An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Wiley - PMC COVID-19 Collection


Effectiveness of COVID‐19 vaccines: findings from real world studies
David a henry.
1 Institute for Evidence-Based Healthcare, Bond University, Gold Coast QLD
2 Gold Coast University Hospital and Health Service, Gold Coast QLD
Mark A Jones
3 University of Queensland, Brisbane QLD
Paulina Stehlik
Paul p glasziou.
Community‐based studies in five countries show consistent strong benefits from early rollouts of COVID‐19 vaccines
By the beginning of June 2021, almost 11% of the world’s population had received at least one dose of a coronavirus disease 2019 (COVID‐19) vaccine. 1 This represents an extraordinary scientific and logistic achievement — in 18 months, researchers, manufacturers and governments collaborated to produce and distribute vaccines that appear effective and acceptably safe in preventing COVID‐19 and its complications. 2 , 3
The initial randomised trials confirmed immunological responses and generated unbiased evidence of vaccine efficacy. They were conducted in selected populations with limited numbers of participants in high risk groups, such as older people and those with serious underlying medical conditions. 2 , 3 They provided sparse information on the impact of vaccination on transmission of severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), were too small to quantify rare but serious harms, and did not take account of the logistic obstacles encountered during the community‐wide rollout of new vaccines. While large cluster randomised trials could address some of these concerns, 4 large observational studies have used large linked routinely collected population datasets in five countries to address important knowledge gaps. 5 , 6 , 7 , 8 , 9
This article reviews findings from the initial real world studies and stresses that researchers in Australia currently do not have timely access to the linked Commonwealth and state datasets needed to perform such analyses.
Real world studies
In five countries (Israel, England, Scotland, Sweden and the United States) researchers have analysed routinely collected data to report the early outcomes of community‐wide vaccination programs with three of the first vaccines to reach market: the BNT162b2 mRNA (Pfizer–BioNTech), mRNA‐1273 (Moderna) and ChAdOx1 adenoviral vector (Oxford–AstraZeneca) vaccines. 5 , 6 , 7 , 8 , 9
At the time of writing, two of the articles (from the US and Sweden ) have not yet been peer reviewed, so details reported here may change after revisions to these reports. 8 , 9 There is a rapidly growing literature on the community impact of COVID‐19 and it has provided very consistent evidence of substantial vaccine effectiveness with the original (Wuhan) viral strain and the Alpha variant. An important focus of future work will be the effectiveness of existing vaccines against emerging viral variants.
The vaccination programs against COVID‐19 commenced in December 2020 in the study countries, so follow‐up is limited. Most of the investigators used rigorous designs and statistical methods to analyse linked routinely collected person‐level data from large community‐wide databases that tracked outcomes in vaccinated and unvaccinated individuals ( Box ). Importantly, allocation to vaccines was not by randomisation, and vaccinated and unvaccinated populations differed in respect of factors that were associated with both the probability of vaccination and with the severe outcomes of COVID‐19. Information that featured in most studies included demographic details, a vaccine register, results of laboratory polymerase chain reaction (PCR) testing, records of hospitalisation and death, and some geographic measures of social deprivation. In addition, the Israeli, US and Scottish studies included linkage to clinical records from which to quantify comorbidities. 5 , 6 , 8 The Israeli study included information on previous adherence to influenza vaccination schedules. 5
Characteristics of five real world community‐based studies of effectiveness of SARS‐CoV‐2 vaccines
BNT162b2 =Pfizer–BioNTech mRNA vaccine; ChAdOx1 = Oxford–AstraZeneca adenoviral vector vaccine; mRNA‐1273 = Moderna mRNA vaccine; NHS = National Health Service; PCR = polymerase chain reaction.
Study designs and adjustments for confounding
The studies used different approaches to adjust for confounding ( Box ). The most advanced design was used to analyse the linked data from members of the Clalit Health Services integrated health care organisation in Israel, which covers around 4.7 million people. 5 The investigators extracted data on matched cohorts of vaccinees and non‐vaccinated controls and analysed study endpoints using rules that emulated the steps taken in a randomised trial. 10 These steps minimised selection or measurement biases and controlled for potential confounders through precise 1:1 matching of vaccinated and non‐vaccinated subjects across seven domains. The investigators took the additional step of calibrating their statistical model against the results of the pivotal phase 3 randomised trial, which found no benefit during the first 2 weeks after vaccination. 2 In contrast, this observational study found lower rates of infection in the first 2 weeks after vaccination, which remained after matching for age and sex — illustrating the potential for confounding. Only after full matching on seven factors was this source of bias eliminated. 5
In England, investigators linked data from a national vaccine register to laboratory PCR swab results, emergency department admissions, demographic and ethnicity data, care home status, and deaths in participants aged 70 years and over ( Box ). 7 The first part was a test‐negative case–control design, which compared vaccination status in those who received a positive PCR swab result with contemporaneous controls who returned a negative result. That both cases and controls had been tested for SARS‐CoV‐2 should have controlled for clinical and behavioural factors that influence the probability of having a test. The second part of the study followed participants aged 80 years and over with a positive PCR test result and analysed them according to vaccination status. The investigators calculated adjusted hazard ratios for death up to and beyond 14 days from the first vaccine dose.
A study in Scotland used an unmatched cohort design comparing hospital admission for COVID‐19 in people who received either the Pfizer–BioNTech or Oxford–AstraZeneca vaccines with an unvaccinated control group. 6 The Oxford–AstraZeneca vaccine was given later to an older population. The study adjusted for age and sex, frequency of prior PCR tests and clinical risk groups extracted from linked health records. The statistical model generated unexpectedly strong protective effects of the vaccines on hospitalisation rates in the first 2 weeks after vaccination, indicating possible bias due to a healthy vaccinee effect.
In the US, researchers working within the Mayo Clinic health system used postcode and propensity scores (based on age, sex, race, ethnicity and records of PCR testing) to match a cohort of individuals who received the Pfizer–BioNTech or Moderna mRNA vaccine with unvaccinated controls, to measure impact on infections and hospitalisations. 8
A simple unmatched cohort design using linkage of routinely collected administrative data measured infection rates in a cohort who received the Pfizer–BioNTech vaccine in a single county in Sweden. 9 The unvaccinated population acted as controls ( Box ). Confounding adjustments in this study were limited to age and sex.
The Box summarises the results of these studies. All included at least one mRNA vaccine and the reductions in infections and hospitalisations were consistent and large. Two studies reported on mortality and the reductions were substantial, although based on small numbers of deaths in Israel. 5 , 7 The studies did not directly compare vaccines, but the Oxford–AstraZeneca vaccine appeared to perform as well as the mRNA vaccines in reducing hospitalisations.
Other approaches to estimating vaccine effectiveness
In the UK, over 600 000 volunteers using a COVID‐19 symptom mobile phone app recorded adverse events after vaccination with either the Pfizer–BioNTech or Oxford–AstraZeneca vaccine. 11 Based on post‐vaccination self‐reports of infections and after adjustment for age, sex, obesity and comorbidities, they estimated effectiveness rates of 60–70% beyond 21 days after administration of either vaccine.
Three studies measured the effectiveness of COVID‐19 vaccines in care home, health care and other frontline workers in the UK, Israel and the US. 12 , 13 , 14 These projects enrolled smaller numbers of participants than the community‐based studies but used similar designs and adjustment techniques. Importantly, workers in these settings undergo routine PCR testing for SARS‐CoV‐2, which enabled detection of asymptomatic infections. These studies also found large protective effects and a potential to reduce viral transmission. The latter possibility has been investigated directly in a study conducted in Scotland that showed that 14 days or more after health care workers received a second dose of vaccine, their household members had a 54% lower rate of COVID‐19 than individuals who shared households with non‐vaccinated health care workers. 15
Conclusions
We can draw important conclusions from these non‐randomised studies of vaccine effectiveness. Most importantly, the currently available COVID‐19 vaccines appear to be very effective in preventing severe complications and deaths from COVID‐19 in adults of all ages. Recent real world studies confirm that substantial protection extends to the Delta variant of SARS‐CoV‐2, although this requires two vaccine doses. 16 , 17 Follow‐up periods in all studies are relatively short, and these reports do not provide information on rare but serious adverse events, such as cerebral venous thrombosis. The use of sophisticated trial emulation methods in the Israeli study 5 replicated some key features of the pivotal randomised trial of the Pfizer–BioNTech vaccine, 2 particularly by controlling for an early healthy cohort effect that confounded the incompletely adjusted endpoint analyses. This design should prove useful in enabling direct head‐to‐head comparisons of effectiveness and safety of vaccines, the duration of their protective effects, the degree to which vaccines prevent transmission of viral variants, and the impact of vaccines on so‐called long COVID.
These studies exemplify the value of advanced analyses of large multiply linked routinely collected community datasets. This resource is not yet readily available to researchers in Australia due to continued lack of agreement on the governance of linked state and Commonwealth datasets. 18 While Australia’s current low rates of community transmission of SARS‐CoV‐2 reduce the feasibility of observational studies of vaccine effectiveness, the available data can provide important information on potential harms of vaccines. With continuing questions about the comparative safety of vaccines, the emergence of viral variants, the long term effects of COVID‐19 and the likelihood of future epidemics, it is essential that Australia urgently removes barriers to allowing prequalified researchers to safely access the linked de‐identified population datasets that are needed to expeditiously conduct the types of studies reviewed here.
Competing interests
No relevant disclosures.
Not commissioned; externally peer reviewed.
The unedited version of this article was published as a preprint on mja.com.au on 20 May 2021.
- Scoping Review
- Open access
- Published: 14 November 2021
Effectiveness and safety of SARS-CoV-2 vaccine in real-world studies: a systematic review and meta-analysis
- Qiao Liu 1 na1 ,
- Chenyuan Qin 1 , 2 na1 ,
- Min Liu 1 &
- Jue Liu ORCID: orcid.org/0000-0002-1938-9365 1 , 2
Infectious Diseases of Poverty volume 10 , Article number: 132 ( 2021 ) Cite this article
56k Accesses
203 Citations
374 Altmetric
Metrics details
To date, coronavirus disease 2019 (COVID-19) becomes increasingly fierce due to the emergence of variants. Rapid herd immunity through vaccination is needed to block the mutation and prevent the emergence of variants that can completely escape the immune surveillance. We aimed to systematically evaluate the effectiveness and safety of COVID-19 vaccines in the real world and to establish a reliable evidence-based basis for the actual protective effect of the COVID-19 vaccines, especially in the ensuing waves of infections dominated by variants.
We searched PubMed, Embase and Web of Science from inception to July 22, 2021. Observational studies that examined the effectiveness and safety of SARS-CoV-2 vaccines among people vaccinated were included. Random-effects or fixed-effects models were used to estimate the pooled vaccine effectiveness (VE) and incidence rate of adverse events after vaccination, and their 95% confidence intervals ( CI ).
A total of 58 studies (32 studies for vaccine effectiveness and 26 studies for vaccine safety) were included. A single dose of vaccines was 41% (95% CI : 28–54%) effective at preventing SARS-CoV-2 infections, 52% (31–73%) for symptomatic COVID-19, 66% (50–81%) for hospitalization, 45% (42–49%) for Intensive Care Unit (ICU) admissions, and 53% (15–91%) for COVID-19-related death; and two doses were 85% (81–89%) effective at preventing SARS-CoV-2 infections, 97% (97–98%) for symptomatic COVID-19, 93% (89–96%) for hospitalization, 96% (93–98%) for ICU admissions, and 95% (92–98%) effective for COVID-19-related death, respectively. The pooled VE was 85% (80–91%) for the prevention of Alpha variant of SARS-CoV-2 infections, 75% (71–79%) for the Beta variant, 54% (35–74%) for the Gamma variant, and 74% (62–85%) for the Delta variant. The overall pooled incidence rate was 1.5% (1.4–1.6%) for adverse events, 0.4 (0.2–0.5) per 10 000 for severe adverse events, and 0.1 (0.1–0.2) per 10 000 for death after vaccination.
Conclusions
SARS-CoV-2 vaccines have reassuring safety and could effectively reduce the death, severe cases, symptomatic cases, and infections resulting from SARS-CoV-2 across the world. In the context of global pandemic and the continuous emergence of SARS-CoV-2 variants, accelerating vaccination and improving vaccination coverage is still the most important and urgent matter, and it is also the final means to end the pandemic.
Graphical Abstract
Since its outbreak, coronavirus disease 2019 (COVID-19) has spread rapidly, with a sharp rise in the accumulative number of infections worldwide. As of August 8, 2021, COVID-19 has already killed more than 4.2 million people and more than 203 million people were infected [ 1 ]. Given its alarming-spreading speed and the high cost of completely relying on non-pharmaceutical measures, we urgently need safe and effective vaccines to cover susceptible populations and restore people’s lives into the original [ 2 ].
According to global statistics, as of August 2, 2021, there are 326 candidate vaccines, 103 of which are in clinical trials, and 19 vaccines have been put into normal use, including 8 inactivated vaccines and 5 protein subunit vaccines, 2 RNA vaccines, as well as 4 non-replicating viral vector vaccines [ 3 ]. Our World in Data simultaneously reported that 27.3% of the world population has received at least one dose of a COVID-19 vaccine, and 13.8% is fully vaccinated [ 4 ].
To date, COVID-19 become increasingly fierce due to the emergence of variants [ 5 , 6 , 7 ]. Rapid herd immunity through vaccination is needed to block the mutation and prevent the emergence of variants that can completely escape the immune surveillance [ 6 , 8 ]. Several reviews systematically evaluated the effectiveness and/or safety of the three mainstream vaccines on the market (inactivated virus vaccines, RNA vaccines and viral vector vaccines) based on random clinical trials (RCT) yet [ 9 , 10 , 11 , 12 , 13 ].
In general, RNA vaccines are the most effective, followed by viral vector vaccines and inactivated virus vaccines [ 10 , 11 , 12 , 13 ]. The current safety of COVID-19 vaccines is acceptable for mass vaccination, but long-term monitoring of vaccine safety is needed, especially in older people with underlying conditions [ 9 , 10 , 11 , 12 , 13 ]. Inactivated vaccines had the lowest incidence of adverse events and the safety comparisons between mRNA vaccines and viral vectors were controversial [ 9 , 10 ].
RCTs usually conduct under a very demanding research circumstance, and tend to be highly consistent and limited in terms of population characteristics and experimental conditions. Actually, real-world studies differ significantly from RCTs in terms of study conditions and mass vaccination in real world requires taking into account factors, which are far more complex, such as widely heterogeneous populations, vaccine supply, willingness, medical accessibility, etc. Therefore, the real safety and effectiveness of vaccines turn out to be a major concern of international community. The results of a mass vaccination of CoronaVac in Chile demonstrated a protective effectiveness of 65.9% against the onset of COVID-19 after complete vaccination procedures [ 14 ], while the outcomes of phase 3 trials in Brazil and Turkey were 50.7% and 91.3%, reported on Sinovac’s website [ 14 ]. As for the Delta variant, the British claimed 88% protection after two doses of BNT162b2, compared with 67% for AZD1222 [ 15 ]. What is surprising is that the protection of BNT162b2 against infection in Israel is only 39% [ 16 ]. Several studies reported the effectiveness and safety of the COVID-19 vaccine in the real world recently, but the results remain controversial [ 17 , 18 , 19 , 20 ]. A comprehensive meta-analysis based upon the real-world studies is still in an urgent demand, especially for evaluating the effect of vaccines on variation strains. In the present study, we aimed to systematically evaluate the effectiveness and safety of the COVID-19 vaccine in the real world and to establish a reliable evidence-based basis for the actual protective effect of the COVID-19 vaccines, especially in the ensuing waves of infections dominated by variants.
Search strategy and selection criteria
Our methods were described in detail in our published protocol [PROSPERO (Prospective register of systematic reviews) registration, CRD42021267110]. We searched eligible studies published by 22 July 2021, from three databases including PubMed, Embase and Web of Science by the following search terms: (effectiveness OR safety) AND (COVID-19 OR coronavirus OR SARS-CoV-2) AND (vaccine OR vaccination). We used EndNoteX9.0 (Thomson ResearchSoft, Stanford, USA) to manage records, screen and exclude duplicates. This study was strictly performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).
We included observational studies that examined the effectiveness and safety of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) vaccines among people vaccinated with SARS-CoV-2 vaccines. The following studies were excluded: (1) irrelevant to the subject of the meta-analysis, such as studies that did not use SARS-CoV-2 vaccination as the exposure; (2) insufficient data to calculate the rate for the prevention of COVID-19, the prevention of hospitalization, the prevention of admission to the ICU, the prevention of COVID-19-related death, or adverse events after vaccination; (3) duplicate studies or overlapping participants; (4) RCT studies, reviews, editorials, conference papers, case reports or animal experiments; and (5) studies that did not clarify the identification of COVID-19.
Studies were identified by two investigators (LQ and QCY) independently following the criteria above, while discrepancies reconciled by a third investigator (LJ).
Data extraction and quality assessment
The primary outcome was the effectiveness of SARS-CoV-2 vaccines. The following data were extracted independently by two investigators (LQ and QCY) from the selected studies: (1) basic information of the studies, including first author, publication year and study design; (2) characteristics of the study population, including sample sizes, age groups, setting or locations; (3) kinds of the SARS-CoV-2 vaccines; (4) outcomes for the effectiveness of SARS-CoV-2 vaccines: the number of laboratory-confirmed COVID-19, hospitalization for COVID-19, admission to the ICU for COVID-19, and COVID-19-related death; and (5) outcomes for the safety of SARS-CoV-2 vaccines: the number of adverse events after vaccination.
We evaluated the risk of bias using the Newcastle–Ottawa quality assessment scale for cohort studies and case–control studies [ 21 ]. and assess the methodological quality using the checklist recommended by Agency for Healthcare Research and Quality (AHRQ) [ 22 ]. Cohort studies and case–control studies were classified as having low (≥ 7 stars), moderate (5–6 stars), and high risk of bias (≤ 4 stars) with an overall quality score of 9 stars. For cross-sectional studies, we assigned each item of the AHRQ checklist a score of 1 (answered “yes”) or 0 (answered “no” or “unclear”), and summarized scores across items to generate an overall quality score that ranged from 0 to 11. Low, moderate, and high risk of bias were identified as having a score of 8–11, 4–7 and 0–3, respectively.
Two investigators (LQ and QCY) independently assessed study quality, with disagreements resolved by a third investigator (LJ).
Data synthesis and statistical analysis
We performed a meta-analysis to pool data from included studies and assess the effectiveness and safety of SARS-CoV-2 vaccines by clinical outcomes (rates of the prevention of COVID-19, the prevention of hospitalization, the prevention of admission to the ICU, the prevention of COVID-19-related death, and adverse events after vaccination). Random-effects or fixed-effects models were used to pool the rates and adjusted estimates across studies separately, based on the heterogeneity between estimates ( I 2 ). Fixed-effects models were used if I 2 ≤ 50%, which represented low to moderate heterogeneity and random-effects models were used if I 2 > 50%, representing substantial heterogeneity.
We conducted subgroup analyses to investigate the possible sources of heterogeneity by using vaccine kinds, vaccination status, sample size, and study population as grouping variables. We used the Q test to conduct subgroup comparisons and variables were considered significant between subgroups if the subgroup difference P value was less than 0.05. Publication bias was assessed by funnel plot and Egger’s regression test. We analyzed data using Stata version 16.0 (StataCorp, Texas, USA).
A total of 4844 records were searched from the three databases. 2484 duplicates were excluded. After reading titles and abstracts, we excluded 2264 reviews, RCT studies, duplicates and other studies meeting our exclude criteria. Among the 96 studies under full-text review, 41 studies were excluded (Fig. 1 ). Ultimately, with three grey literatures included, this final meta-analysis comprised 58 eligible studies, including 32 studies [ 14 , 15 , 17 , 18 , 19 , 20 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 ] for vaccine effectiveness and 26 studies [ 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 ] for vaccine safety. Characteristics of included studies are showed in Additional file 1 : Table S1, Additional file 2 : Table S2. The risk of bias of all studies we included was moderate or low.
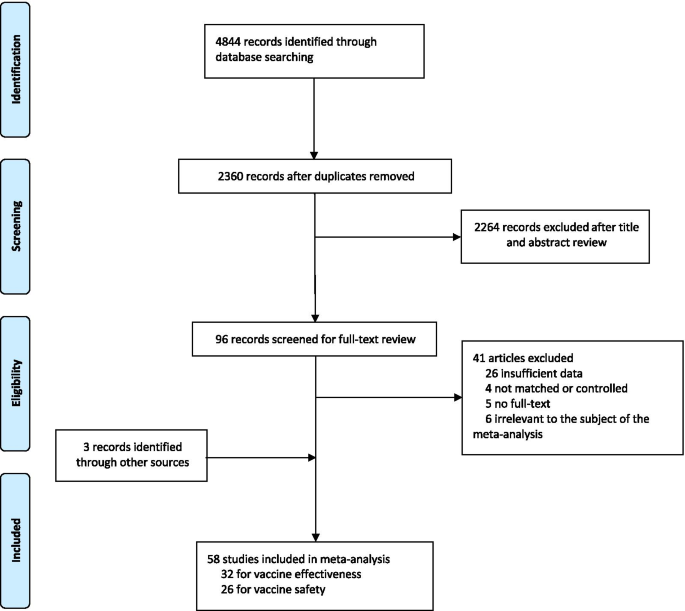
Flowchart of the study selection
Vaccine effectiveness for different clinical outcomes of COVID-19
We separately reported the vaccine effectiveness (VE) by the first and second dose of vaccines, and conducted subgroup analysis by the days after the first or second dose (< 7 days, ≥ 7 days, ≥ 14 days, and ≥ 21 days; studies with no specific days were classified as 1 dose, 2 dose or ≥ 1 dose).
For the first dose of SARS-CoV-2 vaccines, the pooled VE was 41% (95% CI : 28–54%) for the prevention of SARS-CoV-2 infection, 52% (95% CI : 31–73%) for the prevention of symptomatic COVID-19, 66% (95% CI : 50–81%) for the prevention of hospital admissions, 45% (95% CI : 42–49%) for the prevention of ICU admissions, and 53% (95% CI : 15–91%) for the prevention of COVID-19-related death (Table 1 ). The subgroup, ≥ 21 days after the first dose, was found to have the highest VE in each clinical outcome of COVID-19, regardless of ≥ 1 dose group (Table 1 ).
For the second dose of SARS-CoV-2 vaccines, the pooled VE was 85% (95% CI : 81–89%) for the prevention of SARS-CoV-2 infection, 97% (95% CI : 97–98%) for the prevention of symptomatic COVID-19, 93% (95% CI: 89–96%) for the prevention of hospital admissions, 96% (95% CI : 93–98%) for the prevention of ICU admissions, and 95% (95% CI : 92–98%) for the prevention of COVID-19-related death (Table 1 ). VE was 94% (95% CI : 78–98%) in ≥ 21 days after the second dose for the prevention of SARS-CoV-2 infection, higher than other subgroups, regardless of 2 dose group (Table 1 ). For the prevention of symptomatic COVID-19, VE was also relatively higher in 21 days after the second dose (99%, 95% CI : 94–100%). Subgroups showed no statistically significant differences in the prevention of hospital admissions, ICU admissions and COVID-19-related death (subgroup difference P values were 0.991, 0.414, and 0.851, respectively).
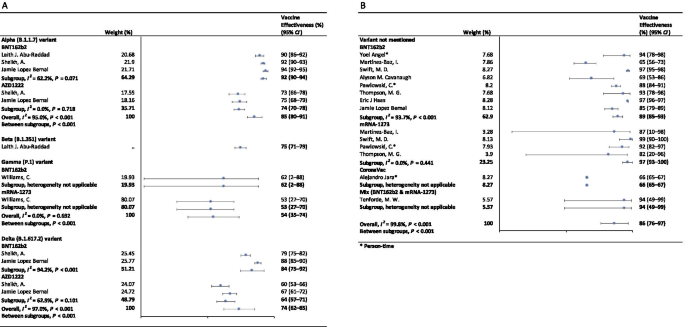
Vaccine effectiveness for different variants of SARS-CoV-2 in fully vaccinated people
In the fully vaccinated groups (over 14 days after the second dose), the pooled VE was 85% (95% CI: 80–91%) for the prevention of Alpha variant of SARS-CoV-2 infection, 54% (95% CI : 35–74%) for the Gamma variant, and 74% (95% CI : 62–85%) for the Delta variant. There was only one study [ 23 ] focused on the Beta variant, which showed the VE was 75% (95% CI : 71–79%) for the prevention of the Beta variant of SARS-CoV-2 infection. BNT162b2 vaccine had the highest VE in each variant group; 92% (95% CI : 90–94%) for the Alpha variant, 62% (95% CI : 2–88%) for the Gamma variant, and 84% (95% CI : 75–92%) for the Delta variant (Fig. 2 ).
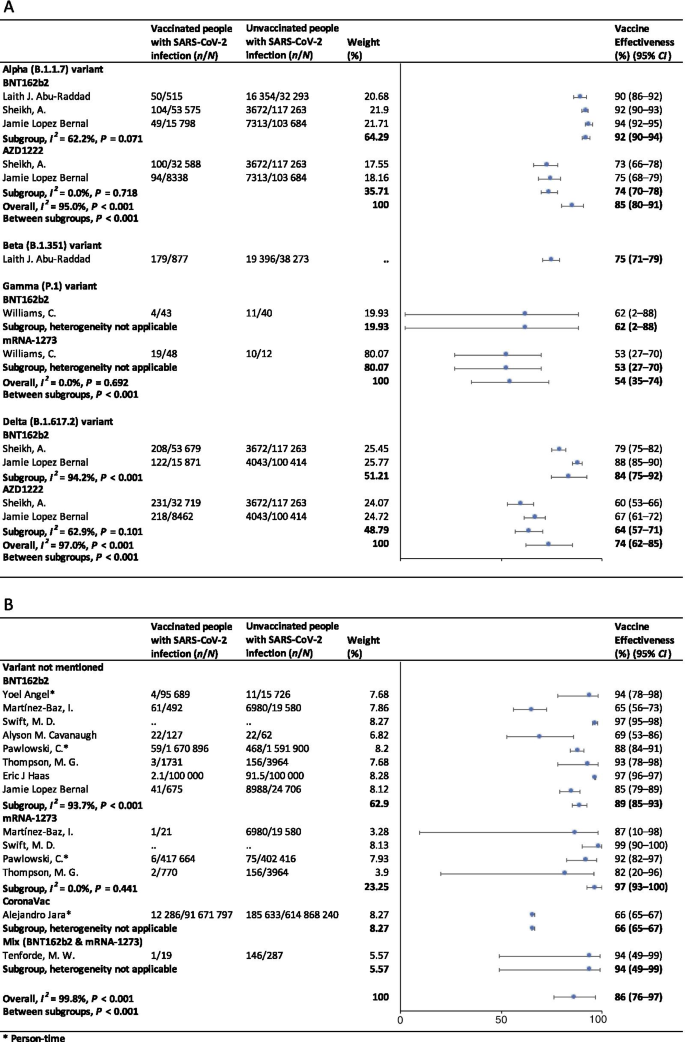
Forest plots for the vaccine effectiveness of SARS-CoV-2 vaccines in fully vaccinated populations. A Vaccine effectiveness against SARS-CoV-2 variants; B Vaccine effectiveness against SARS-CoV-2 with variants not mentioned. SARS-CoV-2 severe acute respiratory syndrome coronavirus 2, COVID-19 coronavirus disease 2019, CI confidence interval
For studies which had not mentioned the variant of SARS-CoV-2, the pooled VE was 86% (95% CI: 76–97%) for the prevention of SARS-CoV-2 infection in fully vaccinated people. mRNA-1273 vaccine had the highest pooled VE (97%, 95% CI: 93–100%, Fig. 2 ).
Safety of SARS-CoV-2 vaccines
As Table 2 showed, the incidence rate of adverse events varied widely among different studies. We conducted subgroup analysis by study population (general population, patients and healthcare workers), vaccine type (BNT162b2, mRNA-1273, CoronaVac, and et al.), and population size (< 1000, 1000–10 000, 10 000–100 000, and > 100 000). The overall pooled incidence rate was 1.5% (95% CI : 1.4–1.6%) for adverse events, 0.4 (95% CI : 0.2–0.5) per 10 000 for severe adverse events, and 0.1 (95% CI : 0.1–0.2) per 10 000 for death after vaccination. Incidence rate of adverse events was higher in healthcare workers (53.2%, 95% CI : 28.4–77.9%), AZD1222 vaccine group (79.6%, 95% CI : 60.8–98.3%), and < 1000 population size group (57.6%, 95% CI : 47.9–67.4%). Incidence rate of sever adverse events was higher in healthcare workers (127.2, 95% CI : 62.7–191.8, per 10 000), Gam-COVID-Vac vaccine group (175.7, 95% CI : 77.2–274.2, per 10 000), and 1000–10 000 population size group (336.6, 95% CI : 41.4–631.8, per 10 000). Incidence rate of death after vaccination was higher in patients (7.6, 95% CI : 0.0–32.2, per 10 000), BNT162b2 vaccine group (29.8, 95% CI : 0.0–71.2, per 10 000), and < 1000 population size group (29.8, 95% CI : 0.0–71.2, per 10 000). Subgroups of general population, vaccine type not mentioned, and > 100 000 population size had the lowest incidence rate of adverse events, severe adverse events, and death after vaccination.
Sensitivity analysis and publication bias
In the sensitivity analyses, VE for SARS-CoV-2 infections, symptomatic COVID-19 and COVID-19-related death got relatively lower when omitting over a single dose group of Maria et al.’s work [ 33 ]; when omitting ≥ 14 days after the first dose group and ≥ 14 days after the second dose group of Alejandro et al.’s work [ 14 ], VE for SARS-CoV-2 infections, hospitalization, ICU admission and COVID-19-related death got relatively higher; and VE for all clinical status of COVID-19 became lower when omitting ≥ 14 days after the second dose group of Eric et al.’s work [ 34 ]. Incidence rate of adverse events and severe adverse events got relatively higher when omitting China CDC’s data [ 74 ]. P values of Egger’s regression test for all the meta-analysis were more than 0.05, indicating that there might not be publication bias.
To our knowledge, this is a comprehensive systematic review and meta-analysis assessing the effectiveness and safety of SARS-CoV-2 vaccines based on real-world studies, reporting pooled VE for different variants of SARS-CoV-2 and incidence rate of adverse events. This meta-analysis comprised a total of 58 studies, including 32 studies for vaccine effectiveness and 26 studies for vaccine safety. We found that a single dose of SARS-CoV-2 vaccines was about 40–60% effective at preventing any clinical status of COVID-19 and that two doses were 85% or more effective. Although vaccines were not as effective against variants of SARS-CoV-2 as original virus, the vaccine effectiveness was still over 50% for fully vaccinated people. Normal adverse events were common, while the incidence of severe adverse events or even death was very low, providing reassurance to health care providers and to vaccine recipients and promote confidence in the safety of COVID-19 vaccines. Our findings strengthen and augment evidence from previous review [ 75 ], which confirmed the effectiveness of the BNT162b2 mRNA vaccine, and additionally reported the safety of SARS-CoV-2 vaccines, giving insight on the future of SARS-CoV-2 vaccine schedules.
Although most vaccines for the prevention of COVID-19 are two-dose vaccines, we found that the pooled VE of a single dose of SARS-CoV-2 vaccines was about 50%. Recent study showed that the T cell and antibody responses induced by a single dose of the BNT162b2 vaccine were comparable to those naturally infected with SARE-CoV-2 within weeks or months after infection [ 76 ]. Our findings could help to develop vaccination strategies under certain circumstances such as countries having a shortage of vaccines. In some countries, in order to administer the first dose to a larger population, the second dose was delayed for up to 12 weeks [ 77 ]. Some countries such as Canada had even decided to delay the second dose for 16 weeks [ 78 ]. However, due to a suboptimum immune response in those receiving only a single dose of a vaccine, such an approach had a chance to give rise to the emergence of variants of SARS-CoV-2 [ 79 ]. There remains a need for large clinical trials to assess the efficacy of a single-dose administration of two-dose vaccines and the risk of increasing the emergence of variants.
Two doses of SARS-CoV-2 vaccines were highly effective at preventing hospitalization, severe cases and deaths resulting from COVID-19, while the VE of different groups of days from the second vaccine dose showed no statistically significant differences. Our findings emphasized the importance of getting fully vaccinated, for the fact that most breakthrough infections were mild or asymptomatic. A recent study showed that the occurrence of breakthrough infections with SARS-CoV-2 in fully vaccinated populations was predictable with neutralizing antibody titers during the peri-infection period [ 80 ]. We also found getting fully vaccinated was at least 50% effective at preventing SARS-CoV-2 variants infections, despite reduced effectiveness compared with original virus; and BNT162b2 vaccine was found to have the highest VE in each variant group. Studies showed that the highly mutated variants were indicative of a form of rapid, multistage evolutionary jumps, which could preferentially occur in the milieu of partial immune control [ 81 , 82 ]. Therefore, immunocompromised patients should be prioritized for anti-COVID-19 immunization to mitigate persistent SARS-CoV-2 infections, during which multimutational SARS-CoV-2 variants could arise [ 83 ].
Recently, many countries, including Israel, the United States, China and the United Kingdom, have introduced a booster of COVID-19 vaccine, namely the third dose [ 84 , 85 , 86 , 87 ]. A study of Israel showed that among people vaccinated with BNT162b2 vaccine over 60 years, the risk of COVID-19 infection and severe illness in the non-booster group was 11.3 times (95% CI: 10.4–12.3) and 19.5 times (95% CI: 12.9–29.5) than the booster group, respectively [ 84 ]. Some studies have found that the third dose of Moderna, Pfizer-BioNTech, Oxford-AstraZeneca and Sinovac produced a spike in infection-blocking neutralizing antibodies when given a few months after the second dose [ 85 , 87 , 88 ]. In addition, the common adverse events associated with the third dose did not differ significantly from the symptoms of the first two doses, ranging from mild to moderate [ 85 ]. The overall incidence rate of local and systemic adverse events was 69% (57/97) and 20% (19/97) after receiving the third dose of BNT162b2 vaccine, respectively [ 88 ]. Results of a phase 3 clinical trial involving 306 people aged 18–55 years showed that adverse events after receiving a third dose of BNT162b2 vaccine (5–8 months after completion of two doses) were similar to those reported after receiving a second dose [ 85 ]. Based on V-safe, local reactions were more frequently after dose 3 (5323/6283; 84.7%) than dose 2 (5249/6283; 83.5%) among people who received 3 doses of Moderna. Systemic reactions were reported less frequently after dose 3 (4963/6283; 79.0%) than dose 2 (5105/6283; 81.3%) [ 86 ]. On August 4, WHO called for a halt to booster shots until at least the end of September to achieve an even distribution of the vaccine [ 89 ]. At this stage, the most important thing we should be thinking about is how to reach a global cover of people at risk with the first or second dose, rather than focusing on the third dose.
Based on real world studies, our results preliminarily showed that complete inoculation of COVID-19 vaccines was still effective against infection of variants, although the VE was generally diminished compared with the original virus. Particularly, the pooled VE was 54% (95% CI : 35–74%) for the Gamma variant, and 74% (95% CI : 62–85%) for the Delta variant. Since the wide spread of COVID-19, a number of variants have drawn extensive attention of international community, including Alpha variant (B.1.1.7), first identified in the United Kingdom; Beta variant (B.1.351) in South Africa; Gamma variant (P.1), initially appeared in Brazil; and the most infectious one to date, Delta variant (B.1.617.2) [ 90 ]. Israel recently reported a breakthrough infection of SARS-CoV-2, dominated by variant B.1.1.7 in a small number of fully vaccinated health care workers, raising concerns about the effectiveness of the original vaccine against those variants [ 80 ]. According to an observational cohort study in Qatar, VE of the BNT162b2 vaccine against the Alpha (B.1.1.7) and Beta (B.1.351) variants was 87% (95% CI : 81.8–90.7%) and 75.0% (95% CI : 70.5–7.9%), respectively [ 23 ]. Based on the National Immunization Management System of England, results from a recent real-world study of all the general population showed that the AZD1222 and BNT162b2 vaccines protected against symptomatic SARS-CoV-2 infection of Alpha variant with 74.5% (95% CI : 68.4–79.4%) and 93.7% (95% CI : 91.6–95.3%) [ 15 ]. In contrast, the VE against the Delta variant was 67.0% (95% CI : 61.3–71.8%) for two doses of AZD1222 vaccine and 88% (95% CI : 85.3–90.1%) for BNT162b2 vaccine [ 15 ].
In terms of adverse events after vaccination, the pooled incidence rate was very low, only 1.5% (95% CI : 1.4–1.6%). However, the prevalence of adverse events reported in large population (population size > 100 000) was much lower than that in small to medium population size. On the one hand, the vaccination population in the small to medium scale studies we included were mostly composed by health care workers, patients with specific diseases or the elderly. And these people are more concerned about their health and more sensitive to changes of themselves. But it remains to be proved whether patients or the elderly are more likely to have adverse events than the general. Mainstream vaccines currently on the market have maintained robust safety in specific populations such as cancer patients, organ transplant recipients, patients with rheumatic and musculoskeletal diseases, pregnant women and the elderly [ 54 , 91 , 92 , 93 , 94 ]. A prospective study by Tal Goshen-lag suggests that the safety of BNT162b2 vaccine in cancer patients is consistent with those previous reports [ 91 ]. In addition, the incidence rate of adverse events reported in the heart–lung transplant population is even lower than that in general population [ 95 ]. On the other hand, large scale studies at the national level are mostly based on national electronic health records or adverse event reporting systems, and it is likely that most mild or moderate symptoms are actually not reported.
Compared with the usual local adverse events (such as pain at the injection site, redness at the injection site, etc.) and normal systemic reactions (such as fatigue, myalgia, etc.), serious and life-threatening adverse events were rare due to our results. A meta-analysis based on RCTs only showed three cases of anaphylactic shock among 58 889 COVID-19 vaccine recipients and one in the placebo group [ 11 ]. The exact mechanisms underlying most of the adverse events are still unclear, accordingly we cannot establish a causal relation between severe adverse events and vaccination directly based on observational studies. In general, varying degrees of adverse events occur after different types of COVID-19 vaccination. Nevertheless, the benefits far outweigh the risks.
Our results showed the effectiveness and safety of different types of vaccines varied greatly. Regardless of SARS-CoV-2 variants, vaccine effectiveness varied from 66% (CoronaVac [ 14 ]) to 97% (mRNA-1273 [ 18 , 20 , 45 , 46 ]). The incidence rate of adverse events varied widely among different types of vaccines, which, however, could be explained by the sample size and population group of participants. BNT162b2, AZD1222, mRNA-1273 and CoronaVac were all found to have high vaccine efficacy and acceptable adverse-event profile in recent published studies [ 96 , 97 , 98 , 99 ]. A meta-analysis, focusing on the potential vaccine candidate which have reached to the phase 3 of clinical development, also found that although many of the vaccines caused more adverse events than the controls, most were mild, transient and manageable [ 100 ]. However, severe adverse events did occur, and there remains the need to implement a unified global surveillance system to monitor the adverse events of COVID-19 vaccines around the world [ 101 ]. A recent study employed a knowledge-based or rational strategy to perform a prioritization matrix of approved COVID-19 vaccines, and led to a scale with JANSSEN (Ad26.COV2.S) in the first place, and AZD1222, BNT162b2, and Sputnik V in second place, followed by BBIBP-CorV, CoronaVac and mRNA-1273 in third place [ 101 ]. Moreover, when deciding the priority of vaccines, the socioeconomic characteristics of each country should also be considered.
Our meta-analysis still has several limitations. First, we may include limited basic data on specific populations, as vaccination is slowly being promoted in populations under the age of 18 or over 60. Second, due to the limitation of the original real-world study, we did not conduct subgroup analysis based on more population characteristics, such as age. When analyzing the efficacy and safety of COVID-19 vaccine, we may have neglected the discussion on the heterogeneity from these sources. Third, most of the original studies only collected adverse events within 7 days after vaccination, which may limit the duration of follow-up for safety analysis.
Based on the real-world studies, SARS-CoV-2 vaccines have reassuring safety and could effectively reduce the death, severe cases, symptomatic cases, and infections resulting from SARS-CoV-2 across the world. In the context of global pandemic and the continuous emergence of SARS-CoV-2 variants, accelerating vaccination and improving vaccination coverage is still the most important and urgent matter, and it is also the final means to end the pandemic.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and its additional information files.
Abbreviations
Coronavirus disease 2019
Severe Acute Respiratory Syndrome Coronavirus 2
Vaccine effectiveness
Confidence intervals
Intensive care unit
Random clinical trials
Preferred reporting items for systematic reviews and meta-analyses
COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). 2021. https://coronavirus.jhu.edu/map.html . Accessed 20 Aug 2021.
Barranco R, Rocca G, Molinelli A, Ventura F. Controversies and challenges of mass vaccination against SARS-CoV-2 in Italy: medico-legal perspectives and considerations. Healthcare (Basel). 2021. https://doi.org/10.3390/healthcare9091163 .
Article Google Scholar
COVID-19 vaccine tracker. 2021. https://vac-lshtm.shinyapps.io/ncov_vaccine_landscape/ . Accessed 20 Aug 2021.
Coronavirus (COVID-19) Vaccinations. 2021. https://ourworldindata.org/covid-vaccinations . Accessed 20 Aug 2021.
Kirby T. New variant of SARS-CoV-2 in UK causes surge of COVID-19. Lancet Respir Med. 2021;9(2):e20–1. https://doi.org/10.1016/s2213-2600(21)00005-9 .
Article CAS PubMed PubMed Central Google Scholar
Callaway E. Fast-spreading COVID variant can elude immune responses. Nature. 2021;589(7843):500–1. https://doi.org/10.1038/d41586-021-00121-z .
Article CAS PubMed Google Scholar
Reardon S. How the Delta variant achieves its ultrafast spread. Nature. 2021. https://doi.org/10.1038/d41586-021-01986-w .
Article PubMed Google Scholar
Li R, Liu J, Zhang H. The challenge of emerging SARS-CoV-2 mutants to vaccine development. J Genet Genomics. 2021;48(2):102–6. https://doi.org/10.1016/j.jgg.2021.03.001 .
Article PubMed PubMed Central Google Scholar
Chen M, Yuan Y, Zhou Y, Deng Z, Zhao J, Feng F, Zou H, Sun C. Safety of SARS-CoV-2 vaccines: a systematic review and meta-analysis of randomized controlled trials. Infect Dis Poverty. 2021;10(1):94. https://doi.org/10.1186/s40249-021-00878-5 .
Ling Y, Zhong J, Luo J. Safety and effectiveness of SARS-CoV-2 vaccines: a systematic review and meta-analysis. J Med Virol. 2021. https://doi.org/10.1002/jmv.27203 .
Pormohammad A, Zarei M, Ghorbani S, Mohammadi M, Razizadeh MH, Turner DL, Turner RJ. Efficacy and safety of COVID-19 vaccines: a systematic review and meta-analysis of randomized clinical trials. Vaccines (Basel). 2021. https://doi.org/10.3390/vaccines9050467 .
Sathian B, Asim M, Banerjee I, Roy B, Pizarro AB, Mancha MA, van Teijlingen ER, Kord-Varkaneh H, Mekkodathil AA, Subramanya SH, et al. Development and implementation of a potential coronavirus disease 2019 (COVID-19) vaccine: a systematic review and meta-analysis of vaccine clinical trials. Nepal J Epidemiol. 2021;11(1):959–82. https://doi.org/10.3126/nje.v11i1.36163 .
Yuan P, Ai P, Liu Y, Ai Z, Wang Y, Cao W, Xia X, Zheng JC. Safety, tolerability, and immunogenicity of COVID-19 vaccines: a systematic review and meta-analysis. medRxiv. 2020. https://doi.org/10.1101/2020.11.03.20224998 .
Jara A, Undurraga EA, González C, Paredes F, Fontecilla T, Jara G, Pizarro A, Acevedo J, Leo K, Leon F, et al. Effectiveness of an inactivated SARS-CoV-2 vaccine in Chile. N Engl J Med. 2021. https://doi.org/10.1056/NEJMoa2107715 .
Lopez Bernal J, Andrews N, Gower C, Gallagher E, Simmons R, Thelwall S, Stowe J, Tessier E, Groves N, Dabrera G, et al. Effectiveness of COVID-19 vaccines against the B.1.617.2 (Delta) variant. N Engl J Med. 2021. https://doi.org/10.1056/NEJMoa2108891 .
Israel says Pfizer Covid vaccine is just 39% effective as delta spreads, but still prevents severe illness. 2021. https://www.cnbc.com/2021/07/23/delta-variant-pfizer-covid-vaccine-39percent-effective-in-israel-prevents-severe-illness.html . Accessed 20 Aug 2021.
Zacay G, Shasha D, Bareket R, Kadim I, Hershkowitz Sikron F, Tsamir J, Mossinson D, Heymann AD. BNT162b2 vaccine effectiveness in preventing asymptomatic infection with SARS-CoV-2 virus: a nationwide historical cohort study. Open Forum Infect Dis. 2021;8(6): ofab262. https://doi.org/10.1093/ofid/ofab262 .
Martínez-Baz I, Miqueleiz A, Casado I, Navascués A, Trobajo-Sanmartín C, Burgui C, Guevara M, Ezpeleta C, Castilla J. Effectiveness of COVID-19 vaccines in preventing SARS-CoV-2 infection and hospitalisation, Navarre, Spain, January to April 2021. Eurosurveillance. 2021. https://doi.org/10.2807/1560-7917.Es.2021.26.21.2100438 .
Tenforde MW, Olson SM, Self WH, Talbot HK, Lindsell CJ, Steingrub JS, Shapiro NI, Ginde AA, Douin DJ, Prekker ME, et al. Effectiveness of Pfizer-BioNTech and moderna vaccines against COVID-19 among hospitalized adults aged ≥65 years—United States, January–March 2021. MMWR Morb Mortal Wkly Rep. 2021;70(18):674–9. https://doi.org/10.15585/mmwr.mm7018e1 .
Pawlowski C, Lenehan P, Puranik A, Agarwal V, Venkatakrishnan AJ, Niesen MJM, O’Horo JC, Virk A, Swift MD, Badley AD, et al. FDA-authorized mRNA COVID-19 vaccines are effective per real-world evidence synthesized across a multi-state health system. Med (N Y). 2021. https://doi.org/10.1016/j.medj.2021.06.007 .
Wells G, Shea B, O'Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp . Accessed 20 Aug 2021.
Rostom A, Dubé C, Cranney A, et al. Celiac Disease. Rockville (MD): Agency for Healthcare Research and Quality (US); 2004 Sep. (Evidence Reports/Technology Assessments, No. 104.) Appendix D. Quality Assessment Forms. Available from: https://www.ncbi.nlm.nih.gov/books/NBK35156/ . Accessed 20 Aug 2021
Abu-Raddad LJ, Chemaitelly H, Butt AA. Effectiveness of the BNT162b2 COVID-19 vaccine against the B.1.1.7 and B.1.351 Variants. N Engl J Med. 2021;385(2):187–9. https://doi.org/10.1056/NEJMc2104974 .
Angel Y, Spitzer A, Henig O, Saiag E, Sprecher E, Padova H, Ben-Ami R. Association between vaccination with BNT162b2 and incidence of symptomatic and asymptomatic SARS-CoV-2 infections among health care workers. JAMA. 2021;325(24):2457–65. https://doi.org/10.1001/jama.2021.7152 .
Azamgarhi T, Hodgkinson M, Shah A, Skinner JA, Hauptmannova I, Briggs TWR, Warren S. BNT162b2 vaccine uptake and effectiveness in UK healthcare workers—a single centre cohort study. Nat Commun. 2021;12(1):3698. https://doi.org/10.1038/s41467-021-23927-x .
Bianchi FP, Germinario CA, Migliore G, Vimercati L, Martinelli A, Lobifaro A, Tafuri S, Stefanizzi P. BNT162b2 mRNA COVID-19 vaccine effectiveness in the prevention of SARS-CoV-2 infection: a preliminary report. J Infect Dis. 2021. https://doi.org/10.1093/infdis/jiab262 .
Britton A, Jacobs Slifka KM, Edens C, Nanduri SA, Bart SM, Shang N, Harizaj A, Armstrong J, Xu K, Ehrlich HY, et al. Effectiveness of the Pfizer-BioNTech COVID-19 vaccine among residents of two skilled nursing facilities experiencing COVID-19 outbreaks—Connecticut, December 2020–February 2021. MMWR Morb Mortal Wkly Rep. 2021;70(11):396–401. https://doi.org/10.15585/mmwr.mm7011e3 .
Cavanaugh AM, Fortier S, Lewis P, Arora V, Johnson M, George K, Tobias J, Lunn S, Miller T, Thoroughman D, et al. COVID-19 outbreak associated with a SARS-CoV-2 R1 lineage variant in a skilled nursing facility after vaccination program—Kentucky, March 2021. MMWR Morb Mortal Wkly Rep. 2021;70(17):639–43. https://doi.org/10.15585/mmwr.mm7017e2 .
Chemaitelly H, Yassine HM, Benslimane FM, Al Khatib HA, Tang P, Hasan MR, Malek JA, Coyle P, Ayoub HH, Al Kanaani Z, et al. mRNA-1273 COVID-19 vaccine effectiveness against the B.1.1.7 and B.1.351 variants and severe COVID-19 disease in Qatar. Nat Med. 2021. https://doi.org/10.1038/s41591-021-01446-y .
Chodick G, Tene L, Patalon T, Gazit S, Ben Tov A, Cohen D, Muhsen K. Assessment of effectiveness of 1 dose of BNT162b2 vaccine for SARS-CoV-2 infection 13 to 24 days after immunization. JAMA Netw Open. 2021;4(6): e2115985. https://doi.org/10.1001/jamanetworkopen.2021.15985 .
Chodick G, Tene L, Rotem RS, Patalon T, Gazit S, Ben-Tov A, Weil C, Goldshtein I, Twig G, Cohen D, et al. The effectiveness of the TWO-DOSE BNT162b2 vaccine: analysis of real-world data. Clin Infect Dis. 2021. https://doi.org/10.1093/cid/ciab438 .
Dagan N, Barda N, Kepten E, Miron O, Perchik S, Katz MA, Hernán MA, Lipsitch M, Reis B, Balicer RD. BNT162b2 mRNA COVID-19 vaccine in a nationwide mass vaccination setting. N Engl J Med. 2021;384(15):1412–23. https://doi.org/10.1056/NEJMoa2101765 .
Flacco ME, Soldato G, Acuti Martellucci C, Carota R, Di Luzio R, Caponetti A, Manzoli L. Interim estimates of COVID-19 vaccine effectiveness in a mass vaccination setting: data from an Italian Province. VacCInes (Basel). 2021. https://doi.org/10.3390/vaccines9060628 .
Haas EJ, Angulo FJ, McLaughlin JM, Anis E, Singer SR, Khan F, Brooks N, Smaja M, Mircus G, Pan K, et al. Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel: an observational study using national surveillance data. Lancet. 2021;397(10287):1819–29. https://doi.org/10.1016/s0140-6736(21)00947-8 .
Hall VJ, Foulkes S, Saei A, Andrews N, Oguti B, Charlett A, Wellington E, Stowe J, Gillson N, Atti A, et al. COVID-19 vaccine coverage in health-care workers in England and effectiveness of BNT162b2 mRNA vaccine against infection (SIREN): a prospective, multicentre, cohort study. Lancet. 2021;397(10286):1725–35. https://doi.org/10.1016/s0140-6736(21)00790-x .
Hyams C, Marlow R, Maseko Z, King J, Ward L, Fox K, Heath R, Tuner A, Friedrich Z, Morrison L, et al. Effectiveness of BNT162b2 and ChAdOx1 nCoV-19 COVID-19 vaccination at preventing hospitalisations in people aged at least 80 years: a test-negative, case-control study. Lancet Infect Dis. 2021. https://doi.org/10.1016/s1473-3099(21)00330-3 .
Khan N, Mahmud N. Effectiveness of SARS-CoV-2 vaccination in a veterans affairs cohort of patients with inflammatory bowel disease with diverse exposure to immunosuppressive medications. Gastroenterology. 2021. https://doi.org/10.1053/j.gastro.2021.05.044 .
Knobel P, Serra C, Grau S, Ibañez R, Diaz P, Ferrández O, Villar R, Lopez AF, Pujolar N, Horcajada JP, et al. COVID-19 mRNA vaccine effectiveness in asymptomatic healthcare workers. Infect Control Hosp Epidemiol. 2021. https://doi.org/10.1017/ice.2021.287 .
Lopez Bernal J, Andrews N, Gower C, Robertson C, Stowe J, Tessier E, Simmons R, Cottrell S, Roberts R, O’Doherty M, et al. Effectiveness of the Pfizer-BioNTech and Oxford-AstraZeneca vaccines on covid-19 related symptoms, hospital admissions, and mortality in older adults in England: test negative case-control study. BMJ. 2021;373: n1088. https://doi.org/10.1136/bmj.n1088 .
Mazagatos C, Monge S, Olmedo C, Vega L, Gallego P, Martín-Merino E, Sierra MJ, Limia A, Larrauri A. Effectiveness of mRNA COVID-19 vaccines in preventing SARS-CoV-2 infections and COVID-19 hospitalisations and deaths in elderly long-term care facility residents, Spain, weeks 53, 2020 to 13 2021. Eurosurveillance. 2021. https://doi.org/10.2807/1560-7917.Es.2021.26.24.2100452 .
Pilishvili T, Fleming-Dutra KE, Farrar JL, Gierke R, Mohr NM, Talan DA, Krishnadasan A, Harland KK, Smithline HA, Hou PC, et al. Interim estimates of vaccine effectiveness of Pfizer-BioNTech and Moderna COVID-19 vaccines among health care personnel—33 US Sites, January–March 2021. MMWR Morb Mortal Wkly Rep. 2021;70(20):753–8. https://doi.org/10.15585/mmwr.mm7020e2 .
Sheikh A, McMenamin J, Taylor B, Robertson C. SARS-CoV-2 Delta VOC in Scotland: demographics, risk of hospital admission, and vaccine effectiveness. Lancet. 2021;397(10293):2461–2. https://doi.org/10.1016/s0140-6736(21)01358-1 .
Shrotri M, Krutikov M, Palmer T, Giddings R, Azmi B, Subbarao S, Fuller C, Irwin-Singer A, Davies D, Tut G, et al. Vaccine effectiveness of the first dose of ChAdOx1 nCoV-19 and BNT162b2 against SARS-CoV-2 infection in residents of long-term care facilities in England (VIVALDI): a prospective cohort study. Lancet Infect Dis. 2021. https://doi.org/10.1016/s1473-3099(21)00289-9 .
Skowronski DM, Setayeshgar S, Zou M, Prystajecky N, Tyson JR, Galanis E, Naus M, Patrick DM, Sbihi H, El Adam S, et al. Single-dose mRNA vaccine effectiveness against SARS-CoV-2, including Alpha and Gamma variants: a test-negative design in adults 70 years and older in British Columbia,Canada. Clin Infect Dis. 2021. https://doi.org/10.1093/cid/ciab616 .
Swift MD, Breeher LE, Tande AJ, Tommaso CP, Hainy CM, Chu H, Murad MH, Berbari EF, Virk A. Effectiveness of mRNA COVID-19 vaccines against SARS-CoV-2 infection in a cohort of healthcare personnel. Clin Infect Dis. 2021. https://doi.org/10.1093/cid/ciab361 .
Thompson MG, Burgess JL, Naleway AL, Tyner H, Yoon SK, Meece J, Olsho LEW, Caban-Martinez AJ, Fowlkes AL, Lutrick K, et al. Prevention and attenuation of COVID-19 with the BNT162b2 and mRNA-1273 Vaccines. N Engl J Med. 2021. https://doi.org/10.1056/NEJMoa2107058 .
Vasileiou E, Simpson CR, Shi T, Kerr S, Agrawal U, Akbari A, Bedston S, Beggs J, Bradley D, Chuter A, et al. Interim findings from first-dose mass COVID-19 vaccination roll-out and COVID-19 hospital admissions in Scotland: a national prospective cohort study. Lancet. 2021;397(10285):1646–57. https://doi.org/10.1016/s0140-6736(21)00677-2 .
Williams C, Al-Bargash D, Macalintal C, Stuart R, Seth A, Latham J, Gitterman L, Fedsin S, Godoy M, Kozak R, et al. COVID-19 outbreak associated with a SARS-CoV-2 P.1 lineage in a long-term care home after implementation of a vaccination program—Ontario, April–May 2021. Clin Infect Dis. 2021. https://doi.org/10.1093/cid/ciab617 .
Alhazmi A, Alamer E, Daws D, Hakami M, Darraj M, Abdelwahab S, Maghfuri A, Algaissi A. Evaluation of side effects associated with COVID-19 vaccines in Saudi Arabia. Vaccines (Basel). 2021. https://doi.org/10.3390/vaccines9060674 .
Andrzejczak-Grządko S, Czudy Z, Donderska M. Side effects after COVID-19 vaccinations among residents of Poland. Eur Rev Med Pharmacol Sci. 2021;25(12):4418–21. https://doi.org/10.26355/eurrev_202106_26153 .
Baldolli A, Michon J, Appia F, Galimard C, Verdon R, Parienti JJ. Tolerance of BNT162b2 mRNA COVI-19 vaccine in patients with a medical history of COVID-19 disease: a case control study. Vaccine. 2021;39(32):4410–3. https://doi.org/10.1016/j.vaccine.2021.06.054 .
Cherian S, Paul A, Ahmed S, Alias B, Manoj M, Santhosh AK, Varghese DR, Krishnan N, Shenoy P. Safety of the ChAdOx1 nCoV-19 and the BBV152 vaccines in 724 patients with rheumatic diseases: a post-vaccination cross-sectional survey. Rheumatol Int. 2021;41(8):1441–5. https://doi.org/10.1007/s00296-021-04917-0 .
Chevallier P, Coste-Burel M, Le Bourgeois A, Peterlin P, Garnier A, Béné MC, Imbert BM, Drumel T, Le Gouill S, Moreau P, et al. Safety and immunogenicity of a first dose of SARS-CoV-2 mRNA vaccine in allogeneic hematopoietic stem-cells recipients. EJHaem. 2021. https://doi.org/10.1002/jha2.242 .
Connolly CM, Ruddy JA, Boyarsky BJ, Avery RK, Werbel WA, Segev DL, Garonzik-Wang J, Paik JJ. Safety of the first dose of mRNA SARS-CoV-2 vaccines in patients with rheumatic and musculoskeletal diseases. Ann Rheum Dis. 2021. https://doi.org/10.1136/annrheumdis-2021-220231 .
Furer V, Eviatar T, Zisman D, Peleg H, Paran D, Levartovsky D, Zisapel M, Elalouf O, Kaufman I, Meidan R, et al. Immunogenicity and safety of the BNT162b2 mRNA COVID-19 vaccine in adult patients with autoimmune inflammatory rheumatic diseases and in the general population: a multicentre study. Ann Rheum Dis. 2021. https://doi.org/10.1136/annrheumdis-2021-220647 .
Gee J, Marquez P, Su J, Calvert GM, Liu R, Myers T, Nair N, Martin S, Clark T, Markowitz L, et al. First month of COVID-19 vaccine safety monitoring—United States, December 14, 2020–January 13, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(8):283–8. https://doi.org/10.15585/mmwr.mm7008e3 .
Hashimoto T, Ozaki A, Bhandari D, Sawano T, Sah R, Tanimoto T. High anaphylaxis rates following vaccination with the Pfizer BNT162b2 mRNA vaccine against COVID-19 in Japanese health care workers; a secondary analysis of initial post-approval safety data. J Travel Med. 2021. https://doi.org/10.1093/jtm/taab090 .
Lv G, Yuan J, Xiong X, Li M. Mortality rate and characteristics of deaths following COVID-19 vaccination. Front Med (Lausanne). 2021;8: 670370. https://doi.org/10.3389/fmed.2021.670370 .
McMurry R, Lenehan P, Awasthi S, Silvert E, Puranik A, Pawlowski C, Venkatakrishnan AJ, Anand P, Agarwal V, O’Horo JC, et al. Real-time analysis of a mass vaccination effort confirms the safety of FDA-authorized mRNA COVID-19 vaccines. Med (N Y). 2021. https://doi.org/10.1016/j.medj.2021.06.006 .
Monin L, Laing AG, Muñoz-Ruiz M, McKenzie DR, Del Molino Del Barrio I, Alaguthurai T, Domingo-Vila C, Hayday TS, Graham C, Seow J, et al. Safety and immunogenicity of one versus two doses of the COVID-19 vaccine BNT162b2 for patients with cancer: interim analysis of a prospective observational study. Lancet Oncol. 2021;22(6):765–78. https://doi.org/10.1016/s1470-2045(21)00213-8 .
Pagotto V, Ferloni A, Mercedes Soriano M, Díaz M, Braguinsky Golde N, González MI, Asprea V, Staneloni MI, Zingoni P, Vidal G, et al. Active monitoring of early safety of Sputnik V vaccine in Buenos Aires, Argentina. MediCIna (B Aires). 2021;81(3):408–14.
Google Scholar
Peled Y, Ram E, Lavee J, Sternik L, Segev A, Wieder-Finesod A, Mandelboim M, Indenbaum V, Levy I, Raanani E, et al. BNT162b2 vaccination in heart transplant recipients: Clinical experience and antibody response. J Heart Lung Transplant. 2021. https://doi.org/10.1016/j.healun.2021.04.003 .
Quiroga B, Sánchez-Álvarez E, Goicoechea M, de Sequera P. COVID-19 vaccination among Spanish nephrologists: acceptance and side effects. J Healthc Qual Res. 2021. https://doi.org/10.1016/j.jhqr.2021.05.002 .
Ram R, Hagin D, Kikozashvilli N, Freund T, Amit O, Bar-On Y, Beyar-Katz O, Shefer G, Moshiashvili MM, Karni C, et al. Safety and immunogenicity of the BNT162b2 mRNA COVID-19 vaccine in patients after allogeneic HCT or CD19-based CART therapy—a single center prospective cohort study. Transplant Cell Ther. 2021. https://doi.org/10.1016/j.jtct.2021.06.024 .
Revon-Riviere G, Ninove L, Min V, Rome A, Coze C, Verschuur A, de Lamballerie X, André N. The BNT162b2 mRNA COVID-19 vaccine in adolescents and young adults with cancer: a monocentric experience. Eur J Cancer. 2021;154:30–4. https://doi.org/10.1016/j.ejca.2021.06.002 .
Riad A, Pokorná A, Mekhemar M, Conrad J, Klugarová J, Koščík M, Klugar M, Attia S. Safety of ChAdOx1 nCoV-19 vaccine: independent evidence from two EU states. Vaccines (Basel). 2021. https://doi.org/10.3390/vaccines9060673 .
Riad A, Sağıroğlu D, Üstün B, Pokorná A, Klugarová J, Attia S, Klugar M. Prevalence and risk factors of CoronaVac Side effects: an independent cross-sectional study among healthcare workers in Turkey. J Clin Med. 2021. https://doi.org/10.3390/jcm10122629 .
Rosman Y, Lavi N, Meir-Shafrir K, Lachover-Roth I, Cohen-Engler A, Mekori YA, Confino-Cohen R. Safety of BNT162b2 mRNA COVID-19 vaccine in patients with mast cell disorders. J Allergy Clin Immunol Pract. 2021. https://doi.org/10.1016/j.jaip.2021.06.032 .
Signorelli C, Odone A, Gianfredi V, Capraro M, Kacerik E, Chiecca G, Scardoni A, Minerva M, Mantecca R, Musarò P, et al. Application of the “immunization islands” model to improve quality, efficiency and safety of a COVID-19 mass vaccination site. Ann Ig. 2021;33(5):499–512. https://doi.org/10.7416/ai.2021.2456 .
Vallée A, Chan-Hew-Wai A, Bonan B, Lesprit P, Parquin F, Catherinot É, Choucair J, Billard D, Amiel-Taieb C, Camps È, et al. Oxford-AstraZeneca COVID-19 vaccine: need of a reasoned and effective vaccine campaign. Public Health. 2021;196:135–7. https://doi.org/10.1016/j.puhe.2021.05.030 .
Wang J, Hou Z, Liu J, Gu Y, Wu Y, Chen Z, Ji J, Diao S, Qiu Y, Zou S, et al. Safety and immunogenicity of COVID-19 vaccination in patients with non-alcoholic fatty liver disease (CHESS2101): a multicenter study. J Hepatol. 2021. https://doi.org/10.1016/j.jhep.2021.04.026 .
Zhang MX, Zhang TT, Shi GF, Cheng FM, Zheng YM, Tung TH, Chen HX. Safety of an inactivated SARS-CoV-2 vaccine among healthcare workers in China. Expert Rev Vaccines. 2021. https://doi.org/10.1080/14760584.2021.1925112 .
Shay DK, Gee J, Su JR, Myers TR, Marquez P, Liu R, Zhang B, Licata C, Clark TA, Shimabukuro TT. Safety monitoring of the Janssen (Johnson & Johnson) COVID-19 Vaccine—United States, March–April 2021. MMWR Morb Mortal Wkly Rep. 2021;70(18):680–4. https://doi.org/10.15585/mmwr.mm7018e2 .
Prevention CCfDCa. Information analysis of COVID-19 vaccine adverse reaction monitoring in China. 2021-5-28. http://www.chinacdc.cn/jkzt/ymyjz/ymyjjz_6758/202105/t20210528_230908.html . Accessed 20 Aug 2021.
Kow CS, Hasan SS. Real-world effectiveness of BNT162b2 mRNA vaccine: a meta-analysis of large observational studies. Inflammopharmacology. 2021;29(4):1075–90. https://doi.org/10.1007/s10787-021-00839-2 .
Angyal A, Longet S, Moore S, Payne RP, Harding A et al. T-Cell and Antibody Responses to First BNT162b2 Vaccine Dose in Previously SARS-CoV-2-Infected and Infection-Naive UK Healthcare Workers: A Multicentre, Prospective, Observational Cohort Study. Available at SSRN: https://ssrn.com/abstract=3820576 or https://doi.org/10.2139/ssrn.3820576 . Accessed 20 Aug 2021.
Pimenta D, Yates C, Pagel C, Gurdasani D. Delaying the second dose of covid-19 vaccines. BMJ. 2021;372: n710. https://doi.org/10.1136/bmj.n710 .
Tauh T, Mozel M, Meyler P, Lee SM. An updated look at the 16-week window between doses of vaccines in BC for COVID-19. BC Med J. 2021;63(3):102–3.
Kadire SR, Wachter RM, Lurie N. Delayed second dose versus standard regimen for COVID-19 vaccination. N Engl J Med. 2021;384(9): e28. https://doi.org/10.1056/NEJMclde2101987 .
Bergwerk M, Gonen T, Lustig Y, Amit S, Lipsitch M, Cohen C, Mandelboim M, Gal Levin E, Rubin C, Indenbaum V, et al. COVID-19 breakthrough infections in vaccinated health care workers. N Engl J Med. 2021. https://doi.org/10.1056/NEJMoa2109072 .
Truong TT, Ryutov A, Pandey U, Yee R, Goldberg L, Bhojwani D, Aguayo-Hiraldo P, Pinsky BA, Pekosz A, Shen L, et al. Persistent SARS-CoV-2 infection and increasing viral variants in children and young adults with impaired humoral immunity. medRxiv. 2021. https://doi.org/10.1101/2021.02.27.21252099 .
Choi B, Choudhary MC, Regan J, Sparks JA, Padera RF, Qiu X, Solomon IH, Kuo HH, Boucau J, Bowman K, et al. Persistence and evolution of SARS-CoV-2 in an Immunocompromised Host. N Engl J Med. 2020;383(23):2291–3. https://doi.org/10.1056/NEJMc2031364 .
Corey L, Beyrer C, Cohen MS, Michael NL, Bedford T, Rolland M. SARS-CoV-2 variants in patients with immunosuppression. N Engl J Med. 2021;385(6):562–6. https://doi.org/10.1056/NEJMsb2104756 .
Bar-On YM, Goldberg Y, Mandel M, Bodenheimer O, Freedman L, Kalkstein N, Mizrahi B, Alroy-Preis S, Ash N, Milo R, et al. Protection of BNT162b2 vaccine booster against Covid-19 in Israel. N Engl J Med. 2021;385(15):1393–400. https://doi.org/10.1056/NEJMoa2114255 .
Hause AM, Baggs J, Gee J, Marquez P, Myers TR, Shimabukuro TT, Shay DK. Safety monitoring of an additional dose of COVID-19 vaccine—United States, August 12–September 19, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(39):1379–84. https://doi.org/10.15585/mmwr.mm7039e4 .
Furlow B. Immunocompromised patients in the USA and UK should receive third dose of COVID-19 vaccine. Lancet Rheumatol. 2021. https://doi.org/10.1016/s2665-9913(21)00313-1 .
Flaxman A, Marchevsky NG, Jenkin D, Aboagye J, Aley PK, Angus B, Belij-Rammerstorfer S, Bibi S, Bittaye M, Cappuccini F, et al. Reactogenicity and immunogenicity after a late second dose or a third dose of ChAdOx1 nCoV-19 in the UK: a substudy of two randomised controlled trials (COV001 and COV002). Lancet. 2021;398(10304):981–90. https://doi.org/10.1016/s0140-6736(21)01699-8 .
Peled Y, Ram E, Lavee J, Segev A, Matezki S, Wieder-Finesod A, Halperin R, Mandelboim M, Indenbaum V, Levy I, et al. Third dose of the BNT162b2 vaccine in heart transplant recipients: immunogenicity and clinical experience. J Heart Lung Transplant. 2021. https://doi.org/10.1016/j.healun.2021.08.010 .
WHO. WHO press conference on coronavirus disease (COVID-19)—4 August 2021. 2021. https://www.who.int/multi-media/details/who-press-conference-on-coronavirus-disease-(covid-19)---4-august-2021 . Accessed 20 Aug 2021.
Cascella M, Rajnik M, Aleem A, Dulebohn SC, Di Napoli R. Features, evaluation, and treatment of coronavirus (COVID-19). In: StatPearls. edn. Treasure Island (FL): StatPearls Publishing Copyright © 2021, StatPearls Publishing LLC.; 2021.
Goshen-Lago T, Waldhorn I, Holland R, Szwarcwort-Cohen M, Reiner-Benaim A, Shachor-Meyouhas Y, Hussein K, Fahoum L, Baruch M, Peer A, et al. Serologic status and toxic effects of the SARS-CoV-2 BNT162b2 vaccine in patients undergoing treatment for cancer. JAMA Oncol. 2021. https://doi.org/10.1001/jamaoncol.2021.2675 .
Ou MT, Boyarsky BJ, Motter JD, Greenberg RS, Teles AT, Ruddy JA, Krach MR, Jain VS, Werbel WA, Avery RK, et al. Safety and reactogenicity of 2 doses of SARS-CoV-2 vaccination in solid organ transplant recipients. Transplantation. 2021. https://doi.org/10.1097/tp.0000000000003780 .
Bookstein Peretz S, Regev N, Novick L, Nachshol M, Goffer E, Ben-David A, Asraf K, Doolman R, Sapir E, Regev Yochay G, et al. Short-term outcome of pregnant women vaccinated by BNT162b2 mRNA COVID-19 vaccine. Ultrasound Obstet Gynecol. 2021. https://doi.org/10.1002/uog.23729 .
Shimabukuro TT, Kim SY, Myers TR, Moro PL, Oduyebo T, Panagiotakopoulos L, Marquez PL, Olson CK, Liu R, Chang KT, et al. Preliminary findings of mRNA COVID-19 vaccine safety in pregnant persons. N Engl J Med. 2021;384(24):2273–82. https://doi.org/10.1056/NEJMoa2104983 .
Peled Y, Ram E, Lavee J, Sternik L, Segev A, Wieder-Finesod A, Mandelboim M, Indenbaum V, Levy I, Raanani E, et al. BNT162b2 vaccination in heart transplant recipients: clinical experience and antibody response. J Heart Lung Transplant. 2021;40(8):759–62. https://doi.org/10.1016/j.healun.2021.04.003 .
Thomas SJ, Moreira ED Jr, Kitchin N, Absalon J, Gurtman A, Lockhart S, Perez JL, Pérez Marc G, Polack FP, Zerbini C, et al. Safety and efficacy of the BNT162b2 mRNA COVID-19 vaccine through 6 months. N Engl J Med. 2021. https://doi.org/10.1056/NEJMoa2110345 .
Falsey AR, Sobieszczyk ME, Hirsch I, Sproule S, Robb ML, Corey L, Neuzil KM, Hahn W, Hunt J, Mulligan MJ, et al. Phase 3 safety and efficacy of AZD1222 (ChAdOx1 nCoV-19) COVID-19 vaccine. N Engl J Med. 2021. https://doi.org/10.1056/NEJMoa2105290 .
El Sahly HM, Baden LR, Essink B, Doblecki-Lewis S, Martin JM, Anderson EJ, Campbell TB, Clark J, Jackson LA, Fichtenbaum CJ, et al. Efficacy of the mRNA-1273 SARS-CoV-2 vaccine at completion of blinded phase. N Engl J Med. 2021. https://doi.org/10.1056/NEJMoa2113017 .
Tanriover MD, Doğanay HL, Akova M, Güner HR, Azap A, Akhan S, Köse Ş, Erdinç F, Akalın EH, Tabak ÖF, et al. Efficacy and safety of an inactivated whole-virion SARS-CoV-2 vaccine (CoronaVac): interim results of a double-blind, randomised, placebo-controlled, phase 3 trial in Turkey. Lancet. 2021;398(10296):213–22. https://doi.org/10.1016/s0140-6736(21)01429-x .
Kumar S, Saurabh MK, Maharshi V. Efficacy and safety of potential vaccine candidates against coronavirus disease 2019: a systematic review. J Adv Pharm Technol Res. 2021;12(3):215–21. https://doi.org/10.4103/japtr.JAPTR_229_20 .
Burgos-Salcedo J. A rational strategy to support approved COVID-19 vaccines prioritization. Hum Vaccin Immunother. 2021;17(10):3474–7. https://doi.org/10.1080/21645515.2021.1922060 .
Download references
Acknowledgements
This study was funded by the National Natural Science Foundation of China (72122001; 71934002) and the National Science and Technology Key Projects on Prevention and Treatment of Major infectious disease of China (2020ZX10001002). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the paper. No payment was received by any of the co-authors for the preparation of this article.
Author information
Qiao Liu and Chenyuan Qin are joint first authors
Authors and Affiliations
Department of Epidemiology and Biostatistics, School of Public Health, Peking University, Beijing, 100191, China
Qiao Liu, Chenyuan Qin, Min Liu & Jue Liu
Institute for Global Health and Development, Peking University, Beijing, 100871, China
Chenyuan Qin & Jue Liu
You can also search for this author in PubMed Google Scholar
Contributions
LQ and QCY contributed equally as first authors. LJ and LM contributed equally as correspondence authors. LJ and LM conceived and designed the study; LQ, QCY and LJ carried out the literature searches, extracted the data, and assessed the study quality; LQ and QCY performed the statistical analysis and wrote the manuscript; LJ, LM, LQ and QCY revised the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Correspondence to Min Liu or Jue Liu .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Supplementary Information
Additional file 1: table s1..
Characteristic of studies included for vaccine effectiveness.
Additional file 2: Table S2.
Characteristic of studies included for vaccine safety.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Liu, Q., Qin, C., Liu, M. et al. Effectiveness and safety of SARS-CoV-2 vaccine in real-world studies: a systematic review and meta-analysis. Infect Dis Poverty 10 , 132 (2021). https://doi.org/10.1186/s40249-021-00915-3
Download citation
Received : 07 September 2021
Accepted : 01 November 2021
Published : 14 November 2021
DOI : https://doi.org/10.1186/s40249-021-00915-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Effectiveness
- Meta-analysis
Infectious Diseases of Poverty
ISSN: 2049-9957
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
COVID-19 vaccines: Immune correlates and clinical outcomes
Affiliations.
- 1 Center for Virology and Vaccine Research, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA, USA.
- 2 Department of Medicine, Tufts University School of Medicine, Boston, MA, USA.
- 3 Division of Infectious Diseases, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA.
- 4 Department of Medicine, Harvard Medical School, Boston, MA, USA.
- 5 Ragon Institute of MGH, MIT and Harvard, Cambridge, MA, USA.
- PMID: 38517241
- PMCID: PMC10962618
- DOI: 10.1080/21645515.2024.2324549
Severe disease due to COVID-19 has declined dramatically as a result of widespread vaccination and natural immunity in the population. With the emergence of SARS-CoV-2 variants that largely escape vaccine-elicited neutralizing antibody responses, the efficacy of the original vaccines has waned and has required vaccine updating and boosting. Nevertheless, hospitalizations and deaths due to COVID-19 have remained low. In this review, we summarize current knowledge of immune responses that contribute to population immunity and the mechanisms how vaccines attenuate COVID-19 disease severity.
Keywords: COVID-19; SARS-CoV-2 variants; T-cells; immune correlates; mucosal immunity; vaccines.
Publication types
- Antibodies, Neutralizing
- Antibodies, Viral
- COVID-19 Vaccines*
- COVID-19* / prevention & control
- Vaccination
- COVID-19 Vaccines
Supplementary concepts
- SARS-CoV-2 variants
Grants and funding
Promoting Public Health with Blunt Instruments: Evidence from Vaccine Mandates
We study the effect of mandates requiring COVID-19 vaccination among healthcare industry workers adopted in 2021 in the United States. There are long-standing worker shortages in the U.S. healthcare industry, pre-dating the COVID-19 pandemic. The impact of COVID-19 vaccine mandates on shortages is ex ante ambiguous. If mandates increase perceived safety of the healthcare industry, marginal workers may be drawn to healthcare, relaxing shortages. On the other hand, if marginal workers are vaccine hesitant or averse, then mandates may push workers away from the industry and exacerbate shortages. We combine monthly data from the Current Population Survey 2021 to 2022 with difference-in-differences methods to study the effects of state vaccine mandates on the probability of working in healthcare, and of employment transitions into and out of the industry. Our findings suggest that vaccine mandates may have worsened healthcare workforce shortages: following adoption of a state-level mandate, the probability of working in the healthcare industry declines by 6%. Effects are larger among workers in healthcare-specific occupations, who leave the industry at higher rates in response to mandates and are slower to be replaced than workers in non-healthcare occupations. Findings suggest trade-offs faced by health policymakers seeking to achieve multiple health objectives.
Research reported in this publication was supported by the National Institute on Mental Health of the National Institutes of Health under Award Number 1R01MH132552 (PI: Johanna Catherine Maclean). John Earle also acknowledges support from the Russell Sage Foundation. The views expressed herein are those of the authors and do not necessarily reflect the views of the National Institutes of Health or the National Bureau of Economic Research.
MARC RIS BibTeΧ
Download Citation Data
More from NBER
In addition to working papers , the NBER disseminates affiliates’ latest findings through a range of free periodicals — the NBER Reporter , the NBER Digest , the Bulletin on Retirement and Disability , the Bulletin on Health , and the Bulletin on Entrepreneurship — as well as online conference reports , video lectures , and interviews .

Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Online First
- The role of COVID-19 vaccines in preventing post-COVID-19 thromboembolic and cardiovascular complications
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Núria Mercadé-Besora 1 , 2 , 3 ,
- Xintong Li 1 ,
- Raivo Kolde 4 ,
- Nhung TH Trinh 5 ,
- Maria T Sanchez-Santos 1 ,
- Wai Yi Man 1 ,
- Elena Roel 3 ,
- Carlen Reyes 3 ,
- http://orcid.org/0000-0003-0388-3403 Antonella Delmestri 1 ,
- Hedvig M E Nordeng 6 , 7 ,
- http://orcid.org/0000-0002-4036-3856 Anneli Uusküla 8 ,
- http://orcid.org/0000-0002-8274-0357 Talita Duarte-Salles 3 , 9 ,
- Clara Prats 2 ,
- http://orcid.org/0000-0002-3950-6346 Daniel Prieto-Alhambra 1 , 9 ,
- http://orcid.org/0000-0002-0000-0110 Annika M Jödicke 1 ,
- Martí Català 1
- 1 Pharmaco- and Device Epidemiology Group, Health Data Sciences, Botnar Research Centre, NDORMS , University of Oxford , Oxford , UK
- 2 Department of Physics , Universitat Politècnica de Catalunya , Barcelona , Spain
- 3 Fundació Institut Universitari per a la recerca a l'Atenció Primària de Salut Jordi Gol i Gurina (IDIAPJGol) , IDIAP Jordi Gol , Barcelona , Catalunya , Spain
- 4 Institute of Computer Science , University of Tartu , Tartu , Estonia
- 5 Pharmacoepidemiology and Drug Safety Research Group, Department of Pharmacy, Faculty of Mathematics and Natural Sciences , University of Oslo , Oslo , Norway
- 6 School of Pharmacy , University of Oslo , Oslo , Norway
- 7 Division of Mental Health , Norwegian Institute of Public Health , Oslo , Norway
- 8 Department of Family Medicine and Public Health , University of Tartu , Tartu , Estonia
- 9 Department of Medical Informatics, Erasmus University Medical Center , Erasmus University Rotterdam , Rotterdam , Zuid-Holland , Netherlands
- Correspondence to Prof Daniel Prieto-Alhambra, Pharmaco- and Device Epidemiology Group, Health Data Sciences, Botnar Research Centre, NDORMS, University of Oxford, Oxford, UK; daniel.prietoalhambra{at}ndorms.ox.ac.uk
Objective To study the association between COVID-19 vaccination and the risk of post-COVID-19 cardiac and thromboembolic complications.
Methods We conducted a staggered cohort study based on national vaccination campaigns using electronic health records from the UK, Spain and Estonia. Vaccine rollout was grouped into four stages with predefined enrolment periods. Each stage included all individuals eligible for vaccination, with no previous SARS-CoV-2 infection or COVID-19 vaccine at the start date. Vaccination status was used as a time-varying exposure. Outcomes included heart failure (HF), venous thromboembolism (VTE) and arterial thrombosis/thromboembolism (ATE) recorded in four time windows after SARS-CoV-2 infection: 0–30, 31–90, 91–180 and 181–365 days. Propensity score overlap weighting and empirical calibration were used to minimise observed and unobserved confounding, respectively.
Fine-Gray models estimated subdistribution hazard ratios (sHR). Random effect meta-analyses were conducted across staggered cohorts and databases.
Results The study included 10.17 million vaccinated and 10.39 million unvaccinated people. Vaccination was associated with reduced risks of acute (30-day) and post-acute COVID-19 VTE, ATE and HF: for example, meta-analytic sHR of 0.22 (95% CI 0.17 to 0.29), 0.53 (0.44 to 0.63) and 0.45 (0.38 to 0.53), respectively, for 0–30 days after SARS-CoV-2 infection, while in the 91–180 days sHR were 0.53 (0.40 to 0.70), 0.72 (0.58 to 0.88) and 0.61 (0.51 to 0.73), respectively.
Conclusions COVID-19 vaccination reduced the risk of post-COVID-19 cardiac and thromboembolic outcomes. These effects were more pronounced for acute COVID-19 outcomes, consistent with known reductions in disease severity following breakthrough versus unvaccinated SARS-CoV-2 infection.
- Epidemiology
- PUBLIC HEALTH
- Electronic Health Records
Data availability statement
Data may be obtained from a third party and are not publicly available. CPRD: CPRD data were obtained under the CPRD multi-study license held by the University of Oxford after Research Data Governance (RDG) approval. Direct data sharing is not allowed. SIDIAP: In accordance with current European and national law, the data used in this study is only available for the researchers participating in this study. Thus, we are not allowed to distribute or make publicly available the data to other parties. However, researchers from public institutions can request data from SIDIAP if they comply with certain requirements. Further information is available online ( https://www.sidiap.org/index.php/menu-solicitudesen/application-proccedure ) or by contacting SIDIAP ([email protected]). CORIVA: CORIVA data were obtained under the approval of Research Ethics Committee of the University of Tartu and the patient level data sharing is not allowed. All analyses in this study were conducted in a federated manner, where analytical code and aggregated (anonymised) results were shared, but no patient-level data was transferred across the collaborating institutions.
This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/ .
https://doi.org/10.1136/heartjnl-2023-323483
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
WHAT IS ALREADY KNOWN ON THIS TOPIC
COVID-19 vaccines proved to be highly effective in reducing the severity of acute SARS-CoV-2 infection.
While COVID-19 vaccines were associated with increased risk for cardiac and thromboembolic events, such as myocarditis and thrombosis, the risk of complications was substantially higher due to SARS-CoV-2 infection.
WHAT THIS STUDY ADDS
COVID-19 vaccination reduced the risk of heart failure, venous thromboembolism and arterial thrombosis/thromboembolism in the acute (30 days) and post-acute (31 to 365 days) phase following SARS-CoV-2 infection. This effect was stronger in the acute phase.
The overall additive effect of vaccination on the risk of post-vaccine and/or post-COVID thromboembolic and cardiac events needs further research.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
COVID-19 vaccines proved to be highly effective in reducing the risk of post-COVID cardiovascular and thromboembolic complications.
Introduction
COVID-19 vaccines were approved under emergency authorisation in December 2020 and showed high effectiveness against SARS-CoV-2 infection, COVID-19-related hospitalisation and death. 1 2 However, concerns were raised after spontaneous reports of unusual thromboembolic events following adenovirus-based COVID-19 vaccines, an association that was further assessed in observational studies. 3 4 More recently, mRNA-based vaccines were found to be associated with a risk of rare myocarditis events. 5 6
On the other hand, SARS-CoV-2 infection can trigger cardiac and thromboembolic complications. 7 8 Previous studies showed that, while slowly decreasing over time, the risk for serious complications remain high for up to a year after infection. 9 10 Although acute and post-acute cardiac and thromboembolic complications following COVID-19 are rare, they present a substantial burden to the affected patients, and the absolute number of cases globally could become substantial.
Recent studies suggest that COVID-19 vaccination could protect against cardiac and thromboembolic complications attributable to COVID-19. 11 12 However, most studies did not include long-term complications and were conducted among specific populations.
Evidence is still scarce as to whether the combined effects of COVID-19 vaccines protecting against SARS-CoV-2 infection and reducing post-COVID-19 cardiac and thromboembolic outcomes, outweigh any risks of these complications potentially associated with vaccination.
We therefore used large, representative data sources from three European countries to assess the overall effect of COVID-19 vaccines on the risk of acute and post-acute COVID-19 complications including venous thromboembolism (VTE), arterial thrombosis/thromboembolism (ATE) and other cardiac events. Additionally, we studied the comparative effects of ChAdOx1 versus BNT162b2 on the risk of these same outcomes.
Data sources
We used four routinely collected population-based healthcare datasets from three European countries: the UK, Spain and Estonia.
For the UK, we used data from two primary care databases—namely, Clinical Practice Research Datalink, CPRD Aurum 13 and CPRD Gold. 14 CPRD Aurum currently covers 13 million people from predominantly English practices, while CPRD Gold comprises 3.1 million active participants mostly from GP practices in Wales and Scotland. Spanish data were provided by the Information System for the Development of Research in Primary Care (SIDIAP), 15 which encompasses primary care records from 6 million active patients (around 75% of the population in the region of Catalonia) linked to hospital admissions data (Conjunt Mínim Bàsic de Dades d’Alta Hospitalària). Finally, the CORIVA dataset based on national health claims data from Estonia was used. It contains all COVID-19 cases from the first year of the pandemic and ~440 000 randomly selected controls. CORIVA was linked to the death registry and all COVID-19 testing from the national health information system.
Databases included sociodemographic information, diagnoses, measurements, prescriptions and secondary care referrals and were linked to vaccine registries, including records of all administered vaccines from all healthcare settings. Data availability for CPRD Gold ended in December 2021, CPRD Aurum in January 2022, SIDIAP in June 2022 and CORIVA in December 2022.
All databases were mapped to the Observational Medical Outcomes Partnership Common Data Model (OMOP CDM) 16 to facilitate federated analytics.
Multinational network staggered cohort study: study design and participants
The study design has been published in detail elsewhere. 17 Briefly, we used a staggered cohort design considering vaccination as a time-varying exposure. Four staggered cohorts were designed with each cohort representing a country-specific vaccination rollout phase (eg, dates when people became eligible for vaccination, and eligibility criteria).
The source population comprised all adults registered in the respective database for at least 180 days at the start of the study (4 January 2021 for CPRD Gold and Aurum, 20 February 2021 for SIDIAP and 28 January 2021 for CORIVA). Subsequently, each staggered cohort corresponded to an enrolment period: all people eligible for vaccination during this time were included in the cohort and people with a history of SARS-CoV-2 infection or COVID-19 vaccination before the start of the enrolment period were excluded. Across countries, cohort 1 comprised older age groups, whereas cohort 2 comprised individuals at risk for severe COVID-19. Cohort 3 included people aged ≥40 and cohort 4 enrolled people aged ≥18.
In each cohort, people receiving a first vaccine dose during the enrolment period were allocated to the vaccinated group, with their index date being the date of vaccination. Individuals who did not receive a vaccine dose comprised the unvaccinated group and their index date was assigned within the enrolment period, based on the distribution of index dates in the vaccinated group. People with COVID-19 before the index date were excluded.
Follow-up started from the index date until the earliest of end of available data, death, change in exposure status (first vaccine dose for those unvaccinated) or outcome of interest.
COVID-19 vaccination
All vaccines approved within the study period from January 2021 to July 2021—namely, ChAdOx1 (Oxford/AstraZeneca), BNT162b2 (BioNTech/Pfizer]) Ad26.COV2.S (Janssen) and mRNA-1273 (Moderna), were included for this study.
Post-COVID-19 outcomes of interest
Outcomes of interest were defined as SARS-CoV-2 infection followed by a predefined thromboembolic or cardiac event of interest within a year after infection, and with no record of the same clinical event in the 6 months before COVID-19. Outcome date was set as the corresponding SARS-CoV-2 infection date.
COVID-19 was identified from either a positive SARS-CoV-2 test (polymerase chain reaction (PCR) or antigen), or a clinical COVID-19 diagnosis, with no record of COVID-19 in the previous 6 weeks. This wash-out period was imposed to exclude re-recordings of the same COVID-19 episode.
Post-COVID-19 outcome events were selected based on previous studies. 11–13 Events comprised ischaemic stroke (IS), haemorrhagic stroke (HS), transient ischaemic attack (TIA), ventricular arrhythmia/cardiac arrest (VACA), myocarditis/pericarditis (MP), myocardial infarction (MI), heart failure (HF), pulmonary embolism (PE) and deep vein thrombosis (DVT). We used two composite outcomes: (1) VTE, as an aggregate of PE and DVT and (2) ATE, as a composite of IS, TIA and MI. To avoid re-recording of the same complication we imposed a wash-out period of 90 days between records. Phenotypes for these complications were based on previously published studies. 3 4 8 18
All outcomes were ascertained in four different time periods following SARS-CoV-2 infection: the first period described the acute infection phase—that is, 0–30 days after COVID-19, whereas the later periods - which are 31–90 days, 91–180 days and 181–365 days, illustrate the post-acute phase ( figure 1 ).
- Download figure
- Open in new tab
- Download powerpoint
Study outcome design. Study outcomes of interest are defined as a COVID-19 infection followed by one of the complications in the figure, within a year after infection. Outcomes were ascertained in four different time windows after SARS-CoV-2 infection: 0–30 days (namely the acute phase), 31–90 days, 91–180 days and 181–365 days (these last three comprise the post-acute phase).
Negative control outcomes
Negative control outcomes (NCOs) were used to detect residual confounding. NCOs are outcomes which are not believed to be causally associated with the exposure, but share the same bias structure with the exposure and outcome of interest. Therefore, no significant association between exposure and NCO is to be expected. Our study used 43 different NCOs from previous work assessing vaccine effectiveness. 19
Statistical analysis
Federated network analyses.
A template for an analytical script was developed and subsequently tailored to include the country-specific aspects (eg, dates, priority groups) for the vaccination rollout. Analyses were conducted locally for each database. Only aggregated data were shared and person counts <5 were clouded.
Propensity score weighting
Large-scale propensity scores (PS) were calculated to estimate the likelihood of a person receiving the vaccine based on their demographic and health-related characteristics (eg, conditions, medications) prior to the index date. PS were then used to minimise observed confounding by creating a weighted population (overlap weighting 20 ), in which individuals contributed with a different weight based on their PS and vaccination status.
Prespecified key variables included in the PS comprised age, sex, location, index date, prior observation time in the database, number of previous outpatient visits and previous SARS-CoV-2 PCR/antigen tests. Regional vaccination, testing and COVID-19 incidence rates were also forced into the PS equation for the UK databases 21 and SIDIAP. 22 In addition, least absolute shrinkage and selection operator (LASSO) regression, a technique for variable selection, was used to identify additional variables from all recorded conditions and prescriptions within 0–30 days, 31–180 days and 181-any time (conditions only) before the index date that had a prevalence of >0.5% in the study population.
PS were then separately estimated for each staggered cohort and analysis. We considered covariate balance to be achieved if absolute standardised mean differences (ASMDs) were ≤0.1 after weighting. Baseline characteristics such as demographics and comorbidities were reported.
Effect estimation
To account for the competing risk of death associated with COVID-19, Fine-and-Grey models 23 were used to calculate subdistribution hazard ratios (sHRs). Subsequently, sHRs and confidence intervals were empirically calibrated from NCO estimates 24 to account for unmeasured confounding. To calibrate the estimates, the empirical null distribution was derived from NCO estimates and was used to compute calibrated confidence intervals. For each outcome, sHRs from the four staggered cohorts were pooled using random-effect meta-analysis, both separately for each database and across all four databases.
Sensitivity analysis
Sensitivity analyses comprised 1) censoring follow-up for vaccinated people at the time when they received their second vaccine dose and 2) considering only the first post-COVID-19 outcome within the year after infection ( online supplemental figure S1 ). In addition, comparative effectiveness analyses were conducted for BNT162b2 versus ChAdOx1.
Supplemental material
Data and code availability.
All analytic code for the study is available in GitHub ( https://github.com/oxford-pharmacoepi/vaccineEffectOnPostCovidCardiacThromboembolicEvents ), including code lists for vaccines, COVID-19 tests and diagnoses, cardiac and thromboembolic events, NCO and health conditions to prioritise patients for vaccination in each country. We used R version 4.2.3 and statistical packages survival (3.5–3), Empirical Calibration (3.1.1), glmnet (4.1-7), and Hmisc (5.0–1).
Patient and public involvement
Owing to the nature of the study and the limitations regarding data privacy, the study design, analysis, interpretation of data and revision of the manuscript did not involve any patients or members of the public.
All aggregated results are available in a web application ( https://dpa-pde-oxford.shinyapps.io/PostCovidComplications/ ).
We included over 10.17 million vaccinated individuals (1 618 395 from CPRD Gold; 5 729 800 from CPRD Aurum; 2 744 821 from SIDIAP and 77 603 from CORIVA) and 10.39 million unvaccinated individuals (1 640 371; 5 860 564; 2 588 518 and 302 267, respectively). Online supplemental figures S2-5 illustrate study inclusion for each database.
Adequate covariate balance was achieved after PS weighting in most studies: CORIVA (all cohorts) and SIDIAP (cohorts 1 and 4) did not contribute to ChAdOx1 subanalyses owing to sample size and covariate imbalance. ASMD results are accessible in the web application.
NCO analyses suggested residual bias after PS weighting, with a majority of NCOs associated positively with vaccination. Therefore, calibrated estimates are reported in this manuscript. Uncalibrated effect estimates and NCO analyses are available in the web interface.
Population characteristics
Table 1 presents baseline characteristics for the weighted populations in CPRD Aurum, for illustrative purposes. Online supplemental tables S1-25 summarise baseline characteristics for weighted and unweighted populations for each database and comparison. Across databases and cohorts, populations followed similar patterns: cohort 1 represented an older subpopulation (around 80 years old) with a high proportion of women (57%). Median age was lowest in cohort 4 ranging between 30 and 40 years.
- View inline
Characteristics of weighted populations in CPRD Aurum database, stratified by staggered cohort and exposure status. Exposure is any COVID-19 vaccine
COVID-19 vaccination and post-COVID-19 complications
Table 2 shows the incidence of post-COVID-19 VTE, ATE and HF, the three most common post-COVID-19 conditions among the studied outcomes. Outcome counts are presented separately for 0–30, 31–90, 91–180 and 181–365 days after SARS-CoV-2 infection. Online supplemental tables S26-36 include all studied complications, also for the sensitivity and subanalyses. Similar pattern for incidences were observed across all databases: higher outcome rates in the older populations (cohort 1) and decreasing frequency with increasing time after infection in all cohorts.
Number of records (and risk per 10 000 individuals) for acute and post-acute COVID-19 cardiac and thromboembolic complications, across cohorts and databases for any COVID-19 vaccination
Forest plots for the effect of COVID-19 vaccines on post-COVID-19 cardiac and thromboembolic complications; meta-analysis across cohorts and databases. Dashed line represents a level of heterogeneity I 2 >0.4. ATE, arterial thrombosis/thromboembolism; CD+HS, cardiac diseases and haemorrhagic stroke; VTE, venous thromboembolism.
Results from calibrated estimates pooled in meta-analysis across cohorts and databases are shown in figure 2 .
Reduced risk associated with vaccination is observed for acute and post-acute VTE, DVT, and PE: acute meta-analytic sHR are 0.22 (95% CI, 0.17–0.29); 0.36 (0.28–0.45); and 0.19 (0.15–0.25), respectively. For VTE in the post-acute phase, sHR estimates are 0.43 (0.34–0.53), 0.53 (0.40–0.70) and 0.50 (0.36–0.70) for 31–90, 91–180, and 181–365 days post COVID-19, respectively. Reduced risk of VTE outcomes was observed in vaccinated across databases and cohorts, see online supplemental figures S14–22 .
Similarly, the risk of ATE, IS and MI in the acute phase after infection was reduced for the vaccinated group, sHR of 0.53 (0.44–0.63), 0.55 (0.43–0.70) and 0.49 (0.38–0.62), respectively. Reduced risk associated with vaccination persisted for post-acute ATE, with sHR of 0.74 (0.60–0.92), 0.72 (0.58–0.88) and 0.62 (0.48–0.80) for 31–90, 91–180 and 181–365 days post-COVID-19, respectively. Risk of post-acute MI remained lower for vaccinated in the 31–90 and 91–180 days after COVID-19, with sHR of 0.64 (0.46–0.87) and 0.64 (0.45–0.90), respectively. Vaccination effect on post-COVID-19 TIA was seen only in the 181–365 days, with sHR of 0.51 (0.31–0.82). Online supplemental figures S23-31 show database-specific and cohort-specific estimates for ATE-related complications.
Risk of post-COVID-19 cardiac complications was reduced in vaccinated individuals. Meta-analytic estimates in the acute phase showed sHR of 0.45 (0.38–0.53) for HF, 0.41 (0.26–0.66) for MP and 0.41 (0.27–0.63) for VACA. Reduced risk persisted for post-acute COVID-19 HF: sHR 0.61 (0.51–0.73) for 31–90 days, 0.61 (0.51–0.73) for 91–180 days and 0.52 (0.43–0.63) for 181–365 days. For post-acute MP, risk was only lowered in the first post-acute window (31–90 days), with sHR of 0.43 (0.21–0.85). Vaccination showed no association with post-COVID-19 HS. Database-specific and cohort-specific results for these cardiac diseases are shown in online supplemental figures S32-40 .
Stratified analyses by vaccine showed similar associations, except for ChAdOx1 which was not associated with reduced VTE and ATE risk in the last post-acute window. Sensitivity analyses were consistent with main results ( online supplemental figures S6-13 ).
Figure 3 shows the results of comparative effects of BNT162b2 versus ChAdOx1, based on UK data. Meta-analytic estimates favoured BNT162b2 (sHR of 0.66 (0.46–0.93)) for VTE in the 0–30 days after infection, but no differences were seen for post-acute VTE or for any of the other outcomes. Results from sensitivity analyses, database-specific and cohort-specific estimates were in line with the main findings ( online supplemental figures S41-51 ).
Forest plots for comparative vaccine effect (BNT162b2 vs ChAdOx1); meta-analysis across cohorts and databases. ATE, arterial thrombosis/thromboembolism; CD+HS, cardiac diseases and haemorrhagic stroke; VTE, venous thromboembolism.
Key findings
Our analyses showed a substantial reduction of risk (45–81%) for thromboembolic and cardiac events in the acute phase of COVID-19 associated with vaccination. This finding was consistent across four databases and three different European countries. Risks for post-acute COVID-19 VTE, ATE and HF were reduced to a lesser extent (24–58%), whereas a reduced risk for post-COVID-19 MP and VACA in vaccinated people was seen only in the acute phase.

Results in context
The relationship between SARS-CoV-2 infection, COVID-19 vaccines and thromboembolic and/or cardiac complications is tangled. Some large studies report an increased risk of VTE and ATE following both ChAdOx1 and BNT162b2 vaccination, 7 whereas other studies have not identified such a risk. 25 Elevated risk of VTE has also been reported among patients with COVID-19 and its occurrence can lead to poor prognosis and mortality. 26 27 Similarly, several observational studies have found an association between COVID-19 mRNA vaccination and a short-term increased risk of myocarditis, particularly among younger male individuals. 5 6 For instance, a self-controlled case series study conducted in England revealed about 30% increased risk of hospital admission due to myocarditis within 28 days following both ChAdOx1 and BNT162b2 vaccines. However, this same study also found a ninefold higher risk for myocarditis following a positive SARS-CoV-2 test, clearly offsetting the observed post-vaccine risk.
COVID-19 vaccines have demonstrated high efficacy and effectiveness in preventing infection and reducing the severity of acute-phase infection. However, with the emergence of newer variants of the virus, such as omicron, and the waning protective effect of the vaccine over time, there is a growing interest in understanding whether the vaccine can also reduce the risk of complications after breakthrough infections. Recent studies suggested that COVID-19 vaccination could potentially protect against acute post-COVID-19 cardiac and thromboembolic events. 11 12 A large prospective cohort study 11 reports risk of VTE after SARS-CoV-2 infection to be substantially reduced in fully vaccinated ambulatory patients. Likewise, Al-Aly et al 12 suggest a reduced risk for post-acute COVID-19 conditions in breakthrough infection versus SARS-CoV-2 infection without prior vaccination. However, the populations were limited to SARS-CoV-2 infected individuals and estimates did not include the effect of the vaccine to prevent COVID-19 in the first place. Other studies on post-acute COVID-19 conditions and symptoms have been conducted, 28 29 but there has been limited reporting on the condition-specific risks associated with COVID-19, even though the prognosis for different complications can vary significantly.
In line with previous studies, our findings suggest a potential benefit of vaccination in reducing the risk of post-COVID-19 thromboembolic and cardiac complications. We included broader populations, estimated the risk in both acute and post-acute infection phases and replicated these using four large independent observational databases. By pooling results across different settings, we provided the most up-to-date and robust evidence on this topic.
Strengths and limitations
The study has several strengths. Our multinational study covering different healthcare systems and settings showed consistent results across all databases, which highlights the robustness and replicability of our findings. All databases had complete recordings of vaccination status (date and vaccine) and are representative of the respective general population. Algorithms to identify study outcomes were used in previous published network studies, including regulatory-funded research. 3 4 8 18 Other strengths are the staggered cohort design which minimises confounding by indication and immortal time bias. PS overlap weighting and NCO empirical calibration have been shown to adequately minimise bias in vaccine effectiveness studies. 19 Furthermore, our estimates include the vaccine effectiveness against COVID-19, which is crucial in the pathway to experience post-COVID-19 complications.
Our study has some limitations. The use of real-world data comes with inherent limitations including data quality concerns and risk of confounding. To deal with these limitations, we employed state-of-the-art methods, including large-scale propensity score weighting and calibration of effect estimates using NCO. 19 24 A recent study 30 has demonstrated that methodologically sound observational studies based on routinely collected data can produce results similar to those of clinical trials. We acknowledge that results from NCO were positively associated with vaccination, and estimates might still be influenced by residual bias despite using calibration. Another limitation is potential under-reporting of post-COVID-19 complications: some asymptomatic and mild COVID-19 infections might have not been recorded. Additionally, post-COVID-19 outcomes of interest might be under-recorded in primary care databases (CPRD Aurum and Gold) without hospital linkage, which represent a large proportion of the data in the study. However, results in SIDIAP and CORIVA, which include secondary care data, were similar. Also, our study included a small number of young men and male teenagers, who were the main population concerned with increased risks of myocarditis/pericarditis following vaccination.
Conclusions
Vaccination against SARS-CoV-2 substantially reduced the risk of acute post-COVID-19 thromboembolic and cardiac complications, probably through a reduction in the risk of SARS-CoV-2 infection and the severity of COVID-19 disease due to vaccine-induced immunity. Reduced risk in vaccinated people lasted for up to 1 year for post-COVID-19 VTE, ATE and HF, but not clearly for other complications. Findings from this study highlight yet another benefit of COVID-19 vaccination. However, further research is needed on the possible waning of the risk reduction over time and on the impact of booster vaccination.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
The study was approved by the CPRD’s Research Data Governance Process, Protocol No 21_000557 and the Clinical Research Ethics committee of Fundació Institut Universitari per a la recerca a l’Atenció Primària de Salut Jordi Gol i Gurina (IDIAPJGol) (approval number 4R22/133) and the Research Ethics Committee of the University of Tartu (approval No. 330/T-10).
Acknowledgments
This study is based in part on data from the Clinical Practice Research Datalink (CPRD) obtained under licence from the UK Medicines and Healthcare products Regulatory Agency. We thank the patients who provided these data, and the NHS who collected the data as part of their care and support. All interpretations, conclusions and views expressed in this publication are those of the authors alone and not necessarily those of CPRD. We would also like to thank the healthcare professionals in the Catalan healthcare system involved in the management of COVID-19 during these challenging times, from primary care to intensive care units; the Institut de Català de la Salut and the Program d’Analítica de Dades per a la Recerca i la Innovació en Salut for providing access to the different data sources accessible through The System for the Development of Research in Primary Care (SIDIAP).
- Pritchard E ,
- Matthews PC ,
- Stoesser N , et al
- Lauring AS ,
- Tenforde MW ,
- Chappell JD , et al
- Pistillo A , et al
- Duarte-Salles T , et al
- Hansen JV ,
- Fosbøl E , et al
- Chen A , et al
- Hippisley-Cox J ,
- Mei XW , et al
- Duarte-Salles T ,
- Fernandez-Bertolin S , et al
- Ip S , et al
- Bowe B , et al
- Prats-Uribe A ,
- Feng Q , et al
- Campbell J , et al
- Herrett E ,
- Gallagher AM ,
- Bhaskaran K , et al
- Raventós B ,
- Fernández-Bertolín S ,
- Aragón M , et al
- Makadia R ,
- Matcho A , et al
- Mercadé-Besora N ,
- Kolde R , et al
- Ostropolets A ,
- Makadia R , et al
- Rathod-Mistry T , et al
- Thomas LE ,
- ↵ Coronavirus (COVID-19) in the UK . 2022 . Available : https://coronavirus.data.gov.uk/
- Generalitat de Catalunya
- Schuemie MJ ,
- Hripcsak G ,
- Ryan PB , et al
- Houghton DE ,
- Wysokinski W ,
- Casanegra AI , et al
- Katsoularis I ,
- Fonseca-Rodríguez O ,
- Farrington P , et al
- Jehangir Q ,
- Li P , et al
- Byambasuren O ,
- Stehlik P ,
- Clark J , et al
- Brannock MD ,
- Preiss AJ , et al
- Schneeweiss S , RCT-DUPLICATE Initiative , et al
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
AMJ and MC are joint senior authors.
Contributors DPA and AMJ led the conceptualisation of the study with contributions from MC and NM-B. AMJ, TD-S, ER, AU and NTHT adapted the study design with respect to the local vaccine rollouts. AD and WYM mapped and curated CPRD data. MC and NM-B developed code with methodological contributions advice from MTS-S and CP. DPA, MC, NTHT, TD-S, HMEN, XL, CR and AMJ clinically interpreted the results. NM-B, XL, AMJ and DPA wrote the first draft of the manuscript, and all authors read, revised and approved the final version. DPA and AMJ obtained the funding for this research. DPA is responsible for the overall content as guarantor: he accepts full responsibility for the work and the conduct of the study, had access to the data, and controlled the decision to publish.
Funding The research was supported by the National Institute for Health and Care Research (NIHR) Oxford Biomedical Research Centre (BRC). DPA is funded through a NIHR Senior Research Fellowship (Grant number SRF-2018–11-ST2-004). Funding to perform the study in the SIDIAP database was provided by the Real World Epidemiology (RWEpi) research group at IDIAPJGol. Costs of databases mapping to OMOP CDM were covered by the European Health Data and Evidence Network (EHDEN).
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting or dissemination plans of this research.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 28 March 2024
An effective COVID-19 vaccine hesitancy intervention focused on the relative risks of vaccination and infection
- Cameron O’Neill Byerley 1 ,
- Dru Horne 1 ,
- Mina Gong 1 ,
- Stacy Musgrave 2 ,
- Laura A. Valaas 3 ,
- Brian Rickard 4 ,
- Hyunkyoung Yoon 2 ,
- Min Sook Park 5 ,
- Alison Mirin 6 ,
- Surani Joshua 7 ,
- Heather Lavender 1 &
- Sukjin You 5
Scientific Reports volume 14 , Article number: 7419 ( 2024 ) Cite this article
174 Accesses
1 Altmetric
Metrics details
- Epidemiology
- Patient education
We designed the Relative Risk Tool (RRT) to help people assess the relative risks associated with COVID-19 vaccination and infection. In May 2022 ( N = 400) and November 2022 ( N = 615), U.S. residents participated in a survey that included questions about the risks of vaccination and infection. In both cohorts, we found an association between relative risk perception and vaccine hesitancy. Participants in the May cohort were randomly assigned an intervention: to see information from the RRT or the Centers for Disease Control and Prevention (CDC). After the intervention, participants answered the same questions about risk perception and vaccination intent again. The RRT was more effective than the CDC at changing risk perception and increasing vaccination intent. In November, the survey structure was the same, but the RRT was the only intervention included, and we confirmed that the RRT was effective at changing opinions in this new sample. Importantly, the RRT provided accurate information about the risks of serious adverse outcomes to vaccination and still increased vaccination intent. Our work suggests that the RRT helps people assess relative risk, which can in turn help empower them to make informed decisions and ultimately reduce vaccine hesitancy.
Similar content being viewed by others
Revisiting COVID-19 vaccine hesitancy around the world using data from 23 countries in 2021
Jeffrey V. Lazarus, Katarzyna Wyka, … Ayman El-Mohandes
Communicating doctors’ consensus persistently increases COVID-19 vaccinations
Vojtěch Bartoš, Michal Bauer, … Julie Chytilová

Exploratory study of the global intent to accept COVID-19 vaccinations
Alexandre de Figueiredo & Heidi J. Larson
Introduction
COVID-19 vaccine hesitancy is a major global issue 1 , and it is important to develop research-based messaging about vaccination that is broadly understandable and supports decision making 2 . Vaccine hesitancy has been defined in multiple ways, including a “state of indecisiveness regarding a vaccination decision” as well as “delay in acceptance or refusal despite availability of vaccines” 3 . We consider vaccine hesitancy to be reluctance, refusal, or indecision regarding future vaccinations, but consider current vaccination status to be related to vaccine hesitancy. As of May 2023, 70.0% of the world’s population had received at least one dose of a COVID-19 vaccine 4 , 5 , and 17.0% of the U.S. population had received recommended boosters 6 .
People are still making decisions about vaccination 7 and, thus, there is a need for accurate and trustworthy communication about COVID-19 vaccines 8 . Strategies for addressing vaccine hesitancy have been met with mixed success 9 , 10 , 11 , 12 , 13 , 14 , and effective interventions require addressing the various drivers of vaccine hesitancy with multifaceted strategies 9 , 15 , 16 . Reasons for vaccine hesitancy include concern about the risks associated with vaccination, lack of concern for the risk due to the disease, ease of access to vaccination, and mistrust in government and health institutions 8 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 . While reasons for vaccine hesitancy vary widely 25 , 26 , 27 , concern about safety and efficacy are significant reasons across populations. For example, the belief “COVID-19 vaccines are not safe” had the highest odds ratio in a statistical model that predicted vaccine hesitancy 28 . Additionally, all 14 studies in a literature review on vaccine hesitancy found that concerns about safety were associated with hesitancy 29 . In order to address people’s concerns about risks due to vaccination, we focused our research on risk perception and risk communication.
The relative risk tool
Based on our models of citizens’ mathematical thinking from prior mathematics education research and interviews conducted about COVID-19 30 , 31 , 32 , 33 , 34 , we created the RRT to help citizens compare the risks associated with COVID-19 infection with risks associated with more familiar situations such as driving, pregnancy, sports, and other events 35 . We designed, tested, and updated the Relative Risk Tool from August 2020 to May 2022 to help people understand the risks associated with COVID-19 vaccination and infection and the efficacy of vaccines 35 . Note, we will use the phrase “risk of vaccination” throughout this paper to mean “risks associated with vaccination” and likewise for infection. We were inspired to create the RRT based on research we conducted in April and May 2020 on people’s understanding of risk associated with COVID-19 infection 36 . The RRT (Fig. 1 ) uses bar graphs to convey that infection is more likely than vaccination to cause hospitalization and death for all ages modeled, that vaccination reduces the risks due to infection substantially, and that unvaccinated adults face more risk from infection than people are typically willing to accept as a part of daily life. The RRT incorporates an epidemiological model 37 that allows participants to move a slider to find the average risk of hospitalization and death if an average person of a particular age was infected with COVID-19. The RRT shows both relative risk and absolute risk due to infection and vaccination.
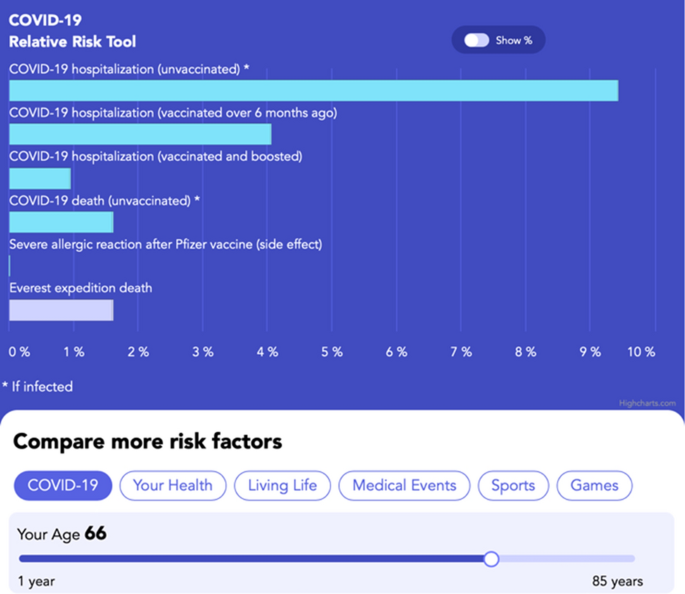
The Relative Risk Tool ( https://www.covidtaser.com/relativerisk ) is an interactive web app that allows users to compare the risks associated with various scenarios and COVID-19 infection after inputting their age. For example, 1.6% of mountaineers who climb above base camp at Mount Everest die, which is similar to the risk of death for an unvaccinated 66-year-old infected with COVID-19.
The design of the RRT was informed by research in mathematics education and risk communication conducted before and during the pandemic 23 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , with the primary aim of making the RRT understandable to most people 35 , 36 , 45 , 46 . The RRT provides a potential template for future risk communication tools that can be used to accurately present both absolute and relative risks to the general public using direct comparisons to related risks. Communicating risks for decision making is more difficult than simply telling people probabilities 42 , 47 , 48 , 49 because percentage and probability are difficult concepts to learn, and people hold widely different understandings of the meaning of a particular percentage 30 , 31 , 34 , 50 , 51 , 52 , 53 , 54 . The thinking needed to accurately compare risks is more sophisticated than what is normally developed in K-12 education 55 , 56 , 57 , 58 , 59 , 60 . Experts often quantify risk using percentages 41 , 61 , and the public often uses non-numerical heuristics to estimate risk and to make decisions 62 , 63 , 64 , 65 , 66 , 67 . Many people unconsciously use the availability heuristic 68 , 69 , wherein how easily an event comes to someone’s mind influences their view of how likely that event is to occur. For example, people can readily imagine driving trips and car accidents to develop a sense of the riskiness of driving. We designed the RRT to help people make sense of the percent estimates of risk by relating COVID-19 risks to other more familiar risks like driving 70 .
The presentation format of numerical risks impacts decision making 44 , so it was critical for us to study how people understood the RRT and improve it using an iterative design-based research method. As part of the design process, we analyzed how citizens learned from the RRT using various methods such as interviewing people while using the RRT 46 , conducting online pilot surveys 45 , and thematically categorizing comments on a New York Times article which mentioned the RRT 71 (see “ Methods ” for details). We also updated the RRT in response to requests for more targeted information. For example, we included the risk of myocarditis due to infection and the risk of myocarditis due to vaccination 72 , 73 . The version of the RRT tested in this paper was consistent with the majority of Patient Decision Aid standards with a focus on “presenting probabilities of outcomes in an unbiased and understandable way” to help people understand positive and negative potential outcomes of vaccination 74 . As recommended by the Patient Decision Aid Standards, the RRT also used plain language, disclosed funding, cited peer-reviewed sources of information, and had a systematic development process.
Overview of study
We tested the 2022 version of the RRT (current version available at http://www.covidtaser.com ) in this study. This paper (1) models the relationship between risk perception and COVID-19 vaccination status and intent. This paper, then, (2) evaluates if the RRT intervention, designed specifically to educate about relative risks associated with COVID-19 infection and vaccination, changes participants’ risk perception or intent to be vaccinated. Based on our interviews and prior regression models 8 , we hypothesized that beliefs about the relative risks of vaccination and infection would be correlated with vaccination status and future vaccination intent. Therefore, we also hypothesized that education about relative risks of vaccination and infection would help people resolve indecision about vaccination and increase their willingness to accept future vaccines. To understand the impact of the RRT, we conducted an online pre-post exposure study in May and November 2022 with U.S. adult residents, outlined in Fig. 2 . In May, half of the participants saw information from the RRT, and the other half constituted a control group that was randomly assigned to see similar information about safety and efficacy of the COVID-19 vaccine from the CDC website (see supplementary materials ). All study participants answered demographic questions, questions about risk (inspired by our earlier interviews), and questions from two large studies on vaccination intent 8 , 75 . We assessed the causal impact of information about safety and efficacy on two dimensions: (1) Belief about the relative risk of COVID-19 vaccination and infection and (2) Intent to receive a COVID-19 vaccine in the future. By May 2022, both the Pfizer and Moderna vaccines were fully approved by the U.S. Food and Drug Administration and freely available to all adults. Because the May survey demonstrated larger effects with the RRT than the CDC, and because we wanted to be able to analyze effects of the RRT in subgroups, we opted to not assign participants to view the CDC website in November.
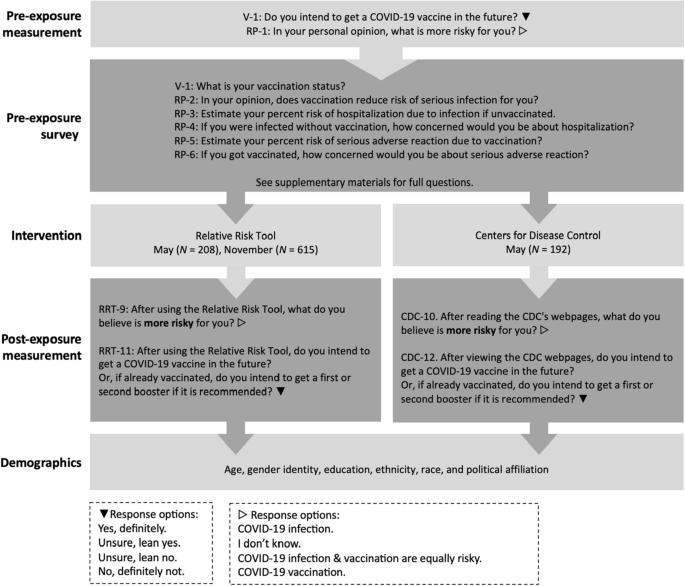
Design of study. All participants were given questions pre-exposure to the intervention about their vaccination status, intention to be vaccinated, and questions about risk. Post exposure participants were asked about vaccination intent, relative risk, and demographics. The questions are abbreviated and labeled in this figure (V-1, RP-1, etc.) with full questions available in supplementary materials and further description in “ Methods ” section.
Sample characteristics
We surveyed U.S. residents using Prime Panels, which samples from a population similar to the U.S. population 76 . The surveys were conducted on May 24, 2022 ( N = 400) and November 11, 2022 ( N = 615). Supplementary Table 1 provides information on the sample demographics with the self-reported age, education level, gender, race, ethnicity, political affiliation, COVID-19 infection history, and COVID-19 vaccination status. There are no statistically significant differences in participants’ demographics between the May and November samples.
U.S. residents’ risk perceptions
Table 1 displays results of pre-intervention questions about risk perception.
Many participants dramatically overestimated the number of U.S. citizens who have died as a result of vaccination (Table 1 ). Figure 3 shows non-vaccinated participants are much more likely than vaccinated participants to think vaccination is equally or more risky than infection.
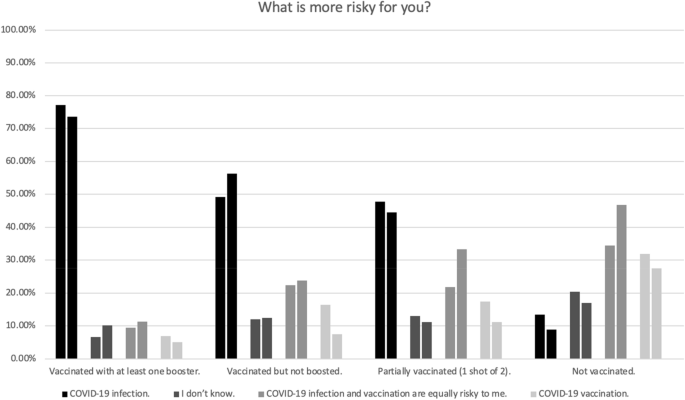
This figure shows the percentage of people with a given COVID-19 vaccination status who gave a particular answer to the question “What is more risky for you?” The left bar in each pair is from May 2022 (N = 400), and the right bar is from November 2022 (N = 615). There was a statistically significant relationship between risk perception and vaccination status, May, \({\chi }^{2}\) (9, N = 400) = 149.05, p < 0.001, W = 0.61; November, \({\chi }^{2}\) (9, N = 615) = 189.75, p < 0.001, W = 0.56.
Most participants gave numerical risk estimates (due to both vaccination and infection) much higher than those estimated in peer-reviewed literature 37 (Fig. 4 ). We also asked: “If you got a COVID-19 vaccine, how concerned would you be about a serious adverse reaction to the vaccine?” and “If you were infected with COVID-19, how concerned would you be about getting hospitalized?” The level of concern participants attached to a given risk estimate varied widely (Fig. 4 ). Many of the participants who estimated their risk of hospitalization if infected at 50% answered that they would be “not at all”, “slightly”, or “somewhat” concerned if infected. Risk estimates of 50% are common (50% Vaccination risk: May, n = 74/400; November, n = 115/615; 50% Infection risk: May, n = 77/400; November, n = 115/615). Some of these responses might be explained by prior research that found that people often give 50% probability estimates to indicate general uncertainty, whether that be uncertainty about specific frequencies or the belief that the event in question’s occurrence is up to chance 34 , 51 . In other words, someone estimating 50% does not necessarily mean that they believe that an event will occur roughly half the time 34 , 51 .
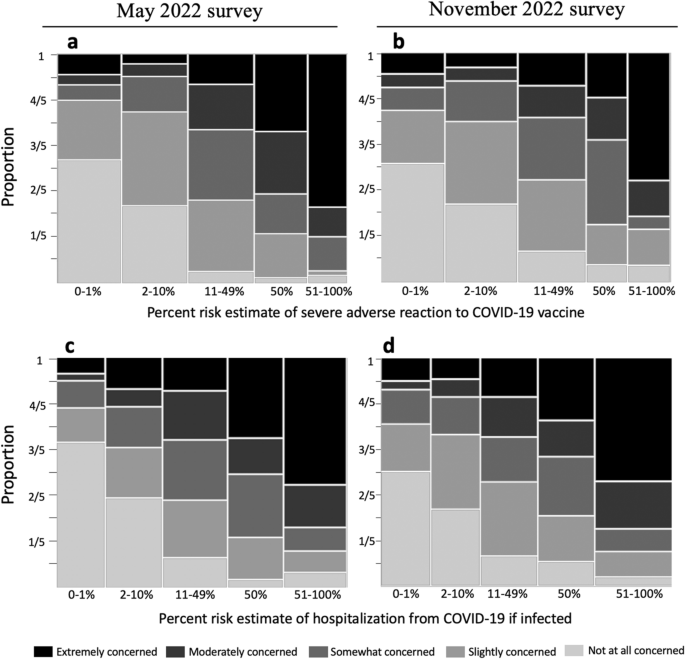
The figure shows the relationship between people’s percent risk estimates and their associated level of concern. We asked “If you receive a COVID-19 vaccine/booster in the future, what do you think your percent risk of a serious adverse reaction would be? An example of a serious adverse reaction is an allergic reaction requiring treatment in a hospital. Do not include your risk of common side effects such as fatigue” and “If you were infected with COVID-19 (without any vaccination), what do you think your percent risk of hospitalization from COVID-19 would be?” The width of the bars is proportional to the number of respondents who selected a response in each category. Figure d, for example, shows that more people selected a response between 51 and 100% than between 0 and 1%. The colors of the bar indicate the level of concern assigned by the participants for a given risk estimate. For example, in Figure d, half of people who estimated the risk of hospitalization from infection between 0–1% were “not at all concerned” (this is reflected in the light grey bar being a height of 1/2).
Although the median estimates for risk due to infection (May 26%; November 38%) were higher than median estimates for risk due to vaccination (May 20%; November 15%), the median responses were the same order of magnitude for both risks. In contrast, for an unvaccinated 40 year old person, the chance of hospitalization from COVID-19 infection (1.42%) is roughly 6000 times as large as the chance of a severe allergic reaction to the Pfizer COVID-19 vaccine (0.00021%) 37 , 77 .
Risk perceptions are correlated with vaccination intent
We quantified the impact of risk perception on vaccination intent while controlling for other variables commonly associated with vaccination intent (see Fig. 2 for intent question and control variables). The adjusted odds ratios shown in Fig. 5 tell us how many times as likely it is for someone with a given trait to be one level higher in vaccination intent than a person in the associated reference category.
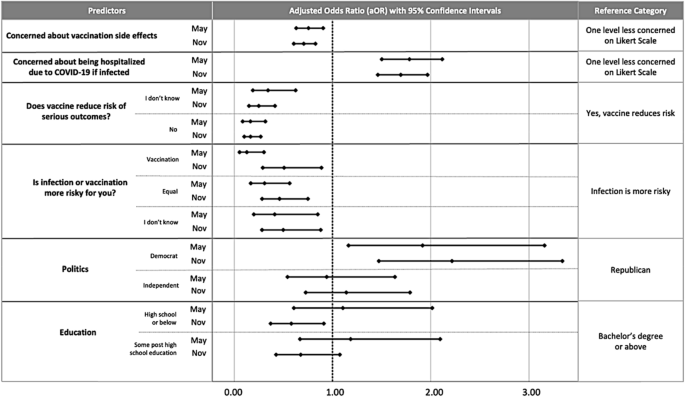
Correlates of COVID-19 vaccination intent include beliefs about the risks associated with COVID-19 vaccination and COVID-19 infection, beliefs about vaccine efficacy, political beliefs, and education. We chose the predictors in the initial full model and the reduced model presented based on the procedure described in the “ Methods ”. The multivariable ordinal logistic regression predicts vaccination intent, May, \({\chi }^{2}\) (11, N = 400) = 299.95, p < 0.001; November, \({\chi }^{2}\) (11, N = 615) = 386.83, p < 0.001. See Supp. Table 6 for exact values of aOR and 95% confidence intervals.
Overall, participants’ beliefs about the risks and benefits of COVID-19 vaccination are correlated with future vaccination intent. Participants who said that vaccination is equally or more risky than infection were less sure about receiving a vaccine in the future than participants who said infection is riskier than vaccination. Consistent with these findings, participants who were concerned about severe adverse reactions to vaccination were less likely to intend to get more vaccination shots, and participants who were more concerned about COVID-19 infection were more likely to intend to be vaccinated in the future. Participants who did not think (or were not sure) that the vaccine reduces risk due to COVID-19 infection were less likely to intend to be vaccinated. The odds ratios show that intent is more strongly associated with beliefs about relative risk than intent is associated with education (which was only statistically significant in November). Additionally, there was no statistically significant association between intent and age, gender, ethnicity, or race (which were therefore removed from the models). See Fig. 5 and Supp. Table 6 for adjusted odds ratios.
RRT impacted beliefs about relative risk
Respondents were asked to express their beliefs on whether COVID-19 vaccination or infection posed a higher risk for them. These beliefs were collected both before and after their visit to the CDC website or RRT tool (for questions, see Fig. 2 , and for responses, see Fig. 6 ).
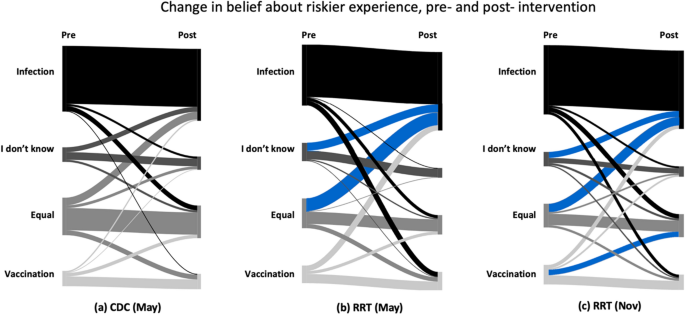
This diagram shows participants' responses to the question “What is riskier for you?” before and after seeing the CDC ( a ) and the RRT ( b , c ). Blue flows indicate a significant result at p < 0.05. Supplementary Tables 2 and 3 includes include statistics used to create diagram.
We used a McNemar–Bowker test to analyze symmetry in dependent responses 78 . A non-symmetrical response indicates a significant net change from one response pre-intervention to a different response post-intervention, i.e., that participants changed their mind in a specific direction after viewing the intervention. For respondents who viewed the CDC website in May, the global test was non-significant ( p = 0.681) indicating symmetrical responses (i.e., the number of respondents who changed from one option to another was not significantly different than the converse). For respondents who viewed the RRT tool in May and November, the overall test was significant, and there was a medium effect size (May, p = 0.001, g = 0.23, 95% CI [0.17, 0.35]; November, p < 0.001, g = 0.16, 95% CI [0.11, 0.23]).
Post-hoc pairwise symmetry tests were conducted, and adjusted p values were calculated using the Benjamini–Hochberg procedure (see Fig. 6 and Supplementary Table 2 ). In Fig. 6 , the blue flows indicate that a significantly greater number of participants changed their responses in the direction of the flow than the converse direction. In May for the RRT, the pairwise tests showed a significant change from participants selecting “COVID-19 infection and vaccination are equally risky” to “COVID-19 infection” as well as from “I don’t know” to “COVID-19 infection”. In November, there were significant changes from participants selecting “COVID-19 infection and vaccination are equally risky” to “COVID-19 infection,” from “I don’t know” to “COVID-19 infection”, and from “Vaccination is more risky” to “COVID-19 infection and vaccination are equally risky.” In May, 48.8% of participants thought infection was riskier than vaccination before seeing the RRT, and this changed to 62.0% post-intervention. In November, 54.5% thought infection was riskier than vaccination before seeing the RRT, and this changed to 61.6% post-intervention (see Supplementary Table 3 for confidence intervals for percentages).
RRT increased intent to accept vaccination
Before and after seeing information from either the CDC or RRT, we asked participants to rate their future intent to be vaccinated (Fig. 7 ). People who were already up to date on vaccinations were asked if they would get an additional booster if it was recommended. In a global test of symmetry, there were statistically significant effects of both the CDC intervention ( p = 0.004, g = 0.23 , 95% CI [0.17, 0.36]) and the RRT intervention (May, p < 0.001, g = 0.28, 95% CI [0.20, 0.39]); November, p < 0.001, g = 0.22, 95% CI [0.18, 0.29]).
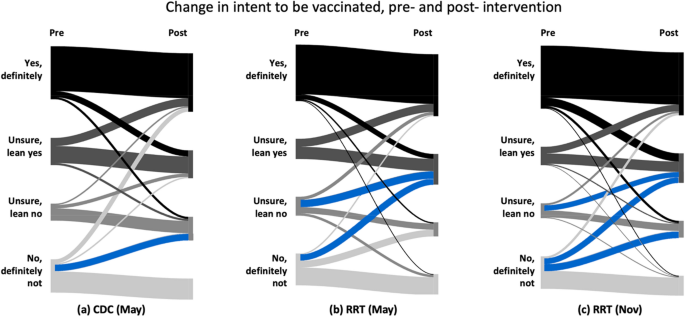
This figure shows citizens' responses to a question about intent to be vaccinated in the future before and after seeing the CDC ( a ) and the RRT ( b , c ) information about vaccination side effects and efficacy. Blue flows indicate a significant result at p < 0.05. Supplementary Tables 4 and 5 include statistics used to create diagram.
Post-hoc pairwise symmetry tests were conducted and adjusted p values were calculated using the Benjamini–Hochberg procedure (see Fig. 7 and Supplementary Table 4 ). In Fig. 7 the blue flows are significantly larger than the corresponding flows in the converse direction. There was a significant change from participants selecting “No, definitely not,” before intervention to selecting “Unsure, lean no” after seeing the CDC information. After seeing the RRT, there was a significant change from selecting “No, definitely not,” to selecting “Unsure, lean yes” as well as from “Unsure, lean no” to “Unsure, lean yes” in both the May and November surveys. Additionally, in November there was a significant change from “No definitely not” to “Unsure, lean no” after seeing the RRT. After seeing the CDC information, the percentage of people who claimed they would “definitely not” be vaccinated decreased from 25.3 to 16.1%. After seeing the RRT, the percentage of people who claimed they would “definitely not” be vaccinated decreased from 25.3 to 16.3% in May and from 25.2 to 15.4% in December (see Supplementary Table 5 for confidence intervals for percentages). Although the RRT had a similar impact as the CDC on reduction in participants who responded “No, definitely not”, only participants exposed to the RRT had a statistically significant increase in responses of “Unsure, lean yes”.
It is important to empower people to assess the risks and benefits of vaccination in a way that is evidence-based, mathematically rigorous, and consistent with real-world data. Interventions must be designed with drivers of vaccine hesitancy in mind to be successful 15 . The RRT is tailored to address concerns about safety and efficacy, and we recommend using the RRT as part of an educational program that considers multiple factors driving vaccine hesitancy.
Consistent with previous studies 24 , the extent to which individuals perceived risks and benefits associated with vaccination emerged as an important factor in predicting COVID-19 vaccine hesitancy. The regression model predicted that people who were more concerned with risks associated with infection are more willing to accept future vaccinations, and people who are more concerned with the risks associated with vaccination are less willing to accept additional vaccinations. People who are uncertain or do not believe vaccination reduces the risk of serious outcomes from infection are less willing to receive future vaccinations. Further, many participants, including those with vaccinations, dramatically overestimated their percent risk of a serious adverse outcome to vaccination and the number of U.S. citizens who have died from vaccination. The combination of participants’ difficulties in assessing risk and the strength of the relationship between risk perceptions and vaccination intent suggests that education around risk has the potential to reduce vaccine hesitancy.
Because most people have limited ability to interpret percentages and decimals in health contexts, careful design of communication regarding numerical information is critical 66 . We designed the RRT to convey the relative risk of COVID-19 vaccination versus infection and the efficacy of vaccination in a way that allowed the general population to compare and comprehend the relative sizes of percentages. The CDC website also provides information about the efficacy of vaccination and the low risk posed by vaccination; however, the information often appears in formats (e.g., fractions and Cartesian coordinate systems) that are known in mathematics education to be hard to understand 30 , 32 , 79 , 80 . As such, it was not surprising that individuals shown the images from the CDC website did not have a statistically significant change in belief about relative risk even though their initial belief misaligned with the numerical information provided. In contrast, the RRT was more effective in changing participants’ beliefs about the relative risk of COVID-19 infection and vaccination. After seeing the RRT, there was a statistically significant shift from responding “infection and vaccination are equally risky” or “I don’t know” to “infection is riskier.”
Both the CDC and RRT had a positive effect on intent to accept COVID-19 vaccination. Even though both the CDC and the RRT conveyed that there are rare but serious risks associated with COVID-19 vaccination, there were no statistically significant decreases in intent to vaccinate. Both conveyed that vaccination reduced risk, but vaccinated individuals could still have severe outcomes from infection. This finding is useful because of the ethical importance of communicating honestly about the magnitude of a health intervention’s effectiveness along with the risks of an intervention to the public 81 , 82 .
It is challenging to design an online intervention that results in a change in vaccination intent, and many (but not all) interventions studied had no statistically significant impact or had impact only in some subgroups 75 , 83 , 84 , 85 , 86 , 87 , 88 . A few interventions had positive statistically significant impact on vaccine hesitancy 13 , 89 , 90 , 91 . A 2023 meta-analysis of 71 behavioral interventions targeting vaccine hesitancy found a small, but statistically significant, overall effect size 92 . Although the RRT and CDC information was effective at increasing intent to vaccinate, it did not significantly increase the number of people who were “definitely” intending to accept a vaccine. These gains in intention to vaccinate are still noteworthy for an online intervention that took participants on average between nine and ten minutes. The most effective educational interventions about vaccines used multiple strategies 15 , and we suspect, based on our interviews on the RRT, that one-on-one conversations using the RRT would better support decision making. Attempts to address misinformation about the COVID-19 vaccines have been most effective when using the following strategies: conveying the weight of evidence, utilizing humor, tailoring communications to target audiences, and incorporating warnings about misinformation 9 .
We also suspect that one-on-one conversations about relative risk with a trusted source could increase the impact of the RRT and CDC information because trust in government, health care providers, and the scientific process is related to vaccine hesitancy 93 . We acknowledge that mistrust in health care organizations and governments has a valid historical rationality, given prior U.S. government atrocities done in the name of medical research, especially against minoritized groups 93 . Although participants were provided links to the peer-reviewed sources on the RRT and told that the RRT appeared on national television and in the Scientific American , we understand that an online tool is not necessarily a highly credible source. After seeing either the CDC or RRT, we asked participants if the information seemed trustworthy. After seeing the RRT tool 81.7% (May) and 78% (November) responded “Yes, definitely” or “Unsure, lean yes.” In May, 72.4% of participants assigned to the CDC responded “Yes, definitely” or “Unsure, lean yes.” This study does not analyze the relationship between trust in information and change in intent after seeing information or the impact of information when conveyed by a trusted source; however, this is an important future consideration.
Several limitations impact the generalizability and applicability of research. The sample, while diverse, only includes U.S. adults with computer access who self-selected to participate in online surveys for monetary compensation. Although previously found to be reflective of the general U.S. population, research is ongoing about the representativeness of Prime Panels samples with regards to risk perceptions and health decision making 94 . Participants in our study provided similar percent risk estimates of hospitalization due to COVID-19 infection as participants in a larger, nationally representative survey of U.S. residents 95 . Paid online surveys allow for the collection of data from large groups, but it is impossible to guarantee all participants understood survey questions as intended or to draw strong conclusions about the reasons for their answers. Further, the COVID-19 global pandemic has been a continuously evolving health crisis since its onset in late 2019. The external influences on participants’ beliefs and decision making that we captured in our surveys are likely continually evolving, and this study does not attempt to quantify change in beliefs. We tested the RRT at two time points to gather stronger evidence of its effectiveness as opposed to studying change in beliefs over time. Finally, although the authors attempted to perform an unbiased a review of the data, our personal beliefs in the public good of widespread vaccination against COVID-19 may have introduced bias.
Early in the pandemic, a variety of risk calculators were rapidly created to help citizens understand COVID-19 risk and seen by millions of people 96 , 97 , 98 , 99 . Most widely-used COVID-19 risk calculators display people’s risk percentages without comparison to other risks. The risk percentages displayed are far lower than most U.S. residents’ estimates, and people struggle to make sense of small probabilities 44 . The research from this study of the RRT demonstrates how carefully communicating the relative risks of vaccination and infection, as well as designing communication tools with attention to prior research in mathematics education and risk communication, can reduce vaccine hesitancy.
Future directions for additional research are multifaceted. These include exploring the perceived trustworthiness of the RRT and the impact this has on effectiveness, testing the RRT in various real-world settings such as in-person with a healthcare provider, and measuring real-world outcomes to see if the RRT has an impact on the number of vaccinations received. It would be useful to compare the RRT across additional populations; a survey we conducted in South Korea showed the RRT had a larger impact in South Korea (in preparation). We also wonder about the impact of risk calculators portraying substantially lower risk estimates than users’ initial overestimates and whether this makes individuals more complacent about the risks of infection, as complacency about risk of disease is relevant to vaccine hesitancy 22 .
Because of the critical importance of vaccination for personal risk reduction and public health, alongside the ethical responsibility to disclose side effects of any medical intervention, additional research into and development of risk communication tools should be pursued.
Survey participants and sampling
Prime Panels are used to collect random human subjects data in multiple fields, including social and behavioral sciences 76 , 100 . By using Prime Panels, we were able to acquire a diverse and randomly selected sample from their participant pool, which is known to be reasonably representative of the U.S. population 76 . It should be noted that our sample had more women than the U.S. average, and a slightly different distribution of races than the U.S. as a whole. The average age of Prime Panel participants aligns with the U.S. average, and age significantly impacts COVID-19 risk. They were paid 1.50 USD for a survey that was completed on average in 9.1 min in May and 10.3 min in November. The payment, research procedures, and survey were approved by the University of Georgia Institutional Review Board with reference number PROJECT00002145. All research conducted followed the approved procedures and University of Georgia human subjects research guidelines and regulations. All participants were over 18 years old and gave informed consent before participating in research.
Surveying participants in May and November allowed us to determine if the RRT had a similar impact on a new sample of participants with 6 months more exposure to information. Public opinion about COVID-19 and its vaccine was highly politicized and shifted dramatically throughout the pandemic in the U.S. 101 . The safety and efficacy of a new bivalent booster was presented in Fall 2022 102 . Information about the risks of vaccination and new variants of COVID-19 were common in the news during those 6 months. For example, on October 7th, 2022 the state of Florida issued widely critiqued guidance recommending against COVID-19 mRNA vaccination in males ages 18 to 39 due to the risk of myocarditis caused by vaccination 103 .
Survey questions
Participants took a 29-question online survey. Participants were asked if they had been infected with COVID-19, how many COVID-19 vaccinations (if any) they had, and why they were vaccinated (V-1 to V-2). Nine questions asked participants about their perceptions of risk associated with COVID-19 infection and vaccination including if they thought vaccination decreased risk due to infection (RP-0 to RP-8). We knew from pilot surveys that many participants thought vaccination and infection were equally risky, so we added follow up questions to see if they thought equal numbers of people have died due to vaccination and infection to better understand what they meant by “equally risky.” One question was a mathematical word problem about disease involving finding 10% of 1000 (RL-1), and six questions were about demographics (D-1 to D-6). As part of the survey, participants were randomly assigned to see information about risks and benefits of vaccination from either the CDC or the RRT and were asked questions related to the intervention (RRT-1 to RRT-11 or CDC-1 to CDC-12).
The survey questions were inspired by previous international surveys 8 , 75 , online pilot surveys with small samples 45 , 46 , and our interviews with U.S., South Korean, and Kenyan residents about COVID-19 infection and vaccination risk 36 . See Supplementary Table 7 for dates, sizes and citations associated with pilot surveys. The analysis of the pilot survey informed decisions on questions to include in the survey of a larger sample. We categorized open-ended responses to questions on the pilot surveys to create multiple-choice options on the survey for this study (Supplementary Figs. 1 – 3 ). We also used similar questions (RP-0, RP-2) to another research group 8 , 104 who used an expert panel and comprehensive literature review to develop their 23-country survey on vaccine hesitancy. Their survey was used in the U.S. and informed by internally and externally validated surveys about COVID-19 105 . Additionally, some questions (V-1, RRT-11, and CDC-12) had similar wording as a prior study 75 that asked participants in the U.S. and U.K. about intent to be vaccinated before and after seeing misinformation. To keep the survey to a manageable length, we intentionally focused our questions on participants’ perceptions of vaccine safety and efficacy and collected basic demographic information relevant to vaccine hesitancy (age, race, ethnicity, gender, education level, and political beliefs). Participants were allowed to select a race or races, ethnicity, and gender from multiple choice options or write in their preference. Multiple choice options were designed to be inclusive and use bias-free language as recommended by APA. Since prior research 8 indicates that trust is an important factor in vaccine hesitancy, we asked a question about how trustworthy the participants found the CDC and the RRT information. Although access to vaccination is a critical global issue 106 , during the study period, COVID-19 vaccinations were provided free of charge by the U.S. government, regardless of insurance status, and thus we did not ask about access. We piloted the questions multiple times in interviews and small samples on Prime Panels and had experts in item design review the wording for clarity before the larger May and November samples. In order to use the most familiar wording, we used the term COVID-19 instead of SARS-COV-2 on survey questions.
CDC and RRT intervention in survey
In May individuals were randomly assigned to see similar (but not identical) information presented by the CDC or RRT. Information from both the CDC and the RRT images stated that there are serious but extremely rare adverse events after vaccination, but each presented the information using different representations of data. We used the CDC estimates of the risk of particular adverse events in the design of the RRT and graphed the percentages provided by the CDC for comparison with other risks. We focused participants on particular parts of the CDC website or the RRT by embedding screenshots of the most relevant information into the survey and asking questions about the images before providing participants with the links to the content online. See images in survey instrument in supplementary materials . In addition to images, participants were provided with a short video about the RRT and a link to a video by the CDC.
Information from the CDC included graphs of the rates of COVID-19 hospitalizations for vaccinated and unvaccinated adults, statements about how many times as many unvaccinated adults were hospitalized due to COVID-19 as vaccinated adults, and information about rare side effects of vaccination such as anaphylaxis, thrombosis, myocarditis, and pericarditis. The CDC information said the vaccines were safe and effective and had been given to hundreds of millions of people, and the CDC also explained that the booster shots can enhance or restore protection that wanes after time. In addition to being provided with images of and links to the CDC website, participants were asked to answer questions about the CDC information to encourage reading the information and to check for comprehension. For example, we asked “According to the CDC, which is more risky for a young, healthy adult?” underneath a screenshot of relevant information. The graphics used by the CDC were significantly more complicated to understand than those recommended for use in health communication 39 .
Survey participants assigned to the RRT received a link to the full tool, but the survey also included specific screenshots of the RRT designed to highlight the relative risk of vaccination and infection and the reduction in risk due to vaccination. For example, we asked participants to compare the risk of death from COVID-19 if infected for a vaccinated and unvaccinated 76-year-old. The graphic included the absolute risk if infected but was designed to help people focus on relative risk. Another question asked participants to use an image of the RRT to compare the risk of hospitalization if infected with COVID-19 to the chance of a severe allergic reaction to the vaccine. Finally, we asked participants a question based on an image showing the risk of being hospitalized if infected for someone vaccinated over 6 months ago, someone vaccinated and boosted, and someone who is unvaccinated. Unlike the CDC website, the RRT provided no direct medical advice. The RRT did not say vaccination was safe and effective, provided no recommendations to get vaccinated or boosted, and did not recommend any particular behaviors with regard to mitigating COVID-19 infection risk.
After viewing the assigned intervention, we asked participants what they thought was riskier, if the information they saw was trustworthy, and whether they wanted to be vaccinated in the future. Based on these results, we found the RRT to be more effective than the CDC materials, so in November 2022, we assigned everyone to the RRT to gather further data about effectiveness.
Refinement of the relative risk tool
In April and May of 2020, we interviewed 25 U.S. and 7 South Korean citizens about their mathematical understandings of quantitative representations of COVID-19 data that were ubiquitous in the media 36 . We conducted additional interviews from November 2020 to June 2022 and used a design-based research methodology 107 to iteratively improve the RRT by incorporating feedback from the interviews and experts in public health and mathematics education. We conducted 14 interviews with U.S. residents, 10 with South Korean residents, and 9 with Kenyan residents. The interview sample was not representative, but it was diverse with respect to age, education, political affiliation, citizenship, income, and profession, which allowed us to iteratively improve the RRT. In the interviews we conducted after adding information about risks and efficacy of vaccination to the RRT, we found viewing the relative risk of vaccination versus infection and the reduction in risk due to vaccination resulted in people being more willing to be vaccinated.
We knew from prior research, interviews, and pilot surveys that citizens thought a risk of death of 1% or 2% was small, so we intentionally designed the RRT to help them understand the magnitude of those risks by comparing the risks to other situations. We knew from prior research 58 and our interviews on RRT that some people think a decimal such as 0.0002 is larger than a decimal such as 0.02 because it has more digits, mirroring the fact that among whole numbers, larger numbers have more digits. Even highly educated people can struggle to determine if a 1, 5, or 10% risk of getting a disease is larger 59 . Previous research shows people especially struggle to make sense of low-probability risks 44 .
Estimating and communicating risks about COVID-19 accurately is complicated by several issues. One, the risk due to COVID-19 infection increases exponentially with age; for instance, an average 85-year-old is about 19,000 times as likely to die if infected than a 10-year-old 37 . Two, although it is possible to roughly compare the likelihood of one adverse outcome due to infection to one (different) adverse outcome due to vaccination, it is essentially impossible to compare the likelihood and seriousness of all risks posed by infection to all risks posed by vaccination. For instance, a severe allergic reaction to vaccination might be more or less serious than a hospitalization due to infection.
There are limitations of the statistical estimates provided on the RRT. Vaccination risk estimates are based on the information available and vary for different strains of SARS-COV-2, the differences of efficacy of vaccinations based on the strain, time since vaccination, and immune system response. COVID-19 infection risks are provided based on peer reviewed studies; however, the risk of infection changed over the course of the pandemic as knowledge about COVID-19 evolved and more treatment recommendations became available as well as with variations in local health care system capacity and preparedness. The risk percentages are averages, but there are differences in risk for people with various medical conditions, and only a few specific medical conditions are on the RRT. Further, it is much more challenging to quantify the likelihood and level of impact of non-acute risks such as long-COVID, the effectiveness of vaccination against long-COVID, and long-COVID-like symptoms triggered by vaccination 108 , 109 , 110 . The risk of death from COVID-19 is based on a particular population used to create the model and varies by access to medical care and general health of a population. In designing the RRT, we were constantly faced with the difficulty of providing risk estimates in an easy-to-understand manner, knowing that various peer-reviewed studies had different estimates.
We determined the sample size for the May 2022 survey using a power analysis for binary logistic regression. This was calculated with G*Power software. We chose a larger sample size in November because there were some interesting relationships in subgroups of original vaccination intent that we wanted to investigate in a larger sample. The sample size was much larger than needed to detect the relationships we focused on, but is not large enough to study the differential impact of RRT in different subgroups.
To create a model to predict vaccination status, which involves a series of vaccine shots, we employed use of ordinal logistic regression for each of the surveys. We used the model:
\(logit\left(P\left(Y\le j\right)\right)={\beta }_{j0}+{\beta }_{j1}{x}_{1}\ldots {\beta }_{jp}{x}_{p}\) for \(j=1,\dots ,J-1\) levels of the ordinal variable and p variables. Analyses were conducted using SPSS version 28. We first included responses to 13 survey questions as predictor variables in the model. Decisions about which question to include in the model were inspired from our pilot data, our observations in interviews, and from other research on vaccination hesitancy (see supplementary materials for the survey). The six survey questions about risk included questions about how concerned participants were about both vaccination and infection, what they thought was more risky, how many people they thought had died from either vaccination and from infection, and whether or not they thought the vaccination reduced risk of serious outcomes from infection. The six demographic predictors were race, ethnicity, age, gender, political party, and education level. Finally, we included responses to one question about previous COVID-19 infection as a predictor. To increase parsimony, we reduced the number of variables based on statistical significance in the first model and prior empirically demonstrated relationships (e.g., political beliefs and vaccination status). Relationships between intent to vaccinate and the independent variables are reported as adjusted odds ratios and 95% confidence intervals. The assumption of proportional odds was tested for each data set using the test of parallel lines. In each case, the test was not significant, indicating that the coefficients are the same across all response categories. The variance inflation factor (VIF) was calculated for each variable to test for multicollinearity. The assumption of no multicollinearity is met with VIF values below 3 for each variable.
The McNemar–Bowker test 78 of symmetry was used to analyze the change in respondent’s perceptions of risk of vaccination and infection, as well as intent to receive a COVID-19 vaccination. These analyses were conducted using R 4.3.0 and the rcompanion package.
Data availability
The data from the May 2022 and November 2022 survey are available to download at http://www.covidtaser.com . Some participants took fewer than 3 min to complete the survey. After group discussion, the authors decide to exclude these responses from the analysis because such participants did not take sufficient time to read the questions and look at the CDC or RRT information.
Code availability
The code for the McNemar–Bowker tests and the data used in SPSS 28 to create the regression model is available at http://www.covidtaser.com .
Sallam, M. COVID-19 vaccine hesitancy worldwide: A concise systematic review of vaccine acceptance rates. Vaccines 9 , 160 (2021).
Article CAS PubMed PubMed Central Google Scholar
Attwell, K., Hannah, A. & Leask, J. COVID-19: Talk of ‘vaccine hesistancy’ lets govenerments off the hook. Nature 602 , 574–577 (2022).
Article ADS CAS PubMed Google Scholar
Bussink-Voorend, D., Hautvast, J. L., Vandeberg, L., Visser, O. & Hulscher, M. E. A systematic literature review to clarify the concept of vaccine hesitancy. Nat. Hum. Behav. 6 , 1634–1648 (2022).
Article PubMed Google Scholar
Our World in Data: Coronavirus (COVID-19) Vaccinations . https://ourworldindata.org/covid-vaccinations (2023).
Mathieu, E. et al. A global database of COVID-19 vaccinations. Nat. Hum. Behav. 5 , 947–953 (2021).
Centers for Disease Control and Prevention. COVID Data Tracker. https://covid.cdc.gov/covid-data-tracker (2023).
Moehring, A. et al. Providing normative information increases intentions to accept a COVID-19 vaccine. Nat. Commun. 14 , 126 (2023).
Article ADS CAS PubMed PubMed Central Google Scholar
Lazarus, J. V. et al. Revisiting COVID-19 vaccine hesitancy around the world using data from 23 countries in 2021. Nat. Commun. 13 , 3801 (2022).
Whitehead, H. S., French, C. E., Caldwell, D. M., Letley, L. & Mounier-Jack, S. A systematic review of communication interventions for countering vaccine misinformation. Vaccine 41 , 1018–1034 (2023).
Article PubMed PubMed Central Google Scholar
Li, P. C. et al. Impact of an education intervention on COVID-19 vaccine hesitancy in a military base population. Mil. Med. 187 , e1516–e1522 (2022).
Article Google Scholar
Abdel-Qader, D. H. et al. Pharmacists-physicians collaborative intervention to reduce vaccine hesitancy and resistance: A randomized controlled trial. Vaccine: X 10 , 100135 (2022).
PubMed Google Scholar
Talmy, T., Cohen, B., Nitzan, I. & Ben Michael, Y. Primary care interventions to address COVID-19 vaccine hesitancy among Israel Defense Forces soldiers. J. Community Health 46 , 1155–1160 (2021).
Johnson, V. et al. The ‘Fauci Effect’: Reducing COVID-19 misconceptions and vaccine hesitancy using an authentic multimodal intervention. Contemp. Educ. Psychol. 70 , 102084 (2022).
Freeman, D. et al. COVID-19 vaccine hesitancy in the UK: The Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychol. Med. 52 , 3127–3141 (2022).
Jarrett, C., Wilson, R., O’Leary, M., Eckersberger, E. & Larson, H. Strategies for addressing vaccine hesitancy—A systematic review. Vaccine 33 , 4180–4190. https://doi.org/10.1016/j.vaccine.2015.04.040 (2015).
Peters, M. D. Addressing vaccine hesitancy and resistance for COVID-19 vaccines. Int. J. Nurs. Stud. 131 , 104241 (2022).
EURO Working Group on Vaccine Communications (2011).
Kumar, S., Shah, Z. & Garfield, S. Causes of vaccine hesitancy in adults for the influenza and COVID-19 vaccines: A systematic literature review. Vaccines 10 , 1518 (2022).
Dror, A. A. et al. Vaccine hesitancy: The next challenge in the fight against COVID-19. Eur. J. Epidemiol. 35 , 775–779 (2020).
Troiano, G. & Nardi, A. Vaccine hesitancy in the era of COVID-19. Public Health 194 , 245–251 (2021).
Article CAS PubMed Google Scholar
Pires, C. Global predictors of COVID-19 vaccine hesitancy: A systematic review. Vaccines 10 , 1349 (2022).
Betsch, C. et al. Beyond confidence: Development of a measure assessing the 5C psychological antecedents of vaccination. PLoS One 13 , e0208601 (2018).
Warren, G. W. & Lofstedt, R. COVID-19 vaccine rollout risk communication strategies in Europe: A rapid response. J. Risk Res. 24 , 369–379. https://doi.org/10.1080/13669877.2020.1870533 (2021).
Wong, J. C. S. & Yang, J. Z. Comparative risk: Dread and unknown characteristics of the COVID-19 pandemic versus COVID-19 vaccines. Risk Anal. 42 , 2214–2230 (2022).
Eskola, J., Duclos, P., Schuster, M. & MacDonald, N. E. How to deal with vaccine hesitancy?. Vaccine 33 , 4215–4217 (2015).
Lee, M. & You, M. Direct and indirect associations of media use with COVID-19 vaccine hesitancy in South Korea: Cross-sectional web-based survey. J. Med. Internet Res. 24 , e32329 (2022).
Nguyen, L. H. et al. Self-reported COVID-19 vaccine hesitancy and uptake among participants from different racial and ethnic groups in the United States and United Kingdom. Nat. Commun. 13 , 636 (2022).
Fajar, J. K. et al. Global prevalence and potential influencing factors of COVID-19 vaccination hesitancy: A meta-analysis. Vaccines 10 , 1356 (2022).
Solís Arce, J. S. et al. COVID-19 vaccine acceptance and hesitancy in low-and middle-income countries. Nat. Med. 27 , 1385–1394 (2021).
Steffe, L. P. & Olive, J. Children’s Fractional Knowledge (Springer, 2010).
Book Google Scholar
Bradshaw, L., Izsák, A., Templin, J. & Jacobson, E. Diagnosing teachers’ understandings of rational numbers: Building a multidimensional test within the diagnostic classification framework. Educ. Meas. Issues Pract. 33 , 2–14 (2014).
Moore, K. C. In Transfer of Learning: Progressive Perspectives for Mathematics Education and Related Fields (eds Hohensee, C. & Lobato, J.) 145–171 (Springer, 2021).
Chapter Google Scholar
Moore, K. C. & Thompson, P. W. In Proceedings of the 18th Meeting of the MAA Special Interest Group on Research in Undergraduate Mathematics Education (eds Fukawa-Connelly, T. et al. ) 782–789 (RUME, 2015).
Google Scholar
Konold, C. Informal conceptions of probability. Cogn. Instr. 6 , 59–98 (1989).
Joshua, S. et al. Exploring relative size with relative risk. Math. Teach. Learn. Teach. PK-12 115 , 339–350 (2022).
Yoon, H. et al. United States and South Korean citizens’ interpretation and assessment of COVID-19 quantitative data. J. Math. Behav. 62 , 100865 (2021).
Herrera-Esposito, D. & de Los Campos, G. Age-specific rate of severe and critical SARS-CoV-2 infections estimated with multi-country seroprevalence studies. BMC Infect. Dis. 22 , 311 (2022).
Dubé, E. et al. Vaccine hesitancy: An overview. Hum. Vaccines Immunother. 9 , 1763–1773 (2013).
Ancker, J. S., Senathirajah, Y., Kukafka, R. & Starren, J. B. Design features of graphs in health risk communication: A systematic review. J. Am. Med. Inform. Assoc. 13 , 608–618 (2006).
Collins, A., Florin, M.-V. & Renn, O. COVID-19 risk governance: Drivers, responses and lessons to be learned. J. Risk Res. 23 , 1073–1082 (2020).
Covello, V. T. Social and behavioral research on risk: Uses in risk management decisionmaking. Environ. Int. 10 , 541–545 (1984).
Fischhoff, B. Risk perception and communication unplugged: Twenty years of process. Risk Anal. 15 , 137–145 (1995).
Wood, M. M. et al. Communicating actionable risk for terrorism and other hazards ⋆ . Risk Anal. 32 , 601–615 (2012).
Stone, E. R., Yates, J. F. & Parker, A. M. Effects of numerical and graphical displays on professed risk-taking behavior. J. Exp. Psychol. Appl. 3 , 243 (1997).
Yoon, H. et al. in 44th Annual Meeting of the North American Chapter of the International Group for the Psychology of Mathematics Education. (eds A. Lischka et al. ) 862–871.
Gong, M., Horne, D., Yoon, H. & Byerley, C. In 25th Annual Conference on Research in Undergraduate Mathematics Education.
Fischhoff, B. The realities of risk-cost-benefit analysis. Science 350 , 6516 (2015).
Article ADS Google Scholar
Fischhoff, B. & Broomell, S. B. Judgment and decision making. Annu. Rev. Psychol. 71 , 331–355 (2020).
Siegrist, M. & Árvai, J. Risk perception: Reflections on 40 years of research. Risk Anal. 40 , 2191–2206 (2020).
Behr, M., Lesh, R., Post, T. & Silver, E. In Acquisition of Mathematics Concepts and Processes (eds Lesh, R. & Landau, M.) 91–125 (Academic Press, 1983).
Konold, C. In Radical Constructivism in Mathematics Education. Mathematics Education Library Vol. 7 (ed. Von Glasersfeld, E.) 139–156 (Springer, Paris, 1991).
Probabilistic Thinking: Presenting Plural Perspectives (Springer, 2014).
Batanero, C., Chernoff, E. J., Engel, J., Lee, H. S. & Sánchez, E. Research on Teaching and Learning Probability (Springer, 2016).
Byerley, C. & Thompson, P. W. Secondary mathematics teachers’ meanings for measure, slope, and rate of change. J. Math. Behav. 48 , 168–193 (2017).
Kollosche, D. & Meyerhöfer, W. COVID-19, mathematics education, and the evaluation of expert knowledge. Educ. Stud. Math. 108 , 401–417 (2021).
Bloom, M. A., Fuentes, S. Q. & Crocker, J. How the COVID-19 pandemic reveals gaps in science and mathematics instruction. Electron. J. Res. Sci. Math. Educ. 24 , 1–6 (2020).
Garfield, J. & Ahlgren, A. Difficulties in learning basic concepts in probability and statistics: Implications for research. J. Res. Math. Educ. 19 , 44–63 (1988).
Carpenter, T. P., Corbitt, M. K., Kepner, H. S., Lindquist, M. M. & Reys, R. Results of the second NAEP mathematics assessment: Secondary school. Math. Teach. 73 , 329–338 (1980).
Lipkus, I. M., Samsa, G. & Rimer, B. K. General performance on a numeracy scale among highly educated samples. Med. Decis. Making 21 , 37–44 (2001).
Cokely, E. T., Galesic, M., Schulz, E., Ghazal, S. & Garcia-Retamero, R. Measuring risk literacy: The Berlin numeracy test. Judgm. Decis. Making 7 , 25–47 (2012).
Slovic, P. & Weber, E. U. Regulation of Toxic Substances and Hazardous Waste (Foundation Press, 2013).
Fischhoff, B., Bostrom, A. & Quadrel, M. J. Risk perception and communication. Annu. Rev. Public Health 14 , 183–203 (1993).
Slovic, P. Perception of risk. Science 236 , 280–285 (1987).
Fischhoff, B., Slovic, P. & Lichtenstein, S. In The Analysis of Actual Versus Perceived Risks Vol. 1 (eds Covello, V. T. et al. ) 235–249 (Springer, 1983).
Slovic, P. & Peters, E. Risk perception and affect. Curr. Dir. Psychol. Sci. 15 , 322–325 (2006).
Ancker, J. S. & Kaufman, D. Rethinking health numeracy: A multidisciplinary literature review. J. Am. Med. Inform. Assoc. 14 , 713–721 (2007).
Peters, E. Beyond comprehension: The role of numeracy in judgments and decisions. Curr. Dir. Psychol. Sci. 21 , 31–35 (2012).
Kahneman, D., Slovic, S. P., Slovic, P. & Tversky, A. Judgment Under Uncertainty: Heuristics and Biases (Cambridge University Press, 1982).
Tversky, A. & Kahneman, D. Judgment under uncertainty: Heuristics and biases. Science 185 , 1124–1131 (1974).
Ginsburg, K. R. et al. National young-driver survey: Teen perspective and experience with factors that affect driving safety. Pediatrics 121 , e1391–e1403 (2008).
Mueller, B. New York Times (The New York Times Company, 2022).
Martinez, M. W. et al. Prevalence of inflammatory heart disease among professional athletes with prior COVID-19 infection who received systematic return-to-play cardiac screening. JAMA Cardiol. 6 , 745–752 (2021).
Montgomery, J. et al. Myocarditis following immunization with mRNA COVID-19 vaccines in members of the US military. JAMA Cardiol. 6 , 1202–1206 (2021).
O’Connor, A. et al. International Patient Decision Aid Standards (IPDAS) Collaboration (2005).
Loomba, S., de Figueiredo, A., Piatek, S. J., de Graaf, K. & Larson, H. J. Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nat. Hum. Behav. 5 , 337–348 (2021).
Chandler, J., Rosenzweig, C., Moss, A. J., Robinson, J. & Litman, L. Online panels in social science research: Expanding sampling methods beyond Mechanical Turk. Behav. Res. Methods 51 , 2022–2038 (2019).
Shimabukuro, T. & Nair, N. Allergic reactions including anaphylaxis after receipt of the first dose of Pfizer-BioNTech COVID-19 vaccine. JAMA 325 , 780–781. https://doi.org/10.1001/jama.2021.0600 (2021).
Bowker, A. H. A test for symmetry in contingency tables. J. Am. Stat. Assoc. 43 , 572–574. https://doi.org/10.2307/2280710 (1948).
Mullis, I. V., Dossey, J. A., Owen, E. H. & Phillips, G. W. The State of Mathematics Achievement: NAEP’s 1990 Assessment of the Nation and the Trial Assessment of the States (National Center for Education Statistics, 1991).
Carlson, M. P., Madison, B. & West, R. D. A study of students’ readiness to learn calculus. Int. J. Res. Undergrad. Math. Educ. 1 , 209–233 (2015).
de Barra, M. & Brown, R. C. Public-health communication should be more transparent. Nat. Hum. Behav. 7 , 662–664 (2023).
Brown, R. & de Barra, M. A taxonomy of non-honesty in public health communication. Public Health Ethics 16 , 86–101 (2023).
Freeman, D. et al. Effects of different types of written vaccination information on COVID-19 vaccine hesitancy in the UK (OCEANS-III): A single-blind, parallel-group, randomised controlled trial. Lancet Public Health 6 , e416–e427 (2021).
Batteux, E., Mills, F., Jones, L. F., Symons, C. & Weston, D. The effectiveness of interventions for increasing COVID-19 vaccine uptake: A systematic review. Vaccines 10 , 386 (2022).
Schwarzinger, M. & Luchini, S. Addressing COVID-19 vaccine hesitancy: Is official communication the key?. Lancet Public Health 6 , e353–e354 (2021).
Yuan, S. & Chu, H. Vaccine for yourself, your community, or your country? Examining audiences’ response to distance framing of COVID-19 vaccine messages. Patient Educ. Couns. 105 , 284–289 (2022).
Reddinger, J. L., Levine, D. & Charness, G. Can targeted messages reduce COVID-19 vaccination hesitancy? A randomized trial. Prev. Med. Rep. 29 , 101903 (2022).
Thorpe, A. et al. Communicating about COVID-19 vaccine development and safety. PLoS One 17 , e0272426 (2022).
Mottelson, A. et al. A self-administered virtual reality intervention increases COVID-19 vaccination intention. Vaccine 39 , 6746–6753 (2021).
Plechatá, A. et al. Experiencing herd immunity in virtual reality increases COVID-19 vaccination intention: Evidence from a large-scale field intervention study. Comput. Hum. Behav. 139 , 107533 (2023).
Okuhara, T. et al. Encouraging COVID-19 vaccination via an evolutionary theoretical approach: A randomized controlled study in Japan. Patient Educ. Couns. 105 , 2248–2255 (2022).
Huang, Y., Huang, X. & Yu, R. The effectiveness of nonfinancial interventions and monetary incentives on COVID-19 vaccination: A meta-analysis. Health Psychol. 42 , 411–424 (2023).
Bajaj, S. S. & Stanford, F. C. Beyond Tuskegee—Vaccine distrust and everyday racism. N. Engl. J. Med. 384 , e12 (2021).
Sharma, A. et al. Differences in demographics and behaviors across two web-based survey platforms: Observations from a study of risk perceptions of heated tobacco products (HTPs). Prev. Med. Rep. 33 , 102194 (2023).
Rothwell, J. & Witters, D. U.S. Adults' Estimates of COVID-19 Hospitalization Risk . https://news.gallup.com/opinion/gallup/354938/adults-estimates-covid-hospitalization-risk.aspx (2021).
StarThower. COVIDAge Risk Calculator . https://calculator.covid-age.com (2020).
Nexoid. COVID-19 Survival Calculator . https://www.covid19survivalcalculator.com/en/research (2023).
Mathematica. 19 and Me: Covid-19 Risk Score Calculator . https://www.mathematica.org/dataviz/19-and-me-covid-19-risk-score-calculator (2021).
Chande, A. et al. Real-time, interactive website for US-county-level COVID-19 event risk assessment. Nat. Hum. Behav. 4 , 1313–1319 (2020).
Litman, L., Robinson, J. & Abberbock, T. TurkPrime.com: A versatile crowdsourcing data acquisition platform for the behavioral sciences. Behav. Res. Methods 49 , 433–442 (2017).
Bolsen, T. & Palm, R. Politicization and COVID-19 vaccine resistance in the US. Prog. Mol. Biol. Transl. Sci. 188 , 81–100 (2022).
Link-Gelles, R. et al. Early estimates of bivalent mRNA booster dose vaccine effectiveness in preventing symptomatic SARS-CoV-2 infection attributable to Omicron BA. 5–and XBB/XBB. 1.5-related sublineages among immunocompetent adults—Increasing Community Access to Testing Program, United States, December 2022–January 2023. Morb. Mortal. Wkly. Rep. 72 , 119 (2023).
Article CAS Google Scholar
Dyer, O. Covid-19: Florida’s surgeon general used “careless” research practice in recommending against vaccination, his university finds. BMJ 380 , 110 (2023).
Lazarus, J. V. et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 27 , 225–228 (2021).
Lazarus, J. V. et al. COVID-SCORE: A global survey to assess public perceptions of government responses to COVID-19 (COVID-SCORE-10). PLoS One 15 , e0240011 (2020).
Ye, Y. et al. Equitable access to COVID-19 vaccines makes a life-saving difference to all countries. Nat. Hum. Behav. 6 , 207–216 (2022).
Anderson, T. & Shattuck, J. Design-based research: A decade of progress in education research?. Educ. Res. 41 , 16–25 (2012).
Notarte, K. I. et al. Impact of COVID-19 vaccination on the risk of developing long-COVID and on existing long-COVID symptoms: A systematic review. eClinicalMedicine 53 , 101624 (2022).
Brodin, P. et al. Studying severe long COVID to understand post-infectious disorders beyond COVID-19. Nat. Med. 28 , 879–882 (2022).
Couzin-Frankel, J. & Vogel, G. Vaccines may cause rare, long covid-like symptoms. Science 375 , 364–366 (2022).
Download references
Acknowledgements
Dr. Kevin Moore, Dr. Anne Waswa, Dr. James Drimalla, and Alexandra Yon contributed to the creation and iterative improvement of the RRT. Ximeng Huang improved the graphic design of RRT. Dr. Katelyn Jetalina (Your Local Epidemiologist) contributed to improving the RRT by reviewing data related to immune compromised populations. Various experts on mathematical and statistical thinking provided feedback on RRT including Dr. Neil Hatfield, Dr. Amy Hackenberg, Dr. Leslie Steffe, Dr. Pat Thompson, Dr. Steven Boyce, and Dr. Halil Tasova. Evan Fimbres edited the manuscript. We disclose support for the research of this work from the National Science Foundation [DUE- 2032688] and University of Georgia Internal Research Grant.
Author information
Authors and affiliations.
Department of Mathematics, Science, and Social Studies Education, University of Georgia, Athens, 30606, USA
Cameron O’Neill Byerley, Dru Horne, Mina Gong & Heather Lavender
Department of Mathematics and Statistics, Cal Poly Pomona, Pomona, 91768, USA
Stacy Musgrave & Hyunkyoung Yoon
Department of Dermatology, University of Washington, Seattle, 98195, USA
Laura A. Valaas
Department of Mathematical Sciences, University of Arkansas, Fayetteville, 72701, USA
Brian Rickard
Department of Information Studies, University of Wisconsin-Milwaukee, Milwaukee, 53201, USA
Min Sook Park & Sukjin You
Department of Mathematics, University of Arizona, Tucson, 85721, USA
Alison Mirin
Yavapai Elementary School, Scottsdale, 85257, USA
Surani Joshua
You can also search for this author in PubMed Google Scholar
Contributions
C.B., M.G., D.H., S.M., L.V., B.R., A.M., and H.Y. contributed to writing, editing, and paper conceptualization. C.B., H.Y., S.J. M.P., S.Y., H.L., L.V., S.M. contributed to conceptualization, design, and iterative improvement of the RRT through qualitative research. L.V. (who is an MD and mathematics major) checked writing and RRT for medical accuracy. B.R., M.G., C.B. and D.H conducted statistical analysis. M.P., H.Y., M.G, C.B., S.J., and S.M. created and conducted the survey. H.Y., C.B., and S.J. secured NSF funding for creation of the RRT. S.Y. programmed the RRT. All authors approved the submitted version of this manuscript.
Corresponding author
Correspondence to Cameron O’Neill Byerley .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary information., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Byerley, C.O., Horne, D., Gong, M. et al. An effective COVID-19 vaccine hesitancy intervention focused on the relative risks of vaccination and infection. Sci Rep 14 , 7419 (2024). https://doi.org/10.1038/s41598-024-57841-1
Download citation
Received : 12 June 2023
Accepted : 22 March 2024
Published : 28 March 2024
DOI : https://doi.org/10.1038/s41598-024-57841-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Support Dal
- Current Students
- Faculty & Staff
- Family & Friends
- Agricultural Campus (Truro)
- Halifax Campuses
- Campus Maps
- Brightspace
Dalhousie University

- Student Life
- Media Centre
- DAL Magazine
Most Commented
News archive.
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
Cardiovascular risks and COVID‑19: New research confirms the benefits of vaccination
Glen Pyle - April 1, 2024
Glen Pyle , Member, IMPART (Initiative on Medication Management, Policy Analysis, Research & Training), Dalhousie University
COVID-19 is a respiratory disease. Yet, from the earliest days of the pandemic, the cardiovascular risks associated with SARS-CoV-2 infection were clear: individuals with severe cases of COVID-19 often died from cardiovascular complications, and those with pre-existing cardiovascular disease were more likely to have severe illness or die.
In short, the cardiovascular system has played a central role in COVID-19 since the beginning.
It is not surprising that as debate over COVID-19 and vaccines flared that cardiovascular disease was a central issue . Those opposed to vaccination often make claims of cardiovascular risks that exceed any benefits. But when data on COVID-19, vaccines and cardiovascular health are reviewed, the conclusions are clear: vaccines are safe and effective at reducing the cardiovascular complications that are a hallmark of COVID-19.
Hot off the presses

A new study of 20.5 million people in the United Kingdom, Spain and Estonia used electronic health records to determine how COVID-19 vaccines affect cardiovascular complications following SARS-CoV-2 infection. Roughly the same number of vaccinated and unvaccinated subjects were included, and the vaccinated group consisted of people who received at least one of the AstraZeneca, Pfizer, Moderna or Janssen vaccines.
The study found that common cardiovascular complications of COVID-19 — including blood clots, stroke, arrhythmias and heart attacks — were substantially reduced in the vaccinated group, with protective effects lasting up to a year after vaccination.
Bigger picture
While this most recent study represents one of the most comprehensive investigations into the cardiovascular benefits of COVID-19 vaccination, its findings are consistent with earlier, smaller studies.
A 2022 study of 231,037 people found two doses of COVID-19 vaccines reduced the risk of stroke and heart attack up to four months after a breakthrough infection.
A subsequent study of 1.9 million people found that while two doses of the mRNA vaccines or one dose of the Johnson & Johnson vaccine protected against major cardiovascular events following COVID-19, even a single dose of the mRNA vaccines offered some benefit in reducing the risk of cardiovascular complications.
Health-care decisions require a weighing of the risk and benefits of treatments, and for COVID-19 vaccines the low cardiovascular risks favour vaccination. A study of over four million vaccinated Australians found no increase in sudden cardiac death. Even patients with pre-existing heart failure do not have an increased risk of worsening heart failure, myocarditis, or blood clots following vaccination.
Weighing the risks
Although the safety of COVID-19 vaccines is well-established, it does not mean there are no risks. A review of 99 million individuals in the Global Vaccine Data Network confirmed earlier studies that found an increased risk of myocarditis and pericarditis, which is seen primarily in young males — historically the group most at risk for myocarditis before COVID-19 emerged.
While individuals at higher risk for these complications should consult with their health-care providers in making decisions about vaccination, it should be noted that the risk for myocarditis and pericarditis is generally higher with COVID-19, even in this cohort.
Studies have also found that extending the time between first and second doses of the COVID-19 mRNA vaccines beyond the initially recommended three-week interval decreases the risk of myocarditis . Furthermore, post-vaccine myocarditis tends to be transient with very good recovery and is less severe than that associated with COVID-19.

The risk of myocarditis in young people has led some to claim that the benefits of COVID-19 vaccines are negated when stacked up against the chance of heart inflammation. A statement from the American Heart Association confirms that the risks of cardiovascular complications in young people with more mild cases of COVID-19 (symptoms lasting less than four days) are low, but notes that there are concerning signs for those who experience more severe illness with infection.
Furthermore, other cardiovascular risks associated with infection must be considered in weighing risks and benefits. These include multisystem inflammatory syndrome or “MIS-C” and cardiac arrhythmias — a far more common risk of COVID-19 than myocarditis.
Finally, the claim that COVID-19 is harmless in children is not true: in Canada COVID-19 is the sixth leading cause of death for children aged one to 14 years, and tenth for people 15 to 19 years old. Overall, studies find that even in young people the benefits of vaccination exceed the risks , particularly when it comes to cardiovascular disease.
Take to heart
This article is republished from The Conversation under a Creative Commons license. Read the original article .
Dal News welcomes discussion from members of the Dalhousie community and beyond, but urge comment writers to be respectful and refrain from personal attacks. False or unsubstantiated allegations, libellous statements and offensive language are not allowed. External links must be appropriate and relevant to the subject being discussed.
We encourage commenters to use their real first and last names.
Please note that comments that appear on the site are not the opinion of Dal News or Dalhousie University but only of the comment writer. The editors reserve the right to post, or not to post comments, edit or not edit, at their discretion.
Halifax, Nova Scotia, Canada B3H 4R2 1-902-494-2211
Agricultural Campus Truro, Nova Scotia, Canada B2N 5E3 1-902-893-6600
- Campus Directory
- Student Career Services
- Employment with Dalhousie
- For Parents
- For Employers
- Privacy Statement
- Terms of Use
Dalhousie University Halifax, Nova Scotia, Canada B3H 4R2 1.902.494.2211
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
New Research Supports an Annual COVID Vaccine Plan
Photo Illustration by Amelia Manley for Verywell Health; Getty Images
Key Takeaways
- New research suggests that most people will benefit from an annual COVID-19 vaccine.
- Certain groups may need two vaccines a year.
- Doctors said more needs to be done to encourage people to get vaccinated.
There have been a lot of changes in recommendations around COVID-19 vaccines over the past few years, making it difficult to know whether you need another shot and how often you should get one. Now, new research from the Yale School of Public Health has recommendations for a vaccine cadence moving forward.
The study, which was published in the Annals of Internal Medicine , used computer simulations to compare five annual vaccination strategies and predict outcomes. The researchers discovered that getting an annual COVID vaccine with a second dose for adults over 50 and children under 2 was linked to fewer hospitalizations, fewer deaths, and less healthcare spending each year.
This isn’t revolutionary: The Centers for Disease Control and Prevention (CDC) already proposed similar interim guidelines, although they’re slightly different. But it backs up existing recommendations around COVID vaccines.
Is an Annual COVID Shot Realistic?
While the COVID vaccine was relatively popular when it first rolled out, many people haven’t gotten the most recent 2023-2024 updated version . Current data show that less than 23% of the adult population in the U.S. has gotten the updated vaccine. The numbers are even lower in children; less than 14% of children aged 6 months to 17 years have received the updated vaccine.
Current recommendations from the CDC say that people 65 and up should receive an additional dose of the COVID-19 vaccine, but the new Yale study suggests it would be more effective if people did this starting at age 50.
Given how few people have gotten the updated vaccine to begin with, do doctors actually think the public will embrace this?
“This sounds familiar and it rather mirrors what, by and large, is happening to date,” William Schaffner, MD , an infectious disease specialist and professor at the Vanderbilt University School of Medicine, told Verywell. While older people have been the most likely to follow recommendations around COVID vaccines, Schaffner said it’s been tricky to get parents on board.
“The vast majority of parents have not taken their child in to be vaccinated with even their first dose,” he said. “Pediatricians are going to have to do a lot of friendly persuasion to get that group vaccinated. Parents just do not see the current Omicron variants distinctly impacting children.”
If a new concerning COVID-19 variant emerges, though, recommendations could change, Schaffner said.
What About People Who Are Immunocompromised?
The study didn’t address the ideal vaccine cadence for people who are immunocompromised. If you have a condition that causes you to be immunocompromised, it’s important to consult your doctor, said infectious disease expert Amesh A. Adalja, MD , senior scholar at the Johns Hopkins Center for Health Security.
“Immunocompromised individuals may have to have individualized vaccination schedules dependent upon their net state of immunosuppression,” Adalja told Verywell. He noted that the word ‘immunosuppression’ is used very generally, “but it is a phenomenon that has degrees.”
The CDC has COVID vaccine recommendations for immunocompromised people, but it’s very specific to age, type of vaccine, and current level of vaccination.
“The standing recommendation is that these individuals can get repeated doses if they are moderately or severely immunocompromised and at least two months have passed since their last dose,” Schaffner said.
How Doctors Can Increase Vaccination Rates
Doctors suggest coupling your COVID vaccine with your flu shot. The convenience of a combined appointment increases the odds people will get both vaccines.
“The annual rate of people getting the flu shot is about 50% of the population, but that’s better than it is for the COVID vaccine,” Timothy Murphy, MD, senior associate dean for clinical and translational research at the University at Buffalo Jacobs School of Medicine and Biomedical Sciences, told Verywell. “Pairing the COVID vaccine with the flu vaccine might increase the likelihood of people getting it.”
Schaffner agrees.
“We have to promote this as a circumstance where in the fall, you roll up both your sleeves,” he said. While it’s not available yet, a combination flu and COVID-19 vaccine would likely increase use of both vaccines even more. “It would also make life easier,” Schaffner said.
What This Means For You
COVID-19 vaccine can lower your risk of being hospitalized and dying from the virus, so you should make sure you have the latest shot available every year. If you’re unsure what your personal needs are regarding the vaccine, consult with your primary care physician for more information.
The information in this article is current as of the date listed, which means newer information may be available when you read this. For the most recent updates on COVID-19, visit our coronavirus news page .
Wells CR, Pandey A, Moghadas SM, Fitzpatrick MC, Singer BH, Galvani AP. Evaluation of strategies for transitioning to annual SARS-CoV-2 vaccination campaigns in the United States . Ann Intern Med . Published online March 26, 2024. doi:10.7326/M23-2451
Centers for Disease Control and Prevention. Interim clinical considerations for use of Covid-19 vaccines in the United States .
Centers for Disease Control and Prevention. COVIDVaxView: adult coverage and intent .
Centers for Disease Control and Prevention. COVIDVaxView: child coverage and parental intent for vaccination .
Centers for Disease Control and Prevention. Interim clinical considerations for use of COVID-19 vaccines in the United States .
By Korin Miller Korin Miller is a health and lifestyle journalist who has been published in The Washington Post, Prevention, SELF, Women's Health, The Bump, and Yahoo, among other outlets.
News & Media
- News Releases
- In The News
- Organization News
- Social Media
- Duke Health Blog
Public had Limited Understanding of Why a COVID-19 Vaccine was Paused
DURHAM, N.C. – Public health guidance about the pause in administering the Johnson & Johnson COVID-19 vaccine in April 2021 was difficult for many people to understand, according to a study led by a Duke Health researcher.
The findings of the study, appearing online April 1 in the Journal of Medical Internet Research, highlight the importance of clear public health guidance that builds trust within communities.
“The pause of the Johnson & Johnson vaccine was an uncertainty-inducing incident in an already uncertainty-ridden time,” said lead author Vishala Mishra, a fellow in the Department of Biostatistics and Bioinformatics at Duke University School of Medicine . “One of the best ways to improve future communication efforts is to study the successes and failures of past ones.”
Researchers conducted an online rapid response survey about the CDC’s messaging around the temporary halt of the vaccine, which occurred after it had received authorization for public use. The CDC and FDA recommended the pause due to six reports of cerebral venous sinus thrombosis (CVST) in recently vaccinated people. CVST occurs when a blood clot forms in the brain and can lead to swelling or a hemorrhage.
For this study, 557 unvaccinated adults were separated into two groups, with group A comprised of people who specifically expressed neutral or negative sentiments about COVID-19 vaccines and group B comprised of people who had no expressed opinion about COVID-19 vaccines.
Survey results show that many respondents greatly overestimated the number of CVST reports that prompted the pause. When asked to guess a specific number, nearly 70% of respondents in group A and nearly 47% of respondents in group B estimated 100 or more cases.
A majority of people also expressed reduced confidence in the safety of the Johnson & Johnson vaccine, but reported no change in their confidence of the safety of COVID-19 vaccines in general or intention to receive competing vaccines.
Researchers said verbal descriptors can be misinterpreted so it is important to use numbers to limit risk perception and promote informed decision making.
“We found significant negative associations between understanding of key information and vaccine hesitancy, suggesting that CDC crisis messaging may have been least accessible to people at the greatest risk of infection” Mishra said.
“However, it was not all doom and gloom,” she said. “Our survey found that overall vaccine hesitancy remained stable following the J&J pause and it did not affect the public’s hesitancy about other mRNA vaccines.”
To improve public health guidance, the researchers said it’s important to recognize that communication and verbal descriptors can be nuanced and misinterpreted. They also encourage academics and science communicators to be more transparent about the limits of human knowledge by using numbers to communicate uncertainty.
Additional authors include Joseph Dexter. The study received funding support from the Poynter Institute.
REVIEW article
The effect of covid-19 vaccine to the omicron variant in children and adolescents: a systematic review and meta-analysis.

- 1 Department of Outpatient, West China Hospital, Sichuan University, Chengdu, China
- 2 Department of Obstetrics and Gynecology, Peking University Third Hospital, Beijing, Beijing Municipality, China
- 3 National Clinical Research Center for Obstetrics and Gynecology, Peking University Third Hospital, Beijing, China
- 4 General Practice Ward/International Medical Center Ward, General Practice Medical Center, West China Hospital, Sichuan University, Chengdu, China
- 5 Department of Pediatrics, West China Second University Hospital, Sichuan University, Chengdu, Sichuan Province, China
- 6 Key Laboratory of Obstetric, Gynecologic and Pediatric Diseases and Birth Defects of Ministry of Education, West China Second University Hospital, Sichuan University, Chengdu, Sichuan Province, China
The final, formatted version of the article will be published soon.
Select one of your emails
You have multiple emails registered with Frontiers:
Notify me on publication
Please enter your email address:
If you already have an account, please login
You don't have a Frontiers account ? You can register here
Background: Omicron (B.1.1.529), a variant of SARS-CoV-2, has emerged as a dominant strain in COVID-19 pandemic. This development has raised concerns about the effectiveness of vaccination to Omicron, particularly in the context of children and adolescents. Our study evaluated the efficacy of different COVID-19 vaccination regimens in children and adolescents during the Omicron epidemic phase. Methods: We searched PubMed, Cochrane, Web of Science, and Embase electronic databases for studies published through March 2023 on the association between COVID-19 vaccination and vaccine effectiveness (VE) against SARS-CoV-2 infection in children and adolescents at the Omicron variant period. The effectiveness outcomes included mild COVID-19 and severe COVID-19. This study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines and was prospectively registered in PROSPERO (CRD42023390481). Results: A total of 33 studies involving 16,532,536 children were included in the analysis. First, in children and adolescents aged 0-19 years, the overall VE of the COVID-19 vaccine is 45% (95% confidence interval [CI]: 40% to 50%). Subgroup analysis of VE during Omicron epidemic phase for different dosage regimens demonstrated that the VE was 50% (95% CI: 44% to 55%) for the 2-dose vaccination and 61% (95% CI: 45% to 73%) for the booster vaccination. Upon further analysis of different effectiveness outcomes during the 2-dose vaccination showed that the VE was 41% (95% CI: 35% to 47%) against mild COVID-19 and 71% (95% CI: 60% to 79%) against severe COVID-19. In addition, VE exhibited a gradual decrease over time, with the significant decline in the efficacy of Omicron for infection before and after 90 days following the 2-dose vaccination, registering 54% (95% CI: 48% to 59%) and 34% (95% CI: 21% to 56%), respectively. Conclusions: During the Omicron variant epidemic, the vaccine provided protection against SARS-CoV-2 infection in children and adolescents aged 0-19 years. Two doses of vaccination can provide effective protection severe COVID-19, with booster vaccination additionally enhancing VE.
Keywords: SARS-COV-2 variants, omicron, COVID-19 vaccines, Child, Adolescent
Received: 14 Nov 2023; Accepted: 27 Mar 2024.
Copyright: © 2024 Lu, Zeng, Yao, Luo and Ruan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Tiechao Ruan, Department of Pediatrics, West China Second University Hospital, Sichuan University, Chengdu, 610041, Sichuan Province, China
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Do you need a spring COVID-19 vaccine? Research backs extra round for high-risk groups
Recent studies suggest staying up-to-date on covid shots helps protect high-risk groups from severe illness.
Social Sharing
New guidelines suggest certain high-risk groups could benefit from having another dose of a COVID-19 vaccine this spring — and more frequent shots in general — while the broader population could be entering once-a-year territory, much like an annual flu shot.
Medical experts told CBC News that falling behind on the latest shots can come with health risks, particularly for individuals who are older or immunocompromised.
"Even when the risk of infection starts to increase, the vaccines still do a really good job at decreasing risk of severe disease," said McMaster University researcher and immunologist Matthew Miller.
Who needs another COVID shot?
Back in January, Canada's national vaccine advisory body set the stage for another round of spring vaccinations. In a statement , the National Advisory Committee on Immunization (NACI) stated that starting in spring 2024, individuals at an increased risk of severe COVID may get an extra dose of the latest XBB.1.5-based vaccines, which better protect against circulating virus variants.

That means:
- Adults aged 65 and up.
- Adult residents of long-term care homes and other congregate living settings for seniors.
- Anyone six months of age or older who is moderately to severely immunocompromised.
The various spring recommendations don't focus on pregnancy, despite research showing clear links between a COVID infection while pregnant, and increased health risks. However, federal guidance does note that getting vaccinated during pregnancy can protect against serious outcomes.
"Vaccinated people can also pass antibodies to their baby through the placenta and through breastmilk," that guidance states .
What do the provinces now recommend?
Multiple provinces have started rolling out their own regional guidance based on those early recommendations — with a focus on allowing similar high-risk groups to get another round of vaccinations.
B.C. is set to announce guidance on spring COVID vaccines in early April, officials told CBC News, and those recommendations are expected to align with NACI's guidance.
In Manitoba , high-risk individuals are already eligible for another dose, provided it's been at least three months since their latest COVID vaccine.
- Older P.E.I. residents, others at risk, urged to get spring COVID vaccine booster
- High-risk groups can now book spring COVID-19 vaccination in Nova Scotia
Meanwhile Ontario's latest guidance , released on March 21, stresses that high-risk individuals may get an extra dose during a vaccine campaign set to run between April and June. Eligibility will involve waiting six months after someone's last dose or COVID infection.
Having a spring dose "is particularly important for individuals at increased risk of severe illness from COVID-19 who did not receive a dose during the Fall 2023 program," the guidance notes.
And in Nova Scotia , the spring campaign will run from March 25 to May 31, also allowing high-risk individuals to get another dose.
Specific eligibility criteria vary slightly from province-to-province, so Canadians should check with their primary care provider, pharmacist or local public health team for exact guidelines in each area.

Age still best determines when to get COVID vaccines, new research suggests
Why do the guidelines focus so much on age.
The rationale behind the latest spring guidelines, Miller said, is that someone's age remains one of the greatest risk factors associated with severe COVID outcomes, including hospitalization, intensive care admission and death.
"So that risk starts to shoot up at about 50, but really takes off in individuals over the age of 75," he noted.
Canadian data suggests the overwhelming majority of COVID deaths have been among older adults, with nearly 60 per cent of deaths among those aged 80 or older, and roughly 20 per cent among those aged 70 to 79.
People with compromised immune systems or serious medical conditions are also more vulnerable, Miller added.

Will people always need regular COVID shots?
While the general population may not require shots as frequently as higher-risk groups, Miller said it's unlikely there will be recommendations any time soon to have a COVID shot less than once a year, given ongoing uncertainty about COVID's trajectory.
"Going forward, I suspect for pragmatic reasons, [COVID vaccinations] will dovetail with seasonal flu vaccine campaigns, just because it makes the implementation much more straightforward," Miller said.
- Just 15% of Canadians got updated COVID vaccines this fall, new figures show
- Spring COVID-19 vaccines available April 2 in N.B. for those at high-risk
"And although we haven't seen really strong seasonal trends with SARS-CoV-2 now, I suspect we'll get to a place where it's more seasonal than it has been."
In the meantime, the guidance around COVID shots remains simple at its core: Whenever you're eligible to get another dose — whether that's once or twice a year — you might as well do it.
What does research say?
One analysis, published in early March in the medical journal Lancet Infectious Diseases , studied more than 27,000 U.S. patients who tested positive for SARS-CoV-2, the virus behind COVID, between September and December 2023.
The team found individuals who had an updated vaccine reduced their risk of severe illness by close to a third — and the difference was more noticeable in older and immunocompromised individuals.
Another American research team from Stanford University recently shared the results from a modelling simulation looking at the ideal frequency for COVID vaccines.
- Elderly Canadians remain at higher risk of serious COVID from first infections, study suggests
- Spring vaccine dose suggested to protect seniors in Canada from severe COVID
The study in Nature Communications suggests that for individuals aged 75 and up, having an annual COVID shot could reduce severe infections from an estimated 1,400 cases per 100,000 people to around 1,200 cases — while bumping to twice a year could cut those cases even further, down to 1,000.
For younger, healthier populations, however, the benefit of regular shots against severe illness was more modest.
The outcome wasn't a surprise to Stanford researcher Dr. Nathan Lo, an infectious diseases specialist, since old age has consistently been a risk factor for severe COVID.
"It's almost the same pattern that's been present the entire pandemic," he said. "And I think that's quite striking."
More frequent vaccination won't prevent all serious infections, he added, or perhaps even a majority of those infections, which highlights the need for ongoing mitigation efforts.
ABOUT THE AUTHOR
Senior Health & Medical Reporter
Lauren Pelley covers health and medical science for CBC News, including the global spread of infectious diseases, Canadian health policy, pandemic preparedness, and the crucial intersection between human health and climate change. Two-time RNAO Media Award winner for in-depth health reporting in 2020 and 2022. Contact her at: [email protected]
- @LaurenPelley
Add some “good” to your morning and evening.
A vital dose of the week's news in health and medicine, from CBC Health. Delivered to your inbox every Saturday morning.

IMAGES
COMMENTS
Community‐based studies in five countries show consistent strong benefits from early rollouts of COVID‐19 vaccines. By the beginning of June 2021, almost 11% of the world's population had received at least one dose of a coronavirus disease 2019 (COVID‐19) vaccine. 1 This represents an extraordinary scientific and logistic achievement ...
A two-dose regimen of BNT162b2 (30 μg per dose, given 21 days apart) was found to be safe and 95% effective against Covid-19. The vaccine met both primary efficacy end points, with more than a 99 ...
The protective effects of vaccination and prior infection against severe Covid-19 are reviewed, with proposed directions for future research, including mucosal immunity and intermittent vaccine boo...
The Coronavirus Efficacy (COVE) phase 3 trial was launched in late July 2020 to assess the safety and efficacy of the mRNA-1273 vaccine in preventing SARS-CoV-2 infection. An independent data and ...
There is no question that the current vaccines are effective and safe. The risk of severe reaction to a COVID-19 jab, say researchers, is outweighed by the protection it offers against the deadly ...
To date, coronavirus disease 2019 (COVID-19) becomes increasingly fierce due to the emergence of variants. Rapid herd immunity through vaccination is needed to block the mutation and prevent the emergence of variants that can completely escape the immune surveillance. We aimed to systematically evaluate the effectiveness and safety of COVID-19 vaccines in the real world and to establish a ...
The effectiveness of the mRNA vaccines in preventing COVID-19 disease progression in 2021 set new expectations about the role of prevention interventions for the disease. Efficacy observed in the trials was more than 90%.1,2 The efficacy of other vaccines evaluated in large randomised trials, such as the Oxford-AstraZeneca (70%) and Sputnik V (91%) vaccines, have been criticised for elements ...
Our analyses indicate that vaccine effectiveness generally decreases over time against SARS-CoV-2 infections, hospitalisations, and mortality. The baseline vaccine effectiveness levels for the omicron variant were notably lower than for other variants. Therefore, other preventive measures (eg, face-mask wearing and physical distancing) might be necessary to manage the pandemic in the long term.
With this in mind, the editors of NPJ Vaccines have selected 17 articles that exemplify the rapid progress made with COVID vaccine development in the last 2 years. Our first COVID paper described ...
The persisting risk of long-term health consequences of SARS-CoV-2 infection and the protection against such risk conferred by COVID-19 vaccination remains unclear. Here we conducted a ...
2020 has been a difficult year for all, but has seen 58 vaccines against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) be developed and in clinical trials,1 with some vaccines reportedly having more than 90% efficacy against COVID-19 in clinical trials. This remarkable achievement is much-needed good news as COVID-19 cases are currently at their highest daily levels globally.2 ...
Abstract. Severe disease due to COVID-19 has declined dramatically as a result of widespread vaccination and natural immunity in the population. With the emergence of SARS-CoV-2 variants that largely escape vaccine-elicited neutralizing antibody responses, the efficacy of the original vaccines has waned and has required vaccine updating and ...
Research; Working Papers; ... We study the effect of mandates requiring COVID-19 vaccination among healthcare industry workers adopted in 2021 in the United States. There are long-standing worker shortages in the U.S. healthcare industry, pre-dating the COVID-19 pandemic. The impact of COVID-19 vaccine mandates on shortages is ex ante ambiguous
Introduction. Since 2019, the global COVID-19 pandemic has affected the lives of billions of people worldwide ().To deal with this situation, countries worldwide began to develop vaccines, including traditional inactivated vaccines, recombinant protein, live-attenuated vaccines, RNA vaccines, etc. (2-15).On October 2nd, 2023, the Nobel Assembly at the Karolinska Institutet decided to award ...
Now, given the urgent need for COVID-19 vaccines, unprecedented financial investments and scientific collaborations are changing how vaccines are developed. This means that some of the steps in the research and development process have been happening in parallel, while still maintaining strict clinical and safety standards.
Participants were enrolled from December 28, 2020 (2 weeks after the introduction of a Covid-19 vaccine), through May 19, 2021, at 33 sites across 25 U.S. states, representing more than 500,000 ...
Objective To study the association between COVID-19 vaccination and the risk of post-COVID-19 cardiac and thromboembolic complications. Methods We conducted a staggered cohort study based on national vaccination campaigns using electronic health records from the UK, Spain and Estonia. Vaccine rollout was grouped into four stages with predefined enrolment periods. Each stage included all ...
Evaluation of Febrile Seizure Risk Following Ancestral Monovalent COVID-19 mRNA Vaccination Among U.S. Children Aged 2-5 Years Richard A, Forshee, PhD,1 Elizabeth R Smith, BS,2 Zhiruo Wan, MS2, Kandace L Amend, PhD, MPH,3 Alex Secora, PhD4, Djeneba Audrey Djibo, PhD, MSBME,5 Kamran Kazemi, BS,2 Jennifer Song, MA, MURP3, Lauren E Parlett, PhD6, John D Seeger, DrPH, PharmD3, Nandini
COVID-19 vaccine hesitancy is a major global issue 1, and it is important to develop research-based messaging about vaccination that is ... 19 vaccination status and intent. This paper, then, (2 ...
Furthermore, post-vaccine myocarditis tends to be transient with very good recovery and is less severe than that associated with COVID-19. Studies have found that extending the time between first and second doses of the COVID-19 mRNA vaccines beyond the initially recommended three-week interval decreases the risk of myocarditis. (CDC)
New research suggests that most people will benefit from an annual COVID-19 vaccine. Certain groups may need two vaccines a year. Doctors said more needs to be done to encourage people to get vaccinated. There have been a lot of changes in recommendations around COVID-19 vaccines over the past few years, making it difficult to know whether you ...
DURHAM, N.C. - Public health guidance about the pause in administering the Johnson & Johnson COVID-19 vaccine in April 2021 was difficult for many people to understand, according to a study led by a Duke Health researcher.. The findings of the study, appearing online April 1 in the Journal of Medical Internet Research, highlight the importance of clear public health guidance that builds ...
3 National Clinical Research Center for Obstetrics and Gynecology, Peking University Third Hospital, Beijing, China ... the overall VE of the COVID-19 vaccine is 45% (95% confidence interval [CI]: 40% to 50%). Subgroup analysis of VE during Omicron epidemic phase for different dosage regimens demonstrated that the VE was 50% (95% CI: 44% to 55% ...
Older P.E.I. residents, others at risk, urged to get spring COVID vaccine booster. High-risk groups can now book spring COVID-19 vaccination in Nova Scotia. Meanwhile Ontario's latest guidance ...