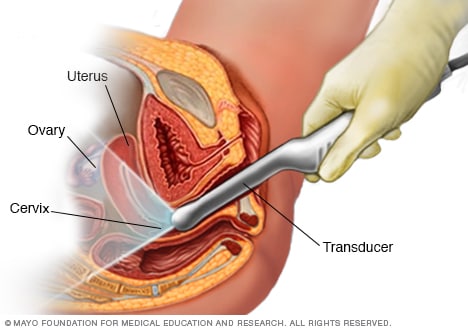
- Transvaginal ultrasound
During a transvaginal ultrasound, you lie on an exam table while a doctor or a medical technician puts a wandlike device, known as a transducer, into the vagina. Sound waves from the transducer create images of the uterus, ovaries and fallopian tubes.
Before your ultrasound begins, you may be asked to do the following:
- Remove any jewelry from the area being examined.
- Remove or reposition some or all of your clothing.
- Change into a gown.
You'll be asked to lie on an examination table.
During the procedure
Gel is applied to your skin over the area being examined. It helps prevent air pockets, which can block the sound waves that create the images. This safe, water-based gel is easy to remove from skin and, if needed, clothing.
A trained technician (sonographer) presses a small, hand-held device (transducer) against the area being studied and moves it as needed to capture the images. The transducer sends sound waves into your body, collects the ones that bounce back and sends them to a computer, which creates the images.
Sometimes, ultrasounds are done inside your body. In this case, the transducer is attached to a probe that's inserted into a natural opening in your body. Examples include:
- Transesophageal echocardiogram. A transducer, inserted into the esophagus, obtains heart images. It's usually done while under sedation.
- Transrectal ultrasound. This test creates images of the prostate by placing a special transducer into the rectum.
- Transvaginal ultrasound. A special transducer is gently inserted into the vagina to look at the uterus and ovaries.
Ultrasound is usually painless. However, you may experience mild discomfort as the sonographer guides the transducer over your body, especially if you're required to have a full bladder, or inserts it into your body.
A typical ultrasound exam takes from 30 minutes to an hour.
When your exam is complete, a doctor trained to interpret imaging studies (radiologist) analyzes the images and sends a report to your doctor. Your doctor will share the results with you.
You should be able to return to normal activities immediately after an ultrasound.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
- Andreas A, et al., eds. Grainger & Allison's Diagnostic Radiology: A Textbook of Medical Imaging. 7th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed Jan. 28, 2022.
- General ultrasound. RadiologyInfo.org. https://www.radiologyinfo.org/en/info/genus. Accessed Jan. 28, 2022.
- McKenzie GA (expert opinion). Mayo Clinic. Feb. 1, 2022.
- Chronic pelvic pain
- Ectopic pregnancy
- Fetal macrosomia
- Heavy menstrual bleeding
- Kidney stones
- Molar pregnancy
- Peritonitis
- Rheumatoid arthritis
- Soft tissue sarcoma
- Undescended testicle
- Urinary incontinence
News from Mayo Clinic
- Advancing ultrasound microvessel imaging and AI to improve cancer detection Oct. 13, 2023, 02:01 p.m. CDT
- Doctors & Departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Let’s celebrate our doctors!
Join us in celebrating and honoring Mayo Clinic physicians on March 30th for National Doctor’s Day.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Maier A, Steidl S, Christlein V, et al., editors. Medical Imaging Systems: An Introductory Guide [Internet]. Cham (CH): Springer; 2018. doi: 10.1007/978-3-319-96520-8_11

Medical Imaging Systems: An Introductory Guide [Internet].
Chapter 11 ultrasound.
Dominik Neumann and Eva Kollorz .
Affiliations
Published online: August 3, 2018.
Acoustic waves with frequencies ξ between 16 Hz and 20 kHz can be sensed by the human hearing and are thus called audible waves or audible sound.
11.1. Introduction
Acoustic waves with frequencies ξ between 16 Hz and 20 kHz can be sensed by the human hearing and are thus called audible waves or audible sound. If ξ > 20 kHz, one speaks of ultrasound ( Tab. 11.1 ). Some animal species such as bats can perceive ultrasound and use it for echolocation: by measuring the time between sending and receiving (after partial reflection on a surface) ultrasonic waves, the distance of an object (e. g., a wall or prey) to the sender (bat) can be computed accurately, assuming that the sound velocity is known. In the previous century, modern technology started to make use of this technique with applications ranging from marine distance measurement (1920: SONAR) to medicine (1958: first ultrasound device in clinical use). A typical system is shown in Fig. 11.1 .
Acoustic spectrum.
Figure 11.1
Clinical Ultrasound System in action. Image courtesy of Siemens Healthineers AG.
Today, medical ultrasound often is the first-resort clinical imaging modality due to its cost-effectiveness and lack of ionizing radiation. Typical medical ultrasound frequencies are between 2 MHz < ξ < 40 Mhz. Traditionally, medical ultrasound is mainly put to use in diagnostic applications, however, more therapeutic applications are emerging.
11.2. Physics of Sound Waves
This section introduces the basic underlying physics of ultrasound imaging.
11.2.1. Sound Waves
Acoustic signals emerge from organized movement of molecules or atoms, which cause local periodic compression of matter (gas, liquids, solid objects). Such spatially propagating, periodically repeating processes are commonly known as waves. Based on the direction of propagation, a distinction between transverse and longitudinal waves is made, where the nature of sound waves is the one of the latter class.
Sound waves are mainly characterized by frequency, velocity, wavelength , and intensity . Frequency ξ is measured in Hertz (Hz) and denotes the oscillation count per second. Sound velocity ν within a medium, measured in meters per second (m s −1 ), is independent of ξ , but varies with material properties such as elasticity and density. For some prominent examples see Tab. 11.2 . The wavelength λ is the distance between two oscillation maxima and measured in meters (m). Recall the fundamental wave equation relates wavelength λ with sound velocity c and frequency ξ : λ = c ξ . (11.1) Finally, the intensity J of a sound wave is measured in Watts per area (W m −2 ) and denotes the acoustic power density. Typical values for J in ultrasound diagnostics are between 1 and 10 mW cm −2 .
Sound velocity v and impedance Z of various media occurring in the human body.
11.2.2. Sound Wave Characteristics at Boundaries
The human body contains various kinds of boundaries between different materials, for instance, at borders between organs and liquids or other tissues. At such boundaries between two media, sound waves are partially reflected and partially transmitted.
11.2.2.1. Reflection
The well known law of reflection states that the angle of incidence equals the angle of reflection. This also holds for reflection of sound waves (cf. Fig. 11.2(b) ). For perpendicular incidence (cf. Fig. 11.2(a) ), the reflection R and transmission T coefficients write: R = J r J 0 = ( Z 2 − Z 1 Z 2 + Z 1 ) 2 (11.2) T = J t J 0 = 4 Z 1 Z 2 ( Z 1 + Z 2 ) 2 , (11.3) where J r , J t , and J 0 denote the wave intensity of the reflected, transmitted, and incident sound, respectively. Z 1 and Z 2 denote the acoustic impedance of two different media. Acoustic impedance Z , which is measured in g cm −2 s −1 , can be computed from the tensile modulus E (elasticity) and the density D of the given medium: Z = ( E ⋅ D ) . (11.4) For some prominent examples see Tab. 11.2 .
Figure 11.2
(a) Reflected J r and transmitted J t wave intensity at border between two different materials with impedance Z 1 and Z 2 , respectively. (b) Reflection of sound waves at smooth surfaces (α 1 = α 2 ).
From Eq. (11.2) , it is interesting to see that for two media with equal impedance Z 1 = Z 2 , no reflection happens. With similar impedance Z 1 ≈ Z 2 , as often occurring inside the human body at boundaries between similar types of tissue, the reflection coefficient R is rather small, while for | Z 1 – Z 2 | ≫ 0, e. g., at boundaries between air (low impedance) and soft tissue (high impedance), almost the entire wave is reflected (total reflection). The latter immediately leads to the conclusion that organs containing air, such as the lungs, cannot be examined via medical ultrasound. For more details see Tab. 11.3 .
Reflectivity at boundaries between two materials.
11.2.2.2. Scattering
Scattering means diffuse reflection of small portions of a wave in various directions. It should be noted that the law of reflection (see above) holds for each of those portions. Small inhomogeneities in the material cause scattering of sound waves, cf. Fig. 11.3(b) . The same holds for boundaries with rough surfaces as shown in Fig. 11.3(a) , where the width of the reflection cone increases with decreasing wavelength λ and increasing roughness of the surface. Scattering at rough surfaces is highly relevant in medical ultrasound, because in the case of perfectly smooth boundaries, waves are only reflected towards the sender if the direction of the wave is perpendicular to the surface (no diffusion), whereas for rough boundaries, the reflections in various directions enable imaging of tilted boundaries.
Figure 11.3
Scattering of sound waves at (a) a rough boundary (diffuse reflection) between two different media with impedance Z 1 and Z 2 ; and scattering at (b) inhomogeneities (depicted as blue dots) in a medium.

11.2.2.3. Diffraction
When sound waves pass barriers, obstacles, or openings on their path, they get diffracted. Diffracion involves a change in direction of the sound wave. Increasing wavelength λ yields an increased amount of diffraction (sharpness of bending), and vice versa. If λ is smaller than the size of the barrier, obstacle, or opening, the occurring diffraction becomes negligible.
11.2.2.4. Refraction
Snell’s law of refraction known from optics states v 1 v 2 = sin α 1 sin α 2 , (11.5) where α 1 and α 2 denote the angle of refraction in two different media, also applies to sound waves. However, since sound velocities ( υ 1 , υ 2 ) in human soft tissue differ only marginally (see Tab. 11.2 ), the little effects of refraction in medical ultrasound are negligible and therefore not considered further in this chapter.
11.2.3. Attenuation
Attenuation is the reduction in sound wave intensity J that occurs when a wave penetrates a medium. It follows the well-known exponential law of attenuation : J ( x ) = J 0 exp ( − μ x ) , (11.6) where J 0 denotes the initial intensity. The attenuation coefficient μ denotes the attenuation that occurs with each cm the sound wave travels inside a medium. It depends on material (tissue type) and ultrasound frequency ξ and is measured in decibel (dB). The attenuation coefficient mainly consists of two additive components μ = μ a + μ s , namely absorption μ a and scattering μ s (see above). Absorption μ a causes tissue to heat.
From Eq. (11.6) , it can be easily seen that the acoustic intensity J decreases with increasing penetration depth x . For a high maximum penetration depth, low frequencies are necessary as shown in Tab. 11.4 . However, the resolution of the acquired images decreases with decreasing frequency (cf. Sec. 11.3.3 ). Thus, the deeper the tissue penetration, the lower the spatial resolution.
Maximum penetration depth d max for various frequencies f .
11.3. Image Acquisition for Diagnostics
11.3.1. transducers.
An ultrasound transducer functions as both: a generator and a detector of ultrasonic waves. It converts mechanical energy into electrical energy and vice versa. When the transducer is pressed against the skin, it directs high-frequency sound waves into the body. Since sound waves produced by the transducer can barely penetrate air (cf. Tab. 11.3 ), gel is applied to the skin to help to minimize the amount of air between the transducer and the skin. As the waves penetrate the body, sound echoes are generated from the body’s fluids and tissues due to (diffuse) reflection and scattering. The strength and character of these sound echoes are recorded by the transducer and, depending on the type of transducer, can be transformed into 1-D, 2-D or 3-D images, which can be rendered and viewed to the user.
11.3.2. Piezoelectric Effect
In order to generate and detect ultrasonic waves, transducers rely on the so-called piezoelectric effect . It describes the conversion of electrical energy into mechanical energy and vice versa in piezoelectric materials. On the one hand, mechanical pressure (pressure translates to “piezo” (gr.)) is converted to electric polarization, which generates electric voltage. The electric voltage can be measured using two electrodes, as shown in Fig. 11.4 . On the other hand, electrical fields cause contraction or stretching of the piezoelectric material. This contraction and stretching can be used to generate ultrasound waves by applying a high frequency alternating voltage.
Figure 11.4
Piezoelectric effect.
Typical piezoelectric materials used in medical ultrasound transducers are barium titanate (BaTiO 3 ) and lead zirconium titanate (PZT).
11.3.3. Spatial Resolution
In ultrasound imaging, a distinction is made between two different kinds of spatial resolutions, in particular axial and lateral resolution (cf. Fig. 11.5 ).
Figure 11.5
Axial and lateral resolution of ultrasound devices. Minimal distance between two structures (blue dots) in axial/lateral direction that allows for distinguishing between them in the ultrasound image.
11.3.3.1. Axial Resolution
Axial resolution concerns structures lying behind each other w. r. t. the direction of the ultrasound waves. The better the axial resolution, the smaller the distance between two structures can be such that they can be distinguished by the transducer. Axial resolution is highly dependent on the ultrasound wave frequency f . The illustration in Fig. 11.6 explains that dependency based on a simple example, where an ultrasonic pulse generated by the transducer consists in a single wave only (shortest possible pulse). The distance d between the structures needs to be d ≥ λ/2 in order to be able distinguish between them.
Figure 11.6
Axial resolution: illustration of dependence on wave frequency f . Left and right shows two different timesteps, where d denotes the distance between two structures (blue dots). The high frequency (top) wave allows for distinguishing between the two structures, (more...)
11.3.3.2. Lateral Resolution
Lateral resolution concerns the distinguishability of structures located next to each other in the same lateral distance to the transducer (same penetration depth). Lateral resolution is always inferior to axial resolution.
11.3.3.3. Frequency Trade-off
As described above, axial and lateral transducer resolution depend on the ultrasound frequency ξ , and thus on the wavelength λ. As a rule of thumb: axial: Δ z ≥ λ / 2 , (11.7) lateral: Δ x ~ 3 ⋅ λ , (11.8) where ∆z and ∆x denote the minimum distance between to structures in axial/lateral direction such that the ultrasound echo is distinguishable. Hence, high ξ yields high resolution, whereas low ξ yields low resolution. However, the frequency is also directly related to attenuation (cf. Sec. 11.2.3 ), where high ξ yields high attenuation and vice versa. Thus, with high frequency f , the penetration depth is low but the images will have high resolution. At low ξ , deeper penetration is possible, but the resolution will be lower. Depending on the application, a trade-off between the desired properties (deep penetration versus high resolution) needs to be found, and the transducer frequency be adjusted accordingly.
11.3.4. Imaging Modes
Ultrasound offers a large variety of different imaging modes. The most common ones include A-mode, B-mode, and M-mode. A- and M-mode generate one-dimensional (1-D) images (signals), whereas B-mode can be used to acquire 2-D or even 3-D images (cf. Geek Box 1.1 ). Doppler (cf. Geek Box 1.2) can be acquired in 1-D and 2-D, and with the most recent generations of transducers also in 3-D.
11.3.4.1. A-Mode (Amplitude Mode)
A-mode is the simplest scanning mode. The height of the amplitude of the reflected ultrasound is displayed over the sonic runtime in the sonic ray direction. Extractable measurements are: frequency, modulated frequency, height of the impulse/amplitude, runtime, wave phase, phase shift, and attenuation. However, the major disadvantage is that only very localized information (one single line through the body) is acquired.
The backward scattered ultrasound intensity along a single ray is called A-mode . From a continuously running high-frequency generator, a wave packet is cut out with a “gate” and is passed to the transducer. The returning echo is given through a duplexer to a time-dependent amplifier (Time Gain Compensation). Later arriving echoes, which are weaker because of the absorption, are more amplified than the signals from the surface. Signals of high depth (15 cm) are raised up to 120 dB. The signal height of an interface reflected signal is independent of the penetration depth from which the echo comes. The signal-to-noise ratio becomes worse with increasing depth. The next sonic impulse will be emitted if all echoes of the preliminary sonic impulse are decayed. The repeat rate depends on the penetration depth and therewith on the used frequency.
11.3.4.2. B-Mode (Brightness Mode)
B-mode is the most common ultrasound mode. B-mode images are generated by systematically combining a multitude of A-mode (1-D) scans into a single 2-D image, where the intensity of a pixel is defined by the amplitude of the corresponding ultrasonic ray. In brief, in order to acquire 2-D images of the inner body, the ultrasound device has to sample not only on a 1-D ray (as in A-mode), but on a 2-D plane in 3-D space. Hence, various rays are sent in different directions. To achieve this, two techniques are commonly used: the mechanical and the electronic method.
Mechanical scanners The transducer librates in front of the patient, without any external movement of the gaging head. Thus, a slice of the human body is represented in the form of a circle segment. The intensity of the echo is transformed into gray scales and is inserted into an image matrix ( B-Mode ). An image consists of a fan of typically 100 lines.
Electronic scanners (linear/curved arrays) Here, many (60 to 100) and very small (0.5 mm to 1 mm) transducers are used, which are arranged in a row (“array”). A group of transducers is activated simultaneously. For scanning, the whole group of elements is shifted. With a curved arrangement of transducers, an image detail can be represented as a circle segment.
Electronic scanners (phased arrays) Every transducer element of an array can be accessed for both sending and receiving with an individual adjustable delay.
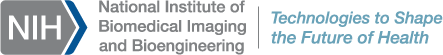
Geek Box 11.1 3-D Ultrasound
In 3-D ultrasound imaging, several 2-D images (B-mode) at different angles (w. r. t. axial direction) are combined into one 3-D volume. Real-time processing and visualization (rendering) of 3-D ultrasound images (volumes) requires high computational power, where graphics processing units can be used. Arbitrary section planes and “virtual travels through the body” are possible. The first 3-D ultrasound system was reported by Kazunori Baba in 1984. Slowly but steadily, 3-D ultrasound is becoming the standard of care in various medical fields (e. g., echocardiography), where 2-D imaging was traditionally used. One common application is to show their children to parents even before birth. An example is found right below this text.

11.3.4.3. M-Mode (Motion Mode)
In motion mode, ultrasonic pulses are emitted from the transducer in quick succession without movement of the transducer. Either an A-mode or a B-mode image is acquired each time. This allows for time-dependent measurement of organ movement relative to the probe. Thus, the velocity of specific organ structures can be obtained. This can be useful, for instance, when the movement of the cardiac wall (myocardium) is to be analyzed (echocardiography).
11.4. Safety Aspects
Geek box 11.2 3-d ultrasound.
Medical Doppler ultrasonography enables the measuring and visualization of blood flow (blood velocities). Two modes are frequently used: continuous wave (CW) Doppler and pulsed wave (PW) Doppler. In CW Doppler, half of the transducer array emits, and the other half detects pulses. It has the advantage that it allows for continuous imaging due to simultaneous emission and detection. However, no distance information can be measured. In PW Doppler, which is pulse-based, distance information can be obtained using time-gating. However, no continuous imaging is possible.
Doppler ultrasonography exploits the well-known Doppler effect . The Doppler effect is named after its discoverer Christian Johann Doppler (1803–1853) and can be observed in various situations, for instance, the noise of the siren of the ambulance when an ambulance passes at high speed. Other examples can be found in astronomy: the astronomical red-shift. Most relevant to medical Doppler ultrasonography, however, is blood flow, i. e., Doppler ultrasonography can visualize blood velocities. The Doppler effect describes the change in wave frequency by a relative movement between source and observer . A characteristic frequency shift appears, which is proportional to the relative velocity. Doppler ultrasonography aims at measuring the shift in frequency to estimate velocities (e. g., of blood in vessels).
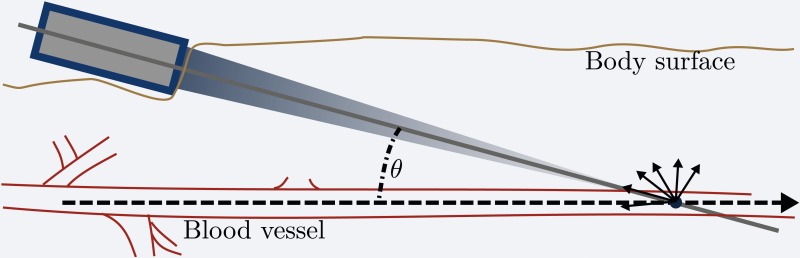
In Doppler blood flow imaging, the source are the moving blood cells, at which the waves scatter. The observer is the ultrasound transducer. The smaller the angle between the direction of blood flow in the vessel and the ultrasound wave direction, the better the Doppler effect can be exploited.
- Image acquisition is fast and relatively easy to learn.
- No ionizing radiation (contrary to X-ray/CT).
- Large number of potential applications: ultrasound can visualize structure, movement, and function of the body’s organs and blood vessels.
- through heating, proportional to absorbed acoustic intensity, or
- through cavitation , which means gas bubbles that emerge in the low pressure phases of sound waves and collapse at high pressure phases.
Since acoustic intensities for medical diagnostics are rather low, the potentially harmful effects described above have proven to be harmless. Medical ultrasound is considered one of the least harmful imaging techniques available today and is even used during pregnancy.
Therapeutical use of ultrasound can be found in gallstone and kidney stone therapies, where high intensity localized ultrasound is used to break up the stones. The heating effect of ultrasound waves can further be used to destroy diseased or cancerous tissue.
- Further Reading
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
- Cite this Page Neumann D, Kollorz E. Ultrasound. 2018 Aug 3. In: Maier A, Steidl S, Christlein V, et al., editors. Medical Imaging Systems: An Introductory Guide [Internet]. Cham (CH): Springer; 2018. Chapter 11. doi: 10.1007/978-3-319-96520-8_11
- PDF version of this page (782K)
- PDF version of this title (47M)
In this Page
- Introduction
- Physics of Sound Waves
- Image Acquisition for Diagnostics
- Safety Aspects
Related Items in Bookshelf
- All Reference Works
- All Textbooks
Similar articles in PubMed
- [Obstetrical ultrasound: can the fetus hear the wave and feel the heat?]. [Ultraschall Med. 2012] [Obstetrical ultrasound: can the fetus hear the wave and feel the heat?]. Abramowicz JS, Kremkau FW, Merz E. Ultraschall Med. 2012 Jun; 33(3):215-7. Epub 2012 Jun 14.
- High-frequency audibility: the effects of audiometric configuration, stimulus type, and device. [J Am Acad Audiol. 2015] High-frequency audibility: the effects of audiometric configuration, stimulus type, and device. Kimlinger C, McCreery R, Lewis D. J Am Acad Audiol. 2015 Feb; 26(2):128-37.
- Review Hearing at low and infrasonic frequencies. [Noise Health. 2004] Review Hearing at low and infrasonic frequencies. Møller H, Pedersen CS. Noise Health. 2004 Apr-Jun; 6(23):37-57.
- High-frequency hearing risk of operators of industrial ultrasonic devices. [Int Arch Occup Environ Health....] High-frequency hearing risk of operators of industrial ultrasonic devices. Grzesik J, Pluta E. Int Arch Occup Environ Health. 1983; 53(1):77-88.
- Review [Basics of ultrasound-guided nerve block]. [Masui. 2008] Review [Basics of ultrasound-guided nerve block]. Yamada M, Seo N. Masui. 2008 May; 57(5):549-55.
Recent Activity
- Ultrasound - Medical Imaging Systems Ultrasound - Medical Imaging Systems
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- U.S. Department of Health & Human Services
- National Institutes of Health
En Español | Site Map | Staff Directory | Contact Us
- Science Education
- Science Topics
What is medical ultrasound?
How does it work, what is ultrasound used for, are there risks, what are examples of nibib-funded projects using ultrasound.
Medical ultrasound falls into two distinct categories: diagnostic and therapeutic.
Diagnostic ultrasound can be further sub-divided into anatomical and functional ultrasound. Anatomical ultrasound produces images of internal organs or other structures. Functional ultrasound combines information such as the movement and velocity of tissue or blood, softness or hardness of tissue, and other physical characteristics, with anatomical images to create “information maps.” These maps help doctors visualize changes/differences in function within a structure or organ.
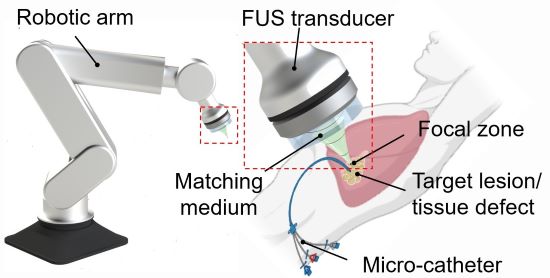
Therapeutic ultrasound also uses sound waves above the range of human hearing but does not produce images. Its purpose is to interact with tissues in the body such that they are either modified or destroyed. Among the modifications possible are: moving or pushing tissue, heating tissue, dissolving blood clots, or delivering drugs to specific locations in the body. These destructive, or ablative, functions are made possible by use of very high-intensity beams that can destroy diseased or abnormal tissues such as tumors. The advantage of using ultrasound therapies is that, in most cases, they are non-invasive. No incisions or cuts need to be made to the skin, leaving no wounds or scars.
Ultrasound waves are produced by a transducer, which can both emit ultrasound waves, as well as detect the ultrasound echoes reflected back. In most cases, the active elements in ultrasound transducers are made of special ceramic crystal materials called piezoelectrics. These materials are able to produce sound waves when an electric field is applied to them, but can also work in reverse, producing an electric field when a sound wave hits them. When used in an ultrasound scanner, the transducer sends out a beam of sound waves into the body. The sound waves are reflected back to the transducer by boundaries between tissues in the path of the beam (e.g. the boundary between fluid and soft tissue or tissue and bone). When these echoes hit the transducer, they generate electrical signals that are sent to the ultrasound scanner. Using the speed of sound and the time of each echo’s return, the scanner calculates the distance from the transducer to the tissue boundary. These distances are then used to generate two-dimensional images of tissues and organs.
During an ultrasound exam, the technician will apply a gel to the skin. This keeps air pockets from forming between the transducer and the skin, which can block ultrasound waves from passing into the body.
Click here to watch a short video about how ultrasound works.
Diagnostic ultrasound. Diagnostic ultrasound is able to non-invasively image internal organs within the body. However, it is not good for imaging bones or any tissues that contain air, like the lungs. Under some conditions, ultrasound can image bones (such as in a fetus or in small babies) or the lungs and lining around the lungs, when they are filled or partially filled with fluid. One of the most common uses of ultrasound is during pregnancy, to monitor the growth and development of the fetus, but there are many other uses, including imaging the heart, blood vessels, eyes, thyroid, brain, breast, abdominal organs, skin, and muscles. Ultrasound images are displayed in either 2D, 3D, or 4D (which is 3D in motion).
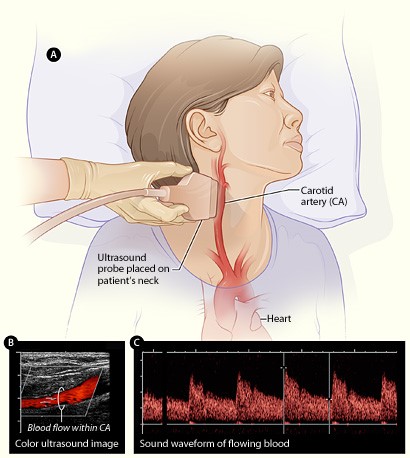
Functional ultrasound. Functional ultrasound applications include Doppler and color Doppler ultrasound for measuring and visualizing blood flow in vessels within the body or in the heart. It can also measure the speed of the blood flow and direction of movement. This is done using color-coded maps called color Doppler imaging. Doppler ultrasound is commonly used to determine whether plaque build-up inside the carotid arteries is blocking blood flow to the brain.
Another functional form of ultrasound is elastography, a method for measuring and displaying the relative stiffness of tissues, which can be used to differentiate tumors from healthy tissue. This information can be displayed as either color-coded maps of the relative stiffness; black-and white maps that display high-contrast images of tumors compared with anatomical images; or color-coded maps that are overlayed on the anatomical image. Elastography can be used to test for liver fibrosis, a condition in which excessive scar tissue builds up in the liver due to inflammation.
Ultrasound is also an important method for imaging interventions in the body. For example, ultrasound-guided needle biopsy helps physicians see the position of a needle while it is being guided to a selected target, such as a mass or a tumor in the breast. Also, ultrasound is used for real-time imaging of the location of the tip of a catheter as it is inserted in a blood vessel and guided along the length of the vessel. It can also be used for minimally invasive surgery to guide the surgeon with real-time images of the inside of the body.
Therapeutic or interventional ultrasound. Therapeutic ultrasound produces high levels of acoustic output that can be focused on specific targets for the purpose of heating, ablating, or breaking up tissue. One type of therapeutic ultrasound uses high-intensity beams of sound that are highly targeted, and is called High Intensity Focused Ultrasound (HIFU). HIFU is being investigated as a method for modifying or destroying diseased or abnormal tissues inside the body (e.g. tumors) without having to open or tear the skin or cause damage to the surrounding tissue. Either ultrasound or MRI is used to identify and target the tissue to be treated, guide and control the treatment in real time, and confirm the effectiveness of the treatment. HIFU is currently FDA approved for the treatment of uterine fibroids, to alleviate pain from bone metastases, and most recently for the ablation of prostate tissue. HIFU is also being investigated as a way to close wounds and stop bleeding, to break up clots in blood vessels, and to temporarily open the blood brain barrier so that medications can pass through.
Diagnostic ultrasound is generally regarded as safe and does not produce ionizing radiation like that produced by x-rays. Still, ultrasound is capable of producing some biological effects in the body under specific settings and conditions. For this reason, the FDA requires that diagnostic ultrasound devices operate within acceptable limits. The FDA, as well as many professional societies, discourage the casual use of ultrasound (e.g. for keepsake videos) and recommend that it be used only when there is a true medical need.
The following are examples of current research projects funded by NIBIB that are developing new applications of ultrasound that are already in use or that will be in use in the future:
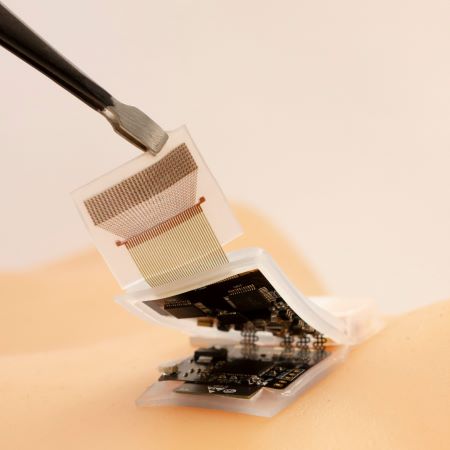
3D printing through the skin : Researchers at Duke University have developed a method to 3D print biocompatible structures through thick, multi-layered tissues. The approach entails using focused ultrasound to solidify a special ink that has been injected into the body to repair bone or repair soft tissues, for example. Initial experiments in animal tissue suggest the method could turn highly invasive surgical procedures into safer, less invasive ones. (Image on left courtesy of Junjie Yao (Duke University) and Yu Shrike Zhang (Harvard Medical School and Brigham and Women’s Hospital)).
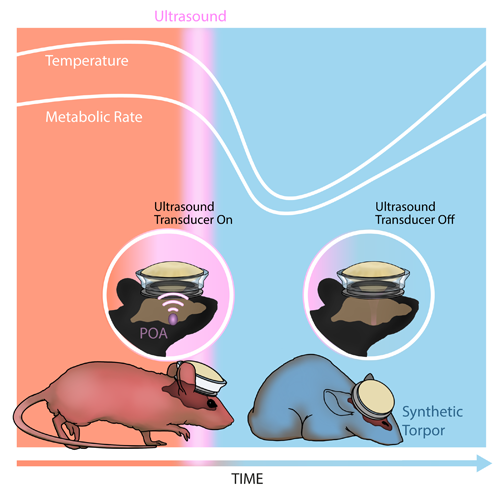
Inducing a hibernation-like state : Researchers at Washington University in St. Louis used ultrasound waves directed into the brain to lower the body temperature and metabolic rates of mice, inducing a hibernation-like state, called torpor. The researchers replicated some of these results in rats, which, like humans, don’t naturally enter torpor. Inducing torpor could help minimize damage from stroke or heart attack and buy precious time for patients in critical care. (Image on right courtesy of Yang et al./Washington University in St. Louis).
High-quality imaging at home : Brigham and Women’s Hospital researchers compared ultrasound scans acquired by experts with those taken by inexperienced volunteers, finding little difference in the image quality of the two groups. The unconventional approach of having patients take ultrasound images of themselves at home and share them with healthcare professionals could allow for remote monitoring and reduce the need for hospitalization. (Image on right courtesy of Duggan et al./Brigham and Women's Hospital).
Reviewed December 2023
Explore More
Heath Topics
- Breast Cancer
- Cardiovascular Disease
- Digestive Diseases
- Heart Disease
- Musculoskeletal Disease
- Reproductive Health
- Women's Health
Research Topics
- Optical Imaging
- Ultrasound (US) diagnostic
- Ultrasound (US) therapy
PROGRAM AREAS
- Ultrasound: Diagnostic and Interventional
Inside NIBIB
- Director's Corner
- Funding Policies
- NIBIB Fact Sheets
- Press Releases

Create Free Account or
- Acute Coronary Syndromes
- Anticoagulation Management
- Arrhythmias and Clinical EP
- Cardiac Surgery
- Cardio-Oncology
- Cardiovascular Care Team
- Congenital Heart Disease and Pediatric Cardiology
- COVID-19 Hub
- Diabetes and Cardiometabolic Disease
- Dyslipidemia
- Geriatric Cardiology
- Heart Failure and Cardiomyopathies
- Invasive Cardiovascular Angiography and Intervention
- Noninvasive Imaging
- Pericardial Disease
- Pulmonary Hypertension and Venous Thromboembolism
- Sports and Exercise Cardiology
- Stable Ischemic Heart Disease
- Valvular Heart Disease
- Vascular Medicine
- Clinical Updates & Discoveries
- Advocacy & Policy
- Perspectives & Analysis
- Meeting Coverage
- ACC Member Publications
- ACC Podcasts
- View All Cardiology Updates
- Earn Credit
- View the Education Catalog
- ACC Anywhere: The Cardiology Video Library
- CardioSource Plus for Institutions and Practices
- ECG Drill and Practice
- Heart Songs
- Nuclear Cardiology
- Online Courses
- Collaborative Maintenance Pathway (CMP)
- Understanding MOC
- Image and Slide Gallery
- Annual Scientific Session and Related Events
- Chapter Meetings
- Live Meetings
- Live Meetings - International
- Webinars - Live
- Webinars - OnDemand
- Certificates and Certifications
- ACC Accreditation Services
- ACC Quality Improvement for Institutions Program
- CardioSmart
- National Cardiovascular Data Registry (NCDR)
- Advocacy at the ACC
- Cardiology as a Career Path
- Cardiology Careers
- Cardiovascular Buyers Guide
- Clinical Solutions
- Clinician Well-Being Portal
- Diversity and Inclusion
- Infographics
- Innovation Program
- Mobile and Web Apps
Point of Care Ultrasound: An Overview
Expert analysis.
Introduction
With the ever-changing landscape of health care delivery in the United States, a greater proportion of patients are receiving their initial care and diagnostic testing in emergency departments (EDs). With this change, significant efforts have been made to improve the speed and accuracy of diagnostic testing, particularly by using point-of-care testing, to minimize the delay between onset of symptoms and initiation of definitive therapy. Expediting triage and time to diagnosis are crucial to decreasing morbidity and mortality in critically ill patients. 1 Point-of-care testing has been shown to achieve these goals, leading to improved operational efficiency and, ultimately, better patient outcomes. 2 Point-of-care ultrasound (PoCUS) in the ED is one of the point-of-care testing tools available to the emergency physician. It answers specific clinical questions that narrow differentials, guide clinical therapy, and direct consultations and disposition. This review is meant to highlight major clinical scenarios in which PoCUS can be used as a rapid, reliable, diagnostic tool. This list of scenarios is just an overview; there are many additional situations in which PoCUS can be crucial, but the presentations are often less acute (for example, musculoskeletal complaints, procedural guidance, and pregnancy evaluation).
Undifferentiated Shock
Broadly defined, shock is a state of tissue hypoxia due to reduced oxygen delivery, increased oxygen consumption, or inadequate oxygen utilization and most commonly occurs as a result of circulatory failure, resulting in hypotension. Identifying the cause of shock and rapidly intervening in patients experiencing it is an essential step in improving patient outcomes. PoCUS in the undifferentiated shock patient allows for rapid and accurate differentiation between the major shock types: distributive (i.e., septic), cardiogenic, hypovolemic (i.e., bleeding or other volume loss), and obstructive. There are several scan protocols that standardize this assessment, and most involve ultrasound imaging of the heart, the lungs, the vena cava, and a focused assessment of the abdomen to look for free fluid. Previous research on the use of PoCUS in the undifferentiated hypotensive patient presenting to the ED showed that despite taking only a short period of time (average of 6 minutes), the use of PoCUS led clinicians to significantly narrow their differential diagnosis and increase overall diagnostic precision. 3 The sonographic footprint for each type of shock guides resuscitation efforts and interventions (see Table 1), such as fluid versus vasopressor support and therapeutic procedural interventions (for example, pericardiocentesis and laparotomy).
Cardiac Arrest
Despite the most recent international consensus on advanced cardiac life support conclusion that "there is insufficient evidence to support or refute the routine use of ultrasound or echocardiography to guide cardiac arrest resuscitation," 4 PoCUS has become a common prognostic and diagnostic tool during cardiac resuscitation, particularly when combined with rhythm strip data. In patients with pulseless electrical activity (PEA) in particular, PoCUS can prove immensely helpful in revealing anatomic causes of PEA such as tension pneumothorax (see Video 1), cardiac tamponade, and pulmonary embolism. Presence of increased right ventricular strain, new tricuspid regurgitation, pericardial effusion, or absence of lung sliding can point in the direction of a reversible cause of PEA, thus rapidly directing the emergency physician to perform tube thoracostomy, pericardiocentesis, or thrombolysis, for example.
Video 1: Lung Point
Additional use of PoCUS during cardiac arrest relates primarily to prognosis. Numerous articles have demonstrated that the absence of any organized systolic contractions after three rounds of advanced cardiac life support medications suggests a minimal likelihood of return of spontaneous circulation. 5-7 Such intra-arrest knowledge can help guide the resuscitation timeline and direct resource utilization appropriately away from heroic measures. Moreover, it can provide some comfort to family and loved ones knowing that there are truly no signs of life, thus facilitating an appropriate withdrawal of care.
The role of PoCUS for trauma patients has been a topic of considerable change and debate over the last 30 years. Using ultrasound as a diagnostic tool for traumatic abdominal/thoracic injuries started in Europe and spread to North America in the 1990s. 8 Currently, ultrasound in trauma is primarily used for detection of intraperitoneal hemorrhage, pericardial tamponade, and hemothorax/pneumothorax. This constellation of applications is commonly referred to as the "extended focused assessment with sonography for trauma" (FAST). 9 The most basic six-view trauma ultrasound exam includes the hepatorenal space ("Morrison's pouch"), perisplenic space, subcostal space, pelvis, and views of each hemi-thorax (see Videos 2-5; these images are the footprint of a negative FAST). Although abdominal ultrasound views are often unable to isolate the source bleed, such diagnostic information can expedite trauma patients to the operating room for exploratory laparotomy when they are hemodynamically unstable. 10-13
Video 2: The Standard FAST Views: Right Upper Quadrant
Video 3: The Standard FAST Views: Left Upper Quadrant
Video 4: The Standard FAST Views: The Pelvis
Video 5: The Standard FAST Views: Abdominal Spine and Diaphragm Coming Together at a Point (Indicating the Chest Is Full of Air and Not Fluid)
The introduction of ultrasound into the standard trauma algorithm work-up has allowed for a more accelerated, definitive surgical approach and, in the right clinical context, a process designed to forgo computed tomography scans.
Studies have shown a high degree of sensitivity and specificity in the detection of pericardial effusions in medical and trauma patients using PoCUS. 16,17 Multiple sonographic signs suggesting cardiac tamponade have been described, but the most sensitive of these findings is the presence of a circumferential pericardial effusion with a hyperdynamic heart and "scalloping" of the right ventricle (i.e., diastolic collapse of the right ventricle). 18
Different etiologies of shortness of breath have different sonographic footprints. The presence or absence of the above-mentioned findings on ultrasound aid providers in making quick, often life-saving, clinical decisions at the bedside.
Video 6: B Lines
Video 7: Consolidation
Abdominal Pain
PoCUS has been described as the "third hand of emergency physicians and surgeons." 19 Ill-appearing patients with abdominal pain require immediate evaluation, particularly if they are elderly, because mortality rates in this population can be as high as 14%. 20 The "acute abdomen" in the emergent patient is a challenging diagnosis due to the wide differential the emergency physician must consider, which in turn causes a considerable amount of difficulty with regard to prompt initiation of treatment.
Fortunately, among the numerous pathologies that present as abdominal pain, many are amenable to PoCUS evaluation. Acute renal colic should demonstrate unilateral hydronephrosis and, on occasion, an obstructing stone at the ureterovesicular junction or within the urinary bladder. 21 Cholelithiasis is characterized by the presence of rounded, acoustically enhanced structures with distal shadowing artifacts; presence of common bile duct dilatation (diameter >6 mm) indicates biliary obstruction. Acute cholecystitis will show gallbladder wall thickening and pericholecystic fluid. 22 An abdominal aortic aneurysm can be identified on ultrasound with a rapid longitudinal evaluation of the abdominal aorta, looking for a diameter measuring >3 cm. 23 Finally, an acute intestinal obstruction can be diagnosed by identifying multiple loops of bowel measuring >3 cm in diameter when performing an abdominal sweep (see Video 8). The severity of the obstruction can be further categorized by determining the presence or absence of peristalsis, extra-luminal fluid, bowel wall thickening, and luminal air. 24
PoCUS has been a practice-changing technology for the care of the emergent and critically ill patient. The ability to look inside the human body in real time without the risk of radiation helps physicians narrow the differential diagnoses early on in a patient's evaluation and helps guide decisions regarding further testing (if any is indicated). Furthermore, findings seen on PoCUS engage consultants early on in workup, ultimately improving initial diagnostic accuracy, initiation of proper management, and thus overall patient care. As the technology becomes more accessible, we can expect it to diffuse throughout the broader institution of medicine.
- Rooney KD, Schilling UM. Point-of-care testing in the overcrowded emergency department--can it make a difference? Crit Care 2014;18:692.
- The College of Emergency Medicine. Crowding in the Emergency Department . Revised ed. London, England: The College of Emergency Medicine; 2014.
- Jones AE, Tayal VS, Sullivan DM, Kline JA. Randomized, controlled trial of immediate versus delayed goal-directed ultrasound to identify the cause of nontraumatic hypotension in emergency department patients. Crit Care Med 2004;32:1703-8.
- Morrison LJ, Deakin CD, Morley PT, et al. Part 8: Advanced life support: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation 2010;122:S345-421.
- Salen P, Melniker L, Chooljian C, et al. Does the presence or absence of sonographically identified cardiac activity predict resuscitation outcomes of cardiac arrest patients? Am J Emerg Med 2005;23:459-62.
- Salen P, O'Connor R, Sierzenski P, et al. Can cardiac sonography and capnography be used independently and in combination to predict resuscitation outcomes? Acad Emerg Med 2001;8:610-5.
- Blaivas M, Fox JC. Outcome in cardiac arrest patients found to have cardiac standstill on the bedside emergency department echocardiogram. Acad Emerg Med 2001;8:616-21.
- Nordenholz KE, Rubin MA, Gularte GG, Liang HK. Ultrasound in the evaluation and management of blunt abdominal trauma. Ann Emerg Med 1997;29:357-66.
- Melanson SW, Heller M. The emerging role of bedside ultrasonography in trauma care. Emerg Med Clin North Am 1998;16:165-89.
- American Institute of Ultrasound in Medicine; American College of Emergency Physicians. AIUM practice guideline for the performance of the focused assessment with sonography for trauma (FAST) examination. J Ultrasound Med 2014;33:2047-56.
- Körner M, Krötz MM, Degenhart C, Pfeifer KJ, Reiser MF, Linsenmaier U. Current Role of Emergency US in Patients with Major Trauma. Radiographics 2008;28:225-42.
- Montoya J, Stawicki SP, Evans DC, et al. From FAST to E-FAST: an overview of the evolution of ultrasound-based traumatic injury assessment. Eur J Trauma Emerg Surg 2016;42:119-26.
- Kirkpatrick AW, Sirois M, Laupland KB, et al. Hand-held thoracic sonography for detecting post-traumatic pneumothoraces: the Extended Focused Assessment with Sonography for Trauma (EFAST). J Trauma 2004;57:288-95.
- Amsterdam EA, Kirk JD, Bluemke DA, et al. Testing of low-risk patients presenting to the emergency department with chest pain: a scientific statement from the American Heart Association. Circulation 2010;122:1756-6.
- Labovitz AJ, Noble VE, Bierig M, et al. Focused cardiac ultrasound in the emergent setting: a consensus statement of the American Society of Echocardiography and American College of Emergency Physicians. J Am Soc Echocardiogr 2010;23:1225-30.
- Jones AE, Tayal VS, Kline JA. Focused training of emergency medicine residents in goal-directed echocardiography: a prospective study. Acad Emerg Med 2003;10:1054-8.
- Mayron R, Gaudio FE, Plummer D, Asinger R, Elsperger J. Echocardiography performed by emergency physicians: impact on diagnosis and therapy. Ann Emerg Med 1988;17:150-4.
- Noble VE, Nelson B, Sutingco AN. Manual of Emergency and Critical Care Ultrasound . 1st ed. New York, New York: Cambridge University Press; 2007.
- Frazzetta G, Faraci C, Mancuso SI, Fragati G, Di Giovani S, Costanzo L. Emergency Ultrasound in Critical Patients: The "Bedside Ultrasonography" as the "Third Hand" of Emergency Surgeon. Austin J Emergency & Crit Care Med 2015;2:1-4.
- McNamara R, Dean AJ. Approach to acute abdominal pain. Emerg Med Clin North Am 2011;29:159-73.
- Smith-Bindman R, Aubin C, Bailitz J, et al. Ultrasonography versus computed tomography for suspected nephrolithiasis. N Engl J Med 2014;371:1100-10.
- Fox CJ, Harry RA, Cairns SR. A prospective series of out-patient endoscopic retrograde cholangiopancreatography. Eur J Gastroenterol Hepatol 2000;12:523-7.
- Hoffmann B, Bessman ES, Um P, Ding R, McCarthy ML. Successful sonographic visualisation of the abdominal aorta differs significantly among a diverse group of credentialed emergency department providers. Emerg Med J 2010;28:472-6.
- Taylor MR, Lalani N. Adult small bowel obstruction. Acad Emerg Med 2013;20:528-44.
Keywords: Diagnostic Imaging, Abdomen, Abdomen, Acute, Abdominal Pain, Acute Coronary Syndrome, Advanced Cardiac Life Support, Algorithms, Aorta, Abdominal, Aortic Aneurysm, Abdominal, Cardiac Tamponade, Chest Pain, Cholecystitis, Acute, Cholelithiasis, Cholestasis, Colonic Pouches, Common Bile Duct, Contusions, Critical Illness, Diagnosis, Differential, Diaphragm, Dilatation, Dyspnea, Edema, Echocardiography, Emergency Service, Hospital, Heart Arrest, Heart Ventricles, Hemothorax, Hydronephrosis, Hydrostatic Pressure, Hypotension, Hypovolemia, Intestinal Obstruction, Laparotomy, Operating Rooms, Oxygen, Oxygen Consumption, Pelvis, Pericardial Effusion, Pericardiocentesis, Peristalsis, Pleura, Pneumothorax, Point-of-Care Systems, Point-of-Care Systems, Pregnancy, Prognosis, Pulmonary Edema, Pulmonary Embolism, Referral and Consultation, Renal Colic, Shock, Surgeons, Thoracic Injuries, Thoracostomy, Thorax, Tomography, Triage, Tricuspid Valve Insufficiency, Ultrasonography, Urinary Bladder
You must be logged in to save to your library.
Jacc journals on acc.org.
- JACC: Advances
- JACC: Basic to Translational Science
- JACC: CardioOncology
- JACC: Cardiovascular Imaging
- JACC: Cardiovascular Interventions
- JACC: Case Reports
- JACC: Clinical Electrophysiology
- JACC: Heart Failure
- Current Members
- Campaign for the Future
- Become a Member
- Renew Your Membership
- Member Benefits and Resources
- Member Sections
- ACC Member Directory
- ACC Innovation Program
- Our Strategic Direction
- Our History
- Our Bylaws and Code of Ethics
- Leadership and Governance
- Annual Report
- Industry Relations
- Support the ACC
- Jobs at the ACC
- Press Releases
- Social Media
- Book Our Conference Center
Clinical Topics
- Chronic Angina
- Congenital Heart Disease and Pediatric Cardiology
- Diabetes and Cardiometabolic Disease
- Hypertriglyceridemia
- Invasive Cardiovascular Angiography and Intervention
- Pulmonary Hypertension and Venous Thromboembolism
Latest in Cardiology
Education and meetings.
- Online Learning Catalog
- Products and Resources
- Annual Scientific Session
Tools and Practice Support
- Quality Improvement for Institutions
- Accreditation Services
- Practice Solutions
Heart House
- 2400 N St. NW
- Washington , DC 20037
- Email: [email protected]
- Phone: 1-202-375-6000
- Toll Free: 1-800-253-4636
- Fax: 1-202-375-6842
- Media Center
- ACC.org Quick Start Guide
- Advertising & Sponsorship Policy
- Clinical Content Disclaimer
- Editorial Board
- Privacy Policy
- Registered User Agreement
- Terms of Service
- Cookie Policy
© 2024 American College of Cardiology Foundation. All rights reserved.

IMAGES
VIDEO
COMMENTS
Clean the ultrasound probe. 4. Apply a tourniquet. 5. Apply gel to the ultrasound probe. 6. Identify the target vein in the transverse plane: note the depth of the anterior wall of the vein and pay attention to any adjacent structures. 7. Once identified, rotate the probe into the longitudinal plane.
Ultrasound is a noninvasive imaging test that shows structures inside your body using high-intensity sound waves. Healthcare providers use ultrasound exams for several purposes, including during pregnancy, for diagnosing conditions and for image guidance during certain procedures. Contents Overview Test Details Results and Follow-Up.
Ultrasound ( US) is an imaging technology that uses high-frequency sound waves to characterize tissue. It is a useful and flexible modality in medical imaging, and often provides an additional or unique characterization of tissues, when compared to other modalities such as conventional radiography or CT.
Frequently Asked Questions. Sonography is a diagnostic medical test that uses high-frequency sound waves, or ultrasound waves, to create images of tissues, glands, organs, and blood or fluid flow within the body. This test is also referred to as an ultrasound or sonogram. Sonography uses a device called a transducer on the surface of the skin ...
Manual of diagnostic ultrasound – Volume 1 4 Properties of ultrasound Sound is a vibration transmitted through a solid, liquid or gas as mechanical pressure waves that carry kinetic energy. A medium must therefore be present for the propagation of these waves. The type of waves depends on the medium. Ultrasound propagates in
Overview. Diagnostic ultrasound, also called sonography or diagnostic medical sonography, is an imaging method that uses sound waves to produce images of structures within your body. The images can provide valuable information for diagnosing and directing treatment for a variety of diseases and conditions. Most ultrasound examinations are done ...
Today, medical ultrasound often is the first-resort clinical imaging modality due to its cost-effectiveness and lack of ionizing radiation. Typical medical ultrasound frequencies are between 2 MHz < ξ < 40 Mhz. Traditionally, medical ultrasound is mainly put to use in diagnostic applications, however, more therapeutic applications are emerging.
This presentation will briefly discuss the most common subtypes, ultrasound characteristics and management options of this group of complex conditions. Ultrasound offers excellent lesion characterisation which guides treatment planning and is often the modality of choice for initial evaluation of these lesions.
Diagnostic ultrasound is a non-invasive diagnostic technique used to image inside the body. Ultrasound probes, called transducers, produce sound waves that have frequencies above the threshold of human hearing (above 20KHz), but most transducers in current use operate at much higher frequencies (in the megahertz (MHz) range).
Video 1 - Point of Care Ultrasound. The point where the visceral pleura separates from the parietal pleura is called the lung point. The lung sliding or shimmering is where the two pleura are still opposed; the static parietal pleura line is where there is air separating the two.